Abstract
To determine the effects of exercise on VLU healing and exercise adherence, and to provide evidence for clinical practice and scientific investigation. PubMed, Embase and Scopus were searched from inception to 31st March, 2022. Pooled relative risks (RRs), standardised mean differences (SMDs), adherence rate with respective 95% confidence intervals (CIs) were calculated. Quality assessment of included studies were performed using the Cochrane Collaboration risk of bias evaluation. Heterogeneity between enrolled studies was evaluated. We identified eight randomised control studies (RCTs) that met the inclusion criteria. The pooled RR for healing rate was 1.38 (95% CI: 1.14 to 1.66; P = 0.0008) with no significant heterogeneity between component studies (I 2 = 0%, P = 0.96). SMD for differences of total range of ankle joint motion (ROAM) at the end and at the initiation of follow‐up in the intervention and control groups was 0.87 (95% CI: 0.22, 1.52; P = 0.0091), no significant heterogeneity was detected (I 2 = 59%, P = 0.0622). Pooled adherence rate was 64% (95% CI: 53%, 75%) with no significant heterogeneity. Exercise manifested positive effects on VLU healing, range of ankle mobility compared with the control group. Patients' adherence to the exercise regimens was favourable.
Keywords: adherence rate, exercise, meta‐analysis, therapy, venous leg ulcer
In this meta‐analysis, exercise manifested positive effects on VLU healing, range of ankle mobility compared with the control group. Patients' adherence to the exercise regimens was favourable. Due to limited information extracted in included studies, further additional systematic review and meta‐analyses are needed to provide more reliable and powerful evidence.
1. INTRODUCTION
Venous leg ulcer (VLU) is the most common type of leg ulcers, accounting for 80% to 90% of lower extremity ulcers. 1 VLU impacts a great number of patients around the world and may impose a significant socio‐economic burden on the health system and pose significantly psychological and physical affections on the affected individuals. 2 Moreover, it is estimated that the VLU cost burden would be on a dramatical rise owing to the aging of population, increased prevalence of diabetes mellitus, and other associated conditions including venous circulation disfunction, elevated body mass index, family history of chronic venous insufficiency, history of pulmonary embolism or venous thrombosis, local osseous or joint diseases. 3 , 4 , 5 , 6 , 7 , 8 , 9 The main cause of VLU is that the calf muscle pump cannot properly return blood from the legs to the heart due to venous reflux and obstruction. 10
Venous leg ulcers are usually irregular in shape with well‐defined borders. 11 Heavy limbs, itching, pain and edema are commonly presented symptoms of VLU, which are exacerbated during the day and improved with elevation of affected limbs. 6 , 10 , 12 Diagnostic strategy comprised of ultrasonography, arterial pulse examination and measurement of ankle‐brachial index is recommended for individuals suspected of VLU. 13 , 14 The primary goals for treating patients with VLU include alleviation of pain and edema, ulcer healing and prophylaxis of ulcer recurrence. 2 , 10 , 15 Elevation of lower extremities is regarded as the simplest approach to reverse the effects of venous insufficiency, Abu‐Own et al. recommended that elevation of the legs above the heart level for 3 to 4 times daily, 30 minutes per time, along with leg elevation throughout the night could improve venous circulation. 16 Nonetheless, a majority of patients cannot tolerate the frequency of leg elevation. Compression remains the mainstay of treatment for patients with VLU. 17 , 18 Multilayer elastic bandages are considered as the gold standard with the most powerful evidence in favour of increased healing rates and decreased recurrence as compared with no compression. 19 , 20 Of note, compression should be employed with caution in patients who suffered from congestive heart failure and arterial insufficiency. 21 Exercise is another approach for the therapy of VLU. During exercise, the calf muscles contraction propels the compression of the intramuscular and deep veins, which increase the venous pressure and promote the blood in the deep vein back to the heart. 22 In addition, increased number of studies investigated the role of exercises on the treatment of VLU by improving calf muscle function and ankle joint range of motion in patients with VLU. 23 , 24 , 25 The results are conflicting and varied based on the characteristics of study design and conduction. The aim of this meta‐analysis was to determine the effects of exercise on the clinical outcome measurement of VLU healing and adherence, and to provide evidence for clinical practice and scientific investigation.
2. MATERIALS AND METHODS
2.1. Statements
This meta‐analysis was conducted in accordance with the Preferred Reporting Items for Systematic Review and Meta‐Analyses (PRISMA) guidelines. 26 , 27 , 28 Dataset in this study was generated from published articles, thus the informed consent was not required.
2.2. Literature search
Potential eligible studies were identified through comprehensive search of several electronic databases, including the PubMed, Embase and Scopus databases. Search terms included a strategic combination of “leg ulcer” and “exercise.” The term “leg ulcer” was used instead of “venous leg ulcer” to retrieve as many eligible studies as we could. All papers published from inception to 31st March, 2022 with the English language were included. Based on the results of the initial literature search. The titles and abstracts of each record searched were screened to exclude duplicates and any obviously irrelevant researches. Afterwards, full texts of the remaining articles were reviewed to determine for final inclusion. The bibliographies of the identified studies or review articles were manually searched for further eligible records. The article search and screening were performed by two authors, any disagreement was addressed through discussion.
2.3. Study selection, data extraction and quality assessment
The inclusive selection criteria were as follows: (1) Randomised control trials or cohort studies used exercise regardless of any form for the treatment of diagnosed venous leg ulcers; (2) Outcomes including healing rates, total range of ankle joint motion and adherence rates were reported in the enrolled studies. Conference abstracts, reviews, case reports, animal studies were excluded. Name of first author, year of publication, country, study design, number of participants, age of participants (in year), details on intervention, details on control, follow‐up duration (in week) and outcomes aforementioned were extracted into a predefined form. Two independent reviewers conducted the entire process of study selection and data extraction, any discrepancy was solved through discussion by the two authors. Two authors then independently assessed the quality of included studies using the Cochrane Collaboration risk of bias evaluation, 29 with discordance resolved by discussion. As the blind of intervention exercises were impossible to the patients, performance bias for blinding was not evaluated.
2.4. Statistical analysis
Data synthesis for each outcome was performed using R software (Version 4.0.3, Comprehensive R Archive Network) using the random effects model. 30 Standardised mean differences (SMDs) (for continuous variables in intervention and control groups), relative risks (RRs) (for dichotomous outcomes in intervention and control groups), pooled adherence rate and their respective 95% confidence intervals (CIs) were calculated. Heterogeneity between component studies was tested by the Q test and I 2 statistic. I 2 values ≥25%, ≥ 50% and ≥75% were regarded as low, moderate and high degree of heterogeneity, respectively. 31 Linear regression test of funnel plot asymmetry was utilised to determine publication bias. A P value <0.05 was considered as statistical significance.
3. RESULTS
3.1. Baseline characteristics of included studies
A total of 523 records were initially retrieved. After excluding 135 duplicate studies and ineligible studies (77 reviews, 18 case reports, 3 animal studies, 18 conference abstracts, 172 irrelevant records), a total of 100 studies were evaluated for eligibility in the next step of screening. After full‐text review of 28 articles, we finally identified eight randomised control studies that met the inclusion criteria, including a total of 270 patients with diagnosed VLU. 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 Details on literature search is depicted in Figure 1. The year of publication for included studies ranged from 2010 to 2022. Mean (median) age of participants in each study was more than 60 years old. More information on the baseline characteristics of the included studies is shown in Table 1. All studies were considered to have low‐risk selection bias in sequence generation. Three trials were judged to be at high risk of bias on blinding of outcome assessment due to the open‐label design of these trials. Overall results of quality assessment for the enrolled records are shown in Figure 2.
FIGURE 1.
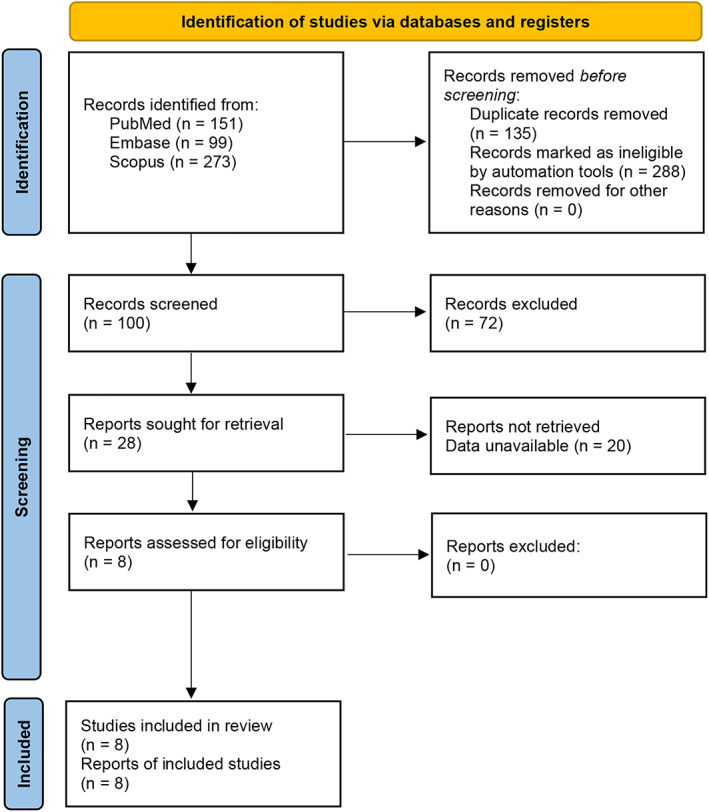
Flow chart of literature search
TABLE 1.
Baseline characteristics of included studies
| Name of First Author | Year of Publication | Country | Study Design | No. of Participants | Age of Participants (years) | Intervention | Control | Follow‐up duration (weeks) |
|---|---|---|---|---|---|---|---|---|
| Szewczyk | 2010 | Poland | Randomised control study | 32 | 73.3 ± 9.7 | The supervised exercises were performed 3 times a day, in series of 15 repetitions; walking 3 km daily; exercising on training bikes. | Performing exercises by themselves | 9 |
| Meagher | 2011 | Ireland | Randomised control study | 35 | 71 (32–91) | Taking 10 000 steps per day. Participants were fully educated on the use of the pedometer and regular contact was maintained to address any queries, as necessary. | The control group were not asked to alter their walking activity at any point in the study, and no specific advice regarding exercise was given. | 12 |
| O'Brien | 2013 | Australia | Randomised control study | 11 | 64.9 ± 13 | An individualised exercise programme | Usual care | 12 |
| O'Brien | 2017 | Australia | Randomised control study | 59 | 71.5 ± 14.6 | A home‐based progressive resistance exercise programme | Usual care | 12 |
| Klonizakis | 2018a | United Kingdom | Randomised control study | 38 | 66.9 ± 13.9 | Usual care plus a supervised exercise programme | Usual care | 12 |
| Klonizakis | 2018b | United Kingdom | Randomised control study | 39 | 63.5 ± 12.8 | Three sessions of supervised exercise each week for 12 weeks | Usual care | 12 |
| Jonker | 2020 | United Kingdom | Randomised control study | 32 | 73 ± 4 | StepIt exercise programme | Standard care | 12 |
| Kulprachakarn | 2022 | Thailand | Randomised control study | 24 | NR | Conventional treatment plus tailored exercise training | Conventional treatment | 12 |
Abbreviation: NR, not reported.
FIGURE 2.
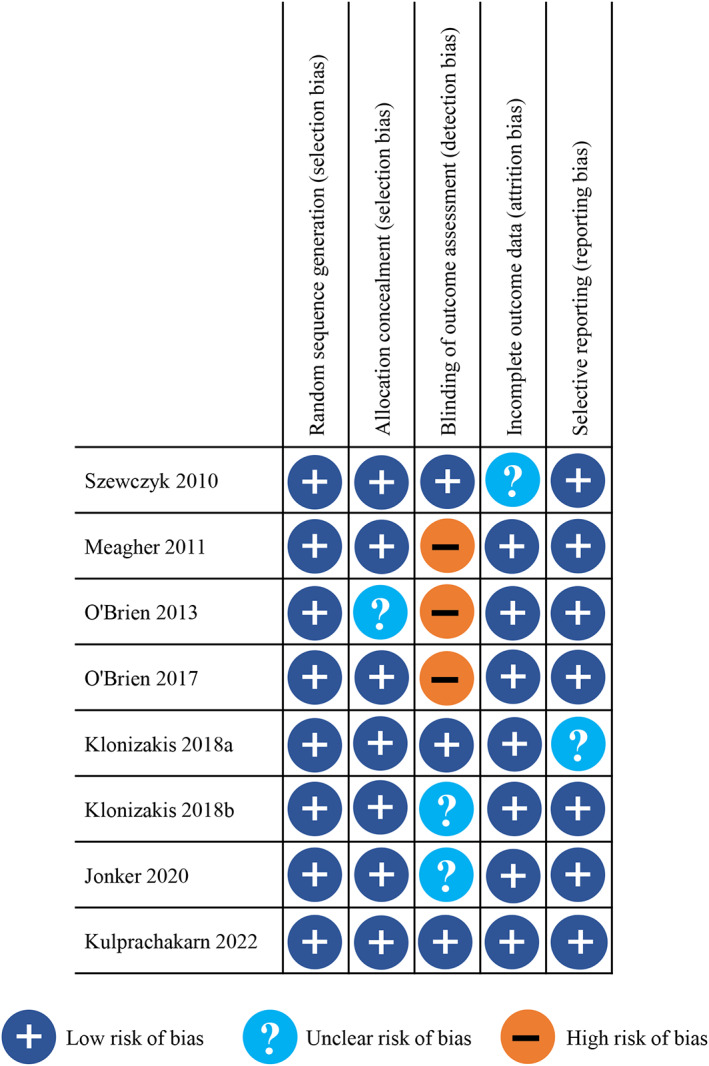
Risk of bias summary for each included study
3.2. Effects on ulcer healing
Seven studies reported the outcomes on ulcer healing at 12 weeks except that one study revealed proportion of patients healed at 9 weeks. The pooled RR for healing rate of the seven included studies was 1.38 (95% CI: 1.14 to 1.66; P = 0.0008), no significant heterogeneity between component studies was detected (I 2 = 0%, P = 0.96) (Figure 3). The overall healing rate at 12 weeks was 1.39 (95% CI: 1.15 to 1.68; P = 0.0007), statistical heterogeneity was considered as not significant (I 2 = 0%, P = 0.96).
FIGURE 3.
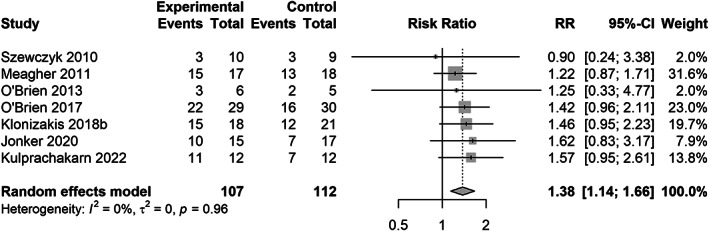
Forest plot of healing rates in included studies
3.3. Effects on total range of ankle joint motion
Four included studies measured the differences of total range of ankle joint motion (ROAM) at the end (12 weeks in 3 studies, 9 weeks in 1 study) and at the initiation of follow‐up in the intervention arm and control arm. Standardised mean difference of differences in the intervention group and control group was 0.87 (95% CI: 0.22, 1.52; P = 0.0091), no significant heterogeneity between included studies was detected (I 2 = 59%, P = 0.0622) (Figure 4). For the studies with a 12‐week follow‐up, the estimated overall SMD was 0.74 (95% CI: −0.09, 1.58; P = 0.0808) with no significant heterogeneity (I 2 = 63%, P = 0.0690).
FIGURE 4.
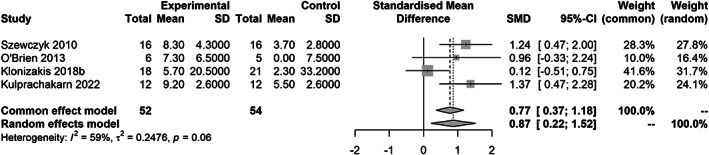
Forest plot of total range of ankle joint motion in included studies
3.4. Adherence on exercise program
Four records assessed the adherence to exercise programs in the intervention arms. Pooled adherence rate was 64% (95% CI: 53%, 75%). Non‐statistical significance for heterogeneity was justified (I 2 = 0%, P = 0.54) (Figure 5).
FIGURE 5.
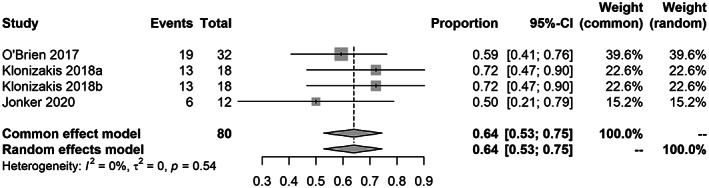
Forest plot of adherence rates in included studies
3.5. Publication bias
The Egger's tests yielded p values of 0.8754, 0.4218 and 0.9810 for the meta‐analysis of healing rates, differences of ROAM and adherence rates, respectively (Figures [Link], [Link]).
4. DISCUSSION
The recovery of VLU is one of the comprehensive clinical issues that requires intervention from specialist and multidisciplinary wound care providers. 40 Exercise interventions could improve the outcomes of VLU healing as demonstrated in previous studies. 32 , 35 , 36 , 37 Moreover, there have been three systematic reviews and meta‐analyses of exercise for VLU, nevertheless, one review included quantitative studies up to April 2014 in absence of assessment for risk of bias in enrolled records, and performed a narrative method to synthesising outcomes. 41 The second review was published in 2018 with the literature search up to January 2017, there was no restrictions on ulcer healing outcomes. 40 The third review included electronic databases searched through October 2017, but it assessed the added beneficial effect of exercise when used in addition to compression. 42 Thereby we performed this meta‐analysis to quantitatively examine the effects of exercise on healing of VLU along with the assessment of adherence.
After a systematic search of the online databases, a total of eight randomised control trials were included in this meta‐analysis. The pooled RR for healing rate was 1.38 (95% CI: 1.14 to 1.66), the result is suggestive of the beneficial effect of exercise on VLU healing. Of note, one study reported the proportion of patients healed at 9 weeks while other studies revealed 12‐week healing rate. Effect on ulcer healing at 12 weeks remained to be significant with a pooled RR of 1.39 (95% CI: 1.15 to 1.68). Difference on the increase of total range of ankle joint motion in the intervention arm and the control arm was measured to determine the effects of exercise therapy. Standardised mean difference was 0.87 (95% CI: 0.22, 1.52; P = 0.0091) which indicated exercise could significantly improve the range of ankle motion. Nonetheless, the pooled outcome (SMD) showed statistical insignificance with no evidence on heterogeneity after removing the study assessing ROAM at Week 9. The potentially underlying reason for this inconsistence was unclear yet based on the information obtained from the included studies, more evidence is needed to address the contradiction. In the current meta‐analysis, the pooled proportion of participants adherent to exercise regimen was 64% (95% CI: 53%, 75%), patients in these studies received clear direction and tutorials on exercise schedule and performance, and were supervised by investigators to improve the compliance with the regimens. 32 , 33 , 34 , 38 Moreover, results of evaluation for Egger's tests suggested nonsignificant publication bias in enrolled studies.
Although comprehensive approaches in database search, data extraction, quality assessment were used to minimise risk of bias, this meta‐analysis remained to be subject to several limitations. Due to limited covariates in this study and insufficient number of in each subgroup, meta‐analyses on different forms of exercise (including progressive resistance exercise, walking, ankle exercises), adverse events, quality of life and cost effectiveness were not conducted. More well‐designed randomised control trials on the effects of exercise are in need for further evaluation.
In conclusion, in this meta‐analysis, exercise manifested positive effects on VLU healing, range of ankle mobility compared with the control group. Patients' adherence to the exercise regimens was favourable. Due to limited information extracted in included studies, further additional systematic review and meta‐analyses are needed to provide more reliable and powerful evidence.
Supporting information
Figure S1. Funnel plot of healing rates in included studies.
Figure S2. Forest plot of total range of ankle joint motion in included studies.
Figure S3. Forest plot of adherence rates in included studies.
ACKNOWLEDGEMENTS
The authors thank the members of their research group for useful discussions.
Zhang Q, Lu L, Song Jl, Wang L. Effects of exercise in treating patients with venous leg ulcers: A systematic review and meta‐analysis. Int Wound J. 2023;20(5):1776‐1783. doi: 10.1111/iwj.14020
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author.
REFERENCES
- 1. Schneider C, Stratman S, Kirsner RS. Lower extremity ulcers. Med Clin North Am. 2021;105(4):663‐679. [DOI] [PubMed] [Google Scholar]
- 2. Raffetto JD, Ligi D, Maniscalco R, Khalil RA, Mannello F. Why venous leg ulcers have difficulty healing: overview on pathophysiology, clinical consequences, and treatment. J Clin Med. 2020;10(1):29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Team V , Chandler PG, Weller CD. Adjuvant therapies in venous leg ulcer management: a scoping review. Wound Repair Regen. 2019;27(5):562‐590. [DOI] [PubMed] [Google Scholar]
- 4. Schofield D, Shrestha RN, Cunich MM, et al. The costs of diabetes among Australians aged 45‐64 years from 2015 to 2030: projections of lost productive life years (PLYs), lost personal income, lost taxation revenue, extra welfare payments and lost gross domestic product from health&WealthMOD2030. BMJ Open. 2017;7(1):e013158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Haby MM, Markwick A, Peeters A, Shaw J, Vos T. Future predictions of body mass index and overweight prevalence in Australia, 2005‐2025. Health Promot Int. 2012;27(2):250‐260. [DOI] [PubMed] [Google Scholar]
- 6. Vivas A, Lev‐Tov H, Kirsner RS. Venous Leg Ulcers. Ann Intern Med. 2016;165(3):ITC17‐ITC32. [DOI] [PubMed] [Google Scholar]
- 7. Vlajinac H, Marinkovic J, Maksimovic M, Radak D. Factors related to venous ulceration: a cross‐sectional study. Angiology. 2014;65(9):824‐830. [DOI] [PubMed] [Google Scholar]
- 8. Abbade LP, Lastória S, Rollo Hde A. Venous ulcer: clinical characteristics and risk factors. Int J Dermatol. 2011;50(4):405‐411. [DOI] [PubMed] [Google Scholar]
- 9. Bérard A, Abenhaim L, Platt R, Kahn SR, Steinmetz O. Risk factors for the first‐time development of venous ulcers of the lower limbs: the influence of heredity and physical activity. Angiology. 2002;53(6):647‐657. [DOI] [PubMed] [Google Scholar]
- 10. Bonkemeyer Millan S, Gan R, Townsend PE. Venous ulcers: diagnosis and treatment. Am Fam Phys. 2019;100(5):298‐305. [PubMed] [Google Scholar]
- 11. Lal BK. Venous ulcers of the lower extremity: definition, epidemiology, and economic and social burdens. Semin Vasc Surg. 2015;28(1):3‐5. [DOI] [PubMed] [Google Scholar]
- 12. Nelson EA, Adderley U. Venous leg ulcers. BMJ Clin Evid. 2016;2016:1902. [PMC free article] [PubMed] [Google Scholar]
- 13. Kokkosis AA, Labropoulos N, Gasparis AP. Investigation of venous ulcers. Semin Vasc Surg. 2015;28(1):15‐20. [DOI] [PubMed] [Google Scholar]
- 14. O'Donnell TF Jr, Passman MA, Marston WA, et al. Management of venous leg ulcers: clinical practice guidelines of the Society for Vascular Surgery® and the American venous forum. J Vasc Surg. 2014;60(2 Suppl):3s‐59s. [DOI] [PubMed] [Google Scholar]
- 15. Anderson I. Treating patients with venous leg ulcers in the acute setting: part 1. Br J Nurs. 2017;26(12):S32‐S41. [DOI] [PubMed] [Google Scholar]
- 16. Abu‐Own A, Scurr JH, Coleridge Smith PD. Effect of leg elevation on the skin microcirculation in chronic venous insufficiency. J Vasc Surg. 1994;20(5):705‐710. [DOI] [PubMed] [Google Scholar]
- 17. Ontario HQ. Compression stockings for the prevention of venous leg ulcer recurrence: a health technology assessment. Ont Health Technol Assess Ser. 2019;19(2):1‐86. [PMC free article] [PubMed] [Google Scholar]
- 18. Fletcher A, Cullum N, Sheldon TA. A systematic review of compression treatment for venous leg ulcers. BMJ. 1997;315(7108):576‐580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Dolibog P, Franek A, Taradaj J, et al. A comparative clinical study on five types of compression therapy in patients with venous leg ulcers. Int J Med Sci. 2014;11(1):34‐43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. O'Meara S, Cullum NA, Nelson EA. Compression for venous leg ulcers. Cochrane Database Syst Rev. 2009;1:Cd000265. [DOI] [PubMed] [Google Scholar]
- 21. Singer AJ, Tassiopoulos A, Kirsner RS. Evaluation and management of lower‐extremity ulcers. N Engl J Med. 2017;377(16):1559‐1567. [DOI] [PubMed] [Google Scholar]
- 22. Tew GA, Michaels J, Crank H, Middleton G, Gumber A, Klonizakis M. Supervised exercise training as an adjunctive therapy for venous leg ulcers: study protocol for a randomised controlled trial. Trials. 2015;16:443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Davies JA, Bull RH, Farrelly IJ, Wakelin MJ. A home‐based exercise programme improves ankle range of motion in long‐term venous ulcer patients. Phlebology. 2007;22(2):86‐89. [DOI] [PubMed] [Google Scholar]
- 24. Padberg FT Jr, Johnston MV, Sisto SA. Structured exercise improves calf muscle pump function in chronic venous insufficiency: a randomized trial. J Vasc Surg. 2004;39(1):79‐87. [DOI] [PubMed] [Google Scholar]
- 25. Yang D, Vandongen YK, Stacey MC. Effect of exercise on calf muscle pump function in patients with chronic venous disease. Br J Surg. 1999;86(3):338‐341. [DOI] [PubMed] [Google Scholar]
- 26. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hutton B, Salanti G, Caldwell DM, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta‐analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162(11):777‐784. [DOI] [PubMed] [Google Scholar]
- 28. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta‐analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7):e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Riley RD, Higgins JP, Deeks JJ. Interpretation of random effects meta‐analyses. Bmj. 2011;342:d549. [DOI] [PubMed] [Google Scholar]
- 31. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ. 2003;327(7414):557‐560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Jonker L, Todhunter J, Schutter J, Halliday C, Fisher S. A multi‐Centre, prospective, randomised controlled feasibility study of plantar resistance exercise therapy for venous leg ulcers—results of the PREVUE study. Phlebology. 2020;35(4):237‐246. [DOI] [PubMed] [Google Scholar]
- 33. Klonizakis M, Gumber A, McIntosh E, et al. Exercise fidelity and progression in a supervised exercise programme for adults with venous leg ulcers. Int Wound J. 2018;15(5):822‐828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Klonizakis M, Tew GA, Gumber A, et al. Supervised exercise training as an adjunct therapy for venous leg ulcers: a randomized controlled feasibility trial. British J Dermato. 2018;178(5):1072‐1082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Kulprachakarn K, Nantakool S, Rojawat C, et al. Effectiveness of combined conventional treatment with a tailored exercise training program on wound healing in patients with venous leg ulcer: a randomized controlled trial. J Tissue Viability. 2022;31(1):190‐196. [DOI] [PubMed] [Google Scholar]
- 36. Meagher H, Ryan D, Clarke‐Moloney M, O'Laighin G, Grace PA. An experimental study of prescribed walking in the management of venous leg ulcers. J Wound Care. 2012;21(9):421‐430. [DOI] [PubMed] [Google Scholar]
- 37. O'Brien J, Edwards H, Stewart I, Gibbs H. A home‐based progressive resistance exercise programme for patients with venous leg ulcers: a feasibility study. Int Wound J. 2013;10(4):389‐396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. O'Brien J, Finlayson K, Kerr G, Edwards H. Evaluating the effectiveness of a self‐management exercise intervention on wound healing, functional ability and health‐related quality of life outcomes in adults with venous leg ulcers: a randomised controlled trial. Int Wound J. 2017;14(1):130‐137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Szewczyk MT, Jawien A, Cwajda‐Bialasik J, Cierzniakowska K, Moscicka P, Hancke E. Randomized study assessing the influence of supervised exercises on ankle joint mobility in patients with venous leg ulcerations. Arch Med Sci. 2010;6(6):956‐963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Smith D, Lane R, McGinnes R, et al. What is the effect of exercise on wound healing in patients with venous leg ulcers? A systematic review. Int Wound J. 2018;15(3):441‐453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Yim E, Kirsner RS, Gailey RS, Mandel DW, Chen SC, Tomic‐Canic M. Effect of physical therapy on wound healing and quality of life in patients with venous leg ulcers: a systematic review. JAMA Dermatol. 2015;151(3):320‐327. [DOI] [PubMed] [Google Scholar]
- 42. Jull A, Slark J, Parsons J. Prescribed exercise with compression vs compression alone in treating patients with venous leg ulcers: a systematic review and meta‐analysis. JAMA Dermatol. 2018;154(11):1304‐1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Funnel plot of healing rates in included studies.
Figure S2. Forest plot of total range of ankle joint motion in included studies.
Figure S3. Forest plot of adherence rates in included studies.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author.


