Abstract
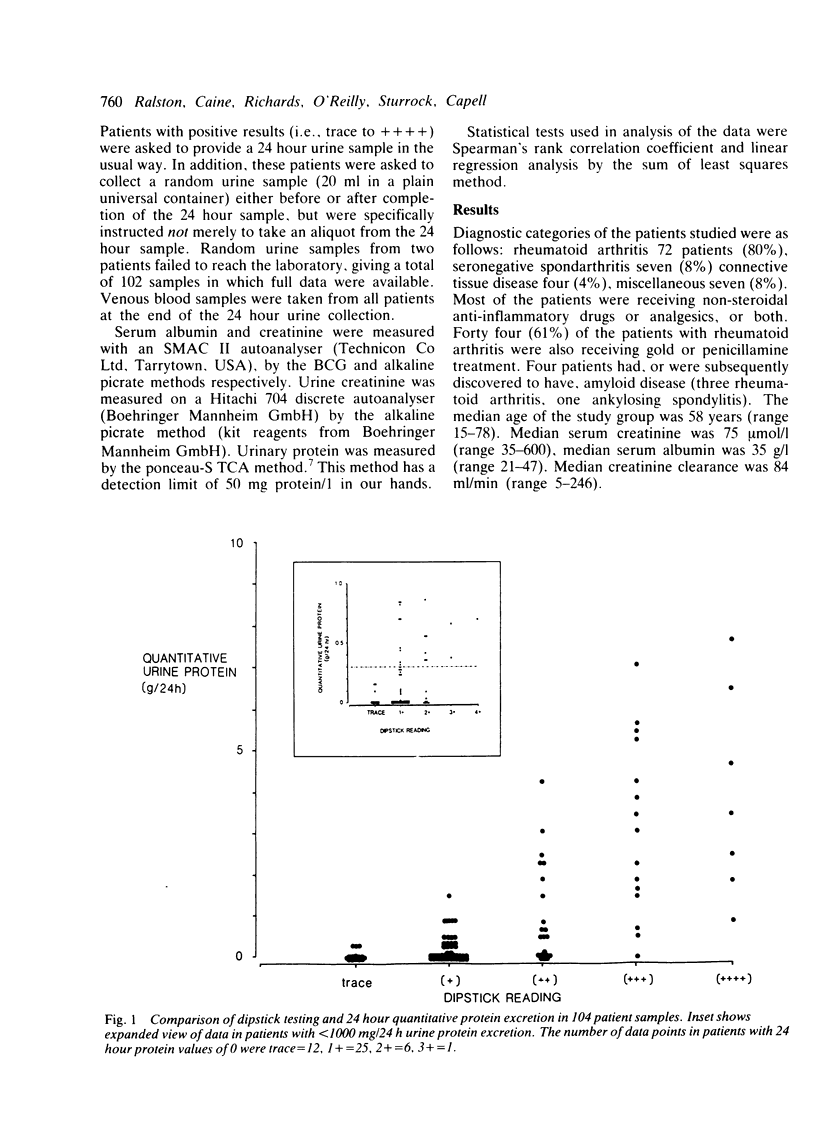
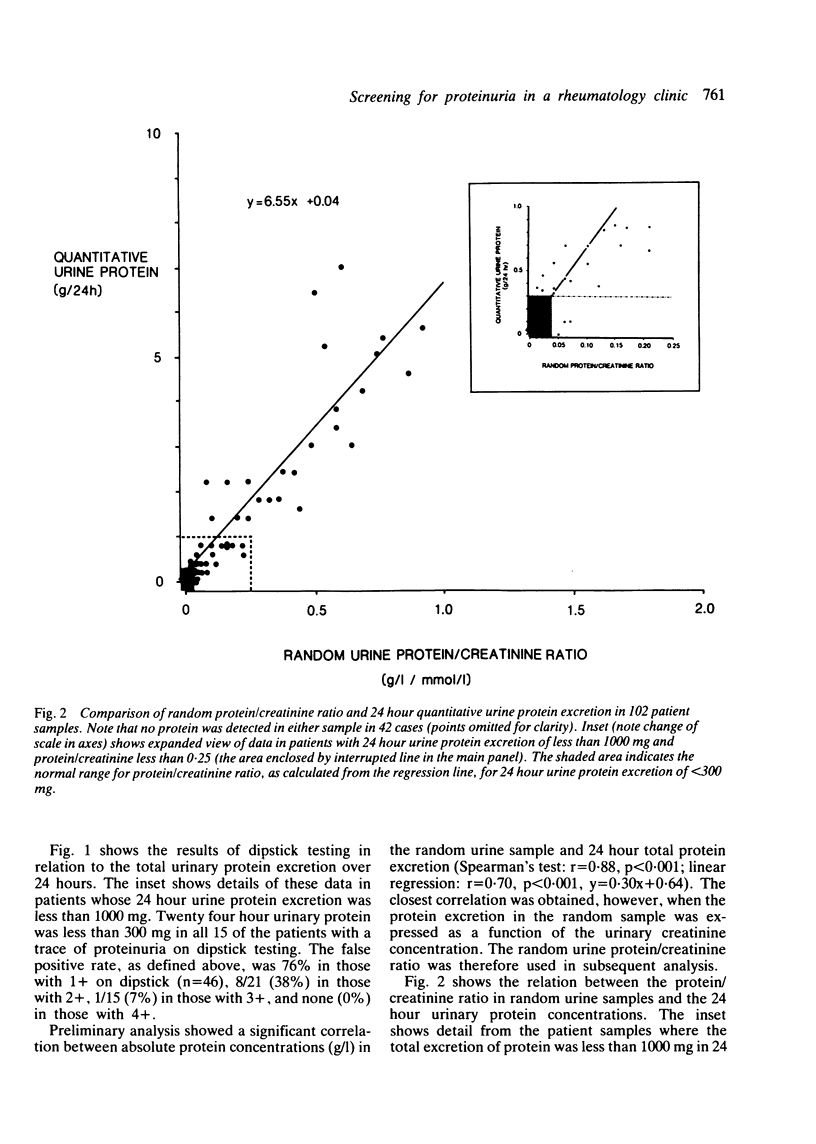
Measurements of protein/creatinine ratio in 'spot' urine samples were compared with measurements of 24 hour quantitative proteinuria and side room 'dipstick' testing in 104 samples from 90 patients presenting consecutively to a rheumatology unit. Linear regression analysis showed a highly significant correlation between the random urinary protein/creatinine ratio and total protein excretion in 24 hour urine samples (r = 0.92, p less than 0.001, y = 6.55x + 0.04). Although an approximation of 24 hour urinary protein excretion could have been made from the regression line: 24 hour urine protein = 6.55 x protein/creatinine ratio + 0.04 (g/l), there was a wide scatter of values, particularly in patients with greater than 1 g/24 h urinary protein excretion. Nevertheless, significant proteinuria (greater than 300 mg/24 h) could have been confirmed or excluded with a sensitivity and specificity of 97% by adopting random protein/creatinine values of less than 0.04 as 'normal'. Specificity and sensitivity could have been increased to 100%, however, by excluding patients with values lying between 0.01 and 0.10 as all the false negatives (n = 3) and false positives (n = 3) lay within this range. In comparison, dipstick testing, although 100% sensitive, had a poor specificity due to the high false positive rate (40/83 (48%] in patients with 1+ to 3+ readings. Assessment of random urinary protein/creatinine ratio may obviate the need for 24 hour urine collections in the initial assessment of suspected proteinuria. A wider application of this technique seems indicated in view of the obvious advantages in terms of cost, time, and patient convenience.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Barratt T. M., McLaine P. N., Soothill J. F. Albumin excretion as a measure of glomerular dysfunction in children. Arch Dis Child. 1970 Aug;45(242):496–501. doi: 10.1136/adc.45.242.496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gyure W. L. Comparison of several methods for semiquantitative determination of urinary protein. Clin Chem. 1977 May;23(5):876–879. [PubMed] [Google Scholar]
- Pesce M. A., Strande C. S. A new micromethod for determination of protein in cerebrospinal fluid and urine. Clin Chem. 1973 Nov;19(11):1265–1267. [PubMed] [Google Scholar]
- Rennie I. D., Keen H. Evaluation of clinical methods for detecting proteinuria. Lancet. 1967 Sep 2;2(7514):489–492. doi: 10.1016/s0140-6736(67)91656-x. [DOI] [PubMed] [Google Scholar]
- Shaw A. B., Risdon P., Lewis-Jackson J. D. Protein creatinine index and Albustix in assessment of proteinuria. Br Med J (Clin Res Ed) 1983 Oct 1;287(6397):929–932. doi: 10.1136/bmj.287.6397.929. [DOI] [PMC free article] [PubMed] [Google Scholar]


