Summary
Background
Public health progress in the Americas has reduced the burden of many infectious diseases, helping more people live longer lives. At the same time, the burden of non-communicable diseases (NCDs) is increasing. NCD prevention rightly focuses on lifestyle risk factors, social, and economic determinants of health. There is less published information on the importance of population growth and aging to the regional NCD burden.
Methods
For 33 countries in the Americas, we used United Nations population data to describe rates of population growth and aging over two generations (1980–2060). We used World Health Organization estimates of mortality and disability (disability-adjusted life years, DALYs) to describe changes in the NCD burden between 2000 and 2019. After combining these data resources, we decomposed the change in the number of deaths and DALYs to estimate the percentage change due to population growth, due to population aging, and due to epidemiological advances, measured by changing mortality and DALY rates. In a supplement, we provide a summary briefing for each country.
Findings
In 1980, the proportion of the regional population aged 70 and older was 4.6%. It rose to 7.8% by 2020 and is predicted to rise to 17.4% by 2060. Across the Americas, DALY rate reductions would have decreased the number of DALYs by 18% between 2000 and 2019 but was offset by a 28% increase due to population aging and a 22% increase due to population growth. Although the region enjoyed widespread reductions in rates of disability, these improvements have not been sufficiently large to offset the pressures of population growth and population aging.
Interpretation
The region of the Americas is aging and the pace of this aging is predicted to increase. The demographic realities of population growth and population aging should be factored into healthcare planning, to understand their implications for the future NCD burden, the health system needs, and the readiness of governments and communities to respond to those needs.
Funding
This work was funded in part by the Pan American Health Organization, Department of Noncommunicable Diseases and Mental Health.
Keywords: Noncommunicable disease, Latin America, Caribbean, Population growth, Aging, Mortality, Disability-adjusted life years
Research in context.
Evidence before this study
The region of the Americas is aging, reflecting important public health successes that have reduced the burden of infectious disease, and a long-term regional drop in fertility. The burden of non-communicable diseases (NCDs) has been increasing, and despite global commitments to NCD control, many countries need to accelerate the implementation of policies and interventions to prevent and manage NCDs. The NCD discourse rightly focuses on lifestyle risk factors, social, and economic determinants of health as drivers of NCD burden and inequality. There is less published information on the role of population growth and aging in driving the regional NCD burden and how these pressures can influence regional NCD inequalities.
Added value of this study
Our research joins two key global data resources to describe the role of population growth and aging on the inequalities in the NCD burden across the Americas. We report on the World Health Organization Global Health Estimates, highlighting an increase in the number of NCD deaths and years lost to disability between 2000 and 2019, despite important improvements in disease rates. We use the United Nations World Population Prospects to detail the dynamics of population growth and aging across the Americas. By linking these datasets, we were able to explore the influence of population growth and aging on the increasing regional NCD burden. We show that there have been important reductions in NCD mortality and disability rates between 2000 and 2019, reflecting the many successful public health programs and health system improvements across the region. However, for every country in the region, these improvements have not been sufficiently large to offset the pressures of population growth and population aging. We highlight that these pressures are uneven between the countries of the region, contributing to increasing regional inequality in the NCD burden. In supplements, we provide country-level briefings to highlight the importance of population growth and aging on the rising NCD burden.
Implications of all the available evidence
Reductions in premature mortality represent a major global success and will lead to further population aging. The extent to which longer lives are lived in good health or with illness is fundamentally important for health system planners, who must understand the healthcare implications of an aging population with potentially longer-term illness and complex multimorbidity. The demographic realities of population growth and population aging should be factored into healthcare planning, to understand their potential implications for the NCD burden, the health system, and social protection needs. This additional evidence can contribute to a more informed response against age-related inequalities, ageism, and the unprecedented public health challenge of older populations.
Introduction
Socioeconomic progress and reductions in the burden of many infectious diseases have led to a dramatic decline in associated mortality and have contributed to an era of demographic and epidemiological transition, which is ongoing in many developing regions.1, 2, 3 These successes have led to new challenges related to aging populations, the associated increase in the proportion of disease burden attributable to noncommunicable diseases including mental health and neurological conditions (NCDs) and in places, a double burden of infectious and non-communicable diseases.4 Rates of NCDs increase with age so that while much of the NCD discourse rightly focuses on prevention, control, and the social and economic determinants of health,5, 6, 7, 8 the absolute burden of NCDs is also influenced by the size and age structure of a nation's population.
In 2013, the World Health Organization (WHO) Member States approved a Global Action Plan on the Prevention and Control of NCDs with a menu of policies and interventions called “NCD Best Buys” and a monitoring framework with an impact indicator that measures premature mortality.9 This was supplemented by Sustainable Development Goal (SDG) 3.4, proposing a one-third NCD premature mortality reduction by 2030.10 More recently, countries approved a Roadmap on NCDs (2013–2020) to accelerate the NCD response.11 These global commitments have underpinned further international initiatives12, 13, 14 to reduce the NCD burden; a collective advocacy that has been vital for recognizing NCDs as a global priority. The hoped-for reduction in premature avoidable mortality – once achieved – will lead to longer lives, aspirationally lived with minimal ill-health – a goal widely encompassed in public health messaging, for example in England – “Living Well for Longer”,15 and formally described in 1980 by James Fries as the compression of morbidity.16,17 Progress towards this healthy aging ideal is likely to be governed by access to health care, as well as social and economic drivers – the inequalities of gender, income, education, race, ethnicity, and other social factors.18
The extent to which longer lives are lived in good health or with illness is fundamentally important for health system planners, who must understand the healthcare implications of an aging population with potentially longer-term illness and complex multimorbidity.19 In this analysis we summarize aging patterns across the Americas and explore to what extent aging offsets national efforts to reduce the burden of ill-health due to NCDs. We first assess country-level differences in population aging and growth across the Americas. We then describe the extent to which these demographic dynamics explain observed changes in the number of years lived with disability due to NCDs.
Methods
Data sources
Every two years the United Nations Department of Economic and Social Affairs updates its population size projections for all member countries. The World Population Projections (WPP) 2019 revision, released in June 2019, is the source for all population data used in this analysis.20 The WPP collects mortality estimates using a variety of sources: vital registration systems, surveillance systems, demographic surveys, and censuses, adjusting estimates for intercensal fertility, mortality, and migration.
The WHO Global Health Estimates (GHEs) are comparable cause of death and disability estimates from the year 2000 onwards. These estimates draw on a range of sources, including official country data and the results of the Global Burden of Disease (2019). Efforts are made to ensure data comparability between countries and across time. Full details of the WHO GHE are available at the WHO Global Health Observatory.21, 22, 23 From the GHE data we extracted information on NCDs in 6 groups: cardiovascular diseases (International Classification of Diseases, ICD: I00-I99), cancers (C00-C97), chronic respiratory diseases (J30-J98), diabetes (E10-E14 minus E10.2, E11.2, E12.2, E13.2, E14.2), mental and substance use disorders (F04-F99, G72.1, Q86.0, X41-X42, X44, X45), and neurological conditions (F01-F03, G06-G98, minus G14, G72.1). Our restriction to these 6 NCD groupings follows the Pan American Health Organization (PAHO) regional plan of action for the prevention and control of noncommunicable diseases. This plan considers the main NCDs as being those defined by the United Nations (2011 UN Resolution on NCDs) as principally cardiovascular diseases, cancers, chronic respiratory diseases and diabetes.24 In 2018 UN Resolution on NCDs was extended to include mental health and neurological conditions.25 We limit our primary analyses to these 6 NCDs groups of conditions.
Countries and subregions of the Americas
The WHO GHEs are available for 183 WHO Member States with populations greater than 90,000 in 2019. In the Americas, 2 member States were therefore excluded: Dominica (United Nations estimated population in 2019, 71,808), and Saint Kitts and Nevis (estimated population 52,834). Estimates for these two countries are included in regional totals. For this analysis we grouped the included countries of the Americas into eight subregions, as defined by The Pan-American Health Organization: North America (2 countries: Canada, USA), Central America (7 countries: Belize, Costa Rica, El Salvador, Guatemala, Honduras, Nicaragua, Panama), Andean (5 countries: Bolivia, Colombia, Ecuador, Peru, Venezuela), Southern Cone (4 countries: Argentina, Chile, Paraguay, Uruguay), Latin Caribbean (3 countries: Cuba, Dominican Republic, Haiti), Non-Latin Caribbean (10 countries: Antigua and Barbuda, Bahamas, Barbados, Grenada, Guyana, Jamaica, Saint Lucia, Saint Vincent and the Grenadines, Suriname, Trinidad and Tobago), Brazil as a separate country, and Mexico as a separate country.
Metrics used: mortality and disability
We used two metrics from the WHO Global Health Estimates. Number of deaths: for each country, we extracted the number of deaths by cause, age, sex, and year. Disability adjusted life years (DALYs): the DALY is a summary measure that combines time lost through premature death and time lived in states of less than optimal health, loosely referred to as “disability”. The DALY adds together the years of life lost (YLL) and the years of lost good health also called the years lived with disability (YLD). One DALY can be thought of as one lost year of ‘healthy’ life. Because the DALY is an aggregation of premature mortality and years lived with disability it offers a more direct link than mortality alone to the associated burden on healthcare systems. We present age-standardized rates for mortality and disability, using the WHO World Standard population.26 There are many uncertainties involved with estimating national mortality and disability. We used uncertainty intervals for age-, sex-, and cause-specific deaths and DALYs developed by the WHO for GHE 2019 and provided as part of their data release. These intervals will not reflect all sources of uncertainty, but do remind us not to over-interpret differences, for example between causes or countries.
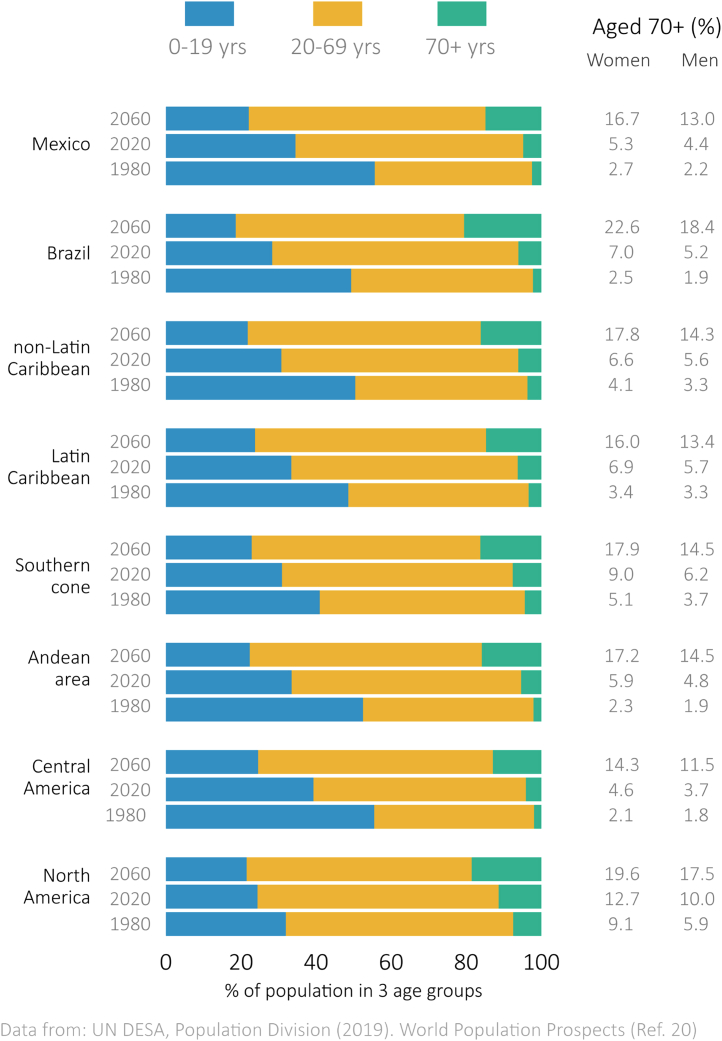
Analysis: describing population demographics
We summarized population aging and population growth in two phases. In phase 1, we described the long-term change in population distributions for each country and for each subregion using 1980 to 2060 as our time frame. In 2020, young adults from 1980 were approaching retirement, and by 2060 a second cohort of adults will be completing their working lives. Our long-term estimates therefore cover demographic change across two generations. We present subregional population distributions in Fig. 1 in three broad age groups: children and adolescents (0–19 years), adults aged 20–69 years, and adults aged 70 years and older, with country-level population distributions provided in a supplement. We also calculated the accompanying change in the old-age dependency ratio as the number of adults aged 70 years and older for every 100 people aged 20–69 years. In phase 2 we focused on a shorter period (2000–2020) to closely match the GHE data availability. For this shorter time frame, for each country and subregion, we calculated one measure of population aging and one measure of population growth. We described population aging using the percentage of each population aged 70 years and older. We described population growth using the annual average rate of growth, calculated as an exponential rate and presented as a percentage growth per year. It is calculated as ln(p2020/p2000)/t where p2020 is the population in 2020, p2000 is the population in 2000, and t is the length of the period, which in our case was 20 years.27
Fig. 1.
Proportion of population classified as children and adolescents (0–19 years), adults (20–69 years) or older adults (70+ years) in eight sub-regions of the Americas in 1980, in 2020, with predicted proportions in 2060.
Analysis: mortality and disability change between 2000 and 2019
Using GHE data, we described NCD mortality and DALYs since 2000 using the six NCD subgroups described above. For women and men, we presented the number of deaths and DALYs in 2019, age-standardized rates per 100,000 people in 2019, and the percent change in these metrics between 2000 and 2019.
Next, following Roth,28 we decomposed the observed change in mortality and disability between 2000 and 2019 into three explanations for each country: growth in the total population size, the change in the age structure of the population, and the change in the age-specific rates. This third explanation includes all changes that are not explained by demographic change (the aging or growth of the population) and includes (for example) the combined effects of lifestyle risk factors and health care. The net change in these three explanations is equal to the observed mortality or disability change. We achieved this decomposition by holding one demographic feature constant at a time and calculating the expected deaths or years of disability under that counterfactual scenario. Using disability as our example, to calculate the change in disability due to population growth, we calculated the additional DALYs expected from the population increase between 2000 and 2019; and using the age-structure and disability rates from the year 2000. For the change in DALYs due to population aging, we repeated the process, this time allowing the age-structure to change between 2000 and 2019; and holding population size and disability rates constant at their 2000 levels. Finally, the difference between the actual change in disability and the combined change due to population growth and population aging is the change due to age-specific disability rates. We examined between-country differences in these decomposed percentage changes by calculating a measure of change inequality, known as the Index of Disparity, following methods described by the WHO.29 Details of this calculation are provided as a footnote to Table 3.
Table 3.
Differences in the percentage change in deaths and DALYs between 2000 and 2019 among 33 countries of The Americas, measured using the index of disparity.a
| Metric | Sex | Overall Change | Lower limit of sensitivity range | Upper limit of sensitivity range | Change (growth) | Change (aging) | Change (epi) |
|---|---|---|---|---|---|---|---|
| Deaths | Men | 85.0 | 66.1 | 106.4 | 52.9 | 33.4 | 65.7 |
| Women | 104.3 | 71.5 | 178.1 | 51.6 | 58.5 | 68.4 | |
| Combined | 92.6 | 67.9 | 131.2 | 52.2 | 44.5 | 65.7 | |
| DALYs | Men | 56.8 | 51.1 | 75.1 | 52.9 | 27.4 | 69.8 |
| Women | 59.6 | 52.9 | 84.7 | 51.6 | 39.8 | 67.0 | |
| Combined | 56.8 | 50.7 | 76.8 | 52.2 | 31.2 | 65.8 |
Calculation note: For each metric (percentage change in deaths or DALYs overall or due to population growth, population aging, epidemiologic change), the index of disparity (ID) presents the proportional difference between each country and the regional average. We use this to highlight the size of the between-country inequality in the Americas for each metric. For each country, , ID is calculated as the sum of the absolute differences between country change and the regional change for the Americas , divided by the regional rate and the number of countries, . The full equation is calculated as: .
For our decomposition results we performed sensitivity analyses based on the 95% uncertainty limits for deaths and DALYs provided by the WHO in their 2019 data release. We repeated our decomposition once using the WHO lower limit of uncertainty and once using the upper limit of uncertainty. This created a ‘sensitivity range’ (SR) which we report as our measure of analysis uncertainty. The WHO additionally categorizes each member state into one of four categories according to the level of evidence available for causes of death, and we use these categories in our visual presentations to further highlight the inherent uncertainty involved in working with national estimates of mortality and disability. In supplements, we provide an example of the full decomposition calculation process as a spreadsheet, we offer more information on data quality and analysis uncertainty, and we present results from sex-stratified analyses.
Country briefings
In a supplement, we provide a 1-page briefing for each country; 33 briefings in total. In each country briefing we summarize the current and future predicted proportion of adults aged 70 and older, mortality rates in 2019 for our six NCD groups compared to subregional and regional rates, and how population growth, population aging, and epidemiological change has contributed to the change in deaths between 2000 and 2019.
All analyses were performed using Stata statistical software.30
Role of the funding source
The Pan American Health Organization funding source provided technical resources for the data analysis including visualizations, and otherwise had no involvement in manuscript design or preparation.
Results
Population growth and aging
Regional and country-level population aging and population growth between 2000 and 2020 is presented in Table 1. The population of the Americas in 2020 was 1018 million, up from 828 million in 2000 – an annual population size increase of 1 percent. The subregions of the Americas have all increased their population sizes since 2000, from a smallest annual increase of 0.6 percent in the non-Latin Caribbean to a largest annual increase of 1.7 percent in Central America.
Table 1.
Population size and proportion aged 70 and older among 33 countries of the Americas in 2000 and in 2020.
| Country | Population in 2020 | Percent of population aged 70+ |
Annual growth rate (2000–2020) |
||
|---|---|---|---|---|---|
| 2000 | 2020 | All ages | Older adults (70+) | ||
| AMERICAS | 1,017,996,032 | 5.6 | 7.8 | 1.03 | 2.64 |
| NORTH AMERICA | 368,744,832 | 9.0 | 11.4 | 0.83 | 2.02 |
| Canada | 37,742,160 | 8.8 | 12.4 | 1.05 | 2.75 |
| United States | 331,002,624 | 9.0 | 11.2 | 0.81 | 1.93 |
| CENTRAL AMERICA | 50,737,432 | 2.8 | 4.1 | 1.66 | 3.63 |
| Belize | 397,621 | 2.5 | 3.2 | 2.37 | 3.50 |
| Costa Rica | 5,094,114 | 3.6 | 6.7 | 1.26 | 4.45 |
| El Salvador | 6,486,201 | 3.3 | 5.8 | 0.48 | 3.23 |
| Guatemala | 17,915,564 | 2.4 | 3.2 | 2.15 | 3.53 |
| Honduras | 9,904,608 | 2.3 | 3.1 | 2.05 | 3.50 |
| Nicaragua | 6,624,554 | 2.4 | 3.4 | 1.34 | 3.16 |
| Panama | 4,314,768 | 3.6 | 5.7 | 1.77 | 4.07 |
| ANDEAN AREA | 141,606,752 | 3.1 | 5.4 | 1.20 | 3.99 |
| Bolivia | 11,673,029 | 3.3 | 5.1 | 1.63 | 3.77 |
| Colombia | 50,882,884 | 3.3 | 5.7 | 1.25 | 4.09 |
| Ecuador | 17,643,060 | 3.1 | 4.8 | 1.65 | 3.81 |
| Peru | 32,971,850 | 3.0 | 5.6 | 1.10 | 4.25 |
| Venezuela | 28,435,942 | 2.8 | 4.9 | 0.81 | 3.69 |
| SOUTHERN CONE | 74,918,248 | 6.0 | 7.6 | 1.04 | 2.26 |
| Argentina | 45,195,776 | 6.6 | 7.7 | 1.02 | 1.83 |
| Chile | 19,116,208 | 5.0 | 8.0 | 1.10 | 3.50 |
| Paraguay | 7,132,530 | 2.8 | 4.3 | 1.46 | 3.48 |
| Uruguay | 3,473,727 | 9.0 | 10.8 | 0.23 | 1.15 |
| LATIN CARIBBEAN | 33,577,056 | 4.3 | 6.3 | 0.90 | 2.78 |
| Cuba | 11,326,616 | 6.8 | 10.9 | 0.09 | 2.42 |
| Dominican Rep | 10,847,904 | 2.9 | 4.8 | 1.24 | 3.77 |
| Haiti | 11,402,533 | 2.4 | 3.1 | 1.49 | 2.76 |
| NON-LATIN CARIBBEAN | 6,919,487 | 4.7 | 6.1 | 0.59 | 1.91 |
| Antigua & Barbuda | 97,928 | 4.6 | 5.9 | 1.27 | 2.53 |
| Bahamas | 393,248 | 3.4 | 4.7 | 1.39 | 3.09 |
| Barbados | 287,371 | 8.8 | 11.5 | 0.28 | 1.62 |
| Grenada | 112,519 | 5.5 | 6.4 | 0.45 | 1.17 |
| Guyana | 786,559 | 2.6 | 4.3 | 0.26 | 2.77 |
| Jamaica | 2,961,161 | 5.5 | 6.0 | 0.55 | 1.04 |
| Saint Lucia | 183,629 | 5.2 | 7.0 | 0.79 | 2.24 |
| St Vincent & Gren | 110,947 | 4.6 | 6.4 | 0.14 | 1.75 |
| Suriname | 586,634 | 3.4 | 4.5 | 1.10 | 2.60 |
| Trinidad & Tobago | 1,399,491 | 4.2 | 7.2 | 0.50 | 3.20 |
| Brazil | 212,559,424 | 3.3 | 6.1 | 0.98 | 4.09 |
| Mexico | 128,932,768 | 3.4 | 4.8 | 1.33 | 3.14 |
The change in subregional population structure over time in three broad age groups is presented in Fig. 1. In 1980, the proportion of the regional population aged 70 and older was 4.6 percent. It rose to 7.8 percent by 2020 and is predicted to rise to 17.4 percent by 2060. These successive 40-year increases of 3.2 and 9.6 percentage points are larger than the global average of 2.3 and 7.1 percentage points. The rate of aging across the region was similar between 1980 and 2020, with the 8 subregions of the Americas reporting increases in the proportion aged 70 and older of between 2.2 and 3.9 percentage points. Predictions suggest a regional divergence in this rate over the next 40 years, with increases of between 7.2 and 14.5 percentage points. This aging trend is set against rather different baseline levels of older adults in 1980 – between 1.9 percent over 70 years of age in Central America and 7.5 percent in North America – so that marked inequalities in the proportion of older adults are predicted to persist in 2060 – between 12.9 percent over 70 years of age in Central America and 20.6 percent in Brazil.
Inequalities in the proportion of older adults were more apparent at the country level. Annual population growth rates for this period ranged from 0.1% to 2.4% across all ages and from 1.0% to 4.5% among adults aged 70 and older, so that the country range of adults aged 70 and older was 6.6 percentage points in 2000 and had increased to 9.3 percentage points by 2020. This proportion of older adults in 2020 ranged from less than 3.5 percent (in Belize, Guatemala, Haiti, Honduras, Nicaragua) to over 10 percent (Barbados, Canada, Cuba, United States, Uruguay) – a threefold difference between these regional extremes (Table 1).
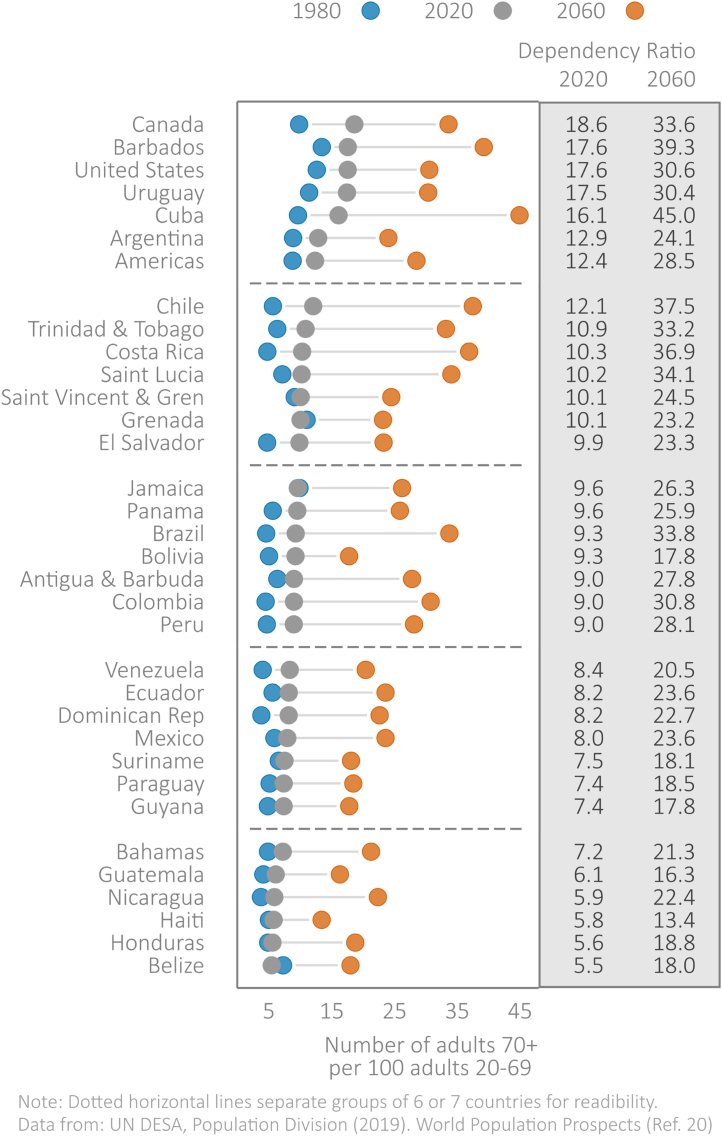
The old-age dependency ratio between 1980 and 2060 is presented in Fig. 2 for the 33 included countries of the Americas. This ratio depends as well on the proportion of working age adults, offers insight on a country's ability to finance an aging population, and has increased broadly in line with the proportion of older adults. In 2020, estimates ranged from a low of 6 older adults for every 100 working age adults in Belize, to 19 in Canada. By 2060, this range will have shifted and widened, from a low of 13 (in Haiti) to 45 (in Cuba). In 2020, countries with the five highest dependency ratios (Canada, Barbados, United States, Uruguay, Cuba) all had a ratio more than twice that of countries with the five lowest ratios (Belize, Honduras, Haiti, Nicaragua, Guatemala).
Fig. 2.
Old age dependency ratio (number of older adults aged 70 and older for every 100 people aged 20–69 years) among 33 countries of the Americas in 1980, 2020, and predicted for 2060.
NCD mortality and disability
Age-standardized rates of NCD mortality and disability in the Americas in 2000 and 2019 are presented in Table 2. Between 2000 and 2019 in the Americas the age-standardized mortality rate from six groups of NCDs combined decreased from 424 to 329 per 100,000, a 20-year mortality rate improvement of 21.7 percent. This improvement was driven by large reductions in cardiovascular disease (CVD) and cancer mortality rates. The age-standardized CVD mortality rate in 2019 was 137 per 100,000 down from 203 per 100,000 in 2000, a 20-year improvement of 32.5 percent, and was driven by mortality rate reductions in ischemic heart disease (2019 mortality rate of 74 per 100,000, a reduction of 37 percent) and stroke (2019 mortality rate of 32 per 100,000, a reduction of 35 percent). The age-standardized cancer mortality rate was down to 101 from 128 per 100,000, a 20-year improvement of 21.3 percent, and was driven by large mortality rate reductions for lung cancer (2019 mortality rate of 19 per 100,000, a reduction of 33 percent), breast cancer in women (2019 mortality rate of 16 per 100,000 women, a reduction of 19 percent) and prostate cancer in men (2019 mortality rate of 15 per 100,000 men, a reduction of 26 percent). The situation for disability was similar. Between 2000 and 2019 in the Americas the age-standardized DALY rate from six groups of NCDs combined decreased from 14,056 to 12,481 years per 100,000, a 20-year DALY rate improvement of 11.2 percent. Despite these important rate improvements the number of regional NCD deaths from our six disease groups increased from 3.60 million in 2000 to 4.86 million in 2019, and the disability years increased from 113 to 150 million, 20-year increases of 35 and 33 percent respectively. All NCD deaths also includes digestive, genitourinary and musculoskeletal conditions, and regional deaths for all NCDs increased from 4.21 million in 2000 to 5.82 million in 2019.
Table 2.
Disease burden of noncommunicable diseases in the Americas in 2000 and in 2019, for 6 groups of conditions: CVD, cancer, respiratory disease, diabetes, mental health conditions, and neurological disorders.
| Number of events in 2019 |
Rate per 100,000 in 2019 |
Percent change (2000–2019) |
||||||
|---|---|---|---|---|---|---|---|---|
| Women | Men | Women | Men | Count (Women) | Rate (Women) | Count (Men) | Rate (Men) | |
| CVD | ||||||||
| Deaths | 981,439 | 1,041,640 | 112 | 167 | 9 | −34 | 22 | −32 |
| DALYs | 17,889,816 | 22,972,044 | 2478 | 3907 | 10 | −30 | 19 | −28 |
| YLLs | 15,513,802 | 20,889,718 | 2137 | 3556 | 5 | −33 | 15 | −30 |
| YLDs | 2,376,014 | 2,082,326 | 341 | 352 | 48 | −4 | 65 | 1 |
| Cancer | ||||||||
| Deaths | 654,124 | 706,653 | 90 | 116 | 31 | −19 | 31 | −25 |
| DALYs | 16,062,270 | 16,661,299 | 2504 | 2858 | 25 | −19 | 23 | −25 |
| YLLs | 15,248,201 | 15,774,216 | 2381 | 2710 | 24 | −19 | 21 | −25 |
| YLDs | 814,068 | 887,083 | 123 | 149 | 43 | −8 | 60 | −5 |
| Respiratory | ||||||||
| Deaths | 266,726 | 267,516 | 31 | 42 | 45 | −13 | 35 | −26 |
| DALYs | 7,194,419 | 7,098,388 | 1071 | 1230 | 36 | −10 | 27 | −19 |
| YLLs | 4,246,822 | 4,676,676 | 580 | 780 | 32 | −18 | 23 | −26 |
| YLDs | 2,947,596 | 2,421,712 | 492 | 451 | 41 | 3 | 34 | −3 |
| Diabetes | ||||||||
| Deaths | 144,398 | 139,651 | 19 | 23 | 44 | −13 | 79 | 4 |
| DALYs | 6,517,318 | 6,912,228 | 983 | 1192 | 74 | 10 | 103 | 25 |
| YLLs | 2,981,395 | 3,260,081 | 443 | 562 | 39 | −13 | 72 | 6 |
| YLDs | 3,535,923 | 3,652,146 | 540 | 631 | 121 | 40 | 140 | 48 |
| Mental health | ||||||||
| Deaths | 36,797 | 85,087 | 7 | 16 | 265 | 170 | 133 | 66 |
| DALYs | 16,080,086 | 16,593,291 | 3066 | 3256 | 36 | 7 | 44 | 13 |
| YLLs | 1,514,770 | 3,634,839 | 283 | 703 | 274 | 187 | 131 | 74 |
| YLDs | 14,565,316 | 12,958,451 | 2784 | 2553 | 28 | 1 | 30 | 3 |
| Neurological | ||||||||
| Deaths | 320,043 | 213,129 | 32 | 33 | 184 | 64 | 183 | 56 |
| DALYs | 9,034,920 | 6,673,793 | 1379 | 1194 | 63 | 12 | 71 | 18 |
| YLLs | 3,940,346 | 3,530,235 | 499 | 604 | 128 | 41 | 116 | 39 |
| YLDs | 5,094,574 | 3,143,558 | 880 | 589 | 34 | 1 | 38 | 2 |
| Combined NCDa | ||||||||
| Deaths | 2,403,526 | 2,453,675 | 290 | 397 | 33 | −19 | 37 | −22 |
| DALYs | 72,778,832 | 76,911,040 | 11,483 | 13,637 | 31 | −10 | 34 | −13 |
| YLLs | 43,445,336 | 51,765,764 | 6323 | 8914 | 26 | −19 | 29 | −20 |
| YLDs | 29,333,492 | 25,145,276 | 5160 | 4724 | 39 | 3 | 45 | 6 |
| All NCDb | ||||||||
| Deaths | 2,861,523 | 2,957,614 | 352 | 483 | 36 | −17 | 40 | −19 |
| DALYs | 114,365,000 | 111,767,600 | 18,591 | 20,096 | 32 | −8 | 34 | −10 |
| YLLs | 54,549,380 | 66,001,960 | 8223 | 11,589 | 26 | −17 | 28 | −18 |
| YLDs | 59,815,620 | 45,765,640 | 10,368 | 8507 | 40 | 2 | 44 | 3 |
Combined NCDs, includes the following six groups of conditions: cardiovascular diseases, cancers, chronic respiratory diseases, diabetes, mental and substance-use disorders, neurological conditions.
All NCDs, includes all noncommunicable diseases.
Demographic contributors to an increasing NCD burden
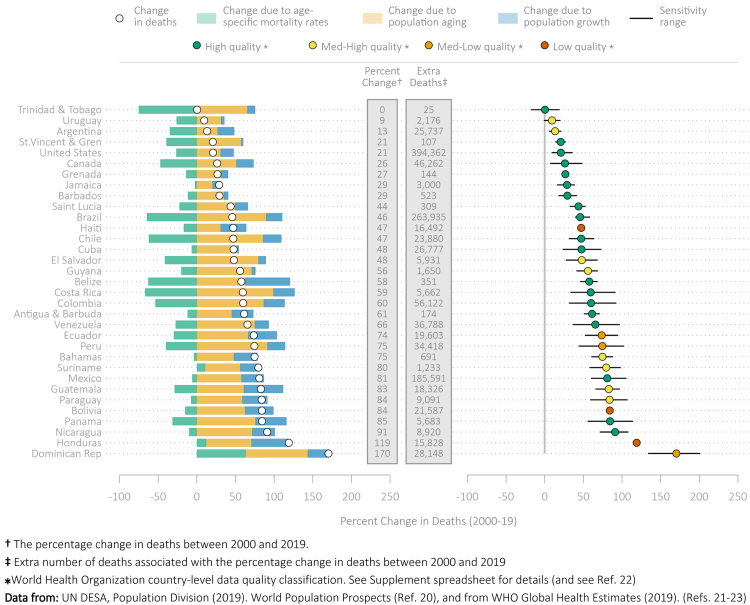
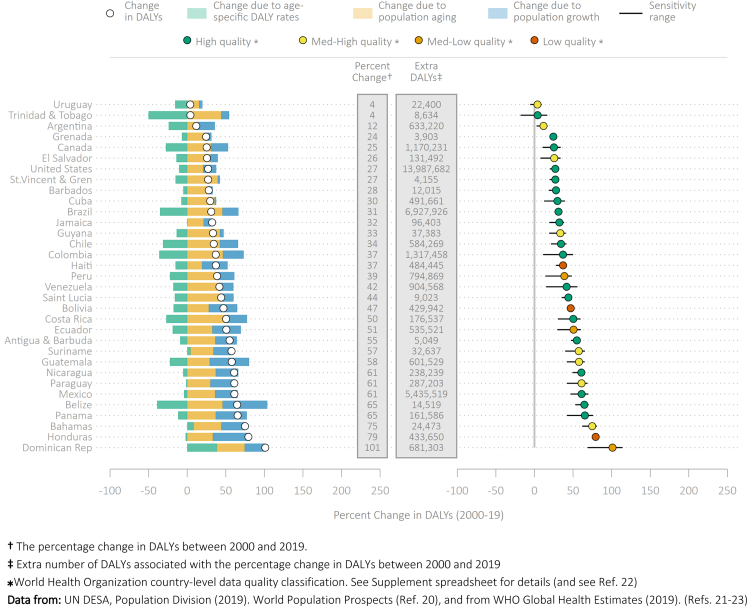
Figs. 3 and 4 present the percentage change in the number of deaths (Fig. 3) and disability years (Fig. 4) due to NCDs (as circles) between 2000 and 2019 for the 33 countries of the Americas. The absolute number of deaths and disability years have increased in the 20-years since 2000 for every country in the region, and there are three broad contributors to this increase: population growth (blue bars), population aging (orange bars), and changes in age-specific rates (green bars). In the Americas, mortality rate improvements alone (i.e., without population aging or population growth) would have decreased the number of deaths by 33.4 percent. This potential improvement has been negated by regional population growth that increased deaths by 21.8 percent, and by regional population aging that increased deaths by 46.6, leading to an overall increase in deaths of 35.0 percent (Sensitivity-based uncertainty range, SR 21.5 to 51.7). The situation for disability was similar. Disability years would have fallen by 18.3 percent because of DALY rate improvements alone. Population growth and aging always negated these potential improvements, so that there was an overall increase in DALYs across the Americas of 32.5 percent (SR 22.7 to 38.3). Population growth across the region increased disability years by 21.8 percent, and population aging increased disability years by 28.9 percent.
Fig. 3.
Contribution of changes in population growth, population aging, and rates of age-specific mortality to the percentage change in mortality due to NCDs, 2000–2019.
Fig. 4.
Contribution of changes in population growth, population aging, and rates of age-specific DALYs to the percentage change in DALYs due to NCDs, 2000–2019.
For almost every country in the region, the number of deaths and the number of DALYs increased between 2000 and 2019. Among women and men combined, the increase in deaths ranged from 0.4 percent in Trinidad and Tobago to 170.3 percent in Dominican Republic, with a typical (median) country increase of 56.8 percent (SR 37.7 to 69.9). The increase in DALYs ranged from 3.9 (SR-5.6 to 9.4) percent in Uruguay and 101.2 percent (95% UI 68.6 to 114.2) in Dominican Republic, with a typical country increase of 37.9 percent (SR 25.4 to 48.0). There were only small differences in these 20-year percentage changes between women and men, with an increase in deaths among women of 32.7 percent (SR 17.7 to 50.5) and among men of 37.3 percent (SR 25.1 to 53.0). The DALY increase among women was 30.1 percent (95% UI 21.2 to 36.5) and among men was 33.8 percent (SR 24.1 to 40.0).
Despite these rather similar percentage change averages between women and men and for mortality and DALY change, there was some evidence for a wider between-country spread of change among women compared to men, and for deaths compared to DALYs (Table 3). The index of disparity for deaths among women was 104.3 (SR 71.5 to 178.1) compared to 85.0 (SR 66.1 to 106.4) among men. The index of disparity for deaths among women and men combined was 92.6 (SR 67.9 to 131.2) compared to 56.8 (SR 50.7 to 76.8) for DALYs.
Discussion
The Americas are aging faster than the world as a whole. Between 1980 and 2060 – roughly the time for two generations of young adults to complete their working lives – the median age in the region is predicted to rise from 19.8 to 43.4 years. The region was below the global average of 22.6 years in 1980, matched the global average of 31.9 years in 2020, and is predicted to exceed the global average of 37.6 years by 2060. Similarly, the proportion of older adults in the Americas is predicted to more than double in the next 40 years, with the old-age dependency ratio rising from 12 in 2020 to 29 in 2060.20
Regional aging is a success story. Our longer lives are a result of public health achievements in reducing many infectious diseases, managing NCDs and enabling healthy living, but also the result of broader economic and educational development. A recent analysis among OECD member states highlighted the importance of health spending, healthier lifestyles, income per capita, and education coverage, with a 10% increase in each resulting in a life expectancy gain of more than 2-months.31 In the Americas, between 2000 and 2019, there have been dramatic declines in NCD mortality rates, notably ischemic heart disease and stroke, falling by 44 and 18 deaths per 100,000 people, respectively. These improvements may be partly ascribed to reductions in smoking rates, improvements in the capacity to control high cholesterol and blood pressure, and in particular greater access to effective care in the event of a heart attack or stroke. Nevertheless, results from the Global Burden of Disease Study suggest that the three leading causes of mortality and DALYs in Latin America and the Caribbean remain high body mass index, high fasting plasma glucose, and high blood pressure.32 Regional tobacco control in the Americas has been guided for the past 15 years by the WHO Framework Convention on Tobacco Control,33 and CVD prevention and control through blood pressure control and secondary CVD prevention – known as the HEARTS initiative.34
These crucial social advances are inexorably tied to aging, and sustained growth of the older population presents profound challenges for healthcare. For most countries in the region, improvements in age-specific mortality rates alone would have led to a decrease in the number of years lived with NCDs, but this potential decrease was always negated by population aging and population growth. Across the Americas, DALY rate reductions would have decreased the number of DALYs by 18 percent between 2000 and 2019, but was offset by a 28 percent increase due to population aging and a 22 percent increase due to population growth. So although the region is enjoying widespread reductions in premature avoidable mortality,35 the increasing number of years lived with NCDs means more healthcare demand. The complexity of healthcare is also set to increase, with multimorbidity likely to become a key challenge for healthcare providers. In the face of increasing and increasingly complex healthcare demand, the move towards universal health coverage (UHC) - with an ultimate goal of maintaining health and avoiding risk factors for all - is an aspirational target for most regional governments. The definition of UHC includes three related dimensions: unfettered access to health services, financial protection when faced with healthcare, and quality healthcare provision that is also cost-effective and sustainable. This UHC goal remains a work in progress across the region, with a recent World Bank report highlighting limited progress towards UHC in many countries, regional variation in that progress, and key vulnerabilities that must be addressed.36 For example, there are recognized bottlenecks of key human and physical resources (doctors, nurses, hospital beds, medical technologies) that limit an effective healthcare response. The level of government healthcare spending in 2017 was estimated at 3.8% of GDP across Latin American and the Caribbean, compared to 6.6% among the OECD countries.31 Alternative estimates from the World Bank in 2019 report healthcare expenditure of 6.4% for Latin America and the Caribbean, compared to 2019 OECD healthcare expenditure of 8.7%.37 Irrespective of estimate, expenditure will vary widely across each region, with for example Cuba spending 10.2% of its GDP on healthcare in 2019, while Haiti spent just 4.1%. Data on quality of care and healthcare inequalities - critical UHC components - remains unavailable for many countries in the Americas.
To date, population growth has accompanied regional aging, and although growth is set to continue for some time, estimates suggest that the population of the Americas will plateau at around 1.2 billion people over the next 30 years, before falling towards the end of the century. Simultaneous population aging and population shrinking intensifies challenges that go beyond healthcare. Formal and informal social systems must support a larger group of older adults without additional resources, limiting the ability of communities and governments to provide resources for older citizens. Nations must quickly recognize this new demographic reality, which requires policy adjustments and resource re-allocation. Experience from OECD nations among others suggest that such adjustments will be painful - changes in retirement ages and medical benefits, for example, are not widely popular. But experience also suggests that it is easier to address problems sooner rather than later, when the cost of waiting may become insurmountable.38
This work draws on international data resources from the UN and the WHO, who invest considerable effort in ensuring cross-country comparability. Nevertheless, the quality of cause-specific mortality data remains a valid concern. Quality can be in terms of data completeness and in terms of accurate allocation of an underlying cause of death when competing causes may lead to misallocation. The use of WHO uncertainty intervals, the WHO categories of mortality evidence, and our associated sensitivity-based uncertainty remind us of the inherent uncertainty when using collated mortality and morbidity and help us to avoid over-interpretation of country-level differences and detailed country rankings. In addition to these uncertainty intervals, the WHO data source methodology provides comprehensive information on methods for assessing country-level data quality.22 The risk of overinterpreting global health estimates have been recognized and discussed previously.39
We draw on data that is exclusively at the country-level, stratified by age and sex. This allows us to explore country-level inequalities in population aging and health outcomes. However, country-level analyses mask the many within-country health inequalities, which are driven by the social determinants of disease, such as race and ethnicity, occupation, gender, religion, education, socioeconomic status, and social capital. Our analysis stratifies by biological sex and is not able to explore gender-based health inequalities.
These data do not include the mortality effects of the COVID-19 pandemic, which led to massive mortality across the Americas in 2020 and 2021, with provisional mortality rates regularly exceeding 100 per 100,000 by 2022 –the crude rate in Brazil was above 300 per 100,000 and in Peru was above 600 – and a burden that disproportionately affected the elderly.40,41 By most estimates, the loss of life has led to a sharp decrease in life expectancy globally.42 Without major future outbreaks, we would expect life expectancy to recover as the deaths of those lives prematurely lost during the pandemic would not figure in future mortality tables. However, it is also clear that it is the wider context of the pandemic which will have longer implications, for example on people's health-seeking behaviors, and on health system support.
Conclusion
Major public health achievements contribute to healthier and longer lives, reducing premature avoidable mortality – commonly classified as a death from a preventable cause before 65 or 70 years of age – and shifting mortality to later life. The extent to which longer lives are lived in good health or with illness is fundamentally important for health system planners, who must understand the healthcare implications of an aging population with potentially longer-term illness and complex multimorbidity. The demographic realities of population growth and population aging should be factored into healthcare planning, to understand their implications for the future NCD burden, health system needs, and the ability of governments and communities to respond to those needs.
Contributors
IRH conceived the study. All authors designed the study. RC, SL, AH provided the curated dataset. IRH analyzed the study and created the study visualizations. IRH and SJ wrote the first manuscript draft. All authors provided critical feedback during the analysis phase and contributed to subsequent manuscript drafts. All authors read and approved the final version of the manuscript.
Data sharing statement
Data used in this article are freely available for download at the following locations. Population data: United Nations World Population Prospects (2019 revision), available at https://population.un.org/wpp/.Health data. World Health Organization Global Health Estimates (2019), available at https://www.who.int/data/gho/data/themes/mortality-and-global-health-estimates. Only aggregated, anonymized data are used.
Declaration of interests
The authors declared no conflicts of interest.
Acknowledgements
This work was funded in part by the Pan American Health Organization, Department of Noncommunicable Diseases and Mental Health.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lana.2023.100483.
Appendix A. Supplementary data
References
- 1.Omran A.R. The epidemiologic transition. A theory of the epidemiology of population change. Milbank Mem Fund Q. 1971;49(4):509–538. [PubMed] [Google Scholar]
- 2.Mackenbach J.P. The contribution of medical care to mortality decline: McKeown revisited. J Clin Epidemiol. 1996;49(11):1207–1213. doi: 10.1016/s0895-4356(96)00200-4. [DOI] [PubMed] [Google Scholar]
- 3.Bloom D.E., Canning D. Commentary: the Preston Curve 30 years on: still sparking fires. Int J Epidemiol. 2007;36(3):498–499. doi: 10.1093/ije/dym079. discussion 502-3. [DOI] [PubMed] [Google Scholar]
- 4.Boutayeb A. The double burden of communicable and non-communicable diseases in developing countries. Trans R Soc Trop Med Hyg. 2006;100(3):191–199. doi: 10.1016/j.trstmh.2005.07.021. [DOI] [PubMed] [Google Scholar]
- 5.Pan American Health Organization . PAHO; Washington, D.C.: 2014. Plan of action for the prevention and control of noncommunicable diseases in the Americas 2013-2019.https://iris.paho.org/handle/10665.2/35009 [Google Scholar]
- 6.United Nations . Sixty-sixth session of the united nations general assembly; 2011 Sep 19-Dec 19; New York (NY), US. United Nations; New York: 2011. Political Declaration of the high-level meeting of the General Assembly on the prevention and control of noncommunicable diseases.https://digitallibrary.un.org/record/710899/?ln=en (Resolution A/RES/66/2). [Google Scholar]
- 7.de Lacy-Vawdon C., Livingstone C. Defining the commercial determinants of health: a systematic review. BMC Publ Health. 2020;20(1):1022. doi: 10.1186/s12889-020-09126-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization, Commission on Social Determinants of Health . WHO; Geneva: 2008. Closing the gap in a generation: health equity through action on the social determinants of health.https://www.who.int/publications/i/item/WHO-IER-CSDH-08.1 CSDH final report. [DOI] [PubMed] [Google Scholar]
- 9.World Health Organization . World Health Organization; 2017. Tackling NCDs: 'best buys' and other recommended interventions for the prevention and control of noncommunicable diseases.https://apps.who.int/iris/handle/10665/259232. License: CC BY-NC-SA 3.0 IGOhttps://apps.who.int/iris/handle/10665/259232 [Google Scholar]
- 10.Sustainable Development Goal 3 Ensure healthy lives and promote well-being for all at all ages. Progress Inform. 2018 https://sustainabledevelopment.un.org/sdg3 [Google Scholar]
- 11.World Health Organization Global Action Plan for the prevention and control of noncommunicable diseases, 2013-2020. 2013. https://www.who.int/nmh/events/ncd_action_plan/en/
- 12.Sacco R.L., Roth G.A., Reddy K.S., et al. The heart of 25 by 25: achieving the goal of reducing global and regional premature deaths from cardiovascular diseases and stroke: a modeling study from the American heart association and world heart federation. Circulation. 2016;133(23):e674–e690. doi: 10.1161/CIR.0000000000000395. [DOI] [PubMed] [Google Scholar]
- 13.World cancer declaration progress report Tomorrow is now: our journey to 2025. 2016. https://www.uicc.org/wcd-report
- 14.NCD Alliance Ensuring healthy lives for all: noncommunicable diseases and universal health coverage. https://ncdalliance.org/resources/ensuring-healthy-lives-for-all-ncds-and-uhc
- 15.Living well for longer: national support for local action to reduce premature avoidable mortality. UK Government; 2014. The reducing premature mortality programme in the department of health.https://www.gov.uk/government/publications/helping-people-live-well-for-longer PHD/IHPHPS/RAMP/12341. [Google Scholar]
- 16.Fries J.F. The compression of morbidity. Ann Acad Med Singap. 1983;12(3):358–367. [PubMed] [Google Scholar]
- 17.Fries J.F., Bruce B., Chakravarty E. Compression of morbidity 1980-2011: a focused review of paradigms and progress. J Aging Res. 2011;2011 doi: 10.4061/2011/261702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.de Andrade L.O., Pellegrini Filho A., Solar O., et al. Social determinants of health, universal health coverage, and sustainable development: case studies from Latin American countries. Lancet (London, England) 2015;385(9975):1343–1351. doi: 10.1016/S0140-6736(14)61494-X. [DOI] [PubMed] [Google Scholar]
- 19.Moffat K., Mercer S.W. Challenges of managing people with multimorbidity in today's healthcare systems. BMC Fam Pract. 2015;16:129. doi: 10.1186/s12875-015-0344-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.United Nations, Department of Economic and Social Affairs, Population Division . United Nations; New York: 2019. World population Prospects: the 2019 revision, methodology of the united nations population estimates and projections.https://population.un.org/wpp/Publications/Files/WPP2019_Methodology.pdf Working Paper No. ST/ESA/SER.A/425. [Google Scholar]
- 21.World Health Organization The global health observatory. Global health estimates: life expectancy and leading causes of death and disability. https://www.who.int/data/gho/data/themes/mortality-and-global-health-estimates
- 22.World Health Organization, Department of Data and Analytics (DNA), Division of Data, Analytics, and Delivery for Impact (DDI) WHO methods and data sources for country-level causes of death 2000-2019. https://cdn.who.int/media/docs/default-source/gho-documents/global-health-estimates/ghe2019_cod_methods.pdf?sfvrsn=37bcfacc_5 Global Health Estimates Technical Paper WHO/DDI/DNA/GHE/2020.2.
- 23.World Health Organization, Department of Data and Analytics (DNA), Division of Data, Analytics, and Delivery for Impact (DDI) WHO methods and data sources for global burden of disease estimates 2000-2019. https://cdn.who.int/media/docs/default-source/gho-documents/global-health-estimates/ghe2019_daly-methods.pdf?sfvrsn=31b25009_7 Global Health Estimates Technical Paper WHO/DDI/DNA/GHE/2020.3.
- 24.United Nations General Assembly . United Nations General Assembly; 2011. Political declaration of the high-level meeting of the general assembly on the prevention and control of non-communicable diseases. A66/L.I. [Google Scholar]
- 25.United Nations General Assembly . United Nations General Assembly; 2018. Political declaration of the third high-level meeting of the General Assembly on the prevention and control of non-communicable diseases. A/73/L.2. [Google Scholar]
- 26.U.S. Department of Health and Human Services. National Cancer Institute World (WHO 2000-2025) Standard. https://seer.cancer.gov/stdpopulations/world.who.html
- 27.United Nations Statistics Division UNdata: a world of information. https://data.un.org/Glossary.aspx Glossary.
- 28.Roth G.A., Forouzanfar M.H., Moran A.E., et al. Demographic and epidemiologic drivers of global cardiovascular mortality. N Engl J Med. 2015;372(14):1333–1341. doi: 10.1056/NEJMoa1406656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.World Health Organization Handbook on Health inequality monitoring with a special focus on low- and middle-income countries. 2013. https://www.who.int/data/inequality-monitor/handbook
- 30.StataCorp . vol. 17. StataCorp LLC; College Station, TX: 2021. Stata statistical software: release. [Google Scholar]
- 31.OECD/The World Bank . OECD Publishing; Paris: 2020. Health at a glance: Latin America and the caribbean 2020. [DOI] [Google Scholar]
- 32.Collaborators G.B.D.R.F. Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet (London, England) 2020;396(10258):1223–1249. doi: 10.1016/S0140-6736(20)30752-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pan American Health Organization . WHO framework convention on tobacco control: 10 years later. PAHO; Washington, DC: 2016. Report on tobacco control for the region of the Americas. [Google Scholar]
- 34.HEARTS in the Americas: guide and essentials for implementation. Pan American Health Organization; Washington, D.C.: 2022. License: CC BY-NC-SA 3.0 IGO. [DOI] [Google Scholar]
- 35.Pan-American Health Organization Health in the Americas. Potentially avoidable premature mortality (PAPM) https://hia.paho.org/en/avoidable-mortality#:∼:text=Although%20advances%20in%20public%20health,2019%2C%20the%20latest%20available%20data
- 36.OECD . OECD Publishing; Paris: 2015. Cardiovascular disease and diabetes: policies for better health and quality of care, OECD health policy studies. [Google Scholar]
- 37.OECD. Health at a glance. 2021. p. 2021.https://www.oecd-ilibrary.org/content/publication/ae3016b9-en [Google Scholar]
- 38.National Institute on Aging. National institues of health. U.S. Department of Health and Human Services, U.S. Department of State . 2007. Why population aging matters. A global perspective. [Google Scholar]
- 39.Agyepong I., Corrah T., Guo Y., et al. Making sense of health estimates. Lancet (London, England) 2015;385(9976):1377–1379. doi: 10.1016/S0140-6736(15)60024-1. [DOI] [PubMed] [Google Scholar]
- 40.Harper S. The impact of the Covid-19 pandemic on global population ageing. J Popul Ageing. 2021;14(2):137–142. doi: 10.1007/s12062-021-09330-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020;20(5):533–534. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Woolf S.H., Masters R.K., Aron L.Y. Changes in life expectancy between 2019 and 2020 in the US and 21 peer countries. JAMA Netw Open. 2022;5(4) doi: 10.1001/jamanetworkopen.2022.7067. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.