Abstract
Objective
This study aimed to assess the prevalence and determinants of the triple burden of malnutrition among mother–child pairs in low-income and middle-income countries.
Design
Cross-sectional study.
Setting
Low-income and middle-income countries.
Participants
Women and children.
Primary outcome
Triple burden of malnutrition (overweight/obese mother with undernourished and anaemic under 5 years child).
Methods
Data for this study were drawn from recent 22 low-income and middle-income countries Demographic and Health Surveys. A total weighted sample of 116 795 mother–child pairs was included in the study. STATA V.14.2 was used to clean, code and analyse the data. Multilevel logistic regression was employed to identify factors associated with the problem. Adjusted OR (AOR) with 95% CI and a p<0.05 was reported to indicate statistical association. Model fitness and comparison were done using intraclass correlation coefficient, median OR, proportional change in variance and deviance.
Result
The pooled prevalence of the triple burden of malnutrition among mother–child pairs was 11.39%. It showed statistically significant positive associations with mothers aged ≥35 years (AOR 2.25, 95% CI 2.08 to 2.44), family size >10 (AOR 1.17, 95% CI 1.08 to 1.26), delivery by caesarean section (AOR 1.93, 95% CI 1.83 to 2.03), the richest household (AOR 1.72, 95% CI 1.56 to 1.88), grand multiparous (AOR 1.62, 95% CI 1.46 to 1.81), age of child 36–47 months (AOR 1.77, 95% CI 1.64 to 1.90), at a p<0.05. Whereas breast feeding (AOR 0.94, 95% CI 0.89 to 0.99), married mothers (AOR 0.87, 95% CI 0.78 to 0.96), female children (AOR 0.88, 95% CI 0.84 to 0.92), improved toilet (AOR 0.23, 95% CI 0.17 to 0.29), improved source of drinking water (AOR 0.28, 95% CI 0.21 to 0.35), rural residents (AOR 0.66, 95% CI 0.62 to 0.69) had a contrasting relationship with the triple burden of malnutrition.
Conclusion
About 1 out of 10 households suffer from the triple burden of malnutrition in low-income and middle-income countries. This study revealed that several maternal, child, household and community-level factors have a significant impact on the triple burden of malnutrition among mother–child pairs.
Keywords: NUTRITION & DIETETICS, EPIDEMIOLOGY, PUBLIC HEALTH, Health policy, Community child health
STRENGTHS AND LIMITATIONS OF THIS STUDY.
The findings were supported by large datasets covering 22 low-income and middle-income countries.
We employed multilevel analysis which is an appropriate methodology for such data.
The data were collected using a common internationally acceptable methodological procedure.
Demographic and Health Survey (DHS) used a cross-sectional survey design, and the causal relationship between the triple burden of malnutrition and the independent variables cannot be established.
We did not include important covariates such as dietary intake, physical activity level or comorbidities as the DHS did not collect information on these variables.
Background
The triple burden of malnutrition, which is the coexistence of overnutrition, undernutrition and micronutrient deficiencies, is increasing in low-income and middle-income countries (LMICs).1 The WHO characterised overnutrition (obesity and overweight) as a pandemic of a major public health concern due to the increased frequency of the problem in many countries.2 It is ranked as the sixth-leading cause of disability-adjusted life-years and accounts for approximately 4 million people dying each year worldwide.3–5 Several previous studies have shown that following marked dietary change, obesity/overweight is increasing more rapidly in LMICs compared with higher-income countries.6 7
Similarly, undernutrition continues to be a major public health concern throughout the developing world.8 9 Nearly half of all deaths in children under 5 are attributable to undernutrition and it encompasses wasting, stunting, underweight and micronutrient deficiencies (anaemia).10 11 Despite stunting having declined steadily, faster progress is needed to reach the 2030 target.12 13 Wasting and underweight persisting at alarming rates require a reversal in trajectory if the 2030 target is to be achieved.14 Since 2000, a significant reduction in the prevalence of anaemia in children under 5 has been observed in many LMICs.15 Children are more vulnerable to inadequate prenatal, infant and young child nutrition, particularly in resource-constrained settings.16 17 Endorsing early childhood feeding best practices is crucial to improve the health of children.18
Malnutrition has a tremendous negative impact on the normal functioning of every organ system.19 It can cause permanent, widespread damage to a child’s growth, development and well-being.20 Scientific evidence has shown that malnutrition in children is associated with poorer school performance, increased susceptibility to infections and slow recovery from illness.21 22 Maternal malnutrition increases the risk of poor pregnancy outcomes including obstructed labour, premature or low birthweight babies and postpartum haemorrhage.23 24 To reduce the problem the United Nations adopted the Sustainable Development Goals (SDGs), targeted to end poverty in all its forms everywhere (SDG 1), end hunger, achieve food security, improve nutrition, promote sustainable agriculture (SDG 2), ensure healthy lives and promote well-being for all at all ages (SDG 3).25 26
Previous literature recognised the basic and underlying causes of malnutrition including the environmental, economic and sociopolitical contextual factors, with poverty having a central role.11 27–29 The triple burden of malnutrition among mother–child pairs is a relatively new issue and only a few country-based studies explored the problem which could not give a panoramic view of the problem in LMICs.30–32 Given the persistent and high levels of the problem in these countries, there is a strong need for action. To design and deliver effective interventions adequate understanding of the socioeconomic, environmental and cultural factors is highly important. Besides if the SDG targets are to be met, coordinated action is required towards not only sustaining current rates of decline but also accelerating progress. Therefore, the objective of this study was to assess the prevalence of the triple burden of malnutrition among mothers and children and the potential factors associated with it in LMICs.
Materials and methods
Study design, setting and period
This study is based on 22 LMICs that have had Demographic and Health Surveys (DHS) from 2016 to 2020. The DHS used a cross-sectional survey study design to collect data and provide population and health indicators at the national level. The list of those countries and the respective year of surveys is provided in table 1.
Table 1.
Study setting and year of surveys
| Country | Year of survey | Region |
| Albania | 2017/2018 | Southeastern Europe |
| Benin | 2017/2018 | West Africa |
| Burundi | 2016/2017 | East-central Africa |
| Cameroon | 2018 | West-central Africa |
| Ethiopia | 2016 | East Africa |
| Gambia | 2019/2020 | West Africa |
| Guinea | 2018 | West Africa |
| Haiti | 2016/2017 | Caribbean |
| India | 2019/2021 | South Asia |
| Liberia | 2019/2020 | West Africa |
| Madagascar | 2021 | East Africa |
| Mali | 2018 | West Africa |
| Mauritania | 2019/2021 | Northwest Africa |
| Maldives | 2016/2017 | South Asia |
| Nigeria | 2018 | West Africa |
| Nepal | 2016 | South Asia |
| Rwanda | 2019/2020 | East Africa |
| Sierra Leone | 2019 | West Africa |
| Tajikistan | 2017 | Central Asia |
| Timor-Leste | 2016 | South Asia |
| Uganda | 2016 | East Africa |
| South Africa | 2016 | South Africa |
Data source and sampling procedure
The current analysis was based on pooled data from DHSs in 22 LMICs. These are nationally representative surveys that collect data on reproductive, maternal, neonatal, child health and nutrition in LMIC. The surveys are similarly designed that used standardised questionnaires and data collection procedures, allowing therefore comparability of results. The survey employed a two-stage cluster sampling technique. In the first stage, the selection of proportional clusters/enumeration areas was performed using each country’s most recent population and housing census as a sampling frame. In the second stage, a systematic selection of households from the newly created cluster was performed. A detailed description of the DHS sampling design and data collection procedures has been found in each country’s DHS report. The study population for this study was mother–child pairs. Weighting was done using the complex sample design weighting and the ‘svyset’ Stata command was applied. Variables v005 (sampling weight), v021 (primary sampling unit) and v023 (stratification used in sample design) were used, and as the result, a total weighted sample of 116 795 mother–child pairs was included in the analysis.
Definition of variables
Outcome variable
The triple burden of malnutrition was the outcome variable of this study where the mother was overweight/obese and children under 5 years of age were undernourished and anaemic.30 31 At the same household level, first, we created four different categories of malnutrition such as overweight/obese mother and stunted child, overweight/obese mother and wasted child, overweight/obese mother and underweight child, and overweight/obese mother and anaemic child. Then we further combined overweight/obese mothers, undernourished children and anaemic children to generate the triple burden of malnutrition. Categorisation was made based on height-for-age z-score (HAZ), SDs, weight-for-height z-score (WHZ), weight-for-age z-score (WAZ), haemoglobin level and body mass index (BMI).
Stunting dichotomised and coded into 0=not stunted (HA −2SD and above) and 1=stunted (HAZ <−2 SD).
Wasting dichotomised and coded into 0=not wasted (WHZ −2 SD to +2 SD) and 1=wasted (WHZ <−2SD).
Underweight dichotomised and coded into 0=not underweight (WHZ −2 SD and above) and 1=underweight (WAZ <−2SD).
Child anaemia dichotomised and coded into 0=not anaemic (haemoglobin level > 11 g/dL) and 1=anaemic (haemoglobin level <11 g/dL).
Mother’s BMI dichotomised and coded into 0=normal (18.5–24.9 kg/m2) and 1=overweight/obese (≥25 kg/m2).
The triple burden of malnutrition was dichotomised and coded into 0=no (not overweight/obese mother and not undernourished child plus not anaemic child, and 1=yes (overweight/obese mother and undernourished child plus anaemic child).
An undernourished child is a child who is stunted or wasted or underweight.
Independent variables
Based on previous works of literature and the likelihood of influencing the outcome of interest, several explanatory variables including the age of mothers, mother’s education, marital status, current breast feeding, delivery by caesarean section, family size, wealth index, media access, parity, age of the child, sex of the child, type of toilet facility, source of drinking water, residence and distance to health facility were considered.
Statistical analyses
We append the dataset of each country to generate pooled data. The data extraction, coding and analysis were carried out using STATA software V.14.2. We weighted the sample to restore the representativeness of the sample so that the total sample looks like the country’s actual population. Due to the hierarchical nature of the DHS, the multilevel analysis was fitted to identify significantly associated factors. Four models were fitted; the null model (with no predictors), model I (adjusted for individual-level variables only), model II (adjusted for community-level variables only) and model III (model adjustment for both individual and community-level variables simultaneously). Adjusted OR (AOR) with 95% CI and p<0.05 was used to determine significant predictors. Model fitness and comparison were done using intraclass correlation coefficient (ICC), proportional change in variance, median OR (MOR), the likelihood ratio test and deviance computed.
Patient and public involvement statement
As our study used secondary analysis of DHS data, participants and the public were not involved in the study design or planning of the study. The study participants were not consulted to interpret the results and write or editing of this document for readability or accuracy.
Results
Demographics and socioeconomic characteristics
A total of 116 795 mother–child pairs were included in the study. Over half (56.48%) of mothers were in the age category of 25–34 years. About 22.98% of mothers were illiterate and the majority (46.39%) had attended secondary education. Approximately 95.73% of mothers were married and 62.89% were currently breast feeding. About 20.33% and 21.21% of the households were in the low wealth quintile of poorest and poorer, respectively. Over a quarter (27.62%) of the families had never been exposed to any type of media. The majority of the children (32.59%) were aged ≤12 months. A large proportion (83.60%) of the households had improved sources of drinking water and almost two-thirds (67.02%) of the households had improved toilet facilities. Almost three-fourth (71.03%) of participants lived in rural areas and for over a quarter (27.42%) of those participants, the distance to access health facilities was a big problem (table 2).
Table 2.
Sociodemographic characteristics of the study participants
| Variables | Categories | Unweighted frequency (%) | Weighted frequency (%) |
| Age of mothers | 15–24 | 34 983 (29.05) | 35 918 (30.75) |
| 25–34 | 68 386 (56.78) | 65 971 (56.48) | |
| ≥35 | 17 073 (14.18) | 14 906 (12.76) | |
| Mothers education | No education | 27 995 (23.24) | 26 845 (22.98) |
| Primary education | 19 684 (16.34) | 18 633 (15.95) | |
| Secondary | 57 008 (47.33) | 54 185 (46.39) | |
| Higher | 15 755 (13.08) | 17 131 (14.67) | |
| Mothers marital status | Not in union | 5583 (4.64) | 4987 (4.27) |
| Married | 114 859 (95.36) | 111 807 (95.73) | |
| Currently breast feeding | No | 44 160 (36.66) | 43 338 (37.11) |
| Yes | 76 282 (63.34) | 73 457 (62.89) | |
| Delivery by caesarean section | No | 99 291 (82.49) | 93 974 (80.51) |
| Yes | 21 077 (17.51) | 22 748 (19.49) | |
| Family size | ≤5 | 56 365 (46.80) | 53 677 (45.96) |
| 6–10 | 54 605 (45.34) | 53 258 (45.60) | |
| >10 | 9472 (7.86) | 9859 (8.44) | |
| Wealth index | Poorest | 28 097 (23.33) | 23 749 (20.33) |
| Poorer | 27 352 (22.71) | 24 774 (21.21) | |
| Middle | 24 741 (20.54) | 24 330 (20.83) | |
| Richer | 22 180 (18.42) | 23 880 (20.45) | |
| Richest | 18 072 (15.00) | 20 061 (17.18) | |
| Media access | No | 33 942 (28.18) | 32 256 (27.62) |
| Yes | 86 500 (71.82) | 84 539 (72.38) | |
| Parity | Primiparous | 36 241 (30.09) | 35 333 (30.25) |
| Multiparous | 76 092 (63.18) | 73 823 (63.21) | |
| Grand multiparous | 8109 (6.73) | 7639 (6.54) | |
| Age of child | ≤12 | 38 959 (32.35) | 38 059 (32.59) |
| 13–23 | 25 382 (21.07) | 24 819 (21.25) | |
| 24–35 | 22 208 (18.44) | 21 478 (18.39) | |
| 36–47 | 17 948 (14.90) | 17 204 (14.73) | |
| 48–59 | 15 945 (13.24) | 15 234 (13.04) | |
| Sex of child | Male | 63 660 (52.86) | 62 008 (53.09) |
| Female | 56 782 (47.14) | 54 787 (46.91) | |
| Type of toilet facility | Unimproved | 37 519 (31.15) | 38 518 (32.98) |
| Improved | 82 923 (68.85) | 78 277 (67.02) | |
| Source of drinking water | Unimproved | 20 959 (17.40) | 19 159 (16.40) |
| Improved | 99 483 (82.60) | 97 636 (83.60) | |
| Residence | Urban | 28 722 (23.85) | 33 838 (28.97) |
| Rural | 91 720 (76.15) | 82 957 (71.03) | |
| Distance to a health facility | No problem | 84 605 (70.25) | 84 776 (72.58) |
| Big problem | 35 837 (29.75) | 32 019 (27.42) |
Prevalence of triple burden of malnutrition
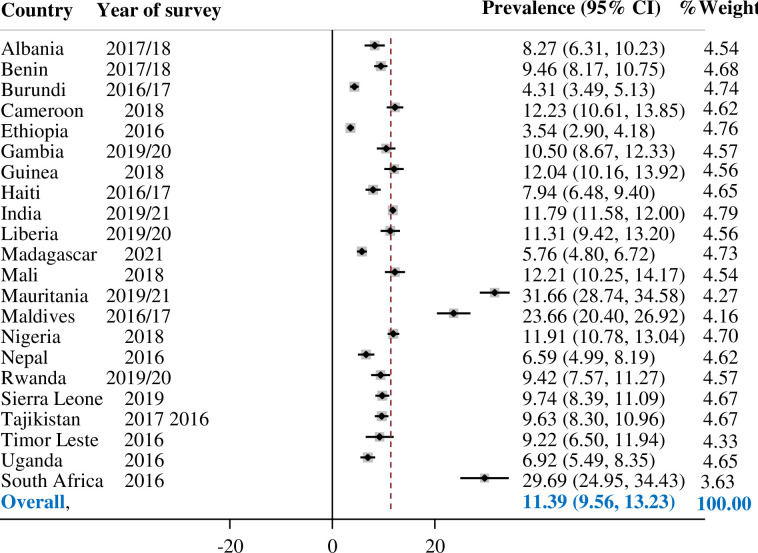
In 22 LMICs, the pooled prevalence of the triple burden of malnutrition among mother–child pairs was found at 11.39% (95% CI 9.56% to 13.23%). Ethiopia has the lowest (3.54%) prevalence of triple burden while Mauritania (31.66%) bears the highest (figure 1).
Figure 1.
The pooled prevalence of the triple burden of malnutrition.
Multilevel analyses
Random parameter estimation and model selection
Based on the result of random effect analysis, the ICC of the null model was 0.30, indicating that 30% of the total variability in triple burden prevalence was attributable to between-cluster variability, while about 70% was due to individual differences. The null model MOR was 3.04, which indicates that a mother/child from a cluster with a high triple burden prevalence has a 3.04 times higher probability of being malnourished than a mother/child from a cluster with a lower prevalence. Model III was the best-fitted model since it has the highest log likelihood (−91 665) and the lowest deviance (183 330) value (table 3).
Table 3.
Multivariable multilevel logistic regression analysis of the triple burden of malnutrition
| Variables | Categories | Null model | Model I AOR 95% CI | Model II AOR 95% CI | Model III AOR 95% CI |
| Age of mothers | 15–24 | 1.00 | 1.00 | ||
| 25–34 | 1.54 (1.46 to 1.63)† | — | 1.54 (1.45 to 1.63)† | ||
| ≥35 | 2.28 (2.11 to 2.47)† | — | 2.25 (2.08 to 2.44)† | ||
| Mothers education | No education | 1.00 | 1.00 | ||
| Primary education | 1.04 (0.97 to 1.12) | — | 1.04 (0.97 to 1.12) | ||
| Secondary | 1.08 (1.01 to 1.15)* | — | 1.08 (1.02 top 1.15)* | ||
| Higher | 0.94 (0.86 to 1.02) | — | 0.94 (0.86 to 1.02) | ||
| Mothers marital status | Not in union | 1.00 | 1.00 | ||
| Married | 0.83 (0.75 to 0.93)* | — | 0.87 (0.78 to 0.96)† | ||
| Currently breastfeeding | No | 1.00 | 1.00 | ||
| Yes | 0.92 (0.87 to 0.97)* | — | 0.94 (0.89 to 0.99)* | ||
| Delivery by CS | No | 1.00 | 1.00 | ||
| Yes | 1.94 (1.84 to 2.04)† | — | 1.93 (1.83 to 2.03)† | ||
| Family size | ≤5 | 1.00 | 1.00 | ||
| 6–10 | 1.00 (0.97 to 1.08) | — | 1.01 (0.98 to 1.08) | ||
| >10 | 1.14 (1.06 to 1.24)† | — | 1.17 (1.08 to 1.26)† | ||
| Wealth index | Poorest | 1.00 | 1.00 | ||
| Poorer | 1.41 (1.31 to 1.52)† | — | 1.38 (1.28 to 1.49)† | ||
| Middle | 1.60 (1.48 to 1.73)† | — | 1.49 (1.38 to 1.62)† | ||
| Richer | 1.86 (1.72 to 2.02)† | — | 1.63 (1.49 to 1.76)† | ||
| Richest | 2.15 (1.97 to 2.35)† | — | 1.72 (1.56 to 1.88)† | ||
| Media access | No | 1.00 | 1.00 | ||
| Yes | 1.01 (0.98 to 1.08) | — | 1.02 (0.99 to 1.11) | ||
| Parity | Primiparous | 1.00 | 1.00 | ||
| Multiparous | 1.42 (1.34 to 1.50)† | — | 1.42 (1.34 to 1.49)† | ||
| Grand multiparous | 1.61 (1.44 to 1.79)† | — | 1.62 (1.46 to 1.81)† | ||
| Age of child | ≤12 | 1.00 | 1.00 | ||
| 13–23 | 1.41 (1.32 to 1.50)† | — | 1.41 (1.32 to 1.50)† | ||
| 24–35 | 1.62 (1.52 to 1.73)† | — | 1.63 (1.53 to 1.74)† | ||
| 36–47 | 1.75 (1.62 to 1.89)† | — | 1.77 (1.64 to 1.90)† | ||
| 48–59 | 1.50 (1.38 to 1.62)† | — | 1.51 (1.39 to 1.64)† | ||
| Sex of child | Male | 1.00 | 1.00 | ||
| Female | 0.88 (0.84 to 0.92)† | — | 0.88 (0.84 to 0.92)† | ||
| Type of toilet facility | Unimproved | 1.00 | 1.00 | ||
| Improved | 0.24 (0.18 to 1.31) | — | 0.23 (0.17 to 0.29)† | ||
| Source of drinking water | Unimproved | 1.00 | 1.00 | ||
| Improved | 0.21 (0.16 to 0.28) | — | 0.28 (0.21 to 0.35)† | ||
| Community-level variables | |||||
| Residence | Urban | 1.00 | 1.00 | ||
| Rural | — | 0.49 (0.46 to 0.52)† | 0.66 (0.62 to 0.69)† | ||
| Distance to a health facility | No problem | 1.00 | 1.00 | ||
| Big problem | — | 0.87 (0.82 to 0.91)† | 0.94 (0.89 to 0.98)† | ||
| Random effect | |||||
| Variance | 1.40 | 1.24 | 1.31 | 1.23 | |
| ICC | 0.30 | 0.27 | 0.28 | 0.27 | |
| MOR | 3.04 | 2.88 | 2.96 | 2.85 | |
| PCV | Reff | 11.42 | 6.43 | 12.14 | |
| Model comparison | |||||
| Log likelihood ratio | −100 585 | −92 108 | −97 815 | −91 665 | |
| Deviance | 201 170 | 184 216 | 195 630 | 183 330 | |
*p<0.05.
†p<0.01.
AOR, adjusted OR; CS, caesarean section; ICC, intraclass correlation coefficient; MOR, median OR; PCV, proportional change in variance.
Factors associated with the triple burden of malnutrition (fixed effects)
The triple burden of malnutrition was statistically significant with mothers aged 25–34 years (AOR 1.54, 95% CI 1.45 to 1.63), ≥35 years (AOR 2.25, 95% CI 2.08 to 2.44), mothers attended secondary education (AOR 1.08, 95% CI 1.02 to 1.15), family size >10 (AOR 1.17, 95% CI 1.08 to 1.26), delivery by CS (AOR 1.93, 95% CI 1.83 to 2.03), the richer household (AOR 1.63, 95% CI 1.49 to 1.76), the richest household (AOR 1.72, 95% CI 1.56 to 1.88), multiparous (AOR 1.42, 95% CI 1.34 to 1.49), grand multiparous (AOR 1.62, 95% CI 1.46 to 1.81), age of child 36–47 months (AOR 1.77, 95% CI 1.64 to 1.90), age of child 48–59 (AOR 1.51, 95% CI 1.39 to 1.64), breast feeding (AOR 0.94, 95% CI 0.89 to 0.99), married mothers (AOR 0.87, 95% CI 0.78 to 0.96), female children (AOR 0.88, 95% CI 0.84 to 0.92), improved toilet facility (AOR 0.23, 95% CI 0.17 to 0.29), improved source of drinking water (AOR 0.28, 95% CI 0.21 to 0.35), rural residents (AOR 0.66, 95% CI 0.62 to 0.69) at a p<0.05 (table 3).
Discussion
LMICs are increasingly facing the triple burden of malnutrition where women and children are among the hardest hit by the problem.33 34 This study assessed the triple burden of malnutrition (co-occurrence of undernutrition, overweight/obesity and anaemia among mother–child pairs) in the same household, using nationally representative data in LMICs. The result showed that the pooled prevalence of triple burden was 11.39% (95% CI 9.56% to 13.23%); Ethiopia had the lowest (3.54 %) prevalence while Mauritania (31.66%) had the highest. The variation among countries could be attributed to differences in socioeconomic status, food environment, physical activity, genetic factors, healthcare system strength, national policy and political commitments.
The study revealed that several maternal, child, household and community-level factors have a significant impact on the triple burden of malnutrition among mother–child pairs. It has found a parallel correlation between the triple burden of malnutrition and maternal age. The odds of being malnourished increase as the age of the mother increases. This is in agreement with previous studies where older mothers bear the highest risk compared with younger ones.31 35 The possible explanation could be because of reduced physical activity, less energy requirement and hormonal changes among older mothers. Similarly, mothers who have attended secondary education were more likely to be malnourished.31 A plausible explanation for this could be the shifts from manual labour to more sedentary occupations and the related decline in physical activity.
Being married reduced the risk of the triple burden of malnutrition. Partners together could generate more money, reduce food insecurity and tend to take better care of themselves and their children. It has been reported that children in single-parent households suffered from undernutrition significantly more than children brought up by both parents.36 37 Likewise, this study revealed breast feeding reduced the triple burden of malnutrition. Breast feeding plays a vital role in the prevention of different forms of childhood malnutrition.38 However, delivery by caesarean section (C-section) delays the timely initiation of breastfeeding and prelacteal feeding.39 Previous studies have reported that C-section increases maternal obesity and negatively affects the breast feeding of children, which results in malnutrition.40 41 Moreover, malnutrition in children is related to gut microbiota alteration and C-section contributes to microbial alterations in the small intestine.42
Our study revealed a parallel relationship between the household wealth quintiles and the triple burden of malnutrition. As household income increases, the odds of malnutrition increase.30 43 High income could increase the purchasing power for food, influencing the type of foods consumed and the intake of prepared or processed food.33 Economic growth and the food industry’s rapid penetration into the market have resulted to depend on energy-dense and nutrient-poor foods.44 In recent years, the dietary preference in LMICs has changed as the food environment is dominated by media advertising, and relatively cheap, energy-dense foods.45
The odds of the triple burden of malnutrition were higher in a household with a family size >10. A plausible explanation is that in a household with a large family, providing optimum nutritious food to all the family members and children could be difficult.46 47 Moreover giving proper care and time to children and the family could be unlikely and this could lead to malnutrition. Likewise, parity was found to be a determinant of the triple burden of malnutrition. Higher parity increased the odds of malnutrition. The possible explanation could be that women could gain weight during pregnancy, and weight loss might not occur in the post-partum period which could lead to child malnutrition.48
This study revealed that child age and sex were significant factors for malnutrition. Older under 5 children were more likely to be malnourished compared with younger ones.49 A previous study50 revealed that there was an increased frequency of parasite infection in older children leading to a higher prevalence of malnutrition compared with the younger ones. In addition, gender was found a significant determinant of malnutrition where a female child was less likely to be malnourished.51 The cause of the gender gap in malnutrition is unknown, however, some studies argued that male children are known to be more vulnerable than females to diseases including lower respiratory infections, diarrhoeal diseases, malaria and preterm birth. Those diseases have been reported as factors for undernutrition among young male children.52 53 Others also claimed that boys are more vulnerable to environmental problems while playing, such as exposure to toxins and air pollution than girls.54
Being rural residents was associated with lower odds of the triple burden of malnutrition. The urban–rural difference could be attributable to factors including access to different food types, overcrowding, concurrent disease and sedentary lifestyles. Previous studies depicted that urbanisation affects the way of life, access to processed and junk foods could exacerbate malnutrition among women and children.30 55
Our study has some strengths and limitations. It used large nationally representative samples with appropriate statistical modelling. The use of large nationally representative data and multilevel analysis helps to provide more robust estimates of observed associations as well as enhance the generalisability of the results. Despite the strengths, this study used cross-sectional data, which did not indicate a temporal relationship between the factors and triple burden. No important covariates, such as dietary intake, physical activity level, comorbidities and nutrition status during pregnancy, were incorporated into the study as the DHS did not provide a complete record of these variables.
Conclusions and recommendations
About 1 out of 10 households suffer from the triple burden of malnutrition in LMICs. This study revealed that several maternal, child, household and community-level factors have a significant impact on the triple burden of malnutrition among mother–child pairs. The triple burden requires the governments, the scientific and medical communities and the industry’s efforts in changing dietary and lifestyle habits to address all forms of malnutrition and should focus on women’s nutrition to break the intergenerational triple burden of malnutrition.
Supplementary Material
Acknowledgments
The authors acknowledge the Measure DHS for providing us with the data set.
Footnotes
Contributors: Conceptualisation: DC. Study design: DC, DGB, MWM, AAK, AZA, MHA, NWT and FMA. Execution: DC, DGB, MWM, AAK, AZA, MHA, NWT and FMA. Acquisition of the data: DC, DGB, MWM, AAK, AZA, MHA, NWT and FMA. Analysis and interpretation: DC, DGB, MWM, AAK, AZA, MHA, NWT and FMA. Writing: DC, DGB, MWM, AAK, AZA, MHA, NWT and FMA. Review and editing: DC, DGB, MWM, AAK, AZA, MHA, NWT and FMA. Guarantor: DC.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available in a public, open access repository.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Meenakshi JV. Trends and patterns in the triple burden of malnutrition in India. Agricultural Economics 2016;47:115–34. 10.1111/agec.12304 Available: http://doi.wiley.com/10.1111/agec.2016.47.issue-S1 [DOI] [Google Scholar]
- 2.The Lancet Gastroenterology & Hepatology . Obesity: another ongoing pandemic. Lancet Gastroenterol Hepatol 2021;6:411.:S2468-1253(21)00143-6. 10.1016/S2468-1253(21)00143-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Organization WH . Diet, nutrition, and the prevention of chronic diseases: report of a joint WHO/FAO expert consultation: World Health organization. 2003.
- 4.GBD 2015 Obesity Collaborators, Afshin A, Forouzanfar MH, et al. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med 2017;377:13–27. 10.1056/NEJMoa1614362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dai H, Alsalhe TA, Chalghaf N, et al. The global burden of disease attributable to high body mass index in 195 countries and territories, 1990-2017: an analysis of the global burden of disease study. PLoS Med 2020;17:e1003198. 10.1371/journal.pmed.1003198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ford ND, Patel SA, Narayan KMV. Obesity in low- and middle-income countries: burden, drivers, and emerging challenges. Annu Rev Public Health 2017;38:145–64. 10.1146/annurev-publhealth-031816-044604 [DOI] [PubMed] [Google Scholar]
- 7.Mahumud RA, Sahle BW, Owusu-Addo E, et al. Association of dietary intake, physical activity, and sedentary behaviours with overweight and obesity among 282,213 adolescents in 89 low and middle income to high-income countries. Int J Obes 2021;45:2404–18. 10.1038/s41366-021-00908-0 [DOI] [PubMed] [Google Scholar]
- 8.Heidkamp RA, Piwoz E, Gillespie S, et al. Mobilising evidence, data, and resources to achieve global maternal and child undernutrition targets and the sustainable development goals: an agenda for action. The Lancet 2021;397:1400–18. 10.1016/S0140-6736(21)00568-7 [DOI] [PubMed] [Google Scholar]
- 9.Osendarp S, Akuoku JK, Black RE, et al. The COVID-19 crisis will exacerbate maternal and child undernutrition and child mortality in low- and middle-income countries. Nat Food 2021;2:476–84. 10.1038/s43016-021-00319-4 [DOI] [PubMed] [Google Scholar]
- 10.World health organisation fact sheets—malnutrition. Available: https://www.who.int/news-room/fact-sheets/detail/malnutrition [Accessed 26 Nov 2022].
- 11.Adepoju AA, Allen S. Malnutrition in developing countries: nutrition disorders, a leading cause of ill health in the world today. Paediatrics and Child Health 2019;29:394–400. 10.1016/j.paed.2019.06.005 [DOI] [Google Scholar]
- 12.Sunguya BF, Zhu S, Mpembeni R, et al. Trends in prevalence and determinants of stunting in Tanzania: an analysis of Tanzania demographic health surveys (1991-2016). Nutr J 2019;18:85. 10.1186/s12937-019-0505-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yang YY, Kaddu G, Ngendahimana D, et al. Trends and determinants of stunting among under-5s: evidence from the 1995, 2001, 2006 and 2011 Uganda demographic and health surveys. Public Health Nutr 2018;21:2915–28. 10.1017/S1368980018001982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Singh KJ, Chiero V, Kriina M, et al. Identifying the trend of persistent cluster of stunting, wasting, and underweight among children under five years in northeastern states of India. Clinical Epidemiology and Global Health 2022;18:101158. 10.1016/j.cegh.2022.101158 [DOI] [Google Scholar]
- 15.Organization. WH . Who global anaemia estimates, 2021 edition. anaemia in women and children. Available: https://www.who.int/data/gho/data/themes/topics/anaemia_in_women_and_children [Accessed 1 Dec 2022].
- 16.Koli HB, Nair MG, Shah MC. Impact of structured pre-natal counselling on early initiation of breast feeding and adherence to exclusive breast feeding: a comparative interventional study. Int J Reprod Contracept Obstet Gynecol 2021;10:2699. 10.18203/2320-1770.ijrcog20212654 [DOI] [Google Scholar]
- 17.Scott N, Delport D, Hainsworth S, et al. Ending malnutrition in all its forms requires scaling up proven nutrition interventions and much more: a 129-country analysis. BMC Med 2020;18:356.:356. 10.1186/s12916-020-01786-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mistry SK, Hossain MB, Arora A. Maternal nutrition counselling is associated with reduced stunting prevalence and improved feeding practices in early childhood: a post-program comparison study. Nutr J 2019;18:47.:47. 10.1186/s12937-019-0473-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Norman K, Haß U, Pirlich M. Malnutrition in older adults-recent advances and remaining challenges. Nutrients 2021;13:2764. 10.3390/nu13082764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Forgie AJ, Drall KM, Bourque SL, et al. The impact of maternal and early life malnutrition on health: a diet-microbe perspective. BMC Med 2020;18:135.:135. 10.1186/s12916-020-01584-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kirolos A, Goyheneix M, Kalmus Eliasz M, et al. Neurodevelopmental, cognitive, behavioural and mental health impairments following childhood malnutrition: a systematic review. BMJ Glob Health 2022;7:e009330. 10.1136/bmjgh-2022-009330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Walson JL, Berkley JA. The impact of malnutrition on childhood infections. Curr Opin Infect Dis 2018;31:231–6.:231. 10.1097/QCO.0000000000000448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Castro-Rodríguez DC, Rodríguez-González GL, Menjivar M, et al. Maternal interventions to prevent adverse fetal programming outcomes due to maternal malnutrition: evidence in animal models. Placenta 2020;102:49–54.:S0143-4004(20)30106-5. 10.1016/j.placenta.2020.04.002 [DOI] [PubMed] [Google Scholar]
- 24.Desyibelew HD, Dadi AF. Burden and determinants of malnutrition among pregnant women in Africa: a systematic review and meta-analysis. PLoS One 2019;14:e0221712. 10.1371/journal.pone.0221712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sachs JD, Schmidt-Traub G, Mazzucato M, et al. Six transformations to achieve the sustainable development goals. Nat Sustain 2019;2:805–14. 10.1038/s41893-019-0352-9 [DOI] [Google Scholar]
- 26.Fonseca LM, Domingues JP, Dima AM. Mapping the sustainable development goals relationships. Sustainability 2020;12:3359. 10.3390/su12083359 [DOI] [Google Scholar]
- 27.Siddiqui F, Salam RA, Lassi ZS, et al. The intertwined relationship between malnutrition and poverty. Front Public Health 2020;8:453.:453. 10.3389/fpubh.2020.00453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rah JH, Melse-Boonstra A, Agustina R, et al. The triple burden of malnutrition among adolescents in indonesia. Food Nutr Bull 2021;42(1_suppl):S4–8. 10.1177/03795721211007114 [DOI] [PubMed] [Google Scholar]
- 29.Luo H, Zyba SJ, Webb P. Measuring malnutrition in all its forms: an update of the net state of nutrition index to track the global burden of malnutrition at country level. Global Food Security 2020;26:100453. 10.1016/j.gfs.2020.100453 [DOI] [Google Scholar]
- 30.Kumar P, Chauhan S, Patel R, et al. Prevalence and factors associated with triple burden of malnutrition among mother-child pairs in India: a study based on national family health survey 2015-16. BMC Public Health 2021;21:.:391. 10.1186/s12889-021-10411-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sunuwar DR, Singh DR, Pradhan PMS. Prevalence and factors associated with double and triple burden of malnutrition among mothers and children in Nepal: evidence from 2016 Nepal demographic and health survey. BMC Public Health 2020;20:.:405. 10.1186/s12889-020-8356-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ahinkorah BO, Amadu I, Seidu A-A, et al. Prevalence and factors associated with the triple burden of malnutrition among mother-child pairs in sub-Saharan Africa. Nutrients 2021;13:2050. 10.3390/nu13062050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Popkin BM, Corvalan C, Grummer-Strawn LM. Dynamics of the double burden of malnutrition and the changing nutrition reality. The Lancet 2020;395:65–74. 10.1016/S0140-6736(19)32497-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Christian AK, Dake FA. Profiling household double and triple burden of malnutrition in sub-Saharan Africa: prevalence and influencing household factors. Public Health Nutr 2022;25:1563–76. 10.1017/S1368980021001750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wong CY, Zalilah MS, Chua EY, et al. Double-burden of malnutrition among the Indigenous peoples (orang asli) of Peninsular Malaysia. BMC Public Health 2015;15:680. 10.1186/s12889-015-2058-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Villena-Esponera MP, Moreno-Rojas R, Molina-Recio G. Food insecurity and the double burden of malnutrition of Indigenous refugee épera siapidara. J Immigr Minor Health 2019;21:1035–42. 10.1007/s10903-018-0807-5 [DOI] [PubMed] [Google Scholar]
- 37.Tiwari N. n.d. The influence of single parent environment on children’s learning and development.
- 38.Malnutrition among adolescents in low- and middle-income countries. Saln2018 2018;2018. 10.52439/FJFX3922 [DOI] [Google Scholar]
- 39.Raihana S, Alam A, Huda TM, et al. Factors associated with delayed initiation of breastfeeding in health facilities: secondary analysis of Bangladesh demographic and health survey 2014. Int Breastfeed J 2021;16:14. 10.1186/s13006-021-00360-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Belachew A. Timely initiation of breastfeeding and associated factors among mothers of infants age 0-6 months old in bahir Dar City, northwest, Ethiopia, 2017: a community based cross-sectional study. Int Breastfeed J 2019;14:5. 10.1186/s13006-018-0196-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Saaka M, Hammond AY. Caesarean section delivery and risk of poor childhood growth. J Nutr Metab 2020;2020:6432754. 10.1155/2020/6432754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pekmez CT, Dragsted LO, Brahe LK. Gut microbiota alterations and dietary modulation in childhood malnutrition-the role of short chain fatty acids. Clin Nutr 2019;38:615–30. 10.1016/j.clnu.2018.02.014 [DOI] [PubMed] [Google Scholar]
- 43.Al Kibria GM, Swasey K, Hasan MZ, et al. Prevalence and factors associated with underweight, overweight and obesity among women of reproductive age in India. Glob Health Res Policy 2019;4:1–12. 10.1186/s41256-019-0117-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sekiyama M, Jiang HW, Gunawan B, et al. Double burden of malnutrition in rural West Java: household-level analysis for father-child and mother-child pairs and the association with dietary intake. Nutrients 2015;7:8376–91. 10.3390/nu7105399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Liguori J, Trübswasser U, Pradeilles R, et al. How do food safety concerns affect consumer behaviors and diets in low- and middle-income countries? A systematic review. Global Food Security 2022;32:100606. 10.1016/j.gfs.2021.100606 [DOI] [Google Scholar]
- 46.Drammeh W, Hamid NA, Rohana AJ. Determinants of household food insecurity and its association with child malnutrition in sub-Saharan Africa: a review of the literature. Curr Res Nutr Food Sci 2019;7:610–23. 10.12944/CRNFSJ.7.3.02 Available: http://www.foodandnutritionjournal.org/current-issue/ [DOI] [Google Scholar]
- 47.Serbesa ML, Iffa MT, Geleto M. Factors associated with malnutrition among pregnant women and lactating mothers in miesso health center, Ethiopia. Eur J Midwifery 2019;3:13. 10.18332/ejm/110131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bhavadharini B, Anjana R, Deepa M, et al. Gestational weight gain and pregnancy outcomes in relation to body mass index in Asian Indian women. Indian J Endocr Metab 2017;21:588. 10.4103/ijem.IJEM_557_16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sinha RK, Dua R, Bijalwan V, et al. Determinants of stunting, wasting, and underweight in five high-burden pockets of four Indian states. Indian Journal of Community Medicine: Official Publication of Indian Association of Preventive & Social Medicine 2018;43:279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pal A, Manna S, Dalui R, et al. Undernutrition and associated factors among children aged 5–10 years in West Bengal, India: a community-based cross-sectional study. Egypt Pediatric Association Gaz 2021;69:1–12. 10.1186/s43054-021-00087-7 [DOI] [Google Scholar]
- 51.Anuradha R, Sivanandham R, Salome SD, et al. Nutritional status of children aged 3-6 years in a rural area of Tamilnadu. Journal of Clinical and Diagnostic Research: JCDR 2014;8:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hawkes S, Buse K. Gender and global health: evidence, policy, and inconvenient truths. The Lancet 2013;381:1783–7. 10.1016/S0140-6736(13)60253-6 [DOI] [PubMed] [Google Scholar]
- 53.Thurstans S, Opondo C, Seal A, et al. Boys are more likely to be undernourished than girls: a systematic review and meta-analysis of sex differences in undernutrition. BMJ Glob Health 2020;5:12.:e004030. 10.1136/bmjgh-2020-004030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Asfaw M, Wondaferash M, Taha M, et al. Prevalence of undernutrition and associated factors among children aged between six to fifty nine months in bule HorA district, South Ethiopia. BMC Public Health 2015;15:41. 10.1186/s12889-015-1370-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Nagarkar AM, Kulkarni SS. Obesity and its effects on health in middle-aged women from slums of Pune. J Midlife Health 2018;9:79–84. 10.4103/jmh.JMH_8_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available in a public, open access repository.