Abstract
Racial/ethnic and sex/gender disparities in sleep duration have been documented in adolescence and adulthood. Identifying racial/ethnic and sex/gender differences in sleep duration trajectories from adolescence to adulthood can inform interventions on the developmental periods individuals are most at risk for short sleep duration. We examined racial/ethnic and sex/gender differences in self-reported sleep duration trajectories from adolescence to adulthood using data from waves I, III, IV, and V of the National Longitudinal Study of Adolescent to Adult Health (1994–2018; n = 12,593). Multigroup growth mixture modeling was used to enumerate sleep duration trajectories from adolescence to adulthood. There were 3 common trajectory types across race/ethnicity and sex/gender groups: 1) consistent increasing short sleepers (i.e., increasing probability of short sleep into adulthood) (67.3%); 2) late-onset short sleepers (i.e., no probability of short sleep duration in adolescence until adulthood) (20.2%); and 3) early-onset short sleepers (i.e., declining probability of short sleep duration from adolescence into adulthood) (12.5%). The prevalence of the consistent-increasing trajectory was highest among Black male respondents, while late onset was highest among White female respondents and early onset greatest among Latinx male respondents. Findings underscore the need to intervene in early adolescence to prevent short sleep duration in adulthood.
Keywords: ethnicity, gender, health status disparities, life span, race, sex, sleep
Abbreviations
- Add Health
National Longitudinal Study of Adolescent to Adult Health
- GMM
growth mixture model
- SD
standard deviation
Sleep is vital for physical and cognitive development across the life span (1, 2). Short sleep duration (<8 hours at ages 13–18 years and <7 hours for adults over age 18) (3, 4) has been linked to negative health outcomes, such as obesity, diabetes, hypertension, and depression, among both adolescents and adults (5–9). Approximately 70% of adolescents and 35% of adults reported short sleep duration (10, 11). The transition from adolescence to adulthood is a critical period with various biological and sociocontextual changes that converge, leading to declining sleep duration into adulthood (12). Possible biological processes include a circadian phase delay during pubertal development that favors an evening chronotype and the development of a sleep-wake homeostatic system that allows for more wakefulness during the daytime; both processes result in a progressively later bedtime from early adolescence into young adulthood (13). In combination with a later bedtime, sociocontextual pressures such as early school start times during adolescence, academic and work demands, increasing responsibilities as young adults become independent from their parents, and family formation present additional barriers to sleep (14–16). However, minoritized racial/ethnic groups and women have unique sociocontextual experiences from adolescence to adulthood that may have different impacts on their sleep duration patterns across the life course that warrant further research.
Significant racial/ethnic disparities in sleep duration have been documented. Asian, Black, and Hispanic/Latino adolescents generally report shorter sleep duration than non-Hispanic White adolescents, with similar disparities found among adults (17, 18). These racial/ethnic disparities in sleep duration may be attributed to the persistent racially discriminatory policies and practices that subject minoritized racial/ethnic groups to greater social disadvantage and restrict them from accessing opportunities and resources beneficial to health (19). In turn, minoritized racial/ethnic groups may have greater exposure to factors detrimental to sleep, such as psychosocial stressors, shift work, lower socioeconomic status, acculturative stress, and adverse physical (e.g., air and noise pollution) and social (e.g., lower social cohesion and safety) neighborhood environments (20–26). These unique harmful sociocontextual experiences among racial/ethnic minoritized groups could result in different sleep duration trajectories from adolescence to adulthood, compared with their White peers.
Findings from research examining sex (i.e., biological characteristics such as chromosomes and reproductive/sexual anatomy) and gender (i.e., social construct to describe norms and behaviors that society associates with being male and female) differences have been mixed among both adolescents and adults, demonstrating shorter (11, 27, 28) and longer (29–33) sleep duration among female participants. Shorter sleep duration among female participants could be attributed to earlier pubertal onset during adolescence or hormonal changes (e.g., estrogen and progesterone) that occur during pregnancy and menopause, coupled with gendered expectations (e.g., childcare and housework) (34, 35). Although women tend to experience greater psychosocial stressors (e.g., gender discrimination, occupational stress, and financial strain) (36–40) that are detrimental to sleep, they may be more likely to seek and receive social support than men (41–43), which could help buffer the impact of these stressors on sleep (44, 45). Research, although sparse, suggests that shorter sleep duration among men may be due to poorer sleep hygiene (e.g., greater caffeine intake and screen time) and less positive attitudes towards healthy sleep behaviors than those held by women (46, 47). The interaction of these various biological and sociocultural factors may play a role in shaping sleep duration from adolescence to adulthood for women that may differ from men.
Studies have generally examined sleep disparities in relation to one social identity (e.g., race/ethnicity or gender), with few attempting to explore the impact of multiple identities (e.g., race/ethnicity and gender) on sleep. In the context of public health, intersectionality is a theoretical framework that seeks to understand how the interplay of multiple social identities (e.g., race, gender, social class, sexual orientation, and disability) grants individuals advantages/disadvantages that will influence their health and create health inequities (48). There is growing recognition of the need for intersectional approaches to address health disparities, especially sleep disparities (17). Evidence suggests that sleep duration differs jointly by race/ethnicity and sex/gender in adolescent and adult populations, with Black male and female participants generally reporting the shortest sleep duration and non-Hispanic White women reporting the longest (30, 49–52). However, these studies have focused primarily on documenting racial/ethnic and sex/gender differences in sleep duration in one developmental period.
Assessing sleep duration across multiple developmental periods is important, given that research suggests that sleep duration from earlier developmental periods can influence health later in life (53, 54). Rather than focusing on the impact of sleep at one point in time, research examining the impact of sleep duration across multiple developmental periods may be more informative in predicting health outcomes. For instance, studies among a national US cohort found that cumulative short sleep duration (<6 hours/day) from adolescence to adulthood was associated with increased risk of obesity and asthma (55, 56).
An important approach to examining sleep duration across developmental periods is through characterizing sleep duration trajectories. Sleep duration trajectories could help determine critical periods of inadequate sleep duration, which may be useful for informing sleep interventions. Yet studies describing sleep duration trajectories across the life course remain limited (56–58). These studies have not applied an intersectionality framework to examine sleep duration trajectories from adolescence to adulthood by race/ethnicity and sex/gender. This information could be used to develop interventions targeting specific developmental periods to reduce sleep disparities and ultimately health disparities.
To expand upon prior literature, the primary purpose of this study was to utilize an intersectionality approach to describe race/ethnicity and sex/gender differences in sleep duration trajectories from adolescence to adulthood.
METHODS
Sample
Participants were from the National Longitudinal Study of Adolescent to Adult Health (Add Health) which is a nationally representative, school-based sample with the purpose of investigating adolescent behaviors and their health in adulthood (59). There were 80 high schools and 52 middle schools selected with respect to region of country, urbanicity, school size, school type, and ethnicity to ensure representativeness of US schools. In 1994–1995, an in-home interview was conducted among 20,745 adolescents from these participating schools, with an additional 4 follow-up interviews: wave II in 1996 (n = 14,738; mean age = 16.2 years), wave III from 2001–2002 (n = 15,197; mean age = 22.0 years), wave IV in 2008 (n = 15,701; mean age = 28.5 years), and wave V from 2016–2018 (n = 12,300; mean age = 37.0 years). A more in-depth description of the study design has been published elsewhere (59). In these analyses, those who identified as Black male, Black female, Hispanic male, Hispanic female, White male, or White female from wave I were included (n = 18,649). Other race and sex groups were excluded due to inadequate sample size for analysis. Those with missing sleep duration data in waves I, III, IV, and V were excluded (n = 51). Long sleepers (defined as >12 hours for ages 6–12 years, >10 hours for ages 13–18 years, >9 hours for ages >18 years) in any of the waves (wave I: n = 556, wave III: n = 3,331, wave IV: n = 2,931, and wave V: n = 480) were excluded (total n = 6,020) instead of being grouped with short sleepers or those with the recommended amount of sleep. The reasons for this exclusion were that mechanisms linking long sleep to health may differ from those linking short sleep to health (60) and the sample size for long sleepers in waves I and V was small. The final analytical sample was 12,593 participants (Web Figure 1, available at https://doi.org/10.1093/aje/kwac156).
Compared with those included in this study, excluded participants were more likely to be female, have higher parental education and educational level, report greater depressive symptoms, and report fair or poor health across all waves (Web Table 1). Supplemental analyses including long sleepers were conducted, with results shown in Web Figure 2. The original Add Health study was approved by the institutional review board of the University of North Carolina, Chapel Hill, and written consent forms were obtained from adolescents and their parents. This present analysis was approved by the institutional review board of Emory University.
Study measures
Sleep duration.
Measurements of sleep duration varied by waves. In waves I and V, participants were asked to respond in whole hours to the question, “How many hours of sleep do you usually get?” In waves III and IV, sleep duration was assessed by asking participants for their sleep and wake times for the weekday and weekend. Total sleep hours per day was calculated by a weighted average based on prior studies conducted on sleep using the Add Health data set, in which sleep hours during the weekday (multiplied by 5/7) was summed with weekend sleep hours (multiplied by 2/7) (28, 55). The recommended nightly amount of sleep by age from the American Academy of Sleep Medicine (AASM) is 9–12 hours for ages 6–12 years, 8–10 hours for ages 13–17 years, and 7–9 hours for ages 18 or older (3, 4) and was categorized in analyses as short sleep duration (less than recommended by AASM) vs. healthy sleep duration (within recommended by AASM).
Race/ethnicity and sex/gender.
Race/ethnicity categories were constructed based on recommendations by the Add Health research team (61). Respondents were first asked whether they were of Hispanic or Latino origin. A separate question asked respondents to indicate their race, with White, Black or African American, American Indian or Native American, Asian or Pacific Islander, or “other” as possible answers and the ability to select multiple racial groups. Those that indicated being of Hispanic or Latino origin were categorized as “Hispanic” for their race/ethnicity. If participants did not indicate they were of Hispanic or Latino origin and selected “Black or African American” as one of their racial identities, they were categorized as Black for their race/ethnicity, and their other selected racial categories were omitted. This was repeated for the remaining racial groups in the following order: Asian, Native American, other, and non-Hispanic White. Hereafter, Hispanic will be referred to as Latinx and non-Hispanic White will be referred to as White. Sex/gender was assessed by asking whether respondents identified as male or female. The combined race/ethnicity and sex/gender categories for the analyses included: Black male, Black female, Latinx male, Latinx female, White male, and White female.
Statistical analysis.
The distributions of participant characteristics were examined by race/ethnicity and sex/gender using χ2 tests and analysis of variance. Given our interest in applying an intersectionality framework, multigroup growth mixture models (GMMs) were fitted to enumerate the sleep duration trajectory classes across the developmental periods for each race/ethnicity and sex/gender group. In the GMMs, the grouping variable was the race and sex groups; the latent trajectory classes represented the changes in probability of short sleep duration across developmental periods. Covariates were not included in the GMMs given that most factors may be potential mediators in the pathway between race/ethnicity, sex, and sleep duration (See Web Figure 3 for conceptual model) (17, 34). Developmental periods included early adolescence (11–14 years), adolescence (15–19 years), emerging adulthood (20–24 years), young adulthood (25–34 years), and adulthood (35–44 years), based on prior literature (62–64). Once the classes were identified, participants were assigned exclusively to one class based on their highest estimated posterior probabilities. Two to four class models were estimated and compared using the Akaike information criterion (AIC), Bayesian information criterion (BIC), and entropy. The 3-class model had the best fit because of the lower AIC and BIC, higher entropy, and interpretability of classes (65). GMMs were fitted using Mplus, version 8.4 (Muthén & Muthén, Los Angeles, California), with a maximum likelihood estimator and expectation maximization algorithm to estimate parameters (66). Missing data was addressed with full information maximum likelihood, a method to calculate unbiased parameter estimates in the presence of missing data using each case’s available data (67). Descriptive analyses were conducted in SAS, version 9.4 (SAS Institute, Inc., Cary, North Carolina).
Since waves I and II data were collected only a year apart, some participants had 2 sleep duration data points in the early adolescence or adolescence developmental periods. Data in GMMs need to be time-structured, and to date no options are available to account for clustering within a time frame (L. K. Muthén, Mplus Support, personal communication, 2020). Thus, we could not include both data points in the analyses. To address this issue, GMMs including data from waves I, III, IV, and V were fitted and compared with models including data from waves II, III, IV, and V. Models including data from wave I had better model fit and interpretability of classes than those with data from wave II. Therefore, results from analyses including wave I are discussed below.
RESULTS
Descriptive analyses
The mean age was 13.4 (standard deviation (SD), 0.7) years in early adolescence, 16.7 (SD, 1.3) years in adolescence, 22.1 (SD, 1.3) years in emerging adulthood, 28.7 (SD, 1.9) years in young adulthood, and 38.2 (SD, 1.8) years in adulthood (Table 1). The prevalence of short sleep duration varied by developmental periods with 29.7% in early adolescence, 46.8% in adolescence, 31.4% emerging adulthood, 30.5% in young adulthood, and 46.1% in adulthood (Table 2). Short sleep duration was most prevalent among Black male participants across all developmental periods, except early adolescence, when Black female participants were more likely to have short sleep duration. The average sleep duration declined from adolescence into adulthood, with the lowest average sleep duration across developmental periods among Black participants irrespective of sex.
Table 1.
Mean (Standard Deviation) Age and Sleep Duration Across Developmental Periodsa According to Race/Ethnicity and Sex/Gender From Waves I, III, IV, and V of the National Longitudinal Study of Adolescent to Adult Health, United States, 1994–2018
| Age, Sleep Duration, and Developmental Period | Total (n = 12,593) | Race/Ethnicity and Sex/Gender | |||||
|---|---|---|---|---|---|---|---|
| Black Female (n = 1,525) | Black Male (n = 1,573) | Latinx Female (n = 1,126) | Latinx Male (n = 1,302) | White Female (n = 3,236) | White Male (n = 3,831) | ||
| Age in years | |||||||
| Early adolescence | 13.4 (0.7) | 13.3 (0.7) | 13.4 (0.7) | 13.4 (0.7) | 13.4 (0.7) | 13.4 (0.7) | 13.4 (0.7) |
| Adolescence | 16.7 (1.3) | 16.7 (1.3) | 16.7 (1.3) | 16.7 (1.2) | 16.8 (1.2) | 16.7 (1.3) | 16.6 (1.3) |
| Emerging adulthood | 22.1 (1.3) | 22.1 (1.3) | 22.1 (1.3) | 22.2 (1.3) | 22.4 (1.3) | 22.1 (1.4) | 22.1 (1.3) |
| Young adulthood | 28.7 (1.9) | 28.6 (1.9) | 28.7 (1.9) | 29.0 (1.8) | 29.1 (1.8) | 28.6 (1.9) | 28.7 (1.8) |
| Adulthood | 38.2 (1.8) | 38.1 (1.8) | 38.3 (1.8) | 38.5 (1.7) | 38.6 (1.8) | 37.9 (1.8) | 38.2 (1.8) |
| Sleep duration in hours | |||||||
| Early adolescence | 8.1 (1.1) | 7.8 (1.3) | 7.9 (1.2) | 8.1 (1.1) | 8.0 (1.2) | 8.1 (1.1) | 8.3 (1.0) |
| Adolescence | 7.4 (1.2) | 7.2 (1.3) | 7.3 (1.3) | 7.5 (1.3) | 7.3 (1.2) | 7.4 (1.2) | 7.5 (1.2) |
| Emerging adulthood | 7.3 (1.0) | 7.3 (1.1) | 7.1 (1.2) | 7.2 (1.1) | 7.4 (1.0) | 7.4 (0.9) | 7.2 (1.0) |
| Young adulthood | 7.2 (1.0) | 7.2 (1.1) | 6.8 (1.2) | 7.2 (1.0) | 7.4 (1.0) | 7.5 (0.9) | 7.2 (1.0) |
| Adulthood | 6.6 (1.1) | 6.3 (1.1) | 6.2 (1.1) | 6.5 (1.0) | 6.5 (1.1) | 6.7 (1.0) | 6.6 (1.0) |
a Developmental periods include early adolescence (11–14 years), adolescence (15–19 years), emerging adulthood (20–24 years), young adulthood (25–34 years), and adulthood (35–44 years).
Table 2.
Distribution of Short Sleep Durationa Across Developmental Periodsb According to Race/Ethnicity and Sex/Gender From Waves I, III, IV, and V of the National Longitudinal Study of Adolescent to Adult Health, United States, 1994–2018
| Race/Ethnicity and Sex/Gender | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Total
(n = 12,593) |
Black Female (n = 1,525) |
Black Male
(n = 1,573) |
Latinx Female
(n = 1,126) |
Latinx Male
(n = 1,302) |
White Female
(n = 3,236) |
White Male
(n = 3,831) |
||||||||
| Short Sleep Duration and Developmental Period | No. | % | No. | % | No. | % | No. | % | No. | % | No. | % | No. | % |
| Developmental period | ||||||||||||||
| Early adolescence | 3,283 | 26.1 | 443 | 29.0 | 432 | 27.5 | 236 | 21.0 | 253 | 19.4 | 955 | 29.5 | 964 | 25.1 |
| Adolescence | 10,111 | 80.3 | 1,201 | 78.8 | 1,221 | 77.6 | 934 | 82.9 | 1,112 | 85.4 | 2,561 | 79.1 | 3,073 | 80.2 |
| Emerging adulthood | 7,018 | 55.7 | 852 | 55.7 | 780 | 49.6 | 578 | 51.3 | 670 | 51.5 | 1,951 | 60.3 | 2,187 | 57.1 |
| Young adulthood | 8,911 | 70.8 | 1,132 | 74.2 | 934 | 59.4 | 762 | 67.7 | 806 | 61.9 | 2,476 | 76.5 | 2,741 | 71.5 |
| Adulthood | 6,938 | 55.1 | 880 | 57.7 | 613 | 39.0 | 614 | 54.5 | 533 | 40.9 | 2,142 | 66.2 | 2,146 | 56.0 |
| Short sleep duration | ||||||||||||||
| Early adolescence | 975 | 29.7 | 174 | 39.3 | 158 | 36.6 | 72 | 30.5 | 76 | 30.0 | 278 | 29.1 | 217 | 22.5 |
| Adolescence | 4,728 | 46.8 | 612 | 51.0 | 625 | 51.2 | 476 | 50.5 | 485 | 43.6 | 1,222 | 47.7 | 1,308 | 42.6 |
| Emerging adulthood | 2,202 | 31.4 | 270 | 31.7 | 309 | 39.6 | 159 | 27.5 | 231 | 34.5 | 501 | 25.7 | 732 | 33.5 |
| Young adulthood | 2,721 | 30.5 | 380 | 33.6 | 471 | 47.4 | 190 | 24.9 | 275 | 34.1 | 548 | 22.1 | 857 | 31.3 |
| Adulthood | 3,197 | 46.1 | 522 | 59.3 | 387 | 63.1 | 286 | 46.6 | 256 | 48.0 | 844 | 39.2 | 902 | 42.0 |
a Defined as <9 hours for ages 6–12 years, <8 hours for ages 13–17 years, and <7 for ages 18 years or older based on the American Academy of Sleep Medicine recommendation for amount of sleep according to age.
b Developmental periods include early adolescence (11–14 years), adolescence (15–19 years), emerging adulthood (20–24 years), young adulthood (25–34 years), and adulthood (35–44 years).
Multigroup GMMs by race/ethnicity and sex/gender
The 3-class model was the best-performing model, with the lowest Akaike and Bayesian information criteria and the highest entropy (Web Table 2). This resulted in 18 trajectories (i.e., 3 trajectories for each of the 6 race/ethnicity and sex/gender intersectionality groups) (Figure 1, Figure 2, and Web Table 3). Through visual inspection, the 18 trajectories were grouped into 3 common sleep duration trajectory types as the 3 trajectories for each intersectionality group varied but were qualitatively comparable. The most prevalent trajectory (67.3%) type was labeled “consistent increasing short sleepers,” as the sleep pattern began in early adolescence at a mid-level probability (ranging from 0.44–0.46) of short sleep duration and consistently increased into adulthood (probability ranging from 0.47–0.67). The second most prevalent trajectory type was labeled “late-onset short sleepers,” as this group represented those who had zero probability of short sleep duration from adolescence to young adulthood but had a probability of short sleep duration in adulthood (20.2%). The least common trajectory type was labeled as “early-onset short sleepers” (12.5%) and included those with a high probability for short sleep duration during early adolescence only as short sleep declines to a low probability in the adult developmental periods.
Figure 1.
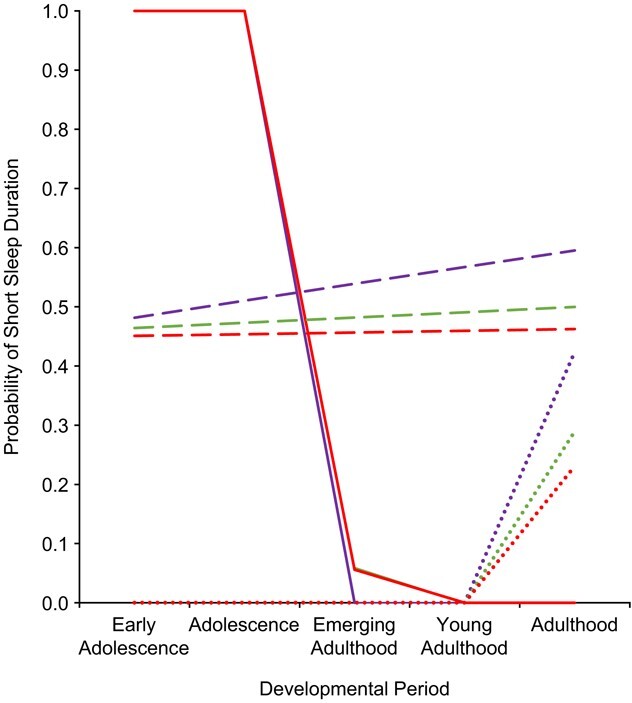
Multigroup growth mixture model short sleep duration trajectories according to race/ethnicity among female respondents, National Longitudinal Study of Adolescent to Adult Health, United States, 1994–2018. Developmental periods include early adolescence (11–14 years), adolescence (15–19 years), emerging adulthood (20–24 years), young adulthood (25–34 years), and adulthood (35–44 years). Trajectories include consistent increasing short sleepers (i.e., increasing probability of short sleep into adulthood), late-onset short sleepers (i.e., no probability of short sleep duration in adolescence until adulthood), early-onset short sleepers (i.e., declining probability of short sleep duration from adolescence into adulthood). Key: Black respondents, purple; Latinx respondents, green; white respondents, red. Early-onset short sleepers, solid lines; consistent increasing short sleepers, dashed lines; and late-onset short sleepers, dotted lines. The early-onset trajectories for Latinx and White respondents are overlapping. The late-onset trajectories are overlapping at zero probability from early adolescence to young adulthood for all racial/ethnic groups.
Figure 2.
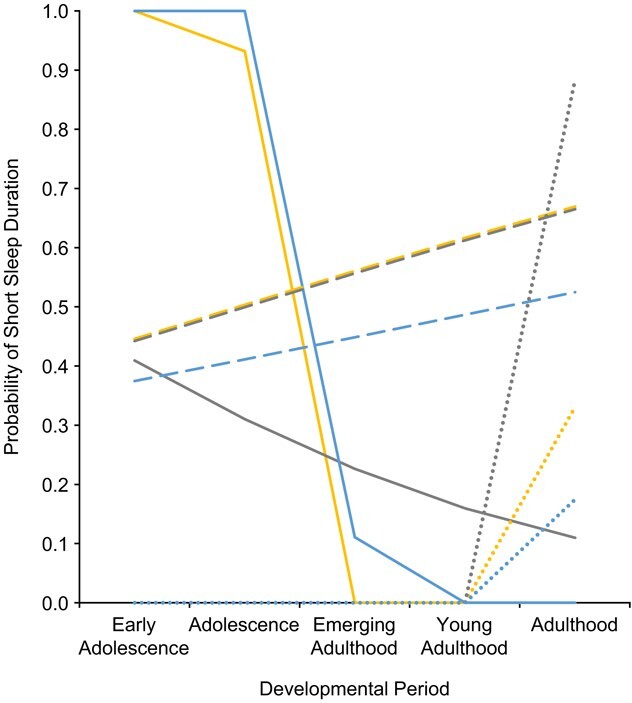
Multigroup growth mixture model short sleep duration trajectories according to race/ethnicity among male respondents, National Longitudinal Study of Adolescent to Adult Health, United States, United States, 1994–2018. Developmental periods include early adolescence (11–14 years), adolescence (15–19 years), emerging adulthood (20–24 years), young adulthood (25–34 years), and adulthood (35–44 years). Trajectories include consistent increasing short sleepers (i.e., increasing probability of short sleep into adulthood), late-onset short sleepers (i.e., no probability of short sleep duration in adolescence until adulthood), early-onset short sleepers (i.e., declining probability of short sleep duration from adolescence into adulthood). Key: Black respondents, yellow; Latinx respondents, gray; and White respondents, blue. Early-onset short sleepers, solid lines; consistent increasing short sleepers, dashed lines; and late-onset short sleepers, dotted lines. The early-onset trajectories for Black and White respondents overlap at zero probability from young adulthood to adulthood. The late-onset trajectories are overlapping at zero probability from early adolescence to young adulthood for all racial/ethnic groups.
Although these 18 trajectories could be grouped into 3 common trajectory types, there were notable differences between the race/ethnicity and sex/gender groups across and within each of these trajectory types (Figures 1 and 2). First, the distribution of the trajectory types varied by racial/ethnic and sex/gender groups (Table 3). Latinx male participants were the most likely to have an early-onset short sleeper trajectory. The consistent increasing short sleeper trajectory was the most prevalent among Black male participants, while the prevalence of late-onset short sleeper trajectory was the highest among White female participants. Second, the trajectories themselves varied across intersectionality groups, with the greatest variation observed among Latinx male participants. Latinx male participants who were early-onset short sleepers began at a mid-level probability (0.41) of short sleep duration and gradually declined to a low probability (0.11) into adulthood, whereas the other race/ethnicity and sex/gender groups had a high probability (1.0) of short sleep duration that sharply declined to a zero probability in adulthood. Latinx male respondents who were late-onset short sleepers had a drastically higher probability (0.88) in adulthood than the other race/ethnicity and sex/gender groups (ranging from 0.17 to 0.50).
Table 3.
Distribution of Short Sleep Duration Trajectories, in a Growth Mixture Model Analysis, According to Race/Ethnicity and Sex/Gender, National Longitudinal Study of Adolescent to Adult Health, United States, 1994–2018
| Sleep Duration Trajectory | ||||||
|---|---|---|---|---|---|---|
|
Consistent Increasing
a
(n = 8,475; 67.3%) |
Late Onset
b
(n = 2,542; 20.2%) |
Early Onset
c
(n = 1,576; 12.5%) |
||||
| Race/Ethnicity and Sex/Gender | n | % | n | % | n | % |
| Black | ||||||
| Female | 1,047 | 68.7 | 346 | 22.7 | 132 | 8.7 |
| Male | 1,363 | 86.7 | 164 | 10.4 | 46 | 2.9 |
| Latinx | ||||||
| Female | 731 | 64.9 | 277 | 24.6 | 118 | 10.5 |
| Male | 630 | 48.4 | 36 | 2.8 | 636 | 48.9 |
| White | ||||||
| Female | 1,787 | 55.2 | 1,039 | 32.1 | 410 | 12.7 |
| Male | 2,917 | 76.1 | 680 | 17.8 | 234 | 6.1 |
a Increasing probability of short sleep into adulthood.
b No probability of short sleep duration in adolescence until adulthood.
c Declining probability of short sleep duration from adolescence into adulthood.
In the supplemental analyses categorizing long sleepers as those who received at least the recommended amount of sleep, results were similar. There was one notable difference for Latinx male respondents in which the early-onset short sleepers with long sleepers included had a sharper decline in the probability of short sleep duration from early adolescence to adulthood, whereas there was a more gradual decline in this group with long sleepers excluded.
DISCUSSION
Our study found 3 common sleep duration trajectory types from adolescence to adulthood across 6 race/ethnicity and sex/gender groups. These 3 duration trajectory types included early-onset short sleepers, who had declining probability of short sleep from adolescence to adulthood; consistent increasing short sleepers, with increasing probability of short sleep duration from adolescence to adulthood; and late-onset short sleepers, with no probability of short sleep duration until adulthood. The distribution of these trajectory types differed across race/ethnicity and sex/gender groups, with some differences across race/ethnicity and sex/gender groups within each of these trajectory types.
The most prevalent sleep trajectory type in the overall sample was that of consistent increasing short sleepers. This suggests that for many individuals, the continual increase would eventually lead to consistent high risk for short sleep in older adulthood. Within each racial/ethnic group, the trajectory was more prevalent among male participants than female participants except among Latinx participants. The higher prevalence among male participants in general may be explained by the poorer sleep hygiene (e.g., greater screen time and caffeine intake) among male participants observed in adolescent and adult studies (46, 47, 68–70). Between racial/ethnic groups, this trajectory was the most prevalent among Black participants, with the highest prevalence particularly among Black male respondents. This is in line with studies that have shown Black male participants were the most likely to have the shortest average sleep duration in both adolescent and adult populations (28, 30, 50, 52). This may be due to stress related to the persistent discrimination in Black male experience (e.g., police brutality and criminal profiling) throughout the life course (71–73). In addition, various sociocultural factors (e.g., masculine socialization, stigma, and lack of access to health care and economic resources) may prevent Black males from seeking and receiving support to help mitigate the harmful psychological effects of discrimination (74–76). The high prevalence of this sleep trajectory among Black male participants may contribute to the significant health disparities (77) among this group across the life span.
The second most common trajectory was late-onset short sleepers. A potential explanation for the healthy sleep duration from early adolescence to young adulthood is that these individuals may be in environments (e.g., higher household socioeconomic status, greater neighborhood safety, and social cohesion) that are more optimal for sleep (20, 78, 79). In adulthood, the increase in probability of short sleep duration may be explained by the growing responsibilities and demands, such as work and starting a family, that reduce the amount of time for sleep (15). Across all racial/ethnic groups, female respondents were more likely to have a late-onset short sleeper trajectory, with the greatest prevalence being among White female respondents. This may be attributed to family formation and gendered expectations that pressure them into being the primary caretaker of the family, allocating less time for sleep (33).
The early-onset short sleepers had the least common trajectory overall. The existence of this trajectory could be due to the sociocontextual changes that occur as people transition from early adolescence into later adolescence. These changes may include earlier school start times, academic pressure, and greater social commitments due to an expanding social network, all of which could prevent adolescents from obtaining a longer sleep duration (14, 80). As these individuals transition into adulthood and become free from early school start times, they may enter the workforce or attend college where there may have greater flexibility in tailoring their sleep schedule (81–83). Across race/ethnicity, this trajectory was generally more prevalent among female participants, except among Latinx individuals. The higher occurrence of this trajectory among female participants may be due to being pressured into more responsibilities than male youth during early adolescence (e.g., caretaking and chores) that reduce the amount of time for sleep (84). However, as these individuals transition into adulthood and seek greater independence, they often enter the workforce or attend postsecondary education, allowing them to relinquish some of these responsibilities (15, 85).
Within the trajectory types, Latinx male respondents had the most distinctive trajectories for early- and late-onset short sleepers. These findings for Latinx respondents could be due to the aggregating of Latinx subgroups—including Mexican Americans, Puerto Ricans, Central/South Americans, and Cubans—into a single classification. By doing so, the diverse sociocultural context of Hispanic subgroups (e.g., levels of acculturation and nativity) was not accounted for, and that could potentially have influenced their sleep duration throughout adolescence and adulthood (24, 86–89).
There are at least 3 strengths to this study. First, this is one of few studies to examine sleep duration trajectories from adolescence to adulthood, including an older adult assessment time point compared with prior trajectory studies (56, 57). Second, to our knowledge, this is one of the first studies to use an intersectionality approach to examine race/ethnicity and sex differences of sleep trajectories. Finally, this study included a large, diverse cohort, which increases the generalizability of the results.
These findings should be interpreted within the context of the limitations in this study. Intersectionality was limited to participants’ racial/ethnic and sex/gender identities and may not have captured the complex underlying social processes that produce these sleep disparities. While we acknowledge that there are more comprehensive approaches for intersectionality, the results from this study were intended to be the foundation for future intersectionality-driven research on sleep disparities (90). Another limitation is the potential measurement error of self-reported sleep duration. Studies have found that participants tend to overestimate their sleep duration when compared with objective measures (e.g., actigraphy), among both adolescents and adults (30, 91–96). Among adults, studies show that measurement error of sleep duration may vary by race/ethnicity and sex/gender (94–96). For instance, in a study with data from the Multi-Ethnic Study of Atherosclerosis comparing self-reported with actigraphy-assessed weekend sleep duration, White participants were more likely to overestimate their sleep duration than Black participants, and Black women were more likely to overestimate their sleep than Black men (95). It is currently unclear whether these differences in measurement error exists among adolescents. Racial/ethnic and sex/gender differences in the overestimation of sleep in both adolescence and adulthood may have led to racial/ethnic and sex/gender variations in the underestimation of the consistent increasing short sleeper trajectory type. Furthermore, sleep duration was assessed differently in waves I and V, which asked “How many hours of sleep do you usually get?” compared with waves III and IV, which asked for weekday and weekend sleep duration. The variation in measurement prevented this study from examining whether the results would have differed by weekend and weekday sleep duration. This may be important since adolescents and adults generally sleep less during the weekdays and more during the weekend (13, 97, 98). Since weekday sleep duration is weighted higher than weekend sleep duration in calculating average sleep duration per day, any changes in weekday sleep duration would more likely influence the trajectories than weekend sleep duration. Moreover, there was a higher proportion of long sleepers in waves III and IV, which could be due to the assessment capturing participants’ amount of time in bed instead of actual time asleep. This study was unable to assess changes in sleep duration trajectories among long sleepers, which is important since long sleep duration has been associated with poorer health outcomes. Finally, Add Health did not assess individual sleep need or sleep quality, precluding us from assessing how racial/ethnic and sex/gender differences may influence these important sleep characteristics.
In conclusion, our findings underscore the need to examine sleep within an intersectionality framework to advance sleep disparities research. The consequences of examining a single social identity may result in inaccurate documentation of sleep disparities and subsequently ineffective strategies to reduce these disparities. The findings further suggest that intervening as early as adolescence to prevent short sleep in adulthood would be particularly important given that a high proportion of the sample had an increasing likelihood of short sleep duration from early adolescence to adulthood. Given that the primary focus of this study was to describe racial/ethnic and sex/gender differences in sleep duration trajectories from adolescence to adulthood, future research should apply an intersectionality framework to examine pathways (e.g., health status, socioeconomic status, and discrimination) driving these differences and whether these trajectories are associated with health outcomes. These future studies will be important in developing more informed strategies to mitigate racial/ethnic and sex/gender sleep disparities and subsequently health disparities.
Supplementary Material
ACKNOWLEDGMENTS
Author affiliations: Department of Epidemiology, Rollins School of Public Health, Emory University, Atlanta, Georgia, United States (Ryan Saelee, Dayna A. Johnson, Julie A. Gazmararian, Shakira F. Suglia); and Department of Behavioral, Social, and Health Education Sciences, Rollins School of Public Health, Emory University, Atlanta, Georgia, United States (Regine Haardörfer).
This work was supported by the National Institutes of Health (grants T32HL130025, R01HL125761, and F31HL151126-01A1).
This research uses data from Add Health, a program project directed by Kathleen Mullan Harris and designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris at the University of North Carolina at Chapel Hill, and funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (grant P01-HD31921), with cooperative funding from 23 other federal agencies and foundations. No direct support was received from grant P01-HD31921 for this analysis. Information on how to obtain the Add Health data files is available on the Add Health website (https://addhealth.cpc.unc.edu/).
The views expressed in this article are those of the authors and do not reflect those of the National Institutes of Health.
Conflict of interest: none declared.
REFERENCES
- 1. Colten HR, Altevogt BM, eds. Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem. Washington, DC: National Academies Press; 2006. [PubMed] [Google Scholar]
- 2. Tarokh L, Saletin JM, Carskadon MA. Sleep in adolescence: physiology, cognition and mental health. Neurosci Biobehav Rev. 2016;70:182–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Paruthi S, Brooks LJ, D'Ambrosio C, et al. Consensus statement of the American Academy of Sleep Medicine on the recommended amount of sleep for healthy children: methodology and discussion. J Clin Sleep Med. 2016;12(11):1549–1561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Watson NF, Badr MS, Belenky G, et al. Recommended amount of sleep for a healthy adult: a Joint Consensus Statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep. 2015;38(6):843–844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Chaput JP, Gray CE, Poitras VJ, et al. Systematic review of the relationships between sleep duration and health indicators in school-aged children and youth. Appl Physiol Nutr Metab. 2016;41(6 suppl 3):S266–S282. [DOI] [PubMed] [Google Scholar]
- 6. Cooper CB, Neufeld EV, Dolezal BA, et al. Sleep deprivation and obesity in adults: a brief narrative review. BMJ Open Sport Exerc Med. 2018;4(1):e000392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wang Y, Mei H, Jiang Y-R, et al. Relationship between duration of sleep and hypertension in adults: a meta-analysis. J Clin Sleep Med. 2015;11(9):1047–1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Shan Z, Ma H, Xie M, et al. Sleep duration and risk of type 2 diabetes: a meta-analysis of prospective studies. Diabetes Care. 2015;38(3):529–537. [DOI] [PubMed] [Google Scholar]
- 9. Zhai L, Zhang H, Zhang D. Sleep duration and depression among adults: a meta-analysis of prospective studies. Depress Anxiety. 2015;32(9):664–670. [DOI] [PubMed] [Google Scholar]
- 10. Liu Y, Wheaton AG, Chapman DP, et al. Prevalence of healthy sleep duration among adults—United States, 2014. MMWR Morb Mortal Wkly Rep. 2016;65(6):137–141. [DOI] [PubMed] [Google Scholar]
- 11. Wheaton AG, Jones SE, Cooper AC, et al. Short sleep duration among middle school and high school students—United States, 2015. MMWR Morb Mortal Wkly Rep. 2018;67(3):85–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hagenauer MH, Perryman JI, Lee TM, et al. Adolescent changes in the homeostatic and circadian regulation of sleep. Dev Neurosci. 2009;31(4):276–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Carskadon MA. Sleep in adolescents: the perfect storm. Pediatr Clin North Am. 2011;58(3):637–647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wheaton AG, Chapman DP, Croft JB. School start times, sleep, behavioral, health, and academic outcomes: a review of the literature. J Sch Health. 2016;86(5):363–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lenz B. The transition from adolescence to young adulthood: a theoretical perspective. J Sch Nurs. 2001;17(6):300–306. [DOI] [PubMed] [Google Scholar]
- 16. Dunietz GL, Matos-Moreno A, Singer DC, et al. Later school start times: what informs parent support or opposition? J Clin Sleep Med. 2017;13(7):889–897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Johnson DA, Jackson CL, Williams NJ, et al. Are sleep patterns influenced by race/ethnicity—a marker of relative advantage or disadvantage? Evidence to date. Nat Sci Sleep. 2019;11:79–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Guglielmo D, Gazmararian JA, Chung J, et al. Racial/ethnic sleep disparities in US school-aged children and adolescents: a review of the literature. Sleep Health. 2018;4(1):68–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Williams DR, Mohammed SA. Discrimination and racial disparities in health: evidence and needed research. J Behav Med. 2009;32(1):20–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Billings ME, Hale L, Johnson DA. Physical and social environment relationship with sleep health and disorders. Chest. 2020;157(5):1304–1312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Grandner MA, Williams NJ, Knutson KL, et al. Sleep disparity, race/ethnicity, and socioeconomic position. Sleep Med. 2016;18:7–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Jackson CL, Redline S, Kawachi I, et al. Racial disparities in short sleep duration by occupation and industry. Am J Epidemiol. 2013;178(9):1442–1451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Martinez-Miller EE, Prather AA, Robinson WR, et al. US acculturation and poor sleep among an intergenerational cohort of adult Latinos in Sacramento, California. Sleep. 2019;42(3):zsy246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ghani SB, Delgadillo ME, Granados K, et al. Acculturation associated with sleep duration, sleep quality, and sleep disorders at the US-Mexico border. Int J Environ Res Public Health. 2020;17(19):7138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Johnson DA, Lisabeth L, Lewis TT, et al. The contribution of psychosocial stressors to sleep among African Americans in the Jackson Heart Study. Sleep. 2016;39(7):1411–1419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kim E-J, Dimsdale JE. The effect of psychosocial stress on sleep: a review of polysomnographic evidence. Behav Sleep Med. 2007;5(4):256–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Keyes KM, Maslowsky J, Hamilton A, et al. The great sleep recession: changes in sleep duration among US adolescents, 1991–2012. Pediatrics. 2015;135(3):460–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Maslowsky J, Ozer EJ. Developmental trends in sleep duration in adolescence and young adulthood: evidence from a national United States sample. J Adolesc Health. 2014;54(6):691–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. James S, Chang AM, Buxton OM, et al. Disparities in adolescent sleep health by sex and ethnoracial group. SSM Popul Health. 2020;11:100581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Matthews KA, Hall M, Dahl RE. Sleep in healthy Black and White adolescents. Pediatrics. 2014;133(5):e1189–e1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Moore M, Kirchner HL, Drotar D, et al. Correlates of adolescent sleep time and variability in sleep time: the role of individual and health related characteristics. Sleep Med. 2011;12(3):239–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Krueger PM, Friedman EM. Sleep duration in the United States: a cross-sectional population-based study. Am J Epidemiol. 2009;169(9):1052–1063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Burgard SA, Ailshire JA. Gender and time for sleep among U.S. adults. Am Sociol Rev. 2013;78(1):51–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Meers J, Stout-Aguilar J, Nowakowski S. Chapter 3: Sex differences in sleep health. In: Grandner MA, ed. Sleep and Health. Cambridge, MA: Academic Press; 2019:21–29. [Google Scholar]
- 35. Pengo MF, Won CH, Bourjeily G. Sleep in women across the life span. Chest. 2018;154(1):196–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Quinn MM, Smith PM. Gender, work, and health. Ann Work Expo Health. 2018;62(4):389–392. [DOI] [PubMed] [Google Scholar]
- 37. England P, Levine A, Mishel E. Progress toward gender equality in the United States has slowed or stalled. Proc Natl Acad Sci U S A. 2020;117(13):6990–6997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Hazel KL, Kleyman KS. Gender and sex inequalities: implications and resistance. J Prev Interv Community. 2020;48(4):281–292. [DOI] [PubMed] [Google Scholar]
- 39. Slopen N, Lewis TT, Williams DR. Discrimination and sleep: a systematic review. Sleep Med. 2016;18:88–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Buxton OM, Shea SA. Bidirectional relationships between sleep and work. Sleep Health. 2020;6(3):259–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Tifferet S. Gender differences in social support on social network sites: a meta-analysis. Cyberpsychol Behav Soc Netw. 2020;23(4):199–209. [DOI] [PubMed] [Google Scholar]
- 42. Reevy GM, Maslach C. Use of social support: gender and personality differences. Sex Roles. 2001;44(7):437–459. [Google Scholar]
- 43. Tamres LK, Janicki D, Helgeson VS. Sex differences in coping behavior: a meta-analytic review and an examination of relative coping. Pers Soc Psychol Rev. 2002;6(1):2–30. [Google Scholar]
- 44. Kent de Grey RG, Uchino BN, Trettevik R, et al. Social support and sleep: a meta-analysis. Health Psychol. 2018;37(8):787–798. [DOI] [PubMed] [Google Scholar]
- 45. Krause N, Rainville G. Exploring the relationship between social support and sleep. Health Educ Behav. 2020;47(1):153–161. [DOI] [PubMed] [Google Scholar]
- 46. Branum AM, Rossen LM, Schoendorf KC. Trends in caffeine intake among US children and adolescents. Pediatrics. 2014;133(3):386–393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Bucksch J, Sigmundova D, Hamrik Z, et al. International trends in adolescent screen-time behaviors from 2002 to 2010. J Adolesc Health. 2016;58(4):417–425. [DOI] [PubMed] [Google Scholar]
- 48. Bowleg L. The problem with the phrase “women and minorities”: intersectionality-an important theoretical framework for public health. Am J Public Health. 2012;102(7):1267–1273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Lauderdale DS, Knutson KL, Yan LL, et al. Objectively measured sleep characteristics among early-middle-aged adults: the CARDIA study. Am J Epidemiol. 2006;164(1):5–16. [DOI] [PubMed] [Google Scholar]
- 50. Chen X, Wang R, Zee P, et al. Racial/ethnic differences in sleep disturbances: the Multi-Ethnic Study of Atherosclerosis (MESA). Sleep. 2015;38(6):877–888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Reither EN, Krueger PM, Hale L, et al. Ethnic variation in the association between sleep and body mass among US adolescents. Int J Obes (Lond). 2014;38(7):944–949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Petrov ME, Long DL, Grandner MA, et al. Racial differences in sleep duration intersect with sex, socioeconomic status, and U.S. geographic region: the REGARDS study. Sleep Health. 2020;6(4):442–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Gangwisch JE, Malaspina D, Babiss LA, et al. Short sleep duration as a risk factor for hypercholesterolemia: analyses of the National Longitudinal Study of Adolescent Health. Sleep. 2010;33(7):956–961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Suglia SF, Kara S, Robinson WR. Sleep duration and obesity among adolescents transitioning to adulthood: do results differ by sex? J Pediatr. 2014;165(4):750–754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Krueger PM, Reither EN, Peppard PE, et al. Cumulative exposure to short sleep and body mass outcomes: a prospective study. J Sleep Res. 2015;24(6):629–638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Bakour C, Schwartz SW, Wang W, et al. Sleep duration patterns from adolescence to young adulthood and the risk of asthma. Ann Epidemiol. 2020;49:20–26. [DOI] [PubMed] [Google Scholar]
- 57. Kramer Fiala Machado A, Wendt A, Baptista Menezes AM, et al. Sleep duration trajectories from adolescence to emerging adulthood: findings from a population-based birth cohort. J Sleep Res. 2020;30(3):e13155. [DOI] [PubMed] [Google Scholar]
- 58. Hayley AC, Skogen JC, Overland S, et al. Trajectories and stability of self-reported short sleep duration from adolescence to adulthood. J Sleep Res. 2015;24(6):621–628. [DOI] [PubMed] [Google Scholar]
- 59. Harris KM, Halpern CT, Whitsel EA, et al. Cohort profile: the National Longitudinal Study of Adolescent to Adult Health (Add Health). Int J Epidemiol. 2019;48(5):1415-k. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Grandner MA, Drummond SP. Who are the long sleepers? Towards an understanding of the mortality relationship. Sleep Med Rev. 2007;11(5):341–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Carolina Population Center . Frequently asked questions. https://addhealth.cpc.unc.edu/documentation/frequently-asked-questions/. Accessed May 31, 2020.
- 62. Blum RW, Astone NM, Decker MR, et al. A conceptual framework for early adolescence: a platform for research. Int J Adolesc Med Health. 2014;26(3):321–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Arnett JJ. Emerging adulthood. A theory of development from the late teens through the twenties. Am Psychol. 2000;55(5):469–480. [PubMed] [Google Scholar]
- 64. Vespa J. The Changing Economics and Demographics of Young Adulthood: 1975–2016. Suitland, MD: US Census Bureau; 2017. [Google Scholar]
- 65. Nylund KL, Asparouhov T, Muthén BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: a Monte Carlo simulation study. Struct Equ Model Multidiscip J. 2007;14(4):535–569. [Google Scholar]
- 66. Muthén LK, Muthén BO. Mplus Statistical Analysis With Latent Variables: User’s Guide. 8th ed. Los Angeles, CA: Muthén and Muthén; 2017. [Google Scholar]
- 67. Allison PD. Missing data techniques for structural equation modeling. J Abnorm Psychol. 2003;112(4):545–557. [DOI] [PubMed] [Google Scholar]
- 68. Ruggiero AR, Peach HD, Gaultney JF. Association of sleep attitudes with sleep hygiene, duration, and quality: a survey exploration of the moderating effect of age, gender, race, and perceived socioeconomic status. Health Psychol Behav Med. 2019;7(1):19–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Yang L, Cao C, Kantor ED, et al. Trends in sedentary behavior among the US population, 2001–2016. JAMA. 2019;321(16):1587–1597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Drewnowski A, Rehm CD. Sources of caffeine in diets of US children and adults: trends by beverage type and purchase location. Nutrients. 2016;8(3):154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Edwards F, Lee H, Esposito M. Risk of being killed by police use of force in the United States by age, race–ethnicity, and sex. Proc Natl Acad Sci. 2019;116(34):16793–16798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Kwate NO, Goodman MS. Racism at the intersections: gender and socioeconomic differences in the experience of racism among African Americans. Am J Orthopsychiatry. 2015;85(5):397–408. [DOI] [PubMed] [Google Scholar]
- 73. McLeod MN, Heller D, Manze MG, et al. Police interactions and the mental health of Black Americans: a systematic review. J Racial Ethn Health Disparities. 2020;7(1):10–27. [DOI] [PubMed] [Google Scholar]
- 74. Watkins DC, Walker RL, Griffith DM. A meta-study of Black male mental health and well-being. J Black Psychol. 2009;36(3):303–330. [Google Scholar]
- 75. Lindsey MA, Marcell AV. "We're going through a lot of struggles that people don't even know about": the need to understand African American males' help-seeking for mental health on multiple levels. Am J Mens Health. 2012;6(5):354–364. [DOI] [PubMed] [Google Scholar]
- 76. Lindsey MA, Korr WS, Broitman M, et al. Help-seeking behaviors and depression among African American adolescent boys. Soc Work. 2006;51(1):49–58. [DOI] [PubMed] [Google Scholar]
- 77. Jones NL, Gilman SE, Cheng TL, et al. Life course approaches to the causes of health disparities. Am J Public Health. 2019;109(S1):S48–S55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Felden ÉPG, Leite CR, Rebelatto CF, et al. Sleep in adolescents of different socioeconomic status: a systematic review. Revista Paulista de Pediatria (English Edition). 2015;33(4):467–473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Hale L, James S. Sociodemographic, psychosocial, and contextual factors in Children’s sleep. In: McHale SM, King V, Buxton OM, eds. Family Contexts of Sleep and Health Across the Life Course.Berlin, Germany: Springer; 2017;153–173. [Google Scholar]
- 80. Crowley SJ, Wolfson AR, Tarokh L, et al. An update on adolescent sleep: new evidence informing the perfect storm model. J Adolesc. 2018;67(1):55–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Moen P, Kelly EL, Tranby E, et al. Changing work, changing health: can real work-time flexibility promote health behaviors and well-being? J Health Soc Behav. 2011;52(4):404–429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Olson R, Crain TL, Bodner TE, et al. A workplace intervention improves sleep: results from the randomized controlled Work, Family, and Health Study. Sleep Health. 2015;1(1):55–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Zimmermann LK. Chronotype and the transition to college life. Chronobiol Int. 2011;28(10):904–910. [DOI] [PubMed] [Google Scholar]
- 84. East PL. Children's provision of family caregiving: benefit or burden? Child Dev Perspect. 2010;4(1):55–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Aronson P. The markers and meanings of growing up: contemporary young Women's transition from adolescence to adulthood. Gend Soc. 2008;22(1):56–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Hale L, Rivero-Fuentes E. Negative acculturation in sleep duration among Mexican immigrants and Mexican Americans. J Immigr Minor Health. 2011;13(2):402–407. [DOI] [PubMed] [Google Scholar]
- 87. Miguez MJ, Bueno D, Perez C. Disparities in sleep health among adolescents: the role of sex, age, and migration. Sleep Disorders. 2020;2020:5316364–5316366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Patel SR, Sotres-Alvarez D, Castañeda SF, et al. Social and health correlates of sleep duration in a US Hispanic population: results from the Hispanic Community Health Study/Study of Latinos. Sleep. 2015;38(10):1515–1522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Ebin VJ, Sneed CD, Morisky DE, et al. Acculturation and interrelationships between problem and health-promoting behaviors among Latino adolescents. J Adolesc Health. 2001;28(1):62–72. [DOI] [PubMed] [Google Scholar]
- 90. Bauer GR, Churchill SM, Mahendran M, et al. Intersectionality in quantitative research: a systematic review of its emergence and applications of theory and methods. SSM - Population Health. 2021;14:100798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Wolfson AR, Carskadon MA, Acebo C, et al. Evidence for the validity of a sleep habits survey for adolescents. Sleep. 2003;26(2):213–216. [DOI] [PubMed] [Google Scholar]
- 92. Arora T, Broglia E, Pushpakumar D, et al. An investigation into the strength of the association and agreement levels between subjective and objective sleep duration in adolescents. PloS One. 2013;8(8):e72406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Matthews KA, Patel SR, Pantesco EJ, et al. Similarities and differences in estimates of sleep duration by polysomnography, actigraphy, diary, and self-reported habitual sleep in a community sample. Sleep Health. 2018;4(1):96–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Cespedes EM, Hu FB, Redline S, et al. Comparison of self-reported sleep duration with Actigraphy: results from the Hispanic Community Health Study/Study of Latinos Sueño Ancillary Study. Am J Epidemiol. 2016;183(6):561–573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Jackson CL, Patel SR, Jackson WB, et al. Agreement between self-reported and objectively measured sleep duration among white, black, Hispanic, and Chinese adults in the United States: Multi-Ethnic Study of Atherosclerosis. Sleep. 2018;41(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Lauderdale DS, Knutson KL, Yan LL, et al. Self-reported and measured sleep duration: how similar are they? Epidemiology. 2008;19(6):838–845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Hale L. Who has time to sleep? J Public Health (Oxf). 2005;27(2):205–211. [DOI] [PubMed] [Google Scholar]
- 98. Monk TH, Buysse DJ, Rose LR, et al. The sleep of healthy people—a diary study. Chronobiol Int. 2000;17(1):49–60. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


