Abstract
Many young individuals at risk for eating disorders spend time on social media and frequently search for information related to their body image concerns. In a large randomized study, we demonstrated that a guided chat-based intervention could reduce weight and shape concerns and eating disorder pathology. The goal of the current study was to determine if a modified single session mini-course, derived from the aforementioned chat-based intervention, could reduce body image concerns among individuals using eating disorder related search terms on a social media platform. Over a two-month period of prompting individuals, 525 people followed the link to the web-based application where the intervention was hosted and subsequently completed the mini-course. This resulted in a significant improvement on the one-time body image satisfaction question pre-to post intervention (p < .001) with a moderate effect size (Cohen’s d = .54). Additionally, individuals completing the program showed significant improvement on motivation to change their body image (p < .001) with a small effect size (Cohen’s d = .28). Additionally, users reported that the program was enjoyable and easy to use. These results suggest that a single session micro-intervention, offered to individuals on social media, can help improve body image.
Keywords: Digital Intervention, Body image, Online Delivery, social media, micro-intervention, Scalability
1. Introduction
Eating disorders (EDs) are common and disabling problems and their prevalence has been increasing over the past 18 years. In a population of adolescents and adults across America, Europe, Asia and Australia, a meta-analysis showed an increase in prevalence from 3.5% in 2000–2006, to 7.8% in 2013–2018 (Galmiche et al., 2019; Klump et al., 2009). Unfortunately, less than 20% of individuals with EDs receive treatment (Kazdin et al., 2017). Therefore, preventing EDs is of significant public health importance given their prevalence, consequences, and limited access to care once problems have developed. Fortunately, risk factors for EDs have been identified and interventions to reduce these risk factors have been shown to reduce ED onset (Jacobi et al., 2004). One such program, Student Bodies, was developed as a web-based program and has been shown to reduce weight and shape concerns as well as the onset of EDs (Taylor et al., 2006; Taylor et al., 2016). Although the program was successful, one major drawback was that an important factor associated with this success was human moderation. Unfortunately, providing this moderation is a substantial barrier for real-world dissemination due to the cost and logistics. With these limitations in mind, we developed a conversational chatbot derived from the original Student Bodies program that could mirror human moderation in a scalable way. This chatbot could be interacted with in an online interface and asked guided questions via the chat window and followed with structured responses (Chan et al., 2022; Kass et al., 2014). A large randomized trial showed that use of the chatbot was associated with significant reduction in weight and shape concerns, which are highly related to body image concerns (Fitzsimmons-Craft et al., 2021). For weight/shape concerns, a risk factor for the onset of eating disorders and the primary outcome, there was a significant reduction in intervention versus control at 3-month follow-up (d = −.20; p = .03) and 6-month follow-up (d = −.19; p = .04) (Fitzsimmons-Craft et al., 2021).
In addition to being risk factors for eating disorders, body image concerns are so widespread that they are often referred to as “normative discontent” among women and are associated with significant distress (Tantleff-Dunn et al., 2011). Given the importance of EDs and the high prevalence of body image concerns in the population, public health strategies to deliver these effective interventions need to be developed. One way to reach individuals who might benefit from a body image program is to identify them via their searches on social media. We have shown that search terms can be used to identify individuals with potential EDs (Sadeh-Sharvit et al., 2020), and a number of studies have noted that many users, particularly younger ones, search for ED websites and content that are potentially harmful (Custers, 2015).
Furthermore, given how poor adherence has been to longer, structured digital interventions, there is a movement towards training in simple skills and ideas derived from more complex programs that are likely to make a difference (Dobias et al., 2022). Previous studies have shown the efficacy of technology-enhanced programs for ED and body image interventions that may be disseminated on a broader scale (Diedrichs et al., 2015). More specifically, micro-interventions informed by existing evidence-based interventions targeting validated risk factors for disordered eating and body image are shown to be effective (Atkinson & Diedrichs, 2021), much like the micro-intervention developed from the Student Bodies program. The current study builds on this model by implementing the intervention, as deployed by Koko, for at-risk users on a social media platform and focusing on body image. Koko is a non-profit that has designed a tool that can be integrated into social media platforms to detect at-risk users via their search terms and redirect them appropriately. For the purposes of this study, through Koko we were able to identify at-risk users for an ED and redirect them to the intervention hosted on Koko’s webpage (https://r.kokocares.org/body-image-journal/).
Therefore, the goal of this study was to determine if a mini-course, based on the previously established chatbot and integrated into a platform that addresses worrisome searches on social media related to EDs and other mental health problems, would (1) improve body image (pre/post) (2) motivation to change (pre/post) and if so (3) whether body image improvement would be moderated by pre-intervention motivation to change, and (4) whether the intervention would be positively received by users.
2. Methods
2.1. Participants/Recruitment
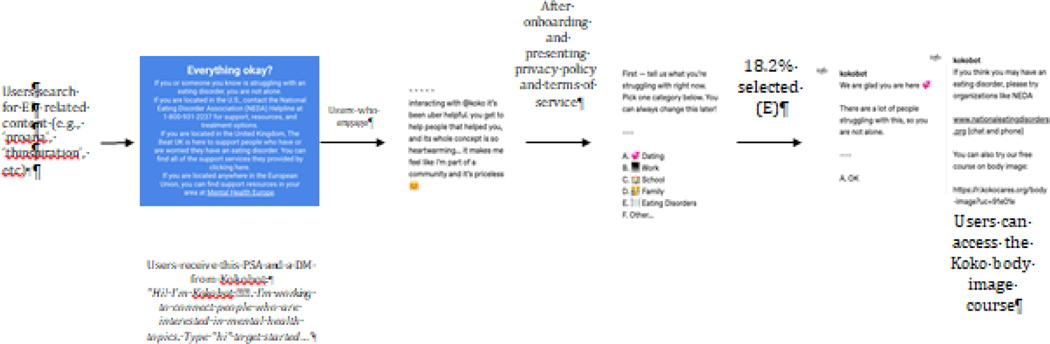
The target audience for this intervention was individuals whose online behavior on a social media platform suggested they might have body/weight and shape concerns and may be at risk for EDs. Specifically, individuals who searched for sub-forums that contained content that may be viewed as relating to anorexia, distorted body image, and other disordered eating content were identified as persons who might benefit from the intervention. To capture these individuals, a broad array of potential terms put together by the Koko team through a variety of methods (prior lists, web scraping, GPT-3 generation, and by hand) was used to flag these searches. The percent of total referrals by specific search terms that led users to the body image specific intervention platform are recorded in Table 1. These individuals were then asked a few pre-scripted questions in the embedded chat window of the social media platform and subsequently prompted to participate in mini-course style body image intervention embedded within a web application hosted by Koko (Figure 1). The process leading individuals from their search to eventually landing on the Koko webpage where the intervention was embedded is outlined in Figure 1. During this onboarding process embedded in the chat window of social media, 18.2% of all users indicated that they were struggling with “eating disorders.” Because Koko serves as a resource for more than just EDs, the 18.2% represents the percentage of all users recruited via any search term that indicated “eating disorders” as an important concern. Given that the goal of this work was only to assess acceptability of the intervention and pre-post changes in body image, demographic information was never collected to maintain anonymity. Only de-identified data were available to the investigators and the Dartmouth Institutional Review Board ruled this study exempt due to the de-identified nature of the data.
Table 1:
This table shows the top 20 search terms that prompted the Kokobot to reach out to users. The relative frequency indicates what percentage of all search terms leading to Kokobot prompts were that specific term
| term | Relative Frequency |
|---|---|
| thinspo | 7.4% |
| organic | 7.1% |
| depression | 3.9% |
| proana | 3.7% |
| self care | 2.9% |
| ana | 2.5% |
| bpd | 2.5% |
| pro ana | 2.5% |
| self harm | 2.3% |
| sad | 2.2% |
| suicide | 2.1% |
| anxiety | 2.0% |
| ed | 1.9% |
| student | 1.7% |
| meanspo | 1.6% |
| anorexia | 1.5% |
| anamia | 1.3% |
| depressed | 1.2% |
| mental illness | 1.1% |
Figure 1.
This figure shows how a typical user might be transferred from the social media platform to the Koko page. When a user searches for a term related to ED content the “Kokobot” sends a user these messages with a PSA and ultimately will refer them to the Koko webpage where the mini-course is embedded.
2.2. Intervention
The interactive mini-course was implemented in collaboration with Koko and delivered to participants that were prompted from within the social media platform. The items of the Koko mini-course were derived from the core components of our previously established chatbot (Chan et al., 2022; Fitzsimmons-Craft et al., 2021), and rewritten to fit the micro-intervention style Koko uses in their platform (Chan et al., 2022). Participants were initially prompted via a chat window (i.e., “Kokobot”) within the social media platform to answer a few questions regarding how they felt about themselves (see Figure 1 for typical journey for interested participants). Once participants had affirmed that body image is an important issue for them, they had the opportunity to follow a link that redirected them to the web application hosted by Koko that allowed users to click through the intervention materials. Within the Koko domain, individuals had the opportunity to complete the mini-course. This streamlined micro-intervention consisted of an interactive series of questions focused on many of the primary concerns and issues for individuals at risk for eating disorders. The focus of the program is on improving body image through reducing comparisons of one’s body to others, having negative conversations about bodies with others and understanding how social media reinforces the thin body ideal. The program also helps users directly challenge the thin body ideal and diet culture and it promotes healthy, regular eating (3 meals a day, eating every 3 to 4 hours and monitoring hunger levels to eat when one is hungry and to stop when one is satisfied. The whole program consists of twenty-nine interactions, including questions, feedback, exercises and other material and based on CBT and psychoeducation (Supplemental Table 1).
2.3. Measures
Participants were assessed at baseline and following the program with these questions: On a scale from 1 (very bad) to 5 (very good), how do you feel about your body image? and on a scale from 1 (not very motivated) to 5 (very motivated), how do you feel about improving your body image? Following their completion of the program, participants were prompted to rate the usefulness of the program on a scale of one to five, with one indicating complete dissatisfaction and five indicating complete satisfaction. In addition to providing quantitative feedback, participants were also prompted to provide qualitative feedback with the following question: “If you have any feedback, please write it below. If not, please proceed to the last question so you can finish the course!”
2.4. Statistical Analysis
2.4.1. Missing Data
For this study, the sample consisted only of participants who consented and subsequently committed to completing the interaction with the program. Unfortunately, because the intervention and data collection are ongoing processes, the data for the number of individuals that dropped out at the recruitment stage during the time frame of data collection for this study is no longer available. However, since the study is ongoing, we have analogous more recent data for the same intervention and recruitment methodology. This indicated that 2,843 individuals clicked on the link from social media (representing a subpopulation of the 18.2% that indicated issues with eating disorders from Figure 1), of whom 2,148 (76%) started the program and 1028 (48%) completed it. For the current study, there were 639 individuals that reached the commitment step in the intervention, and of those people, 532 continued on to the actual interaction with the mini course. At this point, only 7 of 532 individuals didn’t complete the program.
All statistical analyses were conducted twice, once following listwise deletion and once with multiple imputation by chained equations (MICE) for missing data. All multiple imputation was performed in R and utilized the MICE package (van Buuren & Groothuis-Oudshoorn, 2011). For each analysis, data were imputed with five iterations and utilized predictive mean matching to replace missing values with plausible estimates. Ultimately, due to the limited missingness, the results for both of these approaches looked essentially identical.
2.4.2. Primary Outcomes
To evaluate the effects of the intervention on improving body image, the first analysis was a paired samples t-test and Cohen’s test for effect size that assessed the change in participant’s self-indicated body image from prior to the intervention to their body image following completion of the intervention. Standard effect size guidelines were applied with 0.2, 0.5 and 0.8 representing small, medium and large effect sizes (Cohen, 1992). This same analytic approach was applied for the change in motivation to improve body image from pre to post. For the analysis of the imputed data, the test statistic was averaged over the five imputation sets (van Buuren & Groothuis-Oudshoorn, 2011).
To assess how motivation to change moderated the difference in pre-post body image, a linear mixed model was constructed to include motivation, the interaction between motivation and time, and time as fixed effects with random intercepts for individuals’ prior body image. This allowed for an estimation of both the direct impact of motivation as well as modification by motivation for body image improvement. Again, this model was fit for both imputed data as well as data following listwise deletion. All metrics for imputed data were calculated following Rubin’s rules (Rubin, 1987). Model estimates were averaged across imputation sets and standard errors were combined accounting for both the within and between imputation variation.
2.4.3. User Experience
To evaluate how much users enjoyed the mini-course, we report the distribution of user experience ratings on a scale of one to five. Additionally, we report both positive and negative examples of participant feedback following the prompt: “If you have any feedback, please write it below. If not, please proceed to the last question so you can finish the course!”
3. Results
3.1. Participants
3.1.1. Primary Outcome
The results of the paired two-sample t-test clearly indicate that there is a significant change in body image (on the one to five scale) from pre-intervention to post-intervention. On average, the change in body image was an increase of .51 with a mean baseline self-assessment of 1.66 and a mean post self-assessment of 2.17. (t(508) = 12.55, 95% CI [0.43, 0.59], p < .001). This result had a moderate effect size (Cohen’s d = .54). The results for both the analysis on the 532 individuals included in the imputed data as well as the 525 individuals included in the non-imputed data were not meaningfully different.
A secondary goal of the intervention was to increase motivation on the assumption that more motivated individuals would continue to improve their body image. On the one to five scale, the mean prior motivation to change was 3.06 and after the mini-course, the mean motivation to change was 3.42. A paired t-test indicated that this was a significant improvement (t(504) = 7.60; 95% CI [0.28, .47], p < .001). This also represented a small effect size for change in motivation (Cohen’s d = .28). Additionally, the linear mixed effect model assessing prior motivation as a moderator of change in body image suggested that more motivated individuals tended to have higher body image overall as well as greater improvements in their body image (Table 2).
Table 2.
This table shows the results of the linear mixed model with body image as the outcome and random intercepts for ID. The coefficient for time represents the change in body image from pre to post accounting for heterogenous prior body image across individuals. The fixed effect of motivation represents how being motivated effected body image overall and the interaction indicates the effect of motivation on change in body image. The results corroborate the finding that body image improves following the intervention but also shows that high motivation leads to both higher overall body image and greater increase in body image over time.
| Regression Coefficient | SE | t | p | |
|---|---|---|---|---|
| Intercept | 1.322 | 0.101 | 13.028 | <0.0001 |
| Time | 0.324 | 0.099 | 3.262 | 0.001 |
| Motivation | 0.112 | 0.030 | 3.699 | 0.0002 |
| Motivation*Time | 0.057 | 0.030 | 1.914 | 0.056 |
3.1.2. User Experience
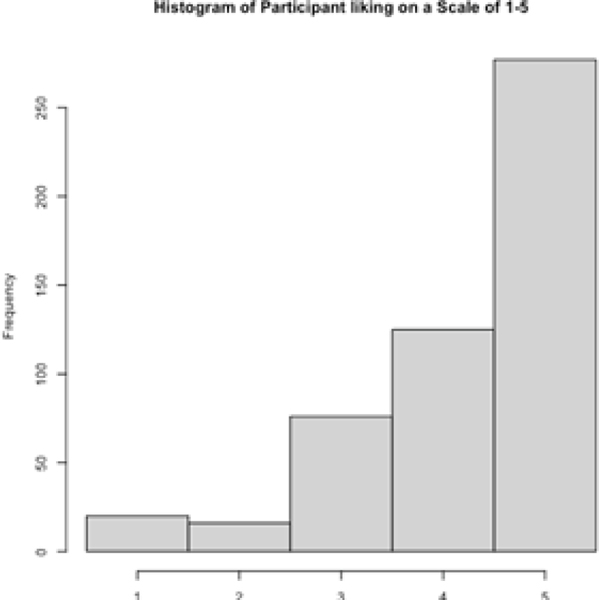
To assess user experience, we evaluated the quantitative ratings on usefulness of the program that participants gave to the mini-course. The distribution of these results can be seen via the histogram in Figure 2. The majority of participants rated the program as a five (277 participants; 54%) or four (125 participants; 24%). There were some neutral participants rating the program at a three (76 participants; 15%) and very few rating it at a one or a two (20 and 16 participants respectively; 4% and 3%). Related to time spent completing the program, it took users on average between seven and eight minutes to complete the entire program (mean = 7:18). For qualitative feedback, similar to the quantitative ratings, most users spoke positively about the program or simply did not believe any change was necessary. A sample of both positive and negative comments are reported in supplementary Figure 1.
Figure 2.
This figure shows a summary of participant feedback for the Koko.ai program. The histogram shows the distribution of participant enjoyment as rated by participant’s on a scale of 1–5.
4. Discussion
The purpose of this study was to evaluate the short-term impact of a scalable, digital, brief preventative intervention targeting body image in a real-world setting. Recruitment utilized a social media platform to identify users that searched for body image-related content. Users then completed a body image mini-course intervention, containing many of the core components of our team’s previously established chatbot, designed to be completed in a single session over the course of just a few minutes on the Koko platform. The overall results suggested that the very brief intervention had a positive effect on body image and motivation to change and that most of those who began to intervention completed it.
For this particular implementation, although the magnitude of change is small, the intervention itself has a moderate effect size which is especially beneficial given that it can be implemented at scale. This work demonstrates its public health potential as the intervention can be inexpensively introduced to individuals who might benefit from it. Perhaps even more importantly, the intervention can help reduce weight and shape concerns and motivate individuals at risk to continue to improve their body image (Jacobi et al., 2004).
Specifically related to the recruitment platform, the outcome of this work exemplifies that the current body image intervention maintains its effectiveness, even when users come from a social media. These outcomes serve as strong evidence that clinically validated interventions, such as BodyPositive, have the potential for adaptation to reach a much broader audience (Fitzsimmons-Craft et al., 2021). This finding is an extension of previous studies on the feasibility of using social media for user recruitment and the effectiveness of Internet-delivered prevention interventions for EDs (Linardon et al., 2019; Munsch et al., 2019; Naslund et al., 2019). Our findings give confidence that this type of body image intervention can be utilized more broadly to impact the many individuals that are currently facing body image issues and lack the ability to identify a need for help.
Finally, this intervention was not only effective, but also well-received as indicated by the distribution of patient ratings (Figure 2) as well as their written feedback (supplemental Figure 1). Studies related to other mental illnesses have found greater satisfaction with an intervention correlating with stronger positive outcomes (Leeuwerik et al., 2020; Regan et al., 2017; Vallentin-Holbech et al., 2019).
Although the results of the current study are promising, there are some limitations. The sample was biased as participants needed to enroll themselves and could potentially enroll multiple times, thus targeting the group able and willing to accept this form of help. This enrollment model additionally did not allow for a control group with which to compare the intervention results. Within these participants, only their immediate change was assessed, and follow-up data were not collected for this group. This lack of follow-up data prohibits us from evaluating whether these changes are maintained or whether or not additional actions would need to be taken to help maintain any positive influence from this intervention. Looking into longer term follow-up is an immediate next step for the team in helping to continue to have this intervention work in real-time and help people outside the research setting.
Related to the method of assessment, single-item questions were used to assess body image as well as motivation to improve body image. Ideally, we would have used standardized scales with more items but decided not to do so to reduce participant burden. Admittedly, individuals may interpret single items differently. For instance, some individuals may have interpreted “motivation to improve body image” as motivation to change their body whereas others may have interpreted it as motivation to change the way they think about their body. Finally, the original program enrolled mainly young (mean age was 21.1), female (100%), white (84.6%) participants (Fitzsimmons-Craft et al., 2021). Without demographic information, we don’t know how well the sample in this study maps on to the populations we have previously studied.
4.1. Conclusions
In short, the present findings converge with previous studies supporting the effectiveness of digital interventions related to body image treatment and ED prevention. This specific work exemplifies the possibility of implementing adaptations of clinically validated interventions via social media platforms and other scalable platforms outside the research domain. These findings, along with the positive sentiment for the intervention itself, give confidence that this method can be extended in implementation to further reach and help individuals with body image issues and those at risk for EDs in their daily lives.
Supplementary Material
Highlights.
Digital interventions are impactful when adapted and delivered in an online setting.
The mini-course improved body image for those searching ED terms on social media.
The mini-course was well received and can be delivered at scale.
Acknowledgments
This research is supported in part by T32 (T32DA037202–07) and P30 (P30DA029926) grants provided by the National Institute of Drug Abuse.
Conflicts of Interest
Rob Morris is the CEO and Co-Founder of Koko.
Ellen Fitzsimmons-Craft receives royalties from UpToDate.
Footnotes
Author Statement
Matthew D. Nemesure: Statistical analysis, manuscript writing, idea conceptualization
Chloe Park: Manuscript writing and revision
Rob Morris: Software design for intervention delievery, recruitment and manuscript revision.
William Chan: Intervention design and manuscript revision
Ellen Fitzsimmons-Craft: Intervention design and manuscript revision
Gavin Rackoff: Manuscript writing and revision
Lauren A. Fowler: Manuscript writing and revision
C. Barr Taylor: Intervention design, manuscript writing and revision, idea conceptualization
Nicholas C. Jacobson: Manuscript revision, statistical analysis.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Atkinson MJ, & Diedrichs PC (2021). Examining the efficacy of video based microinterventions for improving risk and protective factors for disordered eating among young adult women. International Journal of Eating Disorders, 54(5), 708–720. 10.1002/eat.23460 [DOI] [PubMed] [Google Scholar]
- Chan WW, Fitzsimmons-Craft EE, Smith AC, Firebaugh M-L, Fowler LA, DePietro B, Topooco N, Wilfley DE, Taylor CB, & Jacobson NC (2022). The challenges in designing a prevention chatbot for eating disorders: Observational study. JMIR Formative Research, 6(1), e28003. 10.2196/28003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. (1992). Statistical power analysis. Current Directions in Psychological Science, 1(3), 98–101. 10.1111/1467-8721.ep10768783 [DOI] [Google Scholar]
- Custers K. (2015). The urgent matter of online pro-eating disorder content and children: Clinical practice. European Journal of Pediatrics, 174(4), 429–433. 10.1007/s00431-015-2487-7 [DOI] [PubMed] [Google Scholar]
- Diedrichs PC, Atkinson MJ, Steer RJ, Garbett KM, Rumsey N, & Halliwell E. (2015). Effectiveness of a brief school-based body image intervention „Dove Confident Me: Single Session’ when delivered by teachers and researchers: Results from a cluster randomised controlled trial. Behaviour Research and Therapy, 74, 94–104. 10.1016/j.brat.2015.09.004 [DOI] [PubMed] [Google Scholar]
- Dobias ML, Morris RR, & Schleider JL (2022). Single-session interventions embedded within Tumblr: Acceptability, feasibility, and utility study. JMIR Formative Research, 6(7), e39004. 10.2196/39004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzsimmons-Craft EE, Chan WW, Smith AC, Firebaugh ML, Fowler LA, Topooco N, DePietro B, Wilfley DE, Taylor CB, & Jacobson NC (2021). Effectiveness of a chatbot for eating disorders prevention: A randomized clinical trial. International Journal of Eating Disorders, eat.23662. 10.1002/eat.23662 [DOI] [PubMed] [Google Scholar]
- Galmiche M, Déchelotte P, Lambert G, & Tavolacci MP (2019). Prevalence of eating disorders over the 2000–2018 period: A systematic literature review. The American Journal of Clinical Nutrition, 109(5), 1402–1413. 10.1093/ajcn/nqy342 [DOI] [PubMed] [Google Scholar]
- Jacobi C, Hayward C, de Zwaan M, Kraemer HC, & Agras WS (2004). Coming to terms with risk factors for eating disorders: Application of risk terminology and suggestions for a general taxonomy. Psychological Bulletin, 130(1), 19–65. 10.1037/0033-2909.130.1.19 [DOI] [PubMed] [Google Scholar]
- Kass AE, Trockel M, Safer DL, Sinton MM, Cunning D, Rizk MT, Genkin BH, Weisman HL, Bailey JO, Jacobi C, Wilfley DE, & Taylor CB (2014). Internet-based preventive intervention for reducing eating disorder risk: A randomized controlled trial comparing guided with unguided self-help. Behaviour Research and Therapy, 63, 90–98. 10.1016/j.brat.2014.09.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazdin AE, Fitzsimmons-Craft EE, & Wilfley DE (2017). Addressing critical gaps in the treatment of eating disorders. International Journal of Eating Disorders, 50(3), 170–189. 10.1002/eat.22670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klump KL, Bulik CM, Kaye WH, Treasure J, & Tyson E. (2009). Academy for eating disorders position paper: Eating disorders are serious mental illnesses. International Journal of Eating Disorders, 42(2), 97–103. 10.1002/eat.20589 [DOI] [PubMed] [Google Scholar]
- Leeuwerik T, Cavanagh K, Forrester E, Hoadley C, Jones A-M, Lea L, Rosten C, & Strauss C. (2020). Participant perspectives on the acceptability and effectiveness of mindfulness-based cognitive behaviour therapy approaches for obsessive compulsive disorder. PLoS One, 15(10), e0238845. 10.1371/journal.pone.0238845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linardon J, Cuijpers P, Carlbring P, Messer M, & Fuller-Tyszkiewicz M. (2019). The efficacy of app-supported smartphone interventions for mental health problems: A meta-analysis of randomized controlled trials. World Psychiatry, 18(3), 325–336. 10.1002/wps.20673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munsch S, Wyssen A, Vanhulst P, Lalanne D, Steinemann ST, & Tuch A. (2019). Binge-eating disorder treatment goes online – feasibility, usability, and treatment outcome of an Internet-based treatment for binge-eating disorder: Study protocol for a three-arm randomized controlled trial including an immediate treatment, a waitlist, and a placebo control group. Trials, 20(1), 128. 10.1186/s13063-019-3192-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naslund JA, Aschbrenner KA, McHugo GJ, Unützer J, Marsch LA, & Bartels SJ (2019). Exploring opportunities to support mental health care using social media: A survey of social media users with mental illness. Early Intervention in Psychiatry, 13(3), 405–413. 10.1111/eip.12496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Regan P, Cachelin FM, & Minnick AM (2017). Initial treatment seeking from professional health care providers for eating disorders: A review and synthesis of potential barriers to and facilitators of “first contact”. International Journal of Eating Disorders, 50(3), 190–209. 10.1002/eat.22683 [DOI] [PubMed] [Google Scholar]
- Rubin DB (1987). Multiple Imputation for Nonresponse in Surveys. John Wiley & Sons. 10.1002/9780470316696 [DOI] [Google Scholar]
- Sadeh-Sharvit S, Fitzsimmons-Craft EE, Taylor CB, & Yom-Tov E. (2020). Predicting eating disorders from Internet activity. International Journal of Eating Disorders, 53(9), 1526–1533. 10.1002/eat.23338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tantleff-Dunn S, Barnes RD, & Larose JG (2011). It’s not just a “woman thing:” The current state of normative discontent. Eating Disorders, 19(5), 392–402. 10.1080/10640266.2011.609088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor CB, Bryson S, Luce KH, Cunning D, Doyle AC, Abascal LB, Rockwell R, Dev P, Winzelberg AJ, & Wilfley DE (2006). Prevention of eating disorders in at-risk college-age women. Archives of General Psychiatry, 63(8), 881–888. 10.1001/archpsyc.63.8.881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor CB, Kass AE, Trockel M, Cunning D, Weisman H, Bailey J, Sinton M, Aspen V, Schecthman K, Jacobi C, & Wilfley DE (2016). Reducing eating disorder onset in a very high risk sample with significant comorbid depression: A randomized controlled trial. Journal of Consulting and Clinical Psychology, 84(5), 402–414. 10.1037/ccp0000077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vallentin-Holbech L, Rasmussen BM, & Stock C. (2019). Does level of received intervention dose have an impact on the effectiveness of the social norms alcohol prevention program The GOOD Life? Frontiers in Public Health, 7, 245. 10.3389/fpubh.2019.00245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Buuren S, & Groothuis-Oudshoorn K. (2011). mice: Multivariate Imputation by Chained Equations in R. Journal of Statistical Software, 45, 1–67. 10.18637/jss.v045.i03 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.