Abstract
Aim
To evaluate the trends in nursing burnout rates before and during the coronavirus 2019 restrictions.
Method
Meta-analysis was used to extract the data on global nursing burnout from 1 Jan. 2010–15 Dec. 2022. An interrupted time-series analysis using segmented ordinary least squares (OLS) regression models was used to explore if the nursing burnout were affected by the epidemic. Newey-West standard error was used to adjust for autocorrelation and heteroskedasticity.
Results
Before the epidemic (April 2020), the nursing burnout rate rose with 0.0007497 (95% CI: 0.0000316, 0.0014677, t = 2.07, P = 0.041) per month. The trend of nursing burnout rate has increased by 0.0231042 (95 CI%:0.0086818, 0.0375266, t = 3.18, P = 0.002). The increasing trend of nursing burnout rate after the COVID-19 restrictions is 0.0007497 + 0.0231042 = 0.0238539 per month.
Conclusion
The study indicated that the Covid-19 restrictions had an impact on nursing burnout, increasing the occurrence of nursing burnout syndrome.
Keywords: Burnout, Nurse, An interrupted time series analysis, COVID-19
1. Introduction
The COVID-19 restrictions have led to a social and economic crisis and caused much disruption, with long-term impacts on healthcare systems and disrupted delivery of routine healthcare services (Frenk J et al., 2022). After the restrictions, healthcare workers feel more stressful than general population, because they must always face specific challenges and stressors (Chirico et al., 2020). A recent study has shown that nurses suffer more psychological stress from the aftermath of the COVID-19 restrictions, reporting higher depressive symptoms, exhaustion, stress and lower job satisfaction (Lai et al., 2020). Too much psychological stress like exhaustion and low job satisfaction may cause burnout syndrome (Maslach et al., 2018).
Burnout syndrome is a work-related disease defined by the WHO (WHO, 2019), which is a common psychological problem faced by nurses and would have severe negative impacts on their work. For example, Ph. D. Sullivan once summarized that burnout could cause poor overall mental health of nurses, such as chronic stress, anxiety and depression. And these traumas can cause damage to the body through inflammation and metabolic syndrome, leading to more serious diseases such as high blood pressure, cardiovascular disease, stroke and diabetes. Meanwhile, the accumulation of chronic stress may directly affect job satisfaction, patient care and nurse retention (V. Sullivan et al., 2022). Shah MK et al. once found that 31.5% nurses in America wanted to leave their jobs because of burnout (Shah et al., 2021). Before the restrictions, many studies have shown that many nurses suffered from burnout syndrome due to the particularity of hospital work, nurses easily suffer from psychological problems in the environment of high pressure, irregular working hours, shifts and overnight work (Gualano et al., 2021, Woo et al., 2020). During the restrictions, most evidence suggested that nurses were significantly more affected than other professions in the health field. Nurses were demonstrated to have a higher risk of suffering from burnout and be under considerable mental strain, especially those on the frontlines (Badahdah et al., 2021, Pappa et al., 2020). Nurses caring for patients infected with COVID-19 were found deeply troubled by burnout, showing insomnia, depression, somatization, symptoms, anxiety and Post-Traumatic Stress Disorder (Busch et al., 2021, Lavoie-Tremblay et al., 2022). Such psychological trauma even led to the suicide of some medical staff. 1500 nurses from 44 countries have died during the COVID-19 restrictions up to 28 Oct. 2020, according to the International Council of Nurses (Galanis et al., 2021).
In recent years, many articles have studied nursing burnout. Before 2019, Woo et al. found that the global nursing burnout syndrome was 11.23%, which indicated a high burnout rate (Woo et al., 2020). During the restrictions, a study found that more than 40% of nurses in Japan experienced burnout (Matsuo T et al., 2020). Women were about 50% more likely to report burnout syndrome than men (Harry et al., 2022). The European Cancer Society has conducted two online surveys and found that the burnout rate of 1520 cancer workers from 101 countries surveyed from 16 April to 3 May, 2020 was 38%, while in the follow-up survey from 16 July to 6 August 2020, it was found that the burnout rate of respondents had reached 49% (Burki, 2020). Ph. D. Sullivan reviewed the history of the restrictions and conducted a comparative study of symptoms of burnout in nurses before and during the epidemic. Nursing burnout was a severe problem, exacerbated by the COVID-19 restrictions (D. Sullivan et al., 2022). However, most studies only described the severe influence of the restrictions on nursing burnout syndrome and the changing trend of nursing burnout before and during the restrictions has not been studied.
In our study, we aimed to evaluate the trends in nursing burnout rates before and during the COVID-19 restrictions using an interrupted time-series analysis.
2. Methods
2.1. Study design
This study evaluated the impact of ‘the COVID-19 restrictions’ on the nursing burnout rates around the world using an interrupted time-series analysis before and during the restrictions. The meta-analysis was used to obtain the rates of nursing burnout syndrome around the world from 1 Jan. 2010–15 Dec. 2022.
2.2. Definition of the nursing burnout rates
Maslach Burnout Inventory (MBI) was a frequent scale to measure burnout syndrome, which consists of three dimensions: depersonalization (DP), low personal accomplishment (PA) and emotional exhaustion (EE) (Maslach et al., 2018). In the DP (5 items), a score of 12 or more is considered high DP; a score of 6–11 is considered medium and below 6 is considered low. In the PA (8 items), a score of 33 or less indicates low PA, a score of 34–39 indicates moderate PA and a score of 40 or above indicates high PA. In EE (9 items), a score of 30 or more is considered high EE; 18–29 is considered medium and under 18 is considered low. The level of burnout syndrome is high when two or three dimensions are considered severe. The resulting data were the prevalence of nursing burnout syndrome, calculated as follows:
2.3. Data on burnout rates extracted through meta-analysis
Studies published in any language using PubMed, Web of Science (WOS), bioRvix, Cumulative Index to Nursing and Allied Health Literature (CINAHL) and medRVix were searched from1 Jan. 2010–15 Dec. 2022. Search keywords included “nurs* ”, “burnout” and “prevalence”. Specific search strategies were shown in Supplementary materials.
The type of sample in our study was nurse population, including nurses in any department and nursing assistants etc. Inclusion criteria: (a) sample inclusion time indicated in studies and the time is 2010 and later (preferably month, otherwise year); (b) When the samples mentioned in the studies were included in 2020 or April 2020 or later, the studies must mention the nursing burnout affected by the COVID-19 restrictions. Even if the sample inclusion time is mentioned, those who did not mention the COVID-19 restrictions will not be included; (d)outcome data included the rates of nursing burnout syndrome; (e) studies published in English. Exclusion criteria: (a) data error or missing in the studies; (c) duplicated literature; (e) conference abstracts without full articles and (f) reviews. The Newcastle-Ottawa Scale (NOS) scale was applied to assess the quality of the included studies, which contains three parts: selected population (4 scores), comparability of groups (2 scores) and exposure determination (3 scores). Studies with a score of 7–9 are of high quality; 4–6 are of moderate quality; 0–3 are of low quality.
The sample size and rates of nursing burnout of the included studies were imported into Stata 11.0 for calculations. The rates of the same year or month were combined using the method of literature review and meta-analysis and the forest plots were drawn. The Cochrane I-squared test was used to evaluate the heterogeneity. When I² is greater than 75%, the heterogeneity is giant; when between 50% and 90%, it is larger; when between 40%− 60%. it is moderate; when I² is less than 40%, it is low (Higgins J, 2022). The random effect model will be selected if the heterogeneity is high (I²>40%) (Page et al., 2021).
2.4. Data management
Because the meta-analysis was used to get data, not all monthly data can meet our requirements. Annual rates were combined from 1 Jan. 2010–15 Dec. 2022 to get annual nursing burnout rates and the combined annual rate averaged 12 months. They were then combined with other collected months with the same monthly data to obtain monthly nursing burnout rates. If there was no data in some months, the average value of annual data was directly selected. However, one of the drawbacks of processing data this way is that it can result in the same rate for several months.
2.5. Statistical analysis
An interrupted time series analysis using segmented ordinary least squares (OLS) regression models was used to research if the Covid019 restrictions had an impact on the rates and the trends of nursing burnout syndrome in the world. The COVID-19 restrictions were the ‘intervention’ of interest in this study. Newey-West standard errors with a lag of order one were used to adjust for autocorrelation and heteroskedasticity (A, 2015).
| Yt = β0 + β1*Tt + β2*Xt + *Pt + St |
The above formula was used in our study. Yt represents the nursing burnout syndrome monthly rate at time t; β0 is the baseline level; β1 represents the monthly nursing burnout rate slope before the COVID-19 restrictions; Tt refers to the time since the beginning of the study in months; β2 represents the changes in the rate in the month of the restrictions; Xt is a virtual (indicator) variable representing COVID-19 (the period before the restrictions is 0; otherwise it is 1); Pt is a continuous variable used to calculate the number of months. St represents the variable 0 that controls seasonality. Stata software 17.0 was used to analyze results.
3. Results
3.1. Study characteristics
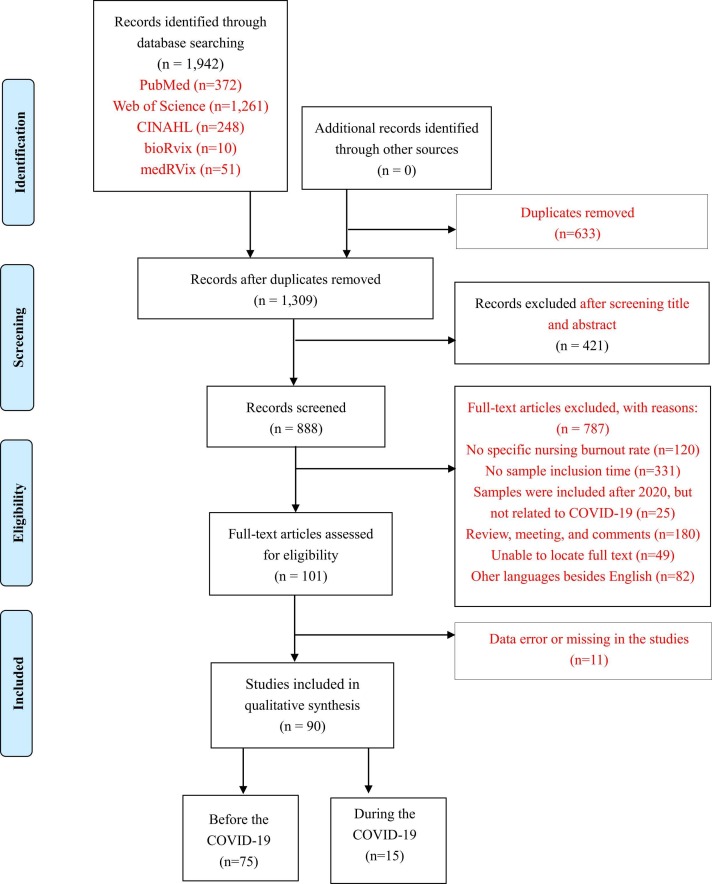
Ninety studies with 113,438 nurses from 38 countries were included from 1 Jan. 2010–15 Dec. 2022 (Supplementary material references). The specific selection process is shown in Fig. 1. In these studies, only 28 reported sample inclusion time as the month and others reported years. Almost half of the studies stated the age of the nurses. Nearly a third of the studies did not report the gender of the nurses. Half of the studies reported whether the nurses had partners. Among different specialties, 15 were from the Intensive Care Unit (ICU); 20 studies were from Multiple specialties. 76.7% of studies used MBI to measure the nursing burnout syndrome ( Table 1).
Fig. 1.
Flow diagram of the trial selection for the meta-analysis.
Table 1.
Baseline description of included studies.
| First author, year | Country | Time period | COVID (before/ during) | Age (Year) | Gender (F/M) | Partner (Yes/No) | Specialty | Burnout tool | Sample size | Number of burnout | Nursing Burnout Rate 95% CI | Quality score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mavrovounis G, 2022 | Greece | 2021 | during | NR | NR | NR | NR | MBI-HSS | 140 | 97 | 0.69 (0.61–0.77) | 7 |
| Dos Santos MA, 2022 | Brazil | Jun.-Aug. 2020 | during | 36.4 | 508/ 64 | NR | NR | MBI | 572 | 99 | 0.17 (0.14–0.20) | 6 |
| Noh EY, 2022 | South Korea | 2021 | during | 27.6 | 143/ 18 | 12/ 149 | NR | CBI | 161 | 90 | 0.56 (0.48–0.64) | 6 |
| Kamali M, 2022 | Iran | 2020 | during | NR | NR | NR | NR | MBI | 4409 | 904 | 0.12 (0.11–0.13) | 8 |
| Zakaria N, 2022 | Malaysia | Aug.-Nov. 2019 | before | 36.9 | NR | 2023/ 395 | NR | MBI | 2418 | 590 | 0.24 (0.23–0.26) | 8 |
| Thumm EB, 2022 | US | 2017 | before | 47.6 | NR | NR | Obstetrics | MBI | 2333 | 933 | 0.40 (0.38–0.42) | 8 |
| Khan Y, 2022 | Belgium | 2020 | during | 39.7 | 3823/ 729 | NR | Multiple specialties | MBI | 4552 | 3205 | 0.70 (0.69–0.71) | 7 |
| Feleke DG, 2022 | Ethiopia | 2020 | during | 20–49 | 206/ 162 | 157/ 211 | Multiple specialties | MBI-HSS | 368 | 207 | 0.56 (0.51–0.61) | 7 |
| Tan KH, 2022 | Singapore | 2019–2020 | before | NR | NR | NR | NR | MBI-HSS | 3032 | 1072 | 0.45 (0.43–0.47) | 6 |
| Membrive-Jimenez MJ, 2022 | Spain | 2021 | during | NR | 50/ 36 | 71/ 15 | Multiple specialties | MBI | 86 | 29 | 0.34 (0.24–0.44) | 7 |
| Azoulay E, 2021 | France | Oct. 30- Dec. 1, 2020 | during | NR | NR | NR | ICU | MBI | 412 | 194 | 0.47 (0.42–0.52) | 7 |
| Zhou LL, 2021 | China | Sept.-Oct, 2020 | during | 20–55 | 1133/ 0 | 604/ 529 | NR | MBI | 1133 | 682 | 0.60 (0.57–0.63) | 7 |
| Li YX, 2021 | China | Dec. 2020-May 2021 | during | NR | 2831/ 137 | 2273/ 695 | Multiple specialties | MBI | 2968 | 2095 | 0.71 (0.69–0.72) | 8 |
| Ferry AV, 2021 | UK | Jun. 2020 | during | NR | NR | NR | NR | CBI | 286 | 245 | 0.86 (0.82–0.90) | 6 |
| Butera S, 2021 | Belgium | Apr. 2020 | during | NR | NR | NR | ICU | MBI | 1149 | 770 | 0.67 (0.64–0.70) | 7 |
| Kakemam E, 2021 | Iran | Sept.-Nov. 2020 | during | NR | 746/ 258 | 688/ 316 | NR | MBI | 1004 | 316 | 0.31 (0.29–034) | 8 |
| Nishimura Y, 2021 | Japan | 2020 | during | NR | NR | NR | Multiple specialties | MBI | 21 | 5 | 0.24 (0.09–0.39) | 7 |
| Zhang XN, 2021 | China | 2020 | during | 28 | 141/ 39 | 123/ 57 | Multiple specialties | MBI-GS | 180 | 27 | 0.15 (0.10–0.20) | 7 |
| Alves MCEC, 2021 | Brazil | Mar.-Apr. 2018 | before | 39.0 | 92/ 30 | 79/ 43 | ICU | MBI | 122 | 23 | 0.19 (0.12–0.27) | 7 |
| Nicholls M, 2021 | New Zealand | 9 Mar.− 3 Apr. 2020 | before | NR | NR | NR | ED | CBI | 711 | 489 | 0.69 (0.65–0.72) | 7 |
| Moller G, 2021 | Brazil | Oct. 2018-Mar. 2019 | before | 37.3 | 53/ 9 | 33/ 29 | ICU | MBI | 62 | 3 | 0.05 (0.01–0.14) | 8 |
| Aragao NSC, 2021 | Brazil | Jul.-Nov. 2016 | before | 33.9 | 59/ 6 | 36/ 27 | ICU | MBI | 56 | 30 | 0.54 (0.40–0.67) | 8 |
| Rubin B, 2021 | Canada | 27 Nov. 2018–31 Jan. 2019 | before | NR | 206/ 31 | NR | Multiple specialties | WBI | 242 | 188 | 0.78 (0.72–0.83) | 8 |
| Magalhaes AMM, 2021 | Brazil | Aug.-Sept. 2020 | before | NR | NR | NR | Multiple specialties | MBI | 161 | 28 | 0.17 (0.12–0.24) | 7 |
| Slusarz R, 2021 | Poland | Jan.2019-Feb. 2020 | before | NR | 196/ 10 | 145/ 61 | Surgery | Self-report questionnaire | 206 | 66 | 0.32 (0.26–0.39) | 8 |
| Dyrbye LN, 2021 | US | Dec. 2016 | before | 51.6 | 894/ 82 | 713/ 263 | Multiple specialties | MBI | 976 | 350 | 0.36 (0.33–0.39) | 8 |
| Butera S, 2021 | Belgium | Jan. 2020 | before | NR | NR | NR | ICU | MBI | 283 | 145 | 0.51 (0.45–0.57) | 7 |
| Kumar A, 2021 | India | Dec. 2019 | before | NR | 104/ 21 | 42/ 83 | ICU | Questionnaire | 125 | 47 | 0.38 (0.29–0.47) | 8 |
| Simonetti M, 2021 | Chile | 2017–2018 | before | 31.6 | 1204/ 191 | NR | Multiple specialties | MBI | 1395 | 484 | 0.35 (0.33–0.38) | 8 |
| Abraham CM, 2021 | UK | 2018–2019 | before | 49.5 | 358/ 38 | 315/ 81 | Multiple specialties | MBI | 396 | 100 | 0.25 (0.21–0.29) | 8 |
| Friganovic A, 2021 | Croatia | 2017 | before | 19–62 | 544/ 76 | 316/ 304 | ICU | MBI | 620 | 72 | 0.12 (0.09–0.15) | 8 |
| De la Fuente-Solana EI, 2021 | Spain | 2019–2020 | before | NR | 73/ 22 | 59/ 36 | Pediatric care | MBI-HSS | 95 | 36 | 0.38 (0.28–0.48) | 7 |
| Paiva BSR, 2021 | Brazil | 2017–2018 | before | 26–46 | 297/ 26 | 184/ 120 | Oncology | MBI-HSS | 305 | 4 | 0.01 (0.00–0.02) | 8 |
| Zakaria MI, 2021 | Malaysia | 2020 | before | NR | NR | NR | ED | MBI | 142 | 31 | 0.22 (0.15–0.29) | 6 |
| Quijada-Martinez PJ, 2021 | Venezuela | 2019 | before | 24–70 | 36/ 4 | 17/ 23 | ICU | MBI | 40 | 9 | 0.23 (0.10–0.36) | 7 |
| Ribeiro EKDA, 2021 | Brazil | 2018 | before | NR | 73/ 10 | 42/ 41 | ICU | MBI | 83 | 12 | 0.14 (0.07–0.21) | 7 |
| De la Fuente-solana EI, 2021 | Spain | 2019 | before | 22–64 | 118/ 32 | 45/ 105 | Obstetrics | MBI | 150 | 42 | 0.28 (0.21–0.35) | 7 |
| Belay AS, 2021 | Ethiopia | 2018 | before | 21–36 | 144/ 138 | 106/ 176 | NR | MBI-HSS | 282 | 96 | 0.34 (0.28–0.40) | 7 |
| Vitale E, 2020 | Italy | Jul. -Aug. 2019 | before | 37.0 | 229/ 71 | NR | NR | MBI-HSS | 300 | 148 | 0.49 (0.44–0.55) | 8 |
| Clark RRS, 2020 | US | 2015 | before | 47.8 | 1531/ 7 | NR | Obstetrics | MBI | 1538 | 381 | 0.25 (0.23–0.27) | 8 |
| Balinbin CBV, 2020 | Philippines | Aug.-Nov. 2017 | before | 30.57 | 84/ 37 | 42/ 79 | Surgery | PROQOL | 121 | 34 | 0.28 (0.20–0.37) | 8 |
| Zeng LN,2020 | China | Oct.-Dec.2017 | before | 32.6 | 1167/ 282 | 908/ 541 | Psychiatry Department | MBI-GS | 1449 | 867 | 0.60 (0.57–0.62) | 8 |
| Tsou MT, 2020 | China | Dec.2018-Mar. 2019 | before | 35.2 | 1685/ 73 | NR | Multiple specialties | MBI-HSS | 1758 | 113 | 0.06 (0.05–0.08) | 8 |
| Rudman A, 2020 | Sweden | 2017–2018 | before | NR | 2225/ 198 | NR | NR | NR | 2423 | 299 | 0.12 (0.11–0.12) | 8 |
| Alvares MEM, 2020 | Brazil | 2011–2013 | before | 28–45 | 109/ 16 | 63/ 62 | ICU | MBI-HSS | 125 | 49 | 0.39 (0.30–0.48) | 7 |
| Jones GAL, 2020 | UK | 2018 | before | NR | 1131/ 63 | NR | ICU | MBI | 1194 | 594 | 0.50 (0.47–0.53) | 8 |
| Vevodova S, 2020 | Czech Republic | 2018 | before | 21–51 | 230/ 20 | NR | NR | MBI | 250 | 96 | 0.38 (0.32–0.44) | 8 |
| Mohammad KI, 2020 | Jordan | 2018 | before | 21–50 | NR | 238/ 83 | Obstetrics | CBI | 321 | 121 | 0.38 (0.33–0.43) | 8 |
| Harizanova S, 2020 | Bulgaria | 2014–2015 | before | 30–52 | 206/ 8 | 136/ 78 | NR | MBI | 214 | 18 | 0.08 (0.04–0.12) | 8 |
| das Merces MC, 2020 | Brazil | 2017–2018 | before | 27–47 | 989/ 136 | 519/ 606 | Multiple specialties | MBI | 1125 | 206 | 0.18 (0.16–0.20) | 8 |
| Portero de la Cruz S, 2020 | Spain | 2016 | before | 39–56 | 125/ 46 | 39/ 132 | ED | MBI | 171 | 14 | 0.08 (0.04–0.12) | 8 |
| Kapu AN, 2019 | US | Jan.-Feb. 2018 | before | 38.0 | 390/ 35 | NR | NR | MBI | 433 | 114 | 0.26 (0.22–0.31) | 7 |
| Ramirez-Baena L, 2019 | Spain | 2017 | before | 22–61 | 214/ 87 | 223/ 50 | NR | MBI | 301 | 109 | 0.36 (0.31–0.41) | 7 |
| Zhang WY, 2019 | China | Jul. 2016-Jul. 2017 | before | NR | 49,898/ 1508 | 34,015/ 16538 | NR | MBI | 51,406 | 25,703 | 0.50 (0.49–0.50) | 8 |
| Arimon-Pages E, 2019 | Spain | 2015 | before | 28–51 | 256/ 41 | NR | Oncology | ProQOL | 297 | 60 | 0.20 (0.15–0.25) | 8 |
| Berry S, 2019 | UK | 2014 | before | 26–47 | NR | NR | Internal medicine | MBI-HSS | 137 | 12 | 0.09 (0.04–0.14) | 7 |
| Nobre DFR, 2019 | Portugal | 2015 | before | NR | 15/ 17 | NR | ED | CBI | 32 | 22 | 0.69 (0.53–0.85) | 5 |
| Chico-Barba G, 2019 | Mexico | 2016–2018 | before | NR | 168/ 0 | 103/ 65 | NR | MBI | 168 | 33 | 0.20 (0.14–0.26) | 8 |
| Card EB, 2019(Card, 2019)3433323130 | US | 2014 | before | NR | 2729/ 108 | NR | Surgery | MBI | 2837 | 1474 | 0.52 (0.50–0.54) | 8 |
| Selamu M, 2019 | Ethiopia | 2014 | before | NR | NR | NR | NR | MBI-HSS | 75 | 30 | 0.40 (0.29–0.51) | 8 |
| Vasconcelos EM, 2018 | Brazil | Jul. 2014 | before | 30.82 | 81/ 10 | 34/ 57 | ICU | MBI | 91 | 13 | 0.14 (0.08–0.23) | 8 |
| Daniel A, 2018 | US | May-Jun. 2017 | before | 24–80 | 228/ 43 | NR | Multiple specialties | A 10-item survey | 371 | 73 | 0.20 (0.16–0.24) | 7 |
| See KC, 2018 | Asian multi-country | 2015–2016 | before | NR | NR | NR | ICU | MBI-HSS | 3100 | 1611 | 0.52 (0.50–0.54) | 7 |
| Sobral RC, 2018 | Brazil | 2013 | before | NR | 250/ 25 | NR | NR | MBI-HSS | 281 | 16 | 0.06 (0.03–0.09) | 8 |
| Wentzel DL, 2018 | South Africa | 2016–2017 | before | 23–65 | 81/ 2 | 39/ 44 | Oncology | ProQOL | 83 | 51 | 0.61 (0.51–0.71) | 8 |
| Sillero A, 2018 | Spain | 2014 | before | 21–65 | 119/ 11 | 75/ 55 | Surgery | MBI | 130 | 53 | 0.41 (0.33–0.49) | 6 |
| Bhagavathula A, 2018 | Ethiopia | 2016 | before | NR | NR | NR | NR | MBI-HSS | 169 | 23 | 0.14 (0.09–0.19) | 7 |
| Vermeir P, 2018 | Belgium | 2015 | before | 30–45 | NR | NR | ICU | MBI | 299 | 9 | 0.03 (0.01–0.05) | 7 |
| Fumis RRL, 2017 | Brazil | Aug.-Sept.2015 | before | NR | NR | NR | Multiple specialties | MBI | 191 | 44 | 0.23 (0.17–0.30) | 7 |
| Creedy DK, 2017 | Australia | Sept.2014 | before | NR | NR | NR | Obstetrics | MBI | 978 | 72 | 0.07 (0.06–0.09) | 7 |
| De la Fuente-Solana EI, 2017 | Spain | 2015 | before | NR | 70/ 31 | 74/ 27 | Oncology | MBI | 101 | 30 | 0.30 (0.21–0.39) | 7 |
| Merces MDC, 2016 | Brazil | 2015–2016 | before | NR | 183/ 6 | NR | Multiple specialties | MBI | 189 | 20 | 0.11 (0.07–0.15) | 8 |
| Henriksen L, 2016 | Norway | 2014 | before | 40–59 | NR | 511/ 87 | Obstetrics | CBI | 598 | 119 | 0.20 (0.17–0.23) | 7 |
| Biksegn A, 2016 | Ethiopia | 2013 | before | NR | NR | NR | NR | MBI-HSS | 237 | 120 | 0.51 (0.45–0.57) | 7 |
| Muliira RS, 2016 | Uganda | 2012–2014 | before | 27–41 | 178/ 46 | 123/ 101 | Obstetrics | ProQOL | 224 | 23 | 0.10 (0.06–0.14) | 8 |
| Abdo SAM, 2016 | Egypt | 2012–2013 | before | 20–53 | NR | NR | ED | MBI | 284 | 76 | 0.27 (0.22–0.32) | 8 |
| Jang I, 2016 | Korea | 2013 | before | NR | 285/ 0 | 95/ 190 | Oncology | ProQOL | 285 | 70 | 0.25 (0.20–0.30) | 7 |
| Maruyama A, 2016 | Japan | 2010–2011 | before | 24–48 | NR | NR | NR | MBI | 523 | 117 | 0.22 (0.18–0.26) | 8 |
| Markwell P, 2015 | US | 2013 | before | NR | 147/ 8 | NR | Multiple specialties | ProQOL | 158 | 40 | 0.25 (0.18–0.32) | 7 |
| Berger J, 2015 | US | 2014 | before | NR | 231/ 5 | NR | Pediatric care | NR | 239 | 70 | 0.29 (0.23–0.35) | 7 |
| Mangoulia P, 2015 | Greece | 2010–2011 | before | 29–45 | 122/ 52 | 98/ 76 | Internal medicine | ProQOL | 174 | 86 | 0.49 (0.42–0.56) | 6 |
| Hegney D, 2015 | Australia | 2013 | before | NR | 1487/ 121 | NR | NR | ProQOL | 1608 | 405 | 0.25 (0.23–0.27) | 7 |
| das Silva JLL, 2015 | Brazil | 2010–2011 | before | 28–41 | 65/ 65 | NR | Multiple specialties | MBI | 130 | 72 | 0.55 (0.46–0.64) | 7 |
| Ferreira Ndo N, 2015 | Brazil | 2011 | before | 28–48 | 452/ 82 | 300/ 234 | NR | MBI-HSS | 534 | 32 | 0.06 (0.04–0.08) | 7 |
| Dolan ED, 2015 | US | 2012 | before | NR | NR | NR | Multiple specialties | MBI | 1380 | 549 | 0.40 (0.37–0.43) | 8 |
| Ariapooran S, 2014 | Iran | 2013 | before | 25–39 | 67/ 106 | 143/ 30 | NR | ProQOL | 173 | 26 | 0.15 (0.10–0.20) | 7 |
| Ribeiro VF, 2014 | Brazil | 2012 | before | NR | 16/ 3 | NR | Surgery | MBI | 188 | 19 | 0.10 (0.06–0.14) | 6 |
| Yatasa YN, 2014 | Ethiopia | 2013 | before | NR | 116/ 59 | 58/ 117 | NR | MBI-HSS | 175 | 33 | 0.19 (0.13–0.25) | 8 |
| Raftopoulos V, 2012 | Cyprus | 2010–2011 | before | NR | 1189/ 282 | 1127/ 337 | Multiple specialties | MBI | 1482 | 190 | 0.13 (0.11–0.15) | 7 |
| Mohammadpoorasl A, 2012 | Iran | 2010 | before | 27–42 | 613/ 99 | 505/ 207 | NR | MBI | 712 | 156 | 0.22 (0.19–0.25) | 6 |
ProQOL: Professional Quality of Life; ICU: Intensive Care Units; ED: Emergency Department; MBI: Maslach Burnout Inventory; MBI-HSS: Maslach Burnout Inventory-Human Services Survey; WBI: MBI-GS: Maslach Burnout Inventory-General Survey; Well- Being Index; SBI: Spanish Burnout Inventory; CBI: Copenhagen Burnout Inventory; NR: Not Reported
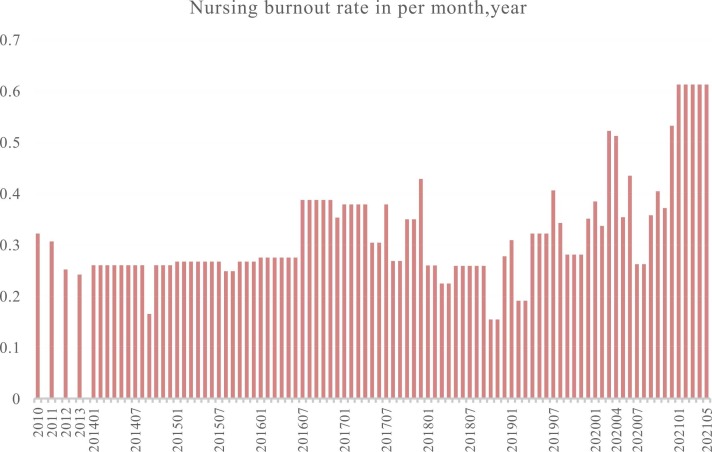
3.2. The burnout rate based on each year and each month
Fig. 2 A shows the summaries of nursing burnout rates from 2010 to May 2021. 2014 was taken as an example to describe our data acquisition process (Supplementary materials Fig. 1E& F). The burnout rate of the samples in 2014 was combined and the result was 0.26 (95%CI: 0.10, 0.42; I²= 99.2%; z = 3.24; p = 0.001). Then we averaged the burnout rate of 2014 over 12 months and combined with the rates of other months in 2014. The results showed that the nursing burnout rate was 0.20 (95%CI: 0.09, 0.32; I²=87.2%; z = 3.39; p = 0.001) in July 2014 and 0.16 (95%CI: −0.02, 0.35; I²= 98.4%; z = 1.72; p = 0.085) in September 2014. Supplementary materials Fig. 1E& F indicated the process of calculating the monthly rates. In 2014, the nursing burnout syndrome rates in other months except July and September were all 0.26. Monthly nursing burnout rates from 2010 to 2013 were not found. The nursing burnout rate was 0.31 (95%CI: 0.21, 0.42; I²= 97.8%; z = 5.67; p < 0.001) in 2010; 0.30 (95%CI: 0.19, 0.40; I²= 98.3%; z = 5.59; p < 0.001) in 2011; 0.25 (95%CI: 0.10, 0.40; I²= 98.3%; z = 3.36; p < 0.001) in 2012; 0.24 (95%CI: 0.17, 0.31; I²= 96.7%; z = 6.28; p < 0.001) in 2013. The process of obtaining nursing burnout rates in other years was also shown in Supplementary material Fig. 1.
Fig. 2.
Summary of nursing burnout rates in each month from 2010 to May 2021.
3.3. Interrupted time-series analysis
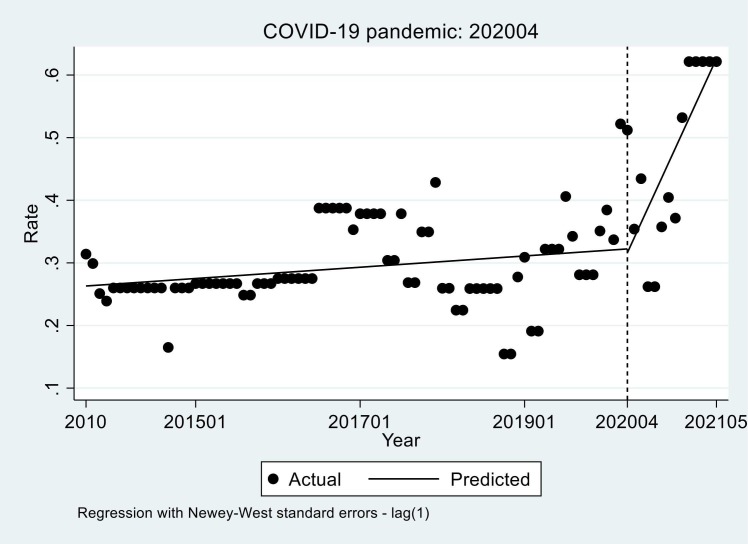
The global nursing rate is 0.52 (95%CI: 0.19, 0.85) at its highest in Mar. 2020 and 0.16 (95%CI: −0.05, 0.36) at its lowest in Oct. 2018. During the restrictions, the highest nursing burnout rate is 0.62 (95%CI: 0.47, 0.81) from January to May 2021. Fig. 3 showed the long-term trend of the global nursing burnout rates before the COVID-19 restrictions (January 2010 to March 2020) and later (April 2020 to May 2021). The black dot indicated the actual rate of nursing burnout each month and the solid line indicated the trend of nursing burnout before and after the restictions.
Fig. 3.
Trends in monthly nursing burnout syndrome rate around the world (pre-COVID-19 pandemic trend: 0.0007497, 95%CI: 0.0000316, 0.0014677, t = 2.07, P = 0.041; COVID-19 pandemic change: 0.0238539, 95%CI: 0.0087134, 0.0389943, P < 0.05).
The interrupted time series regression analyses found an increasing trend of nursing burnout rate from baseline ( Table 2). Statistically significant changes were found in the nursing burnout rates. Before the epidemic (April 2020), the nursing burnout rate rose with 0.0007497 (95% CI: 0.0000316, 0.0014677, t = 2.07, P = 0.041) every month; in the month of the restrictions (April 2020), the nursing burnout rate decreased by 0.0061033 (95%CI: −1401596, 0.1279529, t = −0.09, P = 0.928); compared with the rising trend of 0.0007497 before the COVID-19 restrictions, the rising trend of nursing burnout rate increased by 0.0231042 (95CI%:0.0086818, 0.0375266, t = 3.18, P = 0.002). The rising trend of nursing burnout rate after the COVID-19 restrictions is 0.0007497 + 0.0231042 = 0.0238539 every month (Table 2).
Table 2.
The statistical results of interrupted time series regression analyses of the impact of the COVID-19 pandemic on the nursing burnout rate in total region subgroups.
| Coefficient, 95%CI | ||||
|---|---|---|---|---|
| Pre-COVID-19 pandemic trend (β1) | Rate change (β2) | COVID-19 pandemic trend (β3) | COVID-19 pandemic change (β1 + β3) | |
| Total (n = 90) | 0.0007497 * (0.0000316, 0.0014677) | -0.0061033(−0.1401596, 0.1279529) | 0.0231042 * *(0.0086818, 0.0375266) | 0.0238539 * (0.0087134, 0.0389943) |
| Region subgroup | ||||
| Occident (n = 56) | 0.000603(−0.0005504, 0.0017563) | 0.2362564 * *(0.187537, 0.2849757) | -0.0021181(−0.0061508, 0.0019145) | -0.001578(−0.0067012, 0.0036708) |
| Non-Occident (n = 34) | 0.0017584 * (0.0003755, 0.0031413) | -0.1694088 * *(−0.243112, −0.0957056) | 0.0304174 * *(0.0230258, 0.037809) | 0.0321758 * *(0.0234013, 0.0409503) |
“Pre-COVID-19 pandemic trend” indicates the pre-pandemic slope of nursing burnout rate and is β1.
“Rate change” indicates the changes in nursing burnout rate in the month of the pandemic outbreak and is β2.
“COVID-19 pandemic trend” indicates the difference of the slope of nursing burnout rate after the onset of the pandemic and is β3.
“COVID-19 pandemic change” indicates the slope in nursing burnout rate after the onset of the pandemic and is the sum of β1 and β3.
*P < 0.05, * *P < 0.001
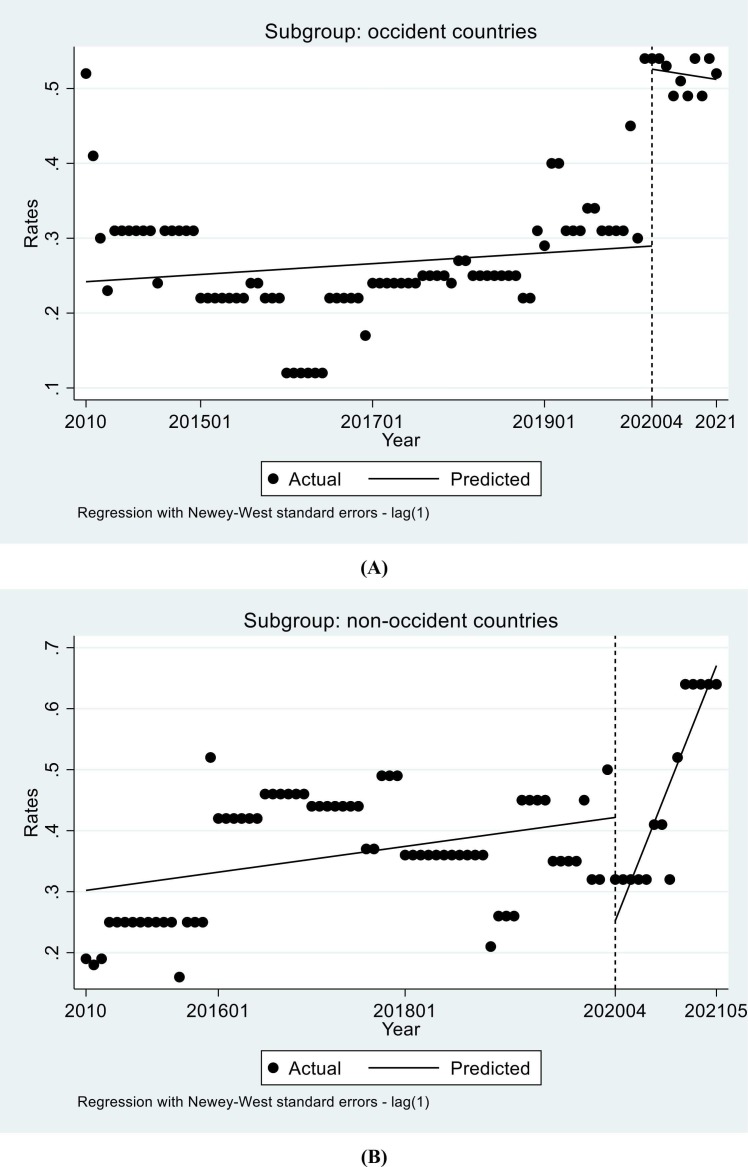
3.4. Subgroup analysis by regions
In occident countries, no significant difference was found in the trend changes before and during the epidemic (Table 2). The nursing burnout rate rose with 0.000603 (95% CI: −0.0005504, 0.0017563, t = 1.04, P = 0.302) every month before the restrictions; in the month of the restrictions (April 2020), the nursing burnout rate increased by 0.2362564 (95%CI: 0.187537, 0.2849757, t = 9.64, P < 0.0001); compared with the rising trend of 0.000603 before the restrictions, the trend of nursing burnout rate decreased by 0.0021181 (95%CI: −0.0061508, 0.0019145, t = −1.04, P = 0.299). The trend of nursing burnout rate after the COVID-19 restrictions is 0.000603–0.0021181 = −0.001578 every month ( Fig. 4A).
Fig. 4.
Trends in monthly nursing burnout syndrome rate in (A) occident countries (Pre-COVID-19 pandemic trend: 0.000603, 95%CI: −0.0005504, 0.0017563, t = 1.04, P = 0.302; COVID-19 pandemic change: −0.001578, 95%CI: −0.0056004, 0.0036708, P = 0.601); (B) non-occident countries (Pre-COVID-19 pandemic trend: 0.0017584, 95%CI: 0.0003755, 0.0031413, t = 2.53, P = 0.013; COVID-19 pandemic change: 0.0321758, 95%CI: 0.0234013, 0.0409503, P < 0.001).
In non-occident countries, there was a statistically significant difference (Table 2). The nursing burnout rate rose with 0.0017584 (95% CI: 0.0003755–0.0031413, t = 2.53, P = 0.013) every month before the restrictions; in the month of the restrictions (April 2020), the nursing burnout rate decreased by 0.1694088 (95%CI: −0.243112,−0.0957056, t = −4.58, P < 0.001); compared with the rising trend of 0.0017584 before the COVID-19 restrictions, the trend of nursing burnout rate increased by 0.0.0304174 (95%CI: 0.0230258, 0.037809, t = 8.19, P < 0.001). The trend of nursing burnout rate after the COVID-19 restrictions is 0.0017584 + 0.0304174 = 0.0321758 every month (Fig. 4B).
4. Discussion
This interrupted time series analysis indicated that the global nursing burnout rate showed a slow upward trend, increasing at 0.0007497 (95% CI: 0.0000316–0.0014677, P = 0.041) per month before the restrictions. After the restrictions, the global nursing burnout rates increased significantly. It grew at a rate of 0.0238539 per month during the restrictions. The restrictions have influenced nursing burnout rates, leading to a rapid increase in nursing burnout rates.
A comparative analysis of nursing burnout before and during the epidemic showed that nurses had a high burnout rate during routine work and that the rate was higher during the COVID-19 restrictions (D. Sullivan et al., 2022), which is consistent with our findings. But the quantity in our study is more and the sample is more sufficient. In addition, another advantage of our study is that the interrupted time series calculated the growth rate of nursing burnout before and after the outbreak of the restrictions, which more intuitively showed the influence of the epidemic on nursing burnout rates.
Before the outbreak of COVID-19 restrictions, nurses were reported high burnout due to the environment of high pressure, irregular working hours, shifts and overnight work (Galanis et al., 2021). After the restrictions, nurses faced even greater challenges. It is well known that nurses play an extraordinary role in combating the COVID-19 restrictions among all healthcare professionals. They put their lives at a risk on the front lines, such as infection control units, emergency departments and intensive care units, etc. (Catton, 2020) COVID-19 has placed enormous stress on nurses and exacerbated pre-existing burnout mechanisms (Pappa et al., 2020). The most direct reason is that they felt anxious, such as lack of knowledge about the infection of COVID-19 (Sun et al., 2020), fear that they may be infected with the virus and exhaustion caused by overwork (Tan et al., 2020). At the same time, concerns about the health of their family are also a factor (Sun et al., 2020). Too many psychological problems easily lead to emotional exhaustion. To prevent infecting their relatives or family members, nurses were isolated in different places most of the time during the restrictions, resulting in a lack of social and emotional support for these nurses, which negatively affected their psychosocial status (Mo et al., 2020). In addition, many nurses perceived little support or management response to increased risk and stress (Foli et al., 2021). An online survey of factors related to nursing burnout during the restrictions found that staffing was negatively associated with the occurrence of burnout, with nurses who were adequately paid during the restrictions experiencing less burnout (D. Sullivan et al., 2022). Due to the high acuity and mortality of COVID-19 patients, nurses working in intensive care may experience feelings of powerlessness, low control, insufficient support, or resources (personal protective equipment, rescue equipment, etc.), high job demands. All these factors increased the risk of moral distress and burnout among nurses (Guttormson et al., 2022).
During the restrictions, nursing staff experienced chronic staffing shortages, high turnover and burnout in long-term care environment (Hung, 2021), with significant implications for the nurses themselves and for nursing work as a whole. Nursing burnout should be paid more attention to. Nurses play an essential role in achieving national and global goals related to health priorities and nursing is an indispensable profession in the world (WHO, 2020). According to our study, the nursing burnout rate was higher and the restrictions increased the nursing burnout rates. At present, the global epidemic has come to an end. To prevent the negative impact of similar public health events on nursing burnout once again, relevant management departments should take corresponding measures to reduce nursing burnout and reduce nurse turnover rates and ensure the high quality of nursing work. Studies have shown that a variety of ways to support nurses and reduce burnout, such as mindfulness training (Luberto et al., 2020), access to psychological and psychosocial support (Kakemam et al., 2021), prioritizing rest and breaks (Sarboozi Hoseinabadi et al., 2020), meditation apps (Janeway, 2020) and self-care techniques (Kakemam et al., 2021). However, theses methods still need to be monitored for their effectives and more policies and measures to protect nurses’ health need to be developed and implemented, such as considering fostering a culture of respect, appreciation, adequate allocation of resources and appropriate financial compensation for nurses during the restrictions. Adjusting nurses’ working hours and providing better psychological support might also good ideas. At the same time, preventive strategies need to be developed to prevent the impact of similar public health events on nursing burnout in the future.
There were some limitations in our study. Firstly, because the data were obtained through the method of meta-analysis, it was inevitable that some data would be missing. According to the data management method in our paper, there were the same data for several months, which was an avoidable limitation. Secondly, due to the limited data, the trend change of nursing burnout rates in various countries or departments cannot be calculated. Thirdly, only papers published in English were included in the study. Therefore, more high-quality research on nursing burnout should be conducted.
In conclusion, the results indicated a slowly rising trend in the nursing burnout rates before the COVID-19 restrictions and the rising trend significantly increased after the restrictions. The COVID-19 restrictions influenced nursing burnout. The study may draw the nursing management departments more attention and provide some basis for changing the phenomenon of nursing burnout.
Funding
None.
CRediT authorship contribution statement
Meng-Wei Ge: Writing – original draft, Data curation, Formal analysis, Writing – review & editing. Fei-Hong Hu: Writing – original draft, Formal analysis. Yi-Jie Jia: Data curation, Software. Wen Tang: Data curation, Software. Wan-Qing Zhang: Investigation. Dan-Yan Zhao: Formal analysis. Wang-Qin Shen: Formal analysis. Hong-Lin Chen: Writing – review & editing, Supervision, Data curation.
Conflict of Interest
There was no conflict of interest in our paper.
Acknowledgments
None.
Supplementary material
Supplementary material associated with this article can be found, in the online version at doi:
Footnotes
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.nepr.2023.103643.
Appendix A. Supplementary material
Supplementary material
.
References
- A L. Conducting interrupted time-series analysis for singleand multiple-group comparisons. Stata J. 2015;15(2):480–500. [Google Scholar]
- Badahdah A., Khamis F., Al Mahyijari N., Al Balushi M., Al Hatmi H., Al Salmi I., Al Noomani J. The mental health of health care workers in Oman during the COVID-19 pandemic. Int J. Soc. Psychiatry. 2021;67(1):90–95. doi: 10.1177/0020764020939596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burki T. Burnout among cancer professionals during COVID-19. Lancet Oncol. 2020;21(11):1402. doi: 10.1016/s1470-2045. (20)30584-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Busch I., Moretti F., Mazzi M., Wu A., Rimondini M. What we have learned from two decades of epidemics and pandemics: a systematic review and meta-analysis of the psychological burden of frontline healthcare workers. Psychother. Psychosom. 2021;90(3):178–190. doi: 10.1159/000513733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catton H. Global challenges in health and health care for nurses and midwives everywhere. Int Nurs. Rev. 2020;67(1):4–6. doi: 10.1111/inr.12578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chirico F., Nucera G., Magnavita N. Protecting the mental health of healthcare workers during the COVID-19 emergency. BJPsych Int. 2020:1–2. [Google Scholar]
- Foli K.J., Forster A., Cheng C., Zhang L., Chiu Y.C. Voices from the COVID-19 frontline: nurses' trauma and coping. J. Adv. Nurs. 2021;77(9):3853–3866. doi: 10.1111/jan.14988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frenk J C.L., Chandran L., Groff E.O.H., King R., Meleis A., Fineberg H.V. Challenges and opportunities for educating health professionals after the COVID-19 pandemic. Lancet. 2022;400(10362):1539–1556. doi: 10.1016/S0140-6736(22)02092-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galanis P., Vraka I., Fragkou D., Bilali A., Kaitelidou D. Nurses' burnout and associated risk factors during the COVID-19 pandemic: a systematic review and meta-analysis. J. Adv. Nurs. 2021;77(8):3286–3302. doi: 10.1111/jan.14839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gualano M., Sinigaglia T., Lo Moro G., Rousset S., Cremona A., Bert F., Siliquini R. The burden of burnout among healthcare professionals of intensive care units and emergency departments during the COVID-19 pandemic: a systematic review. Int. J. Environ. Res. Public Health. 2021;18(15) doi: 10.3390/ijerph18158172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guttormson J.L., Calkins K., McAndrew N., Fitzgerald J., Losurdo H., Loonsfoot D. Critical care nurse burnout, moral distress and mental health during the COVID-19 pandemic: a United States survey. Heart Lung. 2022;55:127–133. doi: 10.1016/j.hrtlng.2022.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harry E., Carlasare L., Sinsky C., Brown R., Goelz E., Nankivil N., Linzer M. Childcare stress, burnout and intent to reduce hours or leave the job during the COVID-19 pandemic among US health care workers. JAMA Netw. Open. 2022;5(7) doi: 10.1001/jamanetworkopen.2022.21776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins J, G.S. ( 2022). Cochrane Handbook for Systematic Reviews for Interventions, Version 5.1.0. 2011. http://handbook-5–1.cochrane.org/.
- Hung L. Caring for residents with dementia during a COVID-19 outbreak in a long-term care home. Alzheimer's Dement.: J. Alzheimer'S. Assoc. 2021 doi: 10.1002/alz.057324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janeway D. The role of psychiatry in treating burnout among nurses during the Covid-19 pandemic. J. Radio. Nurs. 2020;39(3):176–178. doi: 10.1016/j.jradnu.2020.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kakemam E., Chegini Z., Rouhi A., Ahmadi F., Majidi S. Burnout and its relationship to self-reported quality of patient care and adverse events during COVID-19: a cross-sectional online survey among nurses. J. Nurs. Manag. 2021;29(7):1974–1982. doi: 10.1111/jonm.13359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai J., Ma S., Wang Y., Cai Z., Hu J., Wei N., Hu S. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw. Open. 2020;3(3) doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavoie-Tremblay M., Gélinas C., Aubé T., Tchouaket E., Tremblay D., Gagnon M.P., Côté J. Influence of caring for COVID-19 patients on nurse's turnover, work satisfaction and quality of care. J. Nurs. Manag. 2022;30(1):33–43. doi: 10.1111/jonm.13462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luberto C.M., Goodman J.H., Halvorson B., Wang A., Haramati A. Stress and coping among health professions students during COVID-19: a perspective on the benefits of mindfulness. Glob. Adv. Health Med. 2020;9 doi: 10.1177/2164956120977827. 2164956120977827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maslach, C., Jackson S., Leiter M. (2018). Maslach Burnout Inventory, 4th ed. Mind Garden: Menlo Park, CA, USA.
- Matsuo T K.D., Taki F., Sakamoto F., Uehara Y., Mori N., Fukui T. Prevalence of health care worker burnout during the coronavirus disease 2019 (COVID-19) pandemic in Japan. JAMA Netw. Open. 2020;3(8) doi: 10.1001/jamanetworkopen.2020.17271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mo Y., Deng L., Zhang L., Lang Q., Liao C., Wang N., Huang H. Work stress among Chinese nurses to support Wuhan in fighting against COVID-19 epidemic. J. Nurs. Manag. 2020;28(5):1002–1009. doi: 10.1111/jonm.13014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Page M.J., Moher D., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., McKenzie J.E. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372:n160. doi: 10.1136/bmj.n160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pappa S., Ntella V., Giannakas T., Giannakoulis V.G., Papoutsi E., Katsaounou P. Prevalence of depression, anxiety and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav. Immun. 2020;88:901–907. doi: 10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarboozi Hoseinabadi T., Kakhki S., Teimori G., Nayyeri S. Burnout and its influencing factors between frontline nurses and nurses from other wards during the outbreak of Coronavirus Disease -COVID-19- in Iran. Invest Educ. Enferm. 2020;38(2) doi: 10.17533/udea.iee.v38n2e03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah M.K., Gandrakota N., Cimiotti J.P., Ghose N., Moore M., Ali M.K. Prevalence of and factors associated with nurse burnout in the US. JAMA Netw. Open. 2021;4(2) doi: 10.1001/jamanetworkopen.2020.36469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan D., Sullivan V., Weatherspoon D., Frazer C. Comparison of nurse burnout, before and during the COVID-19 pandemic. Nurs. Clin. North Am. 2022;57(1):79–99. doi: 10.1016/j.cnur.2021.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan V., Hughes V., Wilson D.R. Nursing burnout and its impact on health. Nurs. Clin. North Am. 2022;57(1):153–169. doi: 10.1016/j.cnur.2021.11.011. [DOI] [PubMed] [Google Scholar]
- Sun N., Wei L., Shi S., Jiao D., Song R., Ma L., Wang H. A qualitative study on the psychological experience of caregivers of COVID-19 patients. Am. J. Infect. Control, 48 (6), 592-598. 2020 doi: 10.1016/j.ajic.2020.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan R., Yu T., Luo K., Teng F., Liu Y., Luo J., Hu D. Experiences of clinical first-line nurses treating patients with COVID-19: A qualitative study. J. Nurs. Manag. 2020;28(6):1381–1390. doi: 10.1111/jonm.13095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . World Health Organization; Geneva: 2019. Burn-out an “Occupational phenomenon”: International Classification of Diseases. [Google Scholar]
- WHO. (2020). STATE OF THE WORLD’S NURSING. World Health Organization.
- Woo T., Ho R., Tang A., Tam W. Global prevalence of burnout symptoms among nurses: a systematic review and meta-analysis. J. Psychiatr. Res. 2020;123:9–20. doi: 10.1016/j.jpsychires.2019.12.015. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material