Abstract
Objectives
Lung cancer (LC) is the leading cause of cancer death in 2020, responsible for almost one in five (18.0%) deaths. This paper provides an overview of the descriptive epidemiology of LC based on national mortality estimates for 2020 from the International Agency for Research on Cancer (IARC), and in the context of recent tobacco control policies.
Design and setting
For this descriptive study, age-standardised mortality rates per 100 000 person-years of LC for 185 countries by sex were obtained from the GLOBOCAN 2020 database and stratified by Human Development Index (HDI). LC deaths were projected to 2040 based on demographic changes alongside scenarios of annually increasing, stable or decreasing rates from the baseline year of 2020.
Results
LC mortality rates exhibited marked variations by geography and sex. Low HDI countries, many of them within sub-Saharan Africa, tend to have low levels of mortality and an upward trend in LC deaths is predicted for both sexes until 2040 according to demographic projections, irrespective of trends in rates. In very high HDI countries, including Europe, Northern America and Australia/New Zealand, there are broadly decreasing trends in men whereas in women, rates are still increasing or reaching a plateau.
Conclusion
The current and future burden of LC in a country or region largely depends on the present trajectory of the smoking epidemic in its constituent populations, with distinct gender differences in smoking patterns, both in transitioning and transitioned countries. Further elevations in LC mortality are expected worldwide, raising important social and political questions, especially in low-income and middle-income countries.
Keywords: epidemiology, health policy, public health
Strengths and limitations of this study.
This study presents a detailed profile of the present lung cancer (LC) burden in men and women worldwide according to national levels of human development.
Our research applies a simple projection to estimate the future LC mortality burden in 2040.
We discuss the results in the context of key risk factors for LC, particularly the continually evolving smoking epidemic.
This examination is hampered by the limited availability of local cause of death information from national vital registration sources, particularly in transitioning countries.
Introduction
Lung cancer (LC) ranks as the most frequent form of cancer death and premature cancer mortality (ages 30–69) with uniformly low 5-year survival, even in high-income countries.1 With one-fifth of the present cancer mortality worldwide due to LC—an estimated 1.8 million deaths in 20202—the key determinant remains tobacco consumption. Up to 9 in 10 LC cases are caused by smoking in high-income settings, while mortality increases with number of cigarettes smoked and smoking duration.3 Lopez et al drew attention to the phases of the global smoking epidemic and the subsequent impact of smoking on LC occurrence by sex;4 men and women remain in very different phases of the smoking epidemic, as reflected in disease rates by birth cohort. Recent reports have generally described marked variations in rates between sexes, with stable or decreasing rates found predominantly among male populations while increasing rates among female populations.5 6
An emerging pattern is a higher rate of LC incidence among young females than males across geographic areas and income levels, that is, not fully explained by sex-specific differences in smoking prevalence.7 Such temporal patterns forewarn of a higher LC burden in women than men at older ages in decades to follow, especially in higher‐income settings. Women have been increasingly targeted in marketing campaigns, particularly in transitioning countries, while social constraints that precluded women taking up the habit are weakening;8 still, smoking prevalence among women varies markedly, for example, a small proportion of women in China are current smokers, in absolute terms and relative to men.9
This paper presents a global overview of the descriptive epidemiology of LC in relation to recent tobacco control policies, using the GLOBOCAN mortality estimates for the year 2020 provided by the International Agency for Research on Cancer (IARC).10 In addition, we provide projections of the future mortality burden according to different temporal scenarios to the year 2040, estimating the expected future LC deaths according to levels of Human Development Index (HDI).
Data sources and methods
The number of deaths from, cancers of the lung (International Classification of Diseases, Tenth Revision C33-34, including trachea and bronchus) were extracted from IARC’s GLOBOCAN 2020 database for 185 countries or territories, by sex and 18 age groups (0–4, 5–9, …, 80–84, 85 and over).2 10 11 Corresponding population data for 2020 were extracted from the United Nations (UN) website.12 The data sources and hierarchy of methods used in compiling the cancer estimates have been described in detail elsewhere.10 In brief, the GLOBOCAN estimates are assembled at the national level using the best available sources of cancer incidence and mortality data within a given country. The methods used to derive the 2020 estimates corresponding to those used to derived for previous years13–15 where applicable, priority is given to short-term predictions and modelled mortality to incidence ratios, while validity is dependent on the degree of representativeness and quality of the source information.10
We present figures based on the estimated deaths in 2020, as well as two summary measures using direct standardisation, namely the age-standardised mortality rate per 100 000 person-years based on the 1966 Segi-Doll World standard population16 17 and the cumulative risk of dying from cancer before the age of 75 expressed as a percentage, assuming the absence of competing causes of death.18 These measures allow comparisons between populations adjusted for differences in age structures. We also provide a prediction of the future number of LC deaths worldwide for the year 2040, based on demographic projections and scenarios of uniformly increasing (+3%, +2%, +1%), stable (0%) or decreasing (−1%, −2%, −3%) rates annually from the baseline year of 2020. The possible impact of COVID-19 pandemic was not taken into consideration during the calculations.
The results are presented by country and aggregated across 20 UN-defined world regions12 and according to the UN’s four-tier HDI in 2020,19 as a means to assess the cancer burden across four levels of development (low, medium, high and very high HDI). Throughout, we use the terms transitioning, emerging and lower HDI countries/economies as synonyms for nations classified as low or medium HDI, and transitioned or higher HDI countries/economies for those classified as high or very high HDI.
The Global Cancer Observatory (https://gco.iarc.fr) includes facilities for the tabulation and graphical visualisation of the GLOBOCAN database, including explorations of the current2 and future20 burden for 36 cancer types.
Patient and public involvement
Patients or the public were not involved in the design, or conduct, or reporting, or dissemination plans of our research.
Results
LC mortality: national rankings 2020
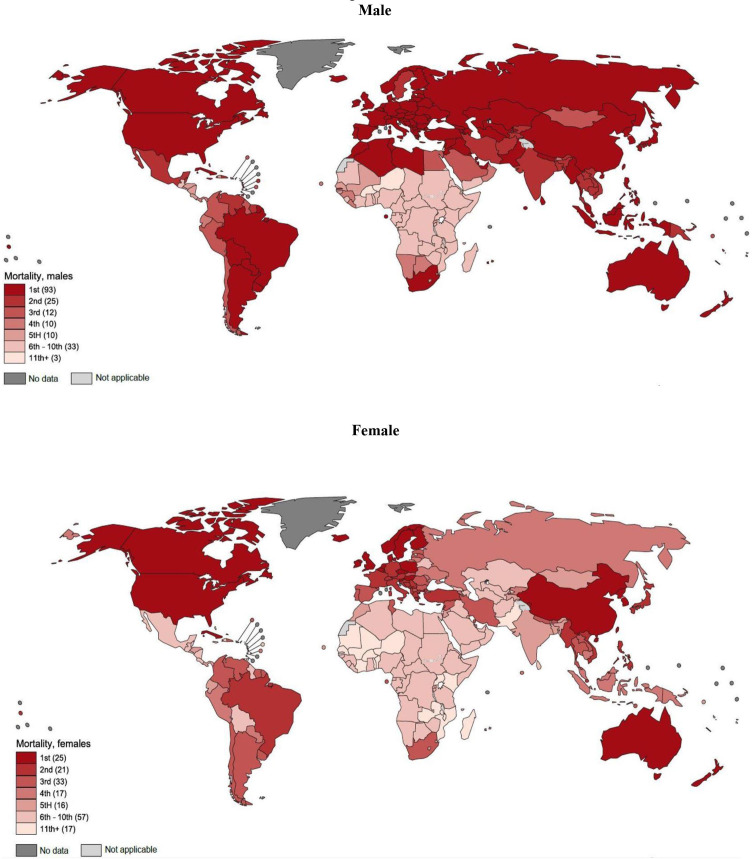
Figure 1 presents global maps that indicate LC’s position in terms of deaths relative to other common tumours at the national level, by sex for the year 2020. In 2020, LC ranks first in terms of cancer death in half (93 out of 185) of the countries included in GLOBOCAN, and either second or third in 37 countries, in men. LC is a major contributor to cancer mortality around the world, including America, Greater Europe, Northern Africa and across the Asian-Pacific region. There is a less dominant role at present in South America and sub-Saharan Africa (but not South Africa). In women, the impact is less than men but still very much in evidence; the disease ranks as the leading form of cancer death in 25 countries including those within North America, Northern, Western and Southern-Central Europe, Eastern Asia and Australia/New Zealand. LC mortality ranks as the second or third leading form of cancer mortality in 54 countries worldwide in women.
Figure 1.
Lung cancer mortality compared with mortality from other causes of malignant neoplasms, 2020, male and female.
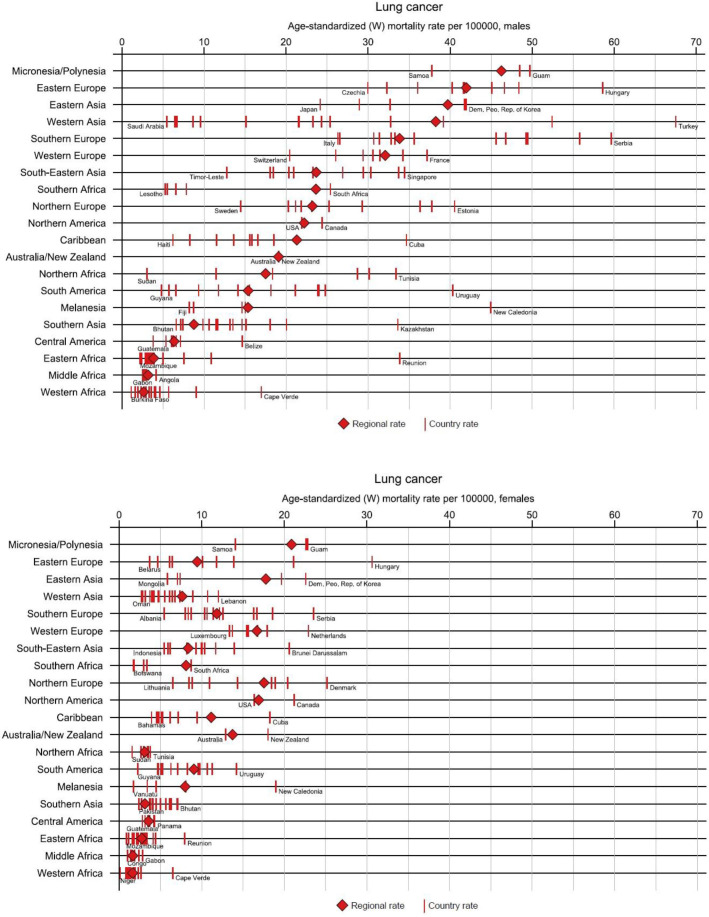
There is at least a 20-fold variation in mortality between the sexes, with rates uniformly higher among men (figure 2). Male mortality rates are higher in Eastern and Southern Europe (especially in Hungary and Serbia with rates of 60 per 100 000), Eastern Asia (particularly the Democratic People’s Republic of Korea) and Polynesia and Micronesia, while rates are lower in Central America, South-Central Asia and most parts of sub-Saharan Africa. The highest female rates are observed in Northern America, Northern and Western Europe, and Australia/New Zealand specifically in Canada, Denmark and the Netherlands, respectively. Relatively low rates are observed in Western, South-Eastern Asia and across the African continent, excluding South Africa.
Figure 2.
Lung cancer age-standardised mortality rates per 100 000 by world regions and sex in 2020, male and female.
LC mortality burden by 2040
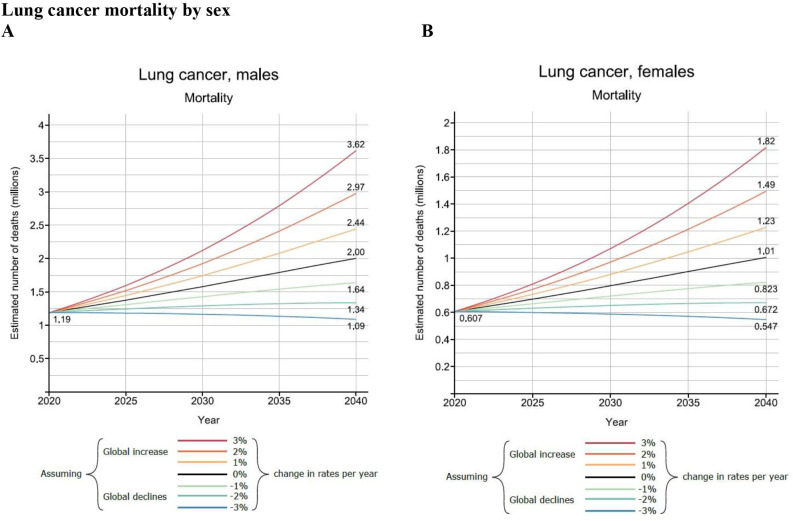
If the current rates were to remain constant over the next two decades, LC will claim around 2 million male deaths in 2040, compared with 1.2 million in 2020 (figure 3). For women, the corresponding deaths are approximately half of their male counterparts: a predicted increase to 1 million in 2040 from 600 000 deaths in 2020. The projection also shows the different scenarios considering the changing rates per year between −3% and +3% based on plausible scenarios of the smoking epidemic in the short-term future; global declines in the number of LC among men but increases for women are perhaps the more realistic scenarios, with national or regional exceptions. Taking this trends-based prediction into account, the predicted number of deaths due to LC for men will likely range between 1.1 and 1.6 million and for women between 1.2 and 1.8 million by 2040. Deaths will markedly increase for both sexes in countries with the lowest HDI, even in the best-case trend scenario (online supplemental appendix figure 1a–h).
Figure 3.
Lung cancer mortality projections worldwide from 2020 to 2040 by sex and the Human Development Index.
bmjopen-2022-065303supp001.pdf (483.9KB, pdf)
Discussion
This study highlights the present geographic diversity in LC mortality worldwide, by sex and by level of human development. Countries with low HDI tend to have low LC mortality rates but may anticipate a higher mortality burden by 2040. For higher HDI countries, the burden of the disease is higher among men, but future trends suggest an increasingly greater proportion of the cancer burden will be seen among women. These different scenarios are due to the impact of historic smoking trends and the increasingly widespread application of tobacco control measures in the last decades.21 While there is an expectation that LC mortality will increase in transitioning countries given there is less implementation of effective tobacco control, there is a positivity in the findings from the Global Tobacco Control Report: the number of people now living in countries with at least two antitobacco policies in place rose from 3.5 billion in 2018 to 4.4 billion in 2020—up from 45% of the world’s population to 56% in 2 years.22
Smoking histories of nations are a key determinant of the current magnitude of LC in many populations worldwide, as described by the classical model of the global smoking epidemic, first introduced by Lopez et al.4 In the model, the effect of different smoking patterns was captured by four stages in the population, by an earlier adoption of the habit in men compared with women, and by the progressive adoption among lower socioeconomic classes, where the habit continues to be an underlying cause of the marked inequalities seen in different educational groups.23 Lopez et al initially applied the hypothesis on just a few developed countries,24 which was later tested on greater geographic scales.25 26 Nevertheless, as smoking prevalence and subsequent LC rates began to peak and decline among men in many populations over the last decades, a key focus has been the deteriorating public health situation affecting women, where in many settings, rates of LC mortality have continued to rise. This raises several relevant biological, epidemiological and sociological concerns,27 including: the changing distribution of the main histological subtypes of LC over time,28 the extent to which women adopted the habit of smoking and their vulnerability to the tobacco industry,29 30 the impact of such a transition in diminishing gender differences in disease burden worldwide31 and the effects of different political systems on the health awareness of individuals.32 33 The impact of these factors is reflected in comparisons of between-country LC mortality rates; for example, the current rate differences in Eastern versus Northern European countries.
Smoking is of course not the only risk factor for LC. There is strong evidence of a relation with other factors, including air pollution, climate change34 and other occupational risk factors such as asbestosis and indoor exposure to cooking fumes, etc.35 The highest exposure to ambient air pollution is the characteristic of mainly countries in transition, where only modest reductions in burden will occur in the most polluted countries unless fine particulate matter (PM 2.5) values are decreased substantially.36
Several other studies have aimed to forecast the future LC burden in very high HDI countries, for example, the USA37 and the UK38 with contradictory findings. While the steeply declining mortality in the USA for both sexes until 2040 fits within the framework of the global smoking epidemic, the rising deaths reported in the UK for men and women until 2035 somewhat contradict previous findings. One explanation could be the rapidly ageing population, which can increase the number of these non-standardised figures. Alternatively, these projections do not take into account the changing smoking prevalence in the past as a key determinant of present and future LCs. Our GLOBOCAN 2020 forecasts do not consider these either, however, we provide possible scenarios on the basis of uniform increases or decreases in rates that may help provide a realistic overview of the changing future burden of LC.
Another limitation of this study is the large variability in the availability and quality of cancer mortality data. Most African and some Asian countries suffer from weak mortality statistics systems. In GLOBOCAN, in countries where mortality series were not available from national vital registration sources, the predominant means of the estimation of rates were from corresponding national incidence estimates via modelling, using incidence-to-mortality ratios derived from cancer registries in neighbouring countries.
With over 3 million deaths predicted by 2040 in the absence of additional interventions according to the finding of this study, it is imperative to emphasise primary prevention as the most cost-effective strategy of tobacco control. It has been shown that raising the price of cigarettes through increased excise taxes can bring marked reductions in cigarette consumption.39 Besides this, developing adaptive tobacco control strategies that target different subgroups is imperative.
One key concern is the limited financial and trained resources in middle-income and lower-income countries, that can hinder health promotion and cancer prevention strategies in these countries. Based on our findings, decreases in LC rates are not likely in these countries until 2040 and presumably tobacco companies are expected to shift and escalate promotional campaigns to preserve business interests and profits where resistance efforts are the weakest.30
Additionally, antitobacco strategies should urgently target women in also higher-income settings such as the European Union, in order to halt their rapidly increasing risk of LC, and prevent unnecessary, premature deaths among future generations of women.40 In Sweden, as an example, gender-specific policies such as those directed at health promotion have been implemented with a focus on young and pregnant women. Scotland also has gender-specific programmes, such as the Women, Low Income and Smoking Project.41 Amos and Haglund have emphasised that building support for female-centred tobacco control programmes through partnerships will be vital to achieve success.30 Furthermore, Amos and Mackay and Amos draw attention to the situation of women in transitioning countries with presently low levels of cigarette smoking among women.8 29 In these countries, smoking among girls is already on the rise, women’s spending power is increasing, cigarettes are becoming affordable and women are more exposed to the marketing strategies of tobacco companies, in an environment where cultural constraints are weakening and female-specific quitting programmes are rare.8
A package of measures to suppress tobacco consumption in a given population has been recommended through continued efforts to increase the proportion of ex-smokers, with a focus on younger generations.42 This could perhaps be achieved by implementing coordinated smoking prevention and control strategies from an early age, in the form of educational programmes in schools. Other measures that could be introduced include community intervention programmes, mass media campaigns and further legislation to ban smoking in public places. One of the main problems is that young people react very differently to antismoking messages compared with adult long-term smokers.42 The harm-reducing role of e-cigarettes and aid to smoking cessation has been proposed,43 however, their impact on future LC mortality is not yet known.44 Successful programmes have also been implemented in rapidly emerging economies such as Brazil, where a reduction in smoking prevalence was observed after the ratification of the WHO Framework Convention on Tobacco Control in 2005, and the adoption of a national ban on tobacco advertising, a national comprehensive smoke-free policy, large pictorial health warnings on cigarette packages, and continuous increases in taxes and prices of tobacco products.45 Other factors may influence the future burden of LC such as the potential introduction of screening in high-risk populations. In a recent trial, LC mortality was significantly lower among those who underwent volume CT screening than those who did not participate.46 Screened patients benefitted from a substantial shift to lower-stage cancers at the time of diagnosis as well as more frequent eligibility for curative treatment (mainly surgery).47 However, concerns have been raised about the potential for overdiagnosis in lung cancer screening.
In summary, this paper has identified marked geographic variations in the current LC burden worldwide and provided potential scenarios regarding the short-term future LC deaths up until 2040. Gredner et al have illustrated the great potential of comprehensive implementation of tobacco control policies in Greater Europe, with over 1.6 million LC cases preventable over a 20-year period through the highest-level implementation of tobacco control policies.48 There is therefore much we can do to halt the rising deaths from LC—as well as many other forms of cancer and non-communicable diseases—through the successful implementation of tobacco control policies.
Supplementary Material
Acknowledgments
The project was implemented with the support from the National Research, Development and Innovation Fund of the Ministry of Culture and Innovation under the National Laboratories Program (National Tumor Biology Laboratory (2022-2.1.1-NL-2022-00010)) and the Hungarian Thematic Excellence Program (under project TKP2021-EGA-44) Grant Agreements with the National Research, Development and Innovation Office.
Footnotes
Contributors: AW: literature search, data analysis, writing – original draft; JV: figures, visualisation; ML: methodology, figures, visualisation; EM, MP, HR, DS, IK, IS: writing – review & editing; PN: writing – review & editing, funding acquisition; FB: methodology, conceptualisation, data analysis, writing – original draft, guarantor.
Funding: This study was supported by the Topic Excellence Program (TKP2020-NKA-26, TKP2021-EGA-44), the National Laboratories Program (National Tumor Biology Laboratory (2022-2.1.1-NL-2022-00010)), and Tasks Related to the National Public Health Strategy (IV/4925/2021/ EKF).
Map disclaimer: The inclusion of any map (including the depiction of any boundaries therein), or of any geographic or locational reference, does not imply the expression of any opinion whatsoever on the part of BMJ concerning the legal status of any country, territory, jurisdiction or area or of its authorities. Any such expression remains solely that of the relevant source and is not endorsed by BMJ. Maps are provided without any warranty of any kind, either express or implied.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available in a public, open access repository.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study does not involve human participants and animal subjects.
References
- 1.Arnold M, Rutherford MJ, Bardot A, et al. Progress in cancer survival, mortality, and incidence in seven high-income countries 1995-2014 (ICBP SURVMARK-2): a population-based study. Lancet Oncol 2019;20:1493–505. 10.1016/S1470-2045(19)30456-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ferlay J, Ervik M, Lam F. Global cancer observatory: cancer today. Lyon, France: International Agency for Research on Cancer, 2020. [Google Scholar]
- 3.National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health . The health consequences of smoking—50 years of progress: a report of the surgeon general. Atlanta, GA: Centers for Disease Control and Prevention, 2014. [PubMed] [Google Scholar]
- 4.Lopez AD, Collishaw NE, Piha T. A descriptive model of the cigarette epidemic in developed countries. Tobacco Control 1994;3:242–7. 10.1136/tc.3.3.242 [DOI] [Google Scholar]
- 5.Bray FI, Weiderpass E. Lung cancer mortality trends in 36 European countries: secular trends and birth cohort patterns by sex and region 1970-2007. Int J Cancer 2010;126:1454–66. 10.1002/ijc.24855 [DOI] [PubMed] [Google Scholar]
- 6.Miranda-Filho A, Piñeros M, Bray F. The descriptive epidemiology of lung cancer and tobacco control: a global overview 2018. Salud Publica Mex 2019;61:219–29. 10.21149/10140 [DOI] [PubMed] [Google Scholar]
- 7.Fidler-Benaoudia MM, Torre LA, Bray F, et al. Lung cancer incidence in young women vs. young men: a systematic analysis in 40 countries. Int J Cancer 2020;147:811–9. 10.1002/ijc.32809 [DOI] [PubMed] [Google Scholar]
- 8.Mackay J, Amos A. Women and tobacco. Respirology 2003;8:123–30. 10.1046/j.1440-1843.2003.00464.x [DOI] [PubMed] [Google Scholar]
- 9.Sansone N, Yong H-H, Li L, et al. Perceived acceptability of female smoking in China: findings from waves 1 to 3 of the ITC China survey. Tob Control 2015;8:tobaccocontrol-2015-052380. 10.1136/tobaccocontrol-2015-052380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ferlay J, Colombet M, Soerjomataram I, et al. Cancer statistics for the year 2020: an overview. Int J Cancer 2021;149:778–89. 10.1002/ijc.33588 [DOI] [PubMed] [Google Scholar]
- 11.Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2021;71:209–49. 10.3322/caac.21660 [DOI] [PubMed] [Google Scholar]
- 12.UNSD . Methodology. n.d. Available: https://unstats.un.org/unsd/methodology/m49/
- 13.Ferlay J, Colombet M, Soerjomataram I, et al. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int J Cancer 2019;144:1941–53. 10.1002/ijc.31937 [DOI] [PubMed] [Google Scholar]
- 14.Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 2015;136:E359–86. 10.1002/ijc.29210 [DOI] [PubMed] [Google Scholar]
- 15.Ferlay J, Shin H-R, Bray F, et al. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer 2010;127:2893–917. 10.1002/ijc.25516 [DOI] [PubMed] [Google Scholar]
- 16.ScienceOpen . Cancer mortality for selected sites in 24 countries (1950–57), n.d.. Available: https://www.scienceopen.com/document?vid=d36053cb-ebfe-4b4c-a7ca-05447aa3cd19
- 17.Schneiderman MA. Cancer incidence in five continents: a technical report. In: Doll R, Payne P, Waterhouse J, eds. Cancer research 1968. New York: Springer-Verlag, 1966: 244–28. [Google Scholar]
- 18.Day NE. Cancer incidence in five continents. cumulative rate and cumulative risk. IARC Sci Publ 1992:862–4. [PubMed] [Google Scholar]
- 19.United Nations Development Programme . Human development reports. n.d. Available: https://hdr.undp.org/
- 20.Ferlay J, Laversanne M, Ervik M. Global cancer observatory: cancer tomorrow. Lyon, France: International Agency for Research on Cancer, 2020Available. https://gco.iarc.fr/tomorrow [Google Scholar]
- 21.Tobacco , 2022. Available: https://tobaccoatlas.org/
- 22.Global tobacco report 2021, n.d.. Available: https://www.who.int/teams/health-promotion/tobacco-control/global-tobacco-report-2021
- 23.Cavelaars AE, Kunst AE, Geurts JJ, et al. Educational differences in smoking: international comparison. BMJ 2000;320:1102–7. 10.1136/bmj.320.7242.1102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Thun M, Peto R, Boreham J, et al. Stages of the cigarette epidemic on entering its second century. Tob Control 2012;21:96–101. 10.1136/tobaccocontrol-2011-050294 [DOI] [PubMed] [Google Scholar]
- 25.Janssen F, El Gewily S, Bardoutsos A. Smoking epidemic in Europe in the 21st century. Tob Control 2021;30:523–9. 10.1136/tobaccocontrol-2020-055658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wensink M, Alvarez J-A, Rizzi S, et al. Progression of the smoking epidemic in high-income regions and its effects on male-female survival differences: a cohort-by-age analysis of 17 countries. BMC Public Health 2020;20:39. 10.1186/s12889-020-8148-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shapiro D. Smoking tobacco: irrationality, addiction, and paternalism. Public Aff Q 1994;8:187–203. [Google Scholar]
- 28.Lortet-Tieulent J, Soerjomataram I, Ferlay J, et al. International trends in lung cancer incidence by histological subtype: adenocarcinoma stabilizing in men but still increasing in women. Lung Cancer 2014;84:13–22. 10.1016/j.lungcan.2014.01.009 [DOI] [PubMed] [Google Scholar]
- 29.Amos A. Women and smoking. Br Med Bull 1996;52:74–89. 10.1093/oxfordjournals.bmb.a011534 [DOI] [PubMed] [Google Scholar]
- 30.Amos A, Haglund M. From social taboo to torch of freedom: the marketing of cigarettes to women. Tob Control 2000;9:3–8. 10.1136/tc.9.1.3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pampel FC. Cigarette use and the narrowing sex differential in mortality. Populat Develop Rev 2002;28:77–104. 10.1111/j.1728-4457.2002.00077.x [DOI] [Google Scholar]
- 32.Carlson E, Hoffmann R. The state socialist mortality syndrome. Popul Res Policy Rev 2011;30:355–79. 10.1007/s11113-010-9192-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Meslé F, Vallin J. The end of east–west divergence in European life expectancies? an introduction to the special issue. Eur J Popul 2017;33:615–27. 10.1007/s10680-017-9452-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vineis P, Huybrechts I, Millett C, et al. Climate change and cancer: converging policies. Mol Oncol 2021;15:764–9. 10.1002/1878-0261.12781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Malhotra J, Malvezzi M, Negri E, et al. Risk factors for lung cancer worldwide. Eur Respir J 2016;48:889–902. 10.1183/13993003.00359-2016 [DOI] [PubMed] [Google Scholar]
- 36.Cohen AJ, Brauer M, Burnett R, et al. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the global burden of diseases study 2015. The Lancet 2017;389:1907–18. 10.1016/S0140-6736(17)30505-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rahib L, Wehner MR, Matrisian LM, et al. Estimated projection of US cancer incidence and death to 2040. JAMA Netw Open 2021;4:e214708. 10.1001/jamanetworkopen.2021.4708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Smittenaar CR, Petersen KA, Stewart K, et al. Cancer incidence and mortality projections in the UK until 2035. Br J Cancer 2016;115:1147–55. 10.1038/bjc.2016.304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jha P, Peto R. Global effects of smoking, of quitting, and of taxing tobacco. N Engl J Med 2014;370:60–8. 10.1056/NEJMra1308383 [DOI] [PubMed] [Google Scholar]
- 40.Bray F, Tyczynski JE, Parkin DM. Going up or coming down? the changing phases of the lung cancer epidemic from 1967 to 1999 in the 15 European Union countries. Eur J Cancer 2004;40:96–125. 10.1016/j.ejca.2003.08.005 [DOI] [PubMed] [Google Scholar]
- 41.Samet J, Yoon S-Y. Women and the tobacco epidemic. challenges for the 21st century. the world Health organization in collaboration with the Institute for global tobacco control Johns Hopkins school of public health 2001.
- 42.Tyczynski JE, Bray F, Aareleid T, et al. Lung cancer mortality patterns in selected central, eastern and southern European countries. Int J Cancer 2004;109:598–610. 10.1002/ijc.20019 [DOI] [PubMed] [Google Scholar]
- 43.Notley C, Ward E, Dawkins L, et al. The unique contribution of e-cigarettes for tobacco harm reduction in supporting smoking relapse prevention. Harm Reduct J 2018;15:31. 10.1186/s12954-018-0237-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Marques P, Piqueras L, Sanz M-J. An updated overview of e-cigarette impact on human health. Respir Res 2021;22:151. 10.1186/s12931-021-01737-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dai X, Gakidou E, Lopez AD. Evolution of the global smoking epidemic over the past half century: strengthening the evidence base for policy action. Tob Control 2022;31:129–37. 10.1136/tobaccocontrol-2021-056535 [DOI] [PubMed] [Google Scholar]
- 46.de Koning HJ, van der Aalst CM, de Jong PA, et al. Reduced lung-cancer mortality with volume CT screening in a randomized trial. N Engl J Med 2020;382:503–13. 10.1056/NEJMoa1911793 [DOI] [PubMed] [Google Scholar]
- 47.Yousaf-Khan U, van der Aalst C, de Jong PA, et al. Final screening round of the Nelson lung cancer screening trial: the effect of a 2.5-year screening interval. Thorax 2017;72:48–56. 10.1136/thoraxjnl-2016-208655 [DOI] [PubMed] [Google Scholar]
- 48.Gredner T, Mons U, Niedermaier T, et al. Impact of tobacco control policies implementation on future lung cancer incidence in Europe: an international, population-based modeling study. Lancet Reg Health Eur 2021;4:100074. 10.1016/j.lanepe.2021.100074 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-065303supp001.pdf (483.9KB, pdf)
Data Availability Statement
Data are available in a public, open access repository.