Abstract
This study reports an epidemiological assessment of laboratory-confirmed group A streptococcal meningitis cases in the Netherlands using more than 40 years of national bacteriological surveillance data.
Streptococcus pyogenes can cause a wide range of invasive infections, collectively referred to as invasive group A streptococcal infections. A rare but severe invasive group A streptococcal infection is meningitis, which has an estimated incidence in adults of 0.2 per 1 million individuals per year.1,2 In several European countries and the US, an increase of invasive group A streptococcal infections has been observed since September 2022, with shifts in affected age groups and clinical presentations relative to historic observations.3,4 We performed an epidemiological assessment of S pyogenes meningitis cases in the Netherlands, defined by culture-positive cerebrospinal fluid (CSF), using more than 40 years of national bacteriological surveillance data.
Methods
Active microbiological surveillance and molecular epidemiology of all-cause bacterial meningitis, including S pyogenes, is performed by the Netherlands Reference Laboratory for Bacterial Meningitis (NRLBM). We analyzed S pyogenes isolates cultured from CSF between January 1, 1982, and March 13, 2023. Typing of S pyogenes is based on sequence variation in 180 base pair of the emm gene and has been routinely performed since 2013 according to the US Centers for Disease Control and Prevention protocol.5 To distinguish between the recently identified toxicogenic M1UK variant and M1global strains,6 all emm1.0 isolates received between January 1, 2019, and December 20, 2022, were analyzed by whole-genome sequencing (Illumina HiSeq). Limited patient information was available with isolates; we analyzed municipality and change in age distribution over time. According to Dutch law (Medical Research Involving Human Subjects Act [WMO]), approval by a medical ethics committee was not necessary because cases were not subject to any actions or rules of conduct. No informed consent was requested and only anonymized data were used for the study.
Results
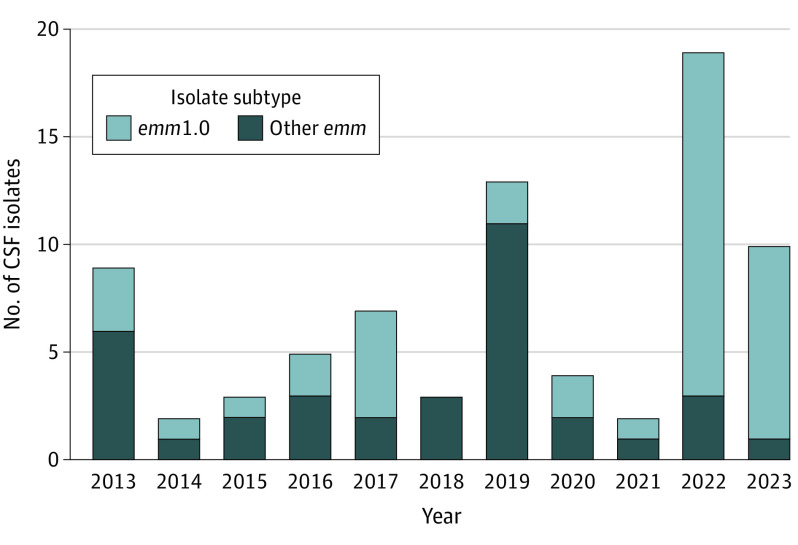
Between 1982 and 2021, the NRLBM received 216 S pyogenes CSF isolates, with an annual mean of 5 isolates (range 1-15). In contrast, 19 S pyogenes CSF isolates were received in 2022, and 10 isolates between January 1 and March 13, 2023.
Among the 48 CSF isolates from 2013-2021, 19 different emm (sub)types were distinguished, with emm1.0 being the dominant type at 35% (n = 17; Figure). However, from the 29 S pyogenes CSF isolates received between 2022 and March 13, 2023, 25 (86%) isolates were emm1.0 (Figure). Using whole-genome sequencing for emm1.0 isolates received between 2019 and December 20, 2022, 15 of 19 isolates (79%) belonged to the toxicogenic M1UK lineage, with all emm1.0 isolates received from May 2022 onward representing this variant. The 15 M1UK isolates originated from different municipalities, spread across the Netherlands. The number of emm1.0 strains by age group for patients 0 through 17 years was 5 in 2013-2021 vs 6 in 2022-2023; for patients 18 through 59 years, 6 in 2013-2021 vs 7 in 2022-2023; and for patients 60 years and older, 6 in 2013-2021 vs 11 in 2022-2023.
Figure. Number of Received Streptococcus pyogenes CSF Isolates With Proportion of emm1.0 Subtype, the Netherlands.
Data for 2023 reported through March 13. CSF indicates cerebrospinal fluid.
Discussion
Since 2022, an increase in S pyogenes meningitis, particularly caused by the emm1.0 type and M1UK variant, has been observed in the Netherlands. This study considered meningitis based on S pyogenes cultured from CSF to provide a consistent comparison over time. Study limitations include the exclusion of patients with meningitis with only a positive S pyogenes blood culture, resulting in an underestimation of the overall national occurrence of S pyogenes meningitis, and the small number of CSF isolates with limited patient information, which precluded more in-depth statistical and clinical evaluation. Furthermore, submission bias to the NRLBM may have played a role, given the increased general submission of S pyogenes isolates throughout 2022. Data from other countries are needed to assess whether the observed increase in S pyogenes meningitis is more widespread.
The overrepresentation of emm1.0 among the received CSF isolates underlines the invasiveness of this emm type. Moreover, the dominance of the toxicogenic M1UK variant among emm1.0 CSF isolates suggests replacement of circulating S pyogenes emm1.0 strains. Clinical studies are required to assess whether invasive group A streptococcal infections caused by the M1UK variant are more severe. Clinicians are urged to be vigilant regarding the occurrence of meningitis with S pyogenes because incidence with the recently emerged M1UK variant may be increasing.
Section Editors: Jody W. Zylke, MD, Deputy Editor; Kristin Walter, MD, Senior Editor.
Data Sharing Statement
References
- 1.Lucas MJ, Brouwer MC, Bovenkerk S, Man WK, van der Ende A, van de Beek D. Group A streptococcal meningitis in adults. J Infect. 2015;71(1):37-42. doi: 10.1016/j.jinf.2015.01.008 [DOI] [PubMed] [Google Scholar]
- 2.Kjærgaard N, Bodilsen J, Justesen US, et al. ; DASGIB Study Group . Community-acquired meningitis caused by beta-haemolytic streptococci in adults: a nationwide population-based cohort study. Eur J Clin Microbiol Infect Dis. 2019;38(12):2305-2310. doi: 10.1007/s10096-019-03678-w [DOI] [PubMed] [Google Scholar]
- 3.Holdstock V, Twynam-Perkins J, Bradnock T, et al. National case series of group A streptococcus pleural empyema in children: clinical and microbiological features. Lancet Infect Dis. 2023;23(2):154-156. doi: 10.1016/S1473-3099(23)00008-7 [DOI] [PubMed] [Google Scholar]
- 4.van Kempen EB, Bruijning-Verhagen PCJ, Borensztajn D, et al. Increase in invasive group A streptococcal infections in children in the Netherlands: a survey among 7 hospitals in 2022. Pediatr Infect Dis J. 2023;42(4):e122-e124. doi: 10.1097/INF.0000000000003810 [DOI] [PubMed] [Google Scholar]
- 5.CDC Streptococcus laboratory. Resources and protocols. Updated July 23, 2021. Accessed April 1, 2023. https://www.cdc.gov/streplab/groupa-strep/resources.html
- 6.Lynskey NN, Jauneikaite E, Li HK, et al. Emergence of dominant toxigenic M1T1 Streptococcus pyogenes clone during increased scarlet fever activity in England: a population-based molecular epidemiological study. Lancet Infect Dis. 2019;19(11):1209-1218. doi: 10.1016/S1473-3099(19)30446-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Sharing Statement