Highlights
-
•
We examined drug-related adverse effects among nightclub/festival attendees in NYC.
-
•
47.6% of adverse effects involved alcohol and 19.0% involved cannabis.
-
•
Use of less prevalent drugs was associated with higher prevalence of adverse effects.
-
•
Younger age was a risk factor, and past-month use of more drugs was protective.
-
•
Adverse drug effects are common in this scene and results can inform harm reduction.
Keywords: Club drugs, New psychoactive substances, Morbidity, Cannabis, Cocaine
Abstract
Background
Research investigating adverse effects from drug use has focused extensively on poisonings and mortality. This study focuses on drug-related adverse effects not necessarily resulting in hospitalization or death among a population known for high prevalence of party drug use—electronic dance music (EDM) nightclub and festival attendees.
Methods
Adults entering EDM venues were surveyed in 2019–2022 (n = 1952). Those reporting past-month use of a drug were asked whether they had experienced a harmful or very unpleasant effect after use. We examined 20 drugs and drug classes with a particular focus on alcohol, cannabis, cocaine, and ecstasy. Prevalence and correlates of adverse effects were estimated.
Results
Almost half (47.6%) of adverse effects involved alcohol and 19.0% involved cannabis. 27.6% of those using alcohol reported an adverse effect, while 19.5%, 15.0%, and 14.9% of participants reported an effect from use of cocaine, ecstasy, and cannabis, respectively. Use of less prevalent drugs, such as NBOMe, methamphetamine, fentanyls, and synthetic cathinones, tended to be associated with higher prevalence of adverse effects. The most consistent risk factor was younger age, while past-month use of a greater number of drugs was often a protective factor against adverse effects. For most drugs, taking too much was the most common perceived reason for the adverse effect, and visiting a hospital after use was most prevalent among those experiencing an adverse effect from cocaine (11.0%).
Conclusions
Adverse drug effects are common in this population and results can inform prevention and harm reduction in this population and the general population.
1. Introduction
There were over 100,000 deaths related to drug use in the United States (US) in 2021 and the number of deaths continues to increase (Ahmad et al., 2022). The majority of deaths have been linked to opioid use, though large proportions were also related to use of cocaine and psychostimulants such as methamphetamine. Granted, mortality may be the gravest adverse outcome that could arise from drug use, but research has largely overlooked less severe outcomes—ranging from symptoms such as nausea or headaches to acute effects in which the person using feels they are in possible danger. Such effects may be more prevalent and perhaps as important for both policymakers and individuals who use drugs alike. Indeed, most information on adverse drug-related adverse effects in the US is based on national data focusing on hospitalizations, reported poisonings, and deaths. However, these data are limited insofar as they tend to represent severe outcomes that can ultimately bias estimates of risk associated with use of specific drugs. Additional research is needed with a focus on adverse effects associated with drug use that does not necessarily result in hospitalizations, poisonings, or death, in order to better inform prevention and harm reduction efforts.
National mortality data suggest that most deaths involving illegal drug use in 2020 involved fentanyl or other novel opioids (56,516), followed by deaths involving use of psychostimulants including methamphetamine (23,837), cocaine (19,447), and heroin (13,165) (Hedegaard et al., 2021). The Drug Abuse Warning Network is the main source of national data on drug-related hospitalizations (emergency department [ED] visits). Recent estimates suggest that the majority (39%) of drug-related ED visits in 2021 involved alcohol use (2.9 million), followed by use of opioids (1 million), methamphetamine (0.8 million), cannabis (7.9 million), and cocaine (0.3 million) (Substance Abuse and Mental Health Services Administration [SAMHSA], 2022). Estimates of deaths or ED visits related to use of most other drugs are not available but may be somewhat approximated by national Poison Control data (Palamar et al., 2022a,b). In 2020, alcohol had the most reported poisonings (53,489), followed by cannabis (16,004), amphetamine (16,001), methamphetamine (8987), heroin (8007), cocaine (5026), fentanyl (4689), other phenethylamines (e.g., MDMA, 2C series; 1998), LSD (1450), and synthetic cannabinoids (1202) (Gummin et al., 2021). Other drugs commonly used in recreational contexts, such as nightclubs, were associated with fewer reported poisonings. For example, there were 766 reported poisonings related to use of gamma-hydroxybutyrate (GHB) and its analogs, 343 poisonings related to ketamine and its analogs, 215 related to use of amyl/butyl nitrites (poppers), and 81 related to use of tryptamines (Gummin et al., 2021).
National morbidity and mortality data are inherently limited as they typically capture the most severe cases of poisoning, while hospitalization and Poison Control data are limited to people who seek professional help to treat adverse effects. This study aims to address these gaps in the literature by focusing on an array of adverse effects reported by a population known for reporting high prevalence of a variety of party drugs and novel psychoactive substances (NPS)—people who attend electronic dance music (EDM) parties at nightclubs and large dance festivals (Hughes et al., 2017; Palamar and Keyes, 2020). More specifically, we examine prevalence of recent self-reported adverse effects relative to use, as well as the reported symptomology and perceived reasons for experiencing such effects, based on rapid survey results from EDM party attendees entering nightlife venues.
2. Methods
2.1. Study population
Time-space sampling was implemented to survey adults entering EDM parties at nightclubs and dance festivals in New York City (NYC). The study was conducted from January 2019 through September 2022, although data collection was halted from February 2020 through June 2021 due to the COVID-19 pandemic. Each week, events were randomly selected based on an ongoing list of nightclubs and parties listed on a popular EDM party ticket website. Recruitment was typically conducted on 1–2 nights per week from Thursday through Sunday. While the majority of participants were surveyed entering nightclubs, participants were also surveyed as they approached 1–2 daytime EDM dance festivals each year. Individuals were eligible if they were age ≥18 and about to enter the selected venue. Participants provided informed consent and subsequently took the rapid anonymous survey at the point of recruitment on an electronic tablet. Survey completers were compensated $10 USD. Participants were surveyed entering 133 events—80 in 2019, 8 in early 2020, 23 in 2021, and 22 in 2022, and survey response rates were 65%, 82%, 63%, and 82%, respectively. The total sample size was 1952, with 1005 surveyed 2019, 104 in 2020, 349 in 2021, and 494 in 2022. All methods were approved by the New York University Langone Medical Center institutional review board.
2.2. Measures
Participants were first asked about demographic characteristics including their age, sex, race/ethnicity, education, and sexual orientation, as well as their frequency of past-year EDM party attendance. Participants were then asked about past-month use of 20 different drugs or drug classes. They were asked about use of common drugs, nonmedical psychoactive drug use, and about use of NPS and uncommon drugs. Specifically, they were asked about use of alcohol, cannabis, cocaine, ecstasy/MDMA/Molly, poppers (amyl/butyl nitrites), ketamine, shrooms (mushrooms, psilocybin), LSD, GHB, methamphetamine, and heroin. While ecstasy and Molly are common ‘street’ names for MDMA, these drugs do not always actually contain MDMA, and people who use are often unaware of the drug's actual contents. Therefore, we assessed ecstasy, MDMA, and Molly together via a single item. Participants were also asked about nonmedical use of amphetamine, benzodiazepines, and prescription opioids. Nonmedical use was defined as use without a prescription or use in a manner in which the drug was not prescribed, such as to get ‘high’ (SAMHSA, 2015). Nonmedical amphetamine use was queried via a single item, and nonmedical use of prescription opioids and benzodiazepines was determined by the participant reporting nonmedical use of any of 8 and 11 drugs in these classes, respectively. With regard to NPS and other novel drugs, participants were asked about use of 13 synthetic cathinones (“bath salts”), 8 tryptamines, 5 2C series drugs, 4 novel opioids including fentanyls, and NBOMe series drugs and synthetic cannabinoids via single items. A list of drugs queried is presented in Supplemental Table 1. Lists of NPS had an answer option for “other” compounds in that class not listed and below this option was a list of other compounds in the drug class not specifically queried. An affirmative response to any drug in a class was coded as an affirmative response to use of that class.
Those reporting past-month use of a drug were asked whether they had experienced a harmful or very unpleasant effect after using the drug in the past 30 days. We further specified that this refers to a drug effect in which the participants felt their health and safety were at immediate risk. This definition was based upon previous literature in which the drug effect was perceived to be harmful and/or unpleasant (Edwards and Aronson, 2000). Those answering affirmatively were provided follow-up questions, inquiring whether they asked someone for help and whether they visited a hospital or ED. They were also asked the reason(s) why they thought the adverse drug outcome happened (with 9 answer options in which they could check all that apply), and they were also provided a 16-item checklist to select which specific effect(s) occurred when the adverse drug effect happened, based on past literature (Cloutier et al., 2013; Degenhardt et al., 2002; Hall, 2017; Parrott, 2013; Zawilska and Andrzejczak, 2015). They were also asked how long ago the event occurred. While participants were asked about adverse effects related to use of each individual drug queried, effects resulting from use of a drug in a class were based on participants reporting an adverse effect to a drug in that class.
2.3. Analyses
Descriptive statistics were first computed to describe sample characteristics, and the prevalence of self-reported past-month use of each drug or drug class was calculated as well as the prevalence of having experienced an adverse effect. Prevalence was determined relative to the sample size (prevalence of reporting any adverse effect) and relative to the total count of adverse effects reported across all drugs. Among those reporting an adverse effect associated with use of a specific drug, the prevalence of the participant asking for help or visiting a hospital/ED were calculated. Prevalence of reported reasons for the adverse effect and for specific symptoms were also computed. To examine stability of adverse effects across time, quarterly trends in reporting an adverse effect were computed for the four most prevalent drugs—alcohol, cannabis, cocaine, and ecstasy. For these analyses, logistic regression was used to determine whether there was a linear trend by estimating odds of reporting an adverse outcome as a linear function of time (quarter). Finally, bivariable and multivariable models were used to delineate potential correlates of reporting an adverse effect focusing on the four most prevalent drugs. Specifically, chi-square was used to determine if prevalence of reporting an adverse effect differed according to demographic characteristics, level of party attendance, number of drugs used in the past month, and where the survey took place (nightclub vs. festival). Then, all independent variables were fit into separate models (for each drug) to examine associations in a multivariable manner. Generalized linear model using Poisson and log link was used to generate adjusted prevalence ratios (aPRs) for each independent variable. Data were analyzed using Stata 17 SE (StataCorp, College Station, TX).
3. Results
Sample characteristics are presented in Table 1. The majority of participants were male (55.0%), heterosexual (67.7%), and had at least a college degree (68.1%). The average age was 26.7 years (SD = 6.0) and the plurality identified as white (48.6%).
Table 1.
Sample characteristics (N = 1952).
| n | % | |
|---|---|---|
| Age | Mean = 26.7 | SD = 6.0 |
| Sex | ||
| Male | 1074 | 55.0 |
| Female | 878 | 45.0 |
| Race/Ethnicity | ||
| White | 948 | 48.6 |
| Black | 159 | 8.2 |
| Hispanic | 377 | 19.3 |
| Asian | 389 | 14.8 |
| Other/Mixed | 179 | 9.2 |
| Education | ||
| College Degree or Higher | 1329 | 68.1 |
| Less than College Degree | 623 | 31.9 |
| Sexual Orientation | ||
| Heterosexual | 1322 | 67.7 |
| Gay/Lesbian | 278 | 14.2 |
| Bisexual | 285 | 14.6 |
| Other | 67 | 3.4 |
| Party Attendance | ||
| Never /1–2 Times Per Year | 408 | 20.9 |
| Every Few Months | 480 | 24.6 |
| Monthly | 353 | 18.1 |
| Every Other Week | 366 | 18.8 |
| Every Week or More Often | 345 | 17.7 |
| Past-Month Drug Use | ||
| 0–2 Drugs | 1187 | 60.8 |
| 3–4 Drugs | 502 | 25.7 |
| 5–6 Drugs | 188 | 9.6 |
| ≥7 Drugs | 75 | 3.8 |
| Where Surveyed | ||
| Nightclub | 1692 | 86.7 |
| Festival | 260 | 13.3 |
The majority of participants (86.7%) reported using at least one queried drug in the past month, with 70.8% reporting use of a drug other than alcohol. Among those reporting use of any drug, 31.9% reported experiencing an adverse effect (17.8% when excluding effects related to alcohol use). Of the 885 adverse effects reported in total for individual drugs among the 622 participants reporting any adverse effect, relative to those reporting any adverse effect, alcohol contributed to almost half of reported instances (47.6%), followed by cannabis (19.0%), cocaine (9.0%), and ecstasy (6.2%) (Table 2). Adverse effects related to heroin, fentanyl, and other novel opioids only accounted for 0.3% of adverse effects.
Table 2.
Prevalence of self-reported adverse effects of specific drugs relative to all adverse effects reported.
| n | % | |
|---|---|---|
| Alcohol | 421 | 47.6 |
| Cannabis | 168 | 19.0 |
| Cocaine | 80 | 9.0 |
| Ecstasy | 55 | 6.2 |
| Ketamine | 27 | 3.1 |
| Poppers | 25 | 2.8 |
| Psilocybin | 17 | 1.9 |
| Amphetamine | 17 | 1.9 |
| LSD | 15 | 1.7 |
| Synthetic Cathinones | 10 | 1.1 |
| Benzodiazepines | 9 | 1.0 |
| Methamphetamine | 9 | 1.0 |
| GHB | 8 | 0.9 |
| 2C Series | 6 | 0.7 |
| Prescription Opioids | 5 | 0.6 |
| Synthetic Cannabinoids | 4 | 0.5 |
| Tryptamines | 4 | 0.5 |
| Fentanyls/Novel Opioids | 2 | 0.2 |
| NBOMe | 2 | 0.2 |
| Heroin | 1 | 0.1 |
Note. Prevalence is relative to the 885 separate drug-related effects reported by 622 participants (31.9% of the full sample). Poppers refer to amyl or butyl nitrites.
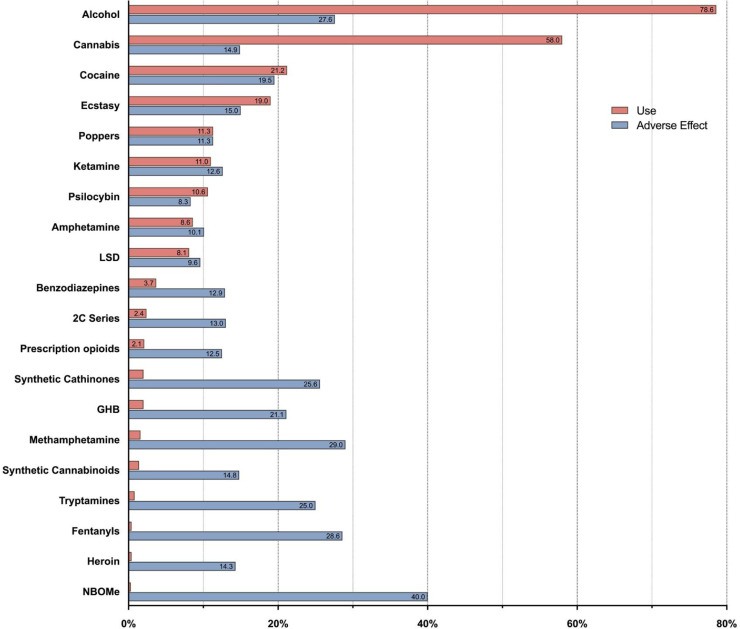
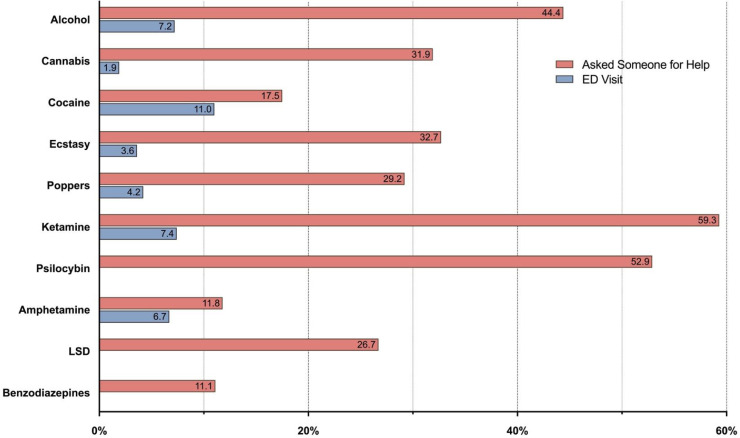
Figure 1 presents the prevalence of past-month use of each drug or drug class and whether an adverse effect was reported. The drugs most commonly used in the past month were alcohol (78.6%), cannabis (58.0%), cocaine (21.2%), and ecstasy (19.0%). Over a third (37.3%) of adverse effects from cannabis involved edibles. Rarer drugs tended to have a higher prevalence of reported adverse effects associated with use, including 40.0% of NBOMe use, followed by methamphetamine (29.0%), fentanyls or other novel opioids (28.6%), synthetic cathinones (25.6%), tryptamines (25.0%), GHB (21.1%), synthetic cannabinoids (14.8%), and heroin (14.3%). Supplemental Table 2 presents data on when the adverse effect occurred, and trend analysis suggests that the prevalence of adverse effects related to use of alcohol, cannabis, cocaine, and ecstasy were stable across the study period (ps > 0.05) (Supplemental Figure 1). Figure 2 presents the prevalence of participants having asked someone for help and for visiting a hospital or ED in response to experiencing an adverse effect for the ten most prevalent drugs. Among those experiencing an adverse effect after using ketamine or psilocybin, 59.3% and 52.9%, respectively, asked someone for help. Visiting a hospital or ED after use was rare, but highest among those reporting an adverse effect related to cocaine use (11.0%), followed by ketamine use (7.4%), alcohol use (7.2%), and amphetamine use (6.7%). Prevalence of past-month use, report of an adverse effect, and prevalence of asking for help and visiting a hospital/ED are reported in detail in Supplemental Table 3.
Fig. 1.
Prevalence of use and report of experiencing an adverse effect.
Fig. 2.
Among those experiencing an adverse effect, prevalence of asking someone for help and of visiting a hospital.
Specific symptoms associated with adverse effects related to use of alcohol, cannabis, cocaine, and ecstasy are presented in Fig. 3. Nausea/vomiting (49.4%), headache (41.3%), and unconsciousness (23.8%) were most commonly reported as symptoms related to alcohol use, and paranoia (36.3%), confusion (29.2%), and hallucination (8.3%) were most commonly experienced as symptoms related to cannabis use. Cocaine use was most commonly associated with tachycardia (heart racing, 42.5%) and anxiety (32.7%), and ecstasy use was commonly associated with anxiety (32.7%) and overheating (27.3%). Figure 4 presents prevalence of suspected reasons why adverse effects occurred, focusing on the four most prevalent drugs. Taking too much was the most common reason for all four drugs, particularly alcohol (72.0%) and cannabis (43.5%). Nearly a third (31.6%) of those experiencing an adverse effect related to cannabis use reportedly had no idea why the effect occurred, while not being in the right mindset (18.2%) and low quality drug (16.4%) were additional common reported reasons for ecstasy. Prevalence of specific effects and suspected reasons for adverse effects for all drugs and drug classes are presented in detail in Supplemental Tables 4 and 5, respectively.
Fig. 3.
Specific adverse effects reported among those reporting experiencing an adverse effect.
Fig. 4.
Perceived reasons for experiencing reported adverse effects.
Bivariable correlates of reporting an adverse effect related to use of alcohol, cannabis, cocaine, or ecstasy are presented in Table 3. With respect to alcohol, younger participants on average were more likely to report an adverse effect (Mean [M] = 25.7 [SD = 5.0] vs. 27.0 [SD = 5.9], p < 0.001), and there was a detected difference regarding sexual orientation (p = 0.006) with a post hoc test suggesting that participants of bisexual and other sexual identity were at risk. Regarding cannabis use, younger participants on average were more likely to report an adverse effect (M = 24.5 [SD = 4.2] vs. 26.7 [SD = 5.6], p < 0.001), as were females (p = 0.033). There were also detected differences regarding race/ethnicity (p = 0.040) and number of drugs used (p = 0.003), with post hoc tests suggesting that Asians and those reporting use of 1–2 drugs were at particularly high risk. With respect to cocaine, those with less than a college education were at risk (p = 0.35), as were those reporting use of 1–2 drugs (p = 0.016). Regarding ecstasy use, younger participants on average were more likely to report an adverse effect (M = 25.5 [SD = 4.3] vs. 27.6 [SD = 5.3], p = 0.005). Multivariable correlates of reporting an adverse effect related to use are presented in Table 4. With all else being equal, younger age remained a risk factor for experiencing an adverse effect related to use of alcohol (aPR = 0.97, 95% CI: 0.95–0.99), cannabis (aPR = 0.92, 95% CI: 0.88–0.96), and ecstasy (aPR = 0.92, 95% CI: 0.86–0.99). Among those who used cannabis, identifying as Asian was associated with increased risk (aPR = 1.52, 95% CI: 1.01–2.30) and among those who used cocaine, identifying as Hispanic was a risk factor (aPR = 1.86, 95% CI: 1.02–3.40). Finally, compared to those using 1–2 drugs, those using 3–4 were at lower risk for reporting an adverse effect related to use of cannabis (aPR = 0.53, 95% CI: 0.37–0.78) and ecstasy (aPR = 0.42, 95% CI: 0.18–0.97), and use of more drugs was associated with lower risk of experiencing an adverse effect related to cocaine use in a dose-response-like manner.
Table 3.
Bivariable correlates of reporting an adverse effect from use of alcohol, cannabis, cocaine, or ecstasy.
| Alcohol (n = 1523) |
Cannabis (n = 1129) |
Cocaine (n = 411) |
Ecstasy (n = 367) |
|||||
|---|---|---|---|---|---|---|---|---|
| No % | Yes % | No % | Yes % | No % | Yes % | No % | Yes % | |
| Age—Mean (SD) | 27.0 (5.9) | 25.7 (5.0)c | 26.7 (5.6) | 24.5 (4.2)c | 26.8 (5.3) | 26.3 (5.1) | 27.6 (5.3) | 25.5 (4.3)b |
| Sex | ||||||||
| Male | 56.1 | 50.8 | 56.5 | 47.6a | 58.3 | 68.8 | 64.7 | 60.0 |
| Female | 43.9 | 49.2 | 43.5 | 52.4 | 41.7 | 31.3 | 35.3 | 40.0 |
| Race/Ethnicity | ||||||||
| White | 50.8 | 50.1 | 50.5 | 46.4a | 58.3 | 46.3 | 51.3 | 43.6 |
| Black | 7.4 | 7.1 | 8.2 | 8.9 | 4.5 | 6.3 | 3.9 | 3.6 |
| Hispanic | 18.6 | 19.5 | 18.9 | 18.5 | 13.6 | 21.3 | 21.5 | 27.3 |
| Asian | 14.3 | 14.5 | 12.8 | 20.8 | 14.2 | 12.5 | 15.4 | 12.7 |
| Other/Mixed | 9.0 | 8.8 | 9.6 | 5.4 | 9.4 | 13.8 | 8.0 | 12.7 |
| Education | ||||||||
| ≥College Degree | 70.9 | 69.4 | 68.8 | 62.5 | 74.3 | 62.5a | 71.5 | 61.8 |
| <College Degree | 29.1 | 30.6 | 31.2 | 37.5 | 25.7 | 37.5 | 28.5 | 38.2 |
| Sexual Orientation | ||||||||
| Heterosexual | 66.7 | 63.9b | 64.4 | 60.7 | 59.8 | 66.3 | 61.2 | 63.6 |
| Gay/Lesbian | 16.2 | 12.1 | 14.5 | 13.7 | 15.1 | 16.3 | 18.6 | 21.8 |
| Bisexual | 14.1 | 18.8 | 16.7 | 20.2 | 21.2 | 13.8 | 17.0 | 12.7 |
| Other | 3.0 | 5.2 | 4.5 | 5.4 | 3.9 | 3.8 | 3.2 | 1.8 |
| Party Attendance | ||||||||
| Never /1–2 Times Per Year | 18.4 | 16.2 | 15.3 | 13.1 | 8.8 | 6.3 | 7.7 | 7.3 |
| Every Few Months | 24.1 | 23.3 | 23.9 | 24.4 | 17.2 | 20.0 | 16.4 | 18..2 |
| Monthly | 19.3 | 19.7 | 20.4 | 17.9 | 19.0 | 13.8 | 20.8 | 12.7 |
| Every Other Week | 19.6 | 20.9 | 20.1 | 26.2 | 24.2 | 21.3 | 25.3 | 27.3 |
| Every Week or More Often | 18.6 | 20.0 | 20.3 | 18.5 | 30.8 | 38.8 | 29.8 | 34.6 |
| Past-Month Drug Use | ||||||||
| 0–2 Drugs | 51.9 | 53.4 | 39.7 | 53.0b | 6.3 | 17.5a | 8.3 | 16.4 |
| 3–4 Drugs | 31.5 | 31.6 | 39.9 | 25.6 | 46.2 | 41.3 | 45.5 | 41.8 |
| 5–6 Drugs | 11.6 | 10.5 | 14.3 | 14.9 | 32.9 | 28.8 | 30.1 | 29.1 |
| ≥7 Drugs | 4.8 | 4.5 | 6.2 | 6.6 | 14.5 | 12.5 | 15.1 | 12.7 |
| Where Surveyed | ||||||||
| Nightclub | 85.9 | 87.9 | 86.0 | 89.9 | 92.2 | 90.0 | 85.3 | 81.8 |
| Festival | 14.1 | 12.1 | 14.0 | 10.1 | 7.8 | 10.0 | 14.7 | 18.2 |
Note. SD = standard deviation.
< 0.05.
p < 0.01.
p < 0.001.
Table 4.
Multivariable correlates of reporting an adverse effect from use of alcohol, cannabis, cocaine, or ecstasy.
| Alcohol aPR (95% CI) | Cannabis aPR (95% CI) | Cocaine aPR (95% CI) | Ecstasy aPR (95% CI) | |
|---|---|---|---|---|
| Age | 0.97 (0.95–0.99)b | 0.92 (0.88–0.96)c | 0.97 (0.93–1.02) | 0.92 (0.86–0.99)a |
| Sex | ||||
| Male | 1.00 | 1.00 | 1.00 | 1.00 |
| Female | 1.02 (0.83–1.26) | 1.13 (0.81–1.57) | 0.70 (0.41–1.18) | 1.22 (0.66–2.25) |
| Race/Ethnicity | ||||
| White | 1.00 | 1.00 | 1.00 | 1.00 |
| Black | 0.90 (0.61–1.33) | 1.05 (0.59–1.88) | 1.35 (0.52–3.50) | 1.05 (0.23–4.76) |
| Hispanic | 1.05 (0.81–1.36) | 1.00 (0.65–1.53) | 1.86 (1.02–3.40)a | 1.39 (0.69–2.83) |
| Asian | 1.02 (0.77–1.36) | 1.52 (1.01–2.30)a | 1.14 (0.55–2.35) | 0.91 (0.37–2.24) |
| Other/Mixed | 0.98 (0.69–1.39) | 0.65 (0.33–1.30) | 1.76 (0.88–3.51) | 1.63 (0.69–3.88) |
| Education | ||||
| ≥College Degree | 1.00 | 1.00 | 1.00 | 1.00 |
| <College Degree | 0.96 (0.77–1.20) | 1.03 (0.73–1.47) | 1.27 (0.78–2.06) | 1.16 (0.63–2.11) |
| Sexual Orientation | ||||
| Heterosexual | 1.00 | 1.00 | 1.00 | 1.00 |
| Gay/Lesbian | 0.94 (0.69–1.28) | 1.35 (0.84–2.19) | 1.01 (0.53–1.93) | 1.39 (0.67–2.85) |
| Bisexual | 1.24 (0.96–1.62) | 1.21 (0.80–1.83) | 0.79 (0.40–1.59) | 0.62 (0.26–1.46) |
| Other | 1.55 (0.99–2.41) | 1.26 (0.63–2.53) | 0.77 (0.23–2.54) | 0.50 (0.06–3.87) |
| Party Attendance | ||||
| Never /1–2 Times Per Year | 1.00 | 1.00 | 1.00 | 1.00 |
| Every Few Months | 0.97 (0.72–1.32) | 1.28 (0.79–2.06) | 0.70 (0.38–1.31) | 0.85 (0.42–1.71) |
| Monthly | 0.94 (0.69–1.29) | 1.00 (0.59–1.69) | 0.63 (0.31–1.29) | 0.56 (0.23–1.38) |
| Every Other Week | 0.93 (0.68–1.27) | 1.12 (0.68–1.86) | 0.89 (0.47–1.69) | 0.81 (0.35–1.87) |
| Every Week or More Often | 0.87 (0.62–1.22) | 0.96 (0.53–1.72) | 0.65 (0.25–1.70) | 0.76 (0.23–2.47) |
| Past-Month Drug Use | ||||
| 1–2 Drugs | 1.00 | 1.00 | 1.00 | 1.00 |
| 3–4 Drugs | 0.95 (0.76–1.19) | 0.53 (0.37–0.78)b | 0.51 (0.26–0.98)a | 0.42 (0.18–0.97)a |
| 5–6 Drugs | 0.90 (0.64–1.26) | 0.89 (0.56–1.42) | 0.43 (0.21–0.87)a | 0.46 (0.19–1.12) |
| ≥7 Drugs | 0.93 (0.57–1.53) | 0.83 (0.42–1.65) | 0.39 (0.16–0.95)a | 0.39 (0.13–1.16) |
| Where Surveyed | ||||
| Nightclub | 1.00 | 1.00 | 1.00 | 1.00 |
| Festival | 0.88 (0.65–1.20) | 0.66 (0.39–1.12) | 1.32 (0.59–2.98) | 1.16 (0.55–2.45) |
Note. Each model controlled for year of survey. aPR = adjusted prevalence ratio; CI = confidence interval.
p < 0.05.
p < 0.01.
4. Discussion
The goal of the present study was to develop a more granular understanding of drug-related adverse effects by investigating the prevalence of adverse outcomes beyond only those that result in mortality, hospitalizations, or poisonings. This study focused on people who attend EDM parties at nightclubs and large dance festivals as drug use is known to be prevalent among attendees (Hughes et al., 2017; Palamar and Keyes, 2020), and in fact is often regarded as an integral part of such party culture (Reynolds, 1999). Alcohol, cannabis, cocaine, and ecstasy were the most commonly used drugs and further accounted for the highest proportion of adverse effects (relative to the total number of adverse effects from all drugs). However, we also detected differential risk of adverse effects relative to use of each drug which can further inform prevention and harm reduction.
Alcohol—the most prevalent drug—resulted in the highest proportion of adverse effects, accounting for almost half (47.6%) of adverse effects reported. This may be unsurprising as alcohol is the most prevalent drug in the US, and the majority of drug-related ED visits in 2021 involved alcohol (SAMHSA, 2022). In 2019, among people aged 18–25 in the US, an estimated 54.3% consumed alcohol in the past month and over a third (34.3%) of people in this age group binge-drank in the past month, with 8.4% engaging in heavy alcohol use (defined as binge drinking five or more times in the past month) (Center for Behavioral Health Statistics and Quality, 2020). Despite some positive social aspects of alcohol consumption, adverse effects commonly include hangover, blackout, regretted or unwelcome behavior including sexual activities, arguments or fights, and injury (Palamar et al., 2014; Park, 2004; Park and Grant, 2005). Hangover, although not typically grave, is particularly common, with studies of college students finding that 27.8–32.5% have gotten sick or hungover after consumption (Park, 2004). This is noteworthy as many adverse effects queried in the present study, such as headache, nausea, and tachycardia, are commonly associated with hangover (Vatsalya et al., 2018), and can be predicted by higher frequency, quantity, and speed of alcohol consumption (Carpenter and Merrill, 2021; Park, 2004; Park and Grant, 2005). Alcohol is also commonly used in combination with other drugs, which can often increase risk of an adverse effect or hospitalization (Palamar et al., 2019b; SAMHSA, 2022) and consequently makes the drug uniquely dangerous.
Cannabis was the second-most prevalent drug and accounted for almost a fifth (19.0%) of adverse effects reported in this study. Prevalence of past-month cannabis use in the US recently increased to 11.5% in 2019, and over 40% of these individuals used ≥20 times per month (Palamar et al., 2021a). Although cannabis is not typically regarded as a very dangerous drug, edibles—due to delayed onset of effects—increase the risk for unexpected highs and paranoia (Allen et al., 2017). Indeed, over a third (37%) of participants reporting an adverse effect from cannabis reported using edibles, which is in accordance with the prevalence of cannabis-related poisonings involving edibles reported to Poison Control in 2020 (37%) (Gummin et al., 2021). Our results also corroborate previous studies; for example, one study of college students found that 20.1% passed out from use, 11.1% experienced nausea and/or vomiting, and 5.7% blacked out (Simons et al., 2012).
Cocaine was the third-most prevalent drug used and accounted for the third-most adverse effects. Among common party drugs, it is widely agreed that cocaine is among the most dangerous (Gable, 1993, 2004; Morgan et al., 2010; Nutt et al., 2010). To this end, we found that cocaine had the highest prevalence (11.0%) of an adverse effect resulting in a hospital visit. Indeed, national data show that cocaine use was linked to 19,447 deaths in 2020 and an estimated 336,516 ED visits in 2021 (Hedegaard et al., 2021; SAMHSA, 2022). Results of our study found that several adverse effects reported in other studies are common; for example, among a study of hospitalized patients, tachycardia was among the most common symptoms (40.9%), followed by anxiety (32.2%), agitation/aggression (27.4%), chest pain (17.6%), vomiting (9.7%), and hallucinations (6.7%) (Miró et al., 2019). A review also reported that 1.7–13% of patients hospitalized for cocaine-related adverse effects reported a headache (Barbanti et al., 2017). Chest pain linked to cocaine use is of particular concern as it is associated with increased risk for myocardial infarction (Bosch et al., 2010; Wang et al., 2021). Given that cocaine is commonly combined with alcohol (Miró et al., 2019; Palamar et al., 2019b), the cocaethylene produced by this combination even further increases risk for adverse effects (Andrews, 1997).
Ecstasy was the fourth-most prevalent drug, with 15.0% of those using in the past month reporting adverse effects. Due to ecstasy's popularity in the EDM scene, it has historically been the main drug of focus for nightclub-related harm reduction (Jacinto et al., 2008; Panagopoulos and Ricciardelli, 2005). While some studies have investigated adverse effects experienced by those who use ecstasy, there are no national data on morbidity or mortality because Poison Control has categorized ecstasy within a broader category of hallucinogenic amphetamines or phenethylamines, while national mortality data includes ecstasy within the category of psychostimulants (Gummin et al., 2021; Kariisa et al., 2019). Results of this study corroborate previous research suggesting that the most common adverse effects from use are increases in core temperature (which are also influenced by ambient temperature, including the temperature in nightclubs), increased sweating, tachycardia, tremor, anxiety, and even agitation (Hall and Henry, 2006; Parrott, 2012). Reviews, however, have found sizeable variation with respect to effects such as nausea or vomiting (2–58%), headache (3–60%), sweating (3–85%), and accelerated heart rate (13–100%) (Baylen and Rosenberg, 2006).
There were many other notable findings in this study regarding adverse effects from use of other drugs. Though associated with a lower prevalence of use, we found that NBOMe was most likely to result in an adverse effect. Previous literature has noted the dangers of this compound, especially among people using the drug believing that it is LSD (Zawilska et al., 2020). Similarly, although use was rare, heroin, fentanyls, and other novel opioids, were also associated with high prevalence of adverse effects. Although intentional use of fentanyls is rare in this population, attendees need to be aware that drugs, such as cocaine, can be adulterated or contaminated with fentanyl (DiSalvo et al., 2020; Palamar et al., 2021c). With respect to psychedelics and hallucinogens, we found that 52.9% and 26.7% of attendees that used psilocybin and LSD, respectively, reported having to ask someone for help, despite these drugs having an adverse effect prevalence of less than 10% and despite there being no reported hospitalizations due to use. Ketamine had 59.3% of people experiencing an adverse effect ask someone for help. This likely indicates that uneasiness or panic are a part of psychedelic or dissociative drug effects. Given that the prevalence of both ketamine use and poisonings appears to be increasing (Palamar et al., 2022a,b; Palamar et al., 2021b), this drug in particular may need additional harm reduction focus in the future. Patrons also need to feel comfortable asking friends, peers, or party staff for help if necessary, without fear of negative ramifications. It may feel particularly risky to ask staff for help at festivals held on public grounds, given that police are often present (Palamar and Sönmez, 2022). In such cases, festival staff should aim to foster a “safe space” atmosphere that allows patrons to feel welcome to ask for help without necessarily openly condoning drug use.
With regard to correlates of adverse effects, we found that younger age was associated with increased risk of experiencing an adverse effect owing to use of alcohol, cannabis, and ecstasy. Recent hospitalization data suggest that the (broad) age group at greatest risk for hospitalization related to use of these drugs is age 26–44 (SAMHSA, 2022). While people tend to become more vulnerable to drug effects as they age into later adulthood (Kuerbis, 2020), younger people may have less experience, potentially leading them to use in a more reckless or unconcerned manner (especially in nightlife settings). For these reasons, younger people may benefit from specific prevention and harm reduction efforts. By this same token, our findings also consistently demonstrated that past-month use of a higher number of drugs tended to be a protective factor against experiencing or reporting an adverse effect related to use of cannabis, cocaine, and ecstasy. In this respect, we believe that use of more drugs is an indicator of more drug-related experience (which can include increased tolerance) and possibly also more education about potential adverse effects from use. We do not know the extent to which participants combined drugs, but more research into mechanisms for this association is needed.
Prevalence results as well as suspected reasons for adverse effects in this study suggest the need for people in this scene to use traditional harm reduction methods to prevent or limit adverse effects. Common harm reduction information for ecstasy and other drugs has suggested being in the right mindset before and during use, planned use, adequate rest before use, avoidance of mixing drugs (especially alcohol), and avoidance of exposure to adulterants by testing drugs or by limiting purchases to trusted dealers (Greenspan et al., 2011; Jacinto et al., 2008; Palamar et al., 2019a; Panagopoulos and Ricciardelli, 2005; Zinberg, 1984). The Illicit Drug Anti-Proliferation Act, formerly titled the Reducing Americans’ Vulnerability to Ecstasy Act (the “RAVE Act”) has been cited by harm reductionists as a major barrier to drug checking and distribution of drug education at nightlife venues (Palamar et al., 2019c). Given that policy overseeing relevant harm reduction practices will be slow to change, public health experts need to continue to try to find ways to promote harm reduction.
4.1. Limitations
While this study specifically focused on adverse effects, it only asked about 15 specific effects because the survey was rapid and conducted quickly at the point of recruitment. There are many more common adverse effects, and these are by no means limited to physical effects. As such, this study only served to help provide general information about adverse drug effects and it does not provide a complete picture. A larger study could also focus on positive effects and not limit effects to sequalae. Frequency or amount of drug used were not queried, and many other factors could have contributed to adverse effects including set and setting, medications, allergies, use disorder, tolerance, experience, expectations, and the general uniqueness of each individual's body. Given that this population in particular uses drugs in nightlife and festival settings, set and setting is of particular relevance, especially for drugs with hallucinogenic or psychedelic effects. For example, sensory overload through loud music, bright light shows, and large crowds—largely of unknown people—can increase one's chances of experiencing unpleasant (e.g., psychological) effects, especially with little-to-no experience with the drug used (Palamar and Sönmez, 2022). As such, experiences can be very different in such contexts compared to more laid-back situations. With regard to experience, it is possible that more frequent users are used to certain adverse effects to the point of them not feeling significant enough to report. However, others may have overreported minor symptoms as serious. It should also be noted that some symptoms (e.g., confusion) may be common, expected, and/or even appreciated effects from specific drugs, but we first asked participants if they experienced any adverse effects and then asked them to check off which. As such, most participants checking off specific effects as “adverse” likely indeed considered them adverse, although it is possible that not all truly considered them adverse. While people reporting use in the past month were asked about adverse effects, effects reported were not limited to effects in the past month. As such, we interpret this as report of recent adverse effects. Many subsample sizes were small (e.g., for rarer drugs) so prevalence of effects and related symptoms should be viewed with caution.
This study did not systematically query the direct combination of drugs that led to reported adverse effects. This study did, however, ask participants if they believed effects resulted from polydrug use although specific drug combinations were not queried. Relatedly, the purity of drugs participants reported taken is unknown and toxicology testing was not conducted. Party drugs such as ecstasy and cocaine are commonly adulterated (DiSalvo et al., 2020; Oliver et al., 2018; Palamar and Salomone, 2021) so it is possible that reported effects are due, in part, to exposure to other drugs. Compared to NYC overall, the percentage of black participants was low (8.2% vs. 23.4% in NYC), but in our extensive experience recruiting in this scene, black individuals tend to be less likely to attend such parties. Despite this being a racially and ethnically diverse sample, participants tended to be of higher socioeconomic status which may make results less generalizable to other populations. Finally, while events (e.g., at nightclubs) were randomly selected based on an ongoing list of parties, it is possible that the overall selection of events was biased towards or against high prevalence of drug use and drug acceptability.
4.2. Conclusions
Drug use and related adverse effects were common in this high-risk population. The most commonly used drugs accounted for the most adverse effects, although relative to use, less prevalent drugs were found to often be riskier in terms of adverse effects. These results can help address gaps in the existing literature regarding morbidity and mortality data. Results can help inform prevention and hard reduction efforts, which are still very much needed not only in this high-risk population but in other populations as well.
Contributors
Both authors are responsible for this reported research. J. Palamar conceptualized and designed the study. J. Palamar conducted the statistical analyses. A. Le oversaw graphical representation of results. Both authors interpreted results, drafted the manuscript, and critically reviewed and revised the manuscript. The authors approved the final manuscript as submitted.
Declaration of Competing Interest
Authors declare that they have no conflict of interest.
Acknowledgments
Role of funding source
Research reported in this publication was supported by the National Institute on Drug Abuse of the National Institutes of Health under Award number R01DA044207. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Acknowledgments
J. Palamar is funded by the National Institutes of Health (NIH) (R01DA044207).
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.dadr.2023.100149.
Appendix. Supplementary materials
References
- Ahmad F.B., Cisewski J.A., Rossen L.M., Sutton P. National Center for Health Statistics; 2022. Provisional Drug Overdose Death Counts. [Google Scholar]
- Allen J.A., Davis K.C., Duke J.C., Nonnemaker J.M., Bradfield B.R., Farrelly M.C. New product trial, use of edibles, and unexpected highs among marijuana and hashish users in Colorado. Drug Alcohol Depend. 2017;176:44–47. doi: 10.1016/j.drugalcdep.2017.03.006. [DOI] [PubMed] [Google Scholar]
- Andrews P. Cocaethylene toxicity. J. Addict. Dis. 1997;16(3):75–84. doi: 10.1300/J069v16n03_08. [DOI] [PubMed] [Google Scholar]
- Barbanti P., Cafforio G., Fofi L. In: The Neuroscience of Cocaine. Preedy VR, editor. Academic Press; 2017. Chapter 37—Headache in cocaine users: epidemiology, clinical features, and putative pathophysiological mechanisms; pp. 363–374. [Google Scholar]
- Baylen C.A., Rosenberg H. A review of the acute subjective effects of MDMA/ecstasy. Addiction. 2006;101(7):933–947. doi: 10.1111/j.1360-0443.2006.01423.x. [DOI] [PubMed] [Google Scholar]
- Bosch X., Loma-Osorio P., Guasch E., Nogué S., Ortiz J.T., Sánchez M. Prevalence, clinical characteristics and risk of myocardial infarction in patients with cocaine-related chest pain. Rev. Esp. Cardiol. 2010;63(9):1028–1034. doi: 10.1016/s1885-5857(10)70206-1. [DOI] [PubMed] [Google Scholar]
- Carpenter R.W., Merrill J.E. How much and how fast: alcohol consumption patterns, drinking-episode affect, and next-day consequences in the daily life of underage heavy drinkers. Drug Alcohol Depend. 2021;218 doi: 10.1016/j.drugalcdep.2020.108407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality . Substance Abuse and Mental Health Services Administration; Rockville, MD: 2020. Results from the 2019 National Survey On Drug Use and Health: Detailed Tables.https://www.samhsa.gov/data/report/2019-nsduh-detailed-tables Available at. Accessed December 6, 2022. [Google Scholar]
- Cloutier R.L., Hendrickson R.G., Fu R.R., Blake B. Methamphetamine-related psychiatric visits to an urban academic emergency department: an observational study. J. Emerg. Med. 2013;45(1):136–142. doi: 10.1016/j.jemermed.2012.11.094. [DOI] [PubMed] [Google Scholar]
- Degenhardt L., Darke S., Dillon P. GHB use among Australians: characteristics, use patterns and associated harm. Drug Alcohol Depend. 2002;67(1):89–94. doi: 10.1016/s0376-8716(02)00017-0. [DOI] [PubMed] [Google Scholar]
- DiSalvo P., Cooper G., Tsao J., Romeo M., Laskowski L.K., Chesney G., Su M.K. Fentanyl-contaminated cocaine outbreak with laboratory confirmation in New York City in 2019. Am. J. Emerg. Med. 2020;40:103–105. doi: 10.1016/j.ajem.2020.12.002. [DOI] [PubMed] [Google Scholar]
- Edwards I.R., Aronson J.K. Adverse drug reactions: definitions, diagnosis, and management. Lancet. 2000;356(9237):1255–1259. doi: 10.1016/S0140-6736(00)02799-9. [DOI] [PubMed] [Google Scholar]
- Gable R.S. Toward a comparative overview of dependence potential and acute toxicity of psychoactive substances used nonmedically. Am. J. Drug Alcohol Abuse. 1993;19(3):263–281. doi: 10.3109/00952999309001618. [DOI] [PubMed] [Google Scholar]
- Gable R.S. Comparison of acute lethal toxicity of commonly abused psychoactive substances. Addiction. 2004;99(6):686–696. doi: 10.1111/j.1360-0443.2004.00744.x. [DOI] [PubMed] [Google Scholar]
- Greenspan N.R., Aguinaldo J.P., Husbands W., Murray J., Ho P., Sutdhibhasilp N., Cedano J., Lau C., Gray T., Maharaj R. ``It's not rocket science, what I do": self-directed harm reduction strategies among drug using ethno-racially diverse gay and bisexual men. Int. J. Drug Policy. 2011;22(1):56–62. doi: 10.1016/j.drugpo.2010.09.004. [DOI] [PubMed] [Google Scholar]
- Gummin D.D., Mowry J.B., Beuhler M.C., Spyker D.A., Bronstein A.C., Rivers L.J., Pham N.P.T., Weber J. 2020 Annual report of the American association of poison control centers' national poison data system (NPDS): 38th annual report. Clin. Toxicol. 2021;59(12):1282–1501. doi: 10.1080/15563650.2021.1989785. [DOI] [PubMed] [Google Scholar]
- Hall A.P., Henry J.A. Acute toxic effects of `ecstasy' (MDMA) and related compounds: overview of pathophysiology and clinical management. Br. J. Anaesth. 2006;96(6):678–685. doi: 10.1093/bja/ael078. [DOI] [PubMed] [Google Scholar]
- Hall W. Alcohol and cannabis: comparing their adverse health effects and regulatory regimes. Int. J. Drug Policy. 2017;42:57–62. doi: 10.1016/j.drugpo.2016.10.021. [DOI] [PubMed] [Google Scholar]
- Hedegaard H., Miniño A.M., Spencer M.R., Warner M. Drug overdose deaths in the United States, 1999–2020. NCHS Data Brief. 2021;(426):1–8. [PubMed] [Google Scholar]
- Hughes C.E., Moxham-Hall V., Ritter A., Weatherburn D., MacCoun R. The deterrent effects of Australian street-level drug law enforcement on illicit drug offending at outdoor music festivals. Int. J. Drug Policy. 2017;41:91–100. doi: 10.1016/j.drugpo.2016.12.018. [DOI] [PubMed] [Google Scholar]
- Jacinto C., Duterte M., Sales P., Murphy S. Maximising the highs and minimising the lows: harm reduction guidance within ecstasy distribution networks. Int. J. Drug Policy. 2008;19(5):393–400. doi: 10.1016/j.drugpo.2007.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kariisa M., Scholl L., Wilson N., Seth P., Hoots B. Drug overdose deaths involving cocaine and psychostimulants with abuse potential—United States, 2003–2017. MMWR Morb. Mortal. Wkly. Rep. 2019;68(17):388–395. doi: 10.15585/mmwr.mm6817a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuerbis A. Substance use among older adults: an update on prevalence, etiology, assessment, and intervention. Gerontology. 2020;66(3):249–258. doi: 10.1159/000504363. [DOI] [PubMed] [Google Scholar]
- Miró Ò., Dargan P.I., Wood D.M., Dines A.M., Yates C., Heyerdahl F., Hovda K.E., Giraudon I., Galicia M. Epidemiology, clinical features and management of patients presenting to European emergency departments with acute cocaine toxicity: comparison between powder cocaine and crack cocaine cases. Clin. Toxicol. 2019;57(8):718–726. doi: 10.1080/15563650.2018.1549735. [DOI] [PubMed] [Google Scholar]
- Morgan C.J., Muetzelfeldt L., Muetzelfeldt M., Nutt D.J., Curran H.V. Harms associated with psychoactive substances: findings of the UK national drug survey. J. Psychopharmacol. 2010;24(2):147–153. doi: 10.1177/0269881109106915. [DOI] [PubMed] [Google Scholar]
- Nutt D.J., King L.A., Phillips L.D. Drug harms in the UK: a multicriteria decision analysis. Lancet. 2010;376(9752):1558–1565. doi: 10.1016/S0140-6736(10)61462-6. [DOI] [PubMed] [Google Scholar]
- Oliver C.F., Palamar J., Salomone A., Simmons S.J., Philogene-Khalid H., Stokes-McCloskey N., Rawls S. Synthetic cathinone adulteration of illegal drugs. Psychopharmacology. 2018;236(3):869–879. doi: 10.1007/s00213-018-5066-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palamar J.J., Acosta P., Cleland C.M. Planned and unplanned drug use during a night out at an electronic dance music party. Subst. Use Misuse. 2019;54(6):885–893. doi: 10.1080/10826084.2018.1529186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palamar J.J., Acosta P., Le A., Cleland C.M., Nelson L.S. Adverse drug-related effects among electronic dance music party attendees. Int. J. Drug Policy. 2019;73:81–87. doi: 10.1016/j.drugpo.2019.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palamar J.J., Acosta P., Sutherland R., Shedlin M.G., Barratt M.J. Adulterants and altruism: a qualitative investigation of “drug checkers” in North America. Int. J. Drug Policy. 2019;74:160–169. doi: 10.1016/j.drugpo.2019.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palamar J.J., Fitzgerald N.D., Grundy D.J., Black J.C., Jewell J.S., Cottler L.B. Characteristics of poisonings involving ketamine in the United States, 2019–2021. J. Psychopharmacol. 2022 doi: 10.1177/02698811221140006. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palamar J.J., Keyes K.M. Trends in drug use among electronic dance music party attendees in New York City, 2016–2019. Drug Alcohol Depend. 2020;209 doi: 10.1016/j.drugalcdep.2020.107889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palamar J.J., Cottler L.B., Goldberger B.A., Severtson S.G., Grundy D.J., Iwanicki J.L., Ciccarone D. Trends in characteristics of fentanyl-related poisonings in the United States, 2015–2021. Am J Drug Alcohol Abuse. 2022;48(4):471–480. doi: 10.1080/00952990.2022.2081923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palamar J.J., Fenstermaker M., Kamboukos D., Ompad D.C., Cleland C.M., Weitzman M. Adverse psychosocial outcomes associated with drug use among US high school seniors: a comparison of alcohol and marijuana. Am. J. Drug Alcohol Abuse. 2014;40(6):438–446. doi: 10.3109/00952990.2014.943371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palamar J.J., Le A., Han B.H. Quarterly trends in past-month cannabis use in the United States, 2015–2019. Drug Alcohol Depend. 2021;219 doi: 10.1016/j.drugalcdep.2020.108494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palamar J.J., Rutherford C., Keyes K.M. Trends in ketamine use, exposures, and seizures in the United States. Am. J. Public Health. 2021;111(11):2046–2049. doi: 10.2105/AJPH.2021.306486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palamar J.J., Salomone A. Shifts in unintentional exposure to drugs among people who use ecstasy in the electronic dance music scene, 2016–2019. Am. J. Addict. 2021;30(1):49–54. doi: 10.1111/ajad.13086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palamar J.J., Salomone A., Keyes K.M. Underreporting of drug use among electronic dance music party attendees. Clin. Toxicol. 2021;59(3):185–192. doi: 10.1080/15563650.2020.1785488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palamar J.J., Sönmez İ. A qualitative investigation exploring why dance festivals are risky environments for drug use and potential adverse outcomes. Harm Reduct. J. 2022;19(1):12. doi: 10.1186/s12954-022-00598-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panagopoulos I., Ricciardelli L.A. Harm reduction and decision making among recreational ecstasy users. Int. J. Drug Policy. 2005;16(1):54–64. [Google Scholar]
- Park C.L. Positive and negative consequences of alcohol consumption in college students. Addict. Behav. 2004;29(2):311–321. doi: 10.1016/j.addbeh.2003.08.006. [DOI] [PubMed] [Google Scholar]
- Park C.L., Grant C. Determinants of positive and negative consequences of alcohol consumption in college students: alcohol use, gender, and psychological characteristics. Addict. Behav. 2005;30(4):755–765. doi: 10.1016/j.addbeh.2004.08.021. [DOI] [PubMed] [Google Scholar]
- Parrott A.C. MDMA and temperature: a review of the thermal effects of `ecstasy' in humans. Drug Alcohol Depend. 2012;121(1–2):1–9. doi: 10.1016/j.drugalcdep.2011.08.012. [DOI] [PubMed] [Google Scholar]
- Parrott A.C. Human psychobiology of MDMA or `ecstasy': an overview of 25 years of empirical research. Hum. Psychopharmacol. 2013;28(4):289–307. doi: 10.1002/hup.2318. [DOI] [PubMed] [Google Scholar]
- Reynolds S. Routledge Press; New York, NY: 1999. Generation ecstasy: Into the World of Techno and Rave Culture. [Google Scholar]
- Simons J.S., Dvorak R.D., Merrill J.E., Read J.P. Dimensions and severity of marijuana consequences: development and validation of the marijuana consequences questionnaire (MACQ) Addict Behav. 2012;37(5):613–621. doi: 10.1016/j.addbeh.2012.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration . Center for Behavioral Health Statistics and Quality; Rockville, MD: 2022. Preliminary Findings from Drug-Related Emergency Department Visits, 2021, Drug Abuse Warning Network (HHS Publication No. PEP22-07-03-001)https://store.samhsa.gov/sites/default/files/SAMHSA_Digital_Download/PEP22-07-03-001.pdf Available at. Accessed on December 6. 2022. [Google Scholar]
- Substance Abuse Mental Health Services Administration . Substance Abuse and Mental Health Services Administration (US); Rockville (MD): 2015. CBHSQ Methodology Report: National Survey On Drug Use and Health: 2014 and 2015 Redesign Changes.https://www.samhsa.gov/data/sites/default/files/NSDUH-RedesignChanges-2015.pdf Available at. Accessed on December 6, 2022. [PubMed] [Google Scholar]
- Vatsalya V., Stangl B.L., Schmidt V.Y., Ramchandani V.A. Characterization of hangover following intravenous alcohol exposure in social drinkers: methodological and clinical implications. Addict. Biol. 2018;23(1):493–502. doi: 10.1111/adb.12469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J., Patel P.S., Andhavarapu S., Bzihlyanskaya V., Friedman E., Jeyaraju M., Palmer J., Raffman A., Pourmand A., Tran Q.K. Prevalence of myocardial infarction among patients with chest pain and cocaine use: a systematic review and meta-analysis. Am. J. Emerg. Med. 2021;50:428–436. doi: 10.1016/j.ajem.2021.08.024. [DOI] [PubMed] [Google Scholar]
- Zawilska J.B., Andrzejczak D. Next generation of novel psychoactive substances on the horizon—A complex problem to face. Drug Alcohol Depend. 2015;157:1–17. doi: 10.1016/j.drugalcdep.2015.09.030. [DOI] [PubMed] [Google Scholar]
- Zawilska J.B., Kacela M., Adamowicz P. NBOMes—Highly potent and toxic alternatives of LSD. Front. Neurosci. 2020;14:78. doi: 10.3389/fnins.2020.00078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zinberg N.E. Yale University Press; New Haven, CT: 1984. Drug, Set, and Setting: The Basis For Controlled Intoxicant Use. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.