Abstract
Delays in vaccinating communities of color to COVID-19 have signaled a need to investigate structural barriers to vaccine uptake, with mass incarceration demanding greater characterization as a potential factor. In a nationally representative survey from February-March 2021 (N = 1,157), exposure to the criminal legal system, defined as having been incarcerated in prison or jail or having had a family member or close friend incarcerated, was associated with higher odds for COVID-19 vaccine deliberation. Individuals with criminal legal system exposure reported lower confidence in physician recommendation as a reason to get vaccinated. They were also more likely to decline vaccination out of fear it would cause COVID-19 infection, and that the vaccine might be promoted as a political tool. Our analysis suggests that populations impacted by the criminal legal system would benefit from targeted vaccine outreach by trusted community members who can address distrust during current and future pandemics.
Keywords: COVID-19, Vaccine, Deliberation, Incarceration, Prison, Jail
1. Introduction
In the early phases of COVID-19 vaccine rollout, uptake of the vaccine had lagged significantly among minoritized populations in the United States (U.S.). Survey estimates from the Centers for Disease Control and Prevention from May 2021 had reported that only about 44% of Black and 43% of Hispanic individuals were found to be fully vaccinated, compared to 56% of non-Hispanic Whites [1]. While research has targeted individual-level explanations of mistrust and low health literacy, increasingly, structural explanations have also been sought [2], [3].
Mass incarceration is a salient yet underexplored factor in COVID-19 vaccine uptake given the high burden of COVID-19 in carceral facilities [4] and its role in structural racism in the U.S. The U.S. imprisons more of its population than any other nation [5], with over two million people detained in prisons or jails at the end of 2019 [6]. The criminal legal system disproportionately criminalizes racial and ethnic minorities, with Black men found to be 5.7 times as likely as their White counterparts to be imprisoned in 2020 [6], impacting Black families and communities. While about 10% of White Americans have ever had an immediate family member incarcerated for longer than a year, this number increases to 31% for Black Americans and 29% for Native Americans [7]. Furthermore, the enduring history of medical experimentation on, and mistreatment of, people in detention centers [8], [9] underlies their levels of medical mistrust [10].
Several studies have described COVID-19 vaccine acceptance among incarcerated people, from 44.9% in a late 2020 study [11] to 66.5% in early 2021 [12]. More recently, data from March to June 2021 reported 56.7% acceptance [13]. However, little attempt has been made to describe vaccine deliberation among community members who have been affected by the criminal legal system. Furthermore, given that entire families and communities are affected by mass incarceration and are also best positioned to support and house incarcerated individuals when they are released [14], a study of people affected by the criminal legal system should ideally encompass those who have had family members incarcerated as well. We aim to evaluate individual level factors that may be associated with COVID-19 vaccine deliberation, employing an expanded definition of people who are affected by the criminal legal system. Doing so will better position public health systems to address mass incarceration, a facet of structural racism, as a driver of vaccine acceptance.
2. Material and methods
We performed a cross-sectional study using de-identified data from Wave 5 of the AmeriSpeak Omnibus survey, conducted by NORC at the University of Chicago between February 10-March 22, 2021. The survey is fielded twice per month and gathers public opinion on a variety of social topics and has been described elsewhere [15]. The AmeriSpeak panel is recruited through a multistage approach to improve demographic representation and is a probability sample based on the US postal service delivery sequence file representing approximately 97% of U.S. households. The AmeriSpeak panel recruitment rate is one of the most robust for panels of this type and applies sampling weights to account for non-response and selection bias [16]. Informed consent and an agreement to NORC’s Privacy Policy and Terms and Conditions were obtained from all participants either verbally or online. The reported survey completion rate for Wave 5 was 34.9%.
The independent variable was exposure to the “criminal legal system,” which in reality encompasses many processes of law enforcement [17]. Exposure in this study was simply defined by prior incarceration among oneself or one’s social networks, identified by an affirmative response to either: “Have you ever been incarcerated in jail or prison?” or “Have any of your family members or close friends ever been incarcerated in jail or prison?”. The dependent variable, vaccine acceptance, was characterized using responses to: “Now that a vaccine against the coronavirus is becoming available, do you plan to get vaccinated, or not?”. In lieu of the common term, “vaccine hesitancy,” “vaccine deliberation” more ethically characterizes patients’ motivations for making informed health decisions [18]. Participants were considered to be engaging in vaccine deliberation if they responded, “No, I will not get a coronavirus vaccine,” “Not sure,” or “Yes, but I will wait until it is proven safe and effective,” or accepting of the vaccine if they responded, “I already got vaccinated,” or “Yes, I will get a coronavirus vaccine as soon as it is available to me.”.
Additionally, respondents were asked about their COVID-19 preventive behaviors within the past two weeks (washing or sanitizing hands more than usual, avoiding public transit, limiting group interactions to 10 people or less, keeping a 6-foot radius from others, and wearing a mask or face covering), as well as risk-increasing behaviors (going to a bar, club, restaurant, or other social gathering; going to someone else’s home or hosting visitors at home; attending a gathering of more than 10 people; sharing items like towels or utensils with others; close contact within 6 feet with someone who was not masked; and close contact within 6 feet while the respondent was not masked).
Covariates included age, gender, self-reported race and ethnicity grouped into Hispanic, non-Hispanic Black, non-Hispanic White, and Other (defined as other non-Hispanic, Asian, and two or more races), highest level of education achieved, experience with COVID-19 (has gotten tested for COVID-19 or personally knows someone who has died because of COVID-19), geographic region, home ownership status, and political affiliation.
Respondents also selected from a list of reasons describing their degree of willingness to accept the vaccine. Reasons for getting the vaccine included: “I want to protect my family,” “I want to protect my community,” “I want to protect myself,” “My doctor recommends vaccines,” “Life won’t go back to normal until most people are vaccinated,” and “I think the majority of the public will get the vaccine,” and “Other.” Reasons for not getting the vaccine included: “I am allergic to vaccines,” “I don’t like needles,” “I’m not concerned about getting seriously ill from the coronavirus,” “I won’t have time to get vaccinated,” “I would be concerned about getting infected with the coronavirus from the vaccine,” “I would be concerned about side effects from the vaccine,” “I don’t think vaccines work very well,” “Politicians might promote a vaccine to win votes even if it is not fully tested or safe,” “The coronavirus outbreak is not as serious as some people say it is,” “I don’t think the majority of the public will get the vaccine,” and “Other.”.
Analyses were conducted after applying sample weights using IBM SPSS statistics version 28.0 (Armonk, NY). Individuals with no response to the questions on criminal legal exposure were excluded, leaving a study sample of 1,157 from a total sample of 1,161. We assessed the association between sociodemographic characteristics and criminal legal exposure using the chi-squared test of independence. We then examined the association between exposure to the criminal legal system and vaccine deliberation, adjusting for covariates using logistic regression for the whole sample, and stratified by race and ethnicity. P-values < 0.05 were considered statistically significant. The Yale Institutional Review Board classified this study as exempt from further review.
3. Results
Overall, 514 of 1157 (44.4%) respondents reported criminal legal system exposure. Individuals reporting criminal legal system exposure were more likely to be Black, have less than a college degree, and lower household income (Table 1 ). 538 (46.5%) respondents reported vaccine deliberation. Those who were reticent to get the vaccine were less likely to partake in all listed COVID-19 preventive behaviors and more likely to have been engaged in at-risk behaviors within the past two weeks compared with the acceptant group. Among those reluctant to get the vaccine, 49.6% had been exposed to the criminal legal system compared to 39.9% for the acceptant respondents (Table 2 ).
Table 1.
Participant characteristics by criminal legal exposure (N = 1157).
|
No exposure (N = 643) |
Exposure to criminal legal system (N = 514) |
Chi-squared p-value | |||
|---|---|---|---|---|---|
| Characteristic | N | % | N | % | |
| Age groups | |||||
| 18–29 | 126 | 19.6% | 114 | 22.2% | 0.2 |
| 30–44 | 165 | 25.7% | 123 | 24.0% | |
| 45–59 | 147 | 22.9% | 135 | 26.3% | |
| 60+ | 206 | 32.0% | 141 | 27.5% | |
| Gender | |||||
| Female | 319 | 49.6% | 280 | 54.6% | 0.1 |
| Male | 324 | 50.4% | 234 | 45.6% | |
| Race and ethnicity | |||||
| Non-Hispanic White | 419 | 65.2% | 307 | 59.8% | <0.001 |
| Non-Hispanic Black | 54 | 8.4% | 84 | 16.4% | |
| Hispanic | 100 | 15.6% | 93 | 18.1% | |
| Other | 70 | 10.9% | 30 | 5.8% | |
| Education | |||||
| Less than HS | 70 | 10.9% | 43 | 8.4% | <0.001 |
| HS graduate | 148 | 23.0% | 173 | 33.7% | |
| Some college | 171 | 26.6% | 150 | 29.2% | |
| Bachelor's degree | 148 | 23.0% | 82 | 16.0% | |
| Post Graduate | 107 | 16.6% | 65 | 12.7% | |
| Marital status | |||||
| Married | 348 | 54.1% | 209 | 40.7% | <0.001 |
| Widowed | 21 | 3.3% | 21 | 4.1% | |
| Divorced | 61 | 9.5% | 70 | 13.6% | |
| Separated | 17 | 2.6% | 17 | 3.3% | |
| Never married | 168 | 26.1% | 129 | 25.1% | |
| Living with partner | 28 | 4.4% | 68 | 13.3% | |
| Employment status | |||||
| Paid employee | 318 | 49.5% | 256 | 49.9% | <0.001 |
| Self employed | 53 | 8.2% | 53 | 10.3% | |
| Looking for work | 47 | 7.3% | 33 | 6.4% | |
| Retired | 143 | 22.2% | 79 | 15.4% | |
| Disabled | 38 | 5.9% | 65 | 12.7% | |
| Unemployed other | 44 | 6.8% | 27 | 5.3% | |
| Household income | |||||
| Less than $30k | 134 | 20.8% | 147 | 28.7% | <0.001 |
| $30k to under $60k | 172 | 26.7% | 159 | 31.0% | |
| $60k to under $100k | 157 | 24.4% | 125 | 24.4% | |
| $100k or more | 181 | 28.1% | 84 | 16.4% | |
| Got tested for COVID-19 | |||||
| No | 342 | 53.2% | 258 | 50.3% | 0.33 |
| Yes | 300 | 46.7% | 254 | 49.5% | |
| Know someone who died of COVID-19 | |||||
| No | 424 | 65.9% | 300 | 58.5% | 0.01 |
| Yes | 218 | 33.9% | 214 | 41.7% | |
| Region | |||||
| Northeast | 132 | 20.5% | 67 | 13.1% | 0.003 |
| Midwest | 125 | 19.4% | 115 | 22.4% | |
| South | 227 | 35.3% | 214 | 41.7% | |
| West | 159 | 24.7% | 117 | 22.8% | |
| Metro status | |||||
| Non metro | 96 | 14.9% | 96 | 18.7% | 0.09 |
| Metro area | 547 | 85.1% | 418 | 81.5% | |
| Housing status | 0.0% | ||||
| Own | 481 | 74.8% | 339 | 66.1% | 0.002 |
| Rent | 150 | 23.3% | 168 | 32.7% | |
| Not paying rent | 12 | 1.9% | 7 | 1.4% | |
| Political affiliation | |||||
| Democrat | 232 | 36.1% | 164 | 32.0% | 0.03 |
| Republican | 188 | 29.2% | 139 | 27.1% | |
| Independent | 150 | 23.3% | 119 | 23.2% | |
| Other | 71 | 11.0% | 87 | 17.0% | |
Table 2.
COVID-19 vaccine deliberation by criminal legal system exposure and COVID-19 related practices.
|
Not vaccine deliberating (N = 619) |
Vaccine deliberating (N = 538) |
Chi-squared p-value | |||
|---|---|---|---|---|---|
| N | % | N | % | ||
| Criminal legal exposure | |||||
| No | 372 | 60.1% | 271 | 50.4% | <0.001 |
| Yes | 247 | 39.9% | 267 | 49.6% | |
| Preventive behaviors | |||||
| Increased handwashing | 579 | 93.5% | 442 | 82.2% | <0.001 |
| Avoiding public transport | 525 | 84.8% | 379 | 70.4% | <0.001 |
| Limiting large group interactions | 566 | 91.4% | 369 | 68.6% | <0.001 |
| Social distancing | 553 | 89.3% | 380 | 70.6% | <0.001 |
| Wearing a face mask | 593 | 95.8% | 460 | 85.5% | <0.001 |
| Other measures | 535 | 86.4% | 397 | 73.8% | <0.001 |
| Risk-increasing behaviors | |||||
| Going out to a bar, club, or restaurant | 152 | 24.6% | 246 | 45.7% | <0.001 |
| Visiting someone's home or hosting guests | 179 | 28.9% | 320 | 59.5% | <0.001 |
| Large group interactions >10 people | 92 | 14.9% | 162 | 30.1% | <0.001 |
| Sharing personal items | 39 | 6.3% | 84 | 15.6% | <0.001 |
| Close contact with someone who was not masked | 206 | 33.3% | 256 | 47.6% | <0.001 |
| Close contact while not wearing a mask | 164 | 26.5% | 239 | 44.4% | <0.001 |
| Got tested for COVID-19 | |||||
| No | 294 | 47% | 305 | 57% | 0.002 |
| Yes | 323 | 52% | 232 | 43% | |
| Know someone who died of COVID-19 | |||||
| No | 365 | 59% | 358 | 67% | 0.01 |
| Yes | 252 | 41% | 180 | 33% | |
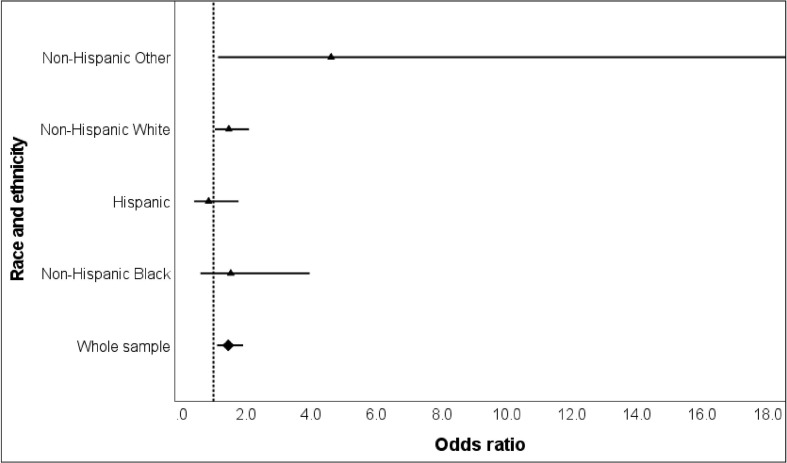
In adjusted analyses, exposure to the criminal legal system was associated with vaccine deliberation (adjusted odds ratio (AOR) = 1.45, 95% CI 1.11 to 1.90, p = 0.007) compared with no exposure. In stratified analysis, non-Hispanic White and the Other non-Hispanic racial categories with criminal legal exposure had higher odds of reporting vaccine deliberation compared to their peers without exposure (AOR = 1.46, 95% CI 1.03 to 2.07, and AOR = 4.61, 95% CI 1.14 to 16.85, respectively, Fig. 1 ).
Fig. 1.
Vaccine deliberation among respondents with criminal justice exposure (OR, and 95% confidence intervals) for whole sample and stratified by race/ethnicity; adjusted for age group, gender, education, prior COVID-19 test, knowing someone who has died of COVID-19, and political affiliation.
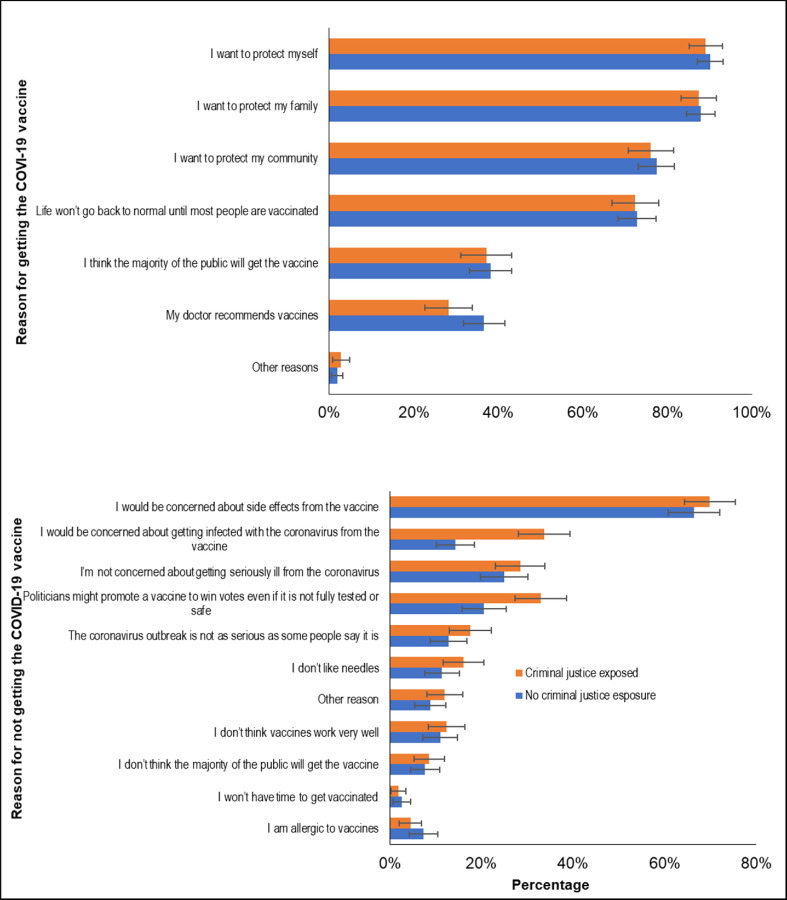
Individuals with criminal legal system exposure were less likely to report a physician’s recommendation as a reason to get vaccinated compared to the non-exposed participants (28% vs. 37%, p = 0.04). In the vaccine deliberation group, individuals with criminal legal exposure reported greater concerns of getting infected by the vaccine (34% vs. 14%, p < 0.001) or of politicians promoting the vaccine to win votes (33% vs. 21%, p = 0.001) compared to the unexposed (Fig. 2 ).
Fig. 2.
Frequency plots of reasons selected for or against COVID-19 vaccine among whole sample, stratified by criminal legal exposure.
4. Discussion
From a nationally representative sample, where half the respondents had a lifetime criminal legal system exposure, individuals with criminal legal system exposure demonstrated higher odds of reporting vaccine deliberation compared with those not exposed to the system.
Those with criminal legal exposure were less likely to accept a physician’s recommendation to get the COVID-19 vaccine. They were more likely to report not getting the vaccine because of concerns of getting infected and suspicion of a political agenda behind the vaccine roll out. In a recent study from within California jails, however, participants largely reported trusting their doctors outside of jail in general health care decisions, though trust was low in jail health workers specifically [13].
Contrary to our hypothesis, criminal legal system involvement was associated with vaccine deliberation only among non-Hispanic White people and not among racialized minorities. Exposure to the criminal legal system may be so common of an experience among racialized minorities that it has less impact on vaccine behaviors or COVID-19 prevention measures as compared with White populations, as has been the case for other health outcomes. Alternatively, there may be other salient structural and environmental factors that influence vaccine acceptance behavior among racialized minorities, including other markers of structural racism, discrimination, inadequate insurance, difficulties navigating healthcare, essential worker status, and community barriers to vaccines outside of criminal legal system exposure. This finding warrants further investigation.
The National Institutes of Health and the Centers of Disease Control and Prevention have proposed a variety of solutions to close the gap in communities under-vaccinated to COVID-19 with some guidance for carceral systems [19] and “clustered subpopulations with high rates of hesitancy” [20]. Our study identifies exposure to the criminal legal system as instrumental to vaccine-related decision making and confirms the need for population-specific strategies. Potential interventions might include community responsive vaccine-related educational interventions, disinformation counter-messaging, and novel implementation strategies in clinical and carceral settings. Interventions should address distrust of political motives and physician messaging and incorporate trustworthy sources, including community health workers or peers who have been incarcerated.
5. Limitations
Our analysis is limited in that vaccines were not available to all respondents until April 19, 2021, and follow-up ended before this date. Furthermore, self-reported exposure to criminal legal exposure can be affected by social desirability bias. Lastly, while AmeriSpeak is a robust and longstanding panel survey, the response rate may limit the generalizability of these findings.
6. Conclusions
Equity in vaccine uptake will require targeted outreach to those exposed to the criminal legal system which acknowledges distrust of health systems and politicians.
Funding
This work was supported by the National Institutes of Health through the RADx-UP initiative (Grant No: 3 UG1 DA050072-02S3), the National Institute on Minority Health and Health Disparities (Grant No: 1R01MD016853-01A1), and the Office of Student Research at the Yale School of Medicine. The sources had no involvement in conducting this study otherwise.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
We thank Phoebe Lamuda, Bruce Taylor, and John Schneider from the NORC Institution at the University of Chicago for survey design and administration, as well as for granting their permission to interpret their data. Study design was conceptualized by CK, JA, LBR, EW, and LP. JA performed statistical analysis along with input from CK, LBR, EW, and LP regarding interpretation of results. CK oversaw manuscript drafting with input from LP, EW, LBR, and JA, who each contributed to the text. All authors have approved the final article. All authors attest to meeting the ICMJE criteria for authorship.
Data availability
Data will be made available on request.
References
- 1.Demographic characteristics of people receiving COVID-19 vaccinations in the United States. Centers for Disease Control and Prevention. Accessed Jan 23, 2022. https://covid.cdc.gov/covid-data-tracker/#vaccination-demographic.
- 2.Balasuriya L., Santilli A., Morone J., Ainooson J., Roy B., Njoku A., et al. COVID-19 Vaccine Acceptance and Access Among Black and Latinx Communities. JAMA Netw Open. 2021;4(10):e2128575. doi: 10.1001/jamanetworkopen.2021.28575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Carson S.L., Casillas A., Castellon-Lopez Y., Mansfield L.N., Morris D., Barron J., et al. COVID-19 Vaccine Decision-making Factors in Racial and Ethnic Minority Communities in Los Angeles, California. JAMA Netw Open. 2021;4(9):e2127582. doi: 10.1001/jamanetworkopen.2021.27582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Saloner B., Parish K., Ward J.A., DiLaura G., Dolovich S. COVID-19 Cases and Deaths in Federal and State Prisons. JAMA. 2020;324(6):602–603. doi: 10.1001/jama.2020.12528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Highest to Lowest – Prison Population Total. World Prison Brief, Institute for Crime & Justice Policy Research. Accessed January 25, 2022. https://www.prisonstudies.org/highest-to-lowest/prison-population-total.
- 6.Carson, EA. Prisoners in 2020 – Statistical Tables. Bureau of Justice Statistics, U.S. Department of Justice; 2021. Accessed January 23, 2022. https://bjs.ojp.gov/library/publications/prisoners-2020-statistical-tables.
- 7.Enns P.K., Yi Y., Comfort M., Goldman A.W., Lee H., Muller C., et al. What Percentage of Americans Have Ever Had a Family Member Incarcerated?: Evidence from the Family History of Incarceration Survey (FamHIS) Socius. 2019;5 doi: 10.1177/2378023119829332. [DOI] [Google Scholar]
- 8.MacLure J. Unnatural Resources: The Colonial Logic of the Holmesburg Prison Experiments. J Med Humanit. 2021;42(3):423–433. doi: 10.1007/s10912-020-09651-5. [DOI] [PubMed] [Google Scholar]
- 9.Ghandakly E.C., Fabi R. Sterilization in US Immigration and Customs Enforcement's (ICE's) Detention: Ethical Failures and Systemic Injustice. Am J Public Health. 2021;111(5):832–834. doi: 10.2105/AJPH.2021.306186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Valera P., Boyas J.F., Bernal C., Chiongbian V.B., Chang Y., Shelton R.C. A Validation of the Group-Based Medical Mistrust Scale in Formerly Incarcerated Black and Latino Men. Am J Mens Health. 2018;12(4):844–850. doi: 10.1177/1557988316645152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stern M.F., Piasecki A.M., Strick L.B., Rajeshwar P., Tyagi E., Dolovich S., et al. Willingness to Receive a COVID-19 Vaccination Among Incarcerated or Detained Persons in Correctional and Detention Facilities — Four States, September–December 2020. MMWR Morb Mortal Wkly Rep. 2021;70(13):473–477. doi: 10.15585/mmwr.mm7013a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chin E.T., Leidner D., Ryckman T., Liu Y.E., Prince L., Alarid-Escudero F., et al. Covid-19 Vaccine Acceptance in California State Prisons. N Engl J Med. 2021;385(4):374–376. doi: 10.1056/NEJMc2105282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu Y.E., Oto J., Will J., LeBoa C., Doyle A., Rens N., et al. Factors associated with COVID-19 vaccine acceptance and hesitancy among residents of Northern California jails. Prev Med Rep. 2022;27:101771. doi: 10.1016/j.pmedr.2022.101771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Freudenberg N., Daniels J., Crum M., Perkins T., Richie B.E. Coming home from jail: the social and health consequences of community reentry for women, male adolescents, and their families and communities. Am J Public Health. 2005;95(10):1725–1736. doi: 10.2105/AJPH.2004.056325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.AmeriSpeak J.C.O.I.N. NORC at the University of Chicago; 2021. Brief Stigma Survey Overview. [Google Scholar]
- 16.Montgomery R, Dennis JM, Ganesh N. Response rate calculation methodology for recruitment of a two- phase probability-based panel: the case of AmeriSpeak. 2016. Accessed January 25, 2022. NORC at the University of Chicago. https://amerispeak.norc.org/Documents/Research/NORC_Labs_and_Amerispeak_launch_plans_Nov_2016_DTP_Formatted.pdf.
- 17.Bellin J., editor. Mass Incarceration Nation: How the United States Became Addicted to Prisons and Jails and How It Can Recover. Cambridge University Press; 2022. pp. 9–30. [Google Scholar]
- 18.Corbie-Smith G. Vaccine Hesitancy Is a Scapegoat for Structural Racism. JAMA Health Forum. 2021;2(3):e210434. doi: 10.1001/jamahealthforum.2021.0434. [DOI] [PubMed] [Google Scholar]
- 19.Mosites E, Nicolae L, and Hagan L. Considerations for Modifying COVID-19 Prevention Measures in Correctional and Detention Facilities. https://www.cdc.gov/coronavirus/2019-ncov/downloads/community/correction-detention/COVID-Corrections-considerations-for-loosening-restrictions-Webinar.pdf. Published June 22, 2021. Accessed March 14, 2022.
- 20.Webb Hooper M., Nápoles A.M., Pérez-Stable E.J. No Populations Left Behind: Vaccine Hesitancy and Equitable Diffusion of Effective COVID-19 Vaccines. J Gen Intern Med. 2021;36(7):2130–2133. doi: 10.1007/s11606-021-06698-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.