Abstract
Objectives
Fatigue is common in patients with chronic liver disease; however, its pathogenesis is unclear. This study aimed to provide insights into the pathogenesis of chronic liver disease-related fatigue by assessing the relationship between fatigue and the degree of inflammation in chronic liver disease.
Design
We performed a cross-sectional study of 1374 patients with pathologically proven chronic liver disease diagnosed at the Affiliated Hospital of Hangzhou Normal University in Hangzhou, China.
Setting
Primary single-centre study.
Participants
One thousand three hundred and seventy-four patients with liver biopsy-proven chronic liver disease.
Interventions
The patients were divided into fatigue and non-fatigue groups according to the Chronic Liver Disease Questionnaire. Propensity score matching was used to match the baseline features of the patients in the two groups.
Primary and secondary outcome measures
Liver steatosis, ballooning, inflammation and fibrosis were measured according to the pathological results of liver biopsy. Fatigue was measured using the Chronic Liver Disease Questionnaire.
Results
Of the 1374 patients, 262 (19.67%) experienced fatigue. There were 242 and 484 patients with and without fatigue, respectively, who were successfully matched for sex, age and classification of chronic liver disease by propensity score matching. After matching, the fatigue group showed higher liver enzyme levels, inflammation grades and fibrosis stages than the non-fatigue group (p<0.05). Multivariate analysis showed that age (OR: 2.026; p=0.003), autoimmune liver disease (OR: 2.749; p=0.002) and active inflammation (OR: 1.587; p=0.003) were independent risk factors for fatigue after adjusting for confounders. The OR of the risk for fatigue increased in a stepwise manner with increasing inflammation grade in young-aged and middle-aged patients (p<0.05). This tendency was not observed in elderly patients (p>0.05).
Conclusion
Patients with chronic liver disease were burdened by fatigue, which increased progressively with rising liver inflammation severity in young-aged and middle-aged rather than elderly patients.
Keywords: Hepatology, Histopathology, Health & safety
STRENGTHS AND LIMITATIONS OF THIS STUDY.
This study was the first comprehensive assessment of the relationship between fatigue and the severity of liver inflammation in a large sample of liver biopsy-proven chronic liver disease.
Propensity score matching was used to exclude the influence of gender, age, blood pressure, blood glucose, liver function and composition ratio of patients with chronic liver disease.
Since this is a retrospective study, some data that could contribute to the development of fatigue, namely plasma iron level, markers of thyroid gland function and blood oxygen tension, are missing.
An important limitation is the dichotomic division of the chronic liver diseases population into suffering and not-suffering from fatigue with no self-assessment of fatigue severity.
Due to the cross-sectional study design, we have not been able determine the causal relationship between the severity of inflammation and fatigue.
Introduction
Chronic liver disease (CLD) affects approximately 1.5 billion people worldwide. The prevalence of CLD is rising rapidly owing to the ongoing impact of viral hepatitis and the rapidly increasing incidence of non-alcoholic fatty liver disease (NAFLD).1–3 Fatigue is commonly experienced by patients with CLD and significantly impairs their quality of life.4 The findings of previous studies suggest that the impact of fatigue on patients with CLD can be substantial,5 with patients reporting that it interferes with several aspects of their lives, including physical activities, family life and job performance.6 These issues add to the personal and societal burdens associated with CLD and indirectly contribute to financial costs. In addition to affecting quality of life, CLD-related fatigue has a negative impact on survival. In a 4-year follow-up study of patients with primary biliary cholangitis (PBC), fatigue was associated with poor outcomes, as patients with higher fatigue scores at the start of the study period had significantly lower survival rates.7
It is difficult to characterise, define and treat fatigue because it encompasses a complex interaction between biological, psychosocial and behavioural processes.8 9 Our understanding of CLD-related fatigue is still incomplete and its pathogenesis remains unclear. The most common view is that there are peripheral pathways between the liver and the brain that, when activated, lead to changes in neurotransmission within the brain and the development of disease-related behaviours, including fatigue.10–12 Better understanding of the relationship between fatigue and liver histology features in different CLD populations may provide further evidence of the mechanism underlying liver disease-related fatigue and facilitate the development of specific and appropriate treatment for it.
In this study, we explored the risk factors for fatigue in CLD by comparing the clinical and histological features of patients with and without fatigue using a large cohort of patients with biopsy-proven CLD. In addition, we analysed the correlation between the severity of liver histology features and CLD-related fatigue in different CLD populations.
Methods
Patients and study design
This was a cross-sectional study of patients with pathologically proven CLD, including NAFLD, alcoholic liver disease (ALD), PBC, primary sclerosing cholangitis (PSC), autoimmune hepatitis (AIH), chronic hepatitis B (CHB) and CHB with fatty liver, diagnosed at the Affiliated Hospital of Hangzhou Normal University in Hangzhou, China between 2011 and 2021. Patients with the following conditions were excluded: psychiatric or mental disorders, or cognitive difficulties that could hinder reliable description of symptoms; CLD combined with any other chronic disorders that may affect fatigue; causes of CLD other than NAFLD, ALD, autoimmune liver diseases (AILDs) (including PBC, PSC, AIH) and CHB; and past COVID-19 infection. The included patients were divided into fatigue and non-fatigue groups according to the presence or absence of fatigue.
Clinical examination and biochemical analysis
The clinical examination consisted of a physical examination and a health habit assessment, which were performed by professional physicians. Diastolic blood pressure, systolic blood pressure, height and body weight were measured according to standard protocols. Body mass index (BMI) was calculated as weight (kg) divided by height (m) squared (kg/m2). Blood samples were collected after 8 hours of fasting within 1 week before liver biopsy, and the biochemical tests performed included measurement of fasting plasma glucose, triglyceride, total cholesterol, high/low-density lipoprotein cholesterol (HDL-c), alanine aminotransferase (ALT), gamma-glutamyl-transferase (GGT), aspartate aminotransferase (AST), alkaline phosphatase, serum total bilirubin, albumin and glycated haemoglobin levels. The biochemical tests were performed using an automated biochemical analyser according to the manufacturer’s instructions (OLYMPUS, Japan AU5821+ISE; OLYMPUS).
Histological analysis
All liver biopsies were reassessed by three professional histopathologists who were blinded to patient details. The steatosis score (positive if >5%, according to the Brunt classification (S0–S3)), fibrosis stage (based on a meta-analysis of histological data on viral hepatitis score (S0–S4)), ballooning score (S0–S2) and inflammation grades (G0–G4) of the patients were evaluated.12–14 Fibrosis stage ≥2, inflammation grade ≥2 and steatosis score ≥2 were defined as indicative of significant liver fibrosis, active inflammation and severe steatosis, respectively.
Fatigue assessment
Fatigue was assessed by a professional physician within 1 week prior to liver biopsy using the Chronic Liver Disease Questionnaire (CLDQ), which defined fatigue as a score of less than 20 according to the items 2, 4, 8, 11 and 13.15
Statistical analysis
Continuous variables were compared between the two groups using Student’s t-test or the Mann-Whitney U test. Categorical variables were compared using the χ2 test. Propensity score matching (PSM) was performed in a ratio of 1:2 and with a calliper value of 0.2 to balance age, sex and CLD classification between the two patient groups. Univariate and multivariate logistic regression analysis was conducted to analyse the factors that contribute to fatigue. We estimated adjusted ORs and relevant 95% CIs using a parametric proportional hazard model. SPSS V.26.0 (IBM) was used for statistical analyses. Statistical significance was set at p<0.05.
Patient and public involvement
Patients or the public were not involved in the design, or conduct, or reporting, or dissemination plans of the current work.
Results
Comparison of the clinical and histological features of patients with CLD with and without fatigue
A total of 1374 patients with biopsy-proven CLD were included in this study. Of these, 262 (19.07%) patients had symptoms of fatigue, while 1112 (80.93%) had no fatigue. The patients with fatigue were older, had lower BMI and higher HDL-c and GGT levels than the patients without fatigue (p<0.05). There were significant differences between the proportions of patients with NAFLD, CHB with fatty liver, CHB, AFLD and AILDs in the two groups (p<0.05) (table 1).
Table 1.
Comparison of clinical and laboratory characteristics between patients with and without fatigue in CLD
| Variables | Before propensity score matching | After propensity score matching(1:2) | ||||
| Fatigue | No fatigue | P value | Fatigue | No fatigue | P value | |
| n | 262 | 1112 | 242 | 484 | ||
| Male (%) | 175 (66.79) | 785 (70.59) | 0.228† | 167 (69.01) | 337 (69.63) | 0.527† |
| Age (year) | 45.30±11.12 | 41.36±11.33 | <0.001 | 44.02±10.48 | 42.46±11.26 | 0.071 |
| BMI (kg/m2) | 24.05±3.86 | 24.82±4.62 | 0.032 | 24.26±3.88 | 24.18±4.02 | 0.84 |
| BP(S) (mm Hg) | 124.33±15.26 | 125.70±15.52 | 0.204 | 123.86±15.43 | 125.96±16.01 | 0.098 |
| FPG (mmol/L) | 5.56±1.66 | 5.65±1.54 | 0.493 | 5.56±1.65 | 5.61±1.40 | 0.718 |
| HbA1c (%) | 6.18±1.54 | 6.12±1.52 | 0.823 | 6.24±1.61 | 6.09±1.52 | 0.639 |
| TG (mmol/L) | 1.23 (0.95–1.85) | 1.08 (1.55–2.18) | 0.793* | 1.19 (0.93–1.84) | 1.31 (0.90–2.00) | 0.543 |
| TC (mmol/L) | 4.74±1.20 | 4.68±1.11 | 0.504 | 4.67±1.16 | 4.63±0.95 | 0.733 |
| LDL-c (mmol/L) | 2.76±0.88 | 2.75±0.82 | 0.875 | 2.72±0.88 | 2.70±0.75 | 0.788 |
| HDL-c (mmol/L) | 1.30±0.36 | 1.24±0.33 | 0.035 | 1.28±0.35 | 1.25±0.35 | 0.298 |
| STB (μmmol/l) | 16.65 (12.82–22.45) | 16.20 (12.90–21.10) | 0.511* | 16.60 (12.85–22.00) | 15.50 (12.50–20.80) | 0.153* |
| ALT (U/L) | 51.00 (32.00–83.00) | 49.00 (30.00–80.00) | 0.432* | 51.00 (32.00–82.00) | 41.00 (26.00–66.00) | <0.001* |
| AST (U/L) | 35.00 (26.00–52.00) | 33.00 (25.00–49.00) | 0.093* | 34.00 (26.00–51.00) | 28.00 (23.00–41.00) | <0.001* |
| GGT(U/L) | 37.00 (23.00–77.00) | 33.00 (20.00–60.00) | 0.005* | 35.00 (21.00–66.00) | 27.00 (17.00–49.00) | <0.001* |
| AKP (U/L) | 110.00 (88.00–137.00 | 108.00 (87.00–136.00) | 0.650* | 107.00 (87.0–129.00) | 106.00 (83.00–133.00) | 0.797* |
| ALB (g/L) | 44.08±4.15 | 44.51±5.85 | 0.297 | 4437±3.95 | 44.70±5.77 | 0.46 |
| CLD category | ||||||
| NAFLD n (%) | 42 (16.03) | 205 (18.44) | <0.001† | 42 (17.36) | 70 (14.46) | 0.190† |
| CHB with fatty liver n (%) | 47 (17.94) | 283 (25.45) | 47 (19.42) | 103 (21.28) | ||
| CHB n (%) | 138 (52.67) | 531 (47.75) | 137 (56.61) | 254 (52.78) | ||
| AFLD n (%) | 16 (6.11) | 69 (6.20) | 12 (4.96) | 46 (9.51) | ||
| AILDs n (%) | 19 (7.25) | 24 (2.16) | 4 (1.65) | 11 (2.27) | ||
Data are expressed as mean±SD or median (IQR).
*P value calculated using the Mann-Whitney U-test.
†P value calculated using the χ2 test.
AFLD, alcoholic fatty liver disease; AILD, autoimmune liver disease; AKP, alkaline phosphatase; ALB, albumin; ALT, alanine aminotransferase; AST, aspartate aminotransferase; BMI, body mass index; BP, blood pressure; CHB, chronic hepatitis B; CLD, chronic liver disease; FPG, fasting plasma glucose; GGT, gamma-glutamyl-transferase; HbA1c, glycated haemoglobin; HDL-c, high-density lipoprotein cholesterol; LDL-c, low-density lipoprotein cholesterol; STB, serum total bilirubin; SUA, serum uric acid; TC, total cholesterol; TG, triglycerides.
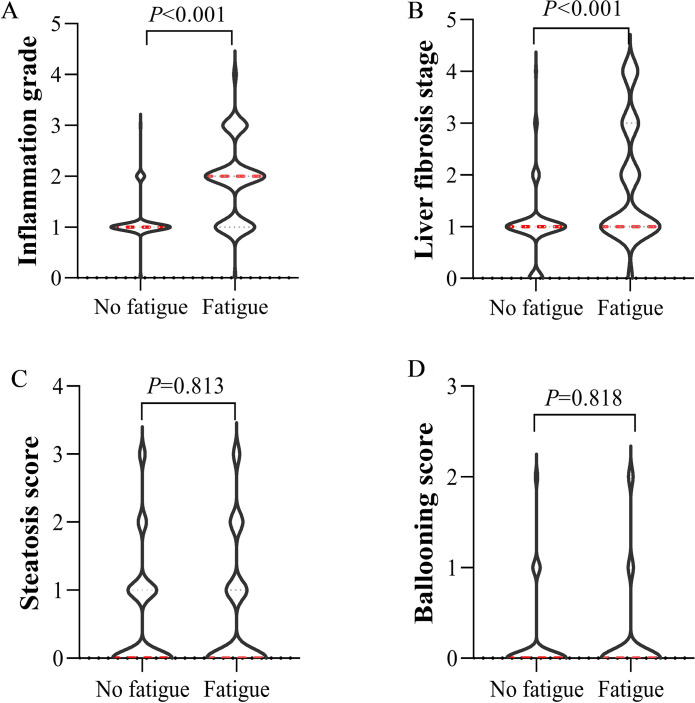
After PSM, 242 patients with fatigue and 484 patients without fatigue were successfully matched, and there were no statistically significant differences between the two groups in terms of sex, age, BMI, blood pressure, fasting blood glucose, lipid profile and liver function (p>0.05) (table 1). The fatigue group had higher ALT, AST and GGT levels than the non-fatigue group. Further comparison of the histological features of the two groups is shown in figure 1. The inflammation grades and liver fibrosis stages of the patients with fatigue were significantly higher than those of the patients without fatigue (p<0.05). There was no difference in hepatic steatosis and ballooning scores between the two groups (p>0.05) (figure 1A–D).
Figure 1.
Comparison of the histopathological characteristics of patients with chronic liver disease with and without fatigue. (A) Comparison of the inflammation grades of patients with CLD stratified according to the presence or absence of fatigue. (B) Comparison of the fibrosis stages of patients with CLD stratified according to the presence or absence of fatigue. (C) Comparison of hepatic steatosis scores of patients with CLD stratified according to the presence or absence of fatigue. (D) Comparison of the ballooning scores of the patients with CLD stratified according to the presence or absence of fatigue. CLD, chronic liver disease.
Distribution and risk factors of fatigue in patients with CLD
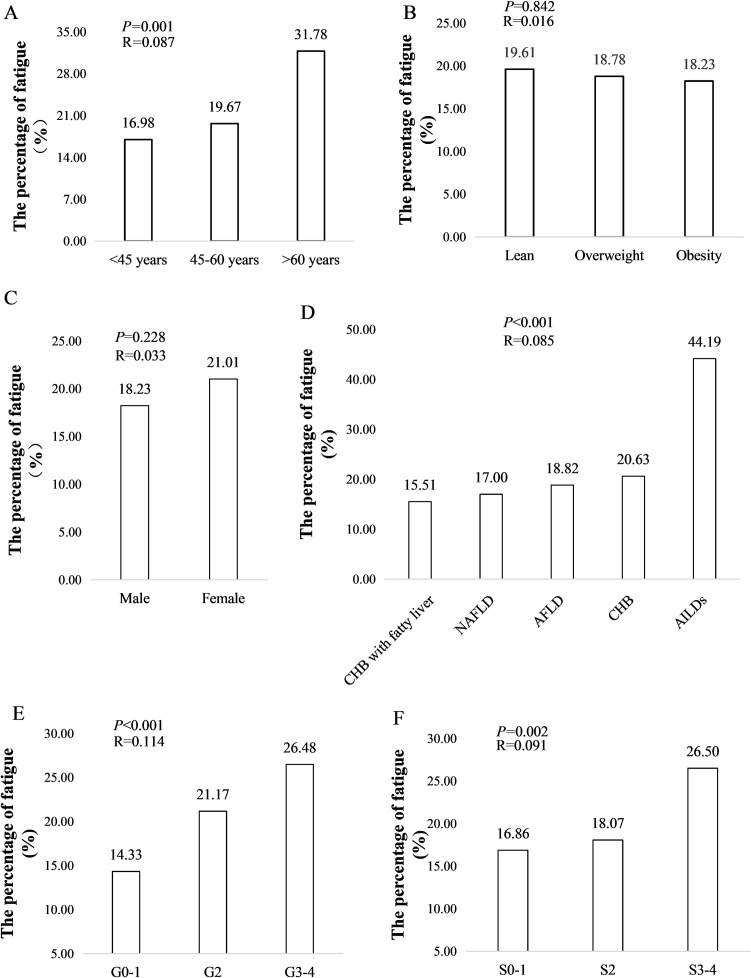
The prevalence of fatigue significantly increased with age (R=0.087, p=0.001) (figure 2A). There was no correlation between fatigue and BMI and sex (p>0.05) (figure 2B, C). The prevalence of fatigue among patients with different types of CLD varied. For patients with AILDs, the prevalence of fatigue was 44.19%, which is more than twice that of patients with other CLDs (p<0.001) (figure 2D). The prevalence of fatigue significantly increased with the degree of liver inflammation and fibrosis stage (p<0.001) (figure 2E, F).
Figure 2.
Prevalence of fatigue in different chronic liver disease populations. (A) Prevalence of fatigue stratified according to age. (B) Prevalence of fatigue stratified according to body mass index. (C) Prevalence of fatigue stratified according to sex. (D) Prevalence of fatigue stratified according to CLD classification. (E) Prevalence of fatigue stratified according to inflammation grade. (F) Prevalence of fatigue stratified according to fibrosis stage. AFLD, alcoholic fatty liver disease; AILD, autoimmune liver diseases; CHB, chronic hepatitis B; CLD, chronic liver disease; NAFLD, non-AFLD.
Univariate and multivariate analyses were performed to define the association between fatigue using clinical and histological features (table 2). Univariate analysis showed that old age (OR 2.122, 95% CI 1.379 to 3.267, p=0.001), AILDs (OR 3.545, 95% CI 1.911 to 6.574, p<0.001), elevated GGT level (OR 1.356, 95% CI 1.012 to 1.816, p=0.042), active inflammation (OR 1.768, 95% CI 1.329 to 2.353, p<0.001) and advanced fibrosis stage (OR 1.743, 95% CI 1.282 to 2.370, p<0.001) were risk factors for fatigue in CLD. Further multivariate analysis indicated that old age (OR 2.026, 95% CI 1.274 to 3.221, p=0.003), AILDs (OR 2.749, 95% CI 1.446 to 5.226, p=0.002) and active inflammation (OR 1.587, 95% CI 1.164 to 2.164, p=0.003) were independent risk factors for fatigue.
Table 2.
Univariate and multivariable regression analysis of risk factors for fatigue in chronic liver disease
| Variables | Univariate analysis | Multivariate analysis | ||
| OR (95% CI) | P value | OR (95% CI) | P value | |
| Old age | ||||
| No | Ref. | Ref. | ||
| Yes | 2.122 (1.379 to 3.267) | 0.001 | 2.026 (1.274 to 3.221) | 0.003 |
| Male | ||||
| No | Ref. | |||
| Yes | 0.838 (0.628 to 1.117) | 0.228 | -- | -- |
| AILDs | ||||
| No | Ref. | |||
| Yes | 3.545 (1.911 to 6.574) | <0.001 | 2.749 (1.446 to 5.226) | 0.002 |
| Metabolic factors | ||||
| Obesity | ||||
| No | Ref. | |||
| Yes | 0.813 (0.591 to 1.121) | 0.207 | -- | -- |
| Hypertension | ||||
| No | Ref. | |||
| Yes | 0.735 (0.536 to 1.008) | 0.056 | -- | -- |
| T2DM | ||||
| No | Ref. | |||
| Yes | 0.694 (0.436 to 1.103) | 0.122 | -- | -- |
| Hypertriglyceridaemia | ||||
| No | Ref. | |||
| Yes | 0.804 (0.577 to 1.121) | 0.198 | -- | -- |
| Hypercholesterolaemia | ||||
| No | Ref. | |||
| Yes | 1.448 (0.974 to 2.153) | 0.068 | -- | -- |
| Hyperuricaemia | ||||
| No | Ref. | |||
| Yes | 0.835 (0.570 to 1.222) | 0.353 | -- | -- |
| High LDL-c | ||||
| No | Ref. | |||
| Yes | 0.943 (0.675 to 1.316) | 0.728 | -- | -- |
| Low HDL-c | ||||
| No | Ref. | |||
| Yes | 1.104 (0.764 to 1.569) | 0.599 | -- | -- |
| Liver enzymes | ||||
| Elevated ALT | ||||
| No | Ref. | |||
| Yes | 1.164 (0.662 to 2.441) | 0.306 | -- | -- |
| Elevated AST | ||||
| No | Ref. | |||
| Yes | 1.205 (0.906 to 1.602) | 0.199 | -- | -- |
| Elevated GGT | ||||
| No | Ref. | |||
| Yes | 1.356 (1.012 to 1.816) | 0.042 | -- | -- |
| Histopathology | ||||
| Severe ballooning | ||||
| No | Ref | |||
| Yes | 1.049 (0.606 to 1.815) | 0.865 | -- | -- |
| Severe steatosis | ||||
| No | Ref | |||
| Yes | 0.850 (0.488 to 1.482) | 0.567 | -- | -- |
| Active inflammation | ||||
| No | Ref. | |||
| Yes | 1.768 (1.329 to 2.353) | <0.001 | 1.587 (1.164 to 2.164) | 0.003 |
| Advanced fibrosis | ||||
| No | Ref | |||
| Yes | 1.743 (1.282 to 2.370) | <0.001 | -- | -- |
AILDs, autoimmune liver diseases; ALT, alanine aminotransferase; AST, aspartate aminotransferase; BMI, body mass index; GGT, gamma-glutamyl-transferase; HDL-c, high-density lipoprotein cholesterol; LDL-c, low-density lipoprotein cholesterol; T2DM, type 2 diabetes mellitus.
Analysis of the correlation between histological features and fatigue in CLD
Multivariate analysis was performed to explore the correlation between fatigue and the severity of histological features. Two different models were used to estimate the ORs for different outcomes. After adjusting for age, sex, BMI, hypertension, type 2 diabetes mellitus, disease classification, ALT level, AST level and GGT level, the OR for the risk of fatigue increased in a stepwise manner from inflammation grades G0–G1 (as a reference) and G2 (OR 1.609, 95% CI 1.085 to 2.386, p=0.018) to G3 (OR 1.745, 95% CI 1.019 to 2.986, p=0.042) (table 3). The severity of steatosis, ballooning and fibrosis were not associated with fatigue (p>0.05).
Table 3.
OR of liver histological severity for fatigue in chronic liver disease
| Crude | Model 1 | Model 2 | ||||
| OR (95% CI) | P value | OR (95% CI) | P value | OR (95% CI) | P value | |
| Steatosis score | ||||||
| S0 | Ref. | Ref. | Ref. | |||
| S1–2 | 1.205 (0.793 to 1.833) | 0.383 | 1.204 (0.787 to 1.841) | 0.392 | 1.360 (0.761 to 2.428) | 0.299 |
| S3 | 0.870 (0.498 to 1.519) | 0.624 | 0.918 (0.522 to 1.615) | 0.767 | 1.328 (0.648 to 2.724) | 0.493 |
| Ballooning score | ||||||
| S0 | Ref. | Ref. | Ref. | |||
| S1 | 0.665 (0.405 to 1.090) | 0.979 | 0.620 (0.376 to 1.023) | 0.942 (0.521 to 1.703) | 0.468 | |
| S2 | 1.007 (0.581 to 1.747) | 0.106 | 0.871 (0.498 to 1.525) | 1.310 (0.632 to 2.716) | 0.843 | |
| Inflammation grade | ||||||
| G0–1 | Ref. | Ref. | Ref. | |||
| G2 | 1.618 (1.190 to 2.200) | 0.002 | 1.570 (1.152 to 2.140) | 0.004 | 1.609 (1.085 to 2.386) | 0.018 |
| G≥3 | 2.170 (1.486 to 3.169) | <0.001 | 2.014 (1.372 to 2.056) | <0.001 | 1.745 (1.019 to 2.986) | 0.042 |
| Liver fibrosis | ||||||
| S0–1 | Ref. | Ref. | Ref. | |||
| S2 | 1.087 (0.751 to 1.574) | 0.657 | 1.006 (0.692 to 1.462) | 0.975 | 0.691 (0.420 to 1.135) | 0.145 |
| S≥3 | 1.777 (1.291 to 2.447) | <0.001 | 1.608 (1.160 to 2.226) | 0.004 | 1.371 (0.897 to 2.096) | 0.144 |
Model 1 adjusted for age and sex; model 2 was adjusted for model 1 plus body mass index hypertension, type 2 diabetes mellitus, alanine aminotransferase, aspartate aminotransferase, gamma-glutamyl-transferase and disease classification.
Sensitivity analysis
Subgroup analysis of the risk of fatigue in CLD showed a significant association between fatigue and increasing severity of liver inflammation among patients aged <60 years old without AILDs (p<0.05). However, the severity of inflammation was not associated with fatigue among patients >60 years old or with AILDs (p>0.05) (table 4).
Table 4.
Sensitivity analysis in the presence of risk factors for fatigue in chronic liver disease
| Variables | No of participants | OR (95% CI) | P value |
| Age | |||
| ≥60 years | 107 | ||
| G0–1 | 37 | Ref. | |
| G2 | 45 | 1.813 (0.668 to 4.919) | 0.632 |
| G≥3 | 25 | 2.848 (0.937 to 8.659) | 0.87 |
| <60 years | 1267 | ||
| G0–1 | 556 | Ref. | |
| G2 | 517 | 1.566 (1.134 to 2.163) | 0.006 |
| G≥3 | 194 | 1.989 (1.324 to 2.988) | 0.001 |
| Elevated GGT | |||
| Yes | 451 | ||
| G0–1 | 141 | Ref. | |
| G2 | 191 | 1.919 (1.077 to 3.420) | 0.027 |
| G≥3 | 119 | 2.420 (1.304 to 4.490) | 0.005 |
| No | 923 | ||
| G0–1 | 452 | Ref. | |
| G2 | 371 | 1.458 (1.011 to 2.105) | 0.019 |
| G≥3 | 100 | 1.880 (1.108 to 3.190) | 0.044 |
| AILDs | |||
| Yes | 43 | ||
| G0–1 | 9 | Ref. | |
| G2 | 13 | 1.714 (0.294 to 9.999) | 0.549 |
| G≥3 | 21 | 1.818 (0.357 to 9.272) | 0.472 |
| No | 1331 | ||
| G0–1 | 584 | Ref | |
| G2 | 549 | 1.587 (1.161 to 2.167) | 0.004 |
| G≥3 | 198 | 1.959 (1.313 to 2.923) | 0.001 |
AILDs, autoimmune liver diseases; GGT, gamma-glutamyl-transferase.
Discussion
Fatigue is a critical component of CLD.11 The findings of the present study indicate an association between fatigue and liver inflammation. In the present study, patients with CLD with fatigue had significantly higher inflammation grades and liver fibrosis stages than patients without fatigue. In addition, multivariate analysis showed that age, AILDs and active inflammation were independent risk factors for fatigue, and that the severity of liver inflammation was strongly associated with fatigue after adjustment for confounders. Further sensitivity analysis showed that this association was present in the young-aged and middle-aged population of the present study but not in the elderly population.
The clinical features of CLD-related fatigue have not been uniformly demonstrated.16 17 In the present study, the patients with CLD with fatigue were older, had lower BMI and higher HDL-c and GGT levels than patients without fatigue. In addition, the fatigue group showed significantly higher inflammation grades and liver fibrosis stages than the non-fatigue group after PSM for age and sex (table 1, figure 1). The results of the present study are in line with those of most studies that showed that old age, AILDs and active inflammation are independent risk factors for fatigue (table 2).18–21 Notably, our research suggested that liver inflammation caused by elevated GGT, and not elevated ALT or AST, was implicated in fatigue. Elevated GGT is usually a sign of cholestasis, and animal studies in bile duct-ligated rats have demonstrated cholestasis-disordered neurotransmission and the development of fatigue. This is suggested to be due to central nervous system damage caused by manganese accumulation. However, further studies are needed to understand the exact mechanism.22
The results of the present study showed that the risk of fatigue increased with the severity of inflammation, but not with the severity of hepatic steatosis, ballooning and liver fibrosis (table 3). Although the issue of fatigue in patients with CLD, including PBC, PSC, CHB, chronic hepatitis C (CHC) and NAFLD, has been extensively studied, the relationship between fatigue and the histological features of CLD remains controversial. Fatigue in NAFLD has been associated with inactivity and excessive daytime sleepiness but not with the severity of liver disease or insulin resistance.16 However, a recent study indicated that the detection of lobular inflammation in biopsies is correlated with lower health-related quality of life (HRQL) in patients with NAFLD.17 Data from clinical trials on CHB or CHC infection also support the dominant role of inflammation in fatigue. In these trials, viral elimination or suppression after antiviral therapy was associated with improved HRQL, which suggests an effect of inflammation on fatigue, whereas improvement of fibrosis did not affect HRQL.23–25
Further subgroup analysis in the present study revealed a significant association between fatigue and the severity of liver inflammation in patients <60 years old, but not in patients ≥60 years old (table 4). Our findings suggest that the severity of liver inflammation may play a dominant role in fatigue in young-aged and middle-aged patients with CLD, whereas age-related factors may play dominant roles in fatigue in elderly patients. Previous studies have shown that fatigue is a significant component of the clinical presentation of patients with AIH, often paralleling hepatic inflammation.26 In line with previous research, the data of the present study showed that patients with AILDs had the highest prevalence of fatigue, and that AILDs was an independent risk factor for CLD-related fatigue. Though fatigue was associated with an AILD diagnosis, it was not correlated with the severity of liver inflammation in patients with AILDs. This may be related to the relatively small number of AILD cases in the present study. Thus, studies with larger samples are needed to confirm this finding.
The strength of this study is that it is the first study, to the best of our knowledge, in which the relationship between fatigue and the severity of liver inflammation in different CLD populations was explored using liver histopathology features. However, the limitations of this study should be noted as well. First, since this was a retrospective study, PSM was used to minimise the influence of available factors. However, some of the retrieved data that could contribute to the development of fatigue, namely plasma iron level, markers of thyroid gland function and blood oxygen tension, were unavailable. Second, although we diagnosed fatigue based on responses to the CLDQ, an important limitation is the dichotomic division of the CLD population into suffering and not-suffering from fatigue with no self-assessment of fatigue severity. Therefore, we could only assess the relationship between the severity of inflammation and the presence or absence of fatigue, but could not clarify the relationship between the severity of liver inflammation and the severity of fatigue. Third, since the study was based on the liver biopsy, there was no control group composed of sex-matched and aged-matched people with healthy livers, which is especially important in the older population. Fourth, since only 43 patients in this study had AILDs, it is difficult to perform statistical analysis after subdividing. Therefore, the AILDs were grouped together irrespective of whether they were parenchymatic or cholestatic, even though it is known that the pathophysiology of fatigue is different in PBC, and AIH may affect the results of AILDs to some extent. Fifth, as this was a cross-sectional study, we could not determine the causal relationship between the severity of inflammation and fatigue. Further studies with longitudinal cohorts are needed to confirm the effects of the severity of inflammation on fatigue in patients with CLD.
In conclusion, the impact of fatigue on the perceived quality of life can be profound for patients with CLD. Since the pathophysiology of fatigue is complex and poorly understood, developing therapeutic trials of symptom-directed therapies is challenging. For fatigue in CLD, the ‘TrACE’ method of Treating the treatable (comorbid causes), Ameliorate the ameliorable causes (sleep, autonomic and mood disorders), Coping strategies (lifestyle changes such as pacing the day, avoiding shift work) and Empathising is generally suggested.4 27 The present study demonstrates that fatigue is correlated with the severity of liver inflammation in young-aged and middle-aged patients with CLD. However, this correlation was not observed in elderly patients. These findings contradict the perception that fatigue is not associated with the severity of liver disease. Since age is an important factor that influences fatigue, our findings highlight the need for age stratification during the evaluation and treatment of patients with CLD with fatigue, which will provide new evidence for the management and treatment of fatigue in patients with CLD.
Supplementary Material
Footnotes
Contributors: Research idea and study design: JS, JL, GC; data acquisition: JL, XG, SL, YJ, GZ, XM, JW, XY, YG and GC; data analysis/interpretation: JL and HL; statistical analysis: JL and HL; supervision or mentorship: JS. Each author contributed important intellectual content during manuscript drafting and revision, agreed to be personally accountable for the individual’s contributions, and ensured questions about the accuracy or integrity of any portion of the work, even one in which the author was not directly involved, are appropriately investigated and resolved. JS was responsible for the overall content.
Funding: This work was supported by the Zhejiang Provincial Department of Health project (grant number 2020KY715).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available on reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study was performed according to the ethical guidelines of the Declaration of Helsinki and was approved by the Ethics Committee of the Affiliated Hospital of Hangzhou Normal University (approval number: 2020 (02)-KS-022). As this was an observational retrospective study, the requirement for informed consent was waived by the ethics committee.
References
- 1.Moon AM, Singal AG, Tapper EB. Contemporary epidemiology of chronic liver disease and cirrhosis. Clin Gastroenterol Hepatol 2020;18:2650–66. 10.1016/j.cgh.2019.07.060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huang DQ, El-Serag HB, Loomba R. Global epidemiology of NAFLD-related HCC: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol 2021;18:223–38. 10.1038/s41575-020-00381-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Locarnini S, Hatzakis A, Chen D-S, et al. Strategies to control hepatitis B: public policy, epidemiology, vaccine and drugs. J Hepatol 2015;62:S76–86. 10.1016/j.jhep.2015.01.018 [DOI] [PubMed] [Google Scholar]
- 4.Swain MG, Jones DEJ. Fatigue in chronic liver disease: new insights and therapeutic approaches. Liver Int 2019;39:6–19. 10.1111/liv.13919 [DOI] [PubMed] [Google Scholar]
- 5.Jopson L, Dyson JK, Jones DEJ. Understanding and treating fatigue in primary biliary cirrhosis and primary sclerosing cholangitis. Clin Liver Dis 2016;20:131–42. 10.1016/j.cld.2015.08.007 [DOI] [PubMed] [Google Scholar]
- 6.Cauch-Dudek K, Abbey S, Stewart DE, et al. Fatigue in primary biliary cirrhosis. Gut 1998;43:705–10. 10.1136/gut.43.5.705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jones DEJ, Bhala N, Burt J, et al. Four year follow up of fatigue in a geographically defined primary biliary cirrhosis patient cohort. Gut 2006;55:536–41. 10.1136/gut.2005.080317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bower JE. Cancer-related fatigue -- mechanisms, risk factors, and treatments. Nat Rev Clin Oncol 2014;11:597–609. 10.1038/nrclinonc.2014.127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gerber LH, Weinstein AA, Mehta R, et al. Importance of fatigue and its measurement in chronic liver disease. World J Gastroenterol 2019;25:3669–83. 10.3748/wjg.v25.i28.3669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.D’Mello C, Swain MG. Liver-brain inflammation axis. Am J Physiol Gastrointest Liver Physiol 2011;301:G749–61. 10.1152/ajpgi.00184.2011 [DOI] [PubMed] [Google Scholar]
- 11.Kośnik A, Wójcicki M. Fatigue in chronic liver disease patients: prevalence, pathophysiology, and management. Prz Gastroenterol 2022;17:21–7. 10.5114/pg.2022.114594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brunt EM, Janney CG, Di Bisceglie AM, et al. Nonalcoholic steatohepatitis: a proposal for grading and staging the histological lesions. Am J Gastroenterol 1999;94:2467–74. 10.1111/j.1572-0241.1999.01377.x [DOI] [PubMed] [Google Scholar]
- 13.Bedossa P, Poynard T. An algorithm for the grading of activity in chronic hepatitis C. Hepatology 1996;24:289–93. 10.1002/hep.510240201 [DOI] [PubMed] [Google Scholar]
- 14.Batts KP, Ludwig J. Chronic hepatitis. An update on terminology and reporting. Am J Surg Pathol 1995;19:1409–17. 10.1097/00000478-199512000-00007 [DOI] [PubMed] [Google Scholar]
- 15.Younossi ZM, Guyatt G, Kiwi M, et al. Development of a disease specific questionnaire to measure health related quality of life in patients with chronic liver disease. Gut 1999;45:295–300. 10.1136/gut.45.2.295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Newton JL, Jones DEJ, Henderson E, et al. Fatigue in non-alcoholic fatty liver disease (NAFLD) is significant and associates with inactivity and excessive daytime sleepiness but not with liver disease severity or insulin resistance. Gut 2008;57:807–13. 10.1136/gut.2007.139303 [DOI] [PubMed] [Google Scholar]
- 17.Huber Y, Boyle M, Hallsworth K, et al. Health-related quality of life in nonalcoholic fatty liver disease associates with hepatic inflammation. Clin Gastroenterol Hepatol 2019;17:2085–92. 10.1016/j.cgh.2018.12.016 [DOI] [PubMed] [Google Scholar]
- 18.Swain MG. Fatigue in liver disease: pathophysiology and clinical management. Can J Gastroenterol 2006;20:181–8. 10.1155/2006/624832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schramm C, Wahl I, Weiler-Normann C, et al. Health-related quality of life, depression, and anxiety in patients with autoimmune hepatitis. J Hepatol 2014;60:618–24. 10.1016/j.jhep.2013.10.035 [DOI] [PubMed] [Google Scholar]
- 20.Bozzini AB, Neder L, Silva CA, et al. Decreased health-related quality of life in children and adolescents with autoimmune hepatitis. J Pediatr (Rio J) 2019;95:87–93. 10.1016/j.jped.2017.10.013 [DOI] [PubMed] [Google Scholar]
- 21.Finsterer J, Mahjoub SZ. Fatigue in healthy and diseased individuals. Am J Hosp Palliat Care 2014;31:562–75. 10.1177/1049909113494748 [DOI] [PubMed] [Google Scholar]
- 22.Milkiewicz P, Heathcote EJ. Fatigue in chronic cholestasis. Gut 2004;53:475–7. 10.1136/gut.2003.025155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Younossi ZM, Stepanova M, Janssen HLA, et al. Effects of treatment of chronic hepatitis B virus infection on patient-reported outcomes. Clin Gastroenterol Hepatol 2018;16:1641–9. 10.1016/j.cgh.2018.02.037 [DOI] [PubMed] [Google Scholar]
- 24.Younossi ZM, Stepanova M, Afdhal N, et al. Improvement of health-related quality of life and work productivity in chronic hepatitis c patients with early and advanced fibrosis treated with ledipasvir and sofosbuvir. J Hepatol 2015;63:337–45. 10.1016/j.jhep.2015.03.014 [DOI] [PubMed] [Google Scholar]
- 25.Younossi ZM, Stepanova M, Jacobson IM, et al. Sofosbuvir and velpatasvir with or without voxilaprevir in direct-acting antiviral-naïve chronic hepatitis C: patient-reported outcomes from polaris 2 and 3. Aliment Pharmacol Ther 2018;47:259–67. 10.1111/apt.14423 [DOI] [PubMed] [Google Scholar]
- 26.Graff LA, Walker JR, Russell AS, et al. Fatigue and quality of sleep in patients with immune-mediated inflammatory disease. J Rheumatol Suppl 2011;88:36–42. 10.3899/jrheum.110902 [DOI] [PubMed] [Google Scholar]
- 27.Phaw NA, Leighton J, Dyson JK, et al. Managing cognitive symptoms and fatigue in cholestatic liver disease. Expert Rev Gastroenterol Hepatol 2021;15:235–41. 10.1080/17474124.2021.1844565 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available on reasonable request.