Abstract
Background
Arthroscopic lunocapitate (LC) fusion can be an alternative surgical treatment for scapholunate advanced collapse (SLAC) or scaphoid nonunion advanced collapse (SNAC) of the wrist. We retrospectively reviewed patients who had arthroscopic LC fusion to estimate clinical and radiological outcomes.
Methods
From January 2013 to February 2017, all patients with SLAC (stage II or III) or SNAC (stage II or III) wrists, who underwent arthroscopic LC fusion with scaphoidectomy and were followed up for a minimum of 2 years, were enrolled in this retrospective study. Clinical outcomes included visual analog scale (VAS) pain, grip strength, active range of wrist motion, Mayo wrist score (MWS), and the Disabilities of Arm, Shoulder and Hand (DASH) score. Radiologic outcomes included bony union, carpal height ratio, joint space height ratio, and loosening of screws. We also performed group analysis between patients with 1 and 2 headless compression screws to fix the LC interval.
Results
Eleven patients were assessed for 32.6 ± 8.0 months. Union was achieved in 10 patients (union rate, 90.9%). There was improvmenet in mean VAS pain score (from 7.9 ± 1.0 to 1.6 ± 0.7, p = 0.003) and grip strength (from 67.5% ± 11.4% to 81.8% ± 8.0%, p = 0.003) postoperatively. The mean MWS and DASH score were 40.9 ± 13.8 and 38.3 ± 8.2, respectively, preoperatively and improved to 75.5 ± 8.2 and 11.3 ± 4.1, respectively, postoperatively (p < 0.001 for all). Radiolucent screw loosening occurred in 3 patients (27.3%), including 1 nonunion patient and 1 patient who underwent screw removal due to the screw migration encroaching the lunate fossa of radius. In group analysis, only the frequency of radiolucent loosening was higher in 1 screw (3 of 4) than 2 screw fixation (0 of 7) (p = 0.024).
Conclusions
Arthroscopic scaphoid excision and LC fusion for patients with advanced SLAC or SNAC of the wrist was effective and safe only in cases fixed with 2 headless compression screws. We recommend arthroscopic LC fusion using 2 screws rather than 1 to decrease radiolucent loosening, which might affect complications such as nonunion, delayed union, or screw migration.
Keywords: Carpal bones, Arthritis, Arthroscope, Arthrodesis
Disconnection of wrist kinematics by either nonunion of the scaphoid or dissociation of the scapholunate joint results in traumatic arthritis in the wrist unless managed appropriately. Such a disconnection is called scaphoid nonunion advanced collapse (SNAC) or scapholunate advanced collapse (SLAC) of the wrist.1) Salvage procedures such as four-corner fusion (4CF) with scaphoid excision or proximal row carpectomy are indicated for symptomatic patients with advanced SNAC and SLAC of the wrist.2,3) Among them, 4CF with scaphoid excision is generally recognized as the most popular procedure, especially in active patients.4,5)
As another way to treat advanced carpal arthritis patients, lunocapitate (LC) fusion with scaphoid excision initially showed high nonunion rates (average, 30%) and surgical complications (average, 62%).6,7) Throughout the development of surgical techniques and instruments such as compressive headless screws, LC fusion appeared to show comparable outcomes with 4CF with low nonunion rate and complications (3.8% and 13.8%, respectively).8,9,10) The fewer surgical procedures in LC fusion than 4CF is merit for surgeons and could be a reliable treatment alternative to 4CF.
With recent innovations in arthroscopic techniques for the wrist, arthroscopic carpal fusion with scaphoid excision has been increasingly performed with improved patient outcomes.11) With the advantage of preserving the carpal ligaments and capsule during arthroscopic surgery,12,13) this minimally invasive procedure can be an alternative in patients with SLAC or SNAC of the wrist. Though an arthroscopic manner for carpal bone fusion, including LC fusion or 4CF, initially resulted in a poor union rate of 71.4%,14) a recent study showed favorable results with a union rate over 90%.15) The purpose of this study was to analyze union rates, clinical and radiological outcomes, and surgical complications in patients who had undergone arthroscopic LC fusion for advanced SNAC or SLAC of the wrist.
METHODS
The Institutional Review Board of Yonsei University Health System, Severance Hospital approved this study (No. 4-2020-0175) and waived informed consent.
We retrospectively reviewed all patients who underwent surgical salvage procedures for symptomatic stage II or III SNAC or SLAC of the wrist including patients who underwent arthroscopic LC fusion with scaphoid excision between January 2013 and February 2017 and all patients were followed up for at least 2 years postoperatively. The exclusion criteria were patients with (1) a previous history of surgery on the same wrist, (2) a simultaneous surgery on the ipsilateral hand or wrist, (3) inadequate follow-up (< 2 years), and (4) worker’s compensation. All patients were treated by the same hand surgeon (YRC).
Surgical Technique
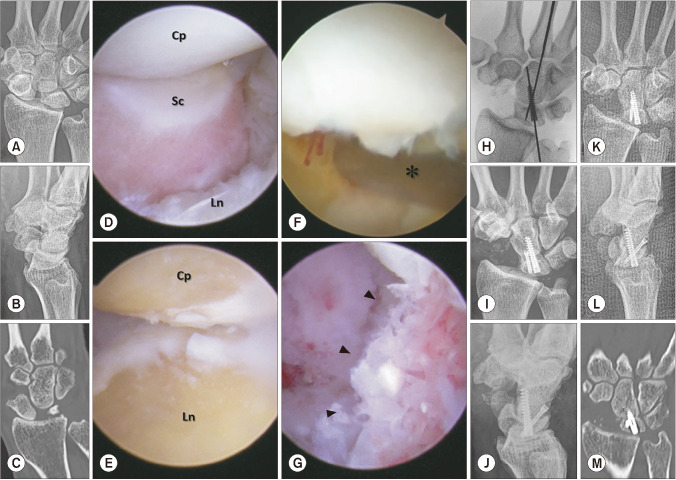
The surgical procedure of arthroscopic scaphoid excision and LC fusion is illustrated in Fig. 1. Under general anesthesia and with the patient placed in supine, the patient’s arm was prepared and draped on a hand table and exsanguinated using an Esmarch bandage and tourniquet. After placing the index, middle, and ring fingers in finger traps, the patient’s arm was suspended in an ARC wrist tower (Acumed, Hillsboro, OR, USA) using 5 to 8 kg of traction. A midcarpal ulnar portal was created first, and a 1.9-mm video arthroscope was passed through it, after which a midcarpal radial portal was constructed for use as a working portal. A 2.9- or 3.5-mm motorized burr and pituitary rongeur forceps were used across the working portal to excise the scaphoid bone. After excising the scaphoid (at least the proximal two-thirds of it), the arthroscope was introduced through the midcarpal radial portal, and a 2.9-mm motorized burr was inserted through the midcarpal ulnar portal to remove the cartilage and subchondral bone from both the distal articular surface of the lunate and the proximal capitate until healthy-looking cancellous bones were revealed on both surfaces (Fig. 1 E and F). At this point, the traction was released, the lunate was reduced relative to the capitate in a slightly flexed manner using a joy-stick wire, and the capitate was ulnarly translated by providing thumb pressure on the radial side of the distal carpal row to achieve greater bony contact between the lunate and the capitate under arthroscopic and fluoroscopic imaging guidance. Then, a 17-gauge needle was inserted percutaneously on the dorsal surface of the capitate, and a 0.9-mm Kirschner wire was inserted into the lunate from the capitate for temporary fixation. An additional 0.9-mm Kirschner wire was inserted using the same technique in case adequate space was available. The gap between the lunate and the capitate was filled with demineralized bone material (DBM) using an arthroscopy-guided bone graft procedure, as described previously.16,17) Briefly, the sheath of a 3.5-mm burr was packed with the DBM and inserted into the LC interval via the midcarpal ulnar portal. The DBM was inserted into the gap using the trocar of a bone biopsy needle. We thought the DBM helped fill the gap between the contact surfaces of the capitate and lunate and facilitated unionization, although the effectiveness of the DBM in arthrodesis was only shown in spinal fusion or hindfoot arthrodesis.18,19) Then, the Kirschner wires were replaced with the guidewires for the headless compression screws, which were used to fix the LC joint (Fig. 1H). After ensuring that the lunate joint surface was free of protruding screws, all arthroscopic procedures were completed, and any loose debris within the joint was removed using a motorized shaver.
Fig. 1. Arthroscopic lunocapitate fusion in a patient with scapholunate advanced collapse (SLAC). (A-C) Preoperative posteroanterior and lateral radiographic views and a coronal computed tomographic scan of a 68-year-old man with stage II SLAC of the right wrist. (D) On the midcarpal ulnar portal (MCU), the scaphoid was dissociated from the scapholunate alignment (Cp: capitate, Sc: scaphoid, Ln: lunate). (E) The midcarpal radial portal (MCR) revealed the cancellous bone underneath the joint surface after curetting the cartilage and subchondral bone via the MCU as a working portal. (F, G) Using the MCR as a viewing portal and the MCU as a working portal, demineralized bone material (arrowheads) was inserted into the lunocapitate interval using a 3.5-mm burr sheath (asterisk) during fixation with temporary Kirschner wires. (H) On the intraoperative radiograph, temporary Kirshner wires were exchanged for headless compression screws. (I, J) Posteroanterior and lateral immediate postoperative radiographic views. (K-M) Posteroanterior and lateral radiographic views and a coronal computed tomographic scan at 10 weeks after surgery, showing that the lunocapitate interval achieved bony union.
After surgery, the patient wore a short-arm thumb spica splint, and digital exercises were encouraged to reduce swelling. In 2 weeks, a well-molded short-arm thumb spica cast was applied to ensure a functional wrist position for 6 to 8 additional weeks. Patients were restricted from moving their wrist until a computed tomography (CT) scan was performed 8 to 10 weeks postoperatively to confirm the bridging of the bone at the LC interval. Wrist motion and progressive strengthening exercises were then initiated.
Clinical and Radiologic Assessments
According to our treatment protocol, all patients enrolled in this study visited the outpatient clinic preoperatively and postoperatively at 2 weeks, 8 to 10 weeks, 6 months, 1 year, and annually thereafter. Four radiographic views of the wrist, including true wrist images (posteroanterior, lateral, posteroanterior with ulnar deviation, and oblique with 45° pronation), were obtained at each follow-up visit. Patients underwent CT scans of the wrist 10 weeks after surgery to confirm the achievement of bony union. Bony union is defined as the bridging of the bone at the LC interval that is visible in at least three of the long-axis sagittal images.16,20) In the absence of evidence of such a union on the CT scans, the patient was reassessed in 1 month with radiographic images. We took a second CT scan when more consolidation was observed in radiographic images.
Clinical measurements included visual analog scale (VAS) pain score, grip strength, active range of wrist motion, Mayo wrist score (MWS), and the Disabilities of Arm, Shoulder and Hand (DASH) score. One observer who was not involved in patient treatment (HNC) assessed these values preoperatively and postoperatively at 6 months, 1 year, and annually thereafter. The VAS score for wrist pain was defined as the severity of pain experienced by patients and ranged from 0 (no pain) to 10 (worst possible pain). Active flexion-extension and radial-ulnar deviation arcs of the wrist were measured using a handheld goniometer. Grip strength was measured using a Jamar hydraulic dynamometer (Asimov Engineering, Los Angeles, CA, USA). The MWS is a commonly used wrist rating system,16) and its total score ranges between 0 and 100 points, with higher scores indicating better results. This system consists of 4 categories: pain (25 points), active flexion-extension arc as a percentage of the opposite side (25 points), grip strength as a percentage of the opposite side (25 points), and the ability to return to regular employment or activities (25 points). Outcomes are classified as excellent (91–100 points), good (80–90 points), fair (65–79 points), or poor (< 65 points). An excellent or good outcome was regarded as satisfactory, whereas fair and poor outcomes were considered unsatisfactory. The DASH score is based on self-reported answers to a questionnaire designed by Davis et al.,21) which contains 30 items: 21 questions that assess difficulties with specific tasks, 5 questions that evaluate symptoms, and 4 questions that evaluate social function, work function, sleep, and confidence. The DASH score ranges between 0 and 100, with higher scores representing greater upper extremity disability.
Two surgeons (WTO and HJP) measured all radiographic values, using the means for analysis in this study. Radiolucent loosening was determined on plain radiographs and CT images, and the criterion was a radiolucent zone greater than 1 mm around the screws distinguishing false-positive results from normal metal artifacts.22,23) On a plain posteroanterior radiograph, the carpal height ratio was calculated by dividing the carpal height by the length of the third metacarpal bone.24) The carpal height was defined as the distance between the base of the third metacarpal and the subchondral bony cortex of the distal radius. The joint space height ratio was defined as the mid-radiolunate joint length described by Bear et al.25) divided by the capitate length. The mid-radiolunate joint length was determined by measuring the length of a line perpendicular to the volar surface of the lunate facet that connects the lunate to the volar surface of the radius. Postoperative complications and the need for secondary surgery were also reviewed. No patient was recalled to our institution specifically for this study. All data were obtained from medical records, and there was no missing information. We divided the enrolled patients into two groups according to the number of screws needed to fix the LC interval: one screw and two screws. All clinical and radiologic variables described above were compared between the two groups.
Statistical Analysis
Data are presented as the mean (standard deviation) unless otherwise indicated. All statistical computations relied on standard software (R freeware v3.4.3; R Foundation for Statistical Computing, www.r-project.org). The paired t-test or Wilcoxon rank-sum test was used to compare preand postoperative VAS pain score, grip strength, active range of wrist motion, MWS, DASH score, carpal height ratio, and joint space height ratio. The two-sample t-test was applied for group comparisons of union time, VAS pain score, grip strength, active range of wrist motion, MWS, DASH score, carpal height ratio, and joint space height ratio. Fisher’s exact test was used to compare categorical data, such as the number of bone unions, radiolucent loosening, secondary surgeries, and complications. Statistical significance was set at p-value less than 0.05. Power analysis of clinical outcomes was performed with variables with a higher effect size (sample size: 11, significance level: 0.05, type: paired). Power analysis of group comparison between screw numbers was performed with a variable with statistically significant difference (sample size: one screw, 4 and two screws, 6; significance level: 0.05).
RESULTS
Twenty-one patients who underwent arthroscopic scaphoid excision and LC fusion for advanced SLAC or SNAC of the wrist at our institution during the study period were included. Among them, 10 patients were excluded due to previous surgery on the same wrist (n = 4), simultaneous surgery on the ipsilateral wrist (n = 1), inappropriate follow-up (n = 3), and and worker’s compensation (n = 1). A total of 11 patients were enrolled in this study, and their demographic data are shown in Table 1. The average age was 53.9 ± 15.7 years, and the mean follow-up duration was 32.6 ± 8.0 months. The number and type of fixation screws used for arthrodesis are also presented in Table 1.
Table 1. Patient Demographics and Number of Screws Used for Surgical Fixation.
| No. | Age (yr) | Sex | Diagnosis, stage | Symptom duration (mo) | Follow-up (mo) | Number of screws | Screw direction | Threadtype |
|---|---|---|---|---|---|---|---|---|
| 1 | 67 | M | SLAC, stage III | 12 | 30 | 1 | Retrograde | Partial |
| 2 | 58 | F | SNAC, stage II | 18 | 36 | 1 | Retrograde | Partial |
| 3 | 50 | M | SNAC, stage III | 24 | 24 | 1 | Retrograde | Partial |
| 4 | 57 | M | SLAC, stage III | 36 | 48 | 1 | Retrograde | Full |
| 5 | 65 | F | SNAC, stage III | 20 | 24 | 2 | Anterograde/retrograde | Partial/partial |
| 6 | 21 | M | SNAC, stage II | 36 | 36 | 2 | Retrograde/retrograde | Full/full |
| 7 | 65 | M | SNAC, stage II | 15 | 36 | 2 | Anterograde/retrograde | Full/partial |
| 8 | 67 | F | SNAC, stage II | 24 | 24 | 2 | Anterograde/retrograde | Partial/partial |
| 9 | 68 | M | SLAC, stage II | 22 | 24 | 2 | Retrograde/retrograde | Full/partial |
| 10 | 41 | M | SLAC, stage II | 24 | 40 | 2 | Retrograde/retrograde | Full/partial |
| 11 | 34 | F | SLAC, stage III | 36 | 30 | 2 | Retrograde/retrograde | Partial/partial |
SLAC: scapholunate advanced collapse, SNAC: scaphoid nonunion advanced collapse.
All clinical outcomes improved postoperatively (Table 2). Unionization of the LC interval was achieved in all but 1 patient, and the union rate was 90.9%. The patient with nonunion underwent an open 4CF procedure as a secondary surgery. There was improvement in the mean VAS pain score (7.9 ± 1.0 preoperatively to 1.6 ± 0.7 postoperatively, p = 0.003) and grip strength (from 67.5% ± 11.4% preoperatively to 81.8% ± 8.0% postoperatively, p = 0.003) after surgery. The average flexion-extension arc (FEA) and radioulnar deviation arc at the last postoperative follow-up (70.5° ± 14.4° and 34.1° ± 8.9°, respectively) were similar to their preoperative values (67.0° ± 15.4° and 32.3° ± 7.9°, respectively) (p = 0.187 and p = 0.267). The mean MWS and DASH score were 40.9 ± 13.8 and 38.3 ± 8.2, respectively, preoperatively and improved to 75.5 ± 8.2 and 11.3 ± 4.1, respectively, postoperatively (p < 0.001 and p < 0.001). MWS classification showed 1 excellent outcome, 3 good outcomes, 6 fair outcomes, and 1 poor outcome at the last follow-up, and the final satisfaction rate was 36.4% (4 of 11). Power analysis with DASH score (effect size: 1.78) indicated power of 0.96 (sample size: 11, significance level: 0.05).
Table 2. Comparison of Preoperative Values and Postoperative Clinical Outcomes.
| Variable | Preoperative | Postoperative | p-value* |
|---|---|---|---|
| VAS pain score | 7.9 ± 1.0 | 1.6 ± 0.7 | 0.003† |
| Grip strength (%)‡ | 67.5 ± 11.4 | 81.8 ± 8.0 | 0.002† |
| Flexion-extension arc | 67.0 ± 15.4 | 70.5 ± 14.4 | 0.187 |
| Radial-ulnar deviation arc | 32.3 ± 7.9 | 34.1 ± 8.9 | 0.267 |
| Mayo wrist score | 40.9 ± 13.8 | 75.5 ± 8.2 | < 0.001† |
| DASH score | 38.3 ± 8.2 | 11.3 ± 4.1 | < 0.001† |
Values are presented as mean ± standard deviation.
VAS: visual analog scale, DASH: Disabilities of Arm, Shoulder and Hand.
*p-values were calculated using Wilcoxon rank-sum test for categorical values and the paired t-test for continuous values. †p < 0.05. ‡Grip strength was calculated in comparison to the normal contralateral hand.
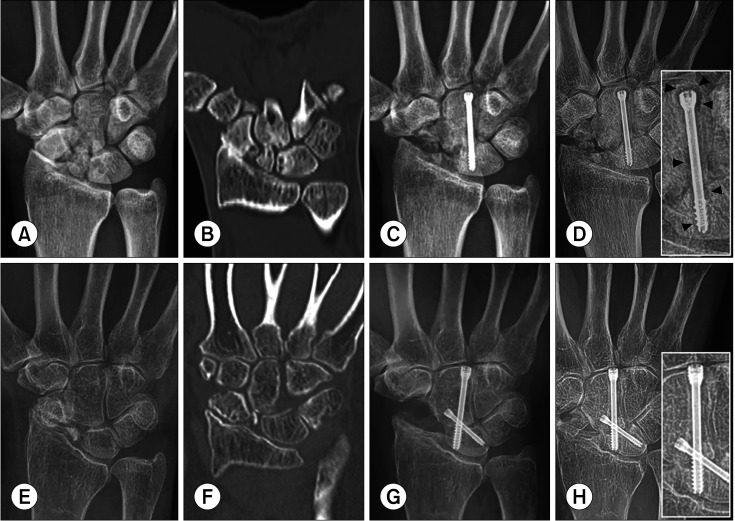
The occurrence of radiolucent loosening around the headless compression screws was 27.3% (3 of 11), including the patient who experienced nonunion, but the other 2 patients with radiographic loosening achieved bony unions (Fig. 2). One of them experienced symptomatic proximal migration of the screw and underwent secondary surgery for screw removal at 12 weeks after the initial procedure (Table 3).
Fig. 2. Arthroscopic lunocapitate (LC) fusion using 1 screw vs. 2 screws. (A, B) Preoperative posteroanterior radiographic and coronal computed tomographic views of a 50-year-old male patient with stage III scaphoid nonunion advanced collapse (SNAC) of the right wrist. (C) Posteroanterior radiographic view taken immediately after arthroscopic LC fusion using 1 screw. (D) Two years after surgery, definite radiolucent loosening (> 1.0 mm of the radiolucent area around the screw: arrowheads) was observed on the posteroanterior radiograph, although the lunocapitate interval achieved bony union. (E, F) Preoperative posteroanterior radiographic and coronal computed tomographic views of a 65-year-old female patient with stage III SNAC of the right wrist. (G) Postoperative posteroanterior radiographic view taken immediately after arthroscopic LC fusion using 2 screws. (H) Two years after surgery, there was no definite radiolucent loosening (< 1.0 mm) on the posteroanterior radiographic view, and the lunocapitate interval achieved bony union.
Table 3. Postoperative Radiologic Outcomes.
| No. | Union | Radiolucent loosening | Preoperative carpal height ratio (1)* | Postoperative carpal height ratio (1)* | Preoperative joint space height ratio (%)† | Postoperative joint space height ratio (%)† | Need for secondary surgery |
|---|---|---|---|---|---|---|---|
| 1‡ | No | Yes | 0.50 | 0.51 | 10.0 | 9.0 | 4CF |
| 2 | Yes | No | 0.59 | 0.57 | 8.0 | 6.0 | No |
| 3 | Yes | Yes | 0.55 | 0.60 | 12.0 | 13.0 | No |
| 4 | Yes | No | 0.46 | 0.46 | 10.0 | 13.0 | No |
| 5 | Yes | Yes | 0.47 | 0.51 | 10.0 | 14.0 | Screw removal§ |
| 6 | Yes | No | 0.48 | 0.42 | 9.0 | 11.0 | No |
| 7 | Yes | No | 0.47 | 0.51 | 8.0 | 10.0 | No |
| 8 | Yes | No | 0.47 | 0.48 | 7.0 | 9.0 | No |
| 9 | Yes | No | 0.55 | 0.48 | 8.00 | 9.0 | No |
| 10 | Yes | No | 0.56 | 0.52 | 8.00 | 10.0 | No |
| 11 | Yes | No | 0.48 | 0.45 | 9.00 | 9.0 | No |
4CF: four-corner fusion.
*Carpal height ratio = carpal height/third metacarpal shaft length. †Joint space height ratio = length between the volar surface of lunate facet and the lunate/capitate length × 100. ‡Postoperative outcomes of this patient (nonunion) were assessed after the secondary surgery. §Removal of the screw due to irritation of the radiolunate joint.
Results of group analyses based on the number of screws are shown in Table 4. Baseline data, including gender, underlying presence of osteoporosis, and the follow-up period, were similar between the groups. Only the frequency of radiolucent loosening was higher in the one-screw group, although the clinical and other radiological variables did not differ between the two groups. Power analysis with radiolucent loosening indicated power of 0.78 (sample size: one screw, 4 and two screws, 6; significance level: 0.05). The calculated sample size of our study when setting the power at 0.8 was over 5.5 in each group. As mentioned earlier, only 1 patient with radiolucent loosening failed to achieve bony union.
Table 4. Comparison of Postoperative Outcomes between Groups.
| Variable | One screw (n = 4) | Two screws (n = 7) | p-value* |
|---|---|---|---|
| Male : female | 3 : 1 | 4 : 3 | 0.999 |
| Underlying osteoporosis | 0 | 1 | 0.999 |
| Follow-up (mo) | 34.5 ± 10.3 | 31.4 ± 7.1 | 0.460 |
| VAS pain score | 2.0 ± 0.8 | 1.4 ± 0.5 | 0.190 |
| Grip strength (%)† | 79.9 ± 6.2 | 83.0 ± 9.1 | 0.561 |
| FEA (°) | 78.8 ± 18.4 | 88.6 ± 16.5 | 0.385 |
| RUA (°) | 43.8 ± 4.8 | 39.3 ± 11.0 | 0.467 |
| MWS | 70.0 ± 7.1 | 78.6 ± 7.5 | 0.096 |
| DASH score | 12.7 ± 3.1 | 10.7 ± 1.3 | 0.964 |
| Union | 3 | 7 | 0.364 |
| Union time (wk)‡ | 12.7 ± 3.1 | 10.7 ± 1.3 | 0.170 |
| Radiolucent loosening | 3 | 0 | 0.024¶ |
| Preoperative carpal height ratio§ | 0.53 ± 0.06 | 0.50 ± 0.04 | 0.362 |
| Postoperative carpal height ratio§ | 0.54 ± 0.06 | 0.48 ± 0.04 | 0.100 |
| Joint space height ratio (%)∥ | 10.3 ± 3.4 | 10.3 ± 1.8 | 0.982 |
| Secondary surgery | 2 | 1 | 0.491 |
| Four-corner fusion | 1 | 0 | 0.364 |
| Screw removal due to irritation | 1 | 1 | 0.999 |
Values are presented as mean ± standard deviation.
VAS: visual analog scale, FEA: flexion-extension arc, RUA: radioulnar deviation arc, MWS: Mayo wrist score, DASH: Disabilities of Arm, Shoulder and Hand.
*p-values were calculated using Fisher’s exact test for categorical variables and the two-sample t-test for continuous variables. †Grip strength was calculated in comparison to the normal contralateral hand. ‡The nonunion patient was excluded from the analysis of union time. §Carpal height ratio = carpal height/third metacarpal shaft length. ∥Joint space height ratio = length between the volar surface of the lunate facet and the lunate/capitate length × 100. ¶p < 0.05.
DISCUSSION
The purpose of this study was to analyze the clinical and radiologic outcomes of arthroscopic scaphoid excision and LC fusion for patients with SLAC or SNAC of the wrist. In our study, this procedure provided acceptable union rates and good clinical outcomes, which could be comparable to those of conventional 4CF reported in other studies. However, radiographic loosening around the headless screws between the lunate and capitate was observed and could be an insidious imminence. With a growing emphasis on the mechanoreceptors of the carpal ligaments and capsule, as well as on their preservation during wrist surgery,12,13) arthroscopic scaphoid excision and LC fusion, performed as a minimally invasive procedure, may be an alternative to 4CF for patients presenting with symptomatic SLAC or SNAC of the wrist.
In our analysis, a bony union between the lunate and capitate was achieved in 90.9% of patients who underwent arthroscopic scaphoid excision and LC fusion. Previously, Baur14) reported a union rate of 71.4% (5 of 7 patients) after mini-open scaphoid excision and arthroscopic LC fusion in 7 patients who presented with symptomatic SLAC or SNAC of the wrist. A review article by Dunn et al.8) reported that open LC fusion could achieve a union rate of 96.2% (77 of 80), which is similar to that of 4CF (union rate of 95% to 97%).4,5) In the currnet study, 2 of the 3 nonunions were fixed with only 1 headless compression screw, whereas only 1 nonunion occurred in patients in whom fixation was performed using 2 headless compression screws. The union rate of arthroscopic LC fusion in our study appears comparable to the currently reported rate of open LC fusion and 4CF. Our finding that nonunion more frequently occurred when fixation was performed using only one screw is also consistent with previous studies.
Preserving the active range of wrist motion after partial arthrodesis is essential to provide patients with better functional outcomes and satisfaction. The FEA in our study averaged 70.5°, similar to results reported in previous open LC fusion studies (63° to 89.3°).9,10,26,27) These values are also comparable to postoperative FEA values reported for 4CF with scaphoid excision, which range from 54° to 89°.28,29,30) A retrospective study by Gaston et al.26) compared open LC fusion and 4CF in 34 patients and showed a statistical difference in FEA values (open LCF was 63° and FCF 73°), although the reported minimal detectable change (MDC) of the wrist FEA was greater than 18° in recent studies.31,32) In a retrospective comparative study of arthroscopic 4CF versus open fusion, Shim et al.15) found that the arthroscopic procedure had a higher FEA (75° vs. 51°), which is larger than the MDC. A well-designed comparative study is needed to demonstrate the advantage of arthroscopic LC fusion in providing a better range of motion than other open procedures.
Both the MWS and DASH score for arthroscopic LC fusion in this study (average MWS: 75.5, DASH score: 10.6) were similar to those of both open LC fusion and 4CF in previously published articles. The mean MWS after open LC fusion has been reported to range from 68 to 89.3, and the DASH score has been shown to average between 7.7 and 17 in previous studies.9,26,27) In additional studies, the mean DASH score after 4CF was found to range from 8 to 28.28) When Gaston et al.26) compared open LC fusion with 4CF in their retrospective study, they did not find a difference in DASH score between these two treatment groups. There are no stratified clinical scores in arthroscopic LC fusion, but Baur found that 71.4% of patients achieved good results, as he had separated patients into only two groups, based on good or bad outcomes.14)
In our study, we observed 3 cases of radiolucent loosening on follow-up radiographs. This loosening could be related to such complications as nonunion, delayed union, or screw migration. One of the 3 cases was related to nonunion, another case required removal of the screw due to joint irritation, and the last case achieved a bony union without any complications within our follow-up period. It appears quite clear that most events of radiolucent loosening result in a critical complication that requires additional surgery. Gaston et al.26) reported on 5 patients with radiolucent loosening of the screws; the screws were removed in all cases because they had migrated and caused joint irritation. Meanwhile, the occurrence rate of a delayed union (or pseudoarthrosis) has been reported to be approximately 1.25%, although it is unknown whether such occurrences were accompanied by radiolucent loosening.8) A longer follow-up study with more participants is needed to clarify the relationship between radiolucent loosening and subsequent complications after LC fusion.
Secondary arthritis after LC fusion in the radiolunate joint is a critical complication, although it may be inevitable. None of our patients experienced secondary arthritis in the radiolunate joint or a significant change in the joint space height ratio. In a 10-year follow-up study, Ferreres et al.9) reported that the incidence of radiolunate joint narrowing, indicating cartilage degeneration, was low. They observed 2 moderate degenerative changes, but both were asymptomatic. One patient in the study by Ferreres et al.9) and 2 in the study by Gaston et al.26) had total wrist arthrodesis not due to secondary arthritis but instead persistent unrelieved pain with idiopathic adjacent bony resorption.
There are some limitations of our study. First, it is a retrospective case study with a relatively small number of patients and no control subjects. It would be hard to argue that arthroscopic LC fusion could provide comparable surgical outcomes to other open methods based on the results of this study. Second, the follow-up period appears insufficient to determine whether there is a relationship between the development of radiolucent loosening and secondary radiolunate arthritis after surgery; thus, longer-term follow-up is required to evaluate this association, as noted above. Third, the material used for intraoperative fixation was inconsistent and differed in both the number of screws and the type of thread pattern used. These features could be confounding factors that considerably affect the outcomes, as an increased incidence of radiolucent loosening was detected in the 1 screw group.
In conclusion, arthroscopic scaphoid excision and LC fusion for patients with advanced SLAC or SNAC of the wrist was effective and safe only in cases fixed with 2 headless compression screws. We recommend arthroscopic LC fusion using 2 screws rather than 1 to decrease radiolucent loosening, which might affect complications such as nonunion, delayed union, or screw migration.
ACKNOWLEDGEMENTS
We would like to thank Ha-Ni Cha (Department of Orthopedic Surgery, Yonsei University College of Medicine) for performing clinical assessments for this study.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Watson HK, Ryu J. Evolution of arthritis of the wrist. Clin Orthop Relat Res. 1986;(202):57–67. [PubMed] [Google Scholar]
- 2.Waitayawinyu T, Pfaeffle HJ, McCallister WV, Nemechek NM, Trumble TE. Management of scaphoid nonunions. Orthop Clin North Am. 2007;38(2):237–249. doi: 10.1016/j.ocl.2007.02.012. [DOI] [PubMed] [Google Scholar]
- 3.Krakauer JD, Bishop AT, Cooney WP. Surgical treatment of scapholunate advanced collapse. J Hand Surg Am. 1994;19(5):751–759. doi: 10.1016/0363-5023(94)90178-3. [DOI] [PubMed] [Google Scholar]
- 4.Enna M, Hoepfner P, Weiss AP. Scaphoid excision with four-corner fusion. Hand Clin. 2005;21(4):531–538. doi: 10.1016/j.hcl.2005.08.012. [DOI] [PubMed] [Google Scholar]
- 5.Bain GI, Watts AC. The outcome of scaphoid excision and four-corner arthrodesis for advanced carpal collapse at a minimum of ten years. J Hand Surg Am. 2010;35(5):719–725. doi: 10.1016/j.jhsa.2010.01.025. [DOI] [PubMed] [Google Scholar]
- 6.Kirschenbaum D, Schneider LH, Kirkpatrick WH, Adams DC, Cody RP. Scaphoid excision and capitolunate arthrodesis for radioscaphoid arthritis. J Hand Surg Am. 1993;18(5):780–785. doi: 10.1016/0363-5023(93)90042-2. [DOI] [PubMed] [Google Scholar]
- 7.Siegel JM, Ruby LK. A critical look at intercarpal arthrodesis: review of the literature. J Hand Surg Am. 1996;21(4):717–723. doi: 10.1016/S0363-5023(96)80037-2. [DOI] [PubMed] [Google Scholar]
- 8.Dunn JC, Polmear MM, Scanaliato JP, Orr JD, Nesti LJ. Capitolunate arthrodesis: a systematic review. J Hand Surg Am. 2020;45(4):365. doi: 10.1016/j.jhsa.2019.10.007. [DOI] [PubMed] [Google Scholar]
- 9.Ferreres A, Garcia-Elias M, Plaza R. Long-term results of lunocapitate arthrodesis with scaphoid excision for SLAC and SNAC wrists. J Hand Surg Eur Vol. 2009;34(5):603–608. doi: 10.1177/1753193409105683. [DOI] [PubMed] [Google Scholar]
- 10.Giannikas D, Karageorgos A, Karabasi A, Syggelos S. Capitolunate arthrodesis maintaining carpal height for the treatment of SNAC wrist. J Hand Surg Eur Vol. 2010;35(3):198–201. doi: 10.1177/1753193409352280. [DOI] [PubMed] [Google Scholar]
- 11.Ho PC. Arthroscopic partial wrist fusion. Tech Hand Up Extrem Surg. 2008;12(4):242–265. doi: 10.1097/BTH.0b013e318190244b. [DOI] [PubMed] [Google Scholar]
- 12.Hagert E, Forsgren S, Ljung BO. Differences in the presence of mechanoreceptors and nerve structures between wrist ligaments may imply differential roles in wrist stabilization. J Orthop Res. 2005;23(4):757–763. doi: 10.1016/j.orthres.2005.01.011. [DOI] [PubMed] [Google Scholar]
- 13.Hagert E, Lluch A, Rein S. The role of proprioception and neuromuscular stability in carpal instabilities. J Hand Surg Eur Vol. 2016;41(1):94–101. doi: 10.1177/1753193415590390. [DOI] [PubMed] [Google Scholar]
- 14.Baur EM. Arthroscopic-assisted partial wrist arthrodesis. Hand Clin. 2017;33(4):735–753. doi: 10.1016/j.hcl.2017.07.013. [DOI] [PubMed] [Google Scholar]
- 15.Shim JW, Kim JW, Park MJ. Comparative study between open and arthroscopic techniques for scaphoid excision and four-corner arthrodesis. J Hand Surg Eur Vol. 2020;45(9):952–958. doi: 10.1177/1753193420908820. [DOI] [PubMed] [Google Scholar]
- 16.Oh WT, Kang HJ, Chun YM, Koh IH, Lee YJ, Choi YR. Retrospective comparative outcomes analysis of arthroscopic versus open bone graft and fixation for unstable scaphoid nonunions. Arthroscopy. 2018;34(10):2810–2818. doi: 10.1016/j.arthro.2018.04.024. [DOI] [PubMed] [Google Scholar]
- 17.Kang HJ, Chun YM, Koh IH, Park JH, Choi YR. Is arthroscopic bone graft and fixation for scaphoid nonunions effective? Clin Orthop Relat Res. 2016;474(1):204–212. doi: 10.1007/s11999-015-4495-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shepard NA, Rush AJ, 3rd, Scarborough NL, Carter AJ, Phillips FM. Demineralized bone matrix in spine surgery: a review of current applications and future trends. Int J Spine Surg. 2021;15(s1):113–119. doi: 10.14444/8059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sherman AE, Mehta MP, Nayak R, et al. Biologic augmentation of tibiotalocalcaneal arthrodesis with allogeneic bone block is associated with high rates of fusion. Foot Ankle Int. 2022;43(3):353–362. doi: 10.1177/10711007211041336. [DOI] [PubMed] [Google Scholar]
- 20.Corrales LA, Morshed S, Bhandari M, Miclau T., 3rd Variability in the assessment of fracture-healing in orthopaedic trauma studies. J Bone Joint Surg Am. 2008;90(9):1862–1868. doi: 10.2106/JBJS.G.01580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Davis AM, Beaton DE, Hudak P, et al. Measuring disability of the upper extremity: a rationale supporting the use of a regional outcome measure. J Hand Ther. 1999;12(4):269–274. doi: 10.1016/s0894-1130(99)80063-5. [DOI] [PubMed] [Google Scholar]
- 22.Wu X, Shi J, Wu J, et al. Pedicle screw loosening: the value of radiological imagings and the identification of risk factors assessed by extraction torque during screw removal surgery. J Orthop Surg Res. 2019;14(1):6. doi: 10.1186/s13018-018-1046-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Spirig JM, Sutter R, Gotschi T, Farshad-Amacker NA, Farshad M. Value of standard radiographs, computed tomography, and magnetic resonance imaging of the lumbar spine in detection of intraoperatively confirmed pedicle screw loosening-a prospective clinical trial. Spine J. 2019;19(3):461–468. doi: 10.1016/j.spinee.2018.06.345. [DOI] [PubMed] [Google Scholar]
- 24.Youm Y, McMurthy RY, Flatt AE, Gillespie TE. Kinematics of the wrist. I: an experimental study of radial-ulnar deviation and flexion-extension. J Bone Joint Surg Am. 1978;60(4):423–431. [PubMed] [Google Scholar]
- 25.Bear DM, Moloney G, Goitz RJ, Balk ML, Imbriglia JE. Joint space height correlates with arthroscopic grading of wrist arthritis. Hand (N Y) 2013;8(3):296–301. doi: 10.1007/s11552-013-9522-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gaston RG, Greenberg JA, Baltera RM, Mih A, Hastings H. Clinical outcomes of scaphoid and triquetral excision with capitolunate arthrodesis versus scaphoid excision and four-corner arthrodesis. J Hand Surg Am. 2009;34(8):1407–1412. doi: 10.1016/j.jhsa.2009.05.018. [DOI] [PubMed] [Google Scholar]
- 27.Hegazy G. Capitolunate arthrodesis for treatment of scaphoid nonunion advanced collapse (SNAC) wrist arthritis. J Hand Microsurg. 2015;7(1):79–86. doi: 10.1007/s12593-015-0182-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wagner ER, Werthel JD, Elhassan BT, Moran SL. Proximal row carpectomy and 4-corner arthrodesis in patients younger than age 45 years. J Hand Surg Am. 2017;42(6):428–435. doi: 10.1016/j.jhsa.2017.03.015. [DOI] [PubMed] [Google Scholar]
- 29.Merrell GA, McDermott EM, Weiss AP. Four-corner arthrodesis using a circular plate and distal radius bone grafting: a consecutive case series. J Hand Surg Am. 2008;33(5):635–642. doi: 10.1016/j.jhsa.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 30.Draeger RW, Bynum DK, Jr, Schaffer A, Patterson JM. Bicolumnar intercarpal arthrodesis: minimum 2-year follow-up. J Hand Surg Am. 2014;39(5):888–894. doi: 10.1016/j.jhsa.2014.01.023. [DOI] [PubMed] [Google Scholar]
- 31.Reissner L, Fischer G, List R, Taylor WR, Giovanoli P, Calcagni M. Minimal detectable difference of the finger and wrist range of motion: comparison of goniometry and 3D motion analysis. J Orthop Surg Res. 2019;14(1):173. doi: 10.1186/s13018-019-1177-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lameijer CM, Ten Duis HJ, Haag CM, El Moumni M, van der Sluis CK. The evolution of radiological measurements and the association with clinician and patient reported outcome following distal radius fractures in non-osteoporotic patients: what is clinically relevant? Disabil Rehabil. 2021;43(26):3777–3788. doi: 10.1080/09638288.2020.1753247. [DOI] [PubMed] [Google Scholar]