Abstract
Young people with neurodevelopmental disorders, such as attention‐deficit hyperactivity disorder (ADHD) and autism spectrum disorder (ASD), show high rates of mental health problems, of which depression is one of the most common. Given that depression in ASD and ADHD is linked with a range of poor outcomes, knowledge of how clinicians should assess, identify and treat depression in the context of these neurodevelopmental disorders is much needed. Here, we give an overview of the latest research on depression in young people with ADHD and ASD, including possible mechanisms underlying the link between ADHD/ASD and depression, as well as the presentation, assessment and treatment of depression in these neurodevelopmental disorders. We discuss the implications for clinicians and make recommendations for critical future research in this area.
Keywords: ADHD, autism spectrum disorders, depression, risk factors, assessment
Introduction
Attention‐deficit hyperactivity disorder (ADHD) and autism spectrum disorder (ASD) are neurodevelopmental disorders (American Psychiatric Association (APA), 2013; Thapar, Cooper, & Rutter, 2017) that represent common reasons for referral to specialist services. Whilst neurodevelopmental disorders (NDDs) in themselves are impairing, individuals are at substantially elevated risk of developing mental health problems, of which depression is one of the most common (Erskine et al., 2016; Ghaziuddin, Ghaziuddin, & Greden, 2002). Given that impairment and outcomes are much worse for young people with NDDs who develop depression (e.g. Kraper, Kenworthy, Popal, Martin, & Wallace, 2017; Rice et al., 2019), timely recognition, prevention and effective treatment of depression is important. Strikingly, depression in NDDs is rarely addressed in clinical guidance and research priority documents. Here, we consider recent research on depression in ADHD and ASD (see Supporting Information for search strategy) and discuss the implications for practitioners. Although ADHD and ASD show strong clinical and aetiological overlap, they have distinct features (Thapar et al., 2017), and most research has focused on one condition alone. Thus, we will consider each in turn, but draw out commonalities and distinctions where possible.
How common is depression in ADHD and ASD?
Depression rates vary widely across studies, likely due to differences in sample characteristics (e.g. age and measurement approaches). In ADHD, rates of depression range from 0% to 44.5% and are more than 5 times higher compared to individuals without ADHD (Angold, Costello, & Erkanli, 1999). The cumulative incidence of depression in individuals with ADHD followed up to age 19 has been estimated at 23% (Yoshimasu et al., 2012), and 44% of individuals with ADHD have experienced a depressive episode before age 30 (Meinzer, Pettit, & Viswesvaran, 2014). In ASD, one recent meta‐analysis estimated 10.6% prevalence of depression, which is four times that seen in typically developing youth, and the prevalence only increases further as individuals transition into adulthood (Hudson, Hall, & Harkness, 2019).
Depression is more common in females, but it is unclear whether the same female bias is observed in ADHD and ASD, given that these disorders show a male excess (Thapar et al., 2017). In ADHD, some studies suggest depression is more common in females (e.g. Jensen & Steinhausen, 2015), however others find no gender difference (e.g. Yoshimasu et al., 2012). In ASD, evidence is also mixed, but the most recent meta‐analysis suggests depression rates are comparable between males and females (Hudson et al., 2019).
Why are young people with ADHD/ASD at risk for depression?
There are multiple possible explanations for the links between NDDs and later depression (Figure 1; Caron & Rutter, 1991). First, associations could be an artefact of shared symptoms or medication side effects (Figure 2). However, studies have shown that associations remain even after these factors are accounted for (e.g. Biederman, Faraone, Mick, & Lelon, 1995). Second, links could be explained by shared aetiology, whereby the same genetic and/or environmental risks contribute to both ASD/ADHD and depression. Third, the clinical features of ADHD/ASD could serve as direct risks for depression, or fourth, lead indirectly to depression via social‐environmental stressors. Finally, links could be explained by a third disorder that commonly accompanies NDDs.
Figure 1.
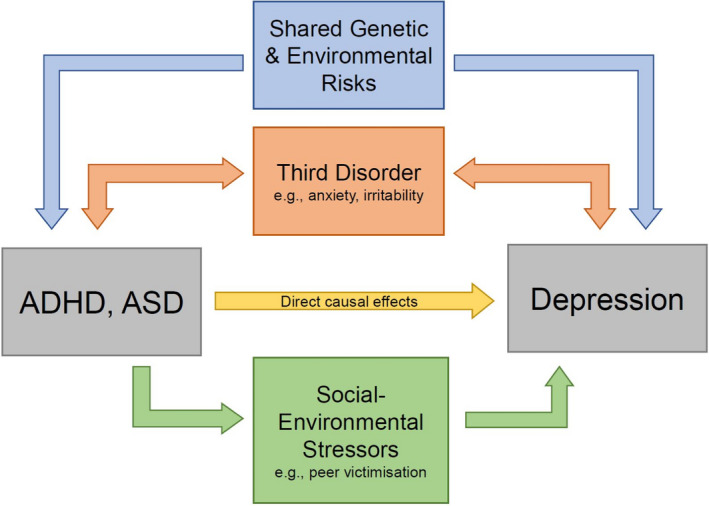
Possible mechanisms linking ADHD/ASD and depression. ADHD and ASD may be linked with depression due to: (1) An artefact of shared symptoms or medication side effects (see Figure 2); (2) shared genetic and environmental risks between ADHD/ASD and depression; (3) direct causal effects of ADHD/ASD on depression; (4) indirect effects via social‐environmental stressors; and/or (5) ADHD/ASD and depression both being associated with a third disorder or difficulty [Color figure can be viewed at wileyonlinelibrary.com]
Figure 2.
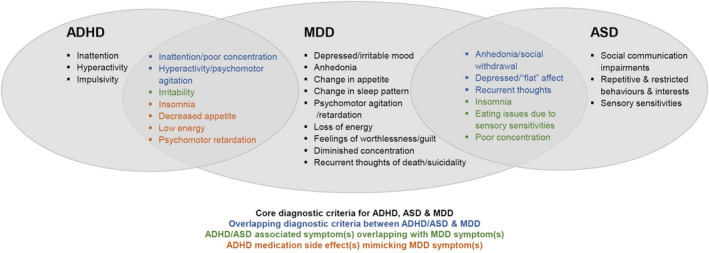
Diagnostic criteria for ADHD, ASD and major depressive disorder (MDD). ADHD and ASD may look similar clinically to MDD due to: (1) Overlapping core diagnostic criteria, for example, poor concentration is a symptom of both ADHD and MDD; (2) ADHD/ASD associated symptoms overlapping with MDD symptoms, for example, insomnia (a symptom of MDD) is highly prevalent in ASD; and/or (3) ADHD medication side effects mimicking MDD symptoms, for example, decreased appetite [Color figure can be viewed at wileyonlinelibrary.com]
Shared genetic and environmental risks
ADHD and ASD are highly heritable (Thapar, 2018; Thapar & Rutter, 2021), and genetic factors modestly contribute to depression. Thus, depression could be more common in NDDs if the same genetic liability contributes to both disorders. Indeed, family studies have shown that parents and other biological relatives of those with ADHD or ASD exhibit heightened rates of depression (Chen et al., 2019; Wang et al., 2022). Twin studies further suggest that familial links between ADHD/ASD and later depression are explained mainly by shared genetic liability (e.g. Stern et al., 2020). Genome‐wide association studies that identify common genetic variants at a molecular level also show a shared genetic aetiology; of all psychiatric disorders, depression shows the highest genetic correlation with both ADHD (Demontis et al., 2019) and ASD (Grove et al., 2017). However, there is little evidence that the same environmental risks contribute to NDDs and depression, as those that contribute to depression, such as bullying and stressful life events (Thapar, Collishaw, Pine, & Thapar, 2012), tend to occur after the typical age‐at‐onset for NDDs.
Of course, substantive genetic contributions to ASD/ADHD do not rule out social‐environmental stressors promoting later depression. Young people with ADHD or ASD are exposed to more social adversities than their peers. This may occur because environments are not independent of one's characteristics or genetic liability. Gene–environment correlation arises when a person's genetic liability to a disorder is also associated with exposure to environmental risks, thereby resulting in a ‘double whammy’ risk effect (Rutter, 2015). For example, one study of children adopted at birth found that child ADHD genetic liability, indexed by biological parent ADHD, led to increased adoptive mother–child hostility (Harold et al., 2013). Maltreatment is also more common in children with NDDs (Clayton, Lee, Cheung, Theule, & Henrikson, 2018; Hoover & Kaufman, 2018). One hypothesis is early childhood maltreatment or trauma cause ADHD/ASD, as well as later depression. However, studies that take into account genetic liability suggest that NDDs increase the likelihood of childhood maltreatment (Stern et al., 2018), rather than maltreatment causing NDDs (Dinkler et al., 2017), although one study could not rule out a causal effect (Capusan et al., 2016).
More recently, other studies have used a composite measure of common genetic risk variants (polygenic risk scores; PRS) as an indicator of genetic liability for NDDs and observed that ADHD and ASD PRS are associated with child maltreatment (e.g. Ratanatharathorn et al., 2021) and broader childhood adverse experiences (e.g. Zwicker et al., 2020). On balance, it seems probable that genetic liability for NDDs and their phenotypic manifestations increase the risk for maltreatment and some of the social‐environmental stressors known to increase depression risk.
Direct causal effects
A second possible mechanism is that ADHD or ASD directly causes depression. Despite strong evidence that ADHD and ASD are associated with later depression, observational designs alone cannot disentangle different explanations for these associations. Treatment‐based designs provide one approach to examine whether ADHD or ASD have direct causal effects on depression. If they do, then effective treatment of ADHD/ASD that reduces core symptoms should reduce risk of depression. However, a recent systematic review found no meta‐analyses of randomised control trials (RCTs) in which depression was an outcome of interventions for ADHD/ASD (Correll et al., 2021). An alternative, quasi‐experimental design, is to investigate within‐individual effects of ADHD/ASD treatment on depression. One such study found a 20% lower rate of depression when individuals were, versus were not, receiving ADHD medication (Chang, D'Onofrio, Quinn, Lichtenstein, & Larsson, 2016). This is consistent with a causal effect of ADHD on depression. However, these designs have limitations, and are less easily applied in the absence of disorder‐specific medication, such as for ASD.
Mendelian randomisation (MR) is an alternative method, utilising genetic data to infer causality (Hemani, Bowden, & Davey Smith, 2018), although it requires many assumptions. One recent MR study found evidence consistent with a causal effect of ADHD genetic liability on major depressive disorder (MDD; Riglin et al., 2020), although findings were less consistent for broader depression. To our knowledge, there are no MR studies investigating the association between ASD and depression. Overall, across treatment‐based and MR designs, two studies suggest that ADHD may have a causal effect on depression, but no conclusions can be made about ASD.
Social‐environmental mechanisms
Another explanation is that NDDs are linked with later depression indirectly via social‐environmental stressors.
In ADHD, studies examining family relationships have found the association between childhood ADHD and depression is partially mediated by parenting (e.g. Ostrander & Herman, 2006) and, for inattention symptoms, by parent–child relationship difficulties (Humphreys et al., 2013). One longitudinal study found that for boys, ADHD symptoms were associated with a steeper increase in negative mother–child relationships across adolescence compared to girls, and that this partly mediated the association between ADHD symptoms and subsequent depression (Meinzer, Felton, Oddo, Rubin, & Chronis‐Tuscano, 2020).
Peer relationships also are implicated. Population‐based studies have observed that friendship quality and peer problems (Powell, Riglin, et al., 2021), and being victimised by peers (Roy, Hartman, Veenstra, & Oldehinkel, 2015), partially mediate the association between ADHD and depression symptoms. One study, however, did not find strong evidence of mediation by declining best‐friend relationship quality across adolescence (Meinzer et al., 2020). Interestingly, Powell, Riglin, et al. (2021) found evidence that the association between ADHD and depression symptoms – mediated via friendship quality – attenuated in children with more positive parent–child relationships. This highlights that positive social relationships in one context may be able to compensate for poor social relationships in others.
Competency‐based (Cole, Martin, & Powers, 1997) and dual‐failure (Patterson & Stoolmiller, 1991) models of depression suggest that ADHD‐linked impairments may affect sense of competency/failure, which thereby increases risk of depression. For example, one cross‐sectional study of Japanese children found that ADHD (inattention) symptoms were associated with depression via low self‐esteem (Kita & Inoue, 2017). In addition, several studies have investigated academic competence as a pathway from ADHD to depression. While some found academic ability, indexed by test/exam scores, to partially mediate the association between ADHD symptoms in childhood and subsequent depression (Herman, Lambert, Ialongo, & Ostrander, 2007; Powell et al., 2020), others have not found strong evidence for this link (Humphreys et al., 2013).
In ASD, research also highlights negative social‐environmental experiences, such as bullying and traumatic events, as a route to later depression. In a population‐based study, Rai et al. (2018) found that being bullied during adolescence partially mediated the relationship between autistic (social communication) difficulties at age 7 and depression at age 18. Further, bullied autistic children showed elevated depressive symptoms across adolescence, compared to non‐bullied autistic and typically developing children. Cross‐sectional studies have also implicated peer victimisation (e.g. Chou, Wang, Hsiao, Hu, & Yen, 2020), which, similar to ADHD, may in part be buffered by parental support (Wright, 2017). A few studies have found less stressful family environments are associated with fewer depressive symptoms in autistic youth (e.g. Greenlee, Winter, & Marcovici, 2020), although there is less research focus on family environments in ASD compared to ADHD.
One prominent explanation for how ASD promotes depression is that depression arises from dysfunctional interpersonal relationships (Smith & White, 2020). Supporting this, evidence suggests that more severe autistic symptoms (Hedley, Uljarević, Foley, Richdale, & Trollor, 2018) and poor quality of social interaction (Dallman, Bailliard, & Harrop, 2022) are associated with greater depression. Further, reduced success with social relationships in ASD may lead to depression via loneliness. Indeed, Hedley et al. (2018) found that among autistic adolescents and adults, loneliness partly mediated the relationship between a lack of social support networks and depression.
Overall, research indicates that there are numerous social‐environmental factors that may mediate risk of depression in young people with ADHD and ASD. However, most evidence from the aforementioned studies is cross‐sectional, thus it is unclear if any of these factors play a causal role.
A third disorder or difficulty
An alternative mechanism is that NDDs are associated with depression due to a third disorder or difficulty that commonly accompanies ASD/ADHD.
Childhood anxiety disorders are important predictors of future depression and common in ADHD, and thus may explain the association between ADHD and depression (Meinzer et al., 2014). One meta‐analysis of general population studies found that anxiety explained the association between ADHD and depression (Angold et al., 2009). Other studies have found that the association between ADHD and depression attenuates when adjusting for anxiety, oppositional defiant, and conduct disorders (e.g. Copeland, Shanahan, Erkanli, Costello, & Angold, 2013; Ford, Goodman, & Meltzer, 2003), however some studies still find a robust association after accounting for comorbid psychiatric disorders (e.g. Meinzer et al., 2013). Substance misuse is another comorbidity associated with ADHD and depression (e.g. Groenman, Janssen, & Oosterlaan, 2017), although whether it is a route to depression in ADHD is currently unclear. In terms of ASD, anxiety disorders are highly prevalent (Copeland et al., 2013), but whether anxiety explains the link between ASD and depression has not to our knowledge been directly tested.
Beyond comorbid psychiatric disorders, there are transdiagnostic difficulties that might promote the link between NDDs and depression. Emotional dysregulation is a common difficulty in NDDs and associated with depression (Cai, Richdale, Uljarević, Dissanayake, & Samson, 2018; Shaw, Stringaris, Nigg, & Leibenluft, 2014). Research suggests it mediates the link between ADHD and depression cross‐sectionally and longitudinally (Seymour et al., 2012; Seymour, Chronis‐Tuscano, Iwamoto, Kurdziel, & MacPherson, 2014). A closely related problem, irritability – difficulty regulating anger – is also strongly associated with ADHD and may be a route to later depression. In one population cohort, irritability explained almost half of the association between a broad range of childhood neurodevelopmental difficulties (including ASD and ADHD) and depression (Eyre et al., 2019). Additionally, sluggish cognitive tempo (SCT) – daydreaming, inattention, and lethargy – which is associated with but distinct from ADHD (Barkley, 2013), is also linked with depression (Smith, Zald, & Lahey, 2020). Whether SCT plays a direct role in promoting depression in ADHD requires investigation.
Finally, alexithymia – difficulty identifying one's own emotions – is highly prevalent in ASD (Kinnaird, Stewart, & Tchanturia, 2019) and also associated with depression (Bloch, Burghof, Lehnhardt, Vogeley, & Falter‐Wagner, 2021). Thus, heightened alexithymia could contribute to depression in ASD. For example, Morie, Jackson, Zhai, Potenza, and Dritschel (2019) found a serial relationship between alexithymia and emotional regulation partly mediated the association between ASD and depression in adults. Alexithymia may also be relevant to ADHD, but has been less studied as a pathway to depression.
Presentation of depression in ADHD and ASD
Timing and severity
When depression is comorbid with ADHD, it is more severe, has an earlier age‐at‐onset and worse prognosis than in the typically developing population. Purper‐Ouakil et al. (2017) found that adults with MDD who retrospectively reported childhood ADHD symptoms had greater depression symptoms and poorer global functioning, compared to those without childhood ADHD. Further, a recent study of women with recurrent depression found that those with broadly defined ADHD, versus not, had an earlier age of depression onset and a higher rate of receiving non‐first‐line antidepressants (Powell, Agha, et al., 2021). This suggests that in some individuals, underlying ADHD may be masked by depression. Prospective population‐based studies also suggest that childhood ADHD is associated with a younger depression age‐at‐onset (Jaffee et al., 2002; Rice et al., 2019).
In ASD, depression onsets in adolescence at a similar age to the typically developing population (Gotham, Brunwasser, & Lord, 2015; Gundel, Pedersen, Munk‐Olsen, & Dalsgaard, 2018; but see Rice et al., 2019), and rates increase across adolescence, particularly for autistic girls. Gotham et al. (2015) found that autistic boys had greater depression symptoms compared to autistic girls at age 13, but autistic girls' symptoms showed an upward trajectory, so that the sex difference was absent by age 21. There is also emerging evidence that ‘late diagnosed’ autistic young people may be at risk for more severe depression. In one cohort study, autistic girls diagnosed with ASD ‘late’ (aged 14–17) showed the greatest risk of later developing depression compared to autistic boys and girls diagnosed in childhood (Gundel et al., 2018). Hosozawa, Sacker, and Cable (2021) found a similar link between late diagnosis in adolescence and later depression, but no sex difference. Interestingly, previous depression diagnoses are highly prevalent among individuals diagnosed with ASD in adulthood (Fusar‐Poli, Brondino, Politi, & Aguglia, 2022), suggesting that like ADHD, ASD might be misdiagnosed as depression or depression might mask underlying ASD. Further research is needed to understand how common it is to miss NDDs in the context of depression, perhaps especially in females.
Symptom presentation
Depression in ADHD and ASD may present differently to depression in the general population.
In ADHD, research suggests a similar factor structure and relative frequency of depression symptoms among those with and without ADHD (Fraser et al., 2018; Joseph et al., 2019). However, Diler et al. (2007) found that, among young people with ADHD, some depression symptoms (e.g. anhedonia, suicidal thoughts, psychomotor retardation) discriminated those with MDD from those without MDD, whereas others did not (e.g. irritability, reduced sleep, appetite, and concentration). Therefore, certain depressive symptoms may be more indicative of a depressive episode in young people with ADHD, although further research is needed. Additionally, young people with ADHD are impulsive and show elevated rates of self‐harm and suicidal behaviour, which may sometimes be the primary presentation of depression in ADHD. Further, irritability – a common feature of both ADHD and depression – may be present. However, ADHD‐related irritability typically onsets early, whereas irritability in depression will be accompanied by other depression symptoms and typically arise later in development (Riglin et al., 2019).
In ASD, some studies have found a similar factor structure for depression symptoms in people with and without ASD (e.g. Uljarević et al., 2018). However, one recent network analysis found that depression in ASD was particularly characterised by insomnia and restlessness (Montazeri, de Bildt, Dekker, & Anderson, 2020), suggesting these might be prominent features of depression in ASD. It is also proposed that there are ‘atypical’ presentations of depression that are more specific to ASD, for example, reduced engagement with special interests and self‐care (Pezzimenti, Han, Vasa, & Gotham, 2019). However, beyond clinical observations, there is a lack of systematic investigation into ASD‐specific manifestations of depression.
Assessment of depression in ADHD and ASD
Although early detection is pivotal, there are numerous barriers to effectively assessing depression in NDDs. First, symptoms of ADHD and ASD overlap with depression symptoms, making it difficult to distinguish between the disorders (Figure 2). For example, difficulty concentrating and restlessness – core symptoms of ADHD – are also symptoms of depression. And irritability – a symptom of adolescent depression – is an associated feature of ADHD. ADHD medication also commonly results in side effects that mimic depression. For example, methylphenidate, the first‐line treatment for ADHD in young people (The National Institute for Health and Care Excellence (NICE), 2018) can cause decreased appetite and insomnia, which are diagnostic criteria for MDD (APA, 2013).
In ASD, individuals can exhibit social withdrawal, which overlaps with anhedonia in depression. Insomnia, another depression symptom, is also highly frequent in ASD (Mazzone, Postorino, Siracusano, Riccioni, & Curatolo, 2018), and autistic people can experience eating difficulties due to sensory sensitivities (Baraskewich, von Ranson, McCrimmon, & McMorris, 2021), which may be mistaken for depression‐related decreased appetite. One way to help differentiate between ADHD/ASD and overlapping depression symptoms is to consider age‐at‐onset of symptoms and evidence of a change in symptoms. NDDs have an earlier age‐at‐onset with symptoms persisting over time, whereas depression onset is later and symptoms are more episodic.
A second challenge is that many commonly used depression measures (e.g. Moods and Feelings Questionnaire) have not been validated for young people with NDDs and therefore may not be as accurate. For example, overlap between ADHD/ASD and depression may result in elevated depression scores. For ADHD, no specific tools have been developed, although it has been suggested that the Child Behaviour Checklist and the Strength and Difficulties Questionnaire (SDQ) may be useful for screening for depression (Biederman, Monuteaux, Kendrick, Klein, & Faraone, 2005; Coutinho, Farias, Felden, & Cordeiro, 2021). In ASD, the SDQ has been shown to be an effective screening tool for emotional difficulties in autistic children (Findon et al., 2016), however the SDQ is not specific to depression, capturing anxiety too. A French tool for screening depression in ASD has recently been developed (Bellalou, Downes, & Cappe, 2021), although to our knowledge is yet to be translated into English. Overall, much more rigorous evaluation of the suitability of common depression measures for use in ASD and ADHD is needed.
The third challenge is that depression may be hard to assess due to differences between various informants. Young people with NDDs may under report their own depressive symptoms. For example, there is evidence of higher parent‐ versus self‐rated depression scores in both ADHD (e.g. Fraser et al., 2018) and ASD (e.g. Schwartzman & Corbett, 2020). In ASD, alexithymia and social communication can make it difficult for individuals to reflect on or explain their internal states verbally, especially those with co‐occurring intellectual disability. Arguably, parents may be a more useful informant. However, it is also possible that they may over report symptoms, or even miss certain symptoms in the presence of other behavioural difficulties. Parents will likely have less insight into their children's internal states as they move through adolescence and into early adulthood, as reflected in reduced concordance between self and parent ratings over development (e.g. in ASD, Andersen, Hovik, Skogli, & Øie, 2017). Taken together, rater differences suggest the need for multiple informants when assessing for depression in NDDs. For those with ASD and intellectual disability, parent and teacher reports of behaviour change and clinician observation are particularly important.
Overall, the assessment of depression in ADHD and ASD can be complicated by numerous factors. Depression screening tools may not be as accurate, so careful clinical assessment is necessary, obtaining information from both the young person and parent, together with observations from school, in relation to new changes in behaviour and functioning.
Effectiveness of standard depression treatments
Psychological therapies
Psychological therapies are effective and recommended for treating depression in young people (NICE, 2019), but there is less evidence regarding their effectiveness for treating depression in those with NDDs.
In ADHD, numerous psychological therapies for depression have been evaluated. One meta‐analysis examined studies targeting emotional symptoms (depression, anxiety and emotional dysregulation) in children and adults with ADHD, using cognitive behavioural therapy (CBT), mindfulness‐based therapy (MBT), parent training, social skills training and (dialectical) behavioural therapy (Guo, Assumpcao, & Hu, 2022). Results suggested that, in children, parent training was effective in reducing depressive symptoms, social skills training was effective for emotional dysregulation, but CBT did not have a significant effect. In adults, CBT was effective for reducing depression, emotional dysregulation and anxiety. Additionally, Lopez et al. (2018) found that when CBT was used to treat core ADHD symptoms in adults, depression symptoms improved when compared to treatment as usual. Therefore, while there is evidence for use of CBT for treating depression in adults with ADHD, this does not seem to be generalisable to young people.
Psychological therapies for depression in ASD also have been evaluated. A meta‐analysis of CBT in young people and adults with ASD found a small‐to‐medium effect size when treating affective disorders (Weston, Hodgekins, & Langdon, 2016). However, results varied according to who rated the outcome, with significant effects seen for informant‐ and clinician‐reported outcomes, but not for self‐reported outcomes. Additionally, most of the studies in the meta‐analysis targeted anxiety rather than depression, and of those studies examining depression, only one included young people (McGillivray & Evert, 2014). In that study, a group CBT intervention was compared to waiting list controls in young people aged 15–25 with ASD, finding a significant reduction of depression symptoms in the intervention compared to waiting list group for those who initially scored highly on depression.
In terms of MBT, evidence of it as an effective depression treatment in ASD is limited to adults (e.g. Sizoo & Kuiper, 2017). Other studies examining the effect of psychological therapies have targeted core symptoms of ASD or anxiety, but included depression as a secondary outcome (e.g. Bemmer et al., 2021; Schiltz et al., 2018). These findings suggest that treating possible mediators of the association between ASD and depression (e.g. social functioning, social anxiety) can improve depression symptoms, but these effects may not generalise to MDD.
The choice of psychological therapy for depression in young people with ASD may also depend on the individual's cognitive and verbal ability. For those who are minimally verbal or have intellectual disability, approaches focusing on behavioural components of CBT, such as behavioural activation, may be a better choice (White et al., 2018). However, full‐scale RCTs to evaluate the effectiveness of such interventions are yet to be published. Psychological therapies also have been adapted to be more accessible and effective for those with ASD (White et al., 2018), for example, focusing on developing emotional awareness, slower pace, inclusion of special interest, reduced use of metaphors, structured sessions, use of visuals and additional time for practice.
Overall, there is some evidence to suggest psychological therapies can be effective in treating depression in young people with ADHD or ASD, but these may work better in older adolescents and young adults. Modified CBT approaches may be effective in autistic young people, with evidence for family‐based approaches in young people with ADHD. Nevertheless, further research on the effectiveness of psychological therapies directly targeting depression in both ADHD and ASD is needed.
Medication
To the best of our knowledge, there are no published RCTs on medication for treating depression in NDDs. There is also no evidence to guide clinicians on the most effective medications for ADHD in the presence of comorbid depression.
For ADHD, there are consensus guidelines on the assessment and treatment of comorbid depression in adult life, some of which are relevant to young people (McIntosh et al., 2009). These guidelines recommend prioritising the treatment of the most severe or impairing condition first. If ADHD is the most concerning disorder and depression is only mild, effective treatment of ADHD is the priority. As ADHD medications, including stimulants, can disrupt sleep and mood, those with depression will need careful monitoring. If depression is severe and impairing, then the priority is to treat depression first using national guidelines before treating ADHD symptoms with medication. Fluoxetine is the only antidepressant currently licenced for use in children and adolescents in the UK, although observational and genetic studies suggest that depression with ADHD may be more likely to be treatment resistant (e.g. Fabbri et al., 2021). Beyond fluoxetine, there is modest evidence for the efficacy of escitalopram, sertraline, and duloxetine in youth depression (Hetrick et al., 2021). Venlafaxine and paroxetine are not recommended for young people. Unfortunately, there is no evidence to guide clinicians on antidepressants specifically in the context of ADHD.
The risk of attempted suicide is higher in those with ADHD (Ljung, Chen, Lichtenstein, & Larsson, 2014), so careful monitoring and supervision are needed in those with depression, whether or not medication is used. Clinicians should also be mindful that, after treatment with selective serotonin reuptake inhibitors, some young people with ADHD with depression could potentially switch to hypomania, given the known association between ADHD and early‐onset bipolar disorder, especially in the offspring of those with bipolar disorder (e.g. Kim et al., 2015). However, this is not a contra‐indication to initiate antidepressant medication. Although it is unclear how common antidepressant‐induced hypomania is in NDCs, and this will represent a small sub‐group, clinicians should carefully monitor young people if there is a family history of bipolar disorder.
For ASD, while psychosocial interventions are considered most important, medication may be required if depression is severe. There is no clear guidance on what works best in ASD based on RCTs (NICE, 2012). Given this, as for ADHD, currently it is recommended that clinicians follow national guidelines in relation to treating depression. However, one set of guidance suggests starting on a very low dose, titrating slowly, setting treatment targets, checking whether there is a family history of bipolar disorder, and being mindful of side effects, including aggression, impulsivity and disinhibition (Pezzimenti et al., 2019). Also, as in ADHD, there is a heightened risk for suicide in ASD (Costa, Loor, & Steffgen, 2020), so this also needs to be carefully monitored.
Clinical implications
Despite growing research on the links between NDDs and depression, there is relatively little to guide clinicians in practice. For those who see young people with ADHD and/or ASD, accompanying irritability, alexithymia, anxiety, a family history of depression and exposure to social‐environmental stressors (e.g. bullying or maltreatment), are indicators of a heightened risk for depression. Social support in one context may help buffer stressors in another. While there are no prevention studies of depression in young people with ADHD or ASD, research to date suggests that effective treatment of core ADHD symptoms, treatment of parent depression (while being aware of the possibility of an underlying NDD in the parent too), reducing exposure to social stressors and increasing social support (at least in one context) may help disrupt the link with later depression. Overall, it is important to address parent mental health and the social context, comorbid difficulties as well as the core deficits of ADHD and ASD. Clinicians also need to be aware that early‐onset or difficult to treat depression, especially in girls and young women, could be masking an underlying NDD that has been missed.
There is limited evidence on how best to assess or treat depression effectively in ADHD and ASD. Therefore, we suggest that clinicians follow existing guidelines for identifying and treating depression in young people (i.e. NICE, 2019), but carefully consider adaptations as needed. For example, clinicians may need to interpret questionnaire measures with some caution and rely on direct clinical assessments as well as information from multiple informants. Similarly, usual depression treatment approaches may need to be adapted depending on the young person, their difficulties and strengths, and their social context. For example, psychological therapies may need to emphasise behavioural aspects, especially in younger individuals, and antidepressant treatment titrated and monitored more cautiously than in the typically developing population.
Future research
This review has highlighted many research gaps. One striking gap is that research has focused exclusively on ADHD or ASD despite their established overlap. Given that, until DSM‐5 was published, research into ASD will have excluded those with a diagnosis of ADHD, many studies may have excluded young people who typify clinic populations where comorbidities are common. A second gap is that although young people with ADHD/ASD are at elevated risk for depression, it remains unknown how best to screen for and assess depression in the context of NDDs. Standard measures of depression need to be validated, particularly for young people, and if necessary, adapted for those with NDDs. A third major gap is there is little evidence to guide treatment choices. Thus, more RCTs of interventions for prevention and treatment of depression in ADHD and ASD are needed. Additionally, whether the aetiology, presentation or treatment of depression in NDDs differs at different developmental time points (e.g. childhood versus adolescence) requires investigation. Finally, most people with a NDD do not develop depression, and if they do, outcomes can be variable. More work is needed to identify how to increase resilience in those with NDDs and whether it is possible to identify those at highest risk of poorer outcomes, including developing a different mental disorder such as bipolar disorder or attempting suicide.
Supporting information
Table S1. Search criteria for literature search.
Acknowledgements
The authors declare no competing or potential conflicts of interest. A.T.'s research is supported by the Wellcome Trust and Wolfson Foundation. O.E. and L.R. are supported by the Wolfson Foundation. L.A.L. is supported by The Waterloo Foundation. The authors thank Lucy H. Waldren for feedback on the manuscript.
Key Points
Family history of depression, emotional dysregulation/irritability, alexithymia, and social stressors are risks for depression in young people with ADHD/ASD.
Ask parents and others (e.g. teachers), as well as the young person, about new changes in mood, behaviour and functioning.
Treat depression with standard psychological therapies, making adaptions where necessary to suit the individual's strengths and difficulties.
Where appropriate, treat depression with medication according to national guidelines but be mindful of higher risks for side effects, a switch to bipolar disorder (in ADHD), and suicide attempt.
Early‐onset, recurrent or treatment‐resistant depression may be masking underlying ASD/ADHD.
What measures best identify depression in ADHD/ASD?
How effective is antidepressant medication in ADHD/ASD and how should psychological interventions for depression be adapted?
What are the optimum depression prevention strategies for those with ADHD/ASD?
Conflict of interest statement: No conflicts declared.
References
- American Psychiatric Association . (2013). Diagnostic and statistical manual of mental disorders (5th edn). Washington, DC: Author. [Google Scholar]
- Andersen, P.N. , Hovik, K.T. , Skogli, E.W. , & Øie, M.G. (2017). Severity of autism symptoms and degree of attentional difficulties predicts emotional and behavioral problems in children with high‐functioning autism; a two‐year follow‐up study. Frontiers in Psychology, 8, 2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angold, A. , Costello, E.J. , & Erkanli, A. (1999). Comorbidity. Journal of Child Psychology and Psychiatry, 40, 57–87. [PubMed] [Google Scholar]
- Baraskewich, J. , von Ranson, K.M. , McCrimmon, A. , & McMorris, C.A. (2021). Feeding and eating problems in children and adolescents with autism: A scoping review. Autism, 25, 1505–1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barkley, R.A. (2013). Distinguishing sluggish cognitive tempo from ADHD in children and adolescents: Executive functioning, impairment, and comorbidity. Journal of Clinical Child & Adolescent Psychology, 42, 161–173. [DOI] [PubMed] [Google Scholar]
- Bellalou, L. , Downes, N. , & Cappe, E. (2021). Development and preliminary validation of a depressive symptomatology detection scale among children and adolescents on the autism spectrum. Autism, 25, 361–373. [DOI] [PubMed] [Google Scholar]
- Bemmer, E.R. , Boulton, K.A. , Thomas, E.E. , Larke, B. , Lah, S. , Hickie, I.B. , & Guastella, A.J. (2021). Modified CBT for social anxiety and social functioning in young adults with autism spectrum disorder. Molecular Autism, 12, 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biederman, J. , Faraone, S. , Mick, E. , & Lelon, E. (1995). Psychiatric comorbidity among referred juveniles with major depression: Fact or artifact? Journal of the American Academy of Child and Adolescent Psychiatry, 34, 579–590. [DOI] [PubMed] [Google Scholar]
- Biederman, J. , Monuteaux, M.C. , Kendrick, E. , Klein, K.L. , & Faraone, S.V. (2005). The CBCL as a screen for psychiatric comorbidity in paediatric patients with ADHD. Archives of Disease in Childhood, 90, 1010–1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bloch, C. , Burghof, L. , Lehnhardt, F.G. , Vogeley, K. , & Falter‐Wagner, C. (2021). Alexithymia traits outweigh autism traits in the explanation of depression in adults with autism. Scientific Reports, 11, 2258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai, R.Y. , Richdale, A.L. , Uljarević, M. , Dissanayake, C. , & Samson, A.C. (2018). Emotion regulation in autism spectrum disorder: Where we are and where we need to go. Autism Research, 11, 962–978. [DOI] [PubMed] [Google Scholar]
- Capusan, A.J. , Kuja‐Halkola, R. , Bendtsen, P. , Viding, E. , McCrory, E. , Marteinsdottir, I. , & Larsson, H. (2016). Childhood maltreatment and attention deficit hyperactivity disorder symptoms in adults: A large twin study. Psychological Medicine, 46, 2637–2646. [DOI] [PubMed] [Google Scholar]
- Caron, C. , & Rutter, M. (1991). Comorbidity in child psychopathology: Concepts, issues and research strategies. Journal of Child Psychology and Psychiatry, 32, 1063–1080. [DOI] [PubMed] [Google Scholar]
- Chang, Z. , D'Onofrio, B.M. , Quinn, P.D. , Lichtenstein, P. , & Larsson, H. (2016). Medication for attention‐deficit/hyperactivity disorder and risk for depression: A nationwide longitudinal cohort study. Biological Psychiatry, 80, 916–922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, M.H. , Pan, T.L. , Huang, K.L. , Hsu, J.W. , Bai, Y.M. , Su, T.P. , … & Chen, T.J. (2019). Coaggregation of major psychiatric disorders in first‐degree relatives of individuals with attention‐deficit/hyperactivity disorder: A nationwide population‐based study. The Journal of Clinical Psychiatry, 80, 18m12371. [DOI] [PubMed] [Google Scholar]
- Chou, W.‐J. , Wang, P.‐W. , Hsiao, R.C. , Hu, H.‐F. , & Yen, C.‐F. (2020). Role of school bullying involvement in depression, anxiety, suicidality, and low self‐esteem among adolescents with high‐functioning autism Spectrum disorder. Frontiers in Psychiatry, 11, 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clayton, K. , Lee, J.B. , Cheung, K. , Theule, J. , & Henrikson, B. (2018). Quantifying the relationship between attention‐deficit/hyperactivity disorder and experiences of child maltreatment: A meta‐analysis. Child Abuse Review, 27, 361–377. [Google Scholar]
- Cole, D.A. , Martin, J.M. , & Powers, B. (1997). A competency‐based model of child depression: A longitudinal study of peer, parent, teacher, and self‐evaluations. Journal of Child Psychology and Psychiatry, 38, 505–514. [DOI] [PubMed] [Google Scholar]
- Copeland, W.E. , Shanahan, L. , Erkanli, A. , Costello, E.J. , & Angold, A. (2013). Indirect comorbidity in childhood and adolescence. Frontiers in Psychiatry, 4, 444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Correll, C.U. , Cortese, S. , Croatto, G. , Monaco, F. , Krinitski, D. , Arrondo, G. , … & Solmi, M. (2021). Efficacy and acceptability of pharmacological, psychosocial, and brain stimulation interventions in children and adolescents with mental disorders: An umbrella review. World Psychiatry, 20, 244–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costa, A.P. , Loor, C. , & Steffgen, G. (2020). Suicidality in adults with autism spectrum disorder: The role of depressive symptomatology, alexithymia, and antidepressants. Journal of Autism and Developmental Disorders, 50, 3585–3597. [DOI] [PubMed] [Google Scholar]
- Coutinho, D. , Farias, A.C. , Felden, E.P.G. , & Cordeiro, M.L. (2021). ADHD comorbid with major depression on parents and teachers perceptions. Journal of Attention Disorders, 25, 508–518. [DOI] [PubMed] [Google Scholar]
- Dallman, A.R. , Bailliard, A. , & Harrop, C. (2022). Identifying predictors of momentary negative affect and depression severity in adolescents with autism: An exploratory ecological momentary assessment study. Journal of Autism and Developmental Disorders, 52, 291–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demontis, D. , Walters, R.K. , Martin, J. , Mattheisen, M. , Als, T.D. , Agerbo, E. , … & Neale, B.M. (2019). Discovery of the first genome‐wide significant risk loci for attention deficit/hyperactivity disorder. Nature Genetics, 51, 63–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diler, R.S. , Daviss, W.B. , Lopez, A. , Axelson, D. , Iyengar, S. , & Birmaher, B. (2007). Differentiating major depressive disorder in youths with attention deficit hyperactivity disorder. Journal of Affective Disorders, 102, 125–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dinkler, L. , Lundström, S. , Gajwani, R. , Lichtenstein, P. , Gillberg, C. , & Minnis, H. (2017). Maltreatment‐associated neurodevelopmental disorders: A co‐twin control analysis. Journal of Child Psychology and Psychiatry, 58, 691–701. [DOI] [PubMed] [Google Scholar]
- Erskine, H.E. , Norman, R.E. , Ferrari, A.J. , Chan, G.C.K. , Copeland, W.E. , Whiteford, H.A. , & Scott, J.G. (2016). Long‐term outcomes of attention‐deficit/hyperactivity disorder and conduct disorder: A systematic review and meta‐analysis. Journal of the American Academy of Child and Adolescent Psychiatry, 55, 841–850. [DOI] [PubMed] [Google Scholar]
- Eyre, O. , Hughes, R.A. , Thapar, A.K. , Leibenluft, E. , Stringaris, A. , Davey Smith, G. , … & Thapar, A. (2019). Childhood neurodevelopmental difficulties and risk of adolescent depression: The role of irritability. Journal of Child Psychology and Psychiatry, 60, 866–874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fabbri, C. , Hagenaars, S.P. , John, C. , Williams, A.T. , Shrine, N. , Moles, L. , … & Lewis, C.M. (2021). Genetic and clinical characteristics of treatment‐resistant depression using primary care records in two UKcohorts. Molecular Psychiatry, 26, 3363–3373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Findon, J. , Cadman, T. , Stewart, C.S. , Woodhouse, E. , Eklund, H. , Hayward, H. , … & McEven, F.S. (2016). Screening for co‐occurring conditions in adults with autism spectrum disorder using the strengths and difficulties questionnaire: A pilot study. Autism Research, 9, 1353–1363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford, T. , Goodman, R. , & Meltzer, H. (2003). The British child and adolescent mental health survey 1999: The prevalence of DSM‐IV disorders. Journal of the American Academy of Child and Adolescent Psychiatry, 42, 1203–1211. [DOI] [PubMed] [Google Scholar]
- Fraser, A. , Cooper, M. , Agha, S.S. , Collishaw, S. , Rice, F. , Thapar, A. , & Eyre, O. (2018). The presentation of depression symptoms in attention‐deficit/hyperactivity disorder: Comparing child and parent reports. Child and Adolescent Mental Health, 23, 243–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar‐Poli, L. , Brondino, N. , Politi, P. , & Aguglia, E. (2022). Missed diagnoses and misdiagnoses of adults with autism spectrum disorder. European Archives of Psychiatry and Clinical Neuroscience, 272, 187–198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghaziuddin, M. , Ghaziuddin, N. , & Greden, J. (2002). Depression in persons with autism: Implications for research and clinical care. Journal of Autism and Developmental Disorders, 32, 299–306. [DOI] [PubMed] [Google Scholar]
- Gotham, K. , Brunwasser, S.M. , & Lord, C. (2015). Depressive and anxiety symptom trajectories from school age through young adulthood in samples with autism spectrum disorder and developmental delay. Journal of the American Academy of Child & Adolescent Psychiatry, 54, 369–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenlee, J.L. , Winter, M.A. , & Marcovici, I.A. (2020). Gender differences in experiences of peer victimization among adolescents with autism Spectrum disorder. Journal of Autism and Developmental Disorders, 50, 3790–3799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groenman, A.P. , Janssen, T.W. , & Oosterlaan, J. (2017). Childhood psychiatric disorders as risk factor for subsequent substance abuse: A meta‐analysis. Journal of the American Academy of Child & Adolescent Psychiatry, 56, 556–569. [DOI] [PubMed] [Google Scholar]
- Grove, J. , Ripke, S. , Als, T.D. , Mattheisen, M. , Walters, R. , Won, H. , … & Børglum, A.D. (2017). Common risk variants identified in autism spectrum disorder. Nature Genetics, 51, 431–444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gundel, L.K. , Pedersen, C.B. , Munk‐Olsen, T. , & Dalsgaard, S. (2018). Longitudinal association between mental disorders in childhood and subsequent depression – A nationwide prospective cohort study. Journal of Affective Disorders, 227, 56–64. [DOI] [PubMed] [Google Scholar]
- Guo, C. , Assumpcao, L. , & Hu, Z. (2022). Efficacy of non‐pharmacological treatments on emotional symptoms of children and adults with attention‐deficit/hyperactivity disorder: A meta‐analysis. Journal of Attention Disorders, 26, 508–524. [DOI] [PubMed] [Google Scholar]
- Harold, G.T. , Leve, L.D. , Barrett, D. , Elam, K. , Neiderhiser, J.M. , Natsuaki, M.N. , … & Thapar, A. (2013). Biological and rearing mother influences on child ADHD symptoms: Revisiting the developmental interface between nature and nurture. Journal of Child Psychology and Psychiatry, 54, 1038–1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedley, D. , Uljarević, M. , Foley, K.‐R. , Richdale, A. , & Trollor, J. (2018). Risk and protective factors underlying depression and suicidal ideation in autism Spectrum disorder. Depression and Anxiety, 35, 648–657. [DOI] [PubMed] [Google Scholar]
- Hemani, G. , Bowden, J. , & Davey Smith, G. (2018). Evaluating the potential role of pleiotropy in Mendelian randomization studies. Human Molecular Genetics, 27(R2), R195–R208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herman, K.C. , Lambert, S.F. , Ialongo, N.S. , & Ostrander, R. (2007). Academic pathways between attention problems and depressive symptoms among urban African American children. Journal of Abnormal Child Psychology, 35, 265–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hetrick, S.E. , McKenzie, J.E. , Bailey, A.P. , Sharma, V. , Moller, C.I. , Badcock, P.B. , … & Meader, N. (2021). New generation antidepressants for depression in children and adolescents: A network meta‐analysis. Cochrane Database of Systematic Reviews, 5, CD013674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoover, D.W. , & Kaufman, J. (2018). Adverse childhood experiences in children with autism spectrum disorder. Current Opinion in Psychiatry, 31, 128–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hosozawa, M. , Sacker, A. , & Cable, N. (2021). Timing of diagnosis, depression and self‐harm in adolescents with autism spectrum disorder. Autism, 25, 70–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudson, C.C. , Hall, L. , & Harkness, K.L. (2019). Prevalence of depressive disorders in individuals with autism spectrum disorder: A meta‐analysis. Journal of Abnormal Child Psychology, 47, 165–175. [DOI] [PubMed] [Google Scholar]
- Humphreys, K.L. , Katz, S.J. , Lee, S.S. , Hammen, C. , Brennan, P.A. , & Najman, J.M. (2013). The association of ADHD and depression: Mediation by peer problems and parent‐child difficulties in two complementary samples. Journal of Abnormal Psychology, 122, 854–867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaffee, S.R. , Moffitt, T.E. , Caspi, A. , Fombonne, E. , Poulton, R. , & Martin, J. (2002). Differences in early childhood risk factors for juvenile‐onset and adult‐onset depression. Archives of General Psychiatry, 59, 215–222. [DOI] [PubMed] [Google Scholar]
- Jensen, C.M. , & Steinhausen, H.C. (2015). Comorbid mental disorders in children and adolescents with attention‐deficit/hyperactivity disorder in a large nationwide study. ADHD Attention Deficit and Hyperactivity Disorders, 7, 27–38. [DOI] [PubMed] [Google Scholar]
- Joseph, C.I. , Evans, S. , Youssef, G.J. , Silk, T. , Anderson, V. , Efron, D. , & Sciberras, E. (2019). Characterisation of depressive symptoms in young children with and without attention deficit hyperactivity disorder. European Child and Adolescent Psychiatry, 28, 1183–1192. [DOI] [PubMed] [Google Scholar]
- Kim, J.W. , Yu, H. , Ryan, N.D. , Axelson, D.A. , Goldstein, B.I. , Goldstein, T.R. , … & Birmaher, B. (2015). Longitudinal trajectories of ADHD symptomatology in offspring of parents with bipolar disorder and community controls. The Journal of Clinical Psychiatry, 76, 599–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinnaird, E. , Stewart, C. , & Tchanturia, K. (2019). Investigating alexithymia in autism: A systematic review and meta‐analysis. European Psychiatry, 55, 80–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kita, Y. , & Inoue, Y. (2017). The direct/indirect association of ADHD/ODD symptoms with self‐esteem, self‐perception, and depression in early adolescents. Frontiers in Psychiatry, 8, 137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraper, C.K. , Kenworthy, L. , Popal, H. , Martin, A. , & Wallace, G.L. (2017). The gap between adaptive behavior and intelligence in autism persists into young adulthood and is linked to psychiatric co‐morbidities. Journal of Autism and Developmental Disorders, 47, 3007–3017. [DOI] [PubMed] [Google Scholar]
- Ljung, T. , Chen, Q. , Lichtenstein, P. , & Larsson, H. (2014). Common etiological factors of attention‐deficit/hyperactivity disorder and suicidal behavior: A population‐based study in Sweden. JAMA Psychiatry, 71, 958–964. [DOI] [PubMed] [Google Scholar]
- Lopez, P.L. , Torrente, F.M. , Ciapponi, A. , Lischinsky, A.G. , Cetkovich‐Bakmas, M. , Rojas, J.I. , … Cochrane Developmental, Psychosocial and Learning Problems Group . (2018). Cognitive‐behavioural interventions for attention deficit hyperactivity disorder (ADHD) in adults. Cochrane Database of Systematic Reviews, 3, CD010840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazzone, L. , Postorino, V. , Siracusano, M. , Riccioni, A. , & Curatolo, P. (2018). The relationship between sleep problems, neurobiological alterations, core symptoms of autism Spectrum disorder, and psychiatric comorbidities. Journal of Clinical Medicine, 7, 102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGillivray, J.A. , & Evert, H.T. (2014). Group cognitive behavioural therapy program shows potential in reducing symptoms of depression and stress among young people with ASD. Journal of Autism and Developmental Disorders, 44, 2041–2051. [DOI] [PubMed] [Google Scholar]
- McIntosh, D. , Kutcher, S. , Binder, C. , Levitt, A. , Fallu, A. , & Rosenbluth, M. (2009). Adult ADHD and comorbid depression: A consensus‐derived diagnostic algorithm for ADHD. Neuropsychiatric Disease and Treatment, 5, 137–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meinzer, M.C. , Felton, J.W. , Oddo, L.E. , Rubin, K.H. , & Chronis‐Tuscano, A. (2020). Do ADHD symptoms and relationship quality with mothers and best friends across high school predict depressive symptoms for adolescents? Journal of Attention Disorders, 25, 1699–1711. [DOI] [PubMed] [Google Scholar]
- Meinzer, M.C. , Lewinsohn, P.M. , Pettit, J.W. , Seeley, J.R. , Gau, J.M. , Chronis‐Tuscano, A. , & Waxmonsky, J.G. (2013). Attention‐deficit/hyperactivity disorder in adolescence predicts onset of major depressive disorder through early adulthood. Depression and Anxiety, 30, 546–553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meinzer, M.C. , Pettit, J.W. , & Viswesvaran, C. (2014). The co‐occurrence of attention‐deficit/hyperactivity disorder and unipolar depression in children and adolescents: A meta‐analytic review. Clinical Psychology Review, 34, 595–607. [DOI] [PubMed] [Google Scholar]
- Montazeri, F. , de Bildt, A. , Dekker, V. , & Anderson, G.M. (2020). Network analysis of behaviors in the depression and autism realms: Inter‐relationships and clinical implications. Journal of Autism and Developmental Disorders, 50, 1580–1595. [DOI] [PubMed] [Google Scholar]
- Morie, K.P. , Jackson, S. , Zhai, Z.W. , Potenza, M.N. , & Dritschel, B. (2019). Mood disorders in high‐functioning autism: The importance of alexithymia and emotional regulation. Journal of Autism and Developmental Disorders, 49, 2935–2945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute for Health and Clinical Excellence . (2012). Autism spectrum disorder in under 19s: recognition, referral and diagnosis [NICE Guideline No. 128] . Available from: https://www.nice.org.uk/guidance/cg128 [last accessed 8 September 2021]. [PubMed]
- National Institute for Health and Clinical Excellence . (2018). Attention deficit hyperactivity disorder: diagnosis and management [NICE Guideline No. 87] . Available from: https://www.nice.org.uk/guidance/ng87 [last accessed 8 September2021]
- National Institute for Health and Clinical Excellence . (2019). Depression in children and young people: identification and management [NICE Guideline No. 134] . Available from: https://www.nice.org.uk/guidance/ng134 [last accessed 8 September2021] [PubMed]
- Ostrander, R. , & Herman, K.C. (2006). Potential cognitive, parenting, and developmental mediators of the relationship between ADHD and depression. Journal of Consulting and Clinical Psychology, 74, 89–98. [DOI] [PubMed] [Google Scholar]
- Patterson, G.R. , & Stoolmiller, M. (1991). Replications of a dual failure model for boys' depressed mood. Journal of Consulting and Clinical Psychology, 59, 491–498. [DOI] [PubMed] [Google Scholar]
- Pezzimenti, F. , Han, G.T. , Vasa, R.A. , & Gotham, K. (2019). Depression in youth with autism Spectrum disorder. Child and Adolescent Psychiatric Clinics of North America, 28, 397–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell, V. , Agha, S.S. , Jones, R.B. , Eyre, O. , Stephens, A. , Weavers, B. , … & Rice, F. (2021). ADHD in adults with recurrent depression. Journal of Affective Disorders, 295, 1153–1160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell, V. , Riglin, L. , Hammerton, G. , Eyre, O. , Martin, J. , Anney, R. , … & Rice, F. (2020). What explains the link between childhood ADHD and adolescent depression? Investigating the role of peer relationships and academic attainment. European Child and Adolescent Psychiatry, 29, 1581–1591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell, V. , Riglin, L. , Ng‐Knight, T. , Frederickson, N. , Woolf, K. , McManus, C. , … & Rice, F. (2021). Investigating friendship difficulties in the pathway from ADHD to depressive symptoms. Can parent‐child relationships compensate? Research on Child and Adolescent Psychopathology, 49, 1031–1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Purper‐Ouakil, D. , Porfirio, M.C. , Le Strat, Y. , Falissard, B. , Gorwood, P. , & Masi, G. (2017). What do childhood attention deficit/hyperactivity symptoms in depressed adults tell us about the bipolar spectrum? Psychiatry Research, 249, 244–251. [DOI] [PubMed] [Google Scholar]
- Rai, D. , Culpin, I. , Heuvelman, H. , Magnusson, C.M.K. , Carpenter, P. , Jones, H.J. , … & Pearson, R.M. (2018). Association of autistic traits with depression from childhood to age 18 years. JAMA Psychiatry, 75, 835–843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ratanatharathorn, A. , Koenen, K.C. , Chibnik, L.B. , Weisskopf, M.G. , Rich‐Edwards, J.W. , & Roberts, A.L. (2021). Polygenic risk for autism, attention‐deficit hyperactivity disorder, schizophrenia, major depressive disorder, and neuroticism is associated with the experience of childhood abuse. Molecular Psychiatry, 26, 1696–1705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rice, F. , Riglin, L. , Thapar, A.K. , Heron, J. , Anney, R. , O'Donovan, M.C. , & Thapar, A. (2019). Characterizing developmental trajectories and the role of neuropsychiatric genetic risk variants in early‐onset depression. JAMA Psychiatry, 76, 306–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riglin, L. , Eyre, O. , Thapar, A.K. , Stringaris, A. , Leibenluft, E. , Pine, D.S. , … & Thapar, A. (2019). Identifying novel types of irritability using a developmental genetic approach. American Journal of Psychiatry, 176, 635–642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riglin, L. , Leppert, B. , Dardani, C. , Thapar, A.K. , Rice, F. , O'Donovan, M.C. , … & Thapar, A. (2020). ADHD and depression: Investigating a causal explanation. Psychological Medicine, 51, 1890–1897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy, A. , Hartman, C.A. , Veenstra, R. , & Oldehinkel, A.J. (2015). Peer dislike and victimisation in pathways from ADHD symptoms to depression. European Child and Adolescent Psychiatry, 24, 887–895. [DOI] [PubMed] [Google Scholar]
- Rutter, M. (2015). Some of the complexities involved in gene‐environment interplay. International Journal of Epidemiology., 44, 1128–1129. [DOI] [PubMed] [Google Scholar]
- Schiltz, H.K. , McVey, A.J. , Dolan, B.K. , Willar, K.S. , Pleiss, S. , Karst, J.S. , … & van Hecke, A.V. (2018). Changes in depressive symptoms among adolescents with ASD completing the PEERS® social skills intervention. Journal of Autism and Developmental Disorders, 48, 834–843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartzman, J.M. , & Corbett, B.A. (2020). Higher depressive symptoms in early adolescents with autism spectrum disorder by self‐ and parent‐report compared to typically‐developing peers. Research in Autism Spectrum Disorders, 77, 101613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seymour, K.E. , Chronis‐Tuscano, A. , Halldorsdottir, T. , Stupica, B. , Owens, K. , & Sacks, T. (2012). Emotion regulation mediates the relationship between ADHD and depressive symptoms in youth. Journal of Abnormal Child Psychology, 40, 595–606. [DOI] [PubMed] [Google Scholar]
- Seymour, K.E. , Chronis‐Tuscano, A. , Iwamoto, D.K. , Kurdziel, G. , & MacPherson, L. (2014). Emotion regulation mediates the association between ADHD and depressive symptoms in a community sample of youth. Journal of Abnormal Child Psychology, 42, 611–621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw, P. , Stringaris, A. , Nigg, J. , & Leibenluft, E. (2014). Emotion dysregulation in attention deficit hyperactivity disorder. American Journal of Psychiatry, 171, 276–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sizoo, B.B. , & Kuiper, E. (2017). Cognitive behavioural therapy and mindfulness based stress reduction may be equally effective in reducing anxiety and depression in adults with autism spectrum disorders. Research in Developmental Disabilities, 64, 47–55. [DOI] [PubMed] [Google Scholar]
- Smith, I.C. , & White, S.W. (2020). Socio‐emotional determinants of depressive symptoms in adolescents and adults with autism spectrum disorder: A systematic review. Autism, 24, 995–1010. [DOI] [PubMed] [Google Scholar]
- Smith, Z.R. , Zald, D.H. , & Lahey, B.B. (2020). Sluggish cognitive tempo and depressive symptoms in children and adolescents predict adulthood psychopathology. Journal of Abnormal Child Psychology, 48, 1591–1601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stern, A. , Agnew‐Blais, J. , Danese, A. , Fisher, H.L. , Jaffee, S.R. , Matthews, T. , … & Arseneault, L. (2018). Associations between abuse/neglect and ADHD from childhood to young adulthood: A prospective nationally‐representative twin study. Child Abuse and Neglect, 81, 274–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stern, A. , Agnew‐Blais, J.C. , Danese, A. , Fisher, H.L. , Matthews, T. , Polanczyk, G.V. , … & Arseneault, L. (2020). Associations between ADHD and emotional problems from childhood to young adulthood: A longitudinal genetically sensitive study. Journal of Child Psychology and Psychiatry, 61, 1234–1242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thapar, A. (2018). Discoveries on the genetics of ADHD in the 21st century: New findings and their implications. The American Journal of Psychiatry, 175, 943–950. [DOI] [PubMed] [Google Scholar]
- Thapar, A. , Collishaw, S. , Pine, D.S. , & Thapar, A.K. (2012). Depression in adolescence. The Lancet, 379, 1056–1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thapar, A. , Cooper, M. , & Rutter, M. (2017). Neurodevelopmental disorders. The Lancet Psychiatry, 4, 339–346. [DOI] [PubMed] [Google Scholar]
- Thapar, A. , & Rutter, M. (2021). Genetic advances in autism. Journal of Autism and Developmental Disorders, 51, 4321–4332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uljarević, M. , Richdale, A.L. , McConachie, H. , Hedley, D. , Cai, R.Y. , Merrick, H. , … & le Couteur, A. (2018). The hospital anxiety and depression scale: Factor structure and psychometric properties in older adolescents and young adults with autism spectrum disorder. Autism Research, 11, 258–269. [DOI] [PubMed] [Google Scholar]
- Wang, H.E. , Cheng, C.M. , Bai, Y.M. , Hsu, J.W. , Huang, K.L. , Su, T.P. , … & Chen, M.H. (2022). Familial coaggregation of major psychiatric disorders in first‐degree relatives of individuals with autism spectrum disorder: A nationwide population‐based study. Psychological Medicine, 52, 1437–1447. [DOI] [PubMed] [Google Scholar]
- Weston, L. , Hodgekins, J. , & Langdon, P.E. (2016). Effectiveness of cognitive behavioural therapy with people who have autistic spectrum disorders: A systematic review and meta‐analysis. Clinical Psychology Review, 49, 41–54. [DOI] [PubMed] [Google Scholar]
- White, S.W. , Simmons, G.L. , Gotham, K.O. , Conner, C.M. , Smith, I.C. , Beck, K.B. , & Mazefsky, C.A. (2018). Psychosocial treatments targeting anxiety and depression in adolescents and adults on the autism spectrum: Review of the latest research and recommended future directions. Current Psychiatry Reports, 20, 82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright, M.F. (2017). Cyber victimization and depression among adolescents with autism spectrum disorder: The buffering effects of parental mediation and social support. Journal of Child & Adolescent Trauma, 11, 17–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoshimasu, K. , Barbaresi, W.J. , Colligan, R.C. , Voigt, R.G. , Killian, J.M. , Weaver, A.L. , & Katusic, S.K. (2012). Childhood ADHD is strongly associated with a broad range of psychiatric disorders during adolescence: A population‐based birth cohort study. Journal of Child Psychology and Psychiatry, 53, 1036–1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zwicker, A. , MacKenzie, L.E. , Drobinin, V. , Bagher, A.M. , Howes Vallis, E. , Propper, L. , … & Uher, R. (2020). Neurodevelopmental and genetic determinants of exposure to adversity among youth at risk for mental illness. Journal of Child Psychology and Psychiatry, 61, 536–544. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Search criteria for literature search.


