Abstract
Objectives
To measure the impact of lost-time occupational injuries on all-cause mortality in Washington State and, using the same data elements and study design, to determine whether the estimated impact was similar to previous estimates for New Mexico.
Methods
We linked injuries in the Washington workers’ compensation system with Social Security Administration data on earnings and mortality. We estimated Cox survival models of mortality for women and men with lost-time compared with medical-only injuries, adjusting for age, pre-injury earnings and industry. We used quantitative bias analysis to account for confounding by pre-injury smoking and obesity.
Results
The estimated mortality HR was 1.24 for women (95% CI 1.21 to 1.28) and 1.22 for men (95% CI 1.20 to 1.24). After adjusting for unmeasured pre-injury smoking and obesity, the estimated HR for women was 1.10, 95% simulation interval (SI) 1.00 to 1.21; for men, it was 1.15, 95% SI 1.04 to 1.27.
Conclusions
All-cause mortality for Washington workers with lost-time injuries was higher than for those with medical-only injuries. Estimated HRs for Washington were consistent with those previously estimated for New Mexico, a less populous state with lower median wages and a different workers’ compensation insurance mechanism. This suggests that the relationship between workplace injury and long-term mortality may be generalisable to other US states. These findings support greater efforts to enhance safety and to investigate factors that improve postinjury employment opportunities and long-term health. This association should be examined in additional locations, with different study conditions, or using additional data on pre-injury risk factors.
INTRODUCTION
Work-related injuries have substantial long-term negative effects on disability,1 earnings,2 3 family roles,4–6 depression6–9 and opioid use.10 11 Studies in Taiwan, Canada and the USA12–17 have shown increases in all-cause mortality following lost-time injury.
Workers’ compensation is a social insurance programme that provides injured workers with cash benefits to partially replace lost earnings and medical benefits to cover injury-related medical care. Almost all US workers’ compensation systems are state-based, with different laws, rules and procedures. This can raise questions about whether study findings in one jurisdiction are likely to apply to others. For this reason, this article measures the impact of lost-time occupational injuries on all-cause mortality in Washington State and determines whether the estimated impact was similar to an earlier estimate for New Mexico. To do this, we use the same data elements and methods to analyse mortality in both states. This issue was studied in a third state, West Virginia, but we lack access to these data, so we could not make a comparison using parallel data and methods.
Washington is a more populous, higher-income state with a different workers’ compensation insurance arrangements than New Mexico. Washington had a population of 7.7 million in 2021, (11th most populous state), while New Mexico’s population was 2.1 million (36th most populous).18 That same year, Washington was the state with the 11th highest median household income (US$56 183), while New Mexico ranked 37th (US$45 134).19 In New Mexico, private insurers provide workers’ compensation insurance to employers. However, in Washington, a state agency is the sole insurer, so its insurance arrangements are more like those in many countries, where the government is the exclusive insurer.
We do not present a causal explanation for why injured worker outcomes might differ between New Mexico and Washington. We note that similar mortality impacts in states that differ on several dimensions would provide support for the generalisability of the findings to additional states.
Our primary data sources provide information on gender, age, industry and pre-injury earnings, important potential confounders of the lost-time-mortality relationship. However, they lack information on two well-recognised confounders: smoking and obesity.20–25 We used quantitative bias analysis (QBA) to assess the impact of these unobserved confounders on point estimates and estimates of uncertainty.
METHODS
Data
We used the same methods to develop our primary dataset for Washington as those in an earlier study of New Mexico.15 We obtained workers’ compensation data on all injuries and illnesses occurring between 1994 and 2000 (the same dates as for New Mexico) from the Washington State Department of Labor and Industries. This included worker, employer, injury and benefit characteristics. For convenience, we refer to injured workers but include injuries and illnesses.
In Washington, injured workers received cash benefits if they experienced >3 days off work (the ‘waiting period’) or had a permanent disability. This is the ‘lost-time’ group, our exposed population. Our comparison population, the ‘medical-only’ group, received only medical benefits and lost 3 or fewer days from work.
A worker may experience more than one injury. An earlier injury might contribute to increased mortality, so we restricted the analysis to each person’s first lost-time injury. Because we focused on the first lost-time injury, we excluded people who had a lost-time injury in 1992 or 1993—before the observation period. We used information from Social Security Administration (SSA) on vital status on 31 December 2018: alive, dead or unknown. If SSA classified an individual as dead, we extracted the date of death from SSA files. If the injury was a fatality or the worker died within 6 months of the injury, we considered the death to be a direct result of the injury and removed that person from the analysis dataset. We restricted the dataset to ages 15–79 years at injury and excluded those missing gender (0.10%) or industry (3.35%).
To validate SSA vital status, we randomly sampled from the Washington dataset within SSA vital status classification (alive, dead or unknown), injury category (lost-time or medical-only) and gender. We submitted to the National Death Index (NDI) 17 000 observations classified as dead, 1000 classified as alive and 600 classified as unknown. The NDI confirmed 97.5% of people classified as dead by SSA. Only 0.67% of those classified as having unknown vital status, and none classified as alive by the SSA, were identified as deceased in the NDI data. Because of this high level of concordance, this study relies on the SSA vital status classification, treating people of unknown status as alive.
Statistical analysis
The statistical approach in this study was the same as that in earlier New Mexico mortality studies.15 16
Cox regression using the primary dataset
We first derived Kaplan-Meier curves for women and men, comparing cumulative mortality of workers with lost-time and medical-only injuries. However, age is associated both with mortality and the incidence of injury26–28 and workers with lost-time injuries tend to be older than comparison workers in our data. The Kaplan-Meier method does not account for age and other relevant covariates, so differences in cumulative incidence between the two injury categories may be confounded by differences in age distribution. Similarly, differences in income29 30 and industry may affect longevity along pathways unrelated to work-related injury.31–34
To address this, we used Cox proportional mortality regression to estimate the mortality hazard of lost-time relative to medical-only injuries, adjusting for age at injury (10-year age categories), pre-injury earnings categories (in constant 2007 US$) and industry. Follow-up began 6 months after injury and ended at whichever came first, death or end of follow-up. Because they have different baseline mortality and labour-market experiences, we estimated separate regressions for women and men. We tested the proportional hazards assumption, which was violated for age, so our estimates are stratified for the age category. For this reason, we do not estimate the effect of age on mortality.
Quantitative bias analysis to account for omitted confounding from pre-injury smoking and obesity
We lacked information on the distribution of pre-injury smoking and obesity within the study population. We used QBA to adjust for these missing confounders. QBA models non-random errors to estimate the direction, magnitude and uncertainty of bias. To account for the bias related to missing pre-injury smoking and obesity information, we simulated what the data would look like had we measured these covariates and adjusted for them. These simulations are informed by external data on the distribution of the confounders in those with and without lost-time injuries and the strength of the effect of these two variables on mortality (figure 1).16
Figure 1.
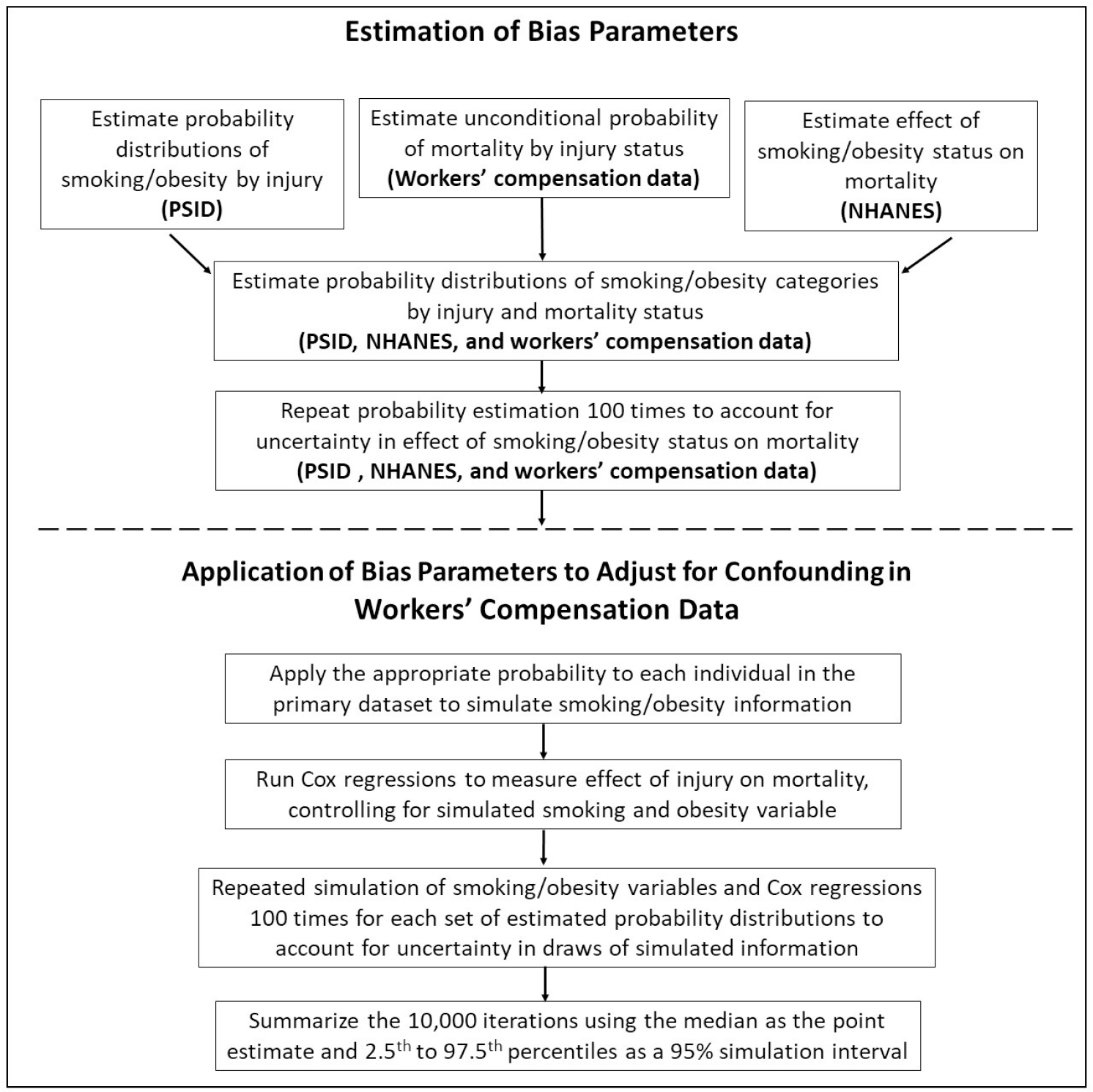
Steps in conducting a quantitative bias analysis to adjust for bias due to unobserved smoking and obesity. The top part of the figure reflects estimation of bias parameters using external datasets, and the bottom part reflects using these parameters to adjust for smoking and obesity in the primary study dataset (Washington workers’ compensation data). This figure was adapted from figure 1 of a publication by the current study’s authors. This quantitative bias analysis approach can apply to any jurisdiction (including New Mexico and Washington).16 NHANES, National Health and Nutrition Examination Survey; PSID, Panel Study of Income Dynamics.
We simulated the unmeasured confounder as a joint six-level variable denoting combinations of obesity and smoking—current/former/never smoker by not obese/obese. To do this, we generated estimates of the distribution of pre-injury smoking and obesity by both lost-time status (lost-time vs medical-only injuries) and mortality (died vs survived). We further stratified our analysis by gender. The joint distribution gave us estimates of having the confounder within levels of gender, medical-only versus lost-time status and mortality that we could use to simulate the confounder within the dataset and adjust for the simulated confounder. We defined obese as body mass index (BMI) ≥30 kg/m2.
To generate estimates of the joint distribution of pre-injury smoking, pre-injury obesity, lost-time versus medical-only injury and survival within our cohort, we first estimated the probability of having a lost-time injury for each level of our pre-injury smoking-obesity variable and then estimated the strength of effect of each level of the smoking-obesity variable on mortality. To estimate the former, we used the 2003–2010 waves of a longitudinal survey of a stratified representative sample of US individuals and their families, the Panel Study of Income Dynamics (PSID).35 From 1999 through 2019, the PSID has had information on pre-injury smoking, obesity and lost-time injury but not on mortality.
Within the PSID, we matched each lost-time injured worker with 20 uninjured workers on key confounders including gender, age group (<25, 25–34, 35–44, 45–54, 55–64, 65+ years), race (white non-Hispanic, black non-Hispanic, Hispanic, other) and education (less than high school, high school graduate, college graduate). We then estimated the proportion and SEs of those with and without lost-time injury (and by gender) in each of the six smoking-obesity groups. We estimated these proportions for lost-time injured workers using data from before the date of injury, while for uninjured workers we used data from before the injury date of their matched injured workers.
To determine the relative increase in mortality associated with pre-injury smoking and obesity (stratified by gender), we used the National Health and Nutrition Examination Survey (NHANES) III (1988–1994) and continuous waves (1999–2014). We included anyone aged 18–79 years at the survey date who was employed in the private sector or state and local government, as this would limit the data to those who would have been covered by state workers’ compensation systems. We then used Cox proportional hazards with age as the time scale to determine the HRs for each of five levels of the smoking and obesity variable compared with the reference group of never smoker/non-obese, also adjusting for gender, race/ethnicity and educational attainment. See the supplementary materials at QBA Methods Example: New Mexico Data, Table A6.
After we obtained these estimated parameters, we used them to simulate the six-level confounder in our primary dataset using methods described in Lash et al,36 with some modifications and additional simulation methods that are elaborated in QBA Methods Example: New Mexico Data. In brief, we combined the NHANES regression estimates of the effect of smoking-obesity on mortality with the relationship between lost-time injury and mortality from the Washington data and the joint distribution of injury and pre-injury smoking and obesity from the PSID to simulate smoking-obesity probability distributions contingent on injury and mortality status. To account for uncertainty in the HR estimates from the NHANES regression, we repeated this process using 100 iterations of HR values based on draws from normal distributions defined by the point estimates and SEs of the NHANES regression coefficients. Because the PSID data matched injured and uninjured workers on gender, race and education, the smoking-obesity probabilities implicitly controlled for these factors. We then applied these smoking-obesity probability distributions to simulate confounder information in the Washington data.
Because we did not know the exact joint distribution of smoking-obesity within levels of injury and mortality in our cohort, we accounted for this uncertainty by sampling the simulated smoking-obesity information using normal distributions around the logit transformations of the probabilities. We repeated this sampling 100 times for each of the 100 iterations of probability distributions calculated from the NHANES regression HRs. For each of the 10 000 simulated datasets, we ran a Cox proportional hazards model of the association between lost-time injury and mortality adjusted for age at injury, pre-injury earnings and industry, and our simulated confounders. Then we accounted for random error by sampling from a standard random normal distribution, multiplying by the estimated SE and subtracting the result from the estimate adjusted for the systematic error. We summarised the resulting 10 000 adjusted HRs using the median as the point estimate and the 2.5th to the 97.5th percentile of the HR distribution as a 95% simulation interval (SI). These simulations, using national data, rely on the same method used and described in an earlier paper.16
Comparison with New Mexico results
We used identical methods and parallel data elements to estimate mortality hazard in Washington and New Mexico. However, to qualify for temporary disability benefits in Washington, injured workers must miss >3 days from work. In contrast, in New Mexico, they must miss >7 days. To compare the two states, we created a second Washington comparison group, excluding temporarily disabled workers who lost 7 or fewer days from work from the lost-time group and including them in the comparison group. We then repeated the analyses above with a comparison group that more closely mirrored the New Mexico medical-only group.
RESULTS
Table 1 presents summary statistics for the Washington analysis dataset. Using name, date of birth, sex and Social Security Number, we successfully linked 97.5% of those in the workers’ compensation data to SSA’s files, which provide information on vital status through 2018 and annual earnings starting with the year prior to injury and all subsequent years. Limiting the data to workers linked to SSA data, we identified 237931 workers with a lost-time injury and 498544 workers with a medical-only injury.
Table 1.
Characteristics of Washington State workers receiving workers’ compensation benefits 1994–2000 and followed through 2018
| Women |
Men |
||||
|---|---|---|---|---|---|
| All injuries | Lost-time injury* | Medical-only injury* | Lost-time injury* | Medical-only injury* | |
|
|
|
|
|
||
| Baseline characteristics | N=736475 | N=84805 | N=188925 | N=153126 | N=309 619 |
|
| |||||
| Age (years), % | |||||
|
| |||||
| <25 | 21.6 | 12.1 | 23.4 | 14.3 | 26.8 |
|
| |||||
| 25–34 | 27.7 | 23.1 | 26.0 | 26.8 | 30.6 |
|
| |||||
| 35–44 | 26.2 | 31.6 | 25.6 | 28.9 | 23.9 |
|
| |||||
| 45–54 | 16.8 | 23.3 | 18.0 | 19.0 | 13.2 |
|
| |||||
| 55–64 | 6.6 | 8.8 | 6.1 | 9.7 | 4.8 |
|
| |||||
| 65+ | 1.0 | 1.3 | 0.9 | 1.4 | 0.7 |
|
| |||||
| Annual pre-injury earnings, %, 2007 US$ | |||||
|
| |||||
| <10000 | 24.3 | 25.6 | 29.5 | 18.7 | 23.6 |
|
| |||||
| 10 000–19999 | 18.1 | 22.6 | 21.7 | 14.9 | 16.3 |
|
| |||||
| 20 000–29999 | 16.0 | 19.2 | 17.6 | 14.6 | 14.8 |
|
| |||||
| 30 000–39999 | 12.8 | 13.4 | 12.2 | 13.6 | 12.6 |
|
| |||||
| 40 000–49999 | 10.0 | 8.2 | 7.7 | 12.3 | 10.7 |
|
| |||||
| 50 000–60 000 | 7.3 | 4.8 | 4.6 | 10.0 | 8.2 |
|
| |||||
| 60 000–70 000 | 5.6 | 3.1 | 3.1 | 7.0 | 5.5 |
|
| |||||
| 70 000+ | 6.9 | 3.0 | 3.5 | 9.0 | 8.3 |
|
| |||||
| Industry, % | |||||
|
| |||||
| Agriculture, Forestry and Fishing | 3.6 | 2.2 | 2.6 | 4.3 | 4.2 |
|
| |||||
| Mining | 0.3 | 0.1 | 0.0 | 0.4 | 0.4 |
|
| |||||
| Construction | 11.3 | 1.8 | 1.6 | 19.0 | 16.1 |
|
| |||||
| Manufacturing | 17.2 | 12.5 | 10.4 | 23.4 | 22.0 |
|
| |||||
| Transportation | 6.2 | 5.5 | 4.0 | 10.2 | 6.2 |
|
| |||||
| Wholesale and Retail Trade | 27.0 | 28.7 | 32.0 | 20.0 | 27.9 |
|
| |||||
| Finance, Insurance and Real Estate | 2.2 | 2.8 | 3.6 | 1.4 | 1.7 |
|
| |||||
| Services | 9.7 | 10.3 | 9.9 | 8.4 | 10.2 |
|
| |||||
| Health | 7.4 | 16.7 | 16.1 | 1.9 | 2.3 |
|
| |||||
| Government | 4.8 | 4.9 | 4.1 | 6.0 | 4.7 |
|
| |||||
| Law, Education and Social | 9.2 | 14.5 | 16.4 | 4.9 | 5.6 |
|
| |||||
| Cumulative mortality, % | |||||
|
| |||||
| 5 years after injury | 1.1 | 1.0 | 0.6 | 1.7 | 1.1 |
|
| |||||
| 10 years after injury | 2.8 | 2.8 | 1.7 | 4.5 | 2.6 |
|
| |||||
| 15 years after injury | 5.2 | 5.7 | 3.4 | 8.2 | 4.8 |
|
| |||||
| 20 years after injury | 8.7 | 9.6 | 6.0 | 13.2 | 7.9 |
|
| |||||
| 25 years after injury | 11.1 | 12.0 | 7.7 | 16.6 | 10.2 |
|
| |||||
| Characteristics at end of follow-up | |||||
|
| |||||
| Years of follow-up, median | 20.8 | 20.9 | 20.9 | 20.8 | 21.0 |
|
| |||||
| Total deaths, n | 81 892 | 25 379 | 31 736 | 10 199 | 14 578 |
Data are linked Washington State workers’ compensation data identifying injured workers, injury type and industry and Social Security Administration data identifying earnings, age and mortality status. Pre-injury earnings converted to 2007 US$ using the Northwest Consumer Price Index for All Urban Consumers.
Lost-time injuries involve >3 calendar days lost from work or permanent disability benefits. Medical-only injuries have 3 or fewer days lost from work and no permanent disability benefits.
Compared with workers with medical-only injuries, those with lost-time injuries were more likely to be 35 years or older. Cumulative mortality was greater for lost-time injuries at every postinjury year. Our data have 20.8 median years and a maximum of 25 years of follow-up.
Mortality cumulative incidence
Figures 2 and 3 display Kaplan-Meier curves comparing Washington lost-time and medical-only injuries. They show a higher cumulative mortality for lost-time injuries.
Figure 2.
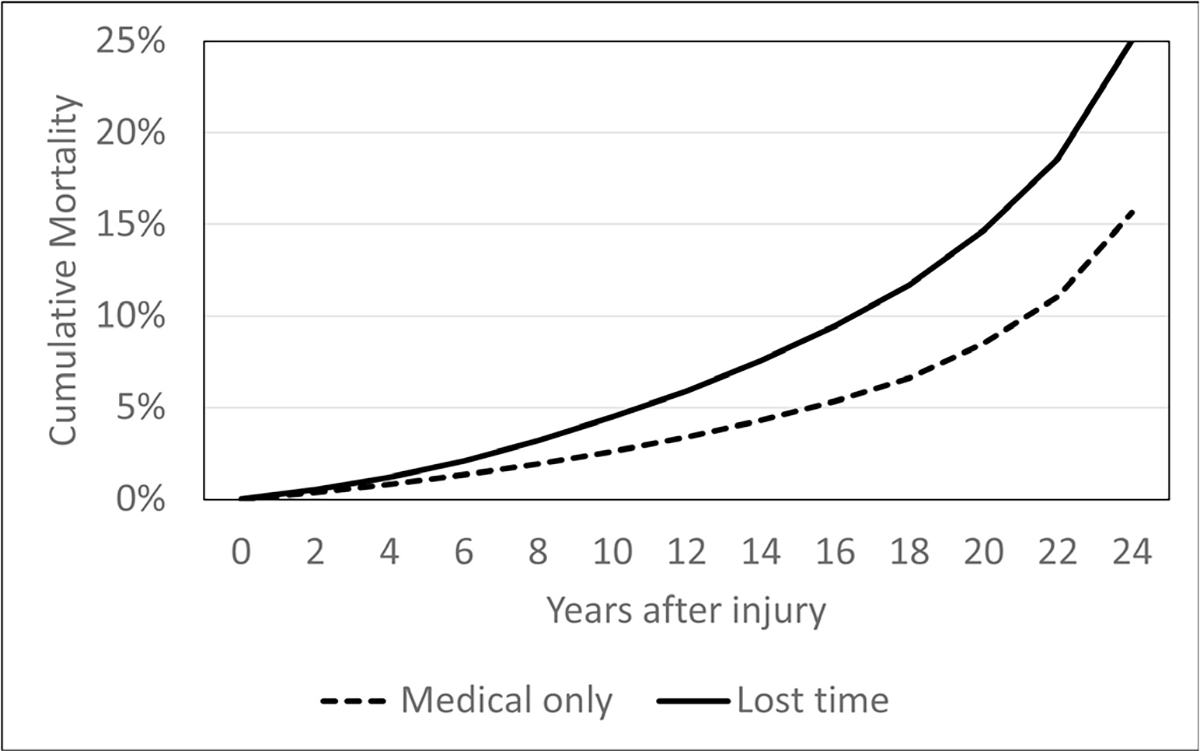
Kaplan-Meier cumulative mortality curves, lost-time and medical-only injuries, Washington State women, 1994–2000 injuries.
Figure 3.
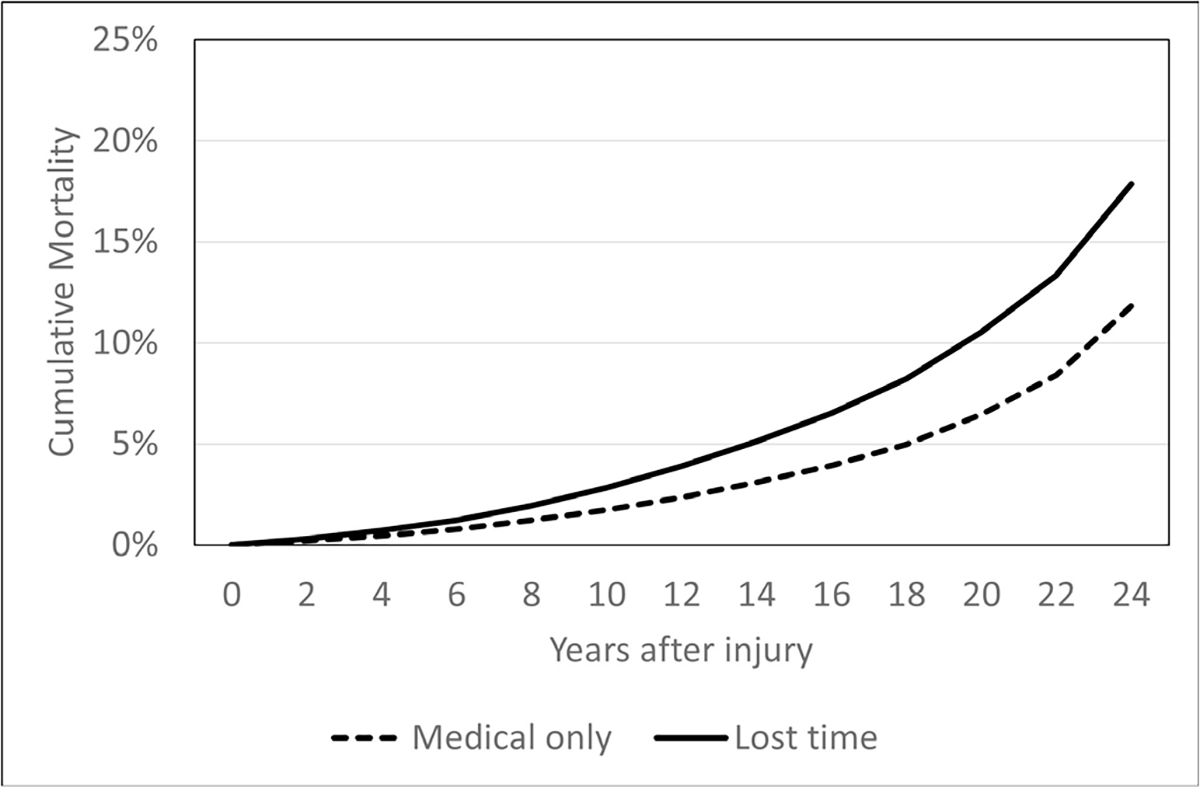
Kaplan-Meier cumulative mortality curves, lost-time and medical-only injuries, Washington State men, 1994–2000 injuries.
Cox proportional hazards regression results
We estimated a Cox proportional hazards regressions by gender, stratifying on age and adjusting for pre-injury earnings and industry. Lost-time injuries are associated with >20% increase in mortality hazard for both women and men, and 95% CIs are narrow, with lower bounds at 1.21 for women and 1.20 for men (table 2). See online supplemental table 1 for all regression HRs.
Table 2.
Conventional and bias-adjusted proportional hazards estimates of the association between lost-time injury and mortality in Washington State and New Mexico, 1994–2000 injuries*
| Partially adjusted | Also adjusted for smoking and obesity* | |||
|---|---|---|---|---|
| HR | 95% CI | Median HR | 2.5th-97.5th percentile | |
| Washington: 3-day comparison group† | ||||
| Women | 1.24 | 1.21 to 1.28 | 1.1 | 1.00–1.21 |
| Men | 1.22 | 1.20 to 1.24 | 1.15 | 1.04–1.27 |
| Washington: 7-day comparison group‡ | ||||
| Women | 1.23 | 1.21 to 1.28 | 1.1 | 1.00–1.21 |
| Men | 1.21 | 1.20 to 1.24 | 1.15 | 1.04–1.27 |
| New Mexico§ | ||||
| Women | 1.26 | 1.16 to 1.37 | 1.13 | 0.97–1.31 |
| Men | 1.21 | 1.15 to 1.27 | 1.12 | 1.00–1.27 |
Data are linked New Mexico and Washington State workers’ compensation data (identifying injured workers, injury type and industry) and Social Security Administration data (identifying earnings, age and mortality status).
Stratified by age and adjusted for pre-injury earnings and industry.
Washington estimates using its definition of lost-time injuries (>3 days days off work or permanent disability). Women: 84 805 lost-time injuries, 188 925 medical-only injuries; men: 153 126 lost-time injuries, 309 619 medical-only injuries.
Washington using New Mexico lost-time definition, >7 days days off work or permanent disability. Women: 69 482 lost-time injuries, 204 248 medical-only injuries; men: 125 062 lost-time injuries, 337 683 medical-only injuries.
Comparison of Washington and New Mexico mortality hazard
Table 2 shows the estimated mortality HR for lost-time injuries for Washington and New Mexico, including applying New Mexico’s injury definition to Washington. The first section shows Washington mortality HRs using a comparison group of workers with <3 days of lost time, adjusted for observed confounders and then further adjusted for pre-injury smoking and obesity. The second panel displays Washington results using a comparison group of temporarily disabled workers who lost 7 or fewer days from work, more closely mirroring the medical-only comparison group for New Mexico. This made very little difference in the Washington estimates. The third panel displays New Mexico estimates. For women and men in both states, HRs adjusted for observed confounders but not for smoking and obesity are between 1.26 and 1.21. Table 2 also shows HR estimates for both states accounting for confounding by smoking and obesity using QBA. For both states, this reduces the estimated HRs between 1.10 and 1.15. It also widens the uncertainty intervals, such that the lower bound of the 95% SI is close to 1.0 for all fully adjusted estimates.
DISCUSSION
For this analysis, we constructed a Washington dataset that was parallel to previously analysed New Mexico data and used the same statistical approach as for the earlier New Mexico studies. The Washington results closely mirrored those for New Mexico.15 16
Accounting for bias induced by unobserved smoking and obesity reduced the observed association between mortality and lost-time injuries. The uncertainty induced by the estimates of the impact of smoking and obesity on injury and on mortality led to 95% SIs that are substantially wider than the 95% CIs for both states. Nevertheless, this study, undertaken in a state that differs along several dimensions from New Mexico, supports the conclusions of the earlier study. Mortality hazard in both states appears increased by non-fatal lost-time workplace injuries.
A separate study in West Virginia17 using a different approach presented an all-cause mortality HR that was greater than observed in either the Washington or New Mexico studies, although the West Virginia study was focused on back injuries and did not account for pre-injury earnings, industry, smoking or obesity. We cannot say why those associations may be stronger, but both the West Virginia study and our results suggest that further examination into injuries and illnesses, including specific types of injuries and illnesses, and their impact on long-term mortality are needed.
The results of this study are also consistent with those of a recent article that found that midlife work limitations are associated with lower odds of survival.37 In that study, even temporary work limitations were associated with 59% lower survival to age 65 years.
Several other approaches estimate how unobserved confounders might affect the estimated HR.38 These typically require assumptions about the strength of unobserved confounding (often that it is equal to the strength of observed confounding) and the amount of the variation in the dependent variable explained by observed and unobserved covariates.39
Here we have taken a different approach, using external data to estimate the HR of interest controlling for two important unobserved confounders. Controlling for smoking and obesity works in the bias analysis because these characteristics differ between exposure categories and have large overall mortality impacts. In all, we have controlled for six variables (gender, age, earnings, industry, smoking and obesity) and would anticipate a diminishing influence of additional variables due to their likely correlation with those that we have already accounted for. Also, additional variables in a bias analysis would be problematic, in part, because available data would become too sparse across joint confounder categories within categories of exposure or outcome.
The postinjury increase in mortality we have documented continues for decades. As such, it may be the result of more than the direct impact of the injury. Factors indirectly related to the proximate effects of injury, including return to the pre-injury employer,40–42 long-term job loss,40 41 decline in earnings,3 43 depression,7–9 and opioid use10 11 may affect the long-term mortality effects we have described. Policies that reduce injury rates, improve medical care and improve postinjury employment can affect these indirect injury consequences.
Limitations
Both smoking and obesity are major sources of increased mortality and have been shown to raise injury risk. Our primary analysis datasets lack information on pre-injury smoking and obesity and on excess mortality related to these factors, posing a substantial threat of bias in estimates of the impact of lost-time injuries on mortality. If the secondary sources do not accurately reflect pre-injury confounder distribution or the mortality risk of the study populations, the QBA may overcorrect or undercorrect.
The PSID is a national sample, but our study population is in Washington State. However, during the observed period the distributions of pre-injury smoking and BMI categories for Washington adults and US adults were similar. For example, using the Behavioural Risk Factor Surveillance System for the year 1998, the median US and Washington per cent of current smokers were 22.9% and 21.4%, respectively. For obesity, these numbers were 18.3% and 18.1%, respectively. This suggests the PSID national data can be used to approximate the distribution of pre-injury smoking and obesity in our study population.
Also, the PSID does not specifically identify medical-only injured workers, so we relied on smoking and BMI information on uninjured workers. This means that the estimates of pre-injury smoking and obesity assume that uninjured (from the PSID) and medical-only workers (from workers compensation data) have the same smoking and obesity probabilities. These probabilities for medical-only workers may well lie between those of uninjured and lost-time injured workers. In that case, our bias analysis will likely overestimate the impact of the missing confounders on our estimates. It will therefore underestimate the mortality hazard of lost-time injuries.
NHANES is also a national survey, and the survey years we used were 1988–1994 and 1999–2014, different from the injury years in this study. Limiting NHANES survey data to the injury years in this study (1994–2000) would not have provided adequate sample size. Also, median follow-up duration differs between our primary data and the NHANES data. Differences in smoking-related and obesity-related mortality relative risks between the NHANES and our study population could affect the validity of the bias analysis.
Basing our estimates on an NDI linkage of all workers in our sample would have provided a more accurate measure of mortality. However, given the close agreement between the SSA and NDI, we do not think that the additional cost (US$5 per SSA-identified death, US$0.21 per year per case with unknown vital status, total cost over US$500 000) would have been justified.
We did not analyse injuries and illnesses separately. However, illnesses comprised 0.6% of cases in Washington and 1.1% of cases in New Mexico. Mortality hazard estimates and CIs changed by <0.01 when we removed illnesses from the data.
CONCLUSIONS
This study used the same data elements and study design as an earlier study in New Mexico to estimate mortality HRs. Estimated HRs for Washington were close to those in New Mexico, a less populous state with lower median wages and a different workers’ compensation insurance mechanism. This suggests that results in these two states may be generalisable to other US states. Still, this association should be examined in additional locations (including other countries with different compensation, healthcare and employment systems) or with additional data on pre-injury risk factors to further understand this relationship.
Increased worker mortality adds to other burdens of workplace injury, including substantial lost earnings and physical and psychological morbidity. These results strengthen the argument for greater efforts to improve workplace safety. Future research should investigate what mechanisms, including medical interventions and improved postinjury employment, are most effective at reducing long-term mortality of workers with non-fatal workplace injuries.
Supplementary Material
WHAT IS ALREADY KNOWN ON THIS TOPIC
Studies in the USA, Canada and Taiwan have shown increased mortality following occupational injuries.
Only one study, in a US state, accounted for potentially substantial confounding by pre-injury smoking and obesity.
WHAT THIS STUDY ADDS
By using quantitative bias analysis, this study takes into account pre-injury smoking and obesity, substantial potential confounders not addressed in most other studies.
After adjusting for gender, age, earnings, industry, smoking and obesity, we found elevated mortality hazard in Washington State for both women and men with lost-time injuries.
Using the same variables and statistical approach, we found that elevated mortality in Washington State was similar to that of New Mexico, a less populous state with lower median income and a different workers’ compensation insurance mechanism.
In both states, using quantitative bias analysis reduced, but did not eliminate, the excess risk related to lost-time occupational injuries.
Estimated HRs in the two states remained similar after adjustment.
Applying the same study design in two settings strengthens the case for external validity.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
These results support greater efforts to reduce workplace injuries.
Future research should investigate what mechanisms, including medical interventions and improved postinjury employment opportunities, are most effective at reducing long-term mortality of workers with non-fatal workplace injuries.
Acknowledgements
Wubin Xie, DrPH, MPHLKC School of Medicine, Nanyang Technological University provided invaluable assistance to derive smoking-obesity mortality estimates using the National Health and Nutrition Examination Survey.
Funding
We thank the SSA and the States of Washington and New Mexico for providing access to their data. The National Institute for Occupational Safety and Health (grants R21 OH010555 and R01 OH011511) supported this work. The Boston University Medical Center Institutional Review Board (number H-32401) and the Washington State Institutional Review Board (number D-110618-L) approved this study. Data use agreements have been signed by Boston University and the Social Security Administration for the use of data from the National Center for Health Statistics, the Washington State Department of Labor and Industries and the New Mexico Workers’ Compensation Administration.
Footnotes
Competing interests None declared.
Patient consent for publication Not applicable.
Ethics approval The Boston University Medical Center Institutional Review Board and the Washington State Institutional Review Board approved this study.
Provenance and peer review Not commissioned; externally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
No data are available. Social Security Administration (SSA) data are not available to researchers who are not SSA employees. National Death Index and Washington and New Mexico Workers’ Compensation data may be available with written agreement with the relevant state agencies. NHANES and PSID data are publicly available.
REFERENCES
- 1.O’Leary P, Boden LI, Seabury SA, et al. Workplace injuries and the take-up of social security disability benefits. Soc Secur Bull 2012;72:1–17. [PubMed] [Google Scholar]
- 2.Boden LI, Reville RT, Biddle J. The adequacy of workers’ compensation cash benefits. In: Burton J, Roberts K, Bodah M, eds. Workplace injuries and disease: prevention and compensation. Kalamazoo, MI: W. E. Upjohn, 2005: 37–68. [Google Scholar]
- 3.Seabury SA, Scherer E, O’Leary P, et al. Using linked federal and state data to study the adequacy of workers’ compensation benefits. Am J Ind Med 2014;57:1165–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Keogh JP, Nuwayhid I, Gordon JL, et al. The impact of occupational injury on injured worker and family: outcomes of upper extremity cumulative trauma disorders in Maryland workers. Am J Ind Med 2000;38:498–506. [DOI] [PubMed] [Google Scholar]
- 5.Morse TF, Dillon C, Warren N, et al. The economic and social consequences of work-related musculoskeletal disorders: the connecticut upper-extremity surveillance project (cusp). Int J Occup Environ Health 1998;4:209–16. [DOI] [PubMed] [Google Scholar]
- 6.Strunin L, Boden LI. Family consequences of chronic back pain. Soc Sci Med 2004;58:1385–93. [DOI] [PubMed] [Google Scholar]
- 7.Asfaw A, Souza K. Incidence and cost of depression after occupational injury. J Occup Environ Med 2012;54:1086–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim J Depression as a psychosocial consequence of occupational injury in the US working population: findings from the medical expenditure panel survey. BMC Public Health 2013;13:303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gerasimaviciute V, Bültmann U, Diamond PM, et al. Reciprocal associations between depression, anxiety and work-related injury. Inj Prev 2020;26:529–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dong XS, Brooks RD, Cain CT. Prescription opioid use and associated factors among US construction workers. Am J Ind Med 2020;63:868–77. [DOI] [PubMed] [Google Scholar]
- 11.Asfaw A, Boden LI. Impact of workplace injury on opioid dependence, abuse, illicit use and overdose: a 36-month retrospective study of insurance claims. Occup Environ Med 2020;77:648–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ho J-J, Hwang J-S, Wang J-D. Life-expectancy estimations and the determinants of survival after 15 years of follow-up for 81 249 workers with permanent occupational disabilities. Scand J Work Environ Health 2006;32:91–8. [DOI] [PubMed] [Google Scholar]
- 13.Lin S-H, Lee H-Y, Chang Y-Y, et al. Increased mortality risk for workers with a compensated, permanent occupational disability of the upper or lower extremities: a 21-year follow-up study. Am J Epidemiol 2010;171:917–23. [DOI] [PubMed] [Google Scholar]
- 14.Scott-Marshall HK, Tompa E, Wang Y, et al. Long-term mortality risk in individuals with permanent work-related impairment. Can J Public Health 2014;105:e330–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Boden LI, O’Leary PK, Applebaum KM, et al. The impact of non-fatal workplace injuries and illnesses on mortality. Am J Ind Med 2016;59:1061–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Busey A, Asfaw A, Applebaum KM, et al. Mortality following workplace injury: quantitative bias analysis. Ann Epidemiol 2021;64:155–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Martin CJ, Jin C, Bertke SJ, et al. Increased overall and cause-specific mortality associated with disability among workers’ compensation claimants with low back injuries. Am J Ind Med 2020;63:209–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.U.S. Census Bureau, Population Division. State population Totals and components of change: 2020–2021, 2022. Available: https://www.census.gov/data/tables/time-series/demo/popest/2020s-state-total.html
- 19.U.S. Census Bureau, Population Division. Median household income by state. table H-8, 2020b. Available: https://www.census.gov/data/tables/time-series/demo/income-poverty/historical-income-households.html [Accessed 27 Dec 2020].
- 20.Doll R, Peto R, Boreham J, et al. Mortality in relation to smoking: 50 years’ observations on male British doctors. BMJ 2004;328:1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pollack KM, Sorock GS, Slade MD, et al. Association between body mass index and acute traumatic workplace injury in hourly manufacturing employees. Am J Epidemiol 2007;166:204–11. [DOI] [PubMed] [Google Scholar]
- 22.Flegal KM, Kit BK, Orpana H, et al. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA 2013;309:71–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lin T-chi, SK Verma, TK Courtney. Does obesity contribute to non-fatal occupational injury? Evidence from the National longitudinal survey of youth. Scand J Work Environ Health 2013;39:268–75. [DOI] [PubMed] [Google Scholar]
- 24.Dong XS, Wang X, Largay JA. Occupational and non-occupational factors associated with work-related injuries among construction workers in the USA. Int J Occup Environ Health 2015;21:142–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stokes A, Preston SH. Revealing the burden of obesity using weight histories. Proc Natl Acad Sci U S A 2016;113:572–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Breslin FC, Smith P. Age-related differences in work injuries: a multivariate, population-based study. Am J Ind Med 2005;48:50–6. [DOI] [PubMed] [Google Scholar]
- 27.Smith PM, Berecki-Gisolf J. Age, occupational demands and the risk of serious work injury. Occup Med 2014;64:571–6. [DOI] [PubMed] [Google Scholar]
- 28.Berecki-Gisolf J, Clay FJ, Collie A, et al. The impact of aging on work disability and return to work: insights from workers’ compensation claim records. J Occup Environ Med 2012;54:318–27. [DOI] [PubMed] [Google Scholar]
- 29.Dowd JB, Albright J, Raghunathan TE, et al. Deeper and wider: income and mortality in the USA over three decades. Int J Epidemiol 2011;40:183–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chetty R, Stepner M, Abraham S, et al. The association between income and life expectancy in the United States, 2001–2014. JAMA 2016;315:1750–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Card D, Chetty R, Weber A. Cash-on-hand and competing models of intertemporal behavior: new evidence from the labor market. Q J Econ 2007;122:1511–60. [Google Scholar]
- 32.Picciotto S, Hertz-Picciotto I . Commentary: healthy worker survivor bias: a still-evolving concept. Epidemiology 2015;26:213–5. [DOI] [PubMed] [Google Scholar]
- 33.Kivimäki M, Kawachi I. Work stress as a risk factor for cardiovascular disease. Curr Cardiol Rep 2015;17:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kivimäki M, Nyberg ST, Fransson EI, et al. Associations of job strain and lifestyle risk factors with risk of coronary artery disease: a meta-analysis of individual participant data. CMAJ 2013;185:763–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.McGonagle KA, Schoeni RF, Sastry N, et al. The panel study of income dynamics: overview, recent innovations, and potential for life course research. Longit Life Course Stud 2012;3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lash TL, Fox MP, Fink AK. Applying quantitative bias analysis to epidemiologic data. Springer Science & Business Media, 2009. [Google Scholar]
- 37.Jajtner KM, Brucker DL, Mitra S. Midlife work limitations are associated with lower odds of survival and healthy aging. Gerontol B Psychol Sci Soc Sci 2022;77:790–802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Altonji JG, Elder TE, Taber CR. Using selection on observed variables to assess bias from unobservables when evaluating Swan-Ganz catheterization. Am Econ Rev 2008;98:345–50. [Google Scholar]
- 39.Oster E Unobservable selection and coefficient stability: theory and evidence. J Bus Econ Stat 2019;37:187–204. [Google Scholar]
- 40.Galizzi M, Boden LI. The return to work of injured workers: evidence from matched unemployment insurance and workers’ compensation data. Labour Econ 2003;10:311–37. [Google Scholar]
- 41.Baldwin ML, Conway KS, Huang J-C. Post-injury work outcomes revisited. South Econ J 2009;76:47–66. [Google Scholar]
- 42.Reville RT, Boden LI, Biddle JE. An evaluation of new Mexico workers’ compensation permanent partial disability and return to work. RAND-PUBLICATIONS-MR-1414, 2001. [Google Scholar]
- 43.Woock C Earnings losses of injured men: reported and unreported injuries. Ind Relat 2009;48:610–28. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No data are available. Social Security Administration (SSA) data are not available to researchers who are not SSA employees. National Death Index and Washington and New Mexico Workers’ Compensation data may be available with written agreement with the relevant state agencies. NHANES and PSID data are publicly available.


