Abstract
Background
Coronary vasospasm is a rare cause of ST-segment elevation myocardial infarction (STEMI) and can be precipitated by numerous inciting factors including endogenous catecholamines. Differentiating coronary vasospasm from an acute atherothrombotic event is diagnostically challenging and requires a careful clinical history combined with electrocardiographic and angiographic abnormalities to make the diagnosis and guide therapy.
Case Summary
We report a case of cardiogenic shock secondary to cardiac tamponade leading to an endogenous catecholamine surge resulting in profound arterial vasospasm and STEMI. The patient presented with chest pain and inferior ST segment elevations prompting emergent coronary angiography, demonstrating subtotal occlusion of the right coronary artery, severe proximal left anterior descending coronary artery stenosis, and diffusely stenosed aortoiliac vessels. Emergent transthoracic echocardiogram revealed a large pericardial effusion and hemodynamics consistent with cardiac tamponade. Pericardiocentesis resulted in dramatic hemodynamic improvement with immediate normalization of ST segments. Repeat coronary angiography performed one day later showed no angiographically significant coronary or peripheral arterial stenosis.
Discussion
This is the first reported case of simultaneous coronary and peripheral arterial vasospasm presenting as inferior STEMI caused by endogenous catecholamines from cardiac tamponade. Several clues suggest coronary vasospasm including the discordant electrocardiography (ECG) and coronary angiographic findings as well as diffusely stenosed aortoiliac vessels. Diffuse vasospasm was confirmed when repeat angiography performed after pericardiocentesis demonstrated angiographic resolution of coronary and peripheral arterial stenosis. Though rare, circulating endogenous catecholamines resulting in diffuse coronary vasospasm may present as STEMI and should be considered based on the clinical history, ECG findings, and coronary angiography.
Keywords: Case Report, Cardiac tamponade, STEMI, Acute coronary syndrome, Coronary vasospasm, Catecholamines
Learning points.
Coronary vasospasm is a clinical entity capable of manifesting as ACS, including STEMI.
Both exogenous and endogenous catecholamines can produce profound coronary and peripheral arterial vasospasm.
In patients presenting with cardiogenic shock, physiologic arterial vasoconstriction can lead to functionally occlusive coronary physiology resulting in ST-segment elevations on ECG.
Introduction
Coronary vasospasm is a rare cause of ST-segment elevation myocardial infarction (STEMI)1 and can be precipitated by numerous inciting factors2 including high levels of circulating catecholamines. The triad of chest pain, ST-segment elevations, and elevated cardiac biomarkers is consistent with a type 1 myocardial infarction.3 The presence of ST-segment elevation, in particular, is strongly suggestive of an atherothrombotic process leading to acute and total occlusion of an epicardial coronary artery.4 Conditions other than plaque rupture resulting in abrupt cessation of coronary filling may also present with the above triad and include coronary vasospasm, myopericarditis,5 stress cardiomyopathy,6 and aortic or coronary dissection.7
Timeline
| Time since presentation | Event |
|---|---|
| 0 min | Patient presented to the emergency department reporting several hours of chest pain with initial HR 130 b.p.m. and BP 80/50 mmHg. |
| 10 min | Initial ECG demonstrating ST elevations in the inferior leads (II, III, aVF). |
| 40 min | CT angiogram chest demonstrates no aortic dissection but identifies large pericardial effusion. |
| 1 h 20 min | Coronary angiogram performed; right coronary artery (RCA) with diffuse subtotal occlusion; left anterior descending (LAD) with 95% proximal stenosis; distal abdominal aorta and bilateral common iliac arteries diffusely diseased. |
| 1 h 40 min | Emergent transthoracic echocardiogram performed in catheterization laboratory with large pericardial effusion and echocardiographic findings of tamponade; pericardiocentesis performed with 800 mL of serosanguinous fluid removed. |
| 2 h 30 min | Repeat ECG showed resolution of inferior ST elevations; HR 100 b.p.m. and BP 140/60 mmHg. |
| 17 h | Repeat coronary angiogram showed RCA with 20% distal stenosis, LAD widely patent without stenosis, and aortoiliac arteries without stenosis. |
| 2 days | Pericardial drain clamped without re-accumulation of pericardial effusion on repeat echocardiogram. |
| 3 Days | Pericardial Drain Removed. |
Case presentation
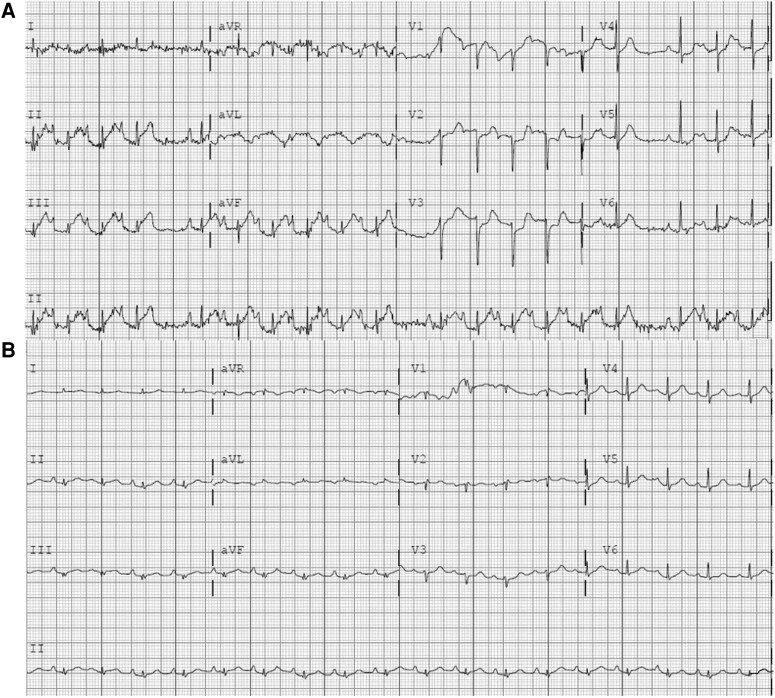
A 72-year-old woman with a history of chronic obstructive pulmonary disease presented with several hours of severe, substernal chest pain at rest. She had accompanying mild upper respiratory tract infection (URI) symptoms, but denied any prior similar episodes of chest pain. She was taking no medications. On presentation, she had a heart rate of 130 b.p.m. and a blood pressure of 80/50 mmHg. She appeared uncomfortable with distant heart sounds and elevated jugular venous pulsations. Initial bloodwork was notable only for leukocytosis of 29.3 k/uL (ref 4.5–10.0 k/uL) and a troponin of 1.6 ng/mL (ref <0.04 ng/mL). Electrocardiography (ECG) revealed inferior ST-segment elevations (Figure 1A).
Figure 1.
(A) ECG on initial presentation with ST elevations in II, III, aVF. (B) ECG post-pericardiocentesis with resolution of inferior ST elevations.
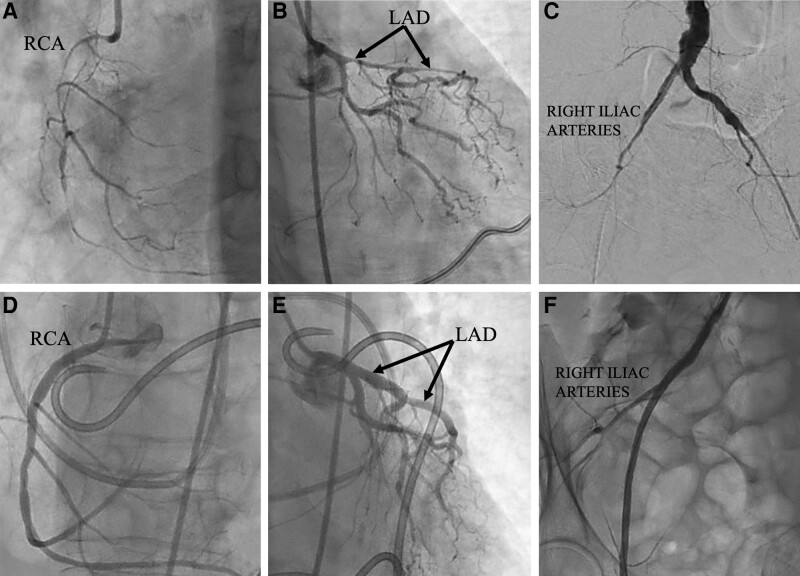
The decision was made to proceed with emergent cardiac catheterization. While the cardiac catheterization lab was being activated, CT angiography of the chest was performed, demonstrating a normal aorta and a pericardial effusion. Emergent coronary angiography revealed a subtotal occlusion of the right coronary artery (RCA) (Figure 2A) and a 95% stenosis of the proximal left anterior descending (LAD) coronary artery (Figure 2B). Recognizing that this might proceed to a complex percutaneous coronary intervention (PCI) requiring mechanical circulatory support, the decision was made to perform pelvic angiography. This demonstrated diffuse severe stenosis of the aortoiliac system in which the six French sheath in the right common femoral artery was occlusive in the right external iliac artery (Figure 2C). An emergent transthoracic echocardiogram (TTE) in the catheterization lab revealed a large circumferential pericardial effusion with echocardiographic criteria for cardiac tamponade. Emergent pericardiocentesis was performed at this time rather than PCI. An eight French pericardial drain was placed and 800 mL of serosanguinous pericardial fluid was evacuated. The opening pericardial pressure of 22 mmHg (ref <10 mmHg) was reduced to 6 mmHg following drain placement, with improvement in systolic blood pressure to 140 mmHg from 80 mmHg and complete resolution of ST-elevations on subsequent ECG (Figure 1B). Similarly, the patient’s chest pain resolved following pericardiocentesis. The patient was transferred to the cardiac intensive care unit where she remained stable overnight. Her serum troponin level peaked at 34.6 ng/mL (ref <0.04 ng/mL). The decision was made to repeat coronary angiography the following morning and pursue PCI of the LAD stenosis. However, repeat coronary angiography was dramatically improved, with no significant stenosis in the RCA (Figure 2D) or the LAD (Figure 2E). There was marked increase in the caliber of the aortoiliac vessels visualized on repeat iliofemoral angiography (Figure 2F).
Figure 2.
Top row: initial angiography of the RCA (A), LAD (B), and aortoiliac system (C). Bottom row: subsequent angiography of the RCA (D), LAD (E), and right iliac system (F) following correction of cardiac tamponade and cardiogenic shock.
The patient remained stable for the remainder of her hospitalization and the pericardial drain was successfully removed. She was discharged and a subsequent TTE 4 weeks later was normal without recurrence of pericardial effusion. Pericardial fluid analysis failed to produce an underlying etiology for the pericardial effusion and we speculate it was secondary to viral pericarditis given her URI symptoms on presentation.
Discussion
Although rapid recognition and prompt revascularization remain the gold standard management for patients with STEMI,4 conditions other than atherothrombotic occlusion of an epicardial coronary artery can present in a manner nearly indistinguishable from a traditional Type 1 MI.
We postulate that this patient’s cardiogenic shock from cardiac tamponade led to an endogenous catecholamine surge resulting in diffuse arterial vasoconstriction, an entity not well-described in the literature.8 This resulted in diffuse coronary and peripheral artery vasospasm.
For this patient who presented in cardiogenic shock and was noted to have features concerning for STEMI, the first clues pointing away from a Type 1 event as the etiology were her angiographic findings. Specifically, angiography of her RCA appeared consistent with a chronic total occlusion and was thus, unlikely to be the culprit vessel despite the inferior ST elevations on the initial ECG. Similarly, though the LAD demonstrated compromised flow initially, it was such that it did not demonstrate complete occlusion and thus did not manifest electrically with ST-segment elevations.
Repeat angiography was performed the following day in the setting of a higher-than-expected troponin and concern for inferior wall transmural myocardial injury due to collateral insufficiency in the setting of a severe LAD stenosis. Repeat angiography demonstrated widely patent LAD, RCA, and left circumflex artery with minimal luminal irregularities. Similarly, there was a dramatic increase in caliber of the right iliac vessels. We postulate that the ST-segment elevations initially seen in the inferior territory reflect the subtotal occlusion of the RCA from vasoconstriction due to high levels of endogenous catecholamines. It is even more compelling that she had evidence of severe, nearly obliterative peripheral arterial stenosis involving the aortoiliac vessels that resolved on repeat angiography post-pericardiocentesis. The fact that her ECG rapidly normalized and repeat angiography was drastically improved without significant atherosclerotic disease after correcting her cardiogenic shock strongly suggests that her STEMI presentation was not due to atherosclerotic plaque rupture but rather the result of vasoconstriction secondary to cardiogenic shock from tamponade.
Tamponade has been shown to cause STEMI as a result of severely elevated pericardial pressure.9 We find this mechanism less applicable to our patient given the fact that the peripheral arteries were also involved. Vasospasm in the setting of exogenous catecholamines is a well-documented phenomenon,10,11 however, our patient received no vasopressors prior to initial angiography. The most likely explanation is the patient’s cardiogenic shock from tamponade caused an endogenous catecholamine surge resulting in diffuse coronary and aortoiliac vasospasm. This hypothesis is supported by the angiographic stenoses of the RCA, LAD, and aortoiliac vessels, all of which dramatically improved after pericardiocentesis alone. The rapid resolution of ST elevations in the inferior leads on ECG are the result of reversing the patient’s cardiogenic shock from tamponade, thus removing the vasoconstrictive response and allowing for improved perfusion to the RCA. Finally, the transient iliac arterial stenosis further supports the diagnosis of diffuse arterial vasoconstriction from shock physiology. Provocative vasospastic testing was not pursued on repeat angiography because the results would not add diagnostic value as the stimulus for vasoconstriction had been corrected.
In states of physiologic stress, high concentrations of endogenous catecholamines, mainly epinephrine, bind to alpha-adrenoreceptors, causing a massive influx of calcium into cardiomyocytes, resulting in coronary vasoconstriction.12 There are reports of endogenous catecholamines in clinical syndromes such as pheochromocytomas13 and Takotsubo cardiomyopathy14 leading to diffuse coronary vasoconstriction. However, this is the first reported case of catecholamine-induced coronary and peripheral vasospasm from tamponade, presenting as an inferior STEMI.
When the patient presented with active chest pain meeting STEMI criteria, the decision was made to perform angiography first instead of pursuing intervention of her pericardial effusion. It was not until she was in the catheterization laboratory that the clinical significance of her pericardial effusion was recognized as tamponade. Had tamponade not been recognized on TTE in the catheterization laboratory, attempts at PCI, rather than pericardiocentesis, could have resulted in a catastrophic clinical outcome. Though type 1 atherothrombotic events will continue to account for the vast majority of STEMI admissions, this is an important new etiology to consider and one for which there must be a high index of clinical suspicion in order to provide a life-saving intervention.
Supplementary Material
Contributor Information
Cara Saxon, Division of General Internal Medicine, Department of Medicine, University of Colorado Anschutz Medical Campus, Aurora, CO 80045, USA.
Scott Freeman, Division of Cardiology, Department of Medicine, University of Colorado Anschutz Medical Campus, Aurora, CO 80045, USA.
Joseph Burke, Division of General Internal Medicine, Department of Medicine, University of Colorado Anschutz Medical Campus, Aurora, CO 80045, USA; Division of Cardiology, Department of Medicine, University of Colorado Anschutz Medical Campus, Aurora, CO 80045, USA; Division of Cardiology, Department of Medicine, Denver Health Medical Center, Denver, CO 80204, USA.
Lead author biography
 Cara E. Saxon is a chief medical resident at the University of Colorado Internal Medicine Residency Program and completed her medical school training at the University of Washington. She is pursuing a career in cardiology and will be a cardiology fellow at the University of Colorado beginning July 2023. Her clinical and research interests focus on preventive cardiology, specifically cardiometabolic risk in women. She looks forward to continuing to improve the culture of inclusiveness for patients and providers in the field of cardiology.
Cara E. Saxon is a chief medical resident at the University of Colorado Internal Medicine Residency Program and completed her medical school training at the University of Washington. She is pursuing a career in cardiology and will be a cardiology fellow at the University of Colorado beginning July 2023. Her clinical and research interests focus on preventive cardiology, specifically cardiometabolic risk in women. She looks forward to continuing to improve the culture of inclusiveness for patients and providers in the field of cardiology.
Supplementary material
Supplementary material is available at European Heart Journal – Case Reports
Slide sets: A fully edited slide set detailing this case and suitable for local presentation is available online as Supplementary data.
Consent: The authors confirm that written consent for submission and publication of this case report has been obtained in accordance with COPE guidelines.
Funding: None declared.
Data availability
The data underlying this article are available in the article and in its online supplementary material.
References
- 1. Wang K, Asinger RW, Marriott HJL. ST-segment elevation in conditions other than acute myocardial infarction. N Engl J Med 2003;349:2128–2135. [DOI] [PubMed] [Google Scholar]
- 2. Lanza GA, Careri G, Crea F. Mechanisms of coronary artery spasm. Circulation 2011;124:1774–1782. [DOI] [PubMed] [Google Scholar]
- 3. Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, et al. Fourth universal definition of myocardial infarction (2018). J Am Coll Cardiol 2018;72:2231–2264. [DOI] [PubMed] [Google Scholar]
- 4. Anderson JL, Morrow DA. Acute myocardial infarction. N Engl J Med 2017;376:2053–2064. [DOI] [PubMed] [Google Scholar]
- 5. Imazio M, Trinchero R. Myopericarditis: etiology, management, and prognosis. Int J Cardiol 2008;127:17–26. [DOI] [PubMed] [Google Scholar]
- 6. Bybee KA, Prasad A. Stress-related cardiomyopathy syndromes. Circulation 2008;118:397–409. [DOI] [PubMed] [Google Scholar]
- 7. Chen A, Ren X. Aortic dissection manifesting as ST-segment elevation myocardial infarction. Circulation 2015;131:503–504. [DOI] [PubMed] [Google Scholar]
- 8. Yasue H, Mizuno Y, Harada E. Coronary artery spasm—clinical features, pathogenesis and treatment. Proc Jpn Acad Ser B Phys Biol Sci 2019;95:53–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Leeies M, Weldon E. STEMI Stymie: metastatic cancer and cardiac tamponade presenting as inferior STEMI. Ann Emerg Med 2011;57:221–224. [DOI] [PubMed] [Google Scholar]
- 10. Qarajeh R, Singh A, Khariton Y, Rafie N, Baweja P. Recurrent ST elevation myocardial infarction from norepinephrine-induced coronary vasospasm. Cureus 2020;12:e7605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Khavandi A, Gatward JJ, Whitaker J, Walker P. Myocardial infarction associated with the administration of intravenous ephedrine and metaraminol for spinal-induced hypotension. Anaesthesia 2009;64:563–566. [DOI] [PubMed] [Google Scholar]
- 12. Hammadah M, Alkhoder A, Al Mheid I, Wilmot K, Isakadze N, Abdulhadi N, et al. Hemodynamic, catecholamine, vasomotor and vascular responses: determinants of myocardial ischemia during mental stress. Int J Cardiol 2017;243:47–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Santos JRU, Brofferio A, Viana B, Pacak K. Catecholamine-Induced cardiomyopathy in pheochromocytoma: how to manage a rare complication in a rare disease? Horm Metab Res 2019;51:458–469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Pelliccia F, Kaski JC, Crea F, Camici PG. Pathophysiology of Takotsubo syndrome. Circulation 2017;135:2426–2441. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article are available in the article and in its online supplementary material.