Abstract
Background and objectives
Overutilization of phlebotomy tubes at healthcare facilities leads to iatrogenic anemia, patient dissatisfaction, and increase in operational costs. In this study, we analyzed the phlebotomy tube usage data at the Zhongshan Hospital, Fudan University, to show potential inefficiencies with phlebotomy tube usage.
Methods
Data of 984,078 patients with 1,408,175 orders and 4,622,349 total phlebotomy tubes were collected during years 2018–2021. Data of different patient types were compared. Furthermore, we assessed the data from subspecialty and test levels to explore the factors influencing the increase in phlebotomy tube usage.
Results
We observed an overall 8% increase in both the mean number of tubes used and blood loss per order over the past 4 years. The mean blood loss per day for intensive care unit (ICU) patients was 18.7 ml (maximum 121.6 ml), which was well under the 200 ml/day threshold. However, the maximum number of tubes used reached more than 30 tubes/day.
Conclusions
The 8% increase of phlebotomy tubes over 4 years should alarm laboratory managements, as tests offered are expected to increase in the future. Importantly, the whole healthcare community needs to work together to solve this problem with more creative solutions.
Keywords: Phlebotomy tube utilization, Iatrogenic anemia, Laboratory management, Laboratory test utilization
1. Introduction
The vast number of phlebotomy tubes used at healthcare facilities have caused serious concerns among medical practitioners and hospital management. Due to the recent phlebotomy tube shortage, Jackups Jr. et al. highlighted the inefficiency with the current utilization of phlebotomy tubes at clinical laboratories [1]. Similarly, Loh et al. have also discussed the concern of inefficient phlebotomy tube usage at healthcare facilities [2]. Importantly, overutilization of blood tubes can lead to patient dissatisfaction, nosocomial or iatrogenic anemia in newborns and intensive care unit (ICU) patients, increasing need for unnecessary blood transfusion [3,4], test unavailability, excessive operative cost, and damage to the environment. Therefore, minimizing the number of phlebotomy tubes used at healthcare facilities is crucial.
In recent years, since more clinical laboratory tests have been developed, we speculate the number of phlebotomy tubes used has also increased. However, since the study on extra blood tubes by Loh et al. [2] in 2010, few articles have discussed the current status of phlebotomy tube usage at hospitals or other healthcare facilities. A majority of publications, including the report by Wisser et al. [5], have focused on the blood loss due to phlebotomy, which only indirectly reflects the extra phlebotomy tube utilization. The lack of information on phlebotomy tube usage has kept the overutilization of phlebotomy tubes hidden for many years until the shortage of tube supply. Understanding the current situation is crucial for persuading hospital managements to act and bring forth practical measures to counter the problem.
To characterize the current status of phlebotomy tube usage, understand the reasons for increased usage, and identify potential inefficiencies, in this study, we analyzed phlebotomy tube usage at the Zhongshan Hospital, at the Fudan University. We also included blood loss analysis to provide a holistic overview of the problem.
2. Materials and methods
2.1. Sample collection
We collected test ordering data from the Zhongshan Hospital, at Fudan University from 2018 to 2021. Due to the large size of the dataset, we only used the fourth quarter (October to December) data from each year. These four quarters were ideal representations of regular workload and were not affected by major events such as the coronavirus disease 2019 (COVID-19) shutdowns. Using only fourth quarter data might distort the number of patients visiting the hospital and the total phlebotomy tube usage due to a seasonal effect. However, in this study, we focused more on the tube usage statistics on the patient level, which are less likely to be affected by seasonal effects. Additionally, we did not use random sampling due to the highly skewed distribution of number of phlebotomy tubes usage per patient per each order. Random sampling could underestimate the right tail of the distribution and left the true maximum and data beyond 97.5th percentile out of our analysis. In total, data from a total of 984,078 patients with 1,408,175 orders and 4,622,349 total phlebotomy tubes were collected from the laboratory information system (LIS). Here, an order is the collection of all tests ordered by a physician at one time for a patient. Zhongshan Hospital is a major tertiary hospital with comprehensive medical specialties located in Shanghai, China. The annual tests reported at the Department of Laboratory Medicine of Zhongshan Hospital surpassed 100, 000, 000 in 2020 with over 400 types of tests offered.
2.2. Subcategory and test-combine-rules
The phlebotomy tube utilization was determined by test subcategories and test-combine-rules at the Zhongshan Hospital. The tests performed on an instrument were put into one subcategory such as routine blood or general chemistry tests. Subsequently, based on phlebotomy tube requirements, workflow, and turn-around-time (TAT) requirements, test-combine-rules were generated to combine different subcategories into one phlebotomy tube by an experienced laboratory division manager. The subcategories were given a specialized token in the LIS for the ordering system to work based on the test-combine-rules.
2.3. Phlebotomy tubes and blood volume
There are six major types of phlebotomy tubes with different nominal volumes that were used. The blood volume estimation described in the results section consisted of the sum of the nominal volumes of the respective phlebotomy tubes. However, similar to the study by Wisser et al. [3], blood volumes drawn were an overestimation and in practice, the actual volumes were most likely smaller.
2.4. Statistical analysis
All data analyses were performed in R statistical programming language. Since the number of tubes used and blood loss per patient could be highly skewed, median, 95th percentile, and maximum values were reported. The trimmed means with 1% truncation were also reported to show the changing trend over the past 4 years without having been affected by the outliers.
3. Results
3.1. Statistics according to patient types
Table 1 shows the statistics for tube usage and blood loss due to phlebotomy from year 2018–2021. The total number of patients visiting the Zhongshan Hospital increased from 206,706 to 286,861 (38.8% increase) and the total phlebotomy tubes used also increased from 959,564 to 1,387,905 (44.6% increase) over the 3-month period across the 4 years. Despite the relatively large growth rate seen in patients and the number of tubes used, the mean number of tubes used per order and the mean blood loss per order both grew at about 8%. Similar trends were observed for different patient types. Among the four major types of patients who visited the hospital, the most tubes per order were used on inpatients and ICU patients followed by emergency patients and outpatients. For inpatients and ICU patients, the 95% percentiles for blood loss were all less than 50 ml in one order as there were huge increases from 2020 to 2021; the maximum blood losses were all around 100 ml in one order.
Table 1.
Statistics for tube usage and blood loss due to phlebotomy from 2018 to 2021.
| Patient Type | Year | Patient No. | Order No. | Tube No. | No. Of Tubes per Order |
Blood Loss per Order (ml) |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | Median | 95th Percentile | Max | Mean | Median | 95th Percentile | Max | |||||
| All Patients | 2018 | 206,706 | 303,243 | 959,564 | 3.08 | 3 | 8 | 22 | 12.2 | 10 | 30 | 106 |
| 2019 | 240,332 | 343,352 | 1,084,054 | 3.07 | 3 | 7 | 25 | 12.1 | 10 | 28.7 | 106.7 | |
| 2020 | 250,179 | 358,503 | 1,190,826 | 3.24 | 3 | 8 | 24 | 12.9 | 12 | 30 | 108 | |
| 2021 | 286,861 | 403,077 | 1,387,905 | 3.34 | 3 | 8 | 27 | 13.3 | 12 | 31.7 | 118.7 | |
| Emergency | 2018 | 25,475 | 30,086 | 84,869 | 2.80 | 3 | 5 | 12 | 10.4 | 12 | 18.7 | 50.7 |
| 2019 | 26,540 | 32,536 | 95,410 | 2.91 | 3 | 5 | 12 | 10.9 | 12 | 18.7 | 51 | |
| 2020 | 24,787 | 29,013 | 94,222 | 3.23 | 3 | 5 | 14 | 12.3 | 12 | 18.7 | 69 | |
| 2021 | 30,058 | 34,612 | 112,891 | 3.25 | 3 | 5 | 15 | 12.3 | 12.7 | 18.7 | 68 | |
| ICU | 2018 | 2753 | 14,683 | 59,567 | 3.97 | 4 | 8 | 22 | 15.2 | 14.7 | 31 | 89.7 |
| 2019 | 2939 | 15,974 | 64,278 | 3.94 | 4 | 8 | 23 | 14.9 | 14.7 | 29.7 | 90.7 | |
| 2020 | 2890 | 17,491 | 71,321 | 3.98 | 4 | 8 | 24 | 15.5 | 14.7 | 33.7 | 105.7 | |
| 2021 | 3314 | 19,069 | 80,131 | 4.10 | 4 | 9 | 27 | 16.2 | 14.7 | 36 | 115.4 | |
| Inpatient | 2018 | 32,476 | 98,423 | 425,046 | 4.24 | 4 | 10 | 22 | 16.4 | 14.7 | 41 | 106 |
| 2019 | 35,698 | 103,954 | 455,443 | 4.30 | 4 | 10 | 25 | 16.5 | 14.7 | 40.7 | 106.7 | |
| 2020 | 37,272 | 110,669 | 497,770 | 4.42 | 4 | 11 | 23 | 17.1 | 14.7 | 42.7 | 108 | |
| 2021 | 39,641 | 117,395 | 566,631 | 4.73 | 4 | 12 | 26 | 18.4 | 14.7 | 48.1 | 112.7 | |
| Outpatient | 2018 | 148,658 | 160,070 | 390,082 | 2.40 | 2 | 5 | 16 | 9.9 | 10 | 22 | 81.4 |
| 2019 | 178,083 | 190,920 | 468,923 | 2.41 | 2 | 5 | 17 | 9.9 | 10 | 22 | 77.4 | |
| 2020 | 187,920 | 201,390 | 527,513 | 2.57 | 2 | 6 | 19 | 10.6 | 10 | 24 | 90.4 | |
| 2021 | 216,910 | 232,040 | 628,252 | 2.65 | 2 | 6 | 23 | 10.9 | 10 | 25 | 97.4 | |
Note: Mean were calculated as the trimmed average with a truncation ratio of 1%.
Table 2 contains data from hospitalized patients for the duration of their stay at the hospital. The mean hospital stays of ICU patients drastically decreased from 13 to 7 days in 4 years, due to a quality initiative at Zhongshan Hospital intend to reduce hospital stay time for surgical patients. This, combined with a minor increase in mean tube usage, has led to a 60% increase in tube usage as well as blood loss per day in ICU patients from 2018 to 2021. For inpatients, the mean tube usage and blood loss decreased in 2019 and 2020, but the trend has since reversed in 2021 and both the mean tube usage and blood loss have grown back to similar levels as was in 2018.
Table 2.
Statistics for tube usage and blood loss due to phlebotomy for ICU and inpatient patients during hospital stay from 2018 to 2021.
| Patient Type |
ICU |
Inpatient |
||||||
|---|---|---|---|---|---|---|---|---|
| Year | 2018 | 2019 | 2020 | 2021 | 2018 | 2019 | 2020 | 2021 |
| Patient Number |
2753 |
2939 |
2890 |
3314 |
39,641 |
32,476 |
35,698 |
37,272 |
|
Hospital Stays (days) | ||||||||
| Mean | 13.0 | 9.1 | 8.0 | 7.2 | 10.3 | 13.2 | 13.3 | 10.4 |
| Median | 9.5 | 6.2 | 4.6 | 4.8 | 3.6 | 6.0 | 6.0 | 4.0 |
| 95% Percentile | 77.1 | 90.5 | 92.0 | 88.0 | 95.9 | 81.8 | 91.7 | 119.8 |
| Maximum |
42.0 |
26.0 |
28.6 |
23.0 |
56.0 |
55.2 |
57.2 |
55.0 |
|
No. Of Tubes per Patient | ||||||||
| Mean | 19.6 | 19.6 | 21.7 | 21.7 | 13.8 | 12.7 | 12.3 | 12.9 |
| Median | 12 | 11 | 12 | 13 | 10 | 10 | 9 | 10 |
| 95% Percentile | 77.4 | 75.1 | 87 | 84 | 37 | 33 | 32 | 34 |
| Maximum | 582 | 370 | 578 | 545 | 175 | 201 | 204 | 173 |
| Mean per Day | 3.9 | 3.8 | 4.6 | 4.8 | 2.4 | 2.3 | 2.8 | 3.2 |
| Median Per Day | 2.5 | 2.5 | 4.3 | 4.0 | 1.7 | 1.6 | 2.2 | 2.6 |
| 95% Percentile per Day | 11.6 | 11.1 | 11.7 | 12.8 | 7.6 | 7.0 | 7.8 | 8.9 |
| Maximum per Day |
26.3 |
26.7 |
27.8 |
30.5 |
34.6 |
32.3 |
24.5 |
31.2 |
|
Blood Loss per Patient (ml) | ||||||||
| Mean | 75.0 | 74.5 | 84.5 | 86.0 | 53.8 | 49.3 | 47.5 | 49.9 |
| Median | 46.7 | 43.4 | 46.8 | 49.4 | 39.4 | 38.7 | 36.4 | 38.4 |
| 95% Percentile | 291.9 | 284.4 | 342.8 | 330.6 | 148.3 | 126.5 | 125.9 | 134.5 |
| Maximum | 2202.7 | 1417.2 | 2300.1 | 2335.7 | 745.9 | 739.1 | 685.0 | 630.1 |
| Mean per Day | 14.7 | 14.5 | 17.9 | 18.7 | 9.5 | 8.9 | 10.8 | 12.5 |
| Median Per Day | 9.8 | 9.6 | 16.4 | 15.6 | 6.6 | 6.2 | 8.3 | 9.9 |
| 95% Percentile per Day | 44.7 | 43.4 | 45.7 | 50.2 | 30.5 | 27.9 | 31.6 | 35.4 |
| Maximum per Day |
100.5 |
98.4 |
107.9 |
121.6 |
158.3 |
139.4 |
110.9 |
130.8 |
|
No. Tubes on the First Order | ||||||||
| Mean | 6.3 | 6.0 | 6.4 | 7.0 | 6.8 | 6.4 | 6.8 | 7.4 |
| Median | 5 | 5 | 5 | 6 | 6 | 6 | 6 | 7 |
| 95% Percentile | 14 | 12 | 14 | 14 | 12 | 12 | 12 | 16 |
| Maximum |
22 |
21 |
21 |
23 |
22 |
25 |
23 |
26 |
|
Blood Loss on the First Order (ml) | ||||||||
| Mean | 25.2 | 23.8 | 25.6 | 28.7 | 26.9 | 25.0 | 26.3 | 29.1 |
| Median | 18.7 | 19.7 | 20.7 | 23.7 | 24.7 | 21.7 | 23.7 | 25.7 |
| 95% Percentile | 58.05 | 48.74 | 56.4 | 60.7 | 50.7 | 49.7 | 50.7 | 67.7 |
| Maximum | 89.7 | 90.7 | 92.1 | 100.8 | 95.7 | 106.7 | 104.7 | 112.7 |
Note: Mean were calculated as the trimmed average with a truncation ratio of 1%.
Physicians usually assess a patient's overall condition with a comprehensive set of tests when a patient is admitted to the hospital. Therefore, the number of tubes per patient on the first order can be much higher than that on subsequent orders. We should pay extra attention to those orders to avoid acute blood loss or anemia in critical patients. Table 2 shows the tube usage and blood loss for inpatients and ICU patients on the first order. The number of tubes sampled for the first order consisted of approximately one third of the total tubes used for ICU patients and about half of the total tubes used for inpatients. The maximum number of tubes drawn on the first order reached as high as 26 tubes per order and the highest blood loss was 112.7 ml. Noticeably, the trend of growth is similar to the overall trend for hospitalized patients on the first order.
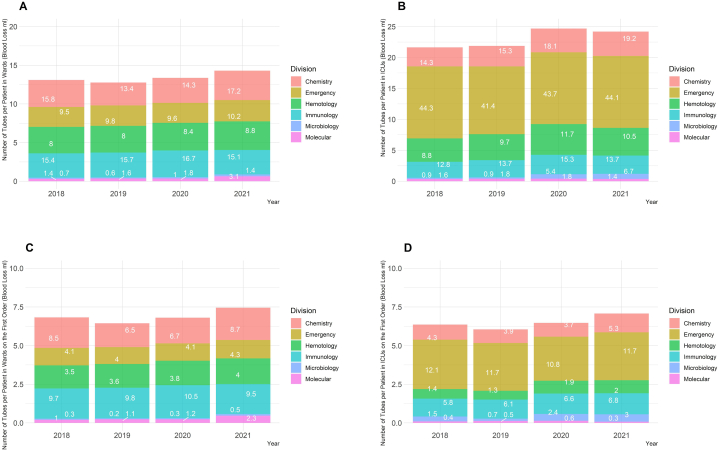
3.2. Statistics according to laboratory subspecialties
In a clinical laboratory, divisions based on laboratory subspecialty were often created to specialize on tests based on different testing methodology. At the Zhongshan Hospital, there are six major divisions that specialize in different tests, including Chemistry, Hematology, Immunology, Microbiology, Molecular, and Emergency. In Fig. 1, the stacked bars show the number of tubes assigned to each division per patient and the label shows the associated volume of blood drawn from hospitalized patients. Fig. 1A and B show the number of tubes used for the patient's entire stay and Fig. 1C and D show the number of tubes used on the first order. For inpatients, clinical chemistry and immunology tests contributed to about half of the total tube usage and blood loss. Tests from the Emergency and Hematology division were also major contributors to tube usage. Although the molecular tests only contributed a small fraction of the total tube usage and blood loss, the number of molecular tests doubled over four years for inpatients. As for ICU patients, the tubes assigned to the Emergency division consisted of more than half of the total tube usage and blood loss as the ICU tests generally require faster TATs than other hospitalized patients. Since year 2019 the number of tubes assigned to each division per patient has increased consistently. Noticeably, the number of tubes assigned to Microbiology has drastically increased since year 2019.
Fig. 1.
Number of phlebotomy tubes and blood volume assigned to each division. (A) Number of tubes per patient in wards during the entire stay. (B) Number of tubes per patient in ICUs during the entire stay. (C) Number of tubes per patient in wards on the first order. (D) Number of tubes per patient in ICUs on the first order. The respective blood loss was labeled on each bar.
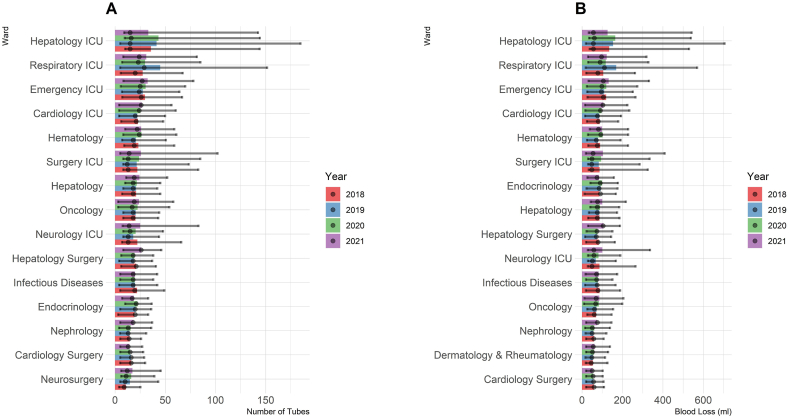
3.3. Statistics by specialties for hospitalized patients
The number of tests ordered by different specialty departments varied greatly. Fig. 2 shows the wards that collected the most tubes (Fig. 2A) and blood (Fig. 2B) during the entire hospital stay of patients. The bars represent the mean number of tubes and mean volume of blood collected. Median, 5th percentiles, and 95th percentiles are indicated by the overlaying dots and whiskers. The ICUs collected the most tubes and blood. The Hepatology ICU, Respiratory ICU, Emergency ICU, and Cardiology ICU were top four in both number of tubes used and blood collected per patient. Hepatology, Oncology, Infectious Diseases, and Endocrinology were among the top of the non-ICU hospitalized departments. Further, most of the wards showed upward trends in tube usage and blood collection.
Fig. 2.
Top 15 wards with highest phlebotomy tube usage and blood loss per patient from 2018 to 2021. (A) The number of tubes per patient in each ward. (B) The blood loss per patient in each ward. The dots represent the median, while the whiskers represent the 5th and 95th percentiles.
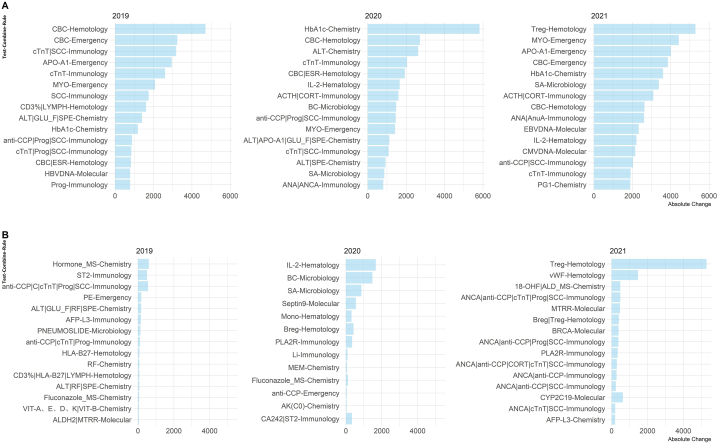
3.4. Source of growth
Fig. 3 shows the top 15 test-combine-rules for phlebotomy tube that have been increasing the most each year since 2019 for hospitalized patients. For subcategories that contain multiple tests, the subcategory tokens have been replaced with the abbreviation of the test category or a representative test to help with the interpretation. For example, the “CBC” represents the entire complete blood count tests, the “ALT” represents all regular chemistry tests. Subcategories that contain only one test such as hemoglobin A1c (HbA1c) and hepatitis C virus (HCV) RNA were represented directly with the test abbreviation. With the test-combine rules, the subcategories can be grouped together into one phlebotomy tubes to reduce blood tube usage. For example, “ALT|GLU_F|SPE-Chemistry” in Fig. 3 refers to a test-combine-rules that have all routine chemistry tests, fasting glucose, and serum protein electrophoresis share the blood sample from one test tube. Fig. 3A shows the top 15 rules with the highest absolute change while Fig. 3B shows the top 15 rules with the highest percentage change. The rules with the highest absolute change consisted of most routine tests such as the complete blood count and general chemistry tests. Those changes were caused by an increase in patients admitted over the past 4 years. The tests mentioned in Fig. 3B consisted of mostly novel tests such as the mass spectrometry tests (“Hormone_MS”) and next generation sequencing tests for cancer.
Fig. 3.
Test-combine-rules with the highest absolute and percentage increase from 2018 to 2021. (A) The test-combine-rules with the highest absolute increase. (B) The test-combine-rules with the highest percentage increase, but the bar shows the absolute increase for easier interpretation. CBC: complete blood count; ALT: alanine aminotransferase; cTNT: Cardiac Troponin T; SCC: squamous cell carcinoma; APO-A1: Apolipoprotein A1; MYO: myoglobin; LYMPH: lymphocyte count; GLU_F: fasting glucose; SPE: serum protein electrophoresis; HbA1c: hemoglobin A1c; anti-CPP: cyclic citrullinated peptide antibody; progesterone; ESR: erythrocyte sedimentation rate; HBVDNA: hepatitis B virus DNA; MS: mass spectrometry; ST2: soluble interleukin 1 receptor-like 1; HLA-B27: human leukocyte antigen B27; RF: rheumatoid factors; AFP-L3: alpha-fetoprotein L3; IL-2: interleukin-2; ACTH: adrenocorticotropic hormone; CORT: cortisol; BC: bacteria culture; SA: antibiotic sensitivity; ANA: antinuclear antibodies; ANCA: antineutrophil cytoplasmic antibodies; Mono: mononucleosis; Breg: regulatory B cells; Treg: regulatory T cells; PLA2R: Anti-phospholipase A2 receptor; Li: lithium; MEM: membrane permeability; AK(C0): amikacin concentration; CA242: carbohydrate antigen 24–2; CMVDNA: Cytomegalovirus DNA; PG1: pepsinogen 1; vWF: on Willebrand factor antigen; 18-OHF: 18-hydroxycortisol; ALD: aldosterone.
4. Discussion
In this study, we demonstrated that phlebotomy tube usage at a large tertiary hospital has been previously overlooked. The total number of phlebotomy tubes used in 3 months span at the Zhongshan Hospital increased from less than 1 million to almost 1.4 million tubes (45% increase) in the past 4 years. Although the number of patients treated also grew from about 200,000 to 280,000 (39% increase), the mean number of tubes collected per patient on each order had grown by about 8% from 2018 to 2021. Novel tests such as genetic cancer biomarkers, mass spectrometry tests, and pathogen tests were the main driving forces for the increase in the number of tubes used per patient. The growth rate of blood tube per patient should be a concern for laboratory managers worldwide.
Previous studies have focused on the blood loss due to phlebotomy that might cause nosocomial anemia for critically ill and neonatal patients. The first report of the issue of excessive usage of phlebotomy tubes dates back to the year 1973 when Eyster and Bernene published their findings [6]. Later, the article published by Smoller et al. [7] and the editorial by Burnum [8] raised the same issue to the entire medical community. Recent studies by Halpern et al. [3] and Beverina et al. [4], also demonstrated that excessive blood drawn can lead to an increasing need for unnecessary blood transfusion. Since then, many efforts have been made to reduce the amount of blood collected for phlebotomy. Most notably, the use of pediatric or other small volume tubes has had the biggest impact on resolving the issue [9]. According to a recent meta-analysis by Helmer et al. that was based on 29 observational and nine interventional studies, replacing phlebotomy tubes for pediatric patients or usage of other smaller tubes significantly reduced the daily blood loss in ICU patients [10]. Generally, shifting to smaller tubes can effectively reduce the daily blood loss from about 30 to 15 ml per day [10]. At Zhongshan Hospital, we have implemented smaller volume tubes in 2008, since then the blood loss has not been an issue for our patients. In our data, the blood loss was not found to be a significant problem for most patients. Even for critically ill patients in the ICU, the maximum blood drawn per day was less than 150 ml and the 95th percentile for blood loss per day was about 50 ml, which was much lower than the 200-ml criteria used in previous studies [5]. However, to collect over 100 ml of blood would require more than 20 phlebotomy tubes.
Although the volume for blood loss can be reduced by replacing larger tubes with smaller tubes, the number of phlebotomy tubes used for the sampling stays the same. This issue has been overlooked until recent shortages of phlebotomy tube supply in many laboratories worldwide that ran out of necessary tubes for routine tests. Both the College of American Pathologists and the US Food and Drug Administration have published recommendations for mitigating such a shortage in future [11,12].
Although the shortage mostly involved the sodium citrate tubes, it is still a good practice for hospitals and clinical laboratories to minimize the utilization of tubes for several reasons besides reducing blood loss. Firstly, excessive numbers of tubes incur huge operational costs for laboratories and hospitals that include ordering, stocking, and waste management of the tubes [2]. Secondly, using many tubes during phlebotomy could lead to low patient satisfaction. We have received several complaints from the patients due to the large number of tubes used during phlebotomy, making us recognize the issue long before the tube shortage. Finally, the massive number of phlebotomy tubes used can cause huge environmental impacts. A study by Lee et al. has shown that the phlebotomy tubes contribute up to 70% and 19% of plastic waste from all laboratories and hospitals, respectively [13]. Due to biosafety regulations, all the plastic waste from phlebotomy tubes cannot be recycled and must be incinerated, causing additional emission of greenhouse gases and pollution [14].
There are several reasons that might cause overutilization of phlebotomy tubes. Importantly, utilization of phlebotomy tubes can be affected by workflow and other operational issues. For example, TAT requirements force laboratory managers to run tests in separate tubes that could be combined together. Another example would be physical separation of testing locations. The Hematology and Chemistry division at the Zhongshan Hospital were at two separate locations on the campus. The tests conducted at the two divisions would be impossible to combined into one tube. Therefore, the workflow related problems are usually difficult to solve and reducing tube usage can involve trade-offs with other important quality indicators or may require significant workflow changes.
Overutilization of blood tubes can be caused by inefficiencies at the laboratories or hospitals. Studies have shown that the problem of unnecessary tube usage was a common issue at healthcare facilities. The “rainbow” of tubes can cause massive waste if not managed properly [15]. Improper phlebotomy procedures could also lead to wastage of tubes due to hemolysis, mislabeling, and other phlebotomy failures. More importantly, overutilization and underutilization of laboratory tests by physicians could also generate waste blood samples. Jackups Jr. et al. provided a practical approach and reasons to reduce the use of the sodium citrate tube by implementing an order alert for physicians with clinical decision support systems to not order prothrombin time (PT)/partial thromboplastin time (PTT) for screening tests. This effort reduced the utilization for international normalized ratio (INR) and PTT tests by 18% and 21%, respectively after 6 weeks [1]. However, a study by Sarkar et al. showed that underutilization of laboratory tests was more common and could also lead to phlebotomy tube waste [16]. If the most informative tests were not performed initially, the physicians may have to order more unrelated tests to determine the patient's conditions and order the missed test later. In general, the unnecessary usage of tubes caused by inefficiencies in laboratories and clinics can be effectively reduced by training, communication, and using electronic systems.
Another driving force for an increase in blood tube usage is the introduction of novel tests. From our results, we can see a clear pattern of growth of newly developed tests. Pathogen specific tests for surgery patients have contributed to the doubling of the tubes assigned to the Molecular and Microbiology divisions for patients in wards and ICUs. Tests such as hepatitis B virus (HBV) DNA, cytomegalovirus (CMV) DNA, Epstein-Barr virus (EBV) DNA, and antibiotic sensitivity all have had growth rates higher than the overall average growth rate. In recent years, regulations for the use of antibiotics have forced more and more pathogen tests to be performed before administration. The philosophy of precision medicine encourages the use of omics information on cancer diagnosis and treatment guidance. In our data, genetic tests such as BRCA and SEPTIN9 tests have also been growing faster than the average growth rate. Mass spectrometry tests can improve the quality of care at the hospital by providing more accurate test results and tests that were previously unavailable by chemistry or immunological methods. In the future, more tests should be available commercially for patients and physicians to improve the quality of care. Therefore, to keep the blood tube usage under control, when an additional test is prescribed, the laboratory management should carefully design the test-combine-rule and remove the possibility of redundant tests.
Our study has a major limitation. The results of the study do not provide methodology to solve the issue. As mentioned earlier, we had recognized the problem in year 2019, when we received several complaints from patients on the massive number of tubes used during phlebotomy. We ask our management team to brainstorm new test-combine-rules to reduce phlebotomy tube usage. Of all the possible rules, combining routine biochemistry tests with serum protein electrophoresis was the most effective, reducing approximately 2000 tubes per week. However, this improvement also caused a significant workflow redesign for our biochemistry department. Our corrective measures slightly reduced the mean number of tubes per patient from 2018 to 2019. In the future, we plan to describe our efforts in reducing the number of phlebotomy tubes by optimizing the test-combine-rules in more detail. We also plan to discuss possible systematic approaches to optimizing blood tube utilization processes. However, we still need to focus on solving the core problems that caused the excessive usage of blood tubes, as we mentioned above. In the future, the laboratories should focus on redesigning the facilities into a single “Core-Lab” structure and fully utilize the pre-analytical systems to reduce blood tubes. We can also use information technology to influence physicians' ordering behavior by designing electronic ordering systems to reduce the tendency for physicians to order unnecessary urgent or emergency tests [17].
To the best of our knowledge, ours is the first longitudinal observational study across multiple years to show the growth of phlebotomy tube utilization at a major medical center. The 8% increase of phlebotomy tubes over 4 years should be alarming to hospital managements worldwide as we are still expecting more tests to be offered in the future. The entire healthcare community should collectively work towards solving this problem with more creative solutions.
Author contribution statement
Xincen Duan: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Wrote the paper.
Wenqi Shao; Jing Zhu; Yin Zhao; Baishen Pan; Wei Guo: Conceived and designed the experiments; Analyzed and interpreted the data.
Wenhai Jiang: Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data.
Xiao Tan: Performed the experiments; Analyzed and interpreted the data.
Jing Yang; Yihui Yang; Jiaye Zhou: Analyzed and interpreted the data.
Chunyan Zhang; Qian Yu: Conceived and designed the experiments.
Beili Wang: Conceived and designed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data.
Funding statement
This research was funded by the National Key Research and Development Program of China [2020AAA0109400], the National Science Foundation of China [82172348, 81902139, 81972000], the Constructing Project of Clinical Key Disciplines in Shanghai [shslczdzk03302], the Specialized Fund for the Clinical Researches of Zhongshan Hospital, Fudan University [2020ZHZS28, 2018ZSLC05, 2020ZSLC54 and 2021ZSGG08], the Key Medical and Health Projects of Xiamen [YDZX20193502000002], the Shanghai Medical Key Specialty [ZK2019B28], Shanghai Youth Medical Talents [Qian Yu], and Xuhui District AI Cooperation Project [2021-001].
Data availability statement
The authors do not have permission to share data.
Contributor Information
Baishen Pan, Email: pan.baishen@zs-hospital.sh.cn.
Beili Wang, Email: wang.beili1@zs-hospital.sh.cn.
Wei Guo, Email: guo.wei@zs-hospital.sh.cn.
References
- 1.Jackups R., Scott M.G., Zhang R. Clinical decision support rapidly improves test utilization during a nationwide phlebotomy tube shortage. Clin. Chem. 2021;67(10):1426–1427. doi: 10.1093/clinchem/hvab139. [DOI] [PubMed] [Google Scholar]
- 2.Loh T.P., Saw S., Sethi S.K. Extra blood tubes - an affordable excess? Clin. Chim. Acta. 2010;411(19–20):1544–1545. doi: 10.1016/j.cca.2010.06.007. [DOI] [PubMed] [Google Scholar]
- 3.Halpern S.D., Becker D., Curtis J.R., Fowler R., Hyzy R., Kaplan L.J., Rawat N., et al. An official American thoracic society/American association of critical-care nurses/American College of chest physicians/society of critical care medicine policy statement: the choosing Wisely® top 5 list in critical care medicine. Am. J. Respir. Crit. Care Med. 2014;190(7):818–826. doi: 10.1164/rccm.201407-1317ST. [DOI] [PubMed] [Google Scholar]
- 4.Beverina I., Borotto E., Novelli C., Radrizzani D., Brando B. Iatrogenic anaemia and transfusion thresholds in ICU patients with COVID-19 disease at a tertiary care hospital. Transfus. Apher. Sci. 2021;60(2):103068. doi: 10.1016/j.transci.2021.103068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wisser D., van Ackern K., Knoll E., Wisser H., Bertsch T. Blood loss from laboratory tests. Clin. Chem. 2003;49(10):1651–1655. doi: 10.1373/49.10.1651. [DOI] [PubMed] [Google Scholar]
- 6.Eyster E., Bernene J. Nosocomial anemia. JAMA. 1973;223(1):73–74. doi: 10.1001/jama.1973.03220010059017. [DOI] [PubMed] [Google Scholar]
- 7.Smoller B.R., Kruskall M.S. Phlebotomy for diagnostic laboratory tests in adults. Pattern of use and effect on transfusion requirements. N. Engl. J. Med. 1986;314(19):1233–1235. doi: 10.1056/NEJM198605083141906. [DOI] [PubMed] [Google Scholar]
- 8.Burnum J.F. Medical vampires. N. Engl. J. Med. 1986;314(19):1250–1251. doi: 10.1056/NEJM198605083141910. [DOI] [PubMed] [Google Scholar]
- 9.Fowler R.A., Berenson M. Blood conservation in the intensive care unit. Crit. Care Med. 2003;31(12 Suppl):S715–S720. doi: 10.1097/01.CCM.0000099350.50651.46. [DOI] [PubMed] [Google Scholar]
- 10.Helmer P., Hottenrott S., Steinisch A., Röder D., Schubert J., Steigerwald U., Choorapoikayil S., et al. Avoidable blood loss in critical care and patient blood management: scoping review of diagnostic blood loss. J. Clin. Med. 2022;11(2):2. doi: 10.3390/jcm11020320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.FDA. Conservation strategies – letter to health care and laboratory personnel. https://www.fda.gov/medical-devices/letters-health-care-providers/update-blood-specimen-collection-tube-conservation-strategies-letter-health-care-and-laboratory (Accessed 2022-July-6).
- 12.Cap CAP. Publishes strategies to mitigate National shortage of “blue top” test tubes. https://newsroom.cap.org/latest-news/cap-publishes-strategies-to-mitigate-national-shortage-of-blue-top-test-tubes (Accessed 2022-July-6).
- 13.Lee B.K., Ellenbecker M.J., Moure-Eraso R. Analyses of the recycling potential of medical plastic wastes. Waste Manag. 2002;22(5):461–470. doi: 10.1016/s0956-053x(02)00006-5. [DOI] [PubMed] [Google Scholar]
- 14.McAlister S., Barratt A.L., Bell K.J., Mcgain F. The carbon footprint of pathology testing. Med. J. Aust. 2020;212(8):377–382. doi: 10.5694/mja2.50583. [DOI] [PubMed] [Google Scholar]
- 15.Humble R.M., Davis S.R., Hounkponou H.G., Krasowski M.D. A rainbow of extra tubes: useful or wasteful practice. Am. J. Clin. Pathol. 2017;147(suppl_2):S150. doi: 10.1093/ajcp/aqw191.056. [DOI] [PubMed] [Google Scholar]
- 16.Sarkar M.K., Botz C.M., Laposata M. An assessment of overutilization and underutilization of laboratory tests by expert physicians in the evaluation of patients for bleeding and thrombotic disorders in clinical context and in real time. Diagnosis (Berl) 2017;4(1):21–26. doi: 10.1515/dx-2016-0042. [DOI] [PubMed] [Google Scholar]
- 17.Strockbine V.L., Gehrie E.A., Zhou Q.P., Guzzetta C.E. Reducing unnecessary phlebotomy testing using a clinical decision support system. J. Healthc. Qual. 2020;42(2):98–105. doi: 10.1097/JHQ.0000000000000245. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors do not have permission to share data.