Highlights
-
•
Climate change, essentially due to global warming, the plundering of the earth's ecosystem.
-
•
Changing climatic circumstances may affect species' range and density.
-
•
Infectious disease can be seen as an outcome derived from multi-factorial correlates.
-
•
“One health” needs more attention, specially in regions more prone to environment.
Keywords: Infectious diseases, Environment, One health, Pathogenesis, Climate change
Dear editor,
Human activity significantly impacts the environment, and the converse, also being equally true, forms a vicious cycle. Evident baseline shifts in terms of increased frequency of peaking in various food/water-borne diseases, and zoonoses, including enzootic jumping species, are testimony enough to fairly assume a strong association between human dynamics and environmental correlates of these diseases. Limited resources and a lack of trained staff expose the strategic and performance gaps in the healthcare system. Most of these gaps lie in South-East Asia, comprising the population from developing countries (low and middle-income ones), including India, Sri Lanka, Bangladesh, Pakistan, Myanmar, etc. For these countries, the consequences are profound. Although we have had many infectious diseases in the last decade attributed to various causes, it is not far-fetched to say that the drastic environmental change has predisposed or precipitated a shift in baseline disease prevalence. For instance, the rise in floods in India, Nepal, and Bangladesh have had a temporal association with various diarrheal illnesses—like cholera—and is supported by the hypothesis of mixing contaminated human and animal fecal matter with water precipitating fecal-oral transmission of diseases [1].
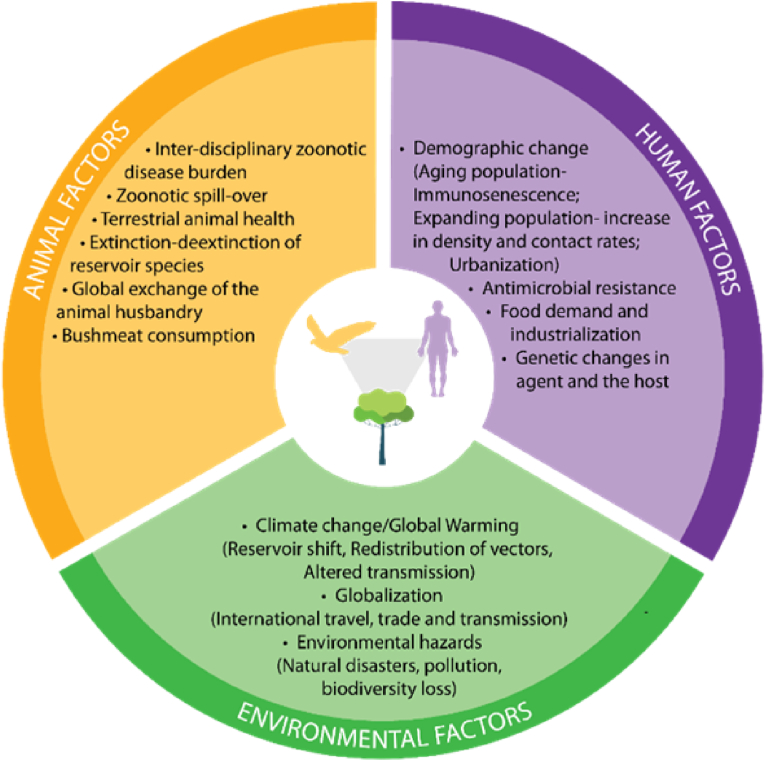
Virchow's coinage of the word ‘zoonoses’ was one of the first attempts to comprehensively understand infectious diseases that factored in human and animal biology variables. The concept of ‘One Health’, ‘One Medicine’, and ‘One World’ has been reshaped, revived, and refined into their contemporary understanding, which presents an idea where infectious disease can be seen as an outcome derived from multi-factorial correlates: animals, plants, ecosystems and the pathogens that thrive in it. This approach links the disease pathogenesis, environment, pathogens, vectors, and their hosts owing to the existing interdependent, integrated, and symbiotic eco-dynamics influencing disease prevalence and can lead to the formulation of health management strategies that are full-proof and broad spectrum (Fig. 1) [2].
Figure 1.
Environmental Correlates of Infectious Diseases and “One Health”. The One Health Concept signifies the interdependence and influence of environmental, human and animal factors in the epidemiological triangle of disease development. Cross-disciplinary collaboration for the management of infectious diseases is imperative to devise inclusive public health intervention.
Emerging and re-emerging pathogens are thought to be the sources of the ever-newer threats of infectious diseases. Climate change, essentially due to global warming, the plundering of the earth's ecosystem, rising urbanization, deforestation, and encroaching animal habitats shifting land-use patterns, will raise the likelihood of disease outbreaks in the future decades. There is growing evidence that climate change is increasing the incidence and distribution of certain infectious diseases, particularly those transmitted by vectors such as mosquitoes and ticks [2,3]. This can have a significant impact on public health and efforts to control the spread of these diseases. Climate change, in particular, may modify the global pathogen spectrum, enabling illnesses, especially vector-borne infections, to spread to new areas. Changing climatic circumstances may affect species' range and density, resulting in new interactions among species and an increased risk of zoonotic emergence. For example, warmer temperatures can expand the range of vectors like mosquitoes that carry malaria and dengue fever. In addition, climate change can affect the development and reproduction of vectors, leading to increased transmission of diseases. Rapid urbanization in low- and middle-income countries and a rise in people living in overcrowded, low-quality housing have provided the new potential for infectious disease outbreaks [3].
Another way in which climate change may impact infectious diseases is through changes in the frequency and intensity of extreme weather events. Natural disasters such as floods, hurricanes, and heatwaves can disrupt healthcare systems and create conditions conducive to spreading infectious diseases. For example, flooding can lead to the contamination of water sources and the proliferation of waterborne diseases, while heat waves can increase the risk of heatstroke and other heat-related illnesses. There are also potential indirect effects of climate change on infectious diseases. To cite an example, climate change may lead to changes in land use and agriculture, which can have knock-on effects on the prevalence of infectious diseases. Furthermore, climate change may lead to population displacement and migration, increasing the risk of disease transmission. Southeast Asia is virtually dominated by a tropical environment. The region is under immense environmental stress because of global warming, urbanization, deforestation, lack of water, and pollution. Since the 1960s, average temperatures in Southeast Asia have progressively increased through the decades. Myanmar, Thailand, Vietnam, and the Philippines are among the ten most impacted nations by climate change worldwide [4] The correlates for infectious diseases in the region have evolved significantly in line with the environmental changes. Among the WHO regions, South East Asia contributes 25% of the global burden of HIV and Tuberculosis and reports the second-highest incidence of Malaria globally. Furthermore, malnutrition renders South-East Asians prone to neglected tropical diseases (NTDs) - arbovirus infections, dengue, chikungunya, Japanese encephalitis, and pandemic influenza. The changes in climate, surroundings, microenvironment and macroenvironment have majorly transformed the present scenario [5].
The recent COVID-19 pandemic has highlighted the need for infectious disease control and pandemic preparedness protocols. We have primarily missed addressing the environmental correlates behind infectious diseases. The diseases considered endemic in a particular region may not be restricted to those regions forever. All infectious diseases are either directly or indirectly influenced by changes in the environment. Vector-borne diseases are directly impacted by changing vector-environment interaction, while water and food-borne diseases are influenced by climatic and environmental change. Inadequate knowledge of the environment-agent interactions that occur in human hosts during infections is one of the greatest barriers to devising effective control strategies against infectious illnesses, given the complex and unpredictable patterns of new diseases. Environmental factors influence the likelihood that humans will come into contact with infected vectors, although the degree to which they do so differs with the disease. Location of human habitation, employment, recreational activities, vector density, and external conditions all contribute to the likelihood of human infection. Improved knowledge of the intricate dynamics of infectious disease transmission and more effective approaches for preventing and controlling emerging infectious diseases would need future studies to include socioecological elements in tandem with climatic variables. To address these difficulties, it will be critical to undertake climate change mitigation and adaptation methods, such as initiatives to decrease greenhouse gas emissions, strengthen public health systems, and expand our knowledge of the link between the environment and infectious diseases. We see a pressing need to shift to an integrative and inclusive public health approach aimed at primary levels of prevention than a mitigative secondary preventive approach.
Author contributions
Yashendra Sethi: Conceptualization, Data curation, Writing-Original draft preparation, Writing- Reviewing and Editing. Nirja Kaka: Conceptualization, Data curation, Writing-Original draft preparation, Writing- Reviewing and Editing. Neil Patel: Data curation, Writing-Original draft preparation, Writing- Reviewing and Editing. Debabrata Roy: Conceptualization, Writing-Original draft preparation, Writing- Reviewing and Editing. Hitesh Chopra: Data curation, Writing-Original draft preparation, Writing- Reviewing and Editing. Talha Bin Emran: Writing- Reviewing and Editing, Visualization, Supervision. All authors critically revised the manuscript concerning intellectual content and approved the final manuscript.
Provenance and peer review
Not commissioned, internally peer-reviewed.
Handling Editor: Patricia Schlagenhauf
Contributor Information
Yashendra Sethi, Email: yashendrasethi@gmail.com.
Talha Bin Emran, Email: talhabmb@bgctub.ac.bd.
References
- 1.Ramana Dhara V., Schramm P.J., Luber G. Climate change & infectious diseases in India: implications for health care providers. Indian J Med Res. 2013;138:847. [PMC free article] [PubMed] [Google Scholar]
- 2.Gyles C. One medicine, one health, one World. Can Vet J. 2016;57:345. [PMC free article] [PubMed] [Google Scholar]
- 3.Baker R.E., Mahmud A.S., Miller I.F., Rajeev M., Rasambainarivo F., Rice B.L., et al. Infectious disease in an era of global change. Nat Rev Microbiol. 2021;20:4. doi: 10.1038/s41579-021-00639-z. 193–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Amit Prakash. The impact of climate change in Southeast Asia – IMF finance & development magazine. 2018. https://www.imf.org/en/Publications/fandd/issues/2018/09/southeast-asia-climate-change-and-greenhouse-gas-emissions-prakash September 2018.
- 5.Daszak P., Cunningham A.A., Hyatt A.D. Emerging infectious diseases of wildlife--threats to biodiversity and human health. Science. 2000;287:443–449. doi: 10.1126/SCIENCE.287.5452.443. [DOI] [PubMed] [Google Scholar]