Abstract
Major depressive disorder (MDD) is a common psychiatric illness with a wide range of symptoms such as mood decline, loss of interest, and feelings of guilt and worthlessness. Women develop depression more often than men, and the diagnostic criteria for depression mainly rely on female patients' symptoms. By contrast, male depression usually manifests as anger attacks, aggression, substance use, and risk-taking behaviors. Various studies have focused on the neuroimaging findings in psychiatric disorders for a better understanding of their underlying mechanisms. With this review, we aimed to summarize the existing literature on the neuroimaging findings in depression, separated by male and female subjects. A search was conducted on PubMed and Scopus for magnetic resonance imaging (MRI), functional MRI (fMRI), and diffusion tensor imaging (DTI) studies of depression. After screening the search results, 15 MRI, 12 fMRI, and 4 DTI studies were included. Sex differences were mainly reflected in the following regions: 1) total brain, hippocampus, amygdala, habenula, anterior cingulate cortex, and corpus callosum volumes, 2) frontal and temporal gyri functions, along with functions of the caudate nucleus and prefrontal cortex, and 3) frontal fasciculi and frontal projections of corpus callosum microstructural alterations. Our review faces limitations such as small sample sizes and heterogeneity in populations and modalities. But in conclusion, it reflects the possible roles of sex-based hormonal and social factors in the depression pathophysiology.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11682-023-00772-8.
Keywords: Depression, Neuroimaging, Systematic review, Sex, Gender, MRI
Introduction
Major depressive disorder (MDD) presents with mood decline, loss of interest, irritability, and feelings of guilt and worthlessness (McCarter, 2008; Yang et al., 2022). Moreover, it is associated with decreased appetite, weight changes, and sleep disturbances (Caroleo et al., 2019). Altogether, these chronic symptoms significantly lower the quality of life and may, in the most extreme of cases, lead to suicide (Hoobehfekr et al., 2021). MDD used to rank fourth in the global burden of the diseases in 2000 (Ustün et al., 2004); however, estimates show that it will be the leading cause of disease by 2030 (Lépine & Briley, 2011). The high prevalence of depression comorbidities among people play a significant role in its pathophysiology (Gadermann et al., 2012). Notably, its presence with chronic medical diseases is associated with increased medical symptoms burden, functional impairment, medical costs, poor adherence to treatments, and elevated morbidity and mortality (Gold et al., 2020; Katon, 2011). Additionally, about 80% of people with depression have other mental illnesses, including anxiety, personality disorder, or alcohol abuse (Melartin et al., 2002).
The manifestation of depression between men and women shows dissimilarities. Women are more likely to develop depression; however, depressed men are more than three times more likely to die from depression-related suicide than women (Herreen et al., 2022). The gender gap in incidence rates starts at age 12, peaks at adolescence (Cavanagh et al., 2016, 2017; Ogrodniczuk & Oliffe, 2011; Romans et al., 2007), and remains constant afterwards (Salk et al., 2017). Moreover, the presentation of depression varies between the two sexes. Male depression usually manifests as anger attacks, aggression, substance use, and risk-taking behaviors that mainly do not fit the diagnosis criteria for depression in the first stages (Cavanagh et al., 2016). In contrast, depressed women show appetite disturbance, impaired sleep, and depressed mood at a higher frequency and intensity than men. These symptoms are included as diagnostic criteria for MDD and are in line with the fact that females are more likely to be diagnosed with depression (Cavanagh et al., 2017; Romans et al., 2007). Depressed men are more prone to escaping behaviors as well; these include over-involvement at work and high sexual activities in the forms of extramarital affairs or a series of limited sexual encounters (Ogrodniczuk & Oliffe, 2011). Meanwhile, when compared to males, depressed females show more frequent depressive episodes in their lives and report higher rates of atypical depressive symptoms (excessive fatigue, overeating, and oversleeping), anxiety, and somatization (Smith et al., 2008).
On the other hand, social factors could affect one’s susceptibility to depression. For example, various studies have reported lower gender equality is significantly associated with higher rates of female depression and that populations with high gender equality experience a lower gender gap in depression (Kuehner, 2017). Other social factors, such as the lack of a partner in the household and having a small social network, can predict the onset of depression in men, and not in women, in later life (Sonnenberg et al., 2013). These factors imply that not only the biological sex but also the socially-constructed roles, behaviors, and expressions of sexes can affect depression.
The introduction of different neuroimaging tools such as magnetic resonance imaging (MRI), functional MRI (fMRI), and diffusion tensor imaging (DTI) in recent years has enabled researchers to study patterns of brain changes in various diseases (Filippi & Agosta, 2016). In healthy people, various studies have demonstrated brain-based sex differences. For example, whole-brain volumes and volumes of the amygdala and cerebellum are commonly reported to be larger in males, while exhibiting a high density of sex steroid receptors (Giedd et al., 2012). In fMRI studies, greater regional homogeneity (ReHo) in the orbitofrontal areas of females has been reported, which may be responsible for females' higher emotion perception ability (Zhang et al., 2020). Moreover, DTI findings indicate higher fractional anisotropy (FA) and radial diffusivity (RD) in healthy males' thalamus, corpus callosum (cc), and cingulum (Menzler et al., 2011). These changes in the thalamus and cingulum might be a result of sex differences in awareness, the neural processing of emotional stimuli, and interpersonal conflicts. Meanwhile, alterations of the corpus callosum might be associated with possible sex differences in hemispheric lateralization (Menzler et al., 2011).
Meanwhile, assessing depressed subjects, these imaging modalities suggest that depression affects the brain in various ways. For example, anatomical MRI studies show that the frontal lobe, parietal lobe, thalamus, caudate, pallidum, putamen, and temporal lobes of people with depression are distinct from those without it (Zhang et al., 2018). Moreover, depression is associated with lateral ventricle enlargement and larger cerebrospinal fluid (CSF) volume in people (Kempton et al., 2011). Ultra-high field (UHF, ≥ 7 T) MRI of depressed subjects has revealed smaller hippocampal in depressed people than controls and smaller subiculum in depressed individuals with multiple major depressive episodes compared to those with one episode (Cattarinussi et al., 2021).
DTI findings also reflect the microstructural changes of white matter: the FA of the corpus callosum (cc), bilateral anterior limb of the internal capsule, right inferior temporal gyrus, and right superior frontal gyrus are reduced in depression (Chen et al., 2017). The most prominent finding of functional studies is the abnormal involvement of the cortico-limbic mood-regulating circuit in depressed subjects (Wang et al., 2012). Although the literature provides data on brain changes in depression and on sex-based differences in the brain of healthy people, there is insufficient data regarding the male and female patterns of brain alterations during depression. Herein, we aim to contrast the sex differences in structural and functional changes of the brain in depression. To our knowledge, this is the first systematic review of neuroimaging studies to discuss so.
Methods and Materials
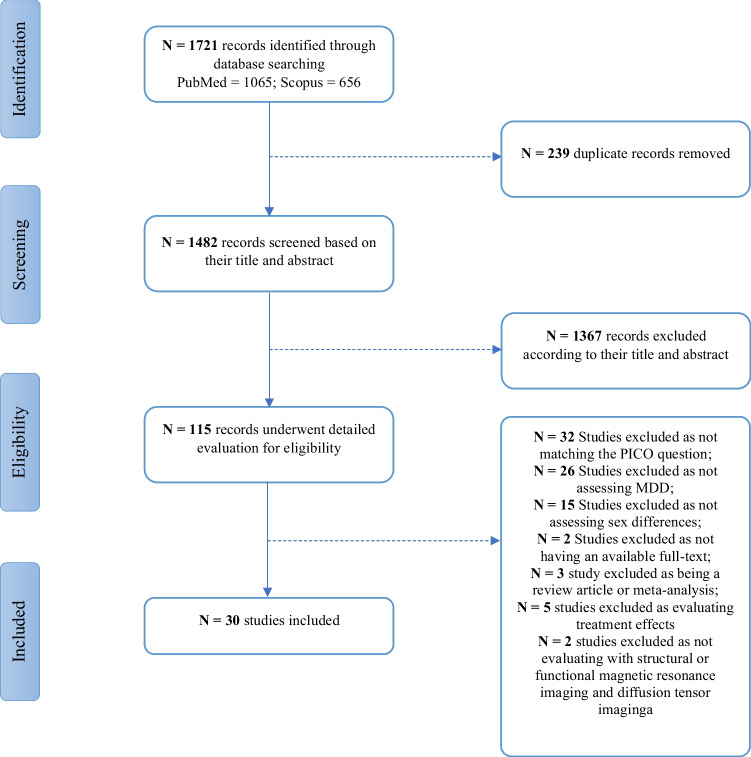
The present systematic review was prepared following the Preferred Reporting Items for Systematic Review and MetaAnalysis (PRISMA) guidelines (Swartz, 2011). Figure 1 illustrates the flow diagram of our study. Moreover, the study protocol was registered on the International Prospective Register of Systematic Reviews (PROSPERO) website (https://www.crd.york.ac.uk/PROSPERO/) with the code CRD42021288043.
Fig. 1.
Flow chart of the study selection
Literature Search and Study Selection
Using a combination of keywords, we searched two major databases, Pubmed and Scopus, to find relevant studies on November 19, 2022. Keywords adopted for the search were: "Diffusion Tensor Imaging" or "Diffusion weighted magnetic resonance imaging" or "Diffusion Tractography" or "Diffusion weighted imaging" or "Diffusion weighted MRI" or "DTI" or "White Matter" or "Grey Matter" or "Gray Matter" or "Magnetic Resonance Imaging" or "NMR Imaging" or "tomography NMR" or "tomography MR" or "Steady State Free Precession MRI" or "MRI" or "Zeugmatography" or "Imaging Chemical Shift" or "Magnetic Resonance Image" or "Magnetization Transfer Contrast Imaging" or "MRI Scan" or "Proton Spin Tomography" or "fMRI" or "Functional MRI" or "Functional Magnetic Resonance Imaging" or "Spin Echo Imaging" or "morphometry" or "VBM" or "cortical thickness" or "cortical surface area" or "subcortical volume" and "Phenotypic Sex" or "sex phenotypic" or "Genotypic Sex" or "Sex" or "Women" or "Female" or "Men" or "Male" or "Gender" or "Sex Difference" or "Gender Difference" and "Major Depressive Disorder" or "MDD" or "Depression" or "Depressive Symptoms" or "Depressive Symptom" or "Emotional Depression." Two reviewers independently screened articles by title and abstract to find potential relevant ones in the first step. Then, the full texts were retrieved to find eligible studies, and the discrepancies were resolved through discussion with a third reviewer. The third reviewer also monitored the whole process.
Inclusion and Exclusion Criteria
In this systematic review, we included observational case–control, cross-sectional, or cohort studies matching the PICO question that aimed to investigate the differences in neuroimaging findings of depression in both sexes. These studies could be case–control or cohort. Furthermore, we excluded the following: 1) studies that included participants suffering from other neurologic disorders 2) studies not related to major depressive disorder,3) studies that did not assess brain neuroimaging alterations, 4) studies that did not evaluate both sexes, 5) review articles, book chapters, opinions, letters, and conference abstracts, 6) animal, in-vitro, and other nonhuman studies.
Data Items
We extracted the following data points from studies: basic study characteristics such as author name, publication date, and study design, the sample size and sex ratio, the age of participants, their medications, means of neuroimaging, and measuring tools of depression. We also mentioned if the probands were matched for variables such as sex, age, and education. Two reviewers independently extracted the aforementioned data. Discrepancies were resolved through discussion with a third reviewer.
Quality Assessment
The quality of included studies was assessed using the e Newcastle–Ottawa scale (NOS) for case–control studies (Stang, 2010). This scale evaluates the data quality in three aspects: selection, comparability, and exposure in case–control studies or cohort study outcomes. A maximum score of nine and eight stars in cohort and case–control studies can be allocated to a particular study in this assessment tool. Furthermore, the risk of publication bias was assessed for each study. We used the publication bias criteria introduced by Viswanathan et al. in a design-specific manner (Viswanathan et al., 2008).
Results
Overview
The initial search yielded 1721 results. After removing the automatic and manual duplicates, we screened the remaining 1482 studies based on titles and abstracts to find potentially eligible studies. 115 studies went through screening the full-texts, of which 85 were excluded due to following reasons: 32 studies due to not matching the PICO question of our study (Acosta et al., 1991; Cohen et al., 2013; Dean et al., 2018; Deng et al., 2018; Elbejjani et al., 2014; Frodl et al., 2002; Gorham et al., 2019; Acosta et al., 2020; Hay et al., 2020; Keller et al., 2021; Lebedeva et al., 2015; Lee et al., 2019; Li et al., 2022; MacMaster et al., 2008; Maller et al., 2007; Meruelo et al., 2021; Perlman et al., 2017; Pettemeridou et al., 2021; Pimontel et al., 2013; Saleh et al., 2012; Savitz et al., 2011; Schmaal et al., 2017a; Soe et al., 2018; Takahashi et al., 2016; Tol et al., 2010; Wang et al., 1991, 2019; Wei et al., 2021; Wen et al., 2017; Woo et al., 2009; Wu et al., 1993; Zhang et al., 1991), 26 studies due to not assessing major depression (Averill et al., 2017; Brébion et al., 2021a, 2021b; Carlson et al., 2015; Čermaková et al., 2020; Chahal et al., 2022a; Dotson et al., 2013; Elbejjani et al., 2015; Ellis et al., 2019; Frodl et al., 2010, 2017; Hayakawa et al., 2014; Kim et al., 2019; Kircanski et al., 2019; Kirton et al., 2014; Kronmüller et al., 2008; Li et al., 2020; Liu et al., 2012; Maglanoc et al., 2020; Moulinet et al., 2021; Murray et al., 2013; Rajagopalan et al., 1994; Rakesh et al., 2021; Spalletta et al., 2014; Tozzi et al., 2020; Victor et al., 2017), 15 due to not assessing sex differences, 5 studies due to evaluating treatment effects (Domschke et al., 2008; Reinlieb et al., 2014; Vakili et al., 2000; Wei et al., 2018; Williams et al., 2021), 2 studies due to unavailable full-texts (Huang et al., 2014; Lavretsky et al., 2004), 2 studies as not assessing with MRI, fMRI, or DTI (Binesh et al., 2004; Staley et al., 2006), and 3 study due to being review articles or meta-analyses (Binnewies et al., 2022; Delvecchio et al., 2017; Peng et al., 2016).
Thirty studies were included in our systematic review: 15 MRI studies (Ancelin et al., 2019; Carceller-Sindreu et al., 2015; Cyprien et al., 2014; Furtado et al., 2008; Hastings et al., 2004; Kong et al., 2013; Kronmüller et al., 2009; Lavretsky et al., 1998; Lewine et al., 1995; MacMaster et al., 2006; Nielsen et al., 2020; Piani et al., 2021; Ritter et al., 2021; Soriano-Mas et al., 2011; Yang et al., 2017), 12 fMRI studies (De Almeida et al., 2011; Amiri et al., 2021; Briceño et al., 2015; Chuang et al., 2017; Dong et al., 2022; Geng et al., 2019; Jenkins et al., 2018; Mei et al., 2022; Piani et al., 2021; Talishinsky et al., 2022; Yao et al., 2014; Young et al., 2017), and 4 DTI ones (Ho et al., 2021; Kliamovich et al., 2021; Lyon et al., 2019; Ugwu et al., 2015) (One study had assessed both MRI and fMRI findings (Piani et al., 2021). The publication year of MRI studies varied from 1995 to 2022. However, due to their novelty, fMRI and DTI studies were all published after 2011. All studies had recruited more females than males, except three with exact equal numbers (Lavretsky et al., 1998; Mei et al., 2022; Young et al., 2017) and one with less females (Yang et al., 2017). Moreover, most studies focused only on the presence of major depressive disorder. Regarding the depression phenotype, however, some others assessed only treatment-resistant (Amiri et al., 2021; Furtado et al., 2008; Talishinsky et al., 2022), late-life (Cyprien et al., 2014), somatic/non-somatic (Geng et al., 2019), remitted (Jenkins et al., 2018), first episode/chronic/recurrent (Carceller-Sindreu et al., 2015), and early/late-onset depression (Lavretsky et al., 1998).
While Healthy probands formed the majority of controls, one study included patients with schizophrenia, schizoaffective, and bipolar disorder as controls as well (Lewine et al., 1995) and another study only compared early-onset and late-onset depression patients (Lavretsky et al., 1998). One study had also categorized both the case and control participants regarding their child adversity history (Ugwu et al., 2015). Details of medication regimens in depressed subjects were provided in 25 studies. Among these, participants of 12 studies did not take any medications (Dong et al., 2022; Hastings et al., 2004; Jenkins et al., 2018; Kliamovich et al., 2021; Kong et al., 2013; Lavretsky et al., 1998; MacMaster et al., 2006; Mei et al., 2022; Piani et al., 2021; Ritter et al., 2021; Yang et al., 2017; Yao et al., 2014; Young et al., 2017). Eleven studies' probands administered antidepressants (De Almeida et al., 2011; Ancelin et al., 2019; Chuang et al., 2017; Cyprien et al., 2014; Furtado et al., 2008; Geng et al., 2019; Kronmüller et al., 2009; Lyon et al., 2019; Piani et al., 2021; Talishinsky et al., 2022; Ugwu et al., 2015). Of note, the probands' medications were a combination of Imipramine, selective serotonin reuptake inhibitors (SSRI), Venlafaxine, Clomipramine, and other antidepressants (Soriano-Mas et al., 2011). The characteristic data of included studies are presented in Table 1.
Table 1.
Characteristics of included studies
| Study | Study design | Study groups | Sample size (F/M) | Age (years) (mean± SD) |
MRI/DTI/fMRI | Measure of depression | Medication | Matched for |
|---|---|---|---|---|---|---|---|---|
| Amiri et al., 2021 | Case-control |
TRD HC |
21/10 18/11 |
35.7±9.1 31.7±6.1 |
fMRI | HAMD-17 | NR | - |
| Ancelin et al., 2019 | Case-control |
Lifetime MDD No lifetime MDD |
320/290 (total) | 70.7 (median) | MRI |
DSM-IV MINI |
Antidepressants | - |
| Briceño et al., 2015 | Case-control |
MDD HC |
27/26 31/26 |
46.1 (mean) 44.1 (mean) |
fMRI |
DSM-IV HDRS |
NR | Age, sex |
| Carceller-Sindreu et al., 2015 | Case-control |
First-episode MDD Remitted-recurrent MDD Chronic MDD HC |
14/7 18/2 16/4 24/10 |
44.4±6.7 47.1±8.2 48.6±8.0 47.9±8.1 |
MRI |
DSM-IV-TR HDRS |
Psychotropic medication | Age, gender distribution, educational level |
| Chuang et al., 2017 | Case-control |
MDD HC |
82/24 24/10 |
15.72±1.10 (F) 15.25±1.52 (M) 15.89±1.42 (F) 15.26+1.22 (M) |
fMRI | DSM-IV | Antidepressants | Age, sex, handedness |
| Cyprien et al., 2014 | Cohort |
LLD Non-LLD |
75/45 137/210 |
70.8±4.0 71.1±4.0 |
MRI |
MINI CES-D Antidepressant intake |
Antidepressants, Antihypertensives | - |
| De Almeida et al., 2011 | Case-control |
MDD HC |
12/7 12/7 |
30.3±7 31.8±6.8 |
fMRI | HDRS | Antidepressant, mood stabilizer, antipsychotic, and anxiolytics | Age, sex |
| Dong et al., 2022 | Case-control |
MDD HC |
76/48 137/106 |
25.68±7.90 (F) 24.75±5.16 (M) 21.33±4.28 (F) 20.54±2.13 (M) |
fMRI |
DSM-IV-TR HAMD-17 |
No | Sex |
| Furtado et al., 2008 | Case-control |
TRD HC |
23/22 17/13 |
37.53±11.3 36.6±11.09 |
MRI |
DSM-IV MINI HDRS |
Antidepressants (TCA, NaSSA, NRI, RIMA, SNRI) | Age, sex |
| Geng et al., 2019 | Case-control |
SD NSD HC |
15/13 16/14 13/17 |
37.21±7.16 34.10±9.91 35.83±8.15 |
fMRI |
DSM-IV MINI HAMD-17 |
Antidepressants (SSRI, SNRI, NaSSA, Benzodiazepines) | Age, education, gender |
| Hastings et al., 2004 | Case-control |
MDD HC |
10/8 10/8 |
38.9±11.4 34.8±13.6 |
MRI |
DSM-III-R SCID-P SCID-NP |
No | Sex |
| Ho et al., 2021 | Case-control |
MDD HC |
34/14 19/16 |
16.32±1.19 15.75±1.22 |
DTI |
DSM-IV K-SADS-PL RADS-2 |
Psychotropic medication | - |
| Jenkins et al., 2018 | Case-control |
rMDD HC |
32/16 25/15 |
21.72±1.28 (F) 20.69±1.62 (M) 21.00±1.63 (F) 20.67±1.76 (M) |
fMRI | DSM-IV-TR | No | Sex |
| Kliamovich et al., 2021 | Cohort |
MDD HC |
39/24 184/215 |
14.88±1.44 14.87±1.78 |
DTI |
DSM-IV SSAGA |
No | - |
| Kong et al., 2013 | Case-control |
MDD HC |
16/13 17/16 |
28.88±9.71 (F) 31.23±8.39 (M) 28.00±9.09 (F) 31.81±7.05 (M) |
MRI |
DSM-IV HAMD |
No | Age, education |
| Kronmuller et al., 2009 | Case-control |
FEMD RMD HC |
13/13 20/11 19/11 |
41.46±16.64 (F) 38.08±11.88 (M) 45.85±11.78 (F) 48.27±8.73 (M) 42.68±13.98 (F) 42.00±11.28 (M) |
MRI |
DSM-IV SCID HDRS |
Antidepressants (TCA, SSRI, Other new antidepressants) | - |
| Lavretsky et al., 1998 | Case-control |
EOD LOD |
21/12 27/36 |
57.0±5.9 63.9±8.0 |
MRI |
DSM-III-R HAM-D |
No | - |
| Lewine et al., 1995 | Case-control |
Schizophrenia Schizoaffective Major depression Bipolar HC |
26/82 13/7 20/7 15/5 91/59 |
33.9±7.3 (F) 32.4±8.1 (M) 39.6±10.1 (F) 39.4±9.0 (M) 41.4±10.4 (F) 39.3±11.9 (M) 39.7±6.9 (F) 32.6±6.3 (M) 35.2±9.9 (F) 31.5±8.2 (M) |
MRI | DSM-III-R | NR | - |
| Lyon et al., 2019 | Cohort |
MDD HC |
115/106 34/33 |
33.6±11.7 30.3±12.8 |
DTI |
DSM-IV HAMD |
Escitalopram, sertraline, or venlafaxine-extended release | Sex, education |
| MacMaster et al., 2006 | Case-control |
MDD HC |
20/15 20/15 |
14.72±2.16 (F) 13.82±2.81 (M) 14.72±2.33 (F) 14.19±2.83 (M) |
MRI |
DSM-IV CDRS-R |
No | Age, sex |
| Mei et al., 2022 | Case-control |
MDD HC |
36/25 36/25 |
36.1±10.7 (F) 36.4±12.8 (M) 36.6±11.8 (F) 34.9±11.9 (M) |
fMRI |
DSM-IV HAMD |
No | Age, sex, education |
| Nielsen et al., 2020 | Cohort |
MDD High-risk Low-risk |
30/22 (total) |
17.34±0.98 (total) |
MRI | CDI | NR | - |
| Piani et al., 2021 | Case-control |
MDD HC |
7/5 5/7 |
66.5±9.1 68.7±12.3 |
MRI fMRI |
DSM-V HDRS DASS-21 |
Antidepressants, anticonvulsants, mood stabilizer, antipsychotics, and NSAIDs | Age |
| Ritter et al., 2021 | Case-control |
Current MDD Past MDD Healthy |
20/12 41/9 128/71 |
24.9±6.23 (F) 27.8±3.93 (M) 23.9±4.34 (F) 23.4±2.88 (M) 24.9±4.48 (F) 24.8±1.53 (M) |
MRI (PWI) |
DSM-IV SCID-IV HAM-D MADRS BDI |
No | - |
| Soriano-Mas et al., 2011 | Cohort |
MDD HC |
41/29 23/17 |
61.56±9.68 59.23±7.09 |
MRI |
DSM-IV HAM-D |
Imipramine SSRI Venlafaxine Clomipramine Other antidepressants |
- |
| Talishinsky et al., 2022 | Cohort |
TRD HC |
223/148 103/79 |
41.9±11.4 35.1±13.0 |
fMRI |
DSM-V HDRS |
Antidepressants, Psychotropic medication | - |
| Ugwu et al., 2015 | Case-control |
MDD with CA MDD without CA HC with CA HC without CA |
11/13 17/5 9/8 18/11 |
40±9.1 41±11.2 36±13.5 36±12.0 |
DTI |
DSM-IV-TR HDRS BDI-II MADRS |
Antidepressants | Age, gender |
| Yang et al., 2017 | Case-control |
MDD HC |
53/29 53/29 |
30.21±10.79 (F) 27.48±7.55 (M) 29.06±9.10 (F) 26.38±6.91 (M) |
MRI |
DSM-IV-TR HAMD |
No | Age, education, intelligence quotient |
| Yao et al., 2014 | Case-control |
MDD HC |
13/14 15/15 |
35.3±7.3 (F) 31.1±9.6 (M) 31.3±7.8 (F) 30.9±6.6 (M) |
fMRI |
DSM-IV-TR HDRS |
NR | Age, education |
| Young et al., 2017 | Case-control |
MDD HC |
20/20 20/20 |
35.5±8.13 (F) 36.1±10.2 (M) (HC NR) |
fMRI |
SCID HDRS |
No | Age, sex |
Abbreviations: MRI: Magnetic resonance imaging, DTI: Diffusion tensor imaging, fMRI: Functional magnetic resonance imaging, DSM (-TR): Diagnostic and Statistical Manual of Mental Disorders (-Text revision), HAMD or HDRS: Hamilton Depression Rating Scale, MINI: Mini-International Neuropsychiatric Interview, CES-D: Centre for Epidemiologic Studies-Depression Scale, SCID: Structured Clinical Interview DSM-III-R, K-SADS-PL: Kiddie Schedule for Affective Disorders and Schizophrenia - Present and Lifetime, RADS: Reynolds Adolescent Depression Scale, SSAGA: Semi-Structured Assessment for the Genetics of Alcoholism, CDRS-R: Childhood Depression Rating Scale-Revised, CDI: Children's Depression Inventory, DASS-21: Depression Anxiety and Stress Scales-21, NSAID: nonsteroidal anti-inflammatory drugs, MADRS: Montgomery-Asberg Depression Rating Scale, BDI: Beck’s Depression Inventory, MDD: Major depressive disorder, rMDD: Remitted major depressive disorder, TRD: Treatment-resistant depression, LLD: Late-life depression, SD: Somatic depression, NSD: Non-somatic depression, FEMD: First episode major depression, RMD: Recurrent major depression, EOD: Early-onset depression, LOD: Late-onset depression, CA: Childhood adversity, HC: Healthy control, TCA: Tricyclic antidepressant, SSRI: Selective serotonin reuptake inhibitor, NaSSA: Noradrenergic and specific serotonergic antidepressant, NRI: Norepinephrine reuptake inhibitor, SNRI: Serotonin-norepinephrine reuptake inhibitor antidepressant, RIMA: Reversible inhibitor of monoamine oxidase A antidepressant, NR: Not reported, F: Female, M: Male, SD: Standard deviation, PWI: Perfusion-weighted imaging.
-: Data not reported.
Quality of the Included Studies
The quality of included studies is provided in Supplementary Tables S1 and S2. Studies were assessed regarding the case selection, comparability, and exposure in case–control studies or cohort study outcomes. Moreover, as presented in Table 1, participants were matched for age in 14 studies, for sex in 14 studies, and for education in 7 studies. The publication bias risk of each included study is demonstrated in Supplementary Table S3.
Analysis of Depression
Included studies used various tools to measure depression in participants. The 17-item Hamilton Depression Rating Scale (HAMD-17/HDRS) (Hamilton, 1960) was the most frequently used depression assessment (De Almeida et al., 2011; Amiri et al., 2021; Briceño et al., 2015; Carceller-Sindreu et al., 2015; Dong et al., 2022; Furtado et al., 2008; Geng et al., 2019; Kong et al., 2013; Kronmüller et al., 2009; Lyon et al., 2019; Mei et al., 2022; Piani et al., 2021; Ritter et al., 2021; Soriano-Mas et al., 2011; Talishinsky et al., 2022; Ugwu et al., 2015; Yang et al., 2017; Yao et al., 2014). Some others used interviews such as the Mini-International Neuropsychiatric Interview (MINI) (Ancelin et al., 2019; Cyprien et al., 2014; Furtado et al., 2008; Geng et al., 2019; Sheehan et al., 1998) and structural clinical interview for DSM disorders (SCID) (Hastings et al., 2004; Kronmüller et al., 2009; Ritter et al., 2021; Spitzer et al., 1992; Young et al., 2017) to evaluate depression in subjects. To diagnose depression, one study (Ho et al., 2021a) also used Kiddie Schedule for Affective Disorders and Schizophrenia—Present and Lifetime (K-SADS-PL) (Kaufman et al., 1997). Another study (Kliamovich et al., 2021) employed the Semi-Structured Assessment for the Genetics of Alcoholism (SSAGA) (Brown et al., 2015). Some studies also scored the severity of depression in participants; the measurement tools included the Centre for Epidemiologic Studies-Depression Scale (CDS-D) (Cyprien et al., 2014; Radloff, 1977), Children's Depression Inventory (CDI) (Kovacs n.d; Nielsen et al., 2020), Beck's Depression Inventory (BDI) (Beck et al., 1961; Ritter et al., 2021; Ugwu et al., 2015), Reynolds Adolescent Depression Scale (RADS-2) (Ho et al., 2021a; Reynolds, 2004), Depression Anxiety and Stress Scales-21 (DASS-21) (Osman et al., 2012; Piani et al., 2021), Childhood Depression Rating Scale-Revised (MacMaster et al., 2006; Poznanski et al., 1985), and Montgomery-Asberg Depression Rating Scale (MADRS) (Montgomery & Asberg, 1979; Ritter et al., 2021; Ugwu et al., 2015). The details of all measurement tools are provided in Table 1.
MRI Studies
A total of 15 studies were selected. As presented in Table 2, most studies explored merely the volume of brain regions. Among these, three studies reported changes in the amygdala. Assessing people with a lifetime history of depression and people with current MDD, the first one revealed that there was an association between depression history and lower gray matter (GM) volumes in men's amygdala, in contrast to women (Ancelin et al., 2019). The other reported that females with MDD tend to have a smaller amygdala than healthy females (Hastings et al., 2004). Other findings of these studies included a larger rostral anterior cingulate cortex in women with a lifetime MDD than their male counterparts (Ancelin et al., 2019) and a smaller inferior anterior cingulate normalized volume in MDD males than their healthy counterparts (Hastings et al., 2004). Their exploration of the orbitofrontal cortex, total cerebral volume, and hippocampus did not show any sex differences.
Table 2.
Overview of MRI studies on sex differences in depression
| Study | Tesla sequence | Measures | Brain areas | Methods for Sex Differences Analyses Sex by Diagnosis Effects |
Covariates | Results | ||
|---|---|---|---|---|---|---|---|---|
| Model | Tested? | Findings | ||||||
| Ancelin et al., 2019 |
1.5 T T1 |
Volume |
Hippocampus Amygdala Orbitofrontal cortex ACC |
GLM | Yes | Yes | Age, total brain volume, education level, head injury, cardiovascular ischemic pathologies and antidepressant use, lifetime anxiety disorder |
A positive association between lifetime MDD and smaller GM volumes in men's amygdala and caudate nucleus. No such association in women. Women exhibited larger rostral ACC volumes than men. |
| Carceller-Sindreu, 2015 |
3 T T1 |
Volume |
Habenular nuclei TIV |
GLM | Yes | Yes | Age, educational level, TIV, medication load | Increased Hb-WM volume in women with a first-episode MDD. |
| Cyprien et al., 2014 |
1.5 T T1 |
Volume |
Corpus callosum TBV |
GLM | Yes | Yes | Education, global cognitive impairment, ischemic pathologies, left-handedness, WML volume, intracranial volume, past major depression episode |
A positive association in women between the incidence of LLD and smaller anterior, mid, posterior, and total CC areas. No associations in men. |
| Furtado et al., 2008 |
1.5 T T1 |
Volume |
ERC ICV TBV |
GLM | Yes | Yes | Age, ICV, TBV |
Lower ICV and TBV/ICV in male patients than male controls. No such association in females. Lower TBV in female patients than female controls. Larger L and R ERC in male patients than female patients. |
| Hastings et al., 2004 |
1.5 T T1 |
Volume |
Amygdala Hippocampus IAC OPFC TCV |
GLM | Yes | Yes | Age, total years of education, age at first episode of major depression, and number of major depressive episodes, family history of depression, reported history of sexual or physical abuse, suicide attempt status |
Depressed females had a 23% smaller R amygdala and a 15% smaller L amygdala than healthy females. Depressed males had a 22% smaller IAC normalized volume than healthy males. |
| Kong et al., 2013 | 3 T |
GM volume GM density |
Bilateral amygdala, hippocampus, striatum, and PFC | ANOVA | Yes | Yes | N/A |
Reduced GM density in the bilateral amygdala and hippocampus of MDD females compared to HC females Reduced GM density in the bilateral caudate extending to the left ventral striatum of MDD males compared to the HC males Reduced GM volume in bilateral caudate of MDD males compared to HC males |
| Kronmuller et al., 2009 |
1.5 T T1 |
Volume |
Hippocampus TBV |
GLM | Yes | Yes | Age, diagnostic group, TCV |
A L-R asymmetry in hippocampal volume with smaller L hippocampal volume in FEMD males than Healthy males. No difference in TBV. |
| Lavretsky et al., 1998 |
1.5 T T1, T2 |
WMH, VBR | Whole brain | GLM | Yes | No | Age, age at onset |
More males had large WMH than females. No significant difference in VBR. |
| Lewine et al., 1995 |
1.5 T T2 |
Volume WMH Ventricular anomaly |
Whole brain | NR | Yes | Yes | History of substance abuse or physical trauma | Less normal scans in schizophrenic and MDD men than women in either group. |
| MacMaster et al., 2006 | 1.5 T | Volume | Pituitary gland | ANCOVA | Yes | Yes | Age, intracranial volume | Larger pituitary gland volumes in MDD males compared to HC males, while there were no significant diagnostic group differences in the pituitary volume of females. |
| Nielsen et al., 2020 | NR | CT | OFC | MLM | Yes | Yes | Age at the time of scan, maternal depression history |
Inverse association between depressive symptoms and CT of the L lateral OFC in males. Positive association in the L medial OFC in females between CT and depressive symptoms. |
| Piani et al., 2021 | 3 T | GM volume | Whole brain | GLM | Yes | Yes | None (univariate) |
Comparable regional GM volumes between MDD and HC groups across diagnosis by sex subsets. Larger normalized GM volumes of calcarine, olfactory, and orbitofrontal regions in healthy females than in healthy males, but lower in MDD females compared to MDD males. |
|
Ritter et al., 2021 (PWI) |
3 T | Perfusion | Whole brain | GLM | Yes | Yes | Whole-brain perfusion |
Negative association between perfusion and depressive symptoms in females for the HAM-D, BDI, and MADRS. Positive association in males for the MADRS. |
| Soriano-Mas et al., 2011 | 1.5 T | Gray and white matter volume | Whole brain | GLM | Yes | Yes | Age, time between scans, global tissue volume | A significant GM volume reduction in the R thalamus in male MDD patients. |
| Yang et al., 2017 | 3 T | GM volume | Whole brain | ANCOVA | Yes | Yes | Age, GM volume, whole brain volume |
Decreased GM volume of middle/superior temporal gyrus and ventromedial prefrontal gyrus in MDD males compared to HC males Increased GM volume of cerebellum in MDD males compared to HC males Decreased GM volume of dorsomedial prefrontal gyrus extending to SMA and lingual extending to parahippocampal gyrus in MDD females compared to HC females |
Abbreviations: MRI: Magnetic resonance imaging, ACC: Anterior cingulate cortex, TIV: Total intracranial volume, TBV: Total brain volume, ICV: Intracranial volume, TCV: Total cerebral volume, ERC: Entorhinal cortex, IAC: Inferior anterior cingulate, OPFC: Orbital prefrontal cortex, OFC: Orbitofrontal cortex, MDD: Major depressive disorder, GM: Gray matter, WM: White matter, WML: White matter lesions, Hb: Habenula, CC: Corpus callosum, LLD: Late-life depression, PFC: prefrontal cortex, FEMD: First episode major depression, MADRS: Montgomery-Asberg Depression Rating Scale, BDI: Beck’s Depression Inventory, HAM-D: Hamilton Depression Rating Scale, WMH: White-matter hyperintensities, VBR: Ventricle-to-brain ratio, CT: Cortical thickness, PWI: Perfusion-weighted imaging, GLM: General linear model, ANCOVA: Analysis of covariance, MLM: Multilevel modeling, SMA: supplementary motor area, T: Tesla, L: Left, R: Right, NR: Not reported, N/A: Not applicable.
Another MRI study assessed both GM density and volume of the amygdala in depressed people and healthy controls (Kong et al., 2013). They reported reduced GM density in the bilateral amygdala of MDD females compared to HC females and reduced GM density and volume in the bilateral caudate of MDD males compared to their healthy counterparts. Regarding the hippocampus, in contrast to previous studies, sex differences were reflected in its lower GM density in MDD females than in HC females, which was not seen in males (Kong et al., 2013).
Similar to the latter study, the hippocampus reflected sex differences in another study. Males with the first episode of MDD exhibited a left–right asymmetry in hippocampal volume with smaller left hippocampal volume compared to healthy controls based on their findings (Kronmüller et al., 2009). The researchers also tested if total brain volume differed in people with MDD and healthy controls, which was disproven (Kronmüller et al., 2009). However, an association between smaller size of total brain volumes and depressive symptoms in women with treatment-resistant depression was observed (Furtado et al., 2008). Other results were as follows: 1) lower intracranial volume and total brain volume to intracranial volume ratios in male patients than in male controls and 2) greater entorhinal cortex volume in male patients than in female patients (Furtado et al., 2008).
In another study assessing late-onset depression (onset after 50), authors investigated whole-brain GM volume of probands. They realized that normalized GM volumes of calcarine, olfactory, and orbitofrontal regions are increased in healthy females than in healthy males but decreased in MDD females compared to MDD males (Piani et al., 2021). Another study by Yang et al. focused on various gyri alterations in MDD (Yang et al., 2017). What they reported was that the GM volume of the middle/superior temporal gyrus and ventromedial prefrontal gyrus were decreased in MDD males compared to HC males. Meanwhile, in females, the dorsomedial prefrontal gyrus (extending to the supplementary motor area) and lingual (extending to the parahippocampal gyrus) were smaller in the patients (Yang et al., 2017). The pituitary gland volume was explored in only one study, suggesting larger volumes in pediatric MDD males compared to HC males, while there were no significant diagnostic group differences in pediatric females (MacMaster et al., 2006). The authors also reported that non-familial (without a family history of mood disorder) males with MDD had significantly larger pituitary glands than familial patients and healthy controls (MacMaster et al., 2006).
More other studies employed structural MRI tools to assess sex or gender disparities in depression. One aimed to measure the habenula changes during the depression and found out females with a first-episode depression had larger habenula white matter (WM) volumes than both healthy probands and people with treatment-resistant/chronic depression (Carceller-Sindreu et al., 2015). On the other hand, another study performed a volumetric MRI study on people with only late-life depression, meaning that they developed depression at age 65 and over (Cyprien et al., 2014). In that study, there was a positive association between late-life depressive symptoms and smaller anterior, mid, posterior, and total corpus callosum regions in women, as opposed to men. Nevertheless, there was no correlation between the total brain volume and depression in the two sexes (Cyprien et al., 2014).
White-matter hyperintensities were also studied in two relatively old studies in the field of depression (Lavretsky et al., 1998; Lewine et al., 1995). One of them employed MRI to find qualitative brain morphologic anomalies in MDD, schizophrenic, schizoaffective, and bipolar disorder patients along with healthy volunteers. They reported that men with either schizophrenia or major depression had more frequently reported abnormal scans than women in either group, predominantly showing deep white matter hyperintensity signals, volume loss, enlargement or asymmetry of ventricles, and other incidental findings (Lewine et al., 1995). Meanwhile, the other study focused on people with early and late-onset depression. In their research, both early-onset (meaning having the first episode before 50) and late-onset males had larger amounts of white matter intensities (Lavretsky et al., 1998).
Assessing the cortical thickness, different matter volumes, and perfusion measures, further studies have reported the sex differences in depression neuroimaging findings. For example, a study examined the thickness of the orbitofrontal cortex (OFC) in adolescents with depression (Nielsen et al., 2020). What they observed was an inverse correlation between depressive symptoms and the left lateral OFC in males and a positive one between depressive symptoms and left medial OFC in females. However, the right hemisphere did not reflect any sex differences (Nielsen et al., 2020). On the other hand, a structural whole-brain study tested white and gray matter disparities between the two sexes. They recruited people with melancholic depression alongside healthy controls; the results indicated a significant reduction in the gray matter volume of the right thalamus in MDD males, which was not seen in their female counterparts (Soriano-Mas et al., 2011). Finally, a recent study conducted perfusion tests in people with depression and reported cerebral perfusion alterations that varied with Hamilton Depression Scale (HAM-D)(Hamilton, 1960),Beck's Depression Inventory (BDI)(Beck et al., 1961), and Montgomery-Asberg Depression Rating Scale (MADRS) (Montgomery and Asberg, 1979) scores. Sexual dimorphism appeared as a positive association between whole-brain perfusion and female depressive symptoms in the HAM-D, BDI, and MADRS scores. In contrast, male patients' cerebral perfusion exhibited a positive association for the MADRS score (Ritter et al., 2021).
DTI Studies
As previously explained, only four studies assessed sex differences in DTI findings in depression. The detailed data of these are presented in Table 3. One study focused on WM pathways involved in emotional regulation in subjects with and without MDD. Their results showed that males with MDD had lower FA in the parahippocampal cingulum and higher longitudinal diffusivity (LD) in fronto-occipital fasciculus than healthy males. Also, MDD males showed greater LD in superior longitudinal fasciculus compared with MDD females (Ugwu et al., 2015). Another study examined the whole brain changes in adolescent-onset depression. They reported that mean diffusion indices of a cluster of precentral gyrus white matter bordering on the superior corona radiata differ in males and females; MDD females showed lower FA and higher radial diffusivity (RD) in this area compared to healthy probands. By contrast, males with MDD had higher FA, higher axial diffusivity (AD), and lower RD in the same region (Kliamovich et al., 2021).
Table 3.
Overview of DTI studies on sex differences in depression
| Study | Tesla sequence | Measures | Brain areas | Methods for Sex Differences Analyses Sex by Diagnosis Effects |
Covariates | Results | ||
|---|---|---|---|---|---|---|---|---|
| Model | Tested? | Findings | ||||||
| Ho et al., 2021 |
3T T1 |
R1, FA, MD, AD, RD | Corpus callosum genu and splenium, cingulum cingulate, uncinate fasciculus | GLM | Yes | Yes | Study group, psychotropic medication status, Tanner stage, age of initial depression onset, duration of current episode, age of menarche |
Increased R1 in the L uncinate fasciculus and corpus callosum genu in MDD females compared to healthy females. Association between higher R1 in the L uncinate fasciculus and severe depressive symptoms in females. No gender-specific association in FA. |
| Kliamovich et al., 2021 | 3T | FA, MD, AD, RD | Whole brain | GLM | Yes | Yes | Age, groups, GAD, OCD, baseline depression symptoms | Lower FA and higher RD in MDD females, higher FA and AD and lower RD in MDD males in a cluster of precentral gyrus WM bordering on the superior corona radiata. |
| Lyon et al., 2019 | 3 T | FA, AD, ADC, RD | Whole brain | GLM | Yes | Yes | Age |
Elevated FA in genu of cc, bilateral cerebral peduncle, and left UF in HC females compared to MDD females Elevated AD in left frontal projection of the cc in HC females compared to MDD females |
| Ugwu et al., 2015 | 3 T | FA, LD, RD | RC, DC, PC, UF, Crus of the fornix, SLF, Inferior FOF | GLM | Yes | Yes | Age |
Lower FA in PC and higher LD in FOF in MDD males than male controls. Greater LD in SLF in MDD males than females |
Abbreviations: DTI: Diffusion tensor imaging, FA: Fractional anisotropy, MD: Mean diffusivity, AD: Axial diffusivity, RD: Radial diffusivity, LD: Longitudinal diffusivity, ADC: Apparent diffusion coefficient, cc: corpus callosum, RC/DC/PC: Rostral/Dorsal/Parahippocampal Cingulum, UF: Uncinate fasciculus, SLF: Superior longitudinal fasciculus, FOF: Fronto-occipital fasciculus, GAD: General anxiety disorder, OCD: Obsessive-Compulsive disorder, MDD: Major depressive disorder, WM: White matter, GLM: General linear model, T: Tesla, L: Left.
Another recent study similarly focused on adolescents with depression. Women with MDD had a significantly higher R1 of left uncinate fasciculus (UF) and corpus callosum genu than healthy women. Furthermore, severe depressive symptoms in females correlated with greater R1 in the left uncinate fasciculus (Ho et al., 2021a). These regions were also assessed in another DTI study. In this study, Lyon et al. observed elevated FA in the genu of the corpus callosum, bilateral cerebral peduncle, and left UF in HC females compared to MDD females and higher AD in the left frontal projection of the corpus callosum in HC females compared to those with MDD (Lyon et al., 2019). Moreover, in their longitudinal assessment of 8-week treatment with escitalopram, sertraline, or venlafaxine-extended release, they assessed if DTI metrics' alterations vary by sex. However, no significant difference was observed in the two sexes regarding the remission vs. non-remission status (Lyon et al., 2019).
fMRI Studies
As provided in Table 4, 12 studies explored sex differences in functional brain alterations during MDD. Two studies focused on the resting-state functional connectivity (rs-FC) of the treatment-resistant depression (TRD) probands and healthy controls. The first one reported that, compared to TRD males, TRD females had higher degree values of functional connectivity in various regions: subcallosal cingulate gyrus, ventral caudate, nucleus accumbens, inferior thalamic peduncle, and left lateral habenula (Amiri et al., 2021). The second study similarly explored the sex differences in rs-FA of TRDs (Talishinsky et al., 2022). Their large cohort study, which comprised 371 TRD patients and 182 HCs, revealed elevated connectivity in subgenual and posterior cingulate areas and decreased connectivity in the anterior insula, temporal pole, and lateral prefrontal cortex in male patients compared to HC males. No significant difference was seen in females (Talishinsky et al., 2022).
Table 4.
Overview of fMRI studies on sex differences in depression
| Study | Tesla sequence | Brain areas | Connectivity/activation | Task | Methods for Sex Differences Analyses Sex by Diagnosis Effects |
Covariates | Results | ||
|---|---|---|---|---|---|---|---|---|---|
| Model | Tested? | Findings | |||||||
| Amiri et al., 2021 | 3 T |
SCG VCa NAc ITP LHb |
Rs-FC | N/A | Nonparametric permuation | Yes | Yes | N/A |
Difference in degree values in the SCG between males and females of the TRD. Higher degree values in all regions in the TRD females except in the R LHb. |
| Briceño et al., 2015 | 3 T | Fronto-limbic regions | Activation | Facial emotion perception test | ANOVA | Yes | No | N/A | Among fronto-limbic regions, there were no regions significant for an MDD status by gender interaction. |
| Chuang et al., 2017 | 3 T | Whole brain | Activation | Affective go/no-go task | GLM | Yes | Yes | Age | Significant group-by-sex differences in the activation of the supramarginal gyrus and posterior cingulate cortex, as those of male controls were more activated than female controls, but the activation of those in depressed males was lower than in depressed females. |
| De Almeida et al., 2011 | 3 T | prefrontal cortical–amygdala neural circuitry | Activation | Facial emotion perception test | Spearman rank correlation tests and Mann–Whitney U-tests | Yes | Yes | N/A |
In MDD patients, there were no significant effects of sex on any of the connectivity measures. In between-group analysis, there were abnormal inverse left-sided top-down vmPFC-amygdala connectivity, left-sided sgACC–amygdala connectivity, and reduced positive left-sided vmPFC-sgACC to happy faces in females with MDD when compared to their healthy counterparts. In response to fearful faces, there was an abnormally increased positive left-sided sgACC–amygdala connectivity in MDD females. For males with MDD relative to healthy males, there were no significant abnormal findings. |
| Dong et al., 2022 | 3 T | Amygdala, hippocampus, medial orbitofrontal cortex, nucleus accumbens, and dorsolateral prefrontal cortex | Activation | Montreal imaging stress task | GLM | Yes | Yes | Age | Less deactivation in the amygdala, hippocampus, and nucleus accumbens of the female MDD group relative to the female HC group, whereas the male MDD and HC did not differ regarding the deactivation/activation of these regions. |
| Geng et al., 2019 | 3 T | Whole brain | Rs-FC | N/A | GLM | Yes | Yes | Age, years of education, disease duration, age at onset, number of depressive episodes, HAMD-17 score |
Increased ReHo in the R STG and decreased ReHo in the R MFG in SD women compared to NSD women. Higher ReHo in the L inferior triangular frontal gyrus in both SD and NSD males. |
| Jenkins et al., 2018 | 3 T | Whole brain | Activation | Facial emotion perception test | GLM | Yes | Yes | Accuracy for each emotion, site | Greater activity in male HCs and rMDD females compared to their counterparts in either groups in the R thalamic cluster for the neutral contrast and in the R SFG cluster for the sad contrast. The opposite pattern in the L MTG and bilateral midbrain for sad contrast. No significant associations in the amygdala. |
| Mei et al., 2022 | 3 T | Whole brain | Rs-FC | N/A | ANOVA | Yes | Yes | N/A |
Decreased ALFF in the bilateral caudate nucleus and posterior cingulate gyrus of MDD males compared to MDD females and HC females. Increased ALFF in the bilateral caudate nucleus and posterior cingulate gyrus of MDD females compared to HC males. |
| Piani et al., 2021 | 3 T | Whole brain | Activation | Affective go/no-go task | GLM | Yes | Yes | Percent of responses to target stimuli, time of response to target stimuli, and percent of responses to non-target stimuli |
More negative responses during the overall task and go/no-go condition in the right parahippocampus of MDD females compared to MDD males and in that of HC males than HC females More negative response during the task in the right calcarine of MDD females compared to MDD males and in that of HC males than HC females |
| Talishinsky et al., 2022 | 3 T | Whole brain | Rs-FC | N/A | ANOVA | Yes | Yes | N/A | Increased connectivity in subgenual cingulate and posterior cingulate areas and decreased connectivity in the anterior insula, temporal pole, and lateral prefrontal cortex in MDD males compared to HC males. None were seen in females. |
| Yao et al., 2014 | 3 T | Frontoparietal networks and attention network | Rs-FC | N/A | ANOVA | Yes | Yes | N/A | Higher ALFF values in the left postcentral gyrus and right superior temporal gyrus and lower ALFF values in the left superior temporal pole, left superior temporal gyrus, and the left superior frontal gyrus in male MDD patients when compared to female MDD patients |
| Young et al., 2017 | 3 T | Whole brain | Activation | Autobiographical memory recall | ANOVA | Yes | Yes | N/A |
Increased activity in the right dmPFC of MDD males compared to all other groups during recall of positive memories. Decreased activity in the right caudate of MDD females compared to all other groups during recall of positive memories. Increased activity in PCC and insula of HC females compared to both male groups during recall of negative memories. Decreased activity in precuneus of HC males compared to all other groups during recall of negative memories |
Abbreviations: fMRI: Functional magnetic resonance imaging, Rs: Resting state, FC: Functional connectivity, SCG: Subcallosal cingulate gyrus, VCa: Ventral caudate, NAc: Nucleus accumbens, LHb: Lateral habenula, ITP: Inferior thalamic peduncle, ANOVA: analysis of variances, vmPFC: ventromedial prefrontal cortex, sgACC: subgenual anterior cingulate cortex, STG: Superior temporal gyrus, MFG: Middle frontal gyrus, MTG: middle temporal gyrus, SFG: Superior frontal gyrus, ReHo: Regional homogeneity, MDD: major depressive disorder, rMDD: Remitted major depressive disorder, SD: Somatic depression, NSD: Non-somatic depression, TRD: Treatment-resistant depression, ALFF: amplitude of low-frequency fluctuation, dmPFC: dorsomedial prefrontal cortex, PCC: posterior cingulate cortex, HC: Healthy control, HAMD: Hamilton Depression Rating Scale, GLM: General linear model, T: Tesla, N/A: Not applicable, R: Right, L: Left.
Literature provided more evidence of sex differences in resting-state fMRI findings by measuring the amplitude of low-frequency fluctuation (ALFF). For example, a study demonstrated decreased ALFF in the bilateral caudate nucleus and posterior cingulate gyrus of MDD males compared to MDD females and HC females (Mei et al., 2022). Plus, ALFF in the bilateral caudate nucleus and posterior cingulate gyrus of MDD females was increased when compared to HC males. Disease duration was also positively correlated with the ALFF of the right caudate nucleus in MDD females (Mei et al., 2022). The other study mainly focused on the gyri of the probands (Yao et al., 2014). In their study, male MDD patients had significant differences when compared to the patients of the opposite sex. These differences included higher ALFF values in the left postcentral gyrus and right superior temporal gyrus and lower ALFF values in the left superior temporal pole, left superior temporal gyrus, and left superior frontal gyrus (Yao et al., 2014).
Various studies also measured fMRI metrics' changes in response to different facial expressions. For instance, to examine the prefrontal cortical–amygdala neural circuitry, a study made the participants complete an emotional dynamic face-processing task (De Almeida et al., 2011). They suggested that in response to happy faces, MDD females show abnormal inverse left ventromedial prefrontal cortex (vmPFC)-amygdala connectivity, left subgenual anterior cingulate cortex (sgACC)–amygdala connectivity, and reduced positive left vmPFC-sgACC compared to healthy females. In response to fearful faces, affected females also had abnormally increased positive left sgACC–amygdala connectivity in this comparison. Regarding males, however, there was not any significant result (De Almeida et al., 2011). Another study also administered facial emotion perception (happy, sad, angry, and fearful) to assess the fMRI metrics' alterations in MDD (Briceño et al., 2015). However, among fronto-limbic regions, there were no regions significant for an MDD status by gender interaction (Briceño et al., 2015). The last study, which assessed resistant MDD patients had different results. Their whole-brain study revealed the effects of depression on facial emotion processing. Compared to their male counterparts, resistant MDD females presented greater activities in the right thalamic cluster and right superior frontal gyrus cluster for neutral and sad contrasts, respectively. In contrast, there were associations between male resistant depression and activities of the left middle temporal gyrus and bilateral midbrain for the sad face contrast (Jenkins et al., 2018).
Interestingly, two studies explored sex differences in depression by using the Go/No-Go paradigm, a well-established tool to measure sustained attention (Piani et al., 2021). The first study showed negative responses during the go/no-go condition in the right parahippocampus of MDD females compared to MDD males and in that of HC males than HC females (Piani et al., 2021). The second study similarly assessed MDD and HC participants of two sexes. Results suggested more activation of the supramarginal gyrus and posterior cingulate cortex in healthy males than healthy females and in MDD females than in MDD males (Chuang et al., 2017). Both studies showed that the diagnosis of depression reverses the fMRI findings.
Two studies implemented different approaches to find the sex differences of MDD. One explored brain activation during the recall of autobiographical memories (Young et al., 2017). Their results of positive memories assessment were as follows: higher activity in the right dorsomedial prefrontal cortex (dmPFC) of MDD males and lower activity in the right caudate of MDD females compared to all other groups. Moreover, they showed that during a negative memory recall, activity in the posterior cingulate cortex (PCC) and insula of HC females increases when compared to both male groups, and the precuneus of HC males becomes less active than all other groups (Young et al., 2017). The other study made participants undergo the Montreal imaging stress task, in which acute psychosocial stressor (time limit to do arithmetic questions) affected the patients and their subsequent fMRI results (Dong et al., 2022). In the study, there was less deactivation in the amygdala, hippocampus, and nucleus accumbens of the female MDD group compared to healthy females. This difference was not seen in males (Dong et al., 2022).
Finally, the last study explored fMRI alterations in people with somatic and non-somatic depression. Based on their reports, depressed participants develop elevated regional homogeneity (ReHo) in the left inferior triangular frontal gyrus (Geng et al., 2019). This measure evaluates functional similarity of a given voxel with its nearest neighbors (Liu et al., 2008). In their study, in contrast to men, women with somatic depression had increased ReHo in the right superior temporal gyrus and decreased ReHo in the right middle frontal gyrus compared to their non-somatic counterparts (Geng et al., 2019).
Discussion
This systematic review summarizes the current literature on sex differences in abnormal neuroimaging findings among depression patients. As the results explained, most conventional MRI studies reflected the sex effect on temporal lobe components in depression; the hippocampus and amygdala, along with total brain volume and orbitofrontal regions, differed between the two sexes. However, the specific changes were heterogeneous. Also, connections of the limbic pathways showed disparities in males and females with MDD; these included habenula, anterior cingulate cortex, and corpus callosum. Meanwhile, DTI findings were mainly associated with frontal connections like uncinate fasciculus, superior longitudinal fasciculus, and fronto-occipital fasciculus, and even frontal projections of the cc. Other microstructural alterations in the white matter involved cingulum, thalamic radiations, and corpus callosum. Moreover, regarding fMRI, functions of various frontal and temporal gyri, along with caudate nucleus and prefrontal cortex, were different between the two sexes. Similar to DTI findings, the cingulum-related regions, especially posterior cingulate cortex, showed disparities as well.
Being a part of the limbic system, the hippocampus has long been implicated in emotional memory recalling and regulation (Zhu et al., 2019). Regarding depression, a systematic review and meta-analysis of late-life depression reported hippocampal size reduction as the most consistent evidence (Geerlings & Gerritsen, 2017). Healthy males and females tend to have similar sizes of the hippocampus (Eijk et al., 2020; Perlaki et al., 2014), but sex might affect the volumetric hippocampal changes in depression. The proof of higher binding potential in healthy females compared with healthy males in positron emission tomography (PET) receptor-binding studies of the serotonin receptor also supports this effect (Parsey et al., 2002). Another component of the limbic system, the amygdala, manages the fear response and processing of facial emotional expressions (Burke et al., 2011). Reports show that lower amygdala volumes are associated with a longer disease duration (Zavorotnyy et al., 2018) and predict anxiety symptoms (Hu et al., 2020). The fact that depressed women experience higher symptom severity and higher lifetime anxiety disorders (Eid et al., 2019; Schuch et al., 2014) might explain a smaller amygdala in female depression than in healthy ones. Regarding its gray matter volumes changes, stress might be involved, as a study showed that mindfulness-based stress reductions decrease right basolateral amygdala gray matter density (Hölzel et al., 2010).
The DTI and fMRI studies reflected gender differences in the cingulum. An example is the active subcallosal cingulate gyrus. Notably, the higher activity of this gyrus is associated with negative emotional processing in a depression setting (Laxton et al., 2013). This higher activity reduces after depression treatment interventions, such as deep brain stimulation, anti-depressants, cingulotomy, electroconvulsive therapy, and repetitive transcranial magnetic stimulation (Hamani et al., 2011). Another gender disparity example was parahippocampal cingulum. More research needs to be conducted on this association, as hippocampal pathways play significant roles in reward processing (Bracht et al., 2015). Recent research on neuroimaging of the two sexes has revealed that diffusion findings could predict susceptibility to depressive symptoms across adolescence during the COVID-19 pandemic: females show lower fiber density and cross-section (FDC) of the cingulum than males, which leads to higher chances of depressive symptoms, lower resilience, and more stress (Chahal et al., 2022b).
The two hemispheres connector, the corpus callosum (cc), has also shown disparities in included volumetric and microstructural studies. Nevertheless, there is evidence of similar cc volumes in depressed and healthy subjects (Piras et al., 2021) and that only familial MDD is associated with cc thinning (Lacerda et al., 2005). However, there might be underlying physiological mechanisms of hormones for the latter sex difference. Low estrogen levels could lead to mood disturbances, and besides, estradiol is reported to regulate interhemispheric communication in women (Weis et al., 2008). Another reported dissimilarity was the corpus callosum genu. In MDD subjects, lower FA of some cc regions is associated with a longer illness duration. These regions include premotor and supplementary motor cortices along with parietal, temporal, and occipital cortices (Zhao et al., 2021). Moreover, a related study suggested epigenetic changes during the cc microstructural changes in depression. They reported higher DNA methylation of the serotonin transporter gene and lower FA of the cc body were significantly correlated (Won et al., 2016). Note that the serotonin transporter gene (SLC6A4) reuptakes serotonin molecules, and the disturbed serotonergic system has been reported as a key factor in depression etiology (El-Mallakh & Ali, 2019).
Finally, a variety of brain fasciculi have also shown sex or gender dissimilarities in white matter studies. In males, it was the FOF and SLF, and in females, it was the left uncinate fasciculus (UF) that reflected sex differences. Notably, the onset time might affect the microstructure of FOF, as only late-onset MDD patients have shown decreased FA in the white matter (WM) of the FOF, with an inverse correlation with the severity of the disease (Cheng et al., 2014). Regarding the SLF, a study has shown that its FA degree values negatively correlate with depression severity, and the right SLF FA values associate with illness duration (Lai & Wu, 2014). Meanwhile, a report shows that lower FA in the left UF correlates with higher anhedonia scores, not the total depression scores (Fernandes et al., 2021). Anhedonia, meaning the inability to feel pleasure from pleasurable experiences, is reported to be comparable in the two sexes (Rueda 2019). However, there are reports that females experience seasonal variations of anhedonia in contrast to males, with peaks in the winter (Lyall et al., 2018).
As demonstrated in the results, there was heterogeneity among the reports of included studies. A potential factor leading to the results' heterogeneity could be the different definitions of sex and gender among the included studies. The term "sex" refers to the biological dissimilarities between males and females, while "gender" indicates a subjective sexual identity, masculine or feminine (Reale et al., 2021). Some of the included studies have used these terms interchangeably (Cyprien et al., 2014; Furtado et al., 2008; Hastings et al., 2004; Kronmüller et al., 2009). Most studies do not define the terms in their methodology. There were inconsistent reports of the same regions in studies using the terms “sex” and “gender”. For example, as explained in the DTI results section, the study by Ho et al. showed no sex-specific changes in the FA of the genu of the corpus callusum (Ho et al., 2021a), while Lyon et al. reported gender differences in this region (Lyon et al., 2019).
One limitation is worth noting. Our study systematically searched all available relevant articles on sMRI, DTI, and fMRI investigations; however, we found no specific brain region showing alterations in all three of these imaging tools. The most frequently repeated regions with significant changes include limbic areas like the amygdala and hippocampus (mentioned in DTI and sMRI studies) and cingulum (in DTI and fMRI papers) as we have discussed in previous paragraphs. This heterogeneity might result from different regions of interest, various methodologies, and the diverse nature of these modalities and the comorbidities of the subjects. Such differences include studies of the whole brain vs. specific brain areas, GM vs. WM, volume vs. density assessments, and activation vs. resting-state connectivity investigations. Moreover, DTI measures the diffusion of water molecules, making it more suitable for WM explorations along tracts, in contrast to fMRI and sMRI modalities which interrogate the gray matter (Ghazi Sherbaf et al., 2019).
We did not include results from other reviews or meta-analyses in the present systematic review. However, the comparison between our findings and well-known meta-analyses might shed light on the precise differences in depression of the two sexes. The Enhancing Neuro Imaging Genetics through Meta-Analysis (ENIGMA) consortium is an international collaborative group that currently includes 40 research samples from 14 different countries globally (Institute UMaMSNaI, 2023). In an sMRI study, the ENIGMA MDD working group assessed subcortical brain alterations in 1728 MDD cases and 7199 normal controls from 15 cohorts. They observed no significant diagnosis-by-sex interaction effects in the subcortical GM of subjects (Schmaal et al., 2016). Similarly, they found no significant impact of sex when assessing structural cortical abnormalities of 2148 MDD patients and 7957 normal controls from 20 research sites (Schmaal et al., 2017b). They also performed a DTI-based analysis of 1305 MDD cases and 1602 HCs from 20 samples. These results revealed a significant diagnosis-by-sex interaction; male adolescent patients (age ≤ 21) had higher uncinate fasciculus radial diffusivity than adolescent male controls, and this interaction was absent in females (Velzen et al., 2020). In our review, uncinate fasciculus alterations mainly reflected differences between females with and without depression. We did find sex differences in the composite of sMRI studies that we reviewed.
Of the underlying mechanisms of depression, the contribution of sex hormones to female and male differences remains to be discussed. As previously explained, the incidence rates of depression are similar in the sexes before puberty, and the gender gap starts afterward (Wesselhoeft et al., 2015). According to a systematic review by Morssinkhof et al., sex hormones, including estradiol, progesterone, luteinizing hormone (LH), and follicle-stimulating hormone (FSH), do not seem to have different absolute levels in depressed subjects and healthy controls (Morssinkhof et al., 2020). Previous reports have demonstrated associations between sex hormones and neuroimaging findings. For example, the GM volumes of the supplementary motor area, inferior frontal gyrus, and superior temporal gyrus are positively correlated with serum levels of estradiol in healthy post- and pre-menopause women (Kim et al., 2018), and there have been reports of associations between higher midlife testosterone levels and larger hemispheric, frontal, and parietal regional brain volumes and with smaller left occipital brain volume (Lessov-Schlaggar et al., 2005).
As most studies have reported comparable levels of sex hormones in healthy and depressed people (Morssinkhof et al., 2020), it is unlikely that brain alterations in depression are directly related to sex hormones. However, the sex hormones may still play a role in depression. For example, post-partum depression affects 7–20% of women following delivery, and there are reports that prophylactically administering conjugated estrogen after delivery can prevent its symptoms (Schiller et al., 2015). This response of patients may suggest the role of estrogen/progesterone withdrawal in depression development (Schiller et al., 2015). Similar hormonal withdrawal happens in the menopause transition in older age, and various studies have indicated the short-term efficacy of estradiol in depressed perimenopausal women (Schmidt & Rubinow, 2009). However, further studies are needed to unravel the interactions between sex hormones and brain alterations in these depressed people.
The findings of our systematic review should be interpreted in light of some limitations. First, we only included case–control and cohort studies, and therefore, clinical trials, case reports, narrative reviews, and systematic reviews were excluded. We could not also add all the eligible demographic and patient characteristic data, as these specifics of some studies were not available. Moreover, the included studies themselves had varying degrees of different biases, which could have affected the power of our systematic review. Concerning the sample of studies, some studies had recruited a small sample size, and not all of them matched participants for potential confounding variables. The onset of the disease, the response to treatment, and history of anti-depressants use might also affect the neuroimaging results, which differed in the included studies.
Another significant limitation of our study was the heterogeneity of study samples regarding the age of patients. Studies have repeatedly reported that depression often emerges during adolescence (Ho et al., 2021b) and that depression symptoms of adolescent and adult patients differ (e.g., adults experience more anhedonia, while appetite and weight change, loss of energy, and insomnia are more common in adolescents) (Rice et al., 2019). These differences in epidemiology and clinical manifestations might have affected the results of our study. Moreover, the diagnosis of patients in studies varied, as some assessed MDD subjects of all ages and status of treatment, while others only assessed treatment-resistant or early/late-onset depression. Finally, the imaging methodology and precision play a role in the final results; for example, not all studies assessed the whole-brain alterations.
In conclusion, our study provides information on the current literature regarding the neuroimaging findings of sex differences in depression. These findings should be interpreted alongside the differences in phenotype and clinical manifestations of the disease so that a better understanding of male and female depression emerges. In order to achieve more reliable results, further studies should be conducted with larger sample sizes and homogenous imaging methodologies considering the depression onset, age, treatment status, and treatment response of the participants. Moreover, future studies would better consider and define gender and biological sex in their investigations, since not all people with the same sex present the same subjective sexual identity and social behaviors. Treating gender as a continuous variable rather than a categorical dichotomous one, as suggested by previous neuropsychiatric researchers (Reilly, 2019), may be a useful research practice in this regard.
Supplementary Information
Below is the link to the electronic supplementary material.
Authors' contributions
Soheil Mohammadi and Mohammad Amin Salehi designed the project, developed the protocol, contributed to screening and data extraction, and contributed to the writing of the original and final draft. Homa Seyedmirzaei contributed to the writing of the original and final draft. Ali Jahanshahi contributed to the data extraction. Seyed Sina Zakavi contributed to the screening. Fatemeh Dehghani Firouzabadi contributed to the writing of the original and final draft. David M. Yousem encouraged and supervised the project and contributed to writing of the original and final draft.
Data availability
Not applicable.
Declarations
Ethical Approval
Not applicable.
Competing interests
Authors declare no conflicts of interest.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Soheil Mohammadi, Homa Seyedmirzaei and Mohammad Amin Salehi contributed equally to this work.
References
- Acosta H, Tuulari JJ, Scheinin NM, Hashempour N, Rajasilta O, Lavonius TI. Prenatal maternal depressive symptoms are associated with smaller amygdalar volumes of four-year-old children. Psychiatry research Neuroimaging. 2020;304:111153. doi: 10.1016/j.pscychresns.2020.111153. [DOI] [PubMed] [Google Scholar]
- Acosta H, Kantojärvi K, Hashempour N, Pelto J, Scheinin NM, Lehtola SJ, et al. Partial Support for an Interaction Between a Polygenic Risk Score for Major Depressive Disorder and Prenatal Maternal Depressive Symptoms on Infant Right Amygdalar Volumes. Cerebral cortex (New York, NY 1991) 2020;30(12):6121–34. doi: 10.1093/cercor/bhaa158. [DOI] [PubMed] [Google Scholar]
- Amiri S, Arbabi M, Kazemi K, Parvaresh-Rizi M, Mirbagheri MM. Characterization of brain functional connectivity in treatment-resistant depression. Progress in Neuro-Psychopharmacology & Biological Psychiatry. 2021;111:110346. doi: 10.1016/j.pnpbp.2021.110346. [DOI] [PubMed] [Google Scholar]
- Ancelin ML, Carrière I, Artero S, Maller J, Meslin C, Ritchie K, et al. Lifetime major depression and grey-matter volume. Journal of Psychiatry & Neuroscience : JPN. 2019;44(1):45–53. doi: 10.1503/jpn.180026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Averill, C.L., Satodiya, R.M., Scott, J.C., Wrocklage, K.M., Schweinsburg, B., Averill, L.A., et al (2017). Posttraumatic Stress Disorder and Depression Symptom Severities Are Differentially Associated With Hippocampal Subfield Volume Loss in Combat Veterans. Chronic stress (Thousand Oaks, Calif) 1. [DOI] [PMC free article] [PubMed]
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Binesh N, Kumar A, Hwang S, Mintz J, Thomas MA. Neurochemistry of late-life major depression: A pilot two-dimensional MR spectroscopic study. Journal of Magnetic Resonance Imaging : JMRI. 2004;20(6):1039–1045. doi: 10.1002/jmri.20214. [DOI] [PubMed] [Google Scholar]
- Binnewies J, Nawijn L, Brandmaier AM, Baaré WFC, Bartrés-Faz D, Drevon CA, et al. Associations of depression and regional brain structure across the adult lifespan: Pooled analyses of six population-based and two clinical cohort studies in the European Lifebrain consortium. Neuroimage Clin. 2022;36:103180. doi: 10.1016/j.nicl.2022.103180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bracht T, Jones DK, Müller TJ, Wiest R, Walther S. Limbic white matter microstructure plasticity reflects recovery from depression. Journal of Affective Disorders. 2015;170:143–149. doi: 10.1016/j.jad.2014.08.031. [DOI] [PubMed] [Google Scholar]
- Brébion G, Núñez C, Lombardini F, Senior C, Sánchez Laforga AM, Siddi S, et al. Subclinical depression and anxiety impact verbal memory functioning differently in men and women —an fMRI study. Journal of Psychiatric Research. 2021;140:308–315. doi: 10.1016/j.jpsychires.2021.05.063. [DOI] [PubMed] [Google Scholar]
- Brébion G, Núñez C, Lombardini F, Senior C, Sánchez Laforga AM, Siddi S, et al. Subclinical depression and anxiety impact verbal memory functioning differently in men and women -an fMRI study. Journal of Psychiatric Research. 2021;140:308–315. doi: 10.1016/j.jpsychires.2021.05.063. [DOI] [PubMed] [Google Scholar]
- Briceño EM, Rapport LJ, Kassel MT, Bieliauskas LA, Zubieta JK, Weisenbach SL, et al. Age and gender modulate the neural circuitry supporting facial emotion processing in adults with major depressive disorder. The American Journal of Geriatric Psychiatry. 2015;23(3):304–313. doi: 10.1016/j.jagp.2014.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown SA, Brumback T, Tomlinson K, Cummins K, Thompson WK, Nagel BJ, et al. The National Consortium on Alcohol and NeuroDevelopment in Adolescence (NCANDA): A Multisite Study of Adolescent Development and Substance Use. Journal of Studies on Alcohol and Drugs. 2015;76(6):895–908. doi: 10.15288/jsad.2015.76.895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke J, McQuoid DR, Payne ME, Steffens DC, Krishnan RR, Taylor WD. Amygdala volume in late-life depression: Relationship with age of onset. The American Journal of Geriatric Psychiatry : Official Journal of the American Association for Geriatric Psychiatry. 2011;19(9):771–776. doi: 10.1097/JGP.0b013e318211069a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carceller-Sindreu M, de Diego-Adeliño J, Serra-Blasco M, Vives-Gilabert Y, Martín-Blanco A, Puigdemont D, et al. Volumetric MRI study of the habenula in first episode, recurrent and chronic major depression. European Neuropsychopharmacology : The Journal of the European College of Neuropsychopharmacology. 2015;25(11):2015–2021. doi: 10.1016/j.euroneuro.2015.08.009. [DOI] [PubMed] [Google Scholar]
- Carlson JM, Depetro E, Maxwell J, Harmon-Jones E, Hajcak G. Gender moderates the association between dorsal medial prefrontal cortex volume and depressive symptoms in a subclinical sample. Psychiatry Research - Neuroimaging. 2015;233(2):285–288. doi: 10.1016/j.pscychresns.2015.06.005. [DOI] [PubMed] [Google Scholar]
- Caroleo M, Carbone EA, Primerano A, Foti D, Brunetti A, Segura-Garcia C. The role of hormonal, metabolic and inflammatory biomarkers on sleep and appetite in drug free patients with major depression: A systematic review. Journal of Affective Disorders. 2019;250:249–259. doi: 10.1016/j.jad.2019.03.015. [DOI] [PubMed] [Google Scholar]
- Cattarinussi G, Delvecchio G, Maggioni E, Bressi C, Brambilla P. Ultra-high field imaging in Major Depressive Disorder: A review of structural and functional studies. Journal of Affective Disorders. 2021;290:65–73. doi: 10.1016/j.jad.2021.04.056. [DOI] [PubMed] [Google Scholar]
- Cavanagh A, Wilson CJ, Caputi P, Kavanagh DJ. Symptom endorsement in men versus women with a diagnosis of depression: A differential item functioning approach. International Journal of Social Psychiatry. 2016;62(6):549–559. doi: 10.1177/0020764016653980. [DOI] [PubMed] [Google Scholar]
- Cavanagh A, Wilson CJ, Kavanagh DJ, Caputi P. Differences in the Expression of Symptoms in Men Versus Women with Depression: A Systematic Review and Meta-analysis. Harvard Review of Psychiatry. 2017;25(1):29–38. doi: 10.1097/HRP.0000000000000128. [DOI] [PubMed] [Google Scholar]
- Čermaková, P., Andrýsková, L., Brázdil, M., Marečková, K. (2020), Socioeconomic deprivation in early life and symptoms of depression and anxiety in young adulthood: mediating role of hippocampal connectivity. Psychological medicine. 1–10. [DOI] [PMC free article] [PubMed]
- Chahal R, Ho TC, Miller JG, Borchers LR, Gotlib IH. Sex-specific vulnerability to depressive symptoms across adolescence and during the COVID-19 pandemic: The role of the cingulum bundle. JCPP Adv. 2022;2(1):e12061. doi: 10.1002/jcv2.12061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chahal R, Ho TC, Miller JG, Borchers LR, Gotlib IH. Sex-specific vulnerability to depressive symptoms across adolescence and during the COVID-19 pandemic: The role of the cingulum bundle. JCPP Advances. 2022;2(1):e12061. doi: 10.1002/jcv2.12061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen G, Guo Y, Zhu H, Kuang W, Bi F, Ai H, et al. Intrinsic disruption of white matter microarchitecture in first-episode, drug-naive major depressive disorder: A voxel-based meta-analysis of diffusion tensor imaging. Progress in Neuro-Psychopharmacology and Biological Psychiatry. 2017;76:179–187. doi: 10.1016/j.pnpbp.2017.03.011. [DOI] [PubMed] [Google Scholar]
- Cheng Y, Xu J, Yu H, Nie B, Li N, Luo C, et al. Delineation of Early and Later Adult Onset Depression by Diffusion Tensor Imaging. PLoS ONE. 2014;9(11):e112307. doi: 10.1371/journal.pone.0112307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chuang JY, Hagan CC, Murray GK, Graham JME, Ooi C, Tait R, et al. Adolescent Major Depressive Disorder: Neuroimaging Evidence of Sex Difference during an Affective Go/No-Go Task. Front Psychiatry. 2017;8:119. doi: 10.3389/fpsyt.2017.00119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen JD, Nichols T, Keller J, Gomez RG, Schatzberg AF, Reiss AL. Insular cortex abnormalities in psychotic major depression: Relationship to gender and psychotic symptoms. Neuroscience Research. 2013;75(4):331–339. doi: 10.1016/j.neures.2013.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cyprien F, Courtet P, Poulain V, Maller J, Meslin C, Bonafé A, et al. Corpus callosum size may predict late-life depression in women: A 10-year follow-up study. Journal of Affective Disorders. 2014;165:16–23. doi: 10.1016/j.jad.2014.04.040. [DOI] [PubMed] [Google Scholar]
- De Almeida, J.R.C., Kronhaus, D.M., Sibille, E.L., Langenecker, S.A., Versace, A., LaBarbara, E.J., et al. (2011). Abnormal left-sided orbitomedial prefrontal cortical-amygdala connectivity during happy and fear face processing: A potential neural mechanism of female MDD. Frontiers in Psychiatry. 2(DEC). [DOI] [PMC free article] [PubMed]
- Dean DC, 3rd, Planalp EM, Wooten W, Kecskemeti SR, Adluru N, Schmidt CK, et al. Association of Prenatal Maternal Depression and Anxiety Symptoms With Infant White Matter Microstructure. JAMA Pediatrics. 2018;172(10):973–981. doi: 10.1001/jamapediatrics.2018.2132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delvecchio G, Altamura AC, Soares JC, Brambilla P. Pituitary gland in Bipolar Disorder and Major Depression: Evidence from structural MRI studies: Special Section on "Translational and Neuroscience Studies in Affective Disorders". Section Editor, Maria Nobile MD, PhD. This Section of JAD focuses on the relevance of translational and neuroscience studies in providing a better understanding of the neural basis of affective disorders. The main aim is to briefly summarise relevant research findings in clinical neuroscience with particular regards to specific innovative topics in mood and anxiety disorders. Journal of affective disorders. 2017;218:446–50. doi: 10.1016/j.jad.2017.03.066. [DOI] [PubMed] [Google Scholar]
- Deng Y, McQuoid DR, Potter GG, Steffens DC, Albert K, Riddle M, et al. Predictors of recurrence in remitted late-life depression. Depression and Anxiety. 2018;35(7):658–667. doi: 10.1002/da.22772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Domschke K, Dannlowski U, Ohrmann P, Lawford B, Bauer J, Kugel H, et al. Cannabinoid receptor 1 (CNR1) gene: Impact on antidepressant treatment response and emotion processing in major depression. European Neuropsychopharmacology : The Journal of the European College of Neuropsychopharmacology. 2008;18(10):751–759. doi: 10.1016/j.euroneuro.2008.05.003. [DOI] [PubMed] [Google Scholar]
- Dong D, Ironside M, Belleau EL, Sun X, Cheng C, Xiong G, et al. Sex-specific neural responses to acute psychosocial stress in depression. Translational Psychiatry. 2022;12(1):2. doi: 10.1038/s41398-021-01768-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dotson VM, Zonderman AB, Kraut MA, Resnick SM. Temporal relationships between depressive symptoms and white matter hyperintensities in older men and women. International Journal of Geriatric Psychiatry. 2013;28(1):66–74. doi: 10.1002/gps.3791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eid RS, Gobinath AR, Galea LAM. Sex differences in depression: Insights from clinical and preclinical studies. Progress in Neurobiology. 2019;176:86–102. doi: 10.1016/j.pneurobio.2019.01.006. [DOI] [PubMed] [Google Scholar]
- Elbejjani M, Fuhrer R, Abrahamowicz M, Mazoyer B, Crivello F, Tzourio C, et al. Hippocampal atrophy and subsequent depressive symptoms in older men and women: Results from a 10-year prospective cohort. American Journal of Epidemiology. 2014;180(4):385–393. doi: 10.1093/aje/kwu132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elbejjani M, Fuhrer R, Abrahamowicz M, Mazoyer B, Crivello F, Tzourio C, et al. Depression, depressive symptoms, and rate of hippocampal atrophy in a longitudinal cohort of older men and women. Psychological Medicine. 2015;45(9):1931–1944. doi: 10.1017/S0033291714003055. [DOI] [PubMed] [Google Scholar]
- Ellis R, Fernandes A, Simmons JG, Mundy L, Patton G, Allen NB, et al. Relationships between adrenarcheal hormones, hippocampal volumes and depressive symptoms in children. Psychoneuroendocrinology. 2019;104:55–63. doi: 10.1016/j.psyneuen.2019.02.016. [DOI] [PubMed] [Google Scholar]
- El-Mallakh RS, Ali Z. Therapeutic implications of the serotonin transporter gene in depression. Biomarkers in Neuropsychiatry. 2019;1:100004. doi: 10.1016/j.bionps.2019.100004. [DOI] [Google Scholar]
- Fernandes B, Diaz AP, Scaini G, Mwangi B, Wu M-J, Quevedo J, et al. C-Reactive Protein and the Uncinate Fasciculus in Anhedonia and Depression. Biological Psychiatry. 2021;89(9):S272. doi: 10.1016/j.biopsych.2021.02.681. [DOI] [Google Scholar]
- Filippi M, Agosta F. Diffusion tensor imaging and functional MRI. Handbook of Clinical Neurology. 2016;136:1065–1087. doi: 10.1016/B978-0-444-53486-6.00056-9. [DOI] [PubMed] [Google Scholar]
- Frodl T, Meisenzahl EM, Zetzsche T, Born C, Groll C, Jäger M, et al. Hippocampal changes in patients with a first episode of major depression. The American Journal of Psychiatry. 2002;159(7):1112–1118. doi: 10.1176/appi.ajp.159.7.1112. [DOI] [PubMed] [Google Scholar]
- Frodl T, Reinhold E, Koutsouleris N, Reiser M, Meisenzahl EM. Interaction of childhood stress with hippocampus and prefrontal cortex volume reduction in major depression. Journal of Psychiatric Research. 2010;44(13):799–807. doi: 10.1016/j.jpsychires.2010.01.006. [DOI] [PubMed] [Google Scholar]
- Frodl T, Janowitz D, Schmaal L, Tozzi L, Dobrowolny H, Stein DJ, et al. Childhood adversity impacts on brain subcortical structures relevant to depression. Journal of Psychiatric Research. 2017;86:58–65. doi: 10.1016/j.jpsychires.2016.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furtado CP, Maller JJ, Fitzgerald PB. A magnetic resonance imaging study of the entorhinal cortex in treatment-resistant depression. Psychiatry Research. 2008;163(2):133–142. doi: 10.1016/j.pscychresns.2007.11.005. [DOI] [PubMed] [Google Scholar]
- Gadermann AM, Alonso J, Vilagut G, Zaslavsky AM, Kessler RC. Comorbidity and disease burden in the National Comorbidity Survey Replication (NCS-R) Depression and Anxiety. 2012;29(9):797–806. doi: 10.1002/da.21924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geerlings MI, Gerritsen L. Late-Life Depression, Hippocampal Volumes, and Hypothalamic-Pituitary-Adrenal Axis Regulation: A Systematic Review and Meta-analysis. Biological Psychiatry. 2017;82(5):339–350. doi: 10.1016/j.biopsych.2016.12.032. [DOI] [PubMed] [Google Scholar]
- Geng J, Yan R, Shi J, Chen Y, Mo Z, Shao J, et al. Altered regional homogeneity in patients with somatic depression: A resting-state fMRI study. Journal of Affective Disorders. 2019;246:498–505. doi: 10.1016/j.jad.2018.12.066. [DOI] [PubMed] [Google Scholar]
- Ghazi Sherbaf F, Aarabi MH, Hosein Yazdi M, Haghshomar M. White matter microstructure in fetal alcohol spectrum disorders: A systematic review of diffusion tensor imaging studies. Human Brain Mapping. 2019;40(3):1017–1036. doi: 10.1002/hbm.24409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giedd JN, Raznahan A, Mills KL, Lenroot RK. Review: Magnetic resonance imaging of male/female differences in human adolescent brain anatomy. Biology of Sex Differences. 2012;3(1):19. doi: 10.1186/2042-6410-3-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold SM, Köhler-Forsberg O, Moss-Morris R, Mehnert A, Miranda JJ, Bullinger M, et al. Comorbid depression in medical diseases. Nature Reviews Disease Primers. 2020;6(1):69. doi: 10.1038/s41572-020-0200-2. [DOI] [PubMed] [Google Scholar]
- Gorham LS, Jernigan T, Hudziak J, Barch DM. Involvement in Sports, Hippocampal Volume, and Depressive Symptoms in Children. Biological Psychiatry Cognitive Neuroscience and Neuroimaging. 2019;4(5):484–492. doi: 10.1016/j.bpsc.2019.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamani C, Mayberg H, Stone S, Laxton A, Haber S, Lozano AM. The subcallosal cingulate gyrus in the context of major depression. Biological Psychiatry. 2011;69(4):301–308. doi: 10.1016/j.biopsych.2010.09.034. [DOI] [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. Journal of Neurology, Neurosurgery and Psychiatry. 1960;23(1):56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hastings RS, Parsey RV, Oquendo MA, Arango V, Mann JJ. Volumetric analysis of the prefrontal cortex, amygdala, and hippocampus in major depression. Neuropsychopharmacology : Official Publication of the American College of Neuropsychopharmacology. 2004;29(5):952–959. doi: 10.1038/sj.npp.1300371. [DOI] [PubMed] [Google Scholar]
- Hay RE, Reynolds JE, Grohs MN, Paniukov D, Giesbrecht GF, Letourneau N, et al. Amygdala-Prefrontal Structural Connectivity Mediates the Relationship between Prenatal Depression and Behavior in Preschool Boys. The Journal of Neuroscience : The Official Journal of the Society for Neuroscience. 2020;40(36):6969–6977. doi: 10.1523/JNEUROSCI.0481-20.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayakawa YK, Sasaki H, Takao H, Hayashi N, Kunimatsu A, Ohtomo K, et al. Depressive symptoms and neuroanatomical structures in community-dwelling women: A combined voxel-based morphometry and diffusion tensor imaging study with tract-based spatial statistics. NeuroImage Clinical. 2014;4:481–487. doi: 10.1016/j.nicl.2014.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herreen D, Rice S, Zajac I. Brief assessment of male depression in clinical care: Validation of the Male Depression Risk Scale short form in a cross-sectional study of Australian men. British Medical Journal Open. 2022;12(3):e053650. doi: 10.1136/bmjopen-2021-053650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho TC, Sisk LM, Kulla A, Teresi GI, Hansen MM, Wu H, et al. Sex differences in myelin content of white matter tracts in adolescents with depression. Neuropsychopharmacology. 2021;46(13):2295–2303. doi: 10.1038/s41386-021-01078-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho, T.C., Sisk, L.M., Kulla, A., Teresi, G.I., Hansen, M.M., Wu, H., et al. (2021a). Sex differences in myelin content of white matter tracts in adolescents with depression. Neuropsychopharmacology : official publication of the American College of Neuropsychopharmacology. [DOI] [PMC free article] [PubMed]
- Hölzel BK, Carmody J, Evans KC, Hoge EA, Dusek JA, Morgan L, et al. Stress reduction correlates with structural changes in the amygdala. Soc Cogn Affect Neurosci. 2010;5(1):11–17. doi: 10.1093/scan/nsp034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoobehfekr S, Moghaddam HS, Shalbafan M, Hashemi MG, Pirmoradi MM, Sakenian A, et al. Efficacy and safety of tipepidine as adjunctive therapy in major depressive disorder: A randomized, double-blind, placebo-controlled clinical trial. Psychiatry and Clinical Neurosciences. 2021;75(2):57–62. doi: 10.1111/pcn.13180. [DOI] [PubMed] [Google Scholar]
- Hu Y, Moore M, Bertels Z, Phan KL, Dolcos F, Dolcos S. Smaller amygdala volume and increased neuroticism predict anxiety symptoms in healthy subjects: A volumetric approach using manual tracing. Neuropsychologia. 2020;145:106564. doi: 10.1016/j.neuropsychologia.2017.11.008. [DOI] [PubMed] [Google Scholar]
- Huang GQ, Wang HB, Xu LY, Wang JW, Li XH, Yu YQ. Functional MRI study on gender-related difference of caudate nucleus activation for emotional memory in major depressive disorder. Chinese Journal of Interventional Imaging and Therapy. 2014;11(9):582–586. [Google Scholar]
- Institute UMaMSNaI. (2023). ENIGMA MDD [Available from: https://enigma.ini.usc.edu/ongoing/enigma-mdd-working-group/.
- Jenkins LM, Kendall AD, Kassel MT, Patrón VG, Gowins JR, Dion C, et al. Considering sex differences clarifies the effects of depression on facial emotion processing during fMRI. Journal of Affective Disorders. 2018;225:129–136. doi: 10.1016/j.jad.2017.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katon WJ. Epidemiology and treatment of depression in patients with chronic medical illness. Dialogues in Clinical Neuroscience. 2011;13(1):7–23. doi: 10.31887/DCNS.2011.13.1/wkaton. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, et al. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): Initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36(7):980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Keller M, Zweerings J, Klasen M, Zvyagintsev M, Iglesias J, Mendoza Quiñones R, et al. fMRI Neurofeedback-Enhanced Cognitive Reappraisal Training in Depression: A Double-Blind Comparison of Left and Right vlPFC Regulation. Frontiers in Psychiatry. 2021;12:715898. doi: 10.3389/fpsyt.2021.715898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kempton MJ, Salvador Z, Munafò MR, Geddes JR, Simmons A, Frangou S, et al. Structural neuroimaging studies in major depressive disorder Meta-analysis and comparison with bipolar disorder. Arch Gen Psychiatry. 2011;68(7):675–90. doi: 10.1001/archgenpsychiatry.2011.60. [DOI] [PubMed] [Google Scholar]
- Kim GW, Park K, Jeong GW. Effects of Sex Hormones and Age on Brain Volume in Post-Menopausal Women. The Journal of Sexual Medicine. 2018;15(5):662–670. doi: 10.1016/j.jsxm.2018.03.006. [DOI] [PubMed] [Google Scholar]
- Kim H, Kwak S, Kim J, Youm Y, Chey J. Social Network Position Moderates the Relationship between Late-life Depressive Symptoms and Memory Differently in Men and Women. Scientific Reports. 2019;9(1):6142. doi: 10.1038/s41598-019-42388-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kircanski K, Sisk LM, Ho TC, Humphreys KL, King LS, Colich NL, et al. Early life stress, cortisol, frontolimbic connectivity, and depressive symptoms during puberty. Development and Psychopathology. 2019;31(3):1011–1022. doi: 10.1017/S0954579419000555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirton JW, Resnick SM, Davatzikos C, Kraut MA, Dotson VM. Depressive symptoms, symptom dimensions, and white matter lesion volume in older adults: A longitudinal study. The American Journal of Geriatric Psychiatry : Official Journal of the American Association for Geriatric Psychiatry. 2014;22(12):1469–1477. doi: 10.1016/j.jagp.2013.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kliamovich D, Jones SA, Chiapuzio AM, Baker FC, Clark DB, Nagel BJ. Sex-specific patterns of white matter microstructure are associated with emerging depression during adolescence. Psychiatry Research Neuroimaging. 2021;315:111324. doi: 10.1016/j.pscychresns.2021.111324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kong L, Chen K, Womer F, Jiang W, Luo X, Driesen N, et al. Sex differences of gray matter morphology in cortico-limbic-striatal neural system in major depressive disorder. Journal of Psychiatric Research. 2013;47(6):733–739. doi: 10.1016/j.jpsychires.2013.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovacs M. (n.d). Children's Depression Inventory (CDI and CDI 2). The Encyclopedia of Clinical Psychology. p. 1–5.
- Kronmüller KT, Pantel J, Götz B, Köhler S, Victor D, Mundt C, et al. Life events and hippocampal volume in first-episode major depression. Journal of Affective Disorders. 2008;110(3):241–247. doi: 10.1016/j.jad.2008.01.022. [DOI] [PubMed] [Google Scholar]
- Kronmüller KT, Schröder J, Köhler S, Götz B, Victor D, Unger J, et al. Hippocampal volume in first episode and recurrent depression. Psychiatry Research. 2009;174(1):62–66. doi: 10.1016/j.pscychresns.2008.08.001. [DOI] [PubMed] [Google Scholar]
- Kuehner C. Why is depression more common among women than among men? Lancet Psychiatry. 2017;4(2):146–158. doi: 10.1016/S2215-0366(16)30263-2. [DOI] [PubMed] [Google Scholar]
- Lacerda AL, Brambilla P, Sassi RB, Nicoletti MA, Mallinger AG, Frank E, et al. Anatomical MRI study of corpus callosum in unipolar depression. Journal of Psychiatric Research. 2005;39(4):347–354. doi: 10.1016/j.jpsychires.2004.10.004. [DOI] [PubMed] [Google Scholar]
- Lai CH, Wu YT. Alterations in white matter micro-integrity of the superior longitudinal fasciculus and anterior thalamic radiation of young adult patients with depression. Psychological Medicine. 2014;44(13):2825–2832. doi: 10.1017/S0033291714000440. [DOI] [PubMed] [Google Scholar]
- Lavretsky H, Lesser IM, Wohl M, Miller BL. Relationship of age, age at onset, and sex to depression in older adults. The American Journal of Geriatric Psychiatry : Official Journal of the American Association for Geriatric Psychiatry. 1998;6(3):248–256. doi: 10.1097/00019442-199808000-00007. [DOI] [PubMed] [Google Scholar]
- Lavretsky H, Kurbanyan K, Ballmaier M, Mintz J, Toga A, Kumar A. Sex differences in brain structure in geriatric depression. The American Journal of Geriatric Psychiatry : Official Journal of the American Association for Geriatric Psychiatry. 2004;12(6):653–657. doi: 10.1097/00019442-200411000-00012. [DOI] [PubMed] [Google Scholar]
- Laxton AW, Neimat JS, Davis KD, Womelsdorf T, Hutchison WD, Dostrovsky JO, et al. Neuronal coding of implicit emotion categories in the subcallosal cortex in patients with depression. Biological Psychiatry. 2013;74(10):714–719. doi: 10.1016/j.biopsych.2013.03.029. [DOI] [PubMed] [Google Scholar]
- Lebedeva A, Borza T, Håberg AK, Idland AV, Dalaker TO, Aarsland D, et al. Neuroanatomical correlates of late-life depression and associated cognitive changes. Neurobiology of Aging. 2015;36(11):3090–3099. doi: 10.1016/j.neurobiolaging.2015.04.020. [DOI] [PubMed] [Google Scholar]
- Lee A, Poh JS, Wen DJ, Guillaume B, Chong YS, Shek LP, et al. Long-term Influences of Prenatal Maternal Depressive Symptoms on the Amygdala-Prefrontal Circuitry of the Offspring From Birth to Early Childhood. Biological Psychiatry Cognitive Neuroscience and Neuroimaging. 2019;4(11):940–947. doi: 10.1016/j.bpsc.2019.05.006. [DOI] [PubMed] [Google Scholar]
- Lépine JP, Briley M. The increasing burden of depression. Neuropsychiatric Disease and Treatment. 2011;7(Suppl 1):3–7. doi: 10.2147/NDT.S19617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lessov-Schlaggar CN, Reed T, Swan GE, Krasnow RE, DeCarli C, Marcus R, et al. Association of sex steroid hormones with brain morphology and cognition in healthy elderly men. Neurology. 2005;65(10):1591–1596. doi: 10.1212/01.wnl.0000184512.08249.48. [DOI] [PubMed] [Google Scholar]
- Lewine RR, Hudgins P, Brown F, Caudle J, Risch SC. Differences in qualitative brain morphology findings in schizophrenia, major depression, bipolar disorder, and normal volunteers. Schizophrenia Research. 1995;15(3):253–259. doi: 10.1016/0920-9964(94)00055-D. [DOI] [PubMed] [Google Scholar]
- Li C, Schreiber J, Bittner N, Li S, Huang R, Moebus S, et al. White Matter Microstructure Underlies the Effects of Sleep Quality and Life Stress on Depression Symptomatology in Older Adults. Frontiers in Aging Neuroscience. 2020;12:578037. doi: 10.3389/fnagi.2020.578037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li GZ, Liu PH, Zhang AX, Andari E, Zhang KR. A resting state fMRI study of major depressive disorder with and without anxiety. Psychiatry Research. 2022;315:114697. doi: 10.1016/j.psychres.2022.114697. [DOI] [PubMed] [Google Scholar]
- Liu Y, Wang K, Yu C, He Y, Zhou Y, Liang M, et al. Regional homogeneity, functional connectivity and imaging markers of Alzheimer's disease: A review of resting-state fMRI studies. Neuropsychologia. 2008;46(6):1648–1656. doi: 10.1016/j.neuropsychologia.2008.01.027. [DOI] [PubMed] [Google Scholar]
- Liu CH, Ma X, Li F, Wang YJ, Tie CL, Li SF, et al. Regional homogeneity within the default mode network in bipolar depression: A resting-state functional magnetic resonance imaging study. PLoS ONE. 2012;7(11):e48181. doi: 10.1371/journal.pone.0048181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyall LM, Wyse CA, Celis-Morales CA, Lyall DM, Cullen B, Mackay D, et al. Seasonality of depressive symptoms in women but not in men: A cross-sectional study in the UK Biobank cohort. Journal of Affective Disorders. 2018;229:296–305. doi: 10.1016/j.jad.2017.12.106. [DOI] [PubMed] [Google Scholar]
- Lyon M, Welton T, Varda A, Maller JJ, Broadhouse K, Korgaonkar MS, et al. Gender-specific structural abnormalities in major depressive disorder revealed by fixel-based analysis. Neuroimage Clin. 2019;21:101668. doi: 10.1016/j.nicl.2019.101668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacMaster FP, Russell A, Mirza Y, Keshavan MS, Taormina SP, Bhandari R, et al. Pituitary volume in treatment-naïve pediatric major depressive disorder. Biological Psychiatry. 2006;60(8):862–866. doi: 10.1016/j.biopsych.2006.04.013. [DOI] [PubMed] [Google Scholar]
- MacMaster FP, Leslie R, Rosenberg DR, Kusumakar V. Pituitary gland volume in adolescent and young adult bipolar and unipolar depression. Bipolar Disorders. 2008;10(1):101–104. doi: 10.1111/j.1399-5618.2008.00476.x. [DOI] [PubMed] [Google Scholar]
- Maglanoc LA, Kaufmann T, Jonassen R, Hilland E, Beck D, Landrø NI, et al. Multimodal fusion of structural and functional brain imaging in depression using linked independent component analysis. Human Brain Mapping. 2020;41(1):241–255. doi: 10.1002/hbm.24802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maller JJ, Daskalakis ZJ, Fitzgerald PB. Hippocampal volumetrics in depression: The importance of the posterior tail. Hippocampus. 2007;17(11):1023–1027. doi: 10.1002/hipo.20339. [DOI] [PubMed] [Google Scholar]
- McCarter T. Depression overview. Am Health Drug Benefits. 2008;1(3):44–51. [PMC free article] [PubMed] [Google Scholar]
- Mei L, Wang Y, Liu C, Mou J, Yuan Y, Qiu L, et al. Study of Sex Differences in Unmedicated Patients With Major Depressive Disorder by Using Resting State Brain Functional Magnetic Resonance Imaging. Frontiers in Neuroscience. 2022;16:814410. doi: 10.3389/fnins.2022.814410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melartin TK, Rytsälä HJ, Leskelä US, Lestelä-Mielonen PS, Sokero TP, Isometsä ET. Current comorbidity of psychiatric disorders among DSM-IV major depressive disorder patients in psychiatric care in the Vantaa Depression Study. The Journal of Clinical Psychiatry. 2002;63(2):126–134. doi: 10.4088/JCP.v63n0207. [DOI] [PubMed] [Google Scholar]
- Menzler K, Belke M, Wehrmann E, Krakow K, Lengler U, Jansen A, et al. Men and women are different: Diffusion tensor imaging reveals sexual dimorphism in the microstructure of the thalamus, corpus callosum and cingulum. NeuroImage. 2011;54(4):2557–2562. doi: 10.1016/j.neuroimage.2010.11.029. [DOI] [PubMed] [Google Scholar]
- Meruelo AD, Brumback T, Nagel BJ, Baker FC, Brown SA, Tapert SF. Neuroimaging markers of adolescent depression in the National Consortium on Alcohol and Neurodevelopment in Adolescence (NCANDA) study. Journal of Affective Disorders. 2021;287:380–386. doi: 10.1016/j.jad.2021.03.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. The British Journal of Psychiatry : The Journal of Mental Science. 1979;134:382–389. doi: 10.1192/bjp.134.4.382. [DOI] [PubMed] [Google Scholar]
- Morssinkhof MWL, van Wylick DW, Priester-Vink S, van der Werf YD, den Heijer M, van den Heuvel OA, et al. Associations between sex hormones, sleep problems and depression: A systematic review. Neuroscience and Biobehavioral Reviews. 2020;118:669–680. doi: 10.1016/j.neubiorev.2020.08.006. [DOI] [PubMed] [Google Scholar]
- Moulinet I, Landeau B, Touron E, De La Sayette V, Desgranges B, Vivien D, et al. Sex-specificities in anxiety and depressive symptoms across the lifespan and their links with multimodal neuroimaging. Journal of Affective Disorders. 2021;296:593–602. doi: 10.1016/j.jad.2021.10.004. [DOI] [PubMed] [Google Scholar]
- Murray AD, Staff RT, McNeil CJ, Salarirad S, Phillips LH, Starr J, et al. Depressive symptoms in late life and cerebrovascular disease: The importance of intelligence and lesion location. Depression and Anxiety. 2013;30(1):77–84. doi: 10.1002/da.22022. [DOI] [PubMed] [Google Scholar]
- Nielsen JD, Case JAC, Divers RM, Kautz MM, Alloy LB, Olino TM. Trajectories of depressive symptoms through adolescence as predictors of cortical thickness in the orbitofrontal cortex: An examination of sex differences. Psychiatry Research Neuroimaging. 2020;303:111132. doi: 10.1016/j.pscychresns.2020.111132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogrodniczuk JS, Oliffe JL. Men and depression. Canadian Family Physician. 2011;57(2):153–155. [PMC free article] [PubMed] [Google Scholar]
- Osman A, Wong JL, Bagge CL, Freedenthal S, Gutierrez PM, Lozano G. The Depression Anxiety Stress Scales-21 (DASS-21): Further examination of dimensions, scale reliability, and correlates. Journal of Clinical Psychology. 2012;68(12):1322–1338. doi: 10.1002/jclp.21908. [DOI] [PubMed] [Google Scholar]
- Parsey RV, Oquendo MA, Simpson NR, Ogden RT, Van Heertum R, Arango V, et al. Effects of sex, age, and aggressive traits in man on brain serotonin 5-HT1A receptor binding potential measured by PET using [C-11]WAY-100635. Brain Research. 2002;954(2):173–182. doi: 10.1016/S0006-8993(02)03243-2. [DOI] [PubMed] [Google Scholar]
- Peng W, Chen Z, Yin L, Jia Z, Gong Q. Essential brain structural alterations in major depressive disorder: A voxel-wise meta-analysis on first episode, medication-naive patients. Journal of Affective Disorders. 2016;199:114–123. doi: 10.1016/j.jad.2016.04.001. [DOI] [PubMed] [Google Scholar]
- Perlaki G, Orsi G, Plozer E, Altbacker A, Darnai G, Nagy SA, et al. Are there any gender differences in the hippocampus volume after head-size correction? A volumetric and voxel-based morphometric study. Neuroscience Letters. 2014;570:119–123. doi: 10.1016/j.neulet.2014.04.013. [DOI] [PubMed] [Google Scholar]
- Perlman G, Bartlett E, DeLorenzo C, Weissman M, McGrath P, Ogden T, et al. Cortical thickness is not associated with current depression in a clinical treatment study. Human Brain Mapping. 2017;38(9):4370–4385. doi: 10.1002/hbm.23664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pettemeridou E, Kallousia E, Constantinidou F. Regional Brain Volume, Brain Reserve and MMSE Performance in Healthy Aging From the NEUROAGE Cohort: Contributions of Sex, Education, and Depression Symptoms. Front Aging Neurosci. 2021;13:711301. doi: 10.3389/fnagi.2021.711301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piani MC, Maggioni E, Delvecchio G, Ferro A, Gritti D, Pozzoli SM, et al. Sexual Dimorphism in the Brain Correlates of Adult-Onset Depression: A Pilot Structural and Functional 3T MRI Study. Front Psychiatry. 2021;12:683912. doi: 10.3389/fpsyt.2021.683912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pimontel MA, Reinlieb ME, Johnert LC, Garcon E, Sneed JR, Roose SP. The external validity of MRI-defined vascular depression. International Journal of Geriatric Psychiatry. 2013;28(11):1189–1196. doi: 10.1002/gps.3943. [DOI] [PubMed] [Google Scholar]
- Piras F, Vecchio D, Kurth F, Piras F, Banaj N, Ciullo V, et al. Corpus callosum morphology in major mental disorders: a magnetic resonance imaging study. Brain Communications. 2021;3(2):fcab100. doi: 10.1093/braincomms/fcab100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poznanski E, Mokros HB, Grossman J, Freeman LN. Diagnostic criteria in childhood depression. American Journal of Psychiatry. 1985;142(10):1168–1173. doi: 10.1176/ajp.142.10.1168. [DOI] [PubMed] [Google Scholar]
- Radloff, L.S. (1977). The CES-D Scale: A self-report depression scale for research in the general population.
- Rajagopalan P, Passe TJ, Doraiswamy PM, Figiel GS, Macfall JR, Krishnan KR. Changes in pituitary gland signal intensity and morphology as evaluated by magnetic resonance imaging in aging, depression, and by gender. Depression. 1994;2(6):303–307. doi: 10.1002/depr.3050020605. [DOI] [Google Scholar]
- Rakesh D, Kelly C, Vijayakumar N, Zalesky A, Allen NB, Whittle S. Unraveling the Consequences of Childhood Maltreatment: Deviations From Typical Functional Neurodevelopment Mediate the Relationship Between Maltreatment History and Depressive Symptoms. Biological Psychiatry Cognitive Neuroscience and Neuroimaging. 2021;6(3):329–342. doi: 10.1016/j.bpsc.2020.09.016. [DOI] [PubMed] [Google Scholar]
- Reale, C., Invernizzi, F., Panteghini, C., Garavaglia, B. (2021). Genetics, sex, and gender. J Neurosci Res. [DOI] [PubMed]
- Reilly D. Gender can be a continuous variable, not just a categorical one: Comment on Hyde, Bigler, Joel, Tate, and van Anders (2019) American Psychologist. 2019;74(7):840–841. doi: 10.1037/amp0000505. [DOI] [PubMed] [Google Scholar]
- Reinlieb ME, Persaud A, Singh D, Garcon E, Rutherford BR, Pelton GH, et al. Vascular depression: Overrepresented among African Americans? International Journal of Geriatric Psychiatry. 2014;29(5):470–477. doi: 10.1002/gps.4029. [DOI] [PubMed] [Google Scholar]
- Reynolds, W. (2004). Reynolds Adolescent Depression Scale (RADS) Second Edition. p. 224–36.
- Rice F, Riglin L, Lomax T, Souter E, Potter R, Smith DJ, et al. Adolescent and adult differences in major depression symptom profiles. Journal of Affective Disorders. 2019;243:175–181. doi: 10.1016/j.jad.2018.09.015. [DOI] [PubMed] [Google Scholar]
- Ritter C, Buchmann A, Müller ST, Hersberger M, Haynes M, Ghisleni C, et al. Cerebral perfusion in depression: Relationship to sex, dehydroepiandrosterone sulfate and depression severity. NeuroImage Clinical. 2021;32:102840. doi: 10.1016/j.nicl.2021.102840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romans SE, Tyas J, Cohen MM, Silverstone T. Gender differences in the symptoms of major depressive disorder. The Journal of Nervous and Mental Disease. 2007;195(11):905–911. doi: 10.1097/NMD.0b013e3181594cb7. [DOI] [PubMed] [Google Scholar]
- Rueda, A. (2019). editor Gender Differences in Rates of Anhedonia and the Effect of Menstrual Cycles in University Students.
- Saleh K, Carballedo A, Lisiecka D, Fagan AJ, Connolly G, Boyle G, et al. Impact of family history and depression on amygdala volume. Psychiatry Research. 2012;203(1):24–30. doi: 10.1016/j.pscychresns.2011.10.004. [DOI] [PubMed] [Google Scholar]
- Salk RH, Hyde JS, Abramson LY. Gender differences in depression in representative national samples: Meta-analyses of diagnoses and symptoms. Psychological Bulletin. 2017;143(8):783–822. doi: 10.1037/bul0000102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savitz JB, Nugent AC, Bogers W, Roiser JP, Bain EE, Neumeister A, et al. Habenula volume in bipolar disorder and major depressive disorder: A high-resolution magnetic resonance imaging study. Biological Psychiatry. 2011;69(4):336–343. doi: 10.1016/j.biopsych.2010.09.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schiller CE, Meltzer-Brody S, Rubinow DR. The role of reproductive hormones in postpartum depression. CNS Spectrums. 2015;20(1):48–59. doi: 10.1017/S1092852914000480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmaal L, Veltman DJ, van Erp TG, Sämann PG, Frodl T, Jahanshad N, et al. Subcortical brain alterations in major depressive disorder: Findings from the ENIGMA Major Depressive Disorder working group. Molecular Psychiatry. 2016;21(6):806–812. doi: 10.1038/mp.2015.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmaal L, Yücel M, Ellis R, Vijayakumar N, Simmons JG, Allen NB, et al. Brain Structural Signatures of Adolescent Depressive Symptom Trajectories: A Longitudinal Magnetic Resonance Imaging Study. Journal of the American Academy of Child and Adolescent Psychiatry. 2017;56(7):593–601.e9. doi: 10.1016/j.jaac.2017.05.008. [DOI] [PubMed] [Google Scholar]
- Schmaal L, Hibar DP, Sämann PG, Hall GB, Baune BT, Jahanshad N, et al. Cortical abnormalities in adults and adolescents with major depression based on brain scans from 20 cohorts worldwide in the ENIGMA Major Depressive Disorder Working Group. Molecular Psychiatry. 2017;22(6):900–909. doi: 10.1038/mp.2016.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt PJ, Rubinow DR. Sex hormones and mood in the perimenopause. Annals of the New York Academy of Sciences. 2009;1179:70–85. doi: 10.1111/j.1749-6632.2009.04982.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuch JJ, Roest AM, Nolen WA, Penninx BW, de Jonge P. Gender differences in major depressive disorder: Results from the Netherlands study of depression and anxiety. Journal of Affective Disorders. 2014;156:156–163. doi: 10.1016/j.jad.2013.12.011. [DOI] [PubMed] [Google Scholar]
- Sheehan, D.V., Lecrubier, Y., Sheehan, K.H., Amorim, P., Janavs, J., Weiller, E., et al. (1998). The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. The Journal of clinical psychiatry. 59 Suppl 20:22–33;quiz 4–57. [PubMed]
- Smith DJ, Kyle S, Forty L, Cooper C, Walters J, Russell E, et al. Differences in depressive symptom profile between males and females. Journal of Affective Disorders. 2008;108(3):279–284. doi: 10.1016/j.jad.2007.10.001. [DOI] [PubMed] [Google Scholar]
- Soe NN, Wen DJ, Poh JS, Chong YS, Broekman BF, Chen H, et al. Perinatal maternal depressive symptoms alter amygdala functional connectivity in girls. Human Brain Mapping. 2018;39(2):680–690. doi: 10.1002/hbm.23873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sonnenberg CM, Deeg DJ, van Tilburg TG, Vink D, Stek ML, Beekman AT. Gender differences in the relation between depression and social support in later life. International Psychogeriatrics. 2013;25(1):61–70. doi: 10.1017/S1041610212001202. [DOI] [PubMed] [Google Scholar]
- Soriano-Mas C, Hernández-Ribas R, Pujol J, Urretavizcaya M, Deus J, Harrison BJ, et al. Cross-sectional and longitudinal assessment of structural brain alterations in melancholic depression. Biological Psychiatry. 2011;69(4):318–325. doi: 10.1016/j.biopsych.2010.07.029. [DOI] [PubMed] [Google Scholar]
- Spalletta G, Piras F, Caltagirone C, Fagioli S. Hippocampal multimodal structural changes and subclinical depression in healthy individuals. Journal of Affective Disorders. 2014;152–154:105–112. doi: 10.1016/j.jad.2013.05.068. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Williams JB, Gibbon M, First MB. The Structured Clinical Interview for DSM-III-R (SCID) I: History, rationale, and description. Arch Gen Psychiatry. 1992;49(8):624–9. doi: 10.1001/archpsyc.1992.01820080032005. [DOI] [PubMed] [Google Scholar]
- Staley JK, Sanacora G, Tamagnan G, Maciejewski PK, Malison RT, Berman RM, et al. Sex differences in diencephalon serotonin transporter availability in major depression. Biological Psychiatry. 2006;59(1):40–47. doi: 10.1016/j.biopsych.2005.06.012. [DOI] [PubMed] [Google Scholar]
- Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. European Journal of Epidemiology. 2010;25(9):603–605. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- Swartz MK. The PRISMA statement: A guideline for systematic reviews and meta-analyses. Journal of Pediatric Health Care. 2011;25(1):1–2. doi: 10.1016/j.pedhc.2010.09.006. [DOI] [PubMed] [Google Scholar]
- Takahashi T, Nishikawa Y, Yücel M, Whittle S, Lorenzetti V, Walterfang M, et al. Olfactory sulcus morphology in patients with current and past major depression. Psychiatry Research Neuroimaging. 2016;255:60–65. doi: 10.1016/j.pscychresns.2016.07.008. [DOI] [PubMed] [Google Scholar]
- Talishinsky A, Downar J, Vértes PE, Seidlitz J, Dunlop K, Lynch CJ, et al. Regional gene expression signatures are associated with sex-specific functional connectivity changes in depression. Nature Communications. 2022;13(1):5692. doi: 10.1038/s41467-022-32617-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tozzi L, Garczarek L, Janowitz D, Stein DJ, Wittfeld K, Dobrowolny H, et al. Interactive impact of childhood maltreatment, depression, and age on cortical brain structure: Mega-analytic findings from a large multi-site cohort. Psychological Medicine. 2020;50(6):1020–1031. doi: 10.1017/S003329171900093X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ugwu ID, Amico F, Carballedo A, Fagan AJ, Frodl T. Childhood adversity, depression, age and gender effects on white matter microstructure: A DTI study. Brain Structure & Function. 2015;220(4):1997–2009. doi: 10.1007/s00429-014-0769-x. [DOI] [PubMed] [Google Scholar]
- Ustün TB, Ayuso-Mateos JL, Chatterji S, Mathers C, Murray CJ. Global burden of depressive disorders in the year 2000. The British Journal of Psychiatry : The Journal of Mental Science. 2004;184:386–392. doi: 10.1192/bjp.184.5.386. [DOI] [PubMed] [Google Scholar]
- Vakili K, Pillay SS, Lafer B, Fava M, Renshaw PF, Bonello-Cintron CM, et al. Hippocampal volume in primary unipolar major depression: A magnetic resonance imaging study. Biological Psychiatry. 2000;47(12):1087–1090. doi: 10.1016/S0006-3223(99)00296-6. [DOI] [PubMed] [Google Scholar]
- van Eijk L, Hansell NK, Strike LT, Couvy-Duchesne B, de Zubicaray GI, Thompson PM, et al. Region-specific sex differences in the hippocampus. NeuroImage. 2020;215:116781. doi: 10.1016/j.neuroimage.2020.116781. [DOI] [PubMed] [Google Scholar]
- van Tol MJ, van der Wee NJ, van den Heuvel OA, Nielen MM, Demenescu LR, Aleman A, et al. Regional brain volume in depression and anxiety disorders. Archives of General Psychiatry. 2010;67(10):1002–1011. doi: 10.1001/archgenpsychiatry.2010.121. [DOI] [PubMed] [Google Scholar]
- van Velzen LS, Kelly S, Isaev D, Aleman A, Aftanas LI, Bauer J, et al. White matter disturbances in major depressive disorder: A coordinated analysis across 20 international cohorts in the ENIGMA MDD working group. Molecular Psychiatry. 2020;25(7):1511–1525. doi: 10.1038/s41380-019-0477-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Victor TA, Drevets WC, Misaki M, Bodurka J, Savitz J. Sex differences in neural responses to subliminal sad and happy faces in healthy individuals: Implications for depression. Journal of Neuroscience Research. 2017;95(1–2):703–710. doi: 10.1002/jnr.23870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viswanathan, M., Ansari, M.T., Berkman, N.D., Chang, S., Hartling, L., McPheeters, M., et al., (2008) AHRQ Methods for Effective Health Care Assessing the Risk of Bias of Individual Studies in Systematic Reviews of Health Care Interventions. Methods Guide for Effectiveness and Comparative Effectiveness Reviews. Rockville (MD): Agency for Healthcare Research and Quality (US). [PubMed]
- Wang L, Hermens DF, Hickie IB, Lagopoulos J. A systematic review of resting-state functional-MRI studies in major depression. Journal of Affective Disorders. 2012;142(1–3):6–12. doi: 10.1016/j.jad.2012.04.013. [DOI] [PubMed] [Google Scholar]
- Wang Q, Poh JS, Wen DJ, Broekman BFP, Chong YS, Yap F, et al. Functional and structural networks of lateral and medial orbitofrontal cortex as potential neural pathways for depression in childhood. Depression and Anxiety. 2019;36(4):365–374. doi: 10.1002/da.22874. [DOI] [PubMed] [Google Scholar]
- Wang Q, Zhang H, Poh JS, Pecheva D, Broekman BFP, Chong YS, et al. Sex-Dependent Associations among Maternal Depressive Symptoms, Child Reward Network, and Behaviors in Early Childhood. Cerebral cortex (New York, NY 1991) 2020;30(3):901–12. doi: 10.1093/cercor/bhz135. [DOI] [PubMed] [Google Scholar]
- Wei, W., Karim, H.T., Lin, C., Mizuno, A., Andreescu, C., Karp, J.F., et al (2018) Trajectories in Cerebral Blood Flow Following Antidepressant Treatment in Late-Life Depression: Support for the Vascular Depression Hypothesis. The Journal of clinical psychiatry. 79(6). [DOI] [PMC free article] [PubMed]
- Wei, D., Zhang, H., Broekman, BFP., Chong, Y.S., Shek, L.P., Yap, F., et al (2021) Cortical Development Mediates Association of Prenatal Maternal Depressive Symptoms and Child Reward Sensitivity: A Longitudinal Study. Journal of the American Academy of Child and Adolescent Psychiatry. [DOI] [PubMed]
- Weis S, Hausmann M, Stoffers B, Vohn R, Kellermann T, Sturm W. Estradiol modulates functional brain organization during the menstrual cycle: An analysis of interhemispheric inhibition. Journal of Neuroscience. 2008;28(50):13401–13410. doi: 10.1523/JNEUROSCI.4392-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen DJ, Poh JS, Ni SN, Chong YS, Chen H, Kwek K, et al. Influences of prenatal and postnatal maternal depression on amygdala volume and microstructure in young children. Translational Psychiatry. 2017;7(4):e1103. doi: 10.1038/tp.2017.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wesselhoeft R, Pedersen CB, Mortensen PB, Mors O, Bilenberg N. Gender-age interaction in incidence rates of childhood emotional disorders. Psychological Medicine. 2015;45(4):829–839. doi: 10.1017/S0033291714001901. [DOI] [PubMed] [Google Scholar]
- Williams LM, Coman JT, Stetz PC, Walker NC, Kozel FA, George MS, et al. Identifying response and predictive biomarkers for Transcranial magnetic stimulation outcomes: Protocol and rationale for a mechanistic study of functional neuroimaging and behavioral biomarkers in veterans with Pharmacoresistant depression. BMC Psychiatry. 2021;21(1):35. doi: 10.1186/s12888-020-03030-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Won E, Choi S, Kang J, Kim A, Han KM, Chang HS, et al. Association between reduced white matter integrity in the corpus callosum and serotonin transporter gene DNA methylation in medication-naive patients with major depressive disorder. Transl Psychiatry. 2016;6(8):e866–e. doi: 10.1038/tp.2016.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woo SL, Prince SE, Petrella JR, Hellegers C, Doraiswamy PM. Modulation of a human memory circuit by subsyndromal depression in late life: A functional magnetic resonance imaging study. The American Journal of Geriatric Psychiatry : Official Journal of the American Association for Geriatric Psychiatry. 2009;17(1):24–29. doi: 10.1097/JGP.0b013e318180056a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu JC, Buchsbaum MS, Johnson JC, Hershey TG, Wagner EA, Teng C, et al. Magnetic resonance and positron emission tomography imaging of the corpus callosum: Size, shape and metabolic rate in unipolar depression. Journal of Affective Disorders. 1993;28(1):15–25. doi: 10.1016/0165-0327(93)90073-S. [DOI] [PubMed] [Google Scholar]
- Yang X, Peng Z, Ma X, Meng Y, Li M, Zhang J, et al. Sex differences in the clinical characteristics and brain gray matter volume alterations in unmedicated patients with major depressive disorder. Science and Reports. 2017;7(1):2515. doi: 10.1038/s41598-017-02828-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Y, Wei K, Zhang H, Hu H, Yan L, Gui W, et al. Identifying functional brain abnormalities in migraine and depression comorbidity. Quantitative Imaging in Medicine and Surgery. 2022;12(4):2288–2302. doi: 10.21037/qims-21-667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao Z, Yan R, Wei M, Tang H, Qin J, Lu Q. Gender differences in brain activity and the relationship between brain activity and differences in prevalence rates between male and female major depressive disorder patients: A resting-state fMRI study. Clinical Neurophysiology. 2014;125(11):2232–2239. doi: 10.1016/j.clinph.2014.03.006. [DOI] [PubMed] [Google Scholar]
- Young KD, Bodurka J, Drevets WC. Functional neuroimaging of sex differences in autobiographical memory recall in depression. Psychological Medicine. 2017;47(15):2640–2652. doi: 10.1017/S003329171700112X. [DOI] [PubMed] [Google Scholar]
- Zavorotnyy M, Zöllner R, Schulte-Güstenberg LR, Wulff L, Schöning S, Dannlowski U, et al. Low left amygdala volume is associated with a longer duration of unipolar depression. Journal of Neural Transmission (vienna) 2018;125(2):229–238. doi: 10.1007/s00702-017-1811-y. [DOI] [PubMed] [Google Scholar]
- Zhang F-F, Peng W, Sweeney JA, Jia Z-Y, Gong Q-Y. Brain structure alterations in depression: Psychoradiological evidence. CNS Neuroscience & Therapeutics. 2018;24(11):994–1003. doi: 10.1111/cns.12835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang H, Wong TY, Broekman BFP, Chong YS, Shek LP, Gluckman PD, et al. Maternal Adverse Childhood Experience and Depression in Relation with Brain Network Development and Behaviors in Children: A Longitudinal Study. Cerebral cortex (New York, NY 1991) 2021;31(9):4233–44. doi: 10.1093/cercor/bhab081. [DOI] [PubMed] [Google Scholar]
- Zhang, X., Liang, M., Qin, W., Wan, B., Yu, C., Ming, D. (2020) Gender Differences Are Encoded Differently in the Structure and Function of the Human Brain Revealed by Multimodal MRI. Frontiers in Human Neuroscience. 14. [DOI] [PMC free article] [PubMed]
- Zhao W, Zhu D, Zhang Y, Zhang C, Zhang B, Yang Y, et al. Relationship between illness duration, corpus callosum changes, and sustained attention dysfunction in major depressive disorder. Quantitative Imaging in Medicine and Surgery. 2021;11(7):2980–2993. doi: 10.21037/qims-20-970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu, Y., Gao, H., Tong, L., Li, Z., Wang, L., Zhang, C., et al (2019) Emotion Regulation of Hippocampus Using Real-Time fMRI Neurofeedback in Healthy Human. Frontiers in Human Neuroscience. 13. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Not applicable.