Significance
The exact autoimmune mechanism responsible for causing Type 1 diabetes (T1D) remains unknown, but is thought to be a result of autoimmune activation by some potent self-antigen. A recent work isolated a unique cell set, termed the X-cell, that displays both T cell receptors (TCR) and B cell receptors (BCR) and encodes an autoantigen that produces a strong immune response in cells from T1D patients. Here, we explored the presentation of the autoantigen mutants to the HLA-TCR immune complex with a combined theoretical and experimental approach and identified several mutated sequences that modify HLA-antigen-TCR binding and therefore change immune responses. Specifically, we identify mutants that bind more strongly to the HLA and hold relevance to unique T1D immunotherapies.
Keywords: autoantigen design, molecular dynamics, free energy perturbation, type 1 diabetes, mutagenesis
Abstract
A previously reported autoreactive antigen, termed the X-idiotype, isolated from a unique cell population in Type 1 diabetes (T1D) patients, was found to stimulate their CD4+ T cells. This antigen was previously determined to bind more favorably than insulin and its mimic (insulin superagonist) to HLA-DQ8, supporting its strong role in CD4+ T cell activation. In this work, we probed HLA-X-idiotype-TCR binding and designed enhanced-reactive pHLA-TCR antigens using an in silico mutagenesis approach which we functionally validated by cell proliferation assays and flow cytometry. From a combination of single, double, and swap mutations, we identified antigen-binding sites p4 and p6 as potential mutation sites for HLA binding affinity enhancement. Site p6 is revealed to favor smaller but more hydrophobic residues than the native tyrosine, such as valine (Y6V) and isoleucine (Y6I), indicating a steric mechanism in binding affinity improvement. Meanwhile, site p4 methionine mutation to hydrophobic residues isoleucine (M4I) or leucine (M4L) modestly increases HLA binding affinity. Select p6 mutations to cysteine (Y6C) or isoleucine (Y6I) exhibit favorable TCR binding affinities, while a swap p5-p6 tyrosine–valine double mutant (V5Y_Y6V) and a p6-p7 glutamine–glutamine double mutant (Y6Q_Y7Q) exhibit enhanced HLA binding affinity but weakened TCR affinity. This work holds relevance to potential T1D antigen-based vaccine design and optimization.
Type 1 diabetes (T1D) is an autoimmune disease stemming from the cooperation of CD4+ and CD8+ T cells to destroy insulin-producing pancreatic -islet cells (1). The identity of immunodominant autoreactive pancreatic antigen(s) which stimulate the CD4+ T cell response remains unclear, though many antigens have been implicated including GAD65, HSP, ZnT8, PDX1, insulin, and neoantigens (2, 3), among others (4, 5). Large efforts have focused on insulin and associated neoantigens as the putative autoantigen (3, 6–8), with frustratingly elusive and complex results. For instance, insulin autoantigen binds HLA-DQ8, the serotype overrepresented in T1D patients (9–11), in both strong and weak registers (12), with a relatively weakly bound register being implicated in autoimmune recognition (13, 14). Recently, we discovered a unique lymphocyte that expressed a potent HLA-DQ8 autoantigen, termed the X-idiotype (15). This autoantigen was taken from a dominant BCR clonotype shared by three unrelated T1D subjects, indicating a potential pathology in T1D.
To further explore X-idiotype autoimmune recognition, it is necessary to understand HLA-X-idiotype-TCR binding. Though some work was presented toward this aim in our original publication (15), questions remain about the binding contribution from individual residues and the collective binding behavior. More importantly, a bigger question is whether we can learn from this information to design more potent mutants as potential antigen-based vaccines for immunotherapies (16–18). One way to explore this is to mutate key X-idiotype residues and quantify the binding affinity changes. Measuring binding affinities experimentally, through, for example, calorimetry techniques or binding assays, is costly and time-consuming. A complementary approach is to perform in silico mutagenesis studies using, for instance, machine learning models trained on sequence datasets and/or molecular mechanics techniques such as free energy perturbation (FEP) calculations. Although machine learning models of pHLA-TCR recognition (19–22) yield fast results and are increasingly powerful, they are limited to learning from finite sequence datasets. One of the advantages of the molecular mechanics FEP method is the ability to study each system de novo, without biases to existing pHLA-TCR sequencing data, however extensive. This flexibility is important for this work given the unique nature of the dual expresser cells from which the X-idiotype antigen and TCR are derived from. We have successfully employed FEP calculations to study a wide range of binding systems (23–26), including HLA-antigen-TCR binding (27–29). We have found that FEP calculations agree well with experiment and represent an inexpensive method to quantify mutational binding affinities.
In this work, we use FEP free energy calculations to study the HLA-DQ8-X-idiotype-TCR binding complex and design enhanced-reactive pHLA-TCR antigens which we validate by carboxyfluorescein succinimidyl ester (CFSE) cell proliferation experiments and flow cytometry assays. From naïve point mutations, we find that binding site p4 in the core epitope can be slightly improved by mutation from methionine to hydrophobic residues leucine (M4L) and isoleucine (M4I). Swap mutations and double mutations further reveal that tyrosine at p6 of the epitope can be mutated to a range of residues for HLA binding affinity improvement. The binding improvement of tyrosine at p6 is modestly correlated with residue size (Pearson’s R2 = 0.37 between binding affinity and residue volume), with a frustration analysis revealing that the native tyrosine p6 is highly frustrated with a frustration index of 1.5. Lastly, we find that several p6 mutants can increase pHLA-TCR affinity, while a swap p5-p6 tyrosine–valine (V5Y+Y6V) and a p6-p7 glutamine–glutamine (Y6Q+Y7Q) increase HLA affinity, but decrease pHLA-TCR affinity. These in silico predictions agree well with our experimental validations, revealing that all designed antigens increased CD69 activation and four out of seven antigens increased or maintained PBMC cell proliferation relative to the native X-idiotype antigen. Thus, this work holds important implications for T1D antigen immunotherapy design.
Results
Fig. 1 presents the antigen X-idiotype-bound HLA-DQ8 binary complex structure modeled in this work. Briefly, this antigen-bound complex structure was selected from 500 ns molecular dynamics (MD) simulations due to its stability based on RMSD analysis (SI Appendix, Fig. S1). After the initial MD simulations, only the HLA-α1 and HLA-β1 domains were modeled; α2 and β2 domains were excluded due to their distance from the antigen. The X-idiotype sequence is CARQEDTAMVYYFDYW with the core epitope highlighted in bold. From HLA-antigen contact analysis (Fig. 1B), the core epitope generally maintains high contact area with the HLA while the flanking N- and C-terminals are more solvent exposed, particularly the N-terminal. The exception is the Arg3′ residue in the N-terminal (here two residue numbering systems were adopted: 1′, 2′, 3′, … for the entire antigen; 1, 2, 3, … for the core epitope; see Fig. 1 caption for more details), which was previously observed to form an intricate salt bridge with HLA-β Gluβ86 residue (15). Anchor residues in the core epitope Asp1, Met4, Tyr6, and Asp9 are clearly visible from the contact analysis. Antigen residue Tyr7 forms an unexpectedly large contact area with HLA but is not considered a traditional anchor residue at p7. The Tyr7 sidechain interacts principally with HLA-β hydrophobic residues with the exception of Thrβ71, where Tyr7 interacts mostly with the peptide backbone (Fig. 1C).
Fig. 1.
HLA-bound X-idiotype structure. (A) HLA-bound X-idiotype structure I. side view and II. top view. X-idiotype epitope is shown in cyan with nonepitope residues in gray sticks and HLA in gray shadow. (B) HLA-bound X-idiotype residue solvent exposure. X-idiotype core epitope DTAMVYYFD is labeled sites 1 to 9, while the X-idiotype antigen (CARQEDTAMVYYFDYW) is labeled sites 1′, 2′, 3′..., 16′. Residue exposure reveals sites bound to HLA (R3′, Y7, and anchor residues D1, M4, Y6). (C) HLA interactions with X-idiotype residue Tyr7. Tyr7 is a nonanchor residue with disproportionately high contact area with the HLA as seen from (B). Tyr7 interacts with a mixture of polar, hydrophobic, and aromatic residues from HLA-β (pink). No Tyr7–HLA-α interactions are observed.
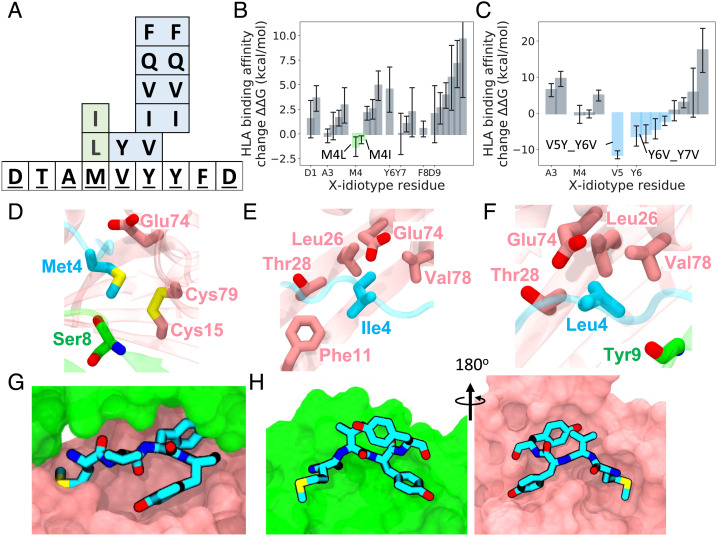
Fig. 2 presents enhanced HLA-antigen-binding affinity calculation results from antigen mutations. All binding affinities were computed using the free energy perturbation (FEP) method that our group has used with success in numerous investigations including antigen-HLA, and antigen–antibody interactions (15, 25, 27, 28, 30). For more information on the in silico mutagenesis studies using FEP, see Methods. Initial point mutations included similar-type residues (e.g. D1 -> E), residues determined previously to enhance antigen structural flexibility (e.g. Y7 -> G) (31), as well as many “educated guesses” from previous experiences with similar systems. SI Appendix, Table S1 shows a list of all computed mutations and binding affinities, including comprehensive categorical mutations for all anchor residues and residues of high contact area (position 7), which we added based on reviewer’s constructive feedback. Fig. 2B reveals that almost all our initial point mutations resulted in a loss of binding affinity; this remains on par with our previous works where only a low rate of the tested mutations turns out to be favorable. Interestingly, two substantially hydrophobic mutations of the same residue were found to be favorable: M4L with kcal/mol and M4I with kcal/mol, 95%CI (more discussions later with experimental validations using CFSE cell proliferation assays). Fig. 2 D–F illustrates the structural neighborhood of Met4 and favorable mutations Ile4 and Leu4. As an anchor residue, the long methionine sidechain is deeply buried into the HLA, with the hydrogen atoms of the terminal C interacting with the backbone carboxyl oxygen of HLA- Serα8. Methionine structure is also influenced by the unexpected juxtaposition of the sulfur atom interacting with the HLA- disulfide group Cysβ15-Cysβ79. Mutants Ile4 and Leu4 largely overlap in their interactions with Leuβ26, Thrβ28, Gluβ74, and Valβ78 of HLA- ; though each mutant coordinates the structure differently. A similar hydrophobic mutation, M4V, was tantalizingly unfavorable kcal/mol. Detailed analysis of Val4 mutant structure (SI Appendix, Fig. S2) reveals poor space-filling propensity and fewer interactions with the anchor pocket, lacking interactions with Thrβ28 and Valβ78 of HLA- . Most of the mutations on residues whose sidechains point away from the HLA, Ala3, and Phe8 were neutral in affinity change; this agrees with the large backbone interactions of these residues. Given the low success rate of point mutations, we next turned to double mutants and swap mutations to find enhanced binding affinity mutations.
Fig. 2.
X-idiotype mutation binding free energy results. (A) Favorable point mutations (green), swap and double mutations (blue) overlaid onto X-idiotype sequence. (B) The change in HLA binding free energy, G for point mutations. Favorable point mutations shown in green. (C) The change in HLA binding free energy G for swap and double mutations, with favorable mutations shown in blue. (B and C) Error bar is ±95% CI. (D) HLA interactions with native X-idiotype anchor residue p4 methionine. HLA- residues shown in green, HLA- in pink. (E and F) HLA interactions with mutated X-idiotype anchor residue p4 isoleucine (E) and leucine (F). (G and H) HLA interactions with native X-idiotype residues p4 to p7 MVYY. HLA- residues shown in green, HLA- in pink. (G) Top and (H) side views.
In our previous investigation of HLA antigen binding, we found that residue-swapping mutations, such as swapping antigen residues p5 and p6, successfully identified favorable mutations (31). We employed the same approach here with favorable binding affinity results along with other double mutants as shown in Fig. 2C (see SI Appendix, Table S2 for a complete list of double mutants tested). Initial residue-swapping mutations included p3-p4, p3-p7, p4-p5, p4-p7, p5-p6, and p3′-p4 epitope position mutations. Surprisingly, the p5-p6 swap mutation of Val5->Tyr and Tyr6->Val (V5Y_Y6V) was determined to be robustly favorable. This was unexpected, because from the contact area analysis in Fig. 1, Tyr6-Tyr7 forms large contact interfaces with the HLA during MD simulation. Our intuition led us to believe that this Tyr6-Tyr7 motif was largely stable and even a “required feature” for the x-idiotype antigen binding. However, numerous double mutants of Tyr6-Tyr7 quickly confirmed that this motif was improvable upon mutation. Not all double mutants were favorable, but generally hydrophobic mutations of the Tyr6-Tyr7 residues increased binding affinity, with the highest affinity increases resulting from Val5->Tyr + Tyr6->Val (V5Y_Y6V) and Tyr6->Val + Tyr7->Val (Y6V_Y7V). Fig. 2 G and H shows different stereo viewpoints of the epitope motif Met4-Val5-Tyr6-Tyr7. The deeply buried nature of Met4 and Tyr6 is readily apparent, as well as the large interaction Tyr7 forms with the HLA- “wall” of the binding groove.
Fig. 3 presents further exploration of the favorable double mutants of the Val5Tyr6Tyr7 triplet. From decomposition of the favorable Val5Tyr6Tyr7 double mutants, it is apparent that gains in binding affinity from Tyr6 mutations drive the enhanced binding affinity interactions. Val5 and Tyr7 mutations largely remain neutral to binding affinity, while the Tyr6 mutations see binding affinity improvements. Fig. 3 C–E illustrates the structure of Tyr6 as well as two mutants Val6 and Ile6. The binding pocket of Tyr6 includes both hydrophobic and aromatic residues: HLA- Leuα66 and HLA- Tyrβ9, Pheβ11, and Tyrβ30. However, in the next section, we show that the favorable Tyr6 mutants (Val, Ile, and Phe) are not solely explained by increased hydrophobic interactions. This explains why the dual hydrophilic/hydrophobic Tyr6Gln mutation (32) is also favorable in binding affinity.
Fig. 3.
X-idiotype double mutation decomposition and Tyr6 mutation free energy results. (A) Favorable double mutations of Tyr6 and decomposition to individual residues, errors are ±95% CI. (B) X-idiotype Tyr6 mutation binding affinity results in relation to residue volume and residue hydrophobicity. Volume relative to Tyr6 is computed as Vmut/VTyr with volumes from ref. 33. Eisenberg hydrophobicity scores from refs. 34, 35. Error bars are for affinity and represent ±95% CI. The R2 Pearson’s correlation shown at top left is correlation between binding affinity and relative volume. (C) Tyr6–HLA residue interactions with (D) Val6 mutant and (E) Ile6 mutant interactions. Native Tyr6 and mutants interact with same residue set.
Lastly, we sought to explore the mutation space of Tyr6 more rigorously by mutating Tyr6 to 13 different residues individually (see SI Appendix, Table S3 for a list) and computing binding affinity changes. The binding affinity changes are plotted in Fig. 3B. From this figure, and in agreement with our previous work (36, 37), we observe that there exists a distinct level of order between mutant binding affinity, residue volume from ref. 33, and residue hydrophobicity according to the Eisenberg hydrophobicity score (34, 35). Residue volume shows modest correlation with mutant affinity, resulting in a Pearson’s product moment correlation of R2 = 0.37. Surprisingly, Eisenberg hydrophobicity has no correlation with affinity, R2 = 0.02, though the strongest tyrosine mutants (Y6I, Y6V) are all hydrophobic or have mixed behavior (Y6C). In SI Appendix, Fig. S3, we present distributions of Pearson’s R2 values for affinity–volume and affinity–hydrophobicity correlations. These distributions more accurately capture the variance of R2 due to the reported 95%CI for each mutation. The reported values (R2 = 0.37 and R2 = 0.02) are roughly located in the center of the correlation distributions.
Fig. 4 presents antigen mutation effects on pHLA-TCR binding. Here, we modeled the TCR previously sequenced in dual expressor cells (15): TRAV29/DV5∗01/J53∗01 (TCRα-x) and TRBV6-5∗01/D1∗01, JB1-1∗01 (TCRβ-x), with the variable chain sequences reported in SI Appendix, Fig. S4. The TCR structure was built with Modeller (38) as described in the Methods. Similar to pHLA interactions, pHLA-TCR binding affinity was probed using FEP calculations following MD simulations. We were principally interested in enhanced HLA affinity X-idiotype mutations to understand how these mutants modulate TCR recognition. X-idiotype Tyr6 mutations Y6C and Y6I resulted in enhanced HLA-TCR binding affinity. As illustrated in Fig. 4 D–H, the HLA-X-idiotype assembly mostly contacts the TCRα. Each X-idiotype mutant results in a unique interaction profile with the TCR. Importantly, the HLA–TCR interaction leading to T cell activation is complex (39–41), and though correlations are observed (42), higher TCR binding affinity does not necessarily correspond with higher T cell functional activity. From a therapeutic perspective, unfavorable TCR binding may even be beneficial for autoimmune diseases, in the case of HLA-blocker type therapeutics, as shown in Celiac’s disease (43, 44). In this case, the X-idiotype mutants V5Y_Y6V and Y6Q_Y7Q are superior due to their enhanced binding affinity for HLA and reduced binding affinity for TCR. Other mutations that retain neutral TCR binding affinity changes (within the 95% CI), Y6V and Y6V_Y7V, may also be considered toward HLA-blocking or thymic deletion effects. In total, favorable HLA-binding X-idiotype mutants display varied binding interactions with TCR, offering latitude for researchers to test and select for desired effects on T cell activation.
Fig. 4.
X-idiotype Tyr6 TCR mutation free energy results. (A) HLA-X-idiotype-TCR structure with Tyr6 of X-idiotype in cyan. Only TCR variable domains were included for free energy analysis. (B) Favorable mutations of Tyr6 for HLA and TCR binding, error bars are ±95% CI. (C) TCR structure for the native Tyr6 with CDR3 loops highlighted. (D) TCR contact surface of HLA-X-idiotype assembly for the native Tyr6. (E–H) Mutational TCR contact surfaces for Tyr5_Val6, Cys6, and Ile6. TCRα shown in orange, TCRβ in yellow. The X-idiotype antigen is in gray sticks, except for enumerated residues in cyan. Note: contact surface represents HLA-TCR and X-idiotype-TCR contacts combined.
To validate our in silico predictions, we next carried out functional experiments with CFSE-based T cells proliferation assays. We tested the X-idiotype antigen as well as predicted enhanced affinity binders (Table 1) to determine if any sequence can induce an autoantigen response, which we measured by CD4 T cell expansion and anti-CD69 staining (Fig. 5). We labeled PBMCs isolated from a DQ8+ T1D subject with CFSE and assessed the proliferation of T cells in response to each peptide. In parallel, we cultured PBMCs with no antigen and in the presence of anti-CD3-CD28 antibody to serve as negative and positive controls, respectively.
Table 1.
Amino acid sequences of antigenic peptides derived from the original CDR3 sequence of x-clonotype (X-idiotype) along with an insulin superagonist termed insulin-mimotope
| x-Id | CARQEDTAMVYYFDYW | x-Id |
|---|---|---|
| x-Id-mutant-1 | CARQEDTAMYVYFDYW | M1 |
| x-Id-mutant-2 | CARQEDTAMVVVFDYW | M2 |
| x-Id-mutant-3 | CARQEDTAMVQQFDYW | M3 |
| x-Id-mutant-4 | CARQEDTAMVCYFDYW | M4 |
| x-Id-mutant-5 | CARQEDTAMVVYFDYW | M5 |
| x-Id-mutant-6 | CARQEDTAMVIYFDYW | M6 |
| x-Id-mutant-7 | CARQEDTAMVRRFDYW | M7 |
| Insulin-mimotope | SHLVEALYLVCGEEG | Ins-mim |
Amino acid mutations are highlighted in red.
Fig. 5.
(A) Representative dot plots show CFSE dilution by gated CD4 T cells among PBMCs from DQ8+ T1D subject that were used at readout (see Table 1 for X-idiotype mutants). Numbers indicate percentages of gated CFSElow CD4 T cells. Uns represents unstimulated CD4 T cells. (B) Percentage of CFSElow CD4 T cells in response to different antigens. (C) CD4 T cell expansion response to different peptides using the response of autologous unstimulated as the denominator. (D) Upregulation of CD69 by gated CFSElow CD4 T cells when compared with CFSEhigh CD4 T cells. (E) Fold change in cell surface CD69 by proliferated CD4 T cells compared with nonproliferated cells on stimulation with indicated peptides.
We used our standard gating strategy (15) to distinguish between proliferating (CFSElow) and nonproliferating (CFSEhigh) CD4 T cell subsets. All peptide antigens induced CD4 T cell proliferation compared with unstimulated CD4 T cells, albeit at different magnitudes (Fig. 5A). This indicates that all x-Id mutants maintained an immunogenic capacity. X-Id mutants M1, M2, M4, and M7 induce a similar or enhanced T cell response compared to the X-idiotype peptide (Fig. 5 B and C). These mutants, along with the X-Idiotype, serve as potent stimulators and expand CD4 T cell populations by four to sevenfold. X-Id mutants M3, M5, and M6 show reduced proliferation capacity as compared to the X-idiotype peptide. Despite differences in proliferation, all CD4 T cell populations were found to be functionally activated as measured by the upregulation of surface CD69 activation marker when compared with unstimulated cells (Fig. 5 D and E). For a comparison of in silico predictions and experimental results, see Discussion.
Discussion
There is an increased interest and push for T1D antigen-based immunotherapies (45). As Roep and colleagues (45) note, however, T1D is a heterogeneous disease involving numerous antigens. The recently discovered X-idiotype, an autoreactive antigen, provides hope for potential T1D immunotherapy. The extensive free energy simulations conducted here investigate X-idiotype residue binding contributions to the overall antigen affinity, which are further explored by our experimental cell proliferation assays. Specifically, we search for enhanced antigen-binding affinity mutants which could potentially have a therapeutic effect via resultant thymic deletion or HLA-blocking mechanisms.
From our in silico point mutation calculations, we find that the methionine in core epitope position p4 can be mutated for increased HLA binding affinity. In our initial exploration of enhanced antigen-binding mutants, we computed binding free energy changes of selected point mutations. We exhaustively computed binding free energy changes for all categorical point mutations of anchor residues (positions 1, 4, 6, and 9) as well as residues with high contact area (position 7), see SI Appendix, Table S1. Categorical mutations included either residues of the same charge (negatively charged aspartic acid residues p1 and p9 mutated to glutamic acid) or noncharged residues (residues p4, p6, and p7 mutated to the set of A, C, F, G, I, L, M, N, Q, S, T, V, W, Y, absent proline due to backbone mutational ambiguities). These calculations revealed enhanced binding affinity mutations of the methionine residue in anchor pocket p4. The p4 methionine is deeply buried and contacts an HLA disulfide bridge alongside hydrophobic residues. We found that mutation of methionine M4 to more hydrophobic residues isoleucine (M4I) and leucine (M4L) results in increased binding affinity and less clash with the large disulfide bonded atoms.
Swap mutation calculations reveal that the tyrosine in core epitope position p6 presents ample mutation opportunities for enhanced HLA binding affinity. We intuitively thought that the double tyrosine motif of p6-p7 was necessary for robust binding due to the intricate packing of the bound residues. However, swap mutation free energy results with enhanced binding affinity led us to reconsider our assumptions about this motif. We have previously found (31), and substantiate here, that swap mutations, such as swapping p5 and p6 residues, present an efficient technique to test HLA-antigen binding affinity and recommend them for future studies. Our swap FEP calculations revealed that tyrosine Y6 can be mutated to both hydrophobic and hydrophilic residues for stronger binding affinity. When we compare binding affinity to residue size, we find that smaller residues enhance binding affinity at the p6 site. This led us to suspect that there exists some structural frustration/steric penalty for the large tyrosine residue to bind the p6 anchor pocket. From a targeted frustration analysis (46, 47) (Methods), we found that the native p6 anchor tyrosine is highly frustrated, with a frustration index of 1.5. Interestingly, we do not observe binding affinity enhancement for the p7 tyrosine, where mutation either decreases or does not change affinity. This supports the importance of the HLA anchor residues in antigen binding (p1, p4, p6, and p9 for HAL-DQ8), as well as the amphiphilic nature of the p7 site. Notably, we do not run extensive MD simulations ( to account for any structural changes that could occur upon mutation (48). Single point mutations in proteins are known to cause sizeable changes in structure (49, 50); however, given that the antigen is deeply buried in the HLA binding pocket, drastic changes are not anticipated.
For pHLA-TCR affinity predictions, we tested a diverse set of p6 tyrosine mutants for pHLA-TCR affinity modulation (Table 1). The strongest predicted p6 pHLA-TCR binders, cysteine and isoleucine, expand the HLA–TCR interaction along the center of the TCRα chain. A p5-p6 swap mutant, V5Y_Y6V, and a p6-p7 double mutant, Y6Q_Y7Q, increase the HLA-X-idiotype binding affinity while decreasing pHLA-TCR affinity. This implies a reduced TCR activation for these mutants and offers a template for an HLA blocker-type therapeutic. Overall, our analysis revealed that similar to pHLA binding, mutation of the core epitope p6 to smaller hydrophobic/hydrophilic residues offered the best chance for HLA-DQ8-X-idiotype binding affinity improvement. Meanwhile, other p6 mutants (Y6V), a p5-p6 swap mutant and a p6-p7 double mutant, offer additional opportunities to modulate pHLA-TCR binding.
Our cell proliferation and flow cytometry experiments confirm that all predicted mutants activated T cells (measured by CD69) to a greater extent than the native X-idiotype and insulin mimic. However, CD4 T cell proliferation differs by one to sevenfold for the antigen mutants and holds only a relatively low correlation with predicted pHLA-TCR affinity (see SI Appendix, Fig. S5 for distributions of Pearson’s R2 values based on 95% CI). This correlation value, though low, agrees with success rates of our previous pHLA-TCR affinity maturation studies (15, 27, 28, 30) and is sufficient to identify enhanced and reduced binders in experiment. For instance, mutants M2 (Y6V_Y7V), M3 (Y6Q_Y7Q), M4 (Y6C), and M5 (Y6V) agree in average pHLA-TCR affinity trend to CD4 T cell proliferation (enhanced or reduced relative to X-idiotype), but their predicted 95% CIs overlap with zero affinity improvement, contesting a statement of conclusive agreement. The M1 (V5Y_Y6V) swap mutant and M6 (Y6I) point mutant diverge the most between modeling and experiment. We note that the predicted TCR contact interfaces of the M1 and M6 mutants are different from the native Tyr6 X-Idiotype (Fig. 4) and posit that we may not have captured important long-time regime pHLA-TCR conformational changes for these systems. The M7 (Y6R_Y7R) mutant was included in experiments to serve as a negative control, but unexpectedly achieved similar CD4 T cell proliferation and CD69 activation as the native X-Idiotype. Given the absence of charged residues in the p6 pocket of DQ8, we speculate that this mutant must undergo a register shift to bind and elicit a T cell response.
Mutants M3, M5, and M6, which have enhanced CD69 potency over the native X-Idiotype but reduced CD4 T cell proliferation, require special consideration. Here, we are principally optimizing pHLA-TCR binding by affinity maturation: mutating the antigen peptide to enhance pHLA-TCR binding. However, affinity maturation does not perfectly correlate with T cell activity (51) and in some cases can lead to off-target effects (52). An alternative technique to optimize the pHLA–TCR interaction for T cell activity is to enhance pHLA-TCR catch bonds (53). For this technique, pHLA-TCR systems with high CD69 activation but low affinity are optimized by adding polar and charged residues that form transient hydrogen bonds to enhance the pHLA–TCR catch bond interaction. Though here, we did not mutate residues outside of the contact interface, the M3, M5, and M6 mutants exhibit tantalizingly similar catch bond behavior of high activation with reduced CD4 T cell proliferation. We speculate that these antigen mutations may have enhanced catch bond formation and encourage additional study to understand the high CD69 activity but low CD4 T cell proliferation of these mutants.
Conclusion
Here, we explore the design of unique antigens based on the X-idiotype autoantigen identified in dual receptors, X-cells from T1D patients using a combined theoretical and experimental approach. We first run extensive MD simulations to obtain stable binary (HLA-antigen) and tertiary (HLA-antigen-TCR or pHLA-TCR) binding complex structures constructed from homology modeling. We then use free energy perturbation calculations to compute HLA binding affinity changes for point mutations, identifying Met4 as modestly improvable by mutation to Leu and Ile. From FEP calculations of swap mutations and double mutants, we determine that several mutations of residue Tyr6 at site p6 in the X-idiotype peptide can improve binding affinity. More specifically, mutation of Tyr6 to Val, Cys, and Ile results in large gains in HLA binding affinity as computed from FEP. We find a modest correlation in Tyr6 mutant binding affinity and residue size (R2 = 0.37), with generally smaller residues having improved HLA binding affinity. pHLA-TCR binding affinity calculations predict that several Tyr6 mutants additionally increase pHLA-TCR affinity, while a swap p5-p6 mutant V5Y_Y6V and a p6-p7 double mutant Y6Q_Y7Q increase HLA affinity but decrease pHLA-TCR affinity. These in silico predictions agree well with our CFSE-based T cells proliferation assays. Ultimately, our work demonstrates the residue by residue binding affinity contributions of the recently identified X-idiotype antigen implicated in T1D through in silico mutagenesis studies. These mutations, summarized in Table 1, particularly V5Y_Y6V, Y6V_Y7V, and Y6C, reveal opportunities for improved antigen binding and antigen immunotherapy design.
Methods
Computer Simulations.
Molecular dynamics simulations.
The HLA-X-idiotype antigen system was built as described previously (15) from PDB ID: 5UJT. Briefly, the intrinsic mimotope in the PDB structure was mutated to the X-idiotype antigen using VMD (54). The protein structure was then solvated with TIP3P water molecules and 100mM NaCl salt concentration. CHARMM36 (55) force field parameters were used for protein modeling. The structure was then minimized for 50,000 steps with heavy atom protein constraints and then an additional 50,000 steps without constraints. After 10 ns of equilibration, we simulated the system for 500 ns MD simulations at 310 K with a 2 fs time step. All simulations were run using NAMD2 (56, 57) on an IBM Power8 cluster.
The HLA-X-idiotype-TCR system was built from the 500ns MD structure of the HLA-X-idiotype system along with a Modeller (38) homology-built TCR structure of the TCR sequence from the dual expressor cells (X-cells) found in our previous work (15) (see SI Appendix, Fig. S4 for sequence information). Note that only the variable domains of the TCR were modeled. The TCR homology structure template was taken from PDB ID: 6DFX (8). The HLA-X-idiotype-TCR system was combined and aligned to the PDB ID: 6DFX structure. The protein assembly was then treated similarly to the HLA systems: solvated with TIP3P water molecules, ionized to 100 mM NaCl salt concentration, and parameterized to CHARMM36 protein force field. Minimization, equilibration, and production simulations followed the HLA simulation protocol described above. The native TCR contact surface shown in Fig. 4D comes from the last frame of the 500 ns production HLA-X-idiotype-TCR simulation, showing contacting TCR atoms within 4.5 Å of HLA-X-idiotype. The mutant contact surfaces in Fig. 4 E–H are from the last frame of FEP calculations, where the system was fully represented by the mutation residue.
A frustration analysis was conducted for site p6 of the pHLA system. Given that we calculated 13 mutational free energies for site p6, we used these values to compute the frustration index according to the SI Eq. 3 from ref (47). This equation, as well as the native (Y6) and 13 p6 amino acid mutational free energy values, is given in SI Appendix, Table S4. The single-residue-level frustration index was computed to be 1.5, meaning the native Y6 is unfavorable by 1.5× the SD of the average free energy of the other residues. Since the native Y6 is unfavorable by more than 1.0 SDs, the Y6 residue is highly frustrated according to ref. 47. Notably, Y6W is the only mutation more unfavorable and hence more frustrated than the native tyrosine.
Free energy perturbation.
After MD simulation, the final structure was selected based on rmsd analysis showing structural stability (<0.5 nm) for 300+ ns. Free energy perturbation calculations were computed similarly to our previous work (26) using a soft-core potential. All FEP calculations were conducted over a course of 34 windows with at least 200 ps per window for a total of 6.8 ns per calculation. Mutations that were found promising (enhanced binding affinity) from this initial round of FEP calculations were run for longer timescales for verification: M4L, V5Y, Y6V, Y6I, Y7W, and V5Y_Y6V HLA-X-idiotype FEP calculations and Y6C, Y6I, and Y6V_Y7V HLA-X-idiotype-TCR calculations were conducted over 34 windows with at least 1 ns per window for a total of 34 ns per calculation. These FEP calculations were computed with at least five replicas and averaged for the final G value, thus an aggregate of at least 34ns × 5 replicas × 2 states (bound, free) = 340 ns for each mutation. The total simulation time for this study is approximately 5 All error bars in this work are 95% CI.
Cell Preparation, Stimulation, and Further Processing.
Human subjects.
Blood samples were obtained from donor using protocols approved by the Johns Hopkins Institutional Review Board. We obtained the written informed consent from all the human subjects participated in the study. The criteria to include T1D subject were made based on meeting the American Diabetes Association criteria for classification and were recruited at Johns Hopkins Comprehensive Diabetes Center. Our subject study was conducted as per accordance with the Declaration of Helsinki principles. Peripheral blood mononuclear cells (PBMCs) were freshly isolated and prepared using our standard Ficoll-Paque density (GE Healthcare) gradient centrifugation method. The profiling of islet autoantibodies panel and HLA genotypes of the enrolled T1D subjects was performed at Autoantibody/HLA Core Service Center at the Barbara Davis Center for Childhood Diabetes.
Peptide design and synthesis.
Our previous work highlighted CDR3 sequence of x-clonotype is a potent CD4 T Cell Epitope. In this study, antigenic peptides, including different mutant version, derived from CDR3 sequence of x-clonotype were produced (Peptide 2.0). Peptide stock (2.0 mg/mL) was prepared by dissolving freeze-dried peptides in sterile water, kept at −80 °C. Working peptide solution was prepared by diluting with phosphate-buffered saline (PBS). Unless otherwise indicated, all antigenic peptides used in this study were purified (>95% purity). The original amino acid sequences of peptide derived from CDR3 sequence of x-clonotype along with indicated mutation are given in Table 1.
CFSE proliferation assay.
To test the effects of X-idiotype-derived peptides on the stimulation of T cells, we have used our established method as described previously (15). Briefly, freshly isolated PBMCs (as described above) were washed two times with prewarm (37 °C) 1x PBS in order to remove the serum that may affect staining and after washing step, PBMCs were resuspended in prewarm (37 °C) 1 × PBS at a density of 1.5 to 2.0 × 106 1 mM CFSE proliferation dye (eBioscience) for brief time (1 to 2 min) at 37 °C with continuous vortexing. The CFSE labeling reaction was stopped by quenching by adding chilled complete culture RPMI media. The labeled cells were washed twice again in 1 × PBS, and finally resuspended in RPMI complete media, and plated into 24-well tissue culture plates (1.5 to 2.0 × 106 cells/well in 1 mL complete culture medium). To evaluate the functionality of peptides, we added indicated X-idiotype-derived mutant variant peptides (table#) along with full X-idiotype and insulin-mimotope peptide as soluble antigen into wells of 24-well plates (10 mM) and examined their ability to stimulate CFSE-labeled CD4 T cells from among PBMCs. The CFSE-labeled cells without stimulation and with CD3-28 stimulation were taken as specific negative and positive controls, respectively. After 7 d of incubation, cell cultures were washed twice with RPMI complete media and stained for flowcytometry as indicated in Figure legends and proliferation was assessed by determining the frequency of CFSElow CD4 T cell population.
Flow cytometric analysis.
Flow data acquisition was carried out on an Attune-Nxt flow cytometer (Thermofisher). Around 400,000 to 500,000 lymphocytes (singlet gated) were acquired for each sample. For data analysis, TCRab+CD4+ events were gated and percentages of the total CD4+ were determined. Percentages of proliferated CD4 T cells in response to peptide stimulation were calculated by determining the percentage of CFSE-low events in corresponding gates from CD4+ subset. Whereas CFSE-high represents nonproliferated CD4 T cells. Unstimulated control samples were used as comparative internal control for peptide stimulated cell culture. We used anti-CD69 staining as a readout to evaluate the activation of CD4 T cells.
Supplementary Material
Appendix 01 (PDF)
Acknowledgments
We thank Qinglu Zhong, Hong Zhou, Lei Fu, and Dong Zhang for helpful discussions. This work was partially supported by the National Key R&D Program of China (2021YFF1200404 and 2021YFA1201200 to R.Z.), the National Natural Science Foundation of China (U1967217 to R.Z.), the Fundamental Research Funds for Central Universities (226-2022-00043, 226-2022-00192 to R.Z.), the National Independent Innovation Demonstration Zone Shanghai Zhangjiang Major Projects (ZJZX2020014 to R.Z.), the Starry Night Science Fund of Zhejiang University Shanghai Institute for Advanced Study (SN-ZJU-SIAS-003), BirenTech Research (BR-ZJU-SIAS-001 to R.Z.), Shanghai Artificial Intelligence Lab (P22KN00272 to R.Z.), and the W. M. Keck Foundation (Grant award 2019-2022 to A.R.A.H. and R.Z.).
Author contributions
A.R.A.H. and R.Z. designed research; Y.S., D.R.B., R.A., K.C.C., and S.L. performed research; A.R.A.H. and R.Z. contributed new reagents/analytic tools; Y.S., D.R.B., R.A., and K.C.C. analyzed data; and D.R.B., K.C.C., A.R.A.H., and R.Z. wrote the paper.
Competing interests
The authors declare no competing interest.
Footnotes
This article is a PNAS Direct Submission.
Contributor Information
Abdel Rahim A. Hamad, Email: ahamad@jhmi.edu.
Ruhong Zhou, Email: rz24@columbia.edu.
Data, Materials, and Software Availability
All study data are included in the article and/or SI Appendix.
Supporting Information
References
- 1.Garyu J. W., Meffre E., Cotsapas C., Herold K. C., Progress and challenges for treating Type 1 diabetes. J. Autoimmunity 71, 1–9 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Marrack P., Kappler J. W., Do MHCII-presented neoantigens drive type 1 diabetes and other autoimmune diseases? Cold Spring Harb. Perspect Med. 2, a007765–a007765 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Delong T., et al. , Pathogenic CD4 T cells in type 1 diabetes recognize epitopes formed by peptide fusion. Science 351, 711–714 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Han S., Donelan W., Wang H., Reeves W., Yang L.-J., Novel autoantigens in type 1 diabetes. Am. J. Transl. Res. 5, 379–392 (2013). [PMC free article] [PubMed] [Google Scholar]
- 5.Roep B. O., Peakman M., Antigen targets of type 1 diabetes autoimmunity. Cold Spring Harb. Perspect Med. 2, a007781–a007781 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wan X., et al. , Pancreatic islets communicate with lymphoid tissues via exocytosis of insulin peptides. Nature 560, 107–111 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang Y., et al. , C-terminal modification of the insulin B:11–23 peptide creates superagonists in mouse and human type 1 diabetes. Proc. Natl. Acad. Sci. U.S.A. 115, 162–167 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang Y., et al. , How C-terminal additions to insulin B-chain fragments create superagonists for T cells in mouse and human type 1 diabetes. Sci. Immunol. 4, eaav7517 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Erlich H., HLA DR-DQ haplotypes and genotypes and type 1 diabetes risk: Analysis of the type 1 diabetes genetics consortium families. Diabetes 57, 1084–1092 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Noble J. A., Erlich H. A., Genetics of type 1 diabetes. Cold Spring Harb. Perspect. Med. 2, a007732–a007732 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Koeleman B. P. C., et al. , Genotype effects and epistasis in type 1 diabetes and HLA-DQ trans dimer associations with disease. Genes Immunity 5, 381–388 (2004). [DOI] [PubMed] [Google Scholar]
- 12.Mohan J. F., Petzold S. J., Unanue E. R., Register shifting of an insulin peptide–MHC complex allows diabetogenic T cells to escape thymic deletion. J. Exp. Med. 208, 2375–2383 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Levisetti M. G., Suri A., Petzold S. J., Unanue E. R., The insulin-specific T cells of nonobese diabetic mice recognize a weak MHC-binding segment in more than one form. J. Immunol. 178, 6051–6057 (2007). [DOI] [PubMed] [Google Scholar]
- 14.Stadinski B. D., et al. , Diabetogenic T cells recognize insulin bound to IAg7 in an unexpected, weakly binding register. Proc. Natl. Acad. Sci. U.S.A. 107, 10978–10983 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ahmed R., et al. , A public BCR present in a unique dual-receptor-expressing lymphocyte from type 1 diabetes patients encodes a potent T cell autoantigen. Cell 177, 1583–1599.e16 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lernmark Å., Larsson H. E., Immune therapy in type 1 diabetes mellitus. Nat. Rev. Endocrinol. 9, 92–103 (2013). [DOI] [PubMed] [Google Scholar]
- 17.Stabler C. L., Li Y., Stewart J. M., Keselowsky B. G., Engineering immunomodulatory biomaterials for type 1 diabetes. Nat. Rev. Materials 4, 429–450 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Petrovsky N., Silva D., Schatz D. A., Vaccine therapies for the prevention of type 1 diabetes mellitus. Pediat. Drugs 5, 575–582 (2003). [DOI] [PubMed] [Google Scholar]
- 19.Dash P., et al. , Quantifiable predictive features define epitope-specific T cell receptor repertoires. Nature 547, 89–93 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Glanville J., et al. , Identifying specificity groups in the T cell receptor repertoire. Nature 547, 94–98 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lin X., et al. , Rapid assessment of T-cell receptor specificity of the immune repertoire. Nat. Comput. Sci. 1, 362–373 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhang W., et al. , A framework for highly multiplexed dextramer mapping and prediction of T cell receptor sequences to antigen specificity. Sci. Adv. 7, eabf5835 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chen S. H., Kang S.-G., Luo J., Zhou R., Charging nanoparticles: Increased binding of Gd@C82(OH)22 derivatives to human MMP-9. Nanoscale 10, 5667–5677 (2018). [DOI] [PubMed] [Google Scholar]
- 24.Kang H., Yang Z., Zhou R., Lanosterol disrupts aggregation of human γD-crystallin by binding to the hydrophobic dimerization interface. J. Am. Chem. Soc. 140, 8479–8486 (2018). [DOI] [PubMed] [Google Scholar]
- 25.Das P., Li J., Royyuru A. K., Zhou R., Free energy simulations reveal a double mutant avian H5N1 virus hemagglutinin with altered receptor binding specificity. J. Comput. Chem. 30, 1654–1663 (2009). [DOI] [PubMed] [Google Scholar]
- 26.Xia Z., Huynh T., Kang S.-G., Zhou R., Free-energy simulations reveal that both hydrophobic and polar interactions are important for influenza hemagglutinin antibody binding. Biophys. J. 102, 1453–1461 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Xia Z., et al. , The complex and specific pMHC interactions with diverse HIV-1 TCR clonotypes reveal a structural basis for alterations in CTL function. Sci. Rep. 4, 4087 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Joglekar A. V., et al. , T cell receptors for the HIV KK10 epitope from patients with differential immunologic control are functionally indistinguishable. Proc. Natl. Acad. Sci. 115, 1877–1882 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bessell C. A., et al. , Commensal bacteria stimulate antitumor responses via T cell cross-reactivity. JCI Insight 5, e135597 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chowell D., et al. , Patient HLA class I genotype influences cancer response to checkpoint blockade immunotherapy. Science 359, 582–587 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hölzemer A., et al. , Selection of an HLA-C*03:04-restricted HIV-1 p24 Gag sequence variant is associated with viral escape from KIR2DL3+ natural killer cells: Data from an observational cohort in South Africa. PLOS Med. 12, e1001900 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kang H., et al. , Emerging β-Sheet rich conformations in supercompact huntingtin exon-1 mutant structures. J. Am. Chem. Soc. 139, 8820–8827 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zamyatnin A. A., Protein volume in solution. Prog. Biophys. Mol. Biol. 24, 107–123 (1972). [DOI] [PubMed] [Google Scholar]
- 34.Eisenberg D., Weiss R. M., Terwilliger T. C., Wilcox W., Hydrophobic moments and protein structure. Faraday Symposia Chem. Soc. 17, 109–120 (1982). [Google Scholar]
- 35.Eisenberg D., Weiss R. M., Terwilliger T. C., The helical hydrophobic moment: a measure of the amphiphilicity of a helix. Nature 299, 371–374 (1982). [DOI] [PubMed] [Google Scholar]
- 36.Bell D. R., Chen S. H., Toward guided mutagenesis: Gaussian process regression predicts MHC class II antigen mutant binding. J. Chem Inf. Model 61, 4857–4867 (2021). [DOI] [PubMed] [Google Scholar]
- 37.Bell D. R., et al. , Dynamics-based peptide–MHC Binding optimization by a convolutional variational autoencoder: A use-case model for CASTELO. J. Chem. Theory Comput. 17, 7962–7971 (2021). [DOI] [PubMed] [Google Scholar]
- 38.Webb B., et al. , Integrative structure modeling with the Integrative Modeling Platform. Protein Sci. 27, 245–258 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Harrison D. L., Fang Y., Huang J., T-cell mechanobiology: Force sensation, potentiation, and translation. Front. Phys. 7, 45 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pullen R. H., Abel S. M., Catch bonds at T cell interfaces: Impact of surface reorganization and membrane fluctuations. Biophys. J. 113, 120–131 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Stone J. D., Chervin A. S., Kranz D. M., T-cell receptor binding affinities and kinetics: impact on T-cell activity and specificity. Immunology 126, 165–176 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cole D. K., et al. , Hotspot autoimmune T cell receptor binding underlies pathogen and insulin peptide cross-reactivity. J. Clin. Inves. 126, 2191–2204 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Xia J., Siegel M., Bergseng E., Sollid L. M., Khosla C., Inhibition of HLA-DQ2-mediated antigen presentation by analogues of a high affinity 33-residue peptide from alpha2-gliadin. J. Am. Chem. Soc. 128, 1859–1867 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sollid L. M., Khosla C., Novel therapies for coeliac disease. J. Intern. Med. 269, 604–613 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Roep B. O., Wheeler D. C. S., Peakman M., Antigen-based immune modulation therapy for type 1 diabetes: The era of precision medicine. Lancet Diabetes Endocrinol. 7, 65–74 (2019). [DOI] [PubMed] [Google Scholar]
- 46.Chen M., et al. , Surveying biomolecular frustration at atomic resolution. Nat. Commun. 11, 5944 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ferreiro D. U., Hegler J. A., Komives E. A., Wolynes P. G., Localizing frustration in native proteins and protein assemblies. Proc. Natl. Acad. Sci. U.S.A. 104, 19819–19824 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chen S. H., Perez-Aguilar J. M., Zhou R., Graphene-extracted membrane lipids facilitate the activation of integrin αvβ8. Nanoscale 12, 7939–7949 (2020). [DOI] [PubMed] [Google Scholar]
- 49.Chen S.-H., Elber R., The energy landscape of a protein switch. Phys. Chem. Chem. Phys. 16, 6407–6421 (2014). [DOI] [PubMed] [Google Scholar]
- 50.Chen S.-H., Meller J., Elber R., Comprehensive analysis of sequences of a protein switch. Protein Sci. 25, 135–146 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sibener L. V., et al. , Isolation of a structural mechanism for uncoupling T cell receptor signaling from peptide-MHC binding. Cell 174, 672–687.e27 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cameron B. J., et al. , Identification of a titin-derived HLA-A1– Presented peptide as a cross-reactive target for engineered MAGE A3– Directed T cells. Sci. Trans. Med. 5, 197ra103 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zhao X., et al. , Tuning T cell receptor sensitivity through catch bond engineering. Science 376, eabl5282 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Humphrey W., Dalke A., Schulten K., VMD: Visual molecular dynamics. J. Mol. Graphics 14, 33–38 (1996). [DOI] [PubMed] [Google Scholar]
- 55.Huang J., MacKerell A. D. Jr., CHARMM36 all-atom additive protein force field: Validation based on comparison to NMR data. J. Comput. Chem. 34, 2135–2145 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kumar S., et al. , Scalable molecular dynamics with NAMD on the IBM Blue Gene/L System. IBM J. Res. Dev. 52, 177–188 (2008). [Google Scholar]
- 57.Phillips J. C., et al. , Scalable molecular dynamics with NAMD. J. Comput. Chem. 26, 1781–1802 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix 01 (PDF)
Data Availability Statement
All study data are included in the article and/or SI Appendix.