Abstract
Objectives
Assess the impact of single rooms versus multioccupancy accommodation on inpatient healthcare outcomes and processes.
Design
Systematic review and narrative synthesis.
Data sources
Medline, Embase, Google Scholar and the National Institute for Health and Care Excellence website up to 17 February 2022.
Eligibility criteria
Eligible papers assessed the effect on inpatients staying in hospital of being assigned to a either a single room or shared accommodation, except where that assignment was for a direct clinical reason like preventing infection spread.
Data extraction and synthesis
Data were extracted and synthesised narratively, according to the methods of Campbell et al.
Results
Of 4861 citations initially identified, 145 were judged to be relevant to this review. Five main method types were reported. All studies had methodological issues that potentially biased the results by not adjusting for confounding factors that are likely to have contributed to the outcomes. Ninety-two papers compared clinical outcomes for patients in single rooms versus shared accommodation. No clearly consistent conclusions could be drawn about overall benefits of single rooms. Single rooms were most likely to be associated with a small overall clinical benefit for the most severely ill patients, especially neonates in intensive care. Patients who preferred single rooms tended to do so for privacy and for reduced disturbances. By contrast, some groups were more likely to prefer shared accommodation to avoid loneliness. Greater costs associated with building single rooms were small and likely to be recouped over time by other efficiencies.
Conclusions
The lack of difference between inpatient accommodation types in a large number of studies suggests that there would be little effect on clinical outcomes, particularly in routine care. Patients in intensive care areas are most likely to benefit from single rooms. Most patients preferred single rooms for privacy and some preferred shared accommodation for avoiding loneliness.
PROSPERO registration number
CRD42022311689.
Keywords: Economics, Health policy, HEALTH ECONOMICS, Organisation of health services, Quality in health care
STRENGTHS AND LIMITATIONS OF THIS STUDY.
This study is a systematic review of a very large, diverse set of papers.
It addresses a topic that is directly of interest to patients using both traditional clinical and patient-reported outcomes.
Meta-analysis was not undertaken because of limitations in the underlying data.
Introduction
Hospital bed capacity in England has roughly halved over the past 30 years,1 with pledges from the UK government to replace, refurbish or reconfigure National Health Service tens of hospitals by 2030.2 There is an opportunity not only to increase bed numbers but also to choose accommodation types: single rooms or multioccupancy spaces, or a mixture of both. It is important to get this right at the start, as once each hospital is built, it is difficult to change the proportion of single rooms to shared accommodation. However, there is no settled, obvious evidence base on which to base decisions.3 Arguments for building exclusively single rooms include patients’ dignity and control over the environment and improved infection control, while those against cite the importance of some patients’ preference for company (particularly during longer stays), feelings of safety being in the presence of other patients, and, of note, the lack of understanding about infection control in single rooms.4 5
For some situations, isolation of the patient in a single room is part of the clinical intervention. For example, a patient with severe immune compromise may be isolated to protect them from acquiring infection. Similarly, patients with highly transmissible infections may be isolated to prevent spread of infection. A single room is also used where privacy is extremely important, for example, delivery units on maternity wards or for dying patients and their families. For most patients, though, there are ranges of risks and benefits and reasons for their preferences, including what would count as a good experience of hospital admission.6
This study set out to find published evidence to investigate whether inpatient stays in single rooms or in shared accommodation (ie, multioccupancy rooms, bays or wards) have been associated with any impact on the processes undertaken by the hospital and on patients’ outcomes. A wide range of clinical, social and economic outcomes were included from the primary perspective of patients across a range of acute hospital types. Staff perspectives, while not formally assessed, were included if reported as part of a study on patient and caregiver views. The objective was to compare staying in a single room versus shared accommodation for care in which the type of accommodation was not part of the intervention itself. This systematic review protocol has been registered with PROSPERO (registration number CRD42022311689).
Methods
Identification of papers
We performed a systematic literature review of content in Medline (via PubMed) and Embase for comparative clinical trials, observational studies and systematic literature reviews published in any language up to 17 February 2022. Additional searches were performed via Google Scholar and the National Institute for Health and Care Excellence. We used combinations of “hospital”, design”, “management”, “health care facility”, “single”, “multi”, “room”, “bay”, “bed” and “accommodation”, optimised for the search platform (see online supplemental appendix: search strategy). Eligible papers addressed care of adult and/or paediatric inpatients staying in hospital for routine, emergency or intensive care, and who were assigned to a particular accommodation type (single room or shared accommodation). We excluded papers that assessed long-stay patients, day patients, and those attending accident and emergency departments who were not later admitted to an acute hospital; patients who were relocated to a single room during admission (eg, for isolation after contracting an infectious disease or for terminal care); no direct comparison condition for staying in a single room; non-clinical outcomes; and impact of care on healthcare professionals (HCPs) and/or support staff. We also excluded narrative reviews, perspective papers, letters, editorials and conference abstracts with no relevant data.
bmjopen-2022-068932supp001.pdf (206.6KB, pdf)
Retrieved abstracts were screened by two researchers (AB and NC) using the inclusion criteria in the online supplemental appendix. Disagreements were resolved by discussion with the project leader. Shortlisted papers were retrieved as full texts. The reference lists of all papers included in this analysis were reviewed to identify any additional publications of primary research that met the inclusion criteria. Full papers were screened for relevance by two researchers (AB and AM) independently.
The quality of each paper was assessed by the same researcher using the Downs and Black checklist for observational studies7 and the Joanna Briggs Institute checklists (https://jbi.global/critical-appraisal-tools) for qualitative studies and for systematic reviews. These checklists enable assessment of reporting quality, generalisability of findings, biases in measurements of intervention and outcome, confounding in the selection of participants and power (whether negative findings could be the result of chance). Each quality assessment checklist score was converted to a percentage of the maximum possible score and was categorised for the purposes of this report into high (75%–100%), moderate (50%–74%) or low quality (<50%; see online supplemental table 1).
bmjopen-2022-068932supp002.pdf (1.2MB, pdf)
Data extraction and synthesis
Data were extracted into an Excel spreadsheet and checked, with final adjudication by the project leader (AM), and were synthesised narratively, according to the methods of Campbell et al.8 Data extracted from systematic literature reviews were cross-checked to avoid double-counting. The fields for extraction were study methodology, baseline characteristics of participants (when provided), clinical outcomes, non-clinical outcomes, resource use and costs. The clinical outcomes of interest were in-hospital mortality, overall mortality (≥30 days), morbidity (eg, falls, deterioration, new pressure ulcers and complications), patient safety incidents and hospital-acquired infections. Non-clinical outcomes of interest were patient and family member experiences, length of stay, cost of stay, experience of accommodation change and number of changes (for the same type of care) during admission, and impact on the caregivers and family members of dependent patients. Outcomes were assessed based on the measures used in the original articles. Extracted data were sorted by outcome and then by population and setting. Relevant data for each outcome were summarised narratively by comparing heterogeneity across studies in terms of whether differences were statistically significant and in favour of single room or shared accommodation.
Statistical analysis
As substantial heterogeneity across studies (eg, how data were reported, study methods, etc) was expected, formal meta-analysis was not deemed feasible. Thus, no formal measures of heterogeneity or overall effect size were performed, and all data reported are descriptive. To aid comparison and assess consistency of the conclusions, data are presented in summary tables.
Certainty of findings was assessed based on whether the direction of benefit was consistently statistically significant for single rooms or shared accommodation (across all studies or those with the lowest risk of bias) or was inconsistent or not statistically significant.
There are special areas of hospitals where responses to the intervention might differ, such as intensive care or paediatric units and areas for women in labour. Therefore, we aimed to present data separately by different subgroups.
Patient and public involvement
Patients and the public were not involved in designing this study. The study aim was to establish what is already published in peer-reviewed literature on the topic, including the views of patients, their parents or caregivers, and the public.
Results
Study characteristics
The initial searches returned 4861 potentially relevant abstracts. After screening and removal of duplicates, 145 publications were included in this review (figure 1). There were five main types of studies: 60 before-and-after comparisons (shared accommodation followed by relocation to single rooms); 75 comparisons of patients allocated to single rooms compared with others simultaneously in shared accommodation; 18 qualitative studies recording the views of patients, caregivers or HCPs on accommodation preferences; 10 evidence syntheses, including systematic literature reviews, guidelines and other reports; and 3 economic evaluations of accommodation type (figure 2). Some studies incorporated more than one design.
Figure 1.
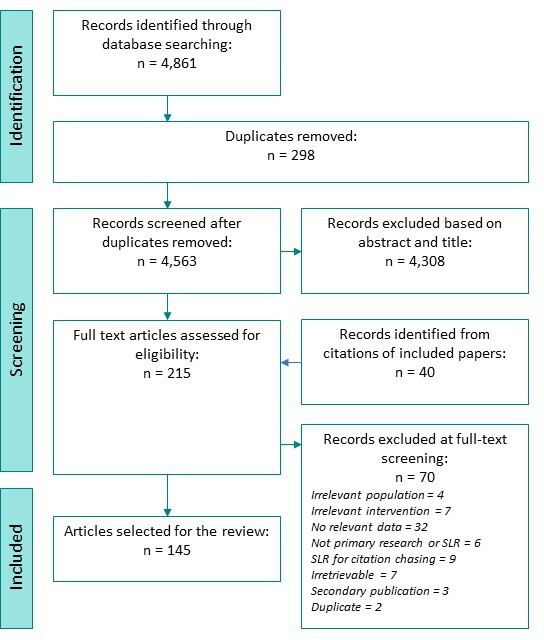
Selection of papers for review. SLR, systematic literature review.
Figure 2.
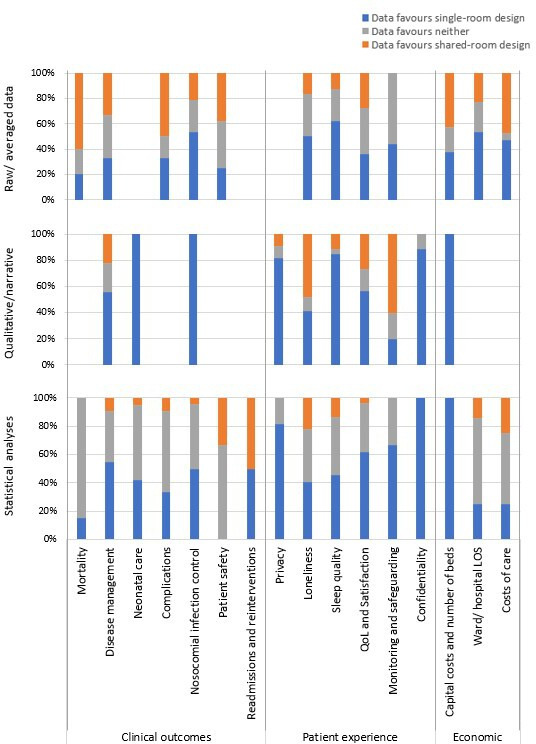
Percentage of studies reporting data in favour of either single-room or shared-room design, according to the type of data available and outcome reported. LOS, length of stay; QoL, quality of life.
All studies had methodological issues that potentially biased the results by not adjusting for confounding factors that are likely to have contributed to the outcomes. In the 60 before-and-after trials, many factors other than accommodation changed due to moving into new facilities, such as unfamiliarity with new layouts and logistics. In the 75 contemporaneous comparisons, reasons for bed space allocations were not generally reported (eg, availability, severity of illness), making their effects on the differences in outcomes unclear. Approximately one-third of studies overall (35 of 104) did not report any baseline characteristics of the study participants, and the rest reported few details other than age and sex. This heterogeneity and uncertainty about the comparability of study populations meant that a formal meta-analysis of outcomes was considered infeasible. Overall, only 25 of the studies included reported p values for differences in baseline characteristics between patients admitted to multibed versus single-bed rooms. Of these 25, only 5 reported significant differences in any parameters (p≤0.05): one study reports lower caregiver’s age at the time of patient’s admission,9 three report lower gestational age of infants admitted to single rooms in neonatal intensive care unit (NICU)10–12 and one reports a higher proportion of female patients were admitted to single rooms.13 The latter study however also notes that patients admitted to single rooms were more frail due to multiple comorbidities and functional dependence. This heterogeneity and uncertainty about the comparability of study populations meant that a formal meta-analysis of outcomes was considered infeasible.
The quality of studies varied widely. Thirty-four studies were assigned high-quality scores (75%‒100%) with a range of 78%‒100% (see online supplemental table 1). Twenty-three studies were classified as being of low quality (<50%) with a range of 10%‒48%.
Mortality
Eighteen studies reported mortality (see figure 3 and online supplemental table 2).9 14–30 Ten were before-and-after studies and the others were contemporary studies. Only one article scored less than 50% for quality and two had high-quality scores. Six studies involved neonates/infants, one assessed children and the remainder were concerned with adult/elderly care. The numbers of deaths were low, meaning that the studies might have been underpowered to detect small or moderate effects, for example, a small difference in mortality. Likewise, whether reported increases in mortality reflected true increases in risk or were due to confounding factors (eg, unreported reasons for patients being allocated single rooms) is unclear.
Figure 3.
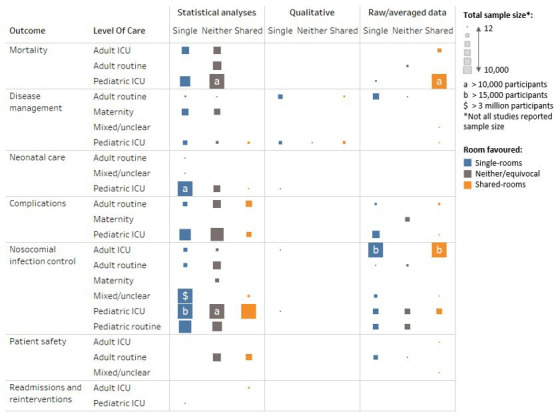
Clinical outcomes represented by the total sample size with data for that outcome, by level of care and the type of data reported and room design favoured. ICU, intensive care unit.
Routine care
Four studies involved patients receiving routine care,14 15 22 28 all in adults, none of which found a significant difference in mortality between those in single rooms versus shared accommodation, including up to 1 year after discharge.
Intensive care
Six studies assessed mortality among adults in intensive care units (ICUs).9 19 23 24 26 30 One study by Bracco et al23 favoured single rooms. That study included 2522 adults in ICUs in Canada and reported mortality of 2.9% among those in single rooms or cubicles compared with 8.3% among those in shared accommodation (p<0.001). A study of 666 adults in ICUs in Korea with COVID-19 favoured shared accommodation, reporting 2.4% mortality vs 4.6% among those treated in single rooms, but no statistical analysis of the difference was reported.26 The other studies showed no differences between accommodation types.
Seven studies assessed mortality specifically among neonates in ICU.16–18 21 25 27 29 Three favoured single rooms. Lehtonen et al29 assessed 4662 neonates in 331 NICUs across 10 countries (Canada, Australia, New Zealand, Finland, Israel, Japan, Spain, Sweden, Switzerland, Italy) and found that those cared for in units with single rooms had lower odds of death or any major morbidity than those in units with no such facilities (adjusted OR 0.76; 95% CI 0.64 to 0.89). Two papers reported reduced mortality in single rooms among a small population of neonates in intensive care, but statistical significance was not reported.16 17 By contrast, two studies favoured shared accommodation. Puumala et al21 reported a lower percentage of deaths among 9995 neonates. Harris et al25 31 assessed NICUs in 11 hospitals in the USA and found fewer deaths among neonates nursed in units with shared accommodation compared with units with single rooms. However, statistical significance was not reported in either.
Lazar et al’s study20 was the only study to assess children in a paediatric ICU and found no difference between accommodation types.
Patient care and disease management
Twelve publications reported on outcomes related to patient care and disease management (see figure 3 and online supplemental table 3).3 15 32–41 All were in adults or non-specified age groups. Three were before-and-after studies, four were contemporaneous studies and five were evidence syntheses. Four studies had quality scores below 50%, but four had scores greater than 75%. All papers assessed routine care.
Most findings favoured single rooms. Significance was shown for improvements in cleanliness,36 pain management,36 and interactions between patients and medical staff,37 and other findings were descriptive. A study in Australia of 1569 orthopaedic patients had fewer emergency calls due to deterioration in condition after a move to single rooms compared with patients in shared accommodation.15 As room allocation was based partly on severity of illness, nurses tended to position themselves nearer higher-risk patients to aid visualisation. Lawson and Phiri33 found better patient satisfaction with care and lower analgesic use in orthopaedic patients in single rooms.
Three systematic reviews found that patients in single rooms may have faster recovery due to better sleep and a more pleasant environment,39 but there was no consistent effect on use of medication.40 An OECD (Organisation for Economic Co-operation and Development) WHO report concluded that single-room occupancy was associated with reduced pain scores, but due to a lack of detail had a very low-quality score (14%).42
Findings in favour of shared accommodation were feelings of safety34 and less use of restraints.3 In a comparison of only single rooms after a move to a new hospital with only shared accommodation in the previous hospital, falls and medication errors in the medical assessment unit increased notably immediately but by 9 months had fallen to levels lower than previously.32 However, in the single-room ward for older adults, falls and pressure ulcers significantly increased after the move and remained higher than before moving. No similar trends were seen after the move in a control hospital with 50% single rooms and 50% shared accommodation, and this was the preferred choice of nurses before and after the move (38% and 40%, respectively).
Maternity and neonatal care
Twenty-three studies were found that assessed maternity and neonatal care (see figure 3 and online supplemental table 4). Most (n=14) were before-and-after studies and the remainder were contemporaneous studies.10 12 17 18 21 43–60 Three studies were low quality and only one had a high-quality score. Many of these studies included statistically assessed findings, with most favouring single rooms or showing no difference between accommodation types.
Maternity care
Nine studies considered maternity care and perceptions of mothers and family members.44 45 47 49 50 52–55
Harris et al46 assessed 976 low-risk patients, 583 of whom received all care in single rooms and 393 in separate labour, delivery, and recovery areas. While overall use of intrapartum interventions was similar, maternal outcomes were better in single rooms. After discharge, Erdeve et al53 reported that mothers of babies in NICUs who received care in shared accommodation had significantly more acute care visits (p=0.046), telephone consultations (p=0.01) and rehospitalisation (p<0.05) than those cared for in single rooms, and the reasons were more likely to be for issues related to prematurity like feeding difficulties compared with anatomical disorders. This perception is supported by the findings of Janssen et al,47 which showed that mothers in single rooms rated information and instructions at discharge as being clearer than those in shared accommodation.
Multiple studies indicated that satisfaction with care teams was greater in single rooms, including duration and quality of interactions and needs met.44 45 47–50 52 In one study, participants felt that parental presence was greater in single rooms than in shared accommodation.54 In a US study, women reported less pain in single rooms than in shared accommodation.48
Neonatal care
Fourteen papers reported on outcomes in neonatal care.10 12 17 21 43 46–48 51 56–60 Many of the results for neonates in ICUs showed no differences in outcomes between accommodation types. Significant improvements were seen in breastfeeding outcomes17 21 58 61 and weight gain51 61 in favour of single rooms. However, Tandberg et al12 reported that longer-term weight gain (4 months) was better after neonatal care in shared accommodation. In two studies, reduced apnoea events were associated with single rooms,17 62 and in another study, less need for mechanical ventilation was reported in single rooms.58 Significantly reduced neonatal pain scores were also reported.48
Complications of disease
Twenty-three articles assessed disease complications (see figure 3 and online supplemental table 5).3 14 15 22–24 28–30 32 46 48 53 57 59 63–68 Nine were before-and-after studies, 10 were contemporaneous studies, 1 used a mix of study designs and 3 were evidence syntheses. Two articles had quality scores below 50% and two had scores greater than 75%. Findings generally favoured single rooms or showed no differences between accommodation types.
Routine care
Eight papers assessed complications specifically in routine care and all assessed care of adults.14 17 22 28 46 67–69 Only one study reported results with significance assessed, which showed reduced incidence of delirium among older adults with dementia nursed in single rooms (HR 0.66, 95% CI 0.48 to 0.93, p<0.02).69 The Scottish guidelines on delirium recommend reducing light and noise and having familiar items around patients with or at risk of developing delirium,68 which might be supported by this finding.
In a small relocation study (n=64),32 pressure injuries seemed to be increased around 10-fold in single rooms and falls in 50% or 100% shared accommodation, but a substantial change in case mix made this finding difficult to interpret. By contrast, in a larger non-controlled UK relocation study (n=1569), no significant difference was noted between different types of accommodation.
The findings for other complications, such as hip fracture rates following falls, thromboembolic events, infections and other medical complications, were not significantly different among orthopaedic patients in single rooms compared with those in shared accommodation in an Australian study.67 Patients in single rooms were more likely to be female and much more likely to have private health insurance, which may have biased the outcomes.
Intensive care
Twelve papers specified assessments in ICU settings, of which three assessed adults23 24 30 and nine concerned neonatal care.29 48 53 57 59 64 64–66 In one study of 1253 adults in Brazil,24 delirium was significantly less likely among those in ICU single rooms than in shared accommodation, but no significant difference was seen between groups of elderly patients in different types of ICU accommodation in the Netherlands.30 Organ failure was reported to be significantly lower in patients managed in single rooms in one study.23 However, few data are available in adults and most studies reported no differences between accommodation types.
An international study of 4662 preterm neonates found a significantly lower risk of death or any major morbidity, including sepsis and retinopathy of prematurity, among those nursed in NICUs with single family rooms (OR 0.76, 95% CI 0.64 to 0.89).29 In contrast, another study showed lower rates of necrotising enterocolitis and intraventricular haemorrhage in shared accommodation.51 However, in other studies, rates of these and other serious complications were similar in all ward types.51 59 62 64 Lester et al64 found that neonatal stress levels were reduced among babies in NICU single maternity care rooms compared with those in shared accommodation.
Prevention of infection
Fifty-two studies discussed prevention of infection (see figure 3 and online supplemental table 6).3 12 15 17–21 23–25 27 32 40 41 51 56 59 65 70–102 Twenty were before-and-after studies, 28 were contemporaneous studies, 1 used a mix of study designs and 3 were evidence syntheses. Seven had low-quality scores and nine had high-quality scores. More than half (n=33) studies reported statistically analysed data.
Routine care
Routine care was assessed in adults in 10 studies,15 73 79 81 83 84 88 91 93 97 and 8 involved mixed age populations and care levels that stated or were assumed to include adults and routine care.32 40 41 71 75 76 92 99 Hospital-acquired infection rates were shown to be reduced in single rooms in six studies.32 41 71 73 75 91 92 However, in Maben et al,32 this finding depended on the ward mix: Clostridium difficile infections were reduced in single rooms where the split with shared accommodation was half and half, whereas all shared accommodation performed better than all single rooms. In Darley et al,71 this finding was only for C. difficile, whereas hospital-acquired Methicillin-resistant Staphylococcus aureus (MRSA) rates did not differ by accommodation type. Bocquet et al82 and Munier-Marion et al91 found reduced nosocomial influenza infections in single rooms and one study showed a reduced risk of norovirus infection.86 By contrast, McDonald et al75 noted reduced infection rates for Enterococcus spp, C. difficile and MRSA. In a systematic review, Voigt et al40 concluded that the quality of evidence did not support the use of single rooms over shared accommodation. Indeed, only two studies showed increased infections in shared accommodation.32 87 Nevertheless, in one study, patients81 preferred single rooms for infection prevention. In a study of more than 1 million patients of all ages across 2018 hospitals in the USA, O’Neill et al99 found that single rooms were significantly associated with reductions in central line-associated bloodstream infections.
Seven studies assessed routine care in children.82 85 90 94 100 101 Two found a decrease in nosocomial infections in single rooms—one overall82 and one for diarrhoea in gastrointestinal and neurosurgical units,85 but the latter found no difference between accommodation types in a cardiological unit. In two large studies in Finland (n=1927 and n=5119), Kinnula et al100 101 saw increases in hospital-acquired infections among children admitted to shared accommodation in an infectious disease ward because there was no grouping by aetiology. All hospital-acquired infections with symptoms during the hospital stay and 49% of those manifesting after discharge led to diarrhoea. The risk of infection was doubled among children sharing accommodation with patients who had respiratory infections (OR 2.3, 95% CI: 1.1 to 4.8; p=0.03). Risk decreased per year of age. Among 83 334 children assessed in two hospitals, Quach et al94 found significantly increased rates of respiratory infections when accommodation was more than 50% single rooms (rate per 1000 patient-days 1.33, 95% CI 1.29 to 1.37).
Intensive care
Outcomes in ICUs were reported specifically in 26 studies, 11 in adults and mixed age populations,19 23 24 70 72 74 77 89 95 96 102 1 in children20 and 14 in neonates.12 17 18 21 25 27 51 56 59 65 76 78 80 98
Among adult populations, only one study showed outcomes in favour of shared accommodation, with reductions per 10 000 patient-days in cultures positive for Enterobacter spp, Haemophilus, Streptococcus viridans, Acinetobacter spp, S. pneumoniae, group B Streptococcus spp, Neisseria spp and MRSA.77 However, in the same study, single rooms showed lower rates of infections with many common organisms, such as Staphylococcus spp, C. difficile and Pseudomonas spp. Four studies showed significant data on reduced bacterial infection and transmission in single rooms based on isolates and antibiotic use,23 70 74 95 although in the study by Halaby et al,74 transmission of Morganella spp, Proteus spp, Serratia spp and Pseudomonas spp did not differ between accommodation types. Two studies indicated reduced risks of bloodstream infections in single rooms.23 96 As for routine care, patients perceived infection prevention to be better in single rooms than in shared spaces.72
Among neonates and among children in ICUs, the findings were mixed. In favour of shared accommodation, four studies reported reduced cases of nosocomial sepsis,17 21 one reduced colonisation with multidrug-resistant organisms51 and one nosocomial infections with pneumonia.25 Four studies indicated no difference between accommodation types for sepsis or septicaemia and/or found that the use of single rooms was associated with fewer sepsis cases.12 21 59 78 Only one study showed an increase in sepsis in shared accommodation, and that was specifically in neonates born at or after term.21
Patient safety
Eleven studies considered patient safety (see figure 3 and online supplemental table 7).3 15 22 28 32 40 41 69 88 103 104 Three were before-and-after studies, four were contemporaneous studies, one used mixed design and three were evidence syntheses. Two had low-quality scores and three had high-quality scores. Most of the studies assessed routine care or mixed care populations, and generally the populations were adults and elderly people.
Overall, the data showed no differences between accommodation types or favoured shared accommodation. Only the OECD study indicated reduced risk of falls in single rooms,41 but the quality of this study was deemed to be very low due to reporting very few details of the research. Significantly lower rates of falls were seen in multibed accommodation in two studies.22 28 The study of Poncette et al,104 which analysed alarm data in an ICU, found that the number of alarms per bed per day was higher in single rooms than in shared accommodation.
Readmissions and reinterventions
Only two studies reported on readmissions and reinterventions (see figure 3 and online supplemental table 8). They were both contemporaneous studies and one had a quality score of 74% and one of 78%. One showed that single rooms were associated with lower rates of rehospitalisation.53 The other favoured shared accommodation, with fewer patients returning to theatre within 6 weeks of treatment.67
Privacy
Forty-eight publications, including six evidence syntheses, reported on privacy (see online supplemental table 9).3 5 15 16 25 32 34 36–39 41 43–47 49 52 55 61 62 72 81 90 102 103 105–125 Eighteen were before-and-after studies, 23 were contemporaneous studies, 1 used mixed designs and 6 were evidence syntheses. Nine had low-quality scores but 19 had high-quality scores. They were mainly descriptive studies but overwhelmingly favoured single rooms.
Routine care
Twenty-eight studies assessed privacy among adults receiving routine care,3 5 15 32 34 36 37 39 41 44 46 47 61 81 103 105 106 109 112 115–122 with seven of these reporting statistical analyses.32 34 36 41 46 47 109 117 Key aspects of privacy in single rooms were improved confidentiality when discussing personal information, use of private bathrooms and privacy during early postpartum care (eg, assistance with feeding). However, in the study by Florey et al,109 83% of patients in shared rooms also reported feeling that they had adequate privacy. Likewise, the systematic reviews by Taylor et al3 and Dowdeswell et al38 found advantages and disadvantages with regard to privacy in all studies they assessed. Patients reported feeling as though they could ask more questions or make more remarks in single rooms than in shared accommodation, and more scored physicians’ responses as being empathetic.37 Qualitative or descriptive studies also strongly supported greater privacy in single rooms.5 15 81 103 105 106 112 115 118–121 124
Four studies assessed routine care among children.90 108 114 123 Boztepe et al114 found that children did not rank privacy highly and were more concerned about procedures being painful. In this study, many of the children had extensive history of hospitalisation. The other three studies reported greater privacy in single rooms, but children also seemed to enjoy the social aspect of shared accommodation. The main reasons for preferring single rooms were private bathrooms and the capacity for family members to stay. Sleep was an important aspect of care in single rooms for children and parents.61 90 123
Intensive care
Nine studies reported on privacy for adults in ICUs, and generally, the findings favoured single rooms.3 38 41 45 49 52 62 72 113 Three studies reported statistical evidence of improved privacy in single rooms among adult patients.41 45 49 The literature reviews by Dowdeswell et al38 and Taylor et al3 showed mixed findings among studies.
Eleven studies addressed neonatal care in ICUs.16 25 43 45 49 52 55 102 107 110 111 All but two43 55 favoured single rooms for privacy.
Loneliness/isolation and family contact
Fifty-five publications, five were evidence syntheses, reported patients’ views about loneliness or family contact associated with single-room accommodation (see figure 4 and online supplemental table 10).3 5 11 12 16 22 25 31 32 34 36 38 39 41 43 44 47 49 50 52–54 57 60–62 72 78 81 90 102 103 106 108–113 117 118 120–123 126–133 Twenty were before-and-after studies, 29 were contemporaneous studies, 1 used mixed study designs and 5 were evidence syntheses. Only nine had quality scores less than 50%, while high-quality scores were assigned to 17.
Figure 4.
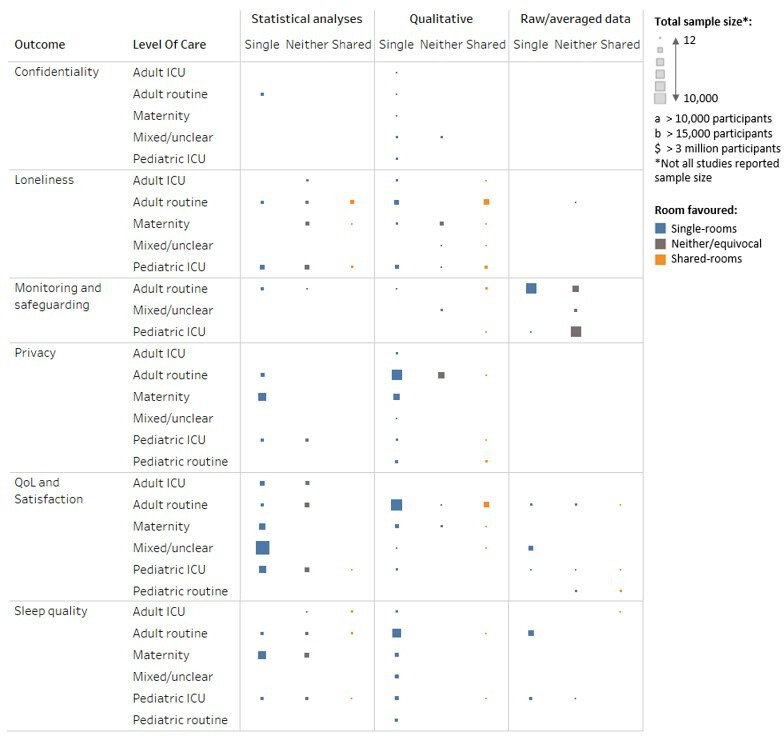
Patient-experience outcomes represented by the total sample size with data for that outcome, by level of care and the type of data reported and room design favoured. ICU, intensive care unit; QoL, quality of life.
Two main themes seemed to be revealed in patients’ perspectives: shared accommodation were strongly preferred for social interaction to avoid loneliness/isolation,5 16 22 32 34 39 43 52 61 72 81 90 106 108 109 117–123 126 127 129 132 whereas single rooms were preferred for privacy (eg, for bathroom use, during consultations and visits, and to spend with children, particularly neonates).5 11 12 16 34 38 43 50 52 54 57 60 62 72 78 81 90 102 108–110 112 113 117 130 133
Noise, disturbance and sleep
Forty-five publications, four of which were evidence syntheses, reported patients’ views about noise, disturbance and sleep associated with single-room accommodation (see figure 4 and online supplemental table 11).3 15 16 30–32 34 36 38 39 41 43–47 52 57 61 62 72 80 81 90 107 109 111–113 115–117 120–122 134–142 Sixteen were before-and-after studies, 24 were contemporaneous studies, 1 used mixed study designs and 4 were evidence syntheses. Nine had quality scores less than 50% and 13 had high-quality scores.
In general, patients felt that single rooms were quieter and led to less sleep disruption. However, measurement of noise levels showed that there were no substantial objective differences between single rooms and shared accommodation.36 57 136 One study reported lower noise levels in single rooms, but the difference was not statistically assessed.80 Stevens et al57 and Meyer et al140 found that respiratory support and other medical devices could raise noise levels in single rooms enough to disturb sleep even when ambient noise had been reduced. HCPs also reported that single rooms improved patients’ sleep.16 Poncette et al104 found that fewer alarms raised in shared accommodation reduced overall noise levels. One study also noted that patients preferred single rooms because they felt they were less likely to disturb other patients.122 Most studies addressing sleep found that it was improved in single rooms.34 36 38 39 41 61 62 90 116 117 120 121 137 141 This was generally due to fewer disturbances and/or a perceived quieter environment than in shared accommodation. Hosseini and Bagheri117 and Sakr et al141 noted that the risk of new-onset insomnia was significantly higher among patients in shared accommodation (95.7% vs 75%, p=0.011).
Humidity and temperature were discussed in one article. Van Enk and Steinberg136 reported that in a NICU with centrally controlled humidity, shared accommodation had non-significantly lower percentage of relative humidity than single rooms but showed much greater variance (26.8% (±17.0) in single rooms vs 26.0% (±89.0)). Both mean values were lower than the recommended range for NICU (30%‒60%). Temperature could be controlled within individual single rooms and mean values were significantly lower than those in the shared accommodation, which had central temperature control per nursery (mean 73.8°F (range 65.3°F–77.5°F) in single rooms vs 76.0°F (range 71.1°F‒84.5°F), p=0.0001). More than 85% of readings in both, though, were within the recommended range of 72°F—78°F, although readings outside the range were too hot in shared accommodation and too cold in single rooms. The authors suggested that thermostats should be allowed to vary only within the recommended range.
Lighting was assessed in three studies, two of which favoured single rooms due to less illumination for neonates45 57 and one study of patients with delirium that favoured lower light in a shared accommodation.30
Satisfaction with care
Fifty-two publications, six of which were evidence syntheses, reported patients’ satisfaction with care (see figure 4 and online supplemental table 12).3 5 9 12 15 25 31 33 34 36 38–41 43–45 47 49 54 60–62 64 66 78 81 90 103 105 107 109 111 112 114–117 119–122 124 128 131 132 134 137 143–146 Fifteen were before-and-after studies, 29 were contemporaneous studies, 1 used mixed study designs, 1 was an economic analysis and 6 were evidence syntheses. The quality scores of 10 studies were less than 50% and of 14 were 75%‒100%.
Overall, results show either little difference between accommodation types or results in favour of single rooms. Single rooms seemed to be favoured most by mothers in maternity units, whereas preference towards shared accommodation seemed to increase with rising age. The economic analysis found that patients were willing to pay for private care to have single rooms.146
Routine care
Routine care was assessed in 30 studies (see online supplemental table 12).3 15 33 34 36 38–41 44 47 61 81 90 103 105 109 114–117 119–121 124 132 134 137 143 144 Patients preferred shared accommodation in seven studies.39 90 119–121 132 134 Generally, they preferred interaction with other patients, and in two reports they stated that they found the shared accommodation more secure and safe.120 121 Specific reasons given for preferring single rooms were privacy,3 36 61 81 103 115 134 comfort/environment,33 47 105 112 143 level of care and information, effect on recovery38 41 47 105 116 117 137 and safety.36 40
Intensive care
We found 24 reports of intensive care.3 9 11 25 31 38 41 43 45 49 54 60–62 64 66 78 107 111 112 128 131 143 145 Only two reported findings that favoured shared accommodation. Campbell-Yeo et al54 found that in an open-bay NICU, mothers reported better self-efficacy and less uncertainty about their babies’ health. Also in a NICU, Pineda et al60 found that the risk of stress among mothers was significantly lower in shared accommodation than in single rooms, although life stress did not differ between accommodation types. By contrast, other assessments of stress found that risk was reduced in single rooms11 25 31 64 78 or did not differ.11 54 66 Satisfaction with design/environment, where assessed, favoured single rooms.62 112
Finding on satisfaction with maternity care was greater for parents in single rooms in three studies9 62 64 but did not differ between accommodation types in two.78 145 Single rooms seemed to have little effect on postpartum depression or irritability, most measures not differing between accommodation types11 60 66 78 145 and only four findings favouring single rooms.11 25 31 54
Only 8 of the 51 studies were related to satisfaction with care in other patient populations, involving cardiovascular, cancer, adolescent or mixed adult care.3 9 38 41 61 112 131 143 All these studies’ findings supported single rooms.
Patient monitoring and safeguarding
Although the impact of single rooms on healthcare staff was not the focus of this review, 14 of the included publications reported the views of HCPs as well as patient-reported outcomes that we used to explore monitoring of patients (see figure 4 and online supplemental table 13).18 19 23 27 34 36 52 72 81 110 112 115 117 134 Four were before-and-after studies, eight were contemporaneous studies, one used mixed study designs and one was an evidence synthesis. No study had a low-quality score. Five of the studies were classified as being of high quality.
Most of the studies presented descriptive/qualitative findings. Three studies reported statistically assessed data, all in relation to routine care and among adult patients. Two34 117 favoured single rooms, reporting that availability to patients, meeting patients’ needs and access to patients were improved. The fourth study showed no difference between single rooms and shared accommodation for responding to patients’ call alerts. One study reported that nurses felt they might spend longer with patients in single rooms, depriving other patients of as much care.110 In another study, safety of patients in units with single rooms was raised as an issue due to increased distances between nurses and patients and impeded observation of patients.72
Patient confidentiality
Confidentiality was assessed in 11 studies (see figure 4 and online supplemental table 14).5 32 41 52 72 81 109 110 117 118 Five were before-and-after studies, four were contemporaneous studies, one used mixed study designs and one was an evidence synthesis. Two studies had low-quality scores, while four had high-quality scores.
All studies concluded that patient confidentiality was better maintained when patients were in single rooms, with one study finding no difference for adults with cardiovascular disease in ICU112 (see online supplemental table 14). Malcolm118 found that the lack of privacy and confidentiality in shared accommodation affected patients’ relationships with other patients.
Availability of beds, space requirements and capital costs
Sixteen studies reported on beds, space and costs associated with different accommodation types (see figure 5 and online supplemental table 15).9 17 19 27 32 33 43 60 71 94 100 101 110 112 129 147 Nine were before-and-after studies, six were contemporaneous studies and one used mixed study designs. Two studies had quality scores below 50% and three were classified as being of high quality.
Figure 5.
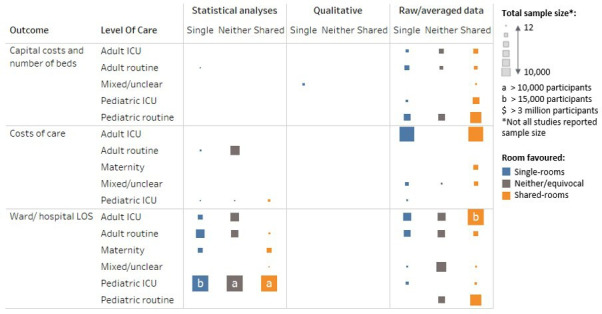
Economic outcomes represented by the total sample size with data for that outcome, by level of care and the type of data reported and room design favoured. ICU, intensive care unit; LOS, length of stay.
There did not seem to be strong evidence in favour of either accommodation type. The inclusion of single rooms substantially increases the amount of floor space required to achieve the same number of beds as in shared accommodation, with estimates suggesting between 30% and 50% more floor space being required per bed, which increases capital costs.9 17 32 33 110 129 147 Shared accommodation provides greater flexibility to add beds in times of need.19 27 60 94 101 Darley et al71 found that numbers of bed-days lost due to ward closures caused by norovirus outbreaks were greatly reduced after moving to a hospital with 75% single rooms from the previous 10% single rooms.
Length of stay
Fifty-three publications, including two evidence syntheses, reported on length of stay associated with single-room accommodation (see figure 5 and online supplemental table 16).9 10 12 14–19 21–26 28–33 40 41 45 46 48 51–53 56 58 59 64–67 69 73 77–79 89 95 100 111 115 116 128 135 143 147–149 Twenty-eight were before-and-after studies, 23 were contemporaneous studies, 1 used mixed study designs and 2 were evidence syntheses. Five of the studies were classified as being of low quality but only seven fell into the high-quality category. The evidence was highly mixed with no clear benefit from either accommodation type.
Routine care
Of 20 studies assessing routine care, 18 concerned adults and the elderly.14 15 28 32 33 40 41 46 67 69 73 81 115 116 135 143 147 149 Among these, eight found that length of stay was shorter in single rooms,14 22 32 33 46 69 115 147 149 but in the study by Maben et al,32 this was true only for an older people’s ward and not for a medical assessment unit, and in that by Lawson and Phiri,33 while it was true for non-surgical orthopaedic patients and psychiatric patients, no difference was seen for surgical orthopaedic patients. One study found that length of stay was shorter in shared accommodation among older patients with dementia, overall and among those who had experienced inpatient falls.28 No difference in overall length of stay was reported in seven studies, including two evidence syntheses.15 40 41 67 73 135 143
The two studies of routine care in children by Kinnula et al showed no difference between accommodation types in one100 but longer duration of admissions among children in shared accommodation in another.101
Intensive care
Of 32 studies assessing length of stay in intensive care, 23 considered neonates10 11 16–18 21 25 29 45 48 51–53 56 58 59 64–66 78 95 111 128 148 and 9 adults.9 19 23 24 26 30 77 79 89 As for routine care, the results were highly mixed.
Among the nine studies assessing care of adults in ICUs, five showed no significant differences between single rooms and shared accommodation.9 19 30 30 79 Teltsch et al77 assessed care after a change from multibed to single rooms and compared the findings with a hospital with no change. The length of stay in the ICU in the comparator hospital increased year on year from 3.8 days to 4.2 days from 2000 to 2005. While higher after the change to single rooms, the length of stay did not change substantially over the same period, and after adjustment was an estimated 10% lower overall (relative ratio 0.90, 95% CI 0 to 19). Bracco and et al23 reported that patients were able to stay longer in the same bed in single rooms during infection outbreaks in an ICU, although overall length of stay was not significantly different.
In NICUs, statistically significant shorter duration of stay in hospital was reported in three studies. Puumala et al21 found that stays were shorter for very and extremely preterm babies, but there was no difference between accommodation types for moderately preterm babies, and stays for term and post-term babies were shorter in shared accommodation. Lehtonen et al29 found that stays were on average 3.4 days shorter (95% CI 3.1 to 4.7) and van Veenendaal et al78 found a median difference of 2 days in favour of single rooms. Qualitative/descriptive studies also favoured single rooms in five studies.16 45 52 111 Three studies identified shorter stays in shared accommodation,25 59 148 but 13 found no difference between accommodation types.10 11 17 18 48 51 53 56 58 64–66 128
Costs of care
Nineteen publications, including two evidence syntheses, reported on costs or resource use associated with different types of accommodation (see figure 5 and online supplemental table 17).15 22 25 28 31 32 40 46 57 67 95 111 113 133 134 146 148 150 Eight were before-and-after studies, seven were contemporaneous studies, two used mixed study designs and two were evidence syntheses. Four studies had low-quality scores and six had high-quality scores.
Several studies reported multiple measures of costs and found evidence supporting both types of accommodation. Therefore, the evidence split was 10 studies finding in favour of single rooms, 10 in favour of shared accommodation and 6 showing no difference in measures.
Boardman and Forbes146 recommended taking into account the following construction and running costs, given that single-room facilities required more space to construct: land costs, construction costs, maintenance (refinishing and updating), housekeeping and operating costs, and healthcare provision (potentially longer distances to cover). Maben et al32 134 estimated in 2015 that the cost of building a hospital solely comprising single rooms could be around 5% more than building one with predominantly shared accommodation but suggested that the difference becomes marginal over time. Harris et al31 found that the most cost-effective configuration in terms of construction costs per square foot was a combination of open bays and single rooms.
Findings in favour of single rooms were due to reduced overall staffing costs,46 150 reduced length of stay,95 111 reduced waiting and transfer times,146 higher proportions of patients being discharged to rehabilitation,67 reduced infections95 and operational efficiencies.40 148 Reasons favouring shared accommodation were lower cleaning and housekeeping costs,32 134 perceived increased nursing staff32 148 and lower labour costs in NICUs.148
Discussion
This systematic review identified a substantial body of evidence associated with hospital accommodation, yet no clearly consistent conclusions could be drawn about overall benefits of single rooms versus multibed ward spaces. The narrative and heterogeneous nature of much of the evidence also meant that a formal statistical synthesis, such as a meta-analysis, was not feasible. Nevertheless, some themes did emerge and might be worth considering further. Single rooms were most likely to be associated with overall clinical benefit for the most severely ill patients, especially neonates in intensive care, although the evidence is mixed even in these high-risk populations. Patients who preferred single rooms tended to do so for privacy, particularly having a private bathroom, and for reduced disturbances. By contrast, there were distinct patterns of men, older adults, children and adolescents being more likely to prefer shared accommodation, particularly for the social aspects. While mixed accommodation types seemed to be the most cost-effective approach to construction because the capital cost of single room building is higher than that for shared accommodation, the running costs seem likely to be recouped over time by other efficiencies.
While patients and HCPs expressed preferences, healthcare outcomes seem unlikely to be substantially affected by hospital accommodation. This is reassuring because most patients also have little influence over this aspect of their care. Likewise, HCPs might also have little influence over which accommodation type their patients are assigned. Patient or family preferences for single rooms are particularly strong in NICUs and maternity wards, but other groups, in particular men, older adults and adolescents, are more likely to prefer shared accommodation. The split of accommodation and whether the predictable adverse effects of accommodation design can be mitigated in these areas would be worth considering at the planning stages of new buildings.
The average cost per patient of units comprising only single rooms was lower than those consisting of only shared accommodation. Mean direct cost per patient in a single room has been estimated to be 15.5% lower for neonates in ICU and 24% lower for care in maternity units but may be similar or reduced in adults in routine care wards. Shorter length of stay was an important contributor to this difference and could increase the number of patients who can be treated in the beds available. However, the effects found were small and local variations may change the economic picture for a particular hospital. It is also unclear how far the reduced length of stay was due to the single room, and how much was caused by confounding factors associated with being in a new hospital. Nearly all the studies we considered were from high-income regions and mostly based in European or anglophone countries. Thus, policymakers should incorporate local building and labour costs in decisions.
Determining the impact of moving to single-room wards will therefore always need to overcome the impact of confounding factors such as concomitant changes to processes and improvements in other facilities and services that may also have led to the changes, or that may have acted in opposition to the direct effects of the different accommodation.
A number of other systematic reviews have been conducted on this topic. Ten scoping or systematic literature reviews were identified by our search, of which only one was able to conduct a meta-analysis of outcome data in premature infants.78 As no quantitative synthesis was undertaken in most cases, the analyses were not adjusted for potential confounding factors such as the interaction between outcomes from patients sharing a room or potential bias from sicker patients being more or less likely to be nursed in single rooms. In NICUs, three systematic reviews with only a narrative synthesis found that single rooms were usually found to improve privacy and parental involvement, improved sleep and reduced hospital-acquired infections, but that these outcomes were usually based on a small number of non-randomised studies.151–153 The meta-analysis found sepsis rates were significantly lower and exclusive breast feeding at discharge was significantly higher in single family rooms. There were no significant differences in cognitive development, length of admission, growth, complications of ICU admission and mortality. Four other systematic reviews3 40 154 155 and two scoping reviews39 156 assessed outcomes in a more general hospital population and generally found mixed evidence of benefits from single rooms, with each review identifying between 12 and 44 studies that reported advantages, disadvantages and neutral findings for most clinical outcomes, but a more positive result for patient privacy and satisfaction.
This study has some limitations. Of 215 articles originally retrieved, we selected 145 for review, which is still a large number. None of the 145 studies used randomised study designs. Randomised controlled studies are not practical to assess hospital accommodation and, therefore, most studies were prone to bias. In particular, in hospitals with mixed single rooms and shared accommodation, patients must be allocated to the rooms, which will be partly due to their medical condition or other personal factors and partly due to bed availability at the time of admission. This introduces selection bias, as the reasons why patients were in single rooms were often not reported. We minimised this bias by excluding studies where the allocation to single rooms or shared accommodation was known to be for an apparent clinical purpose. Additionally, 60 of the publications compared outcomes before and after moving from shared accommodation to single rooms. This introduced confounding, as many factors other than the studied intervention would have changed at the same time, so attributing the outcome to the intervention alone is misleading. The opportunity of building a new hospital is rare. While it provides an ideal platform for before-and-after studies, nearly all of these studies were of a single hospital, so the total number of hospitals studied is low, meaning that uncertainty about risks and benefits remains after this systematic review.
In practical terms, although there are still uncertainties about the true impact of changing to single-room wards, the 145 publications synthesised in this report show that the clinical and economic consequences of such a change are likely to be modest. Focused research on the impact of accommodation type on hospital-acquired airborne-transmitted infections may be warranted, as may studies of sufficient duration to examine long-term productivity changes after opening a new hospital. Because the global effect sizes found were modest, the effects within national systems or for specialist hospitals might be different in size and direction from the global. In particular, none of the included studies were in low-income or middle-income countries, so generalisability to those settings is difficult. Additional research might explore how the trend for sicker patients to be nursed in beds closer to the nursing station interacts with the choice of single or shared accommodation. How much outcomes of patients in shared rooms might be dependent on each other also warrants investigation. This would help clarify the main uncertainties within this review and would therefore allow some adjustment to be made to the assessment of the impact of single rooms on clinically important outcomes.
Supplementary Material
Footnotes
Contributors: AB, AM, NC, CS, RA, WS, AO and DMcP wrote sections of the final manuscript. DMcP conceived the study and defined the research question. AM defined the detailed method and arbitrated disagreements. AB and NC conducted the literature screening and data extraction. CS developed the figures and summary tables. DMcP is guarantor.
Funding: The study was funded by the New Hospital Programme, Department of Health and Social Care, which commissioned the overall research area. All authors, external and internal, had full access to all of the data (including statistical reports and tables) in the study and can take responsibility for the integrity of the data and the accuracy of the data analysis.
Disclaimer: The New Hospital Programme, Department of Health and Social Care, had no input into the study design, the collection, analysis and interpretation of data, the writing of the report or decision to submit the article for publication.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplemental information.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
Ethics approval was not required for this study.
References
- 1.Ewbank L, Thompson J, McKenna H, et al. Nhs Hospital bed numbers: past, present, future. The King’s Fund 2021. Available: https://www.kingsfund.org.uk/publications/nhs-hospital-bed-numbers
- 2.UK Government . Pm confirms £3.7 billion for 40 hospitals in biggest Hospital building programme in a generation. 2020. Available: https://www.gov.uk/government/news/pm-confirms-37-billion-for-40-hospitals-in-biggest-hospital-building-programme-in-a-generation
- 3.Taylor E, Card AJ, Piatkowski M. Single-Occupancy patient rooms: a systematic review of the literature since 2006. HERD 2018;11:85–100. 10.1177/1937586718755110 [DOI] [PubMed] [Google Scholar]
- 4.Pennington H, Isles C. Should hospitals provide all patients with single rooms? BMJ 2013;347:bmj.f5695. 10.1136/bmj.f5695 [DOI] [PubMed] [Google Scholar]
- 5.Roos AKØ, Skaug EA, Grøndahl VA, et al. Trading company for privacy: a study of patients’ experiences. Nurs Ethics 2020;27:1089–102. 10.1177/0969733019874497 [DOI] [PubMed] [Google Scholar]
- 6.Webster CS, Jowsey T, Lu LM, et al. Capturing the experience of the hospital-stay journey from admission to discharge using diaries completed by patients in their own words: a qualitative study. BMJ Open 2019;9:e027258. 10.1136/bmjopen-2018-027258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health 1998;52:377–84. 10.1136/jech.52.6.377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Campbell M, McKenzie JE, Sowden A, et al. Synthesis without meta-analysis (swim) in systematic reviews: reporting guideline. BMJ 2020;368:l6890. 10.1136/bmj.l6890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jongerden IP, Slooter AJ, Peelen LM, et al. Effect of intensive care environment on family and patient satisfaction: a before-after study. Intensive Care Med 2013;39:1626–34. 10.1007/s00134-013-2966-0 [DOI] [PubMed] [Google Scholar]
- 10.Kattelmann K, Jessica R. Traditional open-bay versus single-family room neonatal intensive care unit: a comparison of selected nutrition outcomes. RRN 2011;1:15. 10.2147/RRN.S15539 [DOI] [Google Scholar]
- 11.Tandberg BS, Frøslie KF, Flacking R, et al. Parent-Infant closeness, parents’ participation, and nursing support in single-family room and open Bay nicus. J Perinat Neonatal Nurs 2018;32:E22–32. 10.1097/JPN.0000000000000359 [DOI] [PubMed] [Google Scholar]
- 12.Tandberg BS, Flacking R, Markestad T, et al. Parent psychological wellbeing in a single-family room versus an open Bay neonatal intensive care unit. PLoS ONE 2019;14:e0224488. 10.1371/journal.pone.0224488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Singh I, Krishnan M, Edwards C, et al. Loneliness among older people in hospitals: a comparative study between single rooms and multi-bedded wards to evaluate current health service within the same organisation. Gerontol Geriatr Res 2016;2:1015. [Google Scholar]
- 14.Cantoni N, Weisser M, Buser A, et al. Infection prevention strategies in a stem cell transplant unit: impact of change of care in isolation practice and routine use of high dose intravenous immunoglobulins on infectious complications and transplant related mortality. Eur J Haematol 2009;83:130–8. 10.1111/j.1600-0609.2009.01249.x [DOI] [PubMed] [Google Scholar]
- 15.Davis M, Elliott R, Hills R, et al. Single-room ward design and its impact on service and patient outcomes: an evaluation study. Orthop Nurs 2019;38:317–25. 10.1097/NOR.0000000000000593 [DOI] [PubMed] [Google Scholar]
- 16.Domanico R, Davis DK, Coleman F, et al. Documenting the NICU design dilemma: parent and staff perceptions of open ward versus single family room units. J Perinatol 2010;30:343–51. 10.1038/jp.2009.195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Domanico R, Davis DK, Coleman F, et al. Documenting the NICU design dilemma: comparative patient progress in open-ward and single family room units. J Perinatol 2011;31:281–8. 10.1038/jp.2010.120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jansen SJ, Lopriore E, Berkhout RJM, et al. The effect of single-room care versus open-bay care on the incidence of bacterial nosocomial infections in pre-term neonates: a retrospective cohort study. Infect Dis Ther 2021;10:373–86. 10.1007/s40121-020-00380-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jung J, Choe PG, Choi S, et al. Reduction in the acquisition rate of carbapenem-resistant Acinetobacter baumannii (crab) after room privatization in an intensive care unit. Journal of Hospital Infection 2022;121:14–21. 10.1016/j.jhin.2021.12.012 [DOI] [PubMed] [Google Scholar]
- 20.Lazar I, Abukaf H, Sofer S, et al. Impact of conversion from an open ward design paediatric intensive care unit environment to all isolated rooms environment on incidence of bloodstream infections and antibiotic resistance in southern Israel (2000 to 2008). Anaesth Intensive Care 2015;43:34–41. 10.1177/0310057X1504300106 [DOI] [PubMed] [Google Scholar]
- 21.Puumala SE, Rich RK, Roy L, et al. Single-family room neonatal intensive care unit design: do patient outcomes actually change? J Perinatol 2020;40:867–74. 10.1038/s41372-019-0584-6 [DOI] [PubMed] [Google Scholar]
- 22.Singh I, Okeke J, Edwards C. Outcome of in-patient falls in hospitals with 100 % single rooms and multi-bedded wards. Age Ageing 2015;44:1032–5. 10.1093/ageing/afv124 [DOI] [PubMed] [Google Scholar]
- 23.Bracco D, Dubois M-J, Bouali R, et al. Single rooms may help to prevent nosocomial bloodstream infection and cross-transmission of methicillin-resistant Staphylococcus aureus in intensive care units. Intensive Care Med 2007;33:836–40. 10.1007/s00134-007-0559-5 [DOI] [PubMed] [Google Scholar]
- 24.Caruso P, Guardian L, Tiengo T, et al. Icu architectural design affects the delirium prevalence: a comparison between single-bed and multibed rooms*. Crit Care Med 2014;42:2204–10. 10.1097/CCM.0000000000000502 [DOI] [PubMed] [Google Scholar]
- 25.Harris DD, Shepley MM, White RD, et al. The impact of single family room design on patients and caregivers: Executive summary. J Perinatol 2006;26:S38–48. 10.1038/sj.jp.7211583 [DOI] [Google Scholar]
- 26.Hyun M, Lee JY, Kwon YS, et al. COVID-19: comparing the applicability of shared room and single room occupancy. Transbound Emerg Dis 2021;68:2059–65. 10.1111/tbed.13853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Julian S, Burnham C-AD, Sellenriek P, et al. Impact of neonatal intensive care bed configuration on rates of late-onset bacterial sepsis and methicillin-resistant Staphylococcus aureus colonization. Infect Control Hosp Epidemiol 2015;36:1173–82. 10.1017/ice.2015.144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Knight S, Singh I. Profile of inpatient falls in patients with dementia: a prospective comparative study between 100 % single rooms and traditional multibedded wards. Journal of Clinical Gerontology and Geriatrics 2016;7:87–92. 10.1016/j.jcgg.2016.03.002 [DOI] [Google Scholar]
- 29.Lehtonen L, Lee SK, Kusuda S, et al. Family rooms in neonatal intensive care units and neonatal outcomes: an international survey and linked cohort study. J Pediatr 2020;226:112–7. 10.1016/j.jpeds.2020.06.009 [DOI] [PubMed] [Google Scholar]
- 30.Zaal IJ, Spruyt CF, Peelen LM, et al. Intensive care unit environment may affect the course of delirium. Intensive Care Med 2013;39:481–8. 10.1007/s00134-012-2726-6 [DOI] [PubMed] [Google Scholar]
- 31.Harris D, McCuskey M, White R. The impact of single family NICU rooms. 2006. Available: https://www.healthdesign.org/system/files/impact_of_single_family_nicu_rooms_1.pdf [Accessed 12 Jul 2022].
- 32.Maben J, Griffiths P, Penfold C, et al. One size fits all? mixed methods evaluation of the impact of 100 % single-room accommodation on staff and patient experience, safety and costs. BMJ Qual Saf 2016;25:241–56. 10.1136/bmjqs-2015-004265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lawson B, Phiri M. Hospital design. Room for Improvement Health Serv J 2000;110:24–6. [PubMed] [Google Scholar]
- 34.Ehrlander W, Ali F, Chretien KC. Multioccupancy Hospital rooms: Veterans’ experiences and preferences. J Hosp Med 2009;4:E22–7. 10.1002/jhm.491 [DOI] [PubMed] [Google Scholar]
- 35.McKeown K, Haase T, Pratschke J, et al. Determinants of care outcomes for patients who die in hospital in Ireland: a retrospective study. BMC Palliat Care 2015;14:11. 10.1186/s12904-015-0014-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nahas S, Patel A, Duncan J, et al. Patient experience in single rooms compared with the open ward for elective orthopaedic admissions. Musculoskelet Care 2016;14:57–61. 10.1002/msc.1110 [DOI] [PubMed] [Google Scholar]
- 37.van de Glind I, van Dulmen S, Goossensen A. Physician-Patient communication in single-bedded versus four-bedded Hospital rooms. Patient Educ Couns 2008;73:215–9. 10.1016/j.pec.2008.07.004 [DOI] [PubMed] [Google Scholar]
- 38.Dowdeswell B, Erskine J, Heasman M. Hospital Ward Configuration Determinants Influencing Single Room Provision. A Report for NHS Estates, England by the EU Health Property Network. 2004. Available: https://citeseerx.ist.psu.edu/document?repid=rep1&type=pdf&doi=91223495002f5a83411e51fbe4e589be5ad80218 [Google Scholar]
- 39.Søndergaard SF, Beedholm K, Kolbæk R, et al. Patients’ and nurses’ experiences of all single-room Hospital accommodation: a scoping review. HERD 2022;15:292–314. 10.1177/19375867211047548 [DOI] [PubMed] [Google Scholar]
- 40.Voigt J, Mosier M, Darouiche R. Private rooms in low acuity settings: a systematic review of the literature. HERD 2018;11:57–74. 10.1177/1937586717702597 [DOI] [PubMed] [Google Scholar]
- 41.OECD, World Health Organization . Improving Healthcare Quality in Europe: Characteristics, Effectiveness and Implementation of Different Strategies. OECD. 2019. 10.1787/b11a6e8f-en [DOI] [PubMed] [Google Scholar]
- 42.Rechel B, Erskine J, Dowdeswell B, et al. Capital investment for health: case studies from Europe. Copenhagen, Denmark: European Health Property Network : European Observatory on Health Systems and Policies 2009, Available: file:///C:/Users/rasht/Downloads/9789289041782-eng.pdf [Google Scholar]
- 43.Stelwagen M, van Kempen A, Westmaas A, et al. Parents’ experiences with a model of integrated maternity and neonatal care designed to empower parents. J Obstet Gynecol Neonatal Nurs 2021;50:181–92. 10.1016/j.jogn.2020.11.001 [DOI] [PubMed] [Google Scholar]
- 44.Olson ME, Smith MJ. An evaluation of single-room maternity care. Health Care Superv 1992;11:43–9. [PubMed] [Google Scholar]
- 45.Carter BS, Carter A, Bennett S. Families’ views upon experiencing change in the neonatal intensive care unit environment: from the'‘aby barn'’to the private room. J Perinatol 2008;28:827–9. 10.1038/jp.2008.102 [DOI] [PubMed] [Google Scholar]
- 46.Harris SJ, Farren MD, Janssen PA, et al. Single room maternity care: perinatal outcomes, economic costs, and physician preferences. J Obstet Gynaecol Can 2004;26:633–40. 10.1016/s1701-2163(16)30610-7 [DOI] [PubMed] [Google Scholar]
- 47.Janssen PA, Klein MC, Harris SJ, et al. Single room maternity care and client satisfaction. Birth 2000;27:235–43. 10.1046/j.1523-536x.2000.00235.x [DOI] [PubMed] [Google Scholar]
- 48.Lester BM, Hawes K, Abar B, et al. Single-family room care and neurobehavioral and medical outcomes in preterm infants. Pediatrics 2014;134:754–60. 10.1542/peds.2013-4252 [DOI] [PubMed] [Google Scholar]
- 49.Swanson JR, Peters C, Lee BH. Nicu redesign from open ward to private room: a longitudinal study of parent and staff perceptions. J Perinatol 2013;33:466–9. 10.1038/jp.2012.157 [DOI] [PubMed] [Google Scholar]
- 50.Toivonen M, Lehtonen L, Löyttyniemi E, et al. Effects of single-family rooms on nurse-parent and nurse-infant interaction in neonatal intensive care unit. Early Hum Dev 2017;106–107:59–62. 10.1016/j.earlhumdev.2017.01.012 [DOI] [PubMed] [Google Scholar]
- 51.van der Hoeven A, Bekker V, Jansen SJ, et al. Impact of transition from open Bay to single room design neonatal intensive care unit on multidrug-resistant organism colonization rates. J Hosp Infect 2022;120:90–7. 10.1016/j.jhin.2021.12.006 [DOI] [PubMed] [Google Scholar]
- 52.Bodack E, Schenk O, Karutz H. Die einrichtung von einzelzimmern auf neonatologischen intensivstationen – auswirkungen auf die betreuung AUS sicht Der eltern. Z Geburtshilfe Neonatol 2016;220:124–9. 10.1055/s-0042-102886 [DOI] [PubMed] [Google Scholar]
- 53.Erdeve O, Arsan S, Yigit S, et al. The impact of individual room on rehospitalization and health service utilization in preterms after discharge. Acta Paediatr 2008;97:1351–7. 10.1111/j.1651-2227.2008.00889.x [DOI] [PubMed] [Google Scholar]
- 54.Campbell-Yeo M, Kim T, Disher T, et al. Do single-family rooms increase parental presence, involvement, and maternal well-being in neonatal intensive care? J Perinat Neonatal Nurs 2021;35:350–61. 10.1097/JPN.0000000000000600 [DOI] [PubMed] [Google Scholar]
- 55.Dowling DA, Blatz MA, Graham G. Mothers’ experiences expressing breast milk for their preterm infants: does NICU design make a difference? Adv Neonatal Care 2012;12:377–84. 10.1097/ANC.0b013e318265b299 [DOI] [PubMed] [Google Scholar]
- 56.Hourigan SK, Subramanian P, Hasan NA, et al. Comparison of infant gut and skin microbiota, resistome and virulome between neonatal intensive care unit (NICU) environments. Front Microbiol 2018;9:1361. 10.3389/fmicb.2018.01361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Stevens DC, Helseth CC, Thompson PA, et al. A comprehensive comparison of open-bay and single-family-room neonatal intensive care units at sanford children’s Hospital. HERD 2012;5:23–39. 10.1177/193758671200500403 [DOI] [PubMed] [Google Scholar]
- 58.Grundt H, Tandberg BS, Flacking R, et al. Associations between single-family room care and breastfeeding rates in preterm infants. J Hum Lact 2021;37:593–602. 10.1177/0890334420962709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Vohr B, McGowan E, McKinley L, et al. Differential effects of the single-family room neonatal intensive care unit on 18- to 24-month bayley scores of preterm infants. J Pediatr 2017;185:42–8. 10.1016/j.jpeds.2017.01.056 [DOI] [PubMed] [Google Scholar]
- 60.Pineda RG, Stransky KE, Rogers C, et al. The single-patient room in the NICU: maternal and family effects. J Perinatol 2012;32:545–51. 10.1038/jp.2011.144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Nassery W, Landgren K. Parents’ experience of their sleep and rest when admitted to hospital with their ill child: a qualitative study. Compr Child Adolesc Nurs 2019;42:265–79. 10.1080/24694193.2018.1528310 [DOI] [PubMed] [Google Scholar]
- 62.Stevens DC, Helseth CC, Khan MA, et al. A comparison of parent satisfaction in an open-bay and single-family room neonatal intensive care unit. HERD 2011;4:110–23. 10.1177/193758671100400309 [DOI] [PubMed] [Google Scholar]
- 63.Rechel B, editors, European Health Property Network, European Observatory on Health Systems and Policies . Capital investment for health: case studies from Europe. Copenhagen, Denmark: European Health Property Network : European Observatory on Health Systems and Policies, [Google Scholar]
- 64.Lester BM, Salisbury AL, Hawes K, et al. 18-Month follow-up of infants cared for in a single-family room neonatal intensive care unit. J Pediatr 2016;177:84–9. 10.1016/j.jpeds.2016.06.069 [DOI] [PubMed] [Google Scholar]
- 65.Monson BB, Eaton-Rosen Z, Kapur K, et al. Differential rates of perinatal maturation of human primary and nonprimary auditory cortex. ENeuro 2018;5:ENEURO. 10.1523/ENEURO.0380-17.2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Erdeve O, Arsan S, Canpolat F, et al. Does individual room implemented family-centered care contribute to mother–infant interaction in preterm deliveries necessitating neonatal intensive care unit hospitalization? Amer J Perinatol 2009;26:159–64. 10.1055/s-0028-1095186 [DOI] [PubMed] [Google Scholar]
- 67.Felice Tong YY, Karunaratne S, Youlden D, et al. The impact of room-sharing on length of stay after total hip or knee arthroplasty: a retrospective study. Arthroplast Today 2021;8:289–94. 10.1016/j.artd.2021.03.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Scottish Intercollegiate Guidelines Network, Healthcare Improvement Scotland . Delirium: a booklet for people who have experienced delirium, and for their carers. 2020.
- 69.Blandfort S, Gregersen M, Rahbek K, et al. Single-bed rooms in a geriatric ward prevent delirium in older patients. Aging Clin Exp Res 2020;32:141–7. 10.1007/s40520-019-01173-y [DOI] [PubMed] [Google Scholar]
- 70.Bonizzoli M, Bigazzi E, Peduto C, et al. Microbiological survey following the conversion from a bay-room to single-room intensive care unit design. J Hosp Infect 2011;77:84–6. 10.1016/j.jhin.2010.07.018 [DOI] [PubMed] [Google Scholar]
- 71.Darley ESR, Vasant J, Leeming J, et al. Impact of moving to a new Hospital build, with a high proportion of single rooms, on healthcare-associated infections and outbreaks. J Hosp Infect 2018;98:191–3. 10.1016/j.jhin.2017.06.027 [DOI] [PubMed] [Google Scholar]
- 72.Ferri M, Zygun DA, Harrison A, et al. Evidence-Based design in an intensive care unit: end-user perceptions. BMC Anesthesiol 2015;15:57. 10.1186/s12871-015-0038-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Gregersen M, Mellemkjær A, Foss CH, et al. Use of single-bed rooms may decrease the incidence of hospital-acquired infections in geriatric patients: a retrospective cohort study in central Denmark region. J Health Serv Res Policy 2021;26:282–8. 10.1177/1355819621994866 [DOI] [PubMed] [Google Scholar]
- 74.Halaby T, Al Naiemi N, Beishuizen B, et al. Impact of single room design on the spread of multi-drug resistant bacteria in an intensive care unit. Antimicrob Resist Infect Control 2017;6:117. 10.1186/s13756-017-0275-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.McDonald EG, Dendukuri N, Frenette C, et al. Time-Series analysis of health care-associated infections in a new hospital with all private rooms. JAMA Intern Med 2019;179:1501–6. 10.1001/jamainternmed.2019.2798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Song X, Soghier L, Floyd TT, et al. Reassessing the need for active surveillance of extended-spectrum beta-lactamase-producing Enterobacteriaceae in the neonatal intensive care population. Infect Control Hosp Epidemiol 2018;39:1436–41. 10.1017/ice.2018.260 [DOI] [PubMed] [Google Scholar]
- 77.Teltsch DY, Hanley J, Loo V, et al. Infection acquisition following intensive care unit room privatization. Arch Intern Med 2011;171:32–8. 10.1001/archinternmed.2010.469 [DOI] [PubMed] [Google Scholar]
- 78.van Veenendaal NR, van der Schoor SRD, Heideman WH, et al. Family integrated care in single family rooms for preterm infants and late-onset sepsis: a retrospective study and mediation analysis. Pediatr Res 2020;88:593–600. 10.1038/s41390-020-0875-9 [DOI] [PubMed] [Google Scholar]
- 79.Vietri NJ, Dooley DP, Davis CE, et al. The effect of moving to a new Hospital facility on the prevalence of methicillin-resistant Staphylococcus aureus. Am J Infect Control 2004;32:262–7. 10.1016/j.ajic.2003.12.006 [DOI] [PubMed] [Google Scholar]
- 80.Walsh WF, McCullough KL, White RD. Room for improvement: nurses’ perceptions of providing care in a single room newborn intensive care setting. Adv Neonatal Care 2006;6:261–70. 10.1016/j.adnc.2006.06.002 [DOI] [PubMed] [Google Scholar]
- 81.Bevan V, Edwards C, Woodhouse K, et al. Dignified care for older people: mixed methods evaluation of the impact of the hospital environment-single rooms or multi-bedded wards. Healthy Aging Research 2016;5:1–8. 10.1097/01.HXR.0000511879.99010.5d [DOI] [Google Scholar]
- 82.Bocquet A, Wintenberger C, Lupo J, et al. Description of an influenza outbreak in a French university hospital and risk factors of nosocomial influenza. Eur J Clin Microbiol Infect Dis 2021;40:879–84. 10.1007/s10096-020-04070-9 [DOI] [PubMed] [Google Scholar]
- 83.Cobo J, Asensio A, Moreno S, et al. Risk factors for nosocomial transmission of multidrug-resistant tuberculosis due to Mycobacterium bovis among HIV-infected patients. Int J Tuberc Lung Dis 2001;5:413–8. [PubMed] [Google Scholar]
- 84.Everts RJ, Hanger HC, Jennings LC, et al. Outbreaks of influenza A among elderly hospital inpatients. N Z Med J 1996;109:272–4. [PubMed] [Google Scholar]
- 85.Ford-Jones EL, Mindorff CM, Gold R, et al. The incidence of viral-associated diarrhea after admission to a pediatric hospital. Am J Epidemiol 1990;131:711–8. 10.1093/oxfordjournals.aje.a115555 [DOI] [PubMed] [Google Scholar]
- 86.Fraenkel CJ, Inghammar M, Söderlund-Strand A, et al. Risk factors for hospital norovirus outbreaks: impact of vomiting, genotype, and multi-occupancy rooms. Journal of Hospital Infection 2018;98:398–403. 10.1016/j.jhin.2018.01.011 [DOI] [PubMed] [Google Scholar]
- 87.Jou J, Ebrahim J, Shofer FS, et al. Environmental transmission of Clostridium difficile: association between hospital room size and C. difficile infection. Infect Control Hosp Epidemiol 2015;36:564–8. 10.1017/ice.2015.18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Lorenz SG, Dreher HM. Hospital room design and health outcomes of the aging adult. HERD 2011;4:23–35.:14. 10.1177/193758671100400204 [DOI] [PubMed] [Google Scholar]
- 89.Mattner F, Rüden AS, Mattner L, et al. Thoracic organ transplantation may not increase the risk of bacterial transmission in intensive care units. Int J Hyg Environ Health 2007;210:139–45. 10.1016/j.ijheh.2006.08.008 [DOI] [PubMed] [Google Scholar]
- 90.Morgan H. Single and shared accommodation for young patients in hospital. Paediatr Nurs 2010;22:20–4. 10.7748/paed2010.10.22.8.20.c7997 [DOI] [PubMed] [Google Scholar]
- 91.Munier-Marion E, Bénet T, Régis C, et al. Hospitalization in double-occupancy rooms and the risk of hospital-acquired influenza: a prospective cohort study. Clinical Microbiology and Infection 2016;22:461. 10.1016/j.cmi.2016.01.010 [DOI] [PubMed] [Google Scholar]
- 92.Park S-H, Stockbridge EL, Miller TL, et al. Private patient rooms and hospital-acquired methicillin-resistant Staphylococcus aureus: a hospital-level analysis of administrative data from the United States. PLoS ONE 2020;15:e0235754. 10.1371/journal.pone.0235754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Pilmis B, Billard-Pomares T, Martin M, et al. Can environmental contamination be explained by particular traits associated with patients? J Hosp Infect 2020;104:293–7. 10.1016/j.jhin.2019.12.011 [DOI] [PubMed] [Google Scholar]
- 94.Quach C, Shah R, Rubin LG. Burden of healthcare-associated viral respiratory infections in children’s hospitals. Journal of the Pediatric Infectious Diseases Society 2018;7:18–24. 10.1093/jpids/piw072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Sadatsafavi H, Niknejad B, Zadeh R, et al. Do cost savings from reductions in nosocomial infections justify additional costs of single-bed rooms in intensive care units? A simulation case study. Journal of Critical Care 2016;31:194–200. 10.1016/j.jcrc.2015.10.010 [DOI] [PubMed] [Google Scholar]
- 96.Stiller A, Schröder C, Gropmann A, et al. Icu ward design and nosocomial infection rates: a cross-sectional study in Germany. J Hosp Infect 2017;95:71–5. 10.1016/j.jhin.2016.10.011 [DOI] [PubMed] [Google Scholar]
- 97.Vaisman A, Jula M, Wagner J, et al. Examining the association between hospital-onset Clostridium difficile infection and multiple-bed room exposure: a case-control study. Infect Control Hosp Epidemiol 2018;39:1068–73. 10.1017/ice.2018.163 [DOI] [PubMed] [Google Scholar]
- 98.Washam MC, Ankrum A, Haberman BE, et al. Risk factors for Staphylococcus aureus acquisition in the neonatal intensive care unit: a matched case-case-control study. Infect Control Hosp Epidemiol 2018;39:46–52. 10.1017/ice.2017.234 [DOI] [PubMed] [Google Scholar]
- 99.O’Neill L, Park S-H, Rosinia F, et al. The role of the built environment and private rooms for reducing central line-associated bloodstream infections. PLoS ONE 2018;13:e0201002. 10.1371/journal.pone.0201002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Kinnula SE, Renko M, Tapiainen T, et al. Hospital-Associated infections during and after care in a paediatric infectious disease ward. J Hosp Infect 2008;68:334–40. 10.1016/j.jhin.2008.02.004 [DOI] [PubMed] [Google Scholar]
- 101.Kinnula S, Buettcher M, Tapiainen T, et al. Hospital-Associated infections in children: a prospective post-discharge follow-up survey in three different paediatric hospitals. Journal of Hospital Infection 2012;80:17–24. 10.1016/j.jhin.2011.09.007 [DOI] [PubMed] [Google Scholar]
- 102.Liu LX, Mozafarinia M, Axelin A, et al. Parents’ experiences of support in NICU single-family rooms. Neonatal Netw 2019;38:88–97. 10.1891/0730-0832.38.2.88 [DOI] [PubMed] [Google Scholar]
- 103.Reid J, Wilson K, Anderson KE, et al. Older inpatients’ room preference: single versus shared accommodation. Age Ageing 2015;44:331–3. 10.1093/ageing/afu158 [DOI] [PubMed] [Google Scholar]
- 104.Poncette A-S, Wunderlich MM, Spies C, et al. Patient monitoring alarms in an intensive care unit: observational study with do-it-yourself instructions. J Med Internet Res 2021;23:e26494. 10.2196/26494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Janssen PA, Dennis C-L, Reime B. Development and psychometric testing of the care in obstetrics: measure for testing satisfaction (COMFORTS) scale. Res Nurs Health 2006;29:51–60. 10.1002/nur.20112 [DOI] [PubMed] [Google Scholar]
- 106.Anåker A, von Koch L, Heylighen A, et al. "’t's Lonely'': patie’ts' experiences of the physical environment at a newly built stroke unit. HERD 2019;12:141–52. 10.1177/1937586718806696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Carlson B, Walsh S, Wergin T, et al. Challenges in design and transition to a private room model in the neonatal intensive care unit. Adv Neonatal Care 2006;6:271–80. 10.1016/j.adnc.2006.06.008 [DOI] [PubMed] [Google Scholar]
- 108.Curtis P, Northcott A. The impact of single and shared rooms on family-centred care in children’s hospitals. J Clin Nurs 2017;26:1584–96. 10.1111/jocn.13485 [DOI] [PubMed] [Google Scholar]
- 109.Florey L, Flynn R, Isles C. Patient preferences for single rooms or shared accommodation in a district general Hospital. Scott Med J 2009;54:5–8. 10.1258/rsmsmj.54.2.5 [DOI] [PubMed] [Google Scholar]
- 110.Jones L, Peters K, Rowe J, et al. The influence of neonatal nursery design on mothers’ interactions in the nursery. J Pediatr Nurs 2016;31:e301–12. 10.1016/j.pedn.2016.05.005 [DOI] [PubMed] [Google Scholar]
- 111.Milford CA, Zapalo BJ, Davis G. Transition to an individual-room NICU design: process and outcome measures. Neonatal Netw 2008;27:299–305. 10.1891/0730-0832.27.5.299 [DOI] [PubMed] [Google Scholar]
- 112.Real K, Fay L, Isaacs K, et al. Using systems theory to examine patient and nurse structures, processes, and outcomes in centralized and decentralized units. HERD 2018;11:22–37. 10.1177/1937586718763794 [DOI] [PubMed] [Google Scholar]
- 113.Apple M. A comparative evaluation of Swedish intensive care patient rooms. HERD 2014;7:78–93. 10.1177/193758671400700306 [DOI] [PubMed] [Google Scholar]
- 114.Boztepe H, Çınar S, Ay A. School-Age children’s perception of the hospital experience. J Child Health Care 2017;21:162–70. 10.1177/1367493517690454 [DOI] [PubMed] [Google Scholar]
- 115.Deitrick LM, Bokovoy J, Panik A. The "dance'' continues… evaluating differences in call Bell use between patients in private rooms and patients in double rooms using ethnography. J Nurs Care Qual 2010;25:279–87. 10.1097/NCQ.0b013e3181dde039 [DOI] [PubMed] [Google Scholar]
- 116.Douglas CH, Douglas MR. Patient-Centred improvements in health-care built environments: perspectives and design indicators. Health Expect 2005;8:264–76. 10.1111/j.1369-7625.2005.00336.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Hosseini SB, Bagheri M. Comparison of patient satisfaction with single patient rooms versus shared patient rooms. Ann Mil Health Sci Res 2017;15. 10.5812/amh.80199 [DOI] [Google Scholar]
- 118.Malcolm HA. Does privacy matter? former patients discuss their perceptions of privacy in shared Hospital rooms. Nurs Ethics 2005;12:156–66. 10.1191/0969733005ne772oa [DOI] [PubMed] [Google Scholar]
- 119.Nash P, Vanhoof J, Hall S, et al. Randomized crossover comparison of injection site pain with 40 mg/0.4 or 0.8 ml formulations of adalimumab in patients with rheumatoid arthritis. Rheumatol Ther 2016;3:257–70. 10.1007/s40744-016-0041-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Persson E, Määttä S. To provide care and be cared for in a multiple-bed Hospital room: care in a multiple-bed Hospital room. Scand J Caring Sci 2012;26:663–70. 10.1111/j.1471-6712.2012.00976.x [DOI] [PubMed] [Google Scholar]
- 121.Persson E, Anderberg P, Ekwall AK. A room of one’s own -- being cared for in a hospital with a single-bed room design. Scand J Caring Sci 2015;29:340–6. 10.1111/scs.12168 [DOI] [PubMed] [Google Scholar]
- 122.Rowlands J, Noble S. How does the environment impact on the quality of life of advanced cancer patients? A qualitative study with implications for ward design. Palliat Med 2008;22:768–74. 10.1177/0269216308093839 [DOI] [PubMed] [Google Scholar]
- 123.Schalkers I, Dedding CWM, Bunders JFG. [ I would like ] a place to be alone, other than the toil’t' -- chil’ren's perspectives on paediatric hospital care in the Netherlands. Health Expect 2015;18:2066–78. 10.1111/hex.12174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Bradbury-Jones C, Rattray J, Jones M, et al. Promoting the health, safety and welfare of adults with learning disabilities in acute care settings: a structured literature review. J Clin Nurs 2013;22:1497–509. 10.1111/jocn.12109 [DOI] [PubMed] [Google Scholar]
- 125.Mental welfare Commission for Scotland. Psychiatr Bull 1991;15:254–5. 10.1192/pb.15.4.254-a [DOI] [Google Scholar]
- 126.Anåker A, von Koch L, Sjöstrand C, et al. A comparative study of patients’ activities and interactions in a stroke unit before and after reconstruction—the significance of the built environment. PLoS ONE 2017;12:e0177477. 10.1371/journal.pone.0177477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Cusack L, Wiechula R, Schultz T, et al. Anticipated advantages and disadvantages of a move to 100 % single-room hospital in Australia: a case study. J Nurs Manag 2019;27:963–70. 10.1111/jonm.12753 [DOI] [PubMed] [Google Scholar]
- 128.Kainiemi E, Hongisto P, Lehtonen L, et al. Effects of single family room architecture on parent–infant closeness and family centered care in neonatal environments—a single-center pre–post study. J Perinatol 2021;41:2244–51. 10.1038/s41372-021-01137-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Rosbergen ICM, Tonello I, Clark RA, et al. Does Hospital design impact on patient activity levels and time spent alone? Disability and Rehabilitation 2022;44:3173–80. 10.1080/09638288.2020.1861117 [DOI] [PubMed] [Google Scholar]
- 130.Darcy Mahoney A, White RD, Velasquez A, et al. Impact of restrictions on parental presence in neonatal intensive care units related to coronavirus disease 2019. J Perinatol 2020;40(Suppl 1):36–46. 10.1038/s41372-020-0753-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.de Matos LBN, Fumis RRL, Nassar Junior AP, et al. Single-bed or multibed room designs influence ICU staff stress and family satisfaction, but do not influence ICU staff burnout. HERD 2020;13:234–42. 10.1177/1937586719878445 [DOI] [PubMed] [Google Scholar]
- 132.Pease NJF, Finlay IG. Do patients and their relatives prefer single cubicles or shared wards? Palliat Med 2002;16:445–6. 10.1191/0269216302pm577xx [DOI] [PubMed] [Google Scholar]
- 133.Chaudhury H, Mahmood A, Valente M. The use of single patient rooms versus multiple occupancy rooms in acute care environments. 2004. Available: https://www.healthdesign.org/sites/default/files/use_of_single_patient_rooms_v_multiple_occ._rooms-acute_care.pdf [Accessed 21 Jul 2022].
- 134.Maben J, Griffiths P, Penfold C, et al. Evaluating a major innovation in hospital design: workforce implications and impact on patient and staff experiences of all single room hospital accommodation. Southampton, Available: http://www.ncbi.nlm.nih.gov/books/NBK274434 [PubMed] [Google Scholar]
- 135.Pyrke RJL, McKinnon MC, McNeely HE, et al. Evidence-Based design features improve sleep quality among psychiatric inpatients. HERD 2017;10:52–63. 10.1177/1937586716684758 [DOI] [PubMed] [Google Scholar]
- 136.Van Enk RA, Steinberg F. Comparison of private room with multiple-bed ward neonatal intensive care unit environments. HERD 2011;5:52–63. 10.1177/193758671100500105 [DOI] [PubMed] [Google Scholar]
- 137.Eberhard-Gran M, Eskild A, Opjordsmoen S, et al. Postnatal care -- sleep, rest and satisfaction. Tidsskr Nor Laegeforen 2000;120:1405–9. [PubMed] [Google Scholar]
- 138.Edéll-Gustafsson U, Angelhoff C, Johnsson E, et al. Hindering and buffering factors for parental sleep in neonatal care. A phenomenographic study. J Clin Nurs 2015;24:717–27. 10.1111/jocn.12654 [DOI] [PubMed] [Google Scholar]
- 139.Foo CT, O’Driscoll DM, Ogeil RP, et al. Barriers to sleep in acute hospital settings. Sleep Breath 2022;26:855–63. 10.1007/s11325-021-02415-y [DOI] [PubMed] [Google Scholar]
- 140.Meyer TJ, Eveloff SE, Bauer MS, et al. Adverse environmental conditions in the respiratory and medical ICU settings. Chest 1994;105:1211–6. 10.1378/chest.105.4.1211 [DOI] [PubMed] [Google Scholar]
- 141.Sakr N, Hallit S, Mattar H. Incidence of and factors associated with new-onset insomnia among Lebanese hospitalised patients. Sultan Qaboos Univ Med J 2021;21:e210–220. 10.18295/squmj.2021.21.02.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Tegnestedt C, Günther A, Reichard A, et al. Levels and sources of sound in the intensive care unit-an observational study of three room types: levels and sources of sound in a multidisciplinary ICU. Acta Anaesthesiol Scand 2013;57:1041–50. 10.1111/aas.12138 [DOI] [PubMed] [Google Scholar]
- 143.Labarère J, Fourny M, Jean‐Phillippe V, et al. Refinement and validation of a French in‐patient experience questionnaire. Int J Health Care Qual Assur Inc Leadersh Health Serv 2004;17:17–25. 10.1108/09526860410515909 [DOI] [PubMed] [Google Scholar]
- 144.Miller NO, Friedman SB, Coupey SM. Adolescent preferences for rooming during hospitalization. J Adolesc Health 1998;23:89–93. 10.1016/S1054-139X(98)00015-9 [DOI] [PubMed] [Google Scholar]
- 145.Watson J, DeLand M, Gibbins S, et al. Improvements in staff quality of work life and family satisfaction following the move to single-family room NICU design. Adv Neonatal Care 2014;14:129–36. 10.1097/ANC.0000000000000046 [DOI] [PubMed] [Google Scholar]
- 146.Boardman AE, Forbes D. A benefit-cost analysis of private and semi-private Hospital rooms. J Benefit Cost Anal 2011;2:1–27. 10.2202/2152-2812.1050 [DOI] [Google Scholar]
- 147.Kosuge R, Kobayashi K, Kakehi A. Comparative studies on hospital-bed management between all single-room wards and mixed multi-bed room wards. Nihon Kenchiku Gakkai Keikakukei Ronbunshu 2013;78:765–73. 10.3130/aija.78.765 [DOI] [Google Scholar]
- 148.Stevens DC, Thompson PA, Helseth CC, et al. A comparison of the direct cost of care in an open-bay and single-family room NICU. J Perinatol 2014;34:830–5. 10.1038/jp.2014.178 [DOI] [PubMed] [Google Scholar]
- 149.Blandfort S, Gregersen M, Rahbek K, et al. Analgesic and psychoactive medications and the risk of falls in relation to delirium in single-bed rooms compared to multiple-bed rooms in geriatric inpatients. Aging Clin Exp Res 2020;32:1493–9. 10.1007/s40520-019-01335-y [DOI] [PubMed] [Google Scholar]
- 150.Reed G, Schmid M. Nursing implementation of single-room maternity care. J Obstet Gynecol Neonatal Nurs 1986;15:386–9. 10.1111/j.1552-6909.1986.tb01411.x [DOI] [PubMed] [Google Scholar]
- 151.Servel A-C, Rideau Batista Novais A. Single-family rooms for neonatal intensive care units impacts on preterm newborns, families, and health-care staff. A systematic literature review. Arch Pediatr 2016;23:921–6. 10.1016/j.arcped.2016.04.022 [DOI] [PubMed] [Google Scholar]
- 152.Shahheidari M, Homer C. Impact of the design of neonatal intensive care units on neonates, staff, and families. J Perinat Neonatal Nurs 2012;26:260–6. 10.1097/JPN.0b013e318261ca1d [DOI] [PubMed] [Google Scholar]
- 153.Soleimani F, Azari N, Ghiasvand H, et al. Do NICU developmental care improve cognitive and motor outcomes for preterm infants? A systematic review and meta-analysis. BMC Pediatr 2020;20:67.:67. 10.1186/s12887-020-1953-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.van de Glind I, de Roode S, Goossensen A. Do patients in hospitals benefit from single rooms? A literature review. Health Policy 2007;84:153–61. 10.1016/j.healthpol.2007.06.002 [DOI] [PubMed] [Google Scholar]
- 155.Kelly R, Brown D, McCance T, et al. The experience of person-centred practice in a 100 % single-room environment in acute care settings-A narrative literature review. J Clin Nurs 2019;28:2369–85. 10.1111/jocn.14729 [DOI] [PubMed] [Google Scholar]
- 156.Saha S, Noble H, Xyrichis A, et al. Mapping the impact of ICU design on patients, families and the ICU team: a scoping review. J Crit Care 2022;67:3–13. 10.1016/j.jcrc.2021.07.002 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-068932supp001.pdf (206.6KB, pdf)
bmjopen-2022-068932supp002.pdf (1.2MB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplemental information.


