A central goal of the Academy of Breastfeeding Medicine (ABM) is the development of clinical protocols for managing common medical problems that may impact breastfeeding success. These protocols serve only as guidelines for the care of breastfeeding mothers and infants and do not delineate an exclusive course of treatment or serve as standards of medical care. Variations in treatment may be appropriate according to the needs of an individual patient. The ABM empowers health professionals to provide safe, inclusive, patient-centered, and evidence-based care. Pregnant and lactating people identify with a broad spectrum of genders, pronouns, and terms for feeding and parenting. There are two reasons ABM's use of gender-inclusive language may be transitional or inconsistent across protocols. First, gender-inclusive language is nuanced and evolving across languages, cultures, and countries. Second, foundational research has not adequately described the experiences of gender-diverse individuals. Therefore, ABM advocates for, and will strive to use language that is as inclusive and accurate as possible within this framework. For more explanation, please read ABM Position Statements on Infant Feeding and Lactation-Related Language and Gender (https://doi.org/10.1089/bfm.2021.29188.abm) and Breastfeeding As a Basic Human Right (https://doi.org/10.1089/bfm.2022.29216.abm).
Introduction
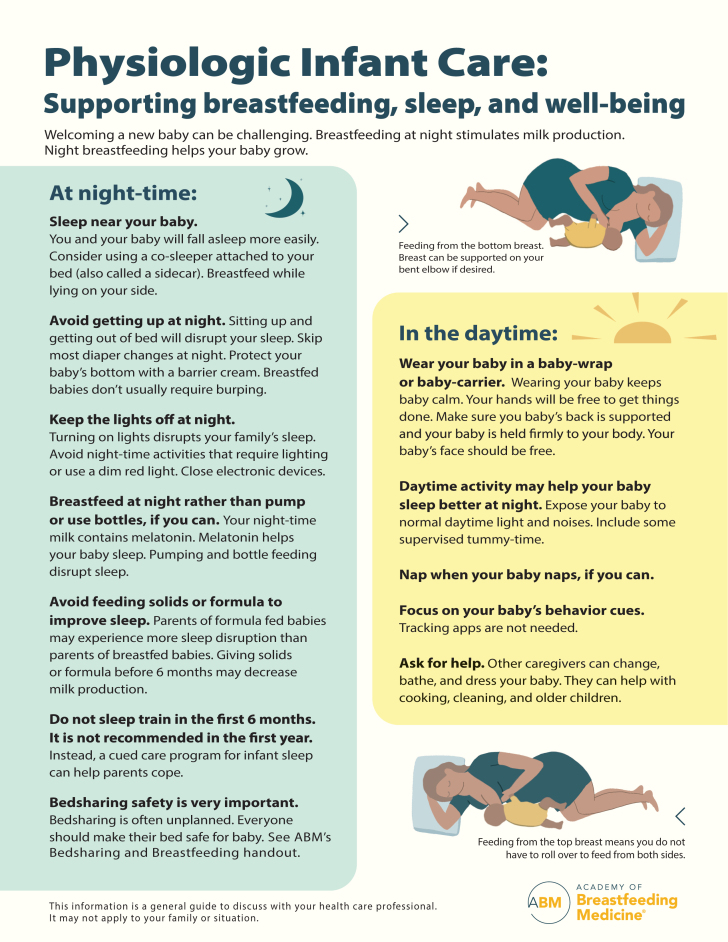
Having a newborn can be overwhelming, even for experienced parents. Infant feeding and getting sufficient sleep are among parents' biggest concerns. Young infants require frequent feedings day and night, particularly those who are breastfeeding. This can be a challenge to parents who are balancing other responsibilities such as work outside the home, caring for older children, and daily household responsibilities. The goal of this protocol is to address managing these challenges in the context of normal physiology for breastfeeding dyads.
Academy of Breastfeeding Medicine (ABM) Protocol #6 (Bedsharing and Breastfeeding),1 serves as an important adjunct to this protocol.
Key Information
Normal maternal–infant physiology
Normal infant feeding patterns
A newborn will breastfeed ∼8 to 12 times per 24 hours but not necessarily at regular intervals. Newborns need to breastfeed according to their feeding cues. As stated in the rationale to step 8 of the revised Baby-Friendly Hospital Initiative, “Breastfeeding involves recognizing and responding to the infant's display of hunger and feeding cues and readiness to feed, as part of a nurturing relationship between the mother and infant.”
Responsive feeding (also called on-demand or baby-led feeding) puts no restrictions on the frequency or length of the infant's feeds, and mothers are advised to breastfeed whenever the infant is hungry or as often as the infant wants, acknowledging that healthy infants self-regulate intake by combining nutritive with non-nutritive suckling.2 Feeding according to infant cues helps assure that an infant receives all the needed daily nutrition,3 as long as a minimum of eight feedings per 24 hours is met.
Once complementary foods are added at 6 months, the infant may be able to feed less often at night. However, when mothers work outside the home and express their milk while away from their infants, some dyads may engage in reverse-cycle feeding, directly breastfeeding more often during the night to make up for the mother's daytime absence. This direct stimulation by the infant at the breast helps maintain milk production. Intentionally limiting nighttime feeding is associated with early cessation of exclusive breastfeeding.4 Expressing milk is less efficient than direct breastfeeding, even with the most efficient breast pumps.5 Direct breastfeeding more often at night may thus help with maintaining milk production after returning to work.
Normal infant sleep patterns
Newborns are born without a functional circadian clock.6 Melatonin in breast milk is secreted and passed on to the infant in a circadian manner, helping to establish the infant's circadian rhythm.7 Being exposed to usual daytime activities, and their differentiation from nighttime activities, helps set an infant's circadian clock and lengthen their nighttime sleep periods. This includes daytime naps without artificially darkening the room or significantly reducing ambient noise.
Continuous proximity and skin-to-skin contact with the mother or other adult help the infant gradually transition to extrauterine life. Infants rely on proximity and skin-to-skin contact with their mothers to regulate their breathing, temperature, and heart rate in the early weeks and months of life.8–10 Mother–infant physical contact among breastfeeding dyads (bedsharing and baby-wearing) predicts maternal responsiveness to infant hunger cues, whereas proximity without physical contact does not.11 Responsive feeding, in turn, is associated with longer duration of exclusive breastfeeding.11
Nighttime separation from the mother in infants as old as 10 months can cause infant distress and elevated cortisol levels, even if the infant does not appear outwardly distressed.12 Furthermore, although nighttime separation during the first 4 months may be associated with longer periods of sleep consolidation in the infant13 and decreased night-time awakenings,14 this may not be physiological or safe, and partially explain why sleeping in proximity to the mother is associated with a decreased risk of sudden infant death syndrome (SIDS).15
Differences in sleep patterns may vary according to race/ethnicity as well as maternal education and household income. Some investigators have examined sleep patterns by race/ethnicity and other sociodemographic variables in an attempt to understand disparities in SIDS rates among certain U.S. groups. Results indicated that lower income and less education, not race/ethnicity, were associated with less sleep duration among dyads.16 These factors may be markers for stress, which may adversely affect sleep physiology.
After 12 to 16 weeks, the infant will spend more time awake, as the suprachiasmatic nucleus, based on external cues, begins to establish a circadian rhythm.17 The infant will be able to go longer stretches between feeds and will be able to feel comfortable outside immediate physical contact with their mother. However, their longest sleep periods may not markedly lengthen between 3 and 12 months, whether they are room sharing or sleeping solitary.18 Mothers may make up for their own nighttime sleep loss with daytime naps.19 However, their naps may not provide the same restorative value as nighttime sleep.20
Infants also benefit from being carried even when not feeding. A randomized controlled trial in a Western high-income setting showed that increased carrying of infants in arms or in a baby carrier with body contact (baby-wearing) was associated with a 43% reduction in fussing and crying at 6 weeks of age.21 Safe baby-wearing (see information)22 can also allow a mother to participate in other tasks. Infants who spend much of their day being carried may benefit from supervised “tummy time” to help achieve developmental motor goals.23
Challenges to physiological infant care
Expectations of sleeping through the night
In Western high-income countries, there is an expectation that a “good baby” should be able to sleep long stretches through the night from a very young age.7 The recommendation of exclusive breastfeeding for the first 6 months of life24 is often the social expectation, but is incompatible with the “good baby” expectation.
The scientific data show that expectations of prolonged infant sleep periods are unrealistic. Infant sleep measured by actigraphy (movement sensors) is similar from ages 4 to 16 weeks, regardless of the infant feeding method or location with respect to mother. However, Western mothers who exclusively formula feed perceive that their infants sleep longer, which reflects and reinforces the myth that it is “normal” for infants to sleep soundly for long periods.25 Parents in Western societies may experience distress and feel unprepared when their infants do not fit the expectation of readily falling asleep alone and staying asleep for long stretches from an early age.26
The mismatch between Western cultural family sleep expectations and the biological realities of human infants undermines parental resilience and compromises family well-being.7 In contrast to Western mothers, one study showed Japanese mothers do not perceive their sleep to be disturbed, despite the objective measures of infant-related sleep disruption being similar to those found in the U.S. studies of postpartum women who reported sleep disturbance.27
Studies have documented that infant's sleep patterns, although fragmented throughout the night, do not correlate with maternal sleep duration after 6 weeks postpartum.28 Breastfeeding infants sleep as well as or better than their formula feeding counterparts.19 A systematic review and meta-analysis demonstrated that breastfeeding may be associated with a longer nighttime sleep postpartum and that bedsharing was associated with longer sleep duration in breastfeeding mothers, compared with non-breastfeeding mothers.29
Expectations around solitary sleep
In Western high-income countries, there is an expectation that solitary infant sleep is standard and desirable. Bedsharing has been stigmatized and considered as uniformly unsafe, even in breastfeeding dyads without risk factors for sudden infant death. Parents in most Western countries have been advised against bedsharing since about 2004–2005,30 and strongly advised against any bedsharing since ∼2010, and many Western countries continue to advise against bedsharing. Other authorities began removing this recommendation after about 2014–2015.31,32 For example, in 2014 the U.K.'s National Institute for Health and Care Excellence advised that there was insufficient research evidence to unambiguously state cosleeping causes SIDS.
In 2016, PrevInfad in Spain gave a Level 1 recommendation that there is insufficient evidence that bedsharing is associated with an increased risk of SIDS in breastfeeding infants when there are no other risk factors.33 In 2019, the United Kingdom removed routine advice against bedsharing, regardless of feeding method.34–36 Australia adopted a risk minimization strategy in 2018, which acknowledges that many parents bedshare37 and some Canadian regional health authorities became more accepting of bedsharing after ∼2017.38,39
The advice against all bedsharing is still very influential in the United States and elsewhere, and continues to be the stance of the American Academy of Pediatrics.40 A famous 2011 U.S. advertising campaign, often cited, replaced a bedsharing mother with a meat cleaver. Mothers who bedshare can be accused of child abuse or neglect in some U.S. jurisdictions.41 In other words, the normative infant sleeping and feeding pattern is often viewed as aberrant, undesirable, or pathological.6,7
Scientific data show bedsharing to be associated with prolonged duration of any and exclusive breastfeeding.42–44 Sleep location is vital to feeding frequency.7 A growing body of anthropological research provides evidence that proximate mother–infant sleep combined with side-lying breastfeeding (“breastsleeping”)45 constitutes the human evolutionary norm.7 Bedsharing is associated with improved quality of child attachment and comforting for mother and infant.46 Bedsharing is common among U.S. infants47 and is common among breastfeeding Turkish infants.48
Aspects of bedsharing may be protective against sleep-related infant death. Proximate mother–infant sleep allows the mother to be immediately responsive to the infant, as demonstrated in physiological studies.12,49 Mothers and infants are both more arousable,49,50 and the mother forms a protective circle around the infant with her arms and legs, as her arm blocks the pillow from the infant (known as the C-position or “cuddle-curl”51). The infant's head is alongside the mother's breast, and after feeding the infant rolls onto their back, as bedsharing breastfeeding infants would not naturally sleep prone.52
By contrast, videographic evidence shows that mothers who bottle feed their infants may exhibit unsafe practices such as placing their infants to sleep on pillows.53 Furthermore, because bedsharing among breastfeeding dyads is so common, it can be difficult if not impossible to separate out the possible protective effects of bedsharing from the protective effects of breastfeeding. In other words, bedsharing confounds the protective effect of breastfeeding on SIDS, and thus could be responsible for some of the decreased risk of death associated with breastfeeding, when hazardous risks are absent.54
Direct breastfeeding at night has important physiological functions. In addition to the role of melatonin, breastfed infants who regularly bedshare feed more frequently than those who sleep solitary.55 More frequent feeding at night may help maintain milk production and is important for lactational amenorrhea.56 Infants' sleeping through the night is associated with a much lower rate of breastfeeding.57
Bedsharing affects maternal and infant sleep. Bedsharing breastfeeding mothers wake frequently to feed, are awake for shorter periods, and fall asleep more rapidly than breastfeeding mothers who do not bedshare.49 In a laboratory study of breastfeeding mothers, 94% of those who routinely bedshared reported they had obtained “enough” sleep after bedsharing, compared with 80% of routinely solitary sleeping mothers who reported enough sleep after solitary sleeping.49
Mothers who routinely slept solitary also rated their sleep quality as lower than bedsharing mothers.55 Bedsharing also promotes infant arousals,50 which may be protective against SIDS. Breastfeeding mothers sleep ∼40–45 minutes more than formula feeding mothers19 and fathers of breastfed infants sleep longer than fathers of formula-fed infant infants.58
In societies that follow this physiological norm, a typical nighttime behavior may consist of mothers and infants sleeping together, breastfeeding frequently, often with the mother not fully awake, and in the morning, the mother cannot say how often she breastfed.7,59 Infants and mothers immediately return to sleep after feedings. Note that infants fed this way are not burped after feeding; burping is rarely necessary in infants fed directly at the breast because they generally do not swallow air during feeding. Note also that infants are not awoken for diaper changes after every bowel movement at night. Research suggests that breastfeeding is associated with a lower risk of diaper dermatitis60,61 although not in all studies.62 Application of a barrier cream to the infant's diaper area helps prevent diaper dermatitis.63
ABM Protocol #6 discusses the evidence to date that bedsharing does not cause SIDS in the absence of hazardous circumstances, despite its association with SIDS,1,64 consistent with other national guidelines.34 A well-done case–control study found bedsharing in the absence of hazards to be protective in infants older than 3 months.64 ABM advises a risk-minimization approach to bedsharing and breastfeeding.1 Hazardous circumstances include, in order of importance: sofa sharing, sleeping with a parent who is impaired by alcohol or drugs, sleeping next to a smoker, sleeping in the prone position, never having initiated (direct) breastfeeding, sleeping in a chair with an adult, sleeping on soft bedding, or sleeping with an infant who is preterm or low birthweight.
Note that most of these circumstances are amenable to parental control. However, in some cases, bedsharing may be unplanned, in which case it is much more hazardous than when it is planned.65 If hazardous circumstances exist, alternatives such as a sidecar may be an option for some families.1 The risk of bedsharing is unknown in dyads who are fed by exclusive pumping, as infant positioning in bed for a breastfeeding dyad is uniquely related to the anatomical demands required for direct feeding and the mother's arms and legs form a safe environment for the infant.1
Concerns that waking to breastfeed may contribute to maternal depression
It has been hypothesized that disrupted sleep may contribute to the development and extent of postpartum depression symptoms.66 However, it is not clear whether postpartum sleep problems and mood disorders can be attributed to infant sleep and feeding, as they often existed in pregnancy. In addition, maternal sleep problems may be caused by anxiety and depression. Research showed that although there are significant correlations among maternal sleep and wake disturbance, fatigue, and depression at 32 weeks postpartum, they are not related to infant sleep patterns among Western mothers.67 Poor sleep maintenance, as measured by wrist actigraphy, is correlated with maternal depression, rather than maternal sleep duration.66
Poor sleep quality is also associated with worsening postpartum depression and anxiety in Western mothers.68 Subjective perception of sleep, rather than its objective quality, is associated with immediate and later postpartum mood disturbances.20,66 In a longitudinal study of Western mothers, pre-existing poor sleep quality, depression, and eating disorders during pregnancy were associated with worse breastfeeding outcomes, leading the authors to conclude that pre-existing sleep and mood disorders are the risk factors for poor breastfeeding outcomes and postpartum sleep disruption, and not that poor breastfeeding causes sleep disruption and postpartum mood disorders.69
Increased maternal depression and anxiety scores are also linked to decreased maternal sleep efficiency. In other words, maternal depression and anxiety are not related to the length of the infant's self-regulated sleep periods, but rather to problems with maternal sleep efficiency, or difficulty of the mother initiating or falling back to sleep.70 Sleep efficiency is related to anxiety and increased sympathetic tone, not to the number of times a mother wakes to feed.70
Nonetheless, one study in Western mothers showed increased infant feeding, and more disturbed infant sleep was correlated with increased maternal depression.28 A study in Japanese mothers suggested that breastfeeding frequency, subjective fatigue, and decreased objective total sleep time in the first days postpartum may be associated with higher scores on depression scales.71 It is notable that a comprehensive review and meta-analysis found a reduced risk of postpartum depression associated with breastfeeding.72
Nonphysiological coping strategies
Variations from the normal physiology of proximate mother–infant sleep while breastfeeding have the potential to undermine maternal well-being. Breastfeeding mothers may have different strategies to maximize their sleep and well-being while avoiding bedsharing. These strategies may include nocturnal pumping with bottle feeding, sleep training, formula feeding or early introduction of solids, and use of infant tracking apps, each of which has its own potential drawbacks. Often these strategies involve turning on lights, which markedly disrupt circadian rhythms73 of the whole family.
Night pumping
Nighttime pumping while feeding an infant a bottle of expressed milk would be expected to markedly disrupt maternal sleep. In addition, feeding milk pumped from a different time of day would not provide the appropriate level of melatonin. Circadian rhythms are not only disrupted by turning on lights, but by sitting up and engaging in any active activity.74
After feeding, a bottle-fed infant may require burping. If the infant is not sleeping next to their parent, further sleep disruption to parents and infant may occur, as the infant may not fall asleep readily while alone, and may require time for calming and soothing. Exclusively pumping is also associated with shorter breast milk feeding duration and earlier introduction of formula compared with feeding at the breast with or without pumping.75
Sleep training
A number of techniques are designed to condition infants and toddlers to sleep for longer periods at night.76 They are based on reducing the infant's expectation of a specific behavior associated with sleep onset and conditioning infants to “soothe themselves” back to sleep, alone, without adult intervention, when they have normal sleep cycle awakening.76,77 Training young infants to sleep alone by failing to respond to their crying in a distant crib causes significant infant stress, as indicated by elevated infant cortisol levels, which persist on the nights when the infant is no longer crying.12 Parents often experience distress at not responding to their infant's cries,78,79 and often find sleep training is not effective.79
Objective measures of infant sleep outcomes do not find that these methods “improve” the sleep of the infants who undergo this training. Infants cease to signal distress to their parents, but they do not cease to wake or remain awake, so they are not actually “soothing themselves back to sleep.”80,81 Sleep training in infants younger than 6 months of age can impact breastfeeding success due to separation from mother and reduced nighttime feedings.80 In addition, having the infant sleep in a separate room as part of sleep training strategy could be associated with an increased risk of SIDS.70
However, some studies show sleep training conducted under research conditions can be effective when the outcomes relate to maternal self-reported sleep outcomes, maternal reports of infant night waking, or maternal mental health.82 One randomized control trial of 14 infants76 showed no connection between graduated sleep interventions and emotional or behavioral problems 12 months later, but these results are too small to be generalizable.
Nonbreast milk feeding
In the pursuit of additional infant sleep, some mothers add or switch to formula to attempt to get more sleep.83,84 However, wrist actigraphy shows that parents of infants who were breastfed in the evening slept an average of 40–45 minutes more than parents who gave formula.19 Wrist actigraphy also showed that parents of infants giving formula reported more sleep disturbance than parents of exclusively breastfed infants.19 Data regarding early introduction of solids are mixed. A randomized clinical trial of infant cereal before bedtime did not show improved sleep.85
A randomized trial of early introduction to solid food at 3 months versus exclusive breastfeeding to 6 months showed an average of 17 minutes increased sleep time with solids, and fewer awakenings.86 However, in another study, there was no improvement in sleep at 1 year of age.87 Possible minimal increased sleep needs to be balanced against the possibility that adding early solids may interfere with the protective mechanisms to prevent SIDS, and lead to overweight88,89 and premature weaning.
Lighting at night
Lighting at night is disruptive to sleep and circadian rhythms.90 Blue light from digital devices (which has a short wavelength) has been found to suppress melatonin and disrupt sleep.91 Thus, activities at night that require lighting, such as pumping or changing diapers, should be minimized. Low-intensity red lighting (which has a long wavelength) has minimal effects on the sleep–wake cycle in mice,92 so may be useful for circumstances that require lighting.
Use of infant tracking apps and related digital technology
Although tracking apps used to monitor infant feeding and sleeping may be marketed with claims of reducing parental anxiety, they can paradoxically increase anxiety and reduce parent–baby interaction when observing the baby becomes replaced by checking the app.93 Apps and devices that allow parents to monitor infant sleep from afar normalize parent–infant separation and imply that some fundamental aspects of infant caregiving can be outsourced to technology.93
Supporting physiological infant care
Provider practices that support physiological infant care
Approaches such as the Possums Sleep Program, which are based on normal physiology, can help support parents.94,95 This type of approach is an infant-centered cued care program that can result in more consolidated sleep when used in infants over 6 months of age and does not negatively impact breastfeeding.96 Aggressive marketing of commercial milk formula has no place in the health care setting and can undermine breastfeeding and mothers' confidence.97,98 Encouraging the family to provide household help in a culturally expected manner has been shown to be a positive factor in preventing postpartum psychological distress.99
Social practices that support physiological care
Physiological infant care is best supported when mothers are able to take sufficient time off from work after giving birth to recover, establish breastfeeding, and bond with their infant. At least 12 weeks of paid leave is associated with improved maternal and infant health, decreased intimate partner violence, improved infant attachment and child development, decreased maternal and infant rehospitalizations, and increased initiation and duration of breastfeeding.100 Flexible work schedules are important for families with infants. Physiological infant care is also supported when partners are able to take time off from work to support the mother and bond with their infant.
Recommendations
For each recommendation, the quality of evidence (levels of evidence 1, 2, and 3) and the strength of recommendation (A, B, and C) are noted as defined by the strength of recommendation taxonomy criteria.101
1. Help parents understand normal physiology and to care for their infants in a responsive manner. It is important for health professionals to understand the normal physiological expectations and educate parents accordingly. Professional organizations should work to minimize the impact that advertising has on promoting nonphysiological practices.
Level of evidence: 2. Strength of recommendation: B.
2. In the absence of hazardous circumstances, mothers sleeping in proximity to their infants is recommended. Breastfeeding with proximate sleep in the absence of hazards may allow mothers to maximize their rest and well-being if sleep deprivation is a concern. Breastfeeding with proximate sleep may protect against sleep-related death, and is associated with responsive infant feeding and longer durations of any and exclusive breastfeeding.
Level of evidence: 2. Strength of recommendation: B.
3. Mitigate potential risks of bedsharing while allowing the infant to sleep within arms' reach. Using a sidecar attached to the adult bed if concerns exist for hazardous circumstances, or if hazardous circumstances could sometimes exist (e.g., if parents occasionally use alcohol or sedating substances).
Level of evidence: 2. Strength of recommendation: B.
4. Mitigate potential risks of bedsharing by teaching safe positioning in bed. Owing to lack of data for exclusively pumping dyads, it is unknown whether these dyads represent a hazardous circumstance for bedsharing. The C-position (cuddle curl) should be taught to exclusively pumping parents, recognizing that bedsharing is common and may occur unintentionally.
Level of evidence: 3. Strength of recommendation: C.
5. Avoid nonphysiological disruptions to maternal and infant nighttime sleep as strategies for improving parental well-being. These include nighttime pumping, bottle feeding, and placing the infant to sleep outside the parents' reach. Consider a dim red light if the need for lighting is anticipated.
Level of evidence: 2. Strength of recommendation: B.
6. Encourage the mother and infant to return to sleep without interruption after nighttime breastfeeding while bedsharing. Avoid burping the infant after breastfeeding, and avoid unnecessary diaper changes during the night. A barrier cream applied to the diaper area can help prevent diaper dermatitis.
Level of evidence: 2–3: Strength of recommendation: C.
7. Sleep training in approximately the first 6 months of life is contraindicated, and sleep training in the first year is not recommended. A cued care program for infant sleep may be a physiological-based alternative for parents who desire a sleep intervention.
Level of evidence: 2. Strength of recommendation: B.
8. Encourage the mother to sleep when the infant sleeps, when this is possible, and remind parents that not all sleep must occur during the nighttime hours.
Level of evidence: 2. Strength of recommendation: B.
9. Encourage the mother to get help with other household tasks so that she can focus on breastfeeding and caring for the infant.
Level of evidence: 2. Strength of recommendation: B.
10. Encourage the safe use of baby carriers during the day to promote physical contact with the infant. Baby-wearing can help mothers manage daytime tasks while keeping the infant calm.
Level of evidence: 1. Strength of recommendation: A.
11. Including some supervised “tummy time” may be important to help achieve developmental motor goals.
Level of evidence 2. Strength of recommendation: B
12. Avoid early introduction of solids or breast milk substitutes such as formula as a strategy to improve infant or maternal sleep. Avoid exposure to formula marketing materials in hospitals and health care settings.
Level of evidence: 2. Strength of recommendation: B
13. Encourage parents to directly monitor infant feeding and sleeping cues, and discourage use of tracking apps and monitoring devices for infant feeding and sleeping.
Level of evidence: 2, 3. Strength of recommendation: C.
14. Advocate for at least 12 weeks of paid maternity leave in countries that currently do not have it.
Level of evidence: 1. Strength of recommendation: A.
Summary
Compared with many strategies that mothers may use to cope with the demands of nighttime parenting, side-lying breastfeeding with proximate sleeping may be one of the safest strategies for maternal and infant well-being, in the absence of hazardous circumstances. Physiological research suggests that it may be protective for the infant,12,49,50,52 and if the natural physiology of proximate sleep is disrupted, these protections are lost. Accidental suffocation death is extremely rare among bedsharing breastfeeding infants in the absence of hazardous circumstances.1 Other coping strategies may have more overall adverse effects to mother and infant.
Areas for Future Research
More research is needed about physiological infant care, particularly in the context of diverse cultural beliefs and values. Research is needed into whether there is a role for pacifiers (dummies) in physiological infant care. Continued research into the optimal duration of paid leave for mothers and their partners would be helpful. More evidence is needed on the benefits of bedsharing and breastsleeping. It is known that breastfeeding is associated with a reduced risk of SIDS,15 but if this association is causal, it is unclear what aspects of breastfeeding are protective. It is likely that the protective effect is at least partially behavioral and not only from the milk itself, and if so, bedsharing would contribute to and confound the protective effectiveness of breastfeeding on SIDS.
More data on bedsharing in dyads who exclusively pump are necessary to ascertain their infants' risk of sleep-related death. More epidemiological and videographic data on an assortment of feeding methods, including in transgender parents, would be helpful. Finally, it would be vitally important to be able to consistently collect infant feeding data on all cases of sleep-related death.
Contributor Information
the Academy of Breastfeeding Medicine:
Elizabeth Stehel, Lawrence Noble, Melissa C. Bartick, Maria Enrica Bettinelli, Lori Feldman-Winter, Laura Kair, Ilse Larson, Yvonne LeFort, Nicole Marshall, Katrina Mitchell, Adora Okogbule-Wonodi, Susan Rothenberg, Tomoko Seo, Heidi Szugye, Gina Weissman, Nancy Wight, Michal Young, Gina Weissman, and Deena Zimmerman
Collaborators: the Academy of Breastfeeding Medicine
Authors' Contributions
All authors contributed to the conception and drafting of this article.
Disclosure Statement
No competing financial interests exist.
Funding Information
No funding was received for this article.
ABM protocols expire 5 years from the date of publication. Content of this protocol is up to date at the time of publication. Evidence-based revisions are made within 5 years or sooner if there are significant changes in the evidence.
Deena Zimmerman, MD, MPH, Lead Author
Melissa Bartick, MD, MS, MPH, FABM
Lori Feldman-Winter, MD, MPH, FABM
Helen L. Ball, PhD, Senior Author
The Academy of Breastfeeding Medicine Protocol,
Committee Members:
Elizabeth Stehel, MD, Chair
Lawrence Noble, MD, FABM, Translations Chair
Melissa C. Bartick, MD, MS, MPH, FABM
Maria Enrica Bettinelli, MD, FABM
Lori Feldman-Winter, MD, MPH, FABM
Laura Kair, MD, MAS, FABM
Ilse Larson, MD
Yvonne LeFort, MD, FABM
Nicole Marshall, MD, MCR
Katrina Mitchell, MD
Adora Okogbule-Wonodi, MD
Susan Rothenberg, MD, FABM
Tomoko Seo, MD, FABM
Heidi Szugye, DO
Gina Weissman, DMD
Nancy Wight, MD, FABM
Michal Young, MD, FABM
Gina Weissman, DMD
Deena Zimmerman, MD, MPH, FABM
References
- 1. Blair PS, Ball HL, McKenna JJ, et al. . Bedsharing and breastfeeding: The Academy of Breastfeeding Medicine protocol #6, revision 2019. Breastfeed Med 2020;15(1):5–16. [DOI] [PubMed] [Google Scholar]
- 2. World Health Organization. Protecting, Promoting, and Supporting Breastfeeding in Facilities Providing Maternity and Newborn Services: The Revised Baby-Friendly Hospital Initiative: Implemention Guidance. World Health Organization and UNICEF: Geneva; 2018. [Google Scholar]
- 3. Kent JC, Mitoulas LR, Cregan MD, et al. . Volume and frequency of breastfeedings and fat content of breast milk throughout the day. Pediatrics 2006;117(3):e387–e395. [DOI] [PubMed] [Google Scholar]
- 4. Vieira TO, Vieira GO, de Oliveira NF, et al. . Duration of exclusive breastfeeding in a Brazilian population: New determinants in a cohort study. BMC Pregnancy Childbirth 2014;14:175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Meier PP, Patel AL, Hoban R, et al. . Which breast pump for which mother: An evidence-based approach to individualizing breast pump technology. J Perinatol 2016;36(7):493–499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ball HL. The mother-infant sleep nexus: Night-time experiences in early infancy and later outcomes. In: Gowland R, Halcrow S, eds. The mother-infant nexus in anthropology: Small beginnings, significant outcomes. Springer: Cham, Switzerland; 2020. [Google Scholar]
- 7. Ball HL, Tomori C, McKenna JJ. Toward an integrated anthropology of infant sleep. Am Anthropol 2019;21(3):595–612. [Google Scholar]
- 8. Small MF. Our Babies Ourselves: How Biology and Culture Shape the Way We Parent. Doubleday Dell Publishing Group: New York, NY, USA; 1998. [Google Scholar]
- 9. Hrdy SB. Mother Nature: A History of Mothers, Infants, and Natural Selection. Ballantine: New York, NY, USA; 1998. [Google Scholar]
- 10. Moore ER, Bergman N, Anderson GC, et al. . Early skin-to-skin contact for mothers and their healthy newborn infants. Cochrane Database Syst Rev 2016;11:CD003519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Little EE, Legare CH, Carver LJ. Mother-infant physical contact predicts responsive feeding among U.S. breastfeeding mothers. Nutrients 2018;10(9):1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Middlemiss W, Granger DA, Goldberg WA, et al. . Asynchrony of mother-infant hypothalamic-pituitary-adrenal axis activity following extinction of infant crying responses induced during the transition to sleep. Early Hum Dev 2012;88(4):227–232. [DOI] [PubMed] [Google Scholar]
- 13. Paul IM, Hohman EE, Loken E, et al. . Mother-infant room-sharing and sleep outcomes in the INSIGHT study. Pediatrics 2017;140(1):e20170122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Messayke S, Franco P, Forhan A, et al. . Sleep habits and sleep characteristics at age one year in the ELFE birth cohort study. Sleep Med 2020;67:200–206. [DOI] [PubMed] [Google Scholar]
- 15. Thompson JMD, Tanabe K, Moon RY, et al. . Duration of breastfeeding and risk of SIDS: An individual participant data meta-analysis. Pediatrics 2017;140(5):e20171324. [DOI] [PubMed] [Google Scholar]
- 16. Yu X, Quante M, Rueschman M, et al. . Emergence of racial/ethnic and socioeconomic differences in objectively measured sleep-wake patterns in early infancy: Results of the Rise & SHINE study. Sleep 2021;44(3):zsaa193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Walker M. Why We Sleep: Unlocking the Power of Sleep and Dreams. Scribner: New York, NY, USA; 2017. [Google Scholar]
- 18. Volkovich E, Ben-Zion H, Karny D, et al. . Sleep patterns of co-sleeping and solitary sleeping infants and mothers: A longitudinal study. Sleep Med 2015;16(11):1305–1312. [DOI] [PubMed] [Google Scholar]
- 19. Doan T, Gardiner A, Gay CL, et al. . Breast-feeding increases sleep duration of new parents. J Perinat Neonatal Nurs 2007;21(3):200–206. [DOI] [PubMed] [Google Scholar]
- 20. Bei B, Milgrom J, Ericksen J, et al. . Subjective perception of sleep, but not its objective quality, is associated with immediate postpartum mood disturbances in healthy women. Sleep 2010;33(4):531–538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Hunziker UA, Barr RG. Increased carrying reduces infant crying: A randomized controlled trial. Pediatrics 1986;77(5):641–648. [PubMed] [Google Scholar]
- 22. American Academy of Pediatrics. Baby Carriers: Backpacks, Front Pback, and Slings. 2021. Available from: https://www.healthychildren.org/English/safety-prevention/on-the-go/Pages/Baby-Carriers.aspx [Last accessed: September 11, 2022].
- 23. Hewitt L, Kerr E, Stanley RM, et al. . Tummy time and infant health outcomes: A systematic review. Pediatrics 2020;145(6). [DOI] [PubMed] [Google Scholar]
- 24. World Health Organization. Infant and Young Child Feeding. 2021. Available from: https://www.who.int/news-room/fact-sheets/detail/infant-and-young-child-feeding [Last accessed: June 8, 2022].
- 25. Rudzik AEF, Ball HL. Biologically normal sleep in the mother-infant dyad. Am J Hum Biol 2021;33(5):e23589. [DOI] [PubMed] [Google Scholar]
- 26. Tomori C. Nighttime Breastfeeding: An American Cultural Dilemma. Berghahn Books, New York, NY, USA; 2014. [Google Scholar]
- 27. Nishihara K, Horiuchi S. Changes in sleep patterns of young women from late pregnancy to postpartum: Relationships to their infants' movements. Percept Mot Skills 1998;87(3 Pt 1):1043–1056. [DOI] [PubMed] [Google Scholar]
- 28. Sharkey KM, Iko IN, Machan JT, et al. . Infant sleep and feeding patterns are associated with maternal sleep, stress, and depressed mood in women with a history of major depressive disorder (MDD). Arch Womens Ment Health 2016;19(2):209–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Srimoragot M, Hershberger PE, Park C, et al. . Infant feeding type and maternal sleep during the postpartum period: A systematic review and meta-analysis. J Sleep Res 2022:e13625. [DOI] [PubMed] [Google Scholar]
- 30. American Academy of Pediatrics Task Force on Sudden Infant Death Syndrome. The changing concept of Sudden Infant Death Syndrome: Diagnostic coding shifts, controversies regarding the sleeping environment, and new variables to consider in reducing risk. Pediatrics 2005;116(5):1245–1255. [DOI] [PubMed] [Google Scholar]
- 31. NICE (National Instittue for Health Care Excellence). Addendum to Clinical Guideline 37, Postnatal Care. Routine Postnatal Care of Women and Their Babies. NICE: London; 2014. [PubMed] [Google Scholar]
- 32. Ball HL. Empowering families to make informed choices about sleep safety. Br J Midwifery 2015;23(3):164–165. [Google Scholar]
- 33. Sánchez Ruiz-Cabello FJ, Grupo PrevInfad/PAPPS. Sudden Infant Death Syndrome [in Spanish]. Asociación Española de Pediatría de Atención Primaria, Madrid; 2016. [Google Scholar]
- 34. NICE (National Institute for Health and Care Excellence). Postnatal Care [M] Benefits and Harms of Bed Sharing: NICE Guideline NG194. NICE: London, United Kingdom; 2021. [PubMed] [Google Scholar]
- 35. Lullaby Trust, Baby Sleep Info Source (Basis), Public Health England, UNICEF UK Baby-Friendly Hospital Initiative. Safer Sleep for Babies: A Guide for Parents. London; 2019. [Google Scholar]
- 36. UNICEF UK Baby-Friendly Hospital Initiative. Caring for Your Baby at Night. UNICEF UK: London, United Kingdom; 2022. [Google Scholar]
- 37. Red Nose National Scientific Advisory Group. Information statement: Sharing a sleep surface with a baby. Available from: https://rednose.org.au/article/sharing-a-sleep-surface-with-a-baby. [Last accessed: September 13, 2019].
- 38. Perinatal Services BC. Safer Sleep for My Baby: Helping Parents and Caregivers Create a Safer Sleep Plan. British Columbia Ministry of Health: Victoria; 2017. [Google Scholar]
- 39. Winnipeg Regional Health Authority. Safer Bed-Sharing. Available from: https://healthyparentingwinnipeg.ca/safer-bed-sharing/ [Last accessed: September 7, 2022].
- 40. Moon RY, Carlin RF, Hand I; Task Force on Sudden Infant Death Syndrome, the Committee on Fetus and Newborn. Sleep-related infant deaths: Updated 2022 recommendations for reducing infant deaths in the sleep environment. Pediatrics 2022;150(1):e2022057990. [DOI] [PubMed] [Google Scholar]
- 41. Editorial Board. Editorials: Infant death and DCFS: Is unsafe sleep abusive? Tribune Publishing, Chicago Tribune. 2017. Available from: https://www.chicagotribune.com/opinion/editorials/ct-edit-cosleep-dcfs-child-abuse-20171116-story.html. [Last accessed: June 8, 2022].
- 42. Huang Y, Hauck FR, Signore C, et al. . Influence of bedsharing activity on breastfeeding duration among US mothers. JAMA Pediatr 2013;167(11):1038–1044. [DOI] [PubMed] [Google Scholar]
- 43. Ball HL, Howel D, Bryant A, et al. . Bed-sharing by breastfeeding mothers: Who bed-shares and what is the relationship with breastfeeding duration? Acta Paediatr 2016;105(6):628–634. [DOI] [PubMed] [Google Scholar]
- 44. Bovbjerg ML, Hill JA, Uphoff AE, et al. . Women who bedshare more frequently at 14 weeks postpartum subsequently report longer durations of breastfeeding. J Midwifery Womens Health 2018;63(4):418–424. [DOI] [PubMed] [Google Scholar]
- 45. McKenna JJ, Gettler LT. There is no such thing as infant sleep, there is no such thing as breastfeeding, there is only breastsleeping. Acta Paediatr 2015;105(1):17–21. [DOI] [PubMed] [Google Scholar]
- 46. Barry ES, McKenna JJ. Reasons mothers bedshare: A review of its effects on infant behavior and development. Infant Behav Dev 2022;66:101684. [DOI] [PubMed] [Google Scholar]
- 47. Colson ER, Willinger M, Rybin D, et al. . Trends and factors associated with infant bed sharing, 1993–2010: The National Infant Sleep Position Study. JAMA Pediatr 2013;167(11):1032–1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Kural B, Gokcay G. Association between infant sleep location and breastfeeding. Breastfeed Med 2022;17(4):305–310. [DOI] [PubMed] [Google Scholar]
- 49. Mosko S, Richard C, McKenna JJ. Maternal sleep and arousals during bedsharing with infants. Sleep 1997;20(2):142–150. [DOI] [PubMed] [Google Scholar]
- 50. Mosko S, Richard C, McKenna JJ. Infant arousals during mother-infant bed sharing: Implications for infant sleep and sudden infant death syndrome research. Pediatrics 1997;100(5):841–849. [DOI] [PubMed] [Google Scholar]
- 51. Weissinger D, West D, Smith LJ, et al. . Sweet Sleep: Nighttime and Naptime Strategies for the Breastfeeding Family. Ballantine Books: New York, NY, USA; 2014. [Google Scholar]
- 52. Baddock SA, Purnell MT, Blair PS, et al. . The influence of bed-sharing on infant physiology, breastfeeding and behaviour: A systematic review. Sleep Med Rev 2019;43:106–117. [DOI] [PubMed] [Google Scholar]
- 53. Volpe LE, Ball HL, McKenna JJ. Nighttime parenting strategies and sleep-related risks to infants. Soc Sci Med 2013;79:92–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Bartick M, Young M, Louis-Jacques A, et al. . Bedsharing may partially explain the reduced risk of sleep-related death in breastfed infants. Front Pedatr 2022;10:1081028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. McKenna JJ, Mosko S, Richard C. Bedsharing promotes breastfeeding. Pediatrics 1997;100:214–219. [DOI] [PubMed] [Google Scholar]
- 56. Labbok MH, Hight-Laukaran V, Peterson AE, et al. . Multicenter study of the lactational amenorrhea method (LAM): I. Efficacy, duration, and implications for clinical application. Contraception 1997;55(6):327–336. [DOI] [PubMed] [Google Scholar]
- 57. Pennestri MH, Laganiere C, Bouvette-Turcot AA, et al. . Uninterrupted infant sleep, development, and maternal mood. Pediatrics 2018;142(6). [DOI] [PubMed] [Google Scholar]
- 58. Doan T, Gay CL, Kennedy HP, et al. . Nighttime breastfeeding behavior is associated with more nocturnal sleep among first-time mothers at one month postpartum. J Clin Sleep Med 2014;10(3):313–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Tomori C. Breastsleeping in four cultures: Comparative analysis of a biocultural body technique. In: Breastfeeding: New Anthropological Approaches. (Tomori C, Palmquist AE, Quinn E, eds.) Routledge: Abington, NY, USA; 2017:55–68. [Google Scholar]
- 60. Jordan WE, Lawson KD, Berg RW, et al. . Diaper dermatitis: Frequency and severity among a general infant population. Pediatr Dermatol 1986;3(3):198–207. [DOI] [PubMed] [Google Scholar]
- 61. Ersoy-Evans S, Akinci H, Dogan S, et al. . Diaper dermatitis: A review of 63 children. Pediatr Dermatol 2016;33(3):332–336. [DOI] [PubMed] [Google Scholar]
- 62. Li CH, Zhu ZH, Dai YH. Diaper dermatitis: A survey of risk factors for children aged 1–24 months in China. J Int Med Res 2012;40(5):1752–1760. [DOI] [PubMed] [Google Scholar]
- 63. Stamatas GN, Tierney NK. Diaper dermatitis: Etiology, manifestations, prevention, and management. Pediatr Dermatol 2014;31(1):1–7. [DOI] [PubMed] [Google Scholar]
- 64. Blair PS, Sidebotham P, Pease A, et al. . Bed-sharing in the absence of hazardous circumstances: Is there a risk of sudden infant death syndrome? An analysis from two case-control studies conducted in the UK. PLoS One 2014;9(9):e107799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Vennemann MM, Hense HW, Bajanowski T, et al. . Bed sharing and the risk of sudden infant death syndrome: Can we resolve the debate? J Pediatr 2012;160(1):44–48.e42. [DOI] [PubMed] [Google Scholar]
- 66. Park EM, Meltzer-Brody S, Stickgold R. Poor sleep maintenance and subjective sleep quality are associated with postpartum maternal depression symptom severity. Arch Womens Ment Health 2013;16(6):539–547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Thomas KA, Spieker S. Sleep, depression, and fatigue in late postpartum. MCN Am J Matern Child Nurs 2016;41(2):104–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Okun ML, Mancuso RA, Hobel CJ, et al. . Poor sleep quality increases symptoms of depression and anxiety in postpartum women. J Behav Med 2018;41(5):703–710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Stuebe AM, Meltzer-Brody S, Propper C, et al. . The Mood, Mother, and Infant Study: Associations between maternal mood in pregnancy and breastfeeding outcome. Breastfeed Med 2019;14(8):551–559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Douglas PS, Hill PS. Behavioral sleep interventions in the first six months of life do not improve outcomes for mothers or infants: A systematic review. J Dev Behav Pediatr 2013;34(7):497–507. [DOI] [PubMed] [Google Scholar]
- 71. Kawashima A, Detsuka N, Yano R. Sleep deprivation and fatigue in early postpartum and their association with postpartum depression in primiparas intending to establish breastfeeding. J Rural Med 2022;17(1):40–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Alimi R, Azmoude E, Moradi M, et al. . The association of breastfeeding with a reduced risk of postpartum depression: A systematic review and meta-analysis. Breastfeed Med 2022;17(4):290–296. [DOI] [PubMed] [Google Scholar]
- 73. Fisk AS, Tam SKE, Brown LA, et al. . Light and cognition: Roles for circadian rhythms, sleep, and arousal. Front Neurol 2018;9:56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Ortiz-Tudela E, Martinez-Nicolas A, Campos M, et al. . A new integrated variable based on thermometry, actimetry and body position (TAP) to evaluate circadian system status in humans. PLoS Comput Biol 2010;6(11):e1000996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Keim SA, Boone KM, Oza-Frank R, et al. . Pumping milk without ever feeding at the breast in the Moms2Moms study. Breastfeed Med 2017;12(7):422–429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Gradisar M, Jackson K, Spurrier NJ, et al. . Behavioral interventions for infant sleep problems: A randomized controlled trial. Pediatrics 2016;137(6):e20151486. [DOI] [PubMed] [Google Scholar]
- 77. Liu A. Sleep training. Pediatr Ann 2020;49(3):e101–e105. [DOI] [PubMed] [Google Scholar]
- 78. Davis AMB, Kramer RSS. Commentary: Does ‘cry it out’ really have no adverse effects on attachment? Reflections on Bilgin and Wolke (2020). J Child Psychol Psychiatry 2021;62(12):1488–1490. [DOI] [PubMed] [Google Scholar]
- 79. Loutzenhiser L, Hoffman J, Beatch J. Parental perceptions of the effectiveness of graduated extinction in reducing infant night-wakings. J Reprod Infant Psychol 2014;32(3):282–291. [Google Scholar]
- 80. Cassels T, Rosier J. The effectiveness of sleep training: Fact or fiction. Clin Lactation 2021;13(2):366–371. [Google Scholar]
- 81. D'Souza L, Cassels T.. Contextual considerations in infant sleep: Offering alternative interventions to families. Sleep Health 2022:S2352-7218(22)00077-8. [DOI] [PubMed] [Google Scholar]
- 82. Hohman EE, Savage JS, Marini ME, et al. . Effect of the INSIGHT firstborn parenting intervention on secondborn sleep. Pediatrics 2022;150(1):e2021055244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Ball HL. Breastfeeding, bed-sharing, and infant sleep. Birth 2003;30(3):181–188. [DOI] [PubMed] [Google Scholar]
- 84. Rudzik AEF, Ball HL. Exploring maternal perceptions of infant sleep and feeding method among mothers in the United Kingdom: A qualitative focus group study. Matern Child Health J 2016;20(1):33–40. [DOI] [PubMed] [Google Scholar]
- 85. Macknin ML, Medendorp SV, Maier MC. Infant sleep and bedtime cereal. Am J Dis Child 1989;143(9):1066–1068. [DOI] [PubMed] [Google Scholar]
- 86. Perkin MR, Bahnson HT, Logan K, et al. . Association of early introduction of solids with infant sleep: A secondary analysis of a randomized clinical trial. JAMA Pediatr 2018;172(8):e180739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Messayke S, Davisse-Paturet C, Nicklaus S, et al. . Infant feeding practices and sleep at 1 year of age in the nationwide ELFE cohort. Matern Child Nutr 2021;17(1):e13072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Almquist-Tangen G, Dahlgren J, Roswall J, et al. . Milk cereal drink increases BMI risk at 12 and 18 months, but formula does not. Acta Paediatr 2013;102(12):1174–1179. [DOI] [PubMed] [Google Scholar]
- 89. Woo Baidal JA, Locks LM, Cheng ER, et al. . Risk factors for childhood obesity in the first 1,000 days: A systematic review. Am J Prev Med 2016;50(6):761–779. [DOI] [PubMed] [Google Scholar]
- 90. Figueiro MG. Disruption of circadian rhythms by light during day and night. Curr Sleep Med Rep 2017;3(2):76–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Heo JY, Kim K, Fava M, et al. . Effects of smartphone use with and without blue light at night in healthy adults: A randomized, double-blind, cross-over, placebo-controlled comparison. J Psychiatr Res 2017;87:61–70. [DOI] [PubMed] [Google Scholar]
- 92. Zhang Z, Wang HJ, Wang DR, et al. . Red light at intensities above 10 lx alters sleep-wake behavior in mice. Light Sci Appl 2017;6(5):e16231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Ball HL, Keegan AA. Digital health tools to support parents with parent-infant sleep and mental well-being. NPJ Digit Med 2022;5(1):185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Whittingham K, Douglas P. Optimizing parent-infant sleep from birth to 6 months: A new paradigm. Infant Ment Health J 2014;35(6):614–623. [DOI] [PubMed] [Google Scholar]
- 95. Ball HL, Taylor CE, Thomas V, et al. . Development and evaluation of ‘Sleep, Baby & You’-An approach to supporting parental well-being and responsive infant caregiving. PLoS One 2020;15(8):e0237240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Ozturk M, Boran P, Ersu R, et al. . Possums-based parental education for infant sleep: Cued care resulting in sustained breastfeeding. Eur J Pediatr 2021;180(6):1769–1776. [DOI] [PubMed] [Google Scholar]
- 97. World Health Organization. Scope and Impact of Digital Marketing Strategies for Promoting Breast Milk Substitutes. WHO, Geneva; 2022. [Google Scholar]
- 98. World Health Organization. How the Marketing of Formula Milk Influences our Decisions on Infant Feeding. WHO, Geneva; 2022. [Google Scholar]
- 99. Gildner TE, Uwizeye G, Milner RL, et al. . Associations between postpartum depression and assistance with household tasks and childcare during the COVID-19 pandemic: Evidence from American mothers. BMC Pregnancy Childbirth 2021;21(1):828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Van Niel MS, Bhatia R, Riano NS, et al. . The impact of paid maternity leave on the mental and physical health of mothers and children: A review of the literature and policy implications. Harv Rev Psychiatry 2020;28(2):113–126. [DOI] [PubMed] [Google Scholar]
- 101. Ebell MH, Siwek J, Weiss BD, et al. . Strength of recommendation taxonomy (SORT): A patient-centered approach to grading evidence in the medical literature. J Am Board Fam Pract 2004;17(1):59–67. [DOI] [PubMed] [Google Scholar]