Abstract
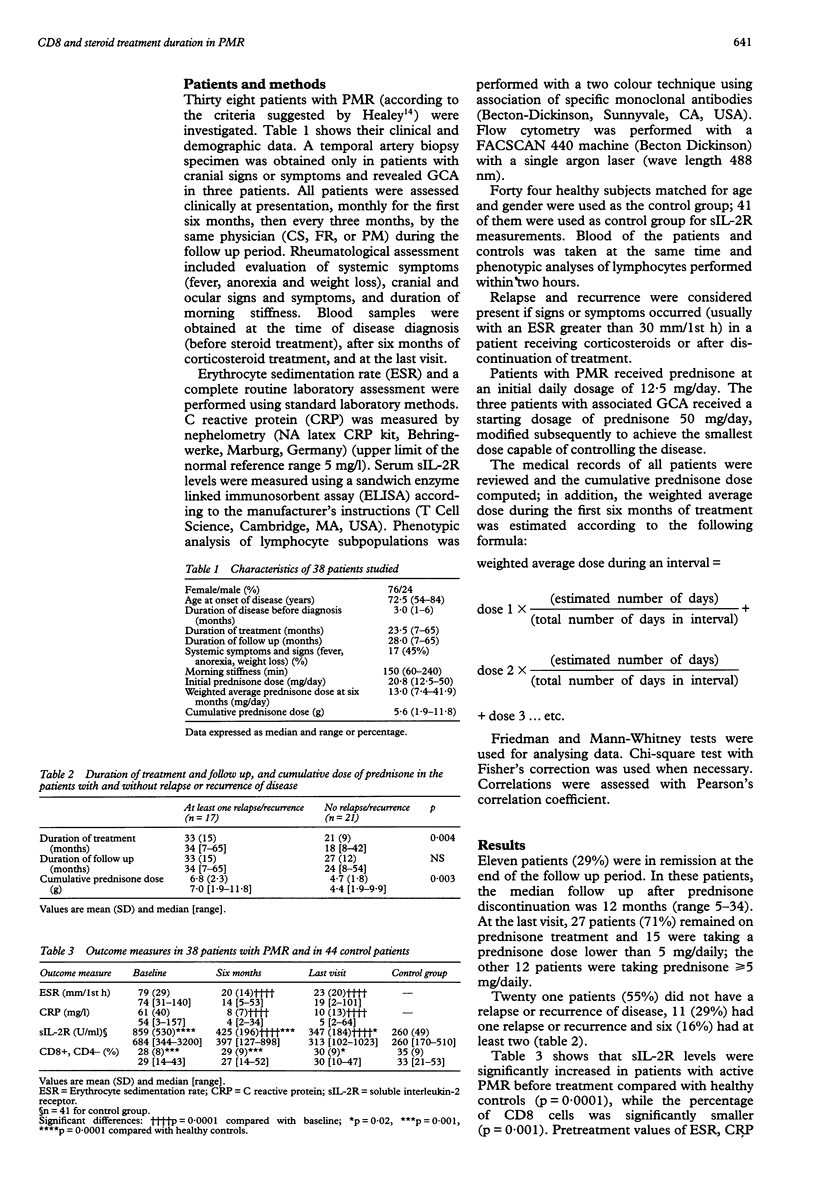
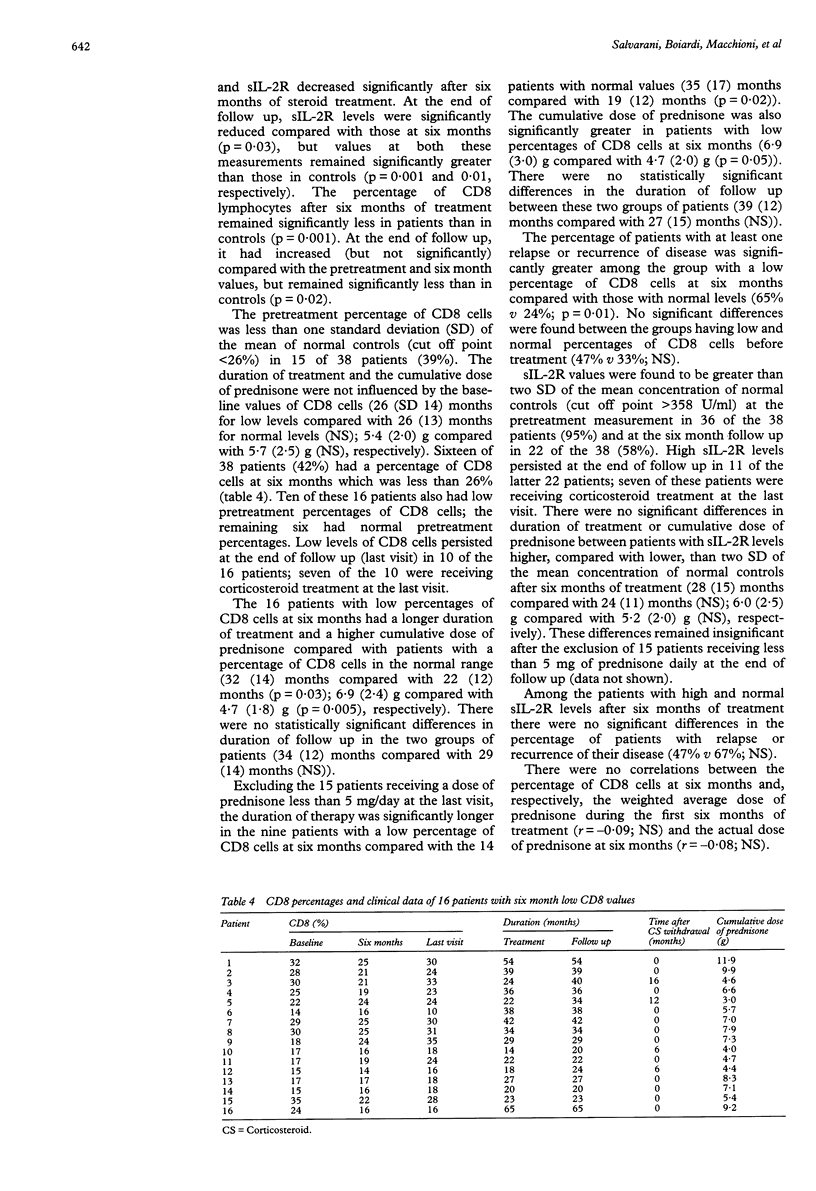
OBJECTIVES--To determine if the presence of low percentages of CD8 positive cells or high levels of soluble interleukin-2 receptors (sIL-2R) define a subgroup of patients with more severe polymyalgia rheumatica and giant cell arteritis (PMR/GCA). METHODS--38 PMR/GCA patients were followed up prospectively. Serum levels of sIL-2R and peripheral blood CD8 lymphocytes were measured before the start of corticosteroid treatment, after six months of treatment and at the last visit. Phenotypical analysis of lymphocyte subpopulations was performed with a two colour technique, and assay of sIL-2R was performed using an enzyme-linked immunosorbent kit. Forty four healthy people matched for age and gender comprised a healthy control group. RESULTS--The median duration of follow up was 28 months (range 7-65). Corticosteroid treatment lasted a median of 23.5 months (7-65). Eleven patients (29%) were in remission at the end of follow up; 45% of the patients had at least one relapse or recurrence. Compared with controls, patients with active disease had a significantly lower percentage of CD8 cells and significantly increased sIL-2R levels. Erythrocyte sedimentation rate, C reactive protein, and sIL-2R values were significantly less after six months of steroid treatment compared with before treatment. The percentage of CD8 cells remained significantly lower at six months and the end of follow up compared with controls, while sIL-2R levels remained significantly greater. Patients in whom the percentage of CD8 cells at six months was lower than one SD of the mean of normal controls (26%) had a significantly longer duration of corticosteroid treatment, a greater cumulative dose of prednisone and more relapses or recurrences compared with patients in whom the percentage was in the normal range. The duration of treatment and the cumulative dose of prednisone were not influenced by the percentage of CD8 cells before treatment therapy or by the levels of sIL-2R after six months of treatment. CONCLUSIONS--A reduced percentage of CD8 cells after six months of treatment may be a useful outcome parameter which would identify a group of PMR/GCA patients likely to experience more severe disease, defined as longer duration of corticosteroid treatment, higher cumulative dose of prednisone, and relapse or recurrence of disease.
Full text
PDF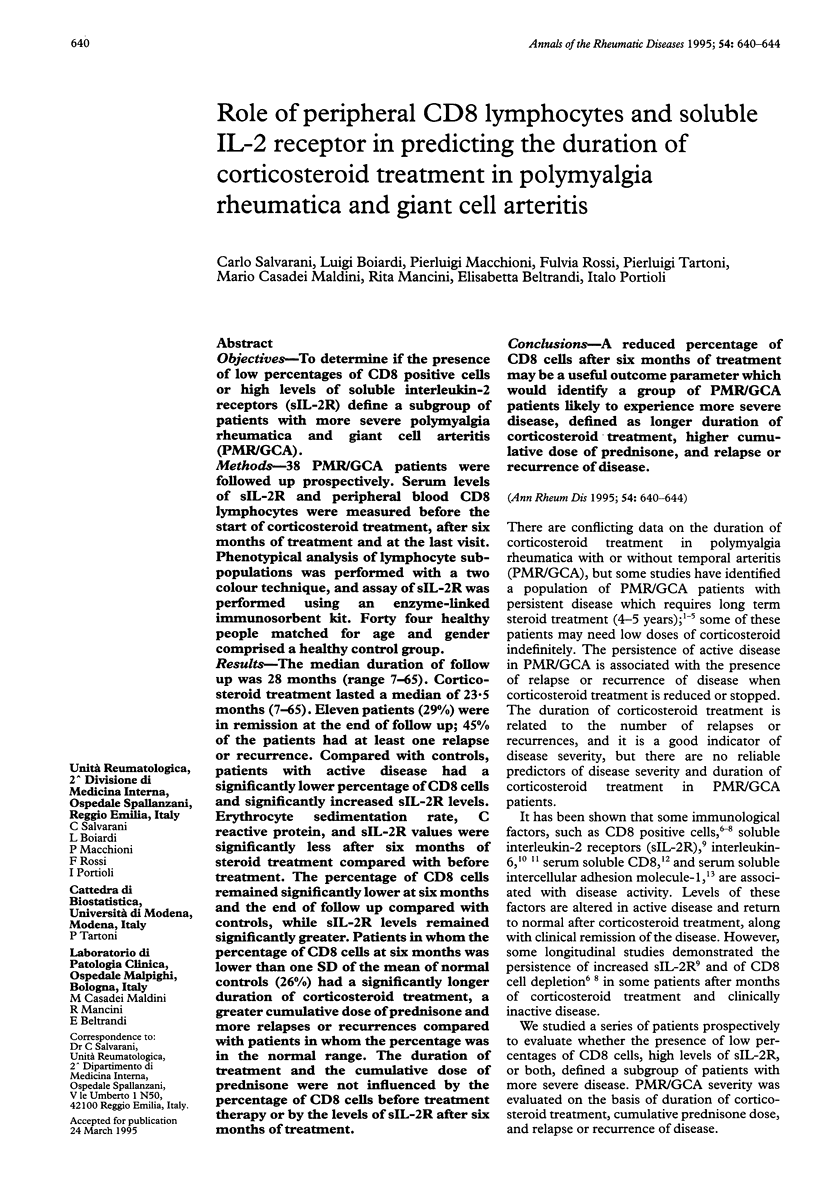

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Andersson R., Malmvall B. E., Bengtsson B. A. Long-term corticosteroid treatment in giant cell arteritis. Acta Med Scand. 1986;220(5):465–469. doi: 10.1111/j.0954-6820.1986.tb02796.x. [DOI] [PubMed] [Google Scholar]
- Arnold M. H., Corrigall V. M., Pitzalis C., Panayi G. S. The sensitivity and specificity of reduced CD8 lymphocyte levels in the diagnosis of polymyalgia rheumatica/giant cell arteritis. Clin Exp Rheumatol. 1993 Nov-Dec;11(6):629–634. [PubMed] [Google Scholar]
- Ayoub W. T., Franklin C. M., Torretti D. Polymyalgia rheumatica. Duration of therapy and long-term outcome. Am J Med. 1985 Sep;79(3):309–315. doi: 10.1016/0002-9343(85)90309-2. [DOI] [PubMed] [Google Scholar]
- Behn A. R., Perera T., Myles A. B. Polymyalgia rheumatica and corticosteroids: how much for how long? Ann Rheum Dis. 1983 Aug;42(4):374–378. doi: 10.1136/ard.42.4.374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chuang T. Y., Hunder G. G., Ilstrup D. M., Kurland L. T. Polymyalgia rheumatica: a 10-year epidemiologic and clinical study. Ann Intern Med. 1982 Nov;97(5):672–680. doi: 10.7326/0003-4819-97-5-672. [DOI] [PubMed] [Google Scholar]
- Dasgupta B., Duke O., Timms A. M., Pitzalis C., Panayi G. S. Selective depletion and activation of CD8+ lymphocytes from peripheral blood of patients with polymyalgia rheumatica and giant cell arteritis. Ann Rheum Dis. 1989 Apr;48(4):307–311. doi: 10.1136/ard.48.4.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dasgupta B., Panayi G. S. Interleukin-6 in serum of patients with polymyalgia rheumatica and giant cell arteritis. Br J Rheumatol. 1990 Dec;29(6):456–458. doi: 10.1093/rheumatology/29.6.456. [DOI] [PubMed] [Google Scholar]
- Delecoeuillerie G., Joly P., Cohen de Lara A., Paolaggi J. B. Polymyalgia rheumatica and temporal arteritis: a retrospective analysis of prognostic features and different corticosteroid regimens (11 year survey of 210 patients). Ann Rheum Dis. 1988 Sep;47(9):733–739. doi: 10.1136/ard.47.9.733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elling P., Olsson A., Elling H. CD8+ T lymphocyte subset in giant cell arteritis and related disorders. J Rheumatol. 1990 Feb;17(2):225–227. [PubMed] [Google Scholar]
- Healey L. A. Long-term follow-up of polymyalgia rheumatica: evidence for synovitis. Semin Arthritis Rheum. 1984 May;13(4):322–328. doi: 10.1016/0049-0172(84)90012-x. [DOI] [PubMed] [Google Scholar]
- Kyle V., Hazelman B. L. Stopping steroids in polymyalgia rheumatica and giant cell arteritis. BMJ. 1990 Feb 10;300(6721):344–345. doi: 10.1136/bmj.300.6721.344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macchioni P., Boiardi L., Meliconi R., Salvarani C., Grazia Uguccioni M., Rossi F., Pulsatelli L., Facchini A. Elevated soluble intercellular adhesion molecule 1 in the serum of patients with polymyalgia rheumatica: influence of steroid treatment. J Rheumatol. 1994 Oct;21(10):1860–1864. [PubMed] [Google Scholar]
- Macchioni P., Boiardi L., Salvarani C., Rossi F., Casadei-Maldini M., Mancini R., Beltrandi E., Portioli I. Lymphocyte subpopulations analysis in peripheral blood in polymyalgia rheumatica/giant cell arteritis. Br J Rheumatol. 1993 Aug;32(8):666–670. doi: 10.1093/rheumatology/32.8.666. [DOI] [PubMed] [Google Scholar]
- Pountain G. D., Keogan M. T., Brown D. L., Hazleman B. L. Circulating T cell subtypes in polymyalgia rheumatica and giant cell arteritis: variation in the percentage of CD8+ cells with prednisolone treatment. Ann Rheum Dis. 1993 Oct;52(10):730–733. doi: 10.1136/ard.52.10.730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pountain G. D., Keogan M. T., Hazleman B. L., Brown D. L. Effects of single dose compared with three days' prednisolone treatment of healthy volunteers: contrasting effects on circulating lymphocyte subsets. J Clin Pathol. 1993 Dec;46(12):1089–1092. doi: 10.1136/jcp.46.12.1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roche N. E., Fulbright J. W., Wagner A. D., Hunder G. G., Goronzy J. J., Weyand C. M. Correlation of interleukin-6 production and disease activity in polymyalgia rheumatica and giant cell arteritis. Arthritis Rheum. 1993 Sep;36(9):1286–1294. doi: 10.1002/art.1780360913. [DOI] [PubMed] [Google Scholar]
- Salvarani C., Boiardi L., Macchioni P., Casadei Maldini M., Mancini R., Beltrandi E., Rossi F., Portioli I. Serum soluble CD4 and CD8 levels in polymyalgia rheumatica. J Rheumatol. 1994 Oct;21(10):1865–1869. [PubMed] [Google Scholar]
- Salvarani C., Macchioni P. L., Tartoni P. L., Rossi F., Baricchi R., Castri C., Chiaravalloti F., Portioli I. Polymyalgia rheumatica and giant cell arteritis: a 5-year epidemiologic and clinical study in Reggio Emilia, Italy. Clin Exp Rheumatol. 1987 Jul-Sep;5(3):205–215. [PubMed] [Google Scholar]
- Salvarani C., Macchioni P., Boiardi L., Rossi F., Casadei Maldini M., Mancini R., Beltrandi E., Spacca C., Lodi L., Portioli I. Soluble interleukin 2 receptors in polymyalgia rheumatica/giant cell arteritis. Clinical and laboratory correlations. J Rheumatol. 1992 Jul;19(7):1100–1106. [PubMed] [Google Scholar]


