Abstract
Background:
Limited published data suggests that absence of uplifts (minor pleasant events) is associated with clinical worsening in patients with chronic fatigue syndrome (CFS). The current study aimed to assess the relation of illness worsening to the trajectories of social and non-social uplifts and hassles in a six-month prospective study in CFS.
Methods:
Participants were primarily in their 40s, female, white, and ill for over a decade. All participants (N=128) met criteria for CFS. The interview-based global impression of change rating was used to classify individual outcomes as improved, unchanged, or worsened at six- month follow-up. Uplifts and hassles, both social and non-social, were assessed with the Combined Hassles and Uplifts Scale (CHUS). The CHUS was administered weekly in online diaries over six months. Linear mixed effect models were utilized to examine linear trends for hassles and uplifts.
Results:
No significant differences were found between the three global outcome groups for age, sex, or illness duration; however, work status was significantly lower for the non-improved groups (p<.001). Non-social hassles intensity showed an increasing slope for the worsened group (p=.03) and a decreasing slope (p=0.05) for the improved group. For the worsened group, a downward trend was found for frequency of non-social (p=0.01) uplifts.
Conclusion:
Individuals with worsening as compared to improving illness in CFS show significantly different six-month trajectories for weekly hassles and a deficit in uplifts. This may have clinical implications for behavioral intervention.
Trial Registration:
Keywords: uplifts, hassles, social events, worsening, chronic fatigue syndrome
Background
Psychological uplifts are minor pleasant events, such as completing a rewarding task, that occur in daily life [1]. Although these events appear to be important to well-being [2], they have not been extensively studied. By comparison, minor stressors or “hassles,” such as misplacing things, have received considerably more empirical attention. Hassles have been associated with increased somatic health symptoms, e.g., backaches, headaches [1], as well as decreases in health and positive mood, whereas uplifts can make a person feel joyful, glad, or satisfied [2]. Uplifts and positive events are correlated with lower fatigue in individuals with chronic fatigue and chronic pain [3, 4].
Uplifts and hassles also appear to have biobehavioral effects. A cross-sectional study of healthy adults [5] suggested that hassles and uplifts significantly and independently predicted changes in inflammation markers (e.g., Interleukin-6 (IL-6)), independent of sociodemographic, biological, and psychological measures, including depressed mood. A later prospective study of over 900 middle-aged adults [6] found that the frequency of daily positive events was associated with lower inflammatory markers (IL-6 and C-Reactive Protein) in the overall sample, and lower fibrinogen among women. Effects were more pronounced for participants in the lowest quartile of positive event frequency, suggesting that lack of positivity in daily life may be particularly consequential for inflammation. Furthermore, interpersonal positive events were more predictive of lower IL-6 overall and lower fibrinogen in women than non-interpersonal positive events. The authors concluded that daily positive events may serve a protective role against inflammation, a biological factor which may contribute to the pathophysiology of particular subgroups in chronic fatigue syndrome (CFS) [7].
Apart from biological correlates, several behavioral papers [8] suggest that social interactions may play a role in determining the magnitude of fatigue experienced by those with chronic pain [9]. Specifically, investigations of rheumatoid arthritis, osteoarthritis, and fibromyalgia (FM) patients have shown that positive interpersonal events are associated with lower daily fatigue and negative interpersonal events are correlated with elevated daily fatigue [9, 10]. Furthermore, the impact of hassles may also play a role in negative outcomes. A cross-sectional study [11] comparing newly diagnosed CFS and FM patients to multiple sclerosis and arthritis patients found that the combined CFS and FM group showed a higher frequency and higher emotional impact of daily hassles. This may indicate a need for better coping with hassles and/or positive behavioral changes that may reduce hassles as part of a self-management program [12]. These reported associations between commonly experienced positive and negative events, and fatigue symptoms in chronic pain and chronic fatigue conditions suggest that clinical approaches to potential illness improvement may be enhanced with careful assessments of these interactive phenomena.
Recently, a six-month observational study of a biobehavioral model in CFS [13] found that decreased intensity of behavioral uplifts, as assessed on the Combined Hassles and Uplifts scale (CHUS)[14], was the only significant behavioral predictor of patient-reported global non-improvement. Given this intriguing, if somewhat imprecise finding, perhaps the CHUS measure could be more informative if greater specificity could be applied to its constructs. For instance, in a study on relationship satisfaction [15], hassles and uplifts on an abbreviated version of the CHUS were grouped into those dealing with social (e.g., family, friends) and non-social (e.g., job, health) events. Contrary to their hypothesis, non-social uplifts had the strongest positive impact on relationship satisfaction. In CFS, the influence of these minor social and non-social events may shed light on their relative importance in influencing outcomes.
With respect to longer-term outcomes, positive impacts of uplifts have been reported in a one-year prospective study of 130 patients with chronic fatigue syndrome (CFS)[3]. This study found that pleasant activities and/or life events implying moderate or major life changes were associated with significantly improved outcomes, including reduced fatigue and impairment. Similarly, a clinical model of behavioral intervention in CFS [12] suggested therapeutic prescription of uplifting activities and the enhancement of positive coping skills to diminish the impact of hassles and improve outcomes. These clinical research threads may have implications for better-targeted approaches to behavioral management for patients with fatiguing illness.
The purpose of the current report was to assess the relation of the global outcomes of illness worsening and improvement to the trajectories of social and non-social uplifts and hassles in a six-month prospective study in CFS. Although the global outcome rating is frequently used as an important indicator of perceived change in CFS observational and intervention studies [16–18], its relation to potentially influential patterns of uplifts, hassles, and social and non-social events has not been studied. Furthermore, validated weekly assessments, rarely reported in CFS observational studies, may have utility in identifying specific behavioral patterns that may influence outcomes, particularly illness worsening that, in turn, may inform therapeutic management strategies.
Methods
Participants and procedure
This report utilized data from a six-month home-based observational study in 128 CFS patients, detailed elsewhere [13] that examined biobehavioral predictors of global outcomes. Most participants were in their 40s (M age = 46.11, SD = 11.8), female (87.2%), white (90.3%), unemployed or on disability (67.9%), and ill with CFS for over a decade (M = 16.5 years, SD = 10.3). Baseline questionnaire scores showed clinically relevant fatigue severity (Fatigue Severity Scale; [19]), impaired physical function (SF-36 Physical Function Subscale; [20]), and elevated autonomic symptoms (COMPASS; [21]. The entire study sample met symptom and impairment criteria for CFS [22], as assessed in a validated phone interview [23] conducted by research nurses (PB, MM) experienced in chronic fatigue and chronic pain assessments.
The primary study protocol [13] (Table 1) classified subjects into improved and non-improved groups with behavioral predictors (e.g., uplifts) based on 26-week means. The current study divided the CFS sample into three outcome groups, i.e., improved, unchanged, and worsened and created new variables for social and non-social uplifts and hassles. Weekly uplifts and hassles scores drawn from assigned web diaries were utilized in the data analysis as behavioral predictors of outcomes across the three outcome groups, which were treated as response variables in our models.
Table 1.
Protocol of primary study
|
Nationwide recruitment in the United States began in September, 2016 and ended in October, 2019. Recruitment methods included study announcements posted on major CFS patient support websites (e.g., Health Rising, SolveME) and in the large private practices of CFS specialized physicians located in New York and Utah. Without a travel requirement, this home-based study was considered more likely to recruit these under-served patients, particularly those who were disabled and homebound [24]. This study was approved by the Stony Brook University Committee on Research Involving Human Subjects which reviewed and approved the study procedure. All participants provided written informed consent via land mail of signed consent forms. Participants were compensated up to $300 for their participation. The study was pre-registered on ClinicalTrials.gov (NCT02948556).
Measures
Hassles and uplifts.
Hassles and uplifts were measured with the Combined Hassles and Uplifts Scale (CHUS)[14]. A 26-week weekly web diary (ScienceTrax, Inc., Macon, Georgia) contained the 53-item CHUS which measures perceived hassles and uplifts. Hassles are defined as “irritants—things that annoy or bother you; that can make you upset or angry.” Uplifts are defined as “events that make you feel good; that can make you joyful, glad, or satisfied.” The CHUS yields subscales of frequency and intensity. Hassles and uplifts frequency scores have a potential range of 0 to 53, with the total score indicating how many items were simply endorsed. When endorsing an item, participants are asked to rate how much of a hassle or uplift the specific item was. Items are rated on a 3-point Likert-based scale ranging from 1 (somewhat), 2 (quite a bit), to 3 (a great deal). The average rating of these items yields intensity scores. Participants may rate events as hassles, uplifts, or both. The CHUS has shown good reliability and validity in predicting mood and somatic health outcomes [11, 25]. The measure has high test–retest reliability and a reported Cronbach’s alpha of 0.71 [2]. The CHUS alpha for the present study was excellent (α = 0.87).
Based on a prior study of relationship satisfaction [15], the CHUS items were subdivided into ten social (e.g., children, relatives, family obligations, friends) events and 43 non-social (e.g., job, Finances, exercise, health, neighborhood, pets, home maintenance, free time, recreation outside the home) events. The possible range of frequency scores for social events is 0–10 and for non-social events, 0–43. Means and standard deviations for intensity ratings in this study were: social hassles (M = 1.37, SD = .04), social uplifts (M = 1.72, SD = .03), non-social hassles (M = 1.66, SD = .02), and non-social uplifts (M = 1.48, SD = .02). Means and standard deviations for frequency totals were: social hassles (M = 3.21, SD = 0.33), social uplifts (M = 4.26, SD = 0.47), non-social hassles (M = 15.36, S D = 1.45), and non-social uplifts (M = 12.40, SD = 1.21).
Global Impression of Change.
The outcome assessment for overall change was measured with the Patient Global Impression of Change (PGIC) rating. The PGIC rating, assessed during the six-month follow-up phone interview of each participant, is based on seven levels of change ranging from very much worse to very much improved as it applied to the prior six months. Subjects who selected a PGIC rating of “very much worse,” “much worse,” or “somewhat worse” were assigned to the “worsened” subgroup. Individuals with an “unchanged” rating were assigned to the “unchanged” subgroup and participants who selected “very much improved,” “much improved,” or “somewhat improved” were assigned to the “improved” subgroup. The PGIC rating, which provides a generalized view of the patient’s perception of overall change [26, 27], has shown construct validity in CFS studies, including an empirical finding that patient-reported global outcomes of even modest improvement (the most commonly endorsed level in CFS), as opposed to no change or worsening, was associated with significantly improved fatigue (Fatigue Severity Scale) and functioning (SF-36 Physical Function Subscale) in a long-term outcome study [23]. More generally, CFS prospective studies have often relied on the PGIC as a broad outcome measure of improvement or worsening [16].
Power estimation
Sample size and power calculation issues were addressed in the primary study [13].
Data Analysis
Linear mixed effect models were utilized to examine and compare the linear trend of four qualitative types of hassles and uplifts over 26 weeks that included social intensity, non-social intensity, social frequency, and non-social frequency. With the assumption that hassles and uplifts exhibit linear trends over time, week was treated as a continuous variable. It was also hypothesized that patients in different outcome groups (improved vs unchanged vs worsened) would exhibit different weekly patterns; thus, an interaction term between week and outcome group was adjusted in our models. No other factors were adjusted in the regression models as this was an exploratory analysis.
Based on Akaike Information Criteria (AIC), the covariance structure to model correlations among longitudinal measurements from the same patient is selected from Compound Symmetry (CS), and first-order autoregressive (AR(1)), Toeplitz (TOEP), and Unstructured (UN). The coefficient of week, based on linear mixed effect models, was used to characterize the longitudinal pattern of behavioral measurement over 26 weeks. A coefficient > 0 suggests an increasing pattern and coefficient < 0 suggests a decreasing pattern. Statistical analysis was performed using SAS 9.4 (SAS Institute Inc., Cary, NC) and significance level is set at 0.05.
Results
The study sample consisted of 128 participants with global ratings at six-month follow-up of improved (29%; n = 37), unchanged (33%; n = 42) or worsened (38%; n = 49). No significant differences were found between groups for age, sex, or illness duration; however, work status was significantly reduced for the non-improved groups (χ2 = 819.72 (8); p < .001). Participant completion of weekly web diaries was excellent (95.6%).
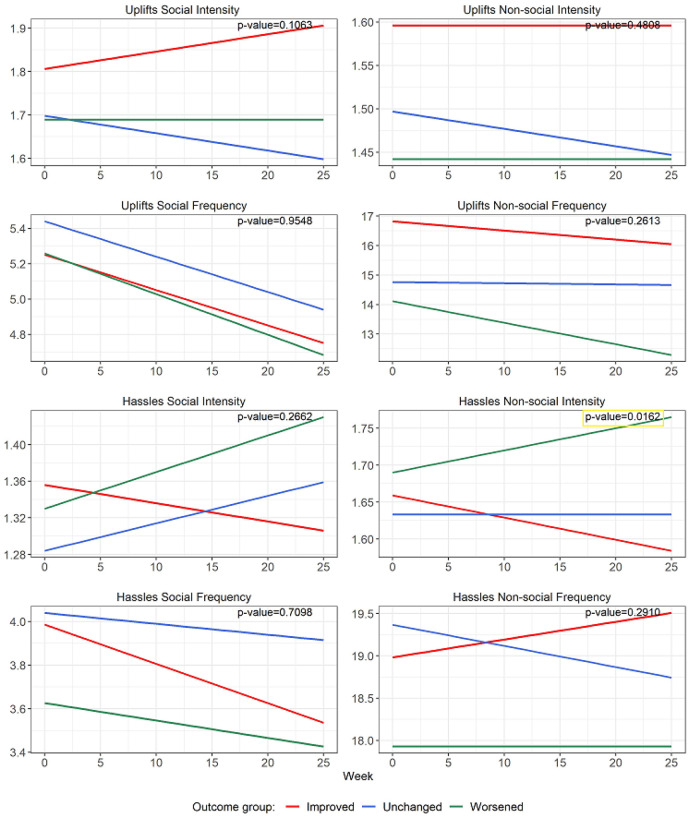
Over 26 weeks, the longitudinal profile of intensity of non-social hassles (Fig. 1; Table 2) was significantly different across the 3 groups (p = 0.016). More specifically, the worsened group showed a significantly increasing pattern (weekly change = 0.003, p = 0.033) of non-social hassles intensity (Table 3), while the improved group evidenced a significant decreasing pattern (weekly change = −0.003, p = 0.05).
Figure 1.
Linear regression lines of hassles and uplifts over 26 weeks based on linear mixed effect models. P-values indicate if there is a significant different among the three groups. This was found only for Hassles Non-social Intensity (right side, third down). The Uplifts Social Frequency graph (left side, second down) shows a significant downtrend in all three groups (p< .04).
Table 2.
Type 3 p-values of explanatory variables in linear mixed models for each type of hassles and uplifts
| Variable | Num DF | Den DF | F Value | P-value1 | Covariance Structure |
|---|---|---|---|---|---|
| Uplifts Social Intensity | |||||
| Week | 1 | 2791 | 0.00 | 0.9503 | |
| Outcome group | 2 | 125 | 0.75 | 0.4766 | |
| Week * Outcome group | 2 | 2791 | 2.24 | 0.1063 | |
| Uplifts Non-social Intensity | |||||
| Week | 1 | 2852 | 0.38 | 0.5371 | |
| Outcome group | 2 | 125 | 2.25 | 0.1098 | |
| Week * Outcome group | 2 | 2852 | 0.73 | 0.4808 | |
| Uplifts Social Frequency | |||||
| Week | 1 | 2881 | 17.44 | < .0001 | |
| Outcome group | 2 | 125 | 0.10 | 0.9055 | |
| Week * Outcome group | 2 | 2881 | 0.05 | 0.9548 | |
| Uplifts Non-social Frequency | |||||
| Week | 1 | 2881 | 4.02 | 0.0450 | |
| Outcome group | 2 | 125 | 1.84 | 0.1628 | |
| Week * Outcome group | 2 | 2881 | 1.34 | 0.2613 | |
| Hassles Social Intensity | |||||
| Week | 1 | 2607 | 1.61 | 0.2052 | |
| Outcome group | 2 | 125 | 0.46 | 0.6296 | |
| Week * Outcome group | 2 | 2607 | 1.32 | 0.2662 | |
| Hassles Non-social Intensity | |||||
| Week | 1 | 2856 | 0.02 | 0.8931 | |
| Outcome group | 2 | 125 | 0.31 | 0.7346 | |
| Week * Outcome group | 2 | 2856 | 4.13 | 0.0162 | |
| Hassles Social Frequency | |||||
| Week | 1 | 2881 | 2.49 | 0.1145 | |
| Outcome group | 2 | 125 | 0.51 | 0.5996 | |
| Week * Outcome group | 2 | 2881 | 0.34 | 0.7098 | |
| Hassles Non-social Frequency | |||||
| Week | 1 | 125 | 0.02 | 0.8968 | |
| Outcome group | 2 | 125 | 1.16 | 0.3165 | |
| Week * Outcome group | 2 | 125 | 1.25 | 0.2910 | |
p-values were based on F-test from linear mixed models
TOEP = Toeplitz; UN = Unstructured
Table 3.
Estimated coefficients of week based on linear mixed models for each type of hassles and uplifts (trend slopes).
| Estimated coefficient of week showing weekly change | |||
|---|---|---|---|
| Group | Coefficient | 95% CI | P-value1 |
| Uplifts Social Intensity | |||
| Improved group | 0.004 | (−0.002, 0.009) | 0.1646 |
| Unchanged group | −0.004 | (−0.008, 0.001) | 0.1057 |
| Worsened group | 0 | (−0.004, 0.004) | 0.9480 |
| Uplifts Non-social Intensity | |||
| Improved group | 0 | (−0.003, 0.004) | 0.8602 |
| Unchanged group | −0.002 | (−0.005, 0.001) | 0.1760 |
| Worsened group | 0 | (−0.003, 0.003) | 0.9327 |
| Uplifts Social Frequency | |||
| Improved group | −0.02 | (−0.039, −0.001) | 0.0386 |
| Unchanged group | −0.02 | (−0.037, −0.003) | 0.0194 |
| Worsened group | −0.023 | (−0.039, −0.008) | 0.0033 |
| Uplifts Non-social Frequency | |||
| Improved group | −0.031 | (−0.098, 0.035) | 0.3554 |
| Unchanged group | −0.004 | (−0.065, 0.057) | 0.8866 |
| Worsened group | −0.073 | (−0.129, −0.017) | 0.0110 |
| Hassles Social Intensity | |||
| Improved group | −0.002 | (−0.007, 0.004) | 0.5620 |
| Unchanged group | 0.003 | (−0.002, 0.008) | 0.2042 |
| Worsened group | 0.004 | (−0.000, 0.008) | 0.0794 |
| Hassles Non-social Intensity | |||
| Improved group | −0.003 | (−0.007, 0.000) | 0.0510 |
| Unchanged group | 0 | (−0.003, 0.003) | 0.9860 |
| Worsened group | 0.003 | (0.000, 0.006) | 0.0330 |
| Hassles Social Frequency | |||
| Improved group | −0.018 | (−0.042, 0.006) | 0.1444 |
| Unchanged group | −0.005 | (−0.027, 0.017) | 0.6814 |
| Worsened group | −0.008 | (−0.029, 0.012) | 0.4210 |
| Hassles Non-social Frequency | |||
| Improved group | 0.021 | (−0.023, 0.066) | 0.3500 |
| Unchanged group | −0.025 | (−0.063, 0.013) | 0.1937 |
| Worsened group | 0 | (−0.035, 0.034) | 0.9817 |
p-values were based on T-test from linear mixed models.
The trend slope (Fig. 1; Table 3) for frequency of social uplifts significantly decreased over time in all three groups as follows: improved (weekly change = −0.02, p = 0.039), unchanged (weekly change = −0.02, p = 0.019), and worsened (weekly change = −0.02, p = 0.003). By comparison, only the worsened group showed a significantly decreasing pattern in the frequency of non-social uplifts (weekly change = −0.07, p = 0.011).
Comparing the trend slope across groups (Fig. 1; Table 3), the improved group and worsened group presented significantly different patterns of change for non-social hassles intensity (improved vs worsened groups: difference of coefficient of week = −0.006, p = 0.004). No other significant trends were found for uplifts or hassles.
Discussion
In this six-month observational study of individuals with CFS involving 26 weekly assessments, only a few clear differences were found between self-report worsened as compared to improved subjects on the dimensions of behavioral uplifts and hassles. The worsened group showing an increasing pattern for non-social hassles, while the improved group evidenced a decreasing pattern. In addition, the frequency of social uplifts significantly decreased in all three group across the six months assessment interval. However, only the worsened group showed a significant decrease in non-social uplifts frequency.
Uplifts Deficits and Worsening
Our finding of a downtrend in the frequency of Specifically “non-social” uplifts in the worsened group may have some overlap with our earlier study [13] in which a lower intensity of uplifts predicted self-report non-improvement (unchanged and worsened) in individuals with CFS. Perhaps non-social activities are more salutary as they are more readily available, more manageable, and potentially less energy-depleting than socially positive interactions [28]. In general, excessive fatigue is triggered in CFS in response to even minor activities [29], regardless of valence, and thus it may be challenging for patients to thread the needle to eventual illness improvement via greater uplifts, fewer hassles, and other positive self-management activities. Even if successful, relatively small improvements in illness symptoms may result, as suggested by the modest 15% downward trend of weekly fatigue ratings in the CFS improver group recorded over six months in the primary study [13]. Not surprisingly, in the current observational study, a far lower percentage of individuals rated themselves as improved as compared to two previous behavioral self-management trials in CFS [24, 30].
Speculatively, these findings could reflect an ongoing change process, only partially captured in this six-month study that may inform specific behavioral pathways to worsening and improvement. Fewer pleasant experiences in CFS have been associated with higher fatigue and lower functioning over 18 months [3]. In addition, our data revealed that the intensity of non-social hassles increased in worsened subjects and decreased in improved subjects (Fig. 1). More broadly, negative social events have been associated with higher daily fatigue in chronically fatiguing illnesses, e.g., fibromyalgia, rheumatic arthritis [8], suggesting that social interactions may play a role in determining the magnitude of ongoing fatigue experienced by those with chronic fatigue and pain [9].
As compared to the primary study [13], our expanded range of significant findings regarding uplifts and hassles as possible outcome predictors may be explained in part by several design changes in the present study: (1) the unit of analysis was weekly scores on the CHUS, rather than single 26-week means used for each subject in the primary study; (2) the use of separate categories for unchanged and worsened outcomes rather than the more generic non-improvement construct; and (3) the subdivision of hassles and uplifts into social and social sub-categories. Overall, the current analysis represents a fine-grained examination of hassles and uplifts in the experiences of individuals with CFS, which was likely to identify more precise and potentially more informative outcome predictors.
Clinical Implications
Although the salient illness variable of fatigue was not assessed as an outcome variable in this study, a critical element of improved outcomes in CFS is based on the patients’ personal efforts to effectively manage their illnesses such that well-being and functioning are maximized. In the absence of curative treatments, this is perhaps the most beneficial type of outcome that can be realistically achieved. In addition, perceived global improvement in CFS, even if modest, has been associated with significantly reduced fatigue and higher functioning over a two-year observational period [23]. Perhaps a clinical focus on selectively assigning uplifts and limiting hassles, as suggested by our findings, could be utilized as a straightforward approach to facilitating improvement in CFS. Potential therapeutic changes in target areas, as suggested by our hassles and uplifts findings, do not necessarily have to be of high magnitude to result in overall improvement.
Although not an intervention or controlled trial, clinically relevant findings in this observational study suggest the potential importance of uplifts to perceived global improvement in this difficult-to-treat illness. Uplifts can be a focus of behavioral management [12] if the clinician collaboratively identifies with the patient pleasant, enjoyable, low-effort activities that are often lacking in the lives of individuals with debilitating CFS [31, 32]. This may have relevance to CFS pathophysiology given that a large biobehavioral study in healthy adults suggested that the absence of positivity in daily life may be particularly consequential for inflammation [6].
Examples of positive events that could be applied clinically in CFS include listening to an inspirational speaker, going to a concert, watching ducks on a pond, sharing a special moment with a spouse or friend, or any other moderately pleasant activity that does not trigger long-duration symptom worsening. To generate ideas, the patient can be asked to make a list of 10 pleasant low-effort activities. Once these possibilities are identified, a flexible schedule is developed so that the patients can participate in pleasant activities at least several times a week. Although illness-related restrictions may have reduced opportunities to engage in pleasant experiences [12], about 1/3 of our (often homebound) study participants were apparently able to engage in uplifting activities and reduce the intensity of their hassles over several months to the point where they rated themselves as “improved.”
Our findings regarding worsening illness in association with fewer non-social uplifts are also consistent with developing beneficial treatment targets in two evidenced-based therapies, Behavioral Activation and Acceptance and Commitment Therapy. Although not described as “uplifts”, both treatments consist of helping patients to identify and clarify chosen values [33, 34], such as who is important to them (e.g., friends, family), what is important to them (e.g., physical and mental health, companionship) and what qualities of action they want to embody (e.g., loyalty, trustworthy, kindness). Once values are identified, clinicians help patients start to behave in ways in line with the chosen values in pursuing the most rewarding or intense socially uplifting activities by identifying who (i.e., spending time with grandchildren) or what (non-social) is in that category rather than participating in social gatherings that do not have the same valence (i.e., spending time with an acquaintance).
Furthermore, by encouraging patients to focus on chosen values, it is possible that they may also be less likely to be bothered by hassles, which were significantly greater in our worsened subjects. Both Behavioral Activation and Acceptance and Commitment Therapy have also been found to be associated with improved well-being [35, 36]. This may explain why in the current study, improved subjects experienced significantly less intense non-social hassles than their worsened counterparts. Future work should continue to examine the effect of improving the frequency of uplifts, or values, in patients with CFS on physical and emotional well-being.
Limitations
As this study was not a randomized treatment trial, clinical approaches to illness improvement may be suggested but not definitively recommended. Also, participant demographics heavily favored white females with long-term illness. Furthermore, weekly trajectories of uplifts and hassles were grouped and analyzed by global change categories which may have obscured potentially important individual patterns. Despite these limitations, the between-group distinctions were particularly notable given the opposing directions of change for hassles and uplifts evidenced in the longitudinal patterns of improved and worsened patients which are potentially of clinical relevance.
Conclusions
Given the controversies regarding the efficacy of well-publicized graded activity interventions in CFS [37], our alternate or perhaps complementary focus on behavioral uplifts and hassles as possible improvement predictors may be clinically useful. For instance, one path to behavioral improvement in CFS that is supported by our findings may be through the scheduling of more frequent non-social uplifts, and perhaps reducing the emotional impact of intense hassles (cf., [11]). These commonly experienced minor events can be voluntarily modified and therapeutically managed, with less potential adverse consequence than standard behavioral approaches in the service of improving well-being and outcomes in CFS.
Table 4.
Estimated difference of the coefficient of week based linear mixed models for each type of hassles and uplifts (difference of trend slope).
| Estimated difference in the coefficient of week | |||
|---|---|---|---|
| Group | Coefficient difference | 95% CI | P-value1 |
| Uplifts Social Intensity | |||
| Improved vs Unchanged | 0.007 | (0.001, 0.014) | 0.0346 |
| Improved vs Worsened | 0.004 | (−0.003, 0.011) | 0.2636 |
| Unchanged vs Worsened | −0.004 | (−0.010, 0.003) | 0.2519 |
| Uplifts Non-social Intensity | |||
| Improved vs Unchanged | 0.002 | (−0.002, 0.007) | 0.2989 |
| Improved vs Worsened | 0 | (−0.004, 0.005) | 0.9353 |
| Unchanged vs Worsened | −0.002 | (−0.006, 0.002) | 0.2924 |
| Uplifts Social Frequency | |||
| Improved vs Unchanged | 0 | (−0.026, 0.026) | 0.9948 |
| Improved vs Worsened | 0.003 | (−0.022, 0.028) | 0.8013 |
| Unchanged vs Worsened | 0.003 | (−0.020, 0.026) | 0.7933 |
| Uplifts Non-social Frequency | |||
| Improved vs Unchanged | −0.027 | (−0.117, 0.063) | 0.5589 |
| Improved vs Worsened | 0.042 | (−0.045, 0.129) | 0.3488 |
| Unchanged vs Worsened | 0.069 | (−0.014, 0.152) | 0.1056 |
| Hassles Social Intensity | |||
| Improved vs Unchanged | −0.005 | (−0.012, 0.003) | 0.2009 |
| Improved vs Worsened | −0.006 | (−0.013, 0.001) | 0.1190 |
| Unchanged vs Worsened | −0.001 | (−0.007, 0.006) | 0.8064 |
| Hassles Non-social Intensity | |||
| Improved vs Unchanged | −0.003 | (−0.008, 0.001) | 0.1495 |
| Improved vs Worsened | −0.006 | (−0.010, −0.002) | 0.0042 |
| Unchanged vs Worsened | −0.003 | (−0.007, 0.001) | 0.1457 |
| Hassles Social Frequency | |||
| Improved vs Unchanged | −0.014 | (−0.046, 0.019) | 0.4191 |
| Improved vs Worsened | −0.01 | (−0.041, 0.022) | 0.5423 |
| Unchanged vs Worsened | 0.004 | (−0.026, 0.034) | 0.8087 |
| Hassles Non-social Frequency | |||
| Improved vs Unchanged | 0.046 | (−0.012, 0.105) | 0.1207 |
| Improved vs Worsened | 0.022 | (−0.035, 0.078) | 0.4511 |
| Unchanged vs Worsened | −0.025 | (−0.076, 0.027) | 0.3420 |
p-values were based on T-test from linear mixed models.
Acknowledgements.
We thank Daniel Gordon, Marie Codella, Sydney Zhang, and Samantha Vasquez for their invaluable assistance in carrying out the essential support tasks involved in conducting this study.
Funding Statement
The project described was supported by National Institutes of Health Grant R01NR015850; (National Institute of Nursing Research; Principal Investigator: F. Friedberg). The work was also supported in part by the National Institute of Health T32 pre-doctoral training grant: T32GM108540 (trainee: J.L.A.) The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Nursing Research or the National Institutes of Health.
Footnotes
Ethnical approval and consent to participate. All procedures performed in studies involving human participants were in accordance with the ethnical standards of the institution and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethnical standards. This article does not contain any studies with animals performed by any of the authors. This study was approved by the Stony Brook University Committee on Research Involving Human Subjects and all participants provided informed consent for participation and publication.
Conflict of Interest Declaration. The authors declare that they have no conflict of interest.
Contributor Information
Fred Friedberg, Stony Brook University Renaissance School of Medicine.
Jenna L. Adamowicz, The University of Iowa
Patricia Bruckenthal, Stony Brook University School of Nursing.
Maria Milazzo, Stony Brook University School of Nursing.
Sameera Ramjan, Memorial Sloan Kettering Cancer Center.
Xiaoyue Zhang, Stony Brook University Renaissance School of Medicine.
Jie Yang, Stony Brook University Renaissance School of Medicine.
Data availability statement:
The data that support the findings of this study are available from the corresponding author (FF), upon reasonable request.
References
- 1.DeLongis A, Coyne JC, Dakof G, Folkman S. Lazarus RS, Relationship of daily hassles, uplifts, and major life events to health status, Health Psychology. 1982;1(2):119. [Google Scholar]
- 2.DeLongis A, Folkman S, Lazarus RS. The impact of daily stress on health and mood: psychological and social resources as mediators, Journal of Personality and Social Psychology. 1988;54(3):486. [DOI] [PubMed] [Google Scholar]
- 3.Ray C, Jefferies S, Weir WR. Life-events and the course of chronic fatigue syndrome, Br J Med Psychol. 1995;68(4):323–31. [DOI] [PubMed] [Google Scholar]
- 4.Dailey PA, Bishop GD, Russell IJ, Fletcher EM. Psychological stress and the fibrositis/fibromyalgia syndrome, J Rheumatol. 1990;17(10):1380–1385. [PubMed] [Google Scholar]
- 5.Jain S, Mills PJ, von Känel R, Hong S, Dimsdale JE, Effects of perceived stress and uplifts on inflammation and coagulability, Psychophysiology. 2007;44(1):154–60. [DOI] [PubMed] [Google Scholar]
- 6.Sin NL, Graham-Engeland JE, Almeida DM. Daily positive events and inflammation: findings from the National Study of Daily Experiences. Brain Behav Immun. 2015;43:130–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Strawbridge R, Sartor ML, Scott F, Cleare AJ. Inflammatory proteins are altered in chronic fatigue syndrome-a systematic review and meta-analysis. Neurosci Biobehav Rev. 2019;107:69–83. [DOI] [PubMed] [Google Scholar]
- 8.Finan PH, Okun MA, Kruszewski D, Davis MC, Zautra A.J., Tennen H., Interplay of concurrent positive and negative interpersonal events in the prediction of daily negative affect and fatigue for rheumatoid arthritis patients. Health Psychol. 2010;29(4):429–437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Davis MC, Zautra AJ, Younger J, Motivala SJ, Attrep J, Irwin MR. Chronic stress and regulation of cellular markers of inflammation in rheumatoid arthritis: implications for fatigue. Brain Behav Immun. 2008;22(1):24–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Parrish BP, Zautra AJ, Davis MC. The role of positive and negative interpersonal events on daily fatigue in women with fibromyalgia, rheumatoid arthritis, and osteoarthritis. Health Psychol. 2008;27(6):694–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Van Houdenhove B, Neerinckx E, Onghena P, Vingerhoets A, Lysens R, Vertommen H. Daily hassles reported by chronic fatigue syndrome and fibromyalgia patients in tertiary care: a controlled quantitative and qualitative study. Psychotherapy and Psychosomatics. 2002;71(4):207–213. [DOI] [PubMed] [Google Scholar]
- 12.Friedberg F. Chronic fatigue syndrome, fibromyalgia, and related illnesses: a clinical model of assessment and intervention. Journal of Clinical Psychology. 2010;66(6):641–665. [DOI] [PubMed] [Google Scholar]
- 13.Friedberg F, Adamowicz JL, Bruckenthal P, Milazzo M, Ramjan S, Quintana D. Non-improvement in chronic fatigue syndrome: relation to activity patterns, uplifts and hassles, and autonomic dysfunction. Psychosom Med (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kanner AD, Coyne JC, Schaefer C, Lazarus RS. Comparison of two modes of stress measurement: Daily hassles and uplifts versus major life events. Journal of Behavioral Medicine. 1981;4(1):1–39. [DOI] [PubMed] [Google Scholar]
- 15.Totenhagen CJ, Serido J, Curran MA, Butler EA. Daily hassles and uplifts: A diary study on understanding relationship quality. Journal of Family Psychology. 2012;26(5):719. [DOI] [PubMed] [Google Scholar]
- 16.Adamowicz JL, Caikauskaite I, Friedberg F. Defining recovery in chronic fatigue syndrome: a critical review. Quality of Life Research. 2014;23(9):2407–2416. [DOI] [PubMed] [Google Scholar]
- 17.Cairns R, Hotopf M. A systematic review describing the prognosis of chronic fatigue syndrome. Occup Med (Lond). 2005;55(1):20–31. [DOI] [PubMed] [Google Scholar]
- 18.Price JR, Mitchell E, Tidy E, Hunot V. Cognitive behaviour therapy for chronic fatigue syndrome in adults. Cochrane Database Syst Rev. 2008(3):Cd001027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Krupp LB, LaRocca NG, Muir-Nash J, Steinberg AD, The fatigue severity scale. Application to patients with multiple sclerosis and systemic lupus erythematosus. Arch Neurol. 1989;46(10):1121–1123. [DOI] [PubMed] [Google Scholar]
- 20.Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473–83. [PubMed] [Google Scholar]
- 21.Sletten DM, Suarez GA, Low PA, Mandrekar J, Singer W. COMPASS 31: a refined and abbreviated Composite Autonomic Symptom Score. Mayo Clin Proc. 2012;87(12):1196–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fukuda K, Straus SE, Hickie I, Sharpe MC, Dobbins JG, Komaroff A. The chronic fatigue syndrome: a comprehensive approach to its definition and study. Annals of Internal Medicine. 1994;121(12):953–959. [DOI] [PubMed] [Google Scholar]
- 23.Friedberg F, Sohl S. Cognitive-behavior therapy in chronic fatigue syndrome: is improvement related to increased physical activity? Journal of Clinical Psychology. 2009;65(4):423–442. [DOI] [PubMed] [Google Scholar]
- 24.Friedberg F, Adamowicz JL, Caikauskaite I, Seva V, Napoli A. Efficacy of two delivery modes of behavioral self-management in severe chronic fatigue syndrome. Fatigue: Biomedicine, Health & Behavior. 2016;4(3):158–174. [Google Scholar]
- 25.Dancey CP, Whitehouse A, Painter J, Backhouse S. The relationship between hassles, uplifts and irritable bowel syndrome: a preliminary study. Journal of Psychosomatic Research. 1995;39(7):827–832. [DOI] [PubMed] [Google Scholar]
- 26.Farrar JT, Young JP, LaMoreaux L, Werth JL, Poole MR. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94(2):149–158. [DOI] [PubMed] [Google Scholar]
- 27.Geisser ME, Clauw DJ, Strand V, Gendreau MR, Palmer R, Williams DA. Contributions of change in clinical status parameters to Patient Global Impression of Change (PGIC) scores among persons with fibromyalgia treated with milnacipran. Pain; 2010;149(2):373–378. [DOI] [PubMed] [Google Scholar]
- 28.Arroll MA, Senior V. Individuals’ experience of chronic fatigue syndrome/myalgic encephalomyelitis: An interpretative phenomenological analysis. Psychology and Health. 2008;23(4):443–458. [DOI] [PubMed] [Google Scholar]
- 29.Stormorken E, Jason LA, Kirkevold M. Fatigue in adults with post-infectious fatigue syndrome: a qualitative content analysis. BMC Nursing. 2015;14(1):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Friedberg F, Napoli A, Coronel J, Adamowicz JL, Seva V, Caikauskaite I, Ngan MC, Chang J, Meng H. Chronic fatigue self-management in primary care: a randomized trial. Psychosomatic Medicine. 2013;75(7):650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Friedberg F, Jason L. Chronic fatigue syndrome: An empirical guide to assessment and treatment,Washington, DC: American Psychological Association; (1998). [Google Scholar]
- 32.Williams DA. Psychological and behavioural therapies in fibromyalgia and related syndromes. Best Practice & Research Clinical Rheumatology. 2003;17(4):649–665. [DOI] [PubMed] [Google Scholar]
- 33.Kanter JW, Manos RC, Bowe WM, Baruch DE, Busch AM, Rusch LC. What is behavioral activation? A review of the empirical literature. Clin Psychol Rev. 2010;30(6):608–620. [DOI] [PubMed] [Google Scholar]
- 34.Hayes SC. Acceptance and commitment therapy: towards a unified model of behavior change. World Psychiatry 18(2) (2019) 226–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mazzucchelli TG, Kane RT, Rees CS. Behavioral activation interventions for well-being: A meta-analysis. J Posit Psychol. 2010;5(2):105–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Stenhoff A, Steadman L, Nevitt S, Benson L, White RG. Acceptance and commitment therapy and subjective wellbeing: a systematic review and meta-analyses of randomised controlled trials in adults. Journal of Contextual Behavioral Science. 2010;18:256–272. [Google Scholar]
- 37.Kim DY, Lee JS, Park SY, Kim SJ, Son CG. Systematic review of randomized controlled trials for chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME). Journal of Translational Medicine. 2020;18(1):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author (FF), upon reasonable request.