Abstract
Purpose: To compare the effects of whole-body vibration training (WBVT) with different frequencies on the balance ability of older adults.
Methods: Randomized controlled trials (RCTs) on the WBVT interventions on balance ability in older adults were searched through PubMed, Web of Science, The Cochrane Library, ProQuest, Embase, Opengrey, China National Knowledge Infrastructure (CNKI), Wanfang, and China Science and Technology Journal Database (CSTJ) databases from the establishment of the database to August 2022, and all literature that met the PICOS (Participants, Intervention, Comparison, Outcomes, Study design) criteria were enrolled. Two reviewers screened and assessed the methodological quality of the included literature according to the physiotherapy evidence database (PEDro) scale criteria. Statistical analysis was performed using Stata 14.0 software after data extraction.
Results: Twenty-five RCTs with a total of 1267 subjects were finally included. The results of the pairwise comparison of the Network Meta-analysis showed that the Timed Up and Go Test (TUGT) values of Low-frequency whole-body vibration training (LF-WBVT) was lower than the placebo and traditional rehabilitation groups, and the difference was statistically significant [WMD = −1.37, 95% CI (−2.53, −0.20)] [WMD = −1.84, 95% CI(-3.17,-0.51)]. The Five-repetition Sit-to-Stand Test (5STS) values of LF-WBVT, Medium-frequency whole-body vibration training (MF-WBVT), and High-frequency whole-body vibration training (HF-WBVT) were lower than the placebo and traditional rehabilitation groups, but none of them were statistically significant. In addition, the TUGT and 5STS values of HF-WBVT had a tendency to be lower than those of LF-WBVT and MF-WBVT, but neither of them was statistically different. The cumulative probability ranking results of both TUGT and 5STS showed that HF-WBVT was the best protocol.
Conclusion: Current evidence shows that HF-WBVT may be the best protocol for improving balance in older adults. Due to the study’s limitations, the conclusion obtained in this study still needs to be further confirmed by more high-quality studies.
Systematic Review Registration: [https://www.crd.york.ac.uk/PROSPERO/], identifier [CRD42021250405].
Keywords: whole body vibration, frequency, older adults, balance, meta-analysis
1 Introduction
Falls are one of the leading causes of disability, injury, and death in older adults and are a significant public health problem worldwide (Montero-Odasso, et al., 2022). Studies have shown that at least 30% of people over 65 experience falls yearly, and this percentage increases to 50% for those over 80 (Montero-Odasso, et al., 2021). Falls can have serious consequences, such as pain, reduced function, limited self-care, and even fractures (Gates, et al., 2008; Gillespie, et al., 2012; Burns, et al., 2016). In addition, falls can lead to severe psychological impairment, fear, and loss of confidence, resulting in reduced physical activity and social interaction in older adults, further reducing mobility and increasing the risk of recurrent falls (Sherrington, et al., 2019). In the elderly, reduced balance and postural control with increasing age have been identified as significant risk factors for falls (Lord, et al., 1992; Ganz and Latham, 2020). Early development of appropriate exercise intervention programs for older adults can reduce the risk of falls (Morley, et al., 2013).
Traditional resistance exercises and balance training can effectively improve physical fitness and reduce the chances of falls in older adults (von Stengel, et al., 2012). However, to obtain significant improvements in balance and other physical functions, the total dose of exercise must be of considerable intensity and sufficiently long duration (Sherrington, et al., 2020). Thus, older adults sometimes feel very fatigued and thus need more motivation (Burton, et al., 2017). In addition, other age-related limitations, such as cardiac limitations, muscle strength limitations, or lack of relevant training conditions, such as space and time, will reduce the feasibility of the training program (Goudarzian, et al., 2017).
Whole-body vibration training (WBVT) generates vibrations through a vibrating platform that produces shock stimuli to body muscle groups, which can increase active muscle activity, improve the biological activity of high threshold motor units and increase neuromuscular excitability (Bernardo-Filho, et al., 2018; Wuestefeld, et al., 2020; van Heuvelen, et al., 2021). It has been demonstrated that WBVT can improve balance and enhance body control in older adults, thereby reducing the incidence of falls (Jepsen, et al., 2017), and compared with traditional training, WBVT reduces stress on the musculoskeletal, cardiovascular, and respiratory systems (Bogaerts, et al., 2009), making it safer and more acceptable for older adults with relatively mild side effects (Kawanabe, et al., 2007; Gomes-Neto, et al., 2019; Tseng, et al., 2021; Liu, et al., 2022). Relevant Meta-analyses have been published and confirmed the method’s effectiveness (Rogan, et al., 2011; Lam, et al., 2012; Orr, 2015; Rogan, et al., 2017). Frequency, a key parameter of WBVT, is necessary for successful fall risk reduction and can determine its effectiveness of WBVT and outcome (Sherrington, et al., 2008; Dutra, et al., 2016; van Heuvelen, et al., 2021). However, current evidence has been obtained by comparing each experimental group with the control group at the same vibration frequency, and valid comparisons between different frequencies still need to be made. Therefore, this study will use a Network Meta-analysis to compare the effects of WBVT with different vibration frequencies on the balance ability of older adults to provide practical, evidence-based clinical support.
2 Materials and methods
The systematic review was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines (Page, et al., 2021). This study has been registered with the International Prospective Registry of Systematic Evaluations (PROSPERO) under the registration number CRD42021250405.
2.1 Eligibility criteria
2.1.1 Inclusion criteria
The inclusion criteria were set based on participants, intervention, comparison, outcomes, and study design (PICOS) strategy. Participants (P): Healthy older adults without chronic diseases, neuromusculoskeletal systems, and joint injuries who had not undergone high-intensity physical training 6 months before the trial. Intervention (I): Received one of the interventions which included LF-WBVT (<30 Hz), MF-WBVT (≥30Hz, <45 Hz), and HF-WBVT (>45 Hz) (Yeung and Yeung, 2015; Wei, et al., 2017; Sajadi, et al., 2019). Comparison (C): The placebo comparison included no intervention and sham intervention, of which the latter referred to the analog vibration without any effective vibration stimulation. Traditional rehabilitation, such as strength training, physical therapy, and usual care, was acceptable as cointervention. Outcomes (O): Primary outcome measures in this study assessed the balance ability, including the Timed Up and Go Test (TUGT) and the Five-repetition Sit-to-Stand Test (5STS). TUGT and 5STS are clinically used to measure balance ability (Podsiadlo and Richardson, 1991; Whitney, et al., 2005; Hwang, et al., 2018; Phu, et al., 2019). Study design (S): Randomized controlled trials (RCTs).
2.1.2 Exclusion criteria
The exclusion criteria adopted in the present study are as follows: 1) reviews, abstracts, and conference reports; 2) lack of outcome measures; 3) multiple publications of the literature; 4) unavailability of full text; 5) concurrent medication therapy during the intervention.
2.2 Operational definitions
WBVT was defined as an exercise intervention, consisting of the application of an oscillation platform that transmits mechanical stimuli to the human body standing on it (de Oliveira, et al., 2023).
2.3 Databases and search strategies
A systematic search was conducted through PubMed, Web of Science, The Cochrane Library, ProQuest, Embase, Opengrey, CNKI, Wanfang, and CSTJ databases on randomized controlled trials of WBVT interventions on balance ability in older adults, and the search time was controlled from the establishment of the database to August 2022.
The search terms include balance, fall, old people, vibration, and whole-body vibration training. The specific search formula (PubMed was used as an example): (balance OR fall OR equilibrium) AND (older adults OR older people OR aging OR elder OR old) AND (vibration OR whole-body vibration training OR WBVT). A second search was conducted for the list of references and citations included in the study to identify other possible relevant studies.
The PICOS strategy (Costantino, et al., 2015) was used to structure the bibliographic search: Participants (P) = older adults; Intervention (I) = WBVT; Comparison (C) = placebo or traditional rehabilitation; O (outcome) = TUGT; 5STS. Study design (S): RCTs.
2.4 Study selection and data extraction
Two reviewers screened the entire retrieved literature. The EndnoteX9 software was used in the first step to delete duplicate data. The titles and abstracts were read according to the previously set inclusion criteria, leaving those that met the requirements. The full text was read later to determine the final inclusion. For any disagreement, the studies will be re-evaluated. If the disagreement cannot be resolved, a group discussion will be held to resolve it.
In the second step, Information related to the included studies was extracted and collected into an Excel sheet. The extracted Information included: the first author’s name, country of publication, year of publication, sample size (experimental and control groups), age, interventions (experimental and control groups), outcome indicators, frequency of intervention, and duration of intervention.
2.5 Methodological quality and risk of bias
Two reviewers evaluated the methodological quality of the included studies according to the criteria of the Physiotherapy Evidence Database (PEDro) scale (Cashin and McAuley, 2020). It consists of 11 items with a total score of 10 (the final score does not include the “inclusion criteria” items). A PEDro score of ≥6 indicates a high methodological quality for an included study. The Cochrane Collaboration’s tool was used to assess the risk of bias of the included studies (Higgins, et al., 2011). The main areas of assessment are randomization, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, completeness of data regarding outcomes, selective reporting, and other bias. When the evaluation was completed, the two reviewers exchanged and compared the results of both evaluations. The study team will decide through a group discussion if there is any disagreement.
2.6 Statistical analysis
2.6.1 Network meta-analysis
Network Meta-analysis and graphical plotting were performed for relevant data using Stata 16.0 software. Since the outcome indicators in this study were all continuous variables and were evaluated by the same scale, the weighted mean difference (WMD) and 95% confidence interval (CI) were used as effect sizes. Network evidence plots for direct comparisons among interventions were first drawn; then, the consistency of the closed loop of each outcome indicator was evaluated by the ring inconsistency test, and when the 95% CI of the ring inconsistency factor (IF) contained 0, it indicated a good agreement between direct and indirect evidence. The results of the Network Meta-analysis were presented by pairwise comparison of forest plots. Cumulative ranking probability plots were drawn based on the surface under the cumulative ranking curve (SUCRA) to determine the optimal training frequency.
2.6.2 Publication bias
We evaluated the publication bias of these studies and minor sample effects by visually measuring the symmetry of funnel plots in Stata16.0 software.
3 Results
3.1 Search results
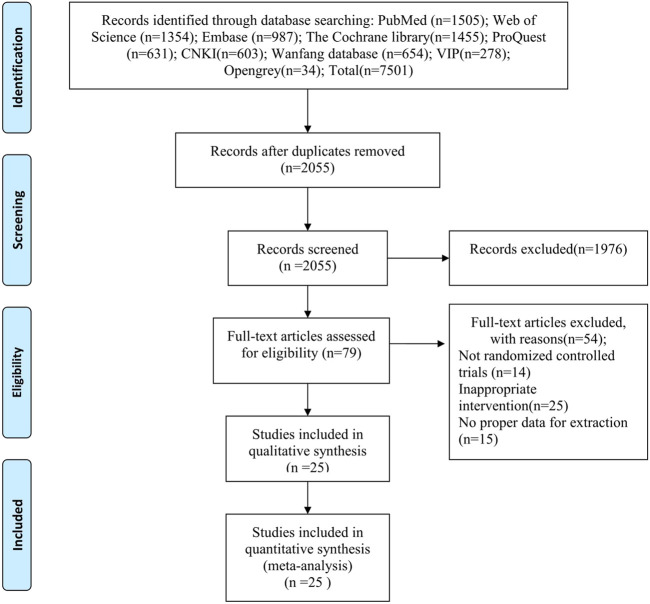
A total of 7501 studies was retrieved, and 25 was finally included after multiple screenings (Bautmans, et al., 2005; Bruyere, et al., 2005; Rees, et al., 2007; Furness and Maschette, 2009; Furness, et al., 2010; Marín, et al., 2011; Pollock, et al., 2012; Calder, et al., 2013; Buckinx, et al., 2014; Zhang, et al., 2014; Álvarez-Barbosa, et al., 2014; Corrie, et al., 2015; Ochi, et al., 2015; Santin-Medeiros, et al., 2015; Sitjà-Rabert, et al., 2015; Sucuoglu, et al., 2015; Lei, et al., 2016; Goudarzian, et al., 2017; Wei, et al., 2017; Lam, et al., 2018; Jingwang, et al., 2019; Zhu, et al., 2019; Sen, et al., 2020; Wadsworth and Lark, 2020; Xiao-feng, 2020). A flowchart of the study selection process is shown in Figure 1. The basic characteristics of included studies are shown in Table 1.
FIGURE 1.
Flowchart of the study selection process.
TABLE 1.
The basic characteristics of included studies.
| Study (author/year) | Country | Sample size (EG/CG) | Age (years old) | Interventions (EG/CG) | WBVT frequency (Hz) | WBVT amplitude (mm) | Duration of intervention (weeks) | Main outcomes |
|---|---|---|---|---|---|---|---|---|
| Álvarez-Barbosa, et al. (2014) | Spain | 22 (11/11) | 84.0 ± 3.0 | MF-WBVT/Traditional rehabilitation | 30–35 | 4 | 8 | ①② |
| Bautmans, et al. (2005) | Belgium | 21 (10/11) | 77.5 ± 11.0 | MF-WBVT/Traditional rehabilitation | 30–40 | 2–5 | 6 | ① |
| Bruyere, et al. (2005) | Belgium | 36 (16/20) | 81.9 ± 6.9 | LF-WBVT/Traditional rehabilitation | 10, 26 | 3, 7 | 6 | ① |
| Buckinx, et al. (2014) | Belgium | 62 (31/31) | 83.2 ± 7.9 | MF-WBVT/Placebo | 30 | 2 | 24 | ① |
| Calder, et al. (2013) | New Zealand | 38 (19/19) | 80.1 | LF-WBVT/Traditional rehabilitation | 20 | 2 | 6 | ①② |
| Corrie, et al. (2015) | United Kingdom | 61 (21/20) | 80.2 ± 6.5 | LF-WBVT/Traditional rehabilitation | 28.4, 29.8 | 1.3, 2.9 | 12 | ①② |
| Furness and Maschette (2009) | Australia | 37 (19/18) | 72.0 ± 8.0 | LF-WBVT/Placebo | 15–25 | 0.05 | 6 | ①② |
| Furness, et al. (2010) | Australia | 37 (19/18) | 69.0 ± 8.0 | LF-WBVT/Placebo | 15–25 | 1 | 12 | ①② |
| Goudarzian, et al. (2017) | Iran | 20 (11/9) | 68.0 ± 5.8 | MF-WBVT/Placebo | 30–35 | 5–8 | 8 | ①② |
| Lam, et al. (2018) | China | 62 (21/19/22) | 82.3 ± 7.3 | MF-WBVT/Traditional rehabilitation/Placebo | 30–40 | 0.9 | 8 | ①② |
| Marín, et al. (2011) | Spain | 60 (11/11) | 84.3 ± 7.4 | MF-WBVT/Placebo | 30–40 | 1.05–2.11 | 8 | ② |
| Ochi, et al. (2015) | Japan | 20 (10/10) | 80.9 ± 2.8 | LF-WBVT/Traditional rehabilitation | 10–21 | 3–7 | 12 | ① |
| Pollock, et al. (2012) | United Kingdom | 77 (38/39) | 80.0 ± 1.4 | LF-WBVT/Traditional rehabilitation | 15–30 | 2–8 | 8 | ① |
| Rees, et al. (2007) | Australia | 28 (15/13) | 74.3 ± 5.0 | LF-WBVT/Traditional rehabilitation | 26 | 5–8 | 32 | ①② |
| Santin-Medeiros, et al. (2015) | Spain | 27 (19/18) | 82.4 ± 5.7 | LF-WBVT/Placebo | 20 | 2 | 32 | ①② |
| Sen, et al. (2020) | Turkey | 33 (15/16/18) | 55.0 ± 4.6 | MF-WBVT/Traditional rehabilitation/Placebo | 30–40 | 2–4 | 12 | ① |
| Sitjà-Rabert, et al. (2015) | Spain | 159 (81/78) | 82.0 | MF-WBVT/Traditional rehabilitation | 30–35 | 2–4 | 6 | ①② |
| Sucuoglu, et al. (2015) | Turkey | 42 (21/21) | 58.76 ± 5.82 | WBVT/Traditional rehabilitation | 30–35 | 4 | ① | |
| Wadsworth and Lark (2020) | New Zealand | 55 (27/30/28) | 82.45 ± 7.9 | LF-WBVT/Traditional rehabilitation/Placebo | 6–26 | 2–4 | 16 | ① |
| Wei, et al. (2017) | China | 120 (20/20/20/20) | 78.0 ± 4.0 | HF-WBVT/MF-WBVT/LF-WBVT/Placebo | 60,40,20 | 4 | 12 | ①② |
| Zhang, et al. (2014) | China | 37 (19/18) | 85.27 ± 3.63 | LF-WBVT/Traditional rehabilitation | 6–26 | 1–3 | 8 | ①② |
| Zhu, et al. (2019) | China | 55 (28/27) | 87.5 ± 3.0 | LF-WBVT/Placebo | 12–16 | 3–5 | 8 | ①② |
| Xiao-feng (2020) | China | 80 (40/40) | 64.75 ± 2.45 | HF-WBVT/MF-WBVT | 30, 45 | 2 | 12 | ①② |
| Lei, et al. (2016) | China | 42 (22/20) | 72.73 ± 1.46 | MF-WBVT/Traditional rehabilitation | 35–45 | 5 | 8 | ① |
| Jingwang, et al. (2019) | China | 36 (20/16) | 84.6 ± 5.7 | LF-WBVT/Traditional rehabilitation | 3–13 | 3 | 12 | ①② |
Note: LF-WBVT, Low-frequency whole-body vibration training; MF-WBVT, Medium frequency whole-body vibration training; HF-WBVT, High-frequency whole-body vibration training; ① = Timed Up and Go Test (TUGT); ② = Five-repetition Sit-to-Stand Test (5STS).
3.2 Quality evaluation
Table 2 shows the results of the methodological quality evaluation of the included studies. The scores of the included studies ranged from 5 to 8, with 18 having a PEDro score of 6 or more. All studies described inclusion criteria and underwent random assignment, and 5 studies underwent allocation concealment; all studies were comparable at baseline; 3 studies were blinded to subjects, no studies were blinded to therapists, and 13 studies were blinded to assessors; all studies had a clinical sample dropout rate of less than 15%; 16 studies used intentional analysis; all included studies underwent between-group statistics, point measures, and difference value statistics.
TABLE 2.
Physiotherapy evidence database (PEDro) scores of the included studies.
| Study | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | PEDro score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Álvarez-Barbosa, et al. (2014) | ● | ● | ○ | ● | ○ | ○ | ○ | ● | ● | ● | ● | 6 |
| Bautmans, et al. (2005) | ● | ● | ● | ● | ○ | ○ | ● | ● | ● | ● | ● | 8 |
| Bruyere, et al. (2005) | ● | ● | ○ | ● | ○ | ○ | ○ | ● | ● | ● | ● | 6 |
| Buckinx, et al. (2014) | ● | ● | ○ | ● | ○ | ○ | ● | ● | ● | ● | ● | 7 |
| Calder, et al. (2013) | ● | ● | ○ | ● | ○ | ○ | ● | ● | ○ | ● | ● | 6 |
| Corrie, et al. (2015) | ● | ● | ○ | ● | ● | ○ | ● | ● | ○ | ● | ● | 7 |
| Furness and Maschette (2009) | ● | ● | ○ | ● | ○ | ○ | ○ | ● | ○ | ● | ● | 5 |
| Furness, et al. (2010) | ● | ● | ○ | ● | ○ | ○ | ○ | ● | ○ | ● | ● | 5 |
| Goudarzian, et al. (2017) | ● | ● | ○ | ● | ○ | ○ | ○ | ● | ○ | ● | ● | 5 |
| Lam, et al. (2018) | ● | ● | ● | ● | ● | ○ | ● | ● | ● | ● | ● | 9 |
| Marín, et al. (2011) | ● | ● | ○ | ● | ○ | ○ | ○ | ● | ○ | ● | ● | 5 |
| Ochi, et al. (2015) | ● | ● | ● | ● | ○ | ○ | ● | ● | ● | ● | ● | 8 |
| Pollock, et al. (2012) | ● | ● | ● | ● | ● | ○ | ● | ● | ● | ● | ● | 9 |
| Rees, et al. (2007) | ● | ● | ○ | ● | ○ | ○ | ○ | ● | ○ | ● | ● | 5 |
| Santin-Medeiros, et al. (2015) | ● | ● | ○ | ● | ○ | ○ | ○ | ● | ● | ● | ● | 6 |
| Sen, et al. (2020) | ● | ● | ○ | ● | ○ | ○ | ○ | ● | ● | ● | ● | 6 |
| Sitjà-Rabert, et al. (2015) | ● | ● | ● | ● | ○ | ○ | ● | ● | ● | ● | ● | 8 |
| Sucuoglu, et al. (2015) | ● | ● | ○ | ● | ○ | ○ | ● | ● | ○ | ● | ● | 6 |
| Wadsworth and Lark (2020) | ● | ● | ○ | ● | ○ | ○ | ○ | ● | ● | ● | ● | 6 |
| Wei, et al. (2017) | ● | ● | ○ | ● | ○ | ○ | ● | ● | ● | ● | ● | 7 |
| Zhang, et al. (2014) | ● | ● | ○ | ● | ○ | ○ | ● | ● | ● | ● | ● | 7 |
| Zhu, et al. (2019) | ● | ● | ○ | ● | ○ | ○ | ○ | ● | ● | ● | ● | 6 |
| Xiao-feng (2020) | ● | ● | ○ | ● | ○ | ○ | ○ | ● | ○ | ● | ● | 5 |
| Lei, et al. (2016) | ● | ● | ○ | ● | ○ | ○ | ● | ● | ● | ● | ● | 7 |
| Jingwang, et al. (2019) | ● | ● | ○ | ● | ○ | ○ | ● | ● | ● | ● | ● | 7 |
Note: 1 = Eligibility criteria; 2 = Randomized Allocation; 3 = Blinded Allocation; 4 = Group homogeneity; 5 = Blinded subjects; 6 = Blinded therapists; 7 = Blinded assessor; 8 = Drop out <15%; 9 = Intention to treat analysis; 10 = Between group comparison; 11 = Point estimates and variability. ● adds a point to the score, ○ adds no point to the score. The item “eligibility criteria” is not included in the final score.
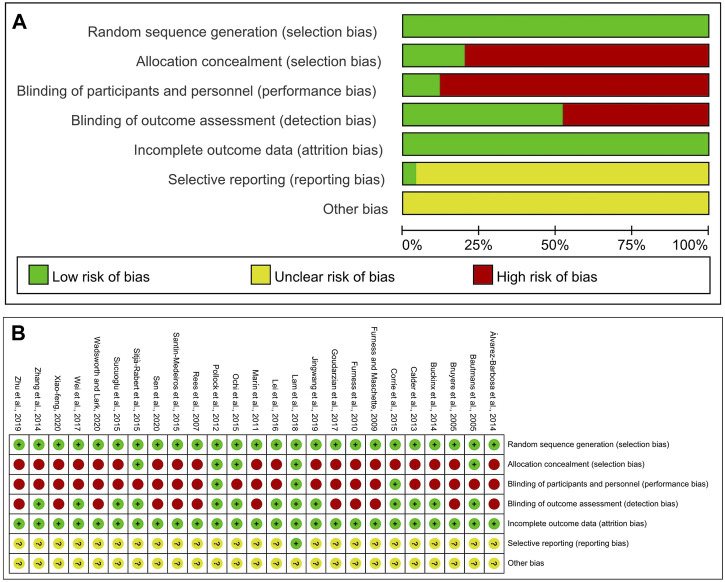
Figure 2 shows the results of the risk of bias in included studies. All studies reported the specific random mode, and 5 studies revealed the detailed allocation concealment; 3 studies were blinded to participants and personnel; 13 studies were blinded to assessors. Regarding the completeness of data regarding outcomes, all studies were rated as having a low risk of bias. Only 1 study showed a small probability of selection bias, and the remaining studies had an unclear risk of bias because they did not provide sufficient information to rule out bias.
FIGURE 2.
Rias of bias assessment results. (A) Risk of bias graph; (B) Risk of bias summary.
3.3 Network meta-analysis
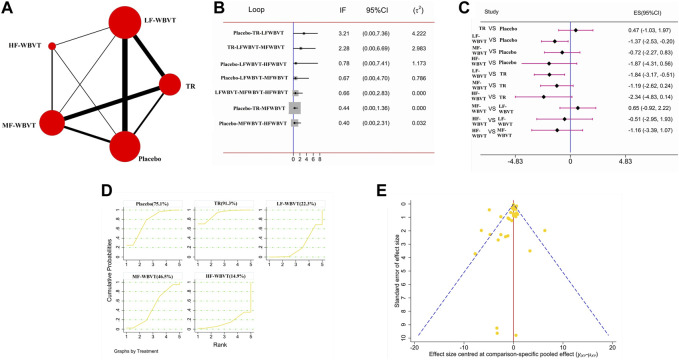
3.3.1 TUGT
A total of 24 studies and 1207 subjects was included. The network evidence diagram is shown in Figure 3A. The results of the loop inconsistency test manifested that the 95% CI of the loop inconsistency factor (IF) contained 0, indicating good consistency (Figure 3B). The forest plot of pairwise comparison (Figure 3C) showed that the TUGT values were lower in LF-WBVT [WMD = −1.37,95% CI (−2.53,−0.20)] [WMD = −1.84,95% CI (−3.17,−0.51)] compared to the placebo and traditional rehabilitation groups, with statistically significant differences; MF-WBVT and HF WBVT had lower TUGT values than the placebo and traditional rehabilitation groups, but the differences were not statistically significant. In addition, TUGT values were lower in HF-WBVT compared to LF-WBVT and MF-WBVT, but the difference was not statistically significant. The cumulative probability ranking results (Figure 3D) showed a SUCRA value of 14.9% for HF-WBVT, indicating that HF-WBVT may be the best option.
FIGURE 3.
Network meta-analysis results for TUGT. (A) Network evidence diagram; (B) loop inconsistency test; (C) Forest plot; (D) The figure of Cumulative probability ranking; (E) funnel plot.
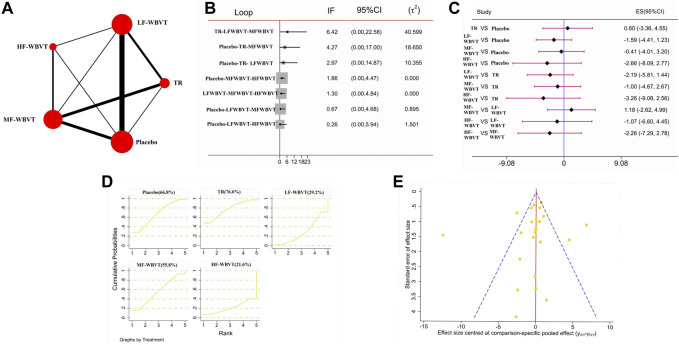
3.3.2 5STS
A total of 16 studies and 879 subjects was included. The network evidence diagram is shown in Figure 4A. The results of the loop inconsistency test manifested that the 95% CI of the loop inconsistency factor (IF) contained 0, indicating good consistency (Figure 4B). The forest plot of pairwise comparison (Figure 4C) showed that the 5STS values were lower for LF-WBVT, MF-WBVT, and HF-WBVT compared to the placebo and traditional rehabilitation groups, but none of them were statistically significant. In addition, the 5STS values were lower in HF-WBVT compared to LF-WBVT and MF-WBVT, but the difference was not statistically significant. The cumulative probability ranking results (Figure 4D) showed a SUCRA value of 21.6% for HF-WBVT, indicating that HF-WBVT may be the best option.
FIGURE 4.
Network meta-analysis results for 5STS. (A) Network evidence diagram; (B) loop inconsistency test; (C) Forest plot; (D) The figure of Cumulative probability ranking; (E) funnel plot.
3.4 Publication bias
As seen in Figure 3E and Figure 4E, the funnel plot of the two indicators was symmetrical, and most of the points were in the upper part of the funnel. Although some of the few points fell outside the funnel plot, the overall results indicate that publication bias was less likely in this study, but the results need to be interpreted with caution.
4 Discussion
To the best of our knowledge, this is the first Network Meta-analysis study exploring the effect of different frequencies of WBVT on balance ability in older adults. The results showed that the SUCRA values of HF-WBVT were 14.9% and 21.6% in TUGT and 5STS, respectively, suggesting that HF-WBVT was the best WBVT protocol.
Previous studies have shown that TUGT and 5STS have good reliability and validity in assessing balance (Goldberg, et al., 2012; Paineiras-Domingos, et al., 2018; Phu, et al., 2019; Nawrat-Szołtysik, et al., 2022). In the present study, the effect of WBVT on balance in older adults was assessed by TUGT and 5STS. The pairwise comparison results showed that the overall majority of the frequency groups had no statistically significant TUGT and 5STS values compared to the placebo and traditional rehabilitation groups but had a tendency to decrease. This improvement may be related to the WBVT-induced tonic vibratory reflex. The vibratory waves induced by the vibration platform stimulate proprioceptors, increase the excitability of afferent fibers, activate α motor neurons, and cause reflex muscle contractions, thus improving neuromuscular performance and balance in older adults (Rogan, et al., 2017; Bemben, et al., 2018). In addition, during WBVT application, the active and synergistic muscles produce muscular contractions, causing changes in the length of the muscle shuttle and activating the tendon apparatus, resulting in a timely relaxation of the antagonist’s muscles, thus increasing the efficiency of muscle contraction, improving the coordination of muscle activity and making it more precise (Ritzmann, et al., 2018). These neural adaptations play a crucial role in the balance and movement of the body.
In addition, the pairwise comparison of each frequency group showed that the TUGT and 5STS values of HF-WBVT tended to be lower than those of MF-WBVT and HF-WBVT. The cumulative probability ranking results also showed that HF-WBVT had the smallest SUCRA values in TUGT and 5STS, suggesting that HF-WBVT may be the best protocol. One possible reason is that neuromuscular tissues resonate under high-frequency vibration stimulation. Vibration frequency is defined in Hertz (Hz) and indicates the number of cycles per second (Rauch, et al., 2010; van Heuvelen, et al., 2021). Within a specific range, the higher the vibration frequency, the faster the intramuscular fiber length of the muscle spindle changes, and the frequency and intensity of nerve-issued impulses increase, triggering a more intense tonic vibration reflex and recruiting more motor units to participate in movement, which increases the level of neuromuscular activation and ultimately leads to improved balance. A previous study has reported that the electromyography (EMG) responses of subjects observed by EMG at different frequencies of WBVT were found to be more active at HF-WBVT, indicating that HF-WBVT triggered more intense muscle activity (Hazell, et al., 2007). Furthermore, HF-WBVT may increase the gravitational loading exerted on the neuromuscular system, thereby improving neuromuscular performance. It has been suggested that WBVT activates muscles through vibration to promote strength and motor performance, a mechanism similar to the neuromuscular effects achieved by traditional resistance training (Delecluse, et al., 2003; Roelants, et al., 2004; Bogaerts, et al., 2007), an exercise method that uses external resistance (such as dumbbells, barbells, elastic bands, etc.) to enhance muscle strength and physical fitness (Zuo, et al., 2022). A previous animal experimental study applied several frequencies and found that the higher the frequency, the better the effect of muscle strength improvement (Lin, et al., 2015). Similarly, the stronger effects of higher frequencies are in agreement with the results findings of reviews of chronic obstructive pulmonary disease (COPD) patients and Parkinson’s disease (PD) patients and can be explained by enhanced neuromuscular activity (Ritzmann, et al., 2018; Berner, et al., 2020; Laurisa, et al., 2022).
It is worth mentioning that, due to the delivery of vibration stimuli from the lower extremities from bottom to top, the damping of the vibration waves through the joints, muscles, and soft tissues leads to a certain degree of attenuation of the stimuli (Luo, et al., 2005; Oroszi, et al., 2020). Lower frequencies may not transmit the vibration stimuli effectively, while higher frequencies will more frequently and better enable the transmission of vibration stimuli and influence the neuromuscular response. Lower (less than 20 Hz) vibration frequencies may not be effective because organs in the body vibrate at similar frequencies (Dincher, et al., 2021). In addition, no adverse effects were reported in any of the studies. However, vibration stimulation of too long a duration may have adverse effects (Cardinale and Wakeling, 2005). Some studies reported that prolonged exposure to HF-WBVT shifts the nerve impulses released by Ia from enhancement to inhibition and predisposes the central nervous system (CNS) to fatigue and protective inhibition (Bongiovanni, et al., 1990; Da Silva-Grigoletto, et al., 2011; Lu, et al., 2021). Therefore, the intervention duration of HF-WBVT still needs further study.
4.1 Strengths
The strengths of this study include that the evidence was obtained from RCTs, followed the PRISMA guidelines of reporting, and registered at PROSPERO to improve transparency. The most effective application frequency of WBVT to improve the balance ability of healthy older adults was determined through Network meta-analysis, providing a valuable reference for clinical application.
4.2 Study limitations
This study also had certain limitations, 1) the methodological quality and intervention duration of the included studies were not entirely consistent, which may bring potential heterogeneity; 2) only Chinese and English studies were included, which may have language bias; 3) the studies related to HF-WBVT was less included, which may affect the validity of the test and weaken the demonstration to a certain extent.
5 Conclusion
In conclusion, HF-WBVT may be the best protocol to improve balance in older adults. Due to the study’s limitations, the conclusions obtained in this study still need to be further confirmed by more high-quality, standardized, and extensive sample-size studies.
Acknowledgments
Thanks to all authors for their contributions.
Funding Statement
This study was supported by the East Lake Scholars Sponsorship Program of Wuhan Sports University in China (2017), Science and Technology Team Foundation of Wuhan Sports University (21KT02), the 14th Five-Year-Plan Advantageous and Characteristic Disciplines (Groups) of Colleges and Universities in Hubei Province [(2021)05].
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
PL and YL drafted the manuscript. All authors participated in article search, study selection, data extraction, and review on the risk of bias. What is more, all authors provided final approval.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- Álvarez-Barbosa F., del Pozo-Cruz J., del Pozo-Cruz B., Alfonso-Rosa R. M., Rogers M. E., Zhang Y. (2014). Effects of supervised whole body vibration exercise on fall risk factors, functional dependence and health-related quality of life in nursing home residents aged 80+. Maturitas 79 (4), 456–463. 10.1016/j.maturitas.2014.09.010 [DOI] [PubMed] [Google Scholar]
- Bautmans I., Van Hees E., Lemper J. C., Mets T. (2005). The feasibility of whole body vibration in institutionalised elderly persons and its influence on muscle performance, balance and mobility: A randomised controlled trial [ISRCTN62535013]. BMC Geriatr. 5, 17. 10.1186/1471-2318-5-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bemben D., Stark C., Taiar R., Bernardo-Filho M. (2018). Relevance of whole-body vibration exercises on muscle strength/power and bone of elderly individuals. Dose Response 16 (4), 1559325818813066. 10.1177/1559325818813066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernardo-Filho M., Taiar R., Sañudo B., Furness T. (2018). Clinical approaches of whole body vibration exercises. Rehabil. Res. Pract. 2018, 9123625. 10.1155/2018/9123625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berner K., Albertyn S., Dawnarain S., Hendricks L. J., Johnson J., Landman A., et al. (2020). The effectiveness of combined lower limb strengthening and whole-body vibration, compared to strengthening alone, for improving patient-centred outcomes in adults with COPD: A systematic review. S Afr. J. Physiother. 76 (1), 1412. 10.4102/sajp.v76i1.1412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogaerts A., Delecluse C., Claessens A. L., Coudyzer W., Boonen S., Verschueren S. M. (2007). Impact of whole-body vibration training versus fitness training on muscle strength and muscle mass in older men: A 1-year randomized controlled trial. J. Gerontol. A Biol. Sci. Med. Sci. 62 (6), 630–635. 10.1093/gerona/62.6.630 [DOI] [PubMed] [Google Scholar]
- Bogaerts A. C., Delecluse C., Claessens A. L., Troosters T., Boonen S., Verschueren S. M. (2009). Effects of whole body vibration training on cardiorespiratory fitness and muscle strength in older individuals (a 1-year randomised controlled trial). Age Ageing 38 (4), 448–454. 10.1093/ageing/afp067 [DOI] [PubMed] [Google Scholar]
- Bongiovanni L. G., Hagbarth K. E., Stjernberg L. (1990). Prolonged muscle vibration reducing motor output in maximal voluntary contractions in man. J. Physiol. 423, 15–26. 10.1113/jphysiol.1990.sp018008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruyere O., Wuidart M. A., Di Palma E., Gourlay M., Ethgen O., Richy F., et al. (2005). Controlled whole body vibration to decrease fall risk and improve health-related quality of life of nursing home residents. Arch. Phys. Med. Rehabil. 86 (2), 303–307. 10.1016/j.apmr.2004.05.019 [DOI] [PubMed] [Google Scholar]
- Buckinx F., Beaudart C., Maquet D., Demonceau M., Crielaard J. M., Reginster J. Y., et al. (2014). Evaluation of the impact of 6-month training by whole body vibration on the risk of falls among nursing home residents, observed over a 12-month period: A single blind, randomized controlled trial. Aging Clin. Exp. Res. 26 (4), 369–376. 10.1007/s40520-014-0197-z [DOI] [PubMed] [Google Scholar]
- Burns E. R., Stevens J. A., Lee R. (2016). The direct costs of fatal and non-fatal falls among older adults - United States. J. Saf. Res. 58, 99–103. 10.1016/j.jsr.2016.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burton E., Hill A. M., Pettigrew S., Lewin G., Bainbridge L., Farrier K., et al. (2017). Why do seniors leave resistance training programs. Clin. Interv. Aging 12, 585–592. 10.2147/CIA.S128324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calder C. G., Mannion J., Metcalf P. A. (2013). Low-intensity whole-body vibration training to reduce fall risk in active, elderly residents of a retirement village. J. Am. Geriatr. Soc. 61 (8), 1424–1426. 10.1111/jgs.12391 [DOI] [PubMed] [Google Scholar]
- Cardinale M., Wakeling J. (2005). Whole body vibration exercise: Are vibrations good for you. Br. J. Sports Med. 39 (9), 585–589. discussion 589. 10.1136/bjsm.2005.016857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cashin A. G., McAuley J. H. (2020). Clinimetrics: Physiotherapy evidence database (PEDro) scale. J. Physiother. 66 (1), 59. 10.1016/j.jphys.2019.08.005 [DOI] [PubMed] [Google Scholar]
- Corrie H., Brooke-Wavell K., Mansfield N. J., Cowley A., Morris R., Masud T. (2015). Effects of vertical and side-alternating vibration training on fall risk factors and bone turnover in older people at risk of falls. Age Ageing 44 (1), 115–122. 10.1093/ageing/afu136 [DOI] [PubMed] [Google Scholar]
- Costantino G., Montano N., Casazza G. (2015). When should we change our clinical practice based on the results of a clinical study? The hierarchy of evidence. Intern Emerg. Med. 10 (6), 745–747. 10.1007/s11739-015-1230-8 [DOI] [PubMed] [Google Scholar]
- Da Silva-Grigoletto M. E., De Hoyo M., Sañudo B., Carrasco L., García-Manso J. M. (2011). Determining the optimal whole-body vibration dose-response relationship for muscle performance. J. Strength Cond. Res. 25 (12), 3326–3333. 10.1519/JSC.0b013e3182163047 [DOI] [PubMed] [Google Scholar]
- de Oliveira R., de Oliveira R. G., de Oliveira L. C., Santos-Filho S. D., Sá-Caputo D. C., Bernardo-Filho M. (2023). Effectiveness of whole-body vibration on bone mineral density in postmenopausal women: A systematic review and meta-analysis of randomized controlled trials. Osteoporos. Int. 34 (1), 29–52. 10.1007/s00198-022-06556-y [DOI] [PubMed] [Google Scholar]
- Delecluse C., Roelants M., Verschueren S. (2003). Strength increase after whole-body vibration compared with resistance training. Med. Sci. Sports Exerc 35 (6), 1033–1041. 10.1249/01.MSS.0000069752.96438.B0 [DOI] [PubMed] [Google Scholar]
- Dincher A., Becker P., Wydra G. (2021). Effect of whole-body vibration on freezing and flexibility in Parkinson's disease-a pilot study. Neurol. Sci. 42 (7), 2795–2801. 10.1007/s10072-020-04884-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dutra M. C., de Oliveira M. L., Marin R. V., Kleine H. C., Silva O. L., Lazaretti-Castro M. (2016). Whole-body vibration improves neuromuscular parameters and functional capacity in osteopenic postmenopausal women. Menopause 23 (8), 870–875. 10.1097/GME.0000000000000644 [DOI] [PubMed] [Google Scholar]
- Furness T. P., Maschette W. E. (2009). Influence of whole body vibration platform frequency on neuromuscular performance of community-dwelling older adults. J. Strength Cond. Res. 23 (5), 1508–1513. 10.1519/JSC.0b013e3181a4e8f9 [DOI] [PubMed] [Google Scholar]
- Furness T. P., Maschette W. E., Lorenzen C., Naughton G. A., Williams M. D. (2010). Efficacy of a whole-body vibration intervention on functional performance of community-dwelling older adults. J. Altern. Complement. Med. 16 (7), 795–797. 10.1089/acm.2009.0366 [DOI] [PubMed] [Google Scholar]
- Ganz D. A., Latham N. K. (2020). Prevention of falls in community-dwelling older adults. N. Engl. J. Med. 382 (8), 734–743. 10.1056/NEJMcp1903252 [DOI] [PubMed] [Google Scholar]
- Gates S., Fisher J. D., Cooke M. W., Carter Y. H., Lamb S. E. (2008). Multifactorial assessment and targeted intervention for preventing falls and injuries among older people in community and emergency care settings: Systematic review and meta-analysis. BMJ 336 (7636), 130–133. 10.1136/bmj.39412.525243.BE [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillespie L. D., Robertson M. C., Gillespie W. J., Sherrington C., Gates S., Clemson L. M., et al. (2012). Interventions for preventing falls in older people living in the community. Cochrane Database Syst. Rev. 2012 (9), CD007146. 10.1002/14651858.CD007146.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg A., Chavis M., Watkins J., Wilson T. (2012). The five-times-sit-to-stand test: Validity, reliability and detectable change in older females. Aging Clin. Exp. Res. 24 (4), 339–344. 10.1007/BF03325265 [DOI] [PubMed] [Google Scholar]
- Gomes-Neto M., de Sá-Caputo D., Paineiras-Domingos L. L., Brandão A. A., Neves M. F., Marin P. J., et al. (2019). Effects of whole-body vibration in older adult patients with type 2 diabetes mellitus: A systematic review and meta-analysis. Can. J. Diabetes 43 (7), 524–529.e2. 10.1016/j.jcjd.2019.03.008 [DOI] [PubMed] [Google Scholar]
- Goudarzian M., Ghavi S., Shariat A., Shirvani H., Rahimi M. (2017). Effects of whole body vibration training and mental training on mobility, neuromuscular performance, and muscle strength in older men. J. Exerc Rehabil. 13 (5), 573–580. 10.12965/jer.1735024.512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hazell T. J., Jakobi J. M., Kenno K. A. (2007). The effects of whole-body vibration on upper- and lower-body EMG during static and dynamic contractions. Appl. Physiol. Nutr. Metab. 32 (6), 1156–1163. 10.1139/H07-116 [DOI] [PubMed] [Google Scholar]
- Higgins J. P., Altman D. G., Gøtzsche P. C., Jüni P., Moher D., Oxman A. D., et al. (2011). The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 343, d5928. 10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang H. Y., Choi J. S., Kim H. E. (2018). Masticatory efficiency contributing to the improved dynamic postural balance: A cross-sectional study. Gerodontology 35 (3), 254–259. 10.1111/ger.12349 [DOI] [PubMed] [Google Scholar]
- Jepsen D. B., Thomsen K., Hansen S., Jørgensen N. R., Masud T., Ryg J. (2017). Effect of whole-body vibration exercise in preventing falls and fractures: A systematic review and meta-analysis. BMJ Open 7 (12), e018342. 10.1136/bmjopen-2017-018342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jingwang T., Jichao W., Xueping W. (2019). Effects of vibration training in sitting posture on the lower extremity muscle strength,balance and walking abilities in older adults. Chin. J. TISSUE Eng. Res. 23, 2350–2355. 10.3969/j.issn.2095-4344.1166 [DOI] [Google Scholar]
- Kawanabe K., Kawashima A., Sashimoto I., Takeda T., Sato Y., Iwamoto J. (2007). Effect of whole-body vibration exercise and muscle strengthening, balance, and walking exercises on walking ability in the elderly. Keio J. Med. 56 (1), 28–33. 10.2302/kjm.56.28 [DOI] [PubMed] [Google Scholar]
- Lam F. M., Chan P. F., Liao L. R., Woo J., Hui E., Lai C. W., et al. (2018). Effects of whole-body vibration on balance and mobility in institutionalized older adults: A randomized controlled trial. Clin. Rehabil. 32 (4), 462–472. 10.1177/0269215517733525 [DOI] [PubMed] [Google Scholar]
- Lam F. M., Lau R. W., Chung R. C., Pang M. Y. (2012). The effect of whole body vibration on balance, mobility and falls in older adults: A systematic review and meta-analysis. Maturitas 72 (3), 206–213. 10.1016/j.maturitas.2012.04.009 [DOI] [PubMed] [Google Scholar]
- Laurisa A. A. Y., Gargi A., Kamsma Y. P. T., Arjan K., van der Zee Eddy A., van Heuvelen Marieke J. G. (2022). Potential of whole-body vibration in Parkinson’s disease: A systematic review and meta-analysis of human and animal studies. Biol. (Basel) 11 (8), 1238. 10.3390/biology11081238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lei M., Yan Z., Shaoyan L., Wei X. (2016). Study on the application of whole body vibration therapy in improving the elderly balance ability. Chin. Comm. Doc. 32 (24), 168–169. 10.3969/j.issn.1007-614x.2016.24.104 [DOI] [Google Scholar]
- Lin C. I., Huang W. C., Chen W. C., Kan N. W., Wei L., Chiu Y. S., et al. (2015). Effect of whole-body vibration training on body composition, exercise performance and biochemical responses in middle-aged mice. Metabolism 64 (9), 1146–1156. 10.1016/j.metabol.2015.05.007 [DOI] [PubMed] [Google Scholar]
- Liu Y., Fan Y., Chen X. (2022). Effects of whole-body vibration training with different body positions and amplitudes on lower limb muscle activity in middle-aged and older women. Dose Response 20 (3), 15593258221112960. 10.1177/15593258221112960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lord S. R., McLean D., Stathers G. (1992). Physiological factors associated with injurious falls in older people living in the community. Gerontology 38 (6), 338–346. 10.1159/000213351 [DOI] [PubMed] [Google Scholar]
- Lu L., Mao L., Feng Y., Ainsworth B. E., Liu Y., Chen N. (2021). Effects of different exercise training modes on muscle strength and physical performance in older people with sarcopenia: A systematic review and meta-analysis. BMC Geriatr. 21 (1), 708. 10.1186/s12877-021-02642-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo J., McNamara B., Moran K. (2005). The use of vibration training to enhance muscle strength and power. Sports Med. 35 (1), 23–41. 10.2165/00007256-200535010-00003 [DOI] [PubMed] [Google Scholar]
- Marín P. J., Martín-López A., Vicente-Campos D., Angulo-Carrere M., García-Pastor T., Garatachea N., et al. (2011). Effects of vibration training and detraining on balance and muscle strength in older adults. J. Sports Sci. Med. 10 (3), 559–564. 10.1016/S0140-6736(02)07666-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montero-Odasso M., van der Velde N., Alexander N. B., Becker C., Blain H., Camicioli R., et al. (2021). New horizons in falls prevention and management for older adults: A global initiative. Age Ageing 50 (5), 1499–1507. 10.1093/ageing/afab076 [DOI] [PubMed] [Google Scholar]
- Montero-Odasso M., van der Velde N., Martin F. C., Petrovic M., Tan M. P., Ryg J., et al. (2022). World guidelines for falls prevention and management for older adults: A global initiative. Age Ageing 51 (9), afac205. 10.1093/ageing/afac205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morley J. E., Vellas B., van Kan G. A., Anker S. D., Bauer J. M., Bernabei R., et al. (2013). Frailty consensus: A call to action. J. Am. Med. Dir. Assoc. 14 (6), 392–397. 10.1016/j.jamda.2013.03.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nawrat-Szołtysik A., Sieradzka M., Nowacka-Chmielewska M., Piejko L., Duda J., Brachman A., et al. (2022). Effect of whole-body vibration training on selected intrinsic risk factors in women aged 60+ at fall risk: A randomized controlled trial. Int. J. Environ. Res. Public Health 19 (24), 17066. 10.3390/ijerph192417066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ochi A., Abe T., Yamada K., Ibuki S., Tateuchi H., Ichihashi N. (2015). Effect of balance exercise in combination with whole-body vibration on muscle activity of the stepping limb during a forward fall in older women: A randomized controlled pilot study. Arch. Gerontol. Geriatr. 60 (2), 244–251. 10.1016/j.archger.2014.11.011 [DOI] [PubMed] [Google Scholar]
- Oroszi T., van Heuvelen M., Nyakas C., van der Zee E. A. (2020). Vibration detection: Its function and recent advances in medical applications. F1000Res 9. 10.12688/f1000research.22649.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orr R. (2015). The effect of whole body vibration exposure on balance and functional mobility in older adults: A systematic review and meta-analysis. Maturitas 80 (4), 342–358. 10.1016/j.maturitas.2014.12.020 [DOI] [PubMed] [Google Scholar]
- Page M. J., McKenzie J. E., Bossuyt P. M., Boutron I., Hoffmann T. C., Mulrow C. D., et al. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. J. Clin. Epidemiol. 134, 178–189. 10.1016/j.jclinepi.2021.03.001 [DOI] [PubMed] [Google Scholar]
- Paineiras-Domingos L. L., da Cunha Sá-Caputo D., Reis A. S., Francisca Santos A., Sousa-Gonçalves C. R., Dos Anjos E. M., et al. (2018). Assessment through the short physical performance battery of the functionality in individuals with metabolic syndrome exposed to whole-body vibration exercises. Dose Response 16 (3), 1559325818794530. 10.1177/1559325818794530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phu S., Vogrin S., Al Saedi A., Duque G. (2019). Balance training using virtual reality improves balance and physical performance in older adults at high risk of falls. Clin. Interv. Aging 14, 1567–1577. 10.2147/CIA.S220890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Podsiadlo D., Richardson S. (1991). The timed "up and Go": A test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 39 (2), 142–148. 10.1111/j.1532-5415.1991.tb01616.x [DOI] [PubMed] [Google Scholar]
- Pollock R. D., Martin F. C., Newham D. J. (2012). Whole-body vibration in addition to strength and balance exercise for falls-related functional mobility of frail older adults: A single-blind randomized controlled trial. Clin. Rehabil. 26 (10), 915–923. 10.1177/0269215511435688 [DOI] [PubMed] [Google Scholar]
- Rauch F., Sievanen H., Boonen S., Cardinale M., Degens H., Felsenberg D., et al. (2010). Reporting whole-body vibration intervention studies: Recommendations of the international society of musculoskeletal and neuronal interactions. J. Musculoskelet. Neuronal Interact. 10 (3), 193–198. 10.1080/0305006910270105 [DOI] [PubMed] [Google Scholar]
- Rees S., Murphy A., Watsford M. (2007). Effects of vibration exercise on muscle performance and mobility in an older population. J. Aging Phys. Act. 15 (4), 367–381. 10.1123/japa.15.4.367 [DOI] [PubMed] [Google Scholar]
- Ritzmann R., Krause A., Freyler K., Gollhofer A. (2018). Acute whole-body vibration increases reciprocal inhibition. Hum. Mov. Sci. 60, 191–201. 10.1016/j.humov.2018.06.011 [DOI] [PubMed] [Google Scholar]
- Roelants M., Delecluse C., Goris M., Verschueren S. (2004). Effects of 24 weeks of whole body vibration training on body composition and muscle strength in untrained females. Int. J. Sports Med. 25 (1), 1–5. 10.1055/s-2003-45238 [DOI] [PubMed] [Google Scholar]
- Rogan S., Hilfiker R., Herren K., Radlinger L., de Bruin E. D. (2011). Effects of whole-body vibration on postural control in elderly: A systematic review and meta-analysis. BMC Geriatr. 11, 72. 10.1186/1471-2318-11-72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogan S., Taeymans J., Radlinger L., Naepflin S., Ruppen S., Bruelhart Y., et al. (2017). Effects of whole-body vibration on postural control in elderly: An update of a systematic review and meta-analysis. Arch. Gerontol. Geriatr. 73, 95–112. 10.1016/j.archger.2017.07.022 [DOI] [PubMed] [Google Scholar]
- Sajadi N., Bagheri R., Amiri A., Maroufi N., Shadmehr A., Pourahmadi M. (2019). Effects of different frequencies of whole body vibration on repositioning error in patients with chronic low back pain in different angles of lumbar flexion. J. Manip. Physiol. Ther. 42 (4), 227–236. 10.1016/j.jmpt.2018.11.006 [DOI] [PubMed] [Google Scholar]
- Santin-Medeiros F., Rey-López J. P., Santos-Lozano A., Cristi-Montero C. S., Garatachea Vallejo N. (2015). Effects of eight months of whole-body vibration training on the muscle mass and functional capacity of elderly women. J. Strength Cond. Res. 29 (7), 1863–1869. 10.1519/JSC.0000000000000830 [DOI] [PubMed] [Google Scholar]
- Sen E. I., Esmaeilzadeh S., Eskiyurt N. (2020). Effects of whole-body vibration and high impact exercises on the bone metabolism and functional mobility in postmenopausal women. J. Bone Min. Metab. 38 (3), 392–404. 10.1007/s00774-019-01072-2 [DOI] [PubMed] [Google Scholar]
- Sherrington C., Fairhall N., Wallbank G., Tiedemann A., Michaleff Z. A., Howard K., et al. (2020). Exercise for preventing falls in older people living in the community: An abridged Cochrane systematic review. Br. J. Sports Med. 54 (15), 885–891. 10.1136/bjsports-2019-101512 [DOI] [PubMed] [Google Scholar]
- Sherrington C., Fairhall N. J., Wallbank G. K., Tiedemann A., Michaleff Z. A., Howard K., et al. (2019). Exercise for preventing falls in older people living in the community. Cochrane Database Syst. Rev. 1 (1), CD012424. 10.1002/14651858.CD012424.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherrington C., Whitney J. C., Lord S. R., Herbert R. D., Cumming R. G., Close J. C. (2008). Effective exercise for the prevention of falls: A systematic review and meta-analysis. J. Am. Geriatr. Soc. 56 (12), 2234–2243. 10.1111/j.1532-5415.2008.02014.x [DOI] [PubMed] [Google Scholar]
- Sitjà-Rabert M., Martínez-Zapata M. J., Fort Vanmeerhaeghe A., Rey Abella F., Romero-Rodríguez D., Bonfill X. (2015). Effects of a whole body vibration (WBV) exercise intervention for institutionalized older people: A randomized, multicentre, parallel, clinical trial. J. Am. Med. Dir. Assoc. 16 (2), 125–131. 10.1016/j.jamda.2014.07.018 [DOI] [PubMed] [Google Scholar]
- Sucuoglu H., Tuzun S., Akbaba Y. A., Uludag M., Gokpinar H. H. (2015). Effect of whole-body vibration on balance using posturography and balance tests in postmenopausal women. Am. J. Phys. Med. Rehabil. 94 (7), 499–507. 10.1097/PHM.0000000000000325 [DOI] [PubMed] [Google Scholar]
- Tseng S. Y., Ko C. P., Tseng C. Y., Huang W. C., Lai C. L., Wang C. H. (2021). Is 20 Hz whole-body vibration training better for older individuals than 40 hz. Int. J. Environ. Res. Public Health 18 (22), 11942. 10.3390/ijerph182211942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Heuvelen M., Rittweger J., Judex S., Sañudo B., Seixas A., Fuermaier A. B. M., et al. (2021). Reporting guidelines for whole-body vibration studies in humans, animals and cell cultures: A consensus statement from an international group of experts. Biol. (Basel) 10 (10), 965. 10.3390/biology10100965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Stengel S., Kemmler W., Engelke K., Kalender W. A. (2012). Effect of whole-body vibration on neuromuscular performance and body composition for females 65 years and older: A randomized-controlled trial. Scand. J. Med. Sci. Sports 22 (1), 119–127. 10.1111/j.1600-0838.2010.01126.x [DOI] [PubMed] [Google Scholar]
- Wadsworth D., Lark S. (2020). Effects of whole-body vibration training on the physical function of the frail elderly: An open, randomized controlled trial. Arch. Phys. Med. Rehabil. 101 (7), 1111–1119. 10.1016/j.apmr.2020.02.009 [DOI] [PubMed] [Google Scholar]
- Wei N., Pang M. Y., Ng S. S., Ng G. Y. (2017). Optimal frequency/time combination of whole body vibration training for developing physical performance of people with sarcopenia: A randomized controlled trial. Clin. Rehabil. 31 (10), 1313–1321. 10.1177/0269215517698835 [DOI] [PubMed] [Google Scholar]
- Whitney S. L., Wrisley D. M., Marchetti G. F., Gee M. A., Redfern M. S., Furman J. M. (2005). Clinical measurement of sit-to-stand performance in people with balance disorders: Validity of data for the five-times-sit-to-stand test. Phys. Ther. 85 (10), 1034–1045. 10.1093/ptj/85.10.1034 [DOI] [PubMed] [Google Scholar]
- Wuestefeld A., Fuermaier A., Bernardo-Filho M., da Cunha de Sá-Caputo D., Rittweger J., Schoenau E., et al. (2020). Towards reporting guidelines of research using whole-body vibration as training or treatment regimen in human subjects-A Delphi consensus study. PLoS One 15 (7), e0235905. 10.1371/journal.pone.0235905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao-feng Z. (2020). Effects of whole-body vibration training with different frequency on balance and core stability for old adults. Chin. J. Rehabil. Theory Pract. 26 (03), 291–294. 10.3969/j.issn.1006-9771.2020.03.005 [DOI] [Google Scholar]
- Yeung S. S., Yeung E. W. (2015). A 5-week whole body vibration training improves peak torque performance but has no effect on stretch reflex in healthy adults: A randomized controlled trial. J. Sports Med. Phys. Fit. 55 (5), 397–404. [PubMed] [Google Scholar]
- Zhang L., Weng C., Liu M., Wang Q., Liu L., He Y. (2014). Effect of whole-body vibration exercise on mobility, balance ability and general health status in frail elderly patients: A pilot randomized controlled trial. Clin. Rehabil. 28 (1), 59–68. 10.1177/0269215513492162 [DOI] [PubMed] [Google Scholar]
- Zhu Y. Q., Peng N., Zhou M., Liu P. P., Qi X. L., Wang N., et al. (2019). Tai chi and whole-body vibrating therapy in sarcopenic men in advanced old age: A clinical randomized controlled trial. Eur. J. Ageing 16 (3), 273–282. 10.1007/s10433-019-00498-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuo C., Bo S., Wang T., Zhang W. (2022). Functional and traditional resistance training are equally effective in increasing upper and lower limb muscular endurance and performance variables in untrained young men. Front. Physiol. 13, 868195. 10.3389/fphys.2022.868195 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.