Abstract
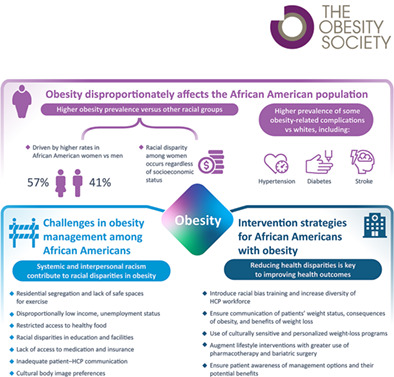
Obesity is a growing public health crisis in the United States and is associated with a substantial disease burden due to an increased risk for multiple complications, including cardiovascular and metabolic diseases. As highlighted in this review, obesity disproportionately affects the African American population, women in particular, regardless of socioeconomic status. Structural racism remains a major contributor to health disparities between African American people and the general population, and it limits access to healthy foods, safe spaces to exercise, adequate health insurance, and medication, all of which impact obesity prevalence and outcomes. Conscious and unconscious interpersonal racism also impacts obesity care and outcomes in African American people and may adversely affect interactions between health care practitioners and patients. To reduce health disparities, structural racism and racial bias must be addressed. Culturally relevant interventions for obesity management have been successfully implemented that have shown benefits in weight management and risk‐factor reduction. Strategies to improve health care practitioner–patient engagement should also be implemented to improve health outcomes in African American people with obesity. When managing obesity in African American people, it is critical to take a holistic approach and to consider an individual's social and cultural context in order to implement a successful treatment strategy.
Study Importance.
What is already known?
Obesity is a growing public health crisis in the United States that disproportionately affects African American people and is associated with a substantial disease burden due to an increased risk for multiple complications, including cardiovascular and metabolic diseases.
Major reviews that have already been published on this subject include Bailey et al. [1] and Bleich et al. [22].
What does this review add?
As noted in this review, long‐standing disparities in health and obesity care for African American people exist, with systemic racism remaining a major cause of these disparities.
Culturally relevant intervention strategies, including community‐ and faith‐based programs, are key to managing obesity in African American people.
How might these results change the direction of research or the focus of clinical practice?
This review underscores the need for health care practitioners to adopt appropriate culturally sensitive practices when engaging with African American people and to address unconscious racial bias in their interactions with patients.
In addition, we highlight the importance of personalizing weight‐loss interventions to be culturally relevant to African American people.
INTRODUCTION
Substantial disparities in obesity prevalence, burden, complications, and outcomes exist between African American people and other racial groups. Many of these disparities in obesity, and in health more broadly, in the African American population result from, and are maintained by, structural racism [1]. There is a need for greater understanding of the challenges in managing obesity among African American people, which in part reflect social, economic, and/or environmental differences between African American and non‐African American people [2].
This review describes the key challenges in managing obesity among African American people and provides practical guidance for health care practitioners (HCPs) and policy makers on how these can be addressed, emphasizing personalized, culturally sensitive treatment. The focus is adults with obesity; pediatric obesity is a significant challenge for HCPs but is beyond the scope of this review.
LITERATURE SEARCH
A narrative literature search was conducted on November 16, 2020. Search terms related to race (African American OR Black* OR racial OR ethnic), obesity (obese OR obesity OR overweight), and topics of interest (prevalence OR etiology OR barrier* OR disparit* OR comorbidit* OR risk*).
The Medline database was searched using a combination of these key words, with results limited to 2010 to 2020 and English language. The articles were reviewed for relevance based on title and abstract.
Additional references were identified from bibliographies of retrieved articles, through additional targeted searches, and through author suggestions.
DISCUSSION
Burden of obesity in African American people
Among US adults in the National Health and Nutrition Survey (NHANES) 2017‐2018, the prevalences of overweight (body mass index [BMI] 25.0‐29.9 kg/m2), obesity (BMI ≥30.0 kg/m2), and severe obesity (BMI ≥40.0 kg/m2) were estimated to be 31%, 42%, and 9%, respectively [3]. Obesity disproportionately affects African American people. Among individuals aged ≥20 years in 2017‐2018, prevalence rates for obesity were highest in African American people (49.6%) compared with other racial groups (e.g., non‐Hispanic White, 42.2%), and rates were higher in African American women (56.9%) than in African American men (41.1%) [1]. Increased obesity prevalence between the African American population and other racial groups was observed for women but not for men, with African American men having slightly lower levels of obesity than non‐Hispanic White men (41.1% vs. 44.7%) [1]. Although reasons for this sex difference are not fully understood, it may be a result of the greater scope that women have to experience weight gain during their life course relative to men (for example, during pregnancy, menarche, and menopause), combined with cultural perspectives on ideal body size [4]. African American women report less internalized weight bias than White women [5] and acceptance of larger body size [4]. In addition, there is evidence that the association between structural racism and increased BMI among African American people is stronger for women than men [6]. Further research on this topic is needed, but it is of interest to note that the trend for African American women to be more likely to experience obesity is not a recent phenomenon. A study of adults born in the United States between 1882 and 1986 evaluated changes in BMI measurements between 1959 and 2006 by sex and race and found that increases in BMI were already under way among the birth cohorts of the early 20th century, with the rate of increase fastest among African American women [7].
One consideration for the cause of the current disparity in obesity prevalence by self‐identified race is that race is only a proxy for social class, as there is typically a lower prevalence of obesity in groups with higher income or educational attainment [8]. However, among women, racial disparities in the prevalence of obesity exist among groups with a higher education level and/or income, suggesting that race has an independent association with weight status. African American women have a higher BMI compared with White women at every level of educational attainment, with the greatest disparity in those with more than a high school education [9]. For African American people, the obesity–income relationship varies by sex. Among African American women, the prevalence of obesity does not differ by income group [10]. However, among African American men, the prevalence of obesity is higher among the highest income group compared with the lowest income group [10].
Obesity increases the risk for complications, including cardiovascular disease, type 2 diabetes, and nonalcoholic fatty liver disease [11]. The prevalence of several complications, including hypertension [12, 13], diabetes [12, 13], and stroke [13], is higher in African American people compared with White people; however, African American people have lower prevalence than White people for dyslipidemia [12, 13] and myocardial infarction [13]. A significant risk reduction in many obesity‐associated conditions can be achieved by weight loss of 5% to ≥15% [11].
Pathophysiology of obesity
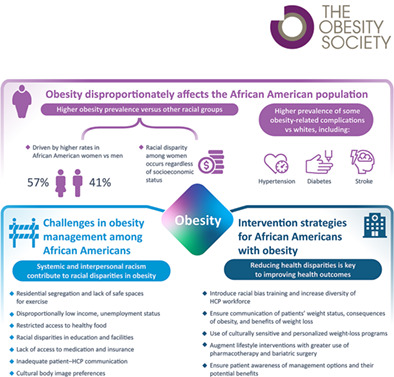
Obesity is a serious, chronic, complex, progressive, and relapsing disease associated with altered quantity, distribution, or function of adipose tissue (Figure 1) [14, 15], and it is caused by the interplay of genetic, physiologic, behavioral, sociocultural, and environmental factors [15]. The pathogenesis of obesity involves abnormal satiety and feeding signaling within the brain through dysregulation of neuroendocrine pathways [16].
FIGURE 1.
Obesity is a chronic disease characterized by altered distribution and metabolism of the adipose tissue. Multiple environmental, genetic, and physiologic factors determine the distribution and metabolism of the adipose tissue. Adiposity can manifest as atherosclerosis or visceral adiposity, which affects a range of organs, leading to complications, including CVD and T2D. In contrast, subcutaneous adiposity has a lesser impact on disease. Adiposity collectively negatively affects quality of life, clinical outcomes, risk factors for disease, and prognosis. CKD, chronic kidney disease; CVD, cardiovascular disease; NAFLD, nonalcoholic fatty liver disease; T2D, type 2 diabetes. aFor example, socioeconomic factors and lack of access to healthy food, physical exercise, and health care
Obesity management should be founded on evidence‐based principles [17]. Less emphasis should be placed on short‐term, absolute weight loss and individuals' willpower (e.g., “eat less, move more”) and more on overall health and well‐being, with access to multiple interventions such as nutritional therapy, physical activity, psychological interventions, pharmacotherapy, and surgery [17].
There are racial differences in physiology with relevance to obesity management. African American people store a lower proportion of fat in visceral tissue than White people [18]. In addition, for a given BMI, African American people have a higher lean body mass than White or Hispanic people [19]. This may help to explain findings that BMI is not always directly correlated with mortality in African American populations [18], supporting the need to adjust BMI cutoffs for use in different racial populations [20].
Challenges in managing obesity in African American people
Several challenges exist in the management of obesity among African American people, including racism, access to healthy food, safe spaces for exercise, health care, and body image preferences.
Historical context and structural racism
African American people have historically experienced worse health outcomes than White people in the United States [1]. However, it is important to note that race is a social construct rather than a fixed biological trait [21], and health inequities must be considered in this light.
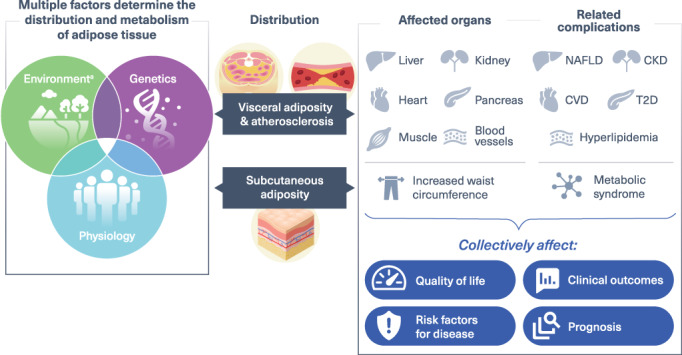
Many of the disparities in health outcomes seen in African American people can be attributed to systemic and interpersonal racism. Systemic or structural racism refers to “the totality of ways in which societies foster [racial] discrimination, via mutually reinforcing [inequitable] systems…(e.g., in housing, education, employment, earnings, benefits, credit, media, health care, criminal justice, etc.) that in turn reinforce discriminatory beliefs, values, and distribution of resources” (Figure 2) [1].
FIGURE 2.
The racial discrimination system and its impact on obesity in African American people. Racial disparities exist within a wide range of systems in the United States, including housing, public health, education, employment, and food access. These disparities are connected through a complex web of reciprocal feedback relationships that give rise to a self‐perpetuating system of racial discrimination. Racial disparities in these systems also impact the risk of obesity and related behaviors among African American people [8, 26, 27, 47, 48, 52, 53, 54, 55, 56, 57, 90, 91].
There is evidence to suggest that long‐standing systemic inequalities and structural racism play a role in driving race disparities in obesity [22]. A study of 324,572 US adults reported that structural racism (assessed at a county level using a model that included domains for residential segregation, employment, education, health care, and criminal justice) was associated with higher BMI in African American people [6]. A prospective study of 4315 incident cases of obesity in African American women also found that both everyday racism and lifetime racism were positively associated with increased incidence of obesity [23]. In addition, a longitudinal prospective cohort study reported an association between higher perceived discrimination and a positive BMI trajectory in African American adults [24].
One conduit through which structural racism makes a major contribution to racial inequities in health between African American people and White people is by driving social circumstance [21, 25]. For example, residential segregation remains common, concentrating African American people in neighborhoods that lack access to adequate education and health care, have increased exposure to air pollutants, and have increased rates of crime [1, 26]. Residential segregation is also associated with an increased risk of obesity specifically among African American women [27]. Furthermore, access to health care is based on ability to pay, rather than on patient needs, causing harm to racial and ethnic minorities, who are disproportionately poor and lack access to health insurance [28, 29]. HCPs should therefore consider the social determinants of health (such as housing, employment, and health care access) that may influence their patients' behaviors and opportunities for health, in order to provide the most appropriate care.
The impact of racism on health outcomes is rooted in a history of unethical experimentation on African American people for medical research and training and segregation of care based on race. One of the most infamous medical experiments was the Tuskegee Study, led by the US government from 1932, which investigated the natural history of syphilis in 600 African American men [30]. The participants were misled as to the purpose of the study and were denied effective treatment, long after penicillin was recognized as the drug of choice for syphilis [30]. The study was ultimately deemed ethically unjustified and was discontinued in 1972.
Another example of federally endorsed inequity in health care is the passage of the Hill–Burton Act in 1946, which created “separate‐but‐equal” health care facilities financed by the US government throughout the country [22]. These facilities were anything but equal, with those for African American people often lacking the resources and equipment of those for White people [22].
This sanctioned segregation of health care resources, combined with a distrust of medical professionals given the experiences of the Tuskegee Study and decades of non‐consented experimentation and medical exploitation, has had long‐lasting effects, with African American people less likely than White people to participate in research and trust the health care system and medical researchers [31, 32].
Interpersonal racism
Individual or interpersonal racism is defined as “directly perceived discriminatory interactions between individuals whether in their institutional roles (…) or as public and private individuals” [33]. Interpersonal racism can be conscious or unconscious, and can manifest in health care via unconscious bias of HCPs [34].
Interpersonal racism between individuals may affect the disparities in obesity rates, as major discrimination (e.g., being unfairly treated/abused by police), overt racial discrimination (e.g., use of racial slurs), and microaggressions (subtle messaging that conveys hostility or exclusion) are associated with obesity among African American people [35, 36]. The association between racism and obesity appears to be in part mediated by stress [37] and through negative behavioral responses such as decreased exercise and increased emotional eating [38, 39].
Increasing the potential for bias among African American people with obesity is the interaction between racism and the stigma of obesity [40]. African American people with obesity are at the intersection of these two types of discrimination and may therefore experience an even greater amount of bias.
Therefore, structural and interpersonal racism impacts health outcomes; however, this is not routinely taught to medical students or covered widely in medical literature [1]. Although the physical links between discrimination and health are understood, this has not translated into educating HCPs about the impact of racism on health. To reduce the health disparities in African American people with obesity, HCPs must understand how structural and interpersonal racism contribute to these disparities and take an active role in addressing the root causes.
Patient–HCP communication
Unconscious or implicit bias is a form of interpersonal racism. Scientific data have demonstrated that HCPs have implicit bias against African American people and people with obesity, and this can affect clinical decision‐making [41].
Although some communication challenges around behaviors and behavior modification are not specific to African American people, suboptimal communication and a lack of shared decision‐making may exist between non‐African American HCPs and African American people. This may lead to poor patient engagement, an important issue in obesity management.
According to patients' reports of their HCPs' behavior, African American people, particularly those with obesity, were less likely to report that their providers explained things well or spent enough time with them, compared with White people [42]. African American people with BMI ≥30.0 kg/m2 were also less likely to receive an obesity diagnosis compared with White people [43]. People with obesity with a provider of the same race/ethnicity were more likely to report receiving diet advice from their provider than those with differing race/ethnicity [44].
The way in which HCPs communicate about obesity and its management influences how patients relate to the messages, potentially affecting weight management success [45].
Access to healthy foods and exercise
Environmental challenges, such as poor‐quality diet, availability of healthy foods, and inactivity, are universal, but there is some evidence that they may be more challenging for African American people. Studies have shown that African American people have a less healthy diet than other racial groups, with a higher consumption of foods and beverages with added sugar and fried food [46]. Several barriers have been identified that limit healthy eating, including lack of knowledge, cost of healthy food, lack of time to prepare healthy meals, need for transportation to access stores and markets, and miscommunication with doctors about healthy eating [47, 48].
African American people aged 45 to 64 years are also less likely to engage in physical activity than other racial groups [49]. Barriers to physical activity among African American women with obesity include lack of awareness of how, where, and how much to exercise, cost of exercise programs, lack of accessible facilities, lack of transportation, and health concerns [50]. However, several factors are associated with increased exercise or motivation for exercise among African American people, including family interaction and connection to the community [51].
Neighborhood factors also contribute to challenges in accessing healthy food and exercise in African American people. Neighborhoods with higher proportions of African American people have higher densities of fast‐food restaurants and advertisements related to unhealthy food and beverages, and fewer safe spaces for activity than predominantly White neighborhoods [52, 53]. Neighborhood factors have been shown to impact obesity prevalence, with lower odds of obesity among African American women living in a neighborhood with a supermarket and among African American men living in a neighborhood with a park [54].
Health insurance and access to medication
Health insurance coverage is often a challenge for people with obesity. Among a sample of urban residents, the prevalence of obesity had grown rapidly over 10 years among uninsured people across racial groups [55].
Safety‐net health systems, in delivering care to under‐ or uninsured, publicly insured, and other vulnerable populations in the United States, generally support a relatively high proportion of African American people [56]. However, few health insurance plans include coverage for comprehensive obesity care, including access to obesity pharmacotherapy; Medicare excludes drug therapy for obesity while Medicaid drug coverage varies by state [57]. In addition, older medications for obesity‐related complications (particularly type 2 diabetes) tend to be more obesogenic than newer alternatives [58] and are often cheaper and therefore likely to have better reimbursement.
Body image perceptions
There are also different perspectives on cultural norms for body image and perceptions of beauty and obesity among African American people.
African American people have a more accepting view of larger body sizes than White people [4]. Being curvier is often seen as desirable, with many women striving for a fuller figure [47]. Many African American women have misconceptions of normal weight, describing their weight as healthy despite being overweight by BMI [59] and underestimating or under‐reporting their weight category [60]. However, due to this acceptance of larger body sizes, it may be easier to set realistic treatment goals, as African American people may not desire the ideal of achieving a normal BMI, which is rarely achieved with treatment.
Strategies for managing obesity in African American people
A holistic approach incorporating multiple strategies is needed to support the management of obesity in African American people.
Addressing health disparities and racial bias
Reducing health disparities among African American people is key to improving health outcomes. The US Office of Minority Health's Strategic Framework for Improving Racial/Ethnic Minority Health and Eliminating Racial/Ethnic Health Disparities includes effective solutions to reduce health disparities [61]. These include strategies to address factors on an individual (e.g., improving knowledge and behaviors), environmental (e.g., promoting a healthy physical and social environment), or systems level (e.g., improving science and knowledge, and promoting workforce diversity) [61]. A review examining whether obesity is a manifestation of systemic racism proposed a 10‐point strategy for study and intervention which highlighted the importance of conducting intersectional research on obesity and racism to evaluate whether obesity is another aspect of structural racism that impacts African American people [62].
Addressing implicit racial bias could also reduce health disparities between African American and non‐African American people. In a prospective, observational study, including implicit racial bias training as part of the formal curriculum at medical school reduced students' racial bias over 4 years [63]. Informal training also has the potential to reduce racial bias. One such initiative is the 21‐Day Racial Equity Habit Building Challenge, which supports HCPs to further their understanding of racial inequities, including addressing unconscious bias [64].
Increasing the diversity of the HCP workforce is also key to addressing racial inequities in health care. Efforts are ongoing among professional medical societies (the American Medical Association), medical schools (the Association of American Medical Colleges), and colleges and universities (Historically Black Colleges and Universities) to increase HCP and researcher diversity [65, 66, 67].
Diagnosis and communication
Ensuring African American people receive a diagnosis of obesity is also key to weight management, particularly given the perceptions related to acceptance of a larger body size in this population [4, 47, 59]. People with overweight or obesity who are told by HCPs that they have overweight are more likely to perceive themselves as having overweight, be interested in losing weight, and have recently attempted to lose weight than those whose HCPs have not acknowledged they have overweight [43]. For many, having this discussion with a provider might be the first time they get a full sense of the impact of excess weight.
When communicating with patients, a diagnosis of obesity should be linked to disease risk, as smaller body size may not be such a motivating factor for African American people as in other racial groups. Among African American people with obesity, health is considered the most important reason to lose weight [68]. However, as many African American people do not recognize the health implications of obesity [59], this must be emphasized when communicating with patients. Focusing on the potential benefits may be an effective motivator for weight loss for African American people [45]. HCPs should also set specific weight goals with patients, as many are unaware of the degree of weight loss required (e.g., sustained weight loss of 5% to 10%) to significantly improve health [11, 45].
Culturally relevant intervention strategies
Health interventions to reduce obesity among African American people should be personalized and culturally specific, with aims that include engaging with and, when necessary, challenging cultural norms.
A systematic review of culturally adapted weight‐loss strategies for African American people identified a number of features common to studies with successful outcomes [69]. These included addressing traditional foods, food insecurity, and spirituality and faith, as well as conducting focus groups and using peer educators [69]. In one successful weight‐loss program for African American people, cultural adaptations included decreasing the cost of the program, using culturally appropriate recipes, addressing attitudes about exercise, and including family in weight‐loss efforts [70]. This program was associated with significant weight loss and improvements in risk factors for obesity‐related complications [70].
Physical activity should also be encouraged as part of weight management for African American people with obesity; however, this too should be culturally sensitive. The type of exercise suggested is important as, for example, swimming may not generally be part of African American people's leisure, exercise, and sports culture, because of past discrimination restricting access to swimming pools [71].
Community‐ and faith‐based initiatives can be successful in managing obesity among African American people [72, 73]. Faith‐based weight‐loss interventions in African American people have been shown to successfully reduce weight, improve diet, and increase physical activity among participants [73]. The inclusion of family and social ties has also been a feature of successful weight‐loss interventions in African American people [70]. However, friends and family may not always be supportive of weight loss, with some African American women reporting relationships becoming more competitive and less supportive, and a loss of identity and companionship that accompanied weight loss [74].
Pharmacological and surgical intervention
Pharmacotherapy, particularly when used alongside lifestyle interventions, can be effective for people with obesity. US Food and Drug Administration‐approved therapies include liraglutide, orlistat, phentermine, phentermine‐topiramate, bupropion‐naltrexone, and most recently, semaglutide.
In a phase 3 study in which 19% of participants were African American, phentermine‐topiramate demonstrated significant efficacy in inducing weight loss [75]. Although data comparing weight loss between racial and ethnic groups are limited, racial differences were not seen to influence the safety or efficacy of semaglutide, liraglutide, or orlistat in studies on obesity that included African American people [76, 77, 78, 79].
Bariatric procedures are also useful tools for the management of obesity, with significant and sustained weight loss and resolution of obesity‐related complications reported regardless of race [80]. However, racial disparities exist in the utilization and outcomes of bariatric surgery. A review of 159,116 records representing 774,000 patients with severe obesity taken from the 2006 Nationwide Inpatient Sample Hospital Discharge Dataset found the demographic features associated with significantly lower odds of receiving bariatric surgery included minority status, male sex, lower income, older age, non‐private insurance status, and more severe comorbidities [81]. In addition, African American people are less likely than White people to consider bariatric surgery and less likely to receive the recommendation for surgery from their doctor [82]. It has been reported that although 11% of patients who were eligible for bariatric surgery were African American men, this group represented only 2.4% of patients who received surgery. African American people undergoing bariatric procedures are heavier and younger, are more likely to be women, and have fewer preoperative comorbidities [83]. They also have worse postoperative complications, with major complications (1.4% vs. 1.1%; p < 0.0001), readmission (5.0% vs. 3.6%; p < 0.0001), and mortality (0.12% vs. 0.08%; p < 0.05) all significantly higher for African American versus non‐African American people [83]. Higher odds of readmission and complications, including mortality rate, for African American people following bariatric surgery have been reported in other studies [84, 85, 86]. African American men are also more likely to require longer hospital stays following bariatric surgery compared with White men [84, 87], and to lose significantly less weight compared with White and Hispanic people [88].
Several barriers to antiobesity pharmacotherapy and bariatric surgery utilization exist among African American people. For pharmacotherapy, these include fear of side effects [89], whereas for bariatric surgery, these include the fear of complications, high cost of surgery, and the perception that it is too extreme and should be a last resort [74, 89]. African American women are also apprehensive about the lack of control over how much weight could be lost with bariatric surgery because of the preference for larger body sizes in this population [74]. Lack of awareness of pharmacotherapy and bariatric surgery is another barrier, as few HCPs have discussions with their patients about these options [89].
It is therefore critical that HCPs communicate the potential benefits of pharmacotherapy and bariatric surgery options with their patients and address concerns.
SUMMARY
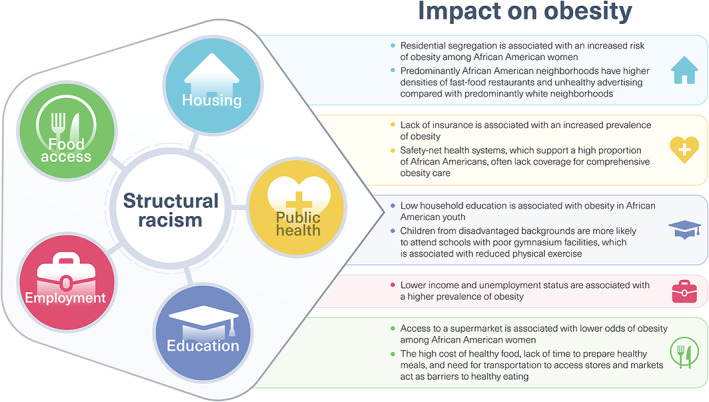
Long‐standing disparities in health and obesity care for African American people have been documented and systemic racism remains a major cause. Systemic racism limits access to healthy foods, safe spaces for exercise, health insurance, and treatment, while HCPs' unconscious racial bias can negatively impact interactions with patients.
Reducing health disparities is key to improving health outcomes (Figure 3). Racial bias can be reduced by racial bias training programs to support HCPs, furthering their understanding of racial inequities and unconscious bias. Efforts should also be made to increase the diversity of the HCP workforce. HCPs are encouraged to develop appropriate culturally sensitive practices when engaging with African American people with obesity. Furthermore, any weight‐loss interventions should be personalized and culturally relevant to African American people. Weight‐loss programs can include use of peer educators and community‐ and faith‐based programs. The response to lifestyle interventions can be augmented with greater use of antiobesity pharmacotherapy and bariatric surgery; these strategies are underutilized in general and even more so in African American people. It is therefore important that HCPs ensure awareness of pharmacotherapy and bariatric surgery options and their potential benefits among African American people.
FIGURE 3.
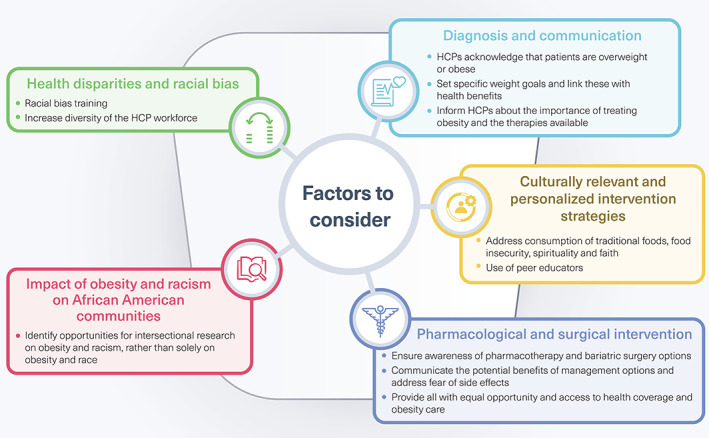
Recommendations for managing obesity in African American people [43, 45, 62, 63, 64, 65, 66, 67, 69, 89]. HCP, health care practitioner
AUTHOR CONTRIBUTIONS
All authors contributed to manuscript writing (assisted by a medical writer paid for by the funder) and approved the final version of the manuscript. All authors had final responsibility for the decision to submit for publication.
CONFLICT OF INTEREST
Holly Lofton has served as a consultant for Allergan, Amgen, Bausch Health Americas, Becton Dickinson & Co, Eisai, Eli Lilly and Company, Endo Pharmaceuticals, Ethicon, Nalpropion, Novo Nordisk, Shire North American Group, and Takeda Pharmaceuticals North America. Jamy D. Ard has served as a consultant for Eli Lilly and Company, Nestle Healthcare Nutrition, and Novo Nordisk and has received research funding from Eli Lilly and Company and Epitomee Medical. Rameck R. Hunt has served as a speaker for Novo Nordisk. Michael G. Knight has served as a consultant for Novo Nordisk.
ACKNOWLEDGMENTS
Medical writing and editorial support were provided by Rebecca Bridgewater‐Gill of Axis, a division of Spirit Medical Communications Group Limited, under the direction of the authors. Novo Nordisk Inc. performed a medical accuracy review.
Lofton H, Ard JD, Hunt RR, Knight MG. Obesity among African American people in the United States: A review. Obesity (Silver Spring). 2023;31(2):306‐315. doi: 10.1002/oby.23640
Funding information Novo Nordisk Inc., Plainsboro, New Jersey, USA
REFERENCES
- 1. Bailey ZD, Krieger N, Agénor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. Lancet. 2017;389:1453‐1463. [DOI] [PubMed] [Google Scholar]
- 2. Petersen R, Pan L, Blanck HM. Racial and ethnic disparities in adult obesity in the United States: CDC's tracking to inform state and local action. Prev Chronic Dis. 2019;16:E46. doi: 10.5888/pcd16.180579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Fryar CD, Carroll MD, Afful J. Prevalence of overweight, obesity, and severe obesity among adults aged 20 and over: United States, 1960–1962 through 2017–2018. National Center for Health Statistics Health E‐Stats. Updated January 29, 2021. Accessed July 2, 2021. https://www.cdc.gov/nchs/data/hestat/obesity-adult-17-18/obesity-adult.htm [Google Scholar]
- 4. Kronenfeld LW, Reba‐Harrelson L, Von Holle A, Reyes ML, Bulik CM. Ethnic and racial differences in body size perception and satisfaction. Body Image. 2010;7:131‐136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Himmelstein MS, Puhl RM, Quinn DM. Intersectionality: an understudied framework for addressing weight stigma. Am J Prev Med. 2017;53:421‐431. [DOI] [PubMed] [Google Scholar]
- 6. Dougherty GB, Golden SH, Gross AL, Colantuoni E, Dean LT. Measuring structural racism and its association with BMI. Am J Prev Med. 2020;59:530‐537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Komlos J, Brabec M. The trend of mean BMI values of US adults, birth cohorts 1882–1986 indicates that the obesity epidemic began earlier than hitherto thought. Am J Hum Biol. 2010;22:631‐638. [DOI] [PubMed] [Google Scholar]
- 8. Wong RJ, Chou C, Ahmed A. Long term trends and racial/ethnic disparities in the prevalence of obesity. J Community Health. 2014;39:1150‐1160. [DOI] [PubMed] [Google Scholar]
- 9. Jackson CL, Szklo M, Yeh HC, et al. Black‐white disparities in overweight and obesity trends by educational attainment in the United States, 1997–2008. J Obes. 2013;2013:140743. doi: 10.1155/2013/140743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ogden CL, Fakhouri TH, Carroll MD, et al. Prevalence of obesity among adults, by household income and education – United States, 2011–2014. MMWR Morb Mortal Wkly Rep. 2017;66:1369‐1373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Garvey WT, Mechanick JI, Brett EM, et al. American Association of Clinical Endocrinologists and American College of Endocrinology comprehensive clinical practice guidelines for medical care of patients with obesity. Endocr Pract. 2016;22:842‐884. [DOI] [PubMed] [Google Scholar]
- 12. Romero CX, Romero TE, Shlay JC, Ogden LG, Dabelea D. Changing trends in the prevalence and disparities of obesity and other cardiovascular disease risk factors in three racial/ethnic groups of USA adults. Adv Prev Med. 2012;2012:172423. doi: 10.1155/2012/172423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Zhang H, Rodriguez‐Monguio R. Racial disparities in the risk of developing obesity‐related diseases: a cross‐sectional study. Ethn Dis. 2012;22:308‐316. [PubMed] [Google Scholar]
- 14. Mechanick JI, Hurley DL, Garvey WT. Adiposity‐based chronic disease as a new diagnostic term: the American Association of Clinical Endocrinologists and American College of Endocrinology position statement. Endocr Pract. 2017;23:372‐378. [DOI] [PubMed] [Google Scholar]
- 15. Bray GA, Frühbeck G, Ryan DH, Wilding JP. Management of obesity. Lancet. 2016;387:1947‐1956. [DOI] [PubMed] [Google Scholar]
- 16. Carroll JF, Kaiser KA, Franks SF, Deere C, Caffrey JL. Influence of BMI and gender on postprandial hormone responses. Obesity (Silver Spring). 2007;15:2974‐2983. [DOI] [PubMed] [Google Scholar]
- 17. Wharton S, Lau DCW, Vallis M, et al. Obesity in adults: a clinical practice guideline. CMAJ. 2020;192:E875‐E891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Clark DO, Unroe KT, Xu H, Keith NR, Callahan CM, Tu W. Sex and race differences in the relationship between obesity and C‐reactive protein. Ethn Dis. 2016;26:197‐204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Rahman M, Berenson AB. Racial difference in lean mass distribution among reproductive‐aged women. Ethn Dis. 2010;20:346‐352. [PMC free article] [PubMed] [Google Scholar]
- 20. Stanford FC, Lee M, Hur C. Race, ethnicity, sex, and obesity: is it time to personalize the scale? Mayo Clin Proc. 2019;94:362‐363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Payne‐Sturges DC, Gee GC, Cory‐Slechta DA. Confronting racism in environmental health sciences: moving the science forward for eliminating racial inequities. Environ Health Perspect. 2021;129:55002. doi: 10.1289/EHP8186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Bleich SN, Ard JD. COVID‐19, obesity, and structural racism: understanding the past and identifying solutions for the future. Cell Metab. 2021;33:234‐241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Cozier YC, Yu J, Coogan PF, Bethea TN, Rosenberg L, Palmer JR. Racism, segregation, and risk of obesity in the Black Women's Health Study. Am J Epidemiol. 2014;179:875‐883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Miller HN, Perrin N, Thorpe RJ Jr, Evans MK, Zonderman AB, Allen J. The association between perceived discrimination and BMI trajectory: a prospective study of African American and white adults. Fam Community Health. 2022;45:206‐213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Gee GC, Ford CL. Structural racism and health inequities: old issues, new directions. Du Bois Rev. 2011;8:115‐132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Reskin B. The race discrimination system. Annu Rev Sociol. 2012;38:17‐35. [Google Scholar]
- 27. Pool LR, Carnethon MR, Goff DC Jr, Gordon‐Larsen P, Robinson WR, Kershaw KN. Longitudinal associations of neighborhood‐level racial residential segregation with obesity among blacks. Epidemiology. 2018;29:207‐214. [DOI] [PubMed] [Google Scholar]
- 28. Berchick ER, Hood E, Barnett JC . Health insurance coverage in the United States: 2017. Current Population Reports, P60‐264, Issued September 2018. Accessed July 2, 2021. https://www.census.gov/content/dam/Census/library/publications/2018/demo/p60‐264.pdf
- 29. US Census Bureau . Real median household income by race and Hispanic origin: 1967 to 2017. Current Population Survey, 1968 to 2018 Annual Social and Economic Supplements. Accessed July 2, 2021. https://www.census.gov/content/dam/Census/library/visualizations/2018/demo/p60-263/figure1.pdf
- 30. US Centers for Disease Control and Prevention . The Syphilis Study at Tuskegee timeline. Updated December 5, 2022. Accessed July 2, 2021. https://www.cdc.gov/tuskegee/timeline.htm
- 31. Shavers VL, Lynch CF, Burmeister LF. Knowledge of the Tuskegee study and its impact on the willingness to participate in medical research studies. J Natl Med Assoc. 2000;92:563‐572. [PMC free article] [PubMed] [Google Scholar]
- 32. Jaiswal J, Halkitis PN. Towards a more inclusive and dynamic understanding of medical mistrust informed by science. Behav Med. 2019;45:79‐85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Krieger N. Embodying inequality: a review of concepts, measures, and methods for studying health consequences of discrimination. Int J Health Serv. 1999;29:295‐352. [DOI] [PubMed] [Google Scholar]
- 34. James SA. The strangest of all encounters: racial and ethnic discrimination in US health care. Cad Saude Publica. 2017;33(suppl 1):e00104416. doi: 10.1590/0102-311X00104416 [DOI] [PubMed] [Google Scholar]
- 35. Thorpe RJ Jr, Parker LJ, Cobb RJ, Dillard F, Bowie J. Association between discrimination and obesity in African‐American men. Biodemography Soc Biol. 2017;63:253‐261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Manns‐James L, Anthony MK, Neal‐Barnett A. Racial discrimination, racial identity, and obesity in collegiate African American women. J Racial Ethn Health Disparities. 2021;8:1217‐1231. [DOI] [PubMed] [Google Scholar]
- 37. Stepanikova I, Baker EH, Simoni ZR, et al. The role of perceived discrimination in obesity among African Americans. Am J Prev Med. 2017;52(1S1):S77‐S85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Moore‐Greene GM, Gross SM, Silver KD, Perrino CS. Chronic stress and decreased physical exercise: impact on weight for African American women. Ethn Dis. 2012;22:185‐191. [PMC free article] [PubMed] [Google Scholar]
- 39. Longmire‐Avital B, McQueen C. Exploring a relationship between race‐related stress and emotional eating for collegiate Black American women. Women Health. 2019;59:240‐251. [DOI] [PubMed] [Google Scholar]
- 40. Sanders R. The color of fat: racializing obesity, recuperating whiteness, and reproducing injustice. Polit Groups Identities. 2019;7:287‐304. [Google Scholar]
- 41. FitzGerald C, Hurst S. Implicit bias in healthcare professionals: a systematic review. BMC Med Ethics. 2017;18:19. doi: 10.1186/s12910-017-0179-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Wong MS, Gudzune KA, Bleich SN. Provider communication quality: influence of patients' weight and race. Patient Educ Couns. 2015;98:492‐498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Post RE, Mainous AG 3rd, Gregorie SH, Knoll ME, Diaz VA, Saxena SK. The influence of physician acknowledgment of patients' weight status on patient perceptions of overweight and obesity in the United States. Arch Intern Med. 2011;171:316‐321. [DOI] [PubMed] [Google Scholar]
- 44. Yang HY, Chen HJ, Marsteller JA, Liang L, Shi L, Wang Y. Patient‐health care professional gender or race/ethnicity concordance and its association with weight‐related advice in the United States. Patient Educ Couns. 2016;99:271‐278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Ward SH, Gray AM, Paranjape A. African Americans' perceptions of physician attempts to address obesity in the primary care setting. J Gen Intern Med. 2009;24:579‐584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Emerson JS, Towns DR, Jones JL, Cain VA, Hull PC. Racial/ethnic and weight status differences in food preparation among WIC participants. J Health Care Poor Underserved. 2015;26:335‐344. [DOI] [PubMed] [Google Scholar]
- 47. McClelland ML, Weekes CV, Bazzi H, et al. Perception of obesity in African‐American and Arab‐American minority groups. J Racial Ethn Health Disparities. 2016;3:160‐167. [DOI] [PubMed] [Google Scholar]
- 48. Ziegahn L, Styne D, Askia J, Roberts T, Lewis ET, Edwards W. Strategies to prevent and reduce diabetes and obesity in Sacramento, California: the African American Leadership Coalition and University of California, Davis. Prev Chronic Dis. 2013;10:E187. doi: 10.5888/pcd10.130074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. August KJ, Sorkin DH. Racial/ethnic disparities in exercise and dietary behaviors of middle‐aged and older adults. J Gen Intern Med. 2011;26:245‐250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Rimmer JH, Hsieh K, Graham BC, Gerber BS, Gray‐Stanley JA. Barrier removal in increasing physical activity levels in obese African American women with disabilities. J Womens Health (Larchmt). 2010;19:1869‐1876. [DOI] [PubMed] [Google Scholar]
- 51. Wilkin HA, Katz VS, Ball‐Rokeach SJ, Hether HJ. Communication resources for obesity prevention among African American and Latino residents in an urban neighborhood. J Health Commun. 2015;20:710‐719. [DOI] [PubMed] [Google Scholar]
- 52. Block JP, Scribner RA, DeSalvo KB. Fast food, race/ethnicity, and income: a geographic analysis. Am J Prev Med. 2004;27:211‐217. [DOI] [PubMed] [Google Scholar]
- 53. Cassady DL, Liaw K, Miller LM. Disparities in obesity‐related outdoor advertising by neighborhood income and race. J Urban Health. 2015;92:835‐842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Barrington DS, James SA, Williams DR. Socioeconomic correlates of obesity in African‐American and Caribbean‐Black men and women. J Racial Ethn Health Disparities. 2021;8:422‐432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Rummo P, Kanchi R, Perlman S, Elbel B, Trinh‐Shevrin C, Thorpe L. Change in obesity prevalence among New York City adults: the NYC Health and Nutrition Examination Survey, 2004 and 2013–2014. J Urban Health. 2018;95:787‐799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Balasubramanian BA, Garcia MP, Corley DA, et al. Racial/ethnic differences in obesity and comorbidities between safety‐net‐ and non safety‐net integrated health systems. Medicine (Baltimore). 2017;96:e6326. doi: 10.1097/MD.0000000000006326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Gomez G, Stanford FC. US health policy and prescription drug coverage of FDA‐approved medications for the treatment of obesity. Int J Obes (Lond). 2018;42:495‐500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. May M, Schindler C, Engeli S. Modern pharmacological treatment of obese patients. Ther Adv Endocrinol Metab. 2020;11:2042018819897527. doi: 10.1177/2042018819897527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Pickett S, Peters RM. Beliefs about personal weight among African American women. Clin Nurs Res. 2017;26:191‐204. [DOI] [PubMed] [Google Scholar]
- 60. Moore SE, Harris C, Wimberly Y. Perception of weight and threat to health. J Natl Med Assoc. 2010;102:119‐124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. US Department of Health and Human Services Office of Minority Health . A strategic framework for improving racial/ethnic minority health and eliminating racial/ethnic health disparities. Published January 29, 2020. Accessed July 2, 2021. https://minorityhealth.hhs.gov/omh/content.aspx?lvl=1&lvlid=5&id=8842
- 62. Aaron DG, Stanford FC. Is obesity a manifestation of systemic racism? A ten‐point strategy for study and intervention. J Intern Med. 2021;290:416‐420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. van Ryn M, Hardeman R, Phelan SM, et al. Medical school experiences associated with change in implicit racial bias among 3547 students: a Medical Student CHANGES study report. J Gen Intern Med. 2015;30:1748‐1756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. America & Moore . 21‐Day Racial Equity Habit Building Challenge. Published 2014. Accessed April 1, 2021. https://www.eddiemoorejr.com/21daychallenge
- 65. New policy aimed at increasing diversity in physician workforce. News release. American Medical Association; June 12, 2019. Accessed July 2, 2021. https://www.ama-assn.org/press-center/press-releases/new-policy-aimed-increasing-diversity-physician-workforce
- 66. Beech BM, Norris KC, Thorpe RJ Jr, Heitman E, Bruce MA. Conversation cafés and conceptual framework formation for research training and mentoring of underrepresented faculty at Historically Black Colleges and Universities: Obesity Health Disparities (OHD) PRIDE program. Ethn Dis. 2020;30:83‐90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Association of American Medical Colleges . Equity, diversity, & inclusion. Accessed June 6, 2022. https://www.aamc.org/what-we-do/diversity-inclusion [DOI] [PubMed]
- 68. Befort CA, Thomas JL, Daley CM, Rhode PC, Ahluwalia JS. Perceptions and beliefs about body size, weight, and weight loss among obese African American women: a qualitative inquiry. Health Educ Behav. 2008;35:410‐426. [DOI] [PubMed] [Google Scholar]
- 69. Kong A, Tussing‐Humphreys LM, Odoms‐Young AM, Stolley MR, Fitzgibbon ML. Systematic review of behavioural interventions with culturally adapted strategies to improve diet and weight outcomes in African American women. Obes Rev. 2014;15:62‐92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Ard JD, Rosati R, Oddone EZ. Culturally‐sensitive weight loss program produces significant reduction in weight, blood pressure, and cholesterol in eight weeks. J Natl Med Assoc. 2000;92:515‐523. [PMC free article] [PubMed] [Google Scholar]
- 71. Wiltse J. The Black–White swimming disparity in America: a deadly legacy of swimming pool discrimination. J Sport Soc Issues. 2014;38:366‐389. [Google Scholar]
- 72. Mitchell NS, Polsky S. Innovative care delivery model to address obesity in older African‐American women: Senior Wellness Initiative and Take Off Pounds Sensibly Collaboration for Health (SWITCH). J Am Geriatr Soc. 2013;61:1971‐1975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Lancaster KJ, Carter‐Edwards L, Grilo S, Shen C, Schoenthaler AM. Obesity interventions in African American faith‐based organizations: a systematic review. Obes Rev. 2014;15:159‐176. [DOI] [PubMed] [Google Scholar]
- 74. Lynch CS, Chang JC, Ford AF, Ibrahim SA. Obese African‐American women's perspectives on weight loss and bariatric surgery. J Gen Intern Med. 2007;22:908‐914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Aronne LJ, Wadden TA, Peterson C, Winslow D, Odeh S, Gadde KM. Evaluation of phentermine and topiramate versus phentermine/topiramate extended‐release in obese adults. Obesity (Silver Spring). 2013;21:2163‐2171. [DOI] [PubMed] [Google Scholar]
- 76. Kushner RF, Garvey WT, Hesse D, et al. Once‐weekly subcutaneous semaglutide 2.4 mg reduces body weight in adults with overweight or obesity regardless of baseline characteristics (STEP 1) [abstract]. J Endocr Soc. 2021;5(suppl 1):A24. [Google Scholar]
- 77. Ard J, Cannon A, Lewis CE, et al. Efficacy and safety of liraglutide 3.0 mg for weight management are similar across races: subgroup analysis across the SCALE and phase II randomized trials. Diabetes Obes Metab. 2016;18:430‐435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Peterson GE, Pollom RD. Liraglutide in clinical practice: dosing, safety and efficacy. Int J Clin Pract Suppl. 2010;64:35‐43. [DOI] [PubMed] [Google Scholar]
- 79. Osei‐Assibey G, Adi Y, Kyrou I, Kumar S, Matyka K. Pharmacotherapy for overweight/obesity in ethnic minorities and White Caucasians: a systematic review and meta‐analysis. Diabetes Obes Metab. 2011;13:385‐393. [DOI] [PubMed] [Google Scholar]
- 80. Turner M, Vigneswaran Y, Dewey E, et al. Weight loss and co‐morbidity resolution between different races and ethnicities after gastric bypass. Surg Obes Relat Dis. 2019;15:1943‐1948. [DOI] [PubMed] [Google Scholar]
- 81. Wallace AE, Young‐Xu Y, Hartley D, Weeks WB. Racial, socioeconomic, and rural‐urban disparities in obesity‐related bariatric surgery. Obes Surg. 2010;20:1354‐1360. [DOI] [PubMed] [Google Scholar]
- 82. Wee CC, Huskey KW, Bolcic‐Jankovic D, Colten ME, Davis RB, Hamel M. Sex, race, and consideration of bariatric surgery among primary care patients with moderate to severe obesity. J Gen Intern Med. 2014;29:68‐75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Hui BY, Roberts A, Thompson KJ, et al. Outcomes of bariatric surgery in African Americans: an analysis of the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) data registry. Obes Surg. 2020;30:4275‐4285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Stone G, Samaan JS, Samakar K. Racial disparities in complications and mortality after bariatric surgery: a systematic review. Am J Surg. 2022;223:863‐878. [DOI] [PubMed] [Google Scholar]
- 85. Welsh LK, Luhrs AR, Davalos G, et al. Racial disparities in bariatric surgery complications and mortality using the MBSAQIP data registry. Obes Surg. 2020;30:3099‐3110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Nguyen GC, Patel AM. Racial disparities in mortality in patients undergoing bariatric surgery in the USA. Obes Surg. 2013;23:1508‐1514. [DOI] [PubMed] [Google Scholar]
- 87. Hoffman AB, Myneni AA, Orom H, Schwaitzberg SD, Noyes K. Disparity in access to bariatric surgery among African‐American men. Surg Endosc. 2020;34:2630‐2637. [DOI] [PubMed] [Google Scholar]
- 88. Samaan JS, Abboud Y, Yuan L, et al. Racial disparities in bariatric surgery postoperative weight loss and patient satisfaction. Am J Surg. 2022;223:969‐974. [DOI] [PubMed] [Google Scholar]
- 89. Huq S, Todkar S, Lahiri SW. Patient perspectives on obesity management: need for greater discussion of BMI and weight‐loss options beyond diet and exercise, especially in patients with diabetes. Endocr Pract. 2020;26:471‐483. [DOI] [PubMed] [Google Scholar]
- 90. Nelson DS, Gerras JM, McGlumphy KC, et al. Racial discrimination and low household education predict higher body mass index in African American youth. Child Obes. 2018;14:114‐121. [DOI] [PubMed] [Google Scholar]
- 91. Fernandes M, Sturm R. Facility provision in elementary schools: correlates with physical education, recess, and obesity. Prev Med. 2010;50(suppl 1):S30‐S35. [DOI] [PMC free article] [PubMed] [Google Scholar]


