Abstract
Given their recent success in counseling and psychiatry, the dialogue around psychedelics has mainly focused on their applications for mental health. Insights from psychedelic research, however, are not limited to treating mental health, but also have much to offer our current understanding of consciousness. The investigation of psychedelic states has offered new perspectives on how different aspects of conscious experience are mediated by brain activity; as such, much more has been learned about consciousness in terms of its phenomenology and potential mechanisms. One theory that describes how psychedelics influence brain activity is the “entropic brain theory” (EBT), which attempts to understand conscious states—normal and psychedelic—in terms of “brain entropy.” Given its wide explanatory reach, this theory has several implications for current debates in consciousness research, namely the issue of whether consciousness exists in levels vs. dimensions; whether the psychedelic state is itself a “higher” level of consciousness; and if so, whether psychedelics could be used to treat disorders of consciousness. To understand how psychedelics could possibly treat a minimally conscious or vegetative patient, one must first understand EBT and how this theory intersects with these ongoing debates. Thus, this article offers a formal summary of EBT, distilling its core principles and their implications for a theoretical model of consciousness. In response to their proposed use in treating disorders of consciousness, we emphasize the importance of “set” and “setting” in ascertaining the therapeutic value of psychedelics for vegetative and/or minimally conscious patients.
Keywords: disorders of consciousness, states of consciousness, entropic brain theory, psilocybin, theories and models, psychedelic states
Introduction
Psychedelic research has recently become a prominent field of inquiry in psychiatry, psychotherapy, neuroscience, and other disciplines. Formal investigations on classical psychedelics—such as psilocybin and lysergic acid diethylamide (LSD)—have touted a range of applications for these peculiar drugs; most impressively, perhaps, is their relevance in treating a variety of psychiatric disorders (Johnson and Griffiths 2017; Fuentes et al. 2020). For instance, various studies on psilocybin have indicated high therapeutic potential in treating a range of mental health disorders, including anxiety and depression, in both terminal cancer patients and the general population (Griffiths et al. 2016; Carhart-Harris et al. 2016a; De Gregorio et al. 2018; Johnson et al. 2019). Further research has illuminated its utility in treating addiction, with unprecedented results (Johnson et al. 2017). Setting aside their therapeutic value, the study of psychedelics has offered a variety of new perspectives for the general study of consciousness.
Through these drugs, researchers have found reliable ways of safely inducing psychedelic states in both clinical and healthy populations, in hopes of better understanding their various perceptual and cognitive effects. By observing how psychedelics alter neural activity and correlating these effects with changes in conscious experience, researchers can discern how various aspects of consciousness are mediated by brain activity and how changes in specific neural systems affect conscious states (Carhart-Harris et al. 2012, 2016b). For instance, changes in the default mode network (DMN)—a network of brain regions thought to be involved in constraining and maintaining regular conscious experience (Carhart-Harris and Friston 2010)—have been associated with various perceptual shifts induced by psilocybin (Carhart-Harris et al. 2012), LSD (Müller et al. 2018), and other psychedelics (Palhano-Fontes et al. 2015). Most notably, perhaps, is the DMN’s role in maintaining our narrative “sense of self” (Lebedev et al. 2015; Millière 2017; Millière et al. 2018), which describes our felt sense of being a subject at the center of conscious experience. In psychedelic research, the disintegration of the DMN and its decoupling from the medial–temporal brain regions has been associated with experiences of “ego-dissolution,” the perceived experience of losing one’s sense of self (Lebedev et al. 2015; Letheby and Gerrans 2017). Novel insights such as this have contributed several new perspectives on how we might understand and further investigate consciousness. Thus, psychedelics have proven to be useful tools for investigating consciousness in both cognitive and phenomenal terms.
One of the dominant theories in this field is the “entropic brain theory” (EBT), a formal account from Carhart-Harris et al. (2014) which attempts to describe consciousness in terms of “brain entropy.” To put it crudely, EBT claims that the level of one’s consciousness (and the richness of their experience) can effectively be measured by their amount of disordered brain activity. This theory has several implications for consciousness research, both theoretical and practical. For instance, how does EBT weigh in on the debate over how we should measure and compare conscious states? Is it accurate to say that the psychedelic experience is a “higher” state of consciousness? If psychedelics are found to “elevate” consciousness in some sense, could they perhaps serve as viable interventions beyond psychiatry and mental health—possibly in the treatment of disorders of consciousness (DOCs)? And finally, what ethical challenges would one face in administering psychedelics to vegetative or minimally conscious (MS) patients?
To understand why psychedelics have been described as inducing a “higher state of consciousness” (Schartner et al. 2017a) and consequently, why some have argued for their use in treating DOCs (Scott and Carhart-Harris 2019), it is first important to understand the core principles of EBT and how this theory explains conscious states in terms of brain entropy. Our principle aim in this article is to highlight the various points of intersection between EBT and a number of ongoing debates in consciousness research, in an attempt to demonstrate what we might learn about consciousness from investigating psychedelic states. We thereby begin this review by summarizing EBT and discussing the role of entropy in distinguishing conscious states. We then move on to address three ongoing debates in the consciousness literature, namely the issue of whether consciousness exists in levels vs. dimensions; whether the psychedelic state really is a “higher” level of consciousness; and finally, whether psilocybin—a classical psychedelic—can (or should) be used to treat DOC patients. We will place particular emphasis on theoretical gaps, where they arise in these debates. In regard to this final issue, we add to the debate by emphasizing the importance of “set” and “setting” in ascertaining the therapeutic value of psilocybin (and other psychedelics) for treating vegetative and/or MS patients. By the end of this article, readers will become aware of the various ways in which the neuroscience of psychedelics can inform a developing taxonomy of conscious states and the practical implications this may have on interventions for DOC patients. By presenting the various perspectives for each of these debates in turn, we hope to demonstrate the insightful contributions that psychedelic research has made to our theoretical understanding of consciousness.
The EBT
In their initial paper, Carhart-Harris et al. (2014) put forth their EBT by weaving together findings from various brain imaging and neuropharmacological studies, which have all investigated psychedelic drugs and their effects on brain communication (within and between specific brain networks). These processes are believed to be involved in maintaining our day-to-day conscious experience. EBT attempts to understand psychedelic states in terms of their underlying neural changes—more specifically, how they rank in terms of brain entropy. By “entropy,” the authors essentially mean “disorder” or “randomness.” To say that conscious states are a function of brain entropy is to say that the level of entropy (or disordered activity) in the brain can serve as an index for one’s “level” of conscious experience. In exploring this view, EBT addresses entropy as it applies to normal waking consciousness and contrasts this with how entropy differs in the psychedelic state. From this comparison, Carhart-Harris et al. (2014) distinguish two kinds of conscious states: “primary states,” which are conscious states that most closely resemble (but are not limited to) the psychedelic experience, and “secondary states,” which are more akin to experiences in normal waking consciousness. It is worth mentioning here that the terms “primary” and “secondary” are borrowed from the psychoanalytic theory of Freud, who elaborated concepts of primary and secondary processes within the human psyche. Freud is perhaps most well known for his concepts of the “ego” and the “id” as competing processes within an individual: the id is the primary process that represents the “primitive” aspects of a person, driven by instinctual desires and tendencies; the ego is the secondary process that uses reason to negotiate these desires, representing the part of the individual that has been shaped by culture.
Although these concepts refer strictly to psychological phenomena, Carhart-Harris and Friston (2010) propose they have strong neurobiological roots. This is evidenced by insights in cognitive neuroscience, which together suggests that large-scale brain networks (such as the DMN) work to predict and constrain the activity of lower-level limbic systems. On their view, one can interpret spontaneous activity in the brain’s more primitive limbic systems as constituting the primary process (the id) and the DMN’s mediation and suppression of this activity as the secondary process (the ego). In the context of EBT, primary and secondary states are distinguished in terms of their underlying entropy—it is thus helpful to clarify what “entropy” is in empirical terms as a description of brain activity. Moreover, we must explore how measures of entropy in the brain can be used to formally determine one’s level of consciousness.
Entropy and conscious states
Carhart-Harris et al. (2014) argue that the qualitative nature of any conscious state essentially depends on the system’s entropy. Here, the “system” may be the whole brain or even particular subsystems, such as higher-level networks including the DMN or the frontoparietal network (another prominent functional brain network). Entropy is a formal quantitative measure that can be derived in a variety of ways by measuring certain aspects of brain function. On their account, entropy essentially captures the randomness or disorder of a system with respect to neural signal diversity; the corollary of this is that entropy also indicates the level of uncertainty we have about the system’s state at any given moment. That is to say that if we were to randomly sample the state of a system at any point in time, we would be least certain about its state when entropy is highest. Carhart-Harris et al. (2014) liken this to the example of gas expansion in a sealed container: when some barrier has been removed the gas begins to occupy a larger volume, making it more difficult to determine the position of an individual molecule as the total system entropy has now increased (Fig. 1). Thus, measures of entropy serve to index the level of “disordered activity” in the system. This is roughly the analogy that the authors wish to make for the psychedelic experience: psychedelic drugs ultimately raise the level of system entropy, thereby allowing an individual to experience a wider number of possible conscious states while making it more difficult to predict their current state at any given time.
Figure 1.
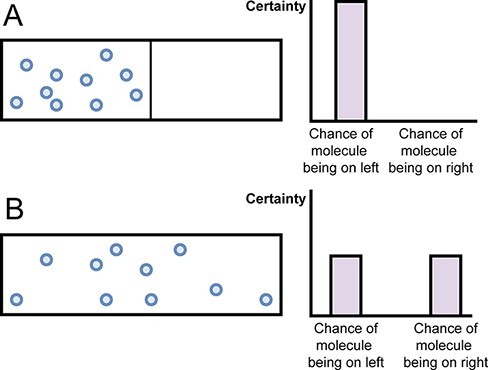
Illustrating an increase in system entropy during gas expansion. The gas molecules in container “A” are restricted to the left side of the vessel due to the internal barrier. Once the barrier is removed (as depicted in container “B”), there is now less certainty over the position of any single gas molecule (adapted from Carhart-Harris et al. 2014)
One might wonder why we should favor entropy in distinguishing conscious states. It is helpful to note here that different measures of brain entropy have been used to describe and compare a variety of conscious states, not limited to normal or psychedelic states. Entropy measures have been used to better understand mood disorders, anxiety disorders, and schizophrenia, as well as the so-called altered states such as hypnosis; researchers have also investigated how levels of entropy change according to the process of aging (Lau et al. 2021). Differences in entropy also appear to be associated with differences in cognitive function, as resting-state functional magnetic resonance imaging (fMRI) research has shown that brain entropy is positively correlated with intelligence in healthy adults, particularly in areas such as the prefrontal cortex, the inferior temporal lobes, and the cerebellum (Saxe et al. 2018). Another study by Shi et al. (2020) found positive correlations between brain entropy and divergent thinking in healthy individuals, in areas including the left dorsal anterior cingulate cortex, the pre-supplementary motor area, and the left dorsolateral prefrontal cortex. If we interpret entropy as a measure of how many distinct states a system can take (Saxe et al. 2018), these findings make intuitive sense—people who are more “intelligent” or “creative” are likely able to inhabit a wider variety of system (or brain) states.
With respect to EBT, the decision to use brain entropy to describe changes in consciousness comes from the authors’ own neuroimaging work on psychedelic states, which suggests that this form of consciousness is mainly characterized by an increase in system disorder. To make sense of this claim, one must understand how entropy is formally determined from neuroimaging data and how different brain regions can vary in their degrees of entropy.
Functional networks and quantifying entropy
Part of what makes our consciousness so unique compared to other animals is that our experience is often mediated by various complex cognitive functions, such as memory, planning, and attention. To meet the demands of daily life, however, the human brain must effectively coordinate these functions with one another, prioritizing the efficient integration of information across multiple brain regions simultaneously, in order to keep up with the vast input of information it processes at any moment. In studying these processes, methods in cognitive neuroscience have identified a variety of functional brain networks that are thought to handle the processing of different kinds of information for various tasks and behaviors (Bressler and Menon 2010). These functional (also called “large-scale”) networks distribute information across multiple regions in a coordinated fashion, which, in turn, allows for the coordination and execution of complex cognitive functions in normal waking consciousness (van den Heuvel and Sporns 2013). Some examples of these networks include the aforementioned “DMN,” composed of the medial prefrontal cortex, the posterior cingulate cortex, and the angular gyrus; another is the salience network, made of the anterior insula and the dorsal anterior cingulate cortex. The DMN appears to be active during episodes of mind-wandering and daydreaming, and it is often understood to be the basis of self-referential thought processes—as such, DMN activity is attenuated when individuals are focused on performing external tasks (Raichle 2015). The salience network is involved in filtering task-relevant information important for successful behavior, as well as recruiting other functional networks for specific cognitive functions (Menon 2015). Both of these networks require information to be efficiently integrated across distinct brain regions so that they can be readily implemented for various cognitive functions at any point in time. These large-scale networks can also be described as “high-level” networks, which can be contrasted with the so-called low-level networks: a low-level network might be one involved in basic sensory processing of auditory or visual information, whereas a high-level network might be involved in determining the “meaning” or significance of that information, in the context of a particular task or goal.
Given that each network has its own set of functions, large-scale networks—such as the DMN or the salience network—tend to exhibit their own stable intra-network (or intrinsic) synchrony over time. Using fMRI, one can determine the average blood-oxygen-level-dependent (BOLD) signal of a particular network and subsequently quantify how much each voxel within that network deviates from the mean signal; little deviation from the mean signal demonstrates low variation, whereas a higher deviation represents higher signal variation. Focusing on nine resting-state networks (whose profiles had previously been established by Smith et al. 2009), Carhart-Harris et al. (2014) measured signal variation within each network and determined mean signals in two experimental conditions: for the administration of a placebo and the administration of psilocybin. In both cases, the average signal was measured before and after the administration of either the placebo or the psilocybin. To summarize, the authors observed a much higher signal variance (i.e. greater entropy) in high-level networks in the psilocybin condition compared to the placebo. However, this effect was limited to specific high-level association networks such as the DMN and salience network, and the effect did not extend to other primary sensory or motor networks. Carhart-Harris et al. (2014) interpret these results as empirical support for EBT and its emphasis on entropy as a measure of conscious states.
As further evidence of increased entropy in the psilocybin state, probability distributions were generated for high-level networks (e.g. for the DMN), illustrating the chance that a signal might vary from its average internal synchrony over time in a given condition (Carhart-Harris et al. 2014). These distributions were nearly identical before and after a placebo had been administered, indicating low variance—this suggests that it is relatively easy to predict the state of a given network after a placebo, based on its state prior to administration. However, following psilocybin administration, the post-infusion signal differed significantly from the synchronous activity detected at pre-infusion, thus reflecting a higher variance. Here, higher variance indicates greater difficulty in being able to predict the network’s state—in other words, higher variance reflects greater system entropy.
Another method of quantifying entropy is to determine the number of connectivity motifs (patterns of functional activation) within a system by using connectivity graphs. In this method, a threshold is set so that only connections that exceed a certain level of signal strength are detected (Carhart-Harris et al. 2014). When performed for both conditions, the results indicated a greater repertoire of connectivity motifs specific to psilocybin administration—some were even exclusive to this condition. Because the sequence of activation for connectivity motifs is highly patterned in specific states, the level of predictability can be used to determine the entropy for a particular sequence; in other words, one can quantify how difficult it might be to predict a particular sequence of motifs in any given state. The authors declared that the sequence of connectivity motifs in the psilocybin state was significantly more random than they were at the baseline, indicating a much higher level of entropy (Carhart-Harris et al. 2014). This bolsters EBT’s fundamental claim, which suggests that the state of the brain becomes more random in the psychedelic state, thus making it harder to predict aspects of one’s conscious experience. Intuitively this makes sense: the more random one’s brain activity, the more variable their conscious experience will be. Indeed, psychedelic states are often characterized by their wide variability among individuals (Turton et al. 2015).
Carhart-Harris et al. (2014) contend that distinct differences in system entropy are one of the key factors that distinguish human brains from the brains of other species in the animal kingdom: because our brains exhibit more entropy, we are essentially able to experience a much wider variety of conscious states that are (presumably) richer and more complex than the so-called lower animals. It is emphasized here that the number of potential mental states one has available to them dictates the kind of consciousness we can expect from that system. Another way of articulating this is to say that the kind of consciousness one can experience largely depends on the number of available brain states (or system states) for that individual; the more possible states, the more possible experiences one can have (Gallimore 2015). This is evident in the psychedelic experience, where increases in entropy are accompanied by a wider variety of system states in prominent cognitive networks, thus allowing for conscious states that are usually not experienced in normal waking consciousness.
Primary states, secondary states, and criticality
In making sense of EBT, we must elaborate on its notion of “self-organized criticality.” This refers to how any complex system begins to take on new properties when it is pulled away from its state of equilibrium and approaches a “critical point” that is now in some transition between two possible system states (Carhart-Harris et al. 2014). Here, we can draw an analogy to phase transitions between different states of matter: in the same way that water begins to exhibit new properties when it transitions from being a solid to a liquid, systems in the brain begin to exhibit different properties when they transition from one state to another (e.g. from a normal conscious state to a psychedelic state). As such, a system is said to be exhibiting “criticality” when it is functioning at an intermediate state or within a transition zone between two distinct states (e.g. order vs. chaos) (Hesse and Gross 2014). Carhart-Harris et al. (2014) argue that our normal waking consciousness is situated at a slightly subcritical state, where we have an optimal balance of order and disorder that allows us to respond flexibly to the demands of our environment. With their entropy-increasing effects, however, psychedelics can push one out of this subcritical state and elevate them toward a critical zone. When the system is moved away from its ordered state in this way, it begins to take on whole new characteristics and behaviors. When looking at differences in neural dynamics, entropy levels, and phenomenology, Carhart-Harris et al. (2014) demonstrate that the adult brain displays more evidence of criticality in the psychedelic state in comparison to normal consciousness.
Taking an evolutionary lens, the authors suggest that shifts in criticality are likely another aspect that separated modern human brains from that of our closest ancestors. They contend that over time human brains evolved an enhanced ability to suppress system entropy, forming an adaptive preference for generally stable conscious states, thereby moving away from the fluctuating dynamics of more critical states (Carhart-Harris et al. 2014). As we evolved, and as our brains developed in their structure and specialized functions, we became more efficient at minimizing our own internal randomness or disorder, which had corollary effects on the nature of our conscious experience. This self-organized criticality situates the system at a slightly subcritical state, allowing it to be more flexible in its response to incoming information, as it is more poised to pivot to different states at any given moment (Hesse and Gross 2014). EBT leverages this notion in its distinction between primary and secondary states and how they compare in terms of criticality (Fig. 2).
Figure 2.
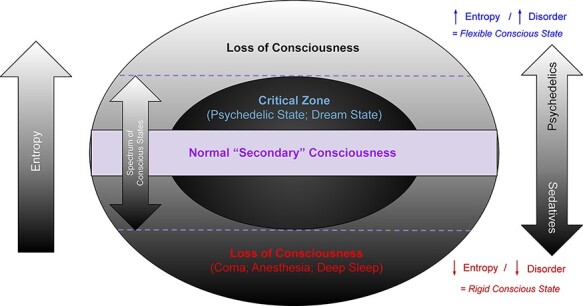
A model for conscious states organized by levels of entropy (adapted from Carhart-Harris 2018)
Primary states are described as “regressive style[s] of cognition” (recall Freud’s primary process and the id) that are phenomenally quite different from typical conscious states in adult humans (Carhart-Harris et al. 2014, 6). This form of consciousness is characterized by a sort of “primitive thinking” that is quite distinguishable from regular consciousness. Other examples of “primary consciousness” (apart from the psychedelic state) would be examples of rapid eye movement (REM) sleep and early psychosis. By their understanding, primary states are a sort of “pre-ego style of consciousness” where the underlying neural dynamics are generally unconstrained, resulting in totally different forms of cognition (Carhart-Harris et al. 2014, 6). In a primary state there is significantly less metacognition (reflection on one’s own thoughts), and less organization of conscious content in one’s experience. Here, the “ego” (or “self”) is thought to play an important role in the structure and maintenance of normal waking consciousness. This is another idea proposed by Carhart-Harris et al. (2014) when comparing human and animal consciousness: in humans, the presence of a mature ego allows for metacognition and thus higher-level abilities to reflect on and modulate representations of one’s environment; in contrast, other animals experience the world in primary states characterized by a “pre-ego style of consciousness,” which lacks the same active modulation—for that reason, these states are deemed “regressive.”
Secondary states, on the other hand, describe our normal waking consciousness. We live most of our lives in “secondary consciousness”—i.e. under regular conscious conditions—and this is thought to be maintained by our developed ego. This notion of the ego as an organizer of consciousness is consistent with Freud’s secondary process, as well as Friston’s (2010) “free energy principle,” which attempts to explain how systems maintain their internal order by developing and finessing their representations of the world in order to minimize any surprise or uncertainty—here, minimizing surprise is synonymous with minimizing entropy (Carhart-Harris and Friston 2010). EBT assumes that the human mind has essentially evolved to represent its external environment with as much precision as possible—this form of secondary consciousness is ultimately upheld by the ego, which is responsible for maintaining and finessing these representations (Carhart-Harris et al. 2014).
We can think of the ego here in one of two ways: (i) as our experienced identity that we typically feel to be the subject of our own consciousness (e.g. we feel as if we see things “out there” while we are “in here” behind our eyes) (Dennett 1992) or (ii) as a series of distinct brain regions and networks that are ultimately responsible for filtering and mediating our experience, in some coordinated fashion. It has been shown, for instance, that the experience of ego-dissolution under psilocybin—the feeling that one’s sense of self has effectively “dissolved”—is associated with a breakdown of the DMN, as well as its de-coupling from the medial–temporal lobes (Lebedev et al. 2015). The disintegration of the salience network and the reduction of inter-hemispheric communication also appear to entail some level of ego-dissolution (Lebedev et al. 2015). How the sense of self can be mediated by these structures may be difficult to appreciate at first—our sense of having “a self” is usually so pervasive (and at times quite subtle) that one is prone to viewing their identity as an “obvious given” in consciousness. One might even argue that any form of consciousness must entail some notion of self: “how can there be an experience, without an ‘experiencer’ behind it?” Letheby and Gerrans (2017) point out, however, that the existence of a subjective self or ego becomes most apparent when one loses it—in flow states, meditation, or, more notably, under psychedelics. When the sense of self remains intact, these “ego-networks” (e.g. the DMN and salience network) and their regulated activity play an essential role in maintaining our normal waking consciousness—EBT describes the ego as playing an important role in constraining our experience primarily through entropy suppression (Carhart-Harris et al. 2014). Carhart-Harris et al. (2014) argue that secondary consciousness is upheld by the ego’s suppression of system entropy and its ability to organize and constrain its forms of cognition; in other words, the maintenance of secondary consciousness requires an intact ego to limit the influence of extraneous information on one’s experience.
From this, we see that the key difference between primary and secondary states is that primary states are higher in both entropy and criticality. Elevations in system entropy are what makes primary states much more flexible and pliant than other ego-constrained secondary states. It is helpful to note that these are not merely conceptual distinctions but are also empirically derived observations—the grounds for distinguishing primary and secondary states come from a variety of neuroimaging studies which, taken together, suggest that the maintenance of normal secondary consciousness depends on connections between cortical areas of the DMN and the medial–temporal lobes (Lebedev et al. 2015). Furthermore, it was observed that hippocampal–DMN coupling decreased under psilocybin conditions, resulting in greater DMN desynchrony and disorder, as well as an elevation in BOLD signal fluctuations within the hippocampus (Carhart-Harris et al. 2014). Hippocampal–DMN decoupling is therefore considered a necessary condition for the regression to primary consciousness.
Increases in entropy confer an increase in criticality as the system moves closer to a potential phase transition (i.e. from secondary to primary consciousness). In terms of stability, primary states are considered less stable than secondary states, as systems in primary states are more sensitive to perturbation which could effectively lead to a phase transition. This suggests that primary consciousness may yield a larger repertoire of possible states that are accessible to the system as entropy and criticality increase (Carhart-Harris et al. 2014). Carhart-Harris et al. (2014) indicate that due to maturational settling the adult human brain (under secondary consciousness) tends to minimize system disorder, and by tending toward order, the neural dynamics of its subsystems are “slightly subcritical.” If we were to sample the brain in a primary state induced by psychedelics or during some dream state, we would find that the rules that govern our normal waking consciousness would no longer apply. A brain in secondary consciousness will tend toward the minimization of disordered activity to the best of its ability—however, strong elevations in entropy will ultimately disrupt this process, further inducing a regression to primary consciousness where system behavior becomes less predictable (Carhart-Harris et al. 2014).
EBT in sum
We can now summarize the general themes of EBT. Its key principles are distilled as follows:
Conscious states are influenced by the degree of system entropy.
Higher entropy means there is greater uncertainty over the current state of that system, from the perspective of any external observer or neuroimaging technique.
The two main kinds of states are primary states and secondary states, where primary states are a regressive pre-ego style of cognition exhibiting higher entropy and less constraint in conscious content. Secondary states are more akin to normal waking consciousness.
The ego, aside from being responsible for metacognition, is also responsible for modulating activity and finessing the system’s representations of the world in order to maintain secondary consciousness. It achieves this through entropy suppression.
Primary states exhibit more characteristics of criticality than secondary states, and psychedelic states are paradigmatic examples of primary consciousness.
EBT and the taxonomy of conscious states
Consciousness in levels vs. dimensions
In EBT, entropy is thought to index both the contents of consciousness and one’s level of consciousness. This is best illustrated in Fig. 2. As depicted, normal waking consciousness arises within a critical (or intermediary) zone where the level of entropy is at an optimal balance between order and disorder. Psychedelics increase system entropy, which then pushes the system to a more critical state within the range of conscious experience. The range of conscious states is defined by both an upper and lower bound; at the upper bound the level of entropy exceeds criticality and consciousness may be lost, presumably because the experience itself can no longer be maintained or remembered (Carhart-Harris 2018); sedatives, however, tend to minimize system entropy, moving one to a more subcritical zone and toward an eventual loss of consciousness at the lower bound.
According to this model, an implication of EBT is the idea that conscious states exist in “levels.” There are two ways of thinking about conscious states: as “local states,” which are distinguished from each other by the objects and experiences that characterize them (e.g. experiencing a tree vs. a dog); and “global states,” which are distinguished by cognitive, behavioral, and physiological differences (e.g. comparing coma patients with healthy adults). Although EBT argues that entropy can index phenomenal richness, the model proposed here more accurately speaks to changes in global states as one shifts in criticality—as such, the terms “global states” and “conscious states” will be used interchangeably from here on.
To say that global states exist in levels is to imply that they can be ordered or ranked along a single dimension in terms of degrees. To illustrate this, consider how the following conscious states would likely be ranked according to this model: normal waking consciousness (or secondary consciousness) lying somewhere within the critical zone; the psychedelic state (or primary consciousness) closer to the upper bound; and vegetative state (VS) or MS state below the lower bound, where there is perceived to be no “level of consciousness.” At first, there does not appear to be anything wrong with this taxonomy. In fact, this approach is fairly practical when it comes to assessing DOC patients relative to one another—vegetative patients are quite often described as having a “lower level of consciousness” than MS patients, due to their lower sense of awareness. Furthermore, some researchers have explicitly described the psychedelic experience as being an “elevated level of consciousness” (with respect to specific neural measures) (Schartner et al. 2017a, 1).
However, according to Bayne et al. (2016), there are two problems in emphasizing a “levels-based” approach to global states: first, if being conscious is simply a matter of having an experience, then it makes no sense to order consciousness along a continuum of being “more or less conscious”—you are either conscious or you are not; secondly, there is good reason to be skeptical that all global states can be ordered relative to one another in any determinate way. Taking both issues into consideration, Bayne et al. (2016) argue that conscious states may best be compared in terms of how they differ with respect to certain “dimensions,” as opposed to different levels. Adopting this approach is more likely to capture the nuance within and between conscious states, in terms of their functional and content-related dimensions.
How one decides to taxonomize conscious states may depend more on the specific aspects of consciousness that one wishes to describe, rather than adhering to any absolute construct. Invoking some form of “construct pluralism” may be appropriate here, as it is perhaps a question of one’s goals and/or values that should determine whether they operationalize consciousness in terms of levels vs. dimensions. For a physician tasked with making clinical distinctions between DOC patients, it seems perfectly reasonable—perhaps even necessary—to think in terms of levels when evaluating degrees of awareness. However, if one is hoping to draw meaningful comparisons in the phenomenology among individuals, it is difficult to see how a unidimensional construct would suffice. In essence, whether one chooses a taxonomy of levels or dimensions largely depends on what one hopes todo with those descriptions. In hopes of understanding the psychedelic state and elucidating its characteristics, a multidimensional view may be more appropriate for capturing its repertoire of perceptual and cognitive effects.
The psychedelic case for a multidimensional view
Bayne and Carter (2018) have made a strong case for a multidimensional account of the psychedelic state. They argue that there are inherent issues with describing the psychedelic state as a “higher” form of consciousness, indicating that it is neither “higher” nor “lower,” but simply a different mode of consciousness. In their view, a full analysis of the psychedelic state—one that accounts for its various phenomenal and cognitive features—ultimately points toward a more “dimensional” view of consciousness, as opposed to a levels-based hierarchy. To make their case they look at three categories of experience, each of which may contain their own functional and content-related dimensions with their own separable scales. These categories include “(i) sensory and perceptual experience; (ii) cognitive capacities; and (iii) experiences relating to time, self, and space” (Bayne and Carter 2018, 2).
In addressing the first category, the authors describe how the psychedelic state is often associated with reports of intense visuals and an improved richness in color perception. However, there has yet to be definitive evidence supporting the claim that color perception is improved in any significant way. On the contrary, they note that Hartman and Hollister (1963) found that participants given either psilocybin or LSD fared much worse at hue discrimination, even though they generally reported having enhanced abilities for color perception (Bayne and Carter 2018). Furthermore, Carter et al. (2004) failed to find any evidence of a significant increase in brightness or contrast sensitivity in psilocybin conditions. According to Bayne and Carter (2018), it is still an open question as to how the experience of richer color perception or heightened brightness sensitivity can be reconciled with the lack of any objective improvements in these faculties.
Despite this discrepancy between anecdotal reports and measurable perceptual improvements, there does seem to be growing evidence suggesting that psychedelics increase the general “bandwidth” of conscious experience, allowing for more phenomenal content to be directly experienced in this state (Bayne and Carter 2018). Here, we can recall EBT’s principles of entropy and criticality to understand why this might be: as entropy and criticality increase, the subject transitions into a primary state that has more possible mental states available to them. This may help explain why psychedelic states appear to be characterized by an increase in sensory bandwidth.
One’s sensitivity to color and brightness and the general volume of sensory experience are examples of “content-related dimensions.” Content-related dimensions refer to the specific contents of consciousness that are experienced by the subject and how these contents are gated or integrated into one’s phenomenal view (in terms of their higher- or lower-level features). They can also refer to the certain kinds of sensory information (visual objects, auditory objects, etc.) that make up a conscious state (Bayne et al. 2016). In the case of visual perception outlined earlier, it becomes clear why ranking conscious states along a single dimension would be problematic: here, we have two distinct content-related dimensions—color discrimination and sensory gating—which appear to be differentially affected in the psychedelic state.
What Bayne and Carter (2018) hope to illustrate is that it would be a mistake to describe the psychedelic state as being a “higher level of consciousness,” given that many dimensions within this state are affected independently from one another to varying degrees—some may be “enhanced” (in some sense), while others could very well be impaired. When looking at particular “functional dimensions” such as different forms of cognition, we find similar dissociations. For instance, Bayne and Carter (2018) highlight that aspects of declarative memory and learned associations were found to be impaired in the psychedelic state, while tasks involving mental manipulation of items (e.g. counting backward) were unaffected (Silverstein 1958). Several studies have found impairments in different forms of attention, including sustained attention (Quednow et al. 2012) and divided attention (Carter et al. 2005). Bayne and Carter (2018) also note a study by Deshon et al. (1952), which observed impaired concentration as one of the more frequent effects of LSD use. Given the wide-ranging deficits incurred on memory, attention, and decision-making, it is difficult to justify the psychedelic state as being an overall “higher level of consciousness” (Bayne and Carter 2018).
Issues with the multidimensional view
Bayne and Carter (2018) insist that a full appreciation of the psychedelic experience, in all its variety and nuance, ultimately persuades us to adopt a multidimensional view of consciousness. While commending (and largely agreeing) with their proposal, Fortier-Davy and Millière (2020) raise a number of conceptual ambiguities in Bayne and Carter’s (2018) argument. To help address these concerns, they offer a few of their own suggestions and amendments.
First, they argue that Bayne and Carter’s (2018) usage of “conscious states” is unclear, as this term may refer to a variety of things that can all be described as a “conscious state.” In this context, a conscious state could refer to:
specific experiences of particular contents of consciousness (e.g. hearing a dog bark or tasting a cherry);
the overall experience of a person at any given moment in time (i.e. the totality of everything it is like to be that person in a specific instance); or
a person’s “mode” or “way” of being conscious, determined by their various cognitive abilities that limit the kinds of content they can be conscious of, and the ability for those contents to have effects on their cognition and behavior (Fortier-Davy and Millière 2020).
To avoid confusion, Fortier-Davy and Millière (2020) introduce the terms “local phenomenal states,” “global phenomenal states,” and “global modes of consciousness” to address the issues raised above, respectively. Implementing this terminology allows one to distinguish between local and global properties of experience while allowing room to describe the dispositional aspects of an individual’s mode of consciousness.
Another concern they raise is how Bayne and Carter (2018) tend to describe the psychedelic state as if it were a “single kind” of state. To speak as if there were a paradigmatic psychedelic state would be to miss the point on how diverse these experiences really are, as they tend to vary drastically in terms of their phenomenal character. This experiential variance depends on a variety of factors including (but not limited to) dosage, the environmental context, personal predispositions, and the pharmacological dynamics of the specific drug taken—it therefore makes no sense to suggest that there is “just one” psychedelic state (Fortier-Davy and Millière 2020). Although the objection here is valid, it does little to undermine Bayne and Carter’s (2018) main thesis, as their taxonomy of conscious states is more or less equipped to account for these differences on a case-by-case basis—this is arguably the principal aim of a multidimensional account of consciousness.
What puts most pressure on the multidimensional view is Fortier-Davy and Millière’s (2020) objection that it still might make sense to describe certain states as “higher” than others even within a multidimensional view. If one were to compare a subject in a psychedelic state to an adult in normal waking consciousness, and found that the former scored consistently higher on all related dimensions, it would be fair to say that this person was in a “higher level of consciousness” (on Bayne and Carter’s 2018 account); however, if they differed in one or two categories, this statement would be incorrect (Fig. 3). Fortier-Davy and Millière (2020) argue that these comparisons between global phenomenal states (to use the authors’ term) are only justified if the dimensions that are considered can easily be aggregated to index a single disposition or property, which will also depend on the extent to which they are inter-related and can meaningfully be compared. To illustrate this point, they provide an example of comparing the well-being of two people, where dimensions of “happiness,” “mental health,” and “sense of meaning” are considered (this example is adapted from Alexandrova 2017): if Person A scores higher in the first two and only slightly lower on the third than Person B, Fortier-Davy and Millière (2020) argue that it would be appropriate to describe the former as having better (or higher) well-being. In the context of conscious states, however, this ultimately runs into the issue of vindicating the levels-based construct that Bayne and Carter (2018) fundamentally oppose. How can one accurately describe a conscious state as being “higher” than another if there are faculties within that state that are empirically “lesser” than the so-called lower conscious state?
Figure 3.
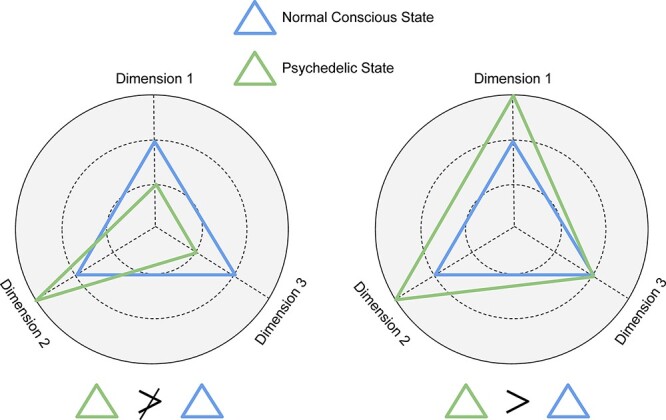
Comparing global states of consciousness with respect to related dimensions (adapted from Fortier-Davy and Millière 2020)
Here, we can consult Bayne et al. (2016) who—in their proposal for the multidimensional account—argue that individual dimensions may be graded in terms of levels themselves and conscious states may even be compared to one another with respect to those dimensions, but this in itself is no exoneration of a levels-based construct as a whole. Again, there is no reason to believe that all global states can easily be ordered on the abstract notion of “levels” along a single dimension (Bayne et al. 2016). Following this logic, Bayne and Carter (2018) might argue that being able to compare conscious states between subjects and contrasting these states with respect to their related dimensions is a testament “in favor” of the multidimensional view. If the goal of a taxonomy of conscious states is to track the myriad of differences between psychedelic experiences, and to allow us to make meaningful comparisons between them and other forms of consciousness, a multidimensional account may offer the necessary precision required for such a project.
DOCs and psychedelic treatment
We have so far examined two theoretical implications of EBT: namely, its relevance in constructing a taxonomy of conscious states and its consequences for imposing a levels-based view of psychedelic experiences. However, we might find other (perhaps more practical) implications of EBT in applying its principles to the treatment of DOCs. Two common examples of DOC patients are individuals who are diagnosed as MC or are in a VS: VS patients are identified by being generally awake but unresponsive, as they have no discernible awareness of their environment; MC patients, on the other hand, are awake, display some degree of awareness of themselves and their environment, and are minimally able to respond to certain command-following gestures to indicate some preserved cognitive function. Under the “levels” view of consciousness, both MC and VS patients are assumed to have a “lower level” of consciousness compared to healthy adults. Now, we can recall that EBT posits conscious states as a function of entropy (or complexity) within the brain and that psychedelics are known to increase the complexity of the system—could psychedelics then offer a way of effectively “raising” a DOC patient’s level of consciousness (Carhart-Harris 2018)?
Entropy as complexity: measuring consciousness with the perturbational complexity index and Lempel–Ziv complexity
Scott and Carhart-Harris (2019) propose that psychedelics be tested as a viable treatment for DOC populations. Their argument rests on their hypothesis that brain complexity is an index of one’s conscious level and that this can be empirically measured. The perturbational complexity index (PCI) is one such measure, and it is gathered by inducing a cortical perturbation via transcranial magnetic stimulation (TMS) and recording one’s electroencephalographic (EEG) response to this perturbation (Casali et al. 2013). These data can then be put through a Lempel–Ziv algorithm which determines to what extent this information can be compressed—redundant or “non-complex” information confers high compressibility, while data with many unique patterns (i.e. complex data) do not compress as readily. Once processed, a Lempel–Ziv complexity (LZC) value is outputted. Thus, the PCI score is essentially an LZC value that captures the complexity measured in response to a perturbation (TMS). However, LZC scores can also be computed from resting-state spontaneous EEG data without the use of a perturbation. DOC patients will typically exhibit lower PCI and LZC values compared to healthy adults; the PCI has been shown to effectively categorize DOC patients, making distinctions between VS and MC patients on the basis of measured complexity differences (Fig. 4) (Casali et al. 2013); and LZC scores have also been successful in discriminating VS and MC patients (Wu et al. 2011; Sitt et al. 2014), and have also been used to differentiate various conscious and unconscious states, including anesthesia and epileptic seizure (Bai et al. 2015), as well as changes in sleep stages (Schartner et al. 2017b).
Figure 4.
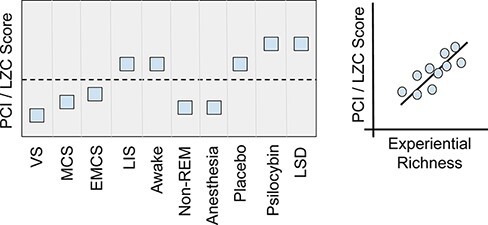
Calculating LZC/PCI values to determine levels of conscious awareness in healthy and DOC subjects. PCI=perturbational complexity index; LZC=Lempel-Ziv complexity; VS=vegetative state; MCS=minimally conscious state; EMCS=emergence from MCS; LIS=locked-in syndrome; non-REM=non-rapid eye movement sleep (adapted from Scott and Carhart-Harris 2019)
Neural complexity in this context is said to encompass two fundamental features of consciousness: “differentiation” and “integration.” Here, “differentiation” refers to the many experiential components that underlie a given experience, and “integration” is the property that unifies these components into their perception as whole objects and experiences. Given that LZC is higher in wakeful/aware states and lower for losses of consciousness, Scott and Carhart-Harris (2019) take it as being fundamentally similar to other explicit entropy measures, as it exhibits a similar trend when tracking one’s level of consciousness. They interpret LZC as capturing the amount of conscious content in terms of spontaneous variability in brain activity (i.e. the differentiation component of consciousness), making it a suitable index for conscious level.
Psilocybin has been found to increase brain complexity in healthy human subjects (Schartner et al. 2017a), and since indices such as LZC are sensitive to these changes, it is hypothesized that psilocybin may be a viable treatment for increasing conscious awareness in DOC patients. Support for this proposal comes in part from Carhart-Harris (2018), who has previously argued that increases in LZC and entropy values ultimately correspond to increases in sensory experience, or rather, the perceived “richness” of consciousness. One should note that Scott and Carhart-Harris (2019) are not suggesting that trials of this sort begin with DOC patients, but rather that this goal be approached incrementally with preliminary studies that can establish the safety and tolerability of psilocybin, as well as confirm its effects on complexity and awareness. An example study they propose would be to test this protocol on healthy sedated individuals by collecting either PCI or LZC before and after psilocybin administration, while also recording behavioral measures that can verify changes in consciousness (e.g. command following). Another preliminary study could determine whether psilocybin increases complexity during non-REM sleep. Other studies would aim to determine the optimal dosage parameters of psilocybin that offer the purported benefits to awareness while prioritizing tolerability. The results from these studies would add corroborative support for their hypothesis and thereby motivate its investigation in DOC patients.
Ethical concerns
The hypothesis put forth by Scott and Carhart-Harris (2019) seems to neglect the main issue we have just observed when relying on a levels-based view of conscious states—namely, the concern that “levels” may be an inadequate framework for measuring and comparing conscious states. Indeed, they explicitly address this objection, stating that it remains unclear how any sort of multidimensional framework can be reconciled with the unidimensional measures that are most prevalent in studies on conscious states (such as LZC and PCI values). However, it is worth noting here that the mere prevalence of complexity measures in consciousness research is not itself an argument in their favor as measures of different aspects of consciousness. It remains unclear how complexity measures can be translated into specific conscious dimensions, functional or content-related; this uncertainty may very well fail to capture the important aspects of a DOC patient’s condition, which would likely have consequences for their reported diagnosis, prognosis, and treatment (Walter 2021). For these reasons, we must now consider the ethical concerns of using psychedelics to treat this patient population.
Peterson et al. (2019) provide a framework for assessing the ethical challenges inherent in using psychedelics as a treatment for DOC patients. Responding to Scott and Carhart-Harris (2019), they outline a series of ethical considerations one must address if psilocybin is to be investigated as a therapeutic tool for this population, including whether the administration of psilocybin should be considered a therapeutic or nontherapeutic procedure; whether administering psilocybin in DOC patients poses an increase above the “minimal risk” threshold (a threshold that protects vulnerable populations from the potential harms of research); whether participants would be selected fairly for a psilocybin trial; and whether surrogate consent would be sought on behalf of DOC patients. Two important questions that Peterson et al. (2019) address are whether the proposed intervention has clinical or social value. A trial is deemed to have “clinical” value if its main hypothesis addresses a pressing clinical concern, such as “Is it possible to raise a DOC patient’s level of awareness?” Moreover, a trial is said to have social value if its hypothesis addresses an important social or scientific problem. With regard to these two concerns, Scott and Carhart-Harris’s (2019) proposal merits true clinical value, as there are unfortunately few pharmacological treatments available for this population that may offer the same benefits. It also has social value, in that finding treatments for DOC patients may help relieve the cost burden of long-term care for these individuals by ultimately improving their prognosis (Peterson et al. 2019).
When questioning the scientific validity of this proposal, however, Peterson et al. (2019) mount some skepticism. In this case, a protocol is considered “scientifically valid” if the experiment is well designed, theoretically sound, and therefore appropriate to answer the main research question. Were a protocol not scientifically valid, imposing the burdens of research on participants would be unjustified regardless of whether the study had social or clinical value (Peterson et al. 2019). Scott and Carhart-Harris (2019) argue that an LZC value would ultimately determine a trial’s efficacy—although here, Peterson et al. (2019) indicate that LZC is currently not a clinically validated measure for assessing consciousness in DOC patients. As a result, the overall validity of this intervention would ultimately depend on the correlative strength of LZC values with already valid diagnostic measures (Peterson et al. 2019). To put further pressure on indices of complexity, Peterson et al. (2019) highlight that increases in both LZC (Schartner et al. 2017a) and PCI (Sarasso et al. 2015) values have been observed in cases of low and anesthetic doses of ketamine; contrary to Scott and Carhart-Harris’s (2019) assumptions, an increase in complexity seems to be fully compatible with overall reductions in conscious awareness.
Furthermore, Scott and Carhart-Harris (2019) bolster their case by drawing from the success of psychedelic treatment in psychiatry, which has shown promising results in improving various mental health outcomes. What they neglect, however—and what Peterson et al. (2019) are careful to point out—is that psychiatric populations are vastly different from DOC patients in the nature of their condition. The etiological factors for DOC patients could include a host of other illnesses or physical injuries; as a result, they may be prescribed medications that could potentially interfere with the drug’s efficacy. Peterson et al. (2019) caution against extrapolating from the successes of psychedelics in psychiatry, as it is unreasonable to expect that a successful treatment for one kind of clinical population will translate equally well for another. This concern seems appropriate when one considers how interventions for both groups are motivated by entirely different clinical outcomes (e.g. reduced depression vs. elevated awareness).
Finally, in determining whether a clinical trial of this kind poses an unacceptable risk, one must consider how the risk profile for DOC patients might change as they improve in conscious awareness. If a patient were to emerge from an MS state and find that they were under the effects of a psychedelic, this might induce stress and lead to further adverse events (a “bad trip”). Should this happen, there would be no assurance that the patient could reliably communicate their experience, making it unlikely for researchers to know if this were the case (Peterson et al. 2019). Although several arguments from Peterson et al. (2019) have been omitted here, this brief overview is meant to offer a few worthy points of consideration when assessing Scott and Carhart-Harris’s (2019) proposal.
The importance of “set” and “setting”
In discussing DOC treatment, both Scott and Carhart-Harris (2019) and Peterson et al. (2019) give little attention to the importance of context in producing therapeutically beneficial psychedelic experiences. Carhart-Harris et al. (2018) have argued that the efficacy of psychedelic treatments is almost wholly reliant on the context in which they are given. Neglecting the role of context would potentially run the risk of reducing the drug’s clinical success, and perhaps worse, inducing an ultimately harmful experience for the patient.
The context that is relevant here can be divided into psychological and environmental factors, which are more colloquially understood as “set” and “setting.” “Set” refers to the intentions and psychological expectations of the individual undergoing treatment, and “setting” describes the environment in which one is taking a psychedelic (e.g. in a clinical setting or at home). According to Carhart-Harris et al. (2018), clinical outcomes for psychedelic treatment have been noticeably less positive in cases where set and setting were not sufficiently addressed ahead of time. To give a sense of what this preparation might look like, the authors highlight recent trials that have used psychedelics to treat psychological distress, mood disorders, and addiction—all of which included extensive psychological preparation for patients, including many visits with the researchers before and after the actual drug administration. In these trials, patients were given ample opportunity to discuss questions or concerns they had regarding their participation in the study while also allowing them to build rapport with the researchers and therapists (Johnson et al. 2008; Carhart-Harris et al. 2018).
One might at first be skeptical that a single bad trip could lead to long-term negative outcomes. However, several studies that have investigated the extra-pharmacological factors associated with bad trips have reported symptoms of anxiety, depression, paranoia, and/or dissociation, persisting for weeks to months following the adverse event. One study that focused exclusively on the bad trips of 231 psychedelics users found that 25.4% of individuals experienced long-term adverse symptoms and 15.1% of individuals had reported their experience as being the worst of their lives (Ona 2018). A separate study that focused on psilocybin users (n = 1993) found that the presence of a guide had been significantly negatively correlated with the length of one’s difficult experience (Carbonaro et al. 2016). Other factors—such as an individual’s emotional state prior to taking psilocybin, the physical comfort of the setting, and the level of social support available—were also all significantly negatively correlated with the intensity and duration of adverse experiences. The authors of this study observed that 24% of users who were surveyed at least 1 year after their session (n = 1339) reported one or more symptoms lasting over a week as a result of psilocybin ingestion, with 65% of these individuals reporting more than one symptom (Carbonaro et al. 2016). Of the 1339 individuals, 10% reported symptoms lasting ≥12 months, and 7.6% sought clinical treatment for these long-term adverse effects. Another study found that short-term negative experiences on psilocybin was heavily linked to anxiety, fear, and/or paranoia responses from the individual, implicating mental distortions as the main cause for bad trips (Bienemann et al. 2020). When taken together, these findings highlight the importance of accounting for set and setting when trying to minimize the potential for a bad trip.
When preparing patients for psychedelic experiences, Carhart-Harris et al. (2018) remark that failing to prioritize context may have harmful consequences for an individual’s mental health, both during and after the treatment. Controlling for context seems to be crucial in ensuring successfully therapeutic psychedelic experiences, along with mitigating any adverse psychological effects. Preliminary evidence from a web-based survey (conducted by the authors) suggests that identifying one’s intentions for a psychedelic experience ahead of time and having a willingness to “surrender” to the experience are crucial for ensuring a clinically positive outcome (Carhart-Harris et al. 2018). Earlier work has also recognized the importance of these factors, and comprehensive guidelines have been published on the best practices for conducting psychedelic research (Johnson et al. 2008). In the context of using psilocybin for DOC patients, Peterson et al. (2019) are careful to note that there are many reported cases of post-traumatic confusional states in patients who have emerged from an MS state (Sherer et al. 2005, 2014). This is important to consider for an intervention of this kind, as it appears that being lifted from an unconscious state can itself be destabilizing—one can easily imagine how this might be made worse under the influence of a psychedelic drug.
One must now ask: how are set and setting supposed to be controlled in the context of DOC patients? Perhaps this demand seems unwarranted, as these factors are important for “psychiatric” patients in pursuit of entirely different clinical outcomes—after all, the goals of treating mood or affective disorders differ greatly from the goals of treating one’s level of conscious awareness. In substantiating their proposal, however, Scott and Carhart-Harris (2019) themselves appeal to psilocybin being well tolerated in psychiatric trials (argued to be dependent on context), and therefore emphasizing context here does not seem unreasonable. One might also argue that Scott and Carhart-Harris (2019) have given context the precedence it deserves, as they emphasize the need to have familiar caregivers present in a known or supportive environment during treatment sessions. Although their reference to setting here is clear, we argue that they are not giving enough weight to the value of set—i.e. the subject’s “conscious intentions” going into the trial.
This may seem like a non-sequitur, as one might assume that most DOC patients are not capable of forming any conscious intentions by virtue of lacking awareness. Research on covert awareness in this population, however, seems to suggest that a considerable proportion of patients are able to retain some residual awareness (Kondziella et al. 2016) and can indicate as such through intentional mental behavior (Owen et al. 2006). It is therefore conceivable that a DOC patient could already have some degree of awareness and be thrust into a psychedelic state without sufficient preparation, on account of being presumed to be “unconscious.” Still, given their characteristically minimal level of awareness, there is a prima facie concern that most VS or MC patients would be unable to generate their own conscious intentions. Even for patients who seem to exhibit some degree of covert awareness, there is no known way to fully ascertain their psychological state leading up to a trial of this sort—and yet, controlling for this might make the difference between a truly therapeutic or destabilizing experience.
At this point, we might recall how the risk profile for DOC patients could change as they regain conscious awareness (Peterson et al. 2019). The reasoning for this is simple: if one is not aware of having any sort of experience, then it seems unlikely that any psychologically destabilizing event could occur—having a “bad trip” (or any sort of negative experience) requires some baseline level of awareness to “know” that one is having a bad trip; however, as awareness is restored, the experience of being suddenly thrust into a psychedelic state (from a state of unconsciousness) could be highly traumatic and run counter to the therapeutic goals of the treatment. It is important to note here that an adverse event could occur even if the research hypothesis happens to be correct and awareness is restored. Consider how healthy subjects and recreational users may spend weeks preparing for a psychedelic session—if it is possible for a healthy subject to still suffer undue stress even with the necessary preparation, then it seems plausible that a DOC patient forced into this state would fare much worse.
Across the range of success that psychedelics have had as clinical treatments, accounting for patient intentions has been imperative in ensuring therapeutic outcomes. If psilocybin is found to be successful in restoring awareness, it seems likely that patients would undergo some form of psychedelic experience without the requisite amount of preparation ahead of time. Furthermore, researchers will be limited in their ability to determine whether the experience is positive or negative, since it is uncertain as to whether a DOC patient could communicate their experience through language. On the one hand, Scott and Carhart-Harris (2019) reassure that various physiological measures would be collected during the trial as a means of monitoring the patient during the intervention. However, they neglect to mention how they would determine if someone were having a bad trip, and what they would do in that instance. If it were obvious that a patient was in distress, a physician could administer a “trip-killing” drug such as diazepam or another benzodiazepine anxiolytic (Johnson et al. 2008). Even still, in order to be certain that someone was having a bad trip, there would need to be some reliable association between the collected physiological markers and bad trips in general, as we cannot rely on language for patients to communicate their experiences. Should psilocybin prove successful in restoring awareness in this population, the benefits must be weighed against the costs of inducing a potentially harmful experience on an unsuspecting patient.
Conclusion
In reviewing EBT and its core principles, we find several points of intersection with current debates in consciousness research. Viewing consciousness in terms of brain entropy and extracting a unidimensional taxonomy of conscious states has a few practical advantages—it allows us to (very roughly) compare global states among individuals, and offers a helpful framework as we continue to investigate treatments for DOC patients. However, it appears unlikely that any levels-based view of consciousness can account for the myriad of functional and content-related differences between healthy and clinical populations. With regard to psychedelic states, it seems that considering the full complexity of these experiences may persuade us to adopt a multidimensional view of consciousness instead.
Furthermore, the therapeutic potential of psychedelics may not be limited to psychiatry and mental health but might also extend to treating DOC patients. Interventions in this context, however, are not without their concerns; it is incumbent upon researchers to grapple with the ethical challenges that are unique to this population, including questions of clinical value, social value, and scientific validity. Beyond these concerns, one must consider the dynamic risk profile of DOC patients and ensure that robust protocols are in place to detect and manage adverse experiences. As our contribution to this debate, we have emphasized the inherent difficulties in managing set and setting in DOC patients and have highlighted how the neglect of these factors could negatively impact the clinical outcomes of using psilocybin (or other psychedelics) to restore conscious awareness. Although it may seem otherwise, we wish to make it clear that we are not in principle opposed to Scott and Carhart-Harris’s (2019) proposal—our discussion merely seeks to bring out concerns that would need to be addressed before carrying out such a trial on DOC patients. Of course, the authors themselves acknowledge this, as they argue for an incremental approach beginning in healthy populations to further validate psilocybin’s effects on complexity and its corollary benefits to awareness. Along with these goals, we suggest that future research be focused on identifying suitable measures that could be used to detect the purported changes in awareness from psilocybin, as well as improve our ability to identify bad trips in the absence of patient communication. With these goals in mind, we do not believe that the ethical or theoretical concerns presented here are insurmountable.
By reviewing EBT and its implications, we find several ways in which the broader psychedelic literature has contributed to our theoretical understanding of consciousness, by offering fresh perspectives on a number of key debates within this field. The summary of views here illustrates the inherent difficulty in understanding consciousness, especially when taking the insights of psychedelic neuroscience into account. These debates demonstrate the overall importance of refining our concepts and models as we continue to approach consciousness from various angles—one of which, of course, being through the lens of psychedelics.
Contributor Information
Sidath Rankaduwa, Graduate Program in Neuroscience, Schulich School of Medicine & Dentistry, Western University, London, ON, Canada; Western Institute for Neuroscience, Western University, London, ON, Canada; Rotman Institute of Philosophy, Western University, London, ON, Canada.
Adrian M Owen, Western Institute for Neuroscience, Western University, London, ON, Canada; Department of Physiology and Pharmacology, Schulich School of Medicine & Dentistry, Western University, London, ON, Canada; Department of Psychology, Faculty of Social Science, Western University, London, ON, Canada.
Conflict of interest statement
The authors have no conflicts of interest to declare.
References
- Alexandrova A. A Philosophy for the Science of Well-Being. New York, NY: Oxford University Press, 2017. [Google Scholar]
- Bai Y, Liang Z, Li X. A permutation Lempel-Ziv complexity measure for EEG analysis. Biomed Signal Process Control 2015;19:102–14. [Google Scholar]
- Bayne T, and Carter O. Dimensions of consciousness and the psychedelic state. Neurosci Conscious 2018;2018:niy008. 10.1093/nc/niy008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bayne T, Hohwy J, Owen AM. Are there levels of consciousness? Trends Cogn Sci 2016;20:405–13. [DOI] [PubMed] [Google Scholar]
- Bienemann B, Ruschel NS, Campos ML. et al. Self-reported negative outcomes of psilocybin users: a quantitative textual analysis. PLoS One 2020;15:e0229067. 10.1371/journal.pone.0229067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bressler SL, Menon V. Large-scale brain networks in cognition: emerging methods and principles. Trends Cogn Sci 2010;14:277–90. [DOI] [PubMed] [Google Scholar]
- Carbonaro TM, Bradstreet MP, Barrett FS. et al. Survey study of challenging experiences after ingesting psilocybin mushrooms: acute and enduring positive and negative consequences. J Psychopharmacol (Oxford, England) 2016;30:1268–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carhart-Harris RL. The entropic brain—revisited. Neuropharmacology 2018;142:167–78. [DOI] [PubMed] [Google Scholar]
- Carhart-Harris RL, Bolstridge M, Rucker J. et al. Psilocybin with psychological support for treatment-resistant depression: an open-label feasibility study. Lancet Psychiatry 2016a;3:619–27. [DOI] [PubMed] [Google Scholar]
- Carhart-Harris RL, Erritzoe D, Williams T. et al. Neural correlates of the psychedelic state as determined by fMRI studies with psilocybin. Proc Natl Acad Sci USA 2012;109:2138–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carhart-Harris RL, Friston KJ. The default-mode, ego-functions and free-energy: a neurobiological account of Freudian ideas. Brain 2010;133:1265–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carhart-Harris RL, Leech R, Hellyer PJ. et al. The entropic brain: a theory of conscious states informed by neuroimaging research with psychedelic drugs. Front Hum Neurosci 2014;8:20. 10.3389/fnhum.2014.00020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carhart-Harris RL, Muthukumaraswamy S, Roseman L. et al. Neural correlates of the LSD experience revealed by multimodal neuroimaging Proc Natl Acad Sci USA 2016b;113:4853–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carhart-Harris RL, Roseman L, Haijen E. et al. Psychedelics and the essential importance of context. J Psychopharmacol 2018;32:725–31. [DOI] [PubMed] [Google Scholar]
- Carter OL, Burr DC, Pettigrew JD. et al. Using psilocybin to investigate the relationship between attention, working memory, and the serotonin 1A and 2A receptors. J Cogn Neurosci 2005;17:1497–508. [DOI] [PubMed] [Google Scholar]
- Carter OL, Pettigrew JD, Burr DC. et al. Psilocybin impairs high-level but not low-level motion perception. NeuroReport 2004;15:1947–51. [DOI] [PubMed] [Google Scholar]
- Casali AG, Gosseries O, Rosanova M. et al. A theoretically based index of consciousness independent of sensory processing and behavior. Sci Transl Med 2013;5:198ra105. 10.1126/scitranslmed.3006294. [DOI] [PubMed] [Google Scholar]
- De Gregorio D, Enns JP, Nuñez NA. et al. d-Lysergic acid diethylamide, psilocybin, and other classic hallucinogens: mechanism of action and potential therapeutic applications in mood disorders. Prog Brain Res 2018;242:69–96. [DOI] [PubMed] [Google Scholar]
- Dennett DC. The self as a center of narrative gravity. In: Kessel FS, Cole PM, Johnson DL (eds.), Self and Consciousness: Multiple Perspectives. Hillsdale, NJ: Lawrence Erlbaum, 1992, 4–237. [Google Scholar]
- Deshon HJ, Rinkel M, Solomon HC. Mental changes experimentally produced by d-lysergic acid diethylamide tartrate. Psychiatr Q 1952;26:33–53. [DOI] [PubMed] [Google Scholar]
- Fortier-Davy M, Millière R. The multi-dimensional approach to drug-induced states: a commentary on Bayne and Carter’s “dimensions of consciousness and the psychedelic state”. Neurosci Conscious 2020;2020:niaa004. 10.1093/nc/niaa004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friston K. The free-energy principle: a unified brain theory? Nat Rev Neurosci 2010;11:127–38. [DOI] [PubMed] [Google Scholar]
- Fuentes JJ, Fonseca F, Elices M. et al. Therapeutic use of LSD in psychiatry: a systematic review of randomized-controlled clinical trials. Front Psychiatry 2020;10:943. 10.3389/fpsyt.2019.00943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallimore AR. Restructuring consciousness—the psychedelic state in light of integrated information theory. Front Hum Neurosci 2015;9:346. 10.3389/fnhum.2015.00346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffiths RR, Johnson MW, Carducci MA. et al. Psilocybin produces substantial and sustained decreases in depression and anxiety in patients with life-threatening cancer: a randomized double-blind trial. J Psychopharmacol (Oxford, England) 2016;30:1181–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartman AM, Hollister LE. Effect of mescaline, lysergic acid diethylamide and psilocybin on color perception. Psychopharmacologia 1963;4:441–51. [DOI] [PubMed] [Google Scholar]
- Hesse J, Gross T. Self-organized criticality as a fundamental property of neural systems. Front Syst Neurosci 2014;8:166. 10.3389/fnsys.2014.00166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson MW, Garcia-Romeu A, Griffiths RR. Long-term follow-up of psilocybin-facilitated smoking cessation. Am J Drug Alcohol Abuse 2017;43:55–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson MW, Griffiths RR. Potential therapeutic effects of psilocybin. Neurotherapeutics 2017;14:734–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson MW, Hendricks PS, Barrett FS. et al. Classic psychedelics: an integrative review of epidemiology, therapeutics, mystical experience, and brain network function. Pharmacol Ther 2019;197:83–102. [DOI] [PubMed] [Google Scholar]
- Johnson MW, Richards WA, Griffiths RR. Human hallucinogen research: guidelines for safety. J Psychopharmacol (Oxford, England) 2008;22:603–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kondziella D, Friberg CK, Frokjaer VG. et al. Preserved consciousness in vegetative and minimal conscious states: systematic review and meta-analysis. J Neurol Neurosurg Psychiatry 2016;87:485–92. [DOI] [PubMed] [Google Scholar]
- Lau ZJ, Pham T, Annabel Chen SH. et al. Brain entropy, fractal dimensions and predictability: a review of complexity measures for EEG in healthy and neuropsychiatric populations. PsyArXiv 2021. 10.31234/osf.io/f8k3x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lebedev AV, Lövdén M, Rosenthal G. et al. Finding the self by losing the self: neural correlates of ego-dissolution under psilocybin. Hum Brain Mapp 2015;36:3137–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Letheby C, Gerrans P. Self unbound: ego dissolution in psychedelic experience. Neurosci Conscious 2017;2017:nix016. 10.1093/nc/nix016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menon V. Salience Network. In: Toga AW (ed.), Brain Mapping: An Encyclopedic Reference. vol. 2, Academic Press: Elsevier, 2015, 597–611. 10.1016/B978-0-12-397025-1.00052-X. [DOI] [Google Scholar]
- Millière R. Looking for the self: phenomenology, neurophysiology and philosophical significance of drug-induced ego dissolution. Front Hum Neurosci 2017;11:245. 10.3389/fnhum.2017.00245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Millière R, Carhart-Harris RL, Roseman L. et al. Psychedelics, meditation, and self-consciousness. Front Psychol 2018;9:1475. 10.3389/fpsyg.2018.01475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Müller F, Dolder PC, Schmidt A. et al. Altered network hub connectivity after acute LSD administration. NeuroImage 2018;18:694–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ona G. Inside bad trips: exploring extra-pharmacological factors. J Psychedelic Stud 2018;2:53–60. [Google Scholar]
- Owen AM, Coleman MR, Boly M. et al. Detecting awareness in the vegetative state. Science 2006;313:1402. 10.1126/science.1130197. [DOI] [PubMed] [Google Scholar]
- Palhano-Fontes F, Andrade KC, Tofoli LF. et al. The psychedelic state induced by ayahuasca modulates the activity and connectivity of the default mode network. PLoS One 2015;10:e0118143. 10.1371/journal.pone.0118143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson A, Tagliazucchi E, Weijer C. The ethics of psychedelic research in disorders of consciousness. Neurosci Conscious 2019;2019:niz013. 10.1093/nc/niz013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quednow BB, Kometer M, Geyer MA. et al. Psilocybin-induced deficits in automatic and controlled inhibition are attenuated by ketanserin in healthy human volunteers. Neuropsychopharmacology 2012;37:630–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raichle ME. The brain’s default mode network. Annu Rev Neurosci 2015;38:433–47. [DOI] [PubMed] [Google Scholar]
- Sarasso S, Boly M, Napolitani M. et al. Consciousness and complexity during unresponsiveness induced by propofol, xenon, and ketamine. Curr Biol 2015;25:3099–105. [DOI] [PubMed] [Google Scholar]
- Saxe GN, Calderone D, Morales LJ. Brain entropy and human intelligence: a resting-state fMRI study. PLoS One 2018;13:e0191582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schartner MM, Carhart-Harris RL, Barrett AB. et al. Increased spontaneous MEG signal diversity for psychoactive doses of ketamine, LSD and psilocybin. Sci Rep 2017a;7:46421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schartner MM, Pigorini A, Gibbs SA. et al. Global and local complexity of intracranial EEG decreases during NREM sleep. Neurosci Conscious 2017b;2017:niw022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott G, Carhart-Harris RL. Psychedelics as a treatment for disorders of consciousness. Neurosci Conscious 2019;2019: niz003. 10.1093/nc/niz003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherer M, Nakase-Thompson R, Yablon SA. et al. Multidimensional assessment of acute confusion after traumatic brain injury. Arch Phys Med Rehabil 2005;86:896–904. [DOI] [PubMed] [Google Scholar]
- Sherer M, Yablon SA, Nick TG. Psychotic symptoms as manifestations of the posttraumatic confusional state: prevalence, risk factors, and association with outcome. J Head Trauma Rehabil 2014;29:E11–18. [DOI] [PubMed] [Google Scholar]
- Shi L, Beaty RE, Chen Q. et al. Brain entropy is associated with divergent thinking. Cereb Cortex 2020;30:708–17. 10.1093/cercor/bhz120. [DOI] [PubMed] [Google Scholar]
- Silverstein AB. Effects of lysergic acid diethylamide (LSD-25) on intellectual functions. Arch Neurol Psychiatry 1958;80:477. [DOI] [PubMed] [Google Scholar]
- Sitt JD, King J-R, El Karoui I. et al. Large scale screening of neural signatures of consciousness in patients in a vegetative or minimally conscious state. Brain 2014;137:2258–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith SM, Fox PT, Miller KL. et al. Correspondence of the brain’s functional architecture during activation and rest. Proc Natl Acad Sci USA 2009;106:13040–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turton S, Nutt DJ, Carhart-Harris RL. A qualitative report on the subjective experience of intravenous psilocybin administered in an fMRI environment. Curr Drug Abuse Rev 2015;7:117–27. [DOI] [PubMed] [Google Scholar]
- van den Heuvel MP, Sporns O. Network hubs in the human brain. Trends Cogn Sci 2013;17:683–96. [DOI] [PubMed] [Google Scholar]
- Walter J. Consciousness as a multidimensional phenomenon: implications for the assessment of disorders of consciousness. Neurosci Conscious 2021;2021:niab047. 10.1093/nc/niab047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu D-Y, Cai G, Yuan Y. et al. Application of nonlinear dynamics analysis in assessing unconsciousness: a preliminary study. Clin Neurophysiol 2011;122:490–8. [DOI] [PubMed] [Google Scholar]


