Abstract
Aim
This systematic review examined recent studies on fragmented care of patients with chronic illnesses in the United States to examine the association between fragmented care and patient outcomes.
Design
Systematic review.
Methods
Studies published from January 1, 2012, to June 1, 2022, were selected from four electronic databases (PubMed, CINAHL, PsycINFO, and Web of Science), following the Cochrane protocols and PRISMA statements. Based on inclusion and exclusion criteria, ten studies that examined associations published between 2015 and 2021 were selected. A methodological assessment was conducted with the Quality Assessment Tool for Observational Cohort and Cross‐Sectional Studies. The studies selected for this systematic review were rated as having fair methodological rigor. The protocol of this review was registered in the International Prospective Register of Systematic Reviews (PROSPERO registration number: CRD42021285379). Because of the heterogeneity of the selected studies' data, a systematic narrative synthesis of the extracted data was conducted.
Results
Three common measures for fragmented care and outcomes were synthesized. A synthesis of the studies found significant association between fragmented care and adverse outcomes of chronic illnesses (emergency department visits, utilization of diagnostic tests, and healthcare costs). Despite the heterogeneity of significant findings between fragmented care and patient outcomes, the relationship between these outcomes and fragmented care was significant. This systematic review provides clear evidence of the association between care fragmentation and its adverse effects on individuals with chronic illnesses. However, mixed relationship findings were also reported.
Conclusion
Given the demands of overcoming fragmented care in healthcare settings in the United States, nurse managers, healthcare leaders, and policymakers should utilize this evidence to reduce fragmented care strategies. It is recommended that nurse researchers and other healthcare practitioners conduct further studies to understand the contexts and mechanisms of fragmented care and develop theoretical frameworks for care fragmentation and chronic illness outcomes.
Keywords: care fragmentation, chronic illnesses, fragmented care, healthcare cost, hospital utilization, patient outcomes, systematic review
1. INTRODUCTION
More than 47% of the US population has at least one chronic illness, and almost 30 million people suffer from multiple chronic illnesses (Centers for Disease Control and Prevention [CDC], 2021). These diseases are responsible for $3.8 trillion in annual healthcare costs and are the leading causes of high care requirement, death, and disability; moreover, about 50% of index hospitalizations (referred to hospitalizations with procedures performed on patients; Ejaz et al., 2016) are readmissions (referred to rehospitalizations within 30 days of discharge from index hospitalizations; Ejaz et al., 2016) or nonindex hospital readmissions (referred to readmissions with different hospital ID numbers for the initial hospitalization and readmission; Chappidi et al., 2017) within 30 days of discharge (Brunner‐La Rocca et al., 2020; CDC, 2021). One reason chronic illness care is in such a state of crisis is care fragmentation, or the state of limited, noncontinuous, episodic, and disorganized care across multiple healthcare practitioners and settings (Bilazarian, 2021; Joo, 2014).
1.1. Background
Fragmented care has been an issue for more than a decade in the healthcare system of the US. Various policies have been formulated, and healthcare models have been conducted to defragment healthcare and provide seamless care (Agha et al., 2017; Cohen‐Mekelburg et al., 2019). There is no common operative definition for fragmented care for individuals with chronic illnesses in healthcare research; it is broadly defined as “care that is poorly coordinated among multiple providers and organizations (Bilazarian, 2021, p. 129) or lack of continuous care” (Liu & Yeung, 2013; Nothelle et al., 2022).
Individuals with chronic illnesses experience high rates of care fragmentation because they often require lifelong continuous care (Kaltenborn et al., 2021). Over time, the services they receive from healthcare practitioners may be limited or redundant, and they may fall into transitional care gaps between healthcare institutions (Galvin, 2019; Joo & Liu, 2021). This is a problem because fragmented care is correlated with adverse patient outcomes, such as overuse of healthcare services and mortality rates (Kern, 2018).
Two major policy initiatives (the Health Information Technology for Economic and Clinical Health [HITECH] Act of 2009 and the Medicare and Medicaid Electronic Health Record [HER] Incentive Programs) were launched to share data of patients across healthcare institutions to reduce fragmented care in the US (Holmgren et al., 2018; Walunas et al., 2017). However, the impact on patient data sharing and its conjunction with fragmentation is vague (Evans, 2016; Walunas et al., 2017).
Some promising research has shown that patient‐centered care, such as case management or coordinated care, can overcome care fragmentation for individuals with chronic illnesses (Joo & Liu, 2017; McKay et al., 2019). To date, however, few studies have investigated the association between fragmented care and chronic illness outcomes, and no review has synthesized recent evidence of these associations in the US. One review examined interhospital care fragmentation and patient outcomes internationally among mixed disease populations (Snow et al., 2020). In this review, we found that fragmented care increased the length of hospital stay and subsequent readmissions to hospitals (Snow et al., 2020). However, this review focused only on interhospital care fragmentation, which is narrow and comparable to various types of fragmentation and disease populations (Snow et al., 2020). Therefore, this study aimed to systematically review recent evidence for association between fragmented care and outcomes of patients with chronic illnesses in the US.
1.2. Purpose
This systematic review aimed to review and collate recent evidence on the association between fragmented care and outcomes in patients with chronic illnesses. The review was limited to empirical studies published between January 1, 2012, and June 1, 2022, to seek the most recent years of evidence of research. The main research question was “how does fragmented care affect outcomes such as hospital use, risk of comorbidities, and healthcare costs, in patients with chronic illness(es) in the US?”
2. METHODS
2.1. Study design
This systematic review was guided by the Cochrane Handbook for Systematic Reviews of Interventions (version 6.2; Higgins & Thomas, 2021). The Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) Statement was also used to refine the report (Page et al., 2021). The protocol of this review was registered in the International Prospective Register of Systematic Reviews (PROSPERO registration number: CRD42021285379). Because this review was not a human subject study, an approval from the institutional review board was not applicable.
2.2. Search strategy
In June 2022, four electronic bibliographic databases, PubMed, CINAHL, PsycINFO, and Web of Science, were searched to identify relevant studies, published between January 1, 2012, and June 1, 2022. The following Medical Subject Headings (MeSH) and key terms were combined with operators: “fragmented care” or “care fragmentation” or “fragmented ambulatory care” or “fragmentation of care” and “chronic disease” or “chronic illness” or “chronic condition.” The following keywords were used: patient care, episode of care, continuity of patient care, discharge, discharge care, hospital use, comorbidity, mortality, healthcare cost, emergency department visits, hospital readmission, and patient outcome. The PubMed pilot search was used to refine the most appropriate entry terms. The final search strings for the four selected databases were combined with operators with Mesh, key terms, and additional keywords. On June 1, 2022, the titles, abstracts, and keywords were searched using key terms. A confirmation search was conducted on June 30, 2022.
2.3. Inclusion and exclusion criteria
To examine the risk of care fragmentation and its associated risk of patient outcomes, this review chose studies focused on settings, such as hospitals, clinics, or ambulatory departments. The inclusion criteria were as follows: (1) quantitative (including descriptive studies; for example, correlational, cross‐sectional, cohort, or case–control designs) studies; (2) studies with adult participants (18 years or older) who were diagnosed with chronic diseases, had been admitted and discharged from index healthcare institutions (hospitals or clinics), had visited or had been readmitted to index or nonindex healthcare institutions, and had transitioned from healthcare institutions to living in their communities; (3) studies focusing on fragmented care between hospitals or clinics delivered to patients with chronic illnesses and conducted in community‐based settings after discharge from hospitals or clinic visits; (4) studies that measured fragmented care and reported patient outcomes, such as hospital usage, risk of comorbidities, or healthcare costs; and (5) studies conducted in the US and published in peer‐reviewed journals in English.
The exclusion criteria for the review were as follows: studies targeting interhospital care fragmentation and its patient outcomes, studies of treatment of postoperative surgery or following postoperative discharge care and its outcomes with chronic illnesses, studies reporting patients' outcomes for anything other than hospital‐to‐community fragmented care, studies conducted outside the US, or studies of care that otherwise do not meet the definition of “fragmented care” or “chronic disease.”
2.4. Study selection
Figure 1 presents a PRISMA flow diagram of the study selection and screening process. From the four electronic databases, 324 articles were initially identified, which became 131 after duplicates were removed using EndNote X9 (Thomson Reuters, Philadelphia). Title and abstract screens excluded another 117 studies. The full texts of the 14 remaining articles were reviewed for eligibility. Among these, four were excluded because the target population did not meet the inclusion criteria (n = 2) or because the studies were conducted outside the US (n = 2). The researcher performed the search with the research team, two research assistants (a professor emeritus and a doctoral student), checked the selection process for accuracy.
FIGURE 1.
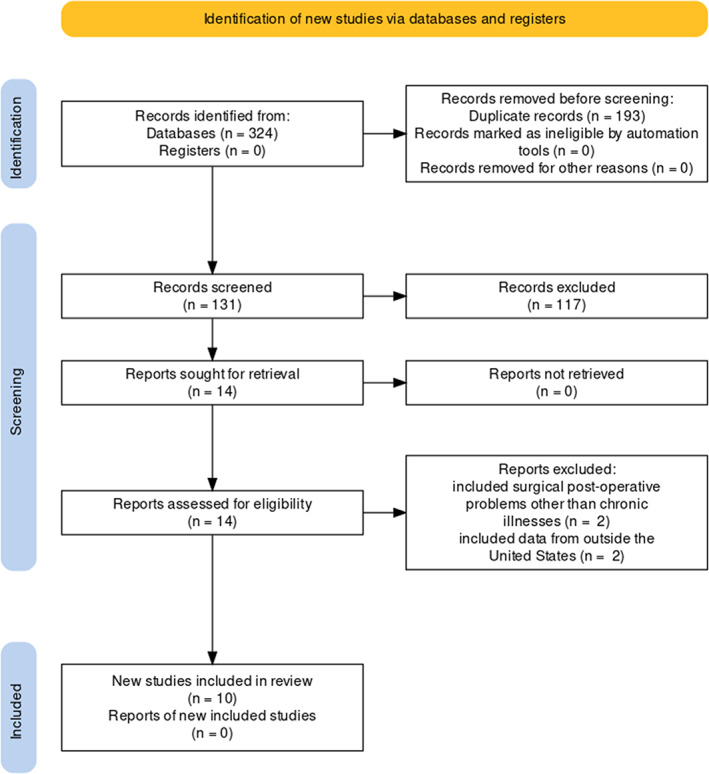
PRISMA flowchart
2.5. Quality appraisal
The Quality Assessment Tool for Observational Cohort and Cross‐Sectional Studies was used to assess the methodological quality of the selected studies (National Institutes of Health [NIH], 2021). This tool was developed by the NIH and consists of 14 “yes,” “no,” or “other” questions assessing study design, sample, measure of exposure and outcomes, and statistical analysis. The sum of the 14 items yields a rating of poor (scored 0; 0–4 of 14 questions), fair (scored i; 5–10), and good (scored ii; 11–14).
The researcher conducted the quality appraisal with the research assistant (a professor emeritus), and the research assistant confirmed the scores. The studies selected for this review were rated as having fair methodological rigor (see Table 1).
TABLE 1.
Quality appraisal of included studies
| Cohen‐Mekelburg et al. (2019) | Frandsen et al. (2015) | Kaltenborn et al. (2021) | Kern et al. (2017) | Kern et al. (2018) | Kern et al. (2019) | Kern et al. (2021) | Pinheiro et al. (2021) | Qayed and Muftah (2018) | Walunas et al. (2017) | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Was the research question or objective in this paper clearly stated? | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| 2. Was the study population clearly specified and defined? | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| 3. Was the participation rate of eligible persons at least 50%? | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| 4. Were all the subjects selected or recruited from the same or similar populations (including the same time period)? Were inclusion and exclusion criteria for being in the study prespecified and applied uniformly to all participants? | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| 5. Was a sample size justification, power description, or variance and effect estimates provided? | N | N | N | N | N | N | N | N | N | N |
| 6. For the analyses in this paper, were the exposure(s) of interest measured prior to the outcome(s) being measured? | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| 7. Was the timeframe sufficient so that one could reasonably expect to see an association between exposure and outcome if it existed? | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| 8. For exposures that can vary in amount or level, did the study examine different levels of the exposure as related to the outcome (e.g., categories of exposure, or exposure measured as continuous variable)? | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| 9. Were the exposure measures (independent variables) clearly defined, valid, reliable, and implemented consistently across all study participants? | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| 10. Was the exposure(s) assessed more than once over time? | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| 11. Were the outcome measures (dependent variables) clearly defined, valid, reliable, and implemented consistently across all study participants? | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| 12. Were the outcome assessors blinded to the exposure status of participants? | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| 13. Was loss to follow‐up after baseline 20% or less? | N | N | N | N | N | N | N | N | N | N |
| 14. Were key potential confounding variables measured and adjusted statistically for their impact on the relationship between exposure(s) and outcome(s)? | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Summary quality rating | i | i | i | i | i | i | i | i | i | i |
Note: i, fair; N, no; NA, not applicable; NR, not reported; Y, yes.
2.6. Data extraction and synthesis
The following information was extracted from the studies under review: author(s), year, aim, design, participants, measure of fragmented care, measure of patient outcomes, data analysis, and significant association between fragmented care and patient outcomes. These data were then tabulated (Table 2).
TABLE 2.
Characteristics of included studies
| Authors (year) | Study design | Sample | Aim | Measure of fragmented care | Measures of patient outcomes | Analysis | Key findings and significance (p > 0.05) of the association with fragmented care |
|---|---|---|---|---|---|---|---|
| Mean age | |||||||
| Number of samples | |||||||
| Data source | |||||||
| Country | |||||||
|
Cohen‐Mekelburg et al. (2019) USA |
Retrospective cohort study |
|
To determine the prevalence of fragmentation among hospitalized patients and identify associated predictors and visit‐level outcomes | Readmission to a nonindex (different) hospital |
|
Multivariable logistic regression | Fragmented inpatient care is associated with a higher likelihood of in‐hospital death, higher rates of inpatient colonoscopy, and a longer readmission LOS |
|
Frandsen et al. (2015) USA |
Retrospective cohort study |
|
To assess the relationship between care fragmentation and both quality and costs of care for chronically ill patients | Reversed HHI: the fragmentation score is 1—HHI; a higher value indicated more fragmentation |
|
Regression |
Patients of primary care providers with high fragmentation had higher rates of preventable hospitalizations (9.1% in highest quartile versus 7.1% in lowest quartile; p < 0.001) High fragmentation was associated with $4542 higher healthcare spending ($10,396 in the highest quartile versus $5854 in the lowest quartile; p < 0.001) |
|
Kaltenborn et al. (2021) USA |
Retrospective cohort analysis |
|
To determine the prevalence of superutilizers (defined as four or more inpatient encounters in a 1‐year period) who receive fragmented care across different hospitals and to describe associated risks, costs, and health outcomes | The number of a nonindex acute hospitals used over a 1‐year period |
|
Multivariate Poisson regression | Patients with fragmentation were more likely to be admitted for chronic disease management, psychiatric illness, and substance abuse. Inpatient fragmentation was associated with higher yearly costs |
|
Kern et al. (2017) USA |
Cross‐sectional study |
|
To determine whether more fragmented care is associated with more radiology and other diagnostic tests, compared with less fragmented care | Reversed BBI: the fragmentation score is 1—BBI; a higher value indicated more fragmented care |
|
Negative binomial regression |
Patients with the most fragmented care had approximately twice as many radiology and other diagnostic tests as patients with the least fragmented care, across all groups stratified by number of chronic conditions (each adjusted p < 0.0001) Among patients with ≥5 chronic conditions, those with the least fragmented care had 258 tests per 100 patients, and those with the most fragmented care had 542 tests per 100 patients (+284 tests per 100 patients, or +110%, adjusted p < 0.0001) |
|
Kern et al. (2018) USA |
Retrospective cohort study |
|
To determine the associations between fragmented ambulatory care and subsequent ED visits and hospital admissions, while considering possible interactions between fragmentation and number of chronic conditions | Reversed BBI: the fragmentation score is 1 – BBI; a higher value indicated more fragmented care |
|
Multivariable logistic regression | Among those with 1–2 or 3–4 chronic conditions, having the most (versus the least) fragmented care significantly increased the hazard of an ED visit and, separately, increased the hazard of an admission (adjusted p < 0.05 for each comparison) |
|
Kern et al. (2019) USA |
Retrospective cohort study |
|
To determine the associations between fragmented ambulatory care and subsequent ED visits and hospital admissions, while considering possible interactions between fragmentation and number of chronic conditions with Medicaid beneficiaries | Reversed BBI: the fragmentation score is 1—BBI; a higher value indicated more fragmented care |
|
Multivariable logistic regression |
For every 0.1‐point increase in fragmentation score, the adjusted hazard of an ED visits over 2 years of follow‐up increased by 1.7% (CI = 0.5%, 2.9%) Having more fragmented care was not associated with a change in the hazard of a hospital admission |
|
Kern et al. (2021) USA |
Retrospective cohort study |
|
To determine whether fragmented care is associated with the risk of incident CHD events, overall and stratified by self‐rated general health | Reversed BBI: the fragmentation score is 1—BBI; a higher value indicated more fragmented care |
|
Cox proportional hazards models Poisson regression |
Overall, the adjusted hazard ratio for the association between high fragmentation and incident CHD events was 1.14 (CI = 0.92, 1.39). Among those with very good or good self‐rated health, high fragmentation was associated with an increased hazard of CHD events (adjusted hazard ratio 1.35; CI = 1.06, 1.73; p = 0.01). There was no association among those with excellent self‐rated health |
|
Pinheiro et al. (2021) USA |
Retrospective cohort study |
|
To determine associations between fragmentation and cardiovascular disease risk factor control among survivors overall and by self‐rated health | Reversed BBI: the fragmentation score is 1—BBI; a higher value indicated more fragmented care |
|
Multivariable logistic regression | Among cancer survivors, more fragmentation was associated with a decreased likelihood of diabetes control (OR 0.78; CI = 0.61, 0.99), adjusting for confounders. However, associations were not observed for control of hypertension or hyperlipidemia |
|
Qayed and Muftah (2018) USA |
Retrospective cohort study |
|
To evaluate rates and predictors of hospital readmission and care fragmentation in patients hospitalized with gastroparesis | Readmission to a nonindex hospital (i.e., different from the hospital of the index admission) |
|
Logistic regression | Patients who were readmitted to a nonindex hospital (care fragmentation) had longer LOS (6.5 vs. 5.8 days, p = 0.03), and higher mean hospitalization cost ($15,645 versus $12,311, p < 0.0001), compared to those readmitted to the index hospital. There were no differences in mortality (1.0% vs. 1.3%, p = 0.84), and 60‐days readmission rate (55.3% vs. 54.6%, p = 0.99) between with or without care fragmentation |
|
Walunas et al. (2017) USA |
Retrospective cohort study |
|
To examine the impact of care fragmentation across multiple health care institutions on disease outcomes in patients with SLE | Having one or more healthcare institution visits with a SLE |
|
Logistic regression | Identified increased risk of infections (OR 1.57, CI = 1.30, 1.88), cardiovascular disease (OR 1.51, CI = 1.23, 1.86), end‐stage renal disease (OR 1.34, CI = 1.05, 1.70), nephritis (OR 1.28, CI = 1.07, 1.54), and stroke (OR 1.28, CI = 1.01, 1.62) among patients with fragmented care, adjusted for age, sex, race, insurance status, length of follow‐up time, and total visit count. Care fragmentation is associated with increased risk of severe infection and comorbidities |
Abbreviations: BBI, Bice‐Boxerman Index; CHD, coronary heart disease; CI, 95% confidence interval; ED, emergency department; HHI, Herfindahl–Hirschman concentration index; IBD, Inflammatory bowel disease; LOS, length of stay; NR, not reported; OR, odd ratio; PCP, primary care provider; SD, standard deviation; SLE, systemic lupus erythematosus.
Because of the heterogeneity of these data, a systematic narrative synthesis of the extracted data was conducted (Higgins & Thomas, 2021). Three common measures for fragmented care and outcomes were synthesized. The researcher and a research assistant (a professor emeritus) extracted and synthesized the studies' data blindly in the review, and the research assistant checked the accuracy.
3. RESULTS
3.1. Study characteristics
The characteristics of the ten studies are summarized in Table 2 (Cohen‐Mekelburg et al., 2019; Frandsen et al., 2015; Kaltenborn et al., 2021; Kern et al., 2017; Kern et al., 2018; Kern et al., 2019; Kern et al., 2021; Pinheiro et al., 2021; Qayed & Muftah, 2018; Walunas et al., 2017). All studies met the inclusion criteria and were published between 2015 and 2021, but nine of them were published in the last five years (2017–2021). Nine studies used a retrospective cohort design and one applied a cross‐sectional design (Kern et al., 2017). Across all studies, the total number of individuals with chronic illnesses was 1,109,958 (range = 1002–506,376). Chronic diseases included asthma, arthritis, coronary heart disease, diabetes, inflammatory bowel disease, systemic lupus erythematosus, and gastroparesis. Three studies had Medicare beneficiaries (Kern et al., 2018; Kern et al., 2021; Pinheiro et al., 2021) and one study had Medicaid beneficiaries (n = 1) from across the US (Kern et al., 2019). In Kern et al. (2021) study, Medicare beneficiaries had no history of coronary heart disease and had four or more ambulatory visits in the baseline year. One study investigated the data of patients in New York and Florida (Cohen‐Mekelburg et al., 2019). All participants had been admitted to an index hospital or had visited clinics for at least one year and were dwelling at home or in community facilities.
All studies analyzed the data using a regression analysis. None of the studies used a theoretical framework. The authors of all the studies were multidisciplinary and came from nursing, medical, and public health fields.
3.2. Fragmented care in the studies
Few studies clearly defined “fragmented care” for chronic illnesses. Studies have reported that fragmented care is readmission to a nonindex hospital setting from a current inpatient setting (Cohen‐Mekelburg et al., 2019; Kaltenborn et al., 2021; Qayed & Muftah, 2018). Most refer to “fragmentation” as noncontinuous, low‐quality, duplicated, or omitted pivotal care from multiple healthcare providers or multiple healthcare settings, which may lead to worsening of chronic illnesses, hospital readmissions to nonindex health systems that are preventable, and increased healthcare costs (Frandsen et al., 2015; Kaltenborn et al., 2021; Pinheiro et al., 2021).
Three measures of fragmented care were used in the selected studies: reversed Bice‐Boxerman Index (BBI), reversed Herfindahl–Hirschman concentration index (HHI), and nonindex hospital usage. The BBI and the HHI are scales originally used to measure the “continuity of care” and range from 0 (most fragmented or least continuous) to 1 (least fragmentated or most continuous). Higher values obtained from reversing the scores by deducting BBI or HHI score from 1 refer to more fragmented care (Kern et al., 2017). Five studies reversed the BBI (Kern et al., 2017; Kern et al., 2018; Kern et al., 2019; Kern et al., 2021; Pinheiro et al., 2021) and one reversed HHI (Frandsen et al., 2015). The remaining four studies measured fragmented care by calculating the rate of nonindex hospital readmissions or clinic visits (Cohen‐Mekelburg et al., 2019; Kaltenborn et al., 2021; Qayed & Muftah, 2018; Walunas et al., 2017).
Some studies identified factors of fragmentation care such as number of healthcare providers (Frandsen et al., 2015; Kern et al., 2021), number of healthcare institution visits (Walunas et al., 2017), or number of interhospital transfers (Kaltenborn et al., 2021).
3.3. Associations between fragmented care and patient outcomes
This review identified three outcomes that are sensitive to fragmented care: hospital use, risk of comorbidities, and healthcare costs. Table 3 presents the associations between fragmented care and patient outcomes for chronic illnesses. Despite the heterogeneity of significant findings between fragmented care and patient outcomes, the relationship between these outcomes and fragmented care was significant. Mixed relationship findings were also reported.
TABLE 3.
Associations between fragmented care and patient outcomes in included reviews
| Fragmented care measures | Patient outcomes | Findings | Sources | ||
|---|---|---|---|---|---|
| 1. Scales | Reversed BBI | Hospital use outcomes | Hospital readmissions or visits | Significant increased | Kern et al. (2018) |
| No associations | Kern et al. (2019) | ||||
| ED visits | Significant increased | Kern et al. (2018) | |||
| Increased | Kern et al. (2019) | ||||
| Utilization of diagnostic tests | Significant increased | Kern et al. (2017) | |||
| Risk of comorbidities | Significant increased | Kern et al. (2021) | |||
| Mixed results | Pinheiro et al. (2021) | ||||
| Reversed HHI | Hospital use outcomes | Hospital readmissions | Significant increased | Frandsen et al. (2015) | |
| Healthcare costs | Significant increased | Frandsen et al. (2015) | |||
| 2. Nonindex hospital uses or healthcare institutions uses | Hospital use outcomes | Hospital readmissions | Increased |
Cohen‐Mekelburg et al. (2019) Kaltenborn et al. (2021) |
|
| No associations | Qayed and Muftah (2018) | ||||
| Utilizations of diagnostic tests | Increased | Cohen‐Mekelburg et al. (2019) | |||
| Risk of comorbidities | Increased | Walunas et al. (2017) | |||
| Healthcare costs | Significant increased |
Kaltenborn et al. (2021) Qayed and Muftah (2018) |
|||
Abbreviations: BBI, Bice‐Boxerman Index; ED, emergency department; HHI, Herfindahl–Hirschman concentration index.
3.3.1. Hospital use outcomes
Three common hospital use outcomes were reported: ED visits, utilization of diagnostic tests, and hospital readmissions. ED visits and utilization of diagnostic tests by patients with chronic illnesses were significantly related to fragmented care in four of the studies.
Two studies had significant findings regarding ED visits related to fragmented care with hospital‐discharged community‐dwelling patients (Kern et al., 2018; Kern et al., 2019). The risk of ED visits was found to increase with an increase in fragmented care scores measured with reversed BBI (Kern et al., 2018; Kern et al., 2019). These associations between fragmented care and increased ED visits were more significant with multiple chronic illnesses (five or more chronic conditions; adjusted p < 0.05 for each comparison) (Kern et al., 2018). In Kern et al. (2019), every 0.1 increase in fragmented care score that was measured with reversed BBI, saw an ED visit increase of 1.7% (95% CI, 0.5%, 2.9%).
Two studies reported significant results connecting fragmented care with higher utilization of diagnostic tests (Cohen‐Mekelburg et al., 2019; Kern et al., 2017). Kern et al. (2017) compared groups that had the least and most fragmented care and found that the most fragmented group had approximately twice as many diagnostic tests as the least fragmented group regardless of the number of chronic conditions (adjusted p < 0.0001).
Six studies examined the relationship between care fragmentation and hospital readmission. The findings were mixed. Two studies (Cohen‐Mekelburg et al., 2019; Kaltenborn et al., 2021) found an association between increased hospital readmissions and fragmented care. However, Qayed and Muftah (2018) found no significant association between fragmented care and hospital readmissions among patients with gastroparesis. Similarly, Kern et al. (2018) found mixed results with Medicare beneficiaries. Among patients with one to four chronic conditions, higher fragmented care scores significantly increased the risk of hospital readmission (adjusted p < 0.05 for each comparison); however, among patients with five or more chronic conditions, no association between hospital readmission and care fragmentation was found.
3.3.2. Risk of comorbidities
Three studies reported associations between care fragmentation and comorbidity risk (Kern et al., 2021; Pinheiro et al., 2021; Walunas et al., 2017). When care fragmentation was greatest, adverse outcomes due to comorbidities increased (Kern et al., 2021; Walunas et al., 2017). Kern et al. (2021) found a significant association between higher fragmented care scores and increased risk of coronary heart failure events (hazard ratio = 1.14, 95% CI = 0.92, 1.39). Similarly, Walunas et al. (2017) found a significant relationship between fragmented care and the risk of severe infections. However, Pinheiro et al. (2021) found mixed associations between care fragmentation and comorbidities among cancer survivors: increased fragmentation was negatively related to glycemic control for diabetes (OR = 0.78, 95% CI = 0.61, 0.99), but no association was found between fragmented care scores and control of hypertension or hyperlipidemia.
3.3.3. Healthcare costs
Three studies examined the impact of fragmented care on healthcare cost outcomes (Frandsen et al., 2015; Kaltenborn et al., 2021; Qayed & Muftah, 2018). All three studies reported that fragmented care significantly increased healthcare costs. Specifically, a high number of nonindex hospital readmissions saw mean healthcare costs increase compared with an index hospital readmission ($15,645 with nonindex hospital readmissions versus $12,311 with index hospital readmissions; p < 0.0001; Qayed & Muftah, 2018). Similarly, patients who were hospital superusers were associated with yearly healthcare costs above the 95th percentile in six US states (Kaltenborn et al., 2021). Among chronically ill patients in Frandsen et al. (2015), higher fragmented care scores were associated with higher healthcare spending ($10,396 in the highest fragmentation quartile versus $5854 in the lowest fragmentation quartile; p < 0.001).
4. DISCUSSION
This systematic review included 10 studies of fair methodological quality that examined the association between fragmented care and patient outcomes in adult patients with chronic illnesses in the US. Evidence of clear associations between fragmented care and patients' adverse outcomes with regard to hospital use, risk of comorbidities, and healthcare costs were identified (see Table 3). This review provides evidence of a significant association between fragmented care and the adverse healthcare outcomes of patients with chronic illnesses, especially increased ED visits, utilization of diagnostic tests, and healthcare costs. Namely, with increases in care fragmentation, these three outcomes also showed significant increases. These results are corroborated by other reviews that have reported similar relationships between interhospital care fragmentation and patient outcomes (Jin et al., 2021; Snow et al., 2020).
This review found mixed associations between fragmented care and hospital readmissions and between fragmented care and the risk of comorbidity with chronic illnesses. Pinheiro et al. (2021) reported a significant association between care fragmentation and comorbidities with regard to heart patients' risk of diabetes. Two studies found no association between readmissions and Medicaid beneficiaries or gastroparesis adults (Kern et al., 2018; Qayed & Muftah, 2018). More rigorous studies with various population groups of chronic illnesses and various socioeconomic backgrounds are needed to better understand these mixed outcomes.
Most studies in this review measured fragmented care by reversing the BBI and HHI scales. Both scales were originally developed to measure continuous, nonfragmented care (Frandsen et al., 2015; Kern et al., 2021). Other studies have reversed the Continuity of Care Index to measure the fragmentation of care (Kern et al., 2017; Kerm et al., 2018; Kern et al., 2021). However, there are constraints to using this index to measure care fragmentation (Rosenberg & Zulman, 2020). All of these scales were used because there is no current standard operative measurement for fragmented care (Frandsen et al., 2015; Rosenberg & Zulman, 2020). Thus, it is recommended that a measurement or tool be developed and validated to quantify care fragmentation mathematically (Rosenberg & Zulman, 2020). With the development of such tools to measure fragmented care, it will be possible to assess how fragmented care impacts patient outcomes more clearly.
All the studies in this review bundled fragmented care; none of the studies outlined the circumstances that lead to fragmented care and its impact on chronic illnesses. (Liu & Yeung, 2013). Some studies have reported that the mechanisms of fragmented care, that is, the factors that lead to patient outcomes, were multiple healthcare providers and redundant and noncontinuous care (Kern et al., 2019). However, few such mechanisms were explicitly connected to individuals with chronic illnesses. Identifying these mechanisms is difficult because healthcare systems are complicated and rarely provide the exact density of multiple healthcare providers or explicitly identify poor care (Liu & Yeung, 2013; Rosenberg & Zulman, 2020). Therefore, more rigorous research is needed to better understand the mechanisms of fragmented care.
There is no consensus about fragmented care in healthcare research because “fragmented care” means different things to patients and healthcare institutions (Agency for Healthcare Research and Quality [AHRQ], 2014). Across the included studies, fragmented care for chronic illnesses means noncontinuous, low‐quality, duplicated, or omitted pivotal care coordination from multiple healthcare providers or multiple healthcare settings, which may lead to worsening of chronic illnesses, hospital readmissions to nonindex health systems that are preventable, and increased healthcare costs (Frandsen et al., 2015; Kaltenborn et al., 2021; Pinheiro et al., 2021). This variety of definitions suggests that more rigorous studies with concept analysis are needed to construct a clear, evidence‐based definition of fragmented care for chronic illnesses.
None of the studies applied a theoretical model. A theoretical program is imperative to identify the mechanisms by which fragmented care impacts patient outcomes, understand how fragmented care impedes patients' care coordination, and represent how to manage the fragmentation of healthcare (Galvin, 2019). There are several conceptual frameworks for care coordination (AHRQ, 2014). One example of a model is the Care Coordination Ring that visualizes the requirement factors of care coordination and three potential perspectives (patient/family, health care providers, or system levels) to deliver high‐quality and high‐value care (AHRQ, 2014). Applying conceptual frameworks to studies is an important step in identifying which healthcare practitioners' activities and systems are affected by fragmentation and produce adverse outcomes with chronic illnesses. Thus, future research is required to develop and provide theoretical models of fragmented care for chronic illnesses.
Most of the research included in this review focused on the associations between care fragmentation and patients' healthcare outcomes. Using quantitative measures with cohort or cross‐sectional designs, these studies examined how care fragmentation increased total healthcare costs. It is also important to understand nurses', healthcare professionals', and patients' perspectives regarding redundant and fragmented fragmentation care; to obtain this, more qualitative studies of care fragmentation are needed. Further studies that development of experimental or quasi‐experimental studies (e.g., regarding transitional care and management care) that measure the contribution of the nursing profession to reduce fragmented care.
Two major policy initiatives aim to reduce fragmented care across healthcare institutions (hospitals and clinics) and systems: HITECH Act of 2009 and the Medicare and Medicaid EHR Incentive Programs. The two programs were launched to construct meaningful electronic health records (EHRs) that can be shared across healthcare institutions (Holmgren et al., 2018; Walunas et al., 2017). Since these initiatives began, most clinics and hospitals have adopted EHRs for their patient medical records, but only a few institutions have begun sharing data (Evans, 2016; Walunas et al., 2017). Sharing patient data is one of the best tools available to reduce fragmented care; thus, it is recommended that healthcare policymakers provide financial benefits or reimbursement in the healthcare system and insurance plans to accept patients' data sharing.
4.1. Limitations of the review
This systematic review has several limitations that must be addressed. First, although this review tried to include all relevant studies that examined fragmented care and patient outcomes published between 2012 and 2021 and conducted in the US, it is possible that not all relevant studies were captured. Second, this review included adult patients with several chronic illnesses dwelling in the US; however, the review could not include all kinds of chronic illnesses or specify the number of chronic illnesses, nor could it analyze results by participants' gender, ethnicity, income, or other demographic characteristics. Moreover, since healthcare systems differ all around the world, this review's results may not be generalizable. Third, the included studies in this review tend to report significant relationships; thus, reporting bias may exist in this review. Finally, this review only included ten retrospective cohort and cross‐sectional studies based on search terms, aim of the review, and inclusion/exclusion criteria. Thus, the sample size of studies is a limitation. In addition, the vast majority of studies are observational, thereby limiting the strength of the data.
5. CONCLUSION
This is the first systematic review of this topic. This systematic review identified significant associations between care fragmentation and outcomes, such as increased ED visits, diagnostic tests, and healthcare costs in the US in research published between 2012 and 2021. It is recommended that nurse researchers and other healthcare practitioners conduct further studies to understand the contexts and mechanisms of fragmented care and develop theoretical frameworks for care fragmentation and chronic illness outcomes. Healthcare policymakers should consider the evidence in this review as they develop better healthcare systems.
AUTHOR CONTRIBUTIONS
JYJ involved in study design and manuscript writing. JYJ, HL, and MK involved in data collection, analysis, and synthesis. JYJ and HL involved in critical revisions for important intellectual content and study supervision. Neither this manuscript nor parts of it have been submitted elsewhere for publication.
FUNDING INFORMATION
This research was supported by the National Research Foundation of Korea (NRF) grant (2018R1C1B5029635).
CONFLICTS OF INTEREST
The authors declared no conflict of interest for this article.
ETHICS STATEMENT
Because no human subjects were engaged in this study, no Institutional Review Board approval was required.
ACKNOWLEDGMENT
The author thanks Dr. Hae‐kyung Lee (professor emeritus) and Miyoung Kim (a doctoral student) for work in data search, extraction, analysis, and methodological quality assessment. Also, the author acknowledges thoughtful review and feedback of Dr. Lee in the preparation of this manuscript.
Joo, J. Y. (2023). Fragmented care and chronic illness patient outcomes: A systematic review. Nursing Open, 10, 3460–3473. 10.1002/nop2.1607
Prospective Register of Systematic Reviews (PROSPERO) ID: CRD42021285379.
DATA AVAILABILITY STATEMENT
Data openly available in a public repository that issues datasets with DOIs.
REFERENCES
- Agency for Healthcare Research and Quality . (2014). Care coordination measures atlas update. Agency for Healthcare Research and Quality. https://www.ahrq.gov/ncepcr/care/coordination/atlas/chapter2.html [Google Scholar]
- Agha, L. , Frandsen, B. , & Rebitzer, J. B. (2017). Cause and consequences of fragmented care delivery: Theory, evidence, and public policy. National Bureau of Economic Research. https://www.nber.org/system/files/working_papers/w23078/revisions/w23078.rev1.pdf [Google Scholar]
- Bilazarian, A. (2021). High‐need high‐cost patients: A concept analysis. Nursing Forum, 56(1), 127–133. 10.1111/nuf.12500 [DOI] [PubMed] [Google Scholar]
- Brunner‐La Rocca, H.‐P. , Peden, C. J. , Soong, J. , Holman, P. A. , Bogdanovskaya, M. , & Barclay, L. (2020). Reasons for readmission after hospital discharge in patients with chronic diseases—Information from an international dataset. PLoS One, 15(6), e0233457. 10.1371/journal.pone.0233457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Chronic Disease Prevention . (2021). Chronic diseases in America. Center for Chronic Disease Prevention. https://www.cdc.gov/chronicdisease/resources/infographic/chronic‐diseases.htm [Google Scholar]
- Chappidi, M. R. , Kates, M. , Stimson, C. J. , Bivalacqua, T. J. , & Pierorazio, P. M. (2017). Quantifying nonindex hospital readmissions and care fragmentation after major urological oncology surgeries in a nationally representative sample. Journal of Urology, 197(1), 235–240. 10.1016/j.juro.2016.07.078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen‐Mekelburg, S. , Rosenblatt, R. , Gold, S. , Shen, N. , Fortune, B. , Waljee, A. K. , Saini, S. , Scherl, E. , Burakoff, R. , & Unruh, M. (2019). Fragmented care is prevalent among inflammatory bowel disease readmissions and is associated with worse outcomes. The American Journal of Gastroenterol, 114, 276–290. 10.1038/s41395-018-0417-9 [DOI] [PubMed] [Google Scholar]
- Ejaz, A. , Gonzalez, A. A. , Gani, F. , & Pawlik, T. M. (2016). Effect of index hospitalization costs on readmission among patients undergoing major abdominal surgery. JAMA Surgery, 151(8), 718–724. 10.1001/jamasurg.2015.5557 [DOI] [PubMed] [Google Scholar]
- Evans, R. S. (2016). Electronic health records: Then, now, and in the future. IMIA Yearbook of Medical Informatics, 25(S 01), S48–S61. 10.15265/IYS-2016-s006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frandsen, B. R. , Joynt, K. E. , Rebitzer, J. B. , & Jha, A. K. (2015). Care fragmentation, quality, and costs among chronically ill patients. American Journal of Managed Care, 21(5), 355–362. [PubMed] [Google Scholar]
- Galvin, G. (2019). Survey finds fragmented system impedes health care in the U.S. U.S. News. https://www.usnews.com/news/healthiest‐communities/articles/2019‐12‐11/survey‐finds‐fragmented‐us‐health‐care‐impedes‐coordination‐among‐providers
- Higgins, J. P. T. , & Thomas, J. (2021). Cochrane handbook for systematic reviews of interventions (Version 6.2). https://training.cochrane.org/handbook/current
- Holmgren, A. J. , Adler‐Milstein, J. , & McCullough, J. (2018). Are all certified EHRs created equal? Assessing the relationship between EHR vendor and hospital meaningful use performance. Journal of American Medical Informatics Associations, 25(6), 654–660. 10.1093/jamia/ocx135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin, Y. , Tian, X. , Li, Y. , Jiménez‐Herrera, M. , & Wang, H. (2021). Effects of continuous care on health outcomes in patients with stoma: A systematic review and meta‐analysis. Asia‐Pacific Journal of Oncology Nursing, 9, 21–31. 10.1016/j.apjon.2021.12.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joo, J. Y. (2014). Community‐based case management, hospital utilization and patient‐focused outcomes in Medicare beneficiaries. Western Journal of Nursing Research, 36(6), 825–844. 10.1177/0193945913514140 [DOI] [PubMed] [Google Scholar]
- Joo, J. Y. , & Liu, M. F. (2017). Case management effectiveness in reducing hospital use: A systematic review. International Nursing Review, 64(2), 296–308. 10.1111/inr.12335 [DOI] [PubMed] [Google Scholar]
- Joo, J. Y. , & Liu, M. F. (2021). Effectiveness of transitional care interventions for chronic illnesses: A systematic review of reviews. Applied Nursing Research, 61, 151485. 10.1016/j.apnr.2021.151485 [DOI] [PubMed] [Google Scholar]
- Kaltenborn, Z. , Paul, K. , Kirsch, J. D. , Aylward, M. , Rogers, E. A. , Rhodes, M. T. , & Usher, M. G. (2021). Super fragmented: A nationally representative cross‐sectional study exploring the fragmentation of inpatient care among super‐utilizers. BMC Health Service Research, 21(1), 338. 10.1186/s12913-021-06323-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kern, L. M. (2018). Whether fragmented care is hazardous depends on how many chronic conditions a patient has. The Commonwealth Fund. https://www.commonwealthfund.org/publications/journal‐article/2018/oct/fragmented‐care‐chronic‐conditions‐overuse‐hospital [Google Scholar]
- Kern, L. M. , Rajan, M. , Ringel, J. B. , Colantonio, L. D. , Muntner, P. M. , Casalino, L. P. , Pesko, M. , Reshetnyak, E. , Pinheiro, L. C. , & Safford, M. M. (2021). Healthcare fragmentation and incident acute coronary heart disease events: A cohort study. Journal of General Internal Medicine, 36(2), 422–429. 10.1007/s11606-020-06305-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kern, L. M. , Seirup, J. K. , Casalino, L. P. , & Safford, M. M. (2017). Healthcare fragmentation and the frequency of radiology and other diagnostic tests: A cross‐sectional study. Journal of General Internal Medicine, 32(2), 175–181. 10.1007/s11606-016-3883-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kern, L. M. , Seirup, J. K. , Rajan, M. , Jawahar, R. , & Stuard, S. S. (2018). Fragmented ambulatory care and subsequent healthcare utilization among Medicare beneficiaries. American Journal of Managed Care, 24(9), e278–e284. [PubMed] [Google Scholar]
- Kern, L. M. , Seirup, J. K. , Rajan, M. , Jawahar, R. , & Stuard, S. S. (2019). Fragmented ambulatory care and subsequent emergency department visits and hospital admissions among Medicaid beneficiaries. American Journal of Managed Care, 25(3), 107–112. [PubMed] [Google Scholar]
- Liu, S. , & Yeung, P. C. (2013). Measuring fragmentation of ambulatory care in a tripartite healthcare system. BMC Health Service Researcg, 13, 176. 10.1186/1472-6963-13-176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKay, C. , Park, C. , Chang, J. , Brackbill, M. , Choi, J. , Lee, J. H. , & Kim, S. H. (2019). Systematic review and meta‐analysis of pharmacist‐led transitions of care services on the 30‐day all‐cause readmission rate of patients with congestive heart failure. Clinical Drug Investigation, 39(8), 703–712. 10.1007/s40261-019-00797-2 [DOI] [PubMed] [Google Scholar]
- National Institutes of Health . (2021). Study quality assessment tools. National Institutes of Health. https://www.nhlbi.nih.gov/health‐topics/study‐quality‐assessment‐tools [Google Scholar]
- Nothelle, S. , Kelley, A. S. , Zhang, T. , Roth, D. L. , Wolff, J. L. , & Boyd, C. (2022). Fragmentation of care in the last year of life: Does dementia status matter? Journal of the American Geriatric Society, 70(8), 2320–2329. 10.1111/jgs.17827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Page, M. J. , McKenzie, J. E. , Bossuyt, P. M. , Boutron, I. , Hoffmann, T. C. , Mulrow, C. D. , Shamseer, L. , Tetzlaff, J. M. , Akl, E. A. , Brennan, S. E. , Chou, R. , Glanville, J. , Grimshaw, J. M. , Hróbjartsson, A. , Lalu, M. M. , Li, T. , Loder, E. W. , Mayo‐Wilson, E. , McDonald, S. , … Moher, D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ, 372, n71. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinheiro, L. C. , Reshetnyak, E. , Safford, M. M. , Nanus, D. , & Kern, L. M. (2021). Healthcare fragmentation and cardiovascular risk control among older cancer survivors in the Reasons for Geographic And Racial Differences in Stroke (REGARDS) study. Journal of Cancer Survivorship, 15(2), 325–332. 10.1007/s11764-020-00933-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qayed, E. , & Muftah, M. (2018). Frequency of hospital readmission and care fragmentation in gastroparesis: A nationwide analysis. World Journal of Gastrointestinal Endoscopy, 10(9), 200–209. 10.4253/wjge.v10.i9.200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg, N. A. , & Zulman, D. M. (2020). Measures of care fragmentation: Mathematical insights from population genetics. Health Service Research, 55(2), 318–327. 10.1111/1475-6773.13263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snow, K. , Galaviz, K. , & Turbow, S. (2020). Patient outcomes following interhospital care fragmentation: A systematic review. Journal of General Internal Medicine, 35(5), 1550–1558. 10.1007/s11606-019-05366-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walunas, T. L. , Jackson, K. L. , Chung, A. H. , Mancera‐Cuevas, K. A. , Erickson, D. L. , Ramsey‐Goldman, R. , & Kho, A. (2017). Disease outcomes and care fragmentation among patients with systemic lupus erythematosus. Arthritis Care & Research, 69(9), 1369–1376. 10.1002/acr.23161 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data openly available in a public repository that issues datasets with DOIs.


