Abstract
Pediatric chronic pain is typically framed as a purely biomedical problem requiring exclusively biomedical solutions. However, research indicates that pain is biopsychosocial, produced and reduced by a combination of biological, psychological, sociological, and environmental factors, and that treatment must therefore also be biopsychosocial, incorporating interventions such as pain psychology and physical therapy. We report a case of a 16-year-old patient with Crohn disease and complex regional pain syndrome, and the multidisciplinary approach to care that was crucial for his return to function.
Keywords: inflammatory bowel disease, Crohn disease, complex regional pain syndrome, chronic illness, physical therapy
INTRODUCTION
Complex regional pain syndrome (CRPS) is a disease characterized by chronic pain of the distal extremities disproportionate to the triggering event, associated with at least one sign of autonomic dysfunction (temperature asymmetry, skin color change, edema, sweating asymmetry, dystrophic changes) and one symptom of allodynia, hyperalgesia, or motor dysfunction (1). It is typically associated with a preceding injury, immobilization, or trauma. The cause of CRPS is unknown, although it has been associated with dysregulation of the central and autonomic nervous systems. Diagnosis and treatment are still debated, although cutaneous changes are common and often critical for diagnosis of CRPS. Accurate diagnosis is often missed due to extensive evaluations and the paucity of pediatric CRPS guidelines. Crohn disease (CD) is an inflammatory bowel disease (IBD) with a multifactorial etiology with debilitating gastrointestinal and extra intestinal manifestations, for example, bone, skin, and others. Our case highlights the difficulty of recognizing and diagnosing CRPS in a pediatric patient with IBD, as well as the importance of utilizing a biopsychosocial approach to treatment.
CASE REPORT
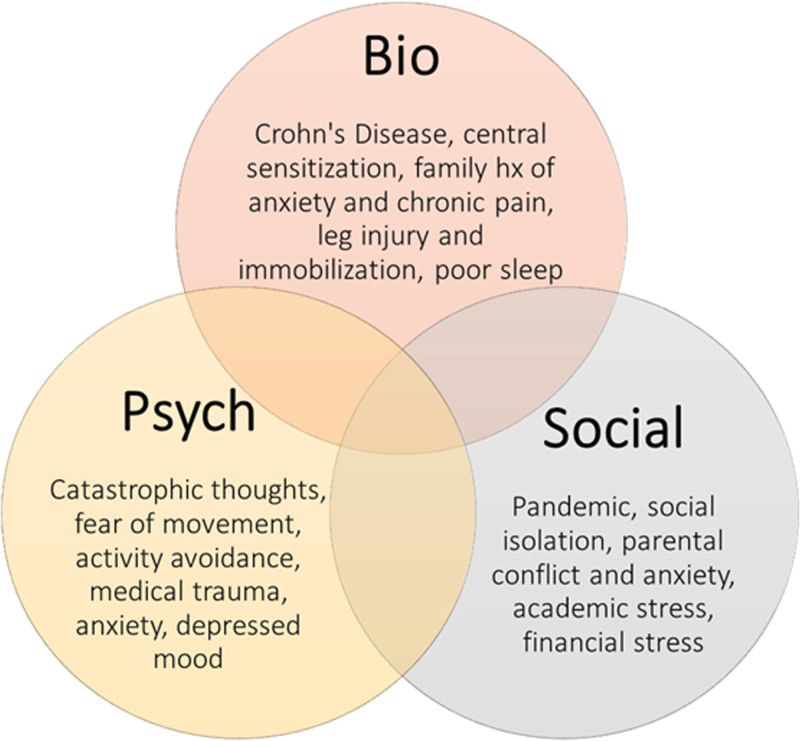
A 16-year-old Caucasian male with small bowel CD, in remission, on Adalimumab presented with acute on chronic bilateral lower extremity pain, peripheral numbness and tingling at a large pediatric academic tertiary care center. He initially noted right foot pain that spread up his leg with periods of numbness, tingling, burning, and cooling. The family believed it was due to an overuse injury after participating in the Junior Olympics. Symptoms continued to worsen with loss of function, muscle weakness, and blue/red skin discoloration which did not improve with Gabapentin. Neurology was consulted due to concern about possible “foot drop” secondary to peripheral demyelination due to anti-TNF therapy (2). This led to a series of extensive evaluations and Electromyography testing. Due to concerns about possible demyelination, he was started on Intravenous Immunoglobulin. IBD treatment was changed to Ustekinumab, and his CD remained in remission. With some initial improvement of leg pain, the patient started an exchange program in Europe, where he suffered a biking accident. This led to a left ankle injury requiring cast and immobilization for 3 months. His left foot and leg then developed the same symptoms as his right: discoloration, temperature changes, tingling, numbness, and pain. Within the month, he developed bilateral, painful, weeping linear lesions on both legs (Fig. 1). He returned to our institution for further care. Initial differential included IBD cutaneous manifestations (eg, pyoderma gangrenosum, neutrophilic dermatitis, metastatic CD). Pediatric Gastroenterology, Dermatology, Immunology, Rheumatology, Neurology and Pain teams were consulted. The sequelae of tests revealed no infection, rheumatic, immunological, or vasculitis disease, and no evidence of small fiber disease on subsequent Electromyographys. Skin lesions were biopsied, revealing nonspecific findings of reactive hypercellular prejunctional fibrosis. Epidermal nerve fibers were normal density. His CD remained in remission. Biological, psychological (medical trauma, anxiety, depressed mood), and social factors (pandemic, social isolation, parental conflict and anxiety, economic stress) combined to create a biopsychosocial cycle of chronic pain, stress, and anxiety (Fig. 2) that was unresponsive to invasive medications, such as nerve blocks and stronger analgesics, and provided no long-term relief. Upon referral to a pain psychologist, his third hospital admission, he was formally assessed and diagnosed with CRPS. On the Wong-Baker Faces Pain Rating Scale (0-10), he rated his pain 10 out of 10, the highest possible score. He also met Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition criteria for somatic symptom disorder and anxiety disorder. Per patient and parent report symptoms included “massive, paralyzing” anxiety about his Gastrointestinal and CRPS symptoms, catastrophic and ruminative thoughts about pain and physical sensations, kinesiophobia and avoidance of physical activities, and daily stomachaches because of anxiety, even while testing negative for Crohn flares. He also reported anxiety and depressed mood related to the pandemic, social isolation, academic stress, family dynamics, economic stressors including potential foreclosure on the family home, his future, and other psychosocial issues. Patient also described repeated, unsuccessful, multi-day hospitalizations for Intravenous Immunoglobulin infusions, ketamine treatments, and other interventions as “traumatic.”
FIGURE 1.
A) January 2021 Eruption of left lower extremity (LLE) ulcers during his international trip post his bike accident. B) One month later (February): New linear lesions on right (the nontraumatized) lower extremity (RLL). C) Three months later (April): Reemergence of ulcers with linear streaks of alopecia of LLE after second treatment of IVIG. D) Four months later (May): return of postweeping lesions on RLL after third treatment of Intravenous Immunoglobulin.
FIGURE 2.
Biopsychosocial model of pain and illness as relates to our patient.
After 4 months (16 sessions total) of coordinated, weekly, in-person physical therapy (PT) plus weekly, in-person cognitive behavioral therapy (CBT), he was off pain medications; weight-bearing, exercising, and running; and able to return to school and life. On the Wong-Baker Faces Pain Rating scale (0–10), he rated his pain a 0 of 10, the lowest possible pain score. He no longer met Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition criteria for Somatic Symptom Disorder, and anxiety and mood were well-managed (3). All symptoms, including pain and lesions, gradually resolved.
Functional improvement was measured using the Lower Extremity Functional Scale (4). The lower the score, the greater the disability is. At the outset of treatment, his lower extremity functional state score was 14 of a total possible score of 80, indicating extreme functional impairment. After 4 months of PT plus CBT, his lower extremity functional state score was 75 of 80, indicating no impairment - an improvement of 436%. The Central Sensitization Inventory (CSI) was also used (5). The CSI is a self-report measure designed to identify patients who have chronic pain related to central sensitization. At treatment outset, patient CSI score was 39, indicating mild sensitization, to 17 after 4 months of PT and CBT, indicating subclinical sensitization.
DISCUSSION
Pain associated with CRPS and IBD is often erroneously framed as a purely biomedical condition. Research confirms that pain is biopsychosocial, produced and reduced by an interplay of cognitive, emotional, physiological, behavioral, sociological, and environmental factors (6,7). Because pain is a biopsychosocial problem, it requires a biopsychosocial solution. This involves a multidisciplinary approach incorporating pain psychology and PT, targeting not only anatomy and physiology but also negative emotions that amplify pain, maladaptive coping strategies, and familial and environmental stressors.
As with treating IBD, a biopsychosocial approach to treating CRPS is therefore critical (8). PT and CBT have notable evidence of effectiveness, and recent CRPS literature reviews conclude that a combination of PT plus CBT is the most efficacious (1,9,10). In this case, exclusively biomedical treatments offered no long-term relief. A shift to pain psychology plus PT led to gradual remission of all symptoms, including hyperalgesia, immobility, and lesions, in a matter of months. CBT has evidence of effectiveness for various conditions, including CRPS, IBD, and irritable bowel syndrome (11,12). CBT targets cognitive, emotional, behavioral, and physiological components of pain by changing negative thoughts and emotions, maladaptive coping, including activity avoidance, and social factors, such as anxious parenting and social isolation. In this case, CBT consisted of a combination of pain education; locating pain in the brain (not the legs), demedicalizing and de-escalating language to reduce panic; helping the child identify somatic symptoms of anxiety (including Gastrointestinal symptoms); distinguishing functional bowel disorders from Crohn flares; relaxation strategies and coping skills; desensitization (touch, temperature) and pacing to increase movement and functionality; parent training; and care coordination with his multidisciplinary treatment team (PT, pediatrics, neurology, gastroenterology, rheumatology, dermatology, anesthesiology, immunology, pain service). Treatment team coaching was conducted by pain psychology with the goals of (1) coordinating care, (2) encouraging all team members to use the same, noncatastrophic, nonnocebic language, including addressing skin changes as “skin fragility” rather than “ulcers,” and labeling motor changes “muscle weakness” instead of “drop foot,” and (3) reframing daily abdominal pain as pain associated with anxiety rather than interpreting every stomachache as a “IBD flare” (as confirmed by negative tests). PT was key, consisting of gradual, controlled exercises with intervals of rest and work, low repetitions, and load to decrease fear, anxiety, and kinesiophobia. Activities such as breathing exercises, static and dynamic balance training, desensitization with vibration, contralateral limb mirror activities (ie, right arm touches left leg), lower extremity stretching and exercises, graded walking, proprioceptive training, self-massage to nonpainful areas gradually working toward more affected body parts, graded exposure to wearing socks and shoes, “pleasure hunts” (finding activities and positions that felt good, not simply nonpainful), establishing regression plans for times of increased pain, and graded progressions to dynamic mobility and running. Over time, repetitions, load, and exercise variety were increased, and rest intervals decreased. Primary goals included yielding control to the patient to give him confidence in his abilities, requesting and respecting his feedback, and offering pain education consistent with CBT. Weekly communication between psychology and PT was critical for coordinating care, gauging progress, and utilizing overlapping coping tools. Rapport and trust between the patient and therapists were critical. PT reinforced CBT-based parent training to reassure parents about the plan of care, and decrease their distress and panic about pain flares, which are often a normal part of CRPS recovery. Advancing the plan of care, exercise, and desensitization were driven by patient tolerance and self-perceived improvement with coordination between PT and psychology.
This case is a prime example of approaching pediatric chronic illness as a biopsychosocial issue requiring a biopsychosocial solution. The efficacy of nonpharmacological treatments for CRPS, functional bowel disorders, and structural Gastrointestinal conditions needs to be prioritized. Incorporating pain psychology and mental health services into coordinated, multidisciplinary treatment, both inpatient and outpatient, is critical for effective care.
ACKNOWLEDGMENTS
Many thanks to the patient and their family. Informed consent was obtained by the parents for the patient to publish this article.
Footnotes
The authors report no conflicts of interest.
REFERENCES
- 1.Weissmann R, Uziel Y. Pediatric complex regional pain syndrome: a review. Pediatr Rheumatol. 2016;14:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Breton J, Ellazam B, Haddad E, et al. Small-fiber neuropathy in a pediatric patient following anti-tumor necrosis factor-α therapy for ulcerative colitis. J Pediatr Gastroenterol Nutr. 2018;66:e159–161. [DOI] [PubMed] [Google Scholar]
- 3.Garra G, Singer AJ, Taira BR, et al. Validation of the Wong-Baker FACES pain rating scale in pediatric emergency department patients. Acad Emerg Med. 2010;17:50–54. [DOI] [PubMed] [Google Scholar]
- 4.Falling C, Stebbings S, Baxter GD, et al. Criterion validity and discriminatory ability of the central sensitization inventory short form in individuals with inflammatory bowel diseases. Scand J Pain. 2021;21:577–585. [DOI] [PubMed] [Google Scholar]
- 5.Neblett R, Cohen H, Choi Y, et al. The Central Sensitization Inventory (CSI): establishing clinically significant values for identifying central sensitivity syndromes in an outpatient chronic pain sample. J Pain. 2013;14:438–445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gatchel RJ, McGeary DD, McGeary CA, et al. Interdisciplinary chronic pain management: past, present, and future. Am Psychol. 2014;69:119–130. [DOI] [PubMed] [Google Scholar]
- 7.Raja SN, Carr DB, Cohen M, et al. The revised International Association for the Study of Pain definition of pain: concepts, challenges, and compromises. Pain. 2020;161:1976–1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Murphy LK, Rights JD, Ricciuto A, et al. Biopsychosocial correlates of presence and intensity of pain in adolescents with inflammatory bowel disease. Front Pediatr. 2020;8:559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vescio A, Testa G, Culmone A, et al. Treatment of complex regional pain syndrome in children and adolescents: a structured literature scoping review. Children. 2020;7:245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rabin J, Brown M, Alexander S. Update in the treatment of chronic pain within pediatric patients. Curr Probl Pediatr Adolesc Health Care. 2017;47:167–172. [DOI] [PubMed] [Google Scholar]
- 11.Coakley R, Wihak T. Evidence-based psychological interventions for the management of pediatric chronic pain: new directions in research and clinical practice. Children. 2017;4:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Person H, Keefer L. Brain-gut therapies for pediatric functional gastrointestinal disorders and inflammatory bowel disease. Curr Gastroenterol Rep. 2019;21:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]