Abstract
Objective
The aim of this study was to examine the processes involved in a guided self‐help (GSH) pre‐treatment intervention (RecoveryMANTRA) for patients with anorexia nervosa (AN), by measuring the levels of patient/mentor Language Style Matching (LSM). RecoveryMANTRA was supported by student mentors or peer mentors (recovered individuals) over six weekly chat‐based sessions. We examined whether LSM during RecoveryMANTRA predicted patients'working alliance with the clinic therapist, motivation, eating disorder (ED) and general psychopathology. A further aim was to examine differences in LSM between student mentors and peer mentors.
Method
87 AN adults received RecoveryMANTRA plus treatment as usual. The LSM algorithm was used to calculate verbal attunement between patient and mentor. Participants were assessed at baseline and at the end of the intervention.
Results
Both early (1st session) and late (6th session) LSM predicted higher working alliance with the clinic therapist. Moreover, late LSM predicted lower EDs symptoms at the end of the RecoveryMANTRA intervention. Patient/peer mentor dyads showed higher late verbal attunement than patient/student mentor dyads.
Conclusions
These findings suggests that in the early phase of treatment relational aspects can impact on engagement with treatment. Verbal attunement in a GSH for AN is associated with working alliance and better clinical outcome.
Keywords: anorexia nervosa, eating disorders, guided self‐help, language style matching, verbal synchrony, working alliance
Highlights
Language Style Matching (LSM) between patients and mentors in both the early and late phase of the RecoveryMANTRA intervention predicted higher working alliance with the clinic therapist.
LSM in the last phase (6th session) was associated with lower eating disorders (EDs) symptoms at the end of the RecoveryMANTRA intervention.
Patients/peer mentors dyads showed higher late LSM than patients/student mentors dyads.
Abbreviations
- ACMTQ
Autonomous and Controlled Motivation for Treatment Questionnaire
- AN
Anorexia nervosa
- BMI
Body Mass Index
- DASS‐21
Depression, Anxiety and Stress Scale
- DSM‐5
Diagnostic and Statistical Manual of Mental Disorders, 5th Edition
- EDE‐Q
Eating Disorder Examination Questionnaire
- EDs
Eating disorders
- GSH
Guided self‐help
- LIWC
Linguistic Inquiry and Word Count software
- LSM
Language Style Matching
- MANTRA
Maudsley Model of Treatment for Adults with Anorexia Nervosa
- MITI
Motivational Interviewing Treatment Integrity
- RCT
Randomized Controlled Trial
- SHARED
Self‐Help And Recovery guide for Eating Disorders
- TAU
Treatment as usual
1. INTRODUCTION
Anorexia nervosa (AN) is a dangerous ED characterized by food‐restriction and dramatic weight loss (American Psychiatric Association [APA], 2013). Its complex aetiology and prognosis lead to high mortality rates, risk of chronicity, relapse (Arcelus et al., 2011; van Hoeken & Hoek, 2020) and many comorbid psychiatric symptoms and diseases (Marucci et al., 2018). There is evidence that a failure to respond to outpatient treatment for AN in the early phase of the illness is associated with persistent symptoms and with the risk of developing an enduring and long‐lasting form of the illness (Nazar et al., 2017). This suggests that augmenting the early stage of therapy, may be a strategy to improve clinical outcomes (Lock et al., 2015; L’Insalata et al., 2020; Wade et al., 2021).
There has been a great deal of interest in using self‐help materials with and without guidance, as the first line of treatment in EDs. For the most part, this approach has been used for Bulimia Nervosa and Binge ED (Hötzel et al., 2014; Perkins et al., 2006), however a recent systematic review suggested that they might have beneficial effects for people with AN too, in terms of reducing drop‐out rates (Albano et al., 2019). Two studies examining the efficacy of short treatment modules to improve patient engagement with treatment as usual (TAU) in AN, found that brief interventions focused on psychoeducation and/or motivational enhancement were associated with greater treatment engagement compared to a comparison condition (Brewin et al., 2016; Denison‐Day et al., 2019). Also peer mentoring, used to augment TAU, was found to increase hope, support and engagement with treatment (Perez et al., 2014). Furthermore, a small pilot randomised study found that peer support produced enhanced clinical outcomes in adults with EDs (Ranzenhofer et al., 2020).
The Self‐Help And Recovery guide for Eating Disorders (SHARED) study is a randomized clinical trial testing whether a guided self‐care intervention (named RecoveryMANTRA) provided in addition to the treatment as usual (TAU; outpatient treatments varied between the participating EDs services, providing psychoeducation, individual or group therapies, and medical monitoring) can result in better outcome than TAU alone. RecoveryMANTRA was derived as a shortened version of the Maudsley Model of Treatment for Adults with Anorexia Nervosa (MANTRA) augmented with peer support through a library of videos. It consists of a 6 week guided self‐help (GSH) intervention targeting AN maintaining factors (cognitive, emotional, behavioural and social factors).
The Recovery MANTRA intervention was developed from an iterative process of co‐design and co‐production of written and digital/video materials with people with lived experience of EDs. In an early feasibility study, we found that a video clip including a meal support script written by someone with lived experience of the illness was more acceptable and effective at reducing anxiety than a psychoeducation script developed by a professional (Treasure et al., 2010) and after 3 months, their weight and engagement with the outpatient service had increased. In a later study, we augmented TAU with brief video‐clips developed by people with lived experience and found higher improvements in weight (medium sized increase in Body Mass Index (BMI), ES = 0.62; Z = −1.9; p = 0.05) and lower levels of ED symptoms and psychological distress over time (effect size range = 0.72/1.35) over 3 weeks (Cardi et al., 2013). In the SHARED trial (the subject of this paper) we included a larger library of peer participant produced recovery‐oriented materials. The guidance was provided by mentors (psychology graduate) and peer‐mentors (a person with lived experience of the illness) trained in motivational interviewing principles to enhance engagement (Cardi et al., 2015).
The primary and secondary outcome results from this trial were that people in RecoveryMANTRA+ TAU arm of the study experienced a greater reduction of anxiety and reported a greater working alliance with their clinic therapist, at the end of the 6 weeks (Cardi et al., 2020). In a study in which we examined the working alliance with the mentors we found that the working alliance during the RecoveryMANTRA sessions predicted a change in symptoms in the following session (Albano et al., 2021).
The aim of this study was to examine other process factors that may impact on patient outcome. There is substantial evidence that factors within the therapeutic relationship such as empathy can predict treatment outcome (Peluso & Freund, 2018; Wampold & Imel, 2015). In this study we assessed dyadic patient‐mentor processes through LSM. Language Style Matching is a largely unconscious process of verbal attunement whereby dyads spontaneously synchronise their word use (Gonzales et al., 2010; Niederhoffer & Pennebaker, 2002). This process can be measured through a LSM index (Ireland & Pennebaker, 2010) that reflects the degree of similarity in the use of so‐called function words (e.g. prepositions, conjunctions, articles, and other relatively content‐free parts of speech) in dyadic interactions. In the clinical setting, LSM has been applied to therapy sessions and there is promising evidence that it may tap into implicit aspects of the therapeutic relationship such as empathy, alliance and goal consensus (Aafjes‐van Doorn et al., 2020; Müller‐Frommeyer et al., 2019), which are significant predictors of outcome (Flückiger et al., 2018; Tryon et al., 2018). For example, language style synchrony between therapist and patient is an indicator of empathy (Lord et al., 2015), a metric of interpersonal synergy and an implicit measure of the alliance (Aafjes‐van Doorn et al., 2020). Moreover, preliminary evidence suggests that early LSM between the therapist‐patient dyad is associated with a greater symptom reduction at end of treatment (Aafjes‐van Doorn et al., 2020; Borelli et al., 2019). In addition, it can be expected that positive (corrective) experiences (e.g. through acceptance, empathy, validation) within the relationship with a mentor in RecoveryMANTRA contribute to a patient being better able to engage in a therapeutic relationship with a future therapist, for example, being more open and more likely to agree to favourable treatment goals. Finally, synchrony (reflecting empathy) between two people might be greater if these two people share the experience of having the same mental disorder. In the current study, we thus examined whether higher interpersonal verbal synchrony, between patient and mentor, possibly reflecting strong goal consensus and empathy, is associated with greater engagement and motivation for a follow‐up treatment as well as with reduced ED, depression and anxiety (DASS) symptoms, and whether synchrony is greater in patient‐peer dyads than in patient‐student dyads. The specific aims of the current study were to investigate: (1) whether greater patient‐mentor LSM at the early, middle and late phase of RecoveryMANTRA is associated with greater motivation for a follow‐up treatment (autonomous or controlled motivation to follow TAU) at the end of the RecoveryMANTRA (H1a) and with a better working alliance between the patient and the subsequent therapist delivering TAU (H1b). (2) whether greater LSM at the early, middle and late phase of RecoveryMANTRA is associated with fewer ED symptoms (EDE‐Q) (H2a) and lower levels of DASS (H2b) at the end of the RecoveryMANTRA; and finally, (3) whether LSM is greater in patient‐peer mentor than in patient‐student mentor dyads.
2. METHOD
2.1. Participants
For the purposes of the current study, we examined the sessions of participants allocated to the RecoveryMANTRA+TAU group only. Inclusion criteria for the trial were: (1) age ≥16 years, (2) assessed at one of the 22 participating UK specialist outpatient ED services, (3) diagnosis of AN or atypical AN according to the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM‐5; APA, 2013), (4) a BMI ≤ 18.5 kg/m2, and (5) with access to the Internet. Treatment as usual delivered by the participating centres consisted of outpatient treatment (including psychoeducation, symptom monitoring, psychotherapy) as recommended by the guidelines of the National Institute for Health and Care Excellence (NICE, 2017). More information about this study are reported in the protocol and main outcome papers (Cardi et al., 2015, 2019). Following an eligibility check and provision of informed consent to participate, patients were randomly allocated to RecoveryMANTRA+TAU (treatment arm) or TAU (control arm) only. Before randomisation, participants completed a baseline assessment consisting of self‐report questionnaires through the Ieso Digital Health platform.
2.2. RecoveryMANTRA+treatment as usual group (treatment arm)
Out of the 99 participants who were originally included in the RecoveryMANTRA + TAU group (Cardi et al., 2019), transcripts of RecoveryMANTRA sessions were available for 95 participants, as four participants chose not to start the online sessions for personal reasons. Two participants were identified as outliers and were subsequently excluded to improve the normality of data (see the Results section). The final sample consisted of 93 participants. Table 1 reports sociodemographic and clinical characteristics of the sample.
TABLE 1.
Participants' sociodemographic and clinical characteristics for the RecoveryMANTRA+Treatment as usual group
| Total group (n = 93) § | Patient/peer mentor (n = 39) | Patient/studentmentor (n =54) | |
|---|---|---|---|
| Age—Mean (SD) | 26.62 (8.63) | 26.35 (8.04) | 26.82 (9.10) |
| Sex (females)—F (%) | 90 (96.8) | 39 (100.0) | 51 (94.4) |
| Years of education—Mean (SD) | 15.51 (2.82) | 15.23 (2.92) | 15.72 (2.51) |
| Marital Status—F (%) | |||
| In a relationship/married/living together | 33 (35.5) | 16 (41.0) | 17 (31.5) |
| Single/separated | 47 (50.5) | 18 (46.2) | 29 (53.7) |
| Missing | 13 (14.0) | 5 (12.8) | 8 (14.8) |
| Duration of illness (years)—Mean (SD) | 7.41 (9.02) | 7.43 (7.88) | 7.38 (9.84) |
| Employment Status—F (%) | |||
| Part time | 17 (18.3) | 7 (17.9) | 10 (18.5) |
| Full time | 27 (29.0) | 12 (30.8) | 15 (27.8) |
| Housewife/sick leave/maternity leave/students/retired | 30 (32.3) | 16 (41.0) | 14 (25.9) |
| Missing | 19 (20.4) | 4 (10.6) | 15 (27.8) |
| Ethnicity—F (%) | |||
| White/Any other white background | 3 (3.2) | 1 (2.6) | 2 (3.7) |
| White/English/Welsh/Scottish/Northers Irish/British | 73 (78.5) | 33 (84.6) | 40 (74.1) |
| Mixed/Multiple ethnic group/white and black carribean | 1 (1.1) | ‐ | 1 (1.8) |
| White/Irish | 1 (1.1) | ‐ | 1 (1.8) |
| Asian/Asian British_Indian | 1 (1.1) | ‐ | 1 (1.8) |
| Missing | 14 (15.1) | 5 (12.8) | 9 (16.7) |
| Psychiatric medication (yes)—F (%) | 36 (38.7) | 17 (43.6) | 19 (35.2) |
| Previous hospital admission (yes)—F (%) | 20 (21.5) | 8 (20.5) | 12 (22.2) |
| Psychiatric comorbidity (yes)—F (%) | 18 (19.4) | 6 (15.4) | 12 (22.2) |
Note: Peer mentor = recovered patient from an eating disorder; Student mentor = a low trained professional. § Total RecoveryMANTRA + Treatment as usual group without participants who refused to start online GSH sessions (n = 4) and outliers (n = 2).
Twenty‐six individuals were involved as mentors to support the use of RecoveryMANTRA; 14 were postgraduate psychology students and 12 were peer mentors with lived experience of the illness (i.e. 10 people with past experience of an ED and two carers of people suffering from an ED). Patients were allocated to peer mentors/student mentors on the basis of mentors' availability; the maximum case load was three participants at any given time, per peer mentor/student mentor. Mentors provided guidance to a range of 1–13 participants/each (mean = 11.12; SD = 6.94). Student mentors assisted a total of 59 patients and peer mentors assisted a total of 40 patients through the trial. Participants were blinded to the type of mentor they were allocated.
The Recovery MANTRA resources consisted of a written workbook and a library of short videos clips. The workbook included psychoeducation about the maintaining factors of EDs and a discussion of behaviour change strategies (e.g. goal setting, anxiety management techniques). The video clips included recovery narratives from individuals with lived experience of an ED or psychoeducation about EDs. The RecoveryMANTRA resources aimed to increase confidence and motivation for treatment, through connectedness to others and hope. The use of these resources was guided by student mentors/peer mentors during online, chat‐based one‐hour sessions (one session/week, for 6 weeks).
Those with lived experience of the illness were asked not to dwell on their own specific experience during the intervention, but to refer to the lived experiences described in the workbook and video‐clips. Both student mentors and peer mentors received 3 days of training in the use of motivational interviewing and goal planning techniques, and supervision from professionals with experience in the assessment and treatment of EDs. Although the supervisor was aware of the experience of all of the mentors, this was not discussed in group settings. Transcripts of the text‐chat messages between mentors and participants were used for supervision and to assess treatment quality and fidelity. Student mentors/peer mentors were offered a small reimbursement for their time, which some chose not to take up.
2.3. Measures
At baseline and at the end of the 6‐week RecoveryMANTRA+TAU intervention, patients completed the 36‐item ED Examination Questionnaire (EDE‐Q; Fairburn & Beglin, 1994). Items are rated on a six‐point Likert scale, where higher scores indicate a greater level of eating pathology. The EDE‐Q includes four subscales (i.e., Restraint, Eating Concern, Shape Concern, and Weight Concern), but for the purpose on the present study only the total score was used. The EDE‐Q showed excellent internal reliability in previous studies (Luce & Crowther, 1999) and also in this study (Cronbach's alpha values: 0.912 and 0.925 at baseline and at the end of the 6 week RecoveryMANTRA+TAU intervention, respectively).
Moreover, at baseline and at the end of the 6‐week RecoveryMANTRA+TAU intervention, patients completed the 21‐item Depression, Anxiety and Stress Scale (DASS‐21; Lovibond & Lovibond, 1995) to assess symptoms of depression, anxiety and stress. Items are scored on a four‐point Likert scale, where higher scores indicate greater severity of symptoms. The DASS‐21 includes three subscales (i.e., anxiety, depression, and stress), but only the total score was considered in this study. The DASS‐21 showed excellent internal reliability in this study (Cronbach's alpha values: 0.912 and 0.923 at baseline and at the end of the 6‐week RecoveryMANTRA+TAU intervention, respectively).
At baseline, the BMI was reported by clinicians from the outpatient centres.
Working alliance with the outpatient therapist was assessed at 6 weeks. The assessment consisted of five single items adapted from the session rating scale used by Duncan et al. (2003) to measure bond and agreement on task. Items were scored on a 7‐point Likert scale. The items were: (1) How often do you feel like your therapist understands you? (2) How often do you feel confident that your therapist is pointing you in the right direction? (3) How often do you feel that you and your therapist are working toward mutually agreed upon goals? (4) How often do you trust your therapist? (5) How often do you feel that your therapist is offering you new ways of looking at your problem? (Cardi et al., 2015). A total score was computed as mean of the item scores (Cronbach's alpha value: 0.953).
Motivation for treatment was assessed at six weeks, using the 12‐item self‐report Autonomous and Controlled Motivation for Treatment Questionnaire (ACMTQ; Zuroff et al., 2007). This questionnaire includes two subscales: Autonomous Motivation (i.e. it refers to motivations with are driven by personal interest and internal incentives; e.g. ‘I feel personally satisfied when I follow my ED treatment’) and Controlled Motivation (it refers to external motivating factors for rewards and punishment, such as praise from others or avoidance of punishment; e.g. ‘I would be ashamed of myself if I didn't’). Items were rated on a seven‐point Likert scale ranging from 1 (strongly disagree) to 7 (strongly agree). The two subscales showed acceptable internal reliability (Cronbach's alpha values: 0.874 and 0.790 for Autonomous and Controlled Motivation, respectively).
Finally, LSM scores were calculated using the Linguistic Inquiry and Word Count software (LIWC; Pennebaker et al., 2007). The LIWC is an automated text analytic technique to examine linguistic features in clinical (e.g. therapy dialogues or patient narratives; Frattaroli, 2006; Lepore & Smith, 2002) and non‐clinical settings (Ireland et al., 2011; Ireland & Pennebaker, 2010; Niederhoffer & Pennebaker, 2002). LIWC generates percentages of total words in the text for nine function word categories. The basic‐level categories are: auxiliary verbs, articles, common adverbs, personal pronouns, indefinite pronouns, prepositions and relative pronouns, negations, conjunctions, and quantifiers (Gonzales et al., 2010). Separate LSM scores were calculated for each category of words using the formula (the numbers 1 and 2 refer to patient and therapist text, respectively): LSM preps = 1—(│preps1—preps2/(preps1+preps2)). The LSM scores could range from 0 to 1, with scores of 0.60 indicating relatively low and scores of 0.85 or larger indicating relatively high verbal synchrony (Cannava & Bodie, 2017).
2.4. Plan of data analyses
Transcripts of patient and student mentor/peer mentor sessions were downloaded from the online platform (http://www.iesohealth.com) and were segmented into patient and mentor scripts, producing two aggregate text files for each session (one for the patient and one for peer mentor/student mentor, respectively). The individual LSM scores for all nine function word categories were aggregated to calculate average LSM scores for each patient‐mentor dyad. Four hundred and sixty transcripts were analysed in total and for the purpose of this study early, mid and late sessions LSM scores (1st, 3rd and 6th sessions, respectively) were calculated.
Preliminary analyses were conducted to check for normality, univariate and multivariate outliers. The identification of univariate outliers was carried out by means of skewness, kurtosis (data with |Sk| > 2 and |Ku| > 7 were considered to present a severe violation of normality, as suggested by Hair et al., 2010 and Bryne, 2010) and boxplots (extreme outliers are defined as data values >3 IQR from the upper or lower ends of the box). Mahalanobis distance criterion (p < 0.001) was used to identify multivariate outliers (Kline, 1998). The internal consistency of the scales (Cronbach's α) was computed. Missing data were imputed by using the Expectation Maximization (Schafer, 1997) algorithm (Little's (1988) Missing Completely At Random test: χ2(46) = 61.340, p = 0.065). Moreover, repeated measures analyses of variance were computed to assess change between early, mid and late LSM, with time of measurement as within‐subject factor.
In order to test the first and the second hypotheses, hierarchical regressions were computed. In the first step, control variables (i.e. baseline EDE‐Q, DASS‐21 and BMI) were entered in the model and LSM was tested in the second step. To test the third hypothesis, independent samples t‐tests were calculated. The first hypothesis was tested controlling for relevant covariates (EDE‐Q, BMI and DASS‐21 at baseline), in order to take into account their relationships with working alliance with the outpatient therapist and motivation for TAU at the end of RecoveryMANTRA. This is in accordance with previous studies which supported the relationship between ED severity, depression, anxiety and motivation for treatment (Cardi et al., 2020; Ostiguy et al., 2017). Also, to test the second hypothesis, the relationship between LSM and EDs and mood symptoms was calculated controlling for baseline symptoms (EDE‐Q, BMI and DASS‐21) severity. Analyses were conducted using the Statistical Package for the Social Sciences software (SPSS, version 22.0).
3. RESULTS
3.1. Preliminary analyses
Analyses revealed a skewed distribution for mid LSM (Skewness = −6.533, kurtosis = 51.922). Two patients were identified as extreme univariate outliers (IQR >3; > 2SD from the mean) and were removed from the data matrix. All other variables had a normal distribution (Sk [−1.376; 0.068]; Ku [−0.342; 2.433]). Moreover, multivariate outliers were examined, with no violation noted. Thus, subsequent analyses were conducted on 93 participants (see Table 1 for participants' demographic and clinical characteristics).
Transcripts from 93 patients/student mentors‐peer mentors dyads were available for the first online session (early LSM); of these, transcripts for the third session were available for 83 dyads (89.2%; mid LSM) and transcripts for the sixth session were available for 62 dyads (66.7%; late LSM). Thus, cases with complete data on all time points totalled 62 (66.7%).
Referring to the cut‐off scores suggested by Cannava and Bodie (2017; see the Method section), there was high verbal attunement in the whole sample at each time point (early LSM: M = 0.853, SD = 0.048; mid LSM: M = 0.851, SD = 0.035; late LSM: M = 0.850, SD = 0.039), with stability across time (Wilks' Lambda = 0.998, F (2, 91) = 0.071, p = 0.932, η2 p = 0.002).
3.2. Relationships between language style matching scores and motivation and working alliance with the clinic therapist at the end of RecoveryMANTRA
No significant relationships were found between LSM and motivation (autonomous or controlled) (see Supporting Information S1). Hierarchical regression analyses (Table 2) indicated that, controlling for baseline EDE‐Q, DASS‐21 and BMI, higher early and late LSM were associated with greater working alliance with the clinic therapist.
TABLE 2.
Hierarchical regression analyses with working alliance with the outpatient therapist and eating disorder (ED) symptoms at the end of the 6‐week RecoveryMANTRA intervention (guided self‐help (GSH)) as dependent variables
| Adj R 2 | ΔR 2 | F | ΔF | B | SE | β | p | |
|---|---|---|---|---|---|---|---|---|
| DV: Working alliance with the outpatient therapist | ||||||||
| Step 1 | 0.138 | 0.166 | 5.904** | 5.904** | ||||
| EDE‐Q | 0.234 | 0.136 | 0.219 | 0.091 | ||||
| BMI | 0.135 | 0.078 | 0.167 | 0.088 | ||||
| DASS‐21 | −0.024 | 0.006 | −0.473 | 0.000 | ||||
| Step 2 | 0.206 | 0.075 | 6.983*** | 8.692** | ||||
| EDE‐Q | 0.232 | 0.131 | 0.217 | 0.080 | ||||
| BMI | 0.111 | 0.075 | 0.137 | 0.147 | ||||
| DASS‐21 | −0.022 | 0.006 | −0.431 | 0.001 | ||||
| Early LSM (1st session) | 6.832 | 2.317 | 0.278 | 0.004 | ||||
| DV: Working alliance with the outpatient therapist | ||||||||
| Step 1 | 0.138 | 0.166 | 5.904** | 5.904** | ||||
| EDE‐Q | 0.234 | 0.136 | 0.219 | 0.091 | ||||
| BMI | 0.135 | 0.078 | 0.167 | 0.088 | ||||
| DASS‐21 | −0.024 | 0.006 | −0.473 | 0.000 | ||||
| Step 2 | 0.235 | 0.102 | 8.063*** | 12.293** | ||||
| EDE‐Q | 0.168 | 0.130 | 0.158 | 0.198 | ||||
| BMI | 0.123 | 0.074 | 0.153 | 0.098 | ||||
| DASS‐21 | −0.020 | 0.006 | −0.395 | 0.002 | ||||
| Late LSM (6th session) | 9.985 | 2.848 | 0.326 | 0.001 | ||||
| DV: EDE‐Q | ||||||||
| Step 1 | 0.727 | 0.736 | 82.649*** | 82.649*** | ||||
| EDE‐Q | 0.709 | 0.076 | 0.670 | 0.000 | ||||
| BMI | 0.094 | 0.044 | 0.117 | 0.035 | ||||
| DASS‐21 | 0.012 | 0.004 | 0.245 | 0.001 | ||||
| Step 2 | 0.739 | 0.015 | 66.200*** | 5.187* | ||||
| EDE‐Q | 0.733 | 0.075 | 0.693 | 0.000 | ||||
| BMI | 0.098 | 0.043 | 0.122 | 0.024 | ||||
| DASS‐21 | 0.011 | 0.004 | 0.216 | 0.003 | ||||
| Late LSM (6th session) | −3.763 | 1.652 | −0.123 | 0.025 | ||||
Abbreviations: BMI, Body Mass Index at baseline; DASS‐21, Depression, Anxiety and Stress Scale at baseline; EDE‐Q, Eating Disorder Examination Questionnaire at baseline; LSM, Language Style Matching.
*p < 0.05, **p < 0.01, ***p < 0.001.
3.3. Relationships between language style matching scores and ED symptoms and levels of depression and anxiety after the end of RecoveryMANTRA+TAU intervention
Hierarchical regression analyses (Table 2) showed that higher late LSM were associated with lower ED symptoms at the end of RecoveryMANTRA. However, no significant relationships between LSM and levels of DASS were found (see Supporting Information S1).
3.4. A comparison of language style matching between patient/student mentor dyads and patient/peer mentor dyads
Figure 1 shows the differences in LSM scores between patient/student mentor and patient/peer mentor dyads. Small non‐significant differences were found between the groups regarding early (patient/peer mentor: M = 0.861, SD = 0.035; patient/student mentor: M = 0.847, SD = 0.056; t (91) = 1.47, p = 0.144, Cohen's d ES = 0.28) and mid (patient/peer mentor: M = 0.857, SD = 0.032; patient/student mentor: M = 0.847, SD = 0.037; t (91) = 1.389, p = 0.168, Cohen's d ES = 0.29) LSM scores between patient/student mentor and patient/peer mentor dyads (Figure 1). Patient/peer mentor dyads (M = 0.862, SD = 0.036) showed higher late LSM scores than patient/student mentor dyads (M = 0.843, SD = 0.039; t (91) = 2.410, p = 0.018, Cohen's d ES = 0.51).
FIGURE 1.
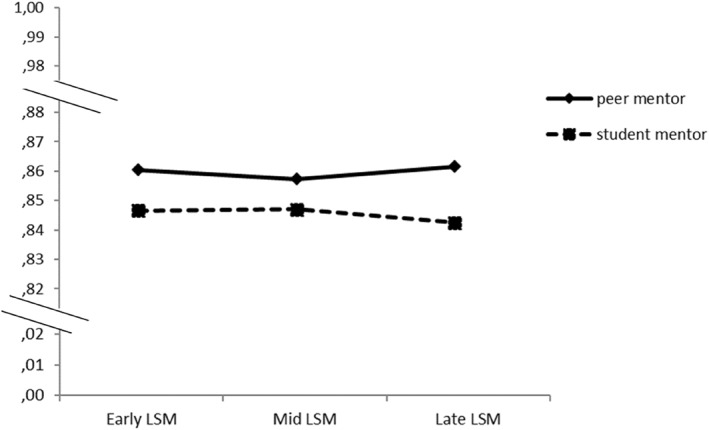
Overall level of Language Style Matching (LSM) in patient/mentor dyads at first (early LSM), third (mid LSM) and sixth (late LSM) sessions for student mentor and peer mentor separately. The LSM score ranges between 0 and 1, with scores of 0.85 or larger indicating relatively high verbal attunement (Cannava & Bodie, 2017)
4. DISCUSSION
This study examined attunement between patients and their mentors over the course of a pre therapy augmentation intervention (RecoveryMANTRA) and the impact on early engagement with therapy and early change. Both early (1st session) and late (6th session) LSM predicted a higher working alliance with the clinic therapist although no impact on motivation was found. Attunement at the end of RecoveryMANTRA predicted lower levels of EDs symptoms. Patient/peer mentor dyads had higher attunement of LSM scores than patient/student mentor dyads.
These findings support previous evidence that an early augmentation intervention for AN might enhance engagement with the outpatient therapist (Cardi et al., 2020). However, motivation was not improved. Nevertheless, these findings highlighted the importance of early patient processes for change in ED symptoms and aligns with previous finding that a poor early alliance with therapist and a weak collaborative relationship can be associated with a premature termination of treatment (Jordan et al., 2017; Traviss et al., 2013). This highlights the need to develop an early positive alliance with shared goals.
Language Style Matching did not predict the small reduction in anxiety previously reported in our primary analysis from the RecoveryMANTRA intervention (Cardi et al., 2019) and had no impact on depression. This aligns with the literature on self‐help interventions for AN in which a systematic review found limited improvements in anxiety and depression (Albano et al., 2019). It is possible that there needs to be more of an early focus on managing mood symptoms. For example, it is perhaps of interest that Transcanical Magnetic Stimulation (a treatments used for treatment resistant depression) was associated with an early change in affective psychopathology and an improvement in ED symptoms followed later (Dalton et al., 2018).
Our findings showed that the levels of verbal attunement between patient and mentor in online chat‐based sessions is influenced by characteristics of the mentor, with a higher level of late verbal synchrony for patients/peer mentors dyads than patients/student mentors dyads. This adds to the growing literature which suggests that people with lived experience may offer an invaluable contribution to the management of people with EDs (Lewis & Foye, 2021; Music et al., 2022). For example, peer mentorship can help patients to better face eating problems, fostering positive affect and reducing psychological distress (Ranzenhofer et al., 2020). Qualitative research suggested that mentorship may be particularly helpful for feeling understood and instilling hope on a positive recovery (Ramjan et al., 2017; Ramjan et al., 2018). In a recent intervention, aimed to help loved ones of people with EDs through lay and professional guidance, has been demonstrated how peer mentors become skilful over time reporting an increase in the own learning as the numbers of participants followed increases (MacDonald et al., 2014). Therefore, in this context an effective training, monitoring, supervision and the opportunity for career development may be necessary to optimize the quality of the intervention, Overall, the results of the current study provide preliminary evidence regarding the importance of LSM as a possible measure of the relational aspect of the mentor patient relationship when delivering online interventions (Kelders et al., 2012). However, some limitations must be considered. We did not measure process with a specific measurement of the technical quality of the Motivational Interviewing using a standardised assessment measure such as the MITI (Moyers et al., 2016). Also, we used a non‐standardized scale to assess working alliance with the clinic therapist. A more comprehensive assessment of working alliance might better represent the breadth of the construct, although brief assessments have many practical benefits for repeated measurements compared to longer questionnaires, and our measure demonstrated excellent internal consistency in the current study. Moreover, there is some evidence that Visual Analogue Scale scales may partially mitigate the ceiling effect which was shown for self‐report working alliance measures (van Haaren et al., 2021; Voutilainen et al., 2016). In terms of data completeness, it is worth noting that a number of patients missed some of the sessions of online guidance, and a participant selection bias cannot be excluded. Finally, the study had limited power to examine differences in the characteristics of the mentors/peer mentors assigned to participants. Future research in the field is needed to provide more available information on mentors, to investigate differences and specific impact they can generate on the process of therapeutic change of patients (Albano et al., 2021).
5. CONCLUSIONS
This study has shown that aspects of the therapeutic relationship with adults with an ED are associated with outcomes. Language Style Matching can be used as a marker of the therapeutic process of interventions for AN. Characteristics of the supporter (lived experience) may impact on the therapeutic process and outcomes. It may be important to focus on change in affective symptoms as well as ED symptoms in the early phase of therapy to improve outcomes.
Considering the findings of this study a more extended periods of guidance and a greater focus on interpersonal elements might provide more data on the therapeutic process of change. Guidance provided by peer mentors may encourage the use of self‐help materials and also contribute to the development of a recovery identity (Leamy et al., 2011). Based on these premises, another large RCTs in progress (Cardi et al., 2017), aimed to test online GSH for patients of AN and their carers wanted to facilitate the transition from intensive hospital treatment into the community fostering the role of social connection by improving patient‐to‐patient support and support from carers.
CONFLICT OF INTEREST
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supporting information
Supporting Information S1
ACKNOWLEDGEMENTS
We are grateful to the recovered individuals who contributed to the video‐clips used in the RecoveryMANTRA intervention and to Scarlet Park and Elise Pacquette, who contributed illustrations for the workbook. We acknowledge the support of the National Institute for Health Research Clinical Research Network (NIHR CRN) and are very grateful to our participating clinical services and local collaborators for their help with participants' recruitment and data collection. We are also grateful to National Institute for Health Research (NIHR) under its Research for Patient Benefit (RfPB) Programme (Grant Reference Number PB‐PG‐0712‐28041). The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care. This work was also supported by the Psychiatry Research Trust, the National Institute for Health Research (NIHR) Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King's College London (VC and JT). VC is supported by a grant from MIUR (Dipartimenti di Eccellenza DM 11/05/2017 n. 262) to the Department of General Psychology at the University of Padova, Italy. The views expressed herein are not necessarily those of the NHS, NIHR or the Department of Health.
Open Access Funding provided by Universita degli Studi di Palermo within the CRUI‐CARE Agreement.
Albano, G. , Salerno, L. , Cardi, V. , Brockmeyer, T. , Ambwani, S. , Treasure, J. , & Lo Coco, G. (2023). Patient and mentor language style matching as a predictor of working alliance, engagement with treatment as usual, and eating disorders symptoms over the course of an online guided self‐help intervention for anorexia nervosa. European Eating Disorders Review, 31(1), 135–146. 10.1002/erv.2948
Gaia Albano and Laura Salerno are the joint first authors.
DATA AVAILABILITY STATEMENT
The dataset generated for this study is available on request to the corresponding author.
References
- Aafjes‐van Doorn, K. , Porcerelli, J. , & Müller‐Frommeyer, L. C. (2020). Language style matching in psychotherapy: An implicit aspect of alliance. Journal of Counseling Psychology, 67(4), 509–522. 10.1037/cou0000433 [DOI] [PubMed] [Google Scholar]
- Albano, G. , Cardi, V. , Kivlighan, D. M., Jr. , Ambwani, S. , Treasure, J. , & Lo Coco, G. (2021). The relationship between working alliance with peer mentors and eating psychopathology in a digital 6‐week guided self‐help intervention for anorexia nervosa. International Journal of Eating Disorders, 54(8), 1519–1526. Advance online publication. 10.1002/eat.23559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albano, G. , Hodsoll, J. , Kan, C. , Lo Coco, G. , & Cardi, V. (2019). Task‐sharing interventions for patients with anorexia nervosa or their carers: A systematic evaluation of the literature and meta‐analysis of outcomes. International Review of Psychiatry, 31(4), 367–381. 10.1080/09540261.2019.1588711 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Author. [Google Scholar]
- Arcelus, J. , Mitchell, A. J. , Wales, J. , & Nielsen, S. (2011). Mortality rates in patients with anorexia nervosa and other eating disorders: A meta‐analysis of 36 studies. Archives of General Psychiatry, 68(7), 724–731. 10.1001/archgenpsychiatry.2011.74 [DOI] [PubMed] [Google Scholar]
- Borelli, J. L. , Sohn, L. , Wang, B. A. , Hong, K. , DeCoste, C. , & Suchman, N. E. (2019). Therapist‐client language matching: Initial promise as a measure of therapist‐client relationship quality. Psychoanalytic Psychology, 36(1), 9–18. 10.1037/pap0000177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewin, N. , Wales, J. , Cashmore, R. , Plateau, C. R. , Dean, B. , Cousins, T. , & Arcelus, J. (2016). Evaluation of a motivation and psycho‐educational guided self‐help intervention for people with eating disorders (MOPED). European Eating Disorders Review, 24(3), 241–246. 10.1002/erv.2431 [DOI] [PubMed] [Google Scholar]
- Bryne, B. M. (2010). Structural equation modeling with AMOS: Basic concepts, applications and programming (multivariate applications series) (Vol. 396). Taylor & Francis Group. [Google Scholar]
- Cannava, K. , & Bodie, G. D. (2017). Language use and style matching in supportive conversations between strangers and friends. Journal of Social and Personal Relationships, 34(4), 467–485. 10.1177/0265407516641222 [DOI] [Google Scholar]
- Cardi, V. , Albano, G. , Ambwani, S. , Cao, L. , Crosby, R. D. , Macdonald, P. , Schmidt, U. , & Treasure, J. (2019). A randomised clinical trial to evaluate the acceptability and efficacy of an early phase, online, guided augmentation of outpatient care for adults with anorexia nervosa. Psychological Medicine, 16(15), 1–12. 10.1017/S0033291719002824 [DOI] [PubMed] [Google Scholar]
- Cardi, V. , Albano, G. , Salerno, L. , Lo Coco, G. , Ambwani, S. , Schmidt, U. , Macdonald, P. , & Treasure, J. (2020). The feasibility of using guided self‐help in anorexia nervosa: An analysis of drop‐out from the study protocol and intervention adherence. Frontiers in Psychology, 11, 707. 10.3389/fpsyg.2020.00707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cardi, V. , Ambwani, S. , Crosby, R. , Macdonald, P. , Todd, G. , Park, J. , Moss, S. , Schmidt, U. , & Treasure, J. (2015). Self‐help and recovery guide for eating disorders (SHARED): Study protocol for a randomized controlled trial. Trials, 16(1), 165. 10.1186/s13063-015-0701-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cardi, V. , Ambwani, S. , Robinson, E. , Albano, G. , MacDonald, P. , Aya, V. , Rowlands, K. , Todd, G. , Schmidt, U. , Landau, S. , Arcelus, J. , Beecham, J. , & Treasure, J. (2017). Transition care in anorexia nervosa through guidance online from peer and carer expertise (TRIANGLE): Study protocol for a randomised controlled trial. European Eating Disorders Review : The Journal of the Eating Disorders Association, 25(6), 512–523. 10.1002/erv.2542 [DOI] [PubMed] [Google Scholar]
- Cardi, V. , Clarke, A. , & Treasure, J. (2013). The use of guided self‐help incorporating a mobile component in people with eating disorders: A pilot study. European Eating Disorders Review, 21(4), 315–322. 10.1002/erv.2235 [DOI] [PubMed] [Google Scholar]
- Dalton, B. , Bartholdy, S. , McClelland, J. , Kekic, M. , Rennalls, S. J. , Werthmann, J. , Carter, B. , O’Daly, O. G. , Campbell, I. C. , David, A. S. , Glennon, D. , Kern, N. , & Schmidt, U. (2018). Randomised controlled feasibility trial of real versus sham repetitive transcranial magnetic stimulation treatment in adults with severe and enduring anorexia nervosa: The TIARA study. BMJ Open, 8(7), e021531. 10.1136/bmjopen-2018-021531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denison‐Day, J. , Muir, S. , Newell, C. , & Appleton, K. M. (2019). A web‐based intervention (MotivATE) to increase attendance at an eating disorder service assessment appointment: Zelen randomized controlled trial. Journal of Medical Internet Research, 21(2), e11874. 10.2196/11874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan, B. L. , Miller, S. D. , Sparks, J. , Claud, D. A. , Reynolds, L. N. , Brown, J. , & Johnson, L. D. (2003). The session rating scale: Preliminary psychometric properties of a “working” alliance measure. Journal of Brief Therapy, 3, 3–12. [Google Scholar]
- Fairburn, C. G. , & Beglin, S. J. (1994). Assessment of eating disorders: Interview or self‐report questionnaire? International Journal of Eating Disorders, 16(4), 363–370. [DOI] [PubMed] [Google Scholar]
- Flückiger, C. , Del Re, A. C. , Wampold, B. E. , & Horvath, A. O. (2018). The alliance in adult psychotherapy: A meta‐analytic synthesis. Psychotherapy, 55(4), 316–340. 10.1037/pst0000172 [DOI] [PubMed] [Google Scholar]
- Frattaroli, J. (2006). Experimental disclosure and its moderators: A meta‐analysis. Psychological Bulletin, 132(6), 823–865. 10.1037/0033-2909.132.6.823 [DOI] [PubMed] [Google Scholar]
- Gonzales, A. L. , Hancock, J. T. , & Pennebaker, J. W. (2010). Language style matching as a predictor of social dynamics in small groups. Communications Research, 37(1), 3–19. 10.1177/0093650209351468 [DOI] [Google Scholar]
- Hair, J. , Black, W. C. , Babin, B. J. , & Anderson, R. E. (2010). Multivariate data analysis (7th ed.). Pearson Educational International. [Google Scholar]
- Hötzel, K. , von Brachel, R. , Schmidt, U. , Rieger, E. , Kosfelder, J. , Hechler, T. , Schulte, D. , & Vocks, S. (2014). An internet‐based program to enhance motivation to change in females with symptoms of an eating disorder: A randomized controlled trial. Psychological medicine, 44(9), 1947–1963. 10.1017/S0033291713002481 [DOI] [PubMed] [Google Scholar]
- Ireland, M. E. , & Pennebaker, J. W. (2010). Language style matching in writing: Synchrony in essays, correspondence, and poetry. Journal of Personality and Social Psychology, 99(3), 549–571. 10.1037/a0020386 [DOI] [PubMed] [Google Scholar]
- Ireland, M. E. , Slatcher, R. B. , Eastwick, P. W. , Scissors, L. E. , Finkel, E. J. , & Pennebaker, J. W. (2011). Language style matching predicts relationship initiation and stability. Psychological Science, 22(1), 39–44. 10.1177/0956797610392928 [DOI] [PubMed] [Google Scholar]
- Jordan, J. , McIntosh, V. , Carter, F. A. , Joyce, P. R. , Frampton, C. , Luty, S. E. , McKenzie, J. M. , Carter, J. D. , & Bulik, C. M. (2017). Predictors of premature termination from psychotherapy for anorexia nervosa: Low treatment credibility, early therapy alliance, and self‐transcendence. International Journal of Eating Disorders, 50(8), 979–983. 10.1002/eat.22726 [DOI] [PubMed] [Google Scholar]
- Kelders, S. M. , Kok, R. N. , Ossebaard, H. C. , & Van Gemert‐Pijnen, J. E. (2012). Persuasive system design does matter: A systematic review of adherence to web‐based interventions. Journal of Medical Internet Research, 14(6), e152. 10.2196/jmir.2104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline, R. B. (1998). Principles and practice of structural equation modeling. The Guilford Press. [Google Scholar]
- Leamy, M. , Bird, V. , Le Boutillier, C. , Williams, J. , & Slade, M. (2011). Conceptual framework for personal recovery in mental health: Systematic review and narrative synthesis. British Journal of Psychiatry, 199(6), 445–452. 10.1192/bjp.bp.110.083733 [DOI] [PubMed] [Google Scholar]
- Lepore, S. J. , & Smith, J. M. (2002). The writing cure: How expressive writing promotes health and emotional well‐being. Crisis: The Journal of Crisis Intervention and Suicide Prevention, 23(3). 10.1037/10451-000 [DOI] [PubMed] [Google Scholar]
- Lewis, H. K. , & Foye, U. (2021). From prevention to peer support: A systematic review exploring the involvement of lived‐experience in eating disorder interventions. Mental Health Review Journal, 27(1), 1–17. 10.1108/mhrj-04-2021-0033 [DOI] [Google Scholar]
- L'Insalata, A. , Trainor, C. , Bohon, C. , Mondal, S. , Le Grange, D. , & Lock, J. (2020). Confirming the efficacy of an adaptive component to family‐based treatment for adolescent anorexia nervosa: Study protocol for a randomized controlled trial. Frontiers in Psychiatry, 11, 41. 10.3389/fpsyt.2020.00041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Little, R. J. A. (1988). A Test of Missing Completely at Random for Multivariate Data with Missing Values. Journal of the American Statistical Association, 83, 1198–1202. 10.1080/01621459.1988.10478722 [DOI] [Google Scholar]
- Lock, J. , Le Grange, D. , Agras, W. S. , Fitzpatrick, K. K. , Jo, B. , Accurso, E. , Forsberg, S. , Anderson, K. , Arnow, K. , & Stainer, M. (2015). Can adaptive treatment improve outcomes in family‐based therapy for adolescents with anorexia nervosa? Feasibility and treatment effects of a multi‐site treatment study. Behaviour Research and Therapy, 73, 90–95. 10.1016/j.brat.2015.07.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lord, S. P. , Sheng, E. , Imel, Z. E. , Baer, J. , & Atkins, D. C. (2015). More than reflections: Empathy in motivational interviewing includes language style synchrony between therapist and client. Behavior Therapy, 46(3), 296–303. 10.1016/j.beth.2014.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovibond, S. H. , & Lovibond, P. F. (1995). Manual for the depression anxiety stress scales (2nd. Ed.). Psychology Foundation. [Google Scholar]
- Luce, K. H. , & Crowther, J. H. (1999). The reliability of the eating disorder examination‐self‐report questionnaire version (EDE‐Q). International Journal of Eating Disorders, 25(3), 349–351. [DOI] [PubMed] [Google Scholar]
- Macdonald, P. , Hibbs, R. , Rhind, C. , Harrison, A. , Goddard, E. , Raenker, S. , Todd, G. , & Treasure, J. (2014). Disseminating skills to carers of people with eating disorders: An examination of treatment fidelity in lay and professional carer coaches. Health Psychology and Behavioral Medicine, 2(1), 555–564. 10.1080/21642850.2014.908716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marucci, S. , Ragione, L. D. , De Iaco, G. , Mococci, T. , Vicini, M. , Guastamacchia, E. , & Triggiani, V. (2018). Anorexia nervosa and comorbid psychopathology. Endocrine, Metabolic & Immune Disorders ‐ Drug Targets, 18(4), 316–324. 10.2174/1871530318666180213111637 [DOI] [PubMed] [Google Scholar]
- Moyers, T. B. , Rowell, L. N. , Manuel, J. K. , Ernst, D. , & Houck, J. M. (2016). The motivational interviewing treatment integrity code (MITI 4): Rationale, preliminary reliability and validity. Journal of Substance Abuse Treatment, 65, 36–42. 10.1016/j.jsat.2016.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Müller‐Frommeyer, L. C. , Frommeyer, N. A. M. , & Kauffeld, S. (2019). Introducing rLSM: An integrated metric assessing temporal reciprocity in language style matching. Behaviour Research Methods, 51(3), 1343–1359. 10.3758/s13428-018-1078-8 [DOI] [PubMed] [Google Scholar]
- Musić, S. , Elwyn, R. , Fountas, G. , Gnatt, I. , Jenkins, Z. M. , Malcolm, A. , Miles, S. , Neill, E. , Simpson, T. , Yolland, C. O. , & Phillipou, A. (2022). Valuing the voice of lived experience of eating disorders in the research process: Benefits and considerations. Australian and New Zealand Journal of Psychiatry, 56(3), 216218–218. 10.1177/0004867421998794 [DOI] [PubMed] [Google Scholar]
- National Institute for Health and Care Excellence . (2017). Eating disorders: Recognition and treatment. National Institute for Health and Clinical Excellence Guideline (NG69). http://www.nice.org.uk [Google Scholar]
- Nazar, B. P. , Gregor, L. K. , Albano, G. , Marchica, A. , Coco, G. L. , Cardi, V. , & Treasure, J. (2017). Early response to treatment in eating disorders: A systematic review and a diagnostic test accuracy meta‐analysis. European Eating Disorders Review, 25(2), 67–79. 10.1002/erv.2495 [DOI] [PubMed] [Google Scholar]
- Niederhoffer, K. G. , & Pennebaker, J. W. (2002). Linguistic style matching in social interaction. Journal of Language and Social Psychology, 21(4), 337–360. 10.1177/026192702237953 [DOI] [Google Scholar]
- Ostiguy, C. , Meilleur, D. , Taddeo, D. , & Frappier, J. (2017). Intensité du trouble alimentaire et motivation au changement chez des adolescentes atteintes d’anorexie mentale. Neuropsychiatrie de l'Enfance et de l'Adolescence, 65(3), 137–145. 10.1016/j.neurenf.2017.02.006 [DOI] [Google Scholar]
- Peluso, P. R. , & Freund, R. R. (2018). Therapist and client emotional expression and psychotherapy outcomes: A meta‐analysis. Psychotherapy, 55(4), 461–472. 10.1037/pst0000165 [DOI] [PubMed] [Google Scholar]
- Pennebaker, J. W. , Booth, R. J. , & Francis, M. E. (2007). Linguistic Inquiry and word Count (LIWC2007): A computer‐based text analysis program [Computer software]. LIWC.net. [Google Scholar]
- Perez, M. , Van Diest, A. K. , & Cutts, S. (2014). Preliminary examination of a mentor‐based program for eating disorders. Journal of Eating Disorders, 2(1), 1–11. 10.1186/s40337-014-0024-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perkins, S. J. , Murphy, R. , Schmidt, U. , & Williams, C. (2006). Self‐help and guided self‐help for eating disorders. Cochrane Database of Systematic Reviews, 3(3), CD004191. 10.1002/14651858.CD004191.pub2 [DOI] [PubMed] [Google Scholar]
- Ramjan, L. M. , Fogarty, S. , Nicholls, D. , & Hay, P. (2018). Instilling hope for a brighter future: A mixedmethod mentoring support programme for individuals with and recovered from anorexia nervosa. Journal of Clinical Nursing, 27(5–6), e845–e857. 10.1111/jocn.14200 [DOI] [PubMed] [Google Scholar]
- Ramjan, L. M. , Hay, P. , & Fogarty, S. (2017). Benefits of a mentoring support program for individuals with an eating disorder: A proof of concept pilot program. BMC Research Notes, 10(1), 709. 10.1186/sl3104-017-3026-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ranzenhofer, L. M. , Wilhelmy, M. , Hochschild, A. , Sanzone, K. , Walsh, B. T. , & Attia, E. (2020). Peer mentorship as an adjunct intervention for the treatment of eating disorders: A pilot randomized trial. International Journal of Eating Disorders, 53(5), 497–509. 10.1002/eat.23258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schafer, J. L. (1997). Analysis of incomplete multivariate data. CRC press. [Google Scholar]
- Traviss, G. D. , Heywood‐Everett, S. , & Hill, A. J. (2013). Understanding the ‘guide’ in guided self‐help for disordered eating: A qualitative process study. Psychology and Psychotherapy: Theory, Research and Practice, 86(1), 86–104. 10.1111/j.2044-8341.2011.02049.x [DOI] [PubMed] [Google Scholar]
- Treasure, J. , Macare, C. , Mentxaka, I. O. , & Harrison, A. (2010). The use of a vodcast to support eating and reduce anxiety in people with eating disorder: A case series. European Eating Disorders Review, 18(6), 515–521. 10.1002/erv.1034 [DOI] [PubMed] [Google Scholar]
- Tryon, G. S. , Birch, S. E. , & Verkuilen, J. (2018). Meta‐analyses of the relation of goal consensus and collaboration to psychotherapy outcome. Psychotherapy, 55(4), 372–383. 10.1037/pst0000170 [DOI] [PubMed] [Google Scholar]
- van Haaren, M. , de Jong, S. , & Roeg, D. P. K. (2021). The foundations of the working alliance in assertive community treatment teams. BMC Psychiatry, 21(1), 559. 10.1186/s12888-021-03563-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Hoeken, D. , & Hoek, H. W. (2020). Review of the burden of eating disorders: Mortality, disability, costs, quality of life, and family burden. Current Opinion in Psychiatry, 33(6), 521–527. 10.1097/YCO.0000000000000641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voutilainen, A. , Pitkäaho, T. , Kvist, T. , & Vehviläinen‐Julkunen, K. (2016). How to ask about patient satisfaction? The visual analogue scale is less vulnerable to confounding factors and ceiling effect than a symmetric Likert scale. Journal of Advanced Nursing, 72(4), 946–957. 10.1111/jan.12875 [DOI] [PubMed] [Google Scholar]
- Wade, T. , Ambwani, S. , Cardi, V. , Albano, G. , & Treasure, J. (2021). Outcomes for adults with anorexia nervosa who do not respond early to outpatient treatment. International Journal of Eating Disorders, 54(7), 1278–1282. 10.1002/eat.23508 [DOI] [PubMed] [Google Scholar]
- Wampold, B. E. , & Imel, Z. E. (2015). The great psychotherapy debate: The evidence for what makes psychotherapy work (2nd ed.). Routledge/Taylor & Francis Group. [Google Scholar]
- Zuroff, D. C. , Koestner, R. , Moskowitz, D. S. , McBride, C. , Marshall, M. , & Bagby, M. R. (2007). Autonomous motivation for therapy: A new common factor in brief treatments for depression. Psychotherapy Research, 17(2), 137–147. 10.1080/10503300600919380 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Information S1
Data Availability Statement
The dataset generated for this study is available on request to the corresponding author.


