Abstract
Lymphedema is a severe debilitating disease characterized by the accumulation of excessive protein-rich fluid in the interstitial space. Given the severe morbidity associated with this disease process, various surgical and nonsurgical treatment modalities have been developed to attempt to reduce the incidence and symptoms associated with lymphedema. Manual lymphatic drainage (MLD) is a component of complete decongestive therapy on-surgical treatment which has demonstrated benefit in reducing the development of lymphedema following surgery. Here we provide a review of literature on MLD and its potential mechanism of action. This paper aims to educate patients, physicians, and surgeons about MLD regarding its efficacy and utility in the treatment paradigm for lymphedema and to translate concepts from the treatment of lymphedema to cosmetic procedures.
Level of Evidence: 5

Lymphedema is a disease process manifested by inadequate drainage of lymphatic vessels, resulting in an accumulation of excess protein-rich interstitial fluid. Under homeostatic conditions, fluid interactions between capillaries, interstitial space, and lymphatic vessels allow for net fluid to extravasate from the arterial end of capillaries, which is then reabsorbed into lymphatic channels at the venous side of capillaries. The delicate balance of hydrostatic pressure and colloid pressure between the capillaries and interstitial spaces normally work in harmony to prevent the accumulation and stasis of fluid. Under normal circumstances, any excess fluid in the interstitial space is easily and readily removed by a nonpathologic lymphatic system. Upon entering the lymphatic vessels, the fluid, now termed lymph, circulates through the lymphatic vessels before ultimately ending up returning into the venous circulation.1 Any disruption to this delicate lymphatic system and its equilibrium can result in the development of severe and debilitating lymphedema. Notably this equilibrium is routinely disrupted by surgical procedures, and cosmetic procedures including liposuction, facial surgery, and body contouring.
Lymphedema has traditionally been classified based on etiology, broadly divided into inherited (primary) or acquired (secondary) forms. Primary causes of lymphedema are rare, when compared with the acquired forms, and often a result of genetic abnormalities.2,3 The majority of lymphedema cases encountered in health care are therefore acquired, occurring secondary to accidental or iatrogenic trauma or other lymphatic-disrupting disease processes. Plastic surgeons are generally familiar with the most common causes of secondary lymphedema which include cancer, chemotherapy, radiation, lymph-node dissection, and various surgical procedures. Additionally, complications that stem from these secondary causes of lymphedema, such as infection and seroma, can further exacerbate or result in lymphedema.
Given the prevalence of secondary causes of lymphedema, many treatment modalities have been developed to help reduce the risk of developing lymphedema or provide symptom relief. Treatments span from nonsurgical complete decongestive therapy (CDT) and massage to surgical interventions which include lymphaticovenous bypass, vascularized lymph node transfer, laser treatment, and stem-cell therapy.4–6 CDT is now widely accepted as the mainstay conservative treatment approach for lymphedema and consists of a multi-factorial approach which include skin care, exercise, compression garments, and manual lymphatic drainage (MLD).7,8 This MLD is a massage technique that is thought to decrease fibrosis and lymphatic rerouting to functioning lymphatic channels and serves as the most common modality used to assist in lymphatic restoration following potential lymphatic disruption during surgery.1,9–11
LYMPHATIC MASSAGE: PROPOSED MECHANISM IN IMPROVING LYMPHATIC DRAINAGE
MLD utilizes gentle massaging along lymphatic channels with slow repetitive movements to reduce buildup of fluid in extremities following surgery; however, the exact physiologic mechanism by which MLD exerts its effect remains unclear.10,12 Multiple studies have attempted to uncover its specific mechanism of action; however, MLD physiology remains poorly understood with various conflicting hypothesis proposed in the literature. Some have proposed that by performing MLD, lymphatic vessels respond by increasing their transport ability through increased contractions.13,14 Others believe that MLD increases interstitial pressure which results in improved lymphatic reabsorption.15,16 Further hypotheses propose that MLD promotes a decrease in distal lymphatic pressure, enhancing uptake, or that MLD improves accessory lymphatic routes that enhance lymphatic reuptake.17,18 There is evidence that this effect may be multifactorial with one study demonstrating reduced limb volume following MLD despite no change in lymph transport.19
Lymphatic function effects have been a primary source of investigation for patients undergoing MLD, but data suggest there may also be beneficial effects on arteriovenous system which in turn helps to reduce fluid accumulation. One possible mechanism by which MLD reduces microlymphatic hypertension is by increasing peripheral arterial blood flow through superficial circulation or skin circulation.13,20 One study utilizing a mouse model demonstrated increased femoral vein blood flow as a result of MLD,17 suggesting this method can help to improve systemic venous return. Other studies have suggested that the mechanism of improvement in lymphatic drainage may even be further upstream, with effects on the autonomic nervous system.21 Various studies have demonstrated improved breathlessness, sleep, and increased urinary secretion of adrenergic hormones, serotonin, and histamine as a result of MLD.22,23
LYMPHATIC MASSAGE VARIATIONS
There are 4 main methods of MLD, which are used in conjunction for the treatment of lymphedema along with exercise, compression therapy, and proper skin-care treatments. In all the 4 most common techniques of MLD, hand movements are strategically placed in areas to apply tension on the skin to subsequently increase interstitial pressures, theoretically promoting lymphatic uptake. Movements are rhythmic, at a controlled pace, and allow for a return phase in which the skin under tension can return to normal tone. Applied pressure can vary and may depend on the tissue, with more severe lymphedema requiring greater pressure if there are fibrotic or sclerotic areas, deeper pressure may be necessary.
Although seemingly counterintuitive, MLD usually begins with treatment of the central or proximal region and works distally, in contrast to pressure garments that depend on a distal to proximal restoration of flow. Additionally, attention may be given to the contralateral (healthy) side to promote better lymphatic drainage at a systemic level.12 All MLD techniques may incorporate training on proper breathing to reduce intrathoracic and intraabdominal pressure to theoretically enhance deeper lymphatic uptake.22
There are various nuances to the different MLD techniques. One of the first treatment methods was developed in the 1930s by Emil Vodder, now coined the “Vodder method.” This method includes different hand movements, emphasizing circular movements of the thumb, including the “thumb circle,” “stationary circle,” “pump,” “scoop,” and “rotary” movements.24 These specialized hand movements are used to direct fluid from one quadrant of the body across an anastomoses—a connection between the body's fluid drainage pathways. This is how a therapist moves fluid from a region of the body where the lymphatics are impaired to another region of the body where the lymphatics are functioning. A trained therapist will locate inter-territorial anastomosis and help re-route the lymph around impaired lymph nodes or absent lymph vessels, toward healthy ones. The Földi technique was developed as an offshoot of the Vodder technique and utilizes similar hand movements described previously, with the addition of a period of increased pressure followed by a relaxation phase. The Földi technique also incorporates the “encircling” stoke to help reduce edema.25 The Casley–Smith method added the technique consisting of using the side of the hand over specific watershed areas between distinct skin lymph territories with a slow and gentle “efflurage” maneuver.15 Leduc added “call-up” and “reabsorption” maneuvers to sequentially promote lymphatic uptake in the distal to proximal regions of lymphatic uptake.16 Any of the 4 most common MLD techniques may be suitable for treating a patient with a lymphedema, and careful selection of the technique may depend on the patient and method in which the therapist is best trained.
DISCUSSION
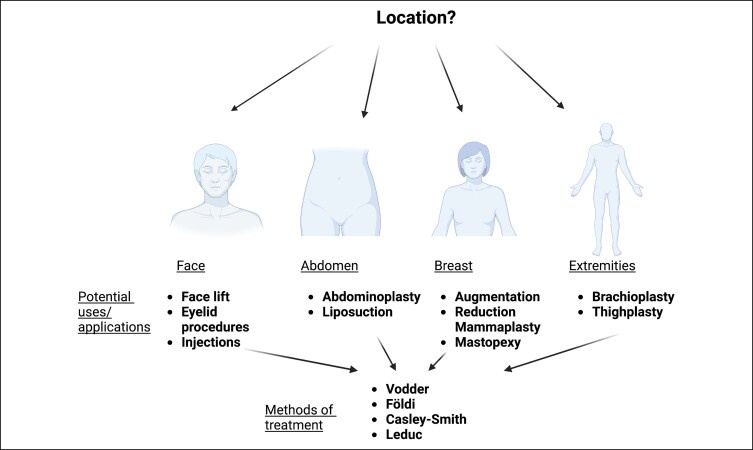
There are many potential use cases for MLD in plastic surgery patients (Figure 1). Originally, MLD had been utilized in postmastectomy breast-cancer patients prior to undergoing reconstruction, with notable improvements in pain and swelling.10,22 Recent studies have begun to expand the use of MLD to those who have undergone cosmetic procedures. In the case of cosmetic plastic surgery, the postoperative period is one of the most critical phases. General postoperative manual lymphatic massage recommendations consist of manual lymphatic massage 2 to 3 times per week during the initial 3 to 4 weeks of recovery to be performed by a certified lymphedema therapist or a licensed massage therapist who have undergone some degree of lymphedema training and are often certified to perform postoperative lymphatic drainage techniques. It is through postoperative care that the expected results are achieved. Rapidly reducing lymphostasis postoperatively may help improve early results and prevent late sequelae. In addition to fighting this accumulation of fluid, doing lymphatic drainage after plastic surgery may help in recovery, improving blood circulation, reducing pain, and facilitating healing. Fibrosis, an inflammatory process that causes hardening of the skin, is a common concern for those recovering from plastic surgery. Aesthetic procedures, especially liposuction, results in postoperative swelling that can take between 3 and 6 months for the body's lymphatic system to resolve. Similar to skin pathophysiology of chronic lymphedema, fluid accumulation after liposuction can create hardened lumps and bumps of the skin. However, unlike lymphedema, these lumps and bumps can be fully resolved with MLD and compression garments; patients undergoing elective cosmetic procedures have healthy intact lymphatic systems, while lymphedema patients do not. Since the recovery process from plastic surgery can be a lengthy one, between 3 and 6 months, utilizing MLD therapy during the postoperative recovery phase, can be beneficial in supporting the lymphatic system in its role in reabsorption of fluid.
Figure 1.
Potential uses and applications of lymphatic massage in plastic and reconstructive surgery.
Abdomen
In patients undergoing abdominal liposuction, the superficial lymphatic system is at an elevated risk of disruption due to large, sweeping cannula strokes, often resulting in lymphatic stasis.26 In abdominoplasty, it has been demonstrated that the primary source of lymphatic drainage may shift from inguinal to axillary after undergoing surgery, also placing one at an elevated risk for stasis and potential edema.27 Lymphedema stemming from cosmetic procedures presents a significant burden to patients who are seeking improved aesthetics by means of often elective procedures, as it can negatively affect comfort, quality of life, and activities of daily living.28 Numerous studies have found that MLD in conjunction with therapeutic adjuncts can provide reductions in edema, fibrosis, as well as provided analgesia in patients undergoing liposuction and/or lipoabdominoplasty.28–31 These been found to extended from the abdomen to all core liposuction areas, including the upper and lower abdomen, flanks, back, and hips.31
Breast
In contrast to mastectomy and reconstruction, there are fewer known benefits to performing MLD in patients undergoing primary cosmetic procedures. Some studies have incorporated MLD in their postoperative protocol for patients undergoing breast augmentation.32–34 Additionally, multiple surgeons performing mastopexy have incorporated MLD into their postoperative protocols.35,36 There are few studies evaluating the use of MLD in reduction mammaplasty, but some studies have shown altered lymphatic drainage following breast procedures, including breast reduction, suggesting a potential benefit for the incorporation of MLD into postoperative management.37,38
Face
MLD use is less well studied in other areas of cosmetic procedures but may have some use in mitigating complications after facial procedures such as injectables, fillers, or botulinum toxin.39,40 Some practices are incorporating MLD into postoperative recovery from facelift, with the goal of minimizing swelling and pain.41–43 Therefore, MLD may further provide benefit in improving postoperative edema in the periorbital region after eyelid procedures.44
Extremity
Studies evaluating the use of MLD following cosmetic procedures are somewhat limited; however, its use is most commonly described following thigh lift or brachioplasty in the massive weight loss population. Although contemporary surgical techniques are effective in improving body contouring and skin tightness, the surgeon should be aware that excess resection can result in significant alterations in lymphatic drainage.45 This has led some surgeons to suggest that MLD be utilized as a useful adjunct to reduce the risk of developing postoperative lymphedema.46,47
CONCLUSIONS
As the number of patients undergoing cosmetic procedures continues to increase, there is a need for adjunctive therapies that promote patient recovery which is paramount to improve postoperative outcomes and enhance patient's satisfaction and aesthetic desires. MLD is an area of active research that has preliminarily shown a benefit in patients undergoing a variety of aesthetic procedures. Due to the paucity of research on MLD in aesthetic procedures, more studies on the topic are warranted.
Disclosures
The authors declared no potential conflicts of interest with respect to the research, authorship, and publication of this article.
Funding
The authors received no financial support for the research, authorship, and publication of this article, including payment of the article processing charge.
REFERENCES
- 1. Ridner SH. Pathophysiology of lymphedema. Semin Oncol Nurs. 2013;29(1):4–11. doi: 10.1016/j.soncn.2012.11.002 [DOI] [PubMed] [Google Scholar]
- 2. Ghalamkarpour A, Holnthoner W, Saharinen P. Recessive primary congenital lymphoedema caused by a VEGFR3 mutation. J Med Genet. 2009;46(6):399–404. doi: 10.1136/jmg.2008.064469 [DOI] [PubMed] [Google Scholar]
- 3. Ferrell RE, Kimak MA, Lawrence EC, Finegold DN. Candidate gene analysis in primary lymphedema. Lymphatic Res Biol. 2008;6(2):69–76. doi: 10.1089/lrb.2007.1022 [DOI] [PubMed] [Google Scholar]
- 4. Damstra RJ, Voesten HGJ, Schelven WD, Lei B. Lymphatic venous anastomosis (LVA) for treatment of secondary arm lymphedema. A prospective study of 11 LVA procedures in 10 patients with breast cancer related lymphedema and a critical review of the literature. Breast Cancer Res Treat. 2009;113(2):199–206. doi: 10.1007/s10549-008-9932-5 [DOI] [PubMed] [Google Scholar]
- 5. Lievens PC. The effect of a combined HeNe and i.r. laser treatment on the regeneration of the lymphatic system during the process of wound healing. Laser Med Sci. 1991;6(2):193–199. doi: 10.1007/BF02032548 [DOI] [Google Scholar]
- 6. Maldonado GEM, Pérez CAA, Covarrubias EEA. Autologous stem cells for the treatment of post-mastectomy lymphedema: a pilot study. Cytotherapy. 2011;13(10):1249–1255. doi: 10.3109/14653249.2011.594791 [DOI] [PubMed] [Google Scholar]
- 7. Lawenda BD, Mondry TE, Johnstone PAS. Lymphedema: a primer on the identification and management of a chronic condition in oncologic treatment. CA Cancer J Clin. 2009;59(1):8–24. doi: 10.3322/caac.20001 [DOI] [PubMed] [Google Scholar]
- 8. Ko DS, Lerner R, Klose G, Cosimi AB. Effective treatment of lymphedema of the extremities. Arch Surg. 1998;133(4):452–458. doi: 10.1001/archsurg.133.4.452 [DOI] [PubMed] [Google Scholar]
- 9. Huang T-W, Tseng S-H, Lin C-C, et al. Effects of manual lymphatic drainage on breast cancer-related lymphedema: a systematic review and meta-analysis of randomized controlled trials. World J Surg Oncol. 2013;11(1):15. doi: 10.1186/1477-7819-11-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ezzo J, Manheimer E, McNeely ML. Manual lymphatic drainage for lymphedema following breast cancer treatment. Cochrane Database Syst Rev. 2015;5:CD003475. doi: 10.1002/14651858.CD003475.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Thompson B, Gaitatzis K, Janse de Jonge X, Blackwell R, Koelmeyer LA. Manual lymphatic drainage treatment for lymphedema: a systematic review of the literature. J Cancer Surviv. 2021;15(2):244–258. doi: 10.1007/s11764-020-00928-1 [DOI] [PubMed] [Google Scholar]
- 12. Williams A. Manual lymphatic drainage: exploring the history and evidence base. Br J Community Nurs. 2010;15(4):S18–S24. doi: 10.12968/bjcn.2010.15.Sup3.47365 [DOI] [PubMed] [Google Scholar]
- 13. Hutzschenreuter P, Brümmer H, Ebberfeld K. Experimental and clinical studies of the mechanism of effect of manual lymph drainage therapy. Z Lymphol. 1989;13(1):62–64. [PubMed] [Google Scholar]
- 14. François A, Richaud C, Bouchet JY, Franco A, Comet M. Does medical treatment of lymphedema act by increasing lymph flow? Vasa. 1989;18(4):281–286. [PubMed] [Google Scholar]
- 15. Casley-Smith JR, Boris M, Weindorf S, Lasinski B. Treatment for lymphedema of the arm-The Casley-Smith method: A noninvasive method produces continued reduction. Cancer. 1998;83(S12B):2843–2860. doi: 10.1002/(SICI)1097-0142(19981215)83:12B [DOI] [PubMed] [Google Scholar]
- 16. Leduc O, Peeters A, Bourgeois P. Bandages—scintigraphic demonstration of its efficacy on colloidal protein reabsorption during muscle-activity. In: Progress in Lymphology. Vol. XII. ELSEVIER SCIENCE PUBL B V; 1890:421–423. [Google Scholar]
- 17. Derdeyn A, Aslam M, Pflugg JJ, Manual lymph drainage-mode of action. Lymphology. 1994;27(27):527–529. [Google Scholar]
- 18. Ferrandez JC, Laroche JP, Serin D, Felix-Faure C, Vinot JM. Lymphoscintigraphic aspects of the effects of manual lymphatic drainage. J Mal Vasc. 1996;21(5):283–289. [PubMed] [Google Scholar]
- 19. Kafejian-Haddad AP, Perez JMC, Castiglioni MLV, Miranda Júnior F, Figueiredo LFP. Lymphscintigraphic evaluation of manual lymphatic drainage for lower extremity lymphedema. Lymphology. 2006;39(1):41–48. [PubMed] [Google Scholar]
- 20. Hutzschenreuter P, Herpertz U. Primary and secondary lymphedema in children treated with manual lymph drainage and compression therapy. Eur J Lymphol. 1993;4(14):51–57. [Google Scholar]
- 21. Hutzschenreuter P, Ehlers R. Effect of manual lymph drainage on the autonomic nervous system. Z Lymphol. 1986;10(2):58–60. [PubMed] [Google Scholar]
- 22. Williams AF, Vadgama A, Franks PJ, Mortimer PS. A randomized controlled crossover study of manual lymphatic drainage therapy in women with breast cancer-related lymphoedema. Eur J Cancer Care (Engl). 2002;11(4):254–261. doi: 10.1046/j.1365-2354.2002.00312.x [DOI] [PubMed] [Google Scholar]
- 23. Kurz W, Wittlinger G, Litmanovitch YI. Effect of manual lymph drainage massage on urinary excretion of neurohormones and minerals in chronic lymphedema. Angiology. 1978;29(10):764–772. doi: 10.1177/000331977802901007 [DOI] [PubMed] [Google Scholar]
- 24. Wittlinger H, Wittlinger G. Introduction to Dr Vodder's Manual Lymph Drainage. Vol 1. Basic Course. Heidelberg: Haug Publishers; 1992. [Google Scholar]
- 25. Mihály F, Strössenreuther R. Foundations of Manual Lymph Drainage. Mosby Elsevier; 2005. [Google Scholar]
- 26. Aldrich MB, Gross D, Morrow JR, Fife CE, Rasmussen JC. Effect of pneumatic compression therapy on lymph movement in lymphedema-affected extremities, as assessed by near-infrared fluorescence lymphatic imaging. J Innov Opt Health Sci. 2017;10(2):1650049. doi: 10.1142/S1793545816500498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Bassalobre M, Liebano RE, Silva MP. Changes in the pattern of superficial lymphatic drainage of the abdomen after abdominoplasty. Plast Reconstr Surg. 2022;149(6):1106e–1113e. doi: 10.1097/PRS.0000000000009114 [DOI] [PubMed] [Google Scholar]
- 28. Masson IFB, Oliveira BDA, Machado AFP, Farcic TS, Júnior IE, Baldan CS. Manual lymphatic drainage and therapeutic ultrasound in liposuction and lipoabdominoplasty post-operative period. Indian J Plast Surg. 2014;47(1):70–76. doi: 10.4103/0970-0358.129627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Chi A, Lange A, Guimarães M, Santos C. Prevention and treatment of ecchymosis, edema, and fibrosis in the pre-, trans-, and postoperative periods of plastic surgery. Rev Bras Cir Plást. 2001;33(3):343–354. doi: 10.5935/2177-1235.2018RBCP0147 [DOI] [Google Scholar]
- 30. Chi A, de Oliveira AV, Ruh AC, Schleder JC. O uso do linfotaping, terapia combinada e drenagem linfática manual sobre a fibrose no pós-operatório de cirurgia plástica de abdome. Fisioterapia Brasil. 2016;17(3):197–203. doi: 10.33233/fb.v17i3.477 [DOI] [Google Scholar]
- 31. Maningas T, Sturm L, Mangler A, Pazdernik VK. Manual lymphatic drainage in postoperative abdominoplasty with core liposuction patients. Am J Cosmet Surg. 2020;37(1):45–49. doi: 10.1177/0748806819874941 [DOI] [Google Scholar]
- 32. Di Giuseppe A, Wolf D.. Breast augmentation with stem cell-enhanced fat transfer: comparison between enhanced and unenhanced fat grafting. In: Shiffman MA, Di Giuseppe A, Bassetto F, eds. Stem Cells in Aesthetic Procedures: Art, Science, and Clinical Techniques. Springer; 2014:529–556. [Google Scholar]
- 33. Giometti M, Sobral C, Abdala J, Gomes D. Comparison of anatomic and round implants using periareolar access in primary breast augmentation. Rev Bras Cir Plást. 2001;31(3):328–338. doi: 10.5935/2177-1235.2016RBCP0055 [DOI] [Google Scholar]
- 34. Beer K, Lupo MP, Narurkar VA. Cosmetic Bootcamp Primer: Comprehensive Aesthetic Management. CRC Press; 2011. [Google Scholar]
- 35. Lagdamen LL, Benitez MO, Fox J, Fitzpatrick M. Preoperative and postoperative nursing considerations for the oncoplastic and reconstructive patient. In: Urban C, Rietjens M, El-Tamer M, Sacchini VS, eds. Oncoplastic and Reconstructive Breast Surgery. Springer International Publishing; 2019:783–790. [Google Scholar]
- 36. Okada A, Saito FL, Hiraki PY. Mastopexy after massive weight loss: dermal suspension, parenchymal reshaping, and augmentation with autologous tissue. Rev Bras Cir Plást. 2012;27(2):283–289. doi: 10.1590/S1983-51752012000200019 [DOI] [Google Scholar]
- 37. Jakub JW, Cox CE, Pippas AW, Gardner M, Pendas S, Reintgen DS. Controversial topics in breast lymphatic mapping. Semin Oncol. 2004;31(3):324–332. doi: 10.1053/j.seminoncol.2004.03.014 [DOI] [PubMed] [Google Scholar]
- 38. van der Ploeg I, Oldenburg H, Rutgers E. Lymphatic drainage patterns from the treated breast. Ann Surg Oncol. 2010;17(4):1069–1075. doi: 10.1245/s10434-009-0841-6 [DOI] [PubMed] [Google Scholar]
- 39. Ferreira MC, Salles AG, Gimenez R, Soares MFD. Complications with the use of botulinum toxin type A in facial rejuvenation: report of 8 cases. Aesth Plast Surg. 2004;28(6):441–444. doi: 10.1007/s00266-004-0031-7 [DOI] [PubMed] [Google Scholar]
- 40. Urdiales-Gálvez F, Delgado NE, Figueiredo V. Treatment of soft tissue filler complications: expert consensus recommendations. Aesth Plast Surg. 2018;42(2):498–510. doi: 10.1007/s00266-017-1063-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Mottura AA. Face lift postoperative recovery. Aesth Plast Surg. 2002;26(3):172–180. doi: 10.1007/s00266-001-0029-3 [DOI] [PubMed] [Google Scholar]
- 42. Saltz R, Ohana B. Thirteen years of experience with the endoscopic midface lift. Aesth Surg J. 2012;32(8):927–936. doi: 10.1177/1090820X12462714 [DOI] [PubMed] [Google Scholar]
- 43. Bull HG. Aesthetic facial surgery. Mund Kiefer Gesichtschirurgie. 2000;4(1):S343–S351. doi: 10.1007/PL00014557 [DOI] [PubMed] [Google Scholar]
- 44. Sami M, Soparkar C, Patrinely J, Tower R. Eyelid edema. Semin Plast Surg. 2007;21(1):24–31. doi: 10.1055/s-2007-967744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Moreno CH, Neto HJG, Junior AH, Malheiros CA. Thighplasty after bariatric surgery: evaluation of lymphatic drainage in lower extremities. Obes Surg. 2008;18(9):1160–1164. doi: 10.1007/s11695-007-9400-z [DOI] [PubMed] [Google Scholar]
- 46. Michaels J, Coon D, Rubin JP. Complications in postbariatric body contouring: postoperative management and treatment. Plast Reconstr Surg. 2011;127(4):1693–1700. doi: 10.1097/PRS.0b013e31820a649f [DOI] [PubMed] [Google Scholar]
- 47. Shiffman MA. New Frontiers in Plastic and Cosmetic Surgery. JP Medical Ltd; 2015. [Google Scholar]