Abstract
Alzheimer’s disease (AD) predominantly occurs as a late onset (LOAD) form involving neurodegeneration and cognitive decline with progressive memory loss. Risk factors that include aging promote accumulation of AD pathologies, such as amyloid-beta and tau aggregates, as well as inflammation and oxidative stress. Homeostatic glial states regulate and suppress pathology buildup; inflammatory states exacerbate pathology by releasing pro-inflammatory cytokines. Multiple stresses likely induce glial senescence, which could decrease supportive functions and reinforce inflammation. In this perspective, we hypothesize that aging first drives AD pathology burden, whereafter AD pathology putatively induces glial senescence in LOAD. We hypothesize that increasing glial senescence, particularly local senescent microglia accumulation, sustains and drives perpetuating buildup and spread of AD pathologies, glial aging, and further senescence. We predict that increasing glial senescence, particularly local senescent microglia accumulation, also transitions individuals from healthy cognition into mild cognitive impairment and LOAD diagnosis. These pathophysiological underpinnings may centrally contribute to LOAD onset, but require further mechanistic investigation.
Subject terms: Alzheimer's disease, Cognitive ageing, Microglia, Neuroimmunology, Complexity
In this perspective, the authors hypothesise that glial senescence, requiring senescent microglia burden, perpetuates further aging, Alzheimer’s pathologies, and senescence. Increasing glial senescence is proposed as necessary to drive individuals from healthy cognition into cognitive decline and dementia.
Introduction
Alzheimer’s disease (AD) is characterized by cognitive decline, most prominently manifested as progressive memory loss. AD risk factors include vascular pathology, declining metabolism, and most significantly, aging1–4. These risk factors contribute towards sporadic or late onset AD (LOAD) (>90% of AD cases), and early-onset or inherited, familial AD (EOAD)3. In LOAD, synaptic loss is pathologically correlated with neurodegeneration and cognitive decline1,2. Widely accepted explanations for neuronal loss and LOAD progression have been proposed in the tau hypothesis and amyloid cascade (Box 1). While clinical trials targeting these two pathologies will hopefully halt AD3,4, focuses on understanding AD have more recently expanded into next-generation sequencing, aging-related oxidative stress, and glia. Particularly, genetic risk factors such as TREM2 and APOE have exclusive roles in glia among the central nervous system3. Some of these genes mediate increased phagocytic function in glia, whereas others allot glia towards adopting pro-inflammatory states leading to chronic damage to cell machinery (i.e., lipids, proteins, nucleic acids) and premature cell death. Possible roles of glial senescence in AD were also recently explored5,6.
Cellular senescence is an irreversible cell arrest caused by replicative senescence or local, environmental challenges7–9. Senescence induction and characterization is heterogeneous, varying across cell types, as well as physiological and pathological environments; DNA damage, oxidative stress via the p38 MAPK pathway, and the NLRP3 inflammasome can induce senescence9–11. Due to heterogeneity, no universal markers for senescence are currently available7. Senescent cells gain apoptotic resistance with organelle dysfunction, increased levels of reactive oxygen species, and substrate build-up7. These substrates can comprise senescence-associated beta-galactosidase (SA-β-gal), ferritin, iron, and lipofuscin accumulation7,12,13. Other senescence markers include p16INK4A and p21 upregulation relating to cell cycle arrest, and senescence-associated heterochromatin foci formation7. Senescent cells often adopt a senescence-associated secretory phenotype (SASP) involving cGAS-cGAMP-STING signaling, subsequent release of type I interferons (IFN), matrix metalloproteases (MMPs), HMGB1 protein, and other mediators varying across cell types7,11,14. SASP regulators include NF-κβ, C/EBP, and HMGB19,10.
Senescence is considered to play physiological roles, yet with aging it becomes implicated with accelerated mortality7. Senolytic drugs selectively removing senescent cells increase lifespan and quality of life in mice15–17. Although senescence involvement in LOAD has been explored5,6,18–20, how senescence relates to LOAD and Braak staging is not well defined. We hypothesize that LOAD progresses based on the (i) severity of glial cell aging and (ii) maladaptive senescence accumulation corresponding to Braak staging. This perspective presents this hypothesis by first explaining LOAD and aging, followed by discussing evidence of glial dysfunction and decline in LOAD. We then propose integrated mechanisms involving AD pathology, glial senescence induction, and neurodegeneration. We predict that an accumulation of senescent microglia in local brain regions may (i) enhance Aβ and hp-tau aggregate spread, (ii) enhance synaptic loss, and (iii) induce paracrine senescence in nearby cells, resulting in heterogeneous, local spread converging into Braak staging progression.
Box 1: A brief summary of Braak staging and dominant LOAD theories of pathology.
The Amyloid Cascade and Tau hypotheses are the best characterized mechanisms for explaining synaptic loss and neurodegeneration observed over LOAD progression.
The Amyloid Cascade Hypothesis asserts that amyloid-beta (Aβ) protein accumulation, especially Aβ oligomers, acts through multiple pathways to cause neurodegeneration and synaptic loss2,3. Misfolded Aβ monomers undergo a slow “seeding”, nucleating phase into damaging Αβ oligomers, which then further aggregate into insoluble Aβ fibrils and diffuse amyloid plaques without hp-tau aggregates3. Misfolded hp-tau and Aβ can also destabilize their respective native conformations and spread equivalently as prions in conditions including increased acidity3. Moreover, Aβ and hp-tau pathology can promote seeding and further accumulation of the other (Fig. 1)3. While Aβ protein levels are generally increased in patients with LOAD vs controls, diffuse amyloid plaques and insoluble Aβ fibril aggregation do not correlate well with LOAD progression1,120,125.
The Tau Hypothesis suggests that upstream enzymes including p38 MAPK and GSK3 phosphorylate multiple residues in tau protein to create hyperphosphorylated tau (hp-tau)1,3. In this hypothesis, hp-tau starts as soluble monomers and oligomers but can form higher-complexity aggregates in insoluble fibrils, neuropil threads, and neurofibrillary tangles (NFTs). Neuritic plaques, which comprise compact amyloid plaques containing Aβ, hp-tau, and dystrophic neurites1,3,106,125, also constitute as hp-tau pathology. Together, all forms of hp-tau aggregation are classified as “neurofibrillary pathology”. Hp-tau or neurofibrillary pathology is considered to correlate well with cognitive impairment and dementia1,100,125.
Braak Staging: Post-mortem assessments of cognitive decline and correlates of neurodegeneration severity in LOAD have been extensively tracked via Braak staging1,120. Here, hp-tau aggregation and neurofibrillary degeneration are clinically documented into a set of six Braak stages125. In stages I and II, initial neurofibrillary pathology spreads from the transentorhinal region into the entorhinal cortex and hippocampus. Stages III and IV involve increased lesions and pathologies in these areas, as well as novel spread into the temporal lobe and insular cortex. Stages V and VI affect the remaining superior temporal gyrus and neocortex. Braak staging tracking hp-tau pathology burden was notably shown to correlate with LOAD progression, where stage IV is associated with an overt dementia diagnosis (Fig. 2)1,100,125.
Hypotheses outside the Tau Hypothesis and Amyloid Cascade Hypothesis focus on other contributors and risk factors associated with LOAD. Although this perspective hypothesizes that these factors eventually converge into increased glial senescence, comprehensive review of these theories is outside this perspective’s scope. Briefly, other factors include impaired metabolism via increased insulin, hypertension, obesity, and/or insufficient sleep3,4. Vascular dementia, consisting of progressive blood supply blockade, cerebral amyloid angiopathy (CAA) and Aβ deposition into the cerebral blood vessels, likely leads to and/or correlates with LOAD incidence1,4. AD pathology is often co-morbid with pathologies from other diseases such as Parkinson’s disease with dementia1. Finally, these different pathologies involve a neuroimmune component; inflammation caused by peripheral and central pro-inflammatory cytokines increases during LOAD, notably as a result of accumulating protein aggregation and compromised cell metabolism2–4.
LOAD and aging
Aging and oxidative stress
LOAD requires aging, during which aged cells accumulate reactive oxygen and nitrogen species (RONS);21 RONS accumulation can overwhelm antioxidant defenses to irreversibly alter and damage nucleotides, lipids, and proteins. This “oxidative stress” occurs repeatedly with age due to accumulating double-stranded DNA breaks, mitochondrial dysfunction, and declining efficiency of metabolic processes5–7,21. Oxidative stress activates pathways that elevate and/or accompany Aβ production, tau hyperphosphorylation, and release of pro-inflammatory cytokines including IL-1 and TNF2,7,11,21,22. With aging, increased pro-inflammatory cytokine production results in a chronic systemic “inflammation” that escalates over time, exacerbating RONS accumulation, cell damage, and leading to premature death3,23. LOAD risk factors including vascular pathology, sleep impairment, and chronic stress result in increased RONS levels as well as chronic, systemic inflammation2–4. Furthermore, increased inflammation and the NLRP3 inflammasome can induce local or paracrine senescence via IL-1α signaling10.
Oxidative stress damages all cell types including neurons. Particularly, RONS inhibit phosphatidylserine (PS) lipid translocases, increase intracellular calcium, deplete ATP, and activate phosphatidylserine scramblases; this “flips” PS from the inner to outer cell membrane, where exposed PS acts as an apoptotic or “eat-me” signal24–26. RONS create “oxysterols” by oxidizing membrane cholesterols; oxysterols are hypothesized to drive LOAD27,28. Oxidative stress acts via DNA damage and p38 MAPK signaling to induce senescence7.
In brain regions relevant to Braak staging, aging and AD pathologies can induce the accumulation of other pathologies causing further cellular damage and death in a circular relationship (Fig. 1)2,3,5,6,11,21–23,28,29.
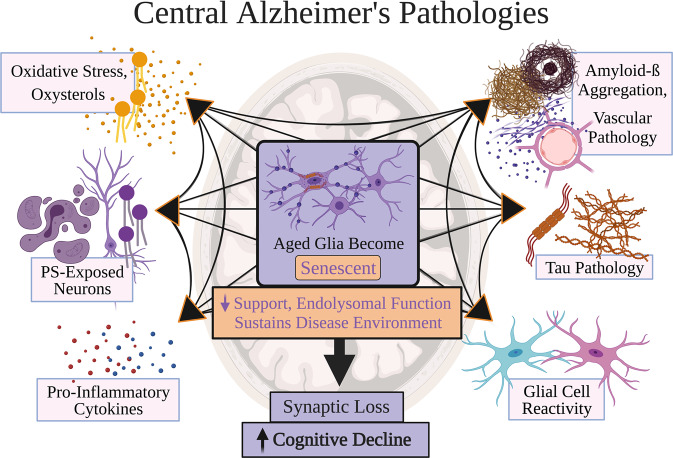
Fig. 1. Central Alzheimer’s pathologies.
Risk factors for late-onset Alzheimer’s disease (LOAD) are proposed to contribute to at least one of six main pathologies: oxidative stress and oxysterol production, phosphatidylserine (PS)-exposed neurons, pro-inflammatory cytokines, amyloid-beta aggregation and vascular pathology, tau pathology, and glial cell reactivity. Each main pathology likely eventually adds to and increases the burden of other main AD pathologies. These pathologies may ultimately converge to drive improper neuronal support, synaptic loss, and death, resulting in neurodegeneration clinically corresponding to cognitive decline. Centrally, the repeated buildup of these six LOAD pathologies proposedly pushes an aged glial system into senescence induction and accumulation. This burden of senescent glia is predicted to sustain a disease environment that determines local neurodegeneration involved in LOAD progression. Glial senescence is briefly characterized as dysfunctional glial states with impaired endolysosomal function and support for nearby cells. What constitutes glial senescence burden may well vary per an individual’s genetics, physiology, and environmental experiences; nonetheless, it is predicted that the glial senescence burden differentiates a cognitively healthy or resilient individual from one diagnosed with LOAD. Purple color designates associations with senescence and dementia progression. Figure created with BioRender.com.
Aging and CNS glia
The CNS contains multiple glial types, including oligodendrocyte progenitor cells (OPCs), astrocytes, and microglia. Glia altogether serve numerous key roles30, and can be divided into “states” notably labeled as “homeostatic”. Homeostatic glial activities sequester and remove cellular products to preserve optimal function30, including degrading products associated with AD pathologies (Fig. 1)31,32. This parenchymal maintenance is achieved by paracrine signaling and endocytosis. Homeostatic glial functions involve release of trophic factors and anti-inflammatory cytokines (e.g., IL-10 and TGF-β), which acutely minimize cellular stress and pro-inflammatory reactions33–35. These molecules mediate communication in bi-directional loops of glia-neuron and glia-glia interactions, through which glia supporting one another facilitate neuronal activity and plasticity30,34,36–40. For instance, OPC-mediated functions via TGF-β2-TGFBR2-CX3CR1 signaling sustain homeostatic microglial activities33,34. Astrocytes also produce trophic factors and cytokines including IL-3 to reduce pro-inflammatory microglial states41, and both glia endocytose neuronal, synaptic, and extracellular elements42–48. Such endocytosed elements include the AD pathologies illustrated in Fig. 1;3,30 microglia phagocytose extracellular Aβ and tau through receptors like TREM2 and IGF1R3.
Receptors that facilitate Aβ and tau clearance can push homeostatic glia into “pro-inflammatory” states. Examples comprise RAGE and LRP1 receptors activating the NLRP3 inflammasome3,49–51. While pro-inflammatory glia can effectively protect against acute illness and infection, their continuous and exaggerated reactions during aging can instead promote cellular stress, premature death, and (indirectly) AD pathologies and neurodegeneration in patients with LOAD vs resilient individuals2,3,5,52. Gradually reducing homeostatic support for glia may equate to “priming”, where aged glia “hyperactivate” pro-inflammatory responses towards smaller amounts of pro-inflammatory cytokines or Aβ11,53,54. In parallel, aging and exposure to RONS reduce homeostatic signaling, notably impairing the TGFβII-Smad pathway in aged microglia46,47,51. Aged microglia and astrocytes can additionally decline in metabolism and endolysosomal systems6,7,51,53,54, likely resulting in reduced phagocytotic capacity leading to exacerbated Aβ and hp-tau deposition54,55. Thus, while homeostatic glial functions normally protect the adult brain, their ability to combat both increasing pro-inflammatory glial responses and traditional AD pathologies likely wanes with aging and risk factor exposure (Fig. 2).
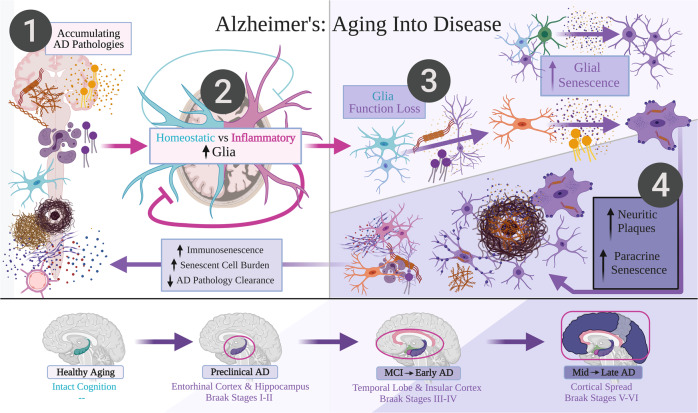
Fig. 2. Alzheimer’s: aging into disease.
A late-onset Alzheimer’s disease (LOAD) framework is proposed from healthy cognitive aging to late-stage Alzheimer’s disease (AD), presenting the following testable hypothesis: Glial senescence accumulation, particularly requiring increased senescent microglia burden, may correspond to clinical LOAD progression. Darker and deeper purple coloring denotes more severe senescent glia burden and Braak staging progression in LOAD. The hypothesis presents that: (i) Aging and AD pathologies from Fig. 1 (including amyloid-beta (Aβ), neurofibrillary pathology in hyper-phosphorylated tau (hp-tau), oxidative stress, and chronic inflammation) are predicted to progressively accrue throughout aging as by-products of central nervous system function and metabolism. (ii) Main AD pathology levels are likely enhanced by inflammatory glial states, and would be sufficiently cleared by glia performing homeostatic roles. However, homeostatic glial functions that putatively decline throughout aging would decrease proficiency in containing AD pathologies. (iii) In preclinical AD, increasing proportions of aged glia likely interact with AD pathologies to become senescent. This would include oligodendrocyte progenitor cells and astrocytes. Microglia performing homeostatic roles would also become senescent especially after engulfing neurons containing hp-tau. (iv) Senescent microglia then likely become incompetent in breaking down further phagocytosed hp-tau and Aβ aggregates, and instead secrete hp-tau to induce paracrine senescence in other microglia, especially those which are actively engulfing Aβ. Failure to suddenly degrade both hp-tau and Aβ likely induces secretion of Aβ and hp-tau aggregates that coalesce into neuritic amyloid plaques. These neuritic plaques correspond to Braak staging and clinical LOAD progression. Finally, this combination of senescent glia, reduced homeostatic glial support, and non-senescent, inflammatory glial states is predicted to drive neurodegeneration and cognitive decline in LOAD. While senescent glia burden is cleared out by immune cells, increasing immunosenescence over aging due to genetic and environmental circumstances likely slowly declines; thus, senescent glia burden is predicted to ultimately differentiate healthy cognition from mild cognitive impairment and LOAD. Figure created with BioRender.com.
Aging and AD as putative inducers of glial senescence
As aging promotes oxidative stress and AD pathology, cells experiencing these stressors can be predisposed towards becoming senescent throughout one’s lifespan (Fig. 3.). In healthy physiology, immune cells including microglia phagocytose cells exposing PS42, which may include stressed and senescent cells24. However, immune cells can also decline over one’s lifespan and become senescent themselves. This “immunosenescence’” is offset by beneficial (epi)genetic variation and the ability of immune cells to renew by proliferation18. As there is a limit to mitotic cycles and environmental stresses that can be tolerated, immune cells can only proliferate a maximum number before becoming senescent. With increasing senescence and immunosenescence burden over time, senescence is considered a pathology of aging7.
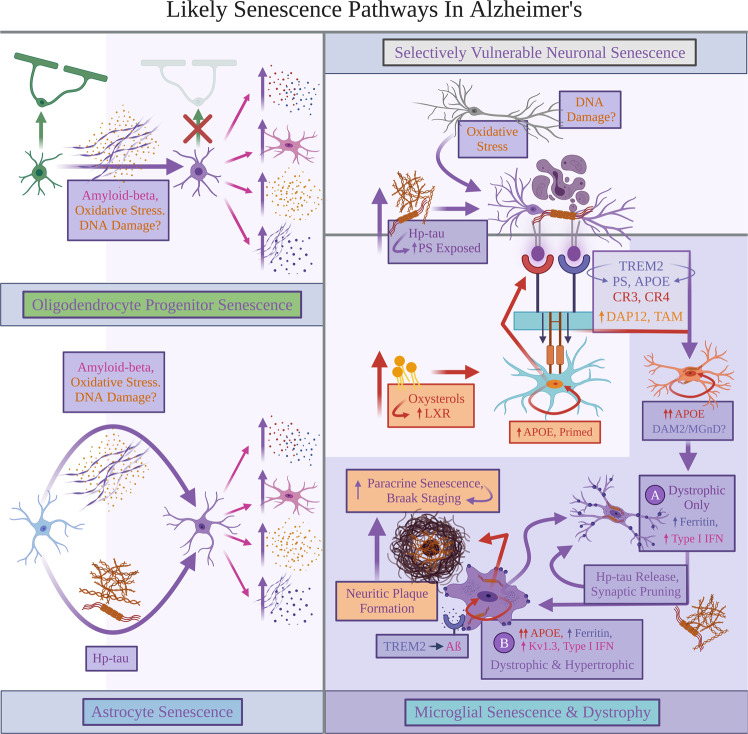
Fig. 3. Likely senescence pathways in Alzheimer’s.
Explanations for Alzheimer’s disease (AD) pathologies inducing senescence are proposed. Oligodendrocyte progenitor cells (OPCs) and astrocytes likely both react with amyloid-beta (Aβ) to become senescent. Oxidative stress and DNA damage may specifically lead to Aβ−induced senescence. Senescent OPCs and astrocytes are predicted to indirectly increase four pathologies: pro-inflammatory cytokines and reactive microglial states, oxidative stress, and Aβ accumulation. In neurons, oxidative stress, inflammation, and possibly DNA damage likely induce tau hyperphosphorylation; this process may also render the affected neurons senescent. Oxidative stress and hyperphosphorylated tau (hp-tau) aggregation likely prompt neurons to translocate and expose outer phosphatidylserine (PS). While aging predisposes sustained increases in local levels of inflammation, oxidative stress, and Aβ pathology burden, senescent OPCs and astrocytes are proposed to further worsen AD pathology. Senescent OPCs and astrocytes speculatively favor AD pathology buildup and environmental conditions that induce exacerbated microglial senescence in LOAD. Particularly, Aβ pathology contributes buildup to oxidative stress that oxidizes cholesterol to form oxysterols; these oxysterols may bind with liver-X-receptor expressed by homeostatic microglia states, resulting in upregulated apolipoprotein E (APOE) expression. Oxidative stress can also prime APOE-upregulated microglia to bind with neuronal PS using various receptors, enabling microglia to prematurely phagocytose and kill PS-exposed neurons containing hp-tau. This likely renders microglia senescent and unable to effectively phagocytose further AD pathologies, becoming proposed subtype or state “A” senescent microglia increasing type I interferon signaling, displaying dystrophic morphology, accumulating ferritin, and facilitating increased synaptic loss. They also proposedly secrete soluble hp-tau rendering paracrine senescence in nearby glia, thereby preceding neurofibrillary tangle accumulation in neurons. Local microglia attempting to actively phagocytose Aβ are predicted to be caught in this paracrine senescence feedback loop, becoming subtype or state “B” senescent microglia characterized by simultaneous dystrophy and a hypertrophic or “ameboid” appearance. We hypothesize that these hypertrophic, dystrophic, and senescent microglia secrete partially-digested aggregates that form neuritic plaques and further induce paracrine glial senescence. Finally, fewer homeostatic microglia proposedly remain available to degrade Aβ; Aβ would likely continuously accumulate and initiate increased pro-inflammatory responses, APOE, and KCNA3 upregulation in state “B” senescent microglia. Figure created with BioRender.com.
Because LOAD is an aging disease involving senescence1,3, we propose that progressive cognitive decline and memory loss observed in LOAD are related to senescence. Indeed, shortened telomere lengths and increased immunosenescence are found in patients with LOAD18,19. Multiple mouse models displaying cognitive impairment and tissue dysfunction demonstrated senescent cells in the brain, where removing p16INK4A-upregulated, likely-senescent cells was able to reduce inflammation and increased performance in spatial memory tasks15,17,39,56. The aged vs younger mouse brain has higher levels of senescent cell markers15,17. This supports the view that LOAD-associated cognitive impairment progresses in an environment associated with increased senescent cell burden. Together, age-associated increases in oxidative stress, Aβ accumulation and hp-tau pathology likely induce senescence among glia.
In LOAD, APP overexpression and subsequent Aβ accumulation likely exacerbate OPC loss of function and senescence (Fig. 3). In APP/PS1 mice overexpressing Aβ, OPCs surrounding Aβ plaques positively stained for senescent markers p21, p16INK4A, and SA-β-gal39. Administering the antihistamine clemastine preserved OPC and oligodendrocyte function leading to restored myelin levels in 7–8 month APP/PS1 mice equivalent to those of age-matched, wild-type controls; clemastine also reduced SA-β-gal and p21-upregulated OPC numbers57. Lower OPC senescence may be tied to increased myelination in APP/PS1 mice; patients with LOAD exhibit decreased white matter integrity vs healthy controls58. 14-month APP/PS1 mouse hippocampi also display decreased OPCs and correlated myelin counts vs controls59, reinforcing that OPC senescence may contribute to the reduced oligodendrocyte differentiation and myelin integrity observed in patients with LOAD57,58. As senescent neural progenitors additionally release HMGB1 and inhibit OPC function leading to decreased remyelination60, glial senescence may simultaneously induce dysfunction in non-senescent, homeostatic OPC states.
NAD + levels deplete over aging and neurodegenerative disease progression, increasing cGAS-cGAMP-STING signaling and inflammation61,62. Hou et al. supplemented 7-month-old APP/PS1 mice with NAD + precursor (NR) for 5 months. In the cortex, NR inhibited cGAS-cGAMP-STING signaling, which alleviated both inflammation and senescence counts (via decreased p16INK4A-upregulated immunostaining)62. Removing senescent OPCs via senolytics, and decreasing senescent cell (including OPC) burden via NAD + supplementation, independently increased spatial memory in APP/PS1 mice39,62, with the treated APP/PS1 mice performing equivalently to wild-type controls. Targeting glial senescence and aging may likely improve cognitive impairment in mild cognitive impairment (MCI) and LOAD.
Zhang et al. investigated patients with LOAD vs diagnosed with MCI vs control subjects without dementia. Control subjects without dementia were categorized as Braak stages 0–I, patients with MCI as Braak stages III–V, and those with LOAD as Braak stage VI (exempting one Braak stage III–IV)39. Braak stage progression speculatively accompanies increased Aβ plaques, where patients with LOAD vs MCI had an average senescent OPC count per plaque significantly higher in the inferior parietal cortex; patients with MCI displayed a higher average, non-significant senescent OPC count vs control subjects without dementia39. We speculate that (i) OPC senescence begins with an increased Aβ burden in older age and precedes clinical dementia diagnosis, then (ii) continues to accumulate along the disease progression into latter Braak stages (Fig. 2). As Aβ contributes to increased RONS levels in neurons23, OPCs may potentially become senescent via DNA damage and/or oxidative stress (Fig. 3).
Astrocytes likely undergo increased senescence with AD pathologies. Oxidative stress, Aβ, and hp-tau can independently induce human astrocyte senescence in-vitro63–65. These senescent astrocytes exhibit a SASP profile, releasing pro-inflammatory cytokines and MMPs63–65. Senescent astrocytes induced by hp-tau uptake display a SASP profile and contribute to cognitive impairment via HMGB1 and NLRP3 inflammasome activation29,64. Their effects may contribute to driving AD pathology buildup, and negatively impact healthy functioning in other cells. Senescent astrocytes down-regulate Kir4.1 and EAAT1/2 transporters, leading to extracellular glutamate, neuronal excitotoxicity and cell death36,38, and increased NMDA-receptor signaling and pro-inflammatory microglial states66. Primary mouse astrocytes aged in-vitro display a SASP profile, where medium containing released extracellular vesicles from aged astrocytes (vs young astrocytes without a SASP profile) failed to support OPC differentiation37. As lacking OPC differentiation induces lower oligodendrocyte counts and myelin generation57, senescent astrocyte activity may promote decreased white matter integrity observed in patients with LOAD58.
Senescent astrocytes (p16INK4+) are abundant during human aging and neurodegenerative disease38, and display increased p16INK4A and MMP-1 expression among the frontal cortex in LOAD63. Over 75% of GFAP + astrocytes were p16INK4A + in the frontal cortex of patients with LOAD, and frequently stained for hp-tau oligomers and γ-H2AX indicating DNA damage64. Furthermore, p16INK4+ mouse astrocytic cells exposed to hp-tau in culture released extracellular HMGB1; this HMGB1 was collected as culture medium and induced further senescence in healthy astrocyte cultures via positive SA-β-gal staining, cell cycle arrest, and increased IL-6 and TNF release64. As senescent astrocytes likely induce dysfunction in other glia36,38,66, this dysfunction may involve paracrine senescence that transforms previously-homeostatic astrocytes64. HMGB1 exposure inhibited OPC differentiation and decreased myelination in rat spinal cord and human cultures derived from induced pluripotent stem cells;60,67 senescent astrocytes may release HMGB1 to induce OPC dysfunction and reduce white matter integrity in LOAD58.
Increased senescent OPCs and astrocytes may together exacerbate AD pathology burden and critically contribute to LOAD (Fig. 3). We hypothesize that senescent glia promote AD pathologies (Fig. 1) by weakening neuronal support and triggering cell death, notably via RONS release and NLRP3 inflammasome activation3,23,29,50, and further inducing pro-inflammatory glial states5,6. Astrocyte and OPC senescence may also induce paracrine glial senescence through RONS release and NLRP3 activation via IL-1α signaling5,10,19. However, while Aβ and/or likely oxidative stress can trigger OPC and astrocyte senescence without hp-tau involvement39,59,65, astrocyte and OPC senescence are not confirmed yet to correlate with neurofibrillary degeneration in Braak staging. Thus, an “additional player” could be needed to predict how glial senescence may mediate a preclinical to clinical LOAD transition.
We speculate that in preclinical LOAD, senescent OPCs and astrocytes withdraw their homeostatic support and exacerbate AD pathology accumulation. These effects are posited to “prime” homeostatic microglial states into becoming mainly pro-inflammatory and phagocytosing more neurons5,6,33,34,41,51,53,66, and may provide local environments that strongly favor microglial senescence–considered here as the “additional factor”. Senescent microglia abundance is argued as the final requirement for a preclinical to clinical LOAD transition, by potentially accelerating neurofibrillary pathology spread (Figs. 2, 3).
Local microglial senescence accumulation in LOAD
Tau and type I IFN responses in microglial senescence
When microglia are primed to phagocytose in LOAD, they likely uptake hp-tau aggregates and then become senescent. In a P301S tauopathy mouse model overproducing hyperphosphorylated human tau, microglia displayed p16INK4A and SA-β-gal staining56. Microglial states associated with neurodegeneration were similarly observed in P301S and P301L mice (also overproducing human hp-tau)68, where these microglia initially upregulated pro-inflammatory genes. These microglia later transitioned into populations displaying gene enrichment linked to senescence, such as inhibited cell cycle, upregulated type I IFN release5–7,14, and reduced pro-inflammatory signaling68. Thus, we speculate increased local concentrations of hp-tau aggregates could induce microglial senescence.
In-vitro tau uptake by primary mouse microglia caused cytoplasmic binding to intracellular PQBP1, PQBP1-cGAS-cGAMP-STING signaling, and an initial inflammatory response69. This work also provided in-vivo confirmation of PQBP1-tau colocalization in R6/2 transgenic mice modeling Huntington’s disease pathology. Using an immunodeficient mouse model with human iPSC-derived microglia from patients with Down syndrome, Jin et al. added tissue containing hp-tau from patients diagnosed with both LOAD and Down syndrome; exposed human microglia were highly enriched in genes implicating senescence, type I IFN release and signaling70. They also found that type I IFN-α/β receptor (IFNAR) knockdown restored impaired synaptic plasticity and neurotransmission, concluding that increased type I IFN release and signaling in microglia exacerbated synaptic pruning70. Senescent microglia were found to display (i) upregulated type I IFN release, by which they (ii) likely mediate increased synapse loss—a central mechanism in LOAD progression and pathology1,2. This explanation aligns with the findings of synapse loss and microglial reactivity preceding NFT formation in P301S mice71.
APP/PS1 and 5xFAD mice feature upregulated microglial type I IFN signaling and increased synaptic loss;72,73 ablating microglia-specific IFNAR also reduced post-synaptic loss in 5xFAD mice73. 5xFAD mice notably demonstrate hp-tau staining73, particularly in neuritic plaques74. By blocking IFNAR and subsequent type I IFN signaling in these mice, interferon and inflammation mRNA levels in 5xFAD hippocampi were lowered; IFNAR inhibition further restored spatial memory and synaptic deficits in 5xFAD mice to levels equivalent to wild-type controls73. This complements the findings by Jin et al.70, where senescent microglia were shown to upregulate type I IFN signaling and increase synaptic loss via pruning. Furthermore, IFNAR blockade did not alleviate Aβ burden in 5xFAD mice73. This supports our prediction that senescent microglia accumulation within key brain regions may determine cognitive impairment and LOAD progression (Figs. 1, 2).
Microglia may selectively become senescent after engulfing hp-tau through their capacity to prematurely kill neurons via phagocytosis, or “phagoptosis” (Box 2). Both extracellular and intracellular hp-tau inducing PS exposure in neurons were shown to lead to microglia phagoptosing neurons in-vitro75,76. In mouse microglial and P301S neuronal co-cultures, microglia phagoptosed neurons containing hp-tau aggregates77. These microglia became senescent via increased NF-κβ activation, MMP-3 release, and positive SA-β-gal staining; these senescent microglia also reduced their phagocytic capacity and phagoptosis of additional P301S neurons containing hp-tau, while further secreting insoluble hp-tau aggregates77. As cultured human microglial cells can also phagoptose PS-exposed, P301S neurons containing hp-tau aggregates57, both human and mouse senescent microglia can likely release and seed insoluble hp-tau aggregates78–80. As senescent microglia cannot remove these neurons, however, increased microglial senescence could indirectly permit increased NFT formation.
Conditioned media isolated from senescent microglia and P301S neuronal co-cultures induced microglial senescence in separate wild-type mouse cultures;77 thus, senescent microglial secretions containing hp-tau triggered local and paracrine, microglial senescence77. Phagotopsis of neurons containing hp-tau aggregates could therefore precede hp-tau-mediated, paracrine senescence77, although these processes are likely inevitably coupled over LOAD progression. Hp-tau seeding and release by senescent microglia putatively induce a pathological cycle of selective neuronal vulnerability to tau hyperphosphorylation, neuronal phagoptosis, synaptic loss, and paracrine senescence70,72,75–77 (Fig. 3).
Microglial priming and senescence in LOAD
As hypothesized above, LOAD would likely require glial aging and AD pathology buildup to induce microglial priming and senescence. We will further speculate here that microglial priming in LOAD involves increased oxidative stress and accelerated oxysterol production over aging27,28. Oxysterol accumulation is recognized by microglial liver X receptor (LXR), whereupon oxysterol and LXR binding, microglial APOE is upregulated81. In AD, upregulated APOE and “primed” microglia may correspond to DAM1 in mouse models82,83 (Box 2). While potential functions remain unclear, this may induce APOE secretion; as oxysterols deplete unoxidized cholesterol, LXR-stimulated microglia may secrete APOE packaged with cholesterol to aid in neuronal, myelin, and synaptic phagocytosis84. Upregulated APOE3/4 can act as a nuclear receptor in microglia (Fig. 3) to accelerate their aging and pro-inflammatory responses, as well as increase Aβ aggregation, tau hyperphosphorylation, and phagoptosis in APOE4 variants85–87. APOE secretion also leads to APOE-PS binding to stressed, desialylated neurons25.
We hypothesize that local environments speculatively promoting microglial APOE may (i) further pressure neurons to expose outer PS and accumulate tau hyperphosphorylation, and (ii) prime particular microglial states to phagotopse neurons (Figs. 2, 3). Reinforcing earlier discussion on hp-tau aggregates and neuronal phagoptosis, APOE knockdown in P301S mice significantly reduced hippocampal and entorhinal cortex loss;40 APOE preservation increased Iba1 + (suggesting microglia and macrophage populations) cells that were positive with CD68 + phagocytic inclusions40,88. As Shi et al. also found that astrocytes secreted APOE in P301S mice, they investigated whether APOE contributions to neurodegeneration and advanced hp-tau deposition resulted from astrocytes or microglia. Depleting a majority of microglia via CSF1R inhibition in P301S mice equally preserved the hippocampus and entorhinal cortex, while leaving astrocytic numbers significantly unaffected40. As microglial ablation blocked advanced deposition of hp-tau pathology, microglia and APOE were concluded to synergistically exacerbate hp-tau pathology progression and neurodegeneration40. APOE likely critically primes microglia towards advancing LOAD progression, suggesting that senescent microglia, involving hp-tau specificity, are likely a “final” requirement needed to advance neurofibrillary pathology and LOAD progression.
Homeostatic microglial states expressing TREM2 and upregulating APOE are predicted to bind PS-exposed neurons with hp-tau aggregates (Fig. 3), likely triggering neuronal and hp-tau phagoptosis via TREM2, complement receptors and opsonins25. It is currently unknown whether a TREM2-dependent, DAM2 program itself initiates senescence, or if phagoptosing neurons with hp-tau induces simultaneous DAM2 and senescence. A DAM2(-like) microglia state can likely overlap with senescence; DAM2 transcriptomic signatures are separately enriched in senescent microglia in aging, tauopathy and Aβ-overproducing transgenic mouse models, and in senescent human microglia exposed to LOAD patient tissue containing hp-tau17,68,70,89.
Mechanisms inducing senescence via hp-tau are currently unclear, but hp-tau may initiate senescence to inhibit apoptosis90. NFT-containing neurons from P301L mice and patients with frontotemporal dementia displayed upregulated senescence markers including CDK2NA, TNF, and IL-1β 5,91. Neurons may moreover induce senescence to prevent apoptosis triggered by oxidative stress and DNA damage8,90,92. Vulnerable neurons affected in Braak staging are often excitatory and display NFT formation93,94. As hp-tau induces microglial and astrocytic senescence56,64,77, “stressed” neurons exposed to ROS may become senescent through oxidative-stress-induced, tau hyperphosphorylation (Fig. 3). These neurons may then expose PS75, prior to rendering microglia senescent. Together, hp-tau pathology could induce senescence among multiple cell types (Fig. 3).
Furthermore, single-cell transcriptomic studies indicate that microglia display APOE priming and senescence in patients with LOAD. Olah et al. found that transcriptomic clusters 7, 8, and 4 were particularly enriched in patients with LOAD vs controls95. All three microglial clusters upregulated APOE; aged and APOE-primed microglial states may represent transcriptomic cluster 7, where microglial states in clusters 8 and 4 further displayed increased ferritin in FTH1 and FTL95. As TREM2-involved phagoptosis is predicted to jointly induce microglial senescence and a DAM2(-like) microglial transcriptome82, cluster 8 microglia may speculatively represent newly-senescent microglia having uptaken hp-tau aggregates.
Cluster 4 microglia were enriched in multiple IRF transcription factors95 that suggest increased type I IFN signaling. Type I IFN signaling and synaptic loss are likely mediated via senescent microglia72,96,97, and are associated with plaque-associated microglia in samples from patients with LOAD72. An increased type I IFN release may sustain pro-inflammatory microglial reactions specifically to Aβ pathology. As senescent cells uniquely upregulate ferritin indicating iron accumulation12,13, senescent microglia may be enriched in LOAD. P301S and P301L mouse microglial transcriptomic signatures presenting cell cycle inhibition and type I IFN upregulation were also preserved in prefrontal and temporal cortex samples from patients with LOAD68. Genes enriched in type I IFN signaling were additionally upregulated and positively correlated with increasing Braak staging in parahippocampal gyri samples from patients with LOAD72.
A microglial population enriched in samples from patients with LOAD was also validated transcriptionally and via immunohistochemistry, exhibiting increased ferritin FTH and FTL expression, association with neurofibrillary pathology and particularly neuritic plaques, and a dystrophic morphology suggesting senescence98. This “dystrophic” microglial population was speculated to represent an “end result” microglial state responding to Aβ accumulation; these Aβ-responding microglia also upregulated APOE98. Finally, multiple microglial clusters were enriched in prefrontal cortex samples from patients with LOAD vs controls, demonstrating upregulated genes related to cellular senescence, including IRF transcription factors and FTH1/FTL99.
Box 2: Changes in microglial priming, ramified morphology, and phagoptosis relevant to LOAD.
While microglia in homeostatic states often display a ramified morphology, this morphological state does not always coincide with homeostatic functions in humans. Pro-inflammatory lipopolysaccharide induces a complex, hyper-ramified morphology in human microglial cells in-vitro124. Pro-inflammatory microglial states are also not necessarily equivalent to the “reactive” or hypertrophic, ameboid-shaped microglia containing phagocytic inclusions and clustering around neuritic plaques in samples from patients with LOAD;88,110,123 however, ameboid or hypertrophic morphologies can suggest that human microglia have phagocytosed extracellular materials88,110. This hypertrophic appearance is likely observed regardless of the microglia’s inflammatory status, as later discussed.
In normal physiological conditions, mouse microglia utilize TREM2 in phagocytosing synapses and whole neurons during CNS development, plasticity, and maintenance26,42. While homeostatic microglia can phagocytose compartments from dead neurons to optimize the surrounding environment, they can also phagocytose neurons that are stressed but not yet apoptotic. This process is referred to as “phagoptosis”, a premature, non-apoptotic death through microglial phagocytosis24,25. Mechanistically, oxidative stress exposes PS at the neuron’s outer cellular membrane to act as a ligand. Simultaneously, microglia reacting to pro-inflammatory stimuli produce sialidase that removes or “desialylates” neuronal sialic acids24,25. While sialic acids protect neurons from being phagocytosed24,25, microglia enter pro-inflammatory states more frequently during aging. Thus, aging likely renders neurons more susceptible to phagoptosis. Microglia in pro-inflammatory states may not directly partake in phagoptosis while secreting pro-inflammatory cytokines, but the resulting increases in oxidative stress may “prime” homeostatic microglia to phagoptose neurons. Exposure to extracellular hp-tau aggregates and generation of intracellular hp-tau complexes, respectively, could also prompt neurons to expose outer PS75,76.
Once neuronal PS is sufficiently exposed, extracellular opsonin proteins can coat outer PS and induce phagoptotic death by microglia24,25. This process occurs via multiple ligand–receptor pairs that converge into the DAP12/TYROBP/KARAP pathway, stimulating downstream signaling and subsequent phagocytosis through the TAM receptor tyrosine kinases Mer and Axl24,25. Specific pathways leading into phagoptosis and DAP12 signaling include TREM2-PS direct binding, or TREM2 binding to an extracellular APOE-PS complex25,43–45,142. Complement C1q is another opsonin that coats PS, allowing for subsequent C3b, iC3b complement binding and phagoptosis by CR1/CR3/CR4 complement receptors25. These complement receptors trigger downstream DAP12 signaling in microglia24,25. A separate pathway involves binding of the calreticulin opsonin to C1q, resulting in the phagoptosis of neurons by microglial LRP1, together with the induction of more pro-inflammatory, microglial responses3,25.
In mice, homeostatic microglial states can phagoptose neurons and correspondingly exhibit a neurodegeneration/disease-associated microglial state (DAM or MGnD)82,83. The transcriptome includes an initial DAM1 state, involving APOE upregulation independently of phagoptosis activation, and a subsequent DAM2 state; DAM2 necessitates TREM2-dependent phagoptosis, and further upregulates APOE and ITGAX relating to the CR4 subunit CD11c82. Further DAM2 substates were identified, with a pro-inflammatory substate upregulating the Kv1.3 channel protein mediating increased RONS and pro-inflammatory cytokine release83. Dark microglia represent another relevant state, observed using electron microscopy in mouse models of chronic stress, aging and Aβ pathology, as well as in aging individuals and patients with schizophrenia119,143. While more research is warranted to study this association, dark microglia display ultrastructural markers of oxidative stress and lipofuscin related to senescence. These cells could hypothetically participate in phagoptosis; dark microglia have increased phagocytic inclusions and commonly enwrap processes around shrunken, but still viable neuronal elements119.
Predicted features of senescent microglia in LOAD
Patients with LOAD present dystrophic microglia88,100–102. While dystrophic microglia have been scored with different criteria, we will define an exclusive set of criterion for dystrophic microglia as a minimum requirement of (i) ferritin enrichment and (ii) progressive reduction in microglial process complexity; additional signs of (iii) spheroidal swellings and (iv) cytoplasmic deterioration in human dystrophic microglia likely only occur in advanced and/or late-stage dystrophy70,102–104. Dystrophic microglia associate with and precede NFT pathology following Braak staging88,100–102. These microglia not only increase in numbers over aging, but also in differing types of dementias vs age-matched healthy controls, notably in the hippocampus104,105.
In samples from patients with LOAD, dystrophic microglia lacking extremely hypertrophic somas (linked to increased reactivity) associate with neuritic plaques, neurofibrillary tangles, and dystrophic neurites positive for hp-tau even in the absence of Aβ aggregates100,106. Dystrophic microglia also contain hp-tau in aged tree shrews107, and are thus considered to correlate well with neurofibrillary burden108. Dystrophic microglia showing extreme hypertrophy or “ameboid” shapes associate with neuritic plaques in humans and marmosets;88,109 hypertrophic microglia clustering around neuritic plaques were observed in prefrontal cortex samples from patients with LOAD; where clustering hypertrophic and dystrophic microglia were speculated to reflect the preclinical to clinical LOAD transition88. This complements examinations of parahippocampal cortex samples from patients with LOAD, where microglia were concluded to transform from a “primed” or ramified appearance into hypertrophic or ameboid morphologies nearby neuritic plaques110. When microglia were investigated with a semi-quantitative “dystrophy” score, samples from the left anterior frontal and temporal lobes of patients with LOAD vs controls featured increased microglial dystrophy104.
Potential heterogeneity of microglial senescence remains to be rigorously confirmed with multiple markers in clinical LOAD. Nonetheless, dystrophic microglia in samples from patients with LOAD present increased APOE, ferritin expression, and iron accumulation, suggesting they are senescent98,102,105,107,111,112. Notably, senescent cells selectively uptake and accumulate iron;12,13 microglia do not normally accumulate iron105. Primary mouse and SV40 human microglial cells exposed to high iron display a dystrophic morphology, iron accumulation, and became ineffective at phagocytosing Aβ103,113. This indicates that iron accumulation could causally induce microglial dystrophy. Both neuritic plaques and NFTs contain hp-tau-positive inclusions1,2. Since dystrophic microglial abundance and proximity are correlated well with this neurofibrillary pathology100, dystrophic microglia are likely senescent due to significant hp-tau exposure.
In a neuron-specific P301S human tauopathy model, mouse microglia exposed to hp-tau did not display beaded processes observed in human dystrophic microglia; they instead presented lysosomal swellings with hp-tau inclusions and reduced morphological complexity indicating dystrophy102,114. In-vivo mouse microglia exposed to hp-tau from LOAD patient tissue upregulated ferritin and displayed reduced morphological complexity and process length70. Multiple senescent cell types contain altered lysosomes with larger sizes, higher counts, and decreased function7. In a neuronal VPS35-knockout mouse model, increased APOE levels positively correlated with Iba1 levels indicating increased microglial reactivity. When assessing this reactivity in-situ, microglial dystrophy and endosome swelling were observed (indicating failure to break down products and endolysosomal impairment)115. Furthermore, this mouse model demonstrated increased ex-vivo tau secretion from neurons116. This reinforces that hp-tau may induce APOE upregulation, resulting in microglia with dystrophic and senescence traits.
Neumann et al. investigated brain samples from aged individuals categorized under Braak I-V, and quantified Iba1+ cell proportions positive for senescence markers across multiple brain regions; Iba1 staining was used to visualize microglial morphology and categorize these cells as dystrophic117. While proportions of Iba1+ dystrophic microglia displaying each senescence marker were not mentioned, several markers associated with senescence (lipofuscin accumulation, γ-H2AX upregulation, and lamin B1 downregulation7) were not concluded as overrepresented in human Iba1+ dystrophic vs ramified microglia117. It should be noted that senescent cells likely have high heterogeneity in their marker expression dependent on local environment, cell type, state and sub-state(s)7. These authors observed both dystrophic Iba1+/ferritin+ microglia and Iba1-/ferritin+ microglia. However, lipofuscin accumulation, γ-H2AX upregulation, and lamin B1 downregulation were not examined in Iba1-/ferritin+ microglia117.
Tischer et al. previously demonstrated that CD68 + inclusions visible in fluorescence microscopy exist between “fragmented” processes from Iba1+ dystrophic microglia118. Correlative light and electron microscopy revealed that these processes were not truly fragmented; rather, Iba1+ dystrophic microglia possessed thin processes devoid of visible Iba1 staining118. Although Iba1 absence in these processes could be due to their thin nature, dystrophic microglia could also exist along a spectrum featuring varying levels of Iba1 downregulation. The dark microglia observed ultrastructurally display decreased Iba1 staining vs non-dark microglia119.
Markers specific to microglial senescence are not yet standardized across the field. As Neumann et al. suggest, Iba1-/ferritin+ microglial states could be senescent and enriched for increased lipofuscin, γ-H2AX positivity, and/or downregulated lamin B1117. As reactive or ameboid morphologies were not examined117, simultaneously dystrophic and senescent microglia per our hypothesis may have been uninvestigated. Such hypertrophic senescent microglia may express some of the investigated senescence markers, based on their putative hypertrophy from numerous phagocytic inclusions (Fig. 3)105,107,112.
Finally, Jin et al. demonstrated that human and mouse dystrophic microglia are ferritin+ and enriched in senescence genes including B2M, ZFP36L1, and genes associated with type I IFN responses70. In-vivo human iPSC-derived microglia grafted into immunodeficient mice and exposed to LOAD samples containing soluble hp-tau displayed upregulated ferritin, interferon transcriptomic markers, and correlated with increased synaptic loss70. This in-vivo hp-tau exposure triggered dystrophic morphologies in human microglia70. As IFNAR knockdown also inhibited development of dystrophic morphologies and upregulated ferritin in these human microglia, even in response to hp-tau, this implies that sustained type I IFN release promotes senescence and iron accumulation in dystrophic microglia70. Senescent microglia likely release type I IFN to facilitate initial inflammation and synaptic loss69,70,72,73, then seed and spread hp-tau aggregates that induce paracrine senescence;77 dystrophic microglia thus may act via multiple mechanisms central in LOAD pathogenesis to promote neurodegeneration.
Neurofibrillary pathology includes neuritic plaque formation and accumulation, which correlates well with Braak staging, cognitive decline, and overall LOAD progression1,120. Neuritic plaques appeared before other hp-tau aggregate types both in human-tau-injected APP knock-in mice and samples from patients with LOAD; in these mice, neuritic plaque tau induced quicker seeding of neuropil threads and NFTs121. Notably, NLRP3 inflammasome staining and enriched gene transcripts related to type I IFN signaling were localized proximal to neuritic plaques in samples from patients with LOAD51,72. In 5xFAD mice, depleting most microglia using CSF1R inhibition reduced neuritic plaque deposition122. As employing smaller CSF1R inhibitor dosages decreased microglial proliferation and senescence in APP/PS1 mice89, microglial senescence likely accounts for increased neuritic plaque deposition. APP/PS1 mouse hippocampi featured higher Iba1+/SA-β-gal+ cell (suggesting senescent microglia) proportions around Aβ plaques vs wild-type controls89. More Iba1+ cells also stained for p16INK4+/p21+ and surrounded Aβ plaques in temporal cortex samples from patients with LOAD vs control subjects without dementia89.
Because dystrophic microglia are likely senescent and specifically associated with hp-tau pathology, we propose that these cells critically advance LOAD progression and Braak staging. Particularly, dystrophic and hypertrophic microglia associating with neuritic plaques are predicted to correspond with “plaque-associated” microglia. In LOAD, “plaque-associated” microglia are classified based on neuritic plaque appearance; human microglia in samples from patients with LOAD do not significantly associate with non-neuritic, diffuse amyloid plaques123.
Here, we posit that primed microglia observed in patients with LOAD initially comprise a (hyper-)ramified morphology124. After endocytosing hp-tau aggregates locally or via phagoptosis, senescent microglia proposedly adopt a state “A” with dystrophic features characterized by ferritin upregulation, increased type I IFN signaling, and reduced morphological process complexity70 (Fig. 3). These dystrophic microglia may further display Iba1 loss117. As senescent microglia are endolysosomally compromised and ineffective at removing hp-tau neurons77, we propose that senescent microglia may uptake, but fail to effectively degrade Aβ and hp-tau aggregates7,44,77. Continued microglial senescence and impaired endolysosomal function are predicted to neglect neuronal support and permit, if not encourage NFT formation98,100,101,125. This aligns with observations that dystrophic microglia can precede NFT pathology accumulation in LOAD100, while microglial reactivity and synaptic loss occur prior to NFT appearance in P301S mice71.
Dystrophic microglia are predicted to secrete hp-tau aggregates77,126, via exosomes containing hp-tau that are taken up by nearby neurons127,128. As extracellular hp-tau induces PS exposure in neurons76, senescent microglia likely sustain premature neurodegeneration by seeding hp-tau aggregates and triggering local phagoptosis77. Secreted hp-tau oligomers from senescent microglia also likely enter local astrocytes to induce additional paracrine senescence and hp-tau spread64. As aggregated hp-tau increases NLRP3 inflammasome activation and pro-inflammatory cytokine release51,79, senescent microglia could additionally drive indirect hp-tau aggregation via pro-inflammatory reactions50,68,70,79.
State “A” dystrophic microglia likely exacerbate synaptic loss and neurodegeneration through increased type I IFN release and signaling70–73. We predict that they also induce paracrine senescence in nearby microglia attempting to phagocytose and digest Aβ aggregates98. Multiple mechanisms may facilitate Aβ endocytosis, including a strong TREM2-Aβ affinity binding;129 because APOE binds to Aβ oligomers81, actively phagocytosing microglia may endocytose via the TREM2-APOE-Aβ pathway. As “ameboid” or hypertrophic microglia can perform active phagocytosis in humans (Box 2), human hypertrophic microglia busily phagocytosing Aβ proposedly could become senescent via paracrine senescence and hp-tau secretion by state “A” dystrophic microglia;77 the posited outcome is a state “B”, which is dystrophic and hypertrophic and enriched in ferritin (Fig. 3)105,112. State “B” senescent microglia may also display Iba1 loss and enrichment in senescence markers not found in other dystrophic microglial states105,107,112. To provide increased rigor in assessing dystrophy in hypertrophic microglia, future quantitative assessments could investigate ferritin enrichment, potential bulbous swellings, and morphological deterioration within the “reactive” microglial states observed in patients with LOAD and aged marmosets88,98,109,110,112,123.
While both states of senescent microglia likely have type I IFN responses14,70,72,96,97,99, state “B” is predicted to respond to exacerbated Aβ aggregation by upregulating pro-inflammatory cytokine secretion and Kv1.3 expression further exacerbating local inflammation96,103,130,131. This contrasts conditions devoid of Aβ pathology, where microglial senescence states induced by hp-tau exposure do not display extended, pro-inflammatory responses70,77. Senescent microglia may correspond to the transcriptomic cluster 4 per reference95, featuring increased FTH1 and FTL expression implicating iron accumulation and senescence12,13,98,105,112, APOE upregulation, and IRF transcription factors expression corresponding to increased type I IFN release14,72,96,97. In mouse models of Aβ pathology, cluster 4 may further represent a pro-inflammatory, TREM2-dependent DAM2 state observed in response to Aβ pathology83. Notably, TREM2 in hypertrophic and/or dystrophic microglial states could be concomitantly downregulated due to inflammation132.
While non-fibrillar, Aβ secretion may form protective diffuse plaques, we propose that state “B” senescent microglia fail to degrade endocytosed Aβ and instead secrete Aβ-hp-tau aggregates1,49,78–80,133. This agrees with positive correlations of dystrophic microglia density and acidic pH environments across samples from multiple cortical areas in patients with LOAD vs non-demented individuals106,134. Acidic pH may reliably correlate with dystrophic senescent microglia, as (i) human microglia and P301S mouse microglia lysosomes feature hp-tau inclusions70,114, (ii) P301S neuron and mouse microglial co-cultures result in hp-tau seeds being secreted by senescent microglia77, and (iii) mouse microglia can pack phagocytosed Aβ fibrils within lysosomes and secrete acidified Aβ fibrils to build Aβ plaques47. Senescent cell lysosomes also retain an acidic pH7.
As hp-tau spread can induce microglia senescence77, Aβ-hp-tau aggregate secretion is also predicted as specific to senescent microglia47–49,79,135. These secreted Aβ-hp-tau aggregates proposedly coalesce into neuritic plaques with dystrophic neurites via microglial TAM receptors47,110,123. Secreted Aβ-hp-tau aggregates may be deposited into blood vessels and contribute to CAA, indirectly causing LOAD progression136. As plaque-associated or state “B” senescent microglia are predicted to seed hp-tau80, secreted hp-tau and Aβ aggregates may be continuously uptaken by nearby microglia attempting to contain AD pathology spread3. This compensatory response may induce further microglial senescence77,98, neuritic plaque formation, and higher senescent microglia counts around neuritic plaques within localized areas89. “Plaque-associated” microglial clustering seen in LOAD is proposed to emerge here due to a positive feedback loop of likely paracrine senescence, aggregate seeding, and neuritic plaque formation by several state “B” senescent microglia88,98,110,123. Exacerbated Aβ and hp-tau seeding may induce further astrocyte and OPC senescence proximal to neuritic plaques (Fig. 2).
As neuritic plaques precede and seed neuropil thread and NFT formation121, senescent microglia and neuritic plaques are predicted to drive both hp-tau spread and cognitive decline in LOAD. Senescent microglia are putatively responsible for sustained Aβ, hp-tau, and inflammatory increases beyond a tolerance limit likely dependent on each individual’s physiology. In an aging CNS milieu, the accumulation of senescent microglia is posited to determine overall LOAD progression1,50,51,79,110,123,125,137. Microglia can additionally proliferate in response to accumulated Aβ pathology48, which can further accelerate transitions towards senescence through telomere shortening5,6,20,89. This mechanism may independently generate senescent microglia that exacerbate Aβ pathology, local inflammation, and hp-tau secretion, indirectly increasing senescent microglia accumulation and hp-tau spread. However, while Aβ aggregation, DNA damage and other triggers may contribute to microglial senescence via replicative senescence or oxidative stress20,89, APP-overexpressing mouse models feature relatively decreased hp-tau pathology and senescent microglia abundance56,77,89. While encouraging experimental validation, this hypothesis reinforces that hp-tau aggregate uptake is likely specific and central towards triggering microglial senescence, neurofibrillary pathology, and ultimately LOAD progression48,100,114,126,127,138.
Microglial senescence likely occurs over one’s lifespan, but is not exclusive to LOAD; senescent microglia could be underrepresented or overrepresented among specific brain regions unrelated to Braak staging. We specifically propose here that buildup and decreased clearance of senescent microglia, within Braak staging-relevant regions, putatively underlie LOAD progression. Furthermore, although immune cells that include microglia can phagocytose and remove senescent cells42, immunosenescence also builds up over aging and likely predisposes a tissue environment for increased glial senescence burden5,18 (Fig. 2). As microglia are innate immune cells, microglial senescence may act as both (i) a final requirement for Braak staging progression and cognitive decline, and (ii) a final maladaptive form of immunosenescence. In LOAD, microglial clustering, presumed formation of neuritic plaques, and extreme hypertrophy among the prefrontal cortex emerge together with the clinical presentation around Braak stages III–IV1,125. Senescent microglia are thus predicted to actively accelerate hp-tau seeding and the build-up of neuritic plaques tipping preclinical LOAD into clinical progression121,133.
We hypothesize overall that buildup and clustering of senescent microglia (i) exacerbates accumulation of Aβ and neurofibrillary pathology, (ii) increases synaptic loss, pro-inflammatory glial responses, and paracrine senescence, and (iii) facilitates local neurodegenerative spread that results in clinical LOAD progression (Fig. 2)52,137. Microglial clustering around neuritic plaques can happen in local areas before any major neurodegeneration;88,106 samples from patients with LOAD demonstrated more microglial hypertrophy and clustering in relatively-spared primary motor cortex vs severely-affected inferior temporal cortex106. We thus predict that local increases in dystrophic microglia and their cumulative effects, including paracrine senescence, may vary between individuals and shape the heterogeneous progression of Braak staging in LOAD1,137.
Finally, we predict that the accumulation of senescent glia and dystrophic microglia differentiates the outcome between patients with LOAD vs resilient individuals with significant AD pathology, and healthy individuals without notable AD pathology52.
Conclusion
In this perspective, we hypothesize that for healthy cognition to transition into MCI and LOAD diagnosis, (i–ii) aging eventually leads into AD pathology buildup that (iii) induces initial glial senescence, where (iv) subsequent paracrine senescence results in a positive feedback loop between all components (i–iv) (Figs. 1, 3). Localized paracrine senescence may vary individually and partially underlie the heterogeneous progression of LOAD1,137. Local, senescent microglia accumulation represents a central consideration in understanding and treating LOAD. Particularly, we predict that patients with LOAD progress into dementia due to senescent glia, dystrophic microglia, and neuritic plaque burden; we propose that dystrophic microglia burden is minimized in resilient individuals with significant AD pathology and healthy individuals without notable AD pathology52. As everyone has a unique cognitive reserve formed through individual physiology, genetics, and environmental experiences, a differing threshold number of senescent microglia may be needed to overwhelm each person’s cognitive reserve. An absolute number of dystrophic and senescent microglia within regions specific to Braak staging may insufficiently cause LOAD in one individual, yet possibly drive dementia progression in another.
Although this hypothesis is compatible with current LOAD explanations, our speculations and predictions should be rigorously assessed for validation or rejection. As we have not covered endothelial cell senescence and blood–brain barrier leakage, other LOAD risk factors, and potential contributions of senescent glia in mixed dementias and co-morbidities, this hypothesis can be expanded upon with future and independent reviews. We also focus on LOAD here, but mutations responsible for EOAD may involve quicker microglial senescence through exhaustion. Particularly, TREM2 R47H microglia may have decreased metabolic capacity to rapidly clear out Aβ and consequent hp-tau buildup in EOAD20,139. Conjecturally, mutations could make it harder for immune cells to clear out senescent microglial accumulation over aging5. Peripheral immune cells, including those in the innate and adaptive immune systems, may also become senescent and contribute to LOAD. There is currently insufficient evidence that infiltrating, non-macrophage populations become senescent and contribute towards AD pathology buildup and spread. It is, however, possible that dystrophic “microglia” (based on markers used to study them) can comprise both yolk-sac derived resident microglia and monocyte-derived macrophages infiltrating the CNS.
Senescent glia, including dystrophic microglia, likely comprise diverse morphologies and molecular signatures. As measuring these morphological and molecular states is not currently standardized across the field, we recommend confirming or rejecting the current framework by assessing microglial senescence in samples from patients with LOAD using multiple methods: ferritin enrichment, iron accumulation, acidic pH and/or SA-β-gal quantification, upregulated gene modules implicating senescence, and lipofuscin accumulation associated with state “B” microglia5,7,89. We also argue that a more universal criteria for dystrophic microglia should be incorporated, utilizing the criteria we proposed (when emphasizing measuring heterogeneity in dystrophy): (i) sustained ferritin enrichment, (ii) reduced process complexity, and optional indications of advanced dystrophy in (iii) spheroidal swellings and (iv) cytoplasmic deterioration especially in humans70,102–104. Although not methodologically feasible yet, strongly rejecting our hypothesis would involve tracking over time cognitive decline and potential increases in dystrophic microglia burden within the same individuals. We believe that this perspective currently offers explanatory power concerning possible dystrophic and senescent microglial contributions to AD pathology70,72,73,77,88,99,100,105,111, and hope that it will potentially shape future, therapeutic efforts for LOAD.
AD pathology is often co-morbid with other dementias and tauopathies1. Solutions targeting senescent glia in LOAD may likely target other disease outcomes; co-morbid pathologies may further involve independent mechanisms inducing glial cell senescence. Positron emission tomography imaging also supports that tau seeding occurs locally from Braak stages III+137. Thus, treating hp-tau seeding via potential senescent microglia targeting may also promote cognitive health along healthy aged individuals, by preventing MCI and age-related, neurodegenerative diseases. If this hypothesis is correct, increasing glial senescence could potentially account for negative previous clinical trial outcomes. As previous clinical trial candidates have not directly killed senescent glia, these treatments were likely unable to significantly halt the AD pathology accumulation sustained by senescent glia buildup. A specific solution towards treating LOAD is encouraged here through senolytics, or drugs that selectively kill senescent cells (Fig. 4)140. Successful senolytic administration is expected to treat the accelerated, traditional AD pathology burden caused by senescent glia, hopefully allowing renewal and recovery of remaining brain parenchyma to increase the quality of life in affected individuals. Using senolytics to treat MCI or early to mid-stage dementia prognosis would directly test our hypothesis, as senescent cell removal is predicted to halt the different proposed, pathological mechanisms propagated by senescent glia.
Fig. 4. Killing senescent glia to treat Alzheimer’s disease.
Building on evidence collected from studies involving mouse models, we conceptually provide a hypothesized outcome of using senolytics to treat Alzheimer’s disease (AD). Senolytics are drugs that selectively kill senescent cells, and were shown to reduce cognitive decline in disease mouse models. If senescent glia sustain synaptic loss and accumulation of the main AD pathologies, senolytics are predicted to provide a best chance for optimal outcomes in individuals with subjective cognitive decline, mild cognitive impairment, and early to mid-stage dementia. Alternatively put, senolytic interventions may best target earlier timepoints across the cognitive aging axis when one has a larger brain reserve, as late-stage AD may have already resulted in too much neurodegeneration and cell death. Remaining glial populations are predicted to repopulate and renew glial homeostatic functions to effectively clear out and reduce main AD pathologies, as reduced senescent glia counts should critically reduce AD pathology accumulation. Resulting plasticity should hopefully revert the aging brain back to a healthy cognition or preclinical late-onset AD (LOAD) state; minimally, we predict that optimized senolytic treatments can halt further LOAD progression at least transiently after administration. We also highly support the combination of other pharmacological and non-pharmacological treatment strategies with senolytics. This would hypothetically allow for better restoring of glial homeostatic functions, and would minimize damage accrued by pro-inflammatory glial states and other AD pathologies. The question mark denotes that it is currently unknown whether disease-associated microglial states are targeted by senolytics. Figure created with BioRender.com.
If senolytics alone are insufficient for stopping LOAD, we predict still that senolytics are necessary as co-treatment with other therapeutics. As senescent cells display apoptosis resistance7, probable senescent glia-mediated contributions to AD pathologies likely cannot be targeted only with non-senolytics. Albeit, sole senolytic administration has successfully treated and prevented cognitive impairment in tauopathy, amyloid, and aged mouse models15,39,56,91. Senolytics dasatinib and quercetin have also succeeded at eliminating senescent cells for patients with diabetic kidney disease141. This purports hope for treating LOAD as a neurodegenerative disease of aging, likely advanced by microglial senescence.
Acknowledgements
As part of the University of Victoria, we acknowledge and respect the lək̓ʷəŋən peoples on whose traditional territory the university stands and the Songhees, Esquimalt and W̱SÁNEĆ peoples whose historical relationships with the land continue to this day. V.Z.L. is supported by a CIHR graduate student award—master and graduate award scholarships from the Faculty of Graduate Studies, University of Victoria. M.E.T. is a Tier II Canada Research Chair in Neurobiology of Aging and Cognition. Both V.Z.L. and M.E.T. are also supported by a CIHR Joint Canada-Israel Health Research Phase II grant.
Author contributions
V.Z.L. led the article conceptualization, manuscript writing, and figure creation; V.Z.L., L.M.R., and M.E.T. critically discussed the content and contributed to editing and revising the manuscript.
Peer review
Peer review information
Nature Communications thanks the anonymous reviewer(s) for their contribution to the peer review of this work.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Victor Lau, Email: vzplau@gmail.com.
Leanne Ramer, Email: lramer@sfu.ca.
Marie-Ève Tremblay, Email: evetremblay@uvic.ca.
References
- 1.DeTure MA, Dickson DW. The neuropathological diagnosis of Alzheimer’s disease. Mol. Neurodegener. 2019;14:32. doi: 10.1186/s13024-019-0333-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tönnies E, Trushina E. Oxidative stress, synaptic dysfunction, and Alzheimer’s disease. J. Alzheimers Dis. 2017;57:1105. doi: 10.3233/JAD-161088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Long JM, Holtzman DM. Alzheimer disease: an update on pathobiology and treatment strategies. Cell. 2019;179:312–339. doi: 10.1016/j.cell.2019.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Milionis HJ, Florentin M, Giannopoulos S. Metabolic syndrome and Alzheimer’s disease: a link to a vascular hypothesis? CNS Spectr. 2008;13:606–613. doi: 10.1017/S1092852900016886. [DOI] [PubMed] [Google Scholar]
- 5.Guerrero A, De Strooper B, Arancibia-Cárcamo IL. Cellular senescence at the crossroads of inflammation and Alzheimer’s disease. Trends Neurosci. 2021;S0166-2236:00119–3. doi: 10.1016/j.tins.2021.06.007. [DOI] [PubMed] [Google Scholar]
- 6.Saez-Atienzar S, Masliah E. Cellular senescence and Alzheimer disease: the egg and the chicken scenario. Nat. Rev. Neurosci. 2020;21:433–444. doi: 10.1038/s41583-020-0325-z. [DOI] [PubMed] [Google Scholar]
- 7.Gorgoulis V, et al. Cellular senescence: defining a path forward. Cell. 2019;179:813–827. doi: 10.1016/j.cell.2019.10.005. [DOI] [PubMed] [Google Scholar]
- 8.Fielder E, von Zglinicki T, Jurk D. The DNA damage response in neurons: die by apoptosis or survive in a senescence-like state? J. Alzheimers Dis. 2017;60:S107–S131. doi: 10.3233/JAD-161221. [DOI] [PubMed] [Google Scholar]
- 9.Barascu A, et al. Oxidative stress induces an ATM-independent senescence pathway through p38 MAPK-mediated lamin B1 accumulation. EMBO J. 2012;31:1080–1094. doi: 10.1038/emboj.2011.492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Acosta JC, et al. A complex secretory program orchestrated by the inflammasome controls paracrine senescence. Nat. Cell Biol. 2013;15:978–990. doi: 10.1038/ncb2784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Freund A, Orjalo AV, Desprez P-Y, Campisi J. Inflammatory networks during cellular senescence: causes and consequences. Trends Mol. Med. 2010;16:238. doi: 10.1016/j.molmed.2010.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Killilea DW, Wong SL, Cahaya HS, Atamna H, Ames BN. Iron accumulation during cellular senescence. Ann. N.Y. Acad. Sci. 2004;1019:365–367. doi: 10.1196/annals.1297.063. [DOI] [PubMed] [Google Scholar]
- 13.Masaldan S, et al. Iron accumulation in senescent cells is coupled with impaired ferritinophagy and inhibition of ferroptosis. Redox Biol. 2018;14:100–115. doi: 10.1016/j.redox.2017.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yang H, Wang H, Ren J, Chen Q, Chen ZJ. cGAS is essential for cellular senescence. Proc. Natl. Acad. Sci. U.S.A. 2017;114:E4612. doi: 10.1073/pnas.1705499114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ogrodnik, M. et al. Whole‐body senescent cell clearance alleviates age‐related brain inflammation and cognitive impairment in mice. Aging Cell20, e13296 (2021). Ogrodnik et al. (2021) demonstrate that systemic administration of two different senolytics improves spatial memory in p16INK4A-overexpressing aged mice, while also decreasing SASP factors expression and brain inflammation relevant to senescent cells. [DOI] [PMC free article] [PubMed]
- 16.Xu M, et al. Senolytics improve physical function and increase lifespan in old age. Nat. Med. 2018;24:1246. doi: 10.1038/s41591-018-0092-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang X, et al. Rejuvenation of the aged brain immune cell landscape in mice through p16-positive senescent cell clearance. Nat. Commun. 2022;13:5671. doi: 10.1038/s41467-022-33226-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fulop, T. et al. Immunosenescence and Alzheimer’s Disease. in Healthy Longevity and Immune System (eds. Bueno, V. & Pawelec, G.) 177–199 (Springer International Publishing, 2022). 10.1007/978-3-030-87532-9_9.
- 19.Walton CC, Begelman D, Nguyen W, Andersen JK. Senescence as an amyloid cascade: the amyloid senescence hypothesis. Front. Cell. Neurosci. 2020;14:129. doi: 10.3389/fncel.2020.00129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Flanary BE, Sammons NW, Nguyen C, Walker D, Streit WJ. Evidence that aging and amyloid promote microglial cell senescence. Rejuvenation Res. 2007;10:61–74. doi: 10.1089/rej.2006.9096. [DOI] [PubMed] [Google Scholar]
- 21.Liguori I, et al. Oxidative stress, aging, and diseases. Clin. Interv. Aging. 2018;13:757. doi: 10.2147/CIA.S158513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Morley JE, Baumgartner RN. Cytokine-related aging process. J. Gerontol. Ser. A. 2004;59:M924–M929. doi: 10.1093/gerona/59.9.M924. [DOI] [PubMed] [Google Scholar]
- 23.Kadowaki H, et al. Amyloid β induces neuronal cell death through ROS-mediated ASK1 activation. Cell Death Differ. 2005;12:19–24. doi: 10.1038/sj.cdd.4401528. [DOI] [PubMed] [Google Scholar]
- 24.Brown GC, Neher JJ. Microglial phagocytosis of live neurons. Nat. Rev. Neurosci. 2014;15:209–216. doi: 10.1038/nrn3710. [DOI] [PubMed] [Google Scholar]
- 25.Butler CA, et al. Microglial phagocytosis of neurons in neurodegeneration, and its regulation. J. Neurochem. 2021;158:621–639. doi: 10.1111/jnc.15327. [DOI] [PubMed] [Google Scholar]
- 26.Hsieh CL, et al. A role for TREM2 ligands in the phagocytosis of apoptotic neuronal cells by microglia. J. Neurochem. 2009;109:1144. doi: 10.1111/j.1471-4159.2009.06042.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Testa G, et al. Changes in brain oxysterols at different stages of Alzheimer’s disease: their involvement in neuroinflammation. Redox Biol. 2016;10:24. doi: 10.1016/j.redox.2016.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gamba, P. et al. Oxidized cholesterol as the driving force behind the development of Alzheimer’s disease. Front. Aging Neurosci. 7, (2015). [DOI] [PMC free article] [PubMed]
- 29.Song, L., Pei, L., Yao, S., Wu, Y. & Shang, Y. NLRP3 inflammasome in neurological diseases, from functions to therapies. Front. Cell. Neurosci. 11, 63 (2017). [DOI] [PMC free article] [PubMed]
- 30.Allen NJ, Lyons DA. Glia as architects of central nervous system formation and function. Science. 2018;362:181. doi: 10.1126/science.aat0473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chesser, A., Pritchard, S. & Johnson, G. Tau clearance mechanisms and their possible role in the pathogenesis of Alzheimer disease. Front. Neurol. 4, 122 (2013). [DOI] [PMC free article] [PubMed]
- 32.Yoon S-S, Jo SA. Mechanisms of amyloid-β peptide clearance: potential therapeutic targets for Alzheimer’s disease. Biomol. Ther. 2012;20:245–255. doi: 10.4062/biomolther.2012.20.3.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhang S, et al. NG2 glia regulate brain innate immunity via TGF-β2/TGFBR2 axis. BMC Med. 2019;17:204. doi: 10.1186/s12916-019-1439-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Liu Y, Aguzzi A. NG2 glia are required for maintaining microglia homeostatic state. Glia. 2020;68:345–355. doi: 10.1002/glia.23721. [DOI] [PubMed] [Google Scholar]
- 35.Tichauer JE, et al. Age-dependent changes on TGFβ1 Smad3 pathway modify the pattern of microglial cell activation. Brain. Behav. Immun. 2014;37:187. doi: 10.1016/j.bbi.2013.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Limbad C, et al. Astrocyte senescence promotes glutamate toxicity in cortical neurons. PLOS ONE. 2020;15:e0227887. doi: 10.1371/journal.pone.0227887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Willis CM, et al. Astrocyte support for oligodendrocyte differentiation can be conveyed via extracellular vesicles but diminishes with age. Sci. Rep. 2020;10:828. doi: 10.1038/s41598-020-57663-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Turnquist C, et al. p53 isoforms regulate astrocyte-mediated neuroprotection and neurodegeneration. Cell Death Differ. 2016;23:1515–1528. doi: 10.1038/cdd.2016.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhang P, et al. Senolytic therapy alleviates Aβ-associated oligodendrocyte progenitor cell senescence and cognitive deficits in an Alzheimer’s disease model. Nat. Neurosci. 2019;22:719–728. doi: 10.1038/s41593-019-0372-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shi Y, et al. Microglia drive APOE-dependent neurodegeneration in a tauopathy mouse model. J. Exp. Med. 2019;216:2546–2561. doi: 10.1084/jem.20190980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.McAlpine CS, et al. Astrocytic interleukin-3 programs microglia and limits Alzheimer’s disease. Nature. 2021;595:701–706. doi: 10.1038/s41586-021-03734-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Scott-Hewitt N, et al. Local externalization of phosphatidylserine mediates developmental synaptic pruning by microglia. EMBO J. 2020;39:e105380. doi: 10.15252/embj.2020105380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wang Y, et al. TREM2 lipid sensing sustains microglia response in an Alzheimer’s disease model. Cell. 2015;160:1061. doi: 10.1016/j.cell.2015.01.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Atagi Y, et al. Apolipoprotein E is a ligand for triggering receptor expressed on myeloid cells 2 (TREM2) J. Biol. Chem. 2015;290:26043. doi: 10.1074/jbc.M115.679043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Shirotani K, et al. Aminophospholipids are signal-transducing TREM2 ligands on apoptotic cells. Sci. Rep. 2019;9:7508. doi: 10.1038/s41598-019-43535-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zhao Y, et al. TREM2 is a receptor for β-amyloid which mediates microglial function. Neuron. 2018;97:1023. doi: 10.1016/j.neuron.2018.01.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Huang Y, et al. Microglia use TAM receptors to detect and engulf amyloid β plaques. Nat. Immunol. 2021;22:586–594. doi: 10.1038/s41590-021-00913-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rodríguez JJ, Witton J, Olabarria M, Noristani HN, Verkhratsky A. Increase in the density of resting microglia precedes neuritic plaque formation and microglial activation in a transgenic model of Alzheimer’s disease. Cell Death Dis. 2010;1:e1. doi: 10.1038/cddis.2009.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Venegas C, et al. Microglia-derived ASC specks cross-seed amyloid-β in Alzheimer’s disease. Nature. 2017;552:355–361. doi: 10.1038/nature25158. [DOI] [PubMed] [Google Scholar]
- 50.Ising C, et al. NLRP3 inflammasome activation drives tau pathology. Nature. 2019;575:669. doi: 10.1038/s41586-019-1769-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ahmed ME, et al. Co-localization of glia maturation factor with NLRP3 inflammasome and autophagosome markers in human Alzheimer’s disease brain. J. Alzheimers Dis. 2017;60:1143. doi: 10.3233/JAD-170634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Taddei RN, et al. Changes in glial cell phenotypes precede overt neurofibrillary tangle formation, correlate with markers of cortical cell damage, and predict cognitive status of individuals at Braak III-IV stages. Acta Neuropathol. Commun. 2022;10:72. doi: 10.1186/s40478-022-01370-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Niraula A, Sheridan JF, Godbout JP. Microglia priming with aging and stress. Neuropsychopharmacology. 2017;42:318. doi: 10.1038/npp.2016.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Verkhratsky A, Zorec R, Rodriguez-Arellano JJ, Parpura V. Neuroglia in ageing. Adv. Exp. Med. Biol. 2019;1175:181. doi: 10.1007/978-981-13-9913-8_8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wegmann S, et al. Experimental evidence for the age dependence of tau protein spread in the brain. Sci. Adv. 2019;5:eaaw6404. doi: 10.1126/sciadv.aaw6404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bussian TJ, et al. Clearance of senescent glial cells prevents tau-dependent pathology and cognitive decline. Nature. 2018;562:578–582. doi: 10.1038/s41586-018-0543-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Xie Y-Y, et al. Clemastine ameliorates myelin deficits via preventing senescence of oligodendrocytes precursor cells in Alzheimer’s disease model mouse. Front. Cell Dev. Biol. 2021;9:733945. doi: 10.3389/fcell.2021.733945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Papuć E, Rejdak K. The role of myelin damage in Alzheimer’s disease pathology. Arch. Med. Sci. 2018;16:345–351. doi: 10.5114/aoms.2018.76863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Chacon-De-La-Rocha I, et al. Accelerated dystrophy and decay of oligodendrocyte precursor cells in the APP/PS1 model of Alzheimer’s-Like pathology. Front. Cell. Neurosci. 2020;14:383. doi: 10.3389/fncel.2020.575082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Nicaise AM, et al. Cellular senescence in progenitor cells contributes to diminished remyelination potential in progressive multiple sclerosis. Proc. Natl. Acad. Sci. 2019;116:9030–9039. doi: 10.1073/pnas.1818348116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lautrup S, Sinclair DA, Mattson MP, Fang EF. NAD+ in brain aging and neurodegenerative disorders. Cell Metab. 2019;30:630–655. doi: 10.1016/j.cmet.2019.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hou Y, et al. NAD+ supplementation reduces neuroinflammation and cell senescence in a transgenic mouse model of Alzheimer’s disease via cGAS–STING. Proc. Natl. Acad. Sci. 2021;118:e2011226118. doi: 10.1073/pnas.2011226118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Bhat, R. et al. Astrocyte senescence as a component of Alzheimer’s disease. PLoS One7, e45069 (2012). [DOI] [PMC free article] [PubMed]
- 64.Gaikwad S, et al. Tau oligomer induced HMGB1 release contributes to cellular senescence and neuropathology linked to Alzheimer’s disease and frontotemporal dementia. Cell Rep. 2021;36:109419. doi: 10.1016/j.celrep.2021.109419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Han, X., Zhang, T., Liu, H., Mi, Y. & Gou, X. Astrocyte senescence and alzheimer’s disease: a review. Front. Aging Neurosci. 12, 148 (2020). [DOI] [PMC free article] [PubMed]
- 66.Raghunatha P, Vosoughi A, Kauppinen TM, Jackson MF. Microglial NMDA receptors drive pro-inflammatory responses via PARP-1/TRMP2 signaling. Glia. 2020;68:1421–1434. doi: 10.1002/glia.23790. [DOI] [PubMed] [Google Scholar]
- 67.Rouillard, M. E. et al. The cellular senescence factor extracellular HMGB1 directly inhibits oligodendrocyte progenitor cell differentiation and impairs CNS remyelination. Front. Cell. Neurosci. 16, 833186 (2022). [DOI] [PMC free article] [PubMed]
- 68.Rexach JE, et al. Tau pathology drives dementia risk-associated gene networks toward chronic inflammatory states and immunosuppression. Cell Rep. 2020;33:108398. doi: 10.1016/j.celrep.2020.108398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Jin M, et al. Tau activates microglia via the PQBP1-cGAS-STING pathway to promote brain inflammation. Nat. Commun. 2021;12:6565. doi: 10.1038/s41467-021-26851-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Jin M, et al. Type-I-interferon signaling drives microglial dysfunction and senescence in human iPSC models of Down syndrome and Alzheimer’s disease. Cell Stem Cell. 2022;29:1135–1153.e8. doi: 10.1016/j.stem.2022.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Yoshiyama Y, et al. Synapse loss and microglial activation precede tangles in a P301S tauopathy mouse model. Neuron. 2007;53:337–351. doi: 10.1016/j.neuron.2007.01.010. [DOI] [PubMed] [Google Scholar]
- 72.Roy ER, et al. Type I interferon response drives neuroinflammation and synapse loss in Alzheimer disease. J. Clin. Investig. 2020;130:1912. doi: 10.1172/JCI133737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Roy, E. R. et al. Concerted type I interferon signaling in microglia and neural cells promotes memory impairment associated with amyloid β plaques. Immunity55, 879–894.e6 (2022). [DOI] [PMC free article] [PubMed]
- 74.Shin J, Park S, Lee H, Kim Y. Thioflavin-positive tau aggregates complicating quantification of amyloid plaques in the brain of 5XFAD transgenic mouse model. Sci. Rep. 2021;11:1617. doi: 10.1038/s41598-021-81304-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Brelstaff J, Tolkovsky AM, Ghetti B, Goedert M, Spillantini MG. Living neurons with tau filaments aberrantly expose phosphatidylserine and are phagocytosed by microglia. Cell Rep. 2018;24:1939. doi: 10.1016/j.celrep.2018.07.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Pampuscenko K, et al. Extracellular tau induces microglial phagocytosis of living neurons in cell cultures. J. Neurochem. 2020;154:e14940. doi: 10.1111/jnc.14940. [DOI] [PubMed] [Google Scholar]
- 77.Brelstaff, J. H. et al. Microglia become hypofunctional and release metalloproteases and tau seeds when phagocytosing live neurons with P301S tau aggregates. Sci. Adv. 7, eabg4980 (2021). Brelstaff et al. (2021) demonstrate that human hp-tau aggregates induce lysosomal dysfunction (via SA-b-gal staining) and senescence in mouse microglia, by phagoptosing neurons with hp-tau (further leaving reduced clearance of these neurons with hp-tau) or uptaking hp-tau secretions from senescent microglia. [DOI] [PMC free article] [PubMed]
- 78.Hopp SC, et al. The role of microglia in processing and spreading of bioactive tau seeds in Alzheimer’s disease. J. Neuroinflammation. 2018;15:269. doi: 10.1186/s12974-018-1309-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Stancu I-C, et al. Aggregated Tau activates NLRP3–ASC inflammasome exacerbating exogenously seeded and non-exogenously seeded Tau pathology in vivo. Acta Neuropathol. 2019;137:599. doi: 10.1007/s00401-018-01957-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Clayton K, et al. Plaque associated microglia hyper-secrete extracellular vesicles and accelerate tau propagation in a humanized APP mouse model. Mol. Neurodegener. 2021;16:18. doi: 10.1186/s13024-021-00440-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Jiang Q, et al. ApoE promotes the proteolytic degradation of Aβ. Neuron. 2008;58:681. doi: 10.1016/j.neuron.2008.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Keren-Shaul H, et al. A unique microglia type associated with restricting development of Alzheimer’s disease. Cell. 2017;169:1276–1290.e17. doi: 10.1016/j.cell.2017.05.018. [DOI] [PubMed] [Google Scholar]
- 83.Rangaraju S, et al. Identification and therapeutic modulation of a pro-inflammatory subset of disease-associated-microglia in Alzheimer’s disease. Mol. Neurodegener. 2018;13:24. doi: 10.1186/s13024-018-0254-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Nugent AA, et al. TREM2 regulates microglial cholesterol metabolism upon chronic phagocytic challenge. Neuron. 2020;105:837–854.e9. doi: 10.1016/j.neuron.2019.12.007. [DOI] [PubMed] [Google Scholar]
- 85.Theendakara V, Peters-Libeu CA, Bredesen DE, Rao RV. Transcriptional effects of ApoE4: relevance to Alzheimer’s disease. Mol. Neurobiol. 2018;55:5243–5254. doi: 10.1007/s12035-017-0757-2. [DOI] [PubMed] [Google Scholar]
- 86.Rohn, T. T. & Moore, Z. D. Nuclear localization of apolipoprotein E4: a new trick for an old protein. Int. J. Neurol. Neurother. 4, 067 (2017). [DOI] [PMC free article] [PubMed]
- 87.Muth, C., Hartmann, A., Sepulveda-Falla, D., Glatzel, M. & Krasemann, S. Phagocytosis of apoptotic cells is specifically upregulated in ApoE4 expressing microglia in vitro. Front. Cell. Neurosci. 13, 181 (2019). [DOI] [PMC free article] [PubMed]
- 88.Streit WJ, et al. Microglial activation occurs late during preclinical Alzheimer’s disease. Glia. 2018;66:2550–2562. doi: 10.1002/glia.23510. [DOI] [PubMed] [Google Scholar]
- 89.Hu Y, et al. Replicative senescence dictates the emergence of disease-associated microglia and contributes to Aβ pathology. Cell Rep. 2021;35:109228. doi: 10.1016/j.celrep.2021.109228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Wang J-Z, Wang Z-H. Senescence may mediate conversion of tau phosphorylation-induced apoptotic escape to neurodegeneration. Exp. Gerontol. 2015;68:82–86. doi: 10.1016/j.exger.2015.03.007. [DOI] [PubMed] [Google Scholar]
- 91.Musi, N. et al. Tau protein aggregation is associated with cellular senescence in the brain. Aging Cell17, e12840 (2018). [DOI] [PMC free article] [PubMed]
- 92.Jurk D, et al. Postmitotic neurons develop a p21-dependent senescence-like phenotype driven by a DNA damage response. Aging Cell. 2012;11:996. doi: 10.1111/j.1474-9726.2012.00870.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Leng K, et al. Molecular characterization of selectively vulnerable neurons in Alzheimer’s disease. Nat. Neurosci. 2021;24:276–287. doi: 10.1038/s41593-020-00764-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Wang, X., Michaelis, E. Selective neuronal vulnerability to oxidative stress in the brain. Front. Aging Neurosci. 2, 12 (2010). [DOI] [PMC free article] [PubMed]
- 95.Olah M, et al. Single cell RNA sequencing of human microglia uncovers a subset associated with Alzheimer’s disease. Nat. Commun. 2020;11:6129. doi: 10.1038/s41467-020-19737-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Nazmi A, et al. Chronic neurodegeneration induces type I interferon synthesis via STING, shaping microglial phenotype and accelerating disease progression. Glia. 2019;67:1254. doi: 10.1002/glia.23592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Moore, Z., Mobilio, F., Walker, F. R., Taylor, J. M. & Crack, P. J. Abrogation of type-I interferon signalling alters the microglial response to Aβ1–42. Sci. Rep. 10, 3153 (2020). [DOI] [PMC free article] [PubMed]
- 98.Nguyen AT, et al. APOE and TREM2 regulate amyloid responsive microglia in Alzheimer’s disease. Acta Neuropathol. 2020;140:477. doi: 10.1007/s00401-020-02200-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Prater, K. et al. Transcriptomically unique endolysosomal and homeostatic microglia populations in Alzheimer’s Disease and aged human brain. https://www.researchsquare.com/article/rs-1836861/v1 (2022) 10.21203/rs.3.rs-1836861/v1.
- 100.Streit WJ, Braak H, Xue Q-S, Bechmann I. Dystrophic (senescent) rather than activated microglial cells are associated with tau pathology and likely precede neurodegeneration in Alzheimer’s disease. Acta Neuropathol. 2009;118:475. doi: 10.1007/s00401-009-0556-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Cras P, Kawai M, Siedlak S, Perry G. Microglia are associated with the extracellular neurofibrillary tangles of Alzheimer disease. Brain Res. 1991;558:312–314. doi: 10.1016/0006-8993(91)90783-R. [DOI] [PubMed] [Google Scholar]
- 102.Streit WJ, Khoshbouei H, Bechmann I. Dystrophic microglia in late-onset Alzheimer’s disease. Glia. 2020;68:845–854. doi: 10.1002/glia.23782. [DOI] [PubMed] [Google Scholar]
- 103.Angelova DM, Brown DR. Altered processing of β-amyloid in SH-SY5Y cells induced by model senescent microglia. ACS Chem. Neurosci. 2018;9:3137–3152. doi: 10.1021/acschemneuro.8b00334. [DOI] [PubMed] [Google Scholar]
- 104.Woollacott IOC, et al. Microglial burden, activation and dystrophy patterns in frontotemporal lobar degeneration. J. Neuroinflammation. 2020;17:234. doi: 10.1186/s12974-020-01907-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Shahidehpour RK, et al. Dystrophic microglia are associated with neurodegenerative disease and not healthy aging in the human brain. Neurobiol. Aging. 2021;99:19–27. doi: 10.1016/j.neurobiolaging.2020.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Paasila, P. J., Davies, D. S., Sutherland, G. T. & Goldsbury, C. Clustering of activated microglia occurs before the formation of dystrophic neurites in the evolution of Aβ plaques in Alzheimer’s disease. Free Neuropathol. 1, 10.17879/freeneuropathology-2020-2845 (2020). [DOI] [PMC free article] [PubMed]
- 107.Rodriguez-Callejas JD, Fuchs E, Perez-Cruz C. Increased oxidative stress, hyperphosphorylation of tau, and dystrophic microglia in the hippocampus of aged Tupaia belangeri. Glia. 2020;68:1775–1793. doi: 10.1002/glia.23804. [DOI] [PubMed] [Google Scholar]
- 108.Swanson MEV, et al. Identification of a dysfunctional microglial population in human Alzheimer’s disease cortex using novel single-cell histology image analysis. Acta Neuropathol. Commun. 2020;8:170. doi: 10.1186/s40478-020-01047-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Rodríguez-Callejas J, et al. Loss of ferritin-positive microglia relates to increased iron, RNA oxidation, and dystrophic microglia in the brains of aged male marmosets. Am. J. Primatol. 2019;81:e22956. doi: 10.1002/ajp.22956. [DOI] [PubMed] [Google Scholar]
- 110.Sheng JG, Mrak RE, Griffin WS. Neuritic plaque evolution in Alzheimer’s disease is accompanied by transition of activated microglia from primed to enlarged to phagocytic forms. Acta Neuropathol. 1997;94:1–5. doi: 10.1007/s004010050664. [DOI] [PubMed] [Google Scholar]
- 111.Lopes KO, Sparks DL, Streit WJ. Microglial dystrophy in the aged and Alzheimer’s disease brain is associated with ferritin immunoreactivity. Glia. 2008;56:1048–1060. doi: 10.1002/glia.20678. [DOI] [PubMed] [Google Scholar]
- 112.Kenkhuis B, et al. Iron loading is a prominent feature of activated microglia in Alzheimer’s disease patients. Acta Neuropathol. Commun. 2021;9:27. doi: 10.1186/s40478-021-01126-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.McIntosh A, et al. Iron accumulation in microglia triggers a cascade of events that leads to altered metabolism and compromised function in APP/PS1 mice. Brain Pathol. 2019;29:606. doi: 10.1111/bpa.12704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.van Olst L, et al. Microglial activation arises after aggregation of phosphorylated-tau in a neuron-specific P301S tauopathy mouse model. Neurobiol. Aging. 2020;89:89–98. doi: 10.1016/j.neurobiolaging.2020.01.003. [DOI] [PubMed] [Google Scholar]
- 115.Qureshi YH, et al. The neuronal retromer can regulate both neuronal and microglial phenotypes of Alzheimer’s disease. Cell Rep. 2022;38:110262. doi: 10.1016/j.celrep.2021.110262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Simoes S, et al. Tau and other proteins found in Alzheimer’s disease spinal fluid are linked to retromer-mediated endosomal traffic in mice and humans. Sci. Transl. Med. 2020;12:eaba6334. doi: 10.1126/scitranslmed.aba6334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Neumann, P., Lenz, D. E., Streit, W. J. & Bechmann, I. Is microglial dystrophy a form of cellular senescence? An analysis of senescence markers in the aged human brain. Glia71, 377–390 (2023). [DOI] [PubMed]
- 118.Tischer J, et al. Inhomogeneous distribution of Iba-1 characterizes microglial pathology in Alzheimer’s disease. Glia. 2016;64:1562–1572. doi: 10.1002/glia.23024. [DOI] [PubMed] [Google Scholar]
- 119.Bisht K, et al. Dark microglia: a new phenotype predominantly associated with pathological states. Glia. 2016;64:826–839. doi: 10.1002/glia.22966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Mufson EJ, Malek-Ahmadi M, Perez SE, Chen K. Braak staging, plaque pathology and APOE status in elderly persons without cognitive impairment. Neurobiol. Aging. 2016;37:147. doi: 10.1016/j.neurobiolaging.2015.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.He Z, et al. Amyloid-β plaques enhance Alzheimer’s brain tau-seeded pathologies by facilitating neuritic plaque tau aggregation. Nat. Med. 2018;24:29–38. doi: 10.1038/nm.4443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Sosna J, et al. Early long-term administration of the CSF1R inhibitor PLX3397 ablates microglia and reduces accumulation of intraneuronal amyloid, neuritic plaque deposition and pre-fibrillar oligomers in 5XFAD mouse model of Alzheimer’s disease. Mol. Neurodegener. 2018;13:11. doi: 10.1186/s13024-018-0244-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Mackenzie IR, Hao C, Munoz DG. Role of microglia in senile plaque formation. Neurobiol. Aging. 1995;16:797–804. doi: 10.1016/0197-4580(95)00092-S. [DOI] [PubMed] [Google Scholar]
- 124.Healy LM, Yaqubi M, Ludwin S, Antel JP. Species differences in immune-mediated CNS tissue injury and repair: a (neuro)inflammatory topic. Glia. 2020;68:811–829. doi: 10.1002/glia.23746. [DOI] [PubMed] [Google Scholar]
- 125.Braak H, Braak E. Frequency of stages of Alzheimer-related lesions in different age categories. Neurobiol. Aging. 1997;18:351–357. doi: 10.1016/S0197-4580(97)00056-0. [DOI] [PubMed] [Google Scholar]
- 126.Wang C, et al. Microglial NF-κB drives tau spreading and toxicity in a mouse model of tauopathy. Nat. Commun. 2022;13:1969. doi: 10.1038/s41467-022-29552-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Asai H, et al. Depletion of microglia and inhibition of exosome synthesis halt tau propagation. Nat. Neurosci. 2015;18:1584. doi: 10.1038/nn.4132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Wang Y, et al. The release and trans-synaptic transmission of Tau via exosomes. Mol. Neurodegener. 2017;12:5. doi: 10.1186/s13024-016-0143-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Lessard CB, et al. High-affinity interactions and signal transduction between Aβ oligomers and TREM2. EMBO Mol. Med. 2018;10:e9027. doi: 10.15252/emmm.201809027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Rangaraju S, Gearing M, Jin L-W, Levey A. Potassium channel Kv1.3 is highly expressed by microglia in human Alzheimer’s disease. J. Alzheimers Dis. 2015;44:797. doi: 10.3233/JAD-141704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Yin Z, et al. Immune hyperreactivity of Aβ plaque-associated microglia in Alzheimer’s disease. Neurobiol. Aging. 2017;55:115–122. doi: 10.1016/j.neurobiolaging.2017.03.021. [DOI] [PubMed] [Google Scholar]
- 132.Liu W, et al. Trem2 promotes anti-inflammatory responses in microglia and is suppressed under pro-inflammatory conditions. Hum. Mol. Genet. 2020;29:3224–3248. doi: 10.1093/hmg/ddaa209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Leyns CEG, et al. TREM2 function impedes tau seeding in neuritic plaques. Nat. Neurosci. 2019;22:1217–1222. doi: 10.1038/s41593-019-0433-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Paasila PJ, Davies DS, Kril JJ, Goldsbury C, Sutherland GT. The relationship between the morphological subtypes of microglia and Alzheimer’s disease neuropathology. Brain Pathol. 2019;29:726–740. doi: 10.1111/bpa.12717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Spangenberg E, et al. Sustained microglial depletion with CSF1R inhibitor impairs parenchymal plaque development in an Alzheimer’s disease model. Nat. Commun. 2019;10:3758. doi: 10.1038/s41467-019-11674-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Richard E, et al. Characteristics of dyshoric capillary cerebral amyloid angiopathy. J. Neuropathol. Exp. Neurol. 2010;69:1158–1167. doi: 10.1097/NEN.0b013e3181fab558. [DOI] [PubMed] [Google Scholar]
- 137.Meisl, G. et al. In vivo rate-determining steps of tau seed accumulation in Alzheimer’s disease. Sci. Adv.7, eabh1448. [DOI] [PMC free article] [PubMed]
- 138.Pascoal TA, et al. Microglial activation and tau propagate jointly across Braak stages. Nat. Med. 2021;27:1592–1599. doi: 10.1038/s41591-021-01456-w. [DOI] [PubMed] [Google Scholar]
- 139.Ulland TK, et al. TREM2 maintains microglial metabolic fitness in Alzheimer’s disease. Cell. 2017;170:649–663.e13. doi: 10.1016/j.cell.2017.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Gonzales MM, et al. A geroscience motivated approach to treat Alzheimer’s disease: Senolytics move to clinical trials. Mech. Ageing Dev. 2021;200:111589. doi: 10.1016/j.mad.2021.111589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Hickson LJ, et al. Senolytics decrease senescent cells in humans: Preliminary report from a clinical trial of Dasatinib plus Quercetin in individuals with diabetic kidney disease. EBioMedicine. 2019;47:446–456. doi: 10.1016/j.ebiom.2019.08.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Sokolova, D., Childs, T. & Hong, S. Insight into the role of phosphatidylserine in complement-mediated synapse loss in Alzheimer’s disease. Fac. Rev. 10, (2021). [DOI] [PMC free article] [PubMed]
- 143.St-Pierre M-K, et al. Ultrastructural characterization of dark microglia during aging in a mouse model of Alzheimer’s disease pathology and in human post-mortem brain samples. J. Neuroinflammation. 2022;19:235. doi: 10.1186/s12974-022-02595-8. [DOI] [PMC free article] [PubMed] [Google Scholar]