Abstract
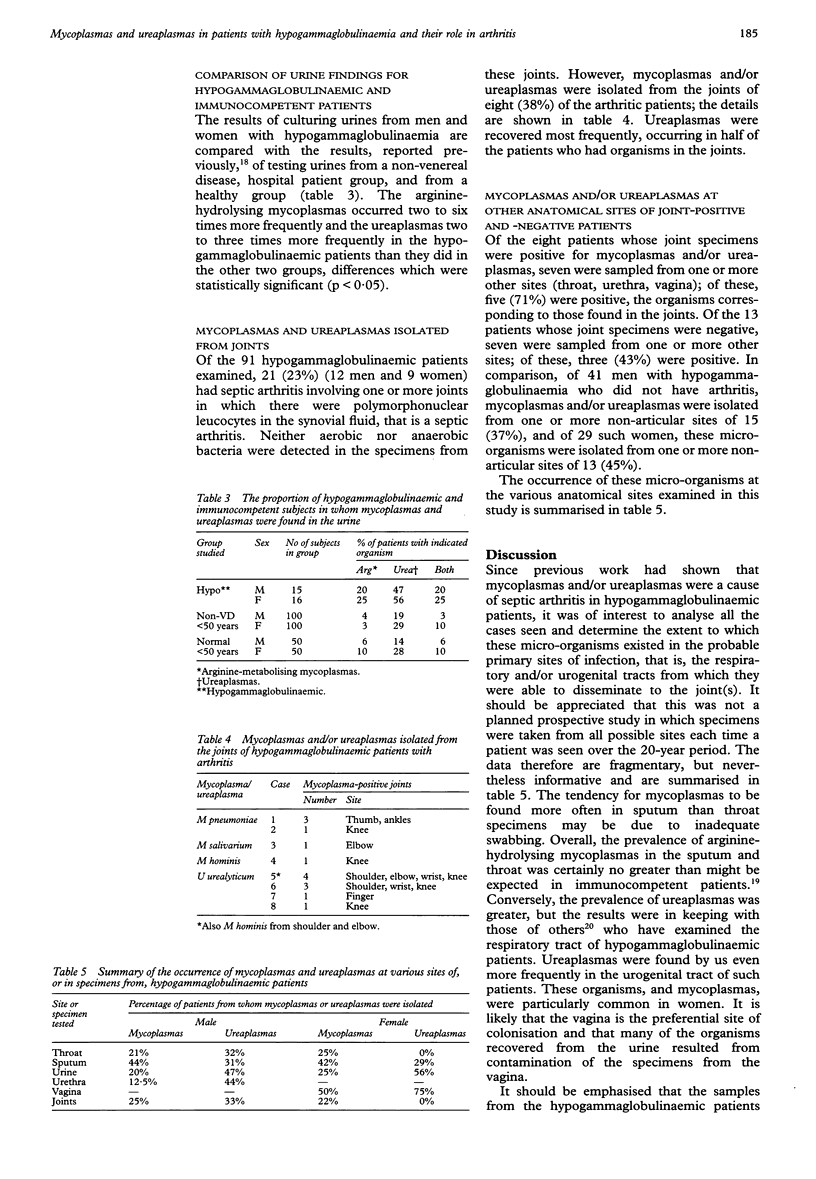
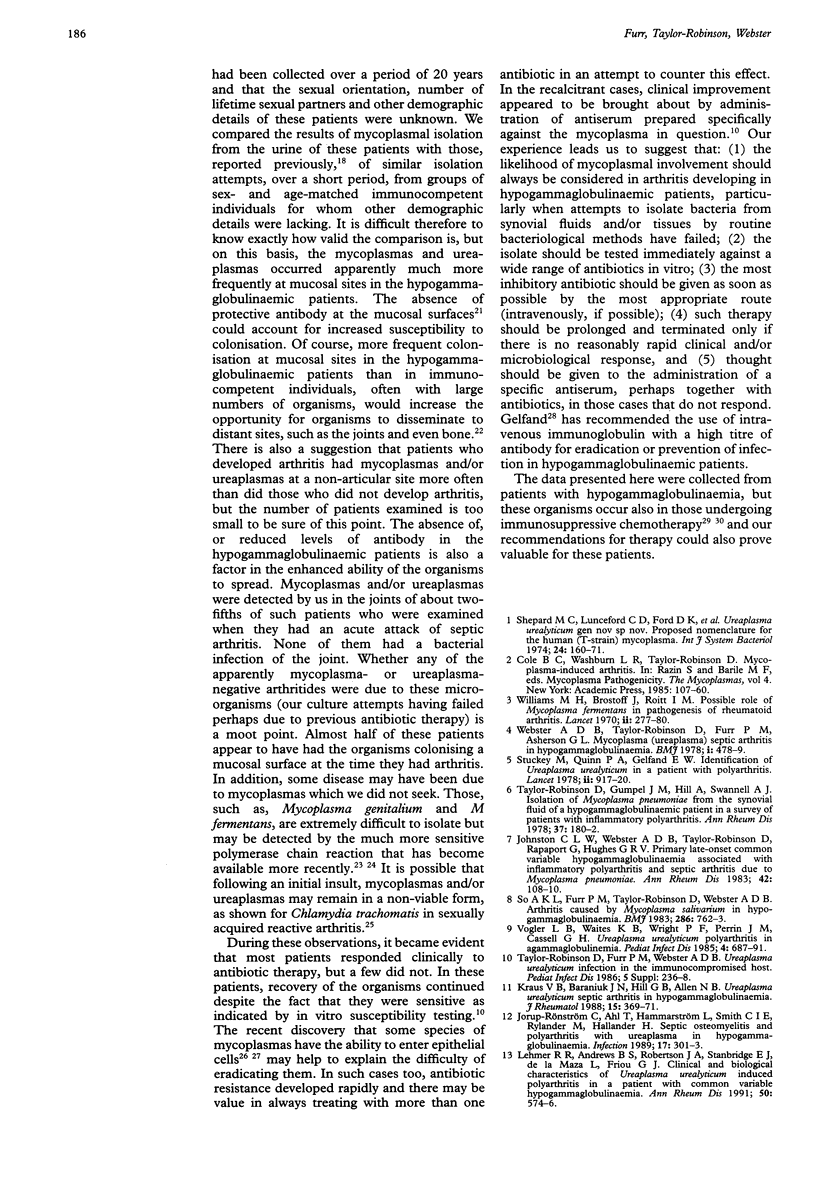
OBJECTIVES--To study the occurrence of mycoplasmas and ureaplasmas in patients with hypogammaglobulinaemia and the relationship of these micro-organisms to septic arthritis. METHODS--Over a period of about 20 years, 53 men and 38 women with hypogammaglobulinaemia, most of whom were less than 50 years old, were examined clinically and microbiologically. Mycoplasmas and ureaplasmas were sought in the throat, urogenital tract and joints by standard cultural methods, although not consistently in the three sites of all patients. RESULTS--Arginine-hydrolysing mycoplasmas and ureaplasmas occurred with similar frequency in the sputum/throat of the hypogammaglobulinaemic patients, but no more often than might be expected in immunocompetent patients. Ureaplasmas, however, dominated in the urogenital tracts of both men and women, being found in 75% of vaginal specimens. Arginine-hydrolysing mycoplasmas occurred two to six times more frequently and ureaplasmas two to three times more frequently in urine specimens from hypogammaglobulinaemic patients than they did in such specimens from sex- and age-matched non-venereal disease, hospital patients or healthy subjects; these differences were statistically significant (p < 0.05). Enhanced mucosal colonisation probably increases the chance of spread to distant sites, such as the joints. Of the 91 patients, 21 (23%) had septic arthritis involving one or more joints. Mycoplasmas and/or ureaplasmas, but not bacteria, were isolated from the joints of eight (38%) of these patients. However, dissemination to joints apparently had not occurred in some despite the opportunity by virtue of mycoplasmal or ureaplasmal colonisation at a mucosal site. Sometimes antibiotic therapy failed clinically, and microbiologically and recommendations for management are outlined. CONCLUSIONS--Hypogammaglobulinaemic patients appear to be more susceptible to colonisation of mucous membranes, especially of the urogenital tract, with mycoplasmas and ureaplasmas than are immunocompetent individuals. These micro-organisms are responsible for about two fifths of the septic arthritides occurring in these patients.
Full text
PDF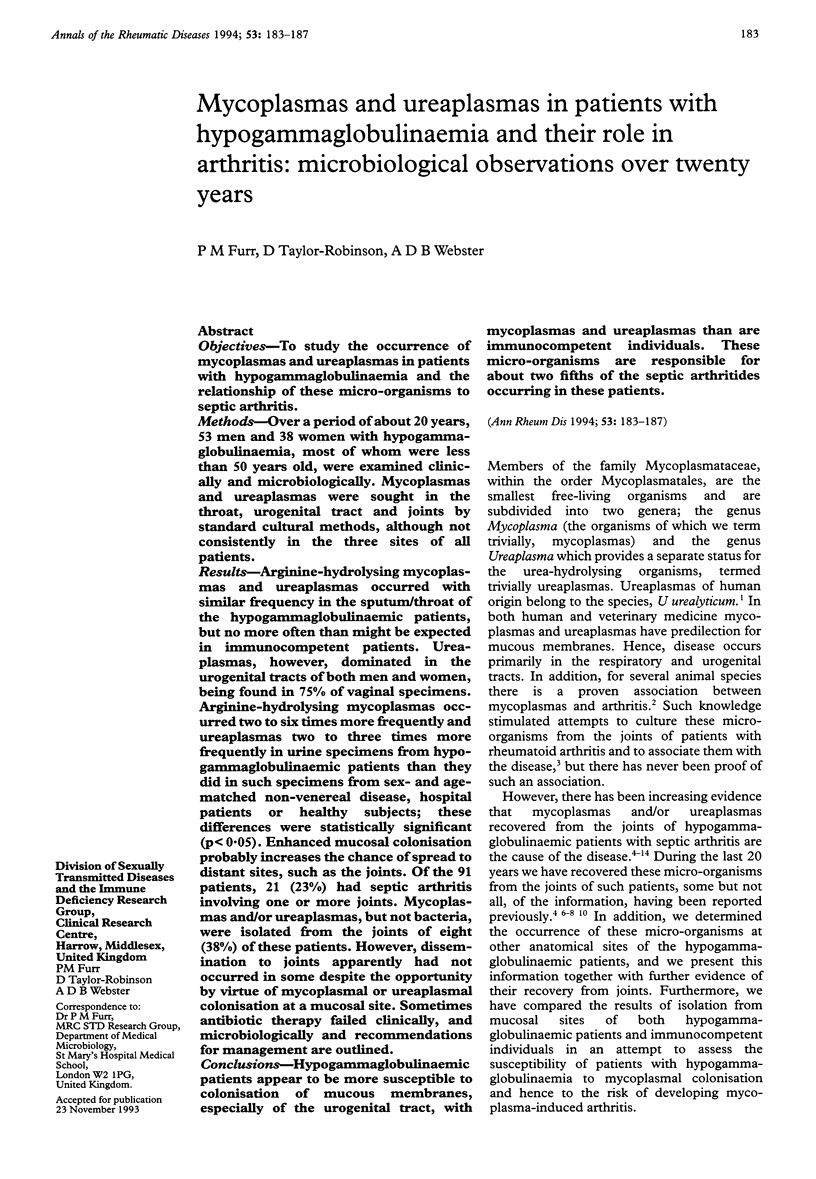

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Cimolai N. Mycoplasma pneumoniae in the immunocompromised host. Chest. 1992 Oct;102(4):1303–1304. doi: 10.1378/chest.102.4.1303b. [DOI] [PubMed] [Google Scholar]
- Johnston C. L., Webster A. D., Taylor-Robinson D., Rapaport G., Hughes G. R. Primary late-onset hypogammaglobulinaemia associated with inflammatory polyarthritis and septic arthritis due to Mycoplasma pneumoniae. Ann Rheum Dis. 1983 Feb;42(1):108–110. doi: 10.1136/ard.42.1.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jorup-Rönström C., Ahl T., Hammarström L., Smith C. I., Rylander M., Hallander H. Septic osteomyelitis and polyarthritis with ureaplasma in hypogammaglobulinemia. Infection. 1989 Sep-Oct;17(5):301–303. doi: 10.1007/BF01650712. [DOI] [PubMed] [Google Scholar]
- Katseni V. L., Gilroy C. B., Ryait B. K., Ariyoshi K., Bieniasz P. D., Weber J. N., Taylor-Robinson D. Mycoplasma fermentans in individuals seropositive and seronegative for HIV-1. Lancet. 1993 Jan 30;341(8840):271–273. doi: 10.1016/0140-6736(93)92617-3. [DOI] [PubMed] [Google Scholar]
- Keat A., Thomas B., Dixey J., Osborn M., Sonnex C., Taylor-Robinson D. Chlamydia trachomatis and reactive arthritis: the missing link. Lancet. 1987 Jan 10;1(8524):72–74. doi: 10.1016/s0140-6736(87)91910-6. [DOI] [PubMed] [Google Scholar]
- Lee A. H., Ramanujam T., Ware P., Edelstein P. H., Brooks J. J., Freundlich B., Schumacher H. R., Jr, Zurier R. B., Weiner D. B., Williams W. V. Molecular diagnosis of Ureaplasma urealyticum septic arthritis in a patient with hypogammaglobulinemia. Arthritis Rheum. 1992 Apr;35(4):443–448. doi: 10.1002/art.1780350414. [DOI] [PubMed] [Google Scholar]
- Lehmer R. R., Andrews B. S., Robertson J. A., Stanbridge E. J., de la Maza L., Friou G. J. Clinical and biological characteristics of Ureaplasma urealyticum induced polyarthritis in a patient with common variable hypogammaglobulinaemia. Ann Rheum Dis. 1991 Aug;50(8):574–576. doi: 10.1136/ard.50.8.574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo S. C., Hayes M. M., Wang R. Y., Pierce P. F., Kotani H., Shih J. W. Newly discovered mycoplasma isolated from patients infected with HIV. Lancet. 1991 Dec 7;338(8780):1415–1418. doi: 10.1016/0140-6736(91)92721-d. [DOI] [PubMed] [Google Scholar]
- Mohiuddin A. A., Corren J., Harbeck R. J., Teague J. L., Volz M., Gelfand E. W. Ureaplasma urealyticum chronic osteomyelitis in a patient with hypogammaglobulinemia. J Allergy Clin Immunol. 1991 Jan;87(1 Pt 1):104–107. doi: 10.1016/0091-6749(91)90219-e. [DOI] [PubMed] [Google Scholar]
- Palmer H. M., Gilroy C. B., Furr P. M., Taylor-Robinson D. Development and evaluation of the polymerase chain reaction to detect Mycoplasma genitalium. FEMS Microbiol Lett. 1991 Jan 15;61(2-3):199–203. doi: 10.1016/0378-1097(91)90551-k. [DOI] [PubMed] [Google Scholar]
- Roifman C. M., Rao C. P., Lederman H. M., Lavi S., Quinn P., Gelfand E. W. Increased susceptibility to Mycoplasma infection in patients with hypogammaglobulinemia. Am J Med. 1986 Apr;80(4):590–594. doi: 10.1016/0002-9343(86)90812-0. [DOI] [PubMed] [Google Scholar]
- So A. K., Furr P. M., Taylor-Robinson D., Webster A. D. Arthritis caused by Mycoplasma salivarium in hypogammaglobulinaemia. Br Med J (Clin Res Ed) 1983 Mar 5;286(6367):762–763. doi: 10.1136/bmj.286.6367.762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stuckey M., Quinn P. A., Gelfand E. W. Identification of Ureaplasma urealyticum (T-strain Mycoplasma) in patient with polyarthritis. Lancet. 1978 Oct 28;2(8096):917–920. doi: 10.1016/s0140-6736(78)91632-x. [DOI] [PubMed] [Google Scholar]
- Taylor-Robinson D., Davies H. A., Sarathchandra P., Furr P. M. Intracellular location of mycoplasmas in cultured cells demonstrated by immunocytochemistry and electron microscopy. Int J Exp Pathol. 1991 Dec;72(6):705–714. [PMC free article] [PubMed] [Google Scholar]
- Taylor-Robinson D., Gumpel J. M., Hill A., Swannell A. J. Isolation of Mycoplasma pneumoniae from the synovial fluid of a hypogrammaglobulinaemic patient in a survey of patients with inflammatory polyarthritis. Ann Rheum Dis. 1978 Apr;37(2):180–182. doi: 10.1136/ard.37.2.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor-Robinson D., Purcell R. H. Mycoplasmas of the human urogenital tract and oropharynx and their possible role in disease: a review with some recent observations. Proc R Soc Med. 1966 Nov;59(11 Pt 1):1112–1116. [PMC free article] [PubMed] [Google Scholar]
- Taylor-Robinson D., Webster A. D., Furr P. M., Asherson G. L. Prolonged persistence of Mycoplasma pneumoniae in a patient with hypogammaglobulinaemia. J Infect. 1980 Jun;2(2):171–175. doi: 10.1016/s0163-4453(80)91284-0. [DOI] [PubMed] [Google Scholar]
- Webster A. D., Furr P. M., Hughes-Jones N. C., Gorick B. D., Taylor-Robinson D. Critical dependence on antibody for defence against mycoplasmas. Clin Exp Immunol. 1988 Mar;71(3):383–387. [PMC free article] [PubMed] [Google Scholar]
- Webster A. D., Taylor-Robinson D., Furr P. M., Asherson G. L. Mycoplasmal (ureaplasma) septic arthritis in hypogammaglobulinaemia. Br Med J. 1978 Feb 25;1(6111):478–479. doi: 10.1136/bmj.1.6111.478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams M. H., Brostoff J., Roitt I. M. Possible role of Mycoplasma fermentans in pathogenesis of rheumatoid arthritis. Lancet. 1970 Aug 8;2(7667):277–280. doi: 10.1016/s0140-6736(70)91328-0. [DOI] [PubMed] [Google Scholar]


