Abstract
Amid incremental progress in establishing an enabling legal and policy environment for lesbian, gay, bisexual, transgender and queer-identified people, and people with intersex variations (LGBTQI+) in India, evidence gaps on LGBTQI+ health are of increasing concern. To that end, we conducted a scoping review to map and synthesize the current evidence base, identify research gaps, and provide recommendations for future research. We conducted a scoping review using the Joanna Briggs Institute methodology. We systematically searched 14 databases to identify peer-reviewed journal articles published in English language between January 1, 2010 and November 20, 2021, that reported empirical qualitative, quantitative or mixed methods data on LGBTQI+ people’s health in India. Out of 3,003 results in total, we identified 177 eligible articles; 62% used quantitative, 31% qualitative, and 7% mixed methods. The majority (55%) focused on gay and other men who have sex with men (MSM), 16% transgender women, and 14% both of these populations; 4% focused on lesbian and bisexual women, and 2% on transmasculine people. Overall, studies reported high prevalence of HIV and sexually transmitted infections; multilevel risk factors for HIV; high levels of mental health burden linked to stigma, discrimination, and violence victimization; and non-availability of gender-affirmative medical care in government hospitals. Few longitudinal studies and intervention studies were identified. Findings suggest that LGBTQI+ health research in India needs to move beyond the predominant focus on HIV, and gay men/MSM and transgender women, to include mental health and non-communicable diseases, and individuals across the LGBTQI+ spectrum. Future research should build on largely descriptive studies to include explanatory and intervention studies, beyond urban to rural sites, and examine healthcare and service needs among LGBTQI+ people across the life course. Increased Indian government funding for LGBTQI+ health research, including dedicated support and training for early career researchers, is crucial to building a comprehensive and sustainable evidence base to inform targeted health policies and programs moving forward.
Introduction
The right to the highest attainable standard of health is both universal and fundamental in international law [1]. This is enshrined in Article 12 [2] of the Convention on Social, Economic, and Cultural Rights and underlies United Nations Sustainable Development Goal 3 (SDG-3), which promises “Health for All” by 2030 and that “no one will be left behind.” This includes lesbian, gay, bisexual, transgender, queer identified, and people with intersex variations (LGBTQI+), who are entitled to the same standard of health as everyone else [3].
Despite the promise of the SDGs, evidence from across the globe suggests that LGBTQI+ health consistently lags behind that of the general public. Systematic and scoping reviews on health and healthcare access among LGBTQI+ people in high-income countries have shown that these populations continue to face disproportionate physical and mental health burdens in contrast to heterosexual populations [4–9]. For example, global reviews and large-scale studies have documented high levels of problematic alcohol use [10], sexualized drug use [11], mental health problems [4, 12], and high rates of HIV and other sexually transmitted infections (STIs) [13–15] among various LGBTQI+ subpopulations. Consistent with the minority stress model [16], many of these poor health outcomes are associated with societal stigma, discrimination, and violence, and systemic barriers in access to health services experienced by LGBTQI+ individuals [9, 17, 18].
Increasing recognition of health issues and disparities faced by LGBTQI+ people in the context of advances in LGBTQI+ rights movements globally have contributed to an evolving legal and policy environment that is becoming more supportive of LGBTQI+ rights, and more attuned to addressing LGBTQI+ health disparities and discrimination [19]. These advances in the recognition of LGBTQI+ rights have concomitantly contributed to increasing awareness of the need for research evidence to meaningfully implement this policy shift. Population-specific data are sorely needed to document gaps, disparities, and progress in LGBTQI+ health over time, as recognized by numerous bodies including the World Bank and UNDP; both have called for more attention and investment in research on LGBTQI+ health [20]. This trend is evident in India where the decriminalization of adult consensual same-sex relationships (2018) [21] and the enactment of the Transgender Persons Protection of Rights Act (2019) [22] have recently emerged in rapid succession. The latter act was designed, among other things, to support and promote the delivery of non-discriminatory and gender-affirmative health services to transgender people. Subsequently, India’s Ministry of Social Justice and Empowerment’s expert committee on issues related to transgender persons has called for research evidence to design interventions to improve the health of transgender people [23].
We are aware of no overview and thorough mapping of the evidence base on LGBTQI+ health in India. A few published reviews of LGBTQI+ health in India have focused on specific topics, such as HIV research among MSM or mental health issues among LGBTQI+ individuals [24–26]. To address the fragmented nature of current research knowledge, we conducted a scoping review to synthesize the evidence on LGBTQI+ health in India. The aim of this review was to characterize the breadth of published research on LGBTQI+ health in India and identify gaps in the evidence base, to provide recommendations for future research, and to synthesize existing evidence to inform health policies and interventions to advance LGBTQI+ health.
Methods
We used the scoping review framework initially proposed by Arksey and O’Malley [27] and advanced by the Joanna Briggs Institute [28]. The key steps involved: (1) identifying the research questions; (2) identifying relevant studies; (3) study selection using a pre-defined set of inclusion and exclusion criteria; (4) charting the data; and (5) collating, summarizing and reporting the results.
Research questions
The specific questions guiding this review were: (1) What are the peer-reviewed literature sources available on LGBTQI+ health in India?; (2) What health problems and conditions are reported among LGBTQI+ people?; and (3) What are the gaps in the available evidence on LGBTQI+ health in India? We conceptualized health problems and conditions broadly, including physical and mental health problems and conditions commonly addressed in the research with LGBTQI+ populations, such as HIV, depression, anxiety, and problematic alcohol use, as well as their social determinants, including stigma, discrimination, violence, and access to care.
Identifying studies from academic databases
As the first comprehensive review of a broad range of health research among LGBTQI+ people across the vast geography and population of India, we limited our search to academic peer-reviewed journal articles. A literature search was conducted using the following academic databases: Medline, Education Resources Information Centre (ERIC), Applied Social Sciences Index and Abstracts (ASSIA), Public Affairs Information Service Index (PAIS Index), Bibliography of Asian Studies, EconLit, Education Source, Social Work Abstracts, Sociological Abstracts, PsychInfo, LGBTLife, Gender Studies, HeinOnline, ProQuest Thesis, Worldwide Political Science Abstracts, and Child and Adolescent Development. Search strings previously validated for LGBT+ populations [29] were used for identifying relevant articles. Search strings were customized to account for the unique syntax of each database surveyed (see S1 Appendix). We added relevant Indian LGBTQI+ terminology, including indigenous sexual role-based identity terms, such as kothi (feminine same-sex attracted males, primarily receptive sexual role), panthi (masculine and insertive role) and double-decker (both insertive and receptive role). We also searched for indigenous trans identities, such as hijras, thirunangai, jogappas, mangalmukhi, jogti hijras, and shivshaktis; however, as hijras was the only Indian language term used for trans identity in the article titles and abstracts, we used English language terms, such as trans men, trans women, trans person, and transgender. To delimit the results geographically, we added the term “India*” to all search strings. The searches from each database were documented, duplicates were eliminated, and citations were imported to Covidence (Veritas Health Innovation, Melbourne) for abstract and full-text screening.
Study selection
Studies were selected according to pre-defined inclusion criteria. Studies must have been: 1) published between January 1, 2010 and November 20, 2021; conducted among LGBTQI+ people in India; 3) written in English; 4) peer reviewed; and 5) report primary data (qualitative, quantitative, or mixed methods). Two independent reviewers first screened the titles and abstracts for inclusion. In the case of discrepancies, a third reviewer was consulted to reach consensus. Full texts of potentially relevant articles were screened using a similar process. We selected the time frame to focus on recent articles relevant to current public health programs and policies in India, in order to identify extant research gaps and inform the future research agenda. Additionally, the third phase of India’s National AIDS Control Programme (NACP-III), launched in late 2009, explicitly addressed targeted HIV interventions for men who have sex with men and transgender women, which brought national attention to the health issues of sexual and gender minority populations.
Charting, collating and summarizing the results
The following data were extracted for analysis: year of publication, study location, sample size, study population, objectives, design, methodology (qualitative, quantitative or mixed methods) and key findings. We summarized the results using frequencies, and thematic analysis and synthesis [28]. Studies were grouped by key themes that emerged from the synthesis: prevalence of HIV and STIs, and risk factors; stigma, discrimination and violence, and health impact; access to health services; interventions to improve health outcomes among LGBTQI+ populations; new HIV prevention technologies and their acceptability; and under-represented LGBTQI+ populations.
Results
Study selection
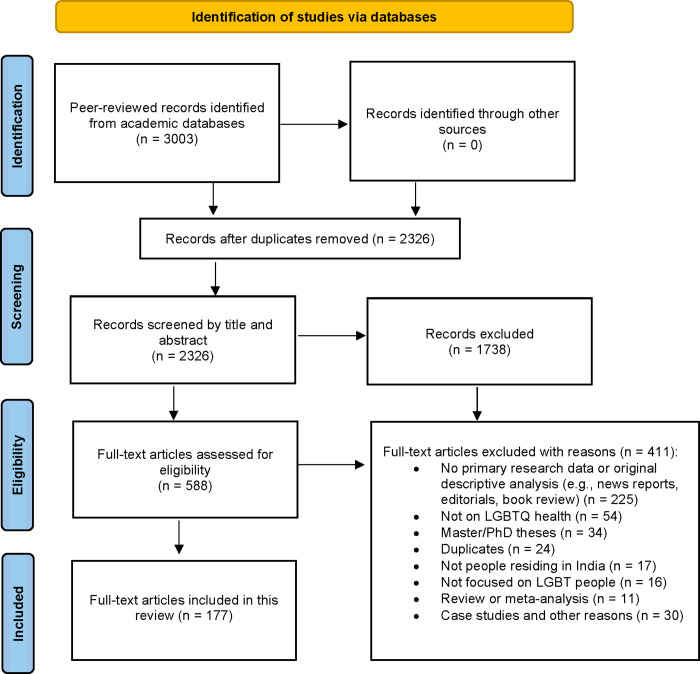
The search strategy yielded 2,326 sources after removing duplicates. Screening of the titles and abstracts yielded 588 articles included in full-text review. Of these, 177 peer-reviewed articles met the a priori eligibility criteria and were included in the scoping review (Fig 1). We extracted study characteristics and key findings for the included articles (Table 1).
Fig 1. PRISMA flowchart of study selection.
Table 1. Study characteristics and themes of inclusion (n = 177).
|
Author(s) |
Year |
N |
Focal Population(s) |
Methods | Themes | Main Funding Source | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Quantitative | Qualitative | Mixed | HIV/STI | Stigma/Discrimination | Access to Services | Interventionsa | New Prevention Tech | ||||||||||
| GBMSM | TGW | LBWSW | TGM | Ppl with intersex var. | Other |
||||||||||||
| Solomon et al. [30] | 2010 | 721 | X | X | X | Fogarty International Center, United States; NIHe, United States | |||||||||||
| Ghosh et al. [31] | 2011 | 32 | X | X | X | No funding information provided | |||||||||||
| Sahastrabuddhe et al. [32] | 2012 | 84 | X | X | X | ICMRf, India; NIAIDg United States; NIH | |||||||||||
| Ghosh et al. [33] | 2012 | 26 | X | X | X | NACOh, India | |||||||||||
| Solomon et al. [34] | 2015 | 12,022 | X | X | X | NIH; John Hopkins Centre for AIDS Research, United States | |||||||||||
| Mayer et al. [35] | 2015 | 307 | X | X | X | Indo-US grant | |||||||||||
| Hernandez et al. [36] | 2016 | 300 | X | X | X | Indo-US grant | |||||||||||
| Aggarwal et al. [37] | 2016 | 52 | X | X | X | No funding | |||||||||||
| Solomon et al. [38] | 2016 | 12,022 | X | X | X | NIH; Elton John AIDS Foundation | |||||||||||
| Raghavendran et al. [39] | 2017 | 300 | X | X | X | Indo-US grant | |||||||||||
| Hussain et al. [40] | 2018 | 277 | X | X | X | No funding information provided | |||||||||||
| Gupte et al. [41] | 2011 | 2,633 | X | X | X | X | Bill & Melinda Gates Foundation | ||||||||||
| Clipman et al. [42] | 2020 | 4,994 | X | X | X | NIH; John Hopkins Centre for AIDS Research, United States | |||||||||||
| Haldar et al. [43] | 2020 | 2,584 | X | X | X | No funding | |||||||||||
| Hernandez et al. [44] | 2021 | 302 | X | X | X | Indo-US grant | |||||||||||
| Palakkal et al. [45] | 2020 | 560 | X | X | X | No funding | |||||||||||
| Prabhu et al. [46] | 2021 | 1,639 | X | X | X | NIH; John Hopkins Centre for AIDS Research, United States; Elton John AIDS Foundation | |||||||||||
| Patel et al. [47] | 2021 | 20,002 | X | X | X | NIH; Elton John AIDS Foundation | |||||||||||
| Kumta et al. [48] | 2010 | 831 | X | X | X | Mumbai District AIDS Control Society, India | |||||||||||
| Phillips et al. [49] | 2010 | 357 | X | X | X | Bill & Melinda Gates Foundation | |||||||||||
| Solomon et al. [50] | 2010 | 781 | X | X | X | Indo-US grant | |||||||||||
| Setia et al. [51] | 2010 | 511 | X | X | X | CIHRi, Canada | |||||||||||
| Gutierrez et al. [52] | 2010 | 4,321 | X | X | X | Bill & Melinda Gates Foundation | |||||||||||
| Lorway et al. [53] | 2010 | 120 | X | X | X | CIHR | |||||||||||
| Mimiaga et al. [54] | 2011 | 210 | X | X | X | NIH; NIAID | |||||||||||
| Hendriksen et al. [55] | 2011 | 5 | X | X | X | NIAID | |||||||||||
| Hemmige et al. [56] | 2011 | 676 | X | X | X | American Foundation for AIDS Research; Centers for Disease Control and Prevention (CDC) Global AIDS Program (GAP), United States | |||||||||||
| Lorway et al. [57] | 2011 | -- | X | X | X | CIHR | |||||||||||
| Thomas et al. [58] | 2012 | 210 | X | X | X | NIH; NIAID | |||||||||||
| Tomori et al. [59] | 2018 | 47 | X | X | X | NIH; John Hopkins Centre for AIDS Research, United States | |||||||||||
| Wilkerson et al. [60] | 2018 | 433 | X | X | X | Indo-US grant | |||||||||||
| Srivastava et al. [61] | 2019 | 10 | X | X | X | Asian Network to Address Masculinities; The University Grants Commission, India | |||||||||||
| Mimiaga et al. [62] | 2013 | 150 | X | X | X | Fenway Institute, United States; NIH | |||||||||||
| Saggurti et al. [63] | 2013 | 2,399 | X | X | X | X | Bill & Melinda Gates Foundation | ||||||||||
| Chakrapani et al. [64] | 2013 | 88 | X | X | X | Department for International Development, United Kingdom | |||||||||||
| Ramanathan et al. [65] | 2013 | 1618 | X | X | X | Bill & Melinda Gates Foundation | |||||||||||
| Narayanan et al. [66] | 2013 | 483 | X | X | X | Bill & Melinda Gates Foundation | |||||||||||
| Kumar et al. [67] | 2014 | 3,229 | X | X | X | Bill & Melinda Gates Foundation | |||||||||||
| Yadav et al. [68] | 2014 | 3,880 | X | X | X | Bill & Melinda Gates Foundation | |||||||||||
| Ramesh et al. [69] | 2014 | 1,608 | X | X | X | Bill & Melinda Gates Foundation | |||||||||||
| Mitchell et al. [70] | 2014 | 595 | X | X | X | Wellcome Trust; Bill & Melinda Gates Foundation | |||||||||||
| Closson et al. [71] | 2014 | 32 | X | X | X | Indo-US grant | |||||||||||
| Ramanathan et al. [72] | 2014 | 1,305 | X | X | X | X | Bill & Melinda Gates Foundation | ||||||||||
| Godbole et al. [73] | 2014 | 4,682 | X | X | X | Department of AIDS Control, Ministry of Health and Family Welfare, Government of India | |||||||||||
| Mitchell et al. [74] | 2014 | 320 | X | X | X | Wellcome Trust; Bill & Melinda Gates Foundation | |||||||||||
| Saha et al. [75] | 2015 | 227 | X | X | X | NACO | |||||||||||
| Saha et al. [76] | 2015 | 243 | X | X | X | NACO | |||||||||||
| Ramakrishnan et al. [77] | 2015 | 3,833 | X | X | X | Bill & Melinda Gates Foundation | |||||||||||
| Mahapatra et al. [78] | 2015 | 1,237 | X | X | X | NACO | |||||||||||
| Shaw et al. [79] | 2016 | 456 | X | X | X | X | Bill & Melinda Gates Foundation | ||||||||||
| Tomori et al. [80] | 2016 | 12,151 | X | X | X | NIH; Johns Hopkins Center for AIDS Research, United States | |||||||||||
| Sinha et al. [81] | 2017 | 90 | X | X | X | No funding | |||||||||||
| Banik et al. [82] | 2019 | 72 | X | X | X | Indiana University, Bloomington, United States; National Institute on Drug Abuse, United States | |||||||||||
| Deshpande et al. [83] | 2015 | 689 | X | X | X | Bill & Melinda Gates Foundation | |||||||||||
| Chakrapani et al. [84] | 2015 | 151 | X | X | X | X | Department for International Development, United Kingdom | ||||||||||
| Dodge et al. [85] | 2016 | 72 | X | X | X | Indiana University, Bloomington, United States; NIH | |||||||||||
| Willie et al. [86] | 2017 | 299 | X | X | X | ICMR | |||||||||||
| Ferguson et al. [87] | 2016 | 30 | X | X | X | X | Yale University, United States | ||||||||||
| Banik et al. [88] | 2014 | 36 | X | X | X | NIH; Cleveland State University, United States | |||||||||||
| Wilkerson et al. [89] | 2019 | 449 | X | X | X | X | Indo-US grant | ||||||||||
| Bhambhani et al. [90] | 2021 | 4,321 | X | X | X | NIH | |||||||||||
| Sudharshan et al. [91] | 2020 | 33 | X | X | X | No funding | |||||||||||
| Safren et al. [92] | 2021 | 608 | X | X | X | NIH | |||||||||||
| Kumar et al. [93] | 2020 | 23,081 | X | X | X | NACO | |||||||||||
| Rajan et al. [94] | 2020 | 3,325 | X | X | X | No funding | |||||||||||
| Sivasubramanian et al. [95] | 2011 | 150 | X | X | X | Fenway Health, United States | |||||||||||
| Logie et al. [96] | 2012 | 200 | X | X | X | CIHR; SSHRCj; CIDAk | |||||||||||
| Shaw et al. [97] | 2012 | 543 | X | X | X | X | Bill & Melinda Gates Foundation | ||||||||||
| Tomori et al. [98] | 2018 | 484 | X | X | X | NIMHl; Johns Hopkins Center for AIDS Research, United States | |||||||||||
| Tomori et al. [99] | 2018 | 11,771 | X | X | X | NIH; Johns Hopkins Center for AIDS Research, United States | |||||||||||
| Thaker et al. [100] | 2018 | 225 | X | X | X | X | National University, Singapore | ||||||||||
| Chakrapani et al. [101] | 2019 | 300 | X | X | X | ICMR | |||||||||||
| Thompson et al. [102] | 2013 | 39 | X | X | X | CIHR | |||||||||||
| Elouard et al. [103] | 2013 | 11 | X | X | X | No funding information provided | |||||||||||
| Maroky et al. [104] | 2015 | 51 | X | X | X | No funding | |||||||||||
| Mimiaga et al. [105] | 2015 | 55 | X | X | X | Indo-US grant | |||||||||||
| Tomori et al. [106] | 2016 | 12,355 | X | X | X | NIH; Johns Hopkins Center for AIDS Research, United States | |||||||||||
| Tomori et al. [107] | 2016 | 363 | X | X | X | NIH; Johns Hopkins Center for AIDS Research, United States | |||||||||||
| Chakrapani et al. [108] | 2017 | 600 | X | X | X | X | ICMR | ||||||||||
| Ganju et al. [109] | 2016 | 68 | X | X | X | Bill & Melinda Gates Foundation | |||||||||||
| Chakrapani et al. [110] | 2017 | 600 | X | X | X | X | ICMR | ||||||||||
| Kalra et al. [111] | 2013 | 50 | X | X | X | No funding information provided | |||||||||||
| Lorway et al. [112] | 2013 | 70 | X | X | X | Bill & Melinda Gates Foundation | |||||||||||
| Manian [113] | 2014 | 10 | X | X | X | X | No funding | ||||||||||
| Chakrapani et al. [114] | 2017 | 300 | X | X | X | ICMR | |||||||||||
| Chakrapani et al. [115] | 2018 | 40 | X | X | X | Wellcome Trust / DBT India Alliance Senior Fellowship | |||||||||||
| Rao et al. [116] | 2018 | 227 | Xb | X | X | Psi Chi, the international honor society in psychology, United States |
|||||||||||
| Pandya [117] | 2010 | 250 | X | X | X | No funding information provided | |||||||||||
| Dutta et al. [118] | 2019 | 41 | X | X | X | CIHR; SSHRC | |||||||||||
| Bowling et al. [119] | 2019 | 58 | X | X | X | X | X | Bill & Melinda Gates Foundation | |||||||||
| Rao et al. [120] | 2020 | 170 | Xb | X | X | Psi Chi, the international honor society in psychology, United States |
|||||||||||
| Li et al. [121] | 2017 | 487 | X | X | X | X | Indo-US grant | ||||||||||
| Chavada et al. [122] | 2021 | 100 | X | X | X | No funding | |||||||||||
| Bhattacharya et al. [123] | 2020 | 98 | X | X | X | X | NIH; Department of Geography, University of Connecticut, United States | ||||||||||
| Dhabhar et al. [124] | 2020 | 112 | X | X | X | X | No funding | ||||||||||
| Banerjee et al. [125] | 2020 | 10 | X | X | X | No funding information provided | |||||||||||
| Azhar et al. [126] | 2021 | 16 | Xc | X | X | Minority Fellowship Program; University of Chicago Center for the Study of Gender and Sexuality, United States |
|||||||||||
| Srivastava et al. [127] | 2021 | 20 | X | X | X | No funding information provided | |||||||||||
| Prabhu et al. [128] | 2020 | 1,454 | X | X | X | NIH; Elton John AIDS Foundation | |||||||||||
| Arvind et al. [129] | 2021 | 20 | X | X | X | No funding information provided | |||||||||||
| Thirunavukkarasu et al. [130] | 2021 | 235 | X | X | X | No funding | |||||||||||
| Sharma et al. [131] | 2020 | 296 | X | X | X | X | X |
|
Department of Science and Technology, India; Indian Institute of Technology, Gandhinagar | ||||||||
| Dhaor [132] | 2021 | 21 | X | X | X | X | No funding | ||||||||||
| Safren et al. [133] | 2021 | 608 | X | X | X | National Institute of Mental Health, United States | |||||||||||
| Pufahl et al. [134] | 2021 | 184 | Xc | X | X | US Consulate, Mumbai, India | |||||||||||
| Majumder et al. [135] | 2020 | 37 | X | X | X | No funding | |||||||||||
| Joshi et al. [136] | 2021 | 33 | X | X | X | World Pranic Healing Foundation, India | |||||||||||
| Jesus et al. [137] | 2020 | 23 | X | X | X | Sanford School of Public Policy; Duke Global Health Institute, Duke University, United States |
|||||||||||
| Sharma et al. [138] | 2020 | 207 | X | X | X | No funding | |||||||||||
| Sartaj et al. [139] | 2021 | 50 | X | X | X | No funding | |||||||||||
| Srivastava et al. [140] | 2021 | 3,548 | X | X | X | X | No funding | ||||||||||
| Jethwani et al. [141] | 2014 | 124 | X | X | X | No funding | |||||||||||
| Singh et al. [142] | 2018 | 15 | X | X | X | No funding information provided | |||||||||||
| Mogasale et al. [143] | 2010 | -- | X | X | X | X | Bill & Melinda Gates Foundation | ||||||||||
| Chakrapani et al. [144] | 2011 | 38 | X | X | X | X | The International Treatment Preparedness Coalition (ITPC); European Union (EU)/The Humanist Institute for Development Cooperation (HIVOS) |
||||||||||
| Gurung et al. [145] | 2011 | 8,9621 | X | X | X | X | Bill & Melinda Gates Foundation | ||||||||||
| Woodford et al. [146] | 2012 | 132 | X | X | X | Canada Research Chairs Program; SSHRC | |||||||||||
| Beattie et al. [147] | 2012 | 90 | X | X | X | X | Bill & Melinda Gates Foundation | ||||||||||
| Pina et al. [148] | 2018 | 300 | X | X | X | X | The Global Health Scholarship from the Rosenbluth Fund, Einstein’s Global Health Center; NIH | ||||||||||
| Patel et al. [149] | 2018 | 4,179 | X | X | X | NIH | |||||||||||
| Samuel et al. [150] | 2018 | 212 | X | X | X | No funding information provided |
|||||||||||
| Ramesh et al. [151] | 2015 | 3,229 | X | X | X | Bill & Melinda Gates Foundation | |||||||||||
| Mehta et al. [152] | 2015 | 1,146 | X | X | X | NIH; Johns Hopkins University Center for AIDS Research, United States | |||||||||||
| McFall et al. [153] | 2016 | 503 | X | X | X | NIH; Johns Hopkins University Center for AIDS Research, United States | |||||||||||
| Singh et al. [154] | 2014 | 94 | X | X | X | Global Fund to Fight AIDS, Tuberculosis and Malaria | |||||||||||
| Woodford et al. [155] | 2016 | 47 | X | X | X | X | CIHR; Canada Research Chairs Program | ||||||||||
| Acharya et al. [156] | 2021 | 18 | X | X | X | X | No funding | ||||||||||
| Pandya et al. [157] | 2021 | 12 | X | X | X | No funding information provided | |||||||||||
| Pollard et al. [158] | 2021 | 28 | X | X | X | X | U.S. President’s Emergency Plan for AIDS Relief (PEPFAR); USAIDm | ||||||||||
| Achuthan et al. [159] | 2021 | 51 | Xd | X | X | Ford Foundation | |||||||||||
| Kulkarni et al. [160] | 2021 | 6 | X | X | X | No funding | |||||||||||
| Kurian et al. [161] | 2021 | 40 | X | X | X | No funding | |||||||||||
| Ghosh et al. [162] | 2020 | 22 | X | X | X | NACO | |||||||||||
| Tom et al. [163] | 2021 | 22 | X | X | X | No funding information provided | |||||||||||
| Ranade et al [164] | 2013 | 25 | Xd | X | X | No funding information provided | |||||||||||
| Snyder et al. [165] | 2012 | 298 | X | X | X | American Foundation for AIDS Research (amFAR); NIH |
|||||||||||
| Thomas et al. [166] | 2012 | 55 | X | X | X | Indo-US grant | |||||||||||
| Safren et al. [167] | 2014 | 96 | X | X | X | Indo-US grant | |||||||||||
| Shaikh et al. [168] | 2016 | 268 | X | X | X | Global Fund to Fight AIDS, Tuberculosis, and Malaria | |||||||||||
| Solomon et al. [169] | 2016 | 10,000 | X | X | X | NIH; Elton John AIDS Foundation | |||||||||||
| Thomas et al. [170] | 2017 | 75 | X | Xc | X | Indo-US grant | |||||||||||
| Mimiaga et al. [171] | 2017 | 100 | X | X | X | Indo-US grant | |||||||||||
| Roy et al. [172] | 2015 | 16 | X | X | X | No funding information provided | |||||||||||
| Chakrapani et al. [173] | 2020 | 119 | X | X | X | ICMR | |||||||||||
| Chakrapani et al. [174] | 2020 | 459 | X | X | X | Postgraduate Institute of Medical Education and Research (PGIMER), India | |||||||||||
| Patel et al. [175] | 2020 | 244 | X | X | X | NIH | |||||||||||
| Eisingerich et al. [176] | 2012 | 128 | X | X | X | Bill & Melinda Gates foundation | |||||||||||
| Uthappa et al. [177] | 2018 | 400 | X | X | X | X | ICHHA foundation, India | ||||||||||
| Chakrapani et al. [178] | 2012 | 82 | X | X | X | CIHR; SSHRC; Canada Research Chairs program | |||||||||||
| Chakrapani et al. [179] | 2013 | 82 | X | X | X | CIHR; Canada Research Chairs program; Canada Foundation for Innovation | |||||||||||
| Newman et al. [180] | 2014 | 400 | X | X | X | CIHR; Canada Research Chairs program; Canada Foundation for Innovation | |||||||||||
| McClarty et al. [181] | 2015 | 379 | Xd | X | X | CIHR; Canadian HIV Vaccine Initiative | |||||||||||
| Chakrapani et al. [182] | 2015 | 71 | X | X | X | CIHR; Canada Research Chairs Program | |||||||||||
| Ramanaik et al. [183] | 2015 | 50 | Xd | X | X | The International Infectious Disease and Global Health Training Program, University of Manitoba, Canada; CIHR |
|||||||||||
| Mitchell et al. [184] | 2016 | -- | X | X | X | Bill & Melinda Gates Foundation; NIH | |||||||||||
| Chakrapani et al. [185] | 2017 | 71 | X | X | X | CIHR | |||||||||||
| Schneider et al. [186] | 2012 | 387 | X | X | X | American Foundation for AIDS Research; NIH | |||||||||||
| Chakrapani et al. [187] | 2020 | 44 | X | X | X | CIHR; Canada Research Chairs Program | |||||||||||
| Chakrapani et al. [188] | 2021 | 197 | X | X | X | CIHR; Canada Foundation for Innovation | |||||||||||
| Belludi et al. [189] | 2021 | 8,621 | X | X | X | National Institute on Drug Abuse, United States; NIMH | |||||||||||
| Chakrapani et al. [190] | 2021 | 197 | X | X | X | CIHR | |||||||||||
| Rao et al. [191] | 2020 | 56 | X | X | X | X | World Health Organization | ||||||||||
| Kazemian et al. [192] | 2020 | -- | X | X | X | NIH; Harvard University Center for AIDS Research, United States | |||||||||||
| Chakrapani et al. [193] | 2021 | 360 | X | X | X | ViiV Health Care | |||||||||||
| Bowling et al. [194] | 2018 | 67 | X | X | Indiana University’s School of Public Health, Bloomington, United States | ||||||||||||
| Apoorva et al. [195] | 2016 | 8 | X | X | No funding information provided | ||||||||||||
| Chithrangathan [196] | 2018 | 1 | X | X | No funding information provided | ||||||||||||
| Banerjea [197] | 2015 | 8 | X | X | No funding information provided | ||||||||||||
| Bowling et al. [198] | 2016 | 20 | X | X | Indiana University’s School of Public Health, Bloomington, United States | ||||||||||||
| Bowling et al. [199] | 2018 | 18 | X | X | Indiana University’s School of Public Health, Bloomington, United States | ||||||||||||
| Srivastava [200] | 2020 | 25 | X | X | Indian University Grant Commission Doctoral Fellowship |
||||||||||||
| Bowling et al. [201] | 2019 | 58 | X | X | X | X | Bill & Melinda Gates Foundation | ||||||||||
| Bowling et al. [202] | 2019 | 33 | X | X | X | X | Bill & Melinda Gates Foundation | ||||||||||
| Chakrapani et al. [203] | 2021 | 27 | X | X | DBT/Wellcome Trust India Alliance Senior Fellowship | ||||||||||||
| Majumder et al. [204] | 2021 | 120 | X | X | X | No funding | |||||||||||
| Das [205] | 2020 | 29 | X | X | No funding information provided | ||||||||||||
| Joseph et al. [206] | 2017 | 205 | X | X | No funding information provided | ||||||||||||
Note: Terminologies for focal populations are derived from original sources, with indigenous sexual and gender identities in italics. GBMSM = Gay, bisexual and other men who have sex with men; TGW = Transgender women; LBWSW = Lesbian, bisexual, and other women who have sex with women; TGM = Transgender men; Ppl with intersex var. = People with intersex variations.
aInterventions to improve health outcomes
bSexual gender minority
cGender non-confirming
dHealth service providers
eNational Institute of Health (NIH), United States
fIndian Council of Medical Research (ICMR), India
gNational Institute of Allergy and Infectious Diseases (NIAID), United States
hNational AIDS Control Organization (NACO), India
iCanadian Institutes of Health Research (CIHR), Canada
jSocial Sciences and Humanities Research Council (SSHRC), Canada
kCanadian International Development Agency (CIDA), Canada
lNational Institute of Mental Health (NIMH), United States
mUnited States Agency for International Development, United States
Study characteristics
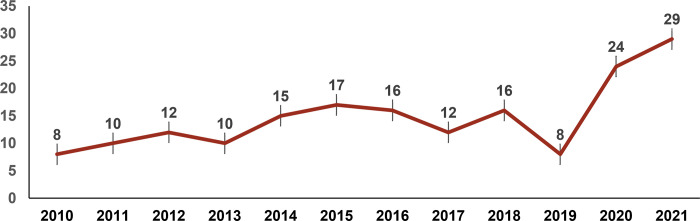
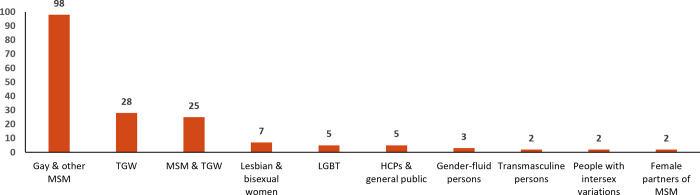
Of the 177 articles, the majority (59%; n = 105) were published from 2016 onward (Fig 2). In terms of methodology, 62% were quantitative, 31% qualitative, and 7% mixed methods studies. A majority (55%; n = 98) of studies were conducted among MSM, 16% (n = 28) among TGW, and 14% (n = 25) among both MSM and TGW (Fig 3). Seven studies (4%) were conducted among lesbian or bisexual women, five (3%) among LGBTQI+ people as a whole, and two each among transmasculine people, and people with intersex variations.
Fig 2. Distribution of peer-reviewed articles by year of publication (N = 177).
Fig 3. Distribution of focal populations in the peer-reviewed articles (N = 177).
HCP, healthcare professional; LGBT, lesbian, gay, bisexual and transgender; MSM, men who have sex with men; TGW, transgender women.
Nearly half (47%; n = 84) of the studies were conducted in four (of 28) Indian states—Maharashtra (n = 30), Tamil Nadu (n = 23), Karnataka (n = 19) or Andhra Pradesh (n = 12), with the majority of these in state capitals—Mumbai, Chennai, Bangalore, or Hyderabad. Over a third (36%; n = 65) of the studies were conducted in multiple Indian states.
Overall, 77% of studies (n = 137/177) reported sources of funding support, and 12% (n = 21) reported not receiving any specific funding; 11% (n = 19) did not report sources of funding. Of those studies that reported a funding source, the majority (72%; n = 99/137) were foreign sources (largely from the U.S. National Institutes of Health [NIH] and the Bill and Melinda Gates Foundation); 12% (n = 17) were Indo-U.S. collaborative research projects funded jointly by the Indian Council of Medical Research (ICMR) and NIH. Twenty studies (15%) received primary funding from the government of India (Indian Council of Medical Research [ICMR] and the National AIDS Control Organization [NACO]) and other Indian institutions.
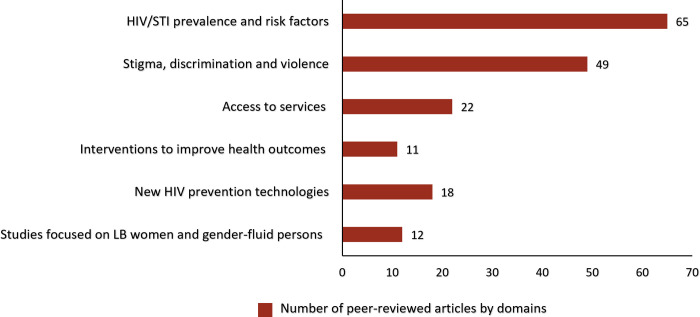
HIV/STI prevalence and risk factors
Thirty-seven percent (n = 65) of the articles focused on reporting STI/HIV prevalence estimates [30–47] and correlates of HIV-related risk behaviors [48–94] among MSM and TGW (Fig 4). In the 18 studies [30–47] that reported HIV and STI prevalence estimates among MSM and TGW, nine [31–33, 37, 39–42, 45] were conducted in clinical settings, six [30, 34, 35, 38, 43, 46] in community settings, and three [36, 44, 47] in both clinical and community settings. Of these 18 studies, eight [30, 34, 35, 37, 40, 43, 45, 46] reported HIV/STI prevalence and risk factors among MSM, three [36, 39, 44] human papillomavirus (HPV) prevalence among MSM living with HIV, and three [31, 33, 45] reported prevalence of perianal dermatoses, HPV and other STIs (such as syphilis, chlamydia and gonorrhea) among MSM. Two studies [38, 47] reported correlates of HIV incidence among MSM, with one study each reporting Hepatitis C prevalence among MSM living with HIV [42], and one study the prevalence of herpes [45].
Fig 4. Distribution of peer-reviewed articles by domains (N = 177).
LB, lesbian and bisexual.
Overall, HIV prevalence among MSM ranged from 3.8% to 23.0% across different study sites. Among MSM, HPV/genital warts (23.0% to 95.0%), syphilis (0.8% to 11.9%), HSV/genital herpes (7.1 to 32.0%), and genital molluscum contagium (9.6%) were the most commonly reported STIs [30, 31, 33, 34, 36, 37, 39, 40, 42, 45]. One study [42] reported Hepatitis-C prevalence among MSM as 1.3%. Syphilis rates tended to be higher among single MSM (8.3%) than married MSM (1.0%) [35]. In a study [32] conducted among 84 TGW who attended STI clinics in Pune, HIV prevalence was 45.2%.
Forty-seven articles [48–94] reported correlates of HIV-related risk among MSM and TGW. Among MSM, significant correlates of HIV risk behaviors/indicators such as condomless sex [48–50, 58, 64, 77, 78, 92, 93], infrequent HIV testing [60, 65, 72, 74], and HIV/STI positivity [48, 51, 55, 79] were low literacy and unemployment [48, 76, 77], alcohol and/or drug use [54, 60, 64, 65, 79, 90, 93], engagement in sex work [49, 60, 61, 65, 67, 68, 75, 76, 78], higher number of male sexual partners [48–50, 53, 56, 72, 74], early age of sexual debut [93], and low HIV risk perception [60, 65, 72, 74]. Six of the 47 articles included data on TGW; five of these [79, 81, 84, 87, 89] did not provide details on correlates of HIV risk behaviors, with one study [94] reporting that having a male regular partner was associated with HIV seropositivity.
Stigma, discrimination, and violence, and health impacts
Over one-fourth of the articles (27%; n = 48) [95–142] reported on stigma, discrimination, violence, and their associations with physical and mental health. Among these, 16 articles focused on stigma-related aspects of LGBTQI+ health [96, 100–102, 109, 110, 112, 114, 119, 124–126, 129, 132, 137, 140], 3 on violence [97, 103, 118], 17 on mental health and its correlates, such as quality of life [95, 99, 105, 106, 108, 111, 115, 123, 127, 128, 130, 131, 135, 136, 138, 139, 142], two on resilience [122, 133] and one article each on coping skills [141] and promoting LGBTQI+ acceptance [134]. Three articles reported on stress [116], perceived psychological impact [120] and violence [121] associated with Section-377 of the Indian Penal Code, which until September 2018 criminalised adult consensual same-sex relationships.
Several studies highlighted various types of stigma and discrimination experienced by MSM and TGW, which include perceived stigma, felt normative stigma, HIV-related stigma, family-enacted stigma, gender non-conformity stigma, and internalized stigma [96, 100, 101, 109, 124–126, 129, 132, 138], gender discrimination, workplace discrimination [137, 139] and polyvictimization [140]. Perpetrators of discrimination and violence against MSM and TGW, including those living with HIV, included peers, sexual partners, family members, healthcare providers, and police [98, 102, 103, 109, 112, 118, 119, 129, 130, 137, 139]. Fear of discrimination and suboptimal care [112] or refusal of care [109] prevented some persons from disclosing their sexual or gender identity to healthcare providers.
Fifteen studies [98, 99, 107–109, 112, 115, 125, 127–130, 137, 139, 140] indicated that stigma and discrimination contribute to depression and other negative mental health outcomes, such as suicidal ideation or attempts, among sexual and gender minorities. Two studies documented a high prevalence of mental health issues among MSM: depression (29% to 45%), anxiety (24% to 40%), suicidal ideation (45% to 53%), suicide attempts (23%), substance abuse (28%) including alcohol dependence (15% to 22%) [95, 130]. Similarly, among TGW, high levels of depression (43%), problematic alcohol use (37%) [108], anxiety (39%), depression (21%), suicide risk (75.8%) [136] and violence (52%) [139] were reported. Three studies with MSM [99, 108, 109, 115] and one with MSM and TGW [108] reported psychosocial syndemics, that is, co-occurring psychosocial conditions such as problematic alcohol use and internalized homonegativity, and their synergistic impact on HIV risk. The COVID-19 pandemic was also addressed as exacerbating psychological distress among LGBTQI+ people [125, 131].
Several studies addressed resilience, coping, and social support. A few studies documented various types of social support and other resilience resources available to MSM and TGW [107, 109, 117], with one study reporting moderate or high levels of resilience among 72% of TGW [122]. In terms of coping with adversity, MSM and TGW reported supportive roles of peers, NGOs [109], family, friends and partners [107], and gharanas (‘clans’ or houses of hijra-identified trans people) [127]. Some MSM and TGW reported strategies to prevent violence, discrimination and psychological distress, which included bribing police, running away from unsafe places and persons, and negotiating condom use during forced sex encounters [109], hiding sexual identities [103], denial [123], and behavioral disengagement [141]. One study documented positive coping strategies among older transgender people, such as spirituality, hope, and acceptance of gender dissonance [125]. In a few studies, social support and resilient coping strategies were identified as predictors of HIV risk [108] or mediators and moderators of the effects of discrimination on HIV risk or depression [110]. A resilience-based psychosocial intervention that integrated counselling was found to be effective in reducing HIV risk among MSM, with self-esteem and depressive symptoms mediating this effect [133]. A community-based theatre intervention was identified as effective in improving positive attitudes and knowledge, and promoting acceptance and solidarity towards LGBTQI+ communities among young adult heterosexual audiences [134].
Access to services: HIV/STIs and gender-affirmative procedures
In total, 22 studies [143–164]—10 quantitative [143, 145, 146, 148–153, 156] and 12 qualitative [144, 147, 154, 155, 157–164]—investigated access to HIV/STI services, gender transition services, and other clinical services. Four of these studies focused on HIV testing [145, 148, 150, 154] and four [144, 148, 156, 162] on antiretroviral treatment (ART) access and uptake among MSM and TGW living with HIV. Two studies [152, 153] addressed the HIV care continuum and linkages to care, three [147, 157, 158] challenges in accessing HIV testing, treatment and care services among MSM and TGW. Five studies focused on access to healthcare and support services for TGW: access to gender transition services [154], barriers to dental [150] and eye care [160], gender-affirmative technologies [159], and welfare schemes for TGW [161].
In relation to HIV testing among MSM, quantitative studies [146, 149, 151] reported that a majority of those recruited through community-based organizations (CBOs) or public sex environments were tested for HIV (61% to 86%) [146, 151], in contrast to MSM recruited through online social networking sites (47%) [149]. Factors such as high literacy levels, being 25 to 34 years old, engagement in sex work, and exposure to HIV intervention programs were associated with higher rates of HIV testing. Qualitative studies [147, 155] on HIV testing among MSM and TGW in two cities highlighted barriers such as HIV stigma and discrimination in healthcare settings and fears of adverse social consequences of testing HIV positive, and facilitators such as access to outreach programs operated by CBOs/NGOs, and accurate HIV risk perception.
Four studies (2 qualitative [144, 162] and 2 quantitative [148, 156]) conducted among MSM and TGW living with HIV reported that multilevel barriers prevented or significantly delayed access to free ART: the qualitative studies reported support from healthcare providers and peers as facilitators of ART adherence, while the quantitative studies [148, 156] indicated that 76% (n = 65/85) were on ART and 48% of these (n = 31/65) reported nonadherence [148]. Those who were younger and who had negative beliefs about ART were less likely to be adherent [148]. Low levels of knowledge, negative perceptions about ART, and ART nonadherence were significantly associated with lower levels of viral suppression [156].
In relation to access to gender-affirmative medical care, a qualitative study [154] reported a near-total absence of gender-affirmative hormone therapy and surgeries in public hospitals. Among three qualitative studies on challenges in accessing HIV testing and treatment services among MSM and TGW, two [157, 158] reported challenges faced by MSM and TGW in accessing HIV and gender transition-related services in the time of COVID-19.
Interventions to improve health outcomes among LGBTQI+ populations
Eleven articles [165–175] focused on health-related interventions, especially in relation to HIV prevention, of which 10 were exclusively conducted with MSM. Six of the 12 studies were pilot studies, including four pilot RCTs [167, 171, 173, 175]. Two articles reported qualitative formative research studies to design counselling-based [166] and mobile phone-based interventions [170]. Studies of interventions to increase condom use or HIV testing utilized diverse modalities, such as face-to-face risk reduction counseling [167], provision of community-friendly services [168], virtual counseling [165], internet-based [175] and mobile phone-based messages [171], and motivational interviewing techniques [173, 174]. Other intervention studies used video-based technologies such as mobile game-based learning for peer education [172], and a video-based counseling session [165].
New HIV prevention technologies and their acceptability
Overall, 18 studies [176–193] (11 quantitative, 7 qualitative) focused on new HIV prevention technologies, including oral pre-exposure prophylaxis (PrEP) [176, 177, 182, 184, 187–190, 192, 193], future HIV vaccines [178–181, 183] and rectal microbicides [185], as well as medical male circumcision [186], and oral HIV self-testing [191].
Of the ten articles on PrEP, eight examined acceptability or willingness to use PrEP among MSM and TGW; one explored the impact of prioritizing PrEP for MSM [184], and one compared the cost-effectiveness of offering PrEP to MSM with semiannual HIV testing as opposed to WHO-recommended 3-month testing [192]. Quantitative studies [176, 177, 188–190, 193] reported generally high willingness to use PrEP among MSM and TGW despite low levels of awareness. Qualitative studies [183, 188] reported factors associated with PrEP uptake, including perceived effectiveness in serodiscordant relationships, providing protection in cases of forced sex encounters, ability to use covertly, ability to have sex without condoms, and anxiety-less sex; barriers included PrEP stigma, fear of disclosure to one’s family or partners/spouse, and being labelled as HIV-positive or ‘promiscuous’ by peers. A mathematical modelling study [184] in Bangalore reported that PrEP could prevent a substantial proportion of infections among MSM (27% of infections over 10 years, with 60% coverage and 50% adherence).
Of the 5 studies on future HIV vaccine acceptability [178–181, 183], two [178, 180] assessed willingness to participate (WTP) in hypothetical HIV vaccine trials among MSM; one [179] explored mental models of candidate HIV vaccines and clinical trials; and two [181, 183] assessed frontline health service providers’ perspectives on HIV vaccine trials and their likelihood of recommending HIV vaccines to MSM populations.
Underrepresented LGBTQI+ populations: Sexual minority women, transmasculine people and people with intersex variations
Sexual minority women
Seven studies (4%) focused on sexual minority women [194–200], while two additional studies [201, 202] included sexual minority women as part of a larger sample. Among the seven studies, most focused on romantic relationships, such as communication and prioritization in relationships [199], difficulties in maintaining relationships [196], understanding of intimacy [197, 198], and lack of legal recognition of same-gender romantic partnerships [198]. One study [197] used a collaborative ethnographic approach to capture the understanding of community and activism from the perspectives of “women loving women” which had indirect connections to mental health. Another study [200] documented resilience sources (for example, self-confidence, optimism) used by sexual minority women to cope with major stressors.
The sexual health of sexual minority women was explored in two studies [194, 198]. One used photo-elicitation interviews and a survey to explore health behaviors and concerns [194], reporting that a majority of sexual minority women were not accessing preventive healthcare services: 36% reported having been screened for breast cancer and 14% for cervical cancer, and only 20% had ever been tested for STIs. The other study [198] reported lack of knowledge regarding STIs and difficulty in identifying LGBTQ-friendly service providers as major barriers to accessing preventive services.
Transmasculine people
Two studies (1%) [203, 204] focused on transmasculine people’s health: one [203] documented challenges in negotiating gender identity in various spaces, such as family, educational settings, workplace and neighborhoods; and one [204] reported that a substantially higher proportion of transmasculine persons (36.3%) attempted suicide when compared with transfeminine persons (24.7%).
People with intersex variations
Among the two studies (1%) [205, 206] that focused on people with intersex variations, one [205] examined how healthcare professionals decide on gender assignment of intersex children, and the other study [206] documented the social stigma faced by people with intersex variations and their families. Findings from both of these studies highlighted that gender assignment decisions are influenced by sociocultural factors: parents of intersex children preferred a male gender assignment possibly because of the social advantages of growing up as a male in a patriarchal society.
Discussion
This scoping review of a decade of peer-reviewed research on the health of LGBTQI+ people in India demonstrates a trend of increased publications addressing the health of sexual and gender minorities; however, it also identifies substantial gaps in the research—in terms of focal populations, geographical coverage, health conditions, and methods. Overall, this review demonstrates a predominant research focus on HIV and HIV-related risk behaviors among MSM and TGW populations; of these studies, a small subset were intervention studies aiming to improve the health of MSM and TGW. Notably, this review reveals the near complete omission of research on the health of sexual minority women—less than 4% of the studies identified. And amid the substantial focus on transgender women, largely in the context of HIV, scant research addressed the health of transmasculine people.
From a methodological perspective, among the quantitative studies that constituted the majority of the research, most were cross-sectional and descriptive in nature; few studies used longitudinal designs or mixed methods approaches, with very few intervention trials. The inclusion of a substantial proportion of qualitative and mixed methods studies, however, suggests a strength in the potential for characterizing the lived experiences of diverse LGBTQI+ people and experiences in the context of health disparities and challenges in healthcare access. Nevertheless, these too were dominated by a focus on MSM and TGW. A scoping review on LGBT inclusion in Thailand similarly reported substantial underrepresentation of lesbian and bisexual women, and transmasculine people, in the peer-reviewed literature [6].
The persistent and substantial gaps identified, even amid the overall increase in LGBTQI+ health research in India, have important implications for future research and research funding, health policies and programs, and healthcare services and practices for LGBTQI+ populations. There is a clear and compelling need to expand the evidence base on LGBTQI+ health in India to the many health and mental health conditions beyond HIV, and to the health challenges experienced across the diversity of LGBTQI+ people.
Specific population gaps identified in health research among LGBTQI+ people in India indicate the need for greater attention to lesbian and bisexual women, including potential health and mental health disparities compared to cisgender heterosexual women. Additional focus on lesbian and bisexual women’s experiences in access to and use of health services is sorely needed across an array of health conditions and healthcare settings, particularly given that studies reported their underutilization of routine preventive healthcare services. Reviews conducted on the health of sexual minority women in other countries arrived at similar conclusions [207, 208]. Further gaps emerged in the dearth of research with transmasculine people [209], and more broadly in research on access to medical and surgical gender-affirmative care needs for trans people. Greater attention to studies of healthcare providers and healthcare settings, and on healthcare provider training, that aim to improve access to gender-affirmative clinical services are needed [210]. Finally, there is a wholesale lack of health research among people with intersex variations. Future studies should focus on general health profiles, experiences in access to healthcare, and impact of non-essential or ‘corrective’ surgeries on health and mental health outcomes among people with intersex variations [211, 212].
Overall, the relatively small number of intervention studies were largely conducted with MSM in relation to HIV prevention. Nevertheless, while NACO supports several targeted interventions among MSM and TGW, with estimated programmatic coverage of nearly 88% to 95% of at-risk MSM and TGW [213], the lack of peer-reviewed publications on the effectiveness of such interventions limits their contribution to evidence-informed HIV prevention programs and policies in India. Although these interventions are primarily for programmatic purposes, the absence of published data represents a missed opportunity.
The stark lack of formal health outreach structures in India for lesbian and bisexual women, and for transmasculine people, makes it challenging to reach these populations through established organizational partners. Accordingly, greater involvement of a diversity of LGBTQI+ community-led groups in collaborative and participatory research studies is needed to expand opportunities to engage their inputs on research priorities, recruitment, and data collection methods, thereby also building their capacity in guiding and implementing research [214]. Such participatory mechanisms may be key to meaningful involvement of diverse and under-represented groups among LGBTQI+ communities and expanding relevant research evidence to advance their health. Strategic research funding mechanisms that target such underrepresented groups, as well as requiring community partnerships in certain health research streams, may be mechanisms to support such initiatives moving forward. For example, the U.S. NIH has established a sexual and gender minority research office, increased dedicated research funds, and released a five-year strategic plan to advance health research among sexual and gender minorities [215]. Similar steps need to be taken by the Indian Council of Medical Research, Department of Health Research. With just over one-fourth of the studies in this review funded fully or in part (in collaboration with NIH) by Indian government agencies, such as ICMR and NACO, there is a clear need to increase funding for LGBTQI+ health research by the Government of India.
This synthesis also highlights the connections between stigma, discrimination and violence, and the health issues faced by LGBTQI+ people. Several studies advance evidence on how discrimination and violence victimization contribute to psychosocial health problems and HIV risk among MSM and TGW [101, 216]. Stigma and violence elimination programs, and interventions in multiple sectors (for example, healthcare, education, employment) and social campaigns to promote understanding and acceptance of LGBTQI+ people are needed. The lack of access to gender-affirmative hormone therapy and surgeries for trans people highlights the need to improve access to such services, especially in the context of the Transgender Persons (Protection of Rights) Act, 2019, of India. This act clearly places the responsibility on the Indian central government and state governments to provide medical gender-affirmative health services and health insurance for trans people [22].
Other research areas that require increased exploration include the role of family and peer support in LGBTQI+ mental health, interventions to increase support from families and communities, and programs to eliminate discrimination and promote acceptance in healthcare, educational and workplace settings [25]. Given the deleterious impacts of stigma and discrimination on mental health and access to care, and the protective effects of social support and resilience resources, studies that integrate an understanding of social-structural contexts that affect mental health are key to effective approaches to advancing LGBTQI+ health [26]. Expanding the evidence base on LGBTQI+ health will require additional investments by national and state health research funders, including targeted funding for non-HIV-specific LGBTQI+ health research in the academic sector and in government-funded and government-run health programs on HIV (National AIDS Control Program of NACO), sexual and reproductive health and mental health (under National Health Mission), and non-communicable diseases (for example, National Program for Prevention and Control of Cancers, Diabetes and Cardiovascular Diseases and Stroke).
Finally, few studies made explicit reference to theoretical frameworks (for example, syndemic theory [216], minority stress theory [96], and structural violence [217]), that guided study design, analysis or interpretation. For one, such theories can advance research and understanding of the needs of understudied populations, such as sexual minority women, with studies also benefitting from community-based participatory methodologies and partnerships [198, 199]. The latter can advance application of theoretical frameworks that are sensitized to community-identified concerns, self-identifications, and priorities in Indian cultural contexts [199]. Several theoretical frameworks such as gender minority stress [218], gender affirmation [219] and intersectionality [220] that have been used productively in research among trans people in western countries, especially the U.S., appear not to be explicitly used in studies from India. Future research should include a focus on adapting existing frameworks to meaningfully address the Indian cultural context, as well as developing new indigenous frameworks for research with LGBTQI+ people in India. Future investigations should also ensure the inclusion of diverse subgroups of trans people—not solely gender binary, but also gender non-binary people—and portray local gender identity terms they use as well as indigenous constructions of gender identity, rather than defaulting to western terminologies, some of which do not translate well culturally or linguistically to the Indian LGBTQI+ experience [221].
Strengths and limitations
This scoping review should be understood in the context of study limitations. First, we limited searches to English-language texts and those included in major academic databases; however, we are not aware of Indian native language-based academic journals, given that academics and researchers largely publish in English. Second, we did not conduct quality assessments of individual studies as this is outside the purview of a scoping review; we aimed to map the field of available research, and research gaps, rather than answer a specific research question [28]. Third, we limited our review to peer-reviewed articles, for which we identified a substantial number of sources. Future scoping or systematic reviews should include grey literature from across India to broaden understanding of the landscape of research and gaps in regard to LGBTQI+ health; this is particularly the case given the concentration of studies identified among a minority of Indian states, and conducted almost exclusively in urban areas. Further, we did not include asexual-identified people in this review; future reviews should include this subpopulation to understand their health needs and healthcare experiences [222].
Conclusion
This scoping review identified key research gaps on LGBTQI+ health in India, with investigations largely limited to HIV-related issues, MSM and TGW populations, and urban study sites. This underscores the need for expanding health research in India to address the broad spectrum of LGBTQI+ people’s lives, specifically in moving beyond HIV-focused research to address mental health and non-communicable diseases as well. Future research should address the extensive gender gap in LGBTQI+ health research in India by focusing on health needs and healthcare experiences of lesbian and bisexual women. The broader spectrum of transgender and gender nonbinary people also merits increased focus, including studies on health needs and gaps with transmasculine people.
Finally, it is crucial to include sexual orientation and gender identity in national health surveys and to provide disaggregated data among LGBTQI+ subpopulations so that extant inequalities between heterosexual and cisgender people, and within LGBTQI+ people, can be documented [223]. Large-scale government-supported national health surveys among LGBTQI+ people provide a unique opportunity to document and explain health inequalities, and to identify potential solutions [224]. Strategies to enhance health research among LGBTQI+ people in India include developing a national LGBTQI+ health research agenda, providing dedicated LGBTQI+ health research funding from various government bodies, and investing in the training of researchers and new investigators to competently conduct LGBTQI+ health research. Additionally, investments in improving and sustaining the research and service provision capacities of community-based organizations are crucial as they already assume responsibility for serving a substantial number of LGBTQI+ people who are otherwise underserved by government-funded healthcare systems.
Supporting information
(DOCX)
(DOCX)
Acknowledgments
We would like to thank Luke Reid, JD, PhD (cand.), Research Fellow, University of Toronto Factor-Inwentash Faculty of Social Work, for assistance in implementing the literature search.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was financially supported by the Social Sciences and Humanities Research Council of Canada in the form of a grant (Partnership Grant, 895–2019-1020 [MFARR-Asia]) awarded to PAN. This work was also financially supported by the DBT/Wellcome Trust India Alliance Senior Fellowship (IA/CPHS/16/1/502667) in the form of salary for VC. The specific roles of these authors are articulated in the ‘author contributions’ section. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.UN Committee on Economic SaCRC. General Comment No. 14: The right to the highest attainable standard of health (Art. 12 of the Covenant). 2000.
- 2.International Covenant on Economic, Social and Cultural Rights. UN General Assembly; 1966.
- 3.Logie CH. Sexual rights and sexual pleasure: Sustainable development goals and the omitted dimensions of the leave no one behind sexual health agenda. Glob Public Health. 2021:1–12. doi: 10.1080/17441692.2021.1953559 [DOI] [PubMed] [Google Scholar]
- 4.Moagi MM, van Der Wath AE, Jiyane PM, Rikhotso RS. Mental health challenges of lesbian, gay, bisexual and transgender people: An integrated literature review. Health SA. 2021;26:1487. doi: 10.4102/hsag.v26i0.1487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.King WM, Gamarel KE. A scoping review examining social and legal gender affirmation and health among transgender populations. Transgend Health. 2021;6(1):5–22. doi: 10.1089/trgh.2020.0025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Newman PA, Reid L, Tepjan S, Akkakanjanasupar P. LGBT+ inclusion and human rights in Thailand: A scoping review of the literature. BMC Public Health. 2021;21(1):1816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kneale D, Henley J, Thomas J, French R. Inequalities in older LGBT people’s health and care needs in the United Kingdom: A systematic scoping review. Ageing Soc. 2021;41(3):493–515. doi: 10.1017/S0144686X19001326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Aggarwal NK, Consavage KE, Dhanuka I, Clement KW, Bouey JH. Health and health care access barriers among transgender women engaged in sex work: A synthesis of U.S.-based studies published 2005–2019. LGBT Health. 2020. doi: 10.1089/lgbt.2019.0243 [DOI] [PubMed] [Google Scholar]
- 9.Zeeman L, Sherriff N, Browne K, McGlynn N, Mirandola M, Gios L, et al. A review of lesbian, gay, bisexual, trans and intersex (LGBTI) health and healthcare inequalities. Eur J Public Health. 2019;29(5):974–80. doi: 10.1093/eurpub/cky226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hughes TL, Veldhuis CB, Drabble LA, Wilsnack SC. Research on alcohol and other drug (AOD) use among sexual minority women: A global scoping review. PLoS One. 2020;15(3):e0229869. doi: 10.1371/journal.pone.0229869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hibbert MP, Hillis A, Brett CE, Porcellato LA, Hope VD. A narrative systematic review of sexualised drug use and sexual health outcomes among LGBT people. Int J Drug Policy. 2021;93:103187. doi: 10.1016/j.drugpo.2021.103187 [DOI] [PubMed] [Google Scholar]
- 12.Huang YT, Ma YT, Craig SL, Wong DFK, Forth MW. How intersectional are mental health interventions for sexual minority people? A systematic review. LGBT Health. 2020;7(5):220–36. doi: 10.1089/lgbt.2019.0328 [DOI] [PubMed] [Google Scholar]
- 13.Baral SD, Grosso A, Holland C, Papworth E. The epidemiology of HIV among men who have sex with men in countries with generalized HIV epidemics. Curr Opin HIV AIDS. 2014;9(2):156–67. doi: 10.1097/COH.0000000000000037 [DOI] [PubMed] [Google Scholar]
- 14.Beyrer C, Baral SD, van Griensven F, Goodreau SM, Chariyalertsak S, Wirtz AL, et al. Global epidemiology of HIV infection in men who have sex with men. Lancet. 2012;380(9839):367–77. doi: 10.1016/S0140-6736(12)60821-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Poteat T, Scheim A, Xavier J, Reisner S, Baral S. Global epidemiology of HIV infection and related syndemics affecting transgender people. J Acquir Immune Defic Syndr. 2016;72 Suppl 3:S210–9. doi: 10.1097/QAI.0000000000001087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychol Bull. 2003;129(5):674–97. doi: 10.1037/0033-2909.129.5.674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cicero EC, Reisner SL, Silva SG, Merwin EI, Humphreys JC. Health care experiences of transgender adults: An integrated mixed research literature review. ANS Adv Nurs Sci. 2019;42(2):123–38. doi: 10.1097/ANS.0000000000000256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reisner SL, Poteat T, Keatley J, Cabral M, Mothopeng T, Dunham E, et al. Global health burden and needs of transgender populations: A review. Lancet. 2016;388(10042):412–36. doi: 10.1016/S0140-6736(16)00684-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Belmonte LA. The international LGBT rights movement: A history. London: Bloomsbury Academic; 2021. [Google Scholar]
- 20.Badgett MVL, Crehan PR. Investing in a research revolution for LGBTI inclusion. Washington, D.C.: World Bank Group; 2016. [Google Scholar]
- 21.Dixit P. Navtej Singh Johar v Union of India: Decriminalising India’s sodomy law. Int J Hum Rights. 2020;24(8):1011–30. [Google Scholar]
- 22.The Transgender Persons (Protection of Rights) Act, 2019. No. 40. In: Justice MoLa, editor. New Delhi 2019.
- 23.MoSJE. Report of the expert committee on the issues relating to transgender persons. New Delhi: Ministry of Social Justice and Empowerment, Government of India, 2014.
- 24.Setia MS, Brassard P, Jerajani HR, Bharat S, Kumta S, Row-Kavi A, et al. Men who have sex with men in India: A systematic review of the literature. J LGBT Health Res. 2008;4(2–3):51–70. doi: 10.1080/15574090902913727 [DOI] [PubMed] [Google Scholar]
- 25.Chakrapani V, Newman PA, Shunmugam M. Stigma toward and mental health of hijras/trans women and self-identified men who have sex with men in India. In: Nakamura N, Logie CH, editors. LGBTQ mental health: International perspectives and experiences. Washington: American Psychological Association; 2020. p. 103–19. [Google Scholar]
- 26.Wandrekar JR, Nigudkar AS. What do we know about LGBTQIA+ mental health in India? A review of research from 2009 to 2019. J Psychosexual Health. 2020;2(1):26–36. [Google Scholar]
- 27.Arksey H, O’Malley L. Scoping studies: Towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. [Google Scholar]
- 28.Peters MDJ, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. JBI Evid Implement. 2015;13(3). doi: 10.1097/XEB.0000000000000050 [DOI] [PubMed] [Google Scholar]
- 29.Lee JGL, Ylioja T, Lackey M. Identifying lesbian, gay, bisexual, and transgender search terminology: A systematic review of health systematic reviews. PLoS One. 2016;11(5):e0156210. doi: 10.1371/journal.pone.0156210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Solomon SS, Srikrishnan AK, Sifakis F, Mehta SH, Vasudevan CK, Balakrishnan P, et al. The emerging HIV epidemic among men who have sex with men in Tamil Nadu, India: Geographic diffusion and bisexual concurrency. AIDS Behav. 2010;14(5):1001–10. doi: 10.1007/s10461-010-9711-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ghosh SK, Bandyopadhyay D, Ghosh A, Biswas S, Mandal RK, Zamadar NS. Perianal dermatoses among men who have sex with men: A clinical profile of 32 Indian patients. Dermatol Online J. 2011;17(1):9. [PubMed] [Google Scholar]
- 32.Sahastrabuddhe S, Gupta A, Stuart E, Godbole S, Ghate M, Sahay S, et al. Sexually transmitted infections and risk behaviors among transgender persons (Hijras) of Pune, India. J Acquir Immune Defic Syndr (1999). 2012;59(1):72–8. doi: 10.1097/QAI.0b013e318236bd6f [DOI] [PubMed] [Google Scholar]
- 33.Ghosh I, Ghosh P, Bharti AC, Mandal R, Biswas J, Basu P. Prevalence of human papillomavirus and co-existent sexually transmitted infections among female sex workers, men having sex with men and injectable drug abusers from eastern India. Asian Pac J Cancer Prev. 2012;13(3):799–802. doi: 10.7314/apjcp.2012.13.3.799 [DOI] [PubMed] [Google Scholar]
- 34.Solomon SS, Mehta SH, Srikrishnan AK, Vasudevan CK, McFall AM, Balakrishnan P, et al. High HIV prevalence and incidence among MSM across 12 cities in India. AIDS. 2015;29(6):723–31. doi: 10.1097/QAD.0000000000000602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mayer KH, Gangakhedkar R, Sivasubramanian M, Biello KB, Abuelezam N, Mane S, et al. Differing identities but comparably high HIV and bacterial sexually transmitted disease burdens among married and unmarried men who have sex with men in Mumbai, India. Sex Transm Dis. 2015;42(11):629–33. doi: 10.1097/OLQ.0000000000000344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hernandez AL, Karthik R, Sivasubramanian M, Raghavendran A, Gnanamony M, Lensing S, et al. Prevalence of anal HPV infection among HIV-positive men who have sex with men in India. J Acquir Immune Defic Syndr. 2016. Apr 1; 71(4):437–43. doi: 10.1097/QAI.0000000000000855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Aggarwal P, Bhattar S, Sahani SK, Bhalla P, Garg VK. Sexually transmitted infections and HIV in self reporting men who have sex with men: A two-year study from India. J Infect Public Health. 2016;9(5):564–70. doi: 10.1016/j.jiph.2015.12.007 [DOI] [PubMed] [Google Scholar]
- 38.Solomon SS, Mehta SH, McFall AM, Srikrishnan AK, Saravanan S, Laeyendecker O, et al. Community viral load, antiretroviral therapy coverage, and HIV incidence in India: A cross-sectional, comparative study. Lancet HIV. 2016;3(4):e183–90. doi: 10.1016/S2352-3018(16)00019-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Raghavendran A, Hernandez AL, Lensing S, Gnanamony M, Karthik R, Sivasubramanian M, et al. Genital human papillomavirus infection in Indian HIV-seropositive men who have sex with men. Sex Transm Dis. 2017;44(3):173–80. doi: 10.1097/OLQ.0000000000000564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hussain T, Kulshreshtha KK, Yadav VS. Prevalence of HIV and syphilis infections among men who have sex with men attending an integrated counseling and testing centre at Agra: Comparison with studies in other regions of India. J HIV/AIDS Soc Serv. 2018;17(4):353–68. [Google Scholar]
- 41.Gupte S, Daly C, Agarwal V, Gaikwad SB, George B. Introduction of rapid tests for large-scale syphilis screening among female, male, and transgender sex workers in Mumbai, India. Sex Transm Dis. 2011;38(6):499–502. doi: 10.1097/OLQ.0b013e318205e45d [DOI] [PubMed] [Google Scholar]
- 42.Clipman SJ, Duggal P, Srikrishnan AK, Saravanan S, Balakrishnan P, Vasudevan CK, et al. Prevalence and phylogenetic characterization of hepatitis C virus among Indian men who have sex with men: Limited evidence for sexual transmission. J Infect Dis. 2020. May 11;221(11):1875–83. doi: 10.1093/infdis/jiaa006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Haldar P, Jha S, Rath R, Goswami K, Thakur N, Kumar P. Is inclusion of informed consent associated with HIV seropositivity rate? findings from 2017 HIV sentinel surveillance among men having sex with men in select states of India. Indian J Public Health. 2020;64(Suppl):S22–S5. doi: 10.4103/ijph.IJPH_37_20 [DOI] [PubMed] [Google Scholar]
- 44.Hernandez AL, Karthik R, Sivasubramanian M, Raghavendran A, Lensing S, Lee JY, et al. Prevalence of oral human papillomavirus infection among Indian HIV-positive men who have sex with men: A cross-sectional study. BMC Infect Dis. 2021;21(1):675. doi: 10.1186/s12879-021-06301-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Palakkal S, Anila K, Sobhanakumari K, Celine MI, Vineetha M. Viewing the resurgence of early syphilis in light of increasing male homosexuality and childhood sexual abuse. Indian J Sex Transm Dis AIDS. 2020;41(2):188–91. doi: 10.4103/ijstd.IJSTD_104_16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Prabhu S, Mehta SH, McFall AM, Srikrishnan AK, Vasudevan CK, Lucas GM, et al. Role of geospatial mapping in the planning of HIV programs: A case study from Southern India. Med. 2021;100(34):e27092. doi: 10.1097/MD.0000000000027092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Patel EU, Solomon SS, Lucas GM, McFall AM, Srikrishnan AK, Kumar MS, et al. Temporal change in population-level prevalence of detectable HIV viraemia and its association with HIV incidence in key populations in India: A serial cross-sectional study. Lancet HIV. 2021;8(9):e544–e53. doi: 10.1016/S2352-3018(21)00098-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kumta S, Lurie M, Weitzen S, Jerajani H, Gogate A, Row-kavi A, et al. Bisexuality, sexual risk taking, and HIV prevalence among men who have sex with men accessing voluntary counseling and testing services in Mumbai, India. J Acquir Immune Defic Syndr. 2010;53(2):227–33. doi: 10.1097/QAI.0b013e3181c354d8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Phillips AE, Lowndes CM, Boily MC, Garnett GP, Gurav K, Ramesh BM, et al. Men who have sex with men and women in Bangalore, South India, and potential impact on the HIV epidemic. Sex Transm Infect. 2010;86(3):187–92. doi: 10.1136/sti.2009.038216 [DOI] [PubMed] [Google Scholar]
- 50.Solomon SS, Mehta SH, Latimore A, Srikrishnan AK, Celentano DD. The impact of HIV and high-risk behaviours on the wives of married men who have sex with men and injection drug users: Implications for HIV prevention. J Int AIDS Soc. 2010;13 Suppl 2(Suppl 2):S7. doi: 10.1186/1758-2652-13-S2-S7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Setia MS, Sivasubramanian M, Anand V, Row-Kavi A, Jerajani HR. Married men who have sex with men: The bridge to HIV prevention in Mumbai, India. Int J Public Health. 2010;55(6):687–91. doi: 10.1007/s00038-010-0173-0 [DOI] [PubMed] [Google Scholar]
- 52.Gutierrez J-P, McPherson S, Fakoya A, Matheou A, Bertozzi SM. Community-based prevention leads to an increase in condom use and a reduction in sexually transmitted infections (STIs) among men who have sex with men (MSM) and female sex workers (FSW): The Frontiers Prevention Project (FPP) evaluation results. BMC Public Health. 2010;10:497. doi: 10.1186/1471-2458-10-497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lorway R, Shaw SY, Hwang SDH, Reza-Paul S, Pasha A, Wylie JL, et al. From individuals to complex systems: Exploring the sexual networks of men who have sex with men in three cities of Karnataka, India. Sex Transm Infect. 2010;86(Suppl 3):iii70–8. doi: 10.1136/sti.2010.044909 [DOI] [PubMed] [Google Scholar]
- 54.Mimiaga MJ, Thomas B, Mayer KH, Reisner SL, Menon S, Swaminathan S, et al. Alcohol use and HIV sexual risk among MSM in Chennai, India. Int J STD AIDS. 2011;22(3):121–5. doi: 10.1258/ijsa.2009.009059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hendriksen ES, Krishnan AKS, Vallabhaneni S, Johnson S, Raminani S, Kumarasamy N, et al. Primary prevention lessons learned from those with HIV in Chennai, India. Sex Health. 2011;8(2):199–206. doi: 10.1071/SH10015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hemmige V, Snyder H, Liao C, Mayer K, Lakshmi V, Gandham SR, et al. Sex position, marital status, and HIV risk among Indian men who have sex with men: Clues to optimizing prevention approaches. AIDS Patient Care STDS. 2011;25(12):725–34. doi: 10.1089/apc.2011.0079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lorway R, Hwang SDH, Reza-Paul S, Pasha A, Rahman SHU, Moses S, et al. Sex in the city: Privacy-making practices, spatialized intimacies and the environmental risks of men-who-have-sex-with-men in South India. Health Place. 2011;17(5):1090–7. doi: 10.1016/j.healthplace.2011.05.015 [DOI] [PubMed] [Google Scholar]
- 58.Thomas B, Mimiaga MJ, Mayer KH, Perry NS, Swaminathan S, Safren SA. The influence of stigma on HIV risk behavior among men who have sex with men in Chennai, India. AIDS Care. 2012;24(11):1401–6. doi: 10.1080/09540121.2012.672717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Tomori C, Srikrishnan AK, Mehta SH, Nimmagadda N, Anand S, Vasudevan CK, et al. HIV risks among women who are married to men who have sex with men in India: A qualitative investigation. Cult Health Sex. 2018;20(8):873–87. doi: 10.1080/13691058.2017.1390161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wilkerson JM, Di Paola A, Rawat S, Patankar P, Rosser BRS, Ekstrand ML. Substance use, mental health, HIV testing, and sexual risk behavior among men who have sex with men in the state of Maharashtra, India. AIDS Educ Prev. 2018;30(2):96–107. doi: 10.1521/aeap.2018.30.2.96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Srivastava A, Goldbach JT. Pathways to male transactional sex in Mumbai, India. J Homosex. 2019;66(2):173–88. doi: 10.1080/00918369.2017.1398018 [DOI] [PubMed] [Google Scholar]
- 62.Mimiaga MJ, Biello KB, Sivasubramanian M, Mayer KH, Anand VR, Safren SA. Psychosocial risk factors for HIV sexual risk among Indian men who have sex with men. AIDS Care. 2013;25(9):1109–13. doi: 10.1080/09540121.2012.749340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Saggurti N, Mishra RM, Proddutoor L, Tucker S, Kovvali D, Parimi P, et al. Community collectivization and its association with consistent condom use and STI treatment-seeking behaviors among female sex workers and high-risk men who have sex with men/transgenders in Andhra Pradesh, India. AIDS Care. 2013;25(Suppl 1):S55–66. doi: 10.1080/09540121.2012.749334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Chakrapani V, Boyce P, Newman PA, Row Kavi A. Contextual influences on condom use among men who have sex with men in India: Subjectivities, practices and risks. Cult Health Sex. 2013;15(8):938–51. doi: 10.1080/13691058.2013.798032 [DOI] [PubMed] [Google Scholar]
- 65.Ramanathan S, Chakrapani V, Ramakrishnan L, Goswami P, Yadav D, Subramanian T, et al. Consistent condom use with regular, paying, and casual male partners and associated factors among men who have sex with men in Tamil Nadu, India: Findings from an assessment of a large-scale HIV prevention program. BMC Public Health. 2013;13:827. doi: 10.1186/1471-2458-13-827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Narayanan P, Das A, Morineau G, Prabhakar P, Deshpande GR, Gangakhedkar R, et al. An exploration of elevated HIV and STI risk among male sex workers from India. BMC Public Health. 2013;13:1059. doi: 10.1186/1471-2458-13-1059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kumar GA, Dandona R, Poluru R, Chandran SA, Alary M, Dandona L. Patterns of condom use by men who have sex with men before and after the Avahan intervention in Andhra Pradesh state of India. BMC Public Health. 2014;14:64. doi: 10.1186/1471-2458-14-64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Yadav D, Chakrapani V, Goswami P, Ramanathan S, Ramakrishnan L, George B, et al. Association between alcohol use and HIV-related sexual risk behaviors among men who have sex with men (MSM): Findings from a multi-site bio-behavioral survey in India. AIDS Behav. 2014;18(7):1330–8. doi: 10.1007/s10461-014-0699-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ramesh S, Mehrotra P, Mahapatra B, Ganju D, Nagarajan K, Saggurti N. The effect of mobility on sexual risk behaviour and HIV infection: A cross-sectional study of men who have sex with men in southern India. Sex Transm Infect. 2014;90(6):491–7. doi: 10.1136/sextrans-2013-051350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Mitchell KM, Foss AM, Prudden HJ, Mukandavire Z, Pickles M, Williams JR, et al. Who mixes with whom among men who have sex with men? Implications for modelling the HIV epidemic in southern India. J Theor Biol. 2014;355(100):140–50. doi: 10.1016/j.jtbi.2014.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Closson EF. The other side of the bridge: exploring the sexual relationships of men who have sex with men and their female partners in Mumbai, India. Cult Health Sex. 2014;16:780–91. doi: 10.1080/13691058.2014.911960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ramanathan S, Deshpande S, Gautam A, Pardeshi DB, Ramakrishnan L, Goswami P, et al. Increase in condom use and decline in prevalence of sexually transmitted infections among high-risk men who have sex with men and transgender persons in Maharashtra, India: Avahan, the India AIDS Initiative. BMC Public Health. 2014;14:784. doi: 10.1186/1471-2458-14-784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Godbole S, Sane S, Kamble P, Raj Y, Dulhani N, Venkatesh S, et al. Predictors of bisexual behaviour among MSM attending intervention sites may help in prevention interventions for this bridge to the heterosexual epidemic in India: Data from HIV sentinel surveillance. PloS One. 2014;9(9):e107439. doi: 10.1371/journal.pone.0107439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Mitchell KM, Foss AM, Ramesh BM, Washington R, Isac S, Prudden HJ, et al. Relationship between exposure to the Avahan intervention and levels of reported condom use among men who have sex with men in southern India. BMC Public Health. 2014;14:1245. doi: 10.1186/1471-2458-14-1245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Saha MK, Mahapatra T, Biswas S, Ghosh P, Mahapatra S, Deb AK, et al. Sociobehavioral correlates of HIV risk among men who have sex with men in Chhattisgarh, India: Analysis of sentinel surveillance data. Jpn J Infect Dis. 2015;68(1):38–44. doi: 10.7883/yoken.JJID.2013.068 [DOI] [PubMed] [Google Scholar]
- 76.Saha MK, Mahapatra T, Biswas S, Ghosh P, Kire M. Burden and correlates of HIV risk among men who have sex with men in Nagaland, India: Analysis of sentinel surveillance data. PloS One. 2015;10(2):e0117385. doi: 10.1371/journal.pone.0117385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ramakrishnan L, Ramanathan S, Chakrapani V, Goswami P, Deshpande S, Yadav D, et al. Comparison of sexual risk, HIV/STI prevalence and intervention exposure among men who have sex with men and women (MSMW) and men who have sex with men only (MSMO) in India: Implications for HIV prevention. AIDS Behav. 2015;19(12):2255–69. doi: 10.1007/s10461-015-1058-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Mahapatra T, Biswas S, Nandi S, Ghosh P, Ghosh M, Mondal S, et al. Burden and correlates of HIV among men who have sex with men in West Bengal, India: Analysis of sentinel surveillance data. PloS One. 2015;10(5):e0127232. doi: 10.1371/journal.pone.0127232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Shaw SY, Lorway R, Bhattacharjee P, Reza-Paul S, du Plessis E, McKinnon L, et al. Descriptive epidemiology of factors associated with HIV infections among men and transgender women who have sex with men in South India. LGBT Health. 2016;3(4):292–9. doi: 10.1089/lgbt.2015.0023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Tomori C, McFall AM, Srikrishnan AK, Mehta SH, Nimmagadda N, Anand S, et al. The prevalence and impact of childhood sexual abuse on HIV-risk behaviors among men who have sex with men (MSM) in India. BMC Public Health. 2016;16:784. doi: 10.1186/s12889-016-3446-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Sinha A, Goswami DN, Haldar D, Mallik S, Bisoi S, Karmakar PR. Sexual behavior of transgenders and their vulnerability to HIV/AIDS in an urban area of eastern India. Indian J Public Health. 2017;61(2):141–3. doi: 10.4103/ijph.IJPH_248_14 [DOI] [PubMed] [Google Scholar]
- 82.Banik S, Dodge B, Schmidt-Sane M, Sivasubramanian M, Bowling J, Rawat SM, et al. Humanizing an invisible population in India: Voices from bisexual men concerning identity, life experiences, and sexual health. Arch Sex Behav. 2019;48(1):305–316. doi: 10.1007/s10508-018-1361-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Deshpande S, Bharat S. Sexual partner mixing and differentials in consistent condom use among men who have sex with men in Maharashtra, India. Glob Public Health. 2015;10(1):103–118. doi: 10.1080/17441692.2014.972968 [DOI] [PubMed] [Google Scholar]
- 84.Chakrapani V, Shunmugam M, Newman PA, Kershaw T, Dubrow R. HIV status disclosure and condom use among HIV-positive men who have sex with men and Hijras (male-to-female transgender people) in India: Implications for prevention. J HIV/AIDS Soc Serv. 2015;14(1):26–44. [Google Scholar]
- 85.Dodge B, Banik S, Bowling J, Sivasubramanian M, Mengle S, Schick V, et al. Sexual relationships, behaviors, and experiences among bisexual men in Mumbai, India. Int J Sex Health. 2016;28(1):70–84. doi: 10.1080/19317611.2015.1116482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Willie TC, Chakrapani V, White Hughto JM, Kershaw TS. Victimization and human immunodeficiency virus-related risk among transgender women in India: A latent profile analysis. Violence Gend. 2017;4(4):121–129. doi: 10.1089/vio.2017.0030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ferguson H. Virtual Risk: How MSM and TW in India use media for partner selection [Public Health Theses. 1084]. New Haven: Yale University; 2016. [Google Scholar]
- 88.Banik S, Fisher LE, Anand VR. Expression and experiences of sexual identity among married men who have sex with men in India. Health Educ Monograph Series. 2014;31(2):61–7. [Google Scholar]
- 89.Wilkerson JMjmwute Rhoton JM, Li D Rawat SA, Patankar P Rosser BRS, et al. Information, motivation, and self-efficacy among men who have sex with men and transgender women in the state of Maharashtra, India. Health Educ Behav. 2019;46(2):304–311. doi: 10.1177/1090198118796880 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Bhambhani Y, Rawat S, Norton BL, Patel VV. Alcohol and drug use surrounding sex among men who have sex with men in India. Sex Cult. 2021;25(4):1383–96. [Google Scholar]
- 91.Sudharshan S, Menia NK, Selvamuthu P, Tyagi M, Kumarasamy N, Biswas J. Ocular syphilis in patients with human immunodeficiency virus/acquired immunodeficiency syndrome in the era of highly active antiretroviral therapy. Indian J Ophthalmol. 2020;68(9):1887–1893. doi: 10.4103/ijo.IJO_1070_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Safren SA, Devaleenal B, Biello KB, Rawat S, Thomas BE, Regenauer KS, et al. Geographic and behavioral differences associated with sexually transmitted infection prevalence among Indian men who have sex with men in Chennai and Mumbai. Int J STD AIDS. 2021;32(2):144–151. doi: 10.1177/0956462420943016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Kumar P, Aridoss S, Mathiyazhakan M, Balasubramanian G, Jaganathasamy N, Natesan M, et al. Substance use and risk of HIV infection among men who have sex with men in India: Analysis of national IBBS data, India. Med. 2020;99(35):e21360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Rajan S, Kumar P, Sangal B, Kumar A, Ramanathan S, Ammassari S. HIV/AIDS-related risk behaviors, HIV prevalence, and determinants for HIV prevalence among hijra/transgender people in India: Findings from the 2014–2015 integrated biological and behavioural surveillance. Indian J Public Health. 2020;64(Suppl):S53–S60. doi: 10.4103/ijph.IJPH_55_20 [DOI] [PubMed] [Google Scholar]
- 95.Sivasubramanian M, Mimiaga MJ, Mayer KH, Anand VR, Johnson CV, Prabhugate P, et al. Suicidality, clinical depression, and anxiety disorders are highly prevalent in men who have sex with men in Mumbai, India: Findings from a community-recruited sample. Psychol Health Med. 2011;16(4):450–62. doi: 10.1080/13548506.2011.554645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Logie CH, Newman PA, Chakrapani V, Shunmugam M. Adapting the minority stress model: Associations between gender non-conformity stigma, HIV-related stigma and depression among men who have sex with men in South India. Soc Sci Med. 2012;74(8):1261–8. doi: 10.1016/j.socscimed.2012.01.008 [DOI] [PubMed] [Google Scholar]
- 97.Shaw SY, Lorway RR, Deering KN, Avery L, Mohan HL, Bhattacharjee P, et al. Factors associated with sexual violence against men who have sex with men and transgendered individuals in Karnataka, India. PloS One. 2012;7(3):e31705. doi: 10.1371/journal.pone.0031705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Tomori C, Srikrishnan AK, Ridgeway K, Solomon SS, Mehta SH, Solomon S, et al. Perspectives on sexual identity formation, identity practices, and identity transitions among men who have sex with men in India. Arch Sex Behav. 2018;47(1):235–244. doi: 10.1007/s10508-016-0775-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Tomori C, McFall AM, Solomon SS, Srikrishnan AK, Anand S, Balakrishnan P, et al. Is there synergy in syndemics? Psychosocial conditions and sexual risk among men who have sex with men in India. Soc Sci Med. 2018;206:110–116. doi: 10.1016/j.socscimed.2018.03.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Thaker J, Dutta M, Nair V, Rao VP. The interplay between stigma, collective efficacy, and advocacy communication among men who have sex with men and transgender females. J Health Commun. 2018;23(7):614–623. doi: 10.1080/10810730.2018.1499833 [DOI] [PubMed] [Google Scholar]
- 101.Chakrapani V, Willie TC, Shunmugam M, Kershaw TS. Syndemic classes, stigma, and sexual risk among transgender women in India. AIDS Behav. 2019;23(6):1518–1529. doi: 10.1007/s10461-018-2373-1 [DOI] [PubMed] [Google Scholar]
- 102.Thompson LH, Khan S, du Plessis E, Lazarus L, Reza-Paul S, Hafeez Ur Rahman S, et al. Beyond internalised stigma: Daily moralities and subjectivity among self-identified kothis in Karnataka, South India. Cult Health Sex. 2013;15(10):1237–51. doi: 10.1080/13691058.2013.818714 [DOI] [PubMed] [Google Scholar]
- 103.Elouard Y, Essen B. Psychological violence experienced by men who have sex with men in Puducherry, India: A qualitative study. J Homosex. 2013;60(11):1581–601. doi: 10.1080/00918369.2013.824325 [DOI] [PubMed] [Google Scholar]
- 104.Maroky AS, Ratheesh A, Viswanath B, Math SB, Chandrashekar CR, Seshadri SP. ’Ego-dystonicity’ in homosexuality: An Indian perspective. Int J Soc Psychiatry. 2015;61(4):311–8. doi: 10.1177/0020764014543709 [DOI] [PubMed] [Google Scholar]
- 105.Mimiaga MJ, Closson EF, Thomas B, Mayer KH, Betancourt T, Menon S, et al. Garnering an in-depth understanding of men who have sex with men in Chennai, India: A qualitative analysis of sexual minority status and psychological distress. Arch Sex Behav. 2015;44(7):2077–86. doi: 10.1007/s10508-014-0369-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Tomori C, McFall AM, Srikrishnan AK, Mehta SH, Solomon SS, Anand S, et al. Diverse rates of depression among men who have sex with men (MSM) across India: Insights from a multi-site mixed method study. AIDS Behav. 2016;20(2):304–16. doi: 10.1007/s10461-015-1201-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Tomori C, Srikrishnan AK, Ridgeway K, Solomon SS, Mehta SH, Solomon S, et al. Friends, sisters, and wives: Social support and social risks in peer relationships among men who have sex with men (MSM) in India. AIDS Educ Prev. 2016;28(2):153–64. doi: 10.1521/aeap.2016.28.2.153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Chakrapani V, Newman PA, Shunmugam M, Logie CH, Samuel M. Syndemics of depression, alcohol use, and victimisation, and their association with HIV-related sexual risk among men who have sex with men and transgender women in India. Glob Public Health. 2017;12(2):250–65. doi: 10.1080/17441692.2015.1091024 [DOI] [PubMed] [Google Scholar]
- 109.Ganju D, Saggurti N. Stigma, violence and HIV vulnerability among transgender persons in sex work in Maharashtra, India. Cult Health Sex. 2017;19(8):903–917. doi: 10.1080/13691058.2016.1271141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Chakrapani V, Vijin PP, Logie CH, Newman PA, Shunmugam M, Sivasubramanian M, et al. Understanding how sexual and gender minority stigmas influence depression among trans women and men who have sex with men in India. LGBT Health. 2017;4(3):217–226. doi: 10.1089/lgbt.2016.0082 [DOI] [PubMed] [Google Scholar]
- 111.Kalra G, Shah N. The cultural, psychiatric, and sexuality aspects of hijras in India. Int J Transgend. 2013;14(4):171–81. [Google Scholar]
- 112.Lorway R, Thompson LH, Lazarus L, du Plessis E, Pasha A, Mary PF, et al. Going beyond the clinic: Confronting stigma and discrimination among men who have sex with men in Mysore through community-based participatory research. Crit Public Health. 2014;24(1):73–87. [Google Scholar]
- 113.Manian S. Behind the shroud of heteronormative silence: Tales of same-sex desire. Sexualities. 2014;17(5–6):742–57. [Google Scholar]
- 114.Chakrapani V, Vijin PP, Logie CH, Newman PA, Shunmugam M, Sivasubramanian M, et al. Assessment of a "Transgender Identity Stigma" scale among trans women in India: Findings from exploratory and confirmatory factor analyses. Int J Transgend. 2017;18(3):271–81. [Google Scholar]
- 115.Chakrapani V, Kaur M, Newman PA, Mittal S, Kumar R. Syndemics and HIV-related sexual risk among men who have sex with men in India: Influences of stigma and resilience. Cult Health Sex. 2019;21(4):416–431. doi: 10.1080/13691058.2018.1486458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Rao S, Mason CD. Minority stress and well-being under anti-sodomy legislation in India. Psychology of Sexual Orientation and Gender Diversity. 2018;5(4):432–44. [Google Scholar]
- 117.Pandya A. Voices of invisibles: Coping responses of men who have sex with men. In: Blaznia C, Shen-Miller DS, editors. An international psychology of men: Theoretical advances, case studies, and clinical innovations. NY: Routledge. 2010. p. 233–58. [Google Scholar]
- 118.Dutta S, Khan S, Lorway R. Following the divine: An ethnographic study of structural violence among transgender jogappas in South India. Cult Health Sex. 2019. Nov;21(11):1240–1256. doi: 10.1080/13691058.2018.1555718 [DOI] [PubMed] [Google Scholar]
- 119.Bowling J, Mennicke A, Blekfeld-Sztraky D, Simmons M, Dodge B, Sundarraman V, et al. The influences of stigma on sexuality among sexual and gender minoritized individuals in urban India. Int J Sex Health. 2019;31:3:269–82. [Google Scholar]
- 120.Rao S, Mason CD, Galvao RW, Clark BA, Calabrese SK. "You are illegal in your own country": The perceived impact of antisodomy legislation among Indian sexual and gender minorities. Stigma Health. 2020;5(4):451–62. [Google Scholar]
- 121.Li DH, Rawat S, Rhoton J, Patankar P, Ekstrand ML, Rosser BR, et al. Harassment and violence among men who have sex with men (MSM) and hijras after reinstatement of India’s "Sodomy Law". Sex Res Social Policy. 2017;14(3):324–330. doi: 10.1007/s13178-016-0270-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Chavada VK, R P, Kurushev J. Level of resilience among transgenders in selected areas of Puducherry, India: An exploratory research. Cureus. 2021;13(9):e18413. doi: 10.7759/cureus.18413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Bhattacharya S, Ghosh D. Studying physical and mental health status among hijra, kothi and transgender community in Kolkata, India. Soc Sci Med. 2020;265:113412. doi: 10.1016/j.socscimed.2020.113412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Dhabhar MC, Deshmukh AS. Implicit internalized homophobia in India: Cognitive and sociodemographic factors. J Gay Lesbian Ment Health. 2021;25(2):226–49. [Google Scholar]
- 125.Banerjee D, Rao TSS. "The Graying Minority": Lived experiences and psychosocial challenges of older transgender adults during the COVID-19 pandemic in India, A qualitative exploration. Front Psychiatry. 2020;11:604472. doi: 10.3389/fpsyt.2020.604472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Azhar S, Vaudrey J, Gandham S, Burr S, Oruganti G, Yeldandi V. Secret lives and gender fluidity of people living with HIV in Hyderabad, India. J Community Psychol. 2021;50(1):221–37. doi: 10.1002/jcop.22541 [DOI] [PubMed] [Google Scholar]
- 127.Srivastava A, Sivasubramanian M, Goldbach JT. Mental health and gender transitioning among hijra individuals: A qualitative approach using the minority stress model. Cult Health Sex. 2021;23(6):757–71. doi: 10.1080/13691058.2020.1727955 [DOI] [PubMed] [Google Scholar]
- 128.Prabhu S, McFall AM, Mehta SH, Srikrishnan AK, Kumar MS, Anand S, et al. Psychosocial barriers to viral suppression in a community-based sample of human immunodeficiency virus-infected men who have sex with men and people who inject drugs in India. Clin Infect Dis. 2020;70(2):304–13. doi: 10.1093/cid/ciz175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Arvind A, Pandya A, Amin L, Aggarwal M, Agrawal D, Tiwari K, et al. Social strain, distress, and gender dysphoria among transgender women and hijra in Vadodara, India. Int J Transgend Health. 2021;23(1–2):149–63. doi: 10.1080/26895269.2020.1845273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Thirunavukkarasu B, Khandekar J, Parasha M, Dhiman B, Yadav K. Psychosocial health and its associated factors among men who have sex with men in India: A cross-sectional study. Indian J Psychiatry. 2021;63(5):490–94. doi: 10.4103/indianjpsychiatry.indianjpsychiatry_18_21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Sharma AJ, Subramanyam MA. A cross-sectional study of psychological wellbeing of Indian adults during the Covid-19 lockdown: Different strokes for different folks. PloS One. 2020;15(9):e0238761. doi: 10.1371/journal.pone.0238761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Dhaor SS. Lived experiences of internalized stigma among HIV-positive adults in Delhi, India. Community Health Equity Res Policy. 2021;43(3):301–9. doi: 10.1177/0272684X211022580 [DOI] [PubMed] [Google Scholar]
- 133.Safren SA, Thomas B, Biello KB, Mayer KH, Rawat S, Dange A, et al. Strengthening resilience to reduce HIV risk in Indian MSM: A multicity, randomised, clinical efficacy trial. Lancet Glob Health. 2021;9(4):e446–55. doi: 10.1016/S2214-109X(20)30547-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Pufahl J, Rawat S, Chaudary J, Shiff NJ. Even mists have silver linings: Promoting LGBTQ+ acceptance and solidarity through community-based theatre in India. Public Health. 2021;194:252–9. doi: 10.1016/j.puhe.2021.02.027 [DOI] [PubMed] [Google Scholar]
- 135.Majumder A, Roychaudhuri S, Chakraborty S, Bhattacherjee K. An observational study of the quality of life among gender incongruent individuals from "Hijra" community of India. Indian J Endocrinol Metab. 2020;24(4):301–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Joshi N, Vinu V, Jois SN, Begum F, Salagame KK. The need, feasibility and willingness to explore "Meditation on Twin Hearts" as a self-administered tool for mental health management among transgender women: An exploratory survey. Community Ment Health J. 2021;58(4):666–72. doi: 10.1007/s10597-021-00869-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Gomes de Jesus J, Belden CM, Huynh HV, Malta M, LeGrand S, Kaza VGK, et al. Mental health and challenges of transgender women: A qualitative study in Brazil and India. Int J Transgend Health. 2020;21(4):418–30. doi: 10.1080/26895269.2020.1761923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Sharma AJ, Subramanyam MA. Psychological wellbeing of middle-aged and older queer men in India: A mixed-methods approach. PloS One. 2020;15(3):e0229893. doi: 10.1371/journal.pone.0229893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Sartaj D, Krishnan V, Rao R, Ambekar A, Dhingra N, Sharan P. Mental illnesses and related vulnerabilities in the Hijra community: A cross-sectional study from India. Int J Soc Psychiatry. 2021;67(3):290–7. doi: 10.1177/0020764020950775 [DOI] [PubMed] [Google Scholar]
- 140.Srivastava A, Davis JP, Patel P, Daniel EE, Karkal S, Rice E. Polyvictimization, sex work, and depressive symptoms among transgender women and men who have sex with men. J Interpers Violence. 2021;37(13–14):NP11089–109. doi: 10.1177/0886260521990840 [DOI] [PubMed] [Google Scholar]
- 141.Jethwani KS, Mishra SV, Jethwani PS, Sawant NS. Surveying Indian gay men for coping skills and HIV testing patterns using the internet. J Postgrad Med. 2014;60(2):130–4. doi: 10.4103/0022-3859.132315 [DOI] [PubMed] [Google Scholar]
- 142.Singh LK, Srivastava K. Depression and quality of life in homosexual and heterosexual youth. Indian J Community Psychol. 2018;14(1):180–5. [Google Scholar]
- 143.Mogasale V, Wi TC, Das A, Kane S, Singh AK, George B, et al. Quality assurance and quality improvement using supportive supervision in a large-scale STI intervention with sex workers, men who have sex with men/transgenders and injecting-drug users in India. Sex Transm Infect. 2010;86(Suppl 1):i83–8. doi: 10.1136/sti.2009.038364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Chakrapani V, Newman PA, Shunmugam M, Dubrow R. Barriers to free antiretroviral treatment access among kothi-identified men who have sex with men and aravanis (transgender women) in Chennai, India. AIDS Care. 2011;23(12):1687–94. doi: 10.1080/09540121.2011.582076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Gurung A, Narayanan P, Prabhakar P, Das A, Ranebennur V, Tucker S, et al. Large-scale STI services in Avahan improve utilization and treatment seeking behaviour amongst high-risk groups in India: An analysis of clinical records from six states. BMC Public Health. 2011;11(Suppl 6):S10. doi: 10.1186/1471-2458-11-s6-s10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Woodford MR, Newman PA, Chakrapani V, Shunmugam M, Kakinami L. Correlates of HIV testing uptake among kothi-identified men who have sex with men in public sex environments in Chennai, India. AIDS Behav. 2012;16(1):53–62. [DOI] [PubMed] [Google Scholar]
- 147.Beattie TSH, Bhattacharjee P, Suresh M, Isac S, Ramesh BM, Moses S. Personal, interpersonal and structural challenges to accessing HIV testing, treatment and care services among female sex workers, men who have sex with men and transgenders in Karnataka state, South India. J Epidemiol Community Health. 2012;66(Suppl 2):ii42–48. doi: 10.1136/jech-2011-200475 [DOI] [PubMed] [Google Scholar]
- 148.Pina C, Dange A, Rawat S, Jadhav U, Arnsten JH, Chhabra R, et al. Antiretroviral treatment uptake and adherence among men who have sex with men and transgender women with HIV in Mumbai, India: A cross-sectional study. J Assoc Nurses AIDS Care. 2018;29(2):310–316. doi: 10.1016/j.jana.2017.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Patel VV, Dange A, Rawat S, Arnsten JH, Pina C, Golub SA, et al. Barriers to HIV Testing Among Men Who Have Sex With Men in India Reached Online: Implications for Interventions. J Acquir Immune Defic Syndr. 2018;78(4):e30–e4. doi: 10.1097/QAI.0000000000001698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Samuel SR, Muragaboopathy V, Patil S. Transgender HIV status, self-perceived dental care barriers, and residents’ stigma, willingness to treat them in a community dental outreach program: Cross-sectional study. Special Care Dentistry. 2018;38(5):307–12. [DOI] [PubMed] [Google Scholar]
- 151.Ramesh S, Mehrotra P, Saggurti N. Contributions of an intensive HIV prevention programme in increasing HIV testing among men who have sex with men in Andhra Pradesh, India. Glob Public Health. 2015;10(4):474–84. doi: 10.1080/17441692.2014.1003571 [DOI] [PubMed] [Google Scholar]
- 152.Mehta SH, Lucas GM, Solomon S, Srikrishnan AK, McFall AM, Dhingra N, et al. HIV care continuum among men who have sex with men and persons who inject drugs in India: Barriers to successful engagement. Clin Infect Dis. 2015;61(11):1732–41. doi: 10.1093/cid/civ669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.McFall AM, Mehta SH, Srikrishnan AK, Lucas GM, Vasudevan CK, Celentano DD, et al. Getting to 90: Linkage to HIV care among men who have sex with men and people who inject drugs in India. AIDS Care. 2016;28(10):1230–9. doi: 10.1080/09540121.2016.1168915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Singh Y, Aher A, Shaikh S, Mehta S, Robertson J, Chakrapani V. Gender transition services for hijras and other male-to-female transgender people in India: Availability and barriers to access and use. Int J Transgend. 2014;15(1):1–15. [Google Scholar]
- 155.Woodford MR, Chakrapani V, Newman PA, Shunmugam M. Barriers and facilitators to voluntary HIV testing uptake among communities at high risk of HIV exposure in Chennai, India. Glob Public Health. 2016;11(3):363–79. doi: 10.1080/17441692.2015.1057757 [DOI] [PubMed] [Google Scholar]
- 156.Acharya S, Parthasarathy M, Palkar A, Keskar P, Setia MS. Barriers for Antiretroviral Therapy Adherence and Viral Suppression in Members of the Key Population in Mumbai, India: Implications for Interventions. Indian J Dermatol. 2021;66(4):378–85. doi: 10.4103/ijd.IJD_640_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Pandya A, Redcay A. Impact of COVID-19 on transgender women and hijra: Insights from Gujarat, India. Journal of human rights and social work. 2021(101730181):1–10. doi: 10.1007/s41134-021-00184-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Pollard R, Gopinath U, Reddy YA, Kumar BR, Mugundu P, Vasudevan CK, et al. HIV service delivery in the time of COVID-19: Focus group discussions with key populations in India. Journal of the International AIDS Soc. 2021;24 Suppl 6(101478566):e25800. doi: 10.1002/jia2.25800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Achuthan A. Gender-affirmative technologies and the contemporary making of gender in India. Econ Soc. 2021;50(3):423–47. [Google Scholar]
- 160.Kulkarni S, Lawande DD, Dharmadhikari S, Deshpande CM. Exploring the barriers for eye care among transgenders and commercial sex workers in Pune, Maharashtra. Indian J Ophthalmol. 2021;69(9):2277–81. doi: 10.4103/ijo.IJO_3480_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Kurian M, Manoj G. Transgenders in the Mainstream: Welfare Schemes in Kerala-Kochi Metro Rail Project, Education Programme, Health Clinics, and Old-Age Pension. Indian Journal of Gender Studies. 2021;28(2):167–87. [Google Scholar]
- 162.Ghosh GK, Biswas S, Ghosh P, Ganguly S, Saha MK. Motivation for adherence to antiretroviral therapy by transgender people living with HIV—A study in West Bengal, India. Indian J Public Health. 2020;64(Supplement):S79–S82. doi: 10.4103/ijph.IJPH_74_20 [DOI] [PubMed] [Google Scholar]
- 163.Tom L, Menon S. Living with the Norm: The Nirvanam ritual in South Indian transfeminine narratives of self and transition. Gay Lesbian Quarterly. 2021;27(1):39–59. [Google Scholar]
- 164.Ranade K, Chakravarty S. Conceptualising gay affirmative counselling practice in India: Building on local experiences of counselling with sexual minority clients. Indian J Soc Work. 2013;74(2):237–53. [Google Scholar]
- 165.Snyder H, Yeldandi VV, Prem Kumar G, Liao C, Lakshmi V, Gandham SR, et al. Field-based video pre-test counseling, oral testing, and telephonic post-test counseling: ณmplementation of an HIV field testing package among high-risk Indian men. AIDS Educ Prev. 2012;24(4):309–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Thomas B, Mimiaga MJ, Mayer KH, Closson EF, Johnson CV, Menon S, et al. Ensuring it works: a community-based approach to HIV prevention intervention development for men who have sex with men in Chennai, India. AIDS Educ Prev. 2012;24(6):483–99. doi: 10.1521/aeap.2012.24.6.483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Safren SA, Thomas BE, Mayer KH, Biello KB, Mani J, Rajagandhi V, et al. A pilot RCT of an intervention to reduce HIV sexual risk and increase self-acceptance among MSM in Chennai, India. AIDS Behav. 2014;18(10):1904–12. doi: 10.1007/s10461-014-0773-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Shaikh S, Mburu G, Arumugam V, Mattipalli N, Aher A, Mehta S, et al. Empowering communities and strengthening systems to improve transgender health: Outcomes from the Pehchan programme in India. J Int AIDS Soc. 2016;19(3 Suppl 2):20809. doi: 10.7448/IAS.19.3.20809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Solomon SS, Lucas GM, Celentano DD, McFall AM, Ogburn E, Moulton LH, et al. Design of the Indian NCA study (Indian national collaboration on AIDS): A cluster randomized trial to evaluate the effectiveness of integrated care centers to improve HIV outcomes among men who have sex with men and persons who inject drugs in India. BMC Health Serv Res. 2016;16(1):652. doi: 10.1186/s12913-016-1905-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Thomas B, Closson EF, Biello K, Menon S, Navakodi P, Dhanalakshmi A, et al. Development and open pilot trial of an HIV-prevention intervention integrating mobile-phone technology for male sex workers in Chennai, India. Arch Sec Behav. 2017;46(4):1035–46. doi: 10.1007/s10508-015-0665-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Mimiaga MJ, Thomas B, Biello K, Johnson BE, Swaminathan S, Navakodi P, et al. A pilot randomized controlled trial of an integrated in-person and mobile phone delivered counseling and text messaging intervention to reduce HIV transmission risk among male sex workers in Chennai, India. AIDS Behav. 2017;21(11):3172–81. doi: 10.1007/s10461-017-1884-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Roy A, Sharples M. Mobile game based learning: Can it enhance learning of marginalized peer educators? Int J Mob Blended Learn. 2015;7(1):1–12. [Google Scholar]
- 173.Venkatesan C, Subramanian T, Vijin PP, Nelson R, Shunmugam M, Kershaw T. Reducing sexual risk and promoting acceptance of men who have sex with men living with HIV in India: Outcomes and process evaluation of a pilot randomised multi-level intervention. Glob Public Health. 2020;15(3):438–51. doi: 10.1080/17441692.2019.1675081 [DOI] [PubMed] [Google Scholar]
- 174.Chakrapani V, Kaur M, Tsai AC, Newman PA, Kumar R. The impact of a syndemic theory-based intervention on HIV transmission risk behaviour among men who have sex with men in India: Pretest-posttest non-equivalent comparison group trial. Social science & medicine (1982). 2020(ut9, 8303205):112817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Patel VV, Rawat S, Dange A, Lelutiu-Weinberger C, Golub SA. An internet-based, peer-delivered messaging intervention for HIV testing and condom use among men who have sex with men in india (CHALO!): Pilot randomized comparative trial. JMIR Public Health Surveill. 2020;6(2):e16494. doi: 10.2196/16494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Eisingerich AB, Wheelock A, Gomez GB, Garnett GP, Dybul MR, Piot PK. Attitudes and acceptance of oral and parenteral HIV preexposure prophylaxis among potential user groups: a multinational study. PloS one. 2012;7(1):e28238. doi: 10.1371/journal.pone.0028238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Uthappa CK, Allam RR, Pant R, Pal S, Dinaker M, Oruganti G, et al. Pre-exposure prophylaxis: awareness, acceptability and risk compensation behaviour among men who have sex with men and the transgender population. HIV Med. 2018;19(4):243–51. doi: 10.1111/hiv.12572 [DOI] [PubMed] [Google Scholar]
- 178.Chakrapani V, Newman PA, Singhal N, Jerajani J, Shunmugam M. Willingness to participate in HIV vaccine trials among men who have sex with men in Chennai and Mumbai, India: A social ecological approach. PloS one. 2012;7(12):e51080. doi: 10.1371/journal.pone.0051080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Chakrapani V, Newman PA, Singhal N, Nelson R, Shunmugam M. "If it’s not working, why would they be testing it?": Mental models of HIV vaccine trials and preventive misconception among men who have sex with men in India. BMC Public Health. 2013;13(100968562):731. doi: 10.1186/1471-2458-13-731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Newman PA, Chakrapani V, Weaver J, Shunmugam M, Rubincam C. Willingness to participate in HIV vaccine trials among men who have sex with men in Chennai and Mumbai, India. Vaccine. 2014;32(44):5854–61. doi: 10.1016/j.vaccine.2014.08.043 [DOI] [PubMed] [Google Scholar]
- 181.McClarty LM, Lorway RR, Ramanaik S, Wylie J, Becker ML. Factors influencing frontline health service providers’ likelihood to recommend a future, preventive HIV vaccine to key populations in Karnataka, south India. Vaccine. 2015;33(5):656–63. doi: 10.1016/j.vaccine.2014.12.009 [DOI] [PubMed] [Google Scholar]
- 182.Chakrapani V, Newman PA, Shunmugam M, Mengle S, Varghese J, Nelson R, et al. Acceptability of HIV pre-exposure prophylaxis (PrEP) and implementation challenges among men who have sex with men in India: A qualitative investigation. AIDS Patient Care STDs. 2015;29(10):569–77. doi: 10.1089/apc.2015.0143 [DOI] [PubMed] [Google Scholar]
- 183.Ramanaik S, McClarty LM, Khan S, Ramesh BM, Doshi M, Becker ML, et al. Frontline health service providers’ perspectives on HIV vaccine trials among female sex workers and men who have sex with men in Karnataka, South India. PloS one. 2015;10(10):e0141822. doi: 10.1371/journal.pone.0141822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Mitchell KM, Prudden HJ, Washington R, Isac S, Rajaram SP, Foss AM, et al. Potential impact of pre-exposure prophylaxis for female sex workers and men who have sex with men in Bangalore, India: A mathematical modelling study. J Int AIDS Soc. 2016;19(1):20942. doi: 10.7448/IAS.19.1.20942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Chakrapani V, Newman PA, Shunmugam M, Mengle S, Nelson R, Rubincam C, et al. "Like holding an umbrella before it rains": Acceptability of future rectal microbicides among men who have sex with men in India-A modified technology acceptance model. Qual Health Res. 2017;27(8):1236–48. doi: 10.1177/1049732317697947 [DOI] [PubMed] [Google Scholar]
- 186.Schneider JA, Michaels S, Gandham SR, McFadden R, Liao C, Yeldandi VV, et al. A protective effect of circumcision among receptive male sex partners of Indian men who have sex with men. AIDS Behav. 2012;16(2):350–9. doi: 10.1007/s10461-011-9982-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Chakrapani V, Shunmugam M, Rawat S, Baruah D, Nelson R, Newman PA. Acceptability of HIV pre-exposure prophylaxis among transgender women in India: A qualitative investigation. AIDS Patient Care STDs. 2020;34(2):92–8. doi: 10.1089/apc.2019.0237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Chakrapani V, Newman PA, Cameron M, Shunmugam M, Roungprakhon S, Rawat S, et al. Willingness to use pre-exposure prophylaxis (PrEP) and preferences among men who have sex with men in Mumbai and Chennai, India: A discrete choice experiment. AIDS Behav. 2021;25(10):3074–84. doi: 10.1007/s10461-021-03253-5 [DOI] [PubMed] [Google Scholar]
- 189.Belludi A, McFall AM, Solomon SS, Celentano DD, Mehta SH, Srikrishnan AK, et al. Awareness of and willingness to use pre-exposure prophylaxis (PrEP) among people who inject drugs and men who have sex with men in India: Results from a multi-city cross-sectional survey. PLoS One. 2021;16(2):e0247352. doi: 10.1371/journal.pone.0247352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Chakrapani V, Newman PA, Shunmugam M, Rawat S, Baruah D, Nelson R, et al. PrEP eligibility, HIV risk perception, and willingness to use PrEP among high-risk men who have sex with men in India: A cross-sectional survey. AIDS Care. 2021(8915313, a1o):1–9. doi: 10.1080/09540121.2021.1887801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Rao A, Patil S, Aheibam S, Kshirsagar P, Hemade P, Panda S. Acceptability of HIV oral self-test among men having sex with men and transgender population: A qualitative investigation from Pune, India. Infectious diseases. 2020;13(101603964):1178633720962809. doi: 10.1177/1178633720962809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Kazemian P, Costantini S, Kumarasamy N, Paltiel AD, Mayer KH, Chandhiok N, et al. The Cost-effectiveness of human immunodeficiency virus (HIV) preexposure prophylaxis and hiv testing strategies in high-risk groups in India. Clin Infect Dis. 2020;70(4):633–42. doi: 10.1093/cid/ciz249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Chakrapani V, Shaikh S, Arumugam V, Chawla U, Mehta S. Factors influencing willingness to use human immunodeficiency virus preexposure prophylaxis among transgender women in India. Transgend Health. 2021;6(2):64–73. doi: 10.1089/trgh.2019.0076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Bowling J, Dodge B, Banik S, Bartelt E, Rawat S, Guerra-Reyes L, et al. A multi-method study of health behaviours and perceived concerns of sexual minority females in Mumbai, India. Sex Health. 2018;15(1):29–38. doi: 10.1071/SH17042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Apoorva B, Thomas E. Interpersonal experiences of lesbians with their parent’s: An interpretative phenomenological analysis. J Psychosoc Res. 2016;11(2):251–8. [Google Scholar]
- 196.Chithrangathan C. Mapping the bisexual experience of a Keralite woman: Glimpses into India. Sex Relation Ther. 2018;33(1–2):135–45. [Google Scholar]
- 197.Banerjea N. Critical urban collaborative ethnographies: Articulating community with Sappho for Equality in Kolkata, India. Gender Place Culture. 2015;22(8):1058. [Google Scholar]
- 198.Bowling J. Perceived health concerns among sexual minority women in Mumbai, India: An exploratory qualitative study. Cult Health Sex. 2016;18(7):826–40. doi: 10.1080/13691058.2015.1134812 [DOI] [PubMed] [Google Scholar]
- 199.Bowling J. Social support relationships for sexual minority women in Mumbai, India: A photo elicitation interview study. Cult Health Sex. 2018;20(2):183–200. doi: 10.1080/13691058.2017.1337928 [DOI] [PubMed] [Google Scholar]
- 200.Srivastava S. Resilience in the lives of sexual minority women dealing with twofold peril in India. Cult Health Sex. 2021:23(9);1302–12. doi: 10.1080/13691058.2020.1805022 [DOI] [PubMed] [Google Scholar]
- 201.Bowling J, Blekfeld-Sztraky D, Simmons M, Dodge B, Sundarraman V, Lakshmi B, et al. Definitions of sex and intimacy among gender and sexual minoritised groups in urban India. Cult Health Sex. 2019. doi: 10.1080/13691058.2019.1614670 [DOI] [PubMed] [Google Scholar]
- 202.Bowling J, Simmons M, Dodge B, Sundarraman V, Brindaa L, Dharuman ST, et al. Family formation goals among sexual and gender minority individuals in urban India. Stud Fam Plann. 2019;50(4):357–73. doi: 10.1111/sifp.12102 [DOI] [PubMed] [Google Scholar]
- 203.Chakrapani V, Scheim AI, Newman PA, Shunmugam M, Rawat S, Baruah D, et al. Affirming and negotiating gender in family and social spaces: Stigma, mental health and resilience among transmasculine people in India. Cul Health Sex. 2021(100883416):1–17. doi: 10.1080/13691058.2021.1901991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Majumder A, Chatterjee S, Bhattacharjee K. Exploring cross-sectional predictors of suicide ideation, attempt, and risk in gender incongruent adults in India. Indian J Endocrinol Metab. 2021;25(2):103–9. doi: 10.4103/ijem.IJEM_100_21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Das A. ‘Aching to be a boy’: A preliminary analysis of gender assignment of intersex persons in India in a culture of son preference. Bioethics. 2020;34(6):585–92. doi: 10.1111/bioe.12750 [DOI] [PubMed] [Google Scholar]
- 206.Joseph AA, Kulshreshtha B, Shabir I, Marumudi E, George TS, Sagar R, et al. Gender issues and related social stigma affecting patients with a disorder of sex development in India. Arch Sex Behav. 2017;46(2):361–7. doi: 10.1007/s10508-016-0841-0 [DOI] [PubMed] [Google Scholar]
- 207.Caceres BA, Jackman KB, Ferrer L, Cato KD, Hughes TL. A scoping review of sexual minority women’s health in Latin America and the Caribbean. Int J Nurs Stud. 2019;94:85–97. doi: 10.1016/j.ijnurstu.2019.01.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Muller A, Hughes TL. Making the invisible visible: A systematic review of sexual minority women’s health in Southern Africa. BMC Public Health. 2016;16:307. doi: 10.1186/s12889-016-2980-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Scheim A, Kacholia V, Logie C, Chakrapani V, Ranade K, Gupta S. Health of transgender men in low-income and middle-income countries: A scoping review. BMJ Global Health. 2020;5(11):e003471. doi: 10.1136/bmjgh-2020-003471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Ayhan CHB, Bilgin H, Uluman OT, Sukut O, Yilmaz S, Buzlu S. A systematic review of the discrimination against sexual and gender minority in health care settings. Int J Health Serv. 2020;50(1):44–61. doi: 10.1177/0020731419885093 [DOI] [PubMed] [Google Scholar]
- 211.Zeeman L, Aranda K. A systematic review of the health and healthcare inequalities for people with intersex variance. Int J Environ Res Public Health. 2020;17(18). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Jones T. Intersex studies: A systematic review of international health literature. SAGE Open. 2018;8(2):2158244017745577. [Google Scholar]
- 213.NACO. Sankalak: Status of National AIDS Response. New Delhi: National AIDS Control Organization. Ministry of Health and Family Welfare, Government of India.; 2021. [Google Scholar]
- 214.Northridge ME, McGrath BP, Krueger SQ. Using community-based participatory research to understand and eliminate social disparities in health for lesbian, gay, bisexual, and transgender populations. In: Meyer IH, Northridge ME, editors. The Health of Sexual Minorities: Public Health Perspectives on Lesbian, Gay, Bisexual and Transgender Populations. Boston, MA: Springer US; 2007. p. 455–70. [Google Scholar]
- 215.NIH. NIH Strategic Plan to Advance Research on the Health and Well-being of Sexual and Gender Minorities FYs 2021–2025 2020. Available from: https://dpcpsi.nih.gov/sites/default/files/SGMStrategicPlan_2021_2025.pdf.
- 216.Chakrapani V, Lakshmi PVM, Tsai AC, Vijin PP, Kumar P, Srinivas V. The syndemic of violence victimisation, drug use, frequent alcohol use, and HIV transmission risk behaviour among men who have sex with men: Cross-sectional, population-based study in India. SSM Popul Health. 2019;7:100348. doi: 10.1016/j.ssmph.2018.100348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Chakrapani V, Newman PA, Shunmugam M, McLuckie A, Melwin F. Structural violence against Kothi-identified men who have sex with men in Chennai, India: A qualitative investigation. AIDS Educ Prev. 2007;19(4):346–64. doi: 10.1521/aeap.2007.19.4.346 [DOI] [PubMed] [Google Scholar]
- 218.Tan KKH, Treharne GJ, Ellis SJ, Schmidt JM, Veale JF. Gender minority stress: A critical review. J Homosex. 2020;67(10):1471–89. doi: 10.1080/00918369.2019.1591789 [DOI] [PubMed] [Google Scholar]
- 219.Sevelius J, Chakravarty D, Neilands TB, Keatley J, Shade SB, Johnson MO, et al. Evidence for the model of gender affirmation: The role of gender affirmation and healthcare empowerment in viral suppression among transgender women of color living with HIV. AIDS Behav. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Wesp LM, Malcoe LH, Elliott A, Poteat T. Intersectionality research for transgender health justice: A theory-driven conceptual framework for structural analysis of transgender health inequities. Transgend Health. 2019;4(1):287–96. doi: 10.1089/trgh.2019.0039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Marshall Z, Welch V, Minichiello A, Swab M, Brunger F, Kaposy C. Documenting research with transgender, nonbinary, and other gender diverse (Trans) individuals and communities: Introducing the global trans research evidence map. Transgend Health. 2019;4(1):68–80. doi: 10.1089/trgh.2018.0020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Flanagan SK, Peters HJ. Asexual-Identified Adults: Interactions with Health-Care Practitioners. Arch Sex Behav. 2020;49(5):1631–43. doi: 10.1007/s10508-020-01670-6 [DOI] [PubMed] [Google Scholar]
- 223.Streed CG Jr, Grasso C, Reisner SL, Mayer KH. Sexual orientation and gender identity data collection: Clinical and public health importance. Am J Public Health. 2020;110(7):991–3. [Google Scholar]
- 224.Grasso C, Goldhammer H, Funk D, King D, Reisner SL, Mayer KH, et al. Required sexual orientation and gender identity reporting by US health centers: First-year data. Am J Public Health. 2019;109(8):1111–8. doi: 10.2105/AJPH.2019.305130 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.