Abstract
Antimicrobial-resistant Escherichia coli isolates have emerged in various ecologic compartments and evolved to spread globally. We sought to (1.) investigate the occurrence of ESBL-producing E. coli (ESBL-Ec) in feces from free-range chickens in a rural region and (2.) characterize the genetic background of antimicrobial resistance and the genetic relatedness of collected isolates. Ninety-five feces swabs from free-range chickens associated with two households (House 1/House 2) in a rural region in northern Tunisia were collected. Samples were screened to recover ESBL-Ec, and collected isolates were characterized for phenotype/genotype of antimicrobial resistance, integrons, and molecular typing (pulsed-field gel electrophoresis (PFGE) and multilocus sequence typing (MLST)). Overall, 47 ESBL-Ec were identified, with the following genes detected: 35 blaCTX-M-1, 5 blaCTX-M-55, 5 blaCTX-M-15, 1 blaSHV-2, and 1 blaSHV-12. Resistance to fluoroquinolones, tetracycline, sulfonamides, and colistin was encoded by aac(6′)-Ib-cr (n = 21), qnrB (n = 1), and qnrS (n = 2); tetA (n = 17)/tetB (n = 26); sul1 (n = 29)/sul2 (n = 18); and mcr-2 (n = 2) genes, respectively. PFGE and MLST identified genetic homogeneity of isolates in House 1; however, isolates from House 2 were heterogeneous. Notably, among nine identified sequence types, ST58, ST69, ST224, and ST410 belong to pandemic high-risk clonal lineages associated with extrapathogenic E. coli. Minor clones belonging to ST410 and ST471 were shared by chickens from both households. The virulence genes fyuA, fimH, papGIII, and iutA were detected in 35, 47, 17, and 23 isolates, respectively. Findings indicate a high occurrence of ESBL-Ec in free-range chickens and highlight the occurrence of pandemic zoonotic clones.
Keywords: free-range chickens, ESBL, Escherichia coli, CTX-M-1, mcr-2, high-risk clone
1. Introduction
Antimicrobial resistance has emerged as a critical public health challenge globally. It has been associated with hospital (nosocomial) environments; however, antimicrobial-resistant bacteria (ARB) are increasingly reported from livestock, animal-derived food products, companion animals, wild animals, aquatic environments, and agricultural and nonagricultural soils [1,2,3] Many opportunistic and pathogenic Enterobacterales species, including Escherichia coli, have been reported as important reservoirs for multiple genes encoding resistance to clinically relevant antibiotics, such as β-lactams, fluoroquinolones, and polymixins (colistin) [4,5]. The major mechanism for β-lactam resistance is the production of β-lactamase enzymes, particularly extended-spectrum β-lactamases (ESBLs), AmpC β-lactamases (AmpC), and carbapenemases (CAP) [5,6]. These enzymes are typically plasmid-borne, thus enabling rapid spread within strains belonging to the same or different Enterobacterales genera [7,8,9]. ESBL-producing Enterobacteriales, including E. coli, are currently listed among the top twelve critical drug-resistant threats by the Centers for Disease Control and Prevention (CDC) [10]. Additionally, they are included in the World Health Organization (WHO) priority list of antibiotic-resistant bacteria to guide research, discovery, and development of new antibiotics [11].
Historically, ESBLs were primarily derived from genes for the narrow-spectrum β-lactamases (TEM-1, TEM-2, or SHV-1); however, since the early 2000s, the new CTX-M type has emerged, dramatically changing the epidemiology of ESBL enzymes, with CTX-M now the dominant enzymes worldwide (Bush and Bradford 2020). It is worth noting that, currently, approximately 243 TEM variants have been described, although not all of them are ESBLs (https://www.ncbi.nlm.nih.gov/pathogens/refgene/#TEM, accessed on 25 January 2022). The same is true for SHV enzymes; indeed, to date, 228 SHV sequence variants have been detected, although not all have been functionally characterized to determine whether they possess the ESBL phenotype (https://www.ncbi.nlm.nih.gov/pathogens/ isolates#/refgene/SHV, accessed on 25 January 2022). On the other hand, to date, at least 263 CTX-M variants, which are all ESBLs, have been identified (https://www.ncbi.nlm.nih.gov/pathogens/refgene/#CTX, accessed on 25 January 2022). The reported genetic linkage between genes encoding these ESBL enzymes with genes encoding resistance to other clinically relevant antibiotics, including aminoglycosides, tetracyclines, sulfonamides, trimethoprim, phenicols, and colistin, represents a very significant concern [12,13]. Traditionally, it was believed that excessive use of antibiotics in healthcare settings and livestock represented the major drivers for selection and transmission of these strains. However, several recent studies have documented their occurrence in wild animals, animals not having undergone antimicrobial therapies, and environments characterized by limited anthropogenic impacts or inputs [1,3,8,14]. Several hypotheses have been proposed to explain these occurrences, with perhaps the most likely being environmental spread of ARB and antimicrobial resistance genes (ARGs) via hospital effluents, municipal wastewater treatment plants (WWTPs), and the use of animal manures as agricultural fertilizers [14]. Additionally, wild animals residing in the vicinity of human conurbations and livestock-based farms have been shown to represent major vectors of ARB and ARGs, contributing to their spread across large geographic area, particularly by wild birds [1,8,15].
E. coli is a commensal bacterium of the lower intestine of warm-blooded animals and is capable of causing several human infections, including acute gastrointestinal illness (AGI), urinary tract infections, and septicemia [16]. Likewise, E. coli may cause several acute infections in agricultural animals, including colibacillosis in poultry and mastitis in cattle [16,17,18]. Since E. coli is considered a key contributor in the environmental spread of antibiotic resistance [19], it has been widely employed as an indicator for monitoring antibiotic resistance in food products and water [20,21]. To date, a paucity of scientific literature exists regarding the presence of ESBL-producing E. coli in “backyard”/free-range poultry or swine [22,23,24]. However, studies have shown that the close proximity between owners and their livestock may potentially increase transmission of ARB or ARGs from humans to animals and vice versa. In Tunisia, while previous studies have reported a high prevalence of ESBL-producing E. coli from industrial avian farms [12,25,26], to the best of the authors’ knowledge, no study has investigated the occurrence of ESBL-producing E. coli isolates in free-range chickens in rural ecosystems.
Over the past decade, many organizations and governments have adopted the “One Health” approach to assist in combating the emergence and spread of antimicrobial resistance, recommending continuous and widespread monitoring of antimicrobial resistance across a diverse range of ecosystems. Accordingly, the current study aimed to investigate the occurrence of ESBL-producing E. coli in feces from free-range chickens (poultry that are raised by free-range farming) in a rural region in northern Tunisia. Collected isolates were characterized via identification of genes encoding antibiotic resistance and virulence factors, integrons, and their phylogenetic grouping, in addition to genetic relatedness via pulsed-field gel electrophoresis (PFGE) and multilocus sequence typing (MLST).
2. Materials and Methods
2.1. Sampling Sites
The presence of ESBL-producing Enterobacteriaceae was investigated using a sample of 95 feces swabs from free-range chickens (Gallus gallus domesticus) owned by two families (House 1: n = 40; House 2: n = 55) in a rural region of northern Tunisia, collected during the period of February–March 2019. The two houses were randomly selected in one of the principal Tunisian regions of wheat crops. The region is under limited anthropogenic impacts or inputs and there were no rivers or riverines (which might contain and bring resistant bacteria or genes encoding antimicrobial resistance). Chickens were raised for supplementary income and/or household consumption, with the households located approximately 300 m apart in an agricultural area. Both subsamples were raised as free-roaming birds and fed locally available grain (wheat and barley) and kitchen scraps. Both families also reared cattle (1–3 per family), ewes (7–15 per family), domestic pets (dogs and cats), and donkeys, with chickens reared in close proximity to these animals. According to both owners, chickens did not previously receive antimicrobial agents for any purpose (therapy or growth promotion).
2.2. Feces Swab Samples and Bacterial Identification
The feces swabs were collected from each bird, stored at 4 °C, and transferred to the laboratory within 24 h, with cold chain constantly maintained. Approximately 5 mL of Brain Heart Infusion (BHI) (Oxoid Ltd., Basingstoke, UK) was added to each sample, followed by incubation at 37 °C for 2 h. Subsequently, 1 mL of enriched suspension was streaked onto tryptone bile X-glucuronide agar (TBX agar; Oxoid Ltd., Basingstoke, UK) plates supplemented with 2 mg/L of cefotaxime (Sigma-Aldrich, Munich, Germany) and incubated overnight at 37 °C [26,27] for recovery of cefotaxime-resistant Enterobacteriaceae (potential producers of ESBL and acquired pAmpC). One colony per sample (bird) was randomly selected, identified using API 20E (Bio-Mérieux. La Balme, les Grottes, France), and confirmed as E. coli via species-specific PCR amplification of the uid gene, encoding for β-glucuronidase (primers used: uid-F: 5′ ATCACCGTGGTGACGCATGTCGC 3′; uid-R: 50 CACCACGATGCCATGTTCATCTGC 3′) [28].
2.3. Antimicrobial Susceptibility Testing
Antimicrobial susceptibility testing was undertaken using the disk diffusion method on Mueller–Hinton agar (Oxoid Ltd.) plates, according to Clinical Laboratory Standard Institute guidelines [29]. The Minimal Inhibitory Concentration (MIC) for colistin was determined by the broth microdilution method [29]; isolates exhibiting an MIC ≥ 4 µg/mL were considered colistin-resistant. The double-disk synergy test (DDST) between amoxicillin/clavulanic acid (AMC, 20/10 µg) and ceftazidime (CAZ, 30 µg), aztreonam (ATM, 30 µg), and cefotaxime (CTX, 30 µg) was used to detect ESBL production (CLSI 2017). E. coli ATCC 25922 and Klebsiella pneumoniae ATCC 700603 were used as ESBL-negative and positive reference strains, respectively, with isolates considered multidrug-resistant (MDR) when found to be resistant to three or more antibiotics from different families [30].
2.4. Resistance Genotypes and Occurrence of Integrons
Genomic DNA was extracted from each isolate using the boiling method [25] and used as the DNA template for all PCR reactions. The presence of ESBL genes blaTEM, blaSHV, and blaCTX-M groups (CTX-M-1, CTX-M-2, CTX-M-8, and CTX-M-9) and OXA-1 and OXA-10 were investigated by PCR reactions [28,31,32]. blaCTX-M and blaSHV amplicons were sequenced and analyzed using BLAST software version BLAST+(2.11.0) (http://blast.ncbi.nlm.nih.gov/Blast.cgi, accessed on 25 January 2022) to determine the ESBL variant.
The following genes encoding resistance to non-β-lactams were investigated by PCR: tetracycline (tetA, tetB and tetC) [33,34], trimethoprim-sulfamethoxazole (sul1, sul2, and sul3) [35,36,37], fluoroquinolones (plasmid-mediated quinolone resistance, PMQR) (qnrA, qnrB, qnrD, qnrS, aac(6′)-Ib, and qepA) [38,39,40,41,42], and colistin (mcr-1 to mcr-5) [43,44]. Amplicons corresponding to mcr genes were sequenced, and sequences were compared with those included in the GenBank database. The presence of class 1 and 2 integrons and the 3′- conserved region (qac∆E-sul1) of class 1 integrons was examined by PCR [34]. Positive controls strains from our collection were included in all PCR reactions [12,26,27].
2.5. Detection of Genes Encoding Virulence Factors
The detection of virulence factors commonly found in pathogenic E. coli (fimH, iutA, fyuA, papG allele III, hlyA, cnf1) were identified via PCR using previously published methods [45,46].
2.6. Phylogrouping of E. coli isolates Genetic Relatedness by Pulsed-Field Gel Electrophoresis (PFGE) and Multilocus Sequence Typing (MLST)
Phylogenetic groups (A, B1, B2, C, D, E, F, and Escherichia cryptic clade I) were identified using the phylogroup assignment method of Clermont et al [47]. To assess the clonality of collected isolates, genomic DNA was prepared, digested by XbaI enzyme and analyzed by PFGE, as reported previously [34]. DNA macrorestriction patterns (pulsotypes) were visually analyzed and interpreted according to Tenover et al [48]. Dendrogram for the main phylotypes was performed using GelJ software (version 1.0) [49], based on the Dice similarity coefficient, and clustering by the unweighted pair group method with arithmetic means (UPGMA method) [50]. Bands were selected by the software and then manually annotated. In addition, representative E. coli isolates belonging to relevant PFGE profiles and harboring specific bla and mcr genes or untypeable by PFGE were studied by MLST using PCR amplification and sequencing of seven conserved housekeeping genes (adk, fumC, gyrB, icd, mdh, purA, and recA) [51]. To determine the specific allele combination and sequence type (ST), all amplicons sequences were compared with MLST databases (http://enterobase.warwick.ac.uk/species/ ecoli/allele_st_search, accessed on 25 January 2022).
3. Results
3.1. Occurrence of ESBL-Producing E. coli and Antibiotic Susceptibilities of Isolates
Overall, based on one presumptive E. coli isolate per bird, which was randomly selected and confirmed to the species level by PCR, 47 (49.4%) sampled chickens were colonized by ESBL-producing E. coli isolates. More specifically, 29 (29/40; 72.5%) and 18 (18/55; 32.7%) ESBL-producing isolates were collected from House 1 and House 2, respectively. All isolates were resistant to at least one non-β-lactam antibiotic, with the majority being characterized as MDR, with isolates primarily resistant to nalidixic acid, tetracycline, and trimethoprim–sulfamethoxazole (Table 1). Nalidixic acid resistance was detected in 25 and 13 isolates from House 1 and 2, respectively, with ciprofloxacin resistance concurrently identified in 17 of the 38 nalidixic-acid-resistant isolates. Colistin resistance was observed in three and ten isolates from chickens from House 1 and 2, respectively. Colistin MICs varied from 4 µg/mL to 16 µg/mL. Resistance to carbapenems (imipenem, meropenem, and ertapenem) was not observed.
Table 1.
Phenotypic and genotypic characteristics of the 47 ESBL-producing E. coli isolates collected from free-range chickens.
| Isolate | Phylogroup | PFGE | ST * | Resistance Profile to Non-β-Lactam Antibiotics | bla Genes | Other Genes Detected/Integrons | Virulence Genes |
|---|---|---|---|---|---|---|---|
| household 1 (29 isolates) | |||||||
| EC20 | A | P1 | ST224 | NAL, TET, SXT, SU | CTX-M-1 | aac(6′)-Ib-cr, tetB, sul1, sul2/int1 | fyuA, fimH, papGIII, |
| EC22 | A | P1 | - | NAL, TET, SXT, SU | CTX-M-1 | aac(6′)-Ib-cr, tetB, sul1, sul2/int1 | fyuA, fimH |
| EC23 | A | P1 | - | NAL, TET, SXT, SU | CTX-M-1 | aac(6′)-Ib-cr, tetB, sul1/int1 | fyuA, fimH, papGIII, |
| EC24 | A | P1 | - | NAL, TET, SXT, SU | CTX-M-1 | aac(6′)-Ib-cr, tetB, sul1, sul2/int1 | fyuA, fimH |
| EC26 | A | P1 | - | NAL, TET, SXT, SU | CTX-M-1 | aac(6′)-Ib-cr, tetB, sul1, sul2/int1 | fyuA, fimH, papGIII |
| EC27 | A | P1 | - | NAL, TET, SXT, SU | CTX-M-1 | aac(6′)-Ib-cr, tetB, sul1, sul2/int1 | fyuA, fimH, papGIII |
| EC28 | A | P1 | - | NAL, TET, SXT, SU, CS | CTX-M-1 | aac(6′)-Ib-cr, tetB, sul1, sul2/int1 | fyuA, fimH |
| EC29 | A | P1 | - | NAL, TET, SXT, SU | CTX-M-1 | aac(6′)-Ib-cr, tetB, sul1, sul2/int1 | fyuA, fimH |
| EC30 | A | P1 | - | NAL, TET, SXT, SU | CTX-M-1 | aac(6′)-Ib-cr, tetB, sul1/int1 + int2 | fyuA, fimH, papGIII |
| EC31 | A | P1 | - | NAL, CIP, TET | CTX-M-1 | -/- | fyuA, fimH, papGIII |
| EC33 | A | P1 | - | NAL, TET, SXT, SU | CTX-M-1 | tetB, sul1/int1 | fimH |
| EC34 | A | P1 | - | NAL, TET, SXT, SU | CTX-M-1 | aac(6′)-Ib-cr, tetB, sul1/int1 | fyuA, fimH, papGIII, iutA |
| EC35 | A | P1 | - | NAL, TET, SXT, SU | CTX-M-1 | aac(6′)-Ib-cr, tetB, sul1/int1 | fyuA, fimH, papGIII, |
| EC36 | A | P1 | ST69 | NAL, TET, SXT, SU | CTX-M-55 | tetB, sul1/int1 | fyuA, fimH, papGIII |
| EC37 | A | P1 | - | TET | CTX-M-1 | tetA/- | fimH, iutA |
| EC38 | A | P1 | - | NAL, TET, SXT, SU | CTX-M-1 | aac(6′)-Ib-cr, tetB, sul1/int1 | fyuA, fimH, papGIII |
| EC39 | A | P1 | - | TET | CTX-M-1 | -/- | fimH, papGIII, iutA |
| EC40 | A | P1 | - | NAL, CIP, TET, GEN, SXT, SU | CTX-M-1 | aac(6′)-Ib-cr, tetB, sul1/int1 | fimH |
| EC41 | A | P1 | ST224 | NAL, CIP, TET | CTX-M-15 | tetA/- | fyuA, fimH, iutA |
| EC43 | A | P1 | - | NAL, CIP | CTX-M-15 | -/- | fyuA, fimH iutA |
| EC45 | A | P1 | - | NAL, TET, SXT, SU | CTX-M-1 | tetB, sul1/int1 | fyuA, fimH, papGIII, iutA |
| EC46 | A | P1 | - | NAL, CIP, SXT, SU | CTX-M-1 | aac(6′)-Ib-cr, sul1/int1 | fyuA, fimH, papGIII |
| EC47 | A | P1 | - | NAL, TET, SXT, SU | CTX-M-1 | aac(6′)-Ib-cr, tetB, sul1/int1 | fyuA, fimH, papGIII |
| EC42 | A | P4 | ST410 | TET | CTX-M-15 | tetA/- | fimH, iutA |
| EC25 | F | P5 | ST471 | TET, SXT, SU | SHV-2 | -/- | fimH, iutA |
| EC21 | A | P10 | - | NAL, TET, SXT, SU | CTX-M-1 | aac(6′)-Ib-cr, tetB, sul1, sul2/int1 | fyuA, fimH |
| EC19 | A | NT | - | NAL, TET, SXT, CS | CTX-M-55 | tetB, sul1, sul2/int1 | fyuA, fimH, papGIII |
| EC32 | C | NT | - | NAL, CIP | CTX-M-15 | aac(6′)-Ib-cr, sul1/int1 | fyuA, fimH |
| EC44 | A | NT | ST617 | NAL, TET, SXT, SU, CS | CTX-M-1 | aac(6′)-Ib-cr, tetB, sul1/int1 | fyuA, fimH, papGIII |
| household 2 (18 isolates) | |||||||
| EC1 | A | P2 | ST410 | NAL, TE, SXT, SU | CTX-M-1 + OXA10 | aac(6′)-Ib-cr, tetB, sul1, sul2/int1 | fyuA, fimH, papGIII |
| EC3 | A | P2 | - | NAL, TET, SXT, SU | CTX-M-1 + OXA10 | qnrS, tetA, sul2/- | fimH |
| EC5 | A | P3 | ST1642 | NAL, CIP, TET, SXT, SU | CTX-M-1 | tetA, tetB, sul1, sul2/int1 | fyuA, fimH, iutA |
| EC6 | A | P3 | - | NAL, CIP, TET, SXT, SU, CS | CTX-M-1 | tetA, sul1, sul2/int1 | fyuA, fimH, iutA |
| EC7 | A | P3 | ST46 | NAL, CIP, TET, SXT, SU, CS | CTX-M-55 | tetA, sul1, sul2/int1 | fimH, iutA |
| EC8 | A | P3 | - | NAL, CIP, TET, SXT, SU, CS | CTX-M-1 | tetA, sul1, sul2, mcr-2/int1 + int2 | fyuA, fimH, iutA |
| EC10 | A | P3 | - | NAL, CIP, TET | CTX-M-1 | aac(6′)-Ib-cr qnrS, tetA/- | fyuA, fimH, iutA |
| EC2 | A | P4 | ST410 | NAL, CIP, TET, CS | CTX-M-1 + OXA10 | tetA, tetB, mcr-2/- | fyuA fimH, iutA |
| EC12 | A | P4 | - | TET | CTX-M-55 | tetA/- | fimH, iutA |
| EC16 | A | P4 | - | TET, CS | CTX-M-1 | tetA/- | fimH, iutA |
| EC18 | D | P4 | ST410 | NAL, CIP, TET, SXT, SU | CTX-M-1 | aac(6′)-Ib-cr, qnrB, tetA, tetB, sul2/int2 | fyuA, fimH, iutA |
| EC14 | A | P5 | ST471 | TET, GEN, CS | CTX-M-1 | tetA/- | fyuA, fimH, iutA |
| EC13 | A | P6 | ST2460 | NAL, CIP, TET, CS | CTX-M-1 | tetA/- | fyuA, fimH, iutA |
| EC17 | A | P6 | - | NAL, CIP, TET, CS | CTX-M-1 | tetA/- | fyuA, fimH, iutA |
| EC4 | C | P7 | - | NAL, CIP, TET, GEN | CTX-M-1 | tetA, sul1/int1 | fimH |
| EC9 | F | P8 | - | TET, SXT, SU, CS | SHV-12 | tetB, sul2/int2 | fyuA, fimH, iutA |
| EC15 | F | P9 | - | NAL, CIP, TET, SXT, SU | CTX-M-15 | tetB/int2 | fyuA, fimH, iutA |
| EC11 | A | NT | ST58 | TET, SXT, SU, CS | CTX-M-55 | sul1, sul2/int1 | fimH, iutA |
EC: E. coli, NAL: nalidixic acid, CIP: ciprofloxacin, SXT: trimethoprim/sulfamethoxazole; SU: sulfonamides, TET: tetracycline, GEN: gentamicin; CS: colistin, NT: not typeable, ST *: sequence type (MLST was performed for representative E. coli isolates).
3.2. Genes Encoding ESBL Enzymes and Non-β-Lactam Antibiotics
PCR analyses showed a predominance of blaCTX-type genes; blaCTX-M-1, blaCTX-M-15, and blaCTX-M-55 were detected in 35, 5, and 5 isolates, respectively, with blaSHV-2 and blaSHV-12 both detected in one (differing) isolate (Table 1). The blaOXA-10 gene was concomitantly present with the blaCTX-M-1 gene in three isolates from chickens from House 2 (Table 1), while the blaTEM gene remained undetected.
Among the 38 nalidixic-acid-resistant isolates, 21, 2, and 1 isolates harbored aac(6′)-Ib-cr, qnrS, and qnrB genes, respectively. The aac(6′)-Ib-cr gene was found in isolates from both houses (House 1: 18/25; House 2: 3/13); however, the qnrS and qnrB genes were only found in isolates from House 2, and they were associated with the aac(6′)-Ib-cr gene (Table 1). Among the 44 tetracycline-resistant isolates, the tetB gene (n = 26) was more prevalent than tetA (n = 14), with both tet genes found to co-occur in three isolates from House 2. Thirty-two isolates were sulfonamides-resistant and concurred with the presence of sul1 and sul2 genes in 29 and 18 isolates, respectively. Both genes were concomitantly detected in 15 isolates. The mcr-2 gene (the sequence is provided in the Supplementary Materials) was detected in two colistin-resistant E. coli isolates from ten resistant isolates (House 2 only), with mcr-1 not detected. Class 1 integron was detected in 29 isolates, while class 2 integron was detected in just five isolates (Table 1). Both integrons were concurrently present in one isolate (House 2). All int1-positive isolates amplified the conserved 3′ region (qac∆E-sul1).
3.3. Virulence Genes
The fimH, fyuA, iutA, and papGIII genes were detected in 47 (100%), 35 (74.4%), 23 (48.9%), and 17 (36.1%) ESBL-producing isolates, respectively. The cnf1 gene was not detected. The papGIII gene was notably more prevalent among E. coli isolates from House 1 (n = 16; 55.1%) than House 2 (n = 1; 5.5%), while conversely, iutA was more prevalent among isolates from House 2 (n = 15; 83.3%) than House 1 (n = 8; 27.5%) (Table 1).
3.4. Phylogenetic Groups and Genetic Relatedness
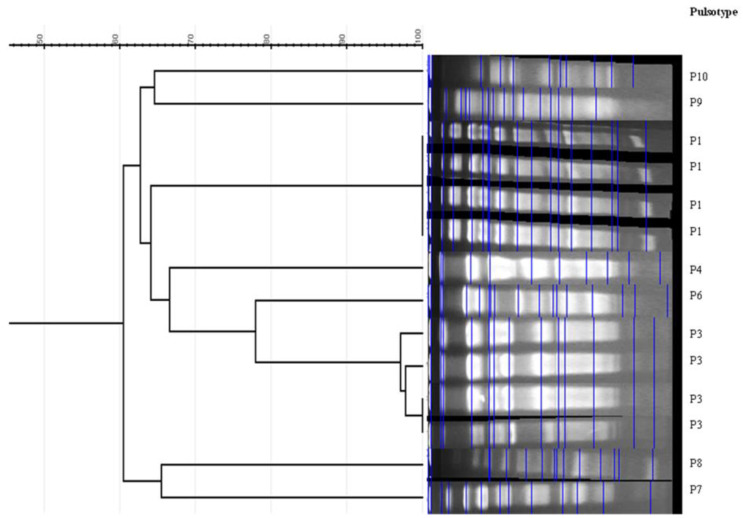
The majority of isolates belonged to phylogroup A (n = 41; 87.2%), with phylogroups F, C, and D represented by 3, 2, and 1 isolates, respectively. Four isolates were untypeable (DNA degraded) via PFGE, with the remaining 43 isolates classified into ten pulsotypes (P1 to P10) (Table 1, Figure 1). The predominant pulsotype P1 encompassed 23 isolates, all of which were collected from House 1. The remaining three typeable isolates in this house belonged to pulsotypes P4, P5, and P10. Conversely, isolates from House 2 exhibited a significantly higher level of diversity, with eight pulsotypes identified: pulsotypes P2, P3, P4, and P6 characterized 2, 5, 4, and 2 isolates, respectively. Pulsotypes P4 and P5 were shared by isolates collected from both Houses (Table 1). MLST was performed for 14 selected isolates, and the following STs were identified: ST224 (House 1/P1, 2 isolates), ST69 (House 1/P1, 1 isolate), ST410 (House 1 and 2/P4, 3 isolates; house 2/P2, 1 isolate), ST471 (House 1 and 2/P5, 2 isolates), ST617 (House 1/PFGE un-typeaple, 1 isolate), ST1642 (House 2/P3, 1 isolate), ST2460 (House 2/P6, 1 isolate), ST46 (House 2/P3, 1 isolate), and ST58 (House 2/PFGE un-typeable, 1 isolate) (Table 1).
Figure 1.
Representative PFGE cluster analysis of the main detected pulsotypes.
4. Discussion
The current study collected 95 feces swab samples from two neighboring (≈300 M) chicken (G. domesticus)-rearing households in a rural area of northern Tunisia, 47 (49.4%) of which were colonized by ESBL-producing E. coli isolates. Chickens from House 1 exhibited a significantly higher percentage of colonization by ESBL-producing E. coli isolates than House 2 (29 (72.5%) versus 18 (32.7%) isolates). The high occurrence of ESBL-producing E. coli found in the current study mirrors the high rates reported from poultry farms employing intensive production methods, both in Tunisia and further afield [52,53,54]. For example, a recent study by Subramanya et al [55] reported that 19 out of 66 (28.8%) cloacal swab samples from healthy G. domesticus were ESBL positive, of which 16 isolates (16/66; 28.7%) were ESBL-producing E. coli. Conversely, Shoaib et al [56] employed nonselective media for E. coli isolation from 150 sick backyard chickens (free-range), identifying just 8 (5.3%) ESBL-producing E. coli isolates. The majority of isolates from the current study were MDR, a trait commonly reported among ESBL-producing E. coli irrespective of their origin [12,26,27,57]. The high rate of gut colonization by ESBL-producing E. coli in organically raised chickens was unexpected, considering the (owner-reported) absence of previous antibiotic usage. Additionally, residents from both sampled houses reported that antibiotics had not previously been used for other proximal animals (cows, owe, dogs, pet, and donkeys). Accordingly, the role of antibiotic use among sampled chickens as a driver of multidrug-resistant ESBL-producing E. coli was deemed unlikely, if not impossible; thus, other pathways for resistance must have been present. For example, in both houses, free-range chickens were frequently in contact with household members and (presumably) wild animals, such as birds and rats, which were potentially colonized with ESBL-producing E. coli. Indeed, notwithstanding consumption of kitchen waste and proximity to wastewater, in many rural communities, householders frequently defecate and/or urinate adjacent to areas where chickens move freely. As such, potential transmission of human- or animal-derived ESBL-producing E. coli to chickens is plausible. Similarly, free-range chickens are omnivorous and permitted to roam freely and consume wheat grains, a variety of insects, plant debris, and vegetable wastes. Previous studies have reported insects (e.g., flies and cockroaches) as important reservoirs for ESBL-producing E. coli in both urban and rural environments [58,59,60]. Similarly, several studies have reported contamination of vegetables and plant organic matter by ESBL-producing E. coli [61,62]. Given the complexity of antimicrobial resistance and its transmission within and between various ecological niches, it is extremely difficult to confidently trace and identify the origins of antimicrobial resistance acquisition. The limit of this study was the absence of analysis of samples from humans, soil, and animals in both houses; this would have provided important data about the reservoirs/vectors of the collected isolates.
An understanding of the epidemiology of genes encoding ESBL enzymes might be employed to indicate the possible origins of ESBL-producing E. coli isolates. In Tunisia, blaCTX-M-1 has been shown to represent the dominant gene encoding ESBL production in E. coli isolated from poultry samples [13,27,52,53], while blaCTX-M-15 typically predominates among human-derived ESBL-producing E. coli [63,64]. In the current study, blaCTX-M-1 was detected in 35 of 47 isolates, followed by blaCTX-M-15 (n = 5) and blaCTX-M-55 (n = 5). The blaCTX-M-55 gene has been frequently reported among livestock in Asian countries [65]; recent studies from Tunisia have reported increasing emergence among avian ESBL-producing E. coli [27], in addition to recently being found for the first time among E. coli isolates from urban wastewater samples [12,26]. Notably, and to the best of the authors knowledge, this is the first report of the presence of blaOXA-10, herein found in three isolates in concurrence with blaCTX-M-1, among ESBL-producing E. coli of animal origin. OXA-10 (PSE-2), belonging to class D β-lactamases, is not an ESBL enzyme but possesses the ability to hydrolyze cephalosporins, hydrolyzing cefotaxime, ceftriaxone, and aztreonam at low levels but sparing ceftazidime, cephamycins, and carbapenems [66]. This enzyme is primarily detected in ESBL-producing Pseudomonas aeruginosa and Acinetobacter baumannii isolates [67,68] but rarely from E. coli [69].
Colistin is one of the “last-resort” antimicrobial agents for treatment of infections caused by ESBL/plasmidic AmpC/Carbpenemase-producing Enterobacteriaceae. Over the past 5–7 years, acquired mobile colistin resistance (mcr) determinants have increasingly been reported worldwide, with at least 10 variants (mcr-1 to mcr-10) having been characterized [70]. In the current study, two of ten colistin-resistant isolates carried the mcr-2 gene, with mcr-1 remaining undetected. To date, while the mcr-1 and mcr-2 genes have never been reported in human-derived enterobacteria in Tunisia, mcr-1 has been increasingly reported among animal-derived ESBL-producing E. coli, including poultry [27,71], dairy cattle [72], camels [53], and wastewater treatment plants [26]. Accordingly, to the best of the authors’ knowledge, the current study is the first to report the occurrence of mcr-2 from animal origin in Tunisia.
In the current study, genetic determinants for tetracycline and sulfonamide resistance were predominantly encoded by the globally ubiquitous tetA/tetB and sul1/sul2 genes, respectively [12,26,27,53,72]. With respect to plasmid-mediated quinolone resistance (PMQR) determinants, the aac(6′)-Ib-cr gene dominated, followed by qnrS and qnrB genes, all of which are frequently reported in ESBL-producing E. coli from various origins [5,12,26,27,72,73,74]. The aforementioned genes were primarily identified as being plasmid borne or a part of integron structures, which enhances their horizontal transfer within strains belonging to the same genera or between different enterobacteria genera. Class 1 integrons were detected in 27 isolates, whereas class 2 integrons were detected in just four isolates. The predominance of class 1 integrons has been well documented [12,25,26,27,72] and is almost certainly associated with the active integrase gene of class 1 integron, which has the ability to integrate several gene cassettes encoding antibiotic resistance in their variable regions [75].
Genetic relatedness determined by PFGE indicated a low level of isolate heterogeneity within each sampled household, albeit one analogous clone (pulsotype) being identified within each subsample. Within household 1, pulsotype P1 comprised 23 out of 29 isolates, with this clone not detected in household 2. Pulsotype P1 exhibited highly variable resistance profiles, antimicrobial resistance genes, virulence factors, and integron content, thus pointing to a high degree of genetic dynamicity. Three isolates of this pulsotype were types by MLST and revealed two isolates belonging to the ST224 (CTX-M-1/CTX-M-15) and one ST69 (CTX-M-55), which are known as pandemic or international high-risk clonal lineages. ST224 appears to be well adapted to the human–animal interface, being reported globally, including Tunisia (North Africa), mostly in association with plasmid-mediated blaCTX-M-type genes [13,76]. The clonal lineage ST69 (CTX-M-55-positive) has been reported in other studies from clinical, livestock, and environmental samples [12,13,77], and it is one of the most common lineages of extraintestinal pathogenic E coli [78]. In addition, the unique isolate of pulsotype P4 in household 1 was assigned to ST410, which is also known as a high-risk clonal lineage associated with both nosocomial and community-acquired infections and is being increasingly detected from multiple origins worldwide, including Tunisia [13,78]. However, the ST471 (pulosotype 5) and ST617 (untypable by PFGE) lineages have been rarely reported from human and animal origins and are mostly associated with ESBL or carabapenemase production [79,80]. Conversely, despite a lower number of studied isolates, isolates from household 2 were more heterogeneous, with four pulsotypes characterizing more than one isolate, all of them also concurrent with variable phenotypic and genotypic traits. In addition, six different STs were identified (ST46, ST58, ST410, ST471, ST1642, and ST2460). Significantly, ST410 and ST471 were shared by isolates collected from both houses, potentially indicating transmission of ESBL-producing E. coli between chickens reared in the two houses. This may be expected, since in this rural zone, contact between chickens and livestock from differing houses within the same neighborhood is relatively common. It is also plausible that chickens were contaminated by a common vector(s) or source(s) within the general vicinity. A sizeable majority of isolates belonged to phylogroup A (87.2%), followed by phylogroups F (n = 3), C (n = 2), and D (n = 1); however, no isolates from phylogroup B2 were identified. Several studies have shown that avian E. coli strains are primarily assigned to commensal phylogroups A and B1, with a majority of extraintestinal pathogenic E. coli isolates of human origin associated with phylogroup B2, and to a lesser degree, group D [81]. However, the detected virulence genes (fyuA, fimH, papGIII, and iutA) are commonly reported among both avian pathogenic E. coli (APEC) and extrapathogenic E. coli causing human infections [17,82], thus highlighting the zoonotic potential of these isolates to cause human infections, albeit additional virulence genes require future investigation to confirm this hypothesis.
5. Conclusions
The presented study highlights the significant prevalence of ESBL-E. coli isolates among free-range chickens, the predominance of blaCTX-M-1 gene, and the likely spread of two minor clones, ST410 and ST471, known as international high-risk clonal lineages, between two proximal subsamples within a rural area of northern Tunisia. However, since only limited chicken samples and rural houses were analyzed, it is impossible to deeply understand the real epidemiology of ESBL-producing E. coli isolates from free-range chickens in this area. Many factors can influence the occurrence of such isolates in these chickens, such as colonization of the residents from both sampled houses and animals (domestic and wild) in their vicinity. Therefore, the main limit of this study was the studying of chickens separately from their biotic and abiotic environment in order to accomplish the goal of the “One health” concept.
Acknowledgments
This work was supported by the Institution of Agricultural Research and Higher Education (IRESA), Tunisia.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/genes14040875/s1, Sequence of mcr-2 gene identified in Escherichi coli EC2 and EC8 isolates. Identical to the sequence accession no: MW811416.
Author Contributions
Conceptualization, S.B. and M.S.A.; methodology, S.B.; validation, S.B.; A.R.; T.G. and S.L.; formal analysis, S.B.; investigation, S.B. and S.C.; resources, M.S.A.; data curation, M.S.A.; writing—original draft preparation, S.B.; writing—review and editing, W.A.; P.H.; and T.G.; visualization, M.S.A.; supervision, T.G.; project administration, M.S.A.; funding acquisition, M.S.A. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Ethical review and approval were waived for this study since feces samples were collected without handling of chickens.
Informed Consent Statement
Not applicable.
Data Availability Statement
All data generated and analyzed during our study are included in this article.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Abbassi M.S., Badi S., Lengliz S., Mansouri R., Salah H., Hynds P. Hiding in plain sight-wildlife as a neglected reservoir and pathway for the spread of antimicrobial resistance: A narrative review. FEMS Microbiol. Ecol. 2022;98:fiac045. doi: 10.1093/femsec/fiac045. [DOI] [PubMed] [Google Scholar]
- 2.Ramos S., Silva V., Dapkevicius M.D.L.E., Caniça M., Tejedor-Junco M.T., Igrejas G., Poeta P. Escherichia coli as Commensal and pathogenic bacteria among food-producing animals: Health implications of extended spectrum β-lactamse (ESBL) production. Animals. 2020;10:2239. doi: 10.3390/ani10122239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Skandalis N., Maeusli M., Papafotis D., Miller S., Lee B., Theologidis I., Luna B. Environmental spread of antibiotic resistance. Antibiotics. 2021;10:640. doi: 10.3390/antibiotics10060640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Azargun R., Gholizadeh P., Sadeghi V., Hosainzadegan H., Tarhriz V., Memar M.Y., Pormohammad A., Eyvazi S. Molecular mechanisms associated with quinolone resistance in Enterobacteriaceae: Review and update. Trans. R. Soc. Trop. Med. Hyg. 2020;114:770–781. doi: 10.1093/trstmh/traa041. [DOI] [PubMed] [Google Scholar]
- 5.De Angelis G., Del Giacomo P., Posteraro B., Sanguinetti M., Tumbarello M. Molecular mechanisms, epidemiology, and clinical importance of β-lactam resistance in Enterobacteriaceae. Int. J. Mol. Sci. 2020;21:5090. doi: 10.3390/ijms21145090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cherak Z., Loucif L., Moussi A., Rolain J.-M. Carbapenemase-producing Gram-negative bacteria in aquatic environments: A review. J. Glob. Antimicrob. Resist. 2021;25:287–309. doi: 10.1016/j.jgar.2021.03.024. [DOI] [PubMed] [Google Scholar]
- 7.Bush K., Bradford P.A. Epidemiology of β-lactamase-producing pathogens. Clin. Microbiol. Rev. 2020;33:e00047-19. doi: 10.1128/CMR.00047-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dolejska M., Papagiannitsis C.C. Plasmid-mediated resistance is going wild. Plasmid. 2018;99:99–111. doi: 10.1016/j.plasmid.2018.09.010. [DOI] [PubMed] [Google Scholar]
- 9.Madec J.-Y., Haenni M. Antimicrobial resistance plasmid reservoir in food and food-producing animals. Plasmid. 2018;99:72–81. doi: 10.1016/j.plasmid.2018.09.001. [DOI] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention (CDC) Antibiotic/Antimicrobial Resistance-Biggest Threats. [(accessed on 14 November 2017)]; Available online: http://www.cdc.gov/drugresistance/biggest_threats.html.
- 11.Tacconelli E., Magrini N., Kahlmeter G., Singh N. Global Priority List of Antibiotic-Resistant Bacteria to Guide Research, Discovery, and Development of New Antibiotics. World Health Organization; Geneva, Switzerland: 2017. [Google Scholar]
- 12.Hassen B., Abbassi M.S., Ruiz-Ripa L., Mama O.M., Ibrahim C., Benlabidi S., Hassen A., Torres C., Hammami S. Genetic characterization of extended-spectrum β-lactamase-producing Enterobacteriaceae from a biological industrial wastewater treatment plant in Tunisia with detection of the colistin-resistance mcr-1 gene. FEMS Microbiol. Ecol. 2021;97:fiaa231. doi: 10.1093/femsec/fiaa231. [DOI] [PubMed] [Google Scholar]
- 13.Sghaier S., Abbassi M.S., Pascual A., Serrano L., De-Alba P.D., Ben Said M., Hassen B., Ibrahim C., Hassen A., López-Cerero L. Extended-spectrum β-lactamase-producing Enterobacteriaceae from animal origin and wastewater in Tunisia: First detection of O25b-B23-CTX-M-27-ST131 Escherichia coli and CTX-M-15/OXA-204-producing Citrobacter freundii from wastewater. J. Glob. Antimicrob. Resist. 2019;17:189–194. doi: 10.1016/j.jgar.2019.01.002. [DOI] [PubMed] [Google Scholar]
- 14.Zhuang M., Achmon Y., Cao Y., Liang X., Chen L., Wang H., Siame B.A., Leung K.Y. Distribution of antibiotic resistance genes in the environment. Environ. Pollut. 2021;285:117402. doi: 10.1016/j.envpol.2021.117402. [DOI] [PubMed] [Google Scholar]
- 15.Samanta A., Mahanti A., Chatterjee S., Joardar S.N., Bandyopadhyay S., Sar T.K., Mandal G.P., Dutta T.K., Samanta I. Pig farm environment as a source of β-lactamase or AmpC-producing Klebsiella pneumoniae and Escherichia coli. Ann. Microbiol. 2018;68:781–791. doi: 10.1007/s13213-018-1387-2. [DOI] [Google Scholar]
- 16.Denamur E., Clermont O., Bonacorsi S., Gordon D. The population genetics of pathogenic Escherichia coli. Nat. Rev. Genet. 2020;19:37–54. doi: 10.1038/s41579-020-0416-x. [DOI] [PubMed] [Google Scholar]
- 17.Kathayat D., Lokesh D., Ranjit S., Rajashekara G. Avian Pathogenic Escherichia coli (APEC): An overview of virulence and pathogenesis factors, zoonotic potential, and control strategies. Pathogens. 2021;10:467. doi: 10.3390/pathogens10040467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wenz J., Barrington G., Garry F., Ellis R., Magnuson R. Escherichia coli isolates’ serotypes, genotypes, and virulence genes and clinical coliform mastitis severity. J. Dairy Sci. 2006;89:3408–3412. doi: 10.3168/jds.S0022-0302(06)72377-3. [DOI] [PubMed] [Google Scholar]
- 19.Szmolka A., Nagy B. Multidrug resistant commensal Escherichia coli in animals and its impact for public health. Front. Microbiol. 2013;4:258. doi: 10.3389/fmicb.2013.00258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Andrade L., Kelly M., Hynds P., Weatherill J., Majury A., O’Dwyer J. Groundwater resources as a global reservoir for antimicrobial-resistant bacteria. Water Res. 2019;170:115360. doi: 10.1016/j.watres.2019.115360. [DOI] [PubMed] [Google Scholar]
- 21.EFSA: European Food Safety Authority Report from the Task Force on Zoonoses Data Collection including guidance for harmonized monitoring and reporting of antimicrobial resistance in commensal Escherichia coli and Enterococcus spp. from food animals. EFSA J. 2008;141:141. [Google Scholar]
- 22.Samanta I., Joardar S.N., Das P.K., Das P., Sar T.K., Dutta T.K., Bandyopadhyay S., Batabyal S., Isore D.P. Virulence repertoire, characterization, and antibiotic resistance pattern analysis of Escherichia coli isolated from backyard layers and their environment in India. Avian Dis. 2014;58:39–45. doi: 10.1637/10586-052913-Reg.1. [DOI] [PubMed] [Google Scholar]
- 23.Samanta I., Joardar S.N., Mahanti A., Bandyopadhyay S., Sar T.K., Dutta T.K. Approaches to characterize extended spectrum β-lactamase/β-lactamase producing Escherichia coli in healthy organized vis-a-vis backyard farmed pigs in India. Infect. Genet. Evol. 2015;36:224–230. doi: 10.1016/j.meegid.2015.09.021. [DOI] [PubMed] [Google Scholar]
- 24.Samanta I., Joardar S.N., Das P.K., Sar T.K. Comparative possession of Shiga toxin, intimin, enterohaemolysin and major extended spectrum β-lactamase (ESBL) genes in Escherichia coli isolated from backyard and farmed poultry. Iran J. Vet. Res. 2015;16:90–93. [PMC free article] [PubMed] [Google Scholar]
- 25.Dhaouadi S., Soufi L., Hamza A., Fedida D., Zied C., Awadhi E., Mtibaa M., Hassen B., Cherif A., Torres C., et al. Co-occurrence of mcr-1 mediated colistin resistance and β-lactamase-encoding genes in multidrug-resistant Escherichia coli from broiler chickens with colibacillosis in Tunisia. J. Glob. Antimicrob. Resist. 2020;22:538–545. doi: 10.1016/j.jgar.2020.03.017. [DOI] [PubMed] [Google Scholar]
- 26.Hassen B., Abbassi M.S., Benlabidi S., Ruiz-Ripa L., Mama O.M., Ibrahim C., Hassen A., Hammami S., Torres C. Genetic characterization of ESBL-producing Escherichia coli and Klebsiella pneumoniae isolated from wastewater and river water in Tunisia: Predominance of CTX-M-15 and high genetic diversity. Environ. Sci. Pollut. Res. 2020;27:44368–44377. doi: 10.1007/s11356-020-10326-w. [DOI] [PubMed] [Google Scholar]
- 27.Hassen B., Abbassi M.S., Ruiz-Ripa L., Mama O.M., Hassen A., Torres C., Hammami S. High prevalence of mcr-1 encoding colistin resistance and first identification of blaCTX-M-55 in ESBL/CMY-2-producing Escherichia coli isolated from chicken faeces and retail meat in Tunisia. Int. J. Food Microbiol. 2020;318:108478. doi: 10.1016/j.ijfoodmicro.2019.108478. [DOI] [PubMed] [Google Scholar]
- 28.Jouini A., Vinué L., Ben Slama K., Sáenz Y., Klibi N., Hammami S., Boudabous A., Torres C. Characterization of CTX-M and SHV extended-spectrum -lactamases and associated resistance genes in Escherichia coli strains of food samples in Tunisia. J. Antimicrob. Chemother. 2007;60:1137–1141. doi: 10.1093/jac/dkm316. [DOI] [PubMed] [Google Scholar]
- 29.Clinical Laboratory Standards Institute . In: Performance Standards for Antimicrobial Susceptibility Testing. 27th ed. Wayne P.A., editor. Clinical and Laboratory Standards Institute; Wayne, PA, USA: 2017. CLSI Supplement, M100. [Google Scholar]
- 30.Magiorakos A.-P., Srinivasan A., Carey R.B., Carmeli Y., Falagas M.E., Giske C.G., Harbarth S., Hindler J.F., Kahlmeter G., Olsson-Liljequist B., et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: An international expert proposal for interim standard definitions for acquired resistance. Clin. Microbiol. Infect. 2012;18:268–281. doi: 10.1111/j.1469-0691.2011.03570.x. [DOI] [PubMed] [Google Scholar]
- 31.Bhattacharjee A., Sen M.R., Prakash P., Anupurba S. Role of beta-lactamase inhibitors in enterobacterial isolates producing extended-spectrum beta-lactamases. J. Antimicrob. Chemother. 2007;61:309–314. doi: 10.1093/jac/dkm494. [DOI] [PubMed] [Google Scholar]
- 32.Steward C.D., Rasheed J.K., Hubert S.K., Biddle J.W., Raney P.M., Anderson G.J., Williams P.P., Brittain K.L., Oliver A., McGowan J.E., et al. Characterization of clinical isolates of Klebsiella pneumoniae from 19 laboratories using the National Committee for Clinical Laboratory Standards extended-spectrum β-lactamase detection methods. J. Clin. Microbiol. 2001;39:2864–2872. doi: 10.1128/JCM.39.8.2864-2872.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Guardabassi L., Dijkshoorn L., Collard J.-M., Olsen J., Dalsgaard A. Distribution and in-vitro transfer of tetracycline resistance determinants in clinical and aquatic Acinetobacter strains. J. Med. Microbiol. 2000;49:929–936. doi: 10.1099/0022-1317-49-10-929. [DOI] [PubMed] [Google Scholar]
- 34.Sáenz Y., Briñas L., Domίnguez E., Ruiz J., Zarazaga M., Vila J., Torres C., Petraitis V., Petraitiene R., Kelaher A.M., et al. Mechanisms of resistance in multiple-antibiotic-resistant Escherichia coli strains of human, animal, and food origins. Antimicrob. Agents Chemother. 2004;48:3959–3967. doi: 10.1128/AAC.48.10.3996-4001.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Maynard C., Fairbrother J.M., Bekal S., Sanschagrin F., Levesque R.C., Brousseau R., Masson L., Larivière S., Harel J. Antimicrobial resistance genes in Enterotoxigenic Escherichia coli O149:K91 isolates obtained over a 23-year period from pigs. Antimicrob. Agents Chemother. 2003;47:3214–3221. doi: 10.1128/AAC.47.10.3214-3221.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mazel D., Dychinco B., Webb V.A., Davies J. Antibiotic resistance in the ECOR collection: Integrons and identification of a novel aad Gene. Antimicrob. Agents Chemother. 2000;44:1568–1574. doi: 10.1128/AAC.44.6.1568-1574.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Perreten V., Boerlin P. A new sulfonamide resistance gene ( sul3 ) in Escherichia coli is widespread in the pig population of Switzerland. Antimicrob. Agents Chemother. 2003;47:1169–1172. doi: 10.1128/AAC.47.3.1169-1172.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gay K., Robicsek A., Strahilevitz J., Park C.H., Jacoby G., Barrett T.J., Medalla F., Chiller T.M., Hooper D.C. Plasmid-Mediated Quinolone Resistance in non-typhi serotypes of Salmonella enterica. Clin. Infect. Dis. 2006;43:297–304. doi: 10.1086/505397. [DOI] [PubMed] [Google Scholar]
- 39.Park C.H., Robicsek A., Jacoby G.A., Sahm D., Hooper D.C. Prevalence in the United States of aac(6 ′ )-Ib-cr encoding a ciprofloxacin-modifying enzyme. Antimicrob. Agents Chemother. 2006;50:3953–3955. doi: 10.1128/AAC.00915-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cattoir V., Poirel L., Rotimi V., Soussy C.-J., Nordmann P. Multiplex PCR for detection of plasmid-mediated quinolone resistance qnr genes in ESBL-producing enterobacterial isolates. J. Antimicrob. Chemother. 2007;60:394–397. doi: 10.1093/jac/dkm204. [DOI] [PubMed] [Google Scholar]
- 41.Yamane K., Wachino J.-I., Suzuki S., Arakawa Y. Plasmid-mediated qepA gene among Escherichia coli clinical isolates from Japan. Antimicrob. Agents Chemother. 2008;52:1564–1566. doi: 10.1128/AAC.01137-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cavaco L.M., Hasman H., Xia S., Aarestrup F.M. qnrD, a novel gene conferring transferable quinolone resistance in Salmonella enterica serovar Kentucky and Bovismorbificans strains of human origin. Antimicrob. Agents Chemother. 2009;53:603–608. doi: 10.1128/AAC.00997-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Xavier B.B., Lammens C., Ruhal R., Kumar-Singh S., Butaye P., Goossens H., Malhotra-Kumar S. Identification of a novel plasmid-mediated colistin-resistance gene, mcr-2, in Escherichia coli, Belgium, June 2016. Eurosurveillance. 2016;21:30280. doi: 10.2807/1560-7917.ES.2016.21.27.30280. [DOI] [PubMed] [Google Scholar]
- 44.Rebelo A.R., Bortolaia V., Kjeldgaard J.S., Pedersen S.K., Leekitcharoenphon P., Hansen I.M., Guerra B., Malorny B., Borowiak M., Hammerl J.A., et al. Multiplex PCR for detection of plasmid-mediated colistin resistance determinants, mcr-1, mcr-2, mcr-3, mcr-4 and mcr-5 for surveillance purposes. Eurosurveillance. 2018;23:17-00672. doi: 10.2807/1560-7917.ES.2018.23.6.17-00672. Erratum in Eurosurveillance 2018, 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chapman T.A., Wu X.-Y., Barchia I., Bettelheim K.A., Driesen S., Trott D., Wilson M., Chin J.J.-C. Comparison of virulence gene profiles of Escherichia coli strains isolated from healthy and diarrheic Swine. Appl. Environ. Microbiol. 2006;72:4782–4795. doi: 10.1128/AEM.02885-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wu X.-Y., Chapman T., Trott D.J., Bettelheim K., Do T.N., Driesen S., Walker M.J., Chin J. Comparative analysis of virulence genes, genetic diversity, and phylogeny of commensal and Enterotoxigenic Escherichia coli isolates from weaned pigs. Appl. Environ. Microbiol. 2007;73:83–91. doi: 10.1128/AEM.00990-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Clermont O., Christenson J.K., Denamur E., Gordon D.M. The Clermont Escherichia coli phylo-typing method revisited: Improvement of specificity and detection of new phylo-groups. Environ. Microbiol. Rep. 2013;5:58–65. doi: 10.1111/1758-2229.12019. [DOI] [PubMed] [Google Scholar]
- 48.Tenover F.C., Arbeit R.D., Goering R.V., Mickelsen P.A., Murray B.E., Persing D.H., Swaminathan B. Interpreting chromosomal DNA restriction patterns produced by pulsed-field gel electrophoresis: Criteria for bacterial strain typing. J. Clin. Microbiol. 1995;33:2233–2239. doi: 10.1128/jcm.33.9.2233-2239.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Heras J., Domínguez C., Mata E., Pascual V., Lozano C., Torres C., Zarazaga M. GelJ—A tool for analyzing DNA fingerprint gel images. BMC Bioinform. 2015;16:270. doi: 10.1186/s12859-015-0703-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Li W.H. Simple method for constructing phylogenetic trees from distance matrices. Proc. Natl. Acad. Sci. USA. 1981;78:1085–1089. doi: 10.1073/pnas.78.2.1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tartof S.Y., Solberg O.D., Manges A.R., Riley L.W. Analysis of a uropathogenic Escherichia coli clonal group by Multilocus Sequence Typing. J. Clin. Microbiol. 2005;43:5860–5864. doi: 10.1128/JCM.43.12.5860-5864.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Maamar E., Hammami S., Alonso C.A., Dakhli N., Abbassi M.S., Ferjani S., Hamzaoui Z., Saidani M., Torres C., Boubaker I.B.-B. High prevalence of extended-spectrum and plasmidic AmpC β-lactamase-producing Escherichia coli from poultry in Tunisia. Int. J. Food Microbiol. 2016;231:69–75. doi: 10.1016/j.ijfoodmicro.2016.05.001. [DOI] [PubMed] [Google Scholar]
- 53.Saidani M., Messadi L., Mefteh J., Chaouechi A., Soudani A., Selmi R., Dâaloul-Jedidi M., Ben Chehida F., Mamlouk A., Jemli M.H., et al. Various Inc-type plasmids and lineages of Escherichia coli and Klebsiella pneumoniae spreading blaCTX-M-15, blaCTX-M-1 and mcr-1 genes in camels in Tunisia. J. Glob. Antimicrob. Resist. 2019;19:280–283. doi: 10.1016/j.jgar.2019.05.007. [DOI] [PubMed] [Google Scholar]
- 54.Apostolakos I., Feudi C., Eichhorn I., Palmieri N., Fasolato L., Schwarz S., Piccirillo A. High-resolution characterisation of ESBL/pAmpC-producing Escherichia coli isolated from the broiler production pyramid. Sci. Rep. 2020;10:11123. doi: 10.1038/s41598-020-68036-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Subramanya S.H., Bairy I., Nayak N., Amberpet R., Padukone S., Metok Y., Bhatta D.R., Sathian B. Detection and characterization of ESBL-producing Enterobacteriaceae from the gut of healthy chickens, Gallus gallus domesticus in rural Nepal: Dominance of CTX-M-15-non-ST131 Escherichia coli clones. PLoS ONE. 2020;15:e0227725. doi: 10.1371/journal.pone.0227725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Shoaib M., Kamboh A.A., Sajid A., Mughal G.A., Leghari R.A., Malhi K.K., Bughio S.U.D., Ali A., Alam S., Khan S., et al. Prevalence of extended spectrum beta-lactamase producing Enterobacteriaceae in commercial broilers and backyard chickens. Adv. Anim. Vet. Sci. 2016;4:209–214. doi: 10.14737/journal.aavs/2016/4.4.209.214. [DOI] [Google Scholar]
- 57.Lee Y.Q., Kamar A.A., Velayuthan R.D., Chong C.W., Teh C.S.J. Clonal relatedness in the acquisition of intestinal carriage and transmission of multidrug resistant (MDR) Klebsiella pneumoniae and Escherichia coli and its risk factors among preterm infants admitted to the neonatal intensive care unit (NICU) Pediatr. Neonatol. 2020;62:129–137. doi: 10.1016/j.pedneo.2020.10.002. [DOI] [PubMed] [Google Scholar]
- 58.Usui M., Iwasa T., Fukuda A., Sato T., Okubo T., Tamura Y. The Role of flies in spreading the extended-spectrum β-lactamase gene from cattle. Microb. Drug Resist. 2013;19:415–420. doi: 10.1089/mdr.2012.0251. [DOI] [PubMed] [Google Scholar]
- 59.Obeng-Nkrumah N., Labi A.-K., Blankson H., Awuah-Mensah G., Oduro-Mensah D., Anum J., Teye J., Kwashie S.D., Bako E., Ayeh-Kumi P.F., et al. Household cockroaches carry CTX-M-15-, OXA-48- and NDM-1-producing enterobacteria, and share β-lactam resistance determinants with humans. BMC Microbiol. 2019;19:272. doi: 10.1186/s12866-019-1629-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Punyadi P., Thongngen P., Kiddee A., Assawatheptawee K., Tansawai U., Bunchu N., Niumsup P.R. Prevalence of blaCTX-M and emergence of blaCTX-M-5-Carrying Escherichia coli in Chrysomya megacephala (Diptera: Calliphoridae), Northern Thailand. Microb. Drug Resist. 2020;27:698–705. doi: 10.1089/mdr.2020.0249. [DOI] [PubMed] [Google Scholar]
- 61.Hölzel C.S., Tetens J.L., Schwaiger K. Unraveling the role of vegetables in spreading antimicrobial-resistant bacteria: A need for quantitative risk assessment. Foodborne Pathog. Dis. 2018;15:671–688. doi: 10.1089/fpd.2018.2501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Song J., Oh S.-S., Kim J., Shin J. Extended-spectrum β-lactamase-producing Escherichia coli isolated from raw vegetables in South Korea. Sci. Rep. 2020;10:19721. doi: 10.1038/s41598-020-76890-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Abbassi M.S., Torres C., Achour W., Vinué L., Sáenz Y., Costa D., Bouchami O., Ben Hassen A. Genetic characterisation of CTX-M-15-producing Klebsiella pneumoniae and Escherichia coli strains isolated from stem cell transplant patients in Tunisia. Int. J. Antimicrob. Agents. 2008;32:308–314. doi: 10.1016/j.ijantimicag.2008.04.009. [DOI] [PubMed] [Google Scholar]
- 64.Ferjani S., Saidani M., Amine F.S., Boubaker I.B.-B. Prevalence and characterization of Plasmid-Mediated Quinolone Resistance genes in extended-spectrum β-lactamase-producing Enterobacteriaceae in a Tunisian Hospital. Microb. Drug Resist. 2015;21:158–166. doi: 10.1089/mdr.2014.0053. [DOI] [PubMed] [Google Scholar]
- 65.Tong P., Sun Y., Ji X., Du X., Guo X., Liu J., Zhu L., Zhou B., Zhou W., Liu G., et al. Characterization of antimicrobial resistance and extended-spectrum β-lactamase genes in Escherichia coli isolated from chickens. Foodborne Pathog. Dis. 2015;12:345–352. doi: 10.1089/fpd.2014.1857. [DOI] [PubMed] [Google Scholar]
- 66.Bert F., Branger C., Lambert-Zechovsky N. Identification of PSE and OXA β-lactamase genes in Pseudomonas aeruginosa using PCR-restriction fragment length polymorphism. J. Antimicrob. Chemother. 2002;50:11–18. doi: 10.1093/jac/dkf069. [DOI] [PubMed] [Google Scholar]
- 67.Mirsalehian A., Feizabadi M., Nakhjavani F.A., Jabalameli F., Goli H., Kalantari N. Detection of VEB-1, OXA-10 and PER-1 genotypes in extended-spectrum β-lactamase-producing Pseudomonas aeruginosa strains isolated from burn patients. Burns. 2010;36:70–74. doi: 10.1016/j.burns.2009.01.015. [DOI] [PubMed] [Google Scholar]
- 68.Yin X.-L., Hou T.-W., Xu S.-B., Ma C.-Q., Yao Z.-Y., Li W., Wei L. Detection of drug resistance–associated genes of multidrug-resistant Acinetobacter baumannii. Microb. Drug Resist. 2008;14:145–150. doi: 10.1089/mdr.2008.0799. [DOI] [PubMed] [Google Scholar]
- 69.Abd El-Baky R.M., Ibrahim R.A., Mohamed D.S., Ahmed E.F., Hashem Z.S. Prevalence of virulence genes and their association with antimicrobial resistance among pathogenic E. coli isolated from Egyptian patients with different clinical infections. Infect. Drug Resist. 2020;13:1221–1236. doi: 10.2147/IDR.S241073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Gelbíčová T., Baráková A., Florianová M., Jamborová I., Zelendová M., Pospíšilová L., Koláčková I., Karpíšková R. Dissemination and comparison of genetic determinants of mcr-mediated colistin resistance in Enterobacteriaceae via retailed raw meat products. Front. Microbiol. 2019;10:2824. doi: 10.3389/fmicb.2019.02824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Maamar E., Alonso C.A., Hamzaoui Z., Dakhli N., Abbassi M.S., Ferjani S., Saidani M., Boubaker I.B.-B., Torres C. Emergence of plasmid-mediated colistin-resistance in CMY-2-producing Escherichia coli of lineage ST2197 in a Tunisian poultry farm. Int. J. Food Microbiol. 2018;269:60–63. doi: 10.1016/j.ijfoodmicro.2018.01.017. [DOI] [PubMed] [Google Scholar]
- 72.Hassen B., Saloua B., Abbassi M.S., Ruiz-Ripa L., Mama O.M., Hassen A., Hammami S., Torres C. mcr-1 encoding colistin resistance in CTX-M-1/CTX-M-15- producing Escherichia coli isolates of bovine and caprine origins in Tunisia. First report of CTX-M-15-ST394/D E. coli from goats. Comp. Immunol. Microbiol. Infect. Dis. 2019;67:101366. doi: 10.1016/j.cimid.2019.101366. [DOI] [PubMed] [Google Scholar]
- 73.Haeili M., Salehzeinali H., Mirzaei S., Pishnian Z., Ahmadi A. Molecular characterization of quinolone resistance and antimicrobial resistance profiles of Klebsiella pneumoniae and Escherichia coli isolated from human and broiler chickens. Int. J. Environ. Health Res. 2021;32:1382–1392. doi: 10.1080/09603123.2021.1885632. [DOI] [PubMed] [Google Scholar]
- 74.Quiñones D., Aung M.S., Carmona Y., González M.K., Pereda N., Hidalgo M., Rivero M., Zayas A., del Campo R., Urushibara N., et al. High prevalence of CTX-M Type extended-spectrum β-lactamase genes and detection of NDM-1 carbapenemase gene in extraintestinal pathogenic Escherichia coli in Cuba. Pathogens. 2020;9:65. doi: 10.3390/pathogens9010065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kaushik M., Kumar S., Kapoor R.K., Virdi J.S., Gulati P. Integrons in Enterobacteriaceae: Diversity, distribution and epidemiology. Int. J. Antimicrob. Agents. 2018;51:167–176. doi: 10.1016/j.ijantimicag.2017.10.004. [DOI] [PubMed] [Google Scholar]
- 76.Riley L.W. Pandemic lineages of extraintestinal pathogenic Escherichia coli. Clin. Microbiol. Infect. 2014;20:380–390. doi: 10.1111/1469-0691.12646. [DOI] [PubMed] [Google Scholar]
- 77.Silva M.M., Sellera F.P., Fernandes M.R., Moura Q., Garino F., Azevedo S.S., Lincopan N. Genomic features of a highly virulent, ceftiofur-resistant, CTX-M-8-producing Escherichia coli ST224 causing fatal infection in a domestic cat. J. Glob. Antimicrob. Resist. 2018;15:252–253. doi: 10.1016/j.jgar.2018.10.023. [DOI] [PubMed] [Google Scholar]
- 78.Manges A.R., Geum H.M., Guo A., Edens T.J., Fibke C.D., Pitout J.D.D. Global extraintestinal pathogenic Escherichia coli (ExPEC) lineages. Clin. Microbiol. Rev. 2019;32:e00135-18. doi: 10.1128/CMR.00135-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kapmaz M., Erdem F., Abulaila A., Yeniaras E., Oncul O., Aktas Z. First detection of NDM-1 with CTX-M-9, TEM, SHV and rmtC in Escherichia coli ST471 carrying IncI2, A/C and Y plasmids from clinical isolates in Turkey. J. Glob. Antimicrob. Resist. 2016;7:152–153. doi: 10.1016/j.jgar.2016.10.001. [DOI] [PubMed] [Google Scholar]
- 80.Rada A.M., Correa A., Restrepo E., Capataz C. Escherichia coli ST471 Producing VIM-4 metallo-β-lactamase in Colombia. Microb. Drug Resist. 2022;28:288–292. doi: 10.1089/mdr.2021.0031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Tivendale K.A., Logue C.M., Kariyawasam S., Jordan D., Hussein A., Li G., Wannemuehler Y., Nolan L.K. Avian-pathogenic Escherichia coli strains are similar to neonatal meningitis E. coli strains and are able to cause meningitis in the rat model of human disease. Infect. Immun. 2010;78:3412–3419. doi: 10.1128/IAI.00347-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Kubelová M., Koláčková I., Gelbíčová T., Florianová M., Kalová A., Karpíšková R. Virulence properties of mcr-1-positive Escherichia coli isolated from retail poultry meat. Microorganisms. 2021;9:308. doi: 10.3390/microorganisms9020308. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated and analyzed during our study are included in this article.