Abstract
Attention-deficit/hyperactivity disorder (ADHD) often co-occurs with substance use (SU) and/or substance use disorder (SUD). Individuals with concurrent ADHD and SU/SUD can have complex presentations that may complicate diagnosis and treatment. This can be further complicated by the context in which services are delivered. Also, when working with young people and adults with co-existing ADHD and SU/SUD, there is uncertainty among healthcare practitioners on how best to meet their needs. In February 2022, the United Kingdom ADHD Partnership hosted a meeting attended by multidisciplinary experts to address these issues. Following presentations providing attendees with an overview of the literature, group discussions were held synthesizing research evidence and clinical experience. Topics included: (1) A review of substances and reasons for use/misuse; (2) identification, assessment and treatment of illicit SU/SUD in young people and adults with ADHD presenting in community services; and (3) identification, assessment and treatment of ADHD in adults presenting in SU/SUD community and inpatient services. Dis-cussions highlighted inter-service barriers and fragmentation of care. It was concluded that a multimodal and multi-agency approach is needed. The consensus group generated a table of practice recommendations providing guidance on: identification and assessment; pharmacological and psychological treatment; and multi-agency interventions.
Keywords: Attention-deficit/hyperactivity disorder, Substance use, Pharmacokinetics, Assessment, Treatment, Comorbidity
Core Tip: Attention-deficit/hyperactivity disorder (ADHD) often co-occurs with substance use (SU) and/or substance use disorder (SUD). The co-occurrence of ADHD and SU/SUD is associated with earlier onset and faster transition to more serious SUD, and reduced treatment effectiveness. This manuscript is the product of a consensus meeting of experts from ADHD and/or SUD services, across a range of clinical, academic, educational, occupational, and service-user sectors. A consensus was reached offering practical guidance to support practitioners working with young people and adults with ADHD and SU/SUD with recommendations for identification and assessment, pharmacological treatment, psychological treatment, and multi-agency interventions.
INTRODUCTION
Attention-deficit/hyperactivity disorder (ADHD) is a neurodevelopmental disorder characterized by age-inappropriate levels of inattention and/or hyperactivity and impulsivity that interfere with functioning across multiple life domains (e.g., personal, academic, work, family, social)[1,2]. Previously only considered a childhood disorder, the persistence of ADHD symptoms into adulthood is now recognised[3,4]. Meta-analyses estimate the prevalence of ADHD to fall between 5% and 7% in children and adolescents[5,6], and between 2.5% and 5% in adults[7,8].
Alongside physical comorbidities[9-11] psychiatric comorbidity is common in the ADHD population[12,13], with 75% reporting to have at least one other diagnosis[14]. One of the most common and impairing comorbidities is substance use disorder (SUD)[15-17]. Meta-analyses have shown that childhood ADHD is significantly associated with later substance use (SU) and SUD during adolescence and young adulthood[18,19]. ADHD is also highly prevalent among individuals with SUD[20-22]; a meta-analysis revealed around 23% of treatment-seeking individuals with SUD met DSM criteria for comorbid ADHD[23]. Accurately identifying ADHD in SUD contexts may be difficult due to high drop-out rates between screening and diagnostic assessments and/or possible unreliable historical information. This is further complicated by presenting symptoms that may be common to both ADHD and SUD, such as inattention, impulsivity and executive dysfunction[24,25].
Hence, the presentation of individuals with comorbid ADHD and SUD is complex. This may complicate identification and treatment[12]. Individuals with a dual diagnosis show more chronic patterns of SU, including earlier onset of SU and a more rapid transition to serious SU[26-28]. They are more likely to engage in polysubstance use[4,29] and experience greater difficulty remaining abstinent[30]. They demonstrate severe functional impairments across several life domains. These include increased risk of depression and suicide attempts[21], reduced quality of life[31], greater psychiatric comorbidity[32], accidents and crime[33,34]. When accompanied by comorbid oppositional defiant disorder (ODD) and conduct disorder (CD), there is an increased risk of premature death[35]. Research indicates poor treatment outcomes[36], with severity of SUD being a predictive factor for treatment outcome[37,38]. In those with a dual diagnosis, pharmacotherapy is less effective for treatment of ADHD when using standard dose, necessitating higher doses of medication[39].
Within the literature, the benefits of treating ADHD and comorbid SUD have been investigated, albeit with mixed findings. A meta-analysis of observational studies published in 2003 showed a significant reduction in risk of SUD in youths treated with stimulants compared with those who did not receive stimulants[40]. More recent observational studies have demonstrated a similar protective effect on later development of SUD[41,42]. Other studies, however, found comparable outcomes between children with and without medication treatment history[43].
Methodological issues with observational studies result in uncertainty regarding conclusions drawn as there may be baseline differences across groups. A meta-analysis of within-individual design studies, which are less prone to bias (although they cannot control totally for temporal effect), demonstrated a reduction of severity of SUD during periods when individuals were receiving medication, compared to periods when they did not[44].
A recent analysis of randomized controlled trials (RCTs) found a range of beneficial effects in the stimulant arm compared with placebo, including reduction of SU, increased abstinence, reduced craving, reduced frequency of ADHD symptoms, improved management of withdrawal symptoms, and decrease in the severity of ADHD symptoms[45]. This contrasts with a previous meta-analysis of 13 RCTs evaluating the effect of ADHD medication on outcomes in individuals with dual diagnosis which found a small to moderate reduction of ADHD symptoms but no beneficial effect for SU, drug abstinence or treatment discontinuation[39]. Carpentier and Levin[46] proffered some possible explanations for negative findings in their systematic review. These included high prevalence of polydrug use, presence of psychiatric comorbidity (additional to ADHD and SUD), possibility of suboptimal dosing of stimulant medication, generally low treatment retention, and influence of concurrent treatment (primarily cognitive behavioral therapy; CBT)[47].
There is increasing recognition of the need to identify and treat inappropriate use of substances by individuals with ADHD; and equally to identify and treat comorbid ADHD among those with SU or SUD. It is understood that treatment for those with concurrent ADHD and SUD may be complicated by the context in which services are being delivered. In the United Kingdom (as for many countries) individuals with ADHD are rarely able to access effective psychological treatments for their SU unless this is associated with a level of impairment considered to be a ‘disorder’[48]. Many young people do not fit within this criterion. Unfortunately, many healthcare practitioners do not feel they have the knowledge and skills to prevent this escalation, as intervention is commonly limited to specialist SUD services. Equally, expertise in treating ADHD within SUD services is rare. Uncertainty among practitioners on how to meet the needs for this complex group motivated the United Kingdom ADHD Partnership (UKAP) to convene a meeting attended by multidisciplinary experts to consider the complexities and challenges of working with young people and adults with concurrent ADHD and SU/SUD with the aim of providing helpful guidance and recommendations.
METHOD
Specialists in the fields of ADHD and SUD convened in London (United Kingdom) on 4th February 2022 for a meeting hosted by the UKAP. Meeting attendees included experts from ADHD and/or SUD services across a range of disciplines. Thirteen participants had medical qualifications/appointments, five had psychological qualifications/appointments and nine had academic qualifications/appointments. There was also representation by a service-user and an educational/occupational specialist.
The consensus group incorporated evidence from a broad range of sources. However, this largely reflects clinical practice and legislature in the United Kingdom, which may differ in other countries.
The meeting commenced with detailed presentations, providing an overview of the literature regarding the relationship between ADHD and SU/SUD. Following this, attendees separated into three breakout groups. Each group was tasked with providing a framework of guidance relevant to their assigned topic. Discussions were facilitated by a nominated group member and summarized by note-takers. Group participants drew on their clinical experience and research evidence, with discussions covering the following overarching topics: (1) Substances and reasons for use; (2) Identification, assessment, and treatment of illicit SU/SUD in young people and adults with ADHD presenting in community services; and (3) Identification, assessment, and treatment of ADHD in adults presenting in SU/SUD community and inpatient services.
Presentations and debate amongst attendees were audio-recorded and transcribed. A note-taker was allocated to each breakout group and following the meeting these notes were circulated to breakout group participants for review and approval. At the end of the meeting breakout groups presented respective conclusions and recommendations for debate, discussion, and approval by all attendees. All materials (transcriptions, electronic slide presentations and breakout group notes) were synthesized by the medical writer (KC) into a draft manuscript. Further drafts were produced by the lead author (SY) working in collaboration with the medical writer (and with consultation with some authors where necessary). A draft was then circulated to all authors for review and revisions; this did not generate any disagreements between authors. Following further revisions, a final draft was circulated to all authors for agreement and approval.
The consensus is based on published research, but it also reflects the views of the authors based on their practical experience. Acknowledging that children, adolescents, adults, and older adults experience different challenges and treatment demands[49,50], the consensus group considered differences in biopsychosocial needs across age groups.
RESULTS AND CONSENSUS OUTCOME
Substances and reasons for their use by people with ADHD
Alcohol and nicotine are the most commonly used recreational substances used among adolescents and adults with ADHD but cannabis is the most used illicit substance[18,19,38,51,52]. Stimulants such as cocaine, amphetamines and methamphetamine (Ice) are also common[53,54]; a meta-analysis reported the prevalence of cocaine use in adults with ADHD to be around 26%. Ten percent had cocaine use disorder[55].
Various reasons have been proposed for SU among individuals with ADHD. Individuals with ADHD often claim that, prior to their diagnosis, they used substances as a form of self-medication to attenuate ADHD symptoms and associated impairments. However, there is no robust empirical evidence to support this proposal[56,57]. Individuals report using substances frequently to help them to sleep, manage fluctuations in mood, and improve attention and executive functioning[58-60]. It has also been posited that individuals with ADHD may be more susceptible to using substances due to impulsivity (behavioral inhibition hypothesis)[61]. This, together with immediate gratification and reward-seeking behaviour may collectively impact on the positive and negative reinforcement of substances and their potency.
Adolescents and adults with ADHD have high rates of comorbidity with other conditions, many of which are associated with increased risk of SU. CD and ODD may explain the association[62-64]. Other studies have shown that depression, bipolar disorder, and antisocial personality disorder all convey an elevated risk for SU/SUD among individuals with ADHD[32,62,65-68]. Other potential reasons include increased exposure to psychosocial risk factors (e.g., parental SU/SUD, peer pressure, predatory grooming and exploitation, financial, family and work-related stressors, chronic low self-esteem, feelings of demoralization and failure, trauma and fear responses)[14,59].
Table 1 shows key aspects of the pharmacology of several commonly used recreational drugs that might be used by people with ADHD. The primary molecular targets and neurotransmitters that are impacted by interactions of different drugs are shown, most of these are not dopamine.
Table 1.
Pharmacology of commonly used recreational drugs that might be used by people with attention-deficit/hyperactivity disorder
|
Drug type
|
Primary target
|
Main effects/transmitters
|
Other actions
|
Antagonists/blockers
|
| Opiates | Mu opiate receptors | Kappa and delta opiate receptors | Naltrexone | |
| Naloxone | ||||
| Nalmefene | ||||
| Stimulants | ||||
| Cocaine | DAT | Inc. Dopamine | Local anesthetic Inc. 5HT | [BP-897 partial agonist] |
| Amphetamines | DAT | Inc. Dopamine | Mecamylamine | |
| Nicotine | Nicotinic ACH receptor | Inc. Dopamine | Varenicline | |
| Sedatives | ||||
| Ethanol | GABA/glut | Inc. GABA | 1Inc. Dopamine | No |
| Benzos | GABA | Dec. glutamate | Flumazenil | |
| GHB | GABA | Inc. GABA | No | |
| Solvents | N/A | No | ||
| Cannabis | CB1 receptors | 1Dopamine | Rimonabant | |
| Ecstasy | 5HT transporter | Inc. 5HT | Some DA release | 1SSRIs |
| LSD | 5HT 2 receptors | Stimulate 5HT | 5HT2 receptor antagonists |
Postulated but not proven.
Column 2 lists the primary molecular targets for the different pharmacological classes of drugs. Column 3 lists the neurotransmitters that are impacted by the interactions listed in column 2. Column 4 lists other molecular targets that these drugs can influence. Column 5 lists antagonists or blockers that can be used to stop or reverse the effects of the drugs. DAT: Dopamine transporter; GABA: Gamma-amino-butyric acid; inc: Increased; dec: decreased.
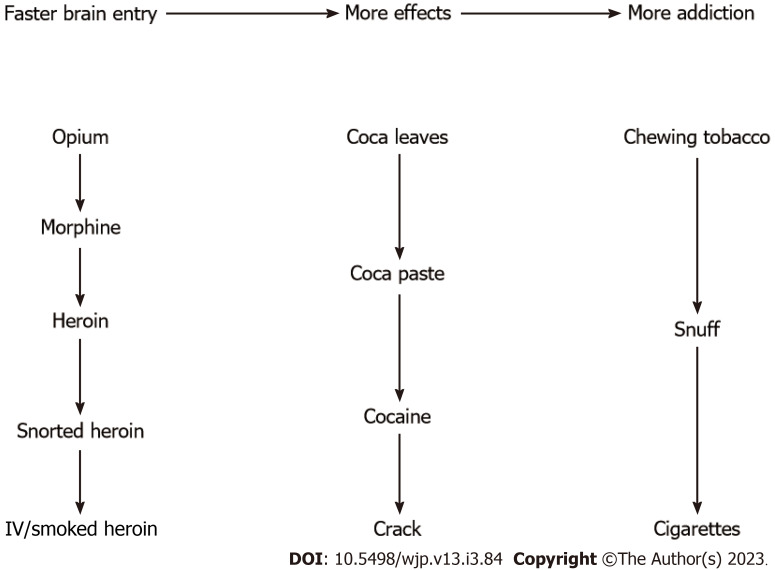
Biological factors such as speed of brain entry of stimulants may influence which substances are used[69]. Figure 1 shows three examples of drugs with accelerated brain entry.
Figure 1.
Examples of drug modification to accelerate brain entry. Brain entry escalates with the downward direction of the arrows.
The consensus group agreed that there is a complex interplay between an array of factors, which results in individuals with ADHD initiating use of illicit substances. Across the lifespan, motivation for using these substances may transition across several phases towards dependency[48,70,71].
Identification, assessment, and treatment of illicit SU/SUD in young people and adults with ADHD presenting in community services
When to refer individuals with ADHD for support for their SU/SUD: There was extensive debate regarding what would be considered a ‘red flag’ indicative of a SU problem developing in young people and adults with ADHD. Experimental drug use is common, with the highest level of experimental use usually occurring during adolescence. This in itself may not necessarily be a cause for concern. The threshold for what may be considered concerning or problematic is likely to vary; a person, parents, family members, teachers and employers may all have differing perspectives. It was agreed that ‘red flags’ should be understood in relation to the person’s community, social, economic, religious, and cultural circumstances. This includes contexts where SU may be normalized within the immediate environment the person inhabits. The boundary between use and misuse is likely to be influenced by what is normative within the individual’s immediate social network (family, peer group and wider neighborhood). It may also be influenced by politics and sociocultural values.
When considering ‘red flags’ (indicating possible SU/SUD), one should focus on any changes in presentation that are out of character for the person. Typically, this is a decline in self-care, physical and/or mental health, and daily functioning, often associated with social and occupational problems. Table 2 details several markers that may prompt concern; however, these are also markers of other evolving mental health and/or social problems. Thus it is the clustering of multiple markers together across various life domains that is informative. The key message is to ensure that SU/SUD is not disregarded as a potential explanatory factor for change in presentation.
Table 2.
Markers of potential concern for substance use/substance use disorder
|
Life domain
|
Markers
|
| Physical | Declining physical health including nausea and abdominal pain |
| Looks fatigued | |
| Disheveled | |
| Unexplained weight loss | |
| Dilated pupils, redness in eyes | |
| Muscle in-coordination | |
| Poor personal hygiene | |
| Sniffing | |
| Administration scars (needle entry marks) | |
| Daily functioning | Unaccountable increase in expenditure |
| Difficulty managing daily living tasks (including budgeting, staying on top of household tasks) | |
| Poor punctuality | |
| Possession of substances, hiding substances | |
| Accessing of prescription drugs in the home | |
| Difficulty managing underlying health conditions (e.g., epilepsy, diabetes) | |
| Home life | Absconding from home (adolescents) |
| Receiving packages in the post which they are eager to intercept | |
| Driving offences | |
| Accidental injuries, including road traffic accidents | |
| Increased risk of injury and assault (both to self and others) | |
| Difficulties fulfilling chores and/or parenting responsibilities | |
| Social services involvement | |
| Debts | |
| Gambling | |
| Housing problems and homelessness | |
| Educationand work | Truancy/absence from school/college or work |
| Deterioration in academic/work performance | |
| School detention, suspension, expulsion | |
| High turnover of short-term employment | |
| Official warnings and disciplinary procedures at work | |
| Social | Social withdrawal |
| Social exclusion | |
| Marginalized | |
| Sudden change in social groupings | |
| Part of a ‘bad crowd’ (gangs, friends much older than peers) | |
| Friendship and intimate relationship problems | |
| Domestic violence | |
| Mental health | Apparent deterioration in mental state and health |
| Signs of emotional or physical withdrawal from others | |
| Paranoia | |
| ‘Unexplained’ onset and/or change of mood swings | |
| Presenting as exhilarated or with excessive confidence | |
| Low mood and depression | |
| Irritability, agitation | |
| Anxiety | |
| Paranoia | |
| Confusion, delusions and/or hallucinations | |
| Emotional lability | |
| A&E admissions due to mental health condition | |
| Behaviour | Early use of experimentation with drugs including early onset vaping/smoking (e.g., under 12 yr) |
| Excessive use of energy drinks | |
| ‘Unexplained’ onset of behaviour that seems ‘out of character’ | |
| Change in personality/demeanor | |
| Lack of constructive interests and activities | |
| Disengagement of ‘healthy’ leisure activities (change in interest) | |
| Increased energy, restlessness and disinhibition | |
| Conduct problems and/or oppositional behaviour | |
| Irritable, agitated, aggressive and/or violent behaviour | |
| Risk taking behaviour (shoplifting, theft from home and/or others) | |
| Risky/compulsive sexual behaviour (promiscuity, risk of pregnancy, sexually transmitted infections) | |
| Solitary drug use | |
| Missing appointments | |
| Parenting issues leading to safeguarding concerns | |
| Self-harming behaviors | |
| Speech and cognition | Changes in cognitive functioning at different times of the day |
| Difficulty sustaining concentration | |
| Increased alertness | |
| Confusion | |
| Memory problems and loss | |
| Change in usual speech presentation (e.g., slurred, rapid or rambling speech) | |
| Reference to ‘needing’ substances (e.g., to help sleep, improve confidence) rather than use for fun or enjoyment | |
| Unexplained improvements in functioning |
The decision to refer to addiction services should be determined by level of impairment and distress and the wishes of the individual (and parents/caregivers/partner), if appropriate. It was noted that the legal class of substance (e.g., Class A drugs which are most likely to result in the most serious harm, compared with Class B and C drugs) and method of use (e.g., injecting) may determine the level of concern and/or the level of impairment due to associated harm to user.
The way in which the referral is made may depend on how the concern has developed; whether the individual has disclosed their use and/or expressed concerns, or whether it has been uncovered by other means (e.g., found on them/urine testing), and whether there are attempts to deny use. The consensus group agreed that it is important to spend time building rapport with the individual and to develop a shared understanding of SU and how it fits in within a broader context.
Referral pathways are different across regions dependent on commissioning and funding. Anecdotal accounts from the consensus group emphasized reduction/closure of young people’s addiction services, resulting in young people being ‘bounced around’ between different services in order to find appropriate support. Some consensus group members reported that some child and adolescent mental health services and adult services do not accept referrals for individuals with SU difficulties. Exclusion criteria may differ according to type of substance and methods used. Later in adolescence, young people may be referred early to adult addiction services, depending on region.
The consensus group agreed that ADHD services should have an agreed procedure for dealing with concurrent SU/SUD, taking into consideration regional available resources (health, social and third sector).
Assessing people with undiagnosed ADHD: Assessment of ADHD and SU/SUD can be challenging, particularly when ADHD has not previously been diagnosed. Like other diagnoses, the diagnosis of ADHD, with or without SU/SUD requires careful and comprehensive clinical assessment. This should include a full developmental history, mental health history and current mental state examination, medical history, educational/employment history, social history, and, when helpful, assessment of cognitive executive functioning difficulties. It is also important to consider family history of ADHD and SU/SUD, and other psychiatric and neurological problems. Gender differences in presentation should be considered (e.g., symptom severity for hyperactive-impulse symptoms may be lower in females) which may result in missed diagnosis or misdiagnosis[72].
Assessment of ADHD with comorbid SU/SUD involves careful examination of symptom severity and frequency, chronicity, pervasiveness, degree of impairment across life domains, and childhood onset. A useful tool to assess impairment may be the Weiss Functional Impairment Rating Scale[73]. Nevertheless, while rating scales are useful aids for clinical assessment, the consensus group emphasized the importance of services not rigidly adhering to thresholds and cut-offs as this may lead to high proportions of false positives and negatives.
It is essential to determine if ADHD or SU/SUD, or both can best explain the presenting symptoms. One key consideration is whether ADHD is masked by SU/SUD. Some individuals report that substances have a countering effect on their ADHD symptoms (e.g., the consensus group shared anecdotal accounts of experiencing patients who report stimulant use has a calming effect rather than an elating effect). Examining the temporal course of ADHD-like symptoms and SU/SUD is crucial. Assessment must be conducted by qualified healthcare professionals with training and expertise in assessing dual disorders so that differential diagnosis can be considered[22]. It is not advisable to conduct an assessment when an individual is under the influence of substances at the time of the assessment and/or when at a stage of withdrawal[24].
Assessing people with diagnosed ADHD: Individuals who already have a primary diagnosis of ADHD should be carefully monitored for SU. This might include alcohol, tobacco, caffeine, study drugs (i.e., accessing prescription stimulants to help focus and/or stay awake). It is important to obtain information regarding the age of initiation for each substance, frequency of use, methods of administration, the social context in which use takes place, the effects of the substance on the person’s cognitive, psychological, physiological, and behavioral functioning, the medical, educational/employment, social and medical problems attributable to SU, and any previous treatment. An association between problematic video gaming and nicotine, alcohol and cannabis use has been reported, so asking about these factors (and internet use more broadly) may be helpful[74].
When conducting the assessment with young people, it is important to consider the role of parents/caregivers (and taking account of the wishes and needs of the young person). There may be additional physical, criminogenic, and safeguarding risks associated with SU which will need to be addressed. Like other assessments, the person should be informed of the confidentiality of information shared and circumstances in which this will be breached.
The utility of SU/SUD screening assessments as an indicator for further assessment was discussed. A commonly used screening tool recommended by the consensus group for young people is CRAFFT. This is an acronym generated from six core questions relating to the experience of young people: (1) Have you ever ridden in a CAR driven by someone (including yourself) who was "high" or had been using alcohol or drugs? (2) Do you ever use alcohol or drugs to RELAX, feel better about yourself, or fit in? (3) Do you ever use alcohol/drugs while you are by yourself, ALONE? (4) Do you ever FORGET things you did while using alcohol or drugs? (5) Do your family or FRIENDS ever tell you that you should cut down on your drinking or drug use? and (6) Have you gotten into TROUBLE while you were using alcohol or drugs?[75].
The authors suggest that young people who complete the CRAFFT before seeing their healthcare practitioner are more likely to answer honestly[76]. Completed self-administered copies can then be used by practitioners to guide discussions about SU.
For adults, commonly used screening tools include the Drug Use Disorders Identification Test[77], Drug Abuse Screening Tool (DAST)[78] and Alcohol Use Disorders Identification Test (AUDIT)[79]. The DAST and AUDIT have demonstrated acceptable reliability and validity among adults seeking ADHD clinical evaluation[80].
For young people and adults alike, it is important to identify the substances the person is using, and to discern the intended (i.e., function) and unintended consequences of use. This may differ for different substances. This can be explored in relation to the five-stage pathway (experimental, social, instrumental, habitual, dependent) (refer to Young and Bramham[81] and/or Young and Woodhouse[48] for more information). Individuals should be encouraged to acknowledge the adverse consequences of their SU across physical health, mental health, personal functioning, risky behaviour, interpersonal relationships, ability to study or work, and contact with criminal justice system (CJS).
However, many people with ADHD have difficulty engaging in consequential thinking processes, requiring them to be empathically guided through the process. It can be helpful to start by first acknowledging the benefits of SU before considering disadvantages.
Understanding how SU and ADHD have interacted in the past and present can help services and the individual to understand internal and contextual motivational mechanisms which increase or attenuate risk of SU. This will be helpful in identifying treatment areas. One assessment method involves a functional analysis of behaviour which systematically assesses the antecedents and consequences of specific behaviors. For SU associated behaviors, this involves the assessment of internal and external factors that trigger SU, including factors of positive reinforcement (e.g., euphoria) and negative reinforcement (e.g., numbing of feelings). In turn, the analysis is a helpful strategy for identifying targets for intervention.
Generating chronological timelines can be a helpful technique to record and identify potential interactions between important aspects of ADHD symptomatology (e.g., periods of heightened/lower symptoms, periods of deterioration/functional improvement) and SU (e.g., onset, drug free periods, escalation of use, serious difficulties including episodes of drug-induced psychosis). Mapping these out in this way can be helpful to discern associations concerning onset and maintenance of use, triggers of risk and optimal management.
Pharmacological treatments
Historically there have been concerns regarding prescribed stimulant medications’ abuse potential, addictive nature, or that they may worsen pre-existing SU/SUD. These concerns are unfounded[43,82-86]; the formulations that are used are not addictive. Tolerance effects are not clear. Some clinicians have noted a reduced benefit from stimulants over time in some patients, although this is not a universal problem. Neuroimaging studies (e.g., PET studies[87]) point to an increase in dopamine reuptake receptors in adults with ADHD treated for up to 12 months with stimulants. This evidence suggest that tolerance may happen during treatment with psychostimulants. However, the experience of consensus group members was that individuals are more likely to be poorly compliant with stimulant medication or choose to stop taking it, rather than seek higher doses.
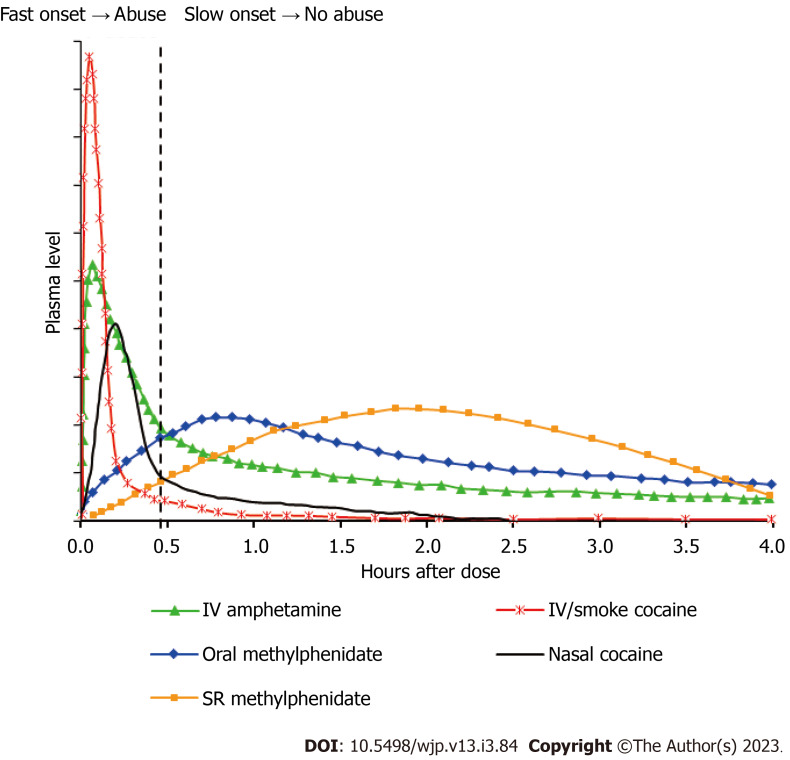
Nevertheless, for individuals with comorbid SU/SUD, long-acting preparations are recommended rather than immediate release due to their lower abuse potential (immediate release stimulants are more likely to be crushed to a powder and snorted or used intravenously)[88]. The time course of common stimulants taken via different routes is shown in Figure 2. Speed of plasma peaks determines abuse ability. The intra-venous route produces the fastest brain entry and highest peak concentration with intra-nasal cocaine somewhat behind. These effects explain the high propensity for liking and hence abuse of these. Oral methylphenidate peaks at about one hour and slow-release forms even later; a similar profile is seen for lisdexamfetamine. In general, drugs with a low peak concentration and where the peak occurs after 30 minutes shows low abuse liability. Notably, lisdexamfetamine is a pro-drug (rather than a slow-release preparation) that has to be metabolized in the blood to release the active ingredient (dexamfetamine). This metabolic step explains why even after intra-venous injection lisdexamfetamine does not produce a noticeable ‘high’ hence providing a low abuse liability[69].
Figure 2.
Speed of plasma peaks for different types of stimulants. IV: Intravenous; SR: Slow release.
The consensus group emphasized that pharmacological treatment nihilism is not appropriate. It is essential that individuals with ADHD and SU/SUD are not deprived of effective medications. However, short-acting preparations should be reserved for a very circumscribed group (e.g., in contexts where there is possibility for supervised consumption).
Medication should be informed not only by the effectiveness of the medication but also by safety and tolerability (i.e., to physical and mental health).
There was agreement that non-stimulant medicines should generally be reserved as a second line treatment option (even in dual diagnosis cases) as research has shown that, on average (i.e., at the group level) they are less effective than stimulants[89] raising risks of non-compliance. Compared with stimulant medications, where the benefits can be very quick (sometimes within a few days), non-stimulant medications take several weeks to have a therapeutic effect[53]. An exception to this, may be for those misusing alcohol; atomoxetine may reduce alcohol cravings[90].
There was debate about whether voluntary drug testing should be used to monitor use of substances. Drug testing is generally used to monitor compliance with drug rehabilitation programs where there may be suspicions of non-adherence. The overarching view was that where clinicians have concerns about severity of SU, support from specialist SUD services should be sought.
Research has shown that heart rate and/or blood pressure increases in individuals with ADHD treated with stimulants[91,92]. Small but persistent increases in heart rate and/or blood pressure over a sustained period has raised concerns. Meta-analyses however have found no significant link between ADHD medication and serious cardiovascular outcomes such as sudden death, stroke, or myocardial infarction[93,94], though this evidence reports at a group-level, so it is not informative at an individual level. Where there are concerns regarding cardiovascular risk, a cardiologist should be consulted. This is considered particularly important when there is a personal or family history of cardiovascular conditions (e.g., premature sudden/unexpected death in children or young adults, clinically important arrhythmias, prolonged QT syndrome, hypertrophic cardiomyopathy, and Marfan syndrome). For safety[95], the group stressed that heart rate and blood pressure should be measured before initiating medications and routinely during treatment, and titration should be slow. It is also worth being aware that people with ADHD may be more sensitive to the effects of or dependence on sedatives such as alcohol.
Treatment with ADHD medication, especially stimulants, may increase the health risks from the concurrent use of recreational drugs[96]. These are presented in Table 3. In general, there are few specific hazards from the interactions of ADHD medication with recreational drugs with the exception of other powerful stimulants (especially cocaine/crack) which add to the burden on dopamine and noradrenaline neurotransmitter effects and the potential for cardiac events and seizures[96].
Table 3.
Potential increased risks from use of recreational drugs in people treated with attention-deficit/hyperactivity disorder medication
|
Substance
|
Risks
|
Risk level
|
Antidotes
|
| Alcohol | Intoxication, dependence | ++ | |
| Cannabis (d9THC) | Anxiety, paranoia | + | Benzodiazepines |
| Cocaine | Cardiac problems, seizures | +++ | b-blockers – benzodiazepines |
| LSD/psychedelics | Paranoia | + | Risperidone/olanzapine |
| Ketamine | Dependence, bladder damage | ++ | |
| MDMA | Cardiac problems | ++ | b-blockers |
| Methamphetamine | Dependence, paranoia | ++ | Risperidone/olanzapine |
| Nitrous oxide | Intoxication, neuropathy | + | Vitamin B12 |
| Opioids | Respiratory depression, dependence | ++ | Naloxone naltrexone |
| Sedatives | Intoxication, ataxia | + | Flumazenil (for benzos) |
| Spice/synthetic cannabinoids | Cardiac problems, seizures | +++ | Rimonabant |
+: Moderate risk; ++: Considerable risk; +++: High risk; LSD: Lysergic acid diethylamide; MDMA: Methylenedioxymethamphetamine.
Considering when to commence ADHD medication was an area of intense debate. Consensus participants acknowledged that ADHD symptoms and associated impairments make it more difficult to treat SU difficulties, and vice versa. The consensus group agreed that ideally SU would be stabilized (e.g., by the individual demonstrating a level of improved functioning with life not being primarily organized around substances) before initiating medication for ADHD. When this is not possible, services may need to be pragmatic, with decisions informed by an individual risk assessment. There was agreement that abstinence is not necessary for individuals to benefit from ADHD medication.
In the United Kingdom there are lengthy waiting lists for an assessment of ADHD (some being two years and over)[97]. Hence individuals may have stabilized SU at point of referral but relapse whilst waiting. It was agreed that there may be a role for prioritization of those with SUD within ADHD services. This is done for other groups across other health services (e.g., pregnant women, veterans, those with long-term conditions).
Prescribing issues for certain groups were highlighted in discussions. Evidence indicates that adherence to medication declines in teenage years. This has been attributed to adverse effects, sub-optimal response, reduction in parent supervision, increased need for autonomy, comorbid conditions, and social stigma associated with ADHD diagnosis and taking medication[98]. The consensus group noted that this may be of particular concern, acknowledging that young people may be vulnerable at this time to misuse substances to manage their symptoms[61]. Research suggests that treatment with ADHD medication may protect against SU/SUD, but only if the medication is taken continuously[40,86,99,100].
It is imperative to provide psychoeducation to encourage young people to understand and take ownership of their treatment[101]. Provision of developmentally appropriate healthcare within services may also be of benefit[102], a summary of which is provided in Table 4[103].
Table 4.
Developmentally appropriate healthcare dimensions and examples of implementing them into practice
|
Dimensions of DAH
|
In practice
|
| Biopsychosocial development and holistic care | Assess wider aspects of young person’s life using approaches such as HEEADSSS tool (Home, Education, Eating, Activities, Drugs, Sexuality, Suicide, Safety) |
| Consider stage young person is at in their development rather than chronological age | |
| Acknowledgement of young people as a distinct group | Opportunity for young person to be seen independently (for some or all of the consultation) |
| Flexible access to service (e.g., outside school/college hours) | |
| Dedicated clinics and space (e.g., age-banded clinics, appropriately sized seating, magazines/posters of relevance and interest) | |
| Consideration of different ways young person can contact the service (e.g., digital technologies rather than letters/phone calls) | |
| Explain confidentiality and rights; display confidentiality policy in waiting room | |
| Adjustment of care as the young person develops | Communication to be adjusted in line with cognitive development |
| Appointment letters addressed directly to young person in addition to parents/caregivers, when needed; language used is clear | |
| Use of simple self-assessment tools which may feel less awkward for young person | |
| Record contact details for both young person and parents/caregivers | |
| Empowerment of the young person by embedding health education and promotion | Psychoeducation provided to young person and parents/caregivers |
| Shifting emphasis and supporting family to move from shared-care to self-management as the young person gets older | |
| Check out with young person how they would like parents/caregivers to be involved | |
| Involve parents/caregivers in treatment decisions in ways that have been agreed with young person | |
| Sign-posting young person to local services, as appropriate | |
| Discuss with young person their confidence and independence in making appointments, managing medication, etc. | |
| Working across teams and organizations | Workforce training in developmentally appropriate healthcare, including strength-based approaches such as solution-focused and motivational interviewing |
| Adult service included in transitioning planning prior to transfer (e.g., multi-disciplinary team meetings with adult and child teams present, adult services copied into correspondence) | |
| Transition planning to start early (aged 13-14) | |
| Opportunity for young person to visit adult service prior to transfer; provide information leaflet about service to be transferred to | |
| Young people issues are considered in service policies and guidelines; consistency of policies in child and adult services | |
| Young people’s participation at all levels of delivery |
DAH: Developmentally appropriate healthcare.
The consensus group acknowledged the complexity of prescribing and monitoring medication among adults. As individuals get older, they are likely to be prescribed other medications to treat comorbid mental health and physical health conditions. Practitioners should refer to summaries of product characteristics when considering prescribing needs and potential interactions with other medications. Cardiac risk increases with increasing age, which should be considered when prescribing. Monitoring of weight may also be appropriate for adults who are misusing substances, as aside from the potential of stimulant related suppression of appetite, they may prioritize buying drugs over food.
ADHD is associated with working in unskilled occupations (i.e., those not requiring formal education)[104]. Anecdotal accounts from consensus group members discussed individuals working in unskilled occupations with varying shift patterns who use substances chronically. This disrupts sleep patterns and makes monitoring and review of pharmacological treatment problematic, for example, setting specific times-a-day prescriptions, and difficulties attending clinic appointments, especially if they need to attend multiple services (ADHD and SUD).
Psychological interventions
Multi-modal treatments are emphasized for young people and adults with comorbid ADHD and SU/SUD[105]. Several RCTs investigating pharmacological interventions for individuals with co-occurring ADHD and SU/SUD have demonstrated few group differences between medication and placebo group. These studies have had adjunct psychological therapies such as CBT or motivational interviewing (MI), leading to some authors positing that observed improvements may be attributed to the psychological therapy. The design of these studies prevents firm conclusions being drawn, although suggests that psychological therapy is a useful intervention for treating SU/SUD among those with ADHD[59].
Psychological approaches vary across the lifespan and the content of the treatment should be tailored to meet individual need[81]. Specific assessment and treatment techniques for young people and adults with ADHD and SU/SUD can be found in Young and Bramham and/or Young and Woodhouse[48,106]. The consensus group agreed that the following adjustments and psychological interventions will be helpful.
Adjustments to treatment: Executive functioning and memory deficits are commonly reported in individuals with ADHD[107,108]. In addition, chronic use of substances has been found to be associated with visuospatial and memory deficits[109]. Such difficulties can make engaging in therapy and sticking to long-term goals challenging[110]. It is important to accommodate for deficits associated with ADHD and/or SU/SUD. Where neuropsychological testing has been conducted, the strengths and weaknesses profile can be used to inform adaptations to the treatment process. Some specific adjustments to traditional treatment approaches that should be considered include: Using text and/or email reminders to reduce non-attendance due to forgetfulness, adapting language and behaviour (implicit rather than explicit conversational approach), adjusting the pace of introducing new elements in treatment, making the treatment more concrete, using material that is easy to understand, greater use of supplementary visual materials, repetition and consolidation of core concepts, a high level of structure, shorter and/or more frequent sessions, mid-session breaks, and identify support between sessions for homework tasks.
It is recommended that individuals are provided with a notebook which they should be encouraged to bring to sessions. This serves as a record of the treatment, including the strategies and techniques they have found most helpful and later becomes a resource when treatment has ended. Any handouts summarizing key information should be secured in the notebook. Exercises should be completed in the person’s own writing and their own words (with careful guidance from the practitioner, as needed) to facilitate ‘ownership’ of the problem, and in turn responsibility and action. For individuals who prefer to keep electronic records, handwritten notes can be scanned for storage on electronic devices.
MI: Motivation is an important predictor of treatment outcome[111]. However, motivation to stop misusing substances may be especially challenging when individuals perceive themselves to use them to self-medicate. MI is a client-centered method for enhancing motivation to change by exploring and resolving ambivalence[112] and it may be an effective model to work for adults with ADHD and coexisting SU/SUD[113]. MI techniques involve expressing empathy, supporting self-efficacy, rolling with resistance, and developing discrepancy. A central tenet of MI is to avoid confrontation as this is posited to incite resistance. Individuals who misuse substances go through several stages in a ‘transtheoretical model of change’ (precontemplation, contemplation, preparation, action, maintenance)[112,114]. MI is suggested to be particularly helpful in the initial motivational stages (precontemplation and contemplation)[48].
Different MI techniques can be used depending on what stage of the ‘transtheoretical model of change’ the person is in (i.e., readiness to change). An individual’s readiness to change is dependent on many factors (e.g., environmental factors such as friends being drug users and/or living in an area where drugs are frequently offered, psychological factors such as beliefs that they are unable to function adequately without using substances), and thus it is important to consider a biopsychosocial perspective. Stages are cyclical (not linear), and it is common for individuals to oscillate between stages. Practitioners need to be aware of the persons current motivational stage and should monitor interest to engage in treatment, adapting treatment interventions as needed. Helpful tools to explore ambivalence and encourage change include use of dissonance charts and decisional balance sheets (please refer to Young and Bramham[106] for further details about these techniques). The group considered that it may be helpful for MI techniques to be employed more broadly by key frontline contacts within services, which may necessitate further training.
Formulation: Formulation (or case conceptualization), beyond diagnosis[115] is central to intervention planning. Within the formulation it is important to consider the bidirectional relationship between ADHD and SU/SUD. Formulation can help both the practitioner and individual make sense of the individual’s experience in a flexible and systematic manner. One framework that may be useful is the Five Ps model[116,117]. This is an idiographic-based framework which enables systematic and holistic examination of multifaceted and complex subjects such as comorbid ADHD and SU/SUD. The Five Ps model organizes information into five sections: (1) Presenting problem; (2) predisposing factors; (3) precipitating factors; (4) perpetuating factors; and (5) protective factors.
Practitioners may find it helpful to rename these using more accessible language for individuals, particularly young people. This may be current (what is happening now?), past (what has happened in the past that may be important?), triggers (what sets things off? what was happening when difficulties started?), what keeps things stuck (things that keep difficulties going and/or make change difficult), and positives (positives in life, including own strengths and support from others). These Five Ps should include biological, cognitive, environmental/systemic and personality considerations and the relationships between factors should be explored.
Psychoeducation: Psychoeducation is an important part of treatment that facilitates treatment engagement. Psychoeducation may be provided more generally to family members, but it is important that key information is also directed to the young person in the absence of family members. This is because without ‘buy-in’ from the individual there is a risk they will just go through the motions to keep people happy or drop out of treatment. It also facilitates informed decision-making and may improve medication adherence and outcomes[118].
Psychoeducation should not be considered a one-off event but rather a process which should be returned to as needed. Psychoeducational interventions are particularly important at key points of service and/or personal transition, with differing topics covered specific to changing biopsychosocial needs and demands. For children and adolescents there may be misconceptions about medication. Discussions should include basic information about ADHD, the purpose and benefits of medication and the long-term consequences of SU. The latter should include legal consequences (e.g., providing substances to a friend can result in supply charges, in turn affecting ability to apply to law or medical schools and travel to destinations such as the United States). For older adolescents and adults, psychoeducation should include discussion about driving including the increased risk of accidents, and legal penalties if convicted of driving under the influence of alcohol or drugs (e.g., losing driving license, a fine, imprisonment, and a criminal record). Both accidents and convictions are likely to substantially increase insurance costs (in the United Kingdom convictions have increased since the introduction of roadside drug testing). Psychoeducation should also include information regarding misconceptions around medication increasing the likelihood of addiction, safety of medication when using substances (e.g., increased risk when binging) and how with age risk significantly increases.
When approaching the care of young people with co-occurring ADHD and SU/SUD, engagement and support of families/carers is critical. Societal connotations about SU can be disparaging and group workshops are helpful in negating feelings of shame through sharing experiences in a supportive environment. Given the heritability for ADHD[108], some parents/caregivers are likely to also have ADHD (possibly unrecognized) and it is important the psychoeducational interventions are facilitated in a manner that aids understanding and engagement. Discussion topics may include the increased risk of SU/SUD for those with ADHD; potential signs and symptoms to be aware of; when and how to seek treatment; treatment options; value of adherence to ADHD medication; how to support a young person (dos and don’ts); refuting myths and misconceptions; dispelling stigma and feelings of shame; and coping skills for parents/caregivers.
CBT: The content of CBT interventions should be adapted to meet individual needs associated with cognitive and emotional functioning of individuals with ADHD and SU/SUD. Individuals with concurrent ADHD and SU/SUD may find it difficult to envisage the potential for change; their impulsivity, together with physiological and/or psychological SU dependency, may leave them perceiving they have little choice and/or will. Agreeing realistic goals is essential and should be based on the individual’s presentation and needs (ADHD symptomatology, severity and complexity of SU/SUD, physical health, mental health, internal and external resources, social and cultural systems, and the person’s motivation). To increase motivation, goal selection should be a collaborative effort and the goal concrete and relevant. When considering level of functioning (emotional, behavioral and cognitive), it is often necessary to help guide the person in ‘fine tuning’ treatment goals. Goals which are abstract and/or unrealistic are less likely to be achieved and in turn are likely to negatively affect motivation, confidence, and self-esteem, which may already be fragile[119,120]. Hence goal negotiation is a process and to do this effectively it is important that a good therapeutic alliance has been developed.
Individuals should be invited to use self-reinforcement techniques as useful reminders of their goals, which can help nudge them toward achieving them. These should have some personal meaning. Examples may include mobile phone screensaver with an important word or phrase or symbol, brightly colored sticker on the strap of a wristwatch or the back of a mobile phone, written message in the ‘notes’ app of a mobile phone, flashcards that are carried in a wallet. A reward system should also be incorporated to motivate new behaviour. Individuals with ADHD struggle to delay gratification; teaching individuals to give themselves rewards on a ‘little and often’ basis may help to satisfy immediate gratification need and reinforce new behaviour. One form of reward is encouraging ‘self-talk’ (e.g. by giving self-praise, encouraging and motivating statements). It may however be that individuals prefer more material/tangible rewards. Small rewards may be awarded for achieving small steps, with larger rewards introduced at the end of longer periods of sustained behaviour. The person should also be encouraged to share their success and progress with their support network (who will respond positively). This will help to maximize motivation and encouragement.
When working with young people, behavioral-oriented interventions may be more of a focus than cognitive interventions (due to the abstract nature of thinking required). It is important that individuals learn behavioral skills that can be applied on a long-term basis. This should encompass developing skills and confidence to manage potentially high-risk situations such as being offered substances and/or when there is peer pressure. One of the best methods of acquiring new behaviors is to practice in role-plays, where individuals can learn and practice strategies that involve problem-solving, planning, and impulse control. The aim is to learn specific skills that can be automatically applied, minimising cognitive load during real-life stressful situations. Overt rehearsal has been found to enhance treatment effects[106]. In-session practice is considered particularly important for individuals with a dual diagnosis of ADHD and SU/SUD as it is expected they may have difficulty completing practice exercises outside of session.
Individuals should be made aware of emotional and physical states that are likely to increase risk of SU, including when they are most likely to be sensitive to cravings, urges and withdrawal. Identifying and engaging in scheduled activities during ‘risk periods’ as part of a wider structured timetable can help young people to maintain abstinence when they are likely to be at their most vulnerable. They should also be guided to use replacement techniques (i.e., replacing substances with something that is less harmful) to assuage cravings and urges. Methadone is commonly prescribed as a replacement for heroin, and nicotine patches, gum, lozenges and vapes/electronic cigarettes as substitutes for cigarettes. Similarly, drinking fizzy drinks may help to alleviate urges to misuse alcohol.
Cognitive interventions should be introduced, as appropriate, to meet the developmental needs of the individual. One such program is the manualized R&R2ADHD program, which is suitable for young people and adults. It covers topics of relevance to both ADHD and SU/SUD, including the development of prosocial competence skills, cognitive and executive functioning skills, critical reasoning, consequential thinking, emotional control, negotiation and assertiveness skills, and social problem-solving skills[61,121-123].
Relapse and prevention: Miller and Rollnick[112] state that individuals with SU/SUD are likely to oscillate between the stages of change several times before abstinence is achieved. Relapse is common for those without ADHD, and those with comorbid ADHD may be at an increased risk[124]. This understanding needs to be built into the expectations of treatment for both the service, individual and family/carers to avoid a sense of disappointment and failure. Services can help prepare individuals for relapse incidents by helping them to develop an action plan. This should include a list of warning signs and triggers for relapses and setbacks, and strategies that they have found helpful over the course of treatment which they can use to help prevent relapse. It is advisable that individuals make a note of these strategies as they progress through treatment. Acknowledging the likelihood of relapse, the plan should include compassionate messages designed to reassure and help motivate the person to get back on track, such as “I am human, we all make mistakes, I can move forward”. Contact information for personal and professional networks to access support should also be included in the plan. This may include family, friends, local support groups, nominated mentors and/or ‘buddies’, occupational health services and confidential services. Information contained in the plan should be in the person’s handwriting using their own words as this will help them to ‘own’ the plan. Individuals with concurrent ADHD and SU/SUD may require ‘booster’ sessions after treatment has concluded[124].
Identification, assessment and treatment of ADHD in adults presenting in SU/SUD community and inpatient services
Identification: Those working in SUD services should be vigilant to ADHD as a possible comorbid diagnosis, given the high prevalence of adult ADHD among those with SUD. The inherent challenges of accurately assessing ADHD in SUD services was highlighted in group discussions. A major problem is the overlap of ADHD symptoms with intoxication and withdrawal states (e.g., agitation, restlessness, impulsive behaviour, concentration difficulties) and common outcomes between the two conditions (e.g., job loss, poor school performance). These factors often result in ADHD being overlooked with symptoms and impairments in functioning erroneously attributed to SU[125]. High rates of comorbidity with other conditions (e.g., anxiety, depression, bipolar disorder, personality disorders and autism) may further complicate diagnosis (see Table 5). Practitioners need to be aware that identification is further complicated by individuals with ADHD developing compensatory strategies that mask symptoms and/or that limit the (negative) impact on their functioning[126].
Table 5.
Overlapping symptoms between attention-deficit/hyperactivity disorder, substance use/substance use disorder and other psychiatric disorders
|
Symptom
|
ADHD
|
SU/SUD
|
Other psychiatric comorbidity1
|
| Agitation | √ | √ | √ |
| Anxiety | √ | √ | √ |
| Hyperactivity | √ | √ | |
| Impulsivity | √ | √ | √ |
| Inattention | √ | √ | √ |
| Intolerance to frustrations | √ | √ | √ |
| Mood instability | √ | √ | √ |
| Poor concentration | √ | √ | √ |
| Poor memory | √ | √ | √ |
| Restlessness | √ | √ | √ |
| Risk-taking behavior | √ | √ | √ |
| Sleep difficulties | √ | √ |
Anxiety, depression, bipolar disorder, personality disorders.
ADHD: Attention-deficit/hyperactivity disorder; SU: Substance use; SUD: Substance use disorder.
Assessment: The consensus group recommended screening for ADHD in adults with SUD. Research suggests that the Adult ADHD Self-Report Scale (ASRS)[127] could be a viable option for screening ADHD in those with SUD in terms of its sensitivity[110]. However, research indicates a lower specificity when compared to general population data[128], resulting in higher probability of false positives. This is likely to be explained by higher prevalence of comorbid psychiatric conditions as well as deficits associated with SUD[129]. Thus, the ASRS may serve as a guide to identify individuals with SUD at high risk for ADHD diagnosis, but this should be interpreted with caution and always followed up with a comprehensive clinical evaluation to differentiate findings from associated psychopathology.
Whilst screening is recommended for everyone accessing SUD services, the consensus group noted that this is not current practice. Observable markers were considered that may trigger screening, noting that some individuals appear to function better than others under SU. In particular, some substances may have a paradoxical effect for those with ADHD (e.g., illicit stimulant use has shown improvement in attentional capacity and lower psychomotor activity rather than an elating effect[130]). Discussing the reasons for use (e.g., to calm, dampen hyperactivity, intrusive thoughts, sleep) may be helpful, although this may be a factor associated with several psychiatric conditions and not solely ADHD. Other markers include presenting behaviors that appear beyond SU (e.g., impulsivity; evidence of chaotic SU; frequent contact with the CJS and/or from an early age; gambling and other addictions, including caffeine; rapid relapse after de-toxification, transition from in-patient or other structured environments and difficulties in engaging with services and/or maintaining treatment). Importantly, for those in the care of institutional settings, their current presentation may be misleading due to high levels of structure and routine that are typical of these environments.
When assessing suspected ADHD in individuals with SUD, it important to bear in mind that substances can mimic the symptoms of ADHD (negatively affecting concentration, organization, and impulsivity)[131]. Huntley and colleagues[24] found a clinically significant reduction in self-rated ADHD symptoms when comparing evaluations a few days after admission to a detoxification unit with evaluations one week later, when individuals had been detoxified or stabilized on long-term medication. This resulted in 40% of participants no longer meeting screening criteria for ADHD. Thus, in settings that prioritize rapid detoxification and discharge, screening may not provide meaningful results. Screening in addiction services should not occur at reception/upon admission but a few weeks later as it is important to obtain a stable baseline for functioning. Should screening at reception/upon admission be service policy, it is recommended that this be followed up with a second screen. Aside from factors associated with SU or its withdrawal hampering assessment, individuals may be reluctant to divulge information and reveal vulnerabilities. They may not trust how information will be used[132].
Ideally, clinical evaluations for ADHD are best conducted during a period of sustained abstinence, or once detoxification or stabilization for substance dependency has been completed. Some authors recommend at least one month of abstinence in order to assess for ADHD symptoms reliably and accurately[133]. The group however acknowledged that this recommendation may be difficult to implement in community contexts, particularly where ADHD symptoms and associated impairments in functioning may be hindering individuals from effectively engaging with SUD services. The consensus group highlighted potential risks associated with detoxification if ADHD remains untreated, including chaotic relapses. In these cases, it is important to guard against diagnosing ADHD-like symptoms that arise because of SU in the absence of underlying ADHD.
Consensus group members noted that for both inpatient and community settings, the assessment content will be the same, although the process is likely to differ, with potentially a slower paced assessment within community settings, accounting for environmental context and time to build relationships in the community.
As discussed previously, assessment must rely on a detailed developmental history for differential diagnosis. This should include a focus on drug and alcohol-free periods of the individual’s life (e.g., checking whether ADHD symptoms are present during periods of abstinence and/or at time prior to onset of SU) to establish if these symptoms are primary or drug induced. It is common for adults with ADHD to have other concurrent conditions including depression, anxiety, antisocial personality disorder, emotionally unstable personality disorder, and bipolar disorder. These conditions are also highly prevalent among adults with SUD. They also share many common symptoms with ADHD. For example, emotionally unstable personality disorder and ADHD share impulsivity characteristics. It is therefore imperative that as part of a comprehensive differential diagnosis assessment, the process also looks to exclude other conditions that could better explain presenting ADHD-like symptoms. Assessing individuals with SUD for ADHD requires specific expertise in psychiatric evaluation to enable differentiation between ADHD and other psychiatric disorders. Group members highlighted the risk of diagnostic overshadowing especially with personality disorder, when practitioners are not well-versed in neurodevelopmental disorders, indicating a need for improved training in psychiatric services.
There may be a small number of individuals with SUD who present for ADHD assessment to access prescribed stimulant medication. As highlighted in the earlier section discussing the pharmacokinetics of stimulant medication for ADHD, long-acting preparations have low abuse liability. Should individuals be seeking stimulant medication for misuse purposes, it is likely that they will be dissatisfied with the effect, as they will not obtain the ‘high’ that they anticipate. Practitioners should ascertain the individual’s expectations of diagnosis and treatment and be mindful that for a small number of individuals, symptoms may be exaggerated and/or feigned for perceived external gain[48].
Where possible, obtaining collateral information from other sources will help to reduce the risk of misdiagnosis. Obtaining informant data on ADHD symptoms for this population however can prove difficult due to the strained interpersonal relationships that many individuals with SUD have with family and friends[24]. The person may also be reluctant to share contact information. In clinical practice, the diagnostic assessment of ADHD for persons with SU/SUD may primarily rely on self-report, despite the fact that cognitive impairments associated with SUD can compromise the reliability of retrospective recall[129]. Nonetheless, where only self-report is available, research indicates that for most cases this may be sufficient, with moderately high correlations identified between informant and self-report ratings[24]. This is increased for individuals with good insight into the condition[134]. The absence of collateral information should not delay or prevent assessment.
SUD may exacerbate ADHD symptoms by as much as 30%[90] and this may alleviate with successful SUD treatment. To prevent misdiagnosis, it is important to follow-up and continue to monitor symptoms. Within adult inpatient contexts and custodial environments, it is possible to observe individuals over a prolonged period (24/7) and record degree of restlessness, inattentiveness, impulsiveness, poor emotional regulation, and problems with self-organization. Within community settings it is similarly important to be aware of behavioral observations during appointments, although quality of information may be comparatively limited due to the environmental constraints.
Pharmacological treatment: NICE guidelines suggest that appropriately qualified healthcare professionals can, with adequate training, acquire the necessary knowledge of ADHD to support assessment and/or treatment[135]. However, the experiences of the consensus group were that in the United Kingdom some healthcare practitioners with the appropriate skills to prescribe are prevented from doing so by local commissioning arrangements and guidelines[97]. Constraining prescribing to scarce and over-stretched specialist services is unnecessarily limiting and does not reflect the range of services involved in the care of individuals with concurrent ADHD and SUD. In accordance with NICE guidelines, the consensus group agreed that expanding local commissioning parameters to allow prescribing more widely would streamline care. In turn this would help individuals to access the support they need and reduce clinical burden on specialist services, allowing them to manage more complex cases.
Some practitioners outside ADHD specialist services may be concerned about assuming responsibility for prescribing ADHD medication. For example, primary care practitioners have voiced concerns about stimulants being ‘controlled drugs’ and the risk of potential misuse and diversion[136] (see previous section on pharmacological treatment in the community and Figure 2 which discusses the pharmacokinetics of stimulant medication that refute this perspective). Facilitating confidence in prescribing was considered crucial with specialist SUD services deemed to have a role in providing readily available specialist advice and guidance via remote clinics (telephone or online). This was considered particularly important for this population where complexity issues with poly-pharmacy are likely to be encountered. Research suggests that clear protocols and clearer advice from specialist services may help to change some hesitant practitioners’ views on prescribing[137]. The effectiveness of integrated care between primary care and specialist services has been demonstrated in other conditions (e.g. heart failure). This has shown to be associated with improved coordination between services, General practitioners (GPs) feel more confident in supporting patients, specialist services receiving more detailed feedback from primary care, and patients receiving more streamlined and holistic care[138].
When considering prescribing pharmacological treatments for this population, discussions centered on risk assessment regarding compliance and safety. In clinical practice this must be considered on an individual case by case basis (rather than categorically), and a decision made following an individual risk-benefit analysis which should be documented. Consensus group members agreed that active users of substances should still be offered pharmacological treatment if shown to be motivated to change and engaged, subject to appropriate risk assessments. Contraindications to stimulant pharmacotherapy may include current abuse of prescription stimulants or a clear indication that the medication would be sold or diverted. In addition there may be concerns regarding cardiovascular safety. Factors such as prior history of misusing stimulant medication and overall clinical stability should be considered. Practitioners should give appropriate weight to the efficacy of stimulant medication when balancing concerns regarding risk of misuse or diversion.
When considering concerns regarding misuse or diversion, the overarching opinion was that long-acting forms of stimulant medication should be prescribed. Despite lowered risk, it nevertheless remains important to be vigilant of any signs of misuse or diversion. Signs which may indicate possible misuse or diversion include: A repeated pattern of requests to replace alleged missing or lost prescriptions; requests for dose increases (not clinically indicated); early re-ordering of prescriptions; demands for immediate release preparations or claims that long-acting prescriptions are not effective; and symptoms associated with heavier use or intoxication[89]. Individualized risk assessment should incorporate clinical management; careful monitoring is likely to detect non-therapeutic use of stimulant medication, enabling treatment plans to be modified appropriately.
Supervised consumption and interval dispensing was recommended in inpatient and custodial settings as options available to minimize risk. These should correspond with dispensing arrangements for prescribed methadone (commonly at weekly or six times per week dispensing frequencies). Consensus group members also noted that in environments which enable supervised consumption, lisdexamfetamine (a long-acting prodrug formulation) may be preferred as it can be dissolved in a drink, limiting potential for misuse or diversion. Furthermore, lisdexamfetamine has to be hydrolyzed by red blood cells to work. This means that when ingested by other routes (e.g., intravenously or intranasally), the abuse potential is significantly limited. Oral and intravenous studies have shown no differences in subjective effects, likeability or blood pressure[53].
It was agreed that emphasis should be placed on adherence to the prescribed medication regimen which will facilitate optimal response. Individuals should be discouraged from binge using substances due to increased toxicity.
The consensus group highlighted the importance of ensuring that the person is part of the treatment planning process. They should feel that treatment is their choice rather than feeling it has been imposed. Educating individuals about the available treatment options including benefits and risks was considered important in helping them to develop a stake in the treatment.
Psychological interventions: Psychological treatment should address the specific difficulties experienced by adults with comorbid ADHD and SUD[139]. This involves using the same interventions discussed previously, including MI, formulation, psychoeducation, CBT, and relapse prevention approaches. The focus of treatment should include emotional liability/dysregulation, education and employment problems, interpersonal difficulties and development of prosocial competence, self-harm, dysfunctional coping strategies, and comorbid conditions such as anxiety and depression.
Psychological interventions are likely only to be effective following detoxification (i.e., the individual no longer needs pharmacological treatment for withdrawal symptoms) and once the individual is stabilized[59,110]. Longer psychological support and treatment may be required for those who use opiates. It was noted that it is not uncommon for service-users to lack support of family members and/or friends due to strained relationships; these individuals may require enhanced supportive scaffolding from healthcare and service-user services.
Multi-agency interventions
Individuals with both ADHD and SUD present with complex problems and often inter-agency working is needed for the successful provision of care.
Multi-agency interventions for young people: Young people and adults with concurrent ADHD and SU/SUD may require access to coordinated ongoing support from a wide variety of agencies. Yet in the United Kingdom, there are local and regional idiosyncrasies in referral and treatment pathways for young people with ADHD that can make it difficult to access care. Some GPs are unable to refer young people suspected of having ADHD directly for an ADHD assessment. For individuals with coexisting SU/SUD (who may be or who say they are self-medicating) the problem may be exacerbated. Referrals may be managed through schools but in some cases before this can take place, parents/caregivers must complete a parenting program. If then deemed appropriate by the school, a referral for an ADHD assessment can be made. Consensus group members acknowledged that some parents who themselves have ADHD, possibly undiagnosed, (heritability of ADHD is reported to range between 70-80%[108]) may have difficulties completing a parenting program. There are potential issues with schools being gatekeepers, particularly for those with ADHD and SU, as the focus may be on the SU. As a result of this, vulnerable young people do not receive the support and/or reasonable adjustments they need (and are entitled to) in order to optimize learning and development in educational settings. This may be further complicated by the mediating role of conduct disorder[64] with young people drifting into an antisocial peer group where substance misuse is common.
Young people with ADHD are at increased risk of being suspended or expelled and dropping out of school[140]. This may be exacerbated for those with SU. If ADHD is unrecognized and undiagnosed, the possibility that these individuals may be attempting to self-medicate (deliberately or unwittingly) may not be considered. All schools should have a drugs policy establishing the ways the school will deal with drugs on school property. This needs to balance the needs of the pupils with the wider school community. In some schools this involves the establishment of a drugs contract which aims to act as a deterrent and incentive to healthy habits and decision-making. The contract is signed by the pupil and their parents or carers on a voluntary basis. Typically, the contract includes a random drug testing regime and sets prescribed sanctions for default from the contract. However, this may present a dilemma for the pupil and parents/carers regarding consent and/or ambivalence over their level of support and co-operation with its implementation.
Community social interventions (e.g. such as Premier League Kicks[141] and Oasis Charitable Trust[142]) have an important role in supporting vulnerable individuals, including those with SU problems. Individuals should be signposted to services which can provide routes into education, training, employment, and steer young people away from a harmful trajectory.
Multi-agency interventions for adults: ADHD in adulthood is associated with work-related problems including impaired work performance and difficulties gaining and maintaining jobs[104]. The impairments associated with ADHD indicate that it should be regarded as a disability under the United Kingdom Equality Act 2010[143], affording individuals with certain rights and access to services. Individuals with ADHD may be entitled to reasonable adjustments in the workplace. Reasonable adjustments are assessed and provided on an individual basis. Some examples of reasonable adjustments include alterations to the workspace to reduce distractions in the environment, work schedule changes, frequent breaks, and use of technology assistance. Individuals may benefit from support in disclosing their ADHD diagnosis, particularly when they experience fear regarding occupational stigma.
However, commencing and sustaining new patterns of behaviour in an occupational setting can be difficult. From the experience of the consensus group, work-related problems may result in individuals using substances as a coping strategy which can further compound workplace difficulties. This is particularly relevant for people with ADHD who have executive functioning difficulties in planning, organizing, initiating, and completing tasks[107].
Relationships can be a useful ‘vehicle for change’ to help with this challenge; for example, a mentor or ‘buddy’ in the workplace can make it easier to facilitate completion of tasks. This principle is in Alcoholics and Narcotics Anonymous programs, where individuals are partnered with a sponsor who can offer help and guidance and provide accountability. Individuals should be sign-posted to formal groups of this nature for support with their treatment goals. In the United Kingdom, individuals may also benefit from a referral to social prescribing services. Social prescribing link workers adopt a holistic approach to wellbeing and can connect individuals to community groups and statutory services for both practical and emotional support.
The consensus group discussed anecdotal accounts of clinicians being asked to attend ‘team around the family’ meetings. This arises when concerns have been raised by other key professionals involved in the care of the family, resulting in clinicians being asked to complete parenting assessments. The consensus group experience was that these requests relate to a lack of awareness and stigma associated with ADHD, and this is further compounded when SU/SUD is present. This led to discussions where it was agreed that ADHD should not be considered a diagnosis that debars individuals from parenting (although severe and/or chronic substance dependency might).
Criminal justice system (CJS): ADHD and comorbid SU/SUD may increase risk that people will have contact with the CJS[144]. Research suggests that ADHD is likely to adversely impact an individual’s pathway through the CJS, leading to further negative sanctions[145]. The consensus group noted that this may be particularly relevant for community treatment options, such as the Community Sentence Treatment Requirement (CSTR) program (available in England). Where a CSTR service operates, it gives magistrates and judges a sentencing option, whereby a community sentence with one or a combination of three treatment requirements can be applied: drug rehabilitation requirements (DRRs), alcohol treatment requirements (ATRs), and/or mental health treatment requirements[146]. From consensus group members’ clinical experiences, individuals with ADHD may find it difficult to comply with DRRs and ATRs. This may result in individuals being in breach of requirements and in some cases lead to incarceration. Non-compliance with community options may be associated with symptoms of ADHD (e.g., forgetfulness), but this may be disregarded if it is perceived that ADHD symptoms and resultant impairments in functioning represent ‘bad behavior’ rather than unmet needs[146]. A National Neurodiversity Lead for CSTRs has been in place, increasing awareness of ADHD and other neurodevelopmental conditions, and has demonstrated examples of good practice for reasonable adjustments which would be of value more broadly across the CJS.
It is important to ensure communication between in-reach and out-reach healthcare services working across CJS services, and improvement in the flow of medical information across these services is likely to enhance safe and effective care for those with comorbid ADHD and SU/SUD.
DISCUSSION
The co-occurrence of ADHD and SU/SUD is common. The presence of both conditions exacerbates difficulties greater than that of either condition alone and is associated with reduced treatment effectiveness. The identification and assessment of ADHD and SU/SUD is complicated not only by overlapping symptoms across the two conditions but by other highly comorbid conditions. Given the high prevalence of ADHD and SU/SUD comorbidity, the consensus highlighted that those working in SUD services should be vigilant to ADHD as a possible comorbid diagnosis, and those working in ADHD services should be vigilant to signs of SU/SUD. Where ADHD or SU/SUD is suspected, assessment should be conducted by practitioners experienced in differential diagnosis. There is a risk of diagnostic overshadowing where practitioners are not well-versed in neurodevelopmental disorders, and vice versa, SU/SUD.
The use of psychostimulant medications in the treatment of concurrent ADHD and SU/SUD is complex. There is no published evidence of abuse of sustained release preparations, but caution is advisable when prescribing immediate release stimulant preparations[88]. This is not because appropriate use can give a high, but because immediate release stimulants are more likely to be crushed to a powder and snorted or used intravenously. Early treatment of ADHD may protect against later SU/SUD and can be useful in reducing ADHD symptoms without worsening pre-existing SU/SUD. Practitioners are encouraged to pharmacologically treat both ADHD and SU/SUD simultaneously, where practicable.
A multi-modal approach combining pharmacological treatment with psychological interventions is recommended, commensurate with studies which suggest that psychological therapy may be a useful strategy to treat SU among those with ADHD. Further research in this area is needed. Psychological interventions should adopt a transdiagnostic approach, targeting difficulties common to both ADHD and SU/SUD and should be adapted to meet the biopsychosocial needs and demands of the person.
Consensus meeting discussions continually highlighted existing inter-service barriers and fragmentation of care. In the United Kingdom, recent legislation has established integrated care systems which are partnerships that bring together local health and care organizations with the aim of providing better coordinated care to meet the needs of the people who live in the area. The consensus group stressed a need for re-evaluation of commissioning arrangements and pathways for those with coexisting ADHD and SU/SUD, offering opportunities for joint working and shared care, in turn resulting in better continuity of care.
Transition planning was considered a primary focus with group members noting that, with increasing age, biopsychosocial demands tend to increase whilst support declines. There is a stark notion that individuals ‘fall off a cliff’ when they turn 18. An emphasis on preventing drop out from services, especially when transitioning from child to adult services, may help prevent onset and/or escalation of SU. The provision of consistent, coordinated care over this important transitional period is vital. Developmentally appropriate healthcare provides an individualized integrated care approach which is responsive to the multiple and changing impacts of health conditions upon the individual and their goals[103]. Whilst currently primarily adopted for those with long-term health conditions, it is recommended more widely, including those with concurrent ADHD and SU/SUD.
Empowering general services was deemed vital. Training is an important step to ensure adequate knowledge and competencies for services to support monitoring and continuation of treatment under shared care arrangements. Access to foundational awareness training in ADHD (that is equivalent to the current provision of autism awareness training) was recommended. Ideally, this should be delivered to healthcare professionals including those in third sector mental health services, educational professionals, employment services, CJS workers, police, housing and homeless services, social workers, youth center workers, and GPs. It was also suggested that a similar level of awareness across services may be required for SUD.
It is hoped that this consensus can be used by practitioners across a range of disciplines to support the effective identification and treatment of individuals with concurrent ADHD and SU/SUD in order to achieve optimal outcomes. The consensus recommendations for practice are summarized in Table 6.
Table 6.
Overview and practice recommendations
|
Recommendations
|
| Identification and assessment |
| Due to the level of complexity, assessments should only be conducted by qualified healthcare professionals with appropriate training and expertise in assessing dual disorders. This may require foundation training in ADHD and SUD across the two services and/or assessments being made jointly by experts in different areas |
| It is critical to examine the temporal course of ADHD-like symptoms and SU/SUD. A focus on drug and alcohol-free periods may help with differential diagnosis |
| Symptoms of ADHD and SU/SUD may be masked for many reasons including overlapping of symptoms between disorders, other comorbid conditions (e.g., personality disorder, bipolar disorder, anxiety, depression), and the individual may have developed compensatory strategies |
| Substances may have a countereffect for individuals with ADHD. Where individuals appear to be functioning better under SU, this may indicate possible underlying ADHD |
| Assessors should be aware that for those in institutional settings, current presentation may be misleading due to structure and routine minimising deficits in functioning |
| A comprehensive assessment should include a full developmental history, mental health history and current mental state examination, medical history, educational/employment history, social history, cognitive executive functioning difficulties, family history of ADHD and SU/SUD, in addition to other psychiatric and neurological problems. Perceived sex differences in presentation should be considered which may result in missed or misdiagnosis |
| Rating scales are not diagnostic. If used to screen, services should not rigidly adhere to cut-offs as this is likely to lead to high proportion of false positives and negatives |
| Young people presenting with an initial diagnosis of ADHD should be continually monitored through development for SU/SUD, given high rates of ADHD and SU/SUD comorbidity |
| ADHD assessment should not be conducted when an individual is under the influence of substances at the time of the assessment and/or when in a stage of withdrawal. Ideally, ADHD clinical evaluations are best conducted during a period of sustained abstinence or following detoxification or stabilization |
| When conducting the assessment with young people, it is important to consider how parents/caregivers are involved commensurate with the wishes and needs of the young person |
| The assessment may need to address additional physical, criminogenic, and safeguarding risks associated with SU. The person should be informed of the confidentiality of information shared and circumstances in which this will be breached |
| There are high rates of comorbidity associated with both ADHD and SU/SUD; the assessment should look to exclude other conditions that could better explain presenting symptoms |
| Follow-up and continued monitoring of symptoms is advised to prevent misdiagnosis |
| Practitioners should be aware of the risk of diagnostic overshadowing, which may require improved training in mental health services |
| Whenever possible, collateral information should be obtained from independent sources. For those with SUD, this may be difficult due to poor/strained relationships; the absence of collateral information should not unduly delay or prevent assessment |
| Pharmacological treatment |
| A nihilistic attitude to pharmacological treatment is not appropriate; active users of substances should be offered ADHD medication, subject to appropriate risk assessment |
| Long-acting stimulant preparations are recommended as first line treatment. Generally non-stimulants should be reserved as a second line due to relative effectiveness and concerns regarding non-compliance |
| Short-acting stimulant preparations are advised for a very circumscribed group (e.g., in contexts where there is possibility for supervised consumption) |
| Abstinence of substance use is not necessary for individuals to benefit from ADHD medication, though SU should ideally be reduced/stabilized before initiating ADHD medication |
| For those with primary alcohol use, atomoxetine may be of specific consideration in light of research indicating effectiveness in reducing alcohol cravings |
| Prescribing needs to consider interactions between ADHD medication and other medications for comorbid conditions, where applicable |
| Practitioners should be aware of personal and family history of cardiovascular conditions. Where there are concerns regarding cardiovascular risk, a cardiologist should be consulted prior to prescribing stimulant medication |
| Heart rate, blood pressure and weight should be measured before initiating medications and routinely monitored during treatment; titration should be slow. Include height monitoring in CYP |
| Individuals with SU/SUD at time of stabilization should be considered for prioritization for assessment in ADHD services |
| Provision of developmentally appropriate healthcare (DAH) within services may be of benefit |
| Commissioning arrangements should permit prescribing beyond specialist services |
| In spite of lowered risk of misuse or diversion with long-acting stimulant preparations, practitioners should still be vigilant of signs including pattern of losing prescriptions, early re-ordering of prescriptions, demands for immediate release preparations or claims that long-acting prescriptions are not effective, and symptoms associated with heavier use or intoxication |
| Supervised consumption and interval dispensing should be considered as options to minimize risk. ADHD medication dispensing arrangements should correspond with prescribed methadone, where applicable |
| Psychoeducation on pharmacological treatment may help to improve adherence and engagement |
| Psychological treatment |
| Where neuropsychological testing has been conducted, the strengths and weaknesses profile should be used to inform adaptations to the treatment process |
| Email/text reminders from service should be used to reduce likelihood of non-attendance. Sessions may require increased frequency of sessions, with greater structure, being delivered at a slower pace in shorter duration and/or including mid-session breaks, with repetition and greater use of supplementary visual material |
| Individuals should be provided with a notebook which serves as a record of strategies learnt. This should be completed in the person’s own writing to facilitate ‘ownership’, responsibility, and action |
| Motivational interviewing (MI) is more suitable for older adolescents and adults and is particularly helpful in the initial motivational stages (precontemplation, contemplation, preparation) |
| Practitioners need to be aware of the individual’s current motivational stage and should monitor interest to engage in treatment throughout, adapting treatment interventions as necessary |
| Functional behavioral analysis should be used to help identify constructive or functional alternatives to substance use |
| Psychoeducation should be provided as an important part of the treatment process and should be returned to at regular intervals over the course of treatment, including key points of service and/or personal transition |
| Psychoeducational programs should differ for children, adolescents, and adult populations in relation to changing biopsychosocial needs and demands. They should be provided to both the young person and their family. Topics should include basic information about ADHD, the purpose and benefits of medication and non-pharmacological interventions, long-term consequences of SU (including legal consequences, misconceptions around medication increasing the likelihood of addiction, how and where to access local support |
| Societal connotations about SU can be disparaging; parent/carer group interventions provide a supportive environment where they can share experiences (common humanity) and assuage feelings of shame |
| Clear and realistic goals should be collaboratively identified and monitored using the SMART framework |
| Individuals should be invited to use self-reinforcement techniques (which hold personal meaning) as reminders of their goals |
| Reward systems should be incorporated into treatment to motivate new constructive behaviour |
| Cognitive behavioral therapy interventions should be adapted commensurate with cognitive and emotional functioning; there may need to be more of a focus on behavioral-oriented interventions when working with young people |
| Young people and adults may benefit from the R&R2ADHD program which adopts a transdiagnostic approach targeting difficulties common to both ADHD and SU/SUD |
| Psychological treatment should include a relapse and prevention action plan, with follow-up ‘booster’ sessions provided, as needed |
| Multiagency interventions |
| Signposting to services which provide routes into education, training, employment, can help to steer people away from a harmful trajectory and prevent relapse |
| Practitioners should be aware that individuals may lack support networks due to strained interpersonal relationships, requiring enhanced supportive scaffolding from healthcare and service-user services |
| Schools should have a drugs policy establishing clearly how schools will deal with SU, where appropriate, this may include a drugs contract. If deemed appropriate, schools should also screen and refer young people for assessment of ADHD |
| Educational and employment support services should be aware of potential challenges for individuals. Reasonable adjustments to education/workplace may be required to help individuals manage demands and prevent harmful trajectories |
| Healthcare services to make reasonable adjustments through offering combined appointments |
| Individuals to be sign-posted to alcoholics/drug addicts anonymous for support with treatment goals |
| Referral to social prescribing services may be helpful in connecting people with community groups and statutory services for practical and emotional support |
| Transition planning between child and adult services should commence early and be a primary focus |
| Services should not work in silos. Foundational awareness training in ADHD and SU/SUD (as individual and comorbid conditions) should be provided to key professionals across health and social care, education and justice services and third sector organizations |
ADHD: Attention-deficit/hyperactivity disorder; SU: Substance use; SUD: Substance use disorder.
We need early and accurate identification and treatment of SU/SUD among young people in ADHD services, and vice versa. The delivery of appropriate interventions is likely to facilitate promising rather than harmful trajectories, leading to better outcomes at both individual and community levels. In the United Kingdom, systemic changes in commissioning arrangements, service delivery, workforce education and training are necessary if we are to effectively meet the needs of this complex group.
CONCLUSION
This review of the relevant current literature, combined with the diligence of the consensus group, has identified the most salient vulnerabilities of individuals with combined ADHD and SU. Furthermore, the consensus statement provides a structure within which the pertinent vulnerabilities can be best identified, treated, and managed by clinical and multi-agency interventions. The statement provides an important readily accessible contribution to the literature for practice, research, and evaluation of treatment effectiveness for young people and adults with combined ADHD and SU/SUD.
Footnotes
Conflict-of-interest statement: Young S, Abbasian C, Cubbin S, Branney P, Colley B, Deeley Q, Hill P, Hollingdale J, Judge D, Lewis A, Mason P, Johnson J and Woodhouse E are affiliated with consultancy firms/private practices. Over the past five years Young S has received honoraria for consultancy and educational talks years from Janssen, Medice and Takeda. She is author of the ADHD Child Evaluation (ACE) and ACE+ for adults; and lead author of R&R2 for ADHD Youths and Adults. Hill P received honoraria for consultancy and educational talks from Takeda and Flynn Pharma. Cortese S declares honoraria and reimbursement for travel and accommodation expenses for lectures from the following non-profit associations: Association for Child and Adolescent Central Health (ACAMH), Canadian ADHD Alliance Resource (CADDRA), British Association of Pharmacology (BAP), and from Healthcare Convention for educational activity on ADHD. Mason P has received honoraria for consultancy and educational talks from Takeda, Flynn Pharma and Lily. Nutt D has received honoraria for educational talks from Takeda and Janssen. Lewis A has received honoraria for consultancy to the Association for Child & Adolescent Mental Health (ACAMH) and Takeda and for educational talks to Forensic Treatment Division, Ministry of Justice, Republic of Korea. Mukherjee R has received honoraria for consultancy and talks related to ADHD from Takeda, Flynn Pharma and Janssen. Johnson J has received honoraria for consultancy and educational talks for Flynn Pharma, Takeda and Janssen. The remaining authors (Gudjonsson GH, Cocallis K, Roberts J, Al-Attar Z, Robinson F) declare that the meeting was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: British Psychological Society, No. 71159; and Health and Care Professions Council, No. PYL22718.
Peer-review started: November 22, 2022
First decision: January 3, 2023
Article in press: March 14, 2023
Specialty type: Psychiatry
Country/Territory of origin: United Kingdom
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Hassel B, Norway; Ozsoy F, Turkey S-Editor: Gong ZM L-Editor: A P-Editor: Gong ZM
Contributor Information
Susan Young, Department of Psychology, Psychology Services Limited, Croydon CR9 7AE, United Kingdom; Department of Psychology, Reykjavik University, Reykjavik, Iceland. suzyyoung@aol.com.
Cyrus Abbasian, Psychiatry-UK Limited, Cornwall PL33 9ET, United Kingdom.
Zainab Al-Attar, Psychiatry-UK Limited, Cornwall PL33 9ET, United Kingdom.
Polly Branney, ADHD and Autism, Oxford ADHD & Autism Centre, Headington OX3 7BX, United Kingdom.
Bill Colley, CLC Consultancy, Dunkeld PH8 0AY, United Kingdom.
Samuele Cortese, Center for Innovation in Mental Health, School of Psychology, Faculty of Environmental and Life Sciences, University of Southampton, Southampton SO17 1BJ, United Kingdom.
Sally Cubbin, Adult ADHD, Adult ADHD Clinic Ltd, Oxford OX3 7RP, United Kingdom.
Quinton Deeley, Forensic and Neurodevelopmental Science, Institute of Psychiatry, Psychology & Neuroscience, King's College London Institute of Psychiatry, London SE5 8AF, United Kingdom.
Gisli Hannes Gudjonsson, Department of Psychology, Institute of Psychiatry, Psychology & Neuroscience, King's College London, London SE5 8AF, United Kingdom.
Peter Hill, Department of Psychiatry, University of London, London WC1E 7HU, United Kingdom.
Jack Hollingdale, Department of Psychology, Compass Psychology Services Ltd, London BR1 9DX, United Kingdom.
Steve Jenden, Birribi Ltd, Narberth SA67 7DU, United Kingdom.
Joe Johnson, Halton and Knowsley Adult ADHD Team, Merseycare NHS Foundation Trust, Winwick WA2 9WA, United Kingdom.
Deborah Judge, Birribi Ltd, Narberth SA67 7DU, United Kingdom.
Alexandra Lewis, Department of Psychiatry, Fulbourn Hospital, Cambridge CB21 5EF, United Kingdom.
Peter Mason, Department of Psychiatry, Dr Peter Mason ADHD & Psychiatry Services Limited, Liverpool L1 9AR, United Kingdom.
Raja Mukherjee, Adult Neurodevelopmental Service, Horizon House, Epsom KT17 4QJ, United Kingdom.
David Nutt, Department of Psychiatry, Imperial College London, London WS12 0NN, United Kingdom.
Jane Roberts, Service User Representative, Gloucestershire GL1 3NN, United Kingdom.
Fiona Robinson, Drug & Alcohol Services, Surrey & Borders Partnership Trust, Leatherhead KT22 7AD, United Kingdom.
Emma Woodhouse, Forensic and Neurodevelopmental Sciences, Institute of Psychiatry, Psychology & Neuroscience, King's College London, London SE5 8AF, United Kingdom.
Kelly Cocallis, Wansbeck General Hospital, Northumbria Healthcare NHS Foundation Trust, Ashington NE63 9JJ, United Kingdom.
References
- 1.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th Edition: DSM-5. American Psychiatric Publishing, 2013. [Google Scholar]
- 2.World Health Organization. International Statistical Classification of Diseases and Related Health Problems. 2019 [Accessed 7 March 2023] Available from: https://www.who.int/standards/classifications/classification-of-diseases .
- 3.Wilens TE, Faraone SV, Biederman J. Attention-deficit/hyperactivity disorder in adults. JAMA. 2004;292:619–623. doi: 10.1001/jama.292.5.619. [DOI] [PubMed] [Google Scholar]
- 4.Kaye S, Ramos-Quiroga JA, van de Glind G, Levin FR, Faraone SV, Allsop S, Degenhardt L, Moggi F, Barta C, Konstenius M, Franck J, Skutle A, Bu ET, Koeter MWJ, Demetrovics Z, Kapitány-Fövény M, Schoevers RA, van Emmerik-van Oortmerssen K, Carpentier PJ, Dom G, Verspreet S, Crunelle CL, Young JT, Carruthers S, Cassar J, Fatséas M, Auriacombe M, Johnson B, Dunn M, Slobodin O, van den Brink W. Persistence and Subtype Stability of ADHD Among Substance Use Disorder Treatment Seekers. J Atten Disord. 2019;23:1438–1453. doi: 10.1177/1087054716629217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thomas R, Sanders S, Doust J, Beller E, Glasziou P. Prevalence of attention-deficit/hyperactivity disorder: a systematic review and meta-analysis. Pediatrics. 2015;135:e994–1001. doi: 10.1542/peds.2014-3482. [DOI] [PubMed] [Google Scholar]
- 6.Polanczyk G, de Lima MS, Horta BL, Biederman J, Rohde LA. The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatry. 2007;164:942–948. doi: 10.1176/ajp.2007.164.6.942. [DOI] [PubMed] [Google Scholar]
- 7.Simon V, Czobor P, Bálint S, Mészáros A, Bitter I. Prevalence and correlates of adult attention-deficit hyperactivity disorder: meta-analysis. Br J Psychiatry. 2009;194:204–211. doi: 10.1192/bjp.bp.107.048827. [DOI] [PubMed] [Google Scholar]
- 8.Willcutt EG. The prevalence of DSM-IV attention-deficit/hyperactivity disorder: a meta-analytic review. Neurotherapeutics. 2012;9:490–499. doi: 10.1007/s13311-012-0135-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Galéra C, Cortese S, Orri M, Collet O, van der Waerden J, Melchior M, Boivin M, Tremblay RE, Côté SM. Medical conditions and Attention-Deficit/Hyperactivity Disorder symptoms from early childhood to adolescence. Mol Psychiatry. 2022;27:976–984. doi: 10.1038/s41380-021-01357-x. [DOI] [PubMed] [Google Scholar]
- 10.Arrondo G, Solmi M, Dragioti E, Eudave L, Ruiz-Goikoetxea M, Ciaurriz-Larraz AM, Magallon S, Carvalho AF, Cipriani A, Fusar-Poli P, Larsson H, Correll CU, Cortese S. Associations between mental and physical conditions in children and adolescents: An umbrella review. Neurosci Biobehav Rev. 2022;137:104662. doi: 10.1016/j.neubiorev.2022.104662. [DOI] [PubMed] [Google Scholar]
- 11.Påhlman M, Gillberg C, Himmelmann K. Autism and attention-deficit/hyperactivity disorder in children with cerebral palsy: high prevalence rates in a population-based study. Dev Med Child Neurol. 2021;63:320–327. doi: 10.1111/dmcn.14736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thapar A, Cooper M. Attention deficit hyperactivity disorder. Lancet. 2016;387:1240–1250. doi: 10.1016/S0140-6736(15)00238-X. [DOI] [PubMed] [Google Scholar]
- 13.Carpentier PJ, van Gogh MT, Knapen LJ, Buitelaar JK, De Jong CA. Influence of attention deficit hyperactivity disorder and conduct disorder on opioid dependence severity and psychiatric comorbidity in chronic methadone-maintained patients. Eur Addict Res. 2011;17:10–20. doi: 10.1159/000321259. [DOI] [PubMed] [Google Scholar]
- 14.Kooij SJ, Bejerot S, Blackwell A, Caci H, Casas-Brugué M, Carpentier PJ, Edvinsson D, Fayyad J, Foeken K, Fitzgerald M, Gaillac V, Ginsberg Y, Henry C, Krause J, Lensing MB, Manor I, Niederhofer H, Nunes-Filipe C, Ohlmeier MD, Oswald P, Pallanti S, Pehlivanidis A, Ramos-Quiroga JA, Rastam M, Ryffel-Rawak D, Stes S, Asherson P. European consensus statement on diagnosis and treatment of adult ADHD: The European Network Adult ADHD. BMC Psychiatry. 2010;10:67. doi: 10.1186/1471-244X-10-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dalsgaard S, Mortensen PB, Frydenberg M, Thomsen PH. ADHD, stimulant treatment in childhood and subsequent substance abuse in adulthood - a naturalistic long-term follow-up study. Addict Behav. 2014;39:325–328. doi: 10.1016/j.addbeh.2013.09.002. [DOI] [PubMed] [Google Scholar]
- 16.Sizoo B, van den Brink W, Koeter M, Gorissen van Eenige M, van Wijngaarden-Cremers P, van der Gaag RJ. Treatment seeking adults with autism or ADHD and co-morbid substance use disorder: prevalence, risk factors and functional disability. Drug Alcohol Depend. 2010;107:44–50. doi: 10.1016/j.drugalcdep.2009.09.003. [DOI] [PubMed] [Google Scholar]
- 17.Steinhausen HC, Bisgaard C. Substance use disorders in association with attention-deficit/hyperactivity disorder, co-morbid mental disorders, and medication in a nationwide sample. Eur Neuropsychopharmacol. 2014;24:232–241. doi: 10.1016/j.euroneuro.2013.11.003. [DOI] [PubMed] [Google Scholar]
- 18.Charach A, Yeung E, Climans T, Lillie E. Childhood attention-deficit/hyperactivity disorder and future substance use disorders: comparative meta-analyses. J Am Acad Child Adolesc Psychiatry. 2011;50:9–21. doi: 10.1016/j.jaac.2010.09.019. [DOI] [PubMed] [Google Scholar]
- 19.Lee SS, Humphreys KL, Flory K, Liu R, Glass K. Prospective association of childhood attention-deficit/hyperactivity disorder (ADHD) and substance use and abuse/dependence: a meta-analytic review. Clin Psychol Rev. 2011;31:328–341. doi: 10.1016/j.cpr.2011.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kaye S, Darke S, Torok M. Attention deficit hyperactivity disorder (ADHD) among illicit psychostimulant users: a hidden disorder? Addiction. 2013;108:923–931. doi: 10.1111/add.12086. [DOI] [PubMed] [Google Scholar]
- 21.Katzman MA, Bilkey TS, Chokka PR, Fallu A, Klassen LJ. Adult ADHD and comorbid disorders: clinical implications of a dimensional approach. BMC Psychiatry. 2017;17:302. doi: 10.1186/s12888-017-1463-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Martinez-Raga J, Szerman N, Knecht C, de Alvaro R. Attention deficit hyperactivity disorder and dual disorders. Educational needs for an underdiagnosed condition. Int J Adolesc Med Health. 2013;25:231–243. doi: 10.1515/ijamh-2013-0057. [DOI] [PubMed] [Google Scholar]
- 23.van Emmerik-van Oortmerssen K, van de Glind G, van den Brink W, Smit F, Crunelle CL, Swets M, Schoevers RA. Prevalence of attention-deficit hyperactivity disorder in substance use disorder patients: a meta-analysis and meta-regression analysis. Drug Alcohol Depend. 2012;122:11–19. doi: 10.1016/j.drugalcdep.2011.12.007. [DOI] [PubMed] [Google Scholar]
- 24.Huntley Z, Maltezos S, Williams C, Morinan A, Hammon A, Ball D, Marshall EJ, Keaney F, Young S, Bolton P, Glaser K, Howe-Forbes R, Kuntsi J, Xenitidis K, Murphy D, Asherson PJ. Rates of undiagnosed attention deficit hyperactivity disorder in London drug and alcohol detoxification units. BMC Psychiatry. 2012;12:223. doi: 10.1186/1471-244X-12-223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bechara A. Decision making, impulse control and loss of willpower to resist drugs: a neurocognitive perspective. Nat Neurosci. 2005;8:1458–1463. doi: 10.1038/nn1584. [DOI] [PubMed] [Google Scholar]
- 26.Fatséas M, Hurmic H, Serre F, Debrabant R, Daulouède JP, Denis C, Auriacombe M. Addiction severity pattern associated with adult and childhood Attention Deficit Hyperactivity Disorder (ADHD) in patients with addictions. Psychiatry Res. 2016;246:656–662. doi: 10.1016/j.psychres.2016.10.071. [DOI] [PubMed] [Google Scholar]
- 27.Moura HF, Faller S, Benzano D, Szobot C, von Diemen L, Stolf AR, Souza-Formigoni ML, Cruz MS, Brasiliano S, Pechansky F, Kessler FH. The effects of ADHD in adult substance abusers. J Addict Dis. 2013;32:252–262. doi: 10.1080/10550887.2013.824359. [DOI] [PubMed] [Google Scholar]
- 28.Molina BSG, Howard AL, Swanson JM, Stehli A, Mitchell JT, Kennedy TM, Epstein JN, Arnold LE, Hechtman L, Vitiello B, Hoza B. Substance use through adolescence into early adulthood after childhood-diagnosed ADHD: findings from the MTA longitudinal study. J Child Psychol Psychiatry. 2018;59:692–702. doi: 10.1111/jcpp.12855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Young JT, Carruthers S, Kaye S, Allsop S, Gilsenan J, Degenhardt L, van de Glind G, van den Brink W, Preen D. Comorbid attention deficit hyperactivity disorder and substance use disorder complexity and chronicity in treatment-seeking adults. Drug Alcohol Rev. 2015;34:683–693. doi: 10.1111/dar.12249. [DOI] [PubMed] [Google Scholar]
- 30.Levin FR, Evans SM, Vosburg SK, Horton T, Brooks D, Ng J. Impact of attention-deficit hyperactivity disorder and other psychopathology on treatment retention among cocaine abusers in a therapeutic community. Addict Behav. 2004;29:1875–1882. doi: 10.1016/j.addbeh.2004.03.041. [DOI] [PubMed] [Google Scholar]
- 31.Kronenberg LM, Goossens PJ, van Etten DM, van Achterberg T, van den Brink W. Need for care and life satisfaction in adult substance use disorder patients with and without attention deficit hyperactivity disorder (ADHD) or autism spectrum disorder (ASD) Perspect Psychiatr Care. 2015;51:4–15. doi: 10.1111/ppc.12056. [DOI] [PubMed] [Google Scholar]
- 32.van Emmerik-van Oortmerssen K, van de Glind G, Koeter MW, Allsop S, Auriacombe M, Barta C, Bu ET, Burren Y, Carpentier PJ, Carruthers S, Casas M, Demetrovics Z, Dom G, Faraone SV, Fatseas M, Franck J, Johnson B, Kapitány-Fövény M, Kaye S, Konstenius M, Levin FR, Moggi F, Møller M, Ramos-Quiroga JA, Schillinger A, Skutle A, Verspreet S IASP research group, van den Brink W, Schoevers RA. Psychiatric comorbidity in treatment-seeking substance use disorder patients with and without attention deficit hyperactivity disorder: results of the IASP study. Addiction. 2014;109:262–272. doi: 10.1111/add.12370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Einarsson E, Sigurdsson JF, Gudjonsson GH, Newton AK, Bragason OO. Screening for attention-deficit hyperactivity disorder and co-morbid mental disorders among prison inmates. Nord J Psychiatry. 2009;63:361–367. doi: 10.1080/08039480902759184. [DOI] [PubMed] [Google Scholar]
- 34.Kousha M, Shahrivar Z, Alaghband-Rad J. Substance use disorder and ADHD: is ADHD a particularly "specific" risk factor? J Atten Disord. 2012;16:325–332. doi: 10.1177/1087054710387265. [DOI] [PubMed] [Google Scholar]
- 35.Dalsgaard S, Østergaard SD, Leckman JF, Mortensen PB, Pedersen MG. Mortality in children, adolescents, and adults with attention deficit hyperactivity disorder: a nationwide cohort study. Lancet. 2015;385:2190–2196. doi: 10.1016/S0140-6736(14)61684-6. [DOI] [PubMed] [Google Scholar]
- 36.Wilens TE, Morrison NR. Substance-use disorders in adolescents and adults with ADHD: focus on treatment. Neuropsychiatry (London) 2012;2:301–312. doi: 10.2217/npy.12.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tamm L, Trello-Rishel K, Riggs P, Nakonezny PA, Acosta M, Bailey G, Winhusen T. Predictors of treatment response in adolescents with comorbid substance use disorder and attention-deficit/hyperactivity disorder. J Subst Abuse Treat. 2013;44:224–230. doi: 10.1016/j.jsat.2012.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yüce Akalın B, Bilici R. The Effect of Attention Deficit and Hyperactivity Disorder on Treatment Compliance in Individuals Undergoing Probation Addiction Program Treatment. Alpha Psychiatry. 2022;23:33–39. doi: 10.5152/alphapsychiatry.2021.21304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cunill R, Castells X, Tobias A, Capellà D. Pharmacological treatment of attention deficit hyperactivity disorder with co-morbid drug dependence. J Psychopharmacol. 2015;29:15–23. doi: 10.1177/0269881114544777. [DOI] [PubMed] [Google Scholar]
- 40.Wilens TE, Faraone SV, Biederman J, Gunawardene S. Does stimulant therapy of attention-deficit/hyperactivity disorder beget later substance abuse? Pediatrics. 2003;111:179–185. doi: 10.1542/peds.111.1.179. [DOI] [PubMed] [Google Scholar]
- 41.Groenman AP, Schweren LJS, Weeda W, Luman M, Noordermeer SDS, Heslenfeld DJ, Franke B, Faraone SV, Rommelse N, Hartman CA, Hoekstra PJ, Buitelaar J, Oosterlaan J. Stimulant treatment profiles predicting co-occurring substance use disorders in individuals with attention-deficit/hyperactivity disorder. Eur Child Adolesc Psychiatry. 2019;28:1213–1222. doi: 10.1007/s00787-019-01283-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Quinn PD, Chang Z, Hur K, Gibbons RD, Lahey BB, Rickert ME, Sjölander A, Lichtenstein P, Larsson H, D'Onofrio BM. ADHD Medication and Substance-Related Problems. Am J Psychiatry. 2017;174:877–885. doi: 10.1176/appi.ajp.2017.16060686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Humphreys KL, Eng T, Lee SS. Stimulant medication and substance use outcomes: a meta-analysis. JAMA Psychiatry. 2013;70:740–749. doi: 10.1001/jamapsychiatry.2013.1273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chang Z, Ghirardi L, Quinn PD, Asherson P, D'Onofrio BM, Larsson H. Risks and Benefits of Attention-Deficit/Hyperactivity Disorder Medication on Behavioral and Neuropsychiatric Outcomes: A Qualitative Review of Pharmacoepidemiology Studies Using Linked Prescription Databases. Biol Psychiatry. 2019;86:335–343. doi: 10.1016/j.biopsych.2019.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Fluyau D, Revadigar N, Pierre CG. Systematic Review and Meta-Analysis: Treatment of Substance Use Disorder in Attention Deficit Hyperactivity Disorder. Am J Addict. 2021;30:110–121. doi: 10.1111/ajad.13133. [DOI] [PubMed] [Google Scholar]
- 46.Carpentier PJ, Levin FR. Pharmacological Treatment of ADHD in Addicted Patients: What Does the Literature Tell Us? Harv Rev Psychiatry. 2017;25:50–64. doi: 10.1097/HRP.0000000000000122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Riggs PD, Winhusen T, Davies RD, Leimberger JD, Mikulich-Gilbertson S, Klein C, Macdonald M, Lohman M, Bailey GL, Haynes L, Jaffee WB, Haminton N, Hodgkins C, Whitmore E, Trello-Rishel K, Tamm L, Acosta MC, Royer-Malvestuto C, Subramaniam G, Fishman M, Holmes BW, Kaye ME, Vargo MA, Woody GE, Nunes EV, Liu D. Randomized controlled trial of osmotic-release methylphenidate with cognitive-behavioral therapy in adolescents with attention-deficit/hyperactivity disorder and substance use disorders. J Am Acad Child Adolesc Psychiatry. 2011;50:903–914. doi: 10.1016/j.jaac.2011.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Young S, Woodhouse E. Assessment and treatment of substance use in adults with ADHD: a psychological approach. J Neural Transm (Vienna) 2021;128:1099–1108. doi: 10.1007/s00702-020-02277-w. [DOI] [PubMed] [Google Scholar]
- 49.Chan E, Fogler JM, Hammerness PG. Treatment of Attention-Deficit/Hyperactivity Disorder in Adolescents: A Systematic Review. JAMA. 2016;315:1997–2008. doi: 10.1001/jama.2016.5453. [DOI] [PubMed] [Google Scholar]
- 50.Sibley MH, Kuriyan AB, Evans SW, Waxmonsky JG, Smith BH. Pharmacological and psychosocial treatments for adolescents with ADHD: an updated systematic review of the literature. Clin Psychol Rev. 2014;34:218–232. doi: 10.1016/j.cpr.2014.02.001. [DOI] [PubMed] [Google Scholar]
- 51.Magon R, Müller U. ADHD with comorbid substance use disorder: review of treatment. Adv Psychiatr Treat. 2012;18:436–446. [Google Scholar]
- 52.Luo SX, Levin FR. Towards Precision Addiction Treatment: New Findings in Co-morbid Substance Use and Attention-Deficit Hyperactivity Disorders. Curr Psychiatry Rep. 2017;19:14. doi: 10.1007/s11920-017-0769-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Johnson J, Morris S, George S. Managing Comorbid Attention Deficit Hyperactivity Disorder (ADHD) in Adults with Substance Use Disorder (SUD): What the Addiction Specialist Needs to Know. Addict Disord Their Treat. 2020;20:181–188. [Google Scholar]
- 54.Obermeit LC, Cattie JE, Bolden KA, Marquine MJ, Morgan EE, Franklin DR Jr, Atkinson JH, Grant I, Woods SP Translational Methamphetamine AIDS Research Center (TMARC) Group. Attention-deficit/hyperactivity disorder among chronic methamphetamine users: frequency, persistence, and adverse effects on everyday functioning. Addict Behav. 2013;38:2874–2878. doi: 10.1016/j.addbeh.2013.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Oliva F, Mangiapane C, Nibbio G, Berchialla P, Colombi N, Vigna-Taglianti FD. Prevalence of cocaine use and cocaine use disorder among adult patients with attention-deficit/hyperactivity disorder: A systematic review and meta-analysis. J Psychiatr Res. 2021;143:587–598. doi: 10.1016/j.jpsychires.2020.11.021. [DOI] [PubMed] [Google Scholar]
- 56.Lembke A. Time to abandon the self-medication hypothesis in patients with psychiatric disorders. Am J Drug Alcohol Abuse. 2012;38:524–529. doi: 10.3109/00952990.2012.694532. [DOI] [PubMed] [Google Scholar]
- 57.Hall DH, Queener JE. Self-medication hypothesis of substance use: testing Khantzian's updated theory. J Psychoactive Drugs. 2007;39:151–158. doi: 10.1080/02791072.2007.10399873. [DOI] [PubMed] [Google Scholar]
- 58.Wilens TE, Adamson J, Sgambati S, Whitley J, Santry A, Monuteaux MC, Biederman J. Do individuals with ADHD self-medicate with cigarettes and substances of abuse? Am J Addict. 2007;16 Suppl 1:14–21; quiz 22. doi: 10.1080/10550490601082742. [DOI] [PubMed] [Google Scholar]
- 59.Zulauf CA, Sprich SE, Safren SA, Wilens TE. The complicated relationship between attention deficit/hyperactivity disorder and substance use disorders. Curr Psychiatry Rep. 2014;16:436. doi: 10.1007/s11920-013-0436-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gehricke JG, Whalen CK, Jamner LD, Wigal TL, Steinhoff K. The reinforcing effects of nicotine and stimulant medication in the everyday lives of adult smokers with ADHD: A preliminary examination. Nicotine Tob Res. 2006;8:37–47. doi: 10.1080/14622200500431619. [DOI] [PubMed] [Google Scholar]
- 61.Young S, Sedgwick O. Attention deficit hyperactivity disorder and substance misuse: an evaluation of causal hypotheses and treatment considerations. Expert Rev Neurother. 2015;15:1005–1014. doi: 10.1586/14737175.2015.1059756. [DOI] [PubMed] [Google Scholar]
- 62.Young S, González RA, Wolff K, Xenitidis K, Mutch L, Malet-Lambert I, Gudjonsson GH. Substance and Alcohol Misuse, Drug Pathways, and Offending Behaviors in Association With ADHD in Prison Inmates. J Atten Disord. 2020;24:1905–1913. doi: 10.1177/1087054716688532. [DOI] [PubMed] [Google Scholar]
- 63.Ottosen C, Petersen L, Larsen JT, Dalsgaard S. Gender Differences in Associations Between Attention-Deficit/Hyperactivity Disorder and Substance Use Disorder. J Am Acad Child Adolesc Psychiatry. 2016;55:227–34.e4. doi: 10.1016/j.jaac.2015.12.010. [DOI] [PubMed] [Google Scholar]
- 64.Serra-Pinheiro MA, Coutinho ES, Souza IS, Pinna C, Fortes D, Araújo C, Szobot CM, Rohde LA, Mattos P. Is ADHD a risk factor independent of conduct disorder for illicit substance use? J Atten Disord. 2013;17:459–469. doi: 10.1177/1087054711435362. [DOI] [PubMed] [Google Scholar]
- 65.Galéra C, Bouvard MP, Messiah A, Fombonne E. Hyperactivity-inattention symptoms in childhood and substance use in adolescence: the youth gazel cohort. Drug Alcohol Depend. 2008;94:30–37. doi: 10.1016/j.drugalcdep.2007.09.022. [DOI] [PubMed] [Google Scholar]
- 66.Bizzarri JV, Rucci P, Sbrana A, Gonnelli C, Massei GJ, Ravani L, Girelli M, Dell'osso L, Cassano GB. Reasons for substance use and vulnerability factors in patients with substance use disorder and anxiety or mood disorders. Addict Behav. 2007;32:384–391. doi: 10.1016/j.addbeh.2006.04.005. [DOI] [PubMed] [Google Scholar]
- 67.Sousa NO, Grevet EH, Salgado CA, Silva KL, Victor MM, Karam RG, Vitola ES, Picon FA, Zeni GD, Rohde LA, Belmonte-de-Abreu P, Bau CH. Smoking and ADHD: an evaluation of self medication and behavioral disinhibition models based on comorbidity and personality patterns. J Psychiatr Res. 2011;45:829–834. doi: 10.1016/j.jpsychires.2010.10.012. [DOI] [PubMed] [Google Scholar]
- 68.Regnart J, Truter I, Meyer A. Critical exploration of co-occurring Attention-Deficit/Hyperactivity Disorder, mood disorder and Substance Use Disorder. Expert Rev Pharmacoecon Outcomes Res. 2017;17:275–282. doi: 10.1080/14737167.2017.1351878. [DOI] [PubMed] [Google Scholar]
- 69.Jasinski DR, Krishnan S. Human pharmacology of intravenous lisdexamfetamine dimesylate: abuse liability in adult stimulant abusers. J Psychopharmacol. 2009;23:410–418. doi: 10.1177/0269881108093841. [DOI] [PubMed] [Google Scholar]
- 70.Lloyd SL, Striley CW. Marijuana Use Among Adults 50 Years or Older in the 21st Century. Gerontol Geriatr Med. 2018;4:2333721418781668. doi: 10.1177/2333721418781668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Lum HD, Arora K, Croker JA, Qualls SH, Schuchman M, Bobitt J, Milavetz G, Kaskie B. Patterns of Marijuana Use and Health Impact: A Survey Among Older Coloradans. Gerontol Geriatr Med. 2019;5:2333721419843707. doi: 10.1177/2333721419843707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Young S, Adamo N, Ásgeirsdóttir BB, Branney P, Beckett M, Colley W, Cubbin S, Deeley Q, Farrag E, Gudjonsson G, Hill P, Hollingdale J, Kilic O, Lloyd T, Mason P, Paliokosta E, Perecherla S, Sedgwick J, Skirrow C, Tierney K, van Rensburg K, Woodhouse E. Females with ADHD: An expert consensus statement taking a lifespan approach providing guidance for the identification and treatment of attention-deficit/ hyperactivity disorder in girls and women. BMC Psychiatry. 2020;20:404. doi: 10.1186/s12888-020-02707-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Weiss MD. Weiss functional impairment rating scale (WFIRS) self-report. Vancouver, Canada: University of British Columbia. 2000 [Accessed 7 March 2023] Available from: http://www.shared-care.ca/files/Weiss_Functional_Impairment_Self-Report.pdf .
- 74.VAN Rooij AJ, Kuss DJ, Griffiths MD, Shorter GW, Schoenmakers MT, VAN DE Mheen D. The (co-)occurrence of problematic video gaming, substance use, and psychosocial problems in adolescents. J Behav Addict. 2014;3:157–165. doi: 10.1556/JBA.3.2014.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.The Center for Adolescent Behavioral Health Research (CABHRe) The CRAFFT 2.1 Manual “Making new discoveries in substance use prevention, identification, and treatment for children and adolescents”. 2019 [Accessed 7 March 2023] Available from: https://crafft.org/wp-content/uploads/2019/12/CRAFFT-2-1-manualN-2019-12-24.pdf .
- 76.The Center for Adolescent Substance Abuse Research (CeASAR) CRAFFT Screening Test. 2020. [Accessed 7 March 2023] Available from: https://crafft.org/
- 77.Berman AH, Bergman H, Palmstierna T, Schlyter F. Drug use disorders identification test (DUDIT). 2005. [Accessed 7 March 2023] Available from: https://www.emcdda.europa.eu/drugs-library/drug-use-disorders-identification-test-dudit_en . [DOI] [PubMed]
- 78.Skinner HA. The drug abuse screening test. Addict Behav. 1982;7:363–371. doi: 10.1016/0306-4603(82)90005-3. [DOI] [PubMed] [Google Scholar]
- 79.World Health Organization. Alcohol use disorders identification test (AUDIT). 2001 [Accessed 7 March 2023] Available from: https://www.who.int/publications/i/item/WHO-MSD-MSB-01.6a .
- 80.McCann BS, Simpson TL, Ries R, Roy-Byrne P. Reliability and validity of screening instruments for drug and alcohol abuse in adults seeking evaluation for attention-deficit/hyperactivity disorder. Am J Addict. 2000;9:1–9. doi: 10.1080/10550490050172173. [DOI] [PubMed] [Google Scholar]
- 81.Young S, Amarasinghe JM. Practitioner review: Non-pharmacological treatments for ADHD: a lifespan approach. J Child Psychol Psychiatry. 2010;51:116–133. doi: 10.1111/j.1469-7610.2009.02191.x. [DOI] [PubMed] [Google Scholar]
- 82.Molina BS, Hinshaw SP, Eugene Arnold L, Swanson JM, Pelham WE, Hechtman L, Hoza B, Epstein JN, Wigal T, Abikoff HB, Greenhill LL, Jensen PS, Wells KC, Vitiello B, Gibbons RD, Howard A, Houck PR, Hur K, Lu B, Marcus S MTA Cooperative Group. Adolescent substance use in the multimodal treatment study of attention-deficit/hyperactivity disorder (ADHD) (MTA) as a function of childhood ADHD, random assignment to childhood treatments, and subsequent medication. J Am Acad Child Adolesc Psychiatry. 2013;52:250–263. doi: 10.1016/j.jaac.2012.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Klassen LJ, Bilkey TS, Katzman MA, Chokka P. Comorbid attention deficit/hyperactivity disorder and substance use disorder: treatment considerations. Curr Drug Abuse Rev. 2012;5:190–198. doi: 10.2174/1874473711205030190. [DOI] [PubMed] [Google Scholar]
- 84.Hammerness P, Petty C, Faraone SV, Biederman J. Do Stimulants Reduce the Risk for Alcohol and Substance Use in Youth With ADHD? J Atten Disord. 2017;21:71–77. doi: 10.1177/1087054712468051. [DOI] [PubMed] [Google Scholar]
- 85.Hammerness P, Joshi G, Doyle R, Georgiopoulos A, Geller D, Spencer T, Petty CR, Faraone SV, Biederman J. Do stimulants reduce the risk for cigarette smoking in youth with attention-deficit hyperactivity disorder? J Pediatr. 2013;162:22–7.e2. doi: 10.1016/j.jpeds.2012.06.046. [DOI] [PubMed] [Google Scholar]
- 86.Chang Z, Lichtenstein P, Halldner L, D'Onofrio B, Serlachius E, Fazel S, Långström N, Larsson H. Stimulant ADHD medication and risk for substance abuse. J Child Psychol Psychiatry. 2014;55:878–885. doi: 10.1111/jcpp.12164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Wang GJ, Volkow ND, Wigal T, Kollins SH, Newcorn JH, Telang F, Logan J, Jayne M, Wong CT, Han H, Fowler JS, Zhu W, Swanson JM. Long-term stimulant treatment affects brain dopamine transporter level in patients with attention deficit hyperactive disorder. PLoS One. 2013;8:e63023. doi: 10.1371/journal.pone.0063023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Bright GM. Abuse of medications employed for the treatment of ADHD: results from a large-scale community survey. Medscape J Med. 2008;10:111. [PMC free article] [PubMed] [Google Scholar]
- 89.Mariani JJ, Levin FR. Treatment strategies for co-occurring ADHD and substance use disorders. Am J Addict. 2007;16 Suppl 1:45–54; quiz 55. doi: 10.1080/10550490601082783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Wilens TE, Adler LA, Tanaka Y, Xiao F, D'Souza DN, Gutkin SW, Upadhyaya HP. Correlates of alcohol use in adults with ADHD and comorbid alcohol use disorders: exploratory analysis of a placebo-controlled trial of atomoxetine. Curr Med Res Opin. 2011;27:2309–2320. doi: 10.1185/03007995.2011.628648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Childress A. The safety of extended-release drug formulations for the treatment of ADHD. Expert Opin Drug Saf. 2017;16:603–615. doi: 10.1080/14740338.2017.1317344. [DOI] [PubMed] [Google Scholar]
- 92.Cortese S, Adamo N, Del Giovane C, Mohr-Jensen C, Hayes AJ, Carucci S, Atkinson LZ, Tessari L, Banaschewski T, Coghill D, Hollis C, Simonoff E, Zuddas A, Barbui C, Purgato M, Steinhausen HC, Shokraneh F, Xia J, Cipriani A. Comparative efficacy and tolerability of medications for attention-deficit hyperactivity disorder in children, adolescents, and adults: a systematic review and network meta-analysis. Lancet Psychiatry. 2018;5:727–738. doi: 10.1016/S2215-0366(18)30269-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Liang EF, Lim SZ, Tam WW, Ho CS, Zhang MW, McIntyre RS, Ho RC. The Effect of Methylphenidate and Atomoxetine on Heart Rate and Systolic Blood Pressure in Young People and Adults with Attention-Deficit Hyperactivity Disorder (ADHD): Systematic Review, Meta-Analysis, and Meta-Regression. Int J Environ Res Public Health. 2018;15 doi: 10.3390/ijerph15081789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Liu H, Feng W, Zhang D. Association of ADHD medications with the risk of cardiovascular diseases: a meta-analysis. Eur Child Adolesc Psychiatry. 2019;28:1283–1293. doi: 10.1007/s00787-018-1217-x. [DOI] [PubMed] [Google Scholar]
- 95.National Institute for Health and Care Excellence. Attention deficit hyperactivity disorder: diagnosis and management NG87. 2019. [Accessed 7 March 2023] Available from: https://www.nice.org.uk/guidance/ng87 .
- 96.Barkla XM, McArdle PA, Newbury-Birch D. Are there any potentially dangerous pharmacological effects of combining ADHD medication with alcohol and drugs of abuse? BMC Psychiatry. 2015;15:270. doi: 10.1186/s12888-015-0657-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Young S, Asherson P, Lloyd T, Absoud M, Arif M, Colley WA, Cortese S, Cubbin S, Doyle N, Morua SD, Ferreira-Lay P, Gudjonsson G, Ivens V, Jarvis C, Lewis A, Mason P, Newlove-Delgado T, Pitts M, Read H, van Rensburg K, Zoritch B, Skirrow C. Failure of Healthcare Provision for Attention-Deficit/Hyperactivity Disorder in the United Kingdom: A Consensus Statement. Front Psychiatry. 2021;12:649399. doi: 10.3389/fpsyt.2021.649399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Zetterqvist J, Asherson P, Halldner L, Långström N, Larsson H. Stimulant and non-stimulant attention deficit/hyperactivity disorder drug use: total population study of trends and discontinuation patterns 2006-2009. Acta Psychiatr Scand. 2013;128:70–77. doi: 10.1111/acps.12004. [DOI] [PubMed] [Google Scholar]
- 99.Mannuzza S, Klein RG, Truong NL, Moulton JL 3rd, Roizen ER, Howell KH, Castellanos FX. Age of methylphenidate treatment initiation in children with ADHD and later substance abuse: prospective follow-up into adulthood. Am J Psychiatry. 2008;165:604–609. doi: 10.1176/appi.ajp.2008.07091465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Wilens TE, Adamson J, Monuteaux MC, Faraone SV, Schillinger M, Westerberg D, Biederman J. Effect of prior stimulant treatment for attention-deficit/hyperactivity disorder on subsequent risk for cigarette smoking and alcohol and drug use disorders in adolescents. Arch Pediatr Adolesc Med. 2008;162:916–921. doi: 10.1001/archpedi.162.10.916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Ford T. Transitional care for young adults with ADHD: transforming potential upheaval into smooth progression. Epidemiol Psychiatr Sci. 2020;29:e87. doi: 10.1017/S2045796019000817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Janssens A, Eke H, Price A, Newlove-Delgado T, Blake S, Ani C, Asherson P, Beresford B, Emmens T, Hollis C, Logan S, Paul M, Sayal K, Young S, Ford T. The transition from children’s services to adult services for young people with attention deficit hyperactivity disorder: the CATCh-uS mixed-methods study. Southampton (UK): NIHR Journals Library; 2020 Nov. [PubMed] [Google Scholar]
- 103.Northumbria Healthcare NHS Foundation Trust. Developmentally Appropriate Healthcare Toolkit. 2022 [Accessed 7 March 2023] Available from: https://www.northumbria.nhs.uk/about-us/quality-and-safety/research-and-clinical-trials/developmentally-appropriate-healthcare-toolkit#18d9549b .
- 104.Kuriyan AB, Pelham WE Jr, Molina BS, Waschbusch DA, Gnagy EM, Sibley MH, Babinski DE, Walther C, Cheong J, Yu J, Kent KM. Young adult educational and vocational outcomes of children diagnosed with ADHD. J Abnorm Child Psychol. 2013;41:27–41. doi: 10.1007/s10802-012-9658-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.De Crescenzo F, Cortese S, Adamo N, Janiri L. Pharmacological and non-pharmacological treatment of adults with ADHD: a meta-review. Evid Based Ment Health. 2017;20:4–11. doi: 10.1136/eb-2016-102415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Young S, Bramham J. Cognitive-behavioural therapy for ADHD in adolescents and adults: A psychological guide to practice. 2nd ed. Chichester: Wiley-Blackwell; 2012. [Google Scholar]
- 107.Fuermaier AB, Tucha L, Koerts J, Aschenbrenner S, Weisbrod M, Lange KW, Tucha O. Cognitive complaints of adults with attention deficit hyperactivity disorder. Clin Neuropsychol. 2014;28:1104–1122. doi: 10.1080/13854046.2014.964325. [DOI] [PubMed] [Google Scholar]
- 108.Kooij JJS, Bijlenga D, Salerno L, Jaeschke R, Bitter I, Balázs J, Thome J, Dom G, Kasper S, Nunes Filipe C, Stes S, Mohr P, Leppämäki S, Casas M, Bobes J, Mccarthy JM, Richarte V, Kjems Philipsen A, Pehlivanidis A, Niemela A, Styr B, Semerci B, Bolea-Alamanac B, Edvinsson D, Baeyens D, Wynchank D, Sobanski E, Philipsen A, McNicholas F, Caci H, Mihailescu I, Manor I, Dobrescu I, Saito T, Krause J, Fayyad J, Ramos-Quiroga JA, Foeken K, Rad F, Adamou M, Ohlmeier M, Fitzgerald M, Gill M, Lensing M, Motavalli Mukaddes N, Brudkiewicz P, Gustafsson P, Tani P, Oswald P, Carpentier PJ, De Rossi P, Delorme R, Markovska Simoska S, Pallanti S, Young S, Bejerot S, Lehtonen T, Kustow J, Müller-Sedgwick U, Hirvikoski T, Pironti V, Ginsberg Y, Félegyházy Z, Garcia-Portilla MP, Asherson P. Updated European Consensus Statement on diagnosis and treatment of adult ADHD. Eur Psychiatry. 2019;56:14–34. doi: 10.1016/j.eurpsy.2018.11.001. [DOI] [PubMed] [Google Scholar]
- 109.Hanson KL, Medina KL, Padula CB, Tapert SF, Brown SA. Impact of Adolescent Alcohol and Drug Use on Neuropsychological Functioning in Young Adulthood: 10-Year Outcomes. J Child Adolesc Subst Abuse. 2011;20:135–154. doi: 10.1080/1067828X.2011.555272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Crunelle CL, van den Brink W, Moggi F, Konstenius M, Franck J, Levin FR, van de Glind G, Demetrovics Z, Coetzee C, Luderer M, Schellekens A ICASA consensus group, Matthys F. International Consensus Statement on Screening, Diagnosis and Treatment of Substance Use Disorder Patients with Comorbid Attention Deficit/Hyperactivity Disorder. Eur Addict Res. 2018;24:43–51. doi: 10.1159/000487767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Groshkova T. Motivation in substance misuse treatment. Addict Res Theory. 2010;18:494–510. [Google Scholar]
- 112.Miller WR, Rollnick S. Motivational interviewing: Helping people change. 3rd ed. New York: Guilford press; 2012. [Google Scholar]
- 113.Van Horn DH, Bux DA. A pilot test of motivational interviewing groups for dually diagnosed inpatients. J Subst Abuse Treat. 2001;20:191–195. doi: 10.1016/s0740-5472(00)00157-4. [DOI] [PubMed] [Google Scholar]
- 114.Prochaska JO, DiClemente CC. Transtheoretical therapy: Toward a more integrative model of change. Psychother Theory Res Pract . 1982;19:276–288. [Google Scholar]
- 115.Hoyos C, Cortese S. Beyond Diagnosis: Formulation-Storytelling and Maps. J Am Acad Child Adolesc Psychiatry. 2023;62:120–122. doi: 10.1016/j.jaac.2022.06.008. [DOI] [PubMed] [Google Scholar]
- 116.Johnstone L, Dallos R. Formulation in Psychology and Psychotherapy. 2nd ed. London: Routledge; 2014. [Google Scholar]
- 117.Macneil CA, Hasty MK, Conus P, Berk M. Is diagnosis enough to guide interventions in mental health? BMC Med. 2012;10:111. doi: 10.1186/1741-7015-10-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Dahl V, Ramakrishnan A, Spears AP, Jorge A, Lu J, Bigio NA, Chacko A. Psychoeducation Interventions for Parents and Teachers of Children and Adolescents with ADHD: a Systematic Review of the Literature. J Dev Phys Disabil. 2020;32:257–292. [Google Scholar]
- 119.Mazzone L, Postorino V, Reale L, Guarnera M, Mannino V, Armando M, Fatta L, De Peppo L, Vicari S. Self-esteem evaluation in children and adolescents suffering from ADHD. Clin Pract Epidemiol Ment Health. 2013;9:96–102. doi: 10.2174/1745017901309010096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Harpin V, Mazzone L, Raynaud JP, Kahle J, Hodgkins P. Long-Term Outcomes of ADHD: A Systematic Review of Self-Esteem and Social Function. J Atten Disord. 2016;20:295–305. doi: 10.1177/1087054713486516. [DOI] [PubMed] [Google Scholar]
- 121.Emilsson B, Gudjonsson G, Sigurdsson JF, Baldursson G, Einarsson E, Olafsdottir H, Young S. Cognitive behaviour therapy in medication-treated adults with ADHD and persistent symptoms: a randomized controlled trial. BMC Psychiatry. 2011;11:116. doi: 10.1186/1471-244X-11-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Young S, Emilsson B, Sigurdsson JF, Khondoker M, Philipp-Wiegmann F, Baldursson G, Olafsdottir H, Gudjonsson G. A randomized controlled trial reporting functional outcomes of cognitive-behavioural therapy in medication-treated adults with ADHD and comorbid psychopathology. Eur Arch Psychiatry Clin Neurosci. 2017;267:267–276. doi: 10.1007/s00406-016-0735-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Young S, Khondoker M, Emilsson B, Sigurdsson JF, Philipp-Wiegmann F, Baldursson G, Olafsdottir H, Gudjonsson G. Cognitive-behavioural therapy in medication-treated adults with attention-deficit/hyperactivity disorder and co-morbid psychopathology: a randomized controlled trial using multi-level analysis. Psychol Med. 2015;45:2793–2804. doi: 10.1017/S0033291715000756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Aviram RB, Rhum M, Levin FR. Psychotherapy of adults with comorbid attention-deficit/hyperactivity disorder and psychoactive substance use disorder. J Psychother Pract Res. 2001;10:179–186. [PMC free article] [PubMed] [Google Scholar]
- 125.Levin FR, Upadhyaya HP. Diagnosing ADHD in adults with substance use disorder: DSM-IV criteria and differential diagnosis. J Clin Psychiatry. 2007;68:e18. doi: 10.4088/jcp.0707e18. [DOI] [PubMed] [Google Scholar]
- 126.Barkley RA, Brown TE. Unrecognized attention-deficit/hyperactivity disorder in adults presenting with other psychiatric disorders. CNS Spectr. 2008;13:977–984. doi: 10.1017/s1092852900014036. [DOI] [PubMed] [Google Scholar]
- 127.Kessler RC, Adler L, Ames M, Demler O, Faraone S, Hiripi E, Howes MJ, Jin R, Secnik K, Spencer T, Ustun TB, Walters EE. The World Health Organization Adult ADHD Self-Report Scale (ASRS): a short screening scale for use in the general population. Psychol Med. 2005;35:245–256. doi: 10.1017/s0033291704002892. [DOI] [PubMed] [Google Scholar]
- 128.van de Glind G, van den Brink W, Koeter MW, Carpentier PJ, van Emmerik-van Oortmerssen K, Kaye S, Skutle A, Bu ET, Franck J, Konstenius M, Moggi F, Dom G, Verspreet S, Demetrovics Z, Kapitány-Fövény M, Fatséas M, Auriacombe M, Schillinger A, Seitz A, Johnson B, Faraone SV, Ramos-Quiroga JA, Casas M, Allsop S, Carruthers S, Barta C, Schoevers RA IASP Research Group, Levin FR. Validity of the Adult ADHD Self-Report Scale (ASRS) as a screener for adult ADHD in treatment seeking substance use disorder patients. Drug Alcohol Depend. 2013;132:587–596. doi: 10.1016/j.drugalcdep.2013.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Fatseas M, Debrabant R, Auriacombe M. The diagnostic accuracy of attention-deficit/hyperactivity disorder in adults with substance use disorders. Curr Opin Psychiatry. 2012;25:219–225. doi: 10.1097/YCO.0b013e3283523d7c. [DOI] [PubMed] [Google Scholar]
- 130.Vergara-Moragues E, González-Saiz F, Trujols-Albet J. Paradoxical effects of cocaine use in patients with comorbid ADHD. Revista de Patología Dual. 2015;2:13. [Google Scholar]
- 131.Levin FR. Diagnosing attention-deficit/hyperactivity disorder in patients with substance use disorders. J Clin Psychiatry. 2007;68 Suppl 11:9–14. [PubMed] [Google Scholar]
- 132.House of Commons. Justice Committee. Mental health in prison. Fifth Report of Session 2021-22. Report, together with formal minutes relating to the report. [Accessed 7th March 2023] Available from: https://committees.parliament.uk/publications/7455/documents/78054/default/
- 133.Brown TE. ADHD comorbidities: Handbook for ADHD complications in children and adults. 1st ed. Washington, DC: American Psychiatric Pub; 2009. [Google Scholar]
- 134.Murphy P, Schachar R. Use of self-ratings in the assessment of symptoms of attention deficit hyperactivity disorder in adults. Am J Psychiatry. 2000;157:1156–1159. doi: 10.1176/appi.ajp.157.7.1156. [DOI] [PubMed] [Google Scholar]
- 135.National Institute for Health and Care Excellence. Attention Deficit Hyperactivity Disorder: Quality Standard. 2013. [Accessed 7 March 2023] Available from: https://www.nice.org.uk/guidance/qs39 .
- 136.Newlove-Delgado T, Blake S, Ford T, Janssens A. Young people with attention deficit hyperactivity disorder in transition from child to adult services: a qualitative study of the experiences of general practitioners in the UK. BMC Fam Pract. 2019;20:159. doi: 10.1186/s12875-019-1046-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Ball C. Attention-deficit hyperactivity disorder and the use of methylphenidate: A survey of the views of general practitioners. Psychiatric Bulletin. 2001;25:301–304. [Google Scholar]
- 138.Coughlan C, Manek N, Razak Y, Klaber RE. How to improve care across boundaries. BMJ. 2020;369:m1045. doi: 10.1136/bmj.m1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.van Emmerik-van Oortmerssen K, Vedel E, Kramer FJ, Blankers M, Dekker JJM, van den Brink W, Schoevers RA. Integrated cognitive behavioral therapy for ADHD in adult substance use disorder patients: Results of a randomized clinical trial. Drug Alcohol Depend. 2019;197:28–36. doi: 10.1016/j.drugalcdep.2018.12.023. [DOI] [PubMed] [Google Scholar]
- 140.LeFever GB, Villers MS, Morrow AL, Vaughn ES. Parental perceptions of adverse educational outcomes among children diagnosed and treated for ADHD: A call for improved school/provider collaboration. Psychol Schs. 2002;39:63–71. [Google Scholar]
- 141.Premier League. Premier League Kicks. 2022. [Accessed 7 March 2023] Available from: https://www.premierleague.com/communities/programmes/community-programmes/pl-kicks .
- 142.Oasis Oasis Global. 2022; [Accessed 7 March 2023] Available from: https://www.oasisuk.org/oasis-global/
- 143.The National Archives. Equality Act 2010. 2010. [Accessed 7 March 2023] Available from: https://www.legislation.gov.uk/ukpga/2010/15/contents .
- 144.Gudjonsson GH, Sigurdsson JF, Sigfusdottir ID, Young S. A national epidemiological study of offending and its relationship with ADHD symptoms and associated risk factors. J Atten Disord. 2014;18:3–13. doi: 10.1177/1087054712437584. [DOI] [PubMed] [Google Scholar]
- 145.Young S, Gudjonsson GH, Wells J, Asherson P, Theobald D, Oliver B, Scott C, Mooney A. Attention deficit hyperactivity disorder and critical incidents in a Scottish prison population. Pers Individ Dif. 2009;46:265–269. [Google Scholar]
- 146.Young S, Cocallis K. ADHD and offending. J Neural Transm (Vienna) 2021;128:1009–1019. doi: 10.1007/s00702-021-02308-0. [DOI] [PubMed] [Google Scholar]