Abstract
We conducted a systematic review to evaluate combinations of physical activity, sedentary behavior, and sleep duration (defined as “movement behaviors”) and their associations with physical, psychological, and educational outcomes in children and adolescents. MEDLINE, CINAHL, PsychInfo, SPORTDiscus, PubMed, EMBASE, and ERIC were searched in June 2020. Included studies needed to 1) quantitatively analyze the association of 2 or more movement behaviors with an outcome, 2) analyze a population between 5 and 17 years of age, and 3) include at least an English abstract. We included 141 studies. Most studies included the combination of physical activity and sedentary behavior in their analyses. Sleep was studied less frequently. In combination, a high level of physical activity and a low level of sedentary behavior were associated with the best physical health, psychological health, and education-related outcomes. Sleep was often included in the combination that was associated with the most favorable outcomes. Sedentary behavior had a stronger influence in adolescents than in children and tended to be associated more negatively with outcomes when it was defined as screen time than when defined as overall time spent being sedentary. More initiatives and guidelines combining all 3 movement behaviors will provide benefit with regard to adiposity, cardiometabolic risk factors, cardiorespiratory fitness, muscular physical fitness, well-being, health-related quality of life, mental health, academic performance, and cognitive/executive function.
Keywords: adolescents, children, physical activity, sedentary behavior, sleep
Abbreviations
- ERIC
Education Resources Information Center
- STROBE
Strengthening the Reporting of Observational Studies in Epidemiology
Child and adolescent movement behaviors (i.e., physical activity, sedentary behavior, and sleep duration) are individually associated with many similar physical (e.g., adiposity) (1–6), psychological (e.g., mental health) (7–9), and educational (e.g., academic performance) (3, 4, 9–14) outcomes. Spending time in one movement behavior displaces time spent in others, which may explain the overlap in associations with outcomes. However, these overlaps make it difficult to disentangle which behaviors are associated with specific outcomes. Therefore, researchers have started studying combinations of movement behaviors instead of studying them in isolation.
A previous systematic review by Saunders et al. (15) included 14 studies from 2011–2015 and found that the combinations of 1) high physical activity with low sedentary behavior, 2) high physical activity with high sleep duration, and 3) high physical activity, low sedentary behavior, and high sleep duration were associated with the most desirable physical health outcomes. This review informed several international health recommendations (16–19), including the Canadian 24-Hour Movement Behavior Guidelines for Children and Youth (20). Due to the popularity of these recommendations and the introduction of new analytical methods, such as compositional data analysis (21), research on movement behaviors has increased substantially. Therefore, an update to the previous review is needed.
While the associations between combinations of movement behaviors and physical health outcomes are known, many psychological and educational outcomes have yet to be systematically reviewed. With rising rates of depression and anxiety among children and adolescents (22, 23), psychological and educational outcomes are a growing concern, and thus research on these outcomes should be synthesized. Reporting of associations for combinations of movement behaviors with psychological and educational outcomes may inspire a wider range of professionals (e.g., teachers, clinical psychologists) to adopt interventions addressing multiple movement behaviors. In turn, these professionals may provide valuable input to alter guidelines to suit a broader range of outcomes. Therefore, we aimed to update and expand on the Saunders et al. review (15).
METHODS
Search strategy and selection criteria
We prospectively registered this systematic review on PROSPERO (https://www.crd.york.ac.uk/PROSPERO/; identification number: CRD42020181097), and we report our findings in line with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (24).
To be included, studies needed to quantitatively analyze the association of at least 2 movement behaviors (i.e., physical activity, sedentary behavior, and sleep duration) with any outcome (i.e., physical, psychological, or educational) in youth (mean age 5–17 years). We modified the exclusion criteria from the previous review by not excluding studies based on sample size or type of physical activity measurement, whereas Saunders et al. (15) required a minimum sample size of 300. We placed no exclusion criteria based on study design, setting, publication status, or publication date. We included studies published in any language, provided they had an abstract in English with quantitative results.
We searched the following electronic databases in June 2020: MEDLINE (National Library of Medicine, Bethesda, Maryland), Cumulative Index to Nursing and Allied Health Literature (CINAHL) (EBSCO Industries, Birmingham, Alabama), PsychInfo (American Psychological Association, Washington, DC), SPORTDiscus (EBSCO Industries), PubMed (National Library of Medicine), Excerpta Medica Database (EMBASE) (Elsevier BV, Amsterdam, the Netherlands), and Education Resources Information Center (ERIC) (EBSCO Industries). We included more databases than the previous review, such as ERIC, to capture studies exploring a wider range of outcomes. Our search strategy can be found in Web Appendix 1 (available at https://doi.org/10.1093/aje/kwac212). We revised the previous search strategy to include the combination of any 2 movement behaviors and to cater the search strategy to more databases.
Study selection, data extraction, and quality assessment
We uploaded all relevant articles to Covidence review management software (Covidence, Melbourne, Victoria, Australia (www.covidence.org)) and removed duplicates. Two independent reviewers screened titles and abstracts. Two reviewers independently screened full-text articles for studies that passed title/abstract screening. We resolved conflicts by consensus. One reviewer conducted bidirectional screening using the 14 articles from the Saunders et al. review (15) and 1 additional recent article. Bidirectional screening is a method wherein a reviewer screens all references within an article and any articles that cited the article (25), providing a more thorough literature search.
Two independent reviewers completed data extraction and quality assessment. Data items included the name of the lead author, the publication date, the sample size, the combination of movement behaviors evaluated, the outcomes measured, the measurement methods used, and the results. Preliminary searches and the Saunders et al. review (15) indicated that mainly observational studies would be included. Therefore, we evaluated study quality using an adapted version of the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Checklist (26). As per previous reviews (27, 28), we rated studies on 9 criteria derived from STROBE items, since the absence of these items could potentially introduce bias. Studies were considered high-quality if they met 7 or more criteria.
Data synthesis
There was substantial methodological heterogeneity across the studies, preventing a meta-analysis. Specifically, movement behaviors were categorized inconsistently. For example, some studies dichotomized movement behaviors (e.g., meeting/not meeting guidelines), others used sample-specific median splits, and others used compositional data analysis. While some studies could have been meta-analyzed (e.g., only those with isotemporal substitution), most would have been excluded, risking systematically biased results. Accordingly, we narratively compared combinations of movement behaviors relative to other combinations within the same study. Per the Cochrane Collaboration (29), comparisons were based on the direction of associations, not statistical significance. Exemplar studies were characterized to obtain potential associations.
Sedentary behavior was defined differently across studies (e.g., “screen time,” “sitting”). In this review, we have generally used the term “sedentary behavior.” We used “screen time” when we synthesized studies that all used “screen time” as their original definition of sedentary behavior. We noted instances where the definition of sedentary behavior influenced the results.
Due to the high number of studies that investigated different combinations of meeting the Canadian 24-Hour Movement Behavior Guidelines for Children and Youth (see Web Appendix 2), we refer to these recommendations as “movement behavior guidelines” in our synthesis. We synthesized data separately for children (mean age 5–13 years) and adolescents (mean age 14–17 years). These age ranges were chosen on the basis of current guidelines that separate sleep recommendations for children and adolescents (17, 20). We also analyzed whether objective versus subjective measures of physical activity influenced the results. Finally, “sleep” refers to sleep duration.
Table 1 provides a concise summary of our results. This table highlights general trends in the included studies on the basis of age group, outcome, and whether the studies investigated the combination of physical activity and sedentary behavior exclusively or whether the combination of all 3 movement behaviors was included. The combination of physical activity and sedentary behavior was addressed in the table because studies evaluating this combination made up a majority of the studies in this review.
Table 1.
Associations of Combinations of Movement Behaviors (Physical Activity, Sedentary Behavior, and Sleep Duration) With Physical, Psychological, and Educational Outcomes in Children and Adolescents in a Systematic Review, 2002–2020
| Combination of Movement Behaviors and Age Group a | ||||
|---|---|---|---|---|
| Physical Activity and Sedentary Behavior | Physical Activity, Sedentary Behavior, and Sleep Duration | |||
| Outcome | Children | Adolescents | Children | Adolescents |
| Adiposity | The combination of high physical activity and low sedentary behavior was most beneficial. | The combination of high physical activity and low sedentary behavior was most beneficial. Evidence suggested that sedentary behavior is more important during adolescence than in childhood. |
The combination of high physical activity, low sedentary behavior, and high sleep level was most beneficial. | The combination of high physical activity, low sedentary behavior, and high sleep level was most beneficial. |
| Cardiometabolic risk factors | The combination of high physical activity and low sedentary behavior was most beneficial. | The combination of high physical activity and low sedentary behavior was most beneficial. | The combination of high physical activity and high sleep level was most beneficial. | No studies included sleep. |
| Cardiorespiratory fitness | A high level of physical activity was important, regardless of sedentary behavior. | The combination of high physical activity and low sedentary behavior was most beneficial. | The combination of high physical activity and high sleep level was most beneficial. | No studies included sleep. |
| Muscular physical fitness | The combination of high physical activity and low sedentary behavior was most beneficial. | No studies included adolescents. | The combination of high physical activity and high sleep level was most beneficial. | No studies included adolescents. |
| Well-being and socioemotional outcomes | The combination of high physical activity and low sedentary behavior was most beneficial. | The combination of high physical activity and low sedentary behavior was most beneficial. | The combination of high physical activity, low sedentary behavior, and high sleep level was most beneficial. | The combination of high physical activity, low sedentary behavior, and high sleep level was most beneficial. |
| Health-related quality of life | The combination of high physical activity and low sedentary behavior was most beneficial. Regarding sedentary behavior, screen time should particularly be addressed. |
The combination of high physical activity and low sedentary behavior was most beneficial. Regarding sedentary behavior, screen time should particularly be addressed. |
The combination of high physical activity, low sedentary behavior, and high sleep level was most beneficial. | No studies included sleep. |
| Mental ill health | The combination of high physical activity and low sedentary behavior was most beneficial. | The combination of high physical activity and low sedentary behavior was most beneficial. | The combination of high physical activity, low sedentary behavior, and high sleep level was most beneficial. | The combination of high physical activity, low sedentary behavior, and high sleep level was most beneficial. |
| Academic performance | The combination of high physical activity and high sedentary behavior was associated with positive academic performance. The combination of high physical activity and low screen time was associated with positive academic performance. |
The combination of high physical activity and high sedentary behavior was associated with positive academic performance. The combination of high physical activity and low screen time was associated with positive academic performance. |
The combination of high physical activity, low sedentary behavior, and high sleep level was most beneficial. | The combination of high physical activity, low sedentary behavior, and high sleep level was most beneficial. |
| Cognitive and executive function | The combination of high physical activity and low screen time was most beneficial. | No studies included adolescents. | The combination of low screen time and high sleep level was most beneficial. | No studies included sleep. |
a Children were defined as participants with a mean age of 5–13 years, and adolescents were defined as those with a mean age of 14–17 years.
RESULTS
Description of studies
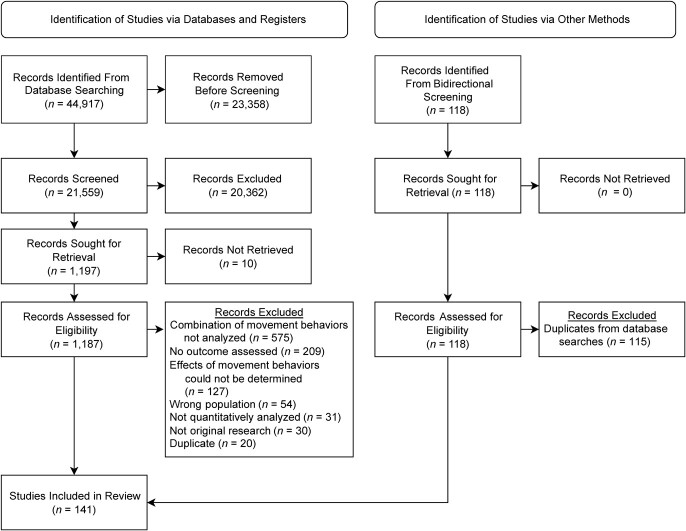
We imported 44,917 references into Covidence. After removal of duplicates, 21,559 studies remained for title/abstract screening and 1,197 studies moved forward to full-text screening. Ten studies could not be retrieved after searching in academic libraries and requesting interlibrary loans. Three additional studies were added for full-text screening from the bidirectional screening process. Our total for data extraction included 141 studies (including 2 conference abstracts), all of which had an English version available (see Figure 1). A list of excluded studies can be found in Web Table 1.
Figure 1.
Selection of studies for inclusion in a systematic review of the associations of combinations of movement behaviors (physical activity, sedentary behavior, and sleep duration) with physical, psychological, and educational outcomes in children and adolescents, 2002–2020 followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (24).
Fifty-seven countries were represented across the studies, which were primarily from the United States (n = 29 studies), Canada (n = 21), and Australia (n = 19). Most studies (84%; 119/141) were high-quality (see Web Table 2) with a mean quality score of 7.4/9. The least reported items were “describe any efforts to address potential sources of bias” and “describe any methods used to examine subgroups and interactions.” Study characteristics can be found in Web Table 3.
Total physical activity, at any time of day or location, was primarily reported. Four studies reported on subdomains (e.g., sports). When studies were evaluated separately based on data being measured objectively or subjectively, the trends were the same. This was also true for study quality. The data set generated and analyzed during the current study is available in the Open Science Framework repository.
Physical health–related outcomes
Adiposity.
Ten longitudinal studies and 79 cross-sectional studies investigated adiposity. Adiposity was measured by body mass index (weight (kg)/height (m)2), waist circumference, waist:height ratio, skinfold thickness, body fat percentage, visceral adipose tissue, and fat mass index (fat mass (kg)/height (m)2). Overall, participants with a higher level of physical activity and a lower level of sedentary behavior had less adiposity than persons with other combinations of these 2 behaviors. Results differed slightly by age group. For children, the most optimal combination was generally high physical activity and low sedentary behavior. For adolescents, a lower level of sedentary behavior was associated with lower adiposity, especially in girls. These results were consistent regardless of whether sedentary behavior was measured as electronic screen time or as total sedentary behavior. When sleep was analyzed, combinations with a high sleep level were associated with lower adiposity.
Ten longitudinal studies and 51 cross-sectional studies investigated the relationship between physical activity and sedentary behavior in adiposity. Investigators in the majority of those studies (6 longitudinal studies (29–34) and 32 cross-sectional studies (35–66)) concluded that the combination of high physical activity and low sedentary behavior was associated with the best adiposity outcomes among children and adolescents. For example, in one longitudinal study of 9,155 children and adolescents, youths with 5 bouts of moderate–vigorous physical activity per week and 4 hours of screen time per week had 25% lower odds of obesity 5 years later as compared with those with 3 bouts of moderate–vigorous physical activity and 25 hours of screen time per week (30). The remaining results differed by age (41–44, 47–49, 57–59, 61, 62, 68–76). Eleven studies used isotemporal substitution (2 longitudinal studies (77, 78) and 9 cross-sectional studies (44, 79–86)), all of which found that substituting sedentary behavior with moderate–vigorous physical activity was associated with lower adiposity.
Sixteen cross-sectional studies investigated the combinations of all 3 movement behaviors. All found that persons with a higher level of sleep had less adiposity than their peers (46, 66, 87–100). In 11 of these studies, the combination of high physical activity, low sedentary behavior, and high sleep had the best association with adiposity (46, 66, 87–93, 96, 97), while the remaining 5 studies had mixed results (90, 94, 95, 98, 99). An additional 12 cross-sectional studies used isotemporal substitution (77, 81, 86, 101–109) and found that substituting sedentary behavior with moderate–vigorous physical activity was associated with lower adiposity. There were mixed results on substituting sedentary behavior with sleep.
Cardiometabolic risk factors.
Three longitudinal studies and 18 cross-sectional studies evaluated cardiometabolic risk factors. Cardiometabolic risk factors assessed included systolic and diastolic blood pressure, insulin-related measures, triglycerides, cholesterol, and C-reactive protein. Overall, active children with a high sleep level had the most desirable levels of cardiometabolic risk factors. For adolescents, the combination of high physical activity and low sedentary behavior was associated with desirable levels of cardiometabolic risk factors.
Two longitudinal studies and 12 cross-sectional studies evaluated the association of combined physical activity and sedentary behavior with cardiometabolic risk factors. Researchers in all of the studies agreed that the combination of high physical activity and low sedentary behavior was associated with the best outcomes for cardiometabolic risk (48, 62, 64, 72, 74–76, 110–116). For example, investigators in one longitudinal study (n = 3,717) conducted a cluster analysis and found that persons with higher physical activity and lower sedentary behavior than their peers with lower physical activity but similar sedentary behavior had 13% lower odds of developing diabetes over a 5-year period (116). Investigators in 5 separate studies generally agreed that substituting sedentary behavior with moderate–vigorous activity was associated with the most desirable cardiometabolic outcomes (81, 85, 86, 108, 117). Researchers in one of these studies included sleep in their analysis and found mixed results, depending on the specific outcome, of substituting sedentary behavior with sleep (108). Findings from 2 studies (1 longitudinal (89) and 1 cross-sectional (118)), both in children, indicated that the addition of high sleep in combination with low screen time and/or physical activity yielded the most favorable cardiometabolic outcomes. No studies included sleep in adolescents.
Cardiorespiratory fitness.
One longitudinal study and 17 cross-sectional studies investigated cardiorespiratory fitness.
Overall, combinations with high moderate–vigorous physical activity were associated with higher cardiorespiratory fitness. Specifically for adolescents, lower sedentary behavior was associated with higher cardiorespiratory fitness. Additionally, sleep was associated with higher cardiorespiratory fitness in children.
One longitudinal study in children (n = 315) found that substituting 30 minutes of sedentary behavior with vigorous-intensity physical activity yielded a positive association with cardiorespiratory fitness (β = 0.307) (119). Authors of 6 cross-sectional studies supported the longitudinal study’s finding by concluding that substituting sedentary behavior with moderate–vigorous physical activity was positively associated with cardiorespiratory fitness for children and adolescents (80, 82, 84, 102, 108, 120). An additional 6 cross-sectional studies found that children with higher physical activity than their peers, regardless of sedentary behavior, had higher cardiorespiratory fitness (37, 38, 121–124). However, in adolescents, 3 cross-sectional studies found that those who were more active and less sedentary than their peers had the highest cardiorespiratory fitness (47, 64, 125). Two studies that included all 3 movement behaviors found that children who were more active and slept longer than their peers had higher cardiorespiratory fitness (89, 126). No studies included sleep for adolescents.
Muscular fitness.
Three cross-sectional studies investigated children’s muscular fitness and found a positive association for those with high physical activity, low sedentary behavior, and high sleep duration.
Two cross-sectional studies determined that children’s spending more time in physical activity and less time in sedentary behavior was associated with better muscular fitness outcomes (70, 79). For example, a study in 2,506 children found those with at least 60 minutes of moderate–vigorous physical activity per day and low sedentary behavior (characterized by a median split) were 2.5 times more likely to fall into the “healthy zone” for flexibility than children with less than 60 minutes of moderate–vigorous physical activity per day and high sedentary behavior (70). The final study (n = 243) evaluated children meeting different combinations of movement behavior guidelines (126). Generally, children meeting physical activity and sleep recommendations had higher muscular strength, muscular endurance, and flexibility than children with any other combination of movement behaviors (126).
Psychological outcomes
Well-being and socioemotional outcomes.
Two longitudinal studies and 10 cross-sectional studies investigated the association between well-being and socioemotional outcomes. The combination of high physical activity, low sedentary behavior, and high sleep had the most favorable outcomes with life satisfaction, happiness, stress, positive affect, negative affect, angriness, confusion, prosocial behavior, emotional health, peer problems, and hyperactivity.
Both longitudinal studies (127, 128) and 6 cross-sectional studies (129–134) found that children and adolescents who were more active and less sedentary than their peers had better socioemotional outcomes. For example, a longitudinal study carried out over 6 years in 3,979 children found that those who maintained low levels of physical activity and screen time or maintained physical activity levels but increased screen time had more socioemotional problems than those who increased their physical activity and maintained low levels of screen time (β = 0.46–0.74) (128). Four studies included sleep in their analysis. All found positive associations of the combination of high physical activity, low sedentary behavior, and high sleep with well-being (32, 89, 100, 108).
Health-related quality of life.
Three longitudinal studies and 6 cross-sectional studies investigated health-related quality of life. The combination of high physical activity and low sedentary behavior (particularly screen time) was associated with the best outcomes. The addition of sleep appeared to improve outcomes.
All studies investigating physical activity and sedentary behavior (3 longitudinal studies (127, 128, 135) and 5 cross-sectional studies (84, 136–139)) concluded that high physical activity and low sedentary behavior had the most positive association with health-related quality of life. The longitudinal study with the largest sample size (n = 3,979) found that children who maintained low levels of physical activity and screen time or maintained physical activity levels but increased screen time over 6 years had lower health-related quality of life than those who increased their physical activity and maintained low levels of screen time (β = −2.29–1.40) (128).
In only 1 study did researchers include sleep in their analysis, and they found that those meeting all movement behavior guidelines had the best health-related quality of life (140).
Mental health.
Twelve cross-sectional studies examined depression and anxiety. Appropriate amounts of all 3 movement behaviors were associated with better mental health, but sleep appeared to have the most consistent positive associations.
Seven studies found that participants who were more active and less sedentary than their peers had better mental health (131, 141–146). All 5 studies that included sleep in their analysis suggested that high sleep may have a protective association with mental health, since combinations that included high sleep usually had the most desirable outcomes (142, 147–150). For example, a study in 20,078 adolescents found that those who met all movement behavior recommendations had the lowest odds of having anxiety or depression (147). However, combinations not including sleep were associated with the highest odds of having anxiety or depression (odds ratio = 3.92–37.14).
Education-related outcomes
Academic performance.
One longitudinal study and 8 cross-sectional studies investigated academic performance. The association of high physical activity with low screen time or high physical activity with high total sedentary behavior was associated with the best academic performance for children and adolescents. Sufficient sleep seemed to be beneficial for academic performance.
Studies that measured sedentary behavior as screen time (1 longitudinal (151) and 2 cross-sectional (152, 153)) found that those who were more active with less screen time than their peers had the best academic performance. The longitudinal study (n = 261) found that children who participated in ≥60 minutes of moderate–vigorous physical activity per day and ≤2 hours of screen time per day were 2.75 times more likely to have better grades than children with less than 60 minutes of moderate–vigorous physical activity per day and more than 2 hours of screen time/day (151). However, children who engaged in more non–screen-based sedentary behavior (e.g., reading) had higher overall academic performance than their peers who spent less time in non–screen-based sedentary behavior, regardless of physical activity (67, 153–157). One study (n = 285) found that children with high physical activity and high total sedentary behavior had the best standardized test scores (504 vs. 471–502) (157). One study investigated the effect of combinations of all 3 movement behaviors on academic performance and found that meeting all movement behavior guidelines was the most beneficial (158). Furthermore, all combinations that included meeting the sleep recommendation were associated with higher academic performance than only meeting the combination of physical activity and screen time recommendations.
Cognitive/executive function.
Three cross-sectional studies examined associations of combinations of movement behaviors with cognitive and executive functioning in children. The combination of low screen time and long sleep duration was most beneficial.
One study found that children who were more active with less screen time than their peers had the highest level of executive functioning (159). Two additional studies included sleep in their analyses. Both studies found that children meeting the screen time and sleep guidelines had the most desirable associations with cognition and impulsivity as compared with all other combinations (160, 161). For example, the β coefficient for the effect of the association between low screen time and high sleep time on cognition was 3.21–5.37 (162).
Additional outcomes
The remaining studies investigated nonalcoholic fatty liver disease, insomnia, and gross motor skills in children. They also studied the associations of vitamin D concentration, bone mineral content, hormone levels, and DNA methylation in adolescents with different combinations of physical activity, sedentary behavior, and sleep (113, 131, 163–167). There were only 1 or 2 studies for each of the above outcomes. Generally, researchers found that children and adolescents who were more active and less sedentary than their peers had the most favorable outcomes.
Although most studies found that those who were the most active, were the least sedentary, and slept the longest had the most optimal outcomes overall, we noted a few considerations based on outcome and age group. See Table 1 for a summary of the findings.
DISCUSSION
In this systematic review, we aimed to improve our understanding of the associations of different combinations of physical activity, sedentary behavior, and sleep duration with physical, psychological, and educational outcomes in children and adolescents. Overall, we found that those who were more active, were less sedentary, and slept longer than their peers appeared to have the most favorable outcomes. Additionally, this review highlights the importance of sleep, both in practice and in future research. On several occasions, when only physical activity and sedentary behavior were considered in studies, we found that high physical activity and low sedentary behavior was the “best” combination. However, studies that included sleep found that combinations including high sleep levels were usually the superior option. For example, all combinations that included high sleep duration were associated with desirable mental health outcomes. Yet, out of 141 eligible studies, only 41 included sleep in their analyses. Fewer sleep studies were available for adolescents than for children. Possible explanations could be that researchers may study sleep more in children, since the onset of some disorders (e.g., attention-deficit/hyperactivity disorder) occurs at a younger age (168), or adolescent data were not available in the analyzed data sets (79, 126, 140, 160, 161).
Compromising on any movement behavior had consequences. A lower level of physical activity appeared to be associated with the most negative changes for physical health. Too much sedentary behavior, particularly screen time, was typically associated with poorer psychological health. Shorter sleep duration negatively affected all types of outcomes. For this reason, we cannot target one movement behavior without acknowledging the importance of the others. Including sleep in more longitudinal and intervention research could help investigators make stronger inferences about the associations of different combinations of movement behaviors with physical, psychological, and educational outcomes.
Limiting sedentary behavior appears to be especially important in adolescents. Low sedentary behavior in combination with high physical activity and/or sleep seemed to be crucial to achieving the most favorable adolescent physical health outcomes (e.g., adiposity). However, for children, studies found that low sedentary behavior did not appear to be important as long as physical activity and sleep levels were high. This may be explained by a potential association with total sitting time and poor dietary habits in adolescents (169). Additionally, the definition of sedentary behavior was important. For example, when sedentary behavior was defined as non–screen-based behavior, its association with academic performance was positive. This suggests that not all sedentary behavior is “bad.” Further, not all domains or types of physical activity may yield the same results. The most ideal combination for cognitive/executive functioning did not include high physical activity. Research shows that physical activity may be beneficial for cognitive development (170), but these associations may only be positive when accumulated through sports (171). Therefore, in future studies, researchers should consider exploring domain-specific movement behaviors and replicate findings on the less well-explored outcomes (e.g., executive function).
We synthesized data from 141 studies on 16 outcomes from 57 countries, making our review more reliable and generalizable than previous syntheses. However, limitations of our review should be considered when interpreting the data. First, we decided not to conduct a meta-analysis due to high heterogeneity in how the studies categorized, analyzed, and reported movement behaviors. For example, of the 3 studies on muscular fitness, 1 used isotemporal substitution, 1 considered whether or not children met all guidelines simultaneously, and 1 used sample-specific sedentary behavior median splits. As a result, we could not quantify the size of the pooled associations for the effect of each combination of movement behaviors on each outcome. More consistent reporting of associations across studies would facilitate meta-analyses. Alternatively, the wider availability of primary data would facilitate secondary analyses such as individual participant meta-analyses (172).
Finally, the included studies made some common methodological decisions that impaired our ability to draw firm conclusions. Many studies dichotomized movement behaviors using the current recommendations. This means that children who participated in 3 minutes of moderate–vigorous physical activity per day were analyzed the same way as children who participated in 59 minutes of moderate–vigorous physical activity per day, as both groups failed to meet the 60 minutes/day recommendation. Thus, the likely dose-response relationship for physical activity (and potentially other behaviors) could not be considered (1, 5, 173, 174). In future studies, investigators should explore isotemporal substitution or compositional data analysis, because these methods analyze the trade-offs in movement behaviors while accounting for dose-response associations. Further, the physical activity recommendation states that “muscle and bone strengthening activities should each be incorporated at least 3 days per week” (20, p. 319), but this was not included in any of the studies’ definition of meeting physical activity recommendations. Future research should account for this component of the guidelines, because resistance training has been shown to improve physical and mental health (175, 176).
In conclusion, the evidence suggests that physical activity, sedentary behavior, and sleep duration should be investigated in combination, not in isolation. Due to the consistent positive associations of sleep with a range of outcomes, we encourage researchers to consider sleep in their studies of movement behaviors. Guidelines, interventions, and public health campaigns should look beyond promoting single movement behaviors and move toward targeting all 3. The needs of children and adolescents could better be considered. Finally, children, adolescents, parents, and schools should be informed that physical activity, sedentary behavior, and sleep affect more than just children’s physical health; they also affect their psychological health and educational development.
Supplementary Material
ACKNOWLEDGMENTS
Author affiliations: Institute of Positive Psychology and Education, Faculty of Health Sciences, Australian Catholic University, North Sydney, New South Wales, Australia (Katrina Wilhite, Bridget Booker, Philip Parker, Chris Lonsdale, Taren Sanders); Charles Perkins Center, School of Health Sciences, Faculty of Medicine and Health, University of Sydney, Sydney, New South Wales, Australia (Bo-Huei Huang); School of Education, Faculty of Social Sciences, University of Wollongong, Wollongong, New South Wales, Australia (Devan Antczak); School of Public Health, Faculty of Medicine and Health Sciences, University of Sydney, Sydney, New South Wales, Australia (Lucy Corbett); Institute of Positive Psychology and Education, School of Behavioral and Health Sciences, Faculty of Health Sciences, Australian Catholic University, North Sydney, New South Wales, Australia (Michael Noetel); College of Medicine and Public Health, Flinders in the Northern Territory (Flinders University), Bedford Park, South Australia, Australia (Chris Rissel); and Center for Active and Healthy Aging, Department of Sport Sciences and Clinical Biomechanics, Faculty of Health Sciences, University of Southern Denmark, Odense, Denmark (Borja del Pozo Cruz).
The data set generated and analyzed during the current study is available in the Open Science Framework repository (https://osf.io/jq8xh/?view_only=8561ee06ed324cb9b99da1520afa8ed7).
We thank the Australian Catholic University librarian, Philippa Crosbie, for her help with development of the search strategy.
This paper was presented at the International Society of Behavorial Nutrition and Physical Activity Meeting and Conference, Phoenix, Arizona, May 18–21, 2022.
Conflict of interest: none declared.
REFERENCES
- 1. Janssen I, Leblanc AG. Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int J Behav Nutr Phys Act. 2010;7:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Must A, Tybor DJ. Physical activity and sedentary behavior: a review of longitudinal studies of weight and adiposity in youth. Int J Obes (Lond). 2005;29(suppl 2):S84–S96. [DOI] [PubMed] [Google Scholar]
- 3. Watson A, Timperio A, Brown H, et al. Effect of classroom-based physical activity interventions on academic and physical activity outcomes: a systematic review and meta-analysis. Int J Behav Nutr Phys Act. 2017;14:114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mavilidi MF, Mason C, Leahy AA, et al. Effect of a time-efficient physical activity intervention on senior school students’ on-task behaviour and subjective vitality: the ‘Burn 2 Learn’ cluster randomised controlled trial. Educ Psychol Rev. 2021;33(1):299–323. [Google Scholar]
- 5. Tremblay MS, LeBlanc AG, Kho ME, et al. Systematic review of sedentary behaviour and health indicators in school-aged children and youth. Int J Behav Nutr Phys Act. 2011;8:98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Spruyt K, Molfese DL, Gozal D. Sleep duration, sleep regularity, body weight, and metabolic homeostasis in school-aged children. Pediatrics. 2011;127(2):e345–e352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Biddle SJ, Asare M. Physical activity and mental health in children and adolescents: a review of reviews. Br J Sports Med. 2011;45(11):886–895. [DOI] [PubMed] [Google Scholar]
- 8. Anokye NK, Trueman P, Green C, et al. Physical activity and health related quality of life. BMC Public Health. 2012;12:624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Donnelly JE, Hillman CH, Castelli D, et al. Physical activity, fitness, cognitive function, and academic achievement in children: a systematic review. Med Sci Sports Exerc. 2016;48(6):1197–1222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Mavilidi MF, Lubans DR, Miller A, et al. Impact of the “Thinking while Moving in English” intervention on primary school children’s academic outcomes and physical activity: a cluster randomised controlled trial. Int J Educ Res. 2020;102:101592. [Google Scholar]
- 11. Greeff JW, Bosker RJ, Oosterlaan J, et al. Effects of physical activity on executive functions, attention and academic performance in preadolescent children: a meta-analysis. J Sci Med Sport. 2018;21(5):501–507. [DOI] [PubMed] [Google Scholar]
- 12. Nixon GM, Thompson JMD, Han DY, et al. Short sleep duration in middle childhood: risk factors and consequences. Sleep. 2008;31(1):71–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Dewald JF, Meijer AM, Oort FJ, et al. The influence of sleep quality, sleep duration and sleepiness on school performance in children and adolescents: a meta-analytic review. Sleep Med Rev. 2010;14(3):179–189. [DOI] [PubMed] [Google Scholar]
- 14. Li S, Arguelles L, Jiang F, et al. Sleep, school performance, and a school-based intervention among school-aged children: a sleep series study in China. PLoS One. 2013;8(7):e67928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Saunders TJ, Gray CE, Poitras VJ, et al. Combinations of physical activity, sedentary behaviour and sleep: relationships with health indicators in school-aged children and youth. Appl Physiol Nutr Metab. 2016;41(6 suppl 3):S283–S293. [DOI] [PubMed] [Google Scholar]
- 16. Draper CE, Tomaz SA, Biersteker L, et al. The South African 24-Hour Movement Guidelines for Birth to 5 Years: an integration of physical activity, sitting behavior, screen time, and sleep. J Phys Act Health. 2020;17(1):109–119. [DOI] [PubMed] [Google Scholar]
- 17. Department of Health and Aged Care, Australian Government . Physical activity and exercise guidelines for all Australians. https://www.health.gov.au/topics/physical-activity-and-exercise/physical-activity-and-exercise-guidelines-for-all-australians. Published 2019. Accessed January 12, 2023.
- 18. World Health Organization . Guidelines on Physical Activity, Sedentary Behaviour and Sleep for Children Under 5 Years of Age. Geneva, Switzerland: World Health Organization; 2019. [PubMed] [Google Scholar]
- 19. Tremblay MS. Introducing 24-hour movement guidelines for the early years: a new paradigm gaining momentum. J Phys Act Health. 2020;17(1):92–95. [DOI] [PubMed] [Google Scholar]
- 20. Tremblay MS, Carson V, Chaput JP, et al. Canadian 24-Hour Movement Guidelines for Children and Youth: an integration of physical activity, sedentary behaviour, and sleep. Appl Physiol Nutr Metab. 2016;41(6 suppl 3):S311–S327. [DOI] [PubMed] [Google Scholar]
- 21. Chastin SFM, Palarea-Albaladejo J, Dontje ML, et al. Combined effects of time spent in physical activity, sedentary behaviors and sleep on obesity and cardio-metabolic health markers: a novel compositional data analysis approach. PLoS One. 2015;10(10):e0139984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Chen Y. A systematic review of interventions for childhood depression. In: Bin MZ, Ghaffar NA, eds. Proceedings of the 2021 4th International Conference on Humanities Education and Social Sciences (ICHESS 2021). (Advances in Social Science, Education and Humanities Research, vol. 615). Amsterdam, the Netherlands: Atlantis Press; 2021:1683–1686. [Google Scholar]
- 23. Gleason MM, Thompson LA. Depression and anxiety disorder in children and adolescents. JAMA Pediatr. 2022;176(5):532. [DOI] [PubMed] [Google Scholar]
- 24. Moher D, Liberati A, Tetzlaff J, et al. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA Statement. PLoS Med. 2009;6(7):e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hinde S, Spackman E. Bidirectional citation searching to completion: an exploration of literature searching methods. Pharmacoeconomics. 2015;33(1):5–11. [DOI] [PubMed] [Google Scholar]
- 26. Elm E, Altman DG, Egger M, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. BMJ. 2007;335(7624):806–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Doherty C, Delahunt E, Caulfield B, et al. The incidence and prevalence of ankle sprain injury: a systematic review and meta-analysis of prospective epidemiological studies. Sports Med. 2014;44(1):123–140. [DOI] [PubMed] [Google Scholar]
- 28. López-Valenciano A, Ruiz-Pérez I, Garcia-Gómez A, et al. Epidemiology of injuries in professional football: a systematic review and meta-analysis. Br J Sports Med. 2020;54(12):711–718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions. New York, NY: John Wiley & Sons, Inc.; 2011. [Google Scholar]
- 30. Boone JE, Gordon-Larsen P, Adair LS, et al. Screen time and physical activity during adolescence: longitudinal effects on obesity in young adulthood. Int J Behav Nutr Phys Act. 2007;4:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Gordon-Larsen P, Adair LS, Popkin BM. Ethnic differences in physical activity and inactivity patterns and overweight status. Obes Res. 2002;10(3):141–149. [DOI] [PubMed] [Google Scholar]
- 32. Lee EY, Spence JC, Tremblay MS, et al. Meeting 24-hour movement guidelines for children and youth and associations with psychological well-being among South Korean adolescents. Ment Health Phys Act. 2018;14:66–73. [Google Scholar]
- 33. Sánchez-Oliva D, Grao-Cruces A, Carbonell-Baeza A, et al. Lifestyle clusters in school-aged youth and longitudinal associations with fatness: the UP&DOWN Study. J Pediatr. 2018;203:317–324.e1. [DOI] [PubMed] [Google Scholar]
- 34. Van den Bulck J, Hofman A. The television-to-exercise ratio is a predictor of overweight in adolescents: results from a prospective cohort study with a two year follow up. Prev Med. 2009;48(4):368–371. [DOI] [PubMed] [Google Scholar]
- 35. Tahir MJ, Willett W, Forman MR. The association of television viewing in childhood with overweight and obesity throughout the life course. Am J Epidemiol. 2019;188(2):282–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Djalalinia S, Qorbani M, Rezaei N, et al. Joint association of screen time and physical activity with anthropometric measures in Iranian children and adolescents: the weight disorders survey of the CASPIAN-IV Study. J Pediatr Endocrinol Metab. 2017;30(7):731–738. [DOI] [PubMed] [Google Scholar]
- 37. Dollman J, Olds T, Ridley K, et al. Clusters of children’s physical activity and sedentary behaviours differ in physiological, social and environmental attributes [abstract]. J Sci Med Sport. 2004;7(suppl 4):85.15139168 [Google Scholar]
- 38. Dollman J, Ridley K. Differences in body fatness, fat patterning and cardio-respiratory fitness between groups of Australian children formed on the basis of physical activity and television viewing guidelines. J Phys Act Health. 2006;3(2):191–199. [DOI] [PubMed] [Google Scholar]
- 39. Drenowatz C, Kobel S, Kettner S, et al. Interaction of sedentary behaviour, sports participation and fitness with weight status in elementary school children. Eur J Sport Sci. 2014;14(1):100–105. [DOI] [PubMed] [Google Scholar]
- 40. Maher C, Olds TS, Eisenmann JC, et al. Screen time is more strongly associated than physical activity with overweight and obesity in 9- to 16-year-old Australians. Acta Paediatr. 2012;101(11):1170–1174. [DOI] [PubMed] [Google Scholar]
- 41. Steele RM, Sluijs EMF, Cassidy A, et al. Targeting sedentary time or moderate- and vigorous-intensity activity: independent relations with adiposity in a population-based sample of 10-y-old British children. Am J Clin Nutr. 2009;90(5):1185–1192. [DOI] [PubMed] [Google Scholar]
- 42. Xi B, Wang C, Wu L, et al. Influence of physical inactivity on associations between single nucleotide polymorphisms and genetic predisposition to childhood obesity. Am J Epidemiol. 2011;173(11):1256–1262. [DOI] [PubMed] [Google Scholar]
- 43. Laurson KR, Eisenmann JC, Welk GJ, et al. Combined influence of physical activity and screen time recommendations on childhood overweight. J Pediatr. 2008;153(2):209–214. [DOI] [PubMed] [Google Scholar]
- 44. Loprinzi PD, Cardinal BJ, Lee H, et al. Markers of adiposity among children and adolescents: implications of the isotemporal substitution paradigm with sedentary behavior and physical activity patterns. J Diabetes Metab Disord. 2015;14:46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. De Bourdeaudhuij I, Verloigne M, Maes L, et al. Associations of physical activity and sedentary time with weight status among school-aged girls and boys across five European countries. J Sci Med Sport. 2012;15(suppl 1):S41–S41. [Google Scholar]
- 46. Hjorth MF, Chaput JP, Ritz C, et al. Fatness predicts decreased physical activity and increased sedentary time, but not vice versa: support from a longitudinal study in 8- to 11-year-old children. Int J Obes (Lond). 2014;38(7):959–965. [DOI] [PubMed] [Google Scholar]
- 47. Bai Y, Chen S, Laurson KR, et al. The associations of youth physical activity and screen time with fatness and fitness: the 2012 NHANES National Youth Fitness Survey. PLoS One. 2016;11(1):e0148038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Chaput JP, Saunders TJ, Mathieu MÈ, et al. Combined associations between moderate to vigorous physical activity and sedentary behaviour with cardiometabolic risk factors in children. Appl Physiol Nutr Metab. 2013;38(5):477–483. [DOI] [PubMed] [Google Scholar]
- 49. Spengler S, Mess F, Mewes N, et al. A cluster-analytic approach towards multidimensional health-related behaviors in adolescents: the MoMo-Study. BMC Public Health. 2012;12:1128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Lane A, Harrison M, Murphy N. Screen time increases risk of overweight and obesity in active and inactive 9-year-old Irish children: a cross sectional analysis. J Phys Act Health. 2014;11(5):985–991. [DOI] [PubMed] [Google Scholar]
- 51. Velde SJ, De Bourdeaudhuij I, Thorsdottir I, et al. Patterns in sedentary and exercise behaviors and associations with overweight in 9–14-year-old boys and girls—a cross-sectional study. BMC Public Health. 2007;7(1):16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Herman KM, Chaput JP. Combined physical activity/sedentary behavior associations with indices of adiposity in 8- to 10-year-old children. J Sci Med Sport. 2015;12(1):20–29. [DOI] [PubMed] [Google Scholar]
- 53. Herman K, Sabiston C, Mathieu M, et al. Active couch-potatoes? Combined physical activity–sedentary behaviour associations with weight status in 8–10 year old children [abstract]. J Sci Med Sport. 2012;15(suppl 1):S250. [Google Scholar]
- 54. Pérez A, Hoelscher DM, Springer AE, et al. Physical activity, watching television, and the risk of obesity in students, Texas, 2004–2005. Prev Chronic Dis. 2011;8(3):A61. [PMC free article] [PubMed] [Google Scholar]
- 55. Crowe M, Sampasa-Kanyinga H, Saunders TJ, et al. Combinations of physical activity and screen time recommendations and their association with overweight/obesity in adolescents. Can J Public Health. 2020;111:515–522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Dowd K, Harrington D, Hannigan A, et al. The development of activity profiles in adolescent females and their association with adiposity. Pediatr Exerc Sci. 2016;28(1):109. [DOI] [PubMed] [Google Scholar]
- 57. Wong SL, Leatherdale ST. Association between sedentary behavior, physical activity, and obesity: inactivity among active kids. Prev Chronic Dis. 2009;6(1):A26. [PMC free article] [PubMed] [Google Scholar]
- 58. Melkevik O, Torsheim T, Rasmussen M. Patterns of screen-based sedentary behavior and physical activity and associations with overweight among Norwegian adolescents: a latent profile approach. Nor Epidemiol. 2010;20(1):109–117. [Google Scholar]
- 59. Melkevik O, Haug E, Rasmussen M, et al. Are associations between electronic media use and BMI different across levels of physical activity? BMC Public Health. 2015;15:497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Pitanga FJG, Alves CFA, Pamponet ML, et al. Combined effect of physical activity and reduction of screen time for overweight prevention in adolescents. Rev Bras Cineantropom Desempenho Hum. 2019;21(3):e58392. [Google Scholar]
- 61. Eisenmann JC, Bartee RT, Smith DT, et al. Combined influence of physical activity and television viewing on the risk of overweight in US youth. Int J Obes (Lond). 2008;32(4):613–618. [DOI] [PubMed] [Google Scholar]
- 62. Heshmat R, Qorbani M, Shahr Babaki AE, et al. Joint association of screen time and physical activity with cardiometabolic risk factors in a national sample of Iranian adolescents: the CASPIANIII Study. PLoS One. 2016;11(5):e0154502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Patnode CD, Lytle LA, Erickson DJ, et al. Physical activity and sedentary activity patterns among children and adolescents: a latent class analysis approach. J Phys Act Health. 2011;8(4):457–467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Rendo-Urteaga T, Moraes ACF, Collese TS, et al. The combined effect of physical activity and sedentary behaviors on a clustered cardio-metabolic risk score: the Helena Study. Int J Cardiol. 2015;186:186–195. [DOI] [PubMed] [Google Scholar]
- 65. Kim Y, Barreira TV, Kang M. Concurrent associations of physical activity and screen-based sedentary behavior on obesity among US adolescents: a latent class analysis. J Epidemiol. 2016;26(3):137–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Pérez-Rodrigo C, Gil Á, González-Gross M, et al. Clustering of dietary patterns, lifestyles, and overweight among Spanish children and adolescents in the ANIBES Study. Nutrients. 2015;8(1):11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Parker KE, Salmon J, Brown HL, et al. Typologies of adolescent activity related health behaviours. J Sci Med Sport. 2019;22(3):319–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Herman KM, Sabiston CM, Mathieu ME, et al. Sedentary behavior in a cohort of 8- to 10-year-old children at elevated risk of obesity. Prev Med. 2014;60:115–120. [DOI] [PubMed] [Google Scholar]
- 69. Monda KL, Popkin BM. Cluster analysis methods help to clarify the activity–BMI relationship of Chinese youth. Obes Res. 2005;13(6):1042–1051. [DOI] [PubMed] [Google Scholar]
- 70. Marques A, Santos R, Ekelund ULF, et al. Association between physical activity, sedentary time, and healthy fitness in youth. Med Sci Sports Exerc. 2015;47(3):575–580. [DOI] [PubMed] [Google Scholar]
- 71. Katzmarzyk PT, Barreira TV, Broyles ST, et al. Physical activity, sedentary time, and obesity in an international sample of children. Med Sci Sports Exerc. 2015;47(10):2062–2069. [DOI] [PubMed] [Google Scholar]
- 72. Ekelund U, Luan J, Sherar LB, et al. Moderate to vigorous physical activity and sedentary time and cardiometabolic risk factors in children and adolescents. JAMA. 2012;307(7):704–712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Sisson SB, Broyles ST, Baker BL, et al. Screen time, physical activity, and overweight in U.S. youth: National Survey of Children’s Health 2003. J Adolesc Health Care. 2010;47(3):309–311. [DOI] [PubMed] [Google Scholar]
- 74. Mielke GI, Brown WJ, Wehrmeister FC, et al. Associations between self-reported physical activity and screen time with cardiometabolic risk factors in adolescents: findings from the 1993 Pelotas (Brazil) Birth Cohort Study. Prev Med. 2019;119:31–36. [DOI] [PubMed] [Google Scholar]
- 75. Bergmann GG, Tassitano RM, Araújo Bergmann ML, et al. Screen time, physical activity and cardiovascular risk factors in adolescents. Rev Bras Atividade Fís Saúde. 2018;23:1–12. [Google Scholar]
- 76. Faria FR, Neves Miranda VP, Howe CA, et al. Behavioral classes related to physical activity and sedentary behavior on the evaluation of health and mental outcomes among Brazilian adolescents. PLoS One. 2020;15(6):e0234374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Dalene KE, Anderssen SA, Andersen LB, et al. Cross-sectional and prospective associations between physical activity, body mass index and waist circumference in children and adolescents. Obes Sci Pract. 2017;3(3):249–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Sardinha LB, Marques A, Minderico C, et al. Cross-sectional and prospective impact of reallocating sedentary time to physical activity on children’s body composition. Pediatr Obes. 2017;12(5):373–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Aggio D, Smith L, Hamer M. Effects of reallocating time in different activity intensities on health and fitness: a cross sectional study. Int J Behav Nutr Phys Act. 2015;12:83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Collings PJ, Westgate K, Väistö J, et al. Cross-sectional associations of objectively-measured physical activity and sedentary time with body composition and cardiorespiratory fitness in mid-childhood: the PANIC Study. Sports Med. 2017;47(4):769–780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Hansen BH, Anderssen SA, Andersen LB, et al. Cross-sectional associations of reallocating time between sedentary and active behaviours on cardiometabolic risk factors in young people: an International Children’s Accelerometry Database (ICAD) analysis. Sports Med. 2018;48(10):2401–2412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Jones MA, Skidmore PM, Stoner L, et al. Associations of accelerometer-measured sedentary time, sedentary bouts, and physical activity with adiposity and fitness in children. J Sports Sci. 2020;38(1):114–120. [DOI] [PubMed] [Google Scholar]
- 83. Gába A, Pedišić Ž, Štefelová N, et al. Sedentary behavior patterns and adiposity in children: a study based on compositional data analysis. BMC Pediatr. 2020;20(1):147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Fairclough SJ, Dumuid D, Mackintosh KA, et al. Adiposity, fitness, health-related quality of life and the reallocation of time between children’s school day activity behaviours: a compositional data analysis. Prev Med Rep. 2018;11:254–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Carson V, Tremblay MS, Chaput JP, et al. Compositional analyses of the associations between sedentary time, different intensities of physical activity, and cardiometabolic biomarkers among children and youth from the United States. PLoS One. 2019;14(7):e0220009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Moura BP, Rufino RL, Faria RC, et al. Effects of isotemporal substitution of sedentary behavior with light-intensity or moderate-to-vigorous physical activity on cardiometabolic markers in male adolescents. PLoS One. 2019;14(11):e0225856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Chaput JP, Leduc G, Boyer C, et al. Objectively measured physical activity, sedentary time and sleep duration: independent and combined associations with adiposity in Canadian children. Nutr Diabetes. 2014;4:e117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Chen ST, Liu Y, Tremblay MS, et al. Meeting 24-hour movement guidelines: prevalence, correlates and the relationships with overweight and obesity among Chinese children and adolescents. J Sport Health Sci. 2020;10(3):349–359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Carson V, Chaput JP, Janssen I, et al. Health associations with meeting new 24-hour movement guidelines for Canadian children and youth. Prev Med. 2017;95:7–13. [DOI] [PubMed] [Google Scholar]
- 90. Jakubec L, Gába A, Dygrýn J, et al. Is adherence to the 24-hour movement guidelines associated with a reduced risk of adiposity among children and adolescents? BMC Public Health. 2020;20(1):1119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Zhu X, Healy S, Haegele JA, et al. Twenty-four-hour movement guidelines and body weight in youth. J Pediatr. 2020;218:204–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Roman-Viñas B, Chaput JP, Katzmarzyk PT, et al. Proportion of children meeting recommendations for 24-hour movement guidelines and associations with adiposity in a 12-country study. Int J Behav Nutr Phys Act. 2016;13:123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Tanaka C, Tremblay MS, Okuda M, et al. Proportion of Japanese primary school children meeting recommendations for 24-h movement guidelines and associations with weight status. Obes Res Clin Pract. 2020;14(3):234–240. [DOI] [PubMed] [Google Scholar]
- 94. Wilkie HJ, Standage M, Gillison FB, et al. Multiple lifestyle behaviours and overweight and obesity among children aged 9–11 years: results from the UK site of the International Study of Childhood Obesity, Lifestyle and the Environment. BMJ Open. 2016;6(2):e010677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Guan H, Zhang Z, Wang B, et al. Proportion of kindergarten children meeting the WHO guidelines on physical activity, sedentary behaviour and sleep and associations with adiposity in urban Beijing. BMC Pediatr. 2020;20(1):70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Laurson KR, Lee JA, Gentile DA, et al. Concurrent associations between physical activity, screen time, and sleep duration with childhood obesity. ISRN Obes. 2014;2014:204540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Yan S, Yajun Huang W, Hui-Ping Sit C, et al. Compliance with 24-hour movement guidelines in Hong Kong adolescents: associations with weight status. J Phys Act Health. 2020;17(3):287–292. [DOI] [PubMed] [Google Scholar]
- 98. Tassitano RM, Weaver RG, Tenório MCM, et al. Clusters of non-dietary obesogenic behaviors among adolescents in Brazil: a latent profile analysis. Int J Public Health. 2020;65(6):881–891. [DOI] [PubMed] [Google Scholar]
- 99. Carson V, Faulkner G, Sabiston CM, et al. Patterns of movement behaviors and their association with overweight and obesity in youth. Int J Public Health. 2015;60(5):551–559. [DOI] [PubMed] [Google Scholar]
- 100. Janssen I, Roberts KC, Thompson W. Is adherence to the Canadian 24-Hour Movement Behaviour Guidelines for Children and Youth associated with improved indicators of physical, mental, and social health? Appl Physiol Nutr Metab. 2017;42(7):725–731. [DOI] [PubMed] [Google Scholar]
- 101. Verswijveren SJJM, Lamb KE, Martín-Fernández JA, et al. Using compositional data analysis to explore accumulation of sedentary behavior, physical activity and youth health. J Sport Health Sci. 2020;11(2):234–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Fairclough SJ, Dumuid D, Taylor S, et al. Fitness, fatness and the reallocation of time between children’s daily movement behaviours: an analysis of compositional data. Int J Behav Nutr Phys Act. 2017;14:64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Dumuid D, Wake M, Clifford S, et al. The association of the body composition of children with 24-hour activity composition. J Pediatr. 2019;208:43–49.e9. [DOI] [PubMed] [Google Scholar]
- 104. Talarico R, Janssen I. Compositional associations of time spent in sleep, sedentary behavior and physical activity with obesity measures in children. Int J Obes (Lond). 2018;42(8):1508–1514. [DOI] [PubMed] [Google Scholar]
- 105. Taylor RW, Haszard JJ, Farmer VL, et al. Do differences in compositional time use explain ethnic variation in the prevalence of obesity in children? Analyses using 24-hour accelerometry. Int J Obes (Lond). 2020;44(1):94–103. [DOI] [PubMed] [Google Scholar]
- 106. Del Pozo-Cruz B, Gant N, Del Pozo-Cruz J, et al. Relationships between sleep duration, physical activity and body mass index in young New Zealanders: an isotemporal substitution analysis. PLoS One. 2017;12(9):e0184472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Huang WY, Wong SHS, He G, et al. Isotemporal substitution analysis for sedentary behavior and body mass index. Med Sci Sports Exerc. 2016;48(11):2135–2141. [DOI] [PubMed] [Google Scholar]
- 108. Carson V, Tremblay MS, Chaput JP, et al. Associations between sleep duration, sedentary time, physical activity, and health indicators among Canadian children and youth using compositional analyses. Appl Physiol Nutr Metab. 2016;41(6 suppl 3):S294–S302. [DOI] [PubMed] [Google Scholar]
- 109. Dumuid D, Stanford TE, Martin-Fernández JA, et al. Compositional data analysis for physical activity, sedentary time and sleep research. Stat Methods Med Res. 2018;27(12):3726–3738. [DOI] [PubMed] [Google Scholar]
- 110. Väistö J, Eloranta AM, Viitasalo A, et al. Physical activity and sedentary behaviour in relation to cardiometabolic risk in children: cross-sectional findings from the Physical Activity and Nutrition in Children (PANIC) Study. Int J Behav Nutr Phys Act. 2014;11:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Moraes ACF, Carvalho HB, Rey-López JP, et al. Independent and combined effects of physical activity and sedentary behavior on blood pressure in adolescents: gender differences in two cross-sectional studies. PLoS One. 2013;8(5):e62006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Cristi-Montero C, Chillón P, Labayen I. Cardiometabolic risk through an integrative classification combining physical activity and sedentary behavior in European adolescents: HELENA Study. J Sport Health Sci. 2019;8(1):55–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Agostinis-Sobrinho C, Gómez-Martínez S, Nova E, et al. Lifestyle patterns and endocrine, metabolic, and immunological biomarkers in European adolescents: the HELENA Study. Pediatr Diabetes. 2018;18:543. [DOI] [PubMed] [Google Scholar]
- 114. Weisser B, Hacke C. Screen time is a risk factor for higher exercise blood pressure independent of moderate-to-vigorous physical activity or fitness in adolescents. Eur Heart J. 2015;36:469–470.25336223 [Google Scholar]
- 115. Cureau FV, Ekelund U, Bloch KV, et al. Does body mass index modify the association between physical activity and screen time with cardiometabolic risk factors in adolescents? Findings from a country-wide survey. Int J Obes (Lond). 2017;41(4):551–559. [DOI] [PubMed] [Google Scholar]
- 116. Lee PH. Association between adolescents’ physical activity and sedentary behaviors with change in BMI and risk of type 2 diabetes. PLoS One. 2014;9(10):e110732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Jones PR, Rajalahti T, Resaland GK, et al. Associations of physical activity and sedentary time with lipoprotein subclasses in Norwegian schoolchildren: the Active Smarter Kids (ASK) Study. Atherosclerosis. 2019;288:186–193. [DOI] [PubMed] [Google Scholar]
- 118. Mota J, Silva-Santos S, Barros M, et al. Influence of different behavioural factors and obesity status on systolic blood pressure among pre-school children. Ann Hum Biol. 2014;41(6):506–510. [DOI] [PubMed] [Google Scholar]
- 119. Santos DA, Marques A, Minderico CS, et al. A cross-sectional and prospective analysis of reallocating sedentary time to physical activity on children’s cardiorespiratory fitness. J Sports Sci. 2018;36(15):1720–1726. [DOI] [PubMed] [Google Scholar]
- 120. Sun Y, Yin X, Li Y, et al. Isotemporal substitution of sedentary behavior for physical activity on cardiorespiratory fitness in children and adolescents. Medicine (Baltimore). 2020;99(30):e21367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Kidokoro T, Suzuki K, Naito H, et al. Moderate-to-vigorous physical activity attenuates the detrimental effects of television viewing on the cardiorespiratory fitness in Asian adolescents: the Asia-Fit Study. BMC Public Health. 2019;19(1):1737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Porter AK, Matthews KJ, Salvo D, et al. Associations of physical activity, sedentary time, and screen time with cardiovascular fitness in United States adolescents: results from the NHANES National Youth Fitness Survey. J Phys Act Health. 2017;14(7):506–512. [DOI] [PubMed] [Google Scholar]
- 123. Moore JB, Beets MW, Barr-Anderson DJ, et al. Sedentary time and vigorous physical activity are independently associated with cardiorespiratory fitness in middle school youth. J Sports Sci. 2013;31(14):1520–1525. [DOI] [PubMed] [Google Scholar]
- 124. Santos R, Mota J, Okely AD, et al. The independent associations of sedentary behaviour and physical activity on cardiorespiratory fitness. Br J Sports Med. 2014;48(20):1508–1512. [DOI] [PubMed] [Google Scholar]
- 125. Martinez-Gomez D, Ortega FB, Ruiz JR, et al. Excessive sedentary time and low cardiorespiratory fitness in European adolescents: the HELENA Study. Arch Dis Child. 2011;96(3):240–246. [DOI] [PubMed] [Google Scholar]
- 126. Tanaka C, Tremblay MS, Okuda M, et al. Association between 24-hour movement guidelines and physical fitness in children. Pediatr Int. 2020;62(12):1381–1387. [DOI] [PubMed] [Google Scholar]
- 127. Sánchez-Oliva D, Esteban-Cornejo I, Padilla-Moledo C, et al. Associations between physical activity and sedentary time profiles transitions and changes in well-being in youth: the UP&DOWN longitudinal study. Psychol Sport Exerc. 2020;47:101558. [Google Scholar]
- 128. Pozo-Cruz B, Perales F, Parker P, et al. Joint physical-activity/screen-time trajectories during early childhood: socio-demographic predictors and consequences on health-related quality-of-life and socio-emotional outcomes. Int J Behav Nutr Phys Act. 2019;16:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. García-Hermoso A, Hormazábal-Aguayo I, Fernández-Vergara O, et al. Physical activity, screen time and subjective well-being among children. Int J Clin Health Psychol. 2020;20(2):126–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Matin N, Kelishadi R, Heshmat R, et al. Joint association of screen time and physical activity on self-rated health and life satisfaction in children and adolescents: the CASPIAN-IV Study. Int Health. 2017;9(1):58–68. [DOI] [PubMed] [Google Scholar]
- 131. Taheri E, Heshmat R, Esmaeil Motlagh M, et al. Association of physical activity and screen time with psychiatric distress in children and adolescents: CASPIAN-IV Study. J Trop Pediatr. 2019;65(4):361–372. [DOI] [PubMed] [Google Scholar]
- 132. Hamer M, Stamatakis E, Mishra G. Psychological distress, television viewing, and physical activity in children aged 4 to 12 years. Pediatrics. 2009;123(5):1263–1268. [DOI] [PubMed] [Google Scholar]
- 133. Khan A, Uddin R, Burton NW. Insufficient physical activity in combination with high screen time is associated with adolescents’ psychosocial difficulties. Int Health. 2018;10(4):246–251. [DOI] [PubMed] [Google Scholar]
- 134. Keane E, Kelly C, Molcho M, et al. Physical activity, screen time and the risk of subjective health complaints in school-aged children. Prev Med. 2017;96:21–27. [DOI] [PubMed] [Google Scholar]
- 135. Omorou AY, Langlois J, Lecomte E, et al. Cumulative and bidirectional association of physical activity and sedentary behaviour with health-related quality of life in adolescents. Qual Life Res. 2016;25(5):1169–1178. [DOI] [PubMed] [Google Scholar]
- 136. Wong M, Olds T, Gold L, et al. Time-use patterns and health-related quality of life in adolescents. Pediatrics. 2017;140(1):e20163656. [DOI] [PubMed] [Google Scholar]
- 137. Motamed-Gorji N, Qorbani M, Nikkho F, et al. Association of screen time and physical activity with health-related quality of life in Iranian children and adolescents. Health Qual Life Outcomes. 2019;17(1):2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138. Werneck AO, Collings PJ, Barboza LL, et al. Associations of sedentary behaviors and physical activity with social isolation in 100,839 school students: the Brazilian Scholar Health Survey. Gen Hosp Psychiatry. 2019;59:7–13. [DOI] [PubMed] [Google Scholar]
- 139. Lacy KE, Allender SE, Kremer PJ, et al. Screen time and physical activity behaviours are associated with health-related quality of life in Australian adolescents. Qual Life Res. 2012;21(6):1085–1099. [DOI] [PubMed] [Google Scholar]
- 140. Sampasa-Kanyinga H, Standage M, Tremblay MS, et al. Associations between meeting combinations of 24-h movement guidelines and health-related quality of life in children from 12 countries. Public Health. 2017;153:16–24. [DOI] [PubMed] [Google Scholar]
- 141. Cao H, Qian Q, Weng T, et al. Screen time, physical activity and mental health among urban adolescents in China. Prev Med. 2011;53(4-5):316–320. [DOI] [PubMed] [Google Scholar]
- 142. Sampasa-Kanyinga H, Chaput JP, Goldfield GS, et al. 24-hour movement guidelines and suicidality among adolescents. J Affect Disord. 2020;274:372–380. [DOI] [PubMed] [Google Scholar]
- 143. Trinh L, Wong B, Faulkner GE. The independent and interactive associations of screen time and physical activity on mental health, school connectedness and academic achievement among a population-based sample of youth. J Can Acad Child Adolesc Psychiatry. 2015;24(1):17–24. [PMC free article] [PubMed] [Google Scholar]
- 144. Uddin R, Burton NW, Maple M, et al. Low physical activity and high sedentary behaviour are associated with adolescents’ suicidal vulnerability: evidence from 52 low- and middle-income countries. Acta Paediatr. 2020;109(6):1252–1259. [DOI] [PubMed] [Google Scholar]
- 145. Hrafnkelsdottir SM, Brychta RJ, Rognvaldsdottir V, et al. Less screen time and more frequent vigorous physical activity is associated with lower risk of reporting negative mental health symptoms among Icelandic adolescents. PLoS One. 2018;13(4):e0196286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146. Liu M, Zhang J, Hu E, et al. Combined patterns of physical activity and screen-related sedentary behavior among Chinese adolescents and their correlations with depression, anxiety and self-injurious behaviors. Psychol Res Behav Manag. 2019;12:1041–1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147. Zhu X, Haegele JA, Healy S. Movement and mental health: behavioral correlates of anxiety and depression among children of 6–17 years old in the U.S. Ment Health Phys Act. 2019;16:60–65. [Google Scholar]
- 148. Gillis BT, El-Sheikh M. Sleep and adjustment in adolescence: physical activity as a moderator of risk. Sleep Health. 2019;5(3):266–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149. Cao R, Gao T, Hu Y, et al. Clustering of lifestyle factors and the relationship with depressive symptoms among adolescents in northeastern China. J Affect Disord. 2020;274:704–710. [DOI] [PubMed] [Google Scholar]
- 150. Ogawa S, Kitagawa Y, Fukushima M, et al. Interactive effect of sleep duration and physical activity on anxiety/depression in adolescents. Psychiatry Res. 2019;273:456–460. [DOI] [PubMed] [Google Scholar]
- 151. Ishii K, Aoyagi K, Shibata A, et al. Joint associations of leisure screen time and physical activity with academic performance in a sample of Japanese children. Int J Environ Res Public Health. 2020;17(3):757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152. García-Hermoso A, Marina R. Relationship of weight status, physical activity and screen time with academic achievement in adolescents. Obes Res Clin Pract. 2017;11(1):44–50. [DOI] [PubMed] [Google Scholar]
- 153. Kantomaa MT, Stamatakis E, Kankaanpää A, et al. Associations of physical activity and sedentary behavior with adolescent academic achievement. J Res Adolesc. 2016;26(3):432–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154. Haapala EA, Väistö J, Lintu N, et al. Physical activity and sedentary time in relation to academic achievement in children. J Sci Med Sport. 2017;20(6):583–589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155. Dumuid D, Olds T, Martín-Fernández JA, et al. Academic performance and lifestyle behaviors in Australian school children: a cluster analysis. Health Educ Behav. 2017;44(6):918–927. [DOI] [PubMed] [Google Scholar]
- 156. Wilson R, Dumuid D, Olds T, et al. Lifestyle clusters and academic achievement in Australian indigenous children: empirical findings and discussion of ecological levers for closing the gap. SSM Popul Health. 2020;10:100535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157. Maher C, Lewis L, Katzmarzyk PT, et al. The associations between physical activity, sedentary behaviour and academic performance. J Sci Med Sport. 2016;19(12):1004–1009. [DOI] [PubMed] [Google Scholar]
- 158. Lien A, Sampasa-Kanyinga H, Colman I, et al. Adherence to 24-hour movement guidelines and academic performance in adolescents. Public Health. 2020;183:8–14. [DOI] [PubMed] [Google Scholar]
- 159. Zeng X, Cai L, Wong SHS, et al. Association of sedentary time and physical activity with executive function among children. Acad Pediatr. 2020;21(1):63–69. [DOI] [PubMed] [Google Scholar]
- 160. Guerrero MD, Barnes JD, Walsh JJ, et al. 24-hour movement behaviors and impulsivity. Pediatrics. 2019;144(3):e20190187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161. Walsh JJ, Barnes JD, Cameron JD, et al. Associations between 24 hour movement behaviours and global cognition in US children: a cross-sectional observational study. Lancet Child Adolesc Health. 2018;2(11):783–791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161. Walsh JJ, Barnes JD, Tremblay MS, et al. Associations between duration and type of electronic screen use and cognition in US children. Comput Human Behav. 2020;108:106312. [Google Scholar]
- 163. Wang S, Song J, Shang X, et al. Physical activity and sedentary behavior can modulate the effect of the PNPLA3 variant on childhood NAFLD: a case-control study in a Chinese population. BMC Med Genet. 2016;17(1):90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164. Burns RD, Youngwon K, Wonwoo B, et al. Associations of school day sedentary behavior and physical activity with gross motor skills: use of compositional data analysis. J Phys Act Health. 2019;16(10):811–817. [DOI] [PubMed] [Google Scholar]
- 165. Silva ACM, Cureau FV, Oliveira CL, et al. Physical activity but not sedentary time is associated with vitamin D status in adolescents: Study of Cardiovascular Risk in Adolescents (ERICA). Eur J Clin Nutr. 2019;73(3):432–440. [DOI] [PubMed] [Google Scholar]
- 166. Vicente-Rodríguez G, Ortega FB, Rey-López JP, et al. Extracurricular physical activity participation modifies the association between high TV watching and low bone mass. Bone. 2009;45(5):925–930. [DOI] [PubMed] [Google Scholar]
- 167. Wu YUE, Goodrich JM, Dolinoy DC, et al. Accelerometer-measured physical activity, reproductive hormones, and DNA methylation. Med Sci Sports Exerc. 2020;52(3):598–607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168. Kieling C, Kieling RR, Rohde LA, et al. The age at onset of attention deficit hyperactivity disorder. Am J Psychiatry. 2010;167(1):14–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169. Fletcher EA, McNaughton SA, Crawford D, et al. Associations between sedentary behaviours and dietary intakes among adolescents. Public Health Nutr. 2018;21(6):1115–1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170. Carson V, Hunter S, Kuzik N, et al. Systematic review of physical activity and cognitive development in early childhood. J Sci Med Sport. 2016;19(7):573–578. [DOI] [PubMed] [Google Scholar]
- 171. Aggio D, Smith L, Fisher A, et al. Context-specific associations of physical activity and sedentary behavior with cognition in children. Am J Epidemiol. 2016;183(12):1075–1082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172. Hartwig TB, Sanders T, Vasconcellos D. School-based interventions modestly increase physical activity and cardiorespiratory fitness but are least effective for youth who need them most: an individual participant pooled analysis of 20 controlled trials. Br J Sports Med. 2021;55(13):721–729. [DOI] [PubMed] [Google Scholar]
- 173. Bowling A, Slavet J, Miller DP, et al. Dose-response effects of exercise on behavioral health in children and adolescents. Ment Health Phys Act. 2017;12:110–115. [Google Scholar]
- 174. Liu M, Wu L, Yao S. Dose-response association of screen time-based sedentary behaviour in children and adolescents and depression: a meta-analysis of observational studies. Br J Sports Med. 2016;50(20):1252–1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175. Collins H, Booth JN, Duncan A, et al. The effect of resistance training interventions on “the self” in youth: a systematic review and meta-analysis. Sports Med Open. 2019;5(1):1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176. Behm DG, Faigenbaum AD, Falk B, et al. Canadian Society for Exercise Physiology position paper: resistance training in children and adolescents. Appl Physiol Nutr Metab. 2008;33(3):547–561. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.