Abstract
PUBLIC CONCERN AND AWARENESS ARE GROWING about adverse health effects of exposure to environmental contaminants. Frequently patients present to their physicians with questions or concerns about exposures to such substances as lead, air pollutants and pesticides. Most primary care physicians lack training in and knowledge of the clinical recognition, management and avoidance of such exposures. We have found that it can be helpful to use the CH2OPD2 mnemonic (Community, Home, Hobbies, Occupation, Personal habits, Diet and Drugs) as a tool to identify a patient's history of exposures to potentially toxic environmental contaminants. In this article we discuss why it is important to take a patient's environmental exposure history, when and how to take the history, and how to interpret the findings. Possible routes of exposure and common sources of potentially toxic biological, physical and chemical substances are identified. A case of sick-building syndrome is used to illustrate the use of the mnemonic.
Case
A 40-year-old married bookkeeper presents with a 3-year history of headaches. She describes having “tight,” bitemporal headaches almost daily that resolve after taking three 325-mg tablets of ASA. She also complains of a “spacey” feeling, difficulty concentrating and remembering, fatigue, a stuffy nose and a full feeling in her ears. Her symptoms improve on weekends and over the holidays and seem to be worse in the winter. Over the past 2 years she has noticed that she gets a stuffy nose and headaches when exposed to perfumes, tobacco smoke and automobile exhaust. Her past medical history is remarkable only for infantile eczema. Her family history is unremarkable other than her mother having hypothyroidism. She is taking no medications other than ASA, does not smoke, reports having no allergies and says she is happily married with no major family, financial or social concerns. She enjoys her work and coworkers. On physical examination she has puffy, dark circles under her eyes, there is loss of light reflex on her left ear drum, and her nasal mucosa appears edematous and erythematous. There are multiple excoriated, erythematous papules 5 mm in diameter on her face, anterior chest and anterior lower legs.
Questions surrounding this case: What is sick-building syndrome and how do patients commonly present? What causes or contributes to sick-building syndrome? What are the risk factors? How should cases be managed?
Why is taking an environmental exposure history important?
Health Canada recently issued a warning to parents about the unacceptable health risks from exposure to diisononyl phthalate in children under 1 year old who chew on toys made of polyvinyl chloride for extended periods.1 When warnings such as these are issued parents seek advice and answers from physicians to such questions as: What is diisononyl phthalate? Are there other sources besides plastic toys? Could something in the environment be causing me to feel this crummy? In a recent survey Ontario family physicians reported that they are asked many questions by patients about the environment, yet most of the physicians rated their level of knowledge on environmental health issues to be very low.2
The task of identifying, measuring and reducing the risks to human health associated with environmental exposure to toxins can be difficult, its accomplishment hindered by the scale of the problem and by the limits of data and methodology. Research bodies such as the International Joint Commission and Health Canada's Great Lakes Health Effects Program may invoke the “precautionary principle” when weighing the accumulated evidence from wildlife studies, toxicological research on laboratory animals, epidemiological data and case reports of accidental poisonings. In 1997 Health Canada issued a statement saying that “the weight of evidence indicates that certain heavy metals and persistent chlorinated contaminants, present as low level contaminants in the Great Lakes basin, can cause adverse health effects in animals and humans.”3 These effects can be acute and chronic. The International Joint Commission compiled a list of 11 critical pollutants: PCBs, dioxins, furans, toxaphene, DDT, mirex, dieldrin, hexachlorobenzene and benzopyrene, methyl mercury and alkyl lead.4 All humans have body burdens of foreign chemicals. These “xenobiotics” enter the body through inhalation, ingestion and skin contact and can be found throughout the body, including serum,5 breast milk,6 semen,7 adipose tissue,8 bone9 and follicular fluid.10
Environmental health problems frequently present as common medical problems (e.g., headache, difficulty concentrating, behavioural problems, rashes, asthma, angina, myalgia, difficulty conceiving, spontaneous abortions).11,12 However, consideration of environmental factors rarely enters into the clinician's history taking or diagnosis. A chart review of 2922 histories taken by 137 third-year medical students showed that smoking status was documented in 91% of cases, occupation in 70% and specific occupational exposures in 8.4%. Patients less than 40 years of age and women were significantly less likely than older patients or men to have their occupation and industry noted.13 Since patterns of history taking and differential diagnoses are set in medical school, it appears that physicians and their educators are lagging behind public concern and awareness about environmental exposures.14 However, with more than 70 000 industrial chemicals in use,11 it is simply not possible for a physician to sit down and run through a checklist of possible exposures with everyone. An organized approach and framework is therefore essential.
When should the history be taken?
It may be fruitful to take an environmental exposure history at a patient's entry into the practice; when a patient has a family history of asthma, allergies or autoimmune disease; during prenatal or preconceptual counselling; when a patient links onset of symptoms to environmental exposures; when a patient reports puzzling, nonspecific symptoms; or when a patient or family presents with frequent office visits for various illnesses.
In the sample case described earlier, a previously healthy patient presents with a 3-year history of various puzzling, nonspecific symptoms.
How should the history be taken?
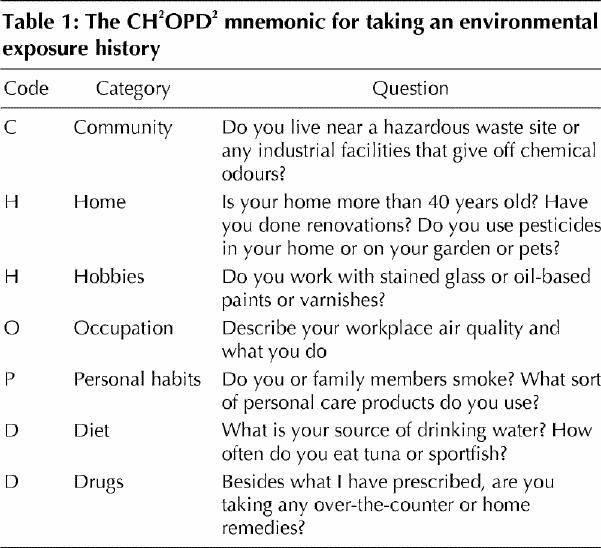
The task of identifying a particular exposure that might be related to an array of symptoms can be like looking for a needle in a haystack. An efficient approach involves searching for a change in the environment related to symptom onset or exacerbation rather than looking for a specific exposure. Since the timing of symptom onset or exacerbation is often linked to the source or setting of the exposure, it helps to organize the exposure history by the possible source or setting using the CH2OPD2 mnemonic (Community, Home, Hobbies, Occupation, Personal habits, Diet and Drugs) to direct general questions (Table 1).
Table 1
More specific questions can be asked about whether the symptoms are temporally related to being in the home, work or community environments and whether the onset was associated with any recent dietary or environmental changes such as a move, a new work location, renovations, new hobbies, furniture, plants or pets. Are symptoms better on weekends? Are they present when away from home or on vacation? Do they occur in other specific settings? Does anyone else at home or at work have these or other symptoms that started around the same time?
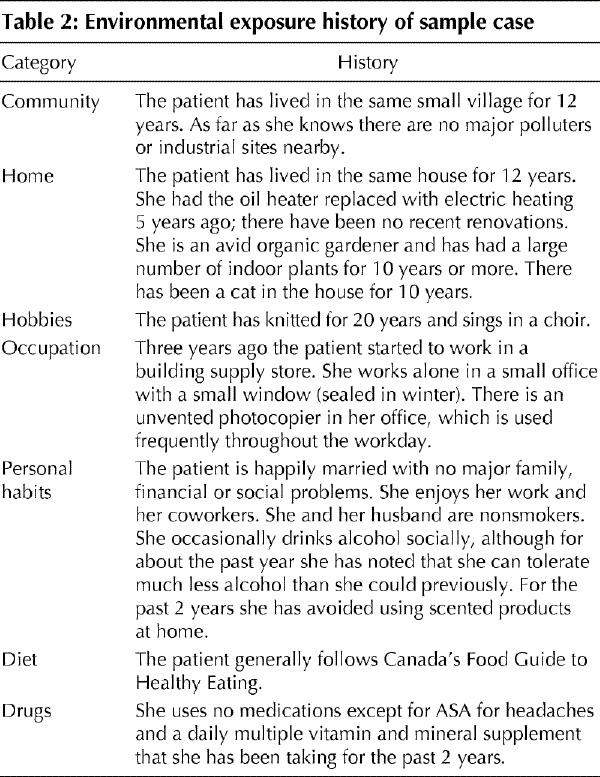
An exposure history questionnaire organized according to the CH2OPD2 mnemonic is available at www.cfpc.ca/ocfp/index.html (click on “Exposure History Sheets in MS Word” in the scrolling menu located in the middle of the Web page). The environmental exposure history of the patient in the sample case is summarized in Table 2.
Table 2
Interpreting the findings
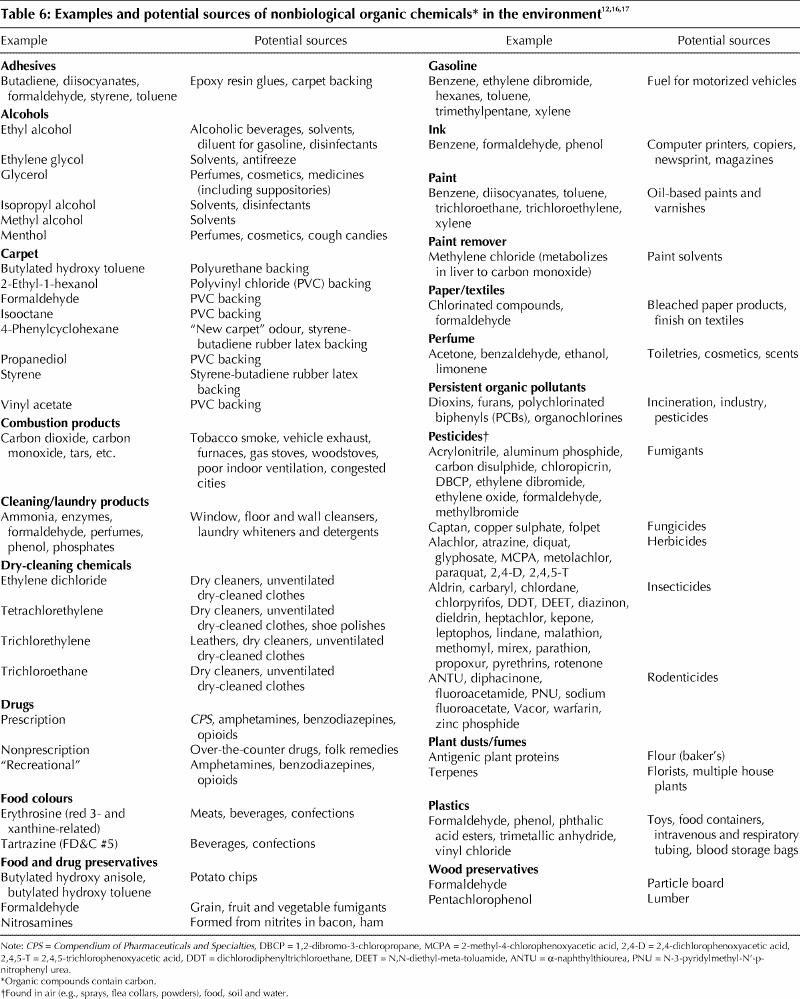
The environmental exposure history of the patient in the sample case suggests that symptom onset was related to her occupational history, indicating a possible toxic occupational exposure. It is helpful to think in terms of major pathways of exposure using a simple schema, adopted by Health Canada's Great Lakes Health Effects Program.15 This schema links the type of exposure (biological, physical or chemical) to the environmental media (air, soil, food or water) and the routes of exposure (inhalation, skin contact or ingestion). It is helpful to think of soil in the broad terms of surface contacts (e.g., plastic toys) rather than simply soil (e.g., playground dirt as a potential source of residual lead). Tables 3-6 identify common examples of biological, physical and chemical contaminants that individuals may encounter.
Table 3
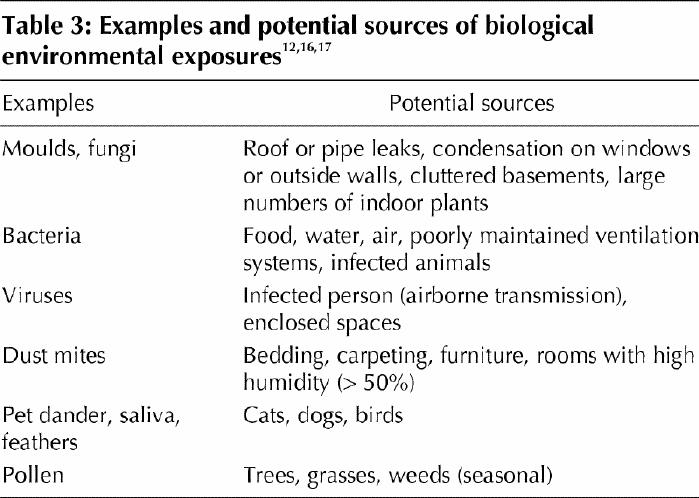
Table 4
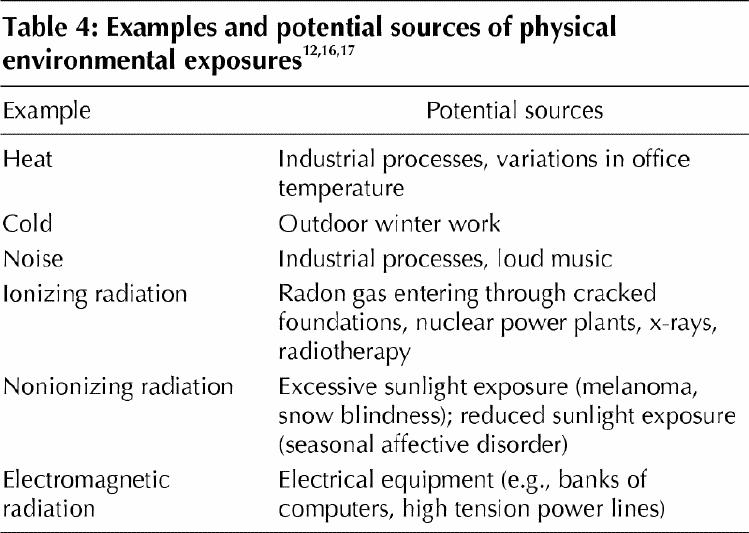
Table 5
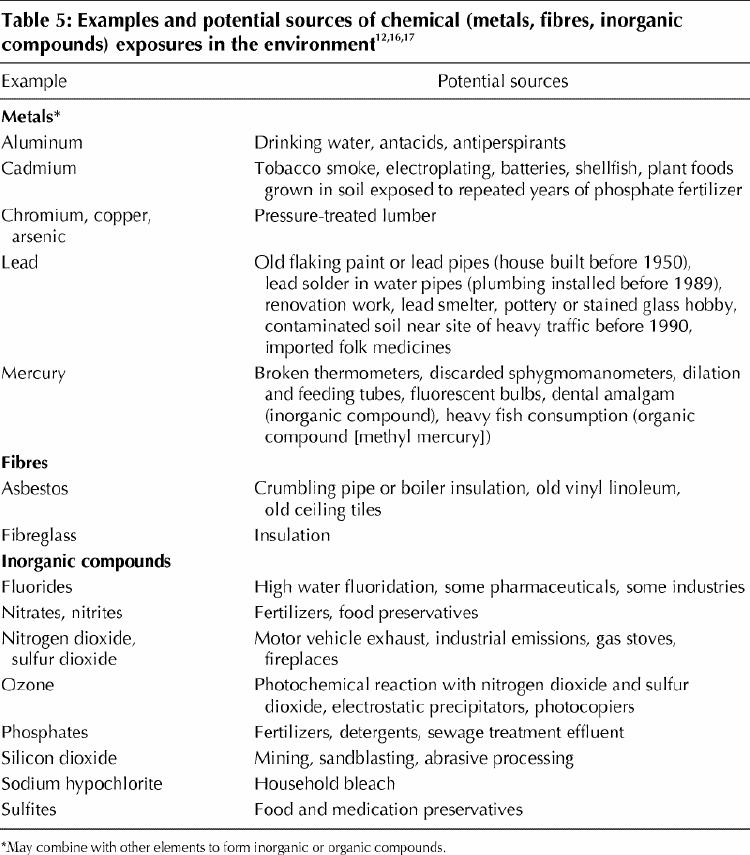
Table 6
Linking the symptoms to the exposure
A possible link between the exposure and the symptoms is established on the basis of observation and correlation. When exposure to potential hazards associated with either the onset or worsening of symptoms is identified by the environmental exposure history, the physician can either advise precautionary avoidance or refer to an environmental, occupational or public health specialist for further assistance with management. Certified industrial hygienists, environmental engineers or home inspectors certified by Canada Mortgage and Housing Corporation can investigate exposures using more detailed measurement tools.
Given the exposure history in the sample case (Table 2), it seems likely that the woman's symptoms are linked to an occupational environmental exposure, in a poorly ventilated office, to volatile organic compounds in the photocopier ink or to ozone produced secondary to the photocopying process.18 The physician adopted a precautionary approach by advising the woman to avoid exposure to the photocopier. After it was removed from her office and the window opened, the patient's symptoms cleared and did not return.
The questions answered
What is sick-building syndrome and how do patients commonly present?
In the 1970s there were reports of symptoms linked with occupancy of buildings that had been deliberately “tightened” to conserve energy during a Middle East oil embargo. In 1982 and 1984 the World Health Organization described “symptoms with increased frequency in buildings with indoor climate problems.”19,20 These nonspecific symptoms included irritation of the eyes, nose and throat, dry, red mucous membranes and skin, headache, upper respiratory tract infections, lower airway symptoms, abnormal taste, distorted sense of smell, general fatigue, dizziness and nausea. These symptoms are associated with being in a particular building by the temporal pattern of their occurrence and the clustering among inhabitants or colleagues, and by the absence of a specific illness such as hypersensitivity pnuemonitis or infection.21
What causes or contributes to sick-building syndrome?
Investigations into sick-building syndrome have suggested that its origins are multifactorial,22,23 and several pathophysiological mechanisms have been hypothesized.24,25,26 Four predominant factors appear to contribute to the syndrome: air contaminants, poor ventilation, host factors and work organization factors (e.g., job satisfaction, stress and social structures).21,22
What are the risk factors?
Risk factors for sick-building syndrome include atopy, female sex, low-paying, low-status job category, handling of paper, a job in a workplace with poor mechanical ventilation and inadequately maintained air conditioning, use of a video-display terminal, outdoor-air flow rates below 10 L/s per person, airway hyperreactivity and existing respiratory or dermatological disease.21,22
Employees exposed to toxic chemical spills at work have subsequently reported symptoms on exposure to apparently chemically unrelated, commonly encountered environmental contaminants at low levels.27 The patient in the sample case noted that the occurrence of her symptoms had spread to occasions when she was exposed to chemicals outside the workplace (perfumes, tobacco smoke, automobile exhaust).
How should cases be managed?
First take an environmental exposure history using the CH2OPD2 mnemonic and then a more extensive history if a site-specific exposure is suspected. Suggest that the patient avoid exposure; for example, in the sample case the volatile emissions from the photocopier (ink, ozone) can be avoided by having the photocopier removed from the office and improving ventilation by opening the office window. Get the patient's signed consent to allow you to make this recommendation to the employer (supervisor or human resources director) directly, either by telephone or letter. Ask the patient to request the Material Safety Data Sheets (MSDS [www.hc-sc.gc.ca/ehp/ehd/psb/whmis/msds.htm]) for materials used in relevant areas of the workplace. These sheets must be made available to the employer by the suppliers of all hazardous products used in the workplace and, in turn, must be readily available to employees. The sheets outline known adverse health effects related to exposure to the materials and recommend precautions. If the employer seems unwilling to accommodate the worker, contact the employer again and use the information in the MSDS to reinforce your recommendation.28,29 The Occupational Health and Safety Act of Ontario30 states that, in general, any workplace in the province that regularly employs 20 or more people must have a joint health and safety committee composed of members who represent the employer and the employees. It is the role of this committee to identify potential health and safety problems and to bring them to the attention of the employer. If the patient is a member of a union, union representatives may be helpful in advocating for the patient. If necessary, the employee can refuse to work in the unremediated environment, and the Ministry of Labour will be compelled to investigate. If the patient's symptoms do not improve after the workplace environment has been modified, then referral to an environmental or occupational health specialist is indicated.
Additional resources
· Case studies in environmental medicine: taking an exposure history. Atlanta: Agency for Toxic Substances and Disease Registry, US Department of Health and Human Services; 1992. Available: www.atsdr.cdc.gov/HEC/CSEM/exphistory/index.html (revised Mar 2000; accessed 2002 Mar 22).
· Children's Health Project: environmental standard setting and children's health. Toronto: Canadian Environmental Law Association and Ontario College of Family Physicians Enviromental Health Committee; 2000. Available: www.cela.ca/ch_health/titlepg.htm (accessed 2002 Mar 15).
· Committee on Environmental Health, American Academy of Pediatrics. Handbook of pediatric environmental health. Elk Grove Village (IL): The Academy; 1999. p. 25-31.
· A guide to the Occupational Health and Safety Act. Toronto: Ontario Ministry of Labour; 2000. Available: www.gov.on.ca/lab/ohs/g_ohse.htm (accessed 2002 Mar 22).
· Guidotti TL, Gosselin P, editors, with the Canadian Association of Physicians for the Environment. The Canadian guide to health and the environment. Edmonton: University of Alberta Press; 1990.
· The health and environment handbook for health professionals. Ottawa: Health Canada; 1998. Available: www.hc-sc.gc.ca/ehp/ehd/catalogue/bch_pubs/98ehd211/98ehd211.htm (accessed 2002 Mar 15).
· In harm's way: toxic threats to child development. Boston: The Greater Boston Physicians for Social Responsibility; 2000. Available: www.igc.org/psr/ihw.htm (accessed 2002 Mar 15).
· Miller CS, Prihoda TJ. The Environmental Exposure and Sensitivity Inventory: A standardized approach for measuring chemical intolerances for research and clinical applications. Toxicol Ind Health 1999;15:370-85.
· Quinlan P, Macher JA, Alvantis LE, Cone JE. Protocol for the comprehensive evaluation of building-associated illness in occupational medicine. In: Problem buildings. Vol 4 of State of the Art Reviews. Philadelphia: Hanley & Belfus; Oct-Dec 1989. p. 771-97.
· Workplace Hazardous Material Information System: www.hc-sc.gc.ca/ehp/ehd/psb/whmis.htm (accessed 2002 Mar 22).
β See related article page 1041
Acknowledgments
Financial support for the original exposure history module was provided by the Ontario Ministry of Health and Long-Term Care.
Footnotes
[A detailed exposure history questionnaire is available on the Ontario College of Family Physicians Web site (www.cfpc.ca/ocfp/index.html — click on “Exposure History Sheets in MS Word” in the scrolling menu located in the middle of the page). The different components (Community, Home and Hobby, Occupation or School, Personal habits, Diet and Drugs) can be printed on coloured paper for easy identification in patient charts. The questionnaire may be given to a patient to complete at home and bring to the next appointment for review and interpretation.]
This article has been peer reviewed.
Contributors: Drs. Marshall and Weir contributed substantially to the conception and design, drafting of the article, and data acquisition, analysis and interpretation. Drs. Abelsohn and Sanborn contributed to the conception and design of the article. All authors contributed to the revising of the manuscript and gave final approval.
Competing interests: None declared.
Correspondence to: Dr. Lynn Marshall, Medical Director, Environmental Health Clinic, Sunnybrook & Women's College Health Sciences Centre, Rm. 538, 76 Grenville St., Toronto ON M5S 1B2
References
- 1.Risk assessment on diisononyl phthalate in vinyl children's products. Ottawa: Consumer Products Division, Product Saftey Bureau, Environmental Health Directorate, Health Protection Branch, Health Canada; 1998. Available: www.hc-sc.gc.ca/english/protection/warnings/1998/risk.html (accessed 2002 Mar 18).
- 2.Sanborn MD, Scott EA. Environmental health concerns in urban and rural family practice. Can Fam Physician 1998;44:1466-72. [PMC free article] [PubMed]
- 3.Reidel D, Tremblay N, Tompkins E. State of knowledge report on environmental contaminants and human health in the Great Lakes Basin. Ottawa: Health Canada; 1997.
- 4.Eighth biennial report under the Great Lakes Water Quality Agreement of 1978 to the governments of the United States and Canada and the state and provincial governments of the Great Lakes Basin. International Joint Commission; 1996. Available: www.ijc.org/comm/8bre.html (accessed 2002 Mar 14).
- 5.Sala M, Sunyer J, Otero R, Santiago-Silva M, Camps C, Grimalt J. Organochlorine in the serum of inhabitants living near an electrochemical factory. Occup Environ med 1999;56(3):152-8. [DOI] [PMC free article] [PubMed]
- 6.Nakagawa R, Hirakawa H, Ida T, Matsueda T, Nagajama J. Maternal body burden of organochlorine pesticides and dioxins. J AOAC Int 1999;82:716-24. [PubMed]
- 7.Schecter A, Mcgee H, Stanley JS, Boggs K, Brandt-Rauf P. Dioxins and dioxin-like chemicals in blood and semen of American Vietnam veterans from the state of Michigan. Am J Ind Med 1996;30:647-54. [DOI] [PubMed]
- 8.Bertram H, Kemper FH, Muller C. Hexachlorobenzene content in human whole blood and adipose tissue: experiences in environmental specimen banking. IARC Sci Publ 1986;77:173-82. [PubMed]
- 9.Ambrose TM, Al-Lozi M, Scott MG. Bone lead concentrations assessed by in vivo x-ray fluorescence. Clin Chem 2000;46:1171-8. [PubMed]
- 10.Baukloh, Bohnet HG, Trapp M, Heeschen W, Feichtinger W, Kemeter P. Biocides in human follicular fluid. Ann N Y Acad Sci 1985;442:240-50. [DOI] [PubMed]
- 11.Wigle D. Child health and the environment. Patient Care Canada 2000;11: 54-62.
- 12.Amdur MO, Doull J, Klaassen CD, editors. Casarett and Doull's toxicology: the basic science of poisons. 4th ed. New York: Pergamon Press; 1991.
- 13.McCurdy SA, Morrin LA, Memmott MM. Occupational history collection by third-year medical students during internal medicine and surgery inpatient clerkships. J Occup Environ Med 1998;40(8):680-4. [DOI] [PubMed]
- 14.Merritt EF. Human health and the environment. Are physician educators lagging behind? JAMA 1999;281:1661. [DOI] [PubMed]
- 15.Health Canada. Investigating human exposure to contaminants in the environment: a handbook for exposure calculations. Ottawa: Health Canada; 1995. Cat no H49-96/1-1995E. Available: www.hc-sc.gc.ca/ehp/ehd/catalogue/bch_pubs/95ehd193.htm (accessed 2002 Mar 15).
- 16.Lippman M, editor. Environmental toxicants, human exposures and their health effects. New York: John Wiley and Sons Inc.; 1992.
- 17.Greenberg MI, Hamilton RJ, Phillips SD. Occupational, industrial, and environmental toxicology. St. Louis: Mosby; 1997.
- 18.Rea WJ. Chemical sensitivity. Vol. 2. Boca Raton (FL): Lewis Publishers; 1994. p. 692-3.
- 19.World Health Organization. Indoor air pollutants. Exposure and health effects assessment, Euro-reports and studies. Report no. 78 Copenhagen: The Organization; 1982.
- 20.World Health Organization. Indoor air quality research. Euro-reports and studies. Report no. 103. Copenhagen: The Organization; 1984.
- 21.Redlich CA, Sparer J, Cullen MR. Sick-building syndrome. Lancet 1997; 349:1013-6. [DOI] [PubMed]
- 22.Stenberg B, Eriksson N, Hoog J, Sundell J, Wall S. The sick building syndrome (SBS) in office workers. A case-referent study of personal, psychosocial and building-related risk indicators. Int J Epidemiol 1994;23(6):1190-7. [DOI] [PubMed]
- 23.Chandrakumar M, Evans J, Arulanantham P. An investigation into sick building syndrome among local authority employees. Ann Occup Hyg 1994;38(5): 789-99. [DOI] [PubMed]
- 24.Cullinan P. Respiratory sensitization by chemical agents. Chem Ind 1994;Sept 5:680-2.
- 25.Meggs WJ. RADS and RUDS — the toxic induction of asthma and rhinitis. J Toxicol Clin Toxicol 1994;32(5):487-501. [DOI] [PubMed]
- 26.Bascom R, Meggs WJ, Framptom M, Hudnell K, Killburn K, Kobal G, et al. Neurogenic inflammation: with additional discussion of central and perceptual integration of nonneurogenic inflammation. Environ Health Perspect. 1997;105(2):531-7. [DOI] [PMC free article] [PubMed]
- 27.Cullen M. The worker with multiple chemical sensitivities: an overview. In: Cullen M, editor. Workers with multiple chemical sensitivitites. Philadelphia: Hanley & Belfus; 1987. p. 655-62. [PubMed]
- 28.Lax M, Henneberger P. Patients with multiple chemical sensitivities in an occupational health clinic: presentation and follow-up. Arch Environ Health 1995;50:425-31. [DOI] [PubMed]
- 29.The physician's role in helping patients return to work after an illness or injury [policy statement]. CMAJ 1997;156:680A-F. Available: www.cma.ca/staticContent/HTML/N0/l2/where_we_stand/return_to_work.pdf (accessed 2002 Mar 22). [PubMed]
- 30.Occupational Health and Safety Act. RSO 1990, c O-1. Available: http://192.75.156.68/DBLaws/Statutes/English/90o01_e.htm (accessed 2002 Mar 22).


