Abstract
Objectives
Polycystic ovary syndrome (PCOS) is a condition that occurs frequently among women of reproductive age and is a polygenic, multifactorial, endocrine, and metabolic disorder. PCOS is becoming more common as a result of risk factors such as current lifestyle, overnutrition, and stress. The use of traditional herbal medicine is higher among the global population. Hence, this review article focuses on the potential of Nigella sativa to manage women with PCOS.
Methods
A literature search was carried out using databases including Medline, Google Scholar, EBSCO, Embase, and Science Direct, as well as reference lists, to identify relevant publications that support the use of N. sativa in the management of women with PCOS.
Results
Several clinical and preclinical studies have demonstrated that the major bioactive constituent of black seed (N. sativa), thymoquinone, has potential for managing women with PCOS. Moreover, N. sativa may help to manage oligomenorrhea and amenorrhea in women with PCOS through its anti-inflammatory and antioxidant properties.
Conclusion
N. sativa has potential for use as a herbal medicine for managing women with PCOS as an integrative medicine along with traditional and modern medicine in conjunction with calorie restriction and regular exercise.
Keywords: nigella sativa, black seeds, thymoquinone, polycystic ovarian syndrome, anti-inflammatory, antioxidant
INTRODUCTION
Ametabolic polycystic ovary syndrome (PCOS) is a condition that occurs frequently among women of reproductive age and it is an ametabolic and endocrine disorder. The global prevalence of PCOS has been estimated to be 6-26% [1]. Endocrinological changes caused by PCOS include increased plasma exposure to luteinizing hormone (LH), estradiol, testosterone, epiandrostenedione, prolactin, and insulin, as well as decreased serum levels of progesterone, follicle-stimulating hormone (FSH), sex hormone-binding globulin (SHBG), and hypothyroidism [2], while metabolic changes associated with PCOS include visceral obesity, insulin resistance, and hyperinsulinemia [3]. Polycystic ovaries are common in approximately 75% of anovulatory women. The incidence of PCOS is increasing, mainly due to risk factors such as current lifestyle, diet, and stress [4].
PCOS is caused by multiple factors, including insulin resistance, hyperinsulinemia, hyperandrogenism, and obesity [5]. Insulin resistance induces excessive release of insulin (hyperinsulinemia), which results in diminished SHBG levels and enhanced insulin-like growth factor-1 (IGF-1) concentrations. Hyperandrogenism is caused by increased testosterone levels and insulin-like androgen production from the ovaries, which are caused by a decrease in SHBG and an increase in IGF-1, respectively [6]. Dysregulation of steroidogenesis induces functional ovarian hyperandrogenism (FOH), which is the most frequent cause of PCOS in women. Hyperinsulinemia aggravates the pathogenesis of PCOS through the stimulation of LH by sensitizing ovarian theca cells. Hyperinsulinemia may cause PCOS-associated obesity via enhanced adipogenesis and lipogenesis, and diminished lipolysis. Ovarian androgen production is upregulated by obesity, primarily via insulin-resistant hyperinsulinemia [7].
Based on earlier studies, women with PCOS are well known to have low-grade inflammation for the long term. Women with PCOS have higher levels of inflammatory markers, such as C-reactive protein (CRP), tumor necrosis factor (TNF), interleukin 6 (IL-6), interleukin 18 (IL-18), monocyte chemoattractant protein-1 (MCP-1), and macrophage inflammatory protein-1 (MIP-1) [8-10]. Moreover, several studies have confirmed that PCOS is associated with oxidative stress. Women with PCOS have significantly higher levels of circulating biomarkers of oxidative stress, including malondialdehyde (MDA), nitric oxide (NO), advanced glycosylated end products (AGEs), and xanthine oxidase (XO). Women with PCOS also have lowered levels of anti-oxidative biomarkers, including total antioxidant capacity (TAC), superoxide dismutase (SOD), glutathione peroxidase (GPx), glutathione (GSH), vitamin E, and vitamin C [11-13].
PCOS is characterized by polycystic ovaries, irregular menstrual cycles, anovulation, hyperandrogenism, infertility, obesity, insulin resistance (IR), hyperinsulinemia, impaired glucose tolerance (type 2 diabetes), dyslipidemia, hirsutism, and acne [14]. The risk of metabolic, cardiovascular, and reproductive disorders is higher among women with PCOS [15]. PCOS-associated problems such as infertility, hirsutism, acne, and alopecia may cause some psychological issues in women with PCOS, such as depression or anxiety [16].
According to the American Society of Reproductive Medicine (ASRM), 70-80% of women with PCOS are infertile. In addition, the Centers for Disease Control and Prevention (CDC) state that PCOS is the most frequent cause of infertility [17]. Drugs like clomiphene citrate and letrozole are usually employed for the induction of ovulation in women with PCOS undergoing fertility treatment [18].
The management of PCOS includes both non-pharmacological and pharmacological therapies. Various guidelines have been proposed by different organizations for managing women with PCOS. More importantly, a multi-year international evidence-based guideline was published by the International PCOS network, consisting of PCOS experts and consumers from all over the world and sponsored by the ASRM and the European Society for Human Reproduction and Embryology (ESHRE) [19]. Moreover, a multidisciplinary international guideline development group (GDG) consisting of experts from 71 countries and 37 organizations developed evidence-based recommendations for the management of PCOS [20, 21].
Obese women with PCOS are recommended to modify their lifestyle, which includes diet and exercise as first-line therapy. In addition, PCOS can also be managed pharmacologically based on major symptoms such as menstrual irregularities, androgen excess, metabolic complications, and infertility. Menstrual irregularities can be managed using dydrogesterone, low-dose ethinylestradiol combined with a third-generation progestin (desogestrel, gestodene, or norgestimate) or a fourth-generation progestin (drospirenone), and metformin. Excess androgen can be managed by drugs such as spironolactone, oral contraceptive pills, and metformin. Metformin improves insulin sensitivity and weight loss in women with PCOS. Moreover, metformin may also help to resolve infertility through weight loss and improved insulin sensitivity. Overall, calorie restriction and regular exercise, followed by pharmacological symptom management, can effectively manage PCOS in women [22].
As per the estimation of the World Health Organization (WHO), the use of traditional herbal medicine is increasing among the global population. Patients with metabolic syndrome, including obesity, hypertension, diabetes, heart disease, cancer, and other chronic conditions, may prefer traditional herbal medicine [23]. Hence, our review focuses on the management of PCOS using Nigella sativa (black seeds). N. sativa is commonly used as a spice and flavoring agent in bread, yogurt, salads, and other food preparations. Numerous studies suggest using N. sativa for the management of chronic conditions such as obesity, diabetes, and hypertension [24].
The phytoconstituents of N. sativa include terpenes (thymoquinone, dithymoquinone, p-cymene, α-pinene, limonene, carvone, anethol, etc.), steroids (α-hederin), alkaloids (nigellicine, negillidine, nigellicimine, nigellicimine-N-oxide), flavonoids (quercetin), saponins, fixed oil, coumarins, amino acids, and many others [25]. Various clinical studies have revealed that the seeds and oil of N. sativa in different doses for different durations have shown no harm in the hepatic and renal parameters of human subjects [26].
Moreover, acute and chronic toxicity studies with N. sativa in mice and rats revealed that it has high LD50 values, stability of key hepatic enzymes, and integrity of organs [27]. In addition, the sub-acute toxicity study of a mixture of N. sativa and honey administered to Sprague-Dawley rats showed an LD50 value of more than 2 g/kg along with delayed hepatoprotective effects [28], while 20 mL/kg administration of a nanoemulsion of a thymoquinone-rich fraction resulted in no mortality or signs of toxicity in an acute and chronic toxicity study [29]. This review article is focused on assessing the available clinical and preclinical studies to support the use of N. sativa in conjunction with diet restriction and increased physical activity to manage women with PCOS.
METHODS
A literature search was carried out using databases including Medline, Google Scholar, EBSCO, Embase, and Science Direct, as well as reference lists, to identify relevant publications that support the use of N. sativa in the management of women with PCOS, using keywords such as Nigella sativa, black seeds, kalonji, poly cystic ovarian syndrome, PCOS, PCOD, anti-inflammatory, and antioxidant. Observations from clinical and preclinical studies written in English were included in this review while duplicates were excluded.
RESULTS AND DISCUSSION
N. sativa possesses potent anti-inflammatory and antioxidant properties along with anti-obesity and antidiabetic potential [30], which are all useful for managing women with PCOS. Various clinical and preclinical studies suggest using N. sativa for the management of women with PCOS.
1. Clinical trials
Numerous clinical studies have confirmed that N. sativa has the potential to manage PCOS in women (Table 1). A significant decrease in average menstrual cycle intervals, along with a significant rise in the average duration of menstruation and the ratio of menstrual cycles per month, was observed with the administration of 2 g/day of N. sativa capsules for 16 weeks in a pilot study, which recruited ten women diagnosed with PCOS having oligomenorrhea and amenorrhea. Moreover, the study participants showed significant improvements in plasma levels of LH, fasting blood glucose (FBG), insulin, homeostatic model assessment for insulin resistance (HOMA-IR) index, cholesterol, triglycerides, and aspartate aminotransferase (AST) [31].
Table 1.
Clinical studies supporting the use of N. sativa to manage PCOS
| S.No | Type of study | Findings |
|---|---|---|
| 1 | Pilot study [31] | • Significant decrease in average menstrual cycle intervals. |
| • Significant raise of average duration of menstruation and the ratio of cycle per month. | ||
| • Significant improvements in serum LH, insulin, FBG, HOMA-IR index, TC, TGs, and AST. | ||
| 2 | Open-labeled, non-randomized clinical trial [32] | • Normal menstrual cycle, normal duration of cycle and complete clearance of cysts. |
| • Mild improvements in BMI score and waist-hip ratio. | ||
| 3 | Double-blinded, placebo-controlled randomized controlled clinical trial [33] | • Significant reduction of menstrual interval. |
| • Significant elevation of frequency of menstrual cycle. |
An open-label, non-randomized clinical trial of 40 women with PCOS found that taking powdered N. sativa (Karunjchirakam Chooranam) twice daily for 60 days resulted in a normal menstrual cycle (28-day cycle) in 50% of participants, a normal cycle duration (3-5 days) in 85% of participants, and complete cyst clearance in 15% of study participants. In addition, the study participants also attained mild improvements in their scores for body mass index (BMI) and waist-hip ratio [32].
Furthermore, in a double-blind, placebo-controlled randomized clinical trial of 84 women with PCOS who had oligomenorrhea and amenorrhea, the administration of N. sativa oil capsules (two capsules of 500 mg) daily at night for 16 weeks resulted in a significant reduction in menstrual interval and a significant elevation in menstrual cycle frequency [33].
2. Preclinical studies
Similarly, various experimental animal studies have determined that N. sativa exhibits potential effects against PCOS (Table 2). The oral administration of a hydro-alcoholic extract of N. sativa (600 mg/kg) for 63 days resulted in a significant increase in TAC and a decrease in malondialdehyde (MDA) in the ovary tissue of PCOS-induced rats [34]. In addition, intraperitoneal administration of 8 and 16 mg/kg of thymoquinone for 30 days in estradiol valerate-induced PCOS rats resulted in significant improvements in ovarian morphology, ovarian function, and ovulation, similar to those observed with metformin. The number of follicular cysts decreased significantly with thymoquinone treatment along with an increase in the number of primary follicles, Graafian follicles, antral follicles, and corpus luteum. Thymoquinone treatment also reversed the elevated biochemical parameters, including plasma glucose, triglycerides (TGs), total cholesterol (TC), low-density lipoprotein-cholesterol (LDL-c), high-density lipoprotein-cholesterol (HDL-c), LH, and FSH [35]. Moreover, an experimental study of letrozole-induced PCOS female Sprague-Dawley rats revealed that N. sativa oil administration (5 and 10 mL/kg) for 7 weeks resulted in a significant increase in the number of rats undergoing regular cycles, the average number of regular cycles, the appearance of corpus luteum, and a decreased number of cystic follicles, along with a reduction of LH, testosterone, FSH, body weight, FBG, TC, LDL-c, TGs, and MDA. Treatment with N. sativa oil also enhanced the levels of HDL-c, SOD, and glutathione peroxidase (GPX) activities among them [36].
Table 2.
Preclinical studies supporting the use of N. sativa to manage PCOS
| S.No | Study design | Outcome |
|---|---|---|
| 1 | Animal study (PCOS-induced rats) [34] | • Marked elevation of TAC and reduction of MDA. |
| 2 | Animal study (estradiol valerate-induced PCOS rats) [35] | • Significant improvements in ovarian morphology, ovarian function, and ovulation similar to metformin. |
| • Significant reduction of number of follicular cysts along with an increase in number of primary follicles, antral follicles, Graafian follicles and corpus luteum. | ||
| • Reversal of serum biochemical parameters including glucose, TGs, TC, LDL-c, HDL-c, LH, and FSH. | ||
| 3 | Animal study (letrozole-induced PCOS female Sprague-Dawley rats) [36] | • Significant increase of number of rats undergoing regular cycle, average number of regular cycles, appearance of corpus luteum and decreased number of cystic follicles. |
| • Reduction of LH, testosterone, FSH, body weight, FBG, TC, LDL-c, TGs, and MDA. | ||
| • Increased levels of HDL-c, SOD, and GPX. | ||
| 4 | Animal study (dehydroepiandrosterone-induced PCOS mice) [37] | • Significant improvements in maturation, fertilization, and blastocyst formation. |
| • Increased glutathione concentration and glutathione peroxidase mRNA expression in oocytes. | ||
| 5 | Animal study (letrozole-induced PCOS Wistar rats) [38] | • Significant improvements in serum levels of LH, FSH, estrogen, testosterone and progesterone. |
| 6 | Animal study (dehydroepiandrosterone (DHEA)-induced PCOS Wistar female rats) [39] | • Significant lowering of serum levels of LH, estrogen, testosterone, insulin, insulin resistance, glucose, and malondialdehyde (MDA). |
| • Increased serum levels of progesterone and antioxidant enzymes such as SOD, GPX and CAT. | ||
| • Reversal of pathological changes of primary follicles by increasing number of graafian follicles and decreasing number of cystic follicles and atretic follicles. |
Significant improvements in maturation, fertilization, and blastocyst formation were observed in the oocytes of dehydroepiandrosterone-induced PCOS mice after the administration of 50 g/mL of a hydro-alcoholic extract of N. sativa. The N. sativa treatment also increased the glutathione concentration and glutathione peroxidase mRNA expression in oocytes [37]. Moreover, an experimental animal study demonstrated that the administration of 300 mg/kg of a hydro-alcoholic extract of N. sativa + 1,200 mg/kg of honey or 600 mg/kg of a hydro-alcoholic extract of N. sativa + 2,400 mg/kg of honey for 28 days in letrozole-induced PCOS Wistar rats both resulted in significant improvements in plasma levels of LH, FSH, estrogen, testosterone, and progesterone [38]. Furthermore, administration of 200 mg/kg of a hydro-alcoholic extract of N. sativa seeds reduced plasma levels of LH, estrogen, testosterone, insulin, IR, glucose, and MDA in dehydroepiandrosterone (DHEA)-induced PCOS Wistar female rats, while it increased the plasma levels of progesterone and antioxidant enzymes such as SOD, GPX, and catalase (CAT). N. sativa treatment has also been shown to reverse the pathological changes of primary follicles by increasing the number of Graafian follicles and decreasing the number of cystic follicles and atretic follicles in PCOS rats [39].
3. Anti-inflammatory effects of N. sativa
Higher levels of inflammation and inflammatory markers are associated with the pathogenesis of PCOS and the disturbance in the levels of inflammatory markers increases the risk of ovary dysfunction [40, 41]. CRP, tumor necrosis factor (TNF-α), interleukin 6 (IL-6), interleukin 18 (IL-18), white blood cell count (WBC), monocyte chemoattractant protein-1 (MCP-1), and macrophage inflammatory protein-1 (MIP-1) are all known to be elevated in women with PCOS [42].
A case-control study of 30 women with PCOS and 30 healthy women revealed that the women with PCOS had elevated levels of highly sensitive CRP (hsCRP) and TNF-α [43], indicating the presence of chronic inflammation, and higher levels of platelet microparticles (PMP), indicating central adiposity and hyperandrogenism [44]. Inflammation of the hypothalamus could be one of the potential pathophysiologic basis for PCOS as the hypothalamus is involved in food intake, weight balance, libido, and reproduction [45]. In addition, mitochondrial dysfunction has also been suggested to be linked with the pathogenesis of PCOS [46].
The anti-inflammatory properties of N. sativa (thymoquinone) might be responsible for its therapeutic efficacy against PCOS, as PCOS is associated with chronic inflammation. Several clinical and preclinical studies have demonstrated the anti-inflammatory potential of N. sativa [47-51]. N. sativa (thymoquinone) is believed to produce anti-inflammatory activity through various molecular and signaling pathways, including suppression of cyclooxygenase-2 (COX2) expression, inhibition of nuclear factor kappa-light-chain-enhancer of activated B (NF-K) pathway, inhibition of phosphatidyl inositol 3-kinase (PI3K)/protein kinase B pathways, and activation of nuclear factor erythroid 2-related factor 2 (Nrf2)-ARE (antioxidant response element) [43].
4. Antioxidant properties of N. sativa
Oxidative stress plays a significant role in the pathogenesis of PCOS [52]. Mitochondrial dysfunction occurs due to excessive production of reactive oxygen species (ROS) via damage of mitochondrial components such as mitochondrial DNA (mtDNA), proteins, and lipids, and PCOS is associated with a decreased number of copies of mtDNA [53].
A case-control study of 51 women with PCOS and 45 control women determined that the women with PCOS had significantly lowered levels of glutathione (GSH) and TAC, which indicates the role of oxidative stress in the pathogenesis of PCOS [54]. In addition, elevated levels of MDA and lowered levels of SOD and TAC have been observed among women with PCOS in a nested case-control study of 50 women with PCOS and 50 control women [55]. Furthermore, another case-control study of 86 women with PCOS and 60 control women found that oxidative stress was higher in the PCOS women’s serum and follicular fluid [56].
The antioxidant efficacy of N. sativa has been confirmed by numerous clinical and preclinical studies [57-61]. N. sativa’s antioxidant activity may be mediated by a variety of mechanisms, including increased free radical scavenging, inhibition of lipid peroxidation, increased activity of antioxidant enzymes, such as SOD, GPX, and CAT, increased glutathione levels, inhibition of NF-K activity, and inhibition of enzymes such as cyclooxygenase and lipoxygenase [62, 63].
5. Proposed mechanisms of action
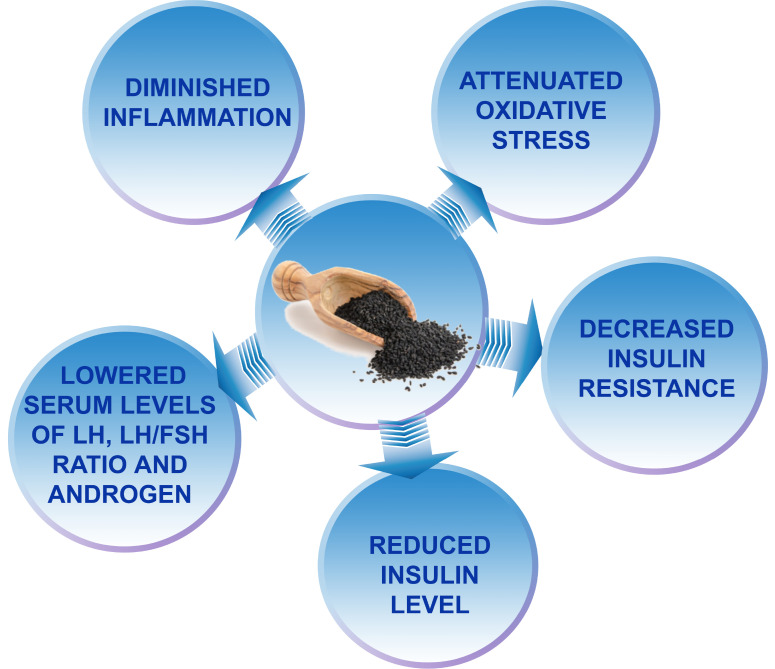
N. Sativa may help in the management of women with PCOS, probably through some remarkable mechanisms (Fig. 1), including its antioxidant and anti-inflammatory properties, which may help to ameliorate PCOS-associated amenorrhea and oligomenorrhea by affecting ovarian function positively. In addition, the antioxidant and anti-inflammatory properties of N. sativa may improve menstrual cycles with normal ovulation by decreasing the plasma exposure of LH and the androgen LH/FSH ratio via reduced IR and diminished insulin levels [33, 36].
Figure 1.
Proposed mechanisms of N. sativa in PCOS management.
CONCLUSION
The use of traditional herbal medicine is increasing among the global population. Several clinical and preclinical studies have demonstrated that black seeds (N. sativa) with their major bioactive constituent thymoquinone have potential for managing women with PCOS. Various mechanisms, including decreased inflammation, attenuated oxidative stress, decreased IR, diminished insulin levels, lowered plasma concentrations of LH, and androgen, and reduced LH/FSH ratio, have been proposed to improve menstrual cycles with normal ovulation in women with PCOS. The studies discussed in this review and the proposed mechanisms suggest that N. sativa can be used as a herbal medicine for the management of PCOS in women as an integrative medicine, along with traditional and modern medicine in conjunction with diet restrictions and increased physical activity.
ACKNOWLEDGMENT
The authors express sincere gratefulness to Principal, J.K.K. Nattraja College of Pharmacy, Komarapalayam, for giving an opportunity and online library facilities to write this article.
Funding Statement
FUNDING None declared.
Footnotes
CONFLICT OF INTEREST
None declared.
REFERENCES
- 1.Rao MMS, Broughton KS, LeMieux MJ. Cross-sectional study on the knowledge and prevalence of PCOS at a multiethnic university. Prog Prev Med. 2020;5(2):e0028. doi: 10.1097/pp9.0000000000000028. [DOI] [Google Scholar]
- 2.De Leo V, Musacchio MC, Cappelli V, Massaro MG, Morgante G, Petraglia F. Genetic, hormonal and metabolic aspects of PCOS: an update. Reprod Biol Endocrinol. 2016;14(1):38. doi: 10.1186/s12958-016-0173-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sanchez-Garrido MA, Tena-Sempere M. Metabolic dysfunction in polycystic ovary syndrome: pathogenic role of androgen excess and potential therapeutic strategies. Mol Metab. 2020;35:100937. doi: 10.1016/j.molmet.2020.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Azziz R, Carmina E, Chen Z, Dunaif A, Laven JS, Legro RS, et al. Polycystic ovary syndrome. Nat Rev Dis Primers. 2016;2:16057. doi: 10.1038/nrdp.2016.57. [DOI] [PubMed] [Google Scholar]
- 5.Zeng X, Xie YJ, Liu YT, Long SL, Mo ZC. Polycystic ovarian syndrome: correlation between hyperandrogenism, insulin resistance and obesity. Clin Chim Acta. 2020;502:214–21. doi: 10.1016/j.cca.2019.11.003. [DOI] [PubMed] [Google Scholar]
- 6.Bednarska S, Siejka A. The pathogenesis and treatment of polycystic ovary syndrome: what's new? Adv Clin Exp Med. 2017;26(2):359–67. doi: 10.17219/acem/59380. [DOI] [PubMed] [Google Scholar]
- 7.Rosenfield RL, Ehrmann DA. The pathogenesis of polycystic ovary syndrome (PCOS): the hypothesis of PCOS as functional ovarian hyperandrogenism revisited. Endocr Rev. 2016;37(5):467–520. doi: 10.1210/er.2015-1104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Escobar-Morreale HF, Luque-Ramírez M, González F. Circulating inflammatory markers in polycystic ovary syndrome: a systematic review and metaanalysis. Fertil Steril. 2011;95(3):1048–58.e1. doi: 10.1016/j.fertnstert.2010.11.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rostamtabar M, Esmaeilzadeh S, Tourani M, Rahmani A, Baee M, Shirafkan F, et al. Pathophysiological roles of chronic low-grade inflammation mediators in polycystic ovary syndrome. J Cell Physiol. 2021;236(2):824–38. doi: 10.1002/jcp.29912. [DOI] [PubMed] [Google Scholar]
- 10.Abraham Gnanadass S, Divakar Prabhu Y, Valsala Gopalakrishnan A. Association of metabolic and inflammatory markers with polycystic ovarian syndrome (PCOS): an update. Arch Gynecol Obstet. 2021;303(3):631–43. doi: 10.1007/s00404-020-05951-2. [DOI] [PubMed] [Google Scholar]
- 11.Mohammadi M. Oxidative stress and polycystic ovary syndrome: a brief review. Int J Prev Med. 2019;10:86. doi: 10.4103/ijpvm.IJPVM_576_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zuo T, Zhu M, Xu W. Roles of oxidative stress in polycystic ovary syndrome and cancers. Oxid Med Cell Longev. 2016;2016:8589318. doi: 10.1155/2016/8589318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dubey P, Reddy S, Boyd S, Bracamontes C, Sanchez S, Chattopadhyay M, et al. Effect of nutritional supplementation on oxidative stress and hormonal and lipid profiles in PCOS-affected females. Nutrients. 2021;13(9):2938. doi: 10.3390/nu13092938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Witchel SF, Oberfield SE, Peña AS. Polycystic ovary syndrome: pathophysiology, presentation, and treatment with emphasis on adolescent girls. J Endocr Soc. 2019;3(8):1545–73. doi: 10.1210/js.2019-00078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Maqbool M, Gani I, Geer MI. Polycystic ovarian syndrome- a multifaceted disease: a review. Int J Pharm Sci Res. 2019;10(3):1072–79. [Google Scholar]
- 16.Chaudhari AP, Mazumdar K, Mehta PD. Anxiety, depression, and quality of life in women with polycystic ovarian syndrome. Indian J Psychol Med. 2018;40(3):239–46. doi: 10.4103/IJPSYM.IJPSYM_561_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lentscher JA, Slocum B, Torrealday S. Polycystic ovarian syndrome and fertility. Clin Obstet Gynecol. 2021;64(1):65–75. doi: 10.1097/GRF.0000000000000595. [DOI] [PubMed] [Google Scholar]
- 18.Bansal S, Goyal M, Sharma C, Shekhar S. Letrozole versus clomiphene citrate for ovulation induction in anovulatory women with polycystic ovarian syndrome: a randomized controlled trial. Int J Gynaecol Obstet. 2021;152(3):345–50. doi: 10.1002/ijgo.13375. [DOI] [PubMed] [Google Scholar]
- 19.Hoeger KM, Dokras A, Piltonen T. Update on PCOS: consequences, challenges, and guiding treatment. J Clin Endocrinol Metab. 2021;106(3):e1071–83. doi: 10.1210/clinem/dgaa839. [DOI] [PubMed] [Google Scholar]
- 20.Costello MF, Misso ML, Balen A, Boyle J, Devoto L, Garad RM, et al. Evidence summaries and recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome: assessment and treatment of infertility. Hum Reprod Open. 2019;2019(1):hoy021. doi: 10.1093/hropen/hoy021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Teede HJ, Misso ML, Costello MF, Dokras A, Laven J, Moran L, et al. Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Hum Reprod. 2018;33(9):1602–18. doi: 10.1093/humrep/dey256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lua ACY, How CH, King TFJ. Managing polycystic ovary syndrome in primary care. Singapore Med J. 2018;59(11):567–71. doi: 10.11622/smedj.2018135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Maideen NMP, Balasubramaniam R. Pharmacologically relevant drug interactions of sulfonylurea antidiabetics with common herbs. J Herbmed Pharmacol. 2018;7(3):200–10. doi: 10.15171/jhp.2018.32. [DOI] [Google Scholar]
- 24.Maideen NMP, Balasubramanian R, Ramanathan S. Nigella sativa (Black Seeds), a potential herb for the pharmacotherapeutic management of hypertension - a review. Curr Cardiol Rev. 2021;17(4):e230421187786. doi: 10.2174/1573403X16666201110125906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ahmad MF, Ahmad FA, Ashraf SA, Saad HH, Wahab S, Khan MI, et al. An updated knowledge of Black seed (Nigella sativa Linn.): review of phytochemical constituents and pharmacological properties. J Herb Med. 2021;25:100404. doi: 10.1016/j.hermed.2020.100404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tavakkoli A, Mahdian V, Razavi BM, Hosseinzadeh H. Review on clinical trials of black seed (Nigella sativa) and its active constituent, thymoquinone. J Pharmacopuncture. 2017;20(3):179–93. doi: 10.3831/KPI.2017.20.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zaoui A, Cherrah Y, Mahassini N, Alaoui K, Amarouch H, Hassar M. Acute and chronic toxicity of Nigella sativa fixed oil. Phytomedicine. 2002;9(1):69–74. doi: 10.1078/0944-7113-00084. [DOI] [PubMed] [Google Scholar]
- 28.Lou WP, Assaw S, Lokman MA, Suhaimin N, Yusof HM. Sub-acute toxicity of black seed (Nigella sativa) and honey mixture. Malays Appl Biol. 2018;47(6):11–8. [Google Scholar]
- 29.Tubesha Z, Imam MU, Mahmud R, Ismail M. Study on the potential toxicity of a thymoquinone-rich fraction nanoemulsion in Sprague Dawley rats. Molecules. 2013;18(7):7460–72. doi: 10.3390/molecules18077460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Maideen NMP. Prophetic medicine-nigella sativa (black cumin seeds) - potential herb for COVID-19? J Pharmacopuncture. 2020;23(2):62–70. doi: 10.3831/KPI.2020.23.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Naeimi SA, Tansaz M, Sohrabvand F, Hajimehdipoor H, Nabimeybodi R, Saber S, et al. Assessing the effect of processed nigella sativa on oligomenorrhea and amenorrhea in patients with polycystic ovarian syndrome: a pilot study. Int J Pharm Sci Res. 2018;9(11):4716–22. [Google Scholar]
- 32.Arivoli D. Government Siddha Medical College; [Palayamkottai]: 2019. A prospective open labelled phase-II non randomized clinical trial on "Karunjchirakam Chooranam" for Raktha Soorai Vaayu (Poly Cystic Ovarian Syndrome) [dissertation] [Google Scholar]
- 33.Naeimi SA, Tansaz M, Hajimehdipoor H, Saber S. Comparing the effect of nigella sativa oil soft gel and placebo on oligomenorrhea, amenorrhea and laboratory characteristics in patients with polycystic ovarian syndrome, a randomized clinical trial. Res J Pharmacogn. 2020;7(1):49–58. [Google Scholar]
- 34.Kohzadi R, Nejati V, Razi M, Najafi G. Effects Hydro-alcoholic extract of (Nigella sativa L.) on the level of malondialdehyde (MDA) and total antioxidant capacity (TAC) of the ovary tissue in a rat model of PCOS. J Anim Environ. 2017;9(3):85–92. [Google Scholar]
- 35.Taghvaee Javanshir S, Yaghmaei P, Hajebrahimi Z. Thymoquinone ameliorates some endocrine parameters and histological alteration in a rat model of polycystic ovary syndrome. Int J Reprod Biomed. 2018;16(4):275–84. doi: 10.29252/ijrm.16.4.275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nafiu AB, Alimi S, Babalola A, Ogunlade AT, Muhammad FD, Abioye ARAI, et al. Anti-androgenic and insulin-sensitizing actions of Nigella sativa oil improve polycystic ovary and associated dyslipidemia and redox disturbances. J Complement Med Res. 2019;10(4):186–99. doi: 10.5455/jcmr.20190613045154. [DOI] [Google Scholar]
- 37.Eini F, Joharchi K, Kutenaei MA, Mousavi P. Improvement in the epigenetic modification and development competence in PCOS mice oocytes by hydro-alcoholic extract of Nigella sativa during in-vitro maturation: an experimental study. Int J Reprod Biomed. 2020;18(9):733–46. doi: 10.18502/ijrm.v13i9.7668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Naseran SN, Mokhtari M, Abedinzade M, Shariati M. Evaluation of the effect of nigella sativa hydro-alcoholic extract and honey on gonadotropins and sex hormones level in the polycystic ovarian syndrome model of Wistar rat. Sci J Kurd Univ Med Sci. 2020;25(1):117–29. doi: 10.52547/sjku.25.1.117. [DOI] [Google Scholar]
- 39.Khani S, Abdollahi M, Khalaj A, Heidari H, Zohali S. The effect of hydroalcoholic extract of Nigella Sativa seed on dehydroepiandrosterone-induced polycystic ovarian syndrome in rats: an experimental study. Int J Reprod Biomed. 2021;19(3):271–82. doi: 10.18502/ijrm.v19i3.8575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.González F. Inflammation in polycystic ovary syndrome: underpinning of insulin resistance and ovarian dysfunction. Steroids. 2012;77(4):300–5. doi: 10.1016/j.steroids.2011.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Aboeldalyl S, James C, Seyam E, Ibrahim EM, Shawki HE, Amer S. The role of chronic inflammation in polycystic ovarian syndrome- a systematic review and meta-analysis. Int J Mol Sci. 2021;22(5):2734. doi: 10.3390/ijms22052734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rudnicka E, Suchta K, Grymowicz M, Calik-Ksepka A, Smolarczyk K, Duszewska AM, et al. Chronic low grade inflammation in pathogenesis of PCOS. Int J Mol Sci. 2021;22(7):3789. doi: 10.3390/ijms22073789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Regidor PA, Mueller A, Sailer M, Gonzalez Santos F, Rizo JM, Egea FM. Chronic Inflammation in PCOS: the potential benefits of specialized pro-resolving lipid mediators (SPMs) in the improvement of the resolutive response. Int J Mol Sci. 2020;22(1):384. doi: 10.3390/ijms22010384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Goswami S, Choudhuri S, Bhattacharya B, Bhattacharjee R, Roy A, Mukhopadhyay S, et al. Chronic inflammation in polycystic ovary syndrome: a case-control study using multiple markers. Int J Reprod Biomed. 2021;19(4):313–20. doi: 10.18502/ijrm.v19i4.9057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Barlampa D, Bompoula MS, Bargiota A, Kalantaridou S, Mastorakos G, Valsamakis G. Hypothalamic inflammation as a potential pathophysiologic basis for the heterogeneity of clinical, hormonal, and metabolic presentation in PCOS. Nutrients. 2021;13(2):520. doi: 10.3390/nu13020520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dabravolski SA, Nikiforov NG, Eid AH, Nedosugova LV, Starodubova AV, Popkova TV, et al. Mitochondrial dysfunction and chronic inflammation in polycystic ovary syndrome. Int J Mol Sci. 2021;22(8):3923. doi: 10.3390/ijms22083923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mahdavi R, Namazi N, Alizadeh M, Farajnia S. Nigella sativa oil with a calorie-restricted diet can improve biomarkers of systemic inflammation in obese women: a randomized double-blind, placebo-controlled clinical trial. J Clin Lipidol. 2016;10(5):1203–11. doi: 10.1016/j.jacl.2015.11.019. [DOI] [PubMed] [Google Scholar]
- 48.Hadi S, Mirmiran P, Daryabeygi-Khotbesara R, Hadi V. Effect of Nigella sativa oil extract on inflammatory cytokine response and oxidative stress among people with type 2 diabetes mellitus: a randomized, double-blind, placebo controlled trial. Prog Nutr. 2018;20 Suppl 1:127–33. [Google Scholar]
- 49.Amizadeh S, Rashtchizadeh N, Khabbazi A, Ghorbanihaghjo A, Ebrahimi AA, Vatankhah AM, et al. Effect of Nigella sativa oil extracts on inflammatory and oxidative stress markers in Behcet's disease: A randomized, double-blind, placebo-controlled clinical trial. Avicenna J Phytomed. 2020;10(2):181–9. [PMC free article] [PubMed] [Google Scholar]
- 50.Almatroodi SA, Alnuqaydan AM, Alsahli MA, Khan AA, Rahmani AH. Thymoquinone, the most prominent constituent of Nigella sativa, attenuates liver damage in streptozotocin-induced diabetic rats via regulation of oxidative stress, inflammation and cyclooxygenase-2 protein expression. Appl Sci. 2021;11(7):3223. doi: 10.3390/app11073223. [DOI] [Google Scholar]
- 51.Hajipour S, Sarkaki A, Dianat M, Rashno M, Khorsandi LS, Farbood Y. The effects of thymoquinone on memory impairment and inflammation in rats with hepatic encephalopathy induced by thioacetamide. Metab Brain Dis. 2021;36(5):991–1002. doi: 10.1007/s11011-021-00688-6. [DOI] [PubMed] [Google Scholar]
- 52.Kohandel Z, Farkhondeh T, Aschner M, Samarghandian S. Anti-inflammatory effects of thymoquinone and its protective effects against several diseases. Biomed Pharmacother. 2021;138:111492. doi: 10.1016/j.biopha.2021.111492. [DOI] [PubMed] [Google Scholar]
- 53.Mancini A, Bruno C, Vergani E, d'Abate C, Giacchi E, Silvestrini A. Oxidative stress and low-grade inflammation in polycystic ovary syndrome: controversies and new insights. Int J Mol Sci. 2021;22(4):1667. doi: 10.3390/ijms22041667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sulaiman MA, Al-Farsi YM, Al-Khaduri MM, Saleh JM, Waly MI. Association of oxidative stress with polycystic ovarian syndrome in Oman: a case-control study. FASEB J. 2018;32 Suppl 1(Suppl 1):787.11. doi: 10.1096/fasebj.2018.32.1_supplement.787.11. [DOI] [Google Scholar]
- 55.Enechukwu CI, Onuegbu AJ, Olisekodiaka MJ, Eleje GU, Ikechebelu JI, Ugboaja JO, et al. Oxidative stress markers and lipid profiles of patients with polycystic ovary syndrome in a Nigerian tertiary hospital. Obstet Gynecol Sci. 2019;62(5):335–43. doi: 10.5468/ogs.2019.62.5.335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Liu Y, Yu Z, Zhao S, Cheng L, Man Y, Gao X, et al. Oxidative stress markers in the follicular fluid of patients with polycystic ovary syndrome correlate with a decrease in embryo quality. J Assist Reprod Genet. 2021;38(2):471–7. doi: 10.1007/s10815-020-02014-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ahmed JH, Ibraheem AY, Al-Hamdi KI. Evaluation of efficacy, safety and antioxidant effect of Nigella sativa in patients with psoriasis: a randomized clinical trial. J Clin Exp Invest. 2014;5(2):186–93. doi: 10.5799/ahinjs.01.2014.02.0387. [DOI] [Google Scholar]
- 58.El-Shanshory M, Hablas NM, Aboonq MS, Fakhreldin AR, Attia M, Arafa W, et al. Nigella sativa improves anemia, enhances immunity and relieves iron overload-induced oxidative stress as a novel promising treatment in children having beta-thalassemia major. J Herb Med. 2019;16:100245. doi: 10.1016/j.hermed.2018.11.001. [DOI] [Google Scholar]
- 59.Alkis H, Demir E, Taysi MR, Sagir S, Taysi S. Effects of Nigella sativa oil and thymoquinone on radiation-induced oxidative stress in kidney tissue of rats. Biomed Pharmacother. 2021;139:111540. doi: 10.1016/j.biopha.2021.111540. [DOI] [PubMed] [Google Scholar]
- 60.Alzohairy MA, Khan AA, Alsahli MA, Almatroodi SA, Rahmani AH. Protective effects of thymoquinone, an active compound of Nigella sativa, on rats with Benzo(a)pyrene-induced lung injury through regulation of oxidative stress and inflammation. Molecules. 2021;26(11):3218. doi: 10.3390/molecules26113218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Liang J, Lian L, Wang X, Li L. Thymoquinone, extract from Nigella sativa seeds, protects human skin keratinocytes against UVA-irradiated oxidative stress, inflammation and mitochondrial dysfunction. Mol Immunol. 2021;135:21–7. doi: 10.1016/j.molimm.2021.03.015. [DOI] [PubMed] [Google Scholar]
- 62.Noh S, Go A, Kim DB, Park M, Jeon HW, Kim B. Role of antioxidant natural products in management of infertility: a review of their medicinal potential. Antioxidants (Basel) 2020;9(10):957. doi: 10.3390/antiox9100957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Forouzanfar F, Hosseinzadeh H. Protective role of Nigella sativa and thymoquinone in oxidative stress: a review. In: Preedy VR, Watson RR, editors. Nuts and seeds in health and disease prevention. 2nd ed. Academic Press; London: 2020. pp. 127–46. [DOI] [Google Scholar]