Abstract
Background
frailty is a condition of reduced function and health due to ageing processes and is associated with a higher risk of falls, hospitalisation, disability and mortality.
Objective
to determine the relationship between household wealth and neighbourhood deprivation with frailty status, independently of demographic factors, educational attainment and health behaviours.
Design
population-based cohort study.
Setting
communities in England.
Subjects
in total 17,438 adults aged 50+ from the English Longitudinal Study of Ageing.
Methods
multilevel mixed-effects ordered logistic regression was used in this study. Frailty was measured using a frailty index. We defined small geographic areas (neighbourhoods) using English Lower layer Super Output Areas. Neighbourhood deprivation was measured by the English Index of Multiple Deprivation, grouped into quintiles. Health behaviours included in this study are smoking and frequency of alcohol consumption.
Results
the proportion of respondents who were prefrail and frail were 33.8% [95% confidence interval (CI) 33.0–34.6%] and 11.7 (11.1–12.2)%, respectively. Participants in the lowest wealth quintile and living in the most deprived neighbourhood quintile had 1.3 (95% CI = 1.2–1.3) and 2.2 (95% CI = 2.1–2.4) times higher odds of being prefrail and frail, respectively, than the wealthiest participants living in the least deprived neighbourhoods Living in more deprived neighbourhood and poorer wealth was associated with an increased risk of becoming frail. Those inequalities did not change over time.
Conclusions
in this population-based sample, living in a deprived area or having low wealth was associated with frailty in middle-aged and older adults. This relationship was independent of the effects of individual demographic characteristics and health behaviours.
Keywords: household wealth, neighbourhood deprivation, frailty, English Longitudinal Study of Ageing, health inequalities, older people
Key points
The most disadvantaged individuals have 2.2 times higher odds of being frail than the most advantaged ones.
Living in more deprived neighbourhood and poorer wealth was associated with an increased risk of becoming frail.
The relationships between individual wealth, household deprivation and frailty did not change over time.
Introduction
As the world population ages, frailty places an increasingly substantial burden on health and wellbeing amongst older people [1]. Frailty is an age-related condition characterised by increased vulnerability to stressor events resulting from a decline in physiologic and cognitive reserves and function [2, 3]. A recent review identified that 49 and 24% of people aged 50 years and older from 62 countries were prefrail and frail, respectively [1]. Frailty is associated with adverse health outcomes, such as falls, need for long-term care, hospitalisation and death [4–6]. Understanding the factors that are associated with frailty is thus important for identifying the target populations for interventions to prevent frailty.
The existence of socioeconomic inequalities in frailty are well established [7–11]. Lower educational attainment, income and wealth have been associated with a higher risk of frailty in different regions and populations [10]. Using longitudinal data from the Whitehall II study, Brunner et al. showed that the higher prevalence of frailty amongst individuals with low economic status in the UK is partly explained by behavioural and cardiometabolic risk factors [9]. Other studies have identified an association between increased neighbourhood deprivation and an increased risk of frailty [4, 7, 12]. A study using UK Biobank found that adults aged 37–73 years living in areas in the most socio-economically deprived quintile were more likely to be frail after adjusting for individual income [4].
Some limitations are evident in the literature. First, relatively little is known on how socioeconomic conditions at the individual and neighbourhood level may act together to influence frailty. We have previously reported substantial differences in prefrailty and frailty between local authority districts in England [11]. Second, a prior study suggesting an association between individual and neighbourhood socioeconomic factors and frailty [7] relied on a cross-sectional data. Finally, that study did not consider the impact of individual health behaviours [7], such as smoking and physical activity, which are known to influence the occurrence of frailty and may mediate the link between individual and neighbourhood socioeconomic factors and health [13, 14]. Previous work has demonstrated differences in health behaviours (including smoking and physical activity) amongst individuals with low socioeconomic status between those who live in deprived areas and those who live in less deprived areas [15]. To fill these gaps, this study aimed to determine whether household wealth and neighbourhood deprivation are related to frailty independently of the effects of demographic, socioeconomic and health behaviours. To achieve this aim, we used eight waves of the English Longitudinal Study of Ageing (ELSA), taken at ⁓2-year intervals from 2002 to 2017, which allow us to use assessment over time.
Methods
Study design and participants
We analysed data from ELSA, a nationally representative prospective cohort study of people aged 50 years and older living in England [16]. Details of the study design are given elsewhere [17]. In this analysis, we used data from ELSA waves 1–8 (covering 2002–2017) [18]. We did not include the final wave of ELSA (Wave 9) as the information on Index of Multiple Deprivation (IMD) was not available for this wave at the time of this study. The original sample of ELSA consisted of 11,391 participants, with occasional refreshment samples recruited to maintain the representation of people aged 50–53 years.
Frailty measures
Frailty was defined according to a frailty index (FI) previously described by Wade et al. [19]. It comprised 60 variables (‘deficits’) representing conditions that accumulate with age and are associated with adverse outcomes, including disability, mobility and sensory impairments, cognitive function and chronic diseases. The 60 variables are presented in Supplementary Table 1.
Although the deficits used to construct an individual FI vary between studies (depending in part on data availability) there is evidence that relative fitness and frailty (in relation to the accumulation of deficits with age) are closely comparable across countries and are highly correlated with mortality [20]. An individual’s FI score is given by the fraction of deficits they present. Although FI scores are determined on a continuous scale, prior studies show that subdivided FIs are associated with institutionalisation [21] and mortality [22]. We categorised the FI into robust (≤0.08), prefrailty (>0.08 and <0.25) and frailty (≥0.25) [22, 23].
Household wealth
Household wealth was measured as net total wealth of a benefit unit and comprises the sum of savings and investments after financial debt has been subtracted. A benefit unit is defined as a single adult or a married or cohabiting couple and any dependent children [24]. We split household wealth into quintiles to demonstrate hierarchical effects of wealth.
Neighbourhood deprivation
Deprivation was measured by the English IMD, grouped into quintiles [18, 25]. The IMD comprises seven domains of deprivation measured at the Lower layer Super Output Area (LSOA) level, including (i) income deprivation, (ii) employment deprivation, (iii) education, skills and training deprivation, (iv) health and disability deprivation, (v) crime, (vi) barriers to housing and services and (vii) living environment deprivation. LSOAs were additionally categorised as urban or rural based upon population density and settlement size [26].
Covariates
Information on socioeconomic factors, demographic factors and health behaviours was obtained by questionnaire [4, 7, 13, 27]. Covariates included age, sex (a binary variable with male as reference), ethnicity (a binary variable with white as reference), and marital status (married as the reference, other categories: single, divorced and widowed) and wealth. We categorised age into four groups (50–59; 60–69; 70–79; 80+). Smoking status was categorised as non-smoker, past smoker and current smoker. We categorised the frequency of alcohol consumption: not at all; 4 days a week or fewer and 5 days a week or more.
Statistical analyses
We performed multilevel mixed-effects ordered logistic regression models to assess the longitudinal relationship between neighbourhood deprivation and frailty status. We performed analyses with three models, comprising different sets of covariates: (i) a simple adjustment (age, sex, ethnicity and area deprivation covariates only); (ii) adjustment as in Model 1 plus adjustment for individual wealth and (iii) adjustment as in Model 2 plus adjustment for education attainment, marital status, smoking behaviour and drinking behaviour. Separate analyses were also conducted with Model 3 for males and females [28]. A possible interaction between household wealth and area deprivation was also explored with Model 3. We further evaluated how wealth inequalities in the incidence of frailty changed over time, by including the interaction between wealth and wave groups (waves 1–4 and waves 5–8).
Finally, we identified the association between household wealth and neighbourhood deprivation at baseline and the risk of frailty over a 15-year period adjusted for the covariates using a Cox proportional hazard model with survey wave as the time scale. Missing data on the FI variables and covariates were determined using multivariate imputation by chained equations [29]. Twenty imputation datasets were created [30, 31]. Survey weight was used in all analyses. Model fitting was conducted with Stata 17 [32]. Further details are included in Supplementary File 1.
Sensitivity analysis
We performed two sensitivity analyses to assess the robustness of our findings (Supplementary File 2). The first comprised analysing the original data without imputation. The second investigated the effect of area type (urban vs rural) on the risks of having prefrailty or frailty. This utilised ELSA waves 6–8, as the Census 2011 rural–urban indicators were not available for earlier waves [17].
Results
In total 17,438 respondents contributed data to the analysis. Baseline characteristics of these participants are summarised in Table 1. The mean age of the respondents at baseline was 65.1 [standard deviation (SD) = 10.4] years. The proportions of respondents who were prefrail and frail using weighted estimates imputed for missing data were 33.8% [95% confidence interval (CI) 33.0–34.6%] frail and 11.7 (95% CI 11.1–12.2)% prefrail. The proportion of respondents who were prefrail and frail by demographic, socioeconomic and health behaviour status is shown in Table 1. Most notably, only 3.7 (3.0–4.4)% of the wealthiest quintile were frail, compared with 20.9 (19.4–22.3)% of the least wealthiest quintile. Table 1 is further described in Supplementary File 3.
Table 1.
Descriptive baseline characteristics and proportion of prefrail and frail adults aged 50 and older in England at baseline. *unweighted frequency (%), original data; **weighted proportion (95% CI), estimated using multiple imputation for missing variables
| Characteristic | Total* | Prefrail** | Frail** |
|---|---|---|---|
| Individual characteristics | |||
| FI, mean (SD) | 0.11 (0.11) | ||
| Frailty status | |||
| Robust | 9,338 (53.6) | ||
| Prefrail | 6,062 (34.8) | 0.338 (0.330–0.346) | |
| Frail | 2,032 (11.7) | 0.117 (0.111–0.122) | |
| Age, mean (SD) | 65.1 (10.4) | ||
| Age group | |||
| 50–59 | 8,505 (48.8) | 0.252 (0.241–0.684) | 0.075 (0.069–0.082) |
| 60–69 | 4,562 (26.2) | 0.361 (0.346–0.542) | 0.112 (0.103–0.122) |
| 70–79 | 3,077 (17.7) | 0.506 (0.487–0.350) | 0.161 (0.148–0.175) |
| 80+ | 1,200 (6.9) | 0.523 (0.493–0.200) | 0.299 (0.272–0.552) |
| Sex | |||
| Men | 8,087 (46.4) | 0.289 (0.277–0.300) | 0.096 (0.045–0.103) |
| Women | 9,351 (53.6) | 0.383 (0.372–0.394) | 0.135 (0.127–0.143) |
| Ethnicity | |||
| White | 16,726 (95.9) | 0.332 (0.288–0.376) | 0.133 (0.101–0.164) |
| Non-white | 712 (4.1) | 0.338 (0.330–0.346) | 0.116 (0.110–0.121) |
| Education | |||
| Less than high school | 7,086 (40.6) | 0.385 (0.372–0.398) | 0.182 (0.172–0.192) |
| High school | 2,890 (16.6) | 0.318 (0.298–0.337) | 0.074 (0.062–0.085) |
| College or higher | 7,462 (42.8) | 0.297 (0.285–0.308) | 0.064 (0.058–0.071) |
| Marital status | |||
| Single | 1,126 (6.4) | 0.330 (0.299–0.361) | 0.139 (0.115–0.164) |
| Married | 11,964 (68.6) | 0.311 (0.302–0.320) | 0.084 (0.079–0.090) |
| Separated/divorced | 2,068 (11.8) | 0.331 (0.308–0.354) | 0.146 (0.129–0.163) |
| Widowed | 2,276 (13.1) | 0.487 (0.465–0.508) | 0.239 (0.220–0.257) |
| Wealth | |||
| 1st quintile (least wealthy) | 3,910 (22.4) | 0.360 (0.343–0.378) | 0.209 (0.194–0.223) |
| 2nd | 3,315 (19.0) | 0.377 (0.359–0.396) | 0.146 (0.133–0.159) |
| 3rd | 3,287 (18.8) | 0.345 (0.326–0.362) | 0.097 (0.087–0.108) |
| 4th | 3,280 (18.8) | 0.324 (0.307–0.342) | 0.057 (0.049–0.065) |
| 5th (most wealthy) | 3,278 (18.8) | 0.271 (0.255–0.287) | 0.037 (0.030–0.044) |
| Smoking behaviour | |||
| Non-smoker | 6,298 (36.1) | 0.297 (0.284–0.310) | 0.090 (0.082–0.098) |
| Past smoker | 8,030 (46.1) | 0.357 (0.346–0.368) | 0.121 (0.113–0.129) |
| Current smoker | 3,110 (17.8) | 0.374 (0.354–0.393) | 0.159 (0.144–0.173) |
| Drinking frequency | |||
| Not at all | 1,793 (10.2) | 0.398 (0.373–0.424) | 0.275 (0.252–0.298) |
| Drink 4 days a week or fewer | 9,245 (53.0) | 0.350 (0.340–0.362) | 0.107 (0.101–0.114) |
| Drink 5 days a week or more | 4.921 (28.2) | 0.289 (0.275–0.303) | 0.071 (0.063–0.079) |
| Area characteristics | |||
| Area deprivation | |||
| 1st quintile (most deprived) | 2,600 (14.9) | 0.401 (0.380–0.422) | 0.220 (0.202–0.239) |
| 2nd | 3,149 (18.1) | 0.366 (0.347–0.385) | 0.147 (0.134–0.161) |
| 3rd | 3,623 (20.8) | 0.345 (0.328–0.362) | 0.107 (0.097–0.118) |
| 4th | 4,023 (23.1) | 0.309 (0.293–0.325) | 0.086 (0.076–0.095) |
| 5th (least deprived) | 4,041 (23.2) | 0.295 (0.279–0.310) | 0.060 (0.052–0.068) |
Influence of household wealth and neighbourhood deprivation on the risk of having prefrailty or frailty over 15 years
Model 1 shows a gradient effect of neighbourhood deprivation on the risk of being prefrail or frail over 15 years (Table 2). Adjusting for age, sex and ethnicity, the expected odds of being frail and prefrail as compared with robust, or frail as compared with prefrail and robust, were almost seven times higher [Adjusted Odds Ratio (AOR) = 6.9; 95% CI 5.9–8.2] amongst respondents who lived in the most deprived neighbourhood quintile than those who lived in the least deprived neighbourhood quintile. Respondents who lived in the fourth-least, third-least and second-least deprived neighbourhood quintiles had 3.4 (95% CI 3.0–3.9), 1.9 (95% CI 1.7–2.1) and 1.3 (95% CI 1.2–1.5) times higher odds of being prefrail as compared with robust (or frail as compared with prefrail) than those living in the least deprived neighbourhood quintile, respectively. The significant relationships between neighbourhood deprivation and prefrailty or frailty were attenuated for all neighbourhood deprivation groups after we included household wealth in the analysis (Model 2).
Table 2.
Multilevel mixed-effects ordered logistic regression showing the odds ratio (and 95% CI) of older adults being prefrail or frail, missing data imputed. Source: ELSA waves 1–8
| Model 1 | Model 2 | Model 3 | |
|---|---|---|---|
| Wealth, reference: 5th | |||
| 4th quintile (most wealthy) | 1.25 (1.14; 1.37) | 1.17 (1.07; 1.28) | |
| 3rd | 1.56 (1.42; 1.72) | 1.39 (1.27; 1.53) | |
| 2nd | 2.11 (1.90; 2.34) | 1.76 (1.58; 1.95) | |
| 1st (least wealthy) | 3.36 (2.98; 3.79) | 2.64 (2.35; 2.98) | |
| Area deprivation, reference: 5th | |||
| 4th quintile (least deprived) | 1.30 (1.17; 1.45) | 1.26 (1.14; 1.41) | 1.19 (1.07; 1.32) |
| 3rd | 1.88 (1.66; 2.13) | 1.72 (1.53; 1.94) | 1.50 (1.33; 1.70) |
| 2nd | 3.39 (2.96; 3.88) | 2.85 (2.50; 3.26) | 2.25 (1.97; 2.57) |
| 1st (most deprived) | 6.99 (5.94; 8.22) | 5.34 (4.58; 6.32) | 3.70 (3.15; 4.34) |
Notes: Model 1 is adjusted for age, gender, ethnicity and area deprivation. Model 2 is adjusted for age, gender, ethnicity, wealth and area deprivation. Model 3 is adjusted for age, gender, ethnicity, education level, marital status, smoking and drinking behaviour, wealth and area deprivation. Details in Supplementary Table 2.
A gradient of the risk of being prefrail or frail also exists for household wealth. Independently of where a person lives, increased wealth decreases their odds of prefrailty or frailty. Wealth is associated with increased prefrailty or frailty across wealth quintiles: the least wealthy quintile had 3.4 times higher odds of being prefrail or frail than the most wealthy quintile (95% CI 3.0–3.8). The fourth-most (AOR = 2.1; 95% CI = 1.9–2.3), third-most (AOR = 1.6; 95% CI = 1.4–1.7) and second-most wealthy households (AOR = 1.3; 95% CI = 1.1–1.4) are associated with greater odds of being prefrail or frail relative to the wealthiest quintile independently of neighbourhood deprivation. The associations between frailty status and the covariates are further explained in Supplementary File 4.
Frailty by household wealth and neighbourhood deprivation
Figure 1 shows the AOR of being prefrail and frail over 15 years according to household wealth and neighbourhood deprivation based on Model 3 (adjusted for the covariates). The reference is the most wealthy respondents who lived in the least deprived neighbourhood. A person in the lowest wealth quintile and living in the most deprived neighbourhood quintile had 1.3 (95% CI 1.2–1.3) and 2.2 (95% CI 2.1–2.4) times higher odds of being prefrail and frail over time, respectively, than the wealthiest person living in the least deprived neighbourhoods (Figure 1).
Figure 1.
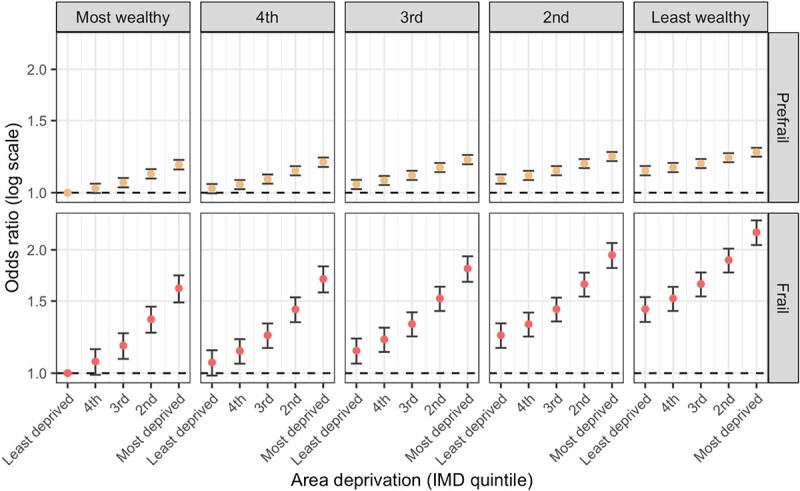
AORs of prefrailty and frailty for each deprivation quintiles, relative to the most advantage individuals (the most wealthy living in the least deprived areas). Models are adjusted for age, gender, ethnicity, education level, marital status, smoking and drinking behaviour. Error bars show 95% CI. Source: ELSA waves 1–8.
Supplementary Figure 1 is similar to Figure 1, but additionally included the interactions between wealth and neighbourhood deprivation. No significant differences appear in the links between household wealth and neighbourhood deprivation with the odds of being prefrail and frail in other groups after we included the interactions between household wealth and neighbourhood deprivation quintiles in the analysis.
We repeated the model separately for men and women (see Figure 2). The magnitude of the associations appeared greater for prefrailty with men and frailty with women. Men in the lowest wealth quintiles and living in the most deprived neighbourhoods had 1.4 (95% CI 1.3–1.5) and 2.0 (95% CI 1.8–2.1) times higher odds of being prefrail and frail, respectively, than the wealthiest men who lived in the least deprived neighbourhoods. For women, these odds ratios were 1.2 (95% CI 1.1–1.2) and 2.5 (95% CI 2.1–2.9), respectively.
Figure 2.
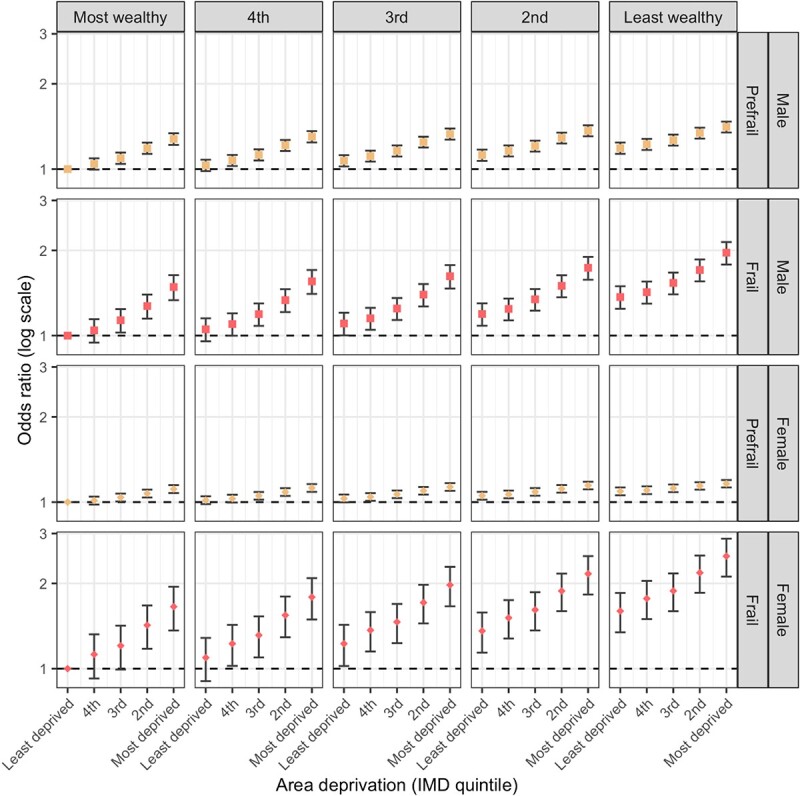
AOR of having prefrailty or frailty by wealth and deprivation (IMD) quintile, for men (squares) and women (diamonds). Models are adjusted for age, gender, ethnicity, education level, marital status, smoking and drinking behaviour. Error bars show 95% CI. Source: ELSA waves 1–8.
A Kaplan–Meier curves analysis for unadjusted rates of incident frailty shows differences in risk according to household wealth (Supplementary Figure 2A) and neighbourhood deprivation (Supplementary Figure 2B). Table 3 shows that respondents living in less wealthy households and in more deprived areas are more likely to be prefrail or frail, and also to become prefrail or frail. The odds ratio for frailty between the least wealthy and wealthiest quintiles was 1.8 [1.5–2.3] during waves 1–4 and 2.2 [1.3–2.8] during waves 5–8 (Supplementary File 5 and Supplementary Table 3). The ratio of these odds ratios is 2.2/1.8 = 1.20 [95% CI 0.7–1.8]. This ratio indicates that there is no evidence that the gap between the wealthiest and least wealthy changed over the course of ELSA waves 1–8.
Table 3.
Survival analysis showing the association between household wealth, neighbourhood deprivation and the risk of frailty
| Unadjusted hazard ratio (95% CI) | Adjusted hazard ratio (95% CI) | ||
|---|---|---|---|
| Model 1 | Model 2 | ||
| Individual characteristics | |||
| Age | 1.08 (1.08; 1.09) | 1.08 (1.07; 1.08) | 1.08 (1.07; 1.09) |
| Female | 1.28 (1.17; 1.41) | 1.20 (1.09; 1.32) | 1.23 (1.12; 1.36) |
| Non-white | 0.60 (0.47; 0.77) | 0.61 (0.47; 0.79) | 0.61 (0.46; 0.78) |
| Education, reference: less than high school | |||
| High school | 0.53 (0.47; 0.61) | 0.89 (0.77; 1.02) | 0.91 (0.79; 1.05) |
| College or higher | 0.48 (0.43; 0.53) | 0.85 (0.76; 0.94) | 0.88 (0.78; 0.98) |
| Marital status, reference: married | |||
| Single | 1.35 (1.11; 1.65) | 1.13 (0.93; 1.38) | 1.13 (0.93; 1.39) |
| Separated/divorced | 1.16 (0.99; 1.36) | 1.11 (0.95; 1.30) | 1.11 (0.95; 1.30) |
| Widowed | 2.65 (2.39; 2.94) | 1.08 (0.96; 1.22) | 1.08 (0.95; 1.22) |
| Smoking behaviour, reference: non-smoker | |||
| Past smoker | 1.18 (1.06; 1.30) | 1.20 (1.08; 1.34) | |
| Active smoker | 1.37 (1.20; 1.56) | 1.62 (1.41; 1.86) | |
| Drinking behaviour, reference: Not at all | |||
| Drink alcohol 4 days a week or less | 0.50 (0.44; 0.57) | 0.72 (0.63; 0.82) | |
| Drink alcohol 5 days a week or more | 0.43 (0.37; 0.50) | 0.71 (0.61; 0.83) | |
| Wealth, reference: 5th (most wealthy) | |||
| 4th quintile | 1.26 (1.07; 1.47) | 1.17 (0.99; 1.36) | 1.14 (0.97; 1.34) |
| 3rd | 1.82 (1.57; 2.11) | 1.42 (1.22; 1.66) | 1.41 (1.21; 1.64) |
| 2nd | 2.38 (2.05; 2.75) | 1.58 (1.35; 1.85) | 1.51 (1.29; 1.77) |
| 1st (least wealthy) | 2.31 (1.98; 2.68) | 2.01 (1.71; 2.37) | 1.86 (1.58; 2.21) |
| Area characteristics | |||
| Area deprivation, reference: 5th (least deprived) | |||
| 4th quintile | 2.33 (2.01; 2.70) | 1.20 (1.04; 1.38) | 1.19 (1.03; 1.37) |
| 3rd | 1.73 (1.50; 2.00) | 1.24 (1.07; 1.44) | 1.22 (1.05; 1.42) |
| 2nd | 1.40 (1.21; 1.62) | 1.42 (1.22; 1.65) | 1.36 (1.17; 1.59) |
| 1st (most deprived) | 1.32 (1.15; 1.52) | 1.61 (1.37; 1.90) | 1.50 (1.27; 1.77) |
Notes: Model 1 is adjusted for age, gender, ethnicity, education level, marital status, wealth and area deprivation. Model 2 is adjusted for age, gender, ethnicity, education level, marital status, smoking and drinking behaviour, wealth and area deprivation.
The sensitivity analysis using data without imputing missing values shows the same pattern of findings, namely that both lower individual wealth and living in a deprived area are independently associated with higher odds of being prefrail or frail (Supplementary Table 4). The second sensitivity analysis shows that living in urban areas is not associated with an increased odds of prefrailty or frailty (Supplementary Table 5).
Discussion
This study provides evidence on longitudinal relationships between household wealth, neighbourhood deprivation and the risk of prefrailty and frailty amongst middle-aged and older people in England. Using frailty measures repeated over 15 years, individuals who are less wealthy and live in more deprived areas are more likely to become prefrail or frail and have higher risks of being prefrail/frail. This finding was robust to adjustment for a range of potential covariates, including health behaviours. This data strengthens the evidence base linking area deprivation and higher levels of mental and physical ill-health amongst older people [7, 33, 34].
The relationship between neighbourhood deprivation, less healthy lifestyles and higher mortality rates is well established [35, 36]. Our findings extend the literature showing that the relationship between area deprivation and the risk of prefrailty and frailty is not explained by differences in individual socioeconomic circumstances, smoking or alcohol consumption.
Other possible causes for the observed relationship between area deprivation and frailty include both the physical environment (e.g. environmental degradation and proximity to major roads [37]) and the characteristics of the neighbourhood (e.g. perceived safety [38], poor health is associated with increased high school dropout rates [39]). We found no evidence of an association between urban status and frailty after adjusting for demographic, socioeconomic, health behaviour and neighbourhood deprivation. However, we used only three waves of the ELSA for the urban–rural analysis due to limitation on the data availability. Further research with a longer follow-up is needed to determine the extent to which these factors may contribute.
Our data confirm that the poorest individuals who live in the most deprived areas are at the highest risk of prefrailty and frailty. The results suggest that the least advantaged people (i.e. in the least wealthy and most deprived area quintiles) were 1.3 and 2.2 times more likely to be prefrail and frail (Figure 1), respectively, compared with the most advantaged (i.e. the most wealthy in the least deprived areas), taking into account demographic, education, marital status and health behaviours. The wealthiest respondents living in the most deprived areas had 1.5 (95% CI 1.4–1.6) higher odds of being prefrail or frail over 15 years than the wealthiest respondents living in the least deprived areas. Those significant associations persisted when we added interactions between individual wealth and neighbourhood deprivation quintiles, suggesting that there is no multiplicative effect modification on the link between individual wealth and neighbourhood deprivation on frailty [40].
We did not find evidence in our data that the inequality in frailty incidence between the wealthiest and least wealthy has changed over time, despite the impact of austerity in the second half of our data set [41, 42]. It is possible that the impact of austerity has not yet manifested in frailty prevalence.
The findings have potentially important public health implications. Data from systematic review studies suggest that frailty is a strong predictor of hospitalisation and mortality [43, 44]. For example, in one previous report an increase of 0.1 in FI score was associated with a 28% higher odds of death [43]. The odds of having prefrailty or frailty were highest in the most deprived neighbourhood. Consequently, targeting the 20% most deprived neighbourhoods provides the best opportunity to benefit from interventions, as these areas present the greatest opportunity for change. National Health Service (NHS) England assesses all patients aged 65 years and older for features of frailty [45]. Patients in deprived areas with, or at risk for, frailty could be offered interventions including advice on physical activity and exercise for older people [46].
Another approach to prevention would be to target the least wealthy, wherever they live. The odds of having prefrailty or frailty in middle-aged and older adults decrease markedly between the least wealthy quintile and three most wealthy quintiles. As middle-aged and older adults in the lowest wealth quintile disproportionately live in the most deprived neighbourhoods (Supplementary Figure 3), targeting those with the least wealth would preference the most deprived neighbourhoods.
We found no evidence of an association between urban status and frailty after adjustment for demographic and socioeconomic characteristics, health behaviour and neighbourhood deprivation variables. However, there is evidence from other studies of higher mortality rates and worse health in people living in urban areas in the UK [39, 47–50]. Consistent with previous studies, we found smoking was related to a higher risk of frailty as was not being married [13, 27, 51]. People who drink alcohol were found to have lower risk of prefrailty and frailty compared with people who do not consume any alcohol. This finding supports a prior meta-analysis, which suggested that heavier alcohol consumption is related to lower incident frailty compared with no alcohol consumption amongst middle-aged and older adults [52]. One plausible explanation is the ‘sick quitters’ effect, in which individuals in worse health stop drinking or do not start drinking, unlike healthier drinkers [53]. Another explanation is that our data was limited to the frequency of drinking alcohol (in days per week) not the quantity of the alcohol. Drinking more frequently does not necessarily mean drinking greater quantities. Frailty was more common amongst white than non-white individuals. This may be due to selection factors as non-white respondents who participated in ELSA tend to be healthier [17].
As with previous studies, frailty was more common in women than men [54, 55]. Possible reasons include the fact that women have a longer life expectancy than men [56, 57]. Men have, for example higher mortality rates due to cardiovascular disease, and cancer [58], while women have a higher risk of having chronic degenerative diseases [57]. We observed though a greater effect of household wealth and neighbourhood deprivation on having prefrailty or frailty amongst men than women. The finding relating to wealth and the odds of frailty amongst women and men is consistent with data from the World Health Survey [28], which found that higher household economic quintiles were significantly associated with better self-reported health for men though for women a positive association was significant only for the fourth and fifth wealthiest quintile.
Our study analyses data from a large number of men and women drawn from a representative longitudinal study of older people in England and includes information about economic, health, behavioural and social aspects of respondents’ lives. Nonetheless, there are limitations which need to be considered when interpreting the results. Information concerning lifestyle exposures was self-reported and therefore subject to misclassification. As outlined earlier, there were relatively few non-white participants, as funding constraints precluded ELSA oversampling ethnic minority respondents [17]. In relation to area type, as we used Census 2011 rural–urban indicators, data on urban/rural location was restricted to ELSA waves 6–8 and analysis on the effect of area type on the risk of frailty was therefore limited to shorter follow-up. Finally, the data used in this study are confined to England and caution is required in generalising the results beyond this nation.
In summary, household wealth and neighbourhood deprivation are associated with having prefrailty or frailty amongst middle-aged and older adults in England, independently of demographic characteristics, educational attainment, marital status and health behaviours. The odds of being prefrail and frail amongst the least wealthy people who lived in the most deprived neighbourhoods were twice and almost three times higher, respectively, than the wealthiest people who lived in the least deprived area quintiles. In policy development, neighbourhood deprivation should be considered in the drive to reduce health inequalities in ageing populations. Public health interventions targeting the most deprived neighbourhoods provide the best opportunity for benefit as these areas present the greatest opportunity for change.
Supplementary Material
Acknowledgement
We thank both our academic and professional support colleagues from National Institute for Health Research Policy Research Unit in Older People and Frailty with whom we discussed the ideas presented in this paper during unit meetings.
Contributor Information
Asri Maharani, National Institute for Health Research (NIHR) Older People and Frailty Policy Research Unit, School of Health Sciences, Faculty of Biology, Medicine and Health, The University of Manchester, Manchester M13 9PL, UK.
David R Sinclair, National Institute for Health Research (NIHR) Older People and Frailty Policy Research Unit, Population Health Sciences Institute, Newcastle University, Newcastle-upon-Tyne NE4 5PL, UK.
Tarani Chandola, Faculty of Social Sciences, The University of Hong Kong, Pokfulam Road, Hong Kong 999077, Hong Kong.
Peter Bower, National Institute for Health Research (NIHR) Older People and Frailty Policy Research Unit, School of Health Sciences, Faculty of Biology, Medicine and Health, The University of Manchester, Manchester M13 9PL, UK.
Andrew Clegg, Academic Unit for Ageing and Stroke Research, Bradford Institute for Health Research, School of Medicine, University of Leeds, Leeds LS2 9JT, UK.
Barbara Hanratty, National Institute for Health Research (NIHR) Older People and Frailty Policy Research Unit, Population Health Sciences Institute, Newcastle University, Newcastle-upon-Tyne NE4 5PL, UK.
James Nazroo, Cathie Marsh Institute for Social Research, School of Social Sciences, Faculty of Humanities, University of Manchester, Manchester M13 9PL, UK.
Neil Pendleton, National Institute for Health Research (NIHR) Older People and Frailty Policy Research Unit, School of Health Sciences, Faculty of Biology, Medicine and Health, The University of Manchester, Manchester M13 9PL, UK.
Gindo Tampubolon, Global Development Institute, School of Environment, Education and Development, School of Social Sciences, Faculty of Humanities, University of Manchester, Manchester M13 9PL, UK.
Chris Todd, National Institute for Health Research (NIHR) Older People and Frailty Policy Research Unit, School of Health Sciences, Faculty of Biology, Medicine and Health, The University of Manchester, Manchester M13 9PL, UK.
Raphael Wittenberg, National Institute for Health Research (NIHR) Older People and Frailty Policy Research Unit, Care Policy and Evaluation Centre, London School of Economics and Political Science, London WC2A 2AE, UK.
Terence W O'Neill, National Institute for Health Research (NIHR) Older People and Frailty Policy Research Unit, School of Health Sciences, Faculty of Biology, Medicine and Health, The University of Manchester, Manchester M13 9PL, UK.
Fiona E Matthews, National Institute for Health Research (NIHR) Older People and Frailty Policy Research Unit, Population Health Sciences Institute, Newcastle University, Newcastle-upon-Tyne NE4 5PL, UK.
Declaration of Conflicts of Interest
None.
Declaration of Sources of Funding
This report presents independent research funded by the National Institute for Health and Care Research, Policy Research Unit in Older People and Frailty. The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care. Policy Research Unit Programme Reference Number PR-PRU-1217-21502.
Data Availability Statement
Data are available in a public, open access repository. The English Longitudinal Study of Ageing dataset is available in a public, open access repository a nd can be accessed through the UK Data Service at: https://ukdataservice.ac.uk/. The data can be used after registration and acceptance of end user licence.
References
- 1. O’Caoimh R, Sezgin D, O’Donovan MR et al. Prevalence of frailty in 62 countries across the world: a systematic review and meta-analysis of population-level studies. Age Ageing 2021; 50: 96–104. [DOI] [PubMed] [Google Scholar]
- 2. Fried LP, Tangen CM, Walston J et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 2001; 56: M146–57. [DOI] [PubMed] [Google Scholar]
- 3. Searle SD, Mitnitski A, Gahbauer EA, Gill TM, Rockwood K. A standard procedure for creating a frailty index. BMC Geriatr 2008; 8: 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hanlon P, Nicholl BI, Jani BD, Lee D, McQueenie R, Mair FS. Frailty and pre-frailty in middle-aged and older adults and its association with multimorbidity and mortality: a prospective analysis of 493 737 UK biobank participants. Lancet Public Health 2018; 3: e323–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Cegri F, Orfila F, Abellana RM, Pastor-Valero M. The impact of frailty on admission to home care services and nursing homes: eight-year follow-up of a community-dwelling, older adult. Spanish Cohort BMC Geriatrics 2020; 20: 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ensrud KE, Ewing SK, Taylor BC et al. Frailty and risk of falls, fracture, and mortality in older women: the study of osteoporotic fractures. J Gerontol A Biol Sci Med Sci 2007; 62: 744–51. [DOI] [PubMed] [Google Scholar]
- 7. Lang IA, Hubbard RE, Andrew MK, Llewellyn DJ, Melzer D, Rockwood K. Neighborhood deprivation, individual socioeconomic status, and frailty in older adults. J Am Geriatr Soc 2009; 57: 1776–80. [DOI] [PubMed] [Google Scholar]
- 8. Franse CB, van Grieken A, Qin L, Melis RJF, Rietjens JAC, Raat H. Socioeconomic inequalities in frailty and frailty components among community-dwelling older citizens. PloS One 2017; 12: e0187946. 10.1371/journal.pone.0187946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Brunner EJ, Shipley MJ, Ahmadi-Abhari S et al. Midlife contributors to socioeconomic differences in frailty during later life: a prospective cohort study. Lancet Public Health 2018; 3: e313–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Majid Z, Welch C, Davies J, Jackson T. Global frailty: the role of ethnicity, migration and socioeconomic factors. Maturitas 2020; 139: 33–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Sinclair D, Maharani A, Chandola T et al. Frailty among older adults and its distribution in England. J Frailty Aging 2021; 11: 1–6. [DOI] [PubMed] [Google Scholar]
- 12. Stow D, Hanratty B, Matthews FE. The relationship between deprivation and frailty trajectories over 1 year and at the end of life: a case–control study. J Public Health 2021; 44: 844–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kojima G, Iliffe S, Walters K. Smoking as a predictor of frailty: a systematic review. BMC Geriatr 2015; 15: 131. 10.1186/s12877-015-0134-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Peterson MJ, Giuliani C, Morey MC et al. Physical activity as a preventative factor for frailty: the health, aging, and body composition study. J Gerontol Series A 2009; 64A: 61–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Winkleby M, Cubbin C, Ahn D. Effect of cross-level interaction between individual and neighborhood socioeconomic status on adult mortality rates. Am J Public Health 2006; 96: 2145–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Banks J, Blake M, Clemens S et al. English Longitudinal Study of Ageing: Waves 0–8, 1998–2017.[Data Collection]. vol. 29. Oxford, UK: Oxford University Press, 2018. [Google Scholar]
- 17. Steptoe A, Breeze E, Banks J, Nazroo J. Cohort profile: the English longitudinal study of ageing. Int J Epidemiol 2012; 42: 1640–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Smith T, Noble M, Noble S, Wright G, McLennan D, Plunkett E. The English Indices of Deprivation 2015: Technical Report. London: Department for Communities and Local Government, 2015. [Google Scholar]
- 19. Wade KF, Marshall A, Vanhoutte B, Wu FC, O’Neill TW, Lee DM. Does pain predict frailty in older men and women? Findings from the English longitudinal study of ageing (ELSA). J Gerontol Series A 2017; 72: 403–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mitnitski A, Song X, Skoog I et al. Relative fitness and frailty of elderly men and women in developed countries and their relationship with mortality. J Am Geriatr Soc 2005; 53: 2184–9. [DOI] [PubMed] [Google Scholar]
- 21. Rockwood K, Andrew M, Mitnitski A. A comparison of two approaches to measuring frailty in elderly people. J Gerontol A Biol Sci Med Sci 2007; 62: 738–43. [DOI] [PubMed] [Google Scholar]
- 22. Song X, Mitnitski A, Rockwood K. Prevalence and 10-year outcomes of frailty in older adults in relation to deficit accumulation. J Am Geriatr Soc 2010; 58: 681–7. [DOI] [PubMed] [Google Scholar]
- 23. Romero-Ortuno R. An alternative method for frailty index cut-off points to define frailty categories. European Geriatric Med 2013; 4: 299–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Department for Work and Pensions . Benefit Units in Receipt of at Least One Income Related Benefit or Tax Credit, and the Number of Individuals within those Benefit Units. Department for Work and Pensions: London, Great Britain, 2012. [Google Scholar]
- 25. Office for National Statistics . English Indices of Deprivation 2019. Ministry of Housing, Communities & Local Government: London. 2019. Available from: https://www.gov.uk/government/statistics/english-indices-of-deprivation-2019. [Google Scholar]
- 26. Office for National Statistics . The 2011 Rural–Urban Classification for Small Area Geographies: A User Guide and Frequently Asked Questions. London: Office for National Statistics, 2013. [Google Scholar]
- 27. Kojima G, Iliffe S, Jivraj S, Liljas A, Walters K. Does current smoking predict future frailty? The English longitudinal study of ageing. Age Ageing 2018; 47: 126–31. [DOI] [PubMed] [Google Scholar]
- 28. Hosseinpoor AR, Stewart Williams J, Amin A et al. Social determinants of self-reported health in women and men: understanding the role of gender in population health. PloS One 2012; 7: e3479923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Azur MJ, Stuart EA, Frangakis C, Leaf PJ. Multiple imputation by chained equations: what is it and how does it work? Int J Methods Psychiatr Res 2011; 20: 40–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Graham JW, Olchowski AE, Gilreath TD. How many imputations are really needed? Some practical clarifications of multiple imputation theory. Prev Sci 2007; 8: 206–13. [DOI] [PubMed] [Google Scholar]
- 31. Von Hippel PT. How many imputations do you need? A two-stage calculation using a quadratic rule. Sociolog Methods Res 2020; 49: 699–718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. StataCorp . Stata Statistical Software: Release 17. StataCorp LLC: College Station, TX, 2021. [Google Scholar]
- 33. Lang IA, Llewellyn DJ, Langa KM, Wallace RB, Huppert FA, Melzer D. Neighborhood deprivation, individual socioeconomic status, and cognitive function in older people: analyses from the English longitudinal study of ageing. J Am Geriatr Soc 2008; 56: 191–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Lang IA, Llewellyn DJ, Langa KM, Wallace RB, Melzer D. Neighbourhood deprivation and incident mobility disability in older adults. Age Ageing 2008; 37: 403–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Lakshman R, McConville A, How S, Flowers J, Wareham N, Cosford P. Association between area-level socioeconomic deprivation and a cluster of behavioural risk factors: cross-sectional, population-based study. J Public Health 2011; 33: 234–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Foster HM, Celis-Morales CA, Nicholl BI et al. The effect of socioeconomic deprivation on the association between an extended measurement of unhealthy lifestyle factors and health outcomes: a prospective analysis of the UK biobank cohort. Lancet Public Health 2018; 3: e576–85. [DOI] [PubMed] [Google Scholar]
- 37. Diez Roux AV. Investigating neighborhood and area effects on health. Am J Public Health 2001; 91: 1783–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Seo Y, Kim M, Shim H, Won CW. Differences in the association of neighborhood environment with physical frailty between urban and rural older adults: the Korean frailty and aging cohort study (KFACS). J Am Med Dir Assoc 2021; 22: 590–597.e1. [DOI] [PubMed] [Google Scholar]
- 39. Kivimäki M, Batty GD, Pentti J et al. Modifications to residential neighbourhood characteristics and risk of 79 common health conditions: a prospective cohort study. Lancet Public Health 2021; 6: e396–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Knol MJ, VanderWeele TJ. Recommendations for presenting analyses of effect modification and interaction. Int J Epidemiol 2012; 41: 514–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Stuckler D, Reeves A, Loopstra R, Karanikolos M, McKee M. Austerity and health: the impact in the UK and Europe. Eur J Public Health 2017; 27: 18–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Stoye G, Zaranko B, Shipley M, Mckee M, Brunner EJ. Educational inequalities in hospital use among older adults in England, 2004-2015. Milbank Q 2020; 98: 1134–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Kojima G, Iliffe S, Walters K. Frailty index as a predictor of mortality: a systematic review and meta-analysis. Age Ageing 2018; 47: 193–200. 10.1093/ageing/afx162. [DOI] [PubMed] [Google Scholar]
- 44. Kojima G. Frailty as a predictor of hospitalisation among community-dwelling older people: a systematic review and meta-analysis. J Epidemiol Community Health 2016; 70: 722–9. [DOI] [PubMed] [Google Scholar]
- 45. NHS England . Identifying Frailty London 2022. NHS: England & London, UK. Available from: https://www.england.nhs.uk/ourwork/clinical-policy/older-people/frailty/frailty-risk-identification/.
- 46. NHS England . Preventing Frailty London 2022. NHS: England & London, UK. Available from: https://www.england.nhs.uk/ourwork/clinical-policy/older-people/frailty/preventing-frailty/.
- 47. Jones NR, Lake IR. The combined impact of rural residence and socio-economic status on premature mortality. Health Place 2013; 24: 90–6. [DOI] [PubMed] [Google Scholar]
- 48. Erskine S, Maheswaran R, Pearson T, Gleeson D. Socioeconomic deprivation, urban-rural location and alcohol-related mortality in England and Wales. BMC Public Health 2010; 10: 99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Teckle P, Hannaford P, Sutton M. Is the health of people living in rural areas different from those in cities? Evidence from routine data linked with the Scottish health survey. BMC Health Serv Res 2012; 12: 43. 10.1186/1472-6963-12-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Allan R, Williamson P, Kulu H. Gendered mortality differentials over the rural-urban continuum: the analysis of census linked longitudinal data from England and Wales. Soc Sci Med 2019; 221: 68–78. [DOI] [PubMed] [Google Scholar]
- 51. Kojima G, Walters K, Iliffe S, Taniguchi Y, Tamiya N. Marital status and risk of physical frailty: a systematic review and meta-analysis. J Am Med Dir Assoc 2020; 21: 322–30. [DOI] [PubMed] [Google Scholar]
- 52. Kojima G, Liljas A, Iliffe S, Jivraj S, Walters K. A systematic review and meta-analysis of prospective associations between alcohol consumption and incident frailty. Age Ageing 2018; 47: 26–34. [DOI] [PubMed] [Google Scholar]
- 53. Seematter-Bagnoud L, Spagnoli J, Büla C, Santos-Eggimann B. Alcohol use and frailty in community-dwelling older persons aged 65 to 70 years. J Frailty Aging 2014; 3: 9–14. [DOI] [PubMed] [Google Scholar]
- 54. Welstead M, Jenkins ND, Russ TC, Luciano M, Muniz-Terrera G. A systematic review of frailty trajectories: their shape and influencing factors. Gerontologist 2021; 61: e463–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Alexandre TS, Corona LP, Brito TR, Santos JL, Duarte YA, Lebrao ML. Gender differences in the incidence and determinants of components of the frailty phenotype among older adults: findings from the SABE study. J Aging Health 2018; 30: 190–212. 10.1177/0898264316671228. [DOI] [PubMed] [Google Scholar]
- 56. Gordon EH, Hubbard RE. Differences in frailty in older men and women. Med J Australia 2020; 212: 183–8. [DOI] [PubMed] [Google Scholar]
- 57. Gordon E, Peel N, Samanta M, Theou O, Howlett S, Hubbard R. Sex differences in frailty: a systematic review and meta-analysis. Exp Gerontol 2017; 89: 30–40. [DOI] [PubMed] [Google Scholar]
- 58. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin 2019; 69: 7–34. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available in a public, open access repository. The English Longitudinal Study of Ageing dataset is available in a public, open access repository a nd can be accessed through the UK Data Service at: https://ukdataservice.ac.uk/. The data can be used after registration and acceptance of end user licence.


