Abstract
OBJECTIVE
The current study aims to prospectively examine the association between postdiagnosis low-carbohydrate diet (LCD) patterns and mortality among individuals with type 2 diabetes (T2D).
RESEARCH DESIGN AND METHODS
Among participants with incident diabetes identified in the Nurses’ Health Study and Health Professionals Follow-up Study, an overall total LCD score (TLCDS) was calculated based on the percentage of energy as total carbohydrates. In addition, vegetable (VLCDS), animal (ALCDS), healthy (HLCDS), and unhealthy (ULCDS) LCDS were further derived that emphasized different sources and quality of macronutrients. Multivariable-adjusted Cox models were used to assess the association between the LCDS and mortality.
RESULTS
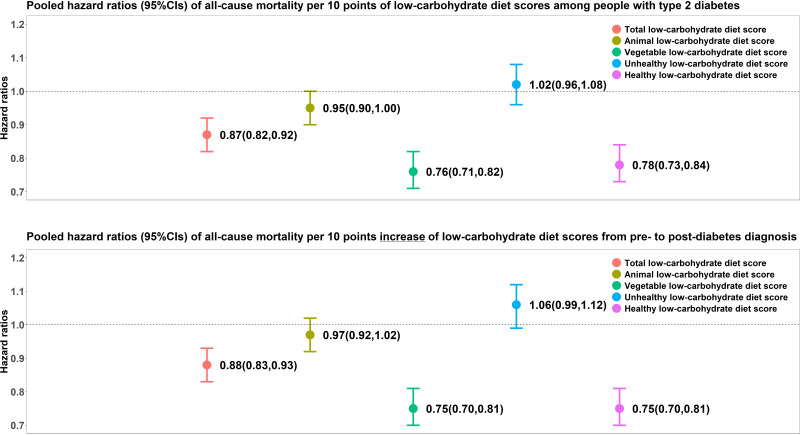
Among 10,101 incident T2D cases contributing 139,407 person-years during follow-up, we documented 4,595 deaths of which 1,389 cases were attributed to cardiovascular disease (CVD) and 881 to cancer. The pooled multivariable-adjusted hazard ratios (HRs, 95% CIs) of total mortality per 10-point increment of postdiagnosis LCDS were 0.87 (0.82, 0.92) for TLCDS, 0.76 (0.71, 0.82) for VLCDS, and 0.78 (0.73, 0.84) for HLCDS. Both VLCDS and HLCDS were also associated with significantly lower CVD and cancer mortality. Each 10-point increase of TLCDS, VLCDS, and HLCDS from prediagnosis to postdiagnosis period was associated with 12% (7%, 17%), 25% (19%, 30%), and 25% (19%, 30%) lower total mortality, respectively. No significant associations were observed for ALCDS and ULCDS.
CONCLUSIONS
Among people with T2D, greater adherence to LCD patterns that emphasize high-quality sources of macronutrients was significantly associated with lower total, cardiovascular, and cancer mortality.
Graphical Abstract
Introduction
The disruption of glucose metabolism is central to the pathogenesis of type 2 diabetes (T2D) (1). Among patients with T2D, insulin resistance leads to persistently elevated blood glucose levels upon the intake of carbohydrates, resulting in occurrence of many comorbidities; as such, carbohydrate restriction is recommended to ameliorate hyperglycemia in patients with diabetes (2,3). Although the macronutrient distributions are suggested to be based on an individualized assessment of current eating patterns, preferences, and metabolic goals in patients with diabetes, the American Diabetes Association (ADA) recognizes potential beneficial effects of reducing overall carbohydrate intake on improving glycemia (4). Dietary intervention studies have suggested overall beneficial effects of a low-carbohydrate diet (LCD) on promoting weight loss and improving cardiovascular risk factors, including HbA1c, blood glucose, and triglycerides, among people with established T2D (5). Recent systematic reviews and meta-analyses of short-term dietary intervention studies concluded that dietary carbohydrate restriction was effective in T2D management (6). However, long-term randomized controlled trials and prospective observational studies that examine the long-term effects of an LCD on health outcomes among individuals with diabetes are lacking. Meanwhile, in the general population, LCDs that emphasize animal products versus plant-based foods or LCDs that consist of different sources of fats and proteins demonstrated divergent associations with mortality (7,8). It is unclear whether these different LCDs might be differentially associated with the health consequences among those with T2D.
In light of these knowledge gaps, the purpose of the current study was to examine the associations between multiple LCD scores (LCDS) and all-cause, cardiovascular disease (CVD), and cancer mortality among individuals with T2D. We leveraged data from two prospective cohorts of U.S. men and women with validated food frequency questionnaire (FFQ) data repeatedly assessed over 30 years to compute five LCDS emphasizing different sources of macronutrients. We also evaluated the changes of LCDS from the prediagnosis to postdiagnosis period in relation to mortality. In secondary analyses, we examined the joint associations between LCD adherence and postdiagnosis lifestyle factors and assessed the substitution effects on mortality of replacing fat and protein with different sources of carbohydrates.
Research Design and Methods
Study Population
The Nurses’ Health Study (NHS) is a prospective cohort established in 1976 and consists of 121,700 registered female nurses between 30 and 55 years of age at baseline (9). The Health Professionals Follow-up Study (HPFS) is a prospective cohort established in 1986 and consists of 51,529 male health professionals between 40 and 75 years of age at baseline (10). Biennial questionnaires on lifestyle and medical history were administered to participants.
The current study considered only participants who developed T2D during the follow-up, and we excluded participants with prevalent diabetes (n = 1,539 in NHS and 1,637 in HPFS) at study baselines, which were 1980 for NHS and 1986 for HPFS. In a sensitivity analysis, we included participants with prevalent T2D at baseline as well. We also excluded participants with prevalent CVD or cancer (n = 2,207 in NHS and 5,441 in HPFS), participants who completed the baseline questionnaire only (n = 694 in NHS and 653 in HPFS), participants who had missing data on LCDS (n = 30,205 time-dependent exclusions from all cycles in NHS and 11,256 time-dependent exclusions from all cycles in HPFS), and participants who developed CVD or cancer before the occurrence of T2D (n = 1,474 in NHS and 402 in HPFS). After exclusions, there were 2,877 men and 7,224 women included in the final analysis. The study protocol was approved by the institutional review boards of the Brigham and Women’s Hospital and Harvard T.H. Chan School of Public Health, and those of participating registries as required.
Assessment of LCDS
Diet was assessed by a validated FFQ every 4 years starting in 1980 and 1986 in the NHS and HPFS, respectively. The energy-adjusted deattenuated Spearman correlations between macronutrients intake assessed by 7-day diet records and the semiquantitative FFQ are 0.69 for total carbohydrates, 0.54 for protein, and 0.67 for fat with reasonable reproducibility over time (r = 0.63–0.66) (11). Daily nutrient and energy intakes were calculated by multiplying the frequency of intake by the nutrient and energy content and summing the products across all food items.
We derived five LCDS which reflected different compositions and quality of macronutrients. Based on the percentage contributions to total energy, the intakes of fat and protein were ranked into 11 equal-sized categories in ascending order, while carbohydrate intake level was ranked in the same way but in descending order (12,13). The carbohydrate categories were scored from 10 (lowest intake) to 0 (highest intake), whereas protein and fat categories were scored from 0 (lowest intake) to 10 (highest intake). We then summed the rank from three macronutrients to create the total LCDS (TLCDS). Animal LCDS (ALCDS) and vegetable LCDS (VLCDS) were calculated in the same manner but using animal fat/protein and vegetable fat/protein instead of total fat/protein. Two additional LCDS were created to further account for the quality of carbohydrates (8). The unhealthy LCDS (ULCDS) was derived by summing the rank of animal protein, the rank of animal fat, and the reverse rank of high-quality carbohydrates which were defined as the sum of carbohydrate intake from nonstarchy vegetables (excluding potatoes and French fries), fruits (excluding added sugar from fruit juice), legumes, and whole grains. Conversely, the healthy LCDS (HLCDS) was calculated as the sum of rank of vegetable protein, rank of vegetable fat, and reverse rank of low-quality carbohydrates defined as the sum of carbohydrates from potato, added sugar, and refined grain from foods. All LCDS had a range of 0 (highest carbohydrates intake) to 30 (lowest carbohydrates intake).
Ascertainment of T2D and Deaths
T2D was ascertained using a supplementary questionnaire sent to those who reported the diagnosis and confirmed by study physicians who were unaware of the study hypothesis. We used the National Diabetes Data Group criteria for cases identified before 1998 and the ADA criteria for cases after 1998 (14,15). Validation studies showed that 97% of participants with self-reported T2D confirmed by the questionnaire were reconfirmed by review of medical records (16,17).
The study outcomes were all-cause, CVD, and cancer mortality after T2D diagnosis. Deaths occurring throughout the study period were identified from vital records, the National Death Index, and reports by the participants’ next of kin or postal service (18). More than 97% of deaths were identified in two cohorts. Cause of death was identified from death certifications or review of medical records. Cardiovascular and cancer deaths were determined by study physicians’ review of medical records and death certificates with diagnostic codes of the International Classification of Diseases, 9th Revision.
Assessment of Covariates
The information on lifestyle factors and disease status including age, smoking status, vitamin supplements use, family history of diabetes, cancer, and myocardial infarction, stroke, alcohol consumption, body weight, menopausal status and hormone use (NHS only), physician diagnosed hypertension and hypercholesterolemia, and other variables was updated through a biennial follow-up questionnaire since baseline in two cohorts. BMI was calculated as weight in kilograms divided by the square of height in meters. Physical activities were repeatedly assessed in both cohorts, and the metabolic equivalent tasks in hours per week were calculated to represent the total physical activity level (19). Overall diet quality was assessed using the Alternative Health Eating Index (AHEI) score (20).
Statistical Analysis
Age-standardized characteristics at diabetes diagnosis are presented according to quintiles of TLCDS as means (SD) or frequencies. We cumulatively averaged the LCDS after the diabetes diagnosis to reflect the long-term postdiagnosis diet. Prediagnosis LCDS were calculated from the most recent FFQ before T2D diagnosis, and the change in LCDS was defined as the absolute difference between time-varying postdiagnosis LCDS and prediagnosis LCDS.
The person-time was calculated from the date of the postdiagnosis questionnaire return to death or the end of the study period, set at 30 June 2018 for NHS and 31 January 2018 for HPFS. To assess the association between LCDS and postdiagnosis survival, we estimated hazard ratios (HRs) and 95% CIs using age (years)– and calendar year–stratified Cox proportional hazards models that adjusted for race (White, African American, Asian, others), total energy (quintile), physical activity (quintile), alcohol intake (0, 0.1–4.9, 5.0–9.9, 10.0–14.9, 15.0–29.9, and ≥30.0 g/d), prediagnosis AHEI (quintile), smoking status (never smoked; past smoker; currently smoke 1–14 cigarettes per day, 15–24 cigarettes per day, or ≥25 cigarettes per day), prediagnosis BMI (<21.0, 21.0–22.9, 23.0–24.9, 25.0–26.9, 27.0–29.9, 30.0–32.9, 33.0–34.9, or ≥35.0 kg/m2), multivitamin use (yes, no), family history of diabetes (yes, no), family history of myocardial infarction (yes, no), family history of cancer (yes, no), diabetes duration (0–5 years, 5.1–10 years, 10.1–15 years, >15 years), time interval between diagnosis date and latest postdiagnosis FFQ return date (months), menopausal hormone use (women only; premenopausal, never, former, current, or missing), oral hypoglycemic drug use (women only; yes, no), and insulin use (women only; yes, no). We also conducted cubic spline regressions for each LCDS to characterize potential nonlinear associations with all-cause mortality, while CVD mortality and cancer mortality were not analyzed because of insufficient statistical power. All LCDS and change of LCDS were categorized into quintiles according to cohort-specific distributions, and the median values in each quintile were used for calculating P values for trend. The interaction terms between each categorical LCDS and duration of follow-up calculated as months from postdiagnosis FFQ return date to death or the end of follow-up were additionally included in the Cox models to test the proportional hazards assumptions, and we did not detect any violations in the analyses. The time-varying covariates were adjusted in all analyses except that changes in these covariates from prediagnosis to postdiagnosis follow-up cycle (time-invariant) were adjusted for in change analysis. The prediagnosis LCDS were additionally adjusted in the change analysis to ensure the results were comparable among participants with diabetes with different LCD adherence statuses before diagnosis. Data from two cohorts were combined to maximize the statistical power.
In a secondary analysis, we evaluated the joint associations between LCDS and the number of postdiagnosis low-risk lifestyle factors. We defined three low-risk lifestyle factors in the first follow-up cycle after diabetes diagnosis (21): noncurrent smoking, moderate to vigorous physical activity (≥7.5 METs h/week), and moderate alcohol consumption (5–15 g/day for women and 5–30 g/day for men). All three factors were dichotomized and summed up to create the number of postdiagnosis low-risk lifestyle factors, which had a range from zero to three. Because only 4% of the participants had zero low-risk lifestyle factors in the two cohorts combined, the zero and one low-risk lifestyle factors groups were collapsed to preserve statistical power. We categorized the number of postdiagnosis low-risk lifestyle factor into three groups: zero to one, two, and three, and calculated the HRs (95% CIs) in each category from the product terms between these categories with continuous LCDS. Another secondary analysis was conducted by stratifying the presence of diabetes symptoms and diabetes drug use to examine whether the disease severity may modify the associations between LCDS and all-cause mortality. The presence of diabetes symptoms was defined as having reported any diabetes-related symptoms including ketoacidosis; coma; unintended weight loss; unusual hunger, thirst, or frequency of urination; and pruritus of vulva. Diabetes drug use status was categorized into four levels: no drug use, oral hypoglycemic drug use only, insulin use only, and oral hypoglycemic drug and insulin use. The P values for interaction in all secondary analyses were calculated using the Wald test. We further conducted a substitution analysis replacing 5% of energy from refined carbohydrates including potato, added sugar, and refined grain with vegetable fat or vegetable protein. The substitution model simultaneously included total energy, animal fat, animal protein, vegetable fat, vegetable protein, and total carbohydrates minus the low-quality carbohydrates being replaced (22).
We conducted several sensitivity analyses to assess the robustness of the primary findings. First, we reanalyzed the data including participants with prevalent T2D at baseline. Second, the time-varying change of covariates was adjusted in the change analysis. Finally, deaths that occurred within 5 years of diabetes diagnosis were excluded to account for potential reverse causality. Data were analyzed using SAS version 9.4 (SAS Institute) and R software (version 4.1.1), at a two-tailed α level of 0.05.
Results
The study population consisted of 10,101 individuals with incident T2D who accrued 139,407 person-years of follow-up. A total of 4,595 deaths were observed, including 1,389 CVD deaths and 881 cancer deaths. Table 1 shows the age-standardized characteristics of study participants at diabetes diagnosis according to postdiagnosis TLCDS. On average, participants having higher TLCDS at diagnosis tended to be younger, were more likely to be male and current nonsmokers, and had higher alcohol consumption, total energy intake, and prediagnosis BMI and TLCDS. The distributions of other variables were similar across quintiles of postdiagnosis TLCDS.
Table 1.
Age-standardized characteristics of study participants according to postdiagnosis TLCDS at T2D diagnosis in NHS (1980–2018) and HPFS (1986–2018)
| TLCDS | ALCDS | VLCDS | ULCDS | HLCDS | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Q1 | Q5 | Q1 | Q5 | Q1 | Q5 | Q1 | Q5 | Q1 | Q5 | |
| Number of participants with T2D | 2,074 | 1,832 | 1,915 | 2.134 | 2,219 | 2,255 | 2,016 | 1,799 | 2,096 | 1,866 |
| Postdiagnosis TLCDS | 7.6 (3.0) | 27.1 (1.7) | 6.3 (3.0) | 27.3 (1.7) | 8.5 (2.5) | 23.9 (2.5) | 6.5 (2.9) | 26.2 (1.9) | 8.6 (2.5) | 24.9 (2.4) |
| Prediagnosis TLCDS | 12.6 (7.0) | 19.6 (6.7) | 12.1 (7.5) | 20.3 (7.0) | 12.3 (5.2) | 17.5 (5.4) | 12.3 (6.9) | 20.7 (5.9) | 11.5 (5.1) | 17.5 (5.5) |
| Age at diagnosis, years | 65.4 (9.1) | 61.5 (8.3) | 65.3 (8.9) | 61.8 (8.4) | 65.3 (9.1) | 63.1 (8.2) | 65.4 (8.6) | 61.9 (8.8) | 64.6 (9.3) | 64.1 (8.0) |
| Male, % | 25.4 | 34.2 | 25.8 | 32.6 | 25.7 | 29.3 | 26.7 | 33.6 | 28.6 | 30.3 |
| Race | ||||||||||
| White, % | 93.3 | 96.3 | 92.5 | 96.6 | 95.1 | 95.5 | 92.8 | 96.6 | 94.8 | 94.7 |
| African American, % | 2.1 | 1.3 | 2.0 | 1.4 | 1.6 | 1.2 | 2.1 | 1.1 | 1.7 | 1.7 |
| Asian, % | 2.8 | 1.1 | 3.1 | 1.1 | 1.5 | 1.6 | 2.9 | 1.2 | 1.9 | 1.6 |
| Others, % | 1.8 | 1.2 | 2.4 | 1.0 | 1.8 | 1.6 | 2.2 | 1.1 | 1.6 | 2.0 |
| Prediagnosis BMI (kg/m2) | 30.1 (5.7) | 31.2 (5.8) | 29.8 (5.6) | 31.6 (5.9) | 31 (5.9) | 30.3 (5.7) | 29.6 (5.5) | 31.8 (6.0) | 31.4 (6.1) | 29.7 (5.4) |
| Physical activity (MET-h/week)* | 8.8 (2.7, 22.2) | 9 (2.4, 22.8) | 9.6 (2.9, 23.4) | 7.7 (1.9, 20.8) | 7.9 (2.1, 20.7) | 11 (3.2, 25.8) | 11.2 (3.4, 26.5) | 6.7 (1.6, 18.5) | 6.8 (1.5, 17.9) | 13.7 (4.2, 29.5) |
| Hypertension, % | 73.0 | 73.4 | 72.3 | 74.2 | 75.5 | 72.3 | 71.6 | 75.9 | 76.7 | 70.6 |
| High cholesterol, % | 71.7 | 68.7 | 73.2 | 67.4 | 68.4 | 73.8 | 74.0 | 69.6 | 71.1 | 73.1 |
| Smoking status | ||||||||||
| Never smokers, % | 45.4 | 36.7 | 44.7 | 38.0 | 44.8 | 38.1 | 43.4 | 38.9 | 41.6 | 39.6 |
| Past smokers, % | 46.5 | 55.1 | 48.1 | 53.7 | 46.8 | 54.3 | 50.3 | 52.0 | 49.0 | 53.5 |
| Current smokers, % | 8.0 | 8.1 | 7.2 | 8.3 | 8.4 | 7.6 | 6.3 | 9.2 | 9.4 | 6.8 |
| Family history of diabetes, % | 46.6 | 46.6 | 47.1 | 46.9 | 46.9 | 47.8 | 47.4 | 46.5 | 45.0 | 47.8 |
| Family history of myocardial infarction, % | 20.2 | 20.4 | 19.6 | 20.1 | 20.6 | 20.0 | 19.3 | 20.2 | 19.7 | 18.4 |
| Family history of cancer, % | 36.2 | 35.4 | 37.3 | 36.1 | 37.0 | 37.6 | 36.3 | 35.0 | 36.4 | 37.8 |
| Multivitamin use, % | 55.9 | 58.0 | 57.4 | 54.9 | 55.1 | 61.9 | 59.0 | 53.7 | 53.0 | 64.4 |
| Oral hypoglycemic drug use, %† | 44.9 | 52.7 | 45.3 | 54.6 | 47.8 | 51.3 | 45.0 | 52.9 | 50.0 | 48.9 |
| Insulin use, %† | 4.8 | 5.7 | 4.5 | 6.0 | 5.3 | 5.3 | 4.8 | 5.4 | 5.5 | 4.8 |
| Postmenopausal hormone use† | ||||||||||
| Premenopausal, % | 6.1 | 6.7 | 6.4 | 6.3 | 6.2 | 6.6 | 6.1 | 6.5 | 6.2 | 6.1 |
| Postmenopausal-never, % | 32.9 | 28.4 | 32.7 | 30.6 | 33.9 | 28.5 | 32.3 | 31.7 | 33.1 | 28.3 |
| Postmenopausal-current, % | 19.5 | 19.3 | 19.2 | 18.6 | 18.2 | 20.0 | 19.3 | 17.1 | 18.9 | 20.0 |
| Postmenopausal-past, % | 41.5 | 45.7 | 41.7 | 44.6 | 41.7 | 44.9 | 42.3 | 44.8 | 41.7 | 45.5 |
| Prediagnosis AHEI | 50.6 (9.6) | 50.3 (9.9) | 51.9 (9.8) | 48.7 (9.3) | 48.3 (9.5) | 53 (9.7) | 53.9 (9.7) | 46.8 (9.0) | 45.8 (8.9) | 55.2 (9.4) |
| Alcohol consumption (g/day)* | 0.6 (0, 3.1) | 1.1 (0.1, 3.8) | 0.7 (0, 3.1) | 1.1 (0.1, 4) | 0.7 (0, 2.9) | 1.1 (0.1, 4) | 0.7 (0, 3.5) | 1.1 (0.2, 3.7) | 0.8 (0, 3.5) | 0.9 (0, 3.7) |
| Total energy intake (Kcal/day) | 1,752 (457) | 1,796 (477) | 1,757 (462) | 1,791 (468) | 1,746 (449) | 1,800 (477) | 1,744 (454) | 1,823 (471) | 1,823 (471) | 1,761 (469) |
| Macronutrients, % of total energy | ||||||||||
| Total carbohydrates | 59.5 (5.5) | 38.7 (5.8) | 58.6 (6.5) | 40.2 (6.2) | 54.4 (8.4) | 44.4 (6.3) | 56.7 (7.9) | 40.7 (7.0) | 50.2 (8.6) | 47.2 (8.2) |
| High-quality carbohydrates | 17.7 (6.1) | 13.7 (4.8) | 17.9 (6.1) | 13.2 (4.4) | 15.8 (5.4) | 15.5 (5.1) | 19.2 (5.7) | 11.8 (3.8) | 12.9 (4.4) | 18 (5.6) |
| Low-quality carbohydrates | 24 (5.8) | 20.7 (5.1) | 24.1 (5.6) | 20.9 (5.1) | 22.8 (5.8) | 21.9 (5.1) | 22.5 (5.2) | 22.3 (5.3) | 24.8 (5.8) | 20.4 (4.6) |
| Total fat | 30.4 (4.6) | 36.9 (4.8) | 31 (4.8) | 36.5 (4.6) | 31.5 (4.8) | 35.5 (4.9) | 31 (4.9) | 36.6 (4.6) | 33.5 (4.8) | 33.9 (5.2) |
| Vegetable fat | 13 (3.5) | 14.6 (3.8) | 14.3 (3.9) | 13.5 (3.4) | 11.5 (2.9) | 16.7 (3.6) | 14.6 (4.0) | 13.6 (3.4) | 12.4 (3.2) | 16.3 (3.9) |
| Animal fat | 17.5 (4.5) | 22.3 (5.3) | 16.7 (4.5) | 23 (4.8) | 20 (4.9) | 18.7 (4.8) | 16.5 (4.6) | 23 (4.8) | 21.1 (4.9) | 17.7 (4.8) |
| Total protein | 17.8 (2.5) | 20.1 (2.6) | 17.6 (2.4) | 20.1 (2.7) | 18.9 (2.9) | 18.8 (2.5) | 18 (2.4) | 19.7 (2.6) | 18.5 (2.8) | 19.1 (2.5) |
| Vegetable protein | 5.2 (1.0) | 4.8 (1.0) | 5.5 (1.1) | 4.6 (0.8) | 4.6 (0.8) | 5.4 (0.9) | 5.6 (1.1) | 4.5 (0.7) | 4.4 (0.7) | 5.7 (1.0) |
| Animal protein | 12.6 (2.6) | 15.3 (2.8) | 12.2 (2.6) | 15.5 (2.8) | 14.3 (3.0) | 13.4 (2.6) | 12.4 (2.6) | 15.2 (2.8) | 14 (2.9) | 13.4 (2.7) |
Values are means (SD) for continuous variables or otherwise indicated, or percentages (%) for categorical variables. Q, quintile.
Values are medians (interquartile range).
Only available in women.
Pooled multivariable-adjusted HRs (95% CIs) of mortality and low-carbohydrate scores are shown in Table 2. Comparing extreme quintiles, the HRs (95% CIs) of all-cause mortality were 0.77 (0.69, 0.85) for TLCDS (P trend < 0.001), 0.91 (0.82, 1.01) for ALCDS (P trend = 0.04), 0.70 (0.63, 0.78) for VLCDS (P trend < 0.001), 1.06 (0.95, 1.18) for ULCDS (P trend = 0.52), and 0.71 (0.63, 0.79) for HLCDS (P trend < 0.001). Each 10 points of TLCDS, VLCDS, and HLCDS were associated with 13% (95% CI 8, 18), 24% (95% CI 18, 29), and 22% (95% CI 16, 27) lower total mortality. Higher VLCDS and HLCDS were also associated with lower CVD mortality (HR [95% CI] per 10 points = 0.84 [0.74, 0.95] for VLCDS and 0.86 [0.75, 0.97] for HLCDS) and cancer mortality (HR [95% CI] per 10 points = 0.80 [0.69, 0.93] for VLCDS and 0.83 [0.72, 0.96] for HLCDS), while no significant associations were found for TLCDS, ALCDS, and ULCDS. We did not detect any nonlinear relationships between LCDS and all-cause mortality in the spline regressions (all P values for nonlinearity > 0.05) (Supplementary Fig. 1).
Table 2.
Pooled HRs (95% CIs) of mortality for low-carbohydrate scores among participants with T2D in NHS (1980–2018) and HPFS (1986–2018)
| Q1 | Q2 | Q3 | Q4 | Q5 | P trend | Per 10 points | |
|---|---|---|---|---|---|---|---|
| All-cause mortality | |||||||
| TLCDS | |||||||
| Median score | 9.5 | 14.5 | 18.0 | 21.2 | 25.5 | ||
| Cases/person-years | 1,198/28,193 | 1,054/27,635 | 864/28,259 | 839/27,633 | 640/27,687 | — | — |
| Age-adjusted model | 1 | 0.99 (0.91, 1.08) | 0.88 (0.81, 0.97) | 0.96 (0.88, 1.06) | 0.84 (0.76, 0.93) | <0.01 | 0.92 (0.88, 0.97) |
| Multivariable-adjusted model | 1 | 0.91 (0.83, 1.00) | 0.77 (0.70, 0.85) | 0.89 (0.81, 0.99) | 0.77 (0.69, 0.85) | <0.0001 | 0.87 (0.82, 0.92) |
| ALCDS | |||||||
| Median score | 8.5 | 14.0 | 18.0 | 21.8 | 26.0 | ||
| Cases/person-years | 1,035/27,598 | 1,006/27,737 | 984/28,360 | 836/28,323 | 734/27,388 | — | — |
| Age-adjusted model | 1 | 1.07 (0.98, 1.18) | 1.11 (1.01, 1.21) | 1.05 (0.95, 1.15) | 1.07 (0.97, 1.18) | 0.15 | 1.04 (0.99, 1.09) |
| Multivariable-adjusted model | 1 | 0.94 (0.85, 1.03) | 0.94 (0.85, 1.03) | 0.92 (0.83, 1.01) | 0.91 (0.82, 1.01) | 0.04 | 0.95 (0.90, 1.00) |
| VLCDS | |||||||
| Median score | 10.0 | 13.3 | 16.0 | 18.8 | 22.7 | ||
| Cases/person-years | 1,200/27,718 | 1,030/27,390 | 973/28,172 | 802/28,104 | 590/28,022 | — | — |
| Age-adjusted model | 1 | 0.93 (0.86, 1.02) | 0.95 (0.87, 1.04) | 0.80 (0.73, 0.88) | 0.65 (0.58, 0.72) | <0.0001 | 0.75 (0.70, 0.79) |
| Multivariable-adjusted model | 1 | 0.93 (0.85, 1.02) | 0.88 (0.80, 0.96) | 0.79 (0.72, 0.88) | 0.70 (0.63, 0.78) | <0.0001 | 0.76 (0.71, 0.82) |
| ULCDS | |||||||
| Median score | 8.0 | 13.3 | 17.0 | 20.0 | 24.5 | ||
| Cases/person-years | 970/28,212 | 998/27,406 | 938/28,369 | 883/27,673 | 806/27,745 | — | — |
| Age-adjusted model | 1 | 1.17 (1.07, 1.28) | 1.15 (1.05, 1.27) | 1.20 (1.09, 1.32) | 1.25 (1.13, 1.38) | <0.0001 | 1.13 (1.07, 1.18) |
| Multivariable-adjusted model | 1 | 1.07 (0.97, 1.18) | 1.02 (0.92, 1.13) | 1.03 (0.93, 1.14) | 1.06 (0.95, 1.18) | 0.52 | 1.02 (0.96, 1.08) |
| HLCDS | |||||||
| Median score | 10.0 | 13.7 | 16.0 | 19.0 | 23.0 | ||
| Cases/person-years | 1,046/27,351 | 1,015/28,609 | 995/27,430 | 888/28,414 | 651/27,601 | — | — |
| Age-adjusted model | 1 | 0.95 (0.86, 1.04) | 0.95 (0.86, 1.04) | 0.83 (0.75, 0.91) | 0.62 (0.56, 0.69) | <0.0001 | 0.74 (0.70, 0.78) |
| Multivariable-adjusted model | 1 | 0.92 (0.84, 1.01) | 0.91 (0.83, 1.00) | 0.83 (0.75, 0.92) | 0.71 (0.63, 0.79) | <0.0001 | 0.78 (0.73, 0.84) |
| CVD mortality | |||||||
| TLCDS | |||||||
| Median score | 9.5 | 14.5 | 18.0 | 21.2 | 25.5 | ||
| Cases/person-years | 378/28,193 | 309/27,635 | 250/28,259 | 253/27,633 | 199/27,687 | — | — |
| Age-adjusted model | 1 | 0.94 (0.81, 1.11) | 0.89 (0.76, 1.06) | 1.00 (0.84, 1.18) | 0.95 (0.79, 1.14) | 0.48 | 0.97 (0.88, 1.06) |
| Multivariable-adjusted model | 1 | 0.85 (0.72, 1.00) | 0.77 (0.65, 0.92) | 0.91 (0.76, 1.09) | 0.86 (0.71, 1.04) | 0.04 | 0.90 (0.82, 1.00) |
| ALCDS | |||||||
| Median score | 8.5 | 14.0 | 18.0 | 21.8 | 26.0 | ||
| Cases/person-years | 319/27,598 | 312/27,737 | 288/28,360 | 246/28,323 | 224/27,388 | — | — |
| Age-adjusted model | 1 | 1.14 (0.96, 1.34) | 1.11 (0.94, 1.32) | 1.08 (0.91, 1.28) | 1.17 (0.98, 1.41) | 0.20 | 1.06 (0.97, 1.15) |
| Multivariable-adjusted model | 1 | 0.94 (0.79, 1.12) | 0.94 (0.79, 1.12) | 0.90 (0.75, 1.08) | 0.97 (0.81, 1.18) | 0.33 | 0.96 (0.87, 1.05) |
| VLCDS | |||||||
| Median score | 10.0 | 13.3 | 16.0 | 18.8 | 22.7 | ||
| Cases/person-years | 357/27,718 | 297/27,390 | 312/28,172 | 270/28,104 | 153/28,022 | — | — |
| Age-adjusted model | 1 | 0.96 (0.81, 1.12) | 1.12 (0.95, 1.32) | 1.00 (0.85, 1.18) | 0.63 (0.52, 0.77) | <0.001 | 0.81 (0.72, 0.90) |
| Multivariable-adjusted model | 1 | 0.94 (0.80, 1.11) | 1.03 (0.87, 1.22) | 1.00 (0.84, 1.20) | 0.69 (0.56, 0.85) | <0.01 | 0.84 (0.74, 0.95) |
| ULCDS | |||||||
| Median score | 8.0 | 13.3 | 17.0 | 20.0 | 24.5 | ||
| Cases/person-years | 305/28,212 | 317/27,406 | 276/28,369 | 255/27,673 | 236/27,745 | — | — |
| Age-adjusted model | 1 | 1.17 (0.99, 1.38) | 1.07 (0.90, 1.27) | 1.12 (0.94, 1.34) | 1.23 (1.03, 1.47) | 0.03 | 1.11 (1.01, 1.21) |
| Multivariable-adjusted model | 1 | 1.04 (0.88, 1.24) | 0.92 (0.77, 1.10) | 0.93 (0.77, 1.12) | 1.01 (0.83, 1.23) | 0.74 | 0.98 (0.89, 1.09) |
| HLCDS | |||||||
| Median score | 10.0 | 13.7 | 16.0 | 19.0 | 23.0 | ||
| Cases/person-years | 303/27,351 | 314/28,609 | 295/27,430 | 287/28,414 | 190/27,601 | — | — |
| Age-adjusted model | 1 | 1.01 (0.86, 1.19) | 0.99 (0.83, 1.17) | 0.93 (0.79, 1.11) | 0.66 (0.55, 0.80) | <0.0001 | 0.79 (0.70, 0.88) |
| Multivariable-adjusted model | 1 | 0.98 (0.82, 1.17) | 0.96 (0.81, 1.15) | 0.93 (0.78, 1.12) | 0.79 (0.64, 0.97) | 0.02 | 0.86 (0.75, 0.97) |
| Cancer mortality | |||||||
| TLCDS | |||||||
| Median score | 9.5 | 14.5 | 18.0 | 21.2 | 25.5 | ||
| Cases/person-years | 180/28,193 | 202/27,635 | 161/28,259 | 194/27,633 | 144/27,687 | — | — |
| Age-adjusted model | 1 | 1.16 (0.94, 1.43) | 0.97 (0.78, 1.21) | 1.28 (1.03, 1.59) | 0.98 (0.77, 1.23) | 0.62 | 1.03 (0.92, 1.16) |
| Multivariable-adjusted model | 1 | 1.11 (0.89, 1.37) | 0.94 (0.75, 1.17) | 1.27 (1.02, 1.59) | 0.92 (0.72, 1.16) | 0.98 | 1.00 (0.89, 1.13) |
| ALCDS | |||||||
| Median score | 8.5 | 14.0 | 18.0 | 21.8 | 26.0 | ||
| Cases/person-years | 168/27,598 | 178/27,737 | 186/28,360 | 186/28,323 | 163/27,388 | — | — |
| Age-adjusted model | 1 | 1.05 (0.84, 1.31) | 1.17 (0.94, 1.45) | 1.24 (1.00, 1.54) | 1.18 (0.94, 1.48) | 0.03 | 1.13 (1.01, 1.26) |
| Multivariable-adjusted model | 1 | 1.02 (0.82, 1.28) | 1.08 (0.86, 1.35) | 1.19 (0.95, 1.49) | 1.06 (0.84, 1.35) | 0.27 | 1.06 (0.95, 1.19) |
| VLCDS | |||||||
| Median score | 10.0 | 13.3 | 16.0 | 18.8 | 22.7 | ||
| Cases/person-years | 220/27,718 | 187/27,390 | 184/28,172 | 149/28,104 | 141/28,022 | — | — |
| Age-adjusted model | 1 | 0.91 (0.75, 1.12) | 0.94 (0.76, 1.15) | 0.73 (0.59, 0.91) | 0.73 (0.58, 0.91) | <0.001 | 0.77 (0.67, 0.88) |
| Multivariable-adjusted model | 1 | 0.96 (0.78, 1.18) | 0.92 (0.74, 1.14) | 0.77 (0.61, 0.96) | 0.80 (0.64, 1.01) | <0.01 | 0.80 (0.69, 0.93) |
| ULCDS | |||||||
| Median score | 8.0 | 13.3 | 17.0 | 20.0 | 24.5 | ||
| Cases/person-years | 162/28,212 | 177/27,406 | 172/28,369 | 186/27,673 | 184/27,745 | — | — |
| Age-adjusted model | 1 | 1.15 (0.92, 1.44) | 1.13 (0.91, 1.42) | 1.33 (1.07, 1.66) | 1.41 (1.13, 1.76) | <0.001 | 1.21 (1.08, 1.36) |
| Multivariable-adjusted model | 1 | 1.09 (0.87, 1.37) | 1.05 (0.83, 1.32) | 1.20 (0.95, 1.51) | 1.23 (0.97, 1.56) | 0.06 | 1.12 (0.99, 1.27) |
| HLCDS | |||||||
| Median score | 10.0 | 13.7 | 16.0 | 19.0 | 23.0 | ||
| Cases/person-years | 197/27,351 | 188/28,609 | 182/27,430 | 178/28,414 | 136/27,601 | — | — |
| Age-adjusted model | 1 | 0.89 (0.72, 1.10) | 0.93 (0.75, 1.15) | 0.85 (0.69, 1.06) | 0.66 (0.52, 0.82) | <0.0001 | 0.75 (0.66, 0.86) |
| Multivariable-adjusted model | 1 | 0.90 (0.72, 1.11) | 0.96 (0.77, 1.19) | 0.92 (0.73, 1.14) | 0.77 (0.60, 0.98) | 0.02 | 0.83 (0.72, 0.96) |
Age (years)– and calendar year–stratified Cox model adjusted for race (White, African American, Asian, others), total energy (quintile), physical activity (quintile), alcohol intake (0, 0.1–4.9, 5.0–9.9, 10.0–14.9, 15.0–29.9, and ≥30.0 g/d), prediagnosis AHEI (quintile), smoking status (never smoked; past smoker; currently smoke 1–14 cigarettes per day, 15–24 cigarettes per day, or ≥25 cigarettes per day), prediagnosis BMI (<21.0, 21.0–22.9, 23.0–24.9, 25.0–26.9, 27.0–29.9, 30.0–32.9, 33.0–34.9, or ≥35.0 kg/m2), multivitamin use (yes, no), family history of diabetes (yes, no), family history of myocardial infarction (yes, no), family history of cancer (yes, no), diabetes duration (0–5 years, 5–10 years, 10–15 years, >15 years), time interval between diagnosis date and latest postdiagnosis FFQ return date (months), postmenopausal hormone use (women only; premenopausal, never, former, current, or missing), oral hypoglycemic drug use (women only; yes, no), and insulin use (women only; yes, no). Q, quintile.
The multivariable-adjusted HR (95% CI) per 10-point increase of TLCDS from prediabetes to postdiabetes diagnosis was 0.88 (0.83, 0.93) for all-cause mortality and 0.90 (0.81, 1.00) for CVD mortality, while no statistically significant associations were found for cancer mortality (Table 3). The corresponding estimates for VLCDS and HLCDS were 0.75 (0.70, 0.81) and 0.75 (0.70, 0.81) for all-cause mortality, 0.81 (0.71, 0.92) and 0.79 (0.69, 0.90) for CVD mortality, and 0.82 (0.70, 0.96) and 0.83 (0.71, 0.97) for cancer mortality, respectively. Increasing ALCDS or ULCDS from prediagnosis to postdiagnosis were not associated with any mortality outcomes.
Table 3.
Pooled HRs (95% CIs) of mortality according to changes in LCDS from prediabetes to postdiabetes diagnosis in NHS (1980–2018) and HPFS (1986–2018)
| Q1 | Q2 | Q3 | Q4 | Q5 | P trend | Per 10 points increase | |
|---|---|---|---|---|---|---|---|
| All-cause mortality | |||||||
| TLCDS | |||||||
| Median score | −8.0 | −2.3 | 1.0 | 5.0 | 11.0 | ||
| Cases/person-years | 1,096/28,317 | 882/27,358 | 905/28,232 | 895/28,021 | 817/27,479 | — | — |
| Age-adjusted model | 1 | 0.86 (0.79, 0.95) | 0.88 (0.80, 0.96) | 0.87 (0.79, 0.96) | 0.86 (0.78, 0.94) | <0.001 | 0.91 (0.86, 0.96) |
| Multivariable-adjusted model | 1 | 0.86 (0.78, 0.95) | 0.86 (0.77, 0.95) | 0.83 (0.74, 0.93) | 0.72 (0.64, 0.82) | <0.0001 | 0.88 (0.83, 0.93) |
| ALCDS | |||||||
| Median score | −9.0 | −3.0 | 1.0 | 5.0 | 11.8 | ||
| Cases/person-years | 1,001/27,692 | 885/27,924 | 882/27,868 | 922/27,971 | 905/27,951 | — | — |
| Age-adjusted model | 1 | 0.91 (0.83, 1.00) | 0.91 (0.83, 1.00) | 0.92 (0.84, 1.01) | 0.96 (0.87, 1.05) | 0.57 | 1.01 (0.96, 1.07) |
| Multivariable-adjusted model | 1 | 0.95 (0.86, 1.05) | 0.94 (0.84, 1.04) | 0.95 (0.85, 1.06) | 0.93 (0.82, 1.05) | 0.21 | 0.97 (0.92, 1.02) |
| VLCDS | |||||||
| Median score | −6.0 | −2.0 | 1.0 | 4.0 | 8.7 | ||
| Cases/person-years | 1,106/28,354 | 949/27,148 | 916/28,661 | 838/27,014 | 786/28,229 | — | — |
| Age-adjusted model | 1 | 0.96 (0.88, 1.06) | 0.90 (0.82, 0.98) | 0.93 (0.85, 1.02) | 0.86 (0.78, 0.94) | <0.0001 | 0.75 (0.70, 0.80) |
| Multivariable-adjusted model | 1 | 0.91 (0.83, 1.01) | 0.84 (0.76, 0.93) | 0.8 1(0.72, 0.90) | 0.68 (0.60, 0.77) | <0.0001 | 0.75 (0.70, 0.81) |
| ULCDS | |||||||
| Median score | −8.5 | −3.0 | 0 | 3.7 | 9.0 | ||
| Cases/person-years | 906/27,539 | 883/27,758 | 940/28,567 | 889/27,731 | 977/27,811 | — | — |
| Age-adjusted model | 1 | 0.95 (0.86, 1.05) | 0.97 (0.88, 1.07) | 0.95 (0.86, 1.05) | 1.04 (0.94, 1.14) | <0.001 | 1.11 (1.04, 1.17) |
| Multivariable-adjusted model | 1 | 0.99 (0.89, 1.09) | 1.01 (0.92, 1.12) | 1.00 (0.90, 1.12) | 1.09 (0.97, 1.23) | 0.07 | 1.06 (0.99, 1.12) |
| HLCDS | |||||||
| Median score | −5.3 | −1.0 | 2.0 | 4.7 | 9.0 | ||
| Cases/person-years | 1,086/27,630 | 1,011/28,591 | 874/27,396 | 846/27,908 | 778/27,881 | — | — |
| Age-adjusted model | 1 | 0.96 (0.87, 1.05) | 0.93 (0.85, 1.02) | 0.89 (0.81, 0.98) | 0.86 (0.78, 0.95) | <0.0001 | 0.74 (0.70, 0.79) |
| Multivariable-adjusted model | 1 | 0.90 (0.82, 0.99) | 0.85 (0.77, 0.95) | 0.78 (0.70, 0.87) | 0.69 (0.61, 0.78) | <0.0001 | 0.75 (0.70, 0.81) |
| CVD mortality | |||||||
| TLCDS | |||||||
| Median score | −8.0 | −2.3 | 1.0 | 5.0 | 11.0 | ||
| Cases/person-years | 329/28,317 | 271/27,358 | 268/28,232 | 290/28,021 | 231/27,479 | — | — |
| Age-adjusted model | 1 | 0.90 (0.76, 1.07) | 0.87 (0.73, 1.03) | 0.96 (0.82, 1.14) | 0.84 (0.70, 1.00) | 0.21 | 0.94 (0.85, 1.04) |
| Multivariable-adjusted model | 1 | 0.94 (0.79, 1.12) | 0.90 (0.74, 1.08) | 0.96 (0.79, 1.18) | 0.80 (0.63, 1.01) | 0.05 | 0.90 (0.81, 1.00) |
| ALCDS | |||||||
| Median score | −9.0 | −3.0 | 1.0 | 5.0 | 11.8 | ||
| Cases/person-years | 306/27,692 | 278/27,924 | 247/27,868 | 290/27,971 | 268/27,951 | — | — |
| Age-adjusted model | 1 | 0.98 (0.83, 1.16) | 0.82 (0.69, 0.98) | 0.95 (0.81, 1.13) | 0.96 (0.81, 1.14) | 0.57 | 1.03 (0.94, 1.13) |
| Multivariable-adjusted model | 1 | 1.02 (0.86, 1.22) | 0.85 (0.71, 1.03) | 1.03 (0.84, 1.26) | 0.98 (0.78, 1.23) | 0.57 | 0.97 (0.88, 1.07) |
| VLCDS | |||||||
| Median score | −6.0 | −2.0 | 1.0 | 4.0 | 8.7 | ||
| Cases/person-years | 333/28,354 | 283/27,148 | 277/28,661 | 264/27,014 | 232/28,229 | — | — |
| Age-adjusted model | 1 | 0.98 (0.83, 1.16) | 0.93 (0.78, 1.10) | 1.00 (0.84, 1.18) | 0.91 (0.76, 1.09) | <0.001 | 0.80 (0.71, 0.90) |
| Multivariable-adjusted model | 1 | 0.96 (0.80, 1.14) | 0.91 (0.75, 1.09) | 0.92 (0.76, 1.13) | 0.81 (0.64, 1.02) | <0.01 | 0.81 (0.71, 0.92) |
| ULCDS | |||||||
| Median score | −8.5 | −3.0 | 0 | 3.7 | 9.0 | ||
| Cases/person-years | 268/27,539 | 270/27,758 | 288/28,567 | 266/27,731 | 297/27,811 | — | — |
| Age-adjusted model | 1 | 1.01 (0.84, 1.20) | 1.00 (0.84, 1.19) | 0.93 (0.78, 1.11) | 1.06 (0.89, 1.26) | 0.11 | 1.09 (0.98, 1.21) |
| Multivariable-adjusted model | 1 | 1.02 (0.85, 1.23) | 1.03 (0.85, 1.24) | 0.96 (0.78, 1.17) | 1.09 (0.88, 1.36) | 0.57 | 1.03 (0.93, 1.15) |
| HLCDS | |||||||
| Median score | −5.3 | −1.0 | 2.0 | 4.7 | 9.0 | ||
| Cases/person-years | 349/27,630 | 292/28,591 | 244/27,396 | 275/27,908 | 229/27,881 | — | — |
| Age-adjusted model | 1 | 0.90 (0.77, 1.07) | 0.83 (0.70, 0.99) | 0.96 (0.82, 1.14) | 0.84 (0.71, 1.01) | <0.0001 | 0.78 (0.69, 0.88) |
| Multivariable-adjusted model | 1 | 0.85 (0.72, 1.02) | 0.76 (0.63, 0.92) | 0.88 (0.72, 1.07) | 0.73 (0.58, 0.91) | <0.001 | 0.79 (0.69, 0.90) |
| Cancer mortality | |||||||
| TLCDS | |||||||
| Median score | −8.0 | −2.3 | 1.0 | 5.0 | 11.0 | ||
| Cases/person-years | 190/28,317 | 173/27,358 | 177/28,232 | 179/28,021 | 162/27,479 | — | — |
| Age-adjusted model | 1 | 0.96 (0.78, 1.20) | 0.96 (0.78, 1.19) | 0.96 (0.77, 1.18) | 0.93 (0.75, 1.16) | 0.90 | 1.01 (0.89, 1.14) |
| Multivariable-adjusted model | 1 | 0.99 (0.79, 1.24) | 0.98 (0.78, 1.24) | 1.03 (0.80, 1.32) | 0.98 (0.74, 1.31) | 0.86 | 1.01 (0.89, 1.15) |
| ALCDS | |||||||
| Median score | −9.0 | −3.0 | 1.0 | 5.0 | 11.8 | ||
| Cases/person-years | 182/27,692 | 174/27,924 | 180/27,868 | 173/27,971 | 172/27,951 | — | — |
| Age-adjusted model | 1 | 0.92 (0.74, 1.15) | 1.00 (0.80, 1.23) | 0.96 (0.77, 1.20) | 0.94 (0.76, 1.17) | 0.15 | 1.09 (0.97, 1.22) |
| Multivariable-adjusted model | 1 | 0.98 (0.79, 1.23) | 1.07 (0.85, 1.35) | 1.10 (0.86, 1.41) | 1.13 (0.85, 1.49) | 0.24 | 1.07 (0.95, 1.21) |
| VLCDS | |||||||
| Median score | −6.0 | −2.0 | 1.0 | 4.0 | 8.7 | ||
| Cases/person-years | 189/28,354 | 199/27,148 | 165/28,661 | 163/27,014 | 165/28,229 | — | — |
| Age-adjusted model | 1 | 1.17 (0.95, 1.43) | 0.91 (0.73, 1.13) | 1.01 (0.81, 1.25) | 0.96 (0.77, 1.19) | <0.01 | 0.79 (0.68, 0.91) |
| Multivariable-adjusted model | 1 | 1.12 (0.90, 1.39) | 0.84 (0.67, 1.06) | 0.90 (0.71, 1.15) | 0.79 (0.60, 1.04) | 0.01 | 0.82 (0.70, 0.96) |
| ULCDS | |||||||
| Median score | −8.5 | −3.0 | 0 | 3.7 | 9.0 | ||
| Cases/person-years | 186/27,539 | 165/27,758 | 183/28,567 | 163/27,731 | 184/27,811 | — | — |
| Age-adjusted model | 1 | 0.86 (0.69, 1.07) | 0.94 (0.76, 1.16) | 0.87 (0.69, 1.08) | 0.96 (0.77, 1.18) | 0.03 | 1.15 (1.02, 1.31) |
| Multivariable-adjusted model | 1 | 0.94 (0.75, 1.17) | 1.05 (0.84, 1.32) | 1.03 (0.81, 1.32) | 1.19 (0.92, 1.56) | 0.06 | 1.13 (0.99, 1.29) |
| HLCDS | |||||||
| Median score | −5.3 | −1.0 | 2.0 | 4.7 | 9.0 | ||
| Cases/person-years | 180/27,630 | 198/28,591 | 161/27,396 | 177/27,908 | 165/27,881 | — | — |
| Age-adjusted model | 1 | 1.07 (0.87, 1.32) | 0.98 (0.79, 1.22) | 1.05 (0.85, 1.30) | 0.98 (0.79, 1.23) | <0.01 | 0.79 (0.68, 0.92) |
| Multivariable-adjusted model | 1 | 0.98 (0.79, 1.22) | 0.90 (0.71, 1.14) | 0.93 (0.73, 1.19) | 0.80 (0.61, 1.04) | 0.02 | 0.83 (0.71, 0.97) |
Age (years)– and calendar year–stratified Cox model adjusted for race (White, African American, Asian, others), prediagnosis LCDS (continuous), pre-post change of total energy (quintile), pre-post change of physical activity change (quintile), pre-post change of alcohol intake change (quintile), pre-post change of AHEI (quintile), pre-post change of smoking status (remain noncurrent smoker; current smoker to noncurrent smoker; remain current smoker; noncurrent smoker to current smoker), pre-post change of BMI (decreased, unchanged, increased), multivitamin use (yes, no), family history of diabetes (yes, no), family history of myocardial infarction (yes, no), family history of cancer (yes, no), diabetes duration (0–5 years, 5–10 years, 10–15 years, >15 years), time interval between diagnosis date and latest postdiagnosis FFQ return date (months), postmenopausal hormone use (women only; premenopausal, never, former, current, or missing), oral hypoglycemic drug use (women only; yes, no), and insulin use (women only; yes, no). Q, quintile.
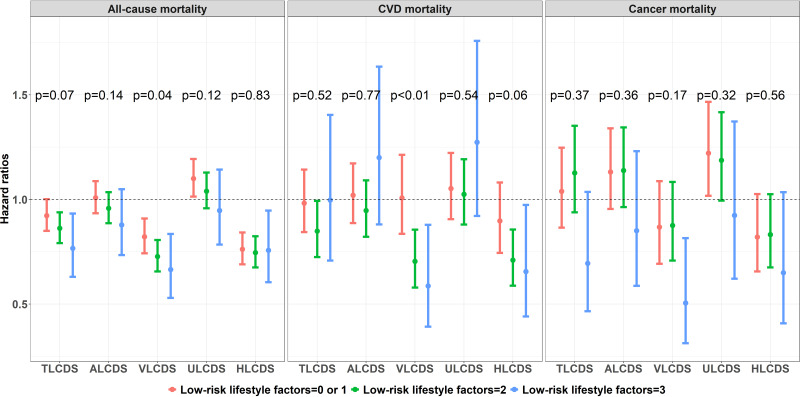
In a secondary analysis assessing potential effect modification by a number of postdiagnosis low-risk lifestyle factors, the inverse associations of TLCDS, VLCDS, and HLCDS with total and CVD mortality appeared to be more pronounced among participants having more low-risk lifestyle factors, although most P values for interactions were not statistically significant (Fig. 1). A statistically significant interaction was found between lifestyle factors and VLCDS for all-cause mortality (P = 0.04 for interaction) where the HRs (95% CIs) per 10 points of VLCDS were 0.82 (0.74, 0.91) for participants with zero or one low-risk lifestyle factors, 0.73 (0.66, 0.81) for two factors, and 0.66 (0.53, 0.84) for three factors. For CVD mortality, significantly lower risks were also found for VLCDS (P value for interaction: <0.01) among participants with more low-risk lifestyle factors. No apparent patterns of effect modifications by number of low-risk lifestyle factors were observed for cancer mortality. In the secondary analyses stratifying by the presence of diabetes symptoms and drug use, the associations appeared to be slightly stronger among patients without symptoms, although none of the P values for interactions were statistically significant (Supplementary Table 1). The risk estimates were also similar across the diabetes drug use categories, and no significant effect modifications were detected (P values for interaction all were >0.05).
Figure 1.
Pooled HRs per 10 points of low-carbohydrate scores by numbers of low-risk lifestyle factors. Age (years)– and calendar year–stratified Cox model adjusted for race (White, African American, Asian, others), total energy (quintile), prediagnosis BMI (<21.0, 21.0–22.9, 23.0–24.9, 25.0–26.9, 27.0–29.9, 30.0–32.9, 33.0–34.9, or ≥35.0 kg/m2), multivitamin use (yes, no), family history of diabetes (yes, no), family history of myocardial infarction (yes, no), family history of cancer (yes, no), diabetes duration (0–5 years, 5–10 years, 10–15 years, >15 years), time interval between diagnosis date and latest postdiagnosis FFQ return date (months), postmenopausal hormone use (women only; premenopausal, never, former, current, or missing), oral hypoglycemic drug use (women only; yes, no), and insulin use (women only; yes, no). Three low-risk lifestyle factors were the following dichotomized variables: non-current smoking, moderate to vigorous physical activity (≥7.5 METs h/week), and moderate alcohol consumption (5–15 g/day for women and 5–30 g/day for men). The P values for interactions were calculated between each continuous LCDS and number of low-risk lifestyle factors on all-cause mortality, CVD mortality, and cancer mortality.
Replacing refined carbohydrates with vegetable fat or vegetable protein was associated with lower all-cause mortality (Supplementary Table 2). The HRs (95% CIs) of all-cause mortality per 5% replacement with vegetable fat were 0.98 (0.93, 1.05) for potato, 0.93 (0.89, 0.98) for refined grain, 0.90 (0.85, 0.95) for added sugar, and 0.90 (0.86, 0.94) for total refined carbohydrates. The corresponding estimates for substituting vegetable protein were 0.75 (0.63, 0.90), 0.76 (0.63, 0.90), 0.72 (0.60, 0.87), and 0.72 (0.61, 0.86). Despite a similar pattern of associations, no statistically significant associations were found for CVD and cancer mortality.
In sensitivity analyses additionally including participants with prevalent diabetes at baseline, the results were largely unchanged (Supplementary Table 3). Excluding participants who died within 5 years of diabetes diagnosis and adjusting for time-varying change of covariates instead of the prediagnosis covariates slightly attenuated the estimates in the change analysis, although the results remained statistically significant (Supplementary Tables 4 and 5).
Conclusions
In the current study among men and women with T2D who were followed for over 30 years, greater adherence to an overall low-carbohydrate dietary pattern as well as reduction of carbohydrate intake from the prediagnosis to postdiagnosis period were associated with significantly lower all-cause mortality. The inverse associations were stronger for LCDs that emphasized macronutrient intake from healthy plant-based foods, and these LCDs were also associated with significantly lower CVD and cancer mortality. In contrast, LCDs that emphasized animal protein or fat were not significantly associated with any study outcomes. The inverse associations were not materially different among participants with different disease severity and drug use status, and the favorable associations of LCDS were more pronounced among participants with more low-risk lifestyle risk factors. Isocaloric substitution of vegetable fat and protein for refined carbohydrates was associated with significantly lower all-cause mortality. These findings persisted after adjustment of a wide range of potential confounders and in multiple sensitivity analyses.
Abundant evidence from clinical trials with intervention duration of up to 2 years suggests favorable effects of LCDs on weight control and improvement on glycemia and lipids profiles in patients with diabetes (6,23). No long-term randomized controlled trials have been conducted to examine effects of LCDs on CVD and other health outcomes among patients with diabetes, largely because of prohibitive cost and expected low adherence. The current analysis is the first prospective cohort study that examines the relationship between adhering to LCD patterns and mortality in a long-term setting in people with T2D. Our findings support current guidelines from international bodies and professional groups such as the ADA that endorse carbohydrate restriction as a legitimate therapeutic strategy for people with T2D (2–4). During up to 34 years of follow-up for people with diabetes, we found a 24% reduction of all-cause mortality, comparing extreme quintiles of an overall LCDS. However, only LCDs that reflected on high-quality macronutrients were robustly associated with lower mortality. The robust beneficial associations of VLCDS and HLCDS were in line with previous general population studies. For example, in an earlier analysis in the NHS and HPFS, comparing extreme deciles, greater adherence to ALCDS was associated with 23% and 14% higher all-cause and CVD mortality, while VLCDS predicted 20% and 23% lower all-cause and CVD mortality (13). In a recent study in the National Health and Nutrition Examination Survey population, similar divergent associations were observed between HLCDS and ULCDS, where higher HLCDS was associated with significantly lower total mortality (HR per 20-percentile increase in scores: 0.89; 95% CI 0.85, 0.93) whereas increased total mortality (HR per 20-percentile increase in scores: 1.07; 95% CI 1.02, 1.12) was found for participants with higher ULCDS (8). The primarily null associations for ALCDS and ULCDS in our analysis suggest that simply reducing overall carbohydrate intake while ignoring macronutrient quality may not be sufficient for maintaining overall health among people with diabetes.
In addition to quantifying the time-varying associations of LCDS and mortality, the results from the change analysis suggested that individuals with diabetes may benefit from transitioning to a healthy version of LCD after diagnosis. Moreover, we found that people with diabetes might gain additional health benefits by adopting concurrent healthy lifestyle behaviors after diagnosis, including not smoking, moderate alcohol consumption, regular moderate-to-vigorous physical activity, and consuming an overall high-quality diet. Our previous analysis has shown the effectiveness of adherence to these healthy lifestyle factors in lowering risk of CVD and CVD mortality after T2D diagnosis (21). In addition, the substitution analysis in the current analysis found 11% and 26% lower all-cause mortality when replacing total refined carbohydrates with vegetable fat and protein, respectively. These results may partly explain the stronger inverse associations observed in VLCDS and HCLDS with mortality and are consistent with the findings in a meta-analysis of prospective cohort studies that shows 18% reduction of total mortality when replacing total carbohydrates with plant protein and fat (7). Such data suggest that an optimal LCD consists of protein and fat from plant-based foods that replace low-quality carbohydrates such as carbohydrates from potatoes, refined grains, and added sugar. In light of findings that suggest whole-grain intake was associated with overall improved health among people with diabetes (24), the current and existing studies collectively suggest that diet quality should remain the focus when people with established T2D construct their diet patterns for disease management.
The mechanisms pertaining to the therapeutic effects of an overall LCD on T2D are postulated to be attributed to its influence on reducing circulating insulin (25). It is suggested that reducing overall energy and carbohydrate intake may reverse the pathogenesis of T2D through lowering circulating insulin, which subsequently leads to reduced fat accumulation in liver and pancreas, weight loss, improved insulin sensitivity, and increased insulin secretion (26). The health benefits were magnified in VLCDS and HLCDS, probably due to their higher proportions of plant-based nutrients, including unsaturated fatty acid, various vitamins and minerals, nuts, and olive oil, which are associated with lower mortality (27–30). Conversely, the favorable associations between lower overall carbohydrate intake may be offset by a higher consumption of red and processed meat featured in ALCDS, which is related to unfavorable health outcomes in both people with T2D and the general populations (31–33). The null associations in ULCDS may be related to its increased proportions of low-quality carbohydrates at the expense of high-quality carbohydrates, which may counteract favorable effects from reducing carbohydrate intake.
Several caveats from our study merit discussion. First, in this observational study, we were unable to establish causal relationships between adopting an LCD and mortality among people with diabetes. Higher compliance with the medical recommendation of an LCD diet may be associated with greater compliance with medications and other factors that we could not directly measure. However, given the extensive adjustment for demographic and lifestyle factors and consistent inverse associations observed in the change analysis, it is unlikely that the significant associations were completely explained by unmeasured and residual confounding. Second, although the cumulative average approach may help reduce random measurement errors in the assessment of macronutrients intake, the residual random errors are inevitable. However, such errors are likely to be nondifferential with respect to the study outcome and attenuate the associations toward the null. Third, in the current analysis, participants in the highest quintile of LCDS still consumed, on average, 30–40% of total energy from carbohydrates. Therefore, our findings cannot be generalized to the effects of much lower carbohydrate intake such as the ketogenic diet. Nevertheless, according to a survey conducted among U.K. dietitians who provide dietary consultations to patients with diabetes, most of the participants would consider 30–39% of energy from carbohydrates to be a realistic goal for long-term adherence (34). Finally, our findings may have limited generalizability because the study participants consisted of health professionals with European ancestries, higher health consciousness, and better access to health care resources.
In conclusion, among individuals with diabetes, adopting LCD patterns that emphasized high-quality sources of macronutrients was significantly associated with lower total, cardiovascular, and cancer mortality. Combining healthy versions of the LCD with other healthy lifestyle behaviors after diabetes diagnosis may confer additional health benefits. Replacing refined carbohydrates with plant-sourced fat and protein was also associated with significantly longer survival. Our findings provide support for the current recommendations of carbohydrate restrictions for T2D management and highlight the importance of the quality and food sources of macronutrients when assessing the health benefits of LCD.
Article Information
Acknowledgments. The authors thank the participants and staff of the Nurses’ Health Study, Nurses’ Health Study II, and Health Professionals Follow-up Study for their valuable contributions. The authors would like to acknowledge the contribution to this study from central cancer registries supported through the Centers for Disease Control and Prevention’s National Program of Cancer Registries and/or the National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) Program. Central registries may also be supported by state agencies, universities, and cancer centers. Participating central cancer registries include the following: Alabama, Alaska, Arizona, Arkansas, California, Colorado, Connecticut, Delaware, Florida, Georgia, Hawaii, Idaho, Indiana, Iowa, Kentucky, Louisiana, Massachusetts, Maine, Maryland, Michigan, Mississippi, Montana, Nebraska, Nevada, New Hampshire, New Jersey, New Mexico, New York, North Carolina, North Dakota, Ohio, Oklahoma, Oregon, Pennsylvania, Puerto Rico, Rhode Island, Seattle SEER Registry, South Carolina, Tennessee, Texas, Utah, Virginia, West Virginia, and Wyoming.
Funding. NHS, HPFS, and the current analysis are supported by National Institutes of Health grants (UM1 CA186107, P01 CA87969, R01 HL034594, U01 CA167552, R01 HL35464, R01 HL60712, R01 DK120870, R01 DK126698, R01 DK119268, U2C DK129670, DK119268, R01 ES022981, and R21 AG070375).
The funding sources did not participate in the design or conduct of the study, collection, management, analysis or interpretation of the data, or preparation, review, or approval of the manuscript.
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. Y.H. and Q.S. provided the concept and design. J.E.M., E.B.R., K.R., W.C.W., and F.B.H. handled acquisition of data. Y.H., E.Y., and B.W. provided statistical analysis. All authors provided interpretation of data. Y.H. drafted the manuscript. All authors contributed to critical revision of the manuscript for important intellectual content. W.C.W., F.B.H., and Q.S. obtained funding. Y.H. and Q.S. are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
This article contains supplementary material online at https://doi.org/10.2337/figshare.21965207.
This article is featured in podcasts available at diabetesjournals.org/journals/pages/diabetes-core-update-podcasts.
References
- 1. Czech MP. Insulin action and resistance in obesity and type 2 diabetes. Nat Med 2017;23:804–814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Davies MJ, D’Alessio DA, Fradkin J, et al. Management of hyperglycemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 2018;41:2669–2701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Evert AB, Dennison M, Gardner CD, et al. Nutrition therapy for adults with diabetes or prediabetes: A consensus report. Diabetes Care 2019;42:731–754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. American Diabetes Association . 5. Facilitating behavior change and well-being to improve health outcomes: Standards of Medical Care in Diabetes—2020. Diabetes Care 2020;43(Suppl. 1):S48–S65 [DOI] [PubMed] [Google Scholar]
- 5. Feinman RD, Pogozelski WK, Astrup A, et al. Dietary carbohydrate restriction as the first approach in diabetes management: critical review and evidence base. Nutrition 2015;31:1–13 [DOI] [PubMed] [Google Scholar]
- 6. Meng Y, Bai H, Wang S, Li Z, Wang Q, Chen L. Efficacy of low carbohydrate diet for type 2 diabetes mellitus management: a systematic review and meta-analysis of randomized controlled trials. Diabetes Res Clin Pract 2017;131:124–131 [DOI] [PubMed] [Google Scholar]
- 7. Seidelmann SB, Claggett B, Cheng S, et al. Dietary carbohydrate intake and mortality: a prospective cohort study and meta-analysis. Lancet Public Health 2018;3:e419–e428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Shan Z, Guo Y, Hu FB, Liu L, Qi Q. Association of low-carbohydrate and low-fat diets with mortality among US adults. JAMA Intern Med 2020;180:513–523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bao Y, Bertoia ML, Lenart EB, et al. Origin, methods, and evolution of the three Nurses’ Health Studies. Am J Public Health 2016;106:1573–1581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Rimm EB, Giovannucci EL, Willett WC, et al. Prospective study of alcohol consumption and risk of coronary disease in men. Lancet 1991;338:464–468 [DOI] [PubMed] [Google Scholar]
- 11. Yuan C, Spiegelman D, Rimm EB, et al. Validity of a dietary questionnaire assessed by comparison with multiple weighed dietary records or 24-hour recalls. Am J Epidemiol 2017;185:570–584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Halton TL, Willett WC, Liu S, et al. Low-carbohydrate-diet score and the risk of coronary heart disease in women. N Engl J Med 2006;355:1991–2002 [DOI] [PubMed] [Google Scholar]
- 13. Fung TT, van Dam RM, Hankinson SE, Stampfer M, Willett WC, Hu FB. Low-carbohydrate diets and all-cause and cause-specific mortality: two cohort studies. Ann Intern Med 2010;153:289–298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. National Diabetes Data Group . Classification and diagnosis of diabetes mellitus and other categories of glucose intolerance. Diabetes 1979;28:1039–1057 [DOI] [PubMed] [Google Scholar]
- 15. American Diabetes Association . Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care 1997;20(suppl. 1):1183–1197 [DOI] [PubMed] [Google Scholar]
- 16. Manson JE, Rimm EB, Stampfer MJ, et al. Physical activity and incidence of non-insulin-dependent diabetes mellitus in women. Lancet 1991;338:774–778 [DOI] [PubMed] [Google Scholar]
- 17. Hu FB, Leitzmann MF, Stampfer MJ, Colditz GA, Willett WC, Rimm EB. Physical activity and television watching in relation to risk for type 2 diabetes mellitus in men. Arch Intern Med 2001;161:1542–1548 [DOI] [PubMed] [Google Scholar]
- 18. Rich-Edwards JW, Corsano KA, Stampfer MJ. Test of the National Death Index and Equifax Nationwide Death Search. Am J Epidemiol 1994;140:1016–1019 [DOI] [PubMed] [Google Scholar]
- 19. Sun Q, Townsend MK, Okereke OI, Franco OH, Hu FB, Grodstein F. Physical activity at midlife in relation to successful survival in women at age 70 years or older. Arch Intern Med 2010;170:194–201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Chiuve SE, Fung TT, Rimm EB, et al. Alternative dietary indices both strongly predict risk of chronic disease. J Nutr 2012;142:1009–1018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Liu G, Li Y, Hu Y, et al. Influence of lifestyle on incident cardiovascular disease and mortality in patients with diabetes mellitus. J Am Coll Cardiol 2018;71:2867–2876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hu FB, Stampfer MJ, Manson JE, et al. Dietary fat intake and the risk of coronary heart disease in women. N Engl J Med 1997;337:1491–1499 [DOI] [PubMed] [Google Scholar]
- 23. Nielsen JV, Joensson EA. Low-carbohydrate diet in type 2 diabetes: stable improvement of bodyweight and glycemic control during 44 months follow-up. Nutr Metab (Lond) 2008;5:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. He M, van Dam RM, Rimm E, Hu FB, Qi L. Whole-grain, cereal fiber, bran, and germ intake and the risks of all-cause and cardiovascular disease-specific mortality among women with type 2 diabetes mellitus. Circulation 2010;121:2162–2168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Taylor R. Banting Memorial Lecture 2012: reversing the twin cycles of type 2 diabetes. Diabet Med 2013;30:267–275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kelly T, Unwin D, Finucane F. Low-carbohydrate diets in the management of obesity and type 2 diabetes: a review from clinicians using the approach in practice. Int J Environ Res Public Health 2020;17:2557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Bao Y, Han J, Hu FB, et al. Association of nut consumption with total and cause-specific mortality. N Engl J Med 2013;369:2001–2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Jiao J, Liu G, Shin HJ, et al. Dietary fats and mortality among patients with type 2 diabetes: analysis in two population based cohort studies. BMJ 2019;366:l4009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Bagheri A, Naghshi S, Sadeghi O, Larijani B, Esmaillzadeh A. Total, dietary, and supplemental magnesium intakes and risk of all-cause, cardiovascular, and cancer mortality: a systematic review and dose-response meta-analysis of prospective cohort studies. Adv Nutr 2021;12:1196–1210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Guasch-Ferré M, Li Y, Willett WC, et al. Consumption of olive oil and risk of total and cause-specific mortality among U.S. adults. J Am Coll Cardiol 2022;79:101–112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Qi L, van Dam RM, Rexrode K, Hu FB. Heme iron from diet as a risk factor for coronary heart disease in women with type 2 diabetes. Diabetes Care 2007;30:101–106 [DOI] [PubMed] [Google Scholar]
- 32. Larsson SC, Orsini N. Red meat and processed meat consumption and all-cause mortality: a meta-analysis. Am J Epidemiol 2014;179:282–289 [DOI] [PubMed] [Google Scholar]
- 33. Guasch-Ferré M, Satija A, Blondin SA, et al. Meta-analysis of randomized controlled trials of red meat consumption in comparison with various comparison diets on cardiovascular risk factors. Circulation 2019;139:1828–1845 [DOI] [PubMed] [Google Scholar]
- 34. McArdle PD, Greenfield SM, Avery A, Adams GG, Gill PS. Dietitians’ practice in giving carbohydrate advice in the management of type 2 diabetes: a mixed methods study. J Hum Nutr Diet 2017;30:385–393 [DOI] [PubMed] [Google Scholar]