Abstract
Background:
The Burn Specific Health Scale-Brief (BSHS-B) evaluates 9 aspects of health and has been validated globally. Existing reports typically focus on outcomes shortly after injury. The purpose of this study is to determine whether quality of life remains a concern for burn survivors ten years after-injury.
Methods:
Cross sectional data of survivors admitted from 1994 to 2006 to four US burn centers were collected in the Burn Model System National Database 10 years after injury. Responses to the items in the nine BSHS-B domains range from 0 to 4. Lower scores indicating poorer quality of life. Median scores are reported and differences were compared using Wilcoxon–Mann–Whitney test.
Results:
Ten-year survivor injury characteristics suggest a moderate severity of injury. Survivors scored lower in heat sensitivity, affect, body image, and work (median=3.2, 3.6, 2.8, and 3.6, respectively). Affect, body image, and interpersonal scores were significantly lower for females (median=3.1, 2.8, 3.8, respectively) than males [median=3.6, 3.3, 4, respectively (p=0.008, 0.004, 0.022, respectively)].
Conclusions:
Our results suggest certain domains of burn specific health benefit from support at 10 years after injury, and select populations such as females may necessitate additional treatment to restore burn-specific health. These results support that burn injuries represent a chronic condition and long-term medical and psychosocial support may benefit burn survivor recovery.
Keywords: Burn Specific Health Scale, Longitudinal research, Burn injury, Rehabilitation
1. Introduction
Advances in burn care management and critical care have decreased mortality leading to greater emphasis in functional, social and psychological outcomes for burn survivors. Survivors often have complex multi-faceted rehabilitation issues, which result in significant short-term and long-term changes in quality of life. The World Health Organization (WHO) defines quality of life as: a state of complete physical, mental and social well-being and not just the absence of disease [1]. Burn injury outcomes have shifted from traditional measures of mortality and hospital length of stay to more specific functional and psychological outcomes [2]. Measuring the outcomes of burn survivors requires metrics such as quality of life instruments. The instruments to examine quality of life can be specific to burn injury or general for the population.
1.1. Burn Specific Health Scale (BSHS)
Initially developed in 1982, the Burn Specific Health Scale (BSHS) was intended to measure long-term outcomes of adult burn-injured survivors [3]. The initial version included 114 items and over time, the Burn Specific Health Scale was revised to address inconsistencies that were not initially addressed, such as work, pain, itching, and treatment regimens [4]. In the latest revision, the BSHS was simplified and shortened to 40 questions and renamed the Burn Specific Health Scale-Brief (BSHS-B). Each of the 40 questions fall within one of nine domains or sub-scales [5]. These domains are simple abilities (bathing or dressing), heat sensitivity (how bothersome is the sun or hot weather), hand function (writing name, eating with utensils, tying shoelaces), treatment regimens, (caring for the burn), work, body image (if appearance is bothersome), affect (feelings of sadness or loneliness), interpersonal relationships (specifically with family), and sexuality (interest in sex or sexual arousal). The BSHS-B has been validated in multiple languages and across different cultures, suggesting significant global utility [6,7].
The International Classification of Functioning, Disability, and Health bio-psycho-social framework from the WHO has been used to determine which health related quality of life (HRQOL) aspects are addressed by various self-reported instruments. Within this framework, the unique features of the BSHS-B are heat sensitivity, sexuality, treatment regimens and body image domains. Comparatively, the Medical Outcomes Trust 36-item short-form health survey (SF-36 or Short Form-36), one of the general quality of life instruments, does not include personal factors, which can affect quality of life for burn survivors [8,9]. Although generic HRQOL instruments, such as the Short Form-36, have been validated in the burn population [10], collectively measuring burn specific outcomes provides better understanding of the long-term effects of burn injury, allowing health care providers to focus on improving care in domains with worse reported outcomes [11]. HRQOL instruments also provide a frame of reference to measure outcomes of interventions and programs for burn survivors.
The purpose of this study is to report BSHS-B findings collected from burn survivors 16 years or older in the United States to determine the effects of injury on quality of life at ten years.
2. Methods
As part of the National Institute on Disability, Independent Living and Rehabilitation Research (NIDILRR) Burn Injury Model System (BMS) program, a comprehensive demographic, injury, and outcomes database was developed to facilitate the study of functional and psychosocial outcomes after burns [12,13]. This database has been used to report on the prevalence of pruritus at 5 and 10 years after injury, but not for other long-term quality of life indicators [14,15].
Data for the longitudinal burn injury database, including the BSHS-B, were collected prospectively via in-person interview, telephone interview or return mail and entered into an electronic, centralized database. BMS-funded institutions that provided data for analysis included Johns Hopkins University (Baltimore, MD), University of Texas Southwestern (Dallas, TX), University of Texas Medical Branch (Galveston, TX), and the University of Washington/Northwest Regional Burn Model System (Seattle, WA). Each BMS center maintains institutional Human Subjects Committee approval for the study. This report is from a cohort of burn survivors, injured between 1994 and 2006 who were followed at 10 years (±12 months) from their injury date. The eligibility criteria for this 10-year study included:
Enrollment in the Burn Model System research program at one of the four funded centers.
Age 16 years or older at the time of study participation.
Able to provide either verbal (via the telephone) or written (via return mailings) consent; parental consent (verbal or written) was required for minor subjects age 16–17 years.
The mean of the responses within each domain of the BSHS-B were calculated and used as the score for the survivor in that particular domain. Due to the non-normal distribution, the medians of each BSHS-B domains for the cohort were reported. Missing data were recorded as missing and no imputation was performed. Responses to the items in each domain range from 0 to 4 on a Likert scale with lower scores indicating poorer quality of life. Data analysis was performed using Stata 12.1 (College Station, TX). Differences in responses were compared using Wilcoxon–Mann–Whitney or Kruskal–Wallis test. Each burn center that provided data maintained IRB approval. The University of Washington Institutional Review Board approved this study.
3. Results
Ten-year survivor injury characteristics shown in Table 1 demonstrate a moderate severity of injury. The median burn size was 22% TBSA and the median burn size grafted was 14%, a surrogate for third degree burns. Two-thirds of the survivors were male and 38% of the survivors were less than 18 years of age at the time of injury. Only one survivor at 10 years was older than 65 years of age at the time of injury. Nearly 80% of the survivors were Caucasian, while the other survivors were primarily black. The most common cause of injury was fire and flame burns. Data on 93 survivors showed a median of 98 days to return to work or school after injury. Twenty seven of survivors had amputations due to the burn. Upon discharge, 77% of survivors went home or to someone’s home.
Table 1 –
Cohort characteristics.
| All (n=221) | Male (n=146) | Female (n=75) | p-Value | |
|---|---|---|---|---|
| Age at time of burn: median (IQR) | 26 (12–44) | 25 (14–44) | 31 (11–43) | 0.7272a |
| % Pediatric (age ≤18) at time of injury | 38% (85) | |||
| % TBSA burn: median (IQR) | 22 (11–43) | 23 (12–45) | 19 (9–39) | 0.1792a |
| % Inhalation injury (n) | 22% (47) | 20% (28) | 26% (19) | 0.277b |
| % Other injury (n) | 17% (37) | 16% (23) | 19% (14) | 0.583b |
| % Substance use | 2% (3) | 2% (2) | 2% (1) | 0.976b |
| % Male | 66% | |||
| Etiology of injury | 0.03c | |||
| Fire/flame/flash | 70% | 71% | 69% | |
| Scald/grease | 16% | 12% | 24% | |
| Contact/tar | 4% | 3% | 4% | |
| Chemical/electricity | 10% | 14% | 3% | |
| % Working at time of burn | 52% (114) | 58% (84) | 41% (30) | 0.012b |
| % TBSA grafted: median (IQR) | 14 (6–30) | 14 (7–30) | 11 (5–34) | 0.4223a |
| Length of stay: median in days, (IQR) | 24 (15–37) | 27 (17–37) | 20 (12–37) | 0.01a |
| % Amputation due to burn at discharge (n) | 13% (27) | 14% (19) | 11% (8) | 0.582b |
| Days to return to work, median (IQR) | 98 (64–214) | 98 (64–234) | 89 (55–197) | 0.4668a |
Wilcoxon rank sum.
Chi square test.
Fisher’s exact test.
Of the nine domains, median BSHS-B scores for all survivors within the cohort were higher for the hand function, simple abilities, sexuality, and interpersonal relationships domains and lower median scores were seen in the heat sensitivity, affect, body image, and work domains (Table 2). Stratifying by sex, median BSHS-B scores (Fig. 1) indicate that affect scores were lower for females (n=75, median=3.1, IQR: 2–3.9) than males (n=145, median=3.6, IQR: 3.0–4.0, p=0.008), body image scores were lower for females (n=74, median=2.8, IQR: 1.0–3.8) than males (n=144, median=3.3, IQR: 2.4–4, p=0.004), and interpersonal relationships scores were lower for females (n=75, median=3.8, IQR: 3.0–4.0) than males (n=144, median=4, IQR: 3.5–4.0, p=0.022). For the subset of survivors that were older than 18 at the time of injury, this effect is magnified with significant worse scores for adult females compared to males. In comparison, there was no difference in scores by sex in survivors that were younger than 18 at the time of injury (Table 3). Furthermore, there was no difference in BSHS-B scores in any domain between Hispanics and non-Hispanics or between races.
Table 2 –
Burn Specific Health Scale-Brief scores at 10 years after injury for cohort, (n=221).
| BSHS-B domain | Median (IQR) |
|---|---|
| Heat sensitivity | 3.0 (2.0–3.6) |
| Affect | 3.6 (2.8–4.0) |
| Hand function | 4.0 (3.6–4.0) |
| Simple abilities | 4.0 (3.7–4.0) |
| Sexuality | 4.0 (3.0–4.0) |
| Treatment regimens | 3.8 (3.2–4.0) |
| Body image | 3.0 (2.0–3.8) |
| Interpersonal relationships | 4.0 (3.5–4.0) |
| Work | 3.5 (2.8–4.0) |
Fig. 1 –
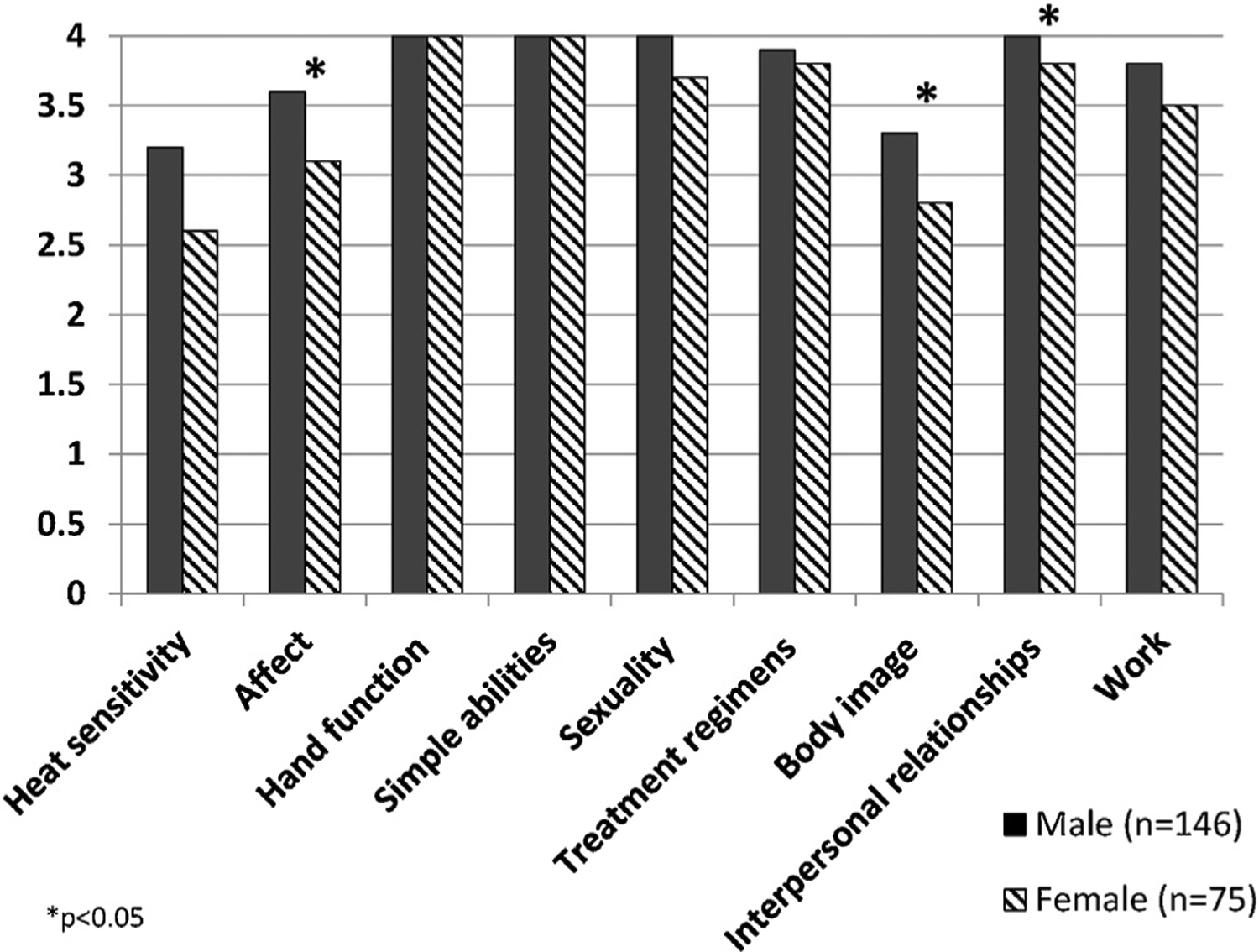
Burn Specific Health Scores-Brief 10 at years after injury stratified by sex.
Table 3 –
Burn Specific Health Scores-Brief scores at 10 years after injury stratified by age at time of injury.
| Adult (age > 18) | Pediatric (age < = 18) | p-Value | |
|---|---|---|---|
| Heat sensitivity | 3.0 (2.0–3.6) | 3.2 (2.0–3.8) | 0.19 |
| Affect | 3.4 (2.94.0) | 3.6 (2.7–4.0) | 0.56 |
| Hand function | 4.0 (3.6–4.0) | 4.0 (3.6–4.0) | 0.61 |
| Simple abilities | 4.0 (3.3–4.0) | 4.0 (3.7–4.0) | 0.69 |
| Sexuality | 3.7 (2.7–4.0) | 4.0 (3.7–4.0) | 0.0002* |
| Treatment regimens | 3.8 (3.2–4.0) | 4.0 (3.2–4.0) | 0.41 |
| Body image | 3.0 (1.8–3.8) | 3.4 (2.1–4.0) | 0.03* |
| Interpersonal relationships | 4.0 (3.5–4.0) | 4.0 (3.5–4.0) | 0.42 |
| Work | 3.5 (2.8–4.0) | 3.8 (3.0–4.0) | 0.38 |
p<0.05, Wilcoxon–Mann–Whitney.
Based on body location of the burn, survivors with head and neck burn injuries reported lower median scores for heat sensitivity and work than survivors without head and neck burns (heat sensitivity-median 2.8, IQR 1.8–3.6; work-median 3.3, IQR 2.8–4). However, this trend was not significant (p=0.06). Visibly grafted areas were defined as head/neck grafts, hand grafts, and foot grafts. Eighty two percent of the survivors had visible grafts. There was no difference in BSHS-B score in survivors with visible grafted areas compared to survivors without visible grafted areas, with the exception of hand function (Median 4.0, IQR: 4.0–4.0 vs median 4.0, IQR: 3.6–4.0, p=0.0008). Hand function was evaluated based on hand dominance. 80% of survivors were right hand dominant, 3.5% were left hand dominant and 1.5% were ambidextrous (14.6% were missing hand dominance). 53% of survivors experienced bilateral hand burns, 16% had right hand only burns, 7% had left hand only burns. In summary, 92.5% of survivors sustained burns of their dominant hand, and the median BSHS-B score for hand function was the same for survivors who had burns on their dominant hands, compared to those who did not sustain a burn to their dominant hand (Median 4, IQR: 3.6–4 vs Median 4, IQR: 3.8–4, p=0.49). Of the survivors, 133 (61%) underwent skin grafting of the hand and thirty-six survivors had hand burns that did not undergo grafting. These survivors had median hand function score of 4.0 (IQR: 4.0–4.0) compared to the survivors that underwent skin grafting had a median hand function score of 3.8 (IQR: 3.4–4.0, p=0.0002).
4. Discussion
This is the first report from individuals who are 10 years from injury using the nine domains of the Burn Specific Health Scale-Brief (BHSH-B) instrument and the Burn Model System (BMS) national database. The BMS database is supported by the National Institute of Disability, Independent Living, and Rehabilitation Research (NIDILRR) and has been in existence since 1994. This study identifies long-term effects on quality of life specific to a burn injury and can serve as benchmarks of health-related patient reported outcomes. By providing these data, future studies and interventions now have a frame of reference.
Previous studies have demonstrated that body image and sexuality are concerns at 12 months after injury. Our results suggest that females continue to have concerns about body image and interpersonal relationships at 10 years after injury, corroborating previous studies of body image issues in female burn survivors. Interestingly, this effect is not seen in survivors injured as children. One hypothesis may be that pediatric survivors have parents and siblings as a source of support whereas adults may not have similar support from family or friends.
Using several HRQOL instruments including the BSHS-B, Wasiak et al also concluded that health-related outcomes improved quicker for males at 12 months. Similar to this study, BSHS-B scores were significantly lower in females than males in the body image, affect, and interpersonal relationships domains. This effect on females is further supported with worse scores of the psychological aspect of generic instruments (Short Form-36 and Kessler Psychological Distress Scale) compared to males [16]. Similar dissatisfaction with body image, affect and interpersonal relationships was noted in our overall cohort further supporting that burns have a long term psychosocial affect. Female survivors may benefit from more long-term psychosocial support than male survivors and psychosocial health remains to be a problem even at 10 years after injury.
The visibility of the graft did not significantly affect the BSHS-B scores, with the exception of hand function. Hand function was affected by grafting, as one would expect more superficial hand burns to heal without grafting and likely affect hand function. Hand function is affected by more than visibility and hand dominance and additional studies are necessary to further identify how hand function impacts HRQOL.
Since this report is a cross sectional study of survivors and we do not know how their quality of life changed from the time from hospital discharge to 10 years after injury, the conclusions and interpretation of the data are limited to understanding quality of life at 10 years. Furthermore, this dataset is limited to four burn centers, which may not represent the general burn population. In addition, treatment of burn injury may have evolved over time and these results may not apply to more recently burned patients. There may also be response bias for the survey instruments. For example, only 6% (13 survivors) had self-reported substance abuse, but substance misuse has been reported to be as high as 34% in the burn population [20]. This difference may suggest that patients that have substance misuse may be difficult to follow up long-term. There may also be survival bias, as only one patient was over 65 years old (at the time of the injury) in our dataset.
5. Conclusion
Certain domains of health may continue to be affected for individuals long after burn injury, and select populations may warrant additional interventions targeting specific domains to restore health and quality of life. These results support the concept that burn injuries represent a chronic condition and long-term medical and psychosocial support may benefit burn survivor recovery. Furthermore, there is a need for measuring long-term recovery and quality of life in burn survivors to better understand how we can effectively help these individuals during their acute recovery.
Acknowledgments
The contents of this report were developed under a grant from the Department of Health and Human Services (HHS), National Institute on Disability, Independent Living and Rehabilitation Research (NIDILRR) grant numbers 90DP0029, 90DP0053, 90DP0035 and 90DPBU0001. NIDILRR is a Center within the Administration for Community Living (ACL), Department of Health and Human Services (HHS). The contents of this publication do not necessarily represent the policy of NIDILRR, ACL, HHS, and you should not assume endorsement by the Federal Government.
Abbreviations:
- BSHS-B
Burn Specific Health Scale-Brief
- HRQOL
Health related quality of life
- NIDILRR
National Institute on Disability, Independent Living and Rehabilitation Research
- BMS
Burn Model System
Footnotes
Conflict of interest
There are no conflicts of interest for any authors.
REFERENCES
- [1].Constitution of the World Health Organization. 1946.
- [2].Palmieri TL, Przkora R, Meyer WJ 3rd, Carrougher GJ. Measuring burn injury outcomes. Surg Clin North Am 2014;94 (4):909–16. [DOI] [PubMed] [Google Scholar]
- [3].Blades B, Mellis N, Munster AM. A burn specific health scale. J Trauma 1982;22(10):872–5. [DOI] [PubMed] [Google Scholar]
- [4].Yoder LH, Nayback AM, Gaylord K. The evolution and utility of the burn specific health scale: a systematic review. Burns 2010;36(8):1143–56. [DOI] [PubMed] [Google Scholar]
- [5].Kildal M, Andersson G, Fugl-Meyer AR, Lannerstam K, Gerdin B. Development of a brief version of the burn specific health scale (BSHS-B). J Trauma 2001;51(4):740–6. [DOI] [PubMed] [Google Scholar]
- [6].Mulay AM, Ahuja A, Ahuja RB. Modification, cultural adaptation and validation of burn specific health scale-brief (BSHS-B) for Hindi speaking population. Burns 2015;41(7):1543–9. [DOI] [PubMed] [Google Scholar]
- [7].Pishnamazi Z, Rejeh N, Heravi-Karimooi M, Vaismoradi M. Validation of the Persian version of the burn specific health scale-brief. Burns 2013;39(1):162–7. [DOI] [PubMed] [Google Scholar]
- [8].Meirte J, van Loey NE, Maertens K, Moortgat P, Hubens G, Van Daele U. Classification of quality of life subscales within the ICF framework in burn research: identifying overlaps and gaps. Burns 2014;40(7):1353–9. [DOI] [PubMed] [Google Scholar]
- [9].Ware JE Jr., Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 1992;30(6):473–83. [PubMed] [Google Scholar]
- [10].Edgar D, Dawson A, Hankey G, Phillips M, Wood F. Demonstration of the validity of the SF-36 for measurement of the temporal recovery of quality of life outcomes in burns survivors. Burns 2010;36(7):1013–20. [DOI] [PubMed] [Google Scholar]
- [11].Holavanahalli RK, Badger K, Acton A. Community reintegration. J Burn Care Res 2017;38(3):e632–4. [DOI] [PubMed] [Google Scholar]
- [12].Klein MB, Lezotte DL, Fauerbach JA, Herndon DN, Kowalske KJ, Carrougher GJ, et al. The National Institute on Disability and Rehabilitation Research burn model system database: a tool for the multicenter study of the outcome of burn injury. J Burn Care Res 2007;28(1):84–96. [DOI] [PubMed] [Google Scholar]
- [13].Goverman J, Mathews K, Holavanahalli RK, Vardanian A, Herndon DN, Meyer WJ, et al. The National Institute on Disability, Independent Living, and Rehabilitation Research burn model system: twenty years of contributions to clinical service and research. J Burn Care Res 2017;38(1):e240–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Amtmann D, McMullen K, Kim J, Bocell FD, Chung H, Bamer A, et al. Psychometric properties of the modified 5-D itch scale in a burn model system sample of people with burn injury. J Burn Care Res 2017;38(1):e402–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Carrougher GJ, Martinez EM, McMullen KS, Fauerbach JA, Holavanahalli RK, Herndon DN, et al. Pruritus in adult burn survivors: postburn prevalence and risk factors associated with increased intensity. J Burn Care Res 2013;34(1):94–101. [DOI] [PubMed] [Google Scholar]
- [16].Wasiak J, Lee SJ, Paul E, Shen A, Tan H, Cleland H, et al. Female patients display poorer burn-specific quality of life 12 months after a burn injury. Injury 2016;48(1):87–93. [DOI] [PubMed] [Google Scholar]
- [20].Rehou S, Mason S, MacDonald J, Pinto R, Jeschke MG. The influence of substance misuse on clinical outcomes following burn. Burns 2017;43(7):1493–8. [DOI] [PMC free article] [PubMed] [Google Scholar]


