Abstract
Purpose:
Our goal was to test transcutaneous focused ultrasound in the form of ultrasonic propulsion and burst wave lithotripsy to reposition ureteral stones and facilitate passage in awake subjects.
Materials and Methods:
Adult subjects with a diagnosed proximal or distal ureteral stone were prospectively recruited. Ultrasonic propulsion alone or with burst wave lithotripsy was administered by a handheld transducer to awake, unanesthetized subjects. Efficacy outcomes included stone motion, stone passage, and pain relief. Safety outcome was the reporting of associated anticipated or adverse events.
Results:
Twenty-nine subjects received either ultrasonic propulsion alone (n = 16) or with burst wave lithotripsy bursts (n = 13), and stone motion was observed in 19 (66%). The stone passed in 18 (86%) of the 21 distal ureteral stone cases with at least 2 weeks follow-up in an average of 3.9±4.9 days post-procedure. Fragmentation was observed in 7 of the burst wave lithotripsy cases. All subjects tolerated the procedure with average pain scores (0–10) dropping from 2.1±2.3 to 1.6±2.0 (P = .03). Anticipated events were limited to hematuria on initial urination post-procedure and mild pain. In total, 7 subjects had associated discomfort with only 2.2% (18 of 820) propulsion bursts.
Conclusions:
This study supports the efficacy and safety of using ultrasonic propulsion and burst wave lithotripsy in awake subjects to reposition and break ureteral stones to relieve pain and facilitate passage.
Keywords: calculi, lithotripsy, urolithiasis, ultrasound
JU Insight
Study Need and Importance:
Our goal was to test transcutaneous focused ultrasound in the form of ultrasonic propulsion and burst wave lithotripsy (BWL) to reposition ureteral stones and facilitate passage in awake subjects.
What We Found:
Adult subjects with a diagnosed Adult subjects with a diagnosed proximal or distal ureteral stone were prospectively recruited. Ultrasonic propulsion alone or with BWL was administered by a handheld transducer to awake, unanesthetized subjects. Twenty-nine subjects received either ultrasonic propulsion alone (n = 16) or with BWL bursts (n = 13), and stone motion was observed in 19 (66%), including 2 where the stone was repositioned into the bladder. The stone passed in 18 (86%) of the 21 distal ureteral stone cases with at least 2 weeks follow-up in an average of 3.9±4.9 days post-procedure (see Table). Fragmentation was observed in 7 of the BWL cases. All subjects tolerated the procedure with average pain scores (0–10) dropping from 2.1±2.3 to 1.6±2.0 (P = .03). Anticipated events were limited to hematuria on initial urination post-procedure and mild pain. In total, 7 subjects had associated discomfort in only 18 of 820 propulsion bursts.
Limitations:
There was no control group for passage rate, although our subjects passed stones at a higher rate than might be expected. The American Urological Association guidelines quote a stone passage rate of 54% for distal ureteral stones smaller than 10 mm based on meta-analyses of 1,205 subjects in 27 studies mostly following for 2 weeks after presentation.
Interpretation for Patient Care:
This study supports the efficacy and safety of using ultrasonic propulsion and BWL to reposition and break ureteral stones, potentially relieving pain and facilitating passage in awake patients. This technology has the potential to provide an advantageous and patient-centered solution for the gap between expectant management and urological intervention for ureteral stones.
Ureteral stones are associated with anxiety and severe pain. Patients with urinary stones frequently present in the emergency department (ED) with over 1.5 million visits per year in the U.S. alone.1,2 Most ureteral stones are initially managed by observation with a trial of spontaneous passage. Observation can last for weeks, and an average of 23% of patients will require surgery.3 Some studies have found that management focuses on decompressing the kidney rather than definitive management, which prolongs the patient’s experience with the stone.3
This study addresses the unmet need for nonsurgical definitive management of ureteral stones at the point-of-care by developing a clinic-based ultrasound system to image, break, and reposition stones and fragments to facilitate their natural clearance.4 The system includes 2 technologies: ultrasonic propulsion to reposition stones and burst wave lithotripsy (BWL) to break or dislodge stones. Both technologies use harmonic bursts of ultrasound and are delivered transcutaneously using the same probe with real-time ultrasound image guidance and targeting. Ultrasonic propulsion pulses have longer duration and lower amplitude than BWL pulses.
A stepwise progression of development and human trials has ensued.5–9 The present study focused on treating distal and proximal ureteral stones, with emphasis on facilitating passage of distal stones into the bladder and pushing proximal stones back into the kidney. Distal ureteral stones are more common than proximal ureteral stones; both are more common and more reliably visualized with ultrasound than middle ureteral stones.10,11 This paper reports on the first human feasibility study of these technologies to reposition ureteral stones and the first application of BWL in awake unanesthetized subjects.
METHODS
Trial Oversight
This was a prospective, nonrandomized convenience sample examining the feasibility and safety of an investigational therapeutic ultrasound device to reposition ureteral stones among awake adult patients.12 The study was approved by the University of Washington Institutional Review Board (IRB no. STUDY00002746) and the U.S. Food and Drug Administration through an investigational device exemption (ClinicalTrials.gov identifier NCT02028559). Recruitment was conducted at a single urban academic institution.
Subject Population
The recruitment population consisted of adult subjects presenting to the ED or endourology clinic with a proximal or distal ureteral stone on a clinical imaging examination from which the clinical radiologist reported the stone size. Exclusion criteria included members of a vulnerable group, non-English speakers, and those patients on dialysis, with signs of sepsis, with a transplant or solitary kidney, exhibiting bilateral hydronephrosis, or whom the clinical team considered to be at high risk for a serious alternate diagnosis. Recruited subjects could undergo the investigational procedure only once.
Trial Procedures
Informed consent was obtained. A urinalysis with reflex culture and pregnancy test, as appropriate, was performed. A screening ultrasound with the investigational device was performed; subjects were excluded if an unobstructed view of the stone in the focal zone could not be obtained. Awake and unanesthetized subjects then underwent the investigational procedure by trained members of the research team, any of 3 sonographers, 3 endourologists, 2 endourology fellows, and 2 emergency medicine physicians. The operator held the transducer on the subject’s skin, aligned the stone with the focus indicator using the real-time ultrasound image guidance, which was recorded, and delivered individual bursts no longer than 3 seconds at a time for ultrasonic propulsion and 30 seconds for BWL for up to a total of 10 minutes exposure time (Fig. 1).
Figure 1.
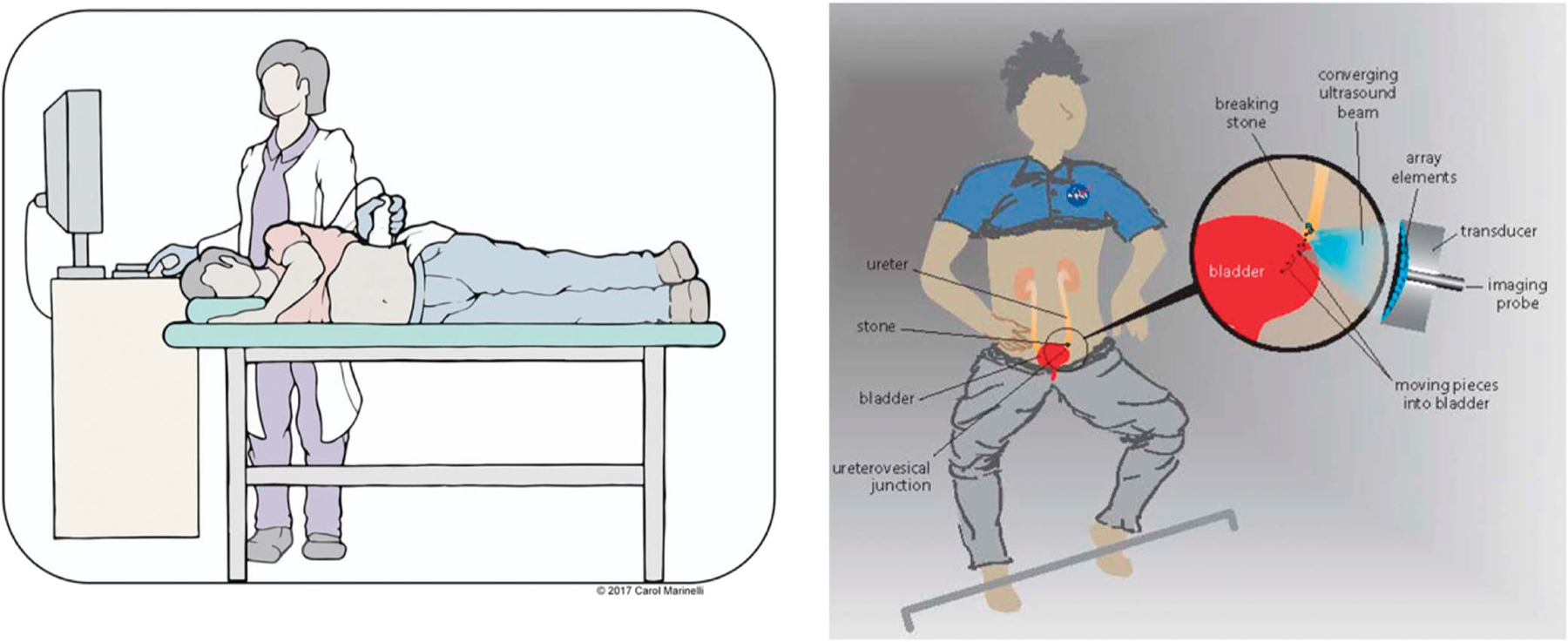
Procedure diagrams of use in the ED or clinic as performed in this study (left) and as envisioned by our National Aeronautics and Space Administration sponsors for use in space travel (right). Courtesy of Carol Marinelli and Kim Reading.
The maximum acoustic exposures for BWL and ultrasonic propulsion measured are listed in Table 1.12.13 The transducer and subject position were varied with ultrasonic propulsion as the force is unidirectional, away from the probe. BWL subjects were treated supine, but the skin-to-stone distance was more restricted to achieve the higher BWL pressure levels.12,13 BWL was added after Subject #10, and thereafter was only included if the skin-to-stone distance on ultrasound was less than 8 cm. The operator paused the procedure if echogenicity was seen extending from the stone into the tissue as our interpretation is such echogenicity is caused by cavitation bubbles which can shield the stone from effective energy delivery and injure the tissue.14,15
Table 1.
Maximum Free-Field Acoustic Exposures for Ultrasonic Propulsion and BWL
| Ultrasound Therapy | Peak Neg Pressure (MPa) | Pulse Duration (ms) | Pulse Repetition Rate (Hz) | Burst Duration (s) | Total Exposure (min) |
|---|---|---|---|---|---|
| Ultrasonic propulsion | 2.4 | 25 | 20 | 3 | 10 |
| BWL | 7 | 0.1 | 17 | 30 |
Abbreviation: BWL, burst wave lithotripsy.
Subjects were asked to describe and score their pain on a visual analog scale of 0 (no pain) to 10 (maximum pain level) before and after the investigational procedure, and for any discomfort following each ultrasound burst. The skin at the location of the transducer was observed for injury and photographed before and after the procedure. The study could end before the full ultrasound exposure if the stone was moved into the kidney (proximal ureteral stone) or bladder (distal ureteral stone), or it was determined by the study team that additional ultrasound exposure would have no further clinical benefit. The study could also be stopped if requested by the subject.
Anticipated and adverse events and stone passage were identified by weekly subject contact for 3 weeks post-procedure and follow-up imaging and review of the electronic health record within 90 days. Subjects were asked to affirm or deny a list of 12 anticipated events based on events associated with stones and reported for shock wave lithotripsy, which included hematuria and renal colic.16 If clinical imaging–CT, plain film x-ray, or ultrasound–was not obtained earlier, a clinical ultrasound examination was obtained 6 weeks after the procedure.
Outcomes
The primary efficacy outcome was stone motion assessed in the recorded ultrasound videos by a radiologist blinded to the exposure conditions. In making the assessment of direct stone motion, the radiologist differentiated and tabulated peristaltic motion–dilation and contraction of the ureter near the stone–and ureteral jets that occurred at least twice during or within 1 second after the therapy burst as well as fragmentation and transient changes in echogenicity around the stone during the burst, which were associated with motion of microbubbles. The secondary efficacy outcome of stone passage was evaluated among a subgroup of subjects with distal ureteral stones and at least 2 weeks of follow-up. Evidence of passage included stone passage reported by the subject confirmed by absence of the stone in the ureter on subsequent imaging. Subjects who went to scheduled surgery within 2 weeks, proximal ureteral subjects, and subjects lost to follow-up were excluded from this subgroup analysis. Change in pain was measured as described above. The safety outcome consisted of anticipated or adverse events associated with the investigational device or procedure, as adjudicated by the Principal Investigator and Data Safety Monitoring Board.
Statistical Analysis
Results were tabulated, and descriptive statistics were used to compare intra-subject pain scores before and after the investigational procedure. The Student’s t test was used, and significance was confirmed by a Wilcoxon’s signed rank test. Correlation was assessed between visible stone motion, ureteral peristalsis, and cases of stone passage.
RESULTS
Characteristics of the Population
Fifty-five subjects were consented for this study from May 2017 to October 2021. Recruitment was paused between March and August 2019 to gain approval for more subjects, photography of the skin, and BWL outputs and between March and October 2020 because of COVID-19 pandemic restriction. Timing of recruitment and procedure ranged from day zero in the ED to after a trial of passage more than a month later on the day before surgery. Twenty-six subjects failed the screening ultrasound; 29 subjects underwent the investigational procedure (Fig. 2). Twenty-one subjects were included in stone passage analysis.
Figure 2.
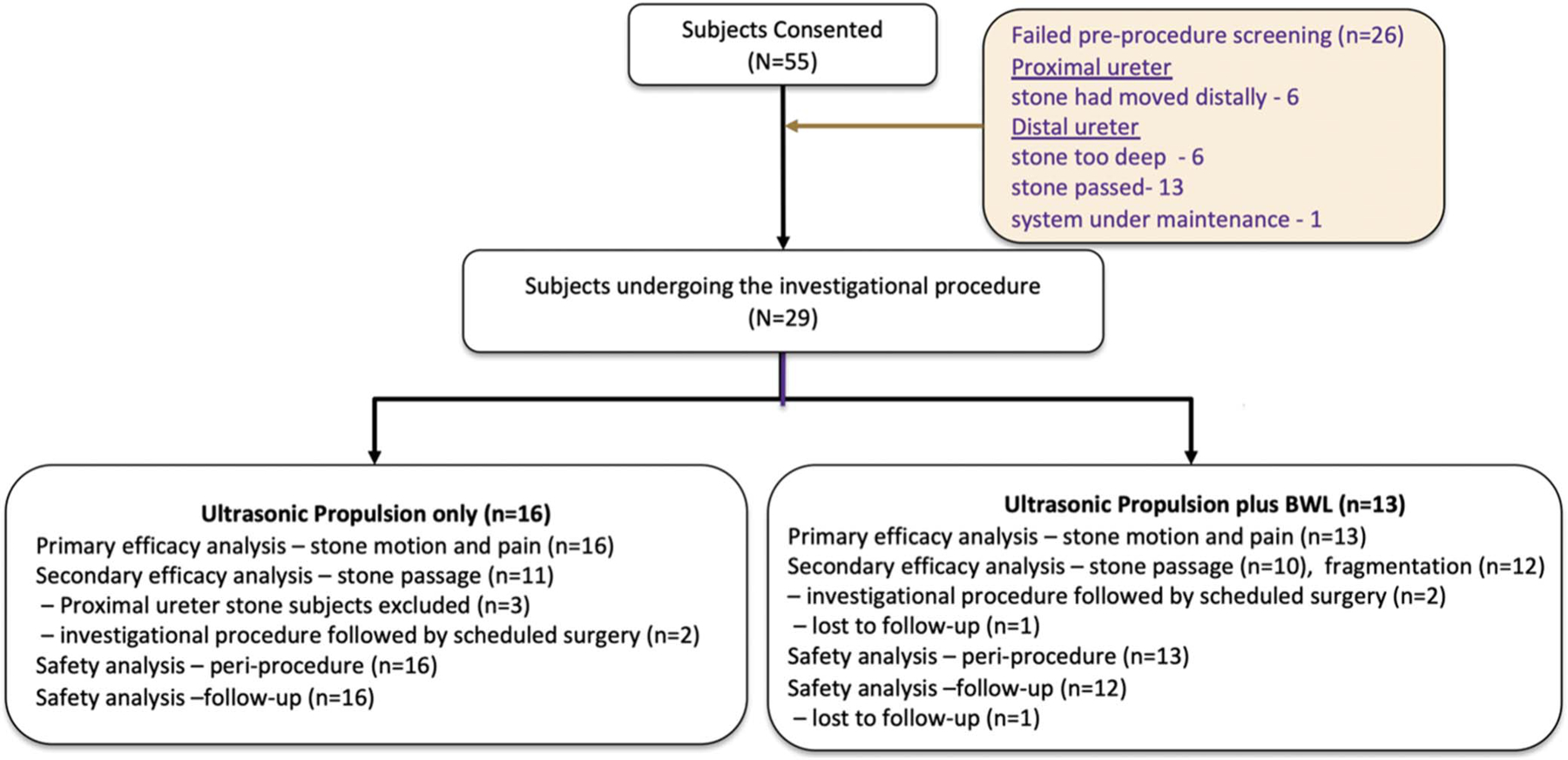
Enrollment of subjects. BWL indicates burst wave lithotripsy.
The demographics of the groups are listed in total and based on which of 2 exposures the subjects received, but the design is not to statistically compare the groups (Table 2). A variety of ages, stone sizes, locations, and days since onset are represented. Stone sizes of the 3 proximal ureteral stones are listed separately and not included in the mean size (± standard deviation [SD]). The timing of the investigational procedure spanned the range from in the ED at initial presentation to months after presentation and 1 day before scheduled surgery: 7 of 29 subjects were treated at first presentation. Average exposure for ultrasonic propulsion alone was shorter than with BWL because the individual bursts were shorter.
Table 2.
Subject Demographics
| Propulsion Only (n = 16) | Propulsion+BWL (n = 13) | Total (n = 29) | |
|---|---|---|---|
| Age, mean±SD, yrs | 51±19 | 40±16 | 46±18 |
| BMI, mean±SD, kg/m2 | 25±4 | 25±5 | 25±4 |
| Sex, No. | |||
| Male | 11 | 9 | 20 |
| Female | 5 | 4 | 9 |
| First time stone former, No. | 6 | 12 | 18 |
| Subjects reported taking medication within 24 hours prior to the investigational procedure, No. | |||
| Tamsulosin | 4 | 4 | 8 |
| Pain medication | 9 | 4 | 13 |
| Imaging modality, No. | |||
| CT | 13 | 12 | 25 |
| Ultrasound | 3 | 1 | 4 |
| Laterality, No. | |||
| Rt | 7 | 5 | 12 |
| Lt | 9 | 8 | 17 |
| Location, No. | |||
| Proximal | 3 | - | 3 |
| Distal | 13 | 13 | 26 |
| Distal ureteral stone size, mean±SD, mm | 4.4±1.8 | 5.2±1.6 | 4.8±1.7 |
| Proximal ureteral stone size, mm | 6, 9, 13 | 6, 9, 13 | |
| Days since presentation, mean±SD | 9.9±15 | 14.3±18.4 | 11.9±16.3 |
| Total exposure duration, min | 0.78±0.5 | 8.5±2.5 (including | 0.88±0.7 of propulsion, |
| 0.98±0.9 of propulsion) | 7.5±2.5 of BWL |
Abbreviations: BMI, body mass index; BWL, burst wave lithotripsy; CT, computerized tomography; Lt, left; Rt, right; SD, standard deviation.
Procedure and Follow-Up
The primary outcome, stone motion by the ultrasonic propulsion burst, was seen in 19 of 29 cases (Table 3). Two subjects had stones that were repositioned into the bladder during the investigational procedure, and in 1 case, the subject felt immediate relief (supplementary Video 1, https://www.jurology.com). Out of 29 cases, peristaltic motion and ureteral jetting occurred in association with the therapy bursts in 14 and 9 cases, respectively (supplementary Video 2, https://www.jurology.com). The presence of ureteral jets was not seen, and was not expected, when targeting proximal ureteral stones, but peristalsis was seen. Echogenicity around the stone was observed in 17 cases: 9 of these were with BWL. In 2 cases, the procedure was paused and the exposure level reduced per protocol because echogenicity appeared to extend from the stone, and the procedure continued to completion. The secondary outcome, distal ureteral stone passage, was reported in 18 of 21 subjects (86%) with at least 14 days of follow-up in a mean±SD of 3.9±4.9 days post-procedure.
Table 3.
Efficacy Outcomes
| Propulsion Only | Propulsion+BWL | Total | |
|---|---|---|---|
| Analysis | |||
| No. pts | 16 | 13 | 29 |
| Stone motion, No. (%) | 11 (69) | 8 (62) | 19 (66) |
| Peristaltic motion | 6 (38) | 8 (62) | 14 (48) |
| Ureteric jets | 5 (31) | 4 (31) | 9 (31) |
| Echogenicity change/potential cavitation | 8 (50) | 9 (69) | 17 (59) |
| Subgroup Analysis | |||
| No. pts | 11 | 10 | 21 |
| Subjects passing stone, No. (%) | 11 (100) | 7 (70) | 18 (86) |
| Days to passage, mean±SD | 2.6±4.0 | 5.9±5.9 | 3.9±4.9 |
Abbreviations: BWL, burst wave lithotripsy; SD, standard deviation.
Although an unplanned study endpoint that appeared as motion, fragmentation of stones into separate discernable fragments was observed on the ultrasound video during BWL exposure of 2 subjects (supplementary Video 3, https://www.jurology.com). Although there was not indisputable evidence of fragmentation in the ultrasound video, 3 other subjects returned ≤ 2 mm fragments (collections of calcium oxalate monohydrate [2] and struvite) to the clinic, all within 48 hours of the procedure, and all 3 proceeded to scheduled ureteroscopy (URS). Complete comminution to several ≤ 2 mm fragments was confirmed by basket extraction in both subjects who proceeded to URS within 48 hours of the BWL procedure. A single 2 mm calcium oxalate monohydrate fragment was confirmed by basket extraction in the third subject, who had URS after 2 weeks. The other 2 stones (calcium oxalate dihydrate and unknown composition) to undergo URS after BWL were intact and impacted with 1 surgery requiring a second wire to gain access. Overall fragmentation was confirmed in 5 of 13 BWL cases without the study design including a specific assessment for stone fragmentation.
Safety
The primary safety outcome includes anticipated or adverse events related to the device/procedure, and all anticipated events were mild and self-limiting, Grade 1 on the Clavien-Dindo Classification (Table 4). All subjects tolerated the procedure. No unanticipated events were reported. No subjects returned to the ED or had an intervention as a result of the procedure. Assessing intra-subject pain scores before and after the procedure, both the mean (P = .03) and median (1.4 [4.0] to 1.0 [2.0], P = .04) showed a significant decrease. Ten of 29 subjects reported a decrease in pain from before to after the procedure, whereas 2 subjects experienced an increase. Any discomfort experienced during the procedure was described as a pinprick or referred sensation to pass urine and the stone. This discomfort occurred in association with ultrasonic propulsion on 2.2% (18/820) of propulsion bursts delivered across all subjects. Ten subjects reported taking pain medication for their stones within 24 hours of the procedure. Hematuria resolved after the initial urination post-procedure. The 2 subjects requiring a pause for echogenicity were among those with discomfort and hematuria. No injuries to the ureter were observed in those who underwent URS. Five subjects experienced mild redness of the skin, which resolved within 24 hours; this was anticipated from the manipulation of an ultrasound transducer against the skin. The subject reported sensation during the procedure was mild. All 3 proximal ureteral stone subjects and all subjects who did not pass their distal ureteral stone in the time given before surgery went on to surgery.
Table 4.
Safety Outcomes and Peri-Procedure Subject-Reported Sensation
| Propulsion Only (n = 16) | Propulsion+BWL (n = 13) | Total (n = 29) | |
|---|---|---|---|
| Anticipated Events | |||
| Pain score, mean±SD | |||
| Immediately pre-procedure | 2.8±2.6 | 1.2±1.4 | 2.1±2.3 |
| Immediately post-procedure | 2.3±2.4 | 0.8±0.9 | 1.6±2.0 |
| Discomfort/pain with procedure, No. (%) | 3 (25) | 4 (33) | 7 (28) |
| Gross hematuria, No. (%) | 1 (6) | 6 (46) | 7 (24) |
| Peri-Procedure Sensation | |||
| Warming of the skin, No. (%) | 9 (56) | 9 (69) | 18 (62) |
| Vibrational sensation, No. (%) | 0 (0) | 3 (23) | 3 (10) |
| Urinary urgency, No. (%) | 5 (31) | 5 (38) | 10 (34) |
Abbreviations: BWL, burst wave lithotripsy; SD, standard deviation.
DISCUSSION
We tested a portable ultrasound-based device to transcutaneously target, break, and expel stones and stone fragments from the urinary system using a single handheld transducer. Ultrasonic propulsion has previously been demonstrated to move asymptomatic renal stones in awake5 and anesthetized subjects,6 and BWL has only been used to break stones in anesthetized subjects.8 This study advances the previous work among a new cohort of awake patients with ureteral stones. It is the first use of BWL in awake subjects and ultrasonic propulsion in the ureter, and the first study to advance a clinical outcome which included pain relief and rate of passage.
The primary outcome of stone displacement by the ultrasound bursts occurred in 66% including 2 stones which were repositioned directly into the bladder. The secondary outcome–distal ureteral stone clearance–was observed in 86% of subjects in an average of 3.9 days. On average, pain scores significantly decreased during the investigative procedure, and anticipated events were mild and self-resolved. All subjects tolerated the procedure.
Stones were shown to be moved in the ureter. Two-thirds of the subjects experienced stone motion, and that number may be an underestimation since studies in the kidney with simultaneous URS showed ultrasound imaging underestimated or missed stone motion from ultrasonic propulsion in 16% of subjects.6 The high rate of passage and possible underestimation in motion may have contributed to the lack of correlation between motion and passage.
Passage was facilitated by 3 mechanisms: direct stone motion (displacement or rotation), fragmentation, and peristalsis. In 7 subjects, the investigational procedure fragmented stones or moved stones into the bladder resulting in stone or fragment passage. After a greater than 1 month trial of passage and then the investigative procedure, 4 of 7 surgeries were cancelled within days of the procedure because of successful stone passage. In addition, 2 stones were clearly seen to be fragmented on ultrasound image, 1 within 45 seconds of BWL application, and at least 3 stones were fragmented but without clear observation on imaging. Undetected fragmentation could have contributed to additional stone passage, and with experience operators may learn to interpret the image for fragmentation as urologists have done for fluoroscopy during shock wave lithotripsy.12,17 Lastly, peristalsis and ureteral jets synchronized with the application of propulsion bursts occurred in in 48% and 31% of the cases, respectively, and were consistent with previous observation of ultrasound-stimulated ureteral peristalsis of urine and debris into the bladder.18,19 Synergy with medical expulsive therapy used to suppress peristalsis was not investigated.
Although stones passed at a high rate, there was no control group for comparison. The American Urological Association (AUA) guidelines quote a stone passage rate of 54% for distal ureteral stones smaller than 10 mm based on meta-analyses of 1,205 subjects in 27 studies, mostly following for 2 weeks after presentation.3,20 These guidelines do not report an average stone size or stratify with size other than to report 62% passage of distal ureteral stones < 5 mm and 35% passage of distal ureteral stones > 5 mm for pediatric patients. Within the AUA data set, a meta-analysis of 16 studies and 292 subjects showed the same 54% passage rate with an average time to passage of 7.4 days.21 The AUA guidelines state even surgery for distal ureteral stones is not completely effective, with 74% stone-free with shock wave lithotripsy and 94% stone-free with URS.3
Two of 3 proximal ureteral stones were moved retrograde proximally, but they were not pursued further to move them into the kidney. However, on clinical advice to hydrate and as one subject changed positions for us to align the procedure, the stone rolled back to the lower pole, where it remained for several weeks.20 In our previous study, the 1 subject with a stone in the ureteral pelvic junction felt immediate relief following 1 propulsion burst within the procedure.6
Overall, the procedure was well tolerated by awake unanesthetized subjects. Pain was significantly reduced even though 8 subjects were asymptomatic from the start, which biases inferences toward the null hypothesis that there is no pain reduction. It is noted that pain scores are inherently subjective, and medication management was left to the discretion of the clinical team. However, we attempted to overcome subjectivity by analyzing pain on an intra-subject level as opposed to group averages. Finally, 6 of 26 screen fails had stones too deep for the transducer; however, this limitation is technically correctable in future transducer designs.
CONCLUSION
This study supports the efficacy and safety of using ultrasonic propulsion and BWL in awake subjects to reposition and break ureteral stones in order to relieve pain and facilitate passage. The study showed stones were repositioned into the bladder, natural peristalsis occurred in synchrony with ultrasonic propulsion bursts, and BWL fragmented ureteral stones. A majority (86%) of distal ureteral stones passed in an average of 3.9 days. The procedure was well tolerated with pain being reduced and showed minimal risk to the subjects. This technology has the potential to provide an advantageous and patient-centered solution for the gap between expectant management and urological intervention for symptomatic ureteral stones.
Supplementary Material
Acknowledgments
We thank our research coordinators and colleagues.
Support:
The study was supported by NASA HRP ExMC MTL ID 1265 through a contract with ZIN Technologies. System and research infrastructure development was supported by NIH NIDDK P01 DK043881, NIH K01 DK104854, and the National Space Biomedical Research Institute.
Footnotes
Conflict of Interest: MB, BC, BD, and MS have consulting agreements with and equity in SonoMotion, Inc., which has licensed this technology from the University of Washington for commercialization. RMS: American Urological Association, Elsevier Publishing (Campbells Urology). ISM: Bard BD, Perceus Inc. MD: Philips Medical Imaging, General Electric Healthcare.
Ethics Statement: This study received Institutional Review Board approval (IRB No. STUDY00002746).
REFERENCES
- 1.Fwu CW, Eggers PW, Kimmel PL, et al. Emergency department visits, use of imaging, and drugs for urolithiasis have increased in the United States. Kidney Int 2013;83(3):479–486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Feinstein L Kidney Stones Washington, DC: Urologic Diseases in America. US Department of Health and Human Services, Public Health Service, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases US Government Printing Office; NIH Publication No. 20172018:12–7865. [Google Scholar]
- 3.Assimos D, Krambeck A, Miller NL, et al. Surgical management of stones: American Urological Association/Endourological Society guideline, PART II. J Urol 2016;196(4):1161–1169. [DOI] [PubMed] [Google Scholar]
- 4.Simon JC, Dunmire B, Bailey MR, et al. Developing complete ultrasonic management of kidney stones for spaceflight. J Space Saf Eng 2016;3(2):50–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Harper JD, Cunitz BW, Dunmire B, et al. First-in-human clinical trial of ultrasonic propulsion of kidney stones. J Urol 2016;195(4 Pt 1):956–964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dai JC, Sorensen MD, Chang HC, et al. Quantitative assessment of effectiveness of ultrasonic propulsion of kidney stones. J Endourol 2019;33(10):850–857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Harper JD, Metzler IS, Hall MK, et al. First in-human burst wave lithotripsy for kidney stone comminution: initial two case studies. J Endourol 2021;35(4):506–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harper JD, Lingeman JE, Sweet RM, et al. Fragmentation of stones by burst wave lithotripsy in the first 19 humans. J Urol 2022;207(5):1067–1076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sorensen MD, Dai JC, Chen TT, et al. LBA01–06 Randomized control trial of ultrasonic propulsion to facilitate clearance of chronic residual fragments. J Urol 2021;206(3S):e1172. [Google Scholar]
- 10.Wong C, Teitge B, Ross M, et al. The accuracy and prognostic value of point-of-care ultrasound for nephrolithiasis in the emergency department: a systematic review and meta-analysis. Acad Emerg Med 2018;25(6):684–698. [DOI] [PubMed] [Google Scholar]
- 11.Eisner BH, Reese A, Sheth S, et al. Ureteral stone location at emergency room presentation with colic. J Urol 2009;182(1):165–168. [DOI] [PubMed] [Google Scholar]
- 12.Ramesh S, Chen TT, Maxwell AD, et al. In vitro evaluation of urinary stone comminution with a clinical burst wave lithotripsy system. J Endourol 2020;34(11):1167–1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Janssen KM, Brand TC, Cunitz BW, et al. Safety and effectiveness of a longer focal beam and burst duration in ultrasonic propulsion for repositioning urinary stones and fragments. J Endourol 2017;31(8):793–799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.May PC, Kreider W, Maxwell AD, et al. Detection and evaluation of renal injury in burst wave lithotripsy using ultrasound and magnetic resonance imaging. J Endourol 2017;31(8):786–792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Maeda K, Colonius T, Kreider W, Maxwell A, Cunitz B, Bailey M. Modeling and experimental analysis of acoustic cavitation bubbles for burst wave lithotripsy. J Phys Conf Ser 2015;656: 012027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Baxley J Document number 1226: content of premarket notifications (510(k)s) for extracorporeal shock wave lithotripters indicated for the fragmentation of kidney and ureteral calculi - guidance for industry and for FDA reviewers. U.S. Department of Health and Human Services; 2000 Updated July 18, 2018. https://www.fda.gov/medical-devices/. [Google Scholar]
- 17.Chaussy CG, Tiselius HG. How can and should we optimize extracorporeal shockwave lithotripsy? Urolithiasis 2018;46(1):3–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Marshall KL, Saade D, Ghitani N, et al. PIEZO2 in sensory neurons and urothelial cells coordinates urination. Nature 2020;588(7837):290–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liao D, Hsiao M-Y, Xiang G, et al. Optimal pulse length of insonification for Piezo1 activation and intracellular calcium response. Scientific Rep 2021;11(1):709–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hall MK, Samson PC, Kessler R, et al. Pearl-unjammed: the Seattle stone maneuver for ureteropelvic junction urolithiasis. J Am Coll Emerg Physicians Open 2020;1(3):252–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cui Y, Chen J, Zeng F, et al. Tamsulosin as a medical expulsive therapy for ureteral stones: a systematic review and meta-analysis of randomized controlled trials. J Urol 2019;201(5): 950–955. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


