Abstract
Objective
Female sex workers(FSW) and adolescent girls and young women(AGYW) face a disproportionately high risk of HIV in South Africa. Oral PrEP can avert new infections, but its effectiveness is linked to consistent use. Early discontinuation of PrEP in this population is high, but less is known about longitudinal patterns of PrEP use, including patterns of re-initiation and cycling.
Design
Longitudinal descriptive analysis of routine program data.
Methods
Between 2016–2021, 40,681 FSW and AGYW initiated PrEP at TB HIV Care, the largest PrEP provider to this population in South Africa and were included. Using survival analyses and group-based trajectory modeling, we described patterns of initiation, discontinuation, re-initiation, and cycling.
Results
Total initiations increased over the life of the program for both FSW and AGYW. About 40% of FSW(0.41, 95%CI [0.40–0.42]) and AGYW(0.38, 95%CI [0.37–0.38]) remained on PrEP at 1-month. FSW were more likely to restart PrEP, however less than 10% restarted PrEP within a year of initiation. Three latent trajectory groups of PrEP use were identified for FSW(low use, early cycling, and ongoing cycling) and two for AGYW(low use and ongoing cycling). Persistence was negatively associated with initiation among AGYW, but there was no clear relationship among FSW. Those initiating later in the program and older women had a reduced risk of discontinuation.
Conclusions
Persistence on PrEP was low, but cycling on and off PrEP was common, with early missed visits and inconsistent, but ongoing use. A push to increase PrEP initiations needs to factor in readiness and persistence support, to achieve public health impact.
Keywords: HIV prevention, PrEP, female sex workers, adolescent girls and young women, survival analysis, routinely collected data, South Africa
INTRODUCTION
HIV incidence is disproportionately high among adolescent girls and young women (AGYW) ages 15–24 years old and female sex workers (FSW) in South Africa. Young women make up only 8% of South Africa’s population but account for approximately one third of the 230,000 new infections reported annually.1,2 Further, as many as 60% of FSW are estimated to be living with HIV. The incidence rate in younger FSW is approximately 13.2 per 100 person years.3 While AGYW and FSW are often treated as separate groups both programmatically and in research settings, they share many risk factors for HIV acquisition, including age-disparate relationships, difficulty negotiating condom use, and economic instability.4–7 Little progress has been made toward mitigating their HIV risk, despite the significant need.2
Daily oral pre-exposure prophylaxis (PrEP) is an HIV prevention tool that has been shown to be between 79–90% efficacious among women when used consistently.8–10 Because it can be accessed without consent or approval from parents or partners as early as age 15, daily oral PrEP is a promising tool for addressing some of the unique structural prevention challenges facing young women.11,12 But early discontinuation and inconsistent pill-taking undermine its effective use.13 In prior demonstration studies in South Africa approximately half of PrEP users, including both AGYW and FSW, discontinued PrEP by 1-month.14–18 However, there are limited longitudinal data on PrEP use among women at high-risk who initiate and discontinue at least once.
The need for PrEP, unlike the need for treatment, can differ not only between individuals, but also within individuals over time.19 Risk of HIV may be episodic, and individuals may cycle on and off PrEP, coinciding with changes to perceived risk, sometimes referred to as risk-use alignment.19–21 Among women who initiate PrEP in South Africa, patterns of use following discontinuation are not well understood, but are important for informing program implementation and management, decisions about who should be initiated, and concerns about potential future resistance to antiretrovirals.19
Prior to 2022 and before full roll-out to public healthcare facilities, PrEP in South Africa was largely delivered through implementing partners, including NGOs and other non-profits that have experience providing health services to prioritized populations. As these programs are primarily donor-funded, these implementing partners have finite resources and staff, and increasing the number of patients who initiate PrEP may mean fewer per-client resources to support adherence and persistence. This relationship between number of people initiated on PrEP and PrEP persistence has not been studied.
The objective of this study was to examine patterns of PrEP initiation, discontinuation, re-initiation, and cycling among FSW and AGYW who initiated PrEP through TB HIV Care (THC), the largest PrEP provider to women in South Africa. In addition, we described the relationship between PrEP persistence and age and year of initiation, and the program-level relationship between initiation and persistence.
METHODS
Study Population and Setting
THC is a South African non-profit that provides integrated health services to populations at high risk, including HIV testing, reproductive health services, and STI syndromic screening and treatment. TB HIV Care has been providing PrEP to FSW since 2016 and AGYW since 2018. Data for this analysis come from site-level (district unit of administration) or clinic-level registers that track PrEP use over time.
FSW were served by nine sites in five provinces across South Africa: KwaZulu-Natal (eThekwini, uMgungundlovu), Mpumalanga (Ehlanzeni, Gert Sibande, Nkangala), North West (Kenneth Kaunda, Ngaka Modiri Molema), Eastern Cape (OR Tambo), and Western Cape (Cape Town). AGYW were served by four sites in three provinces: KwaZulu-Natal (eThekwini, uMgungundlovu), Gauteng (Ekurhuleni), and Western Cape (Cape Town). The program records information on individual clinical encounters, or any time a client comes in to receive services, on paper forms and stores these forms in locked and secure file cabinets. Data capturers then enter these data into registers at least once a week for each site. The secondary use of programmatic data for these analyses was reviewed by the Johns Hopkins Bloomberg School of Public Health Institutional Review Board and the University of Western Cape Research Ethics Committee; a waiver of informed consent was provided, as all of the data were deidentified.
We included FSW and AGYW who accessed health services from THC (e.g. HIV testing, sexual and reproductive health services) and who tested negative for HIV. Because clients in this study were categorized as FSW or AGYW according to the program through which they were recruited and from where they received services, some individuals who were older than 24 years old were categorized as AGYW. TB HIV Care generally provides services to FSW from known sex work venues, including brothels, bars, and street- based venues, and AGYW from locations where young women tend to congregate, like schools, community centers, and areas of commerce. AGYW served by TB HIV Care are at greater risk of HIV acquisition than AGYW more broadly, and may have age-disparate relationships, multiple partnerships, participate in transactional sex, or have unstable home environments and/or school attendance. Specific risk factors for HIV acquisition are documented using the Determined, Resilient, Empowered, AIDS-Free, Mentored and Safe (DREAMS) eligibility criteria. The study period included data from when PrEP was first made available through THC until the administrative censoring date (June 2016-August 2021 for FSW and May 2018-September 2020 for AGYW). The administrative censoring date for AGYW is earlier than for FSW given a change in the structure of the AGYW PrEP registers, which precluded the inclusion of more recent data in these analyses.
Outcomes
The primary outcomes of interest for both FSW and AGYW included PrEP initiation, discontinuation, and re-initiation. PrEP initiation was defined as choosing to start oral PrEP (tenofovir/emtricitabine) and taking home a 1-month supply of pills. We defined the denominator for the proportion initiating PrEP as the number testing negative for HIV during the same month; this was the number of unique encounters, and women could have tested in more than one period. Among women who initiated PrEP, we defined discontinuation as two consecutive missed monthly PrEP visits, a client-initiated stop, or a provider-initiated stop. The discontinuation event was assigned to the first month of the two consecutive missed visits or the month of the client-initiated or provider-initiated stop. This definition of PrEP discontinuation is the one used by the program in alignment with PEPFAR reporting definitions.22 Re-initiation was defined as restarting PrEP within 12 months of an initial PrEP prescription, after a ≥2 month gap in PrEP (a discontinuation). PrEP cycling was defined as going in and out of different states of PrEP use (starting, stopping, and starting again).
Covariates
We also assessed woman’s age and year of PrEP initiation (2016–2021) as potential covariates of PrEP discontinuation.
Statistical analyses
Initiation
We plotted the monthly proportion of HIV negative encounters who initiated PrEP over calendar time, by population (FSW and AGYW) and stratified by site. Data on the number of HIV negative encounters were missing for 2% of FSW months (6/337) and 20% of AGYW months (108/537). We assumed, based on discussions with THC program staff, that data were missing completely at random and excluded those months from our analyses.
Discontinuation
We examined time from PrEP initiation to discontinuation using Kaplan-Meier survival curves, by population and stratified by site. Individuals were censored after 12 months of follow-up based on data on continuation being captured in registers for the 12 months following initiation or at the end of the study period (administrative censoring). During the study period, the program switched to multi-month dispensing after the first month to alleviate the burden of having to return monthly (December 2019 for FSW and March 2020 for AGYW), meaning that women were seen at 1-month and thereafter at 4-months, 7-months, etc. After the switch to multi-month dispensing, a woman was recorded as persistent on PrEP in the intervening months if she had the supply of PrEP for those months in her possession.22 Women were recorded as discontinued if they missed a refill appointment.
Re-initiation
To explore patterns of re-initiation, we estimated time from PrEP discontinuation to re-initiation using the complement of Kaplan-Meier survival function to estimate the cumulative incidence of re-initiation, by population and stratified by site. Individuals were censored at 12 months following their initial initiation due to availability of data.
Group-based trajectory modeling
We used group-based trajectory modeling to describe monthly PrEP use over the one year period following PrEP initiation. Individual trajectories of PrEP use were used to model latent groups of individuals whose outcomes follow a similar pattern over time. Those individuals who were on PrEP in a given month were coded as “1”, while those who were not on PrEP were coded as “0.” We considered linear, quadratic, and cubic specifications for the shape of each trajectory group and options for the number of groups (between 2–6) and systematically compared each permutation using model diagnostics. The final models were selected to optimize Bayesian Information Criteria (BIC), entropy, and alignment with existing models of PrEP persistence in the literature.23,24
Correlates of discontinuation
We also described correlates of discontinuation. We plotted 1-month persistence against the total number of initiations in a given month, stratifying by population and site (to examine the hypothesis that persistence decreases with a greater number of initiations). We also formally assessed the relationship between persistence and initiation using linear regression models for each population, adjusting for site and scaling the number of initiations by 100. We estimated hazard ratios for discontinuation overall and looked at associations between hazard of discontinuation and site, age, and year of initiation using a multivariable complementary log-log regression model. We used a complementary log-log regression model, because while data are collected at discrete time points (monthly), the underlying hazard of discontinuation, which could occur at any point during the month, is continuous.
All analyses were conducted using Stata 14.2 (StataCorp, College Park, Texas, USA).
RESULTS
Overall, 40,681 individuals initiated PrEP at THC during the study period and were included in these analyses, including 12,581 FSW and 28,100 AGYW. Among FSW, the two largest sites were eThekwini (n=3,268, 26%) and uMgungundlovu (n=2,919, 23%). Among AGYW, the two largest sites were Cape Town (n=9,660, 34%) and uMgungundlovu (n=11,866, 43%). Over one third (n=10,622, 38%) of AGYW were adolescents (15–18 years old). A large proportion of both populations was between the ages of 19 and 24 years old: about 2 of 5 FSW (n=4,846, 39%) and more than half of AGYW (n=15,824, 56%)(Table 1).
Table 1.
Characteristics of female sex workers (FSW) and adolescent girls and young women (AGYW) initiating PrEP through TB HIV Care between 2016 and 2021
| Female sex workers N=12,581 |
Adolescent girls and young women N=28,100 |
|
|---|---|---|
|
| ||
| Site | ||
| Cape Town | 12% (1,486) | 34% (9,660) |
| eKurhuleni | 13% (3,684) | |
| eThekwini | 26% (3,268) | 10% (2,890) |
| Ehlanzeni | 6% (813) | |
| Gert Sibande | 5% (629) | |
| Kenneth Kaunda | 5% (659) | |
| Ngaka Modiri Molema | 2% (226) | |
| Nkangala | 8% (988) | |
| OR Tambo | 13% (1,593) | |
| uMgungundlovu | 23% (2,919) | 43% (11,866) |
|
| ||
| Age | ||
| 15–18 years old | 7% (939) | 38% (10,662) |
| 19–24 years old | 39% (4,846) | 56% (15,824) |
| 25–34 years old | 40% (5,039) | 5% (1,318) |
| 35 years old or older | 14% (1,730) | 1 % (290) |
|
| ||
| Year of initiation | ||
| 2016 | 2% (302) | |
| 2017 | 3% (348) | |
| 2018 | 8% (962) | 5% (1,286) |
| 2019 | 25% (3,153) | 44% (12,325) |
| 2020 | 37% (4,618) | 52% (14,489) |
| 2021 | 25% (3,197) | |
Initiation
The number of initiations increased for both populations, from 302 in 2016 to its highest value of 4,618 in 2020 for FSW and 1,286 in 2018 to 14,489 in 2020 for AGYW(Table 1). Across the study period, approximately 19% (12,581/65,782) of negative HIV test encounters resulted in an initiation among FSW, compared with 55% (28,100/51,436) of negative test encounters among AGYW. Among FSW, the proportion of initiations increased over time, with a monotonic increase beginning in 2018(Figure 1). At sites that began providing PrEP later in calendar time, the proportion of HIV negative encounters among FSW who initiated was generally higher early on, and there was not a clear increasing trend in initiations, specifically for Ehlanzeni, Ngaka Modiri Molema, and Kenneth Kaunda(Appendix Figure 1). Among AGYW, while there was an observed increase in the proportion of initiations over time, this increase was not statistically significant and there was substantial heterogeneity across sites(Figure 1). At the two largest sites (Cape Town and uMgungundlovu), there was a clear increase in initiations over time for both populations, while at one smaller site (eKurhuleni) there was a dramatic decrease. Further, one site only contributed 4 months of observations due to missing data(Appendix Figure 1).
Figure 1.
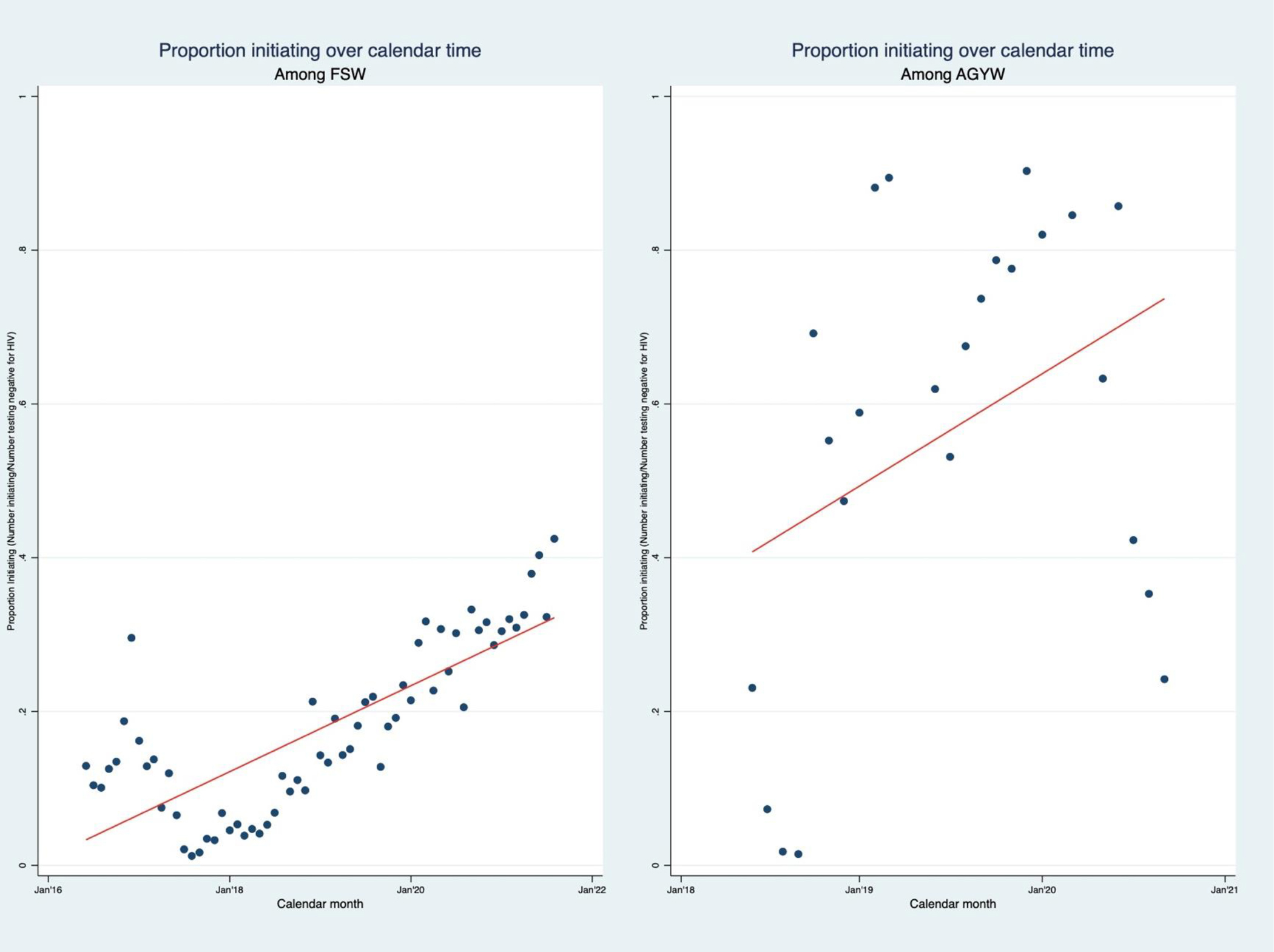
Proportion of eligible HIV negative encounters initiating PrEP over time among female sex workers and adolescent girls and young women at TB HIV Care (2016–2021)
Discontinuation
The 40,681 individuals who initiated PrEP during the study period contributed 90,377 person-months to the analysis of time to discontinuation. Both populations had low persistence, with 41%(95% CI: 40%−42%) of FSW and 38%(95% CI: 37%−38%) persisting at 1-month(Figure 2). Over the 12 months of follow-up, AGYW experienced a slightly earlier drop-off(Figure 2). There were substantial differences in PrEP persistence across sites(Figure 2), particularly for AGYW.
Figure 2.
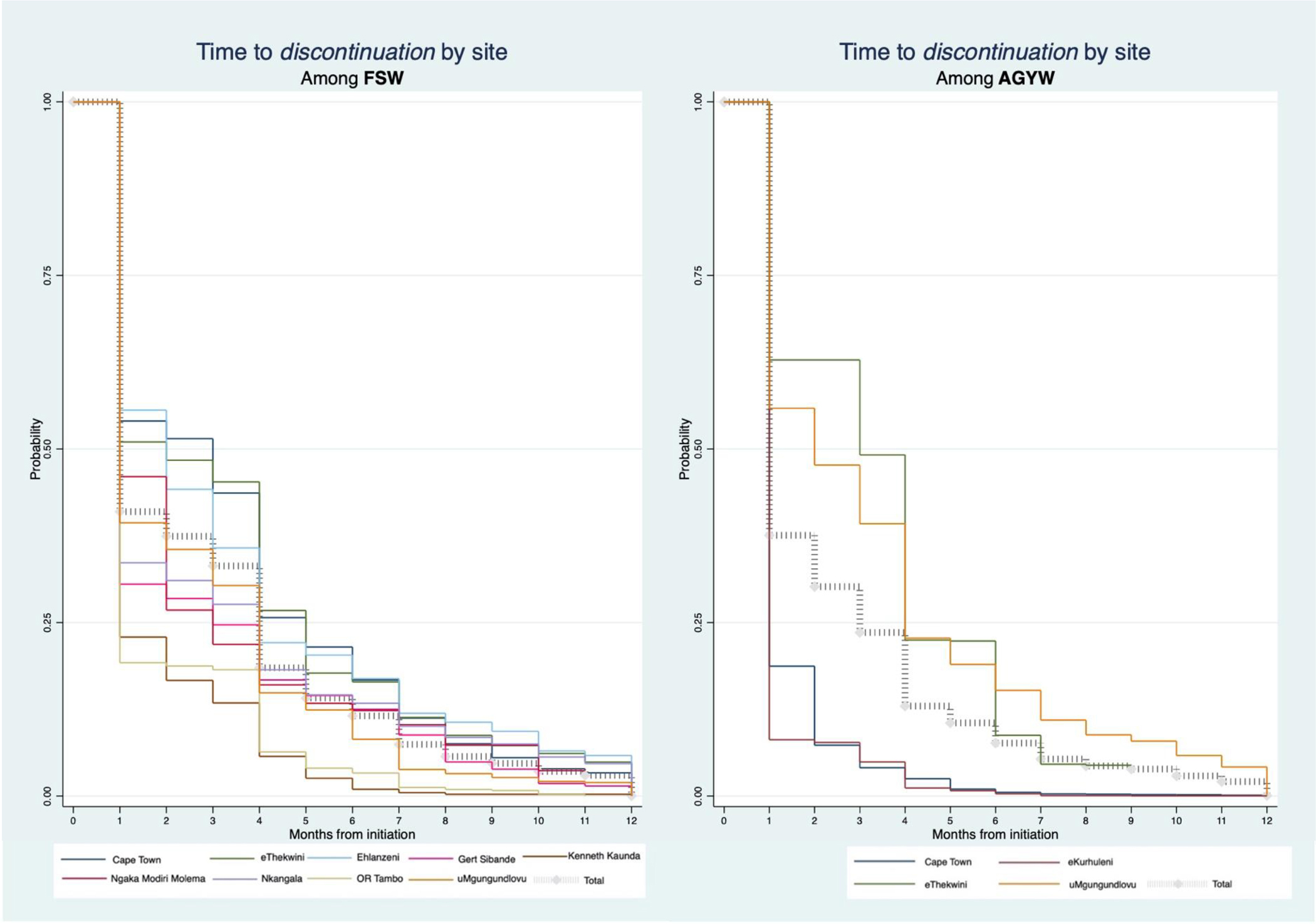
Kaplan-Meier survival curves of the time from initiation to first discontinuation by site among female sex workers (n=12581) and adolescent girls and young women (n=28100) who initiated PrEP between 2016 and 2021 at TB HIV Care
Re-initiation
A total of 2,131 individuals initiated for a second time within 12 months of a first PrEP initiation. The marginal probability of reinitiation was 5%, with a greater proportion of FSW(n=1,146, 9%) reinitiating compared with AGYW(n=985, 3%)(Figure 3). Among FSW, the greatest number of re-initiations occurred at eThekwini and Cape Town, and among AGYW, the greatest number occurred at uMgungundlovu(Appendix Table 1).
Figure 3.
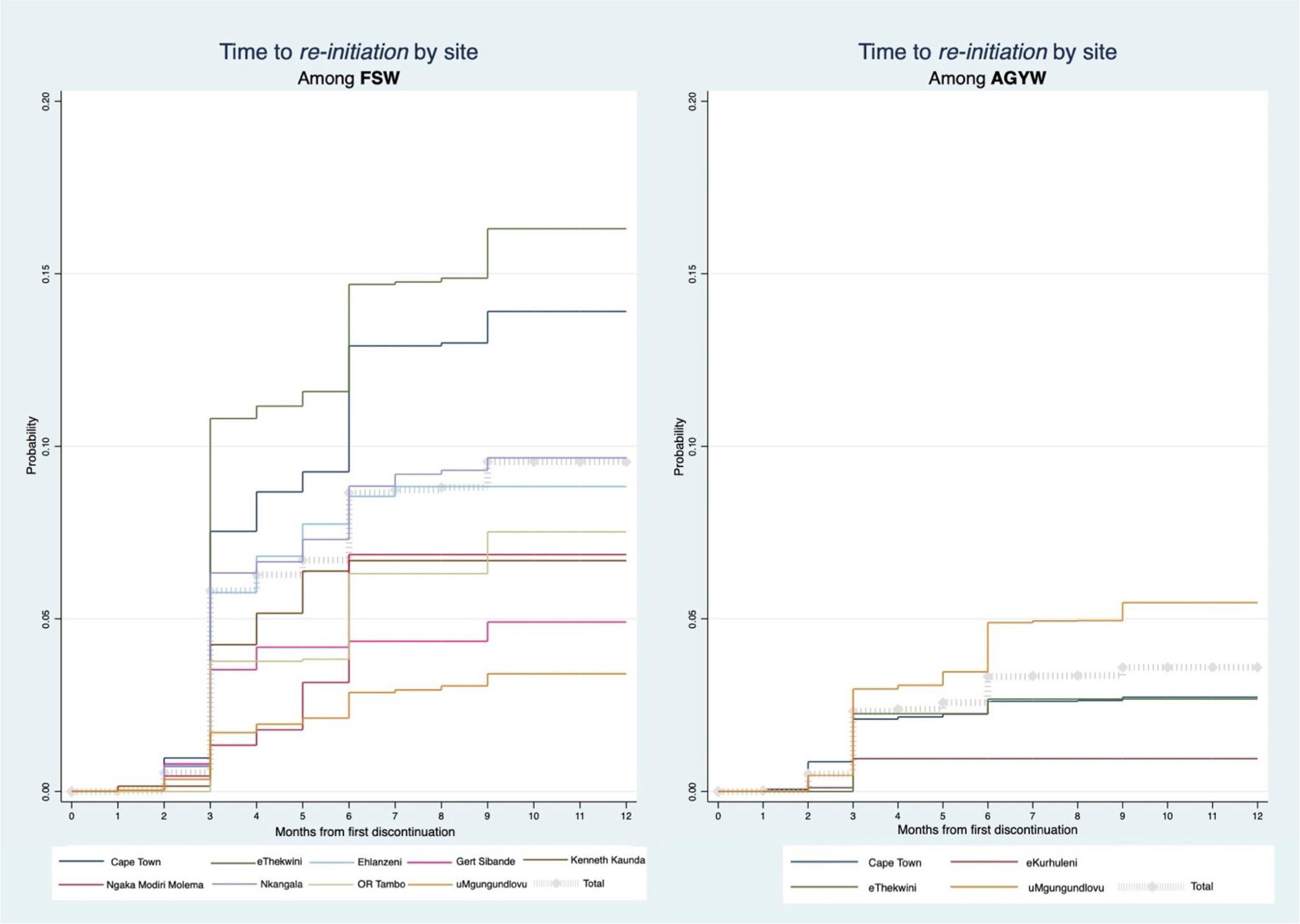
Cumulative incidence curves of the time from discontinuation to re-initiation by site among female sex workers (n=12,581) and adolescent girls and young women (n=28,100) who initiated PrEP between 2016 and 2021 at TB HIV Care
Group-based trajectories of PrEP use
We identified three latent trajectory groups for FSW(BIC: −37,369, Entropy: 0.97, Shape parameter: cubic) and two for AGYW(BIC: −73,738, Entropy: 0.95, Shape parameter: quadratic). (Figure 4)
Figure 4.
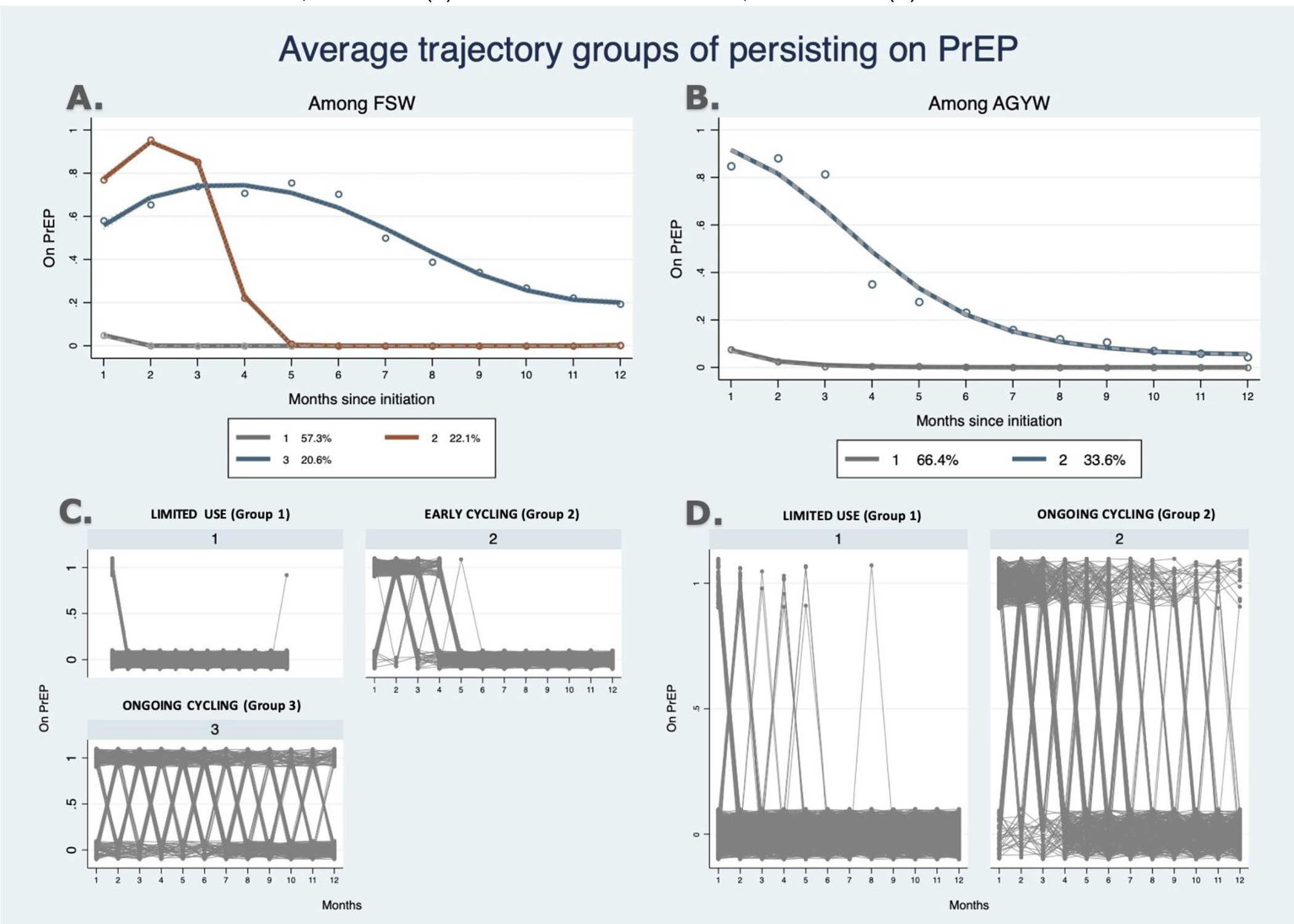
Average trajectory groups based on latent groups of persisting on PrEP from group-based trajectory models, stratified by FSW (a) and AGYW (b) populations and individual trajectories of PrEP use for a random sample of 1000 individuals drawn from 12,581 FSW (c) and 1000 drawn from 28,100 AGYW (d)
For FSW, we identified three groups, which we defined as “limited use,” “early cycling,” and “ongoing cycling” based on the observed trajectories. The majority(57%) of FSW were in the Limited Use group: 5% were on PrEP at one month and 0.1% were on PrEP in any subsequent month. Twenty-two percent of FSW were in the Early Cycling group. In this group, 76% were recorded as on PrEP at one month and this increased at two months to 95%. By 5 months following initiation, less than 0.5% were on PrEP. Twenty-one percent of FSW were in the Ongoing Cycling group, of whom, 62% were on PrEP at one month, 71% at 4 months, 51% at 7 months, and 27% at 10 months(Figure 4).
For AGYW, we identified two groups, which we defined as “limited use” and “ongoing cycling.” Similar to FSW, the majority were in the Limited Use group(66%) and about a third were in the Ongoing Cycling group(34%). Among AGYW in the Limited Use group, 7% were on PrEP at one month and 2% were on PrEP in any subsequent month. Among AGYW in the Ongoing Cycling group, 85% were on PrEP at one month, 36% at 4 months, 16% at 7 months, and 7% at 10 months.(Figure 4)
Correlates of discontinuation
Among FSW, there was no definitive relationship between 1-month persistence and the number of initiations. Among AGYW, 1-month persistence was negatively associated with an increase in initiation, and this pattern was seen across all sites(Appendix Figure 2). An increase of 100 initiations per month was associated with a 2% decrease in 1-month persistence(−0.02 (95% CI: −0.03, −0.01).
For both populations in the adjusted models, older age was associated with lower likelihood of discontinuation. Among FSW, hazard of discontinuation was higher in 2017 and 2018 compared with 2016, but lower in all subsequent years (2019, 2020, and 2021) compared with 2016. Among AGYW, hazard of discontinuation was higher in 2019 and lower in 2020 compared with 2018. (Appendix Table 2).
DISCUSSION
In this study, we described longitudinal patterns of PrEP use among over 40,000 young women in South Africa participating in a real-world PrEP program. The number and proportion of women who initiated PrEP increased each year. The increase in initiations was sustained even during the early part of the COVID-19 pandemic. However, 1-month PrEP persistence was only 41% among FSW and 38% among AGYW. Re-initiations were more common among FSW than AGYW, but represented less than 10% of all individuals. The majority of both FSW and AGYW experienced “limited use” of PrEP, with few returning after the first month, but close to half of FSW and one third of AGYW experienced some form of cycling.
Across the study period, 19% of negative tests among FSW and 55% among AGYW resulted in initiation. Some possible explanations, as provided anecdotally by those delivering PrEP, for the lower levels of initiation seen among FSW include 1)FSW have been using condoms as a trusted prevention method and may not see the need to change or supplement this and 2)FSW experience unstable housing, which may challenge daily pill-taking.25 Additionally, because women can test multiple times each year(FSW are recommended to test quarterly) and because it includes those who are already on PrEP, the denominator overestimates the number eligible, and the proportion initiating in a given month is likely an underestimate of the proportion who ever initiated PrEP. Data on the proportion of eligible women who initiate PrEP in similar settings are limited. For FSW, PrEP uptake was similar to what was documented in a study of Zimbabwean FSW, including the increase in the proportion of initiations over time and the durability of increases to the COVID-19 pandemic.26 The proportion of eligible AGYW who initiated PrEP in our study was lower than in some studies conducted in highly-controlled trial settings and/or in population groups with potentially different motivations for PrEP(e.g. women engaged in antenatal care).16 27 However, the proportion of eligible AGYW initiating PrEP in the present study was comparable, if not slightly higher, to similar observational studies and demonstration projects.28–30
Similar to what has been previously demonstrated in varied settings in sub-Saharan Africa, persistence on PrEP among both FSW14 and AGYW15,31,32 was low. A recent study of similar programmatic data from the DREAMS Initiative in Kenya found that about 37% of 1259 AGYW persisted on PrEP at 3 months.31 This study of DREAMS AGYW data also identified heterogeneity across program sites and found that older age was associated with improved persistence.31 Another study of three JHPIEGO supported programs in Kenya, Lesotho, and Tanzania found that about half of the close to 50,000 individuals initiating PrEP ever returned.21
In our study, only 9% of FSW and 3% of AGYW re-initiated within one year. Though the present data source does not have data on motivation to use PrEP or risk perception, it is possible that FSW had a more established understanding of and reason for using PrEP and therefore returned at a higher frequency to restart.33,34
Many in our study population experienced irregular engagement in PrEP services which, based on our latent trajectory models, we defined as “early cycling” and “ongoing cycling.” While the data on 1-month persistence are disheartening, women are continuing to engage in PrEP use after this initial discontinuation. If we can distinguish between those women who may end up displaying patterns of early or ongoing cycling compared with those who have limited to no use, programs can implement differentiated systems of support or even consider making changes in who to initiate and when to do so. There have been few studies of PrEP use trajectories, and these have been in different populations, including racial and ethnic minorities in Chicago, USA20 and gay men in New South Wales35, or have used PrEP adherence as the primary outcome rather than PrEP persistence. In the two studies conducted in high-resource settings20,35, those who belonged to the “sustained use” group, or the “good” or “excellent” adherence groups made up the majority of the study population. This is very different from what we observed in our study population. This suggests that PrEP use trajectories may also be influenced by sociostructural, economic, and political factors. In a study of trajectories of adherence among 200 young women in a research setting in Cape Town, the authors identified two groups: 48% with low adherence and 52% with high early adherence.24 In this study, individuals initiating PrEP received regular adherence counseling.24 The latent groups identified do align with what we found among AGYW, but a larger proportion of our study population, closer to two-thirds, were in the low use group. There are no prior data on trajectories of PrEP use among FSW.
While the program created and utilizes a process to ensure some form of PrEP readiness prior to initiation in line with the South African National Guidelines12, further resources may be needed to comprehensively address multifactorial barriers36,37 to PrEP use, including patient-related barriers36,38,39 (awareness of PrEP, HIV and PrEP-related stigma, and readiness), clinic-level barriers36,39,40 (provider knowledge, adequate and friendly communication with clients, delivery and availability of refills), community-level barriers37,39 (social pressure, lack of awareness among partners, parents, and the community, and potential violence). Even with tailored adherence support, without a clear understanding and readiness on the part of the user in the context of other social and structural barriers, PrEP pills will go unused at a non-trivial cost to the program. There is a risk of the development of HIV drug resistance,41 with women starting on PrEP, but not maintaining a therapeutic dose.
There are some limitations of these analyses. First, individuals were characterized as FSW or AGYW based on which of the two programs they received services from. This decision led to 1608 women who were 25 years and older being placed in the AGYW group (5.7%, 1608/28,100). While these individuals would not normally be characterized as AGYW, often described as those 15–24 years old, we felt that this categorization was most appropriate as these women were being served by a program with AGYW as the intended target population. Second, for the analysis examining the proportion initiating over calendar time, data were missing for approximately 20% of the site-months among AGYW. Data on the number of women testing negative each month come from aggregated statistics captured in program registers. This indicator was not required for reporting to donors and was not always regularly inputted into the program register. The individual-level data feeding into these aggregate statistics were captured on paper logs, and where possible, we went back to obtain these numbers; there were some months for which these paper logs were no longer available. While we believed these data to be missing completely at random, we could not verify this assumption because of limited data availability, and some bias may have been introduced due to missing data. Finally, during the study period, the program shifted from monthly to multi-month dispensing. The details regarding this change have been described previously.22 For those months in which the woman had PrEP in her possession, but did not need to return for a visit, the PrEP register still documented that woman as being on PrEP. We therefore chose to keep our unit of analysis as monthly ability to use PrEP to ensure comparability across the years. Our measure of PrEP persistence should be comparable before and after the institution of multi-month dispensing, but if the measure of PrEP persistence was implicitly used as a proxy for actual pill-taking, it is possible that it would take longer to detect stopping of use with multi-month dispensing (would not know that they had been off PrEP until next scheduled pick-up visit). It should be noted that our measure of persistence does not imply adherence, which may be, and likely is, lower for many people. These results represent a best-case scenario for adherence given the fact that not all those who pick up their refills are taking pills at the level necessary to confer protection.
CONCLUSION
The results from these analyses reinforce that persistence on PrEP among young women at high-risk for HIV is low. We demonstrated that cycling on and off PrEP is common, with early missed visits and inconsistent, but ongoing use. The traditional approach to capturing and documenting formal discontinuation and re-initiation events may be obfuscating these important patterns of PrEP use, which are varied and may correspond to changes in actual or perceived risk or may be due to barriers to accessing PrEP. While we were unable to unpack individual-level characteristics of who specifically is represented in the different trajectory groups, better understanding of these varying patterns of PrEP use, including early and ongoing cycling, may help us tailor who is immediately started on PrEP and strategies to improve and support persistence. A push to start as many as possible on PrEP without consideration of 1) readiness or ability to stay on PrEP, and 2) a plan for providing clear persistence support, means that many, even a majority, of these initiations will prove futile.
Supplementary Material
Sources of support for this manuscript include:
National Institute of Mental Health: F31MH124458 (PI: Rao)
National Institute of Mental Health: R01MH121161 (PI: Schwartz)
National Institute of Allergy and Infectious Diseases: R01AI170249 (PI: Baral)
National Institute of Mental Health: K01MH129226 (PI: Rucinski)
References
- 1.UNAIDS. South Africa. 2022. https://www.unaids.org/en/regionscountries/countries/southafrica (accessed Oct. 1 2020.
- 2.Karim SSA, Baxter C. HIV incidence rates in adolescent girls and young women in sub-Saharan Africa. Lancet Glob Health 2019; 7(11): e1470–e1. [DOI] [PubMed] [Google Scholar]
- 3.Birdthistle I, Tanton C, Tomita A, et al. Recent levels and trends in HIV incidence rates among adolescent girls and young women in ten high-prevalence African countries: a systematic review and meta-analysis. Lancet Glob Health 2019; 7(11): e1521–e40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kilburn K, Ranganathan M, Stoner MCD, et al. Transactional sex and incident HIV infection in a cohort of young women from rural South Africa. AIDS 2018; 32(12): 1669–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stoner MCD, Nguyen N, Kilburn K, et al. Age-disparate partnerships and incident HIV infection in adolescent girls and young women in rural South Africa. AIDS 2019; 33(1): 83–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dellar RC, Dlamini S, Karim QA. Adolescent girls and young women: key populations for HIV epidemic control. J Int AIDS Soc 2015; 18(2 Suppl 1): 19408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ranganathan M, Heise L, Pettifor A, et al. Transactional sex among young women in rural South Africa: prevalence, mediators and association with HIV infection. J Int AIDS Soc 2016; 19(1): 20749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grant RM, Lama JR, Anderson PL, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med 2010; 363(27): 2587–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Van Damme L, Corneli A, Ahmed K, et al. Preexposure prophylaxis for HIV infection among African women. N Engl J Med 2012; 367(5): 411–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baeten JM, Donnell D, Ndase P, et al. Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. N Engl J Med 2012; 367(5): 399–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Department of Health. Republic of South Africa. Guidelines for the provision of pre-exposure prophylaxis (PrEP) to persons at substantial risk of HIV infection, 2020.
- 12.Bekker LG, Brown B, Joseph-Davey D, et al. Southern African guidelines on the safe, easy and effective use of pre-exposure prophylaxis: 2020. South Afr J HIV Med 2020; 21(1): 1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.van der Straten A, Stadler J, Montgomery E, et al. Women’s experiences with oral and vaginal pre-exposure prophylaxis: the VOICE-C qualitative study in Johannesburg, South Africa. PLoS One 2014; 9(2): e89118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Eakle R, Gomez GB, Naicker N, et al. HIV pre-exposure prophylaxis and early antiretroviral treatment among female sex workers in South Africa: Results from a prospective observational demonstration project. PLoS Med 2017; 14(11): e1002444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gill K, Pidwell T, Dietrich J, et al. A Demonstration Open Label Study to Assess the Acceptability, Safety and Use of Truvada Pre-exposure Prophylaxis in Healthy, HIV-Uninfected Adolescents, 15–19 Years of Age. Conference of the International AIDS Society. Paris, France; 2017. [Google Scholar]
- 16.Celum C, Hosek S, Tsholwana M, et al. PrEP uptake, persistence, adherence, and effect of retrospective drug level feedback on PrEP adherence among young women in southern Africa: Results from HPTN 082, a randomized controlled trial. PLoS Med 2021; 18(6): e1003670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gill K, Johnson L, Dietrich J, et al. Acceptability, safety, and patterns of use of oral tenofovir disoproxil fumarate and emtricitabine for HIV pre-exposure prophylaxis in South African adolescents: an open-label single-arm phase 2 trial. Lancet Child Adolesc Health 2020; 4(12): 875–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Celum CL, Bukusi EA, Bekker LG, et al. PrEP use and HIV seroconversion rates in adolescent girls and young women from Kenya and South Africa: the POWER demonstration project. J Int AIDS Soc 2022; 25(7): e25962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Underhill K, Guthrie KM, Colleran C, Calabrese SK, Operario D, Mayer KH. Temporal Fluctuations in Behavior, Perceived HIV Risk, and Willingness to Use Pre-Exposure Prophylaxis (PrEP). Arch Sex Behav 2018; 47(7): 2109–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pyra M, Brewer R, Rusie L, Kline J, Willis I, Schneider J. Long-term HIV Pre-exposure Prophylaxis Trajectories Among Racial & Ethnic Minority Patients: Short, Declining, & Sustained Adherence. J Acquir Immune Defic Syndr 2022; 89(2): 166–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Reed JB, Shrestha P, Were D, et al. HIV PrEP is more than ART-lite: Longitudinal study of real-world PrEP services data identifies missing measures meaningful to HIV prevention programming. J Int AIDS Soc 2021; 24(10): e25827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rao A, Mhlophe H, Comins C, et al. Persistence on oral pre-exposure prophylaxis (PrEP) among female sex workers in eThekwini, South Africa, 2016–2020. PLoS One 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nagin DS, Odgers CL. Group-based trajectory modeling in clinical research. Annu Rev Clin Psychol 2010; 6: 109–38. [DOI] [PubMed] [Google Scholar]
- 24.Stoner MCD, Rucinski KB, Giovenco D, et al. Trajectories of PrEP Adherence Among Young Women Aged 16 to 25 in Cape Town, South Africa. AIDS Behav 2021; 25(7): 2046–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kadiamada-Ibarra H, Hawley NL, Sosa-Rubi SG, Wilson-Barthes M, Franco RR, Galarraga O. Barriers and facilitators to pre-exposure prophylaxis uptake among male sex workers in Mexico: an application of the RE-AIM framework. BMC Public Health 2021; 21(1): 2174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Matambanadzo P, Busza J, Mafaune H, et al. “It went through the roof”: an observation study exploring the rise in PrEP uptake among Zimbabwean female sex workers in response to adaptations during Covid-19. J Int AIDS Soc 2021; 24 Suppl 6: e25813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Joseph Davey DL, Mvududu R, Mashele N, et al. Early pre-exposure prophylaxis (PrEP) initiation and continuation among pregnant and postpartum women in antenatal care in Cape Town, South Africa. J Int AIDS Soc 2022; 25(2): e25866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Koss CA, Charlebois ED, Ayieko J, et al. Uptake, engagement, and adherence to pre-exposure prophylaxis offered after population HIV testing in rural Kenya and Uganda: 72-week interim analysis of observational data from the SEARCH study. Lancet HIV 2020; 7(4): e249–e61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mayanja Y, Kamacooko O, Lunkuse JF, et al. Oral pre-exposure prophylaxis preference, uptake, adherence and continuation among adolescent girls and young women in Kampala, Uganda: a prospective cohort study. J Int AIDS Soc 2022; 25(5): e25909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Oluoch LM, Roxby A, Mugo N, et al. Does providing laboratory confirmed STI results impact uptake of HIV pre-exposure prophylaxis (PrEP) uptake among Kenyan adolescents girls and young women? A descriptive analysis. Sex Transm Infect 2021; 97(6): 467–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.de Dieu Tapsoba J, Zangeneh SZ, Appelmans E, et al. Persistence of oral pre-exposure prophylaxis (PrEP) among adolescent girls and young women initiating PrEP for HIV prevention in Kenya. AIDS Care 2021; 33(6): 712–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Celum CL, Mgodi N, Bekker L-G, Hosek S, Donnell D, Anderson P, Dye BJ, Pathak S, Agyei Y, Fogel JM, Marzinke MA, & Delany-Moretlwe S PrEP adherence and effect of drug level feedback among young African women in HPTN 082. 10th IAS Conference on HIV Science. Mexico City, Mexico; 2019. [Google Scholar]
- 33.Hill LM, Maseko B, Chagomerana M, et al. HIV risk, risk perception, and PrEP interest among adolescent girls and young women in Lilongwe, Malawi: operationalizing the PrEP cascade. J Int AIDS Soc 2020; 23 Suppl 3: e25502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shea J, Bula A, Dunda W, et al. “The Drug Will Help Protect My Tomorrow”: Perceptions of Integrating PrEP into HIV Prevention Behaviors Among Female Sex Workers in Lilongwe, Malawi. AIDS Educ Prev 2019; 31(5): 421–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jin F, Amin J, Guy R, et al. Adherence to daily HIV pre-exposure prophylaxis in a large-scale implementation study in New South Wales, Australia. AIDS 2021; 35(12): 1987–96. [DOI] [PubMed] [Google Scholar]
- 36.Pinto RM, Berringer KR, Melendez R, Mmeje O. Improving PrEP Implementation Through Multilevel Interventions: A Synthesis of the Literature. AIDS Behav 2018; 22(11): 3681–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Eakle R, Bourne A, Jarrett C, Stadler J, Larson H. Motivations and barriers to uptake and use of female-initiated, biomedical HIV prevention products in sub-Saharan Africa: an adapted meta-ethnography. BMC Public Health 2017; 17(1): 968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Goparaju L, Experton LS, Praschan NC, Warren-Jeanpiere L, Young MA, Kassaye S. Women want Pre-Exposure Prophylaxis but are Advised Against it by Their HIV-positive Counterparts. J AIDS Clin Res 2015; 6(11): 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kambutse I, Igiraneza G, Ogbuagu O. Perceptions of HIV transmission and pre-exposure prophylaxis among health care workers and community members in Rwanda. PLoS One 2018; 13(11): e0207650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pilgrim N, Jani N, Mathur S, et al. Provider perspectives on PrEP for adolescent girls and young women in Tanzania: The role of provider biases and quality of care. PLoS One 2018; 13(4): e0196280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dimitrov DT, Boily MC, Hallett TB, et al. How Much Do We Know about Drug Resistance Due to PrEP Use? Analysis of Experts’ Opinion and Its Influence on the Projected Public Health Impact. PLoS One 2016; 11(7): e0158620. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


