Abstract
One hundred ninety-five patients presenting with post-COVID symptomology, including parosmia and dysgeusia, underwent reversible stellate ganglion blockade. Stellate ganglion blockade was performed at an outpatient facility, and patients were evaluated via survey at seven days post-injection. Of the 195 participants, ages ranged from 18–69 years of age with the breakdown of sexes being females n = 157 and males n = 38. The most significant finding was a reported improvement in olfaction post-injection in 87.4% of subjects. The effectiveness of this novel treatment for post-COVID is promising and warrants further investigation.
Keywords: cervical sympathetic block, COVID, parosmia, dysgeusia, dysautonomia
Introduction
Olfactory and gustatory dysfunction are recognized persistent complaints in patients post-COVID infection.1–5 Anosmia, parosmia, and dysgeusia are symptoms that may prompt individuals to seek treatment due to their impact.6 Much existing research focuses on quantitative olfactory dysfunction including anosmia.4,7–12 Parosmia, a qualitative olfactory dysfunction, has been noted in individuals after COVID infection and can have a devastating impact on their quality of life when it persists.6,13,14 The exact mechanism of parosmia is not known, but the response of olfactory dysfunction to stellate ganglion block (SGB) suggests some types of olfactory dysfunction, including parosmia, may be autonomically mediated.15–17 Iannilli et al (2019) suggested a centrally mediated mechanism of parosmia. Using functional magnetic resonance imaging, an increased activation of the thalamus was noted in patients with parosmia compared to those without, an atypical pathway for olfaction.18 Competing theories exist regarding other central mechanisms for parosmia.6,18–22
Persistent symptomology after COVID infection includes a myriad of symptoms that affect mood and cognition and may be related to an overactive sympathetic nervous system (SNS) response.23 The autonomic nervous system innervates most body tissues, and it is integrated with the immune system to respond to inflammatory insults both with and without tissue damage.23–30 In response to viral infection, inflammation is autonomically mediated and may produce hyperinflammation.15 Post-COVID infection, the interdependence of the autonomic system and inflammation create a positive feedback loop that may contribute to the sympathetic hyperresponsiveness and subsequent dysautonomia experienced by some patients.15,31
Both afferent and efferent nerve transmission occurs through the cervical sympathetic ganglia.32 The inferior cervical sympathetic ganglion fuses with the first thoracic ganglion in roughly 80% of individuals to form the stellate ganglion; these ganglia can also be referred to as the stellate ganglion even when not fused.32 Impulses from these ganglia are transmitted to the head, neck, chest, and upper extremities. Information is transmitted along the preganglionic sympathetic fibers before ascending bilateral sympathetic trunks to the cervical ganglia prior to ascending the sympathetic chain to cervical ganglia.32
Historically, cervical sympathetic ganglia have been reversibly blocked using local anesthetic to restore autonomic balance between the sympathetic and parasympathetic systems.23 Ultrasound-guided placement of local anesthetic at the stellate ganglion or other sites along the cervical sympathetic chain have been used for treatment of various conditions related to these autonomic nerves including pain, vascular, and gastric symptoms.16,23,33,34 Case reports detail a rapid reduction of symptomology in response to a reversible blockade of the cervical sympathetic ganglia — predominantly fatigue, concentration, depression, and anxiety — and affects those areas of the brain and peripheral nervous systems involved in immune function.23,35 An interruption of nerve transmission through the cervical sympathetic ganglia may provide an opportunity for the resumption of normal autonomic function.23 The durable effects of a SGB may allow the sympathetic nervous system to reset sufficiently to provide relief from inflammation and inflammatory sequelae post-COVID infection.
Methods
This retrospective chart review was determined exempt from human subjects’ review by Texas Christian University’s Institutional Review Board (IRB) since this data collection required no intervention with living individuals and no identifying information was collected. This research was conducted in accordance with the Declaration of Helsinki and a waiver of informed consent was granted by TCU’s IRB since the research was done post-procedure with minimal risk of identification of participants given the large sample size.
A convenience sample of 195 subjects was selected from a cohort of patients who presented to a single clinic for treatment of reported fatigue, parosmia, and dysgeusia after COVID infection. Prior to receiving SGB, subjects completed a questionnaire rating their symptoms from a list of common post-COVID symptoms. Using a Likert scale of “0” to indicate “none” and “10” to represent “most severe” — subjects indicated the severity of their symptoms both pre- and post-COVID infection (see Table 1).
Table 1.
Pre- and Post-COVID Symptoms — Questionnaire Completed by Patients Prior to SGB
| Pre-COVID | Post-COVID | Mean Difference | t | p* | Cohen’s d | |||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||||
| Fatigue | 1.48 | 1.78 | 5.03 | 3.28 | −3.55 | −12.26 | <0.001 | −1.267 |
| Cough | 0.18 | 0.71 | 1.00 | 2.10 | −0.82 | −4.39 | 0.00 | −0.448 |
| Dyspnea | 0.35 | 0.80 | 1.64 | 2.46 | −1.29 | −5.78 | <0.001 | −0.601 |
| Chest Pain | 0.03 | 0.23 | 0.31 | 0.97 | −0.28 | −2.85 | 0.04 | −0.308 |
| Memory and Concentration | 1.05 | 1.47 | 5.16 | 3.18 | −4.11 | −13.47 | <0.001 | −1.390 |
| Sleep Issues | 1.55 | 2.28 | 3.60 | 3.61 | −2.05 | −7.18 | <0.001 | −0.740 |
| Muscle Pain and Headache | 1.57 | 2.19 | 4.37 | 3.94 | −2.79 | −7.90 | <0.001 | −0.820 |
| Fast or Pounding Heart Rate | 0.15 | 0.66 | 1.51 | 2.48 | −1.36 | −5.54 | 0.00 | −0.572 |
| Loss Distortion of smell or taste | 0.11 | 1.01 | 8.89 | 2.34 | −8.77 | −32.83 | <0.001 | −3.387 |
| Depression or Anxiety | 1.88 | 2.46 | 5.00 | 3.59 | −3.12 | −9.24 | <0.001 | −0.958 |
| Fever | 0.00 | 0.00 | 0.10 | 0.75 | −0.10 | −1.37 | 0.32 | −0.14 |
| Dizziness upon Standing | 0.41 | 1.06 | 2.74 | 3.01 | −2.33 | −7.87 | <0.001 | −0.818 |
| Postexertional Malaise | 0.46 | 1.10 | 3.04 | 3.35 | −2.58 | −8.31 | <0.001 | −0.852 |
Note: *p-values were calculated using bootstrapping based on 1000 bootstrap samples.
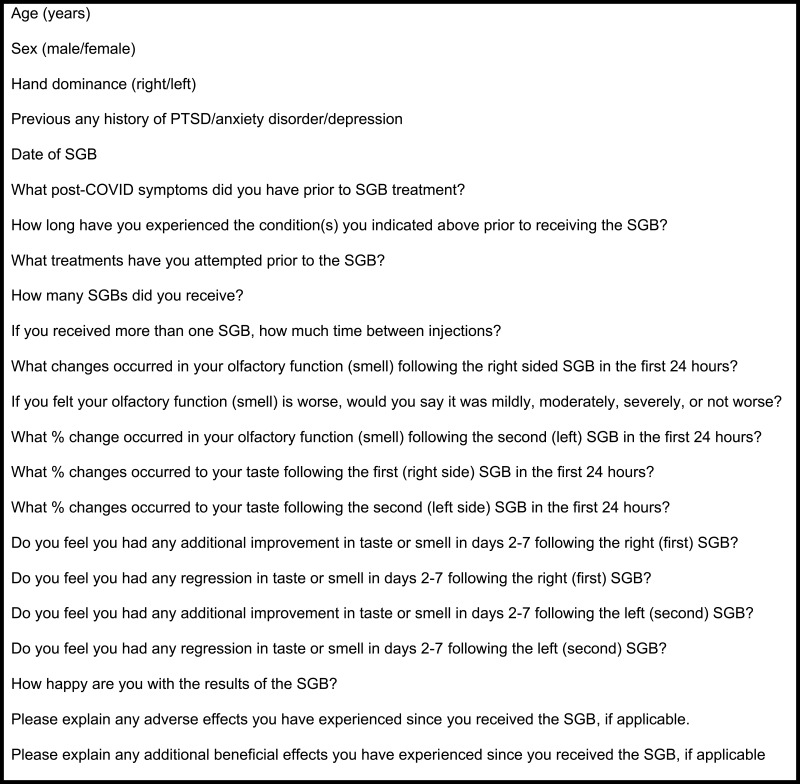
Informed consent was obtained, and subjects were treated with stellate ganglion block. Subjects were placed in a supine position with head elevated. Following aseptic skin preparation, the medial border of the sternocleidomastoid muscle at the level of the cricoid ring was identified by palpation. A high-frequency, linear ultrasound transducer was placed at this location in a transverse plane. Ultrasound visualization of the characteristic “camel-humped” anterior tubercle confirmed the location of the sixth cervical vertebrae (C6). Color Doppler mode was activated to identify the proximity of the inferior thyroid artery and any further vasculature to the intended needle path. Skin and superficial soft tissues were anesthetized using a small volume of lidocaine 1%, and a 25-gauge, short-bevel needle was introduced in-plane beneath the transducer. Utilizing a lateral to medial approach, the needle was advanced under direct ultrasound visualization until it reached the pre-fascial surface of the longus colli muscle at the level of the C6. Injection of one mL of normal saline revealed hydro-dissection within the anterior fascial plane of the longus colli muscle. After confirming negative aspiration of blood, lidocaine 1% 6 mL and preservative-free dexamethasone 4 mg were then injected into the interfascial plane. The needle was removed with gentle pressure applied to the injection site. Subjects were closely observed for any indications of intravascular or intraneural injection. Ipsilateral miosis and ptosis were confirmed and documented. Subjects were presented with a standardized survey within seven days following treatment to evaluate subjective effects on previous symptomology. Demographic data and symptomology were reported via survey (Figure 1 and Table 2). Responses were compiled, and data was generated from survey results to allow for statistical analysis.
Figure 1.
Data Collected on Google Survey Form.
Table 2.
Demographics of Data of the Study Cohort (n = 195)
| Variable | Total | Female | Male |
|---|---|---|---|
| Gender n(%) | 195 | 157 (80.5%) | 38 (19.5%) |
| Age mean (range) | 38.58 (18–76) | 37.1 (18–63) | 41.1 (18–69) |
| Self-report mental health issuea,b n(%) | |||
| No | 104 (53.3%) | 76 (48.4%) | 28 (73.7%) |
| Yes | 91 (46.7%) | 81 (51.6%) | 10 (26.3%) |
Notes: aPatient reported at least one of the mental health issues including anxiety, depression, or PTSD. bChi-Square = 7.85, p = 0.005.
Results
Patients were enrolled from February 2022 through July 2022. The study cohort included 195 patients with 157 females and 38 males, ranging in age from 18–69 years undergoing stellate ganglion blockade (SGB) for parosmia and/or dysgeusia. Approximately seven days post-SGB the patients completed a self-reported survey (see Figure 1). The most significant results noted on the survey were the responses to the items “olfactory function (smell)” and “taste” along with “How happy are you with the results of the SGB?”. While only 81.5% of subjects received a left SGB in addition to their right SGB, 100% of subjects completed the questionnaire for the right and left SGB. The following results pertain to right-sided SGB in the first 24 hours. Some patients reported that they were “not happy” with the results of the SGB despite reporting improvements in their smell (n = 15) and taste (n = 18) after treatment. 75.4% (n = 147) of patients treated reported an improvement in smell after SGB; 89.8% (n = 132) of those patients reporting improved smell also reported being “somewhat happy” or “very happy” with their results (p < 0.001) (see Table 3). 74.4% (n = 145) of patients treated reported an improvement in taste after SGB; 87.6% (n = 127) of those patients reporting improved taste also reported being “somewhat happy” or “very happy” with their results (p < 0.001) (see Table 3).
Table 3.
Relationship Between Self-Report of Happiness Regarding the SGC Results and Smell/Taste Improvement After Right and Left Sided SGB in the First 24 Hours (n = 195 Each Side)
| Happiness Rating Regarding the SGB Results | Smell | Taste | ||
|---|---|---|---|---|
| Reported No Change N (%) | Reported Improvement N (%) | Reported No Change N (%) | Reported Improvement N (%) | |
| SGB Right | Chi-Square=56.72 | p<0.001 | Chi-Square=36.94 | p<0.001 |
| Not happy | 30 (62.5%) | 15 (10.2%) | 27 (54.0%) | 18 (12.4%) |
| Somewhat Happy | 11(22.9%) | 59 (40.1%) | 13 (26.0%) | 57 (39.1%) |
| Very happy | 7 (14.6%) | 73 (49.7%) | 10 (12.5%) | 70 (48.3%) |
| SGB Left | Chi-Square=23.53 | p<0.001 | Chi-Square=20.12 | p<0.001 |
| Not happy | 37 (36.6%) | 8 (8.5%) | 28 (40.0%) | 17 (13.6%) |
| Somewhat Happy | 34 (33.7%) | 36 (38.3%) | 25 (35.7%) | 45 (36.0%) |
| Very happy | 30 (29.7%) | 50 (53.2%) | 17 (24.3%) | 63 (50.4%) |
Discussion
Patients post-COVID with residual symptomology negatively impacting daily life, including significant parosmia and/or dysgeusia, are seeking effective treatments.36 SGB, normally employed for pain, vascular and gastric symptoms, is being employed as a novel therapy post-COVID.23 SGB was found to be effective in attenuating or ameliorating the parosmia and dysgeusia in this cohort and in those individuals with a history of COVID infection.18,26 Reported relief from additional autonomic-mediated symptomology — including anxiety and insomnia — in response to SGB has encouraged further exploration of sympathetic and parasympathetic responses to cervical sympathetic blockade for the treatment of symptoms attributable to dysautonomia.23
The etiology of dysautonomia secondary to inflammation is commonly attributed to sympathetic nervous system hyperresponsiveness.23 While the interruption of sympathetic input is evidenced when eliciting Horner syndrome during cervical sympathectomy, parasympathetic system hypo-responsiveness may explain some of the perturbations.23,37 The contribution of the parasympathetic nervous system function to dysautonomia should be considered in prospective studies evaluating the effects of cervical sympathectomies.
And finally, 46.7% (n = 91) of the respondents self-reported experiencing anxiety, depression, post-traumatic stress disorder, or a combination of these findings along with reports of symptoms of dysautonomia. Valid, reliable reporting of mental health histories may be beneficial when evaluating effectiveness of cervical sympathectomy in conjunction with expanding the scope of this treatment from parosmia and dysgeusia to dysautonomia since some respondents favorably reported responses to treatment without corresponding improvement in their taste or smell (see Table 3). Further investigation of the use of SGB for the treatment of dysautonomia is warranted.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Bagheri S, Asghari A, Farhadi M, et al. Coincidence of COVID-19 epidemic and olfactory dysfunction outbreak in Iran. Med J Islam Repub Iran. 2020;34:62. doi: 10.34171/mjiri.34.62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Giacomelli A, Pezzati L, Conti F, et al. Self-reported olfactory and taste disorders in patients with severe acute respiratory coronavirus 2 infection: a cross-sectional study. Clin Infect Dis. 2020;71:889–890. doi: 10.1093/cid/ciaa330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gorzkowski V, Bevilacqua S, Charmillon A, et al. Evolution of Olfactory Disorders in COVID-19 Patients. Laryngoscope. 2020;130:2667–2673. doi: 10.1002/lary.28957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Meng X, Deng Y, Dai Z, Meng Z. COVID-19 and anosmia: a review based on up-to-date knowledge. Am J Otolaryngol. 2020;41:102581. doi: 10.1016/j.amjoto.2020.102581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Spinato G, Fabbris C, Polesel J, et al. Alterations in smell or taste in mildly symptomatic outpatients with SARS-CoV-2 infection. JAMA. 2020;323:2089–2090. doi: 10.1001/jama.2020.6771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lerner D, Garvey K, Arrighi-Allisan A, et al. Clinical Features of Parosmia Associated With COVID-19 Infection. Laryngoscope. 2022;132(3):633–639. doi: 10.1002/lary.29982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Eliezer M, Hautefort C, Hamel A, et al. Sudden and complete olfactory loss of function as a possible symptom of COVID-19. JAMA Otolaryngol Head Neck Surg. 2020;146:674–675. doi: 10.1001/jamaoto.2020.0832 [DOI] [PubMed] [Google Scholar]
- 8.Moein S, Hashemian S, Mansourafshar B, Khorram-Tousi A, Tabarsi P, Doty R. Smell dysfunction: a biomarker for COVID-19. Int Forum Allergy Rhinol. 2020;10:944–950. doi: 10.1002/alr.22587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pierron D, Pereda-Loth V, Mantel M, et al. Smell and taste changes are early indicators of the COVID-19 pandemic and political decision effectiveness. Nat Commun. 2020;11:5152. doi: 10.1038/s41467-020-18963-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tong J, Wong A, Zhu D, Fastenberg J, Tham T. The prevalence of olfactory and gustatory dysfunction in COVID-19 patients: a systematic review and meta-analysis. Otolaryngol Head Neck Surg. 2020;163:3–11. doi: 10.1177/0194599820926473 [DOI] [PubMed] [Google Scholar]
- 11.Vaira L, Salzano G, Deiana G, De Riu G. Anosmia and ageusia: common findings in COVID-19 patients. Laryngoscope. 2020;130:1787. doi: 10.1002/lary.28692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Whitcroft K, Hummel T. Olfactory dysfunction in COVID-19: diagnosis and management. JAMA. 2020;323:2512–2514. doi: 10.1001/jama.2020.8391 [DOI] [PubMed] [Google Scholar]
- 13.Ercoli T, Masala C, Pinna I, et al. Qualitative smell/taste disorders as sequelae of acute COVID-19. Neurol Sci. 2021;42(12):4921–4926. doi: 10.1007/s10072-021-05611-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Parma V, Ohla K, Veldhuizen MG, et al. More than smell—COVID-19 is associated with severe impairment of smell, taste, and chemesthesis. Chem Senses. 2020;45:609–622. doi: 10.1093/chemse/bjaa041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chauhan G, Upadhyay A, Khanduja S, Emerick T. Stellate ganglion block for anosmia and dysgeusia due to long COVID. Cureus. 2022;14(8):e27779. doi: 10.7759/cureus.27779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liu L, Duricka D. Stellate ganglion block reduces symptoms of Long COVID: a case series. J Neuroimmunol. 2022;362:577784. doi: 10.1016/j.jneuroim.2021.577784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moon H, Chon J, Lee S, Ju Y, Sung C. Long-term results of stellate ganglion block in patients with olfactory dysfunction. Korean J Pain. 2013;26(1):57–61. doi: 10.3344/kjp.2013.26.1.57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Iannilli E, Leopold D, Hornung D, Hummel T. Advances in understanding parosmia: an fMRI study. ORL J Otorhinolaryngol Relat Spec. 2019;81:185–192. doi: 10.1159/000500558 [DOI] [PubMed] [Google Scholar]
- 19.Hummel T, Whitcroft K, Andrews P, et al. Position paper on olfactory dysfunction. Rhinol Suppl. 2017;54(26):1–30. doi: 10.4193/Rhino16.248 [DOI] [PubMed] [Google Scholar]
- 20.Leopold D. Distortion of olfactory perception: diagnosis and treatment. Chem Senses. 2002;27:611–615. doi: 10.1093/chemse/27.7.611 [DOI] [PubMed] [Google Scholar]
- 21.Tan C, Tan B, Tan X, et al. Neuroradiological Basis of COVID‐19 Olfactory Dysfunction: a Systematic Review and Meta‐Analysis. Laryngoscope. 2022;132:1260–1274. doi: 10.1002/lary.30078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Parker J, Kelly C, Gane S. Molecular mechanism of parosmia. medRxiv. 2021. doi: 10.1101/2021.02.21251085 [DOI] [Google Scholar]
- 23.Fischer L, Barop H, Ludin S, Schaible H. Regulation of acute reflectory hyperinflammation in viral and other diseases by means of stellate ganglion block. A conceptual view with a focus on COVID-19. Auton Neurosci. 2022;237:102903. doi: 10.1016/j.autneu.2021.102903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Elenkov I, Wilder R, Chrousos G, Vizi E. The sympathetic nerve–an integrative interface between two supersystems: the brain and the immune system. Pharmacol Rev. 2000;52(4):595–638. [PubMed] [Google Scholar]
- 25.Grebe K, Takeda K, Hickman H, et al. Cutting edge: sympathetic nervous system increases proinflammatory cytokines and exacerbates influenza a virus pathogenesis. J Immunol. 2010;184(2):540–544. doi: 10.4049/jimmunol.0903395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Janig W. Autonomic nervous system and inflammation. Auton Neurosci. 2014;182:1–3. doi: 10.1016/j.autneu.2014.02.002 [DOI] [PubMed] [Google Scholar]
- 27.Libby P, Luscher T. COVID-19 is, in the end, an endothelial disease. Eur Heart J. 2020;41(32):3038–3044. doi: 10.1093/eurheartj/ehaa623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Steenblock C, Todorov V, Kanczkowski W, et al. Severe acute respiratory syndrome Coronavirus 2 (SARS-CoV-2) and the neuroendocrine stress axis. Mol Psychiatry. 2020:1–7. doi: 10.1038/s41380-020-0758-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tracey K. The inflammatory reflex. Nature. 2002;420(6917):853–859. doi: 10.1038/nature01321 [DOI] [PubMed] [Google Scholar]
- 30.Tracey K. Reflex control of immunity. Nat Rev Immunol. 2009;9(6):418–428. doi: 10.1038/nri2566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.DeVere R. Disorders of taste and smell. Continuum. 2017;23:421–446. doi: 10.1212/CON.0000000000000463 [DOI] [PubMed] [Google Scholar]
- 32.Ellis H, Lawson H. Anatomy for Anaesthetists. 9 ed. Wiley Blackwell; 2014. [Google Scholar]
- 33.Liu M, Tian J, Su Y, Wang T, Xiang Q, Wen L. Cervical sympathetic block regulates early systemic inflammatory response in severe trauma patients. Med Sci Monit. 2013;19:194–201. doi: 10.12659/MSM.883833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Xie A, Zhang X, Ju F, Li W, Zhou Y, Wu D. Effects of the ultrasound-guided stellate ganglion block on hemodynamics, stress response, and gastrointestinal function in postoperative patients with colorectal cancer. Comput Intell Neurosci. 2022;2056969. doi: 10.1155/2022/2056969 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 35.Westerhaus M. Loewy. Central representation of the sympathetic nervous system in the cerebral cortex. Brain Res. 2001;903(1–2):117–127. doi: 10.1016/s0006-8993(01 [DOI] [PubMed] [Google Scholar]
- 36.Cho S. Clinical diagnosis and treatment of olfactory dysfunction. Hanyang Med Rev. 2014;34:107. doi: 10.7599/hmr.2014.34.3.107 [DOI] [Google Scholar]
- 37.Kang P, Kloke J, Jain S. Olfactory dysfunction and parasympathetic dysautonomia in Parkinson’s disease. Clin Auton Res. 2012;22(4):161–166. doi: 10.1007/s10286-012-0158-6 [DOI] [PMC free article] [PubMed] [Google Scholar]