Abstract
Introduction:
Polysubstance use is common among individuals seeking treatment for substance use disorders (SUD). However, we know less about patterns and correlates of polysubstance use among treatment-seeking populations. The current study aimed to identify latent patterns of polysubstance use and associated risk factors in persons entering SUD treatment.
Methods:
Patients (N=28,526) being admitted for substance use treatment reported on their use of thirteen substances (e.g., alcohol, cannabis, cocaine, amphetamines, methamphetamines, other stimulants, heroin, other opioids, benzodiazepines, inhalants, synthetics, hallucinogens, and club drugs) in the month before treatment and prior to the month before treatment. Latent class analysis (LCA) determined the relationship between class membership and gender, age, employment status, unstable housing, self-harm, overdose, past treatment, depression, generalized anxiety disorder, and/or post-traumatic stress disorder (PTSD).
Results:
Identified classes included: 1) Alcohol primary, 2) Moderate probability of past-month alcohol, cannabis, and/or opioid use; 3) Alcohol primary, Lifetime cannabis and cocaine use; 4) Opioid primary, Lifetime use of alcohol, cannabis, hallucinogens, club drugs, amphetamines, and cocaine; 5) Moderate probability of past-month alcohol, cannabis, and/or opioid use, Lifetime use of various substances; 6) Alcohol and cannabis primary, Lifetime use of various substances; and 7) High past-month polysubstance use. Individuals who engaged in high past-month polysubstance use were at elevated risk of screening positive for recent unstable housing, unemployment, depression, anxiety, PTSD, self-harm, and overdose.
Conclusions:
Current polysubstance use is associated with significant clinical complexity. Tailored treatments that reduce harms resulting from polysubstance use and related psychiatric comorbidity may improve treatment outcomes in this population.
Keywords: Polysubstance use, Latent class analysis, Comorbidity, Self-harm, PTSD
1. Introduction
The field of substance use disorder (SUD) research often focuses on single classes of substances defined by their pharmacology; yet the real-world experience of persons with SUDs frequently includes present and/or past use of multiple substances. Individuals may engage in polysubstance use due to reinforcing effects of unique effect profiles associated with specific substance combinations, or to alleviate negative side effects associated with a given substance (Valente et al., 2020). Persons engaged in polysubstance use may present to treatment with significant clinical complexity, as co-use of substances can increase the risk of adverse drug effects, overdose, and/or co-occurring psychiatric disorders (Fernández-Calderón et al., 2020; Gudin et al., 2013; Lockwood et al., 2021). Individuals engaged in polysubstance use are also at a greater risk of poorer treatment outcomes, including continued substance use (Wang et al., 2017). Different substance combinations may require distinct treatment considerations. Thus, identifying common patterns of polysubstance use and associated sequelae may help inform how to best tailor treatments in real-world settings.
One way to differentiate between meaningful patterns of polysubstance use is through person-centered statistical approaches such as latent class analysis (LCA). LCA is a data-driven approach that facilitates identification of latent classes, or unobserved subgroups of individuals, based on response patterns within the data (Nylund-Gibson & Choi, 2018). Advantages of LCA include the ability to (1) detect homogenous patterns of responding across different individuals, and 2) empirically compare subgroups of individuals on clinically relevant characteristics, such as exposure to psychosocial stressors, co-occurring psychiatric disorders, and substance-related consequences.
A handful of studies have employed LCA to explore patterns of polysubstance use in subpopulations of individuals presenting in SUD treatment settings, including women (Rodriguez et al., 2021), individuals receiving medication treatment for opioid use disorder (Arnold et al., 2021; Betts et al., 2016), and individuals receiving treatment for injection amphetamine use (Kelly et al., 2017). Results have suggested that persons who engage in polysubstance use vary in terms of their 1) substance use characteristics, including severity (Connor et al., 2013), injection drug use (Betts et al., 2016; Bunting et al., 2020; Kelly et al., 2017), and sharing of needles (Kelly et al., 2017)); 2) psychiatric comorbidities (Bunting et al., 2020; Connor et al., 2013; Wu et al., 2011); 3) medical comorbidities (Betts et al., 2016; Schwartz et al., 2010; Wu et al., 2011); 4) psychosocial stressors (e.g., unstable housing) (Bunting et al., 2020); 5) criminal justice system involvement (Betts et al., 2016; Bunting et al., 2020; Kelly et al., 2017); and 6) mortality (Gjersing & Bretteville-Jensen, 2017).
However, there is limited published literature examining polysubstance use patterns among individuals who are diverse with regard to primary substance and who are entering SUD treatment, as prior LCA examinations have focused on subgroups of persons seeking treatment. Individuals engaged in polysubstance use are more likely to have co-occurring psychiatric disorders and may use multiple substances for self-management of symptoms (Ellis et al., 2022; Valente et al., 2020). Psychiatric comorbidity and psychosocial stressors (e.g., unstable housing, unemployment) are common among patients in SUD treatment, and important considerations for treatment and discharge planning (Tuten et al., 2003; Zhu et al., 2021). Thus, examining clinical comorbidity and psychosocial stress as predictors of latent class membership represents an appropriate initial step to better understand correlates of past and current polysubstance use among individuals in SUD treatment.
Some substances (e.g., hallucinogens, synthetics) have received only some empirical attention in previous examinations of polysubstance use patterns, despite the fact that they may be used concurrently with other substances that are more commonly used (e.g., alcohol; Barrett et al., 2006; Licht et al., 2012). Additionally, clinically relevant covariates such as self-harm and post-traumatic stress disorder (PTSD) symptoms have not been routinely examined as potential correlates of class membership, despite strong theoretical support for examining these constructs in relation to polysubstance use behaviors. For instance, self-harm behavior and polysubstance use share certain risk factors, including impulsivity (Casillas & Clark, 2002; Moody et al., 2016; Rawlings et al., 2015) and affective instability (Gee et al., 2020; Rawlings et al., 2015; Wojciechowski, 2021). Further, certain combinations of substances may increase overdose risk (Schneider et al., 2019; Tori et al., 2020), which is critical to consider given that as many as 51% of opioid overdoses may involve active or passive suicidal ideation (Gicquelais et al., 2020). PTSD is relatively common in persons with SUDs, and previous work suggests that a subset of individuals with severe polysubstance use experience PTSD and major depressive disorder (MDD) symptoms (Anderson et al., 2018) that may require an increased level of care or interventions designed to treat these co-occurring conditions. Taken together, these previous findings highlight the importance of examining PTSD and self-harm as they relate to polysubstance use patterns.
The goals of the present study were to 1) identify whether persons presenting to SUD treatment programs exhibit different patterns of polysubstance use, and 2) examine the clinical correlates uniquely associated with class membership. Consideration of a range of substances, as well as when the use occurred (i.e., in the past month vs. prior to the past month), may help identify a more complete picture of polysubstance use patterns among individuals presenting for SUD treatment and identify co-occurring clinical needs within these sub-populations.
2. Methods
2.1. Participants
The study drew participants from a large, dataset of unique individuals who presented for admission to SUD treatment facilities in the United States. Not all states were represented. Data were collected by a third-party treatment outcomes data collection system (Vista Research Group, Inc.) that partners with inpatient and outpatient SUD treatment providers to track mental health symptoms and substance use behaviors. The sample includes individuals seeking treatment for a range of different substances. The majority of patients in the analyzed sample were drawn from inpatient treatment centers (including both general residential/inpatient and intensive inpatient), and smaller numbers of patients were drawn from outpatient and intensive outpatient facilities. Patient self-report assessed all measures included in the current analysis. The dataset is not publicly available, and we procured it through a data use agreement with Vista Research Group, Inc. The data were de-identified prior to receipt by the study team. The study was submitted to and acknowledged by the Johns Hopkins School of Medicine Institutional Review Board.
Supplemental Figure 1 shows a flowchart summarizing eligibility for the current analyses. We used the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines for presentation of analyses. Participants completed surveys between 2016 and 2020. The analysis excluded participants if they 1) were not an adult presenting for primary SUD treatment (i.e., if they presented for behavioral health treatment), 2) had inconsistent responses on drug use items, or preferred a substance not identified within the substance use questions, or 3) had missingness on any of the latent class predictors. A total of 28,526 individuals (73.0% of full dataset) were identified as eligible for the current study.
2.2. Measures
2.2.1. Demographic information.
Participants reported their age (in years), gender (response options included male, female, or transgender), race (original response options included White non-Hispanic, African American, Hispanic or Latino, Asian, Native American, Other; individuals who responded Hispanic or Latino were recoded to Unknown race), marital status (response options included single/never married, married, separated, divorced, or widowed), and whether they were living in unstable housing (i.e., if they reported that they were homeless, moving from place to place and living with people they just met, in jail, or in another unstable housing situation).
2.2.2. Substance use.
The study asked individuals to identify their primary substance leading into treatment. Next, individuals reported on their use of any substances in the 30 days before treatment. These analyses assessed use of thirteen substances: 1) alcohol, 2) cannabis, 3) cocaine, 4) benzodiazepines, 5) heroin, 6) other opioids, 7) amphetamines, 8) methamphetamine, 9) other stimulants, 10) hallucinogens, 11) club drugs, 12) synthetics, and 13) inhalants. Each substance included a broad classification, followed by several examples (e.g., “Stimulants, such as Concerta, Daytrana, Methylin, Ritalin, Metadate, MPH, R-ball, Skippy”). Response options were 1) Never used, 2) Used in lifetime, but not in the past 30 days, 3) Used in the 30 days before treatment, but not heavily, and 4) Used heavily in the 30 days before treatment. For the present study, categories 3 and 4 were collapsed to capture recent (past 30-day) use.
2.2.3. Positive depression screen.
Individuals completed the following two pre-screening questions from the Patient Health Questionnaire (PHQ-9): 1) feeling down, depressed, or hopeless, 2) losing little interest or pleasure in doing things. Endorsement of either question prompted completion of the full PHQ-9 (Kroenke et al., 2001), a validated measure of depressive symptoms. Reliability for the PHQ-9 was good in the present sample (α = .89). Based on established cutoffs, individuals who screened positive for depression had scores of 10 or higher, indicating moderate, moderately-severe, or severe symptoms. Those who screened negative for depression were individuals who had no symptoms or mild symptoms (i.e., did not endorse the first two items or achieved a total score less than 10).
2.2.4. Positive anxiety screen.
Individuals completed two pre-screening questions related to anxiety symptoms. Prior to 10/7/2018, the pre-screening questions assessed 1) the experience of anxiety attacks and 2) feelings of anxiety, nervousness, being on edge, or worry. Following 10/7/2018, the pre-screening questions were revised to the following: 1) “Do you often feel anxious, nervous or on edge?" and 2) “Have you been unable to stop or control worrying?” Participants who endorsed either of the two pre-screening items completed the Generalized Anxiety Disorder-7 (GAD-7) screening measure for anxiety symptoms (Spitzer et al., 2006). The GAD-7 is a validated measure of anxiety symptoms. Reliability for this measure was excellent in this sample (α = .93). Individuals were identified as screening positive (i.e., moderate or severe symptoms, or a 10 or higher on the GAD-7) or screening negative for anxiety (i.e., a total score of 0-9 on the GAD-7 indicating minimal or mild symptoms, or not endorsing either screening question).
2.2.5. Positive PTSD screen.
Individuals completed the following two pre-screening questions related to exposure and distress resulting from a traumatic event: 1) “Did you often have repeated, disturbing memories, thoughts, or images of a stressful experience from the past?” and 2) “Did you often feel very upset when something reminded you of a stressful experience from the past?” Individuals who endorsed either item completed the Abbreviated Post-Traumatic Checklist (Civilian Version) (Lang & Stein, 2005), a validated measure of PTSD symptoms. Reliability was excellent in this sample (α = .93). We used a cut score of 14 to classify individuals who screened positive for clinically significant PTSD symptoms (Lang & Stein, 2005); individuals who had a score less than 14 or who screened negative on the screening items were coded as having screened negative.
2.2.6. Self-harm.
Participants responded “Yes” or “No” to a question asking whether they had harmed themselves on purpose, such as by cutting themselves during the month before they started treatment.
2.2.7. Overdose.
The survey asked participants to identify on a checklist which experiences they had right before coming to treatment that led them to enter treatment. Individuals who selected that they overdosed on this question were operationalized as having experienced overdose before treatment.
2.2.8. Previous treatment.
Participants responded “Yes” or “No” to the question “Have you been in other treatment programs before this one?”
2.3. Data analysis
The research team conducted analyses in SPSS Version 27 (IBM Corp., 2020) and Mplus Version 8.6 (Muthén & Muthén, 1998). Substance use variables were included as 3-level (i.e., never used, used prior to the past month, used in the past month) categorical substance use indicators in a latent class analysis (LCA). In total, we included thirteen substance use indicators in the LCA: alcohol, cannabis, amphetamines, methamphetamine, other stimulants, cocaine, heroin, other opioids, benzodiazepines, hallucinogens, club drugs, synthetics, and inhalants. Models were compared using standard fit indices, including Akaike's Information Criteria (AIC), Bayesian Information Criteria (BIC), sample size adjusted BIC (SSA-BIC), the size of the smallest class size (>5%), entropy, the Lo-Mendell-Rubin Adjusted Likelihood Ratio Test (LRT), and Vuong-Lo-Mendell-Rubin Likelihood Ratio Test (VLMR). A smaller AIC, BIC, and SSA-BIC was determined to be indicative of better model fit. Entropy values closer to 1 reflect greater class separation. A p-value of <.05 for the LRT and VLMR tests indicated that the k-class model showed significant improvements in fit over the k-1 class model. (Asparouhov & Muthén, 2012).
Following model selection, the study used the R3STEP procedure (Asparouhov & Muthén, 2014) to determine the impact of the following variables on class membership: 1) gender, 2) age (in years), 3) unstable living situation before treatment (yes vs. no), 4) employed full- or part-time before treatment (vs. unemployed), 5) positive depression screen at intake, 6) positive anxiety screen at intake, 7) positive PTSD screen at intake, 8) past month self-harm before treatment (yes vs. no), 9) recent overdose (yes vs. no), and 10) previous treatment (yes vs. no). The R3STEP approach treats variables as latent class predictors. This approach accounts for classification error when estimating class membership when regressing class membership on model predictors (Vermunt, 2010). Simulation studies suggest that the R3STEP approach is associated with reduced bias relative to other approaches, such as the pseudo-class method (Asparouhov & Muthén, 2014).
3. Results
3.1. Descriptive information
The study collected admissions data for N=39,063 individuals from SUD treatment facilities; a total of 10,537 individuals were excluded due to not meeting study criteria, leaving a final study sample of N=28,526 (Supplemental Figure 1). The sample was approximately 34.1% female; around 52.3% had never been married, 27.5% were currently married, and 20.2% were previously married (i.e., separated, widowed, or divorced). The sample included individuals who indicated that their racial background was white (79.9%), Black/African American (6.6%), Asian (0.9%), Native American (1.2%), and other/unknown (11.4%). A sizable number of participants (N = 4,470, 15.7%) reported that their housing status was unstable and nearly a third (N = 9,487, 34.7%) were not employed at treatment intake. Psychiatric comorbidity was common, with a sizable number screening positive for depression (N = 18,487, 64.8%), anxiety (N = 17,388, 61.0%), and PTSD (N = 16,176, 56.7%). Approximately 1,301 individuals (4.6%) reported self-harm in the month before treatment, and 1,967 individuals (6.9%) reported a recent overdose. A little over half of the sample had previously been in any treatment (N =17,013, 59.6%). Descriptive information of latent class predictors by most likely latent class membership is shown in Table 1.
Table 1.
Descriptive information by most likely latent class membership
| Class 1 - Alcohol primary |
Class 2 - Moderate probability of past-month alcohol, cannabis, and/or opioid use |
Class 3 - Alcohol primary, Lifetime cannabis and cocaine use |
Class 4 - Opioid primary, Lifetime use of alcohol, cannabis, hallucinogens, club drugs, amphetamines, and cocaine |
Class 5 - Moderate probability of past-month alcohol, cannabis, and/or opioid use, Lifetime use of various substances |
Class 6 - Alcohol and cannabis primary, Lifetime use of various substances |
Class 7 – High past-month polysubstance use |
|
|---|---|---|---|---|---|---|---|
| Age, M(SD) | 44.6 (12.2) | 36.1 (12.7) | 39.6 (12.8) | 31.5 (10.2) | 29.1 (8.5) | 33.0 (11.1) | 26.8 (7.5) |
| Female | 38.1% | 34.1% | 38.2% | 34.1% | 26.3% | 31.6% | 28.9% |
| Transgender | 0.1% | 0.1% | 0.2% | 0.1% | 0.3% | 0.3% | 0.3% |
| Unstable housing | 6.9% | 15.9% | 9.9% | 20.9% | 27.0% | 15.2% | 34.5% |
| Full or Part-time Employment | 72.9% | 64.1% | 69.1% | 62.1% | 59.7% | 66.3% | 54.4% |
| Positive Depression Screen | 53.0% | 63.0% | 63.5% | 70.3% | 69.6% | 74.4% | 81.5% |
| Positive Anxiety Screen | 48.9% | 59.4% | 60.0% | 64.8% | 66.0% | 71.8% | 77.6% |
| Positive PTSD Screen | 45.4% | 54.4% | 54.4% | 59.9% | 61.7% | 67.0% | 77.2% |
| Self-harm | 2.4% | 3.6% | 4.4% | 3.5% | 4.7% | 7.8% | 10.8% |
| Recent Overdose | 1.2% | 6.3% | 1.9% | 12.4% | 13.8% | 4.1% | 20.3% |
| Previous treatment | 51.2% | 54.2% | 53.4% | 69.0% | 78.6% | 56.2% | 73.7% |
PTSD= Post-traumatic Stress Disorder
3.2. LCA model selection
The study team selected a 7-class model based on several model fit indices. First, the SSA-BIC, AIC, and BIC decreased with each model up to 7 classes, but then showed only marginal improvement between the 7 and 8 class models. Second, although the 2, 3, and 4-class models showed the highest entropy values, entropy was acceptable (i.e., ~.8) for the 7-class model. Third, both the adjusted LRT and VLMRT suggested rejecting the 8-class model in favor of the 7-class model due to a lack of improvement in fit between the 7 and 8 class model. Fourth, the classes in the 7-class model were clinically meaningful (see descriptions below). Finally, the smallest class size of the 8-class model was <5%, indicating potential model overfitting. We present model fit indices in Supplemental Table 1. Table 2 shows probabilities of the substance use indicators based on class membership.
Table 2.
Probabilities of Substance Use in the Past Month and Prior to the Past Month based on Class Membership
| Class 1 - Alcohol primary (25.2%) |
Class 2 - Moderate probability of past-month alcohol, cannabis, and/or opioid use (14.5%) |
Class 3 - Alcohol primary, Lifetime cannabis and cocaine use (15.8%) |
Class 4 - Opioid primary, Lifetime use of alcohol, cannabis, hallucinogens, club drugs, amphetamines, and cocaine (12.3%) |
Class 5 - Moderate probability of past-month alcohol, cannabis, and/or opioid use, Lifetime use of various substances (12.6%) |
Class 6 - Alcohol and cannabis primary, Lifetime use of various substances (12.7%) |
Class 7 – High past-month polysubstance use (6.8%) |
|||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Used in Past Month | |||||||||||
| Alcohol | 0.96 | 0.50 | 0.88 | 0.40 | 0.55 | 0.89 | 0.80 | ||||
| Cannabis | 0.19 | 0.50 | 0.32 | 0.50 | 0.49 | 0.60 | 0.88 | ||||
| Amphetamines | 0.02 | 0.16 | 0.07 | 0.15 | 0.14 | 0.18 | 0.65 | ||||
| Methamphetamine | 0.01 | 0.18 | 0.06 | 0.26 | 0.32 | 0.14 | 0.63 | ||||
| Other Stimulants | 0.00 | 0.03 | 0.01 | 0.02 | 0.02 | 0.03 | 0.30 | ||||
| Cocaine | 0.08 | 0.33 | 0.13 | 0.33 | 0.37 | 0.27 | 0.78 | ||||
| Heroin | 0.00 | 0.29 | 0.00 | 0.63 | 0.53 | 0.00 | 0.64 | ||||
| Other Opioids | 0.02 | 0.47 | 0.09 | 0.59 | 0.40 | 0.12 | 0.78 | ||||
| Benzodiazepines | 0.09 | 0.38 | 0.19 | 0.48 | 0.37 | 0.30 | 0.86 | ||||
| Hallucinogens | 0.00 | 0.05 | 0.01 | 0.01 | 0.05 | 0.09 | 0.45 | ||||
| Club drugs | 0.00 | 0.06 | 0.00 | 0.03 | 0.05 | 0.08 | 0.53 | ||||
| Synthetics | 0.00 | 0.01 | 0.00 | 0.00 | 0.02 | 0.01 | 0.17 | ||||
| Inhalants | 0.00 | 0.01 | 0.00 | 0.00 | 0.02 | 0.02 | 0.20 | ||||
| Use Prior to Past Month | |||||||||||
| Alcohol | 0.04 | 0.27 | 0.12 | 0.58 | 0.44 | 0.11 | 0.18 | ||||
| Cannabis | 0.22 | 0.19 | 0.62 | 0.49 | 0.51 | 0.39 | 0.11 | ||||
| Amphetamines | 0.01 | 0.06 | 0.27 | 0.56 | 0.84 | 0.61 | 0.31 | ||||
| Methamphetamine | 0.00 | 0.03 | 0.14 | 0.32 | 0.61 | 0.34 | 0.20 | ||||
| Other Stimulants | 0.00 | 0.01 | 0.05 | 0.19 | 0.83 | 0.29 | 0.40 | ||||
| Cocaine | 0.02 | 0.10 | 0.54 | 0.60 | 0.63 | 0.68 | 0.20 | ||||
| Heroin | 0.00 | 0.03 | 0.04 | 0.18 | 0.43 | 0.18 | 0.18 | ||||
| Other Opioids | 0.03 | 0.09 | 0.33 | 0.38 | 0.60 | 0.68 | 0.20 | ||||
| Benzodiazepines | 0.04 | 0.08 | 0.28 | 0.43 | 0.63 | 0.54 | 0.12 | ||||
| Hallucinogens | 0.00 | 0.03 | 0.33 | 0.60 | 0.93 | 0.79 | 0.47 | ||||
| Club drugs | 0.00 | 0.03 | 0.24 | 0.57 | 0.94 | 0.72 | 0.43 | ||||
| Synthetics | 0.00 | 0.01 | 0.03 | 0.16 | 0.80 | 0.22 | 0.41 | ||||
| Inhalants | 0.00 | 0.01 | 0.02 | 0.09 | 0.73 | 0.23 | 0.37 | ||||
| Never Used | |||||||||||
| Alcohol | 0.00 | 0.24 | 0.00 | 0.03 | 0.01 | 0.01 | 0.02 | ||||
| Cannabis | 0.59 | 0.32 | 0.06 | 0.02 | 0.01 | 0.01 | 0.01 | ||||
| Amphetamines | 0.98 | 0.78 | 0.66 | 0.29 | 0.02 | 0.21 | 0.04 | ||||
| Methamphetamine | 0.99 | 0.80 | 0.80 | 0.43 | 0.08 | 0.52 | 0.17 | ||||
| Other Stimulants | 1.00 | 0.96 | 0.94 | 0.78 | 0.15 | 0.69 | 0.31 | ||||
| Cocaine | 0.90 | 0.58 | 0.34 | 0.06 | 0.00 | 0.06 | 0.02 | ||||
| Heroin | 1.00 | 0.69 | 0.96 | 0.19 | 0.05 | 0.82 | 0.18 | ||||
| Other Opioids | 0.95 | 0.44 | 0.58 | 0.03 | 0.00 | 0.20 | 0.03 | ||||
| Benzodiazepines | 0.87 | 0.54 | 0.54 | 0.10 | 0.00 | 0.16 | 0.02 | ||||
| Hallucinogens | 1.00 | 0.93 | 0.67 | 0.39 | 0.02 | 0.13 | 0.08 | ||||
| Club drugs | 1.00 | 0.91 | 0.76 | 0.40 | 0.02 | 0.20 | 0.05 | ||||
| Synthetics | 1.00 | 0.98 | 0.97 | 0.84 | 0.19 | 0.77 | 0.42 | ||||
| Inhalants | 1.00 | 0.98 | 0.97 | 0.91 | 0.25 | 0.75 | 0.44 | ||||
| >.9 | Very high probability | .5-.69 | Moderately high probability | .1-.29 | Low probability | ||||||
| .7-.89 | High probability | .3-.49 | Moderately low probability | <.1 | Very low probability | ||||||
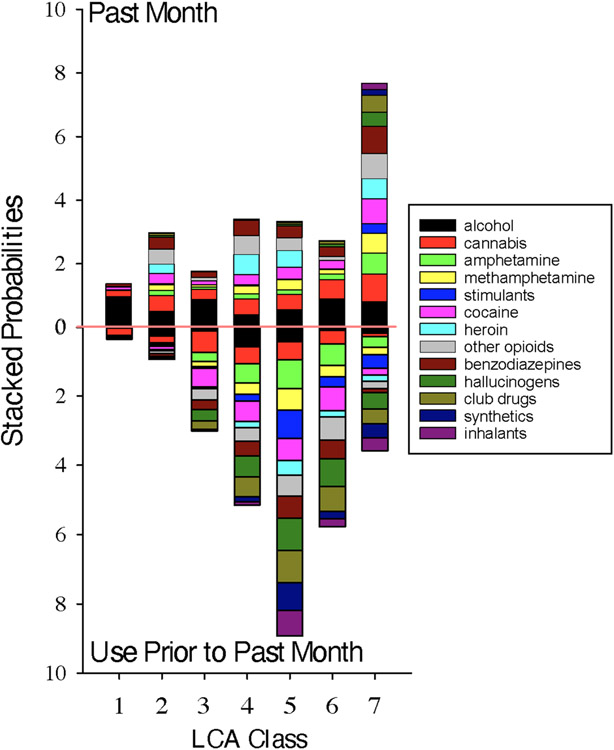
The final model resulted in classes that were characterized by low (classes 1 and 2), moderate (classes 3 and 4), or high (classes 5 -7) lifetime use, and presented to treatment with different types of current use. An overview of the classes is depicted in Figure 1, and more detailed description of each class can be found below.
Figure 1. Stacked probabilities of substance use in each latent class.
In each class, there is a probability (between 0 and 1) of endorsing use of each substance (shown in Table 2). Probabilities of use in the past month are stacked in the upper portion of the figure. Probabilities of use prior to the past month are stacked in the lower portion of the figure. Class 1 = Alcohol primary; Class 2 = Moderate Probability of past-month alcohol, cannabis, and/or opioid use; Class 3 = Alcohol primary, Lifetime cannabis and cocaine use; Class 4= Opioid primary, Lifetime use of alcohol, cannabis, hallucinogens, club drugs, amphetamines, and cocaine, Class 5 = Moderate probability of past-month alcohol, cannabis, and/or opioid use, Lifetime use of various substances; Class 6 = Alcohol and cannabis primary, Lifetime use of various substances; Class 7 = High past-month polysubstance use.
3.3. Description of solution
3.3.1. Classes characterized by low lifetime use
As Table 2 shows, individuals in class 1 (Alcohol primary) had a 96% probability of past month alcohol use, and a low probability of past month use or use prior to the past month of other substances. Probabilities of reporting never having used each substance ranged from 59% (cannabis) to >99% (stimulants, heroin, hallucinogens, club drugs, synthetics, and inhalants). Class 1 composed 25.2% of the sample.
Individuals in class 2 (Moderate probability of past-month alcohol, cannabis, and/or opioid use) had a 50% probability of endorsing alcohol use in the past month and a 50% probability of endorsing cannabis use in the past month. Opioid use was also common in this class with approximately 56% of individuals having used opioids other than heroin in their lifetime (47% probability in the past month, and 9% probability prior to the past month). However, individuals in this class had a low probability of reporting use of other substances prior to the past month (probabilities ≤ 10%). Class 2 composed 14.5% of the sample.
3.3.2. Classes characterized by moderate lifetime use
Individuals in class 3 (Alcohol primary, Lifetime cannabis and cocaine use) had an 88% probability of reporting alcohol use in the past month, and a low probability (<1%- 32%) of use of other substances in the past month. Use of most substances prior to the past month was also low; however, individuals in class 3 had a 94% probability of reporting lifetime cannabis use (32% probability in the past month, 62% probability prior to the past month), and a 67% probability of reporting lifetime cocaine use (13% probability in past month and 54% probability of reporting use prior to the past month). Class 3 composed 15.8% of the sample.
Individuals in class 4 (Opioid primary, Lifetime use of alcohol, cannabis, hallucinogens, club drugs, amphetamines, and cocaine) had a moderate-to-high probability of reporting past month opioid and/or heroin use (probabilities = 63% and 59%, respectively). Individuals in this class also had a 50% probability of reporting past month cannabis use and a 48% probability of reporting past month benzodiazepine use. Individuals in this class had a 93% probability of reporting lifetime cocaine use (33% probability in the past month and 60% probability prior to the past month), a 71% probability of reporting lifetime amphetamine use (15% probability in the past month, 56% probability prior to the past month), a 61% probability of reporting lifetime hallucinogen use (1% probability within the past month, 60% probability prior to the past month), and a 60% probability of reporting lifetime club drug use (3% probability in the past month and 57% probability prior to the past month). Use of stimulants, synthetics, and inhalants were not common in class 4 (probabilities of having never used these substances were 78%, 84% and 91%, respectively). Class 4 composed 12.3% of the sample.
3.3.3. Classes characterized by high lifetime use
Individuals in class 5 (Moderate probability of past-month alcohol, cannabis, and/or opioid use, Lifetime use of various substances) had a 55% probability of endorsing past month alcohol use, a 49% probability of endorsing past month cannabis use, a 53% probability of endorsing past month heroin use, and a 40% of endorsing past month other opioid use,. However, unlike the other classes, individuals in class 5 were characterized by a high probability of using of a number of substances prior to the past month, including club drugs (94%), hallucinogens (93%), amphetamines (84%), other stimulants (83%), synthetics (80%), inhalants (73%), cocaine (63%), benzodiazepines (63%), and methamphetamine (61%). Class 5 composed 12.6% of the sample.
Class 6 (Alcohol and cannabis primary, Lifetime use of various substances) was characterized by 1) a high probability of alcohol (89%) and cannabis (60%) use in the past month, but low probability of other substance use in the past month (probabilities <1 % - 30%), and 2) moderate or high probability of prior to past month use of hallucinogens (79%), club drugs (72%), other opioids (68%), cocaine (68%), amphetamines (61%), and benzodiazepines (54%). Class 6 composed 12.6% of the sample.
Individuals in class 7 (High past-month polysubstance use) had a high probability of reporting past month use of a number of substances. Individuals had an 88% probability of reporting past month cannabis use, 86% probability of past month benzodiazepine use, 80% probability of reporting past month alcohol use, 78% probability of past month cocaine use, 78% probability of past month opioid use, 65% probability of past month amphetamine use, 64% probability of past month heroin use, 63% probability of past month methamphetamine use, and a 53% probability of past month club drug use. Class 7 composed 6.8% of the sample.
3.4. Clinical covariates of class membership
Table 3 presents correlates of class membership 3. First, we present findings related to differences in predictors of class membership when the reference group is Class 1 (Alcohol primary). Relative to individuals in Class 1 (Alcohol primary), membership in all other latent classes were predicted by younger age, lower odds of being employed, having previously been in treatment, screening positive for depression, and screening positive for anxiety. Class 3 (Alcohol primary, Lifetime cannabis and cocaine use) did not differ from Class 1 regarding gender, likelihood of unstable housing status, or recent overdose; however, all other latent classes were associated with lower odds of female gender and higher odds of unstable housing status and recent overdose relative to Class 1. Membership in Classes 6 (Alcohol and cannabis primary, Lifetime use of various substances) and 7 (High past-month polysubstance use) was associated with higher odds of screening positive for PTSD and reporting self-harm in the month before treatment relative to Class 1 (Alcohol primary). Unexpectedly, odds of recent self-harm were lower in Class 4 (Opioid primary, Lifetime use of alcohol, cannabis, hallucinogens, club drugs, amphetamines, and cocaine) and Class 5 (Moderate probability of past-month alcohol, cannabis, and/or opioid use, Lifetime use of various substances) relative to Class 1. Individuals in Class 4 were less likely to be transgender than individuals in Class 1.
Table 3.
Correlates of Class Membership
| Comparisons Between Alcohol primary and All other Classes | ||||||
|---|---|---|---|---|---|---|
| Class 2 vs. Class 1 (Ref) |
Class 3 vs. Class 1 (Ref) |
Class 4 vs. Class 1 (Ref) |
Class 5 vs. Class 1 (Ref) |
Class 6 vs. Class 1 (Ref) |
Class 7 vs. Class 1 (Ref) |
|
| Age | 0.94 (0.93, 0.94)* | 0.97 (0.97, 0.97)* | 0.90 (0.90, 0.91)* | 0.88 (0.87, 0.88)* | 0.92 (0.91, 0.92)* | 0.84 (0.83, 0.85)* |
| Female | 0.69 (0.62, 0.77)* | 0.92 (0.84, 1.02) | 0.71 (0.64, 0.80)* | 0.45 (0.40, 0.50)* | 0.54 (0.48, 0.61)* | 0.41 (0.35, 0.47)* |
| Transgender | 0.16 (0.01, 1.75) | 1.12 (0.32, 3.93) | 0.21 (0.04, 0.99)* | 0.34 (0.10, 1.18) | 0.65 (0.21, 2.03) | 0.29 (0.08, 1.03) |
| Unstable housing | 2.10 (1.77, 2.48)* | 1.19 (0.99, 1.43) | 2.42 (2.05, 2.86)* | 3.16 (2.71, 3.69)* | 1.65 (1.39, 1.97)* | 4.11 (3.44, 4.91)* |
| Full or part-time employment | 0.55 (0.49, 0.62)* | 0.77 (0.69, 0.86)* | 0.60 (0.53, 0.68)* | 0.58 (0.52, 0.66)* | 0.65 (0.58, 0.73)* | 0.56 (0.48, 0.65)* |
| Positive Depression Screen | 1.43 (1.25, 1.62)* | 1.35 (1.19, 1.52)* | 1.97 (1.71, 2.26)* | 1.78 (1.56, 2.04)* | 1.91 (1.66, 2.21)* | 2.57 (2.09, 3.16)* |
| Positive Anxiety Screen | 1.20 (1.05, 1.38)* | 1.26 (1.11, 1.43)* | 1.19 (1.03, 1.37)* | 1.30 (1.14, 1.50)* | 1.67 (1.44, 1.93)* | 1.57 (1.28, 1.91)* |
| Positive PTSD Screen | 0.95 (0.83, 1.07) | 0.99 (0.88, 1.11) | 0.90 (0.79, 1.03) | 0.97 (0.85, 1.10) | 1.35 (1.18, 1.55)* | 1.73 (1.43, 2.08)* |
| Self-harm | 0.86 (0.64, 1.17) | 1.29 (0.97, 1.70) | 0.49 (0.34, 0.70)* | 0.74 (0.55, 1.00)* | 1.84 (1.44, 2.35)* | 1.53 (1.14, 2.05)* |
| Recent Overdose | 6.33 (4.26, 9.40)* | 1.15 (0.66, 2.01) | 11.21 (7.73, 16.26)* | 10.68 (7.38, 15.46)* | 2.22 (1.42, 3.45)* | 15.18 (10.34, 22.29)* |
| Previous treatment | 1.24 (1.12, 1.38)* | 1.15 (1.05, 1.27)* | 2.67 (2.38, 3.00)* | 4.77 (4.23, 5.38)* | 1.31 (1.18, 1.46)* | 3.46 (2.97, 4.04)* |
| Comparisons Between High past-month polysubstance use and All other Classes | ||||||
| Class 2 vs. Class 7 (Ref.) |
Class 3 vs. Class 7 (Ref.) |
Class 4 vs. Class 7 (Ref.) |
Class 5 vs. Class 7 (Ref.) |
Class 6 vs. Class 7 (Ref.) |
||
| Age | 1.11 (1.10, 1.12)* | 1.15 (1.14, 1.16)* | 1.07 (1.06, 1.08)* | 1.04 (1.03, 1.05)* | 1.09 (1.08, 1.10)* | |
| Female | 1.70 (1.45, 1.99)* | 2.28 (1.94, 2.68)* | 1.76 (1.49, 2.06)* | 1.10 (0.93, 1.29) | 1.34 (1.13, 1.58)* | |
| Transgender | 0.53 (0.06, 4.77) | 3.81 (1.11, 13.09)* | 0.71 (0.15, 3.45) | 1.15 (0.34, 3.86) | 2.22 (0.72, 6.90) | |
| Unstable housing | 0.51 (0.43, 0.60)* | 0.29 (0.24, 0.35)* | 0.59 (0.50, 0.70)* | 0.77 (0.66, 0.90)* | 0.40 (0.34, 0.48)* | |
| Full or part-time employment | 0.99 (0.85, 1.15) | 1.37 (1.17, 1.60)* | 1.07 (0.91, 1.25) | 1.04 (0.90, 1.21) | 1.16 (0.99, 1.36) | |
| Positive Depression Screen | 0.55 (0.45, 0.68)* | 0.52 (0.42, 0.65)* | 0.76 (0.61, 0.95)* | 0.69 (0.56, 0.86)* | 0.74 (0.59, 0.93)* | |
| Positive Anxiety Screen | 0.77 (0.63, 0.94)* | 0.81 (0.66, 1.00)* | 0.76 (0.61, 0.94)* | 0.83 (0.68, 1.02) | 1.07 (0.86, 1.33) | |
| Positive PTSD Screen | 0.55 (0.45, 0.66)* | 0.58 (0.47, 0.70)* | 0.52 (0.43, 0.64)* | 0.56 (0.46, 0.68)* | 0.78 (0.64, 0.96)* | |
| Self-harm | 0.56 (0.42, 0.75)* | 0.84 (0.62, 1.13) | 0.32 (0.23, 0.46)* | 0.49 (0.37, 0.64)* | 1.20 (0.93, 1.55) | |
| Recent Overdose | 0.42 (0.34, 0.51)* | 0.08 (0.05, 0.12)* | 0.74 (0.61, 0.89)* | 0.70 (0.59, 0.84)* | 0.15 (0.11, 0.20)* | |
| Previous treatment | 0.36 (0.31, 0.42)* | 0.33 (0.28, 0.39)* | 0.77 (0.65, 0.91)* | 1.38 (1.16, 1.63)* | 0.38 (0.32, 0.44)* | |
Class 1 = Alcohol primary; Class 2 = Moderate probability of past-month alcohol, cannabis, and/or opioid use; Class 3 = Alcohol primary, Lifetime cannabis and cocaine use; Class 4= Opioid primary, Lifetime use of alcohol, cannabis, hallucinogens, club drugs, amphetamines, and cocaine, Class 5 = Moderate probability of past-month alcohol, cannabis, and/or opioid use, Lifetime use of various substances; Class 6 = Alcohol and cannabis primary, Lifetime use of various substances; Class 7 = High past-month polysubstance use. PTSD= Post-traumatic Stress Disorder.
Denotes that the confidence interval does not contain 1.
Next, we present findings related to differences in predictors of class membership when the reference group is Class 7 (High past-month polysubstance use). Relative to Class 7 (High past-month polysubstance use), membership in all other classes was associated with older age, lower odds of unstable housing, lower odds of screening positive for depression, lower odds of screening positive for PTSD, and lower odds of reporting recent overdose. Individuals in all other classes except Class 5 (Moderate probability of past-month alcohol, cannabis, and/or opioid use, Lifetime use of various substances) were more likely to be female and less likely to have previously been in treatment than individuals in Class 7. Individuals in Class 5 were more likely to have previously been in treatment than individuals in Class 7. Individuals in Class 3 (Alcohol primary, Lifetime cannabis and cocaine use) were more likely to be employed and more likely to be transgender than individuals in Class 7. Membership in most latent classes was associated with lower odds of screening positive for anxiety relative to Class 7, with the exceptions of Classes 5 (Moderate probability of past-month alcohol, cannabis, and/or opioid use, Lifetime use of various substances) and 6 (Alcohol and cannabis primary, Lifetime use of various substances). Finally, membership in most latent classes was predicted by lower odds of self-harm relative to Class 7, with the exceptions of Classes 3 (Alcohol primary, Lifetime cannabis and cocaine use) and 6 (Alcohol and cannabis primary, Lifetime use of various substances).
4. Discussion
This study used a large, national database of persons entering SUD treatment to identify latent classes of lifetime and past-month substance use. We identified seven distinct patterns of polysubstance use, which were clinically meaningful and associated with unique patterns of risk for mental health symptoms, self-harm, and recent overdose. Persons presenting to treatment with polysubstance use had greater clinical complexity relative to individuals seeking treatment for primary alcohol use without a history of other substance use. Indeed, individuals reporting past month use of multiple substances had higher odds of presenting to treatment with significant stressors (unemployment, unstable housing status, recent overdose), and psychiatric comorbidity (i.e., screening positive for depression, generalized anxiety, PTSD, and/or self-harm behaviors) when compared to other latent classes characterized by lower degrees of recent polysubstance use.
The findings referenced above have utility for determining, at treatment intake, the unique needs of persons based upon their reports of substance use. For instance, Class 6 (Alcohol and cannabis primary, Lifetime use of various substances) and Class 7 (High past-month polysubstance use) were each characterized by high odds of using more than one substance in the month before treatment and were associated with increased risk of screening positive for clinically significant PTSD relative to individuals using alcohol only. A number of validated behavioral treatments exist for co-occurring PTSD and substance use disorder, including Seeking Safety (Najavits, 2002), Concurrent Treatment of PTSD and Substance Use Disorders Using Prolonged Exposure (COPE) (Back et al., 2014), and integrated cognitive behavioral therapy for co-occurring substance use and PTSD (ICBT) (McGovern et al., 2015). Since these treatments require extensive staff training and time allocation to implement, being able to quickly identify persons who are in greater need of these services can help to expedite their care planning and resource allocation.
Moreover, previous evidence suggests that the type of PTSD treatment be tailored based on substance use patterns. One of the few studies on the moderating role of polysubstance use in COPE treatment found that individuals in treatment for more than one substance showed smaller decreases in PTSD symptoms (albeit larger decreases in substance use severity) over the course of treatment relative to individuals in treatment for a single SUD (Jeffirs et al., 2019). A separate study reported that PTSD criterion D (negative alterations in cognition and mood) and criterion E (alterations in arousal and reactivity) were elevated among individuals with PTSD who were co-using alcohol and cannabis relative to individuals with PTSD reporting past month alcohol use only, whereas criterion B (intrusion symptoms) and criterion C (avoidance symptoms) did not differ between the two groups (Kearns et al., 2019). Although further research is needed, it may be beneficial to explore whether increased attention on negative mood and hyperarousal early in treatment among individuals presenting with PTSD and polysubstance use is associated with better treatment outcomes.
This study also expands our understanding of clinical correlates of polysubstance use by examining risk of self-harm, which provides another metric for clinical consideration, and advances the theoretical link between substance use and self-harm behaviors. Increased self-harm in the month before treatment was associated with Class 6 (Alcohol and cannabis primary, Lifetime use of various substances) and Class 7 (High past-month polysubstance use), relative to Class 1 (Alcohol primary). The high rates of PTSD and self-harm behaviors among classes characterized by a high likelihood of polysubstance use in the past month are noteworthy. Research has identified dissociative symptoms and emotion dysregulation as potential mechanisms linking PTSD to self-harm behaviors, both of which may also be a motive for and/or consequence of polysubstance use (Ford & Gómez, 2014; Rossi et al., 2019). Psychological treatments such as dialectical behavior therapy (DBT) target shared risk factors for self-harm and polysubstance use, such as emotion dysregulation, and research has shown them to be effective in reducing substance use behaviors (Axelrod et al., 2011), as well as self-harm (Westad et al., 2021). However, DBT has not been specifically tested for concurrent polysubstance use and self-harm, an avenue that may be beneficial for future work. Further, dissociation should be considered in investigations exploring motives for polysubstance use in future work, particularly among individuals with co-occurring PTSD.
In addition, unique risks were identified as a function of specific substance use patterns. For instance, classes characterized by a moderate to high probability of opioid use (i.e., Class 2: Moderate probability of past-month alcohol, cannabis, and/or opioid use; Class 5: Moderate probability of past-month alcohol, cannabis, and/or opioid use, Lifetime use of various substances; and Class 4 Opioid primary, Lifetime use of alcohol, cannabis, hallucinogens, club drugs, amphetamines, and cocaine) reported a substantially higher risk of recent overdose relative to individuals in Class 1 (Alcohol primary). However, all latent classes had a lower likelihood of overdose than Class 7 (High past-month polysubstance use). These findings are not surprising, as drug-drug interactions can substantially increase risk for adverse reactions or overdose (Fernández-Calderón et al., 2020; Gudin et al., 2013; Lockwood et al., 2021). These results underscore the importance of naloxone provision among individuals using opioids (Bergeria et al., 2019; Huhn et al., 2018), particularly if these individuals are also using other substances. Psychoeducation about risks associated with mixing substances in treatment settings may be beneficial; however, because membership in the high past month polysubstance group was predicted by younger age, psychoeducation about mixing substances in high school and university settings may be a particularly useful prevention measure.
Finally, these data may also help to inform reasons for co-use patterns. For instance, individuals with a high probability of past month polysubstance use were the most likely to report unstable housing status than individuals in all other classes. It is possible that these individuals may have a harder time avoiding drugs or leaving a situation where substances are present. Moreover, the higher frequency of overdose among individuals engaged in polysubstance use, especially those whose tolerance has decreased due to recent abstinence (Ravndal & Amundsen, 2010), suggests that procuring stable housing options for these patients may substantially reduce risk of negative outcomes. Increasing access to supportive housing services, transitional housing, and extended care facilities may increase the number of viable options for individuals who enter treatment in unstable housing (Mericle et al., 2019; Padwa et al., 2016). In this way, these data provide a testable and actionable strategy for determining meaningful interventions and resource allocation for these individuals.
4.1. Limitations
The results of the current study should be considered in the context of certain limitations. First, although this study included a relatively large number of substance indicators, important clinical information was unavailable. For example, the study did not collect fine-grained information regarding quantity, frequency, or severity of substance use. We also cannot distinguish between concurrent and simultaneous use of substances (i.e., we cannot differentiate which individuals in class 7 were using substances at the same time vs. within the same one-month period, but not necessarily on the same occasion). This question should be considered in future studies, as simultaneous use may pose a higher risk for accident or overdose. Further, nicotine and tobacco use is commonly used as an indicator in latent class analysis. We were unable to include nicotine and tobacco use as an indicator in this study due to the lack of information on use prior to the past month; however, nicotine and tobacco use should be considered in future studies. The study did not collect more detailed information about self-harm engagement (i.e., method of self-harm). Although the current study suggests a relationship between self-harm and polysubstance use, a thorough investigation should attempt to disentangle these relationships. Future work in SUD treatment settings should examine additional latent class predictors (e.g., medical comorbidity, criminal justice system involvement) that have been associated with polysubstance use in other populations.
Finally, the results may not be generalizable to all individuals seeking substance use treatment. First, the sample was not prospectively designed to be representative and is drawn from treatment centers that are using the Vista Research Group, Inc platform to monitor patient symptoms during treatment, and contained a large number of private facilities. Although the participants in the sample are comparable to other data sources (e.g., TEDS) with regard to gender, marital status, and unstable housing status; the current sample contained a relatively large number of individuals who are employed and who described their race as white; similar analyses use samples with greater diversity. Second, many individuals in need of SUD treatment do not access treatment and results pertain only to those entering treatment. Of note, individuals who have historically been marginalized in the United States (e.g., minoritized racial and ethnic groups) often face significant barriers to substance use treatment (Priester et al., 2016). Results should thus be replicated among samples with greater racial and gender diversity given the sample was predominately white and included only a small number of transgender participants.
5. Conclusion
The current study suggests that individuals presenting to SUD treatment can be classified into clinically meaningful subgroups of polysubstance use patterns. Individuals with greater polysubstance use had greater clinical complexity across a number of domains, including psychosocial stress and psychiatric symptoms. Interventions that reduce the likelihood of overdose, such as naloxone provision, may be beneficial among individuals using opioids or among individuals using multiple substances. Integrative psychosocial treatments that target shared risk factors for depressive symptoms, PTSD, and self-harm may be beneficial for certain individuals who present to treatment with these conditions in addition to recent polysubstance use.
Supplementary Material
Highlights.
Individuals presenting to substance use treatment often report use of more than one substance
Latent class analysis was used to examine polysubstance use patterns
A seven-class solution was selected.
Classes characterized by greater polysubstance presented with greater clinical complexity
Acknowledgment:
The authors acknowledge that the reported results are, in whole or in part, based on analyses of addiction treatment outcomes research collected by Vista Research Group, Inc. This manuscript may not represent the opinions of Vista Research Group, Inc., nor is Vista Research Group, Inc. responsible for its contents.
Role of funding source:
This study was supported by the National Institute on Drug Abuse T32 DA007209 (Bigelow/Strain/Weerts) and U01HL150835 (Huhn).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declaration of Interest: KED has consulted with Mind Med, Inc., Canopy Corporation, and DemeRx in the past 3 years. The other authors report no conflicts of interest.
CRediT Author Statement: JDE (conceptualization, data curation, formal analysis, methodology, writing – original draft), JAR (conceptualization, methodology, writing – review & editing), ODW (conceptualization, writing – review & editing), JW (conceptualization, writing – review & editing), KD (writing – review & editing, visualization), AH (conceptualization, resources, supervision, writing – review & editing)
References
- Anderson R, Hruska B, Boros A, Richardson C, & Delahanty D (2018). Patterns of co-occurring addictions, posttraumatic stress disorder, and major depressive disorder in detoxification treatment seekers: Implications for improving detoxification treatment outcomes. Journal of Substance Abuse Treatment, 86, 45–51. [DOI] [PubMed] [Google Scholar]
- Arnold T, Lin L, Cotton B, Bryson W, & Polenick C (2021). Gender Differences in Patterns and Correlates of Continued Substance Use among Patients in Methadone Maintenance Treatment. Substance Use and Misuse, 56(4), 529–538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asparouhov T, & Muthén B (2012). Using Mplus TECH11 and TECH14 to test the number of latent classes. Mplus Web Notes, 14(22), 1–17. [Google Scholar]
- Asparouhov T, & Muthén B (2014). Auxiliary variables in mixture modeling: Three-step approaches using Mplus. Structural Equation Modeling: A Multidisciplinary Journal, 21(3), 329–341. [Google Scholar]
- Axelrod S, Perepletchikova F, Holtzman K, & Sinha R (2011). Emotion regulation and substance use frequency in women with substance dependence and borderline personality disorder receiving dialectical behavior therapy. American Journal of Drug and Alcohol Abuse, 37(1), 37–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Back S, Foa E, Killeen T, & Mills K (2014). Concurrent treatment of PTSD and substance use disorders using prolonged exposure (COPE): Therapist guide. Treatments that Work. [Google Scholar]
- Barrett S, Darredea C, & Pihl R (2006). Patterns of simultaneous polysubstance use in drug using university students. Human Psychopharmacology: Clinical & Experimental, 21(4), 255–263. [DOI] [PubMed] [Google Scholar]
- Bergeria C, Huhn A, & Dunn K (2019). Randomized comparison of two web-based interventions on immediate and 30-day opioid overdose knowledge in three unique risk groups. Preventative Medicine, 128, 105718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betts K, Chan G, McIlwraith F, Dietze P, Wittaker E, Burns L, & Adam R (2016). Differences in polysubstance use patterns and drug-related outcomes between people who inject drugs receiving and not receiving opioid substitution therapies. Addiction, 111, 1214–1223. [DOI] [PubMed] [Google Scholar]
- Bunting C, Staton M, & Knudsen H (2020). Polysubstance Use Patterns among Justice-Involved Individuals Who Use Opioids. Substance Use & Misuse, 55(13), 2165–2174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casillas A, & Clark L (2002). Dependency, impulsivity and self-harm: Traits hypothesized to underlie the association between cluster B personality and substance use disorders. Journal of Personality Disorders, 16(5), 424–436. [DOI] [PubMed] [Google Scholar]
- Connor J, Gullo M, Chan G, Young R, Hall W, & Feeney G (2013). Polysubstance use in cannabis users referredfor treatment: Drug use profdes, psychiatric comorbidity and cannabis-related beliefs. 4, 79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis J, Rabinowitz J, Wells J, Liu F, Finan P, Stein M, Antoine II D, Hobelmann G, & Huhn A (2022). Latent trajectories of anxiety and depressive symptoms among adults in early treatment for nonmedical opioid use. Journal of Affective Disorders, 299, 223–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernández-Calderón F, Vidal-Giné C, Rojas-Tejada A, & Lozano-Rojas O (2020). Patterns of Simultaneous Polysubstance Use among Partygoers: Correlates and Differences in Adverse Acute Effects Experienced. Journal of Psychoactive Drugs, 52(4), 344–356. [DOI] [PubMed] [Google Scholar]
- Ford J, & Gómez J (2014). The relationship of psychological trauma and dissociative and posttraumatic stress disorders to nonsuicidal self-injury and suicidality: A review. Journal of Trauma & Dissociation, 16(3), 232–271. [DOI] [PubMed] [Google Scholar]
- Gee B, Han J, Benassi H, & Batterham P (2020). Suicidal thoughts, suicidal behaviours and self-harm in daily life: A systematic review of ecological momentary assessment studies. Digital Health, 6, 2055207620963958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gicquelais R, Jannausch M, Bohnert A, Thomas L, Sen S, & Fernandez A (2020). Links between suicidal intent, polysubstance use, and medical treatment after non-fatal opioid overdose. Drug and Alcohol Dependence, 212, 108041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gjersing L, & Bretteville-Jensen A (2017). Patterns of substance use andmortality risk in a cohort of ’hard-to-reach’ polysubstance users. Addiction, 113, 729–739. [DOI] [PubMed] [Google Scholar]
- Gudin J, Mogali S, Jones J, & Comer S (2013). Risks, Management, and Monitoring of Combination Opioid, Benzodiazepines, and/or Alcohol Use. Postgraduate Medicine, 125(4), 115–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huhn A, Garcia-Romeu A, & Dunn K (2018). Opioid Overdose Education for Individuals Prescribed Opioids for Pain Management: Randomized Comparison of Two Computer-Based Interventions. Frontiers in Psychiatry, 9, 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IBM Corp. (2020). IBM SPSS Statistics for Windows. (27.0). IBM Corp. [Google Scholar]
- Jeffirs S, Jarnecke A, Flanagan J, Killeen T, Laffey T, & Back S (2019). Veterans with PTSD and comorbid substance use disorders: Does single versus poly-substance use disorder affect treatment outcomes?. Drug and Alcohol Dependence, 199, 70–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kearns N, Cloutier R, & Carey C (2019). Alcohol and marijuana polysubstance use: Comparison of PTSD symptom endorsement and severity patterns. Cannabis (Research Society on Marijuana), 2(1), 39–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly P, Robinson L, Baker A, Deane F, McKetin R, Hudson S, & Keane C (2017). Polysubstance use in treatment seekers who inject amphetamine: Drug use profiles, injecting practices and quality of life. Addictive Behaviors, 71, 25–30. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer R, & Williams J (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lang A, & Stein M (2005). An abbreviated PTSD checklist for use as a screening instrument in primary care. Behaviour Research and Therapy, 43, 585–594. [DOI] [PubMed] [Google Scholar]
- Licht C, Christoffersen M, Okholm M, Damgaard L, Fink-Jensen A, Kundsn G, & Erritoze D (2012). Simultaneous polysubstance use among Danish 3,4-methylenedioxymethamphetamine and hallucinogen users: Combination patterns and proposed biological bases. Human Psychopharmacology: Clinical & Experimental, 27(4), 352–363. [DOI] [PubMed] [Google Scholar]
- Lockwood T, Huynh P, Richard A, Sightes E, Bailey K, Ray B, & Lieberman M (2021). Community overdose surveillance: Comparing substances collected from the death scene investigation to toxicology results. Drug and Alcohol Dependence, 224, 108722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGovern M, Lambert-Harris C, Xie H, Meier A, McLeman B, & Saunders E (2015). A randomized controlled trial of treatments for co-occurring substance use disorders and post-traumatic stress disorder. Addiction, 110(7), 1194–1204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mericle A, Mahoney E, Korcha R, Delucchi K, & Polcin D (2019). Sober living house characteristics: A multilevel analyses of factors associated with improved outcomes. Journal of Substance Abuse Treatment, 98, 28–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moody L, Franck C, Hatz L, & Bickel W (2016). Impulsivity and polysubstance use: A systematic comparison of delay discounting in mono-, dual-, and trisubstance use. Experimental and Clinical Psychopharmacology, 24(1), 30–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén L, & Muthén B (1998). Mphis User ’s Guide (Eighth edition). Muthén & Muthén. [Google Scholar]
- Najavits L (2002). Seeking safety: A treatment manual for PTSD and substance abuse. Guilford Publications. [DOI] [PubMed] [Google Scholar]
- Nylund-Gibson K, & Choi A (2018). Ten frequently asked questions about latent class analysis. Translational Issues in Psychological Science, 4(4), 440–461. [Google Scholar]
- Padwa H, Urada D, Gauthier P, Rieckmann T, Hurley B, Crèvecouer-MacPhail D, & Rawson R (2016). Organizing Publicly Funded Substance Use Disorder Treatment in the United States: Moving Toward a Service System Approach. Journal of Substance Abuse Treatment, 69, 9–18. [DOI] [PubMed] [Google Scholar]
- Priester M, Browne T, Iachni A, Clone S, DeHart D, & Seay K (2016). Treatment access barriers and disparities among individuals with co-occurring mental health and substance use disorders: An integrative literature review. Journal of Substance Abuse Treatment, 61, 47–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ravndal E, & Amundsen E (2010). Mortality among drug users after discharge from inpatient treatment: An 8-year prospective study. Drug and Alcohol Dependence, 108(1–2), 65–69. [DOI] [PubMed] [Google Scholar]
- Rawlings J, Shevlin M, Corcoran R, Morriss R, & Taylor P (2015). Out of the blue: Untangling the association between impulsivity and planning in self-harm. Journal of affective disorders. Journal of Affective Disorders, 184, 29–35. [DOI] [PubMed] [Google Scholar]
- Rodriguez A, Robinson L, Kelly P, & Hudson S (2021). Polysubstance use classes and health outcomes among women attending specialist substance use treatment services. Drug and Alcohol Review. [DOI] [PubMed] [Google Scholar]
- Rossi R, Longo L, Fiore D, Carcione A, Niolu C, Siracusano A, & Di Lorenzo G (2019). Dissociation in stress-related disorders and self-harm: A review of the literature and a systematic review of mediation models. Journal of Psychopathology. [Google Scholar]
- Schneider K, Park J, Allen S, Weir B, & Sherman S (2019). Patterns of polysubstance use and overdose among people who inject drugs in Baltimore, Maryland: A latent class analysis. Drug and Alcohol Dependence, 201, 71–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz B, Wetzler S, Swanson A, & Sung S (2010). Subtyping of substance use disorders in a high-risk welfare-to-work sample: A latent class analysis. Journal of Substance Abuse Treatment, 38, 366–374. [DOI] [PubMed] [Google Scholar]
- Spitzer R, Korenke K, Williams J, & Löwe B (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archieves of Internal Medicine, 166(10), 1092–1097. [DOI] [PubMed] [Google Scholar]
- Tori M, Larochelle M, & Naimi T (2020). Alcohol or benzodiazepine co-involvement with opioid overdose deaths in the United States, 1999-2017. JAMA Network Open, 3(4), e202361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tuten M, Jones H, & Svikis D (2003). Comparing homeless and domiciled pregnant substance dependent women on psychosocial characteristics and treatment outcomes. Drag and Alcohol Dependence, 69(1), 95–99. [DOI] [PubMed] [Google Scholar]
- Valente P, Bazzi A, Childs E, Salhaney P, Earlywine J, Olson J, Biancarelli D, Marshall B, & Biello K (2020). Patterns, contexts, and motivations for polysubstance use among people who inject drugs in non-urban settings in the US Northeast. International Journal of Drug Policy, 85, 102934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vermunt J (2010). Latent class modeling with covariates: Two improved three-step approaches. Political Analysis, 18, 450–469. [Google Scholar]
- Wang L, Min J, Krebs E, Evans E, Huang D, Liu L, Hser Y, & Nosyk B (2017). Polydrug use and its association with drug treatment outcomes among primary heroin, methamphetamine, and cocaine users. International Journal of Drug Policy, 49, 32–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westad Y, Hagen K, Jonshu E, & Solem S (2021). Cessation of Deliberate Self-Harm Behavior in Patients With Borderline Personality Traits Treated With Outpatient Dialectical Behavior Therapy. Frontiers in Psychology, 12, 577230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wojciechowski T (2021). Borderline Personality Disorder as a Predictor of Drug Use Variety: Cognitive Vs. Affective Mechanisms. Journal of Psychoactive Drugs, 1–10. [DOI] [PubMed] [Google Scholar]
- Wu L, Ling W, Burchet B, Blazer D, Yand C, Pan J, Reeve B, & Woody G (2011). Use of item response theory and latent class analysis to link poly-substance use disorders with addiction severity, HIV risk, and quality of life among opioid-dependent patients in the Clinical Trials Network_. Drug and Alcohol Dependence, 118, 186–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Y, Mooney L, Yoo C, Evans E, Kelleghan A, Saxon A, Curtis M, & Hser Y (2021). Psychiatric comorbidity and treatment outcomes in patients with opioid use disorder: Results from a multisite trial of buprenorphine-naloxone and methadone. Drug and Alcohol Dependence, 108996. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.