Abstract
Background
Long COVID is a common, debilitating post-infectious illness for which effective management is unknown. Integrative Medical Group Visits (IMGV) are effective interventions for chronic conditions and could benefit Long COVID patients. More information is needed regarding existing patient reported outcome measures (PROMs) to evaluate efficacy of IMGV for Long COVID.
Objective
This study assessed the feasibility of specific PROMS to evaluate IMGVs for Long COVID. Findings will inform future efficacy trials.
Methods
The Perceived Stress Scale (PSS-10), General Anxiety Disorder two-question tool (GAD-2), Fibromyalgia Symptom Severity scale (SSS), and Measure Yourself Medical Outcome Profile (MYMOP®) were collected pre- and post-group by teleconferencing platform or telephone and compared using paired t-tests. Patients were recruited from a Long COVID specialty clinic where they participated in 2-hour - 8 weekly IMGV sessions online.
Results
Twenty-seven participants enrolled and completed pre-group surveys. Fourteen participants were reachable by phone post-group and completed all pre and post PROMs (78.6% female, 71.4% non-Hispanic White, mean age 49). MYMOP® primary symptomatology was fatigue, shortness of breath and “brain fog”. Symptoms decreased in interference when compared to pre-group levels (mean difference −1.3 [95% CI-2.2, −.5]). PSS scores decreased (−3.4 [95% CI -5.8, −1.1]), and GAD-2 mean difference was −1.43 (95% CI –3.12, .26). There were no changes in SSS scores of fatigue (−.21 [95% CI -.68,0.25]), waking unrefreshed (.00 [95%CI -.32, −.32]), or trouble thinking (−.21 [95% CI -.78,0.35]).
Conclusion
All PROMs were feasible to administer via teleconferencing platform or telephone. The PSS, GAD-2 and MYMOP® are promising PROMs to track Long COVID symptomatology among IMGV participants. The SSS, while feasible to administer, did not change compared to baseline. Larger, controlled studies are needed to determine the efficacy of virtual IMGVs to address the needs of this large and growing population.
Keywords: integrative, long COVID, group visit, telemedicine, whole person care
Introduction
Post-acute sequelae of COVID-19, which frequently constitute a syndrome known as Long COVID, are increasingly recognized as a major public health concern. Following the acute phase of illness, COVID-19 survivors experience ongoing increased burdens of a wide range of health indicators, including medical diagnoses, medical visits, and death. This post-viral syndrome is estimated to affect 25% of COVID-19 survivors. 1 Given high caseloads of COVID-19 within the United States, there are predicted to be large numbers of people with Long COVID.
Most broadly, Long COVID can be considered as a syndrome involving persistent symptoms or health effects after resolution of the acute COVID illness. The Centers for Disease Control (CDC) describes the syndrome as a “lack of return to a usual state of health following acute COVID-19 illness”. 2 The etiology of Long COVID is poorly understood. The limited predictive indicators at time of acute illness include the presence of diabetes, SARS CoV-2 viremia, Epstein-Barr virus viremia at time of acute illness and select autoantibodies. 3 The most common symptoms include fatigue, respiratory discomfort, cognitive impairment, pain, anxiety, and depression, although effects can occur in a variety of organ systems throughout the body.4,5
Due to a lack of clarity on underlying mechanisms, management of Long COVID is primarily symptomatic and can vary between clinic locations. Evaluation and treatment plans are highly dependent on a patient’s symptoms. For example, in those with fatigue, performing a medical evaluation including examination and laboratory testing is indicated to rule out complicating medical conditions such as anemia and thyroid disease. 6 If this evaluation is unrevealing, patients can often be started in an individually titrated return-to-activity program such as with a home exercise plan or physical therapy referral. Further specific guidance is being developed by medical associations.7,8
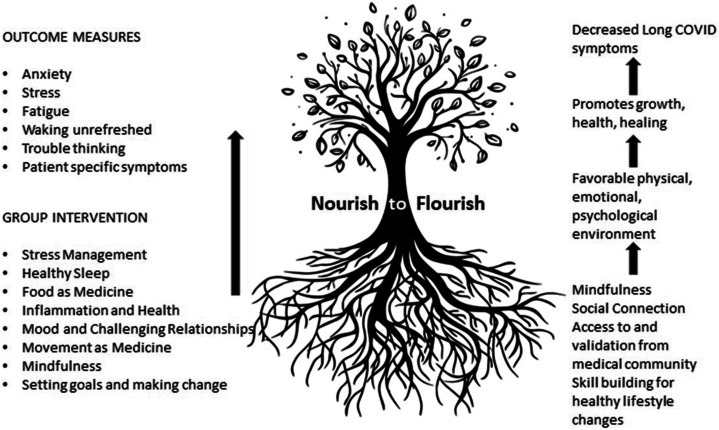
In addition to individualized treatment, our faculty at [redacted for blinding] adapted a telehealth Integrative Medical Group Visit (IMGV) for people with chronic pain to address the needs of Long COVID patients. The IMGV was developed to increase access to integrative comprehensive evidence-based treatment for chronic pain and provides patients with social support, stress reduction skills, validation by the medical community, and motivation to make lifestyle changes (see Figure 1). 9 Participants gather in a group medical visit for 1.5 to 2 hours, and sessions are co-facilitated by a billing healthcare provider (ie, a physician or advanced-practice provider) and either a trained mindfulness instructor or yoga teacher. In a randomized control trial of IMGV for patients with chronic pain and depression, patients who received IMGV compared to usual-care controls had fewer emergency room visits and significantly improved mental health-related quality of life. 10
Figure 1.
Concept map of integrative medical group visits for people with Long COVID: Favorable biopsychosocial environment promotes healing.
An adapted version of IMGV is offered on an ongoing basis to patients of a post-COVID clinic because clinicians hypothesized that the components of IMGV will improve quality of life in Long COVID patients (see Figure 1). Key components of the IMGV program include mindfulness, social connection, access to and validation from medical providers, and skill building for healthy lifestyle changes. The hypothesis is that these components provide a favorable environment, or fertile soil, for health and healing. In the interest of furthering knowledge about Long COVID and IMGV, and in preparation for a larger clinical trial, this manuscript reports on the feasibility of patient-reported outcome measures collected pre- and post-group to measure changes in health status among Long COVID patients who attended IMGVs. Details regarding the curriculum and the implementation of the group are also provided.
Methods
Study Design
This observational study took place among participants who attended a group visit for Long Covid. It was designed to assess feasibility of using patient-reported outcome measures to study telehealth Integrative Medical Group Visits for the treatment of Long COVID delivered via teleconferencing platform (Zoom).
Setting
Participants were patients from a university based post-COVID clinic who were diagnosed with Long COVID and referred to IMGV for Long COVID. The diagnosis was based upon the clinical judgement of clinicians in this specialty clinic. Inclusion criteria included evaluation and diagnosis of Long COVID in the post-COVID clinic, and referral to IMGV for Long COVID. Participants who had been referred to IMGV and agreed to complete pre and post measures were enrolled. Exclusion criteria included any patients who were not evaluated at the post-COVID clinic and referred to IMGV. The group is routinely offered to patients at the post-COVID clinic, and the decision whether to enter the study did not affect patients' opportunity to participate in the group. Study participants received the same care as non-study participants. Since study participants were not assigned to an intervention, this study did not qualify as a clinical trial. This study was reviewed and approved by the University of North Carolina Institutional Review Board under application number 21-1326.
Measures
Four patient-reported outcome measures (PROMs) were utilized in this study. The Perceived Stress Scale (PSS-10), 11 the General Anxiety Disorder 2 question tool (GAD-2), 12 3 questions from the Fibromyalgia Symptom Severity Scale (SSS), 13 and the Measure Yourself Medical Outcome Profile (MYMOP®). 14
The Perceived Stress Scale (PSS-10) is a 10-item self-report psychological instrument designed to measure the perception of stress. The questions ask about thoughts and feelings related to emotional reactions to stress, irritations, and control over the past month. Scores range from 0 to 40 with higher scores indicating higher perceived stress. The PSS-10 has demonstrated internal consistency reliability with a Cronbach’s alpha score of >70. 11
The Generalized Anxiety Disorder Scale two-item questionnaire (GAD-2) is a validated, shortened form of the GAD-7, designed to screen for the presence of generalized anxiety disorder using the first 2 questions from the GAD-7. Participants are asked to report how often over the previous 2 weeks they have been bothered by feeling nervous, anxious or on edge, and how often they were bothered by not being able to stop or control worrying. Scores range from zero to 3. The 2 items are summed. A score of 3 points is the preferred cut-off for identifying possible cases and in which further diagnostic evaluation for generalized anxiety disorder is warranted. Using a cut-off of 3 the GAD-2 has a sensitivity of 86% and specificity of 83% for diagnosis generalized anxiety disorder. 12
Three individual items from the Fibromyalgia Symptoms Severity Scale (SSS) were used to measure fatigue, waking unrefreshed, and trouble thinking. For each symptom, participants were asked to rate the level of severity of each symptom in the past week from zero representing no problem to 3 representing severe, pervasive, continuous, life-disturbing problems. A SSS score equal or greater than 5 is combined with the widespread pain index for diagnostic criteria of fibromyalgia. 13 The SSS score was chosen for its brevity and clinical relevance to assess the presence of fatigue, unrefreshing sleep, and cognitive impairment among Long COVID patients. 14
The Measure Yourself Medical Outcome Profile (MYMOP®) is designed to prioritize and measure changes important to a person/patient. The MYMOP instructs patients to “Choose 1 or 2 symptoms that bother you the most.” Patients then consider these symptoms individually, ranking the severity of symptoms over the past week with a zero indicating “as good as it could be” and a 6 indicating “as bad as it could be.” Using the same scale, the person is directed to “Choose 1 activity (physical, social, or mental) that is important to you, and that your problem makes difficult or prevents you from doing. Score how bad it has been in the last week.” These questions are repeated later, supplying the patient with the symptoms and activity chosen at the first time point. 15 MYMOP® was validated against the Short Form Health Survey (SF-36) in 1996. 16 A more recent critical appraisal, published in 2019, recommended additional validation following the COSMIN criteria. 17 The MYMOP® is scored by comparing change in mean score for each question. The MYMOP® profile score is calculated by comparing the average of the changes in individual component mean scores.
Research Protocol
After being referred to the IMGV from clinicians in the COVID Recovery Clinic, the study was introduced to patients by a physician (JLB) and interest was garnered. If interested, patients were contacted over the phone for verbal research consent and baseline data collection occurred using Zoom teleconferencing software. To all consented participants who were reachable by phone, post-group measures were collected in a similar fashion by a trained research assistant. Deidentified data was stored on Microsoft Teams. Information connecting the study ID to the patient was stored on a password-protected document in Microsoft Teams.
Curriculum
The IMGV was called Nourish to Flourish (N2F) and was adapted from the previously tested IMGV model for people with chronic pain (Gardiner, 2019). IMGV had previously been implemented and adapted for telehealth delivery at [details omitted for double anonymized peer review] 18 After finding that IMGV for patients with chronic pain delivered via telehealth was feasible and acceptable to both patients and providers, 19 faculty at the newly opened post-COVID clinic suggested adapting the IMGV model for patients with Long COVID.
The IMGV curriculum content includes health education on stress, inflammation, sleep, pain, depression, and nutrition. Experiential activities include mindfulness mediations (awareness of breath meditation, body scan, mindful eating, sitting meditation, chair yoga, and loving kindness meditation), self-acupressure, gratitude journaling, self-massage, and goal setting, as well as anti-inflammatory diet recipes. 9 The original IMGV curriculum was adapted for N2F to remove certain topics of particular relevance to people with chronic pain (pain education) and replace them with topics relevant to people with Long COVID such as neuroplasticity and energy pacing (Table 1).
Table 1.
Curriculum by Week, Health Topics and Mind-Body Modalities.
| Title | Topics | Curriculum/Activity |
|---|---|---|
| Week 1: Introduction to the integrative medical group visit | Introduction to mindfulness, ground rules, structure of integrative medical group visit | Grounding and arriving meditation |
| Week 2: Our reactions to stress | Mind-body connection, parasympathetic and sympathetic nervous system, effects of stress | Body scan meditation |
| Week 3: The importance of healthy sleep | Healthy sleeping behaviors, role of neuroplasticity in recovery from injury | Mindful eating meditation Gratitude journaling Pleasant events chart |
| Week 4: Inflammation, nutrition, and acupressure | Goal setting introduced, discussion of nutrition as medicine, omega 3s, fiber, and vitamin D | Acupressure Unpleasant events chart |
| Week 5: Mood, challenging relationships, and health | Challenging communication and effective communication styles, approaches to depression | Sitting meditation Loving kindness meditation |
| Week 6: COVID news, nutrition review, and movement as medicine | Patient directed topics in the news, mind-body approaches for life management, introduction to yoga | Chair yoga Loving kindness meditation |
| Week 7: Mindful eating and setting goals | Mindful eating, new options for enjoying food, setting goals | Breathing space meditation |
| Week 8: Wellness review and graduation | Wellness review, naming participants' strengths | Self-massage |
The original IMGV model provided patients with a printed manual as well as access to an electronic resource aimed at supplementing the curriculum content. For telehealth delivery of the IMGV for patients with chronic pain, patients received a digital copy of the curriculum manual and access to a website with supplemental materials (such as meditation videos and audio recordings, health education videos, and worksheets). For N2F, the manual and website were modified to reflect the updated curriculum content for people with Long COVID.
IMGV was originally designed to be delivered in-person in primary care clinics, usually in a conference room, break room, or other space large enough to accommodate the group. Groups ranged in size from about 8 to twelve patients. 20 The intervention is delivered by a billing provider, either a physician or advanced practice provider, as well as a mindfulness instructor or yoga teacher. The physician and yoga instructor attended a training on facilitation of integrative medical group visits prior to implementation of the program. The training was provided by the Integrated Center for Group Medical Visits in Lawrence, Massachusetts.
To deliver IMGV via telehealth, the intervention was adapted for delivery on the Zoom teleconferencing platform. When needed, patients received an orientation to Zoom, as well as printed instructions on how to use the platform. For N2F, the first cohort of the intervention was delivered by the same physician and yoga instructor team that had previously been leading the IMGV for patients with chronic pain. The second cohort of N2F was co-facilitated by the physician and 1 of the patients with Long COVID who had participated in the first cohort (who had previous experience in mindfulness, yoga, and group facilitation).
The original IMGV was delivered in person for 2 hours weekly over 9 weeks, followed by a 10th session at 21 weeks. For telehealth delivery, and when implementing IMGV in a new context, the 10th session was cut for feasibility purposes. When designing N2F, the intervention was shortened to 8 weeks, again for the purpose of easing scheduling challenges for an ongoing program. The providers found that starting new cohorts on the first week of a month was easier for scheduling purposes.
Statistical Analysis
The outcomes of interest were the 4 PROMS described above: PSS-10, GAD-2, SSS, and MYMOP®. After confirming normality among these continuous variables, we compared baseline and post-intervention scores using paired t-tests to control for within-individual variability. We performed a complete case analysis using the fourteen participants who completed the intervention and both assessments. The a priori alpha was set to .05 for the two-tailed P-values. We were interested in both clinical significance as well as statistical significance, therefore, we calculated the magnitude of differences in the pre and post scores as well as the 95% confidence intervals around the mean difference. Given the small sample size and the exploratory nature of the analysis, no subgroup analyses or interactions were tested. All analyses were performed in SAS 9.4. 21
Results
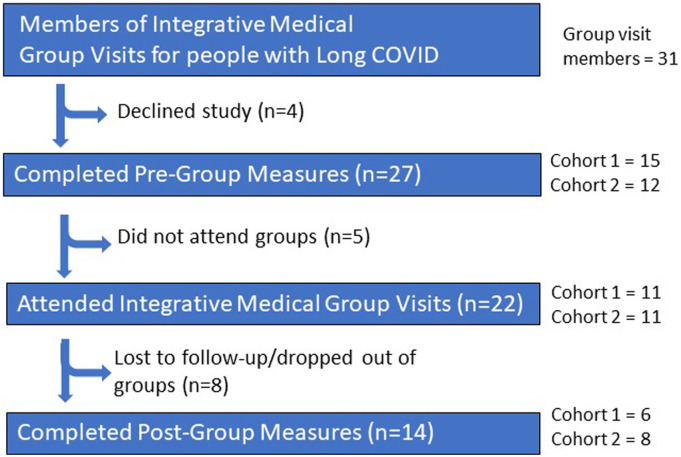
Out of 31 people who attended the groups, a total of 27 participants were enrolled in the study and all of them completed pre-group surveys. All participants reachable by phone at the end of the study completed all PROMS. Cohort 1 contained 15 study participants of whom 4 did not attend any of the group visits. Reasons for not attending were not captured. Cohort 2 contained 12 study participants and 1 study participant did not attend the group (for unknown reasons). Of the 11 participants in Cohort 1, 6 participants completed post-group measures and 5 participants were not reachable. Of the 11 participants in Cohort 2, 8 participants completed post-group measures, and 3 participants were not reachable.
There were 8 sessions in the intervention, and among the 22 participants that attended the intervention, the mean number of sessions in attendance was 5.59 (SD 2.6). Among the subset of 14 participants reachable for post-group surveys, the mean attendance was 7.21 (SD 1.2).
Among these 14 participants who completed the study, the sample was majority female (78.6%), non-Hispanic White (71.4%) and maintained private insurance coverage (78.6%). The mean age of participants was 48.9 years (SD = 13.7 years). The mean number of days since COVID-19 diagnosis was 285.4 days (SD = 116.1 days). See Table 2 for additional details.
Table 2.
Descriptive Statistics and Clinical Characteristics of Sample, n = 14.
| Mean | SD | |
|---|---|---|
| Age | 48.93 | 13.69 |
| Days since COVID diagnosis | 285.36 | 116.05 |
| N | % | |
| Length of time since onset of primary symptom | ||
| 4-12 weeks | 1 | 7.14 |
| 3 months-1 year | 12 | 85.71 |
| 1-5 years | 1 | 7.14 |
| Sex | ||
| Female | 11 | 78.57 |
| Male | 3 | 21.43 |
| Race | ||
| White or European american | 10 | 71.43 |
| Black or african american | 3 | 21.43 |
| Asian or Pacific islander | 1 | 7.14 |
| Ethnicity | ||
| Non-hispanic | 14 | 100 |
| Insurance | ||
| Private insurance | 11 | 78.57 |
| Medicaid | 1 | 7.14 |
| Medicare | 1 | 7.14 |
| Military insurance | 1 | 7.14 |
| MYMOP® patient-generated primary symptom | ||
| Fatigue | 4 | 28.57 |
| Shortness of breath | 3 | 21.43 |
| Brain fog | 2 | 14.29 |
| Other Anxiety (1), headache (1), instability in walking and moving (1), joint pain (1), lightheadedness (1) |
5 | 35.71 |
| MYMOP® patient-generated secondary symptom | ||
| Fatigue | 5 | 35.71 |
| Brain fog | 2 | 14.29 |
| Chest pain, cardiac symptoms | 2 | 14.29 |
| Other Anxiety (1), joint problems (1), lightheadedness (1), Phantom sensory information (1), wheezing (1) |
5 | 35.71 |
| Activity interference | ||
| Work | 6 | 42.86 |
| Walking/running/exercise | 3 | 21.43 |
| Driving | 2 | 14.29 |
| Socializing | 2 | 14.29 |
| Grocery shopping | 1 | 7.14 |
Changes in pre and post means were not significant in this pilot study. A larger study, including a control group, is necessary to evaluate the effectiveness of IMGV for Long COVID. PROMs reflected a trend in decreased symptomology in all measures except the questions about waking unrefreshed and the wellbeing scores (Table 3). Both items remained unchanged comparing pre and post scores using paired t-tests. The perceived stress scale (PSS-10) and primary symptoms reported via the MYMOP® were different from pre to post-group. There was a difference in PSS-10 between the pre (M = 21.9, SD = 6.6) and post (M = 18.5, SD = 5.7); t (3) = -3.2, P = .007 scores. There was also a difference in the primary complaint score between the pre (M = 4.7, SD = .9) and post (M = 3.5, SD = 1.3); t (3) = -3.5, P = .004 scores. There were no symptoms that worsened after the IMGV group. Adverse events were not measured. Participants were asked if they would refer a friend to the group. Sample responses are listed in Table 4.
Table 3.
Mean Change in Preand Post-Group Measures Calculated by Paired t-test (n = 14).
| Pre (SE) | Post (SE) | Difference | 95% CI | P value | |
|---|---|---|---|---|---|
| PSS-10* Total | 21.93 (1.8) | 18.50 (1.5) | −3.43 | −5.75, −1.11 | .007 |
| SSS*: Fatigue | 2.28 (.1) | 2.07 (.2) | −.21 | −.68, .25 | .336 |
| SSS: Waking unrefreshed | 2.29 (.2) | 2.29 (.2) | .00 | −.32, .32 | 1.000 |
| SSS: Trouble thinking | 1.86 (.2) | 1.64 (.3) | −.21 | −.78, .35 | .426 |
| GAD-2* | 3.71 (.8) | 2.29 (.4) | −1.43 | −3.12, .26 | .091 |
| MYMOP®* | |||||
| Primary reported symptom | 4.75 (.2) | 3.50 (.4) | −1.25 | −2.02, −.48 | .004 |
| Secondary reported symptom | 4.18 (.4) | 3.54 (.4) | −.64 | −2.05, .76 | .342 |
| Activity interference | 4.57 (.3) | 3.93 (.5) | −.64 | −1.79, .50 | .247 |
| Well-being | 3.64 (.4) | 3.64 (.3) | .00 | −.75, .75 | 1.000 |
| Overall MYMOP® score | 4.29 (.2) | 3.65 (.2) | −.63 | −1.33, .07 | .073 |
* Abbreviations: GAD-2 = Generalized Anxiety Disorder 2 item questionnaire; MYMOP® = Measure Yourself Medical Outcome Profile; PSS-10 = Perceived Stress Scale 10 question version; SSS = Fibromyalgia Symptom Severity Scale.
Table 4.
Participant feedback from Integrative Medical Group Visit for people with Long COVID.
| Would You Recommend the Group to Your Friends? Why or Why not? |
|---|
| 1. “Definitely, because before then I felt alone. Sometimes I felt like maybe there is something wrong with me, because going to doctors that didn’t understand long haul. And when you got there, it normalized my feelings and made me feel supported.” -Participant 204 |
| 2. “Yes, I think I would definitely recommend it to my friends. One of the biggest things I took away from it, outside of just the educational aspect, was that people are looking for an environment where someone else is sitting in their shoes. And someone can truly empathize vs just sympathizing and that’s pretty difficult given most people that were on the call have gone through this and they seem to be the only long haulers within their immediate circle. Whoever may have contracted it next to them may have turned out fine and they are still the only ones going through these symptoms. So that piece of it was amazing. The level of validation that it provided especially when you go through a lot of clinicians that chalk it up to just anxiety… so, I would definitely recommend it.” -Participant 210 |
| 3. “What I wanted from the group that I really would’ve wanted it would’ve been some cutting-edge data or conversation about what’s really going on with treatments for a long covid. The support was wonderful, in the meditation and…yoga and things like that were absolutely wonderful for us to learn those things so we can get our bodies in a relaxed state. I Was a little disappointed that we didn’t get a lot of the hard data from the sessions.” -Participant 109 |
| 4. “I would because I feel like it’s something that can help, and I think a lot of us look at it as an accomplishment especially once we finish and got the certificate for it. I Thought that was really great.” -Participant 110 |
| 5. “Yeah, absolutely because it gave a lot of information. They touched on mediation and yoga and holistic foods. Also just interaction, that knowing that you’re not alone in the long road that you’ve been on is always good for the spirit.” -Participant 116 |
| 6. “I would recommend it because it kept my sanity. It validated my symptoms when nobody else understood what I was going through, and it made me feel normal.” -Participant 117 |
Fatigue was the most common primary or secondary symptom cited by 64.3% of patients on the MYMOP® (28.6% of patients chose fatigue as their primary symptom and 35.7% chose fatigue as their secondary symptom). Brain fog was reported as the primary or secondary symptom by 3 participants. When asked to report activities where participants experienced the most interference, 6 people or 42.9% of the sample responded with work-related activities. The second most common activity interference was walking/running/exercise, which was reported as impaired in 3 participants.
Missing data
There were no differences in PSS-10, GAD-2, SSS questions, primary symptom, secondary symptom, activity interference, feeling of wellbeing, or total MYMOP® (measured at baseline) comparing the 8 participants without post-group data to the 14 with pre- and post-group data who attended group. People who completed the study were on average 5 years older and had a mean 285.4 (SD 116.1) days since their COVID-19 diagnosis compared to 200.3 days (SD 167.4) among those who did not complete the study.
Discussion
Findings indicate that measures of perceived stress, anxiety, and patient-generated symptomatology are feasible targets for measuring treatment outcomes among Long COVID patients attending IMGV groups. The PSS score decreased by 3.43 points (CI –5.75, −1.11; P value .007). The GAD-2 decreased by 1.43 points (CI -3.12, .26; P value .091). The primary reported symptom improved by 1.25 points (CI –2.02, −.48; P value .004). While study participants showed improvement in these indicators, this pilot study was not designed to test the efficacy of IMGV for Long COVID.
The choice of PROMs for this study was based upon common symptomatology, clinical experience, and interest in the feasibility of an individualized person-centered outcome measure. The heterogeneity of Long COVID presents a challenge for measuring treatment outcomes. An individualized person-centered outcome measure, such as the MYMOP®, is 1 method of identifying key symptomatology and tracking change over time. In this study, participants understood the MYMOP® when delivered verbally by a research assistant. Among participants who remained enrolled in the study and were reachable by phone, there was 100% completion of all study measures. Pilot data shows MYMOP® measures of primary symptoms, secondary symptoms, and “activity interference” improved post-group. These findings support the use of the MYMOP® in future studies. To further validate the MYMOP®, a future trial design could set an a priori hypothesis regarding correlation of effect size of the MYMOP® in relation to other measures as suggested by Ishaque, et al. 16
This pilot data suggests that the PSS, GAD-2, and MYMOP® are feasible measures of Long COVID symptomatology and supports the need for future larger trials that are designed to evaluate efficacy. IMGV is currently offered to Long COVID patients based upon the hypothesis that Integrative Medical Group Visits support wellbeing among patients with Long COVID, and that supporting wellbeing will decrease Long COVID symptomatology (see Figure 1 above). To test this hypothesis, a larger study with a control arm, baseline health indicators such as smoking status, BMI, and chronic illness, and the collection and reporting of adverse events would be necessary.
The pandemic has impacted health care and new ways of delivering that healthcare have begun to surface including synchronous video medical group visits. 22 To our knowledge, this is 1 of the first studies to report patient reported outcomes from group medical visits for the treatment of Long COVID. Another similar model was reported by Lin, et al. They describe a shared medical appointment (SMA) at the Cleveland Clinic that has been used to deliver weekly content over 6 weeks to those with Long COVID symptoms. Like IMGV, the program offers lifestyle education, mindfulness training and group peer support, whereby participants can share their experiences, setbacks, and successes. 23
This study was designed to test the feasibility of measures to evaluate IMGV for Long COVID. Limitations to this study include the lack of a control arm. A randomized controlled trial would control the extent to which patients with Long COVID not receiving the intervention improve over time. A comparison of concomitant diseases, medications and therapies would strengthen a future efficacy trail. Future studies would benefit from a formal protocol to collect and report adverse events. This was a feasibility study, with no control group and not powered to detect a change in pre- and post-group measures. This limits the ability to assert that improvements in measures were due to the intervention.
There were 13 out of 27, or 48.1%, of study participants who did not complete the study (see Figure 2 above for details). This is a larger dropout rate than previous studies of IMGV which have found a 20% dropout rate. 20 Therefore, future studies will be strengthened by capturing barriers to attendance and reasons for discontinuation.
Figure 2.
Flow diagram of study enrollment.
As in previous studies of IMGV, the study sample contained fewer men than women. 24 This may be due in part to the differences observed in women reporting symptoms of Long COVID more frequently than men, and it is also possible that improved recruitment methods are needed to achieve a more gender-balanced sample.
The lack of standardized criteria for Long COVID diagnosis is another limitation. Given the lack of available testing early in the pandemic, not all participants had a history of PCR testing confirmation of COVID-19 infection. There is general agreement that the 2 key factors incorporated in a diagnosis include prior confirmed or presumed SARS-CoV-2 infection and lingering health issues attributed to the prior infection which continue past the window of acute illness. However, health organizations have offered conflicting diagnostic criteria. The CDC suggests health issues must last at least 4 weeks for a diagnosis of Long COVID while The National Institute for Health and Care Excellence in the United Kingdom suggests 12 weeks. 2
Despite these limitations, the results of this study are promising and contribute to this important area of research. Hybrid research designs are needed to continue developing treatments while simultaneously addressing the current needs of Long COVID patients for treatment and support. The prioritized needs of Long COVID patients may change as the persistence of disabling symptoms is further understood. The flexibility of the IMGV model presents an opportunity to address social determinants of health. For example, housing instability, questions about disability insurance, and food insecurity can be addressed within the IMGV model.
There are many unanswered questions regarding key mechanisms of Long COVID. It may take years to answer these questions. In the meantime, a deluge of patients with the constellation of fatigue, cognitive impairment, and psychiatric conditions need help. The health care system faces a challenge to provide interventions that are minimally harmful and maximally helpful. Virtual Integrative Medicine Group Visits are a potential mechanism for meeting the needs of Long COVID patients. The IMGV offers promise with delivering didactic content virtually while simultaneously focusing on integrative strategies to combine mind-body approaches, social support, professional care, and skill building.
Conclusion
Findings support the use of the Perceived Stress Scale, the 2 question Generalized Anxiety Disorder scale, and the patient specific MYMOP® measure of primary symptomatology to measure outcomes in Long COVID patients in Integrative Medical Group Visits. Given the small number of participants, it is not possible to comment on the power of these measures to detect changes in Long COVID symptomatology. Long COVID is a public health emergency, and while research is needed to further refine this intervention, these findings are powerful enough to support a hybrid study design that tests adaptation while simultaneously implementing Integrative Medical Group Visits for Long COVID patients.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the National Center for Complementary and Integrative Health (5T32AT00378-12); National Institute of Mental Health (R01MH124752).
ORCID iDs
Jessica L Barnhill https://orcid.org/0000-0003-3360-4217
John M Baratta https://orcid.org/0000-0002-1124-7928
Paula Gardiner https://orcid.org/0000-0002-3663-000X
References
- 1.Bull-Otterson L, Baca S, Saydah S, et al. Post–COVID conditions among adult COVID-19 survivors aged 18–64 and ≥65 Years — United States, March 2020–November 2021. MMWR Morb Mortal Wkly Rep. 2022;71(21):713-717. doi: 10.15585/MMWR.MM7121E1 [DOI] [Google Scholar]
- 2.https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/post-covid-conditions.html Post-COVID Conditions: Information for Healthcare Providers. (n.d.). Retrieved May 3, 2023, from.
- 3.Su Y, Yuan D, Chen DG, et al. Multiple early factors anticipate post-acute COVID-19 sequelae. Cell. 2022;185(5):881-895.e20. doi: 10.1016/J.CELL.2022.01.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nalbandian A, Sehgal K, Gupta A, et al. Post-acute COVID-19 syndrome. Nat Med. 2021;27(4):601-615. doi: 10.1038/s41591-021-01283-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Whitaker M, Elliott J, Chadeau-Hyam M, et al. Persistent symptoms following SARS-CoV-2 infection in a random community sample of 508,707 people. medRxiv. 2021;28:21259452. Published online July 3, 2021:2021.06. doi: 10.1101/2021.06.28.21259452. [DOI] [Google Scholar]
- 6.Herrera JE, Niehaus WN, Whiteson J, et al. Multidisciplinary collaborative consensus guidance statement on the assessment and treatment of fatigue in postacute sequelae of SARS-CoV-2 infection (PASC) patients. PM&R. 2021;13(9):1027-1043. doi: 10.1002/pmrj.12684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fine JS, Ambrose AF, Didehbani N, et al. Multi‐disciplinary collaborative consensus guidance statement on the assessment and treatment of cognitive symptoms in patients with post‐acute sequelae of SARS‐CoV‐2 infection (PASC). PM&R. 2022;14(1):96-111. doi: 10.1002/pmrj.12745 [DOI] [PubMed] [Google Scholar]
- 8.Maley JH, Alba GA, Barry JT, et al. Multi-disciplinary collaborative consensus guidance statement on the assessment and treatment of breathing discomfort and respiratory sequelae in patients with post-acute sequelae of SARS-CoV-2 infection (PASC). PM R. 2022;14(1):77-95. doi: 10.1002/PMRJ.12744 [DOI] [PubMed] [Google Scholar]
- 9.Gardiner P, Lestoquoy AS, Gergen-Barnett K, et al. Design of the integrative medical group visits randomized control trial for underserved patients with chronic pain and depression. Contemp Clin Trials. 2017;54:25-35. doi: 10.1016/j.cct.2016.12.013 [DOI] [PubMed] [Google Scholar]
- 10.Gardiner P, Dresner D, Barnett KG, Sadikova E, Saper R. Medical group visits: A feasibility study to manage patients with chronic pain in an underserved urban clinic. Glob Adv Health Med. 2014;3(4):20-26. doi: 10.7453/gahmj.2014.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee EH. Review of the psychometric evidence of the perceived stress scale. Asian Nurs Res. 2012;6(4):121-127. doi: 10.1016/J.ANR.2012.08.004 [DOI] [PubMed] [Google Scholar]
- 12.Kroenke K, Spitzer RL, Williams JBW, Monahan PO, Löwe B. Anxiety disorders in primary care: Prevalence, impairment, comorbidity, and detection. Ann Intern Med. 2007;146(5):317-325. doi: 10.7326/0003-4819-146-5-200703060-00004 [DOI] [PubMed] [Google Scholar]
- 13.Wolfe F, Clauw DJ, Fitzcharles MA, et al. The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care Res. 2010;62(5):600-610. doi: 10.1002/ACR.20140 [DOI] [PubMed] [Google Scholar]
- 14.Paterson C.Measuring outcomes in primary care: a patient generated measure, MYMOP, compared with the SF-36 health survey. BMJ (Clinical Research Ed.) 1996;312(7037):1016-1020. 10.1136/bmj.312.7037.1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ishaque S, Johnson JA, Vohra S. Individualized health-related quality of life instrument Measure Yourself Medical Outcome Profile (MYMOP) and its adaptations: A critical appraisal. Qual Life Res. 2019;28(4):879-893. doi: 10.1007/S11136-018-2046-6/TABLES/4 [DOI] [PubMed] [Google Scholar]
- 16.Ursini F, Ciaffi J, Mancarella L, et al. Fibromyalgia: A new facet of the post-COVID-19 syndrome spectrum? Results from a web-based survey. RMD Open. 2021;7(3):e001735. doi: 10.1136/rmdopen-2021-001735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Roth IJ, Tiedt MK, Barnhill JL, et al. Feasibility of implementation mapping for integrative medical group visits. J Altern Complement Med. 2021;27(S1):S71-S80. doi: 10.1089/ACM.2020.0393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Roth I, Kavalakatt B, Chilcoat A, et al. Implementing Integrative Medical Group Visits for Patients with Chronic Pain: Findings from a Pilot Study. APHA.; 2021. [Google Scholar]
- 19.Gardiner P, Luo M, D’Amico S, et al. Effectiveness of integrative medicine group visits in chronic pain and depressive symptoms: A randomized controlled trial. PLoS One. 2019;14(12):e0225540. doi: 10.1371/journal.pone.0225540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.https://support.sas.com/software/94/ SAS 9.4 Software Overview for the Customer. (n.d.). Retrieved May 3, 2023, from.
- 21.Hussain-Shamsy N, McMillan I, Cook S, et al. Operationalizing and evaluating synchronous virtual group health interventions: Wide-scale implementation at a tertiary care academic hospital. J Med Internet Res. 2022;24(4):e29841. doi: 10.2196/29841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lin Y, Saper R, Patil SJ. Long COVID shared medical appointments: Lifestyle and mind-body medicine with peer support. Ann Fam Med. 2022;20:383. Published online April 20. doi: 10.1370/afm.2817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gardiner P, Lestoquoy AS, Negash NL, et al. Lessons learned and strategies for recruitment of diverse, low-income patients into an integrative medical group visit clinical trial. Explore. 2019;15(3):215-221. doi: 10.1016/j.explore.2019.01.003 [DOI] [PubMed] [Google Scholar]
- 24.Sivan M, Taylor S. NICE guideline on long covid. BMJ. 2020;371:m4938. doi: 10.1136/BMJ.M4938 [DOI] [PubMed] [Google Scholar]