Abstract
Asthma and chronic rhinosinusitis with nasal polyps (CRSwNP) or without (CRSsNP) are chronic respiratory diseases. These two disorders often co-exist based on common anatomical, immunological, histopathological, and pathophysiological basis. Usually, asthma with comorbid CRSwNP is driven by type 2 (T2) inflammation which predisposes to more severe, often intractable, disease.
In the past two decades, innovative technologies and detection techniques in combination with newly introduced targeted therapies helped shape our understanding of the immunological pathways underlying inflammatory airway diseases and to further identify several distinct clinical and inflammatory subsets to enhance the development of more effective personalized treatments. Presently, a number of targeted biologics has shown clinical efficacy in patients with refractory T2 airway inflammation, including anti-IgE (omalizumab), anti-IL-5 (mepolizumab, reslizumab)/anti-IL5R (benralizumab), anti-IL-4R-α (anti-IL-4/IL-13, dupilumab), and anti-TSLP (tezepelumab). In non-type-2 endotypes, no targeted biologics have consistently shown clinical efficacy so far. Presently, multiple therapeutical targets are being explored including cytokines, membrane molecules and intracellular signalling pathways to further expand current treatment options for severe asthma with and without comorbid CRSwNP. In this review, we discuss existing biologics, those under development and share some views on new horizons.
Keywords: airway remodelling, asthma, biologics, chronic rhinosinusitis, precision medicine, type 2 inflammation
Introduction
Asthma is a chronic respiratory disease, that is often associated with allergy and/or upper airway involvement and/or other conditions outside of the respiratory tract, such as food allergy and atopic dermatitis [1,2]. The hallmarks of asthma comprise chronic airway inflammation, variable airway narrowing and airway hyperresponsiveness (AHR) to specific and nonspecific triggers as well as structural changes within the airways referred to as airway remodelling [1]. Interestingly, such structural changes were detected within the airways of very young children even before the onset of asthma symptoms [3]. Airway inflammation and structural features may be interrelated in some – though not in all – asthma patients [4–6]. Since the underlying inflammation affects the entire respiratory tract (upper, lower, and small airways), it can be sampled both locally (e.g. nasal brushes, lavage, wash; induced sputum; exhaled breath) and systematically (e.g. peripheral blood and urine) [7].
In the past two decades, our knowledge of the multifaceted nature of asthma and the link to chronic rhinosinusitis has vastly increased [8,9]. So far, two major endotypes have been defined in severe asthma: type 2 ((T2)-high) and non-T2 (or type 2 low) [10].
Type 2 (T2) asthma is presently the best defined endotype, which makes up approximately 50–60% of the asthma population [11,12]. While the majority of patients with T2 asthma usually respond to corticosteroid therapy, a proportion (up to 10%) remains uncontrolled due to unresponsive mechanisms driving their severe asthma [1,13,14]. Targeting these underlying pathways with selective biologics further uncovered the complexity and heterogeneity of severe asthma [15–18]. In parallel, clinically applicable biomarkers (and combinations) helped to identify responders to targeted biologics [19–21]. According to several reports, a substantial proportion of these patients has comorbid chronic rhinosinusitis with nasal polyps (CRSwNP) arising from joint underlying mechanisms [22]. These patients have less favourable disease outcomes, are more difficult to control and are at risk of frequent exacerbations with accelerated lung function decline [23,24]. Although less well-defined in children, the prevalence of severe asthma shows a substantial geographical variability and accounts for approximately 5% of childhood asthma cases. In addition, it is usually characterized by T2 (allergic) inflammation [25].
The definition of non-T2 asthma seems more complex than the one of T2-asthma given the vast heterogeneity of its underlying mechanisms, varying from predominant inflammatory pathways (e.g. airway neutrophilia in the absence of respiratory infections) to the lack of eosinophilic or other inflammation (as in paucigranulocytic asthma), or predominant airway smooth muscle (ASM) dysfunction (characterised by fixed airway narrowing and severe AHR) [6,25]. Pathways and biomarkers underlying non-T2 asthma need further elucidation to allow identification of therapeutic targets, biomarkers and effective targeted treatment options.
In this review, we provide an overview of existing and emerging treatment options for asthma and comorbid CRSwNP, targeting the underlying inflammatory pathways, and discuss our current knowledge and future perspectives.
Inflammatory pathways and mechanisms underlying asthma and chronic rhinosinusitis
Asthma and chronic rhinosinusitis (CRS) represent frequently occurring, often coexisting diseases, located at the ultimate ends of the respiratory tract and interrelated through joint underlying mechanisms which respond to targeted biologics [16]. Both conditions are highly heterogeneous with a vast interplay among external triggers, microbiome, structural, and inflammatory cells as well as mediator networks contributing to their pathophysiology and clinical presentation [15,26–29].
In the late 1940s, asthma was already identified as a heterogeneous condition and since then a plethora of studies has added accumulating evidence on the stratification of asthmatic patients into different clinical phenotypes and later on, based on the predominant inflammatory sputum cell profile, into inflammatory phenotypes [30].
In the 2000s, asthma was further subcategorised into two major endotypes: Th2 and non-Th2 asthma, based on the presence or absence of (i) CD4+ T-helper cell type 2 (Th2)-driven inflammatory responses (IL-4-, IL-5-, and IL-13-mediated), or Th17-driven responses (IL-17, IL-1β, IL-23), (ii) IgE, and (iii) increased levels of eosinophils, neutrophils, basophils, and mast cells in the airways [11]. More recently, the identification of type 2 innate lymphoid cells (ILC2s) with subsequent studies demonstrating their significant contribution to the pool of hallmark type 2 cytokines, resulted in an update of this terminology to type 2 (T2) and non-type 2 (non-T2) (also known as T2-high or T2-low) asthma, respectively [31].
T2 asthma
In T2 asthma, the presence of copious amounts of type 2 cytokines at mucosal sites, as well as intrinsic down-regulation of the expression of claudin-18 and E-cadherins, are linked to the reduced structural integrity of the airway epithelium and the enhanced permeability and responsiveness of the epithelial barrier to exogenous triggers [32–34]. Consequently, airway epithelium in patients with T2 asthma overproduces a broad pallet of pro-inflammatory cytokines and mediators including alarmins (IL-25, IL-33, TSLP), as well as IL-6, IL-8, IL-1α/β, RANTES, or TNF in response to environmental triggers. These mediators create a local pro-inflammatory microenvironment that promotes activation, recruitment and function of other immune cells already residing in the local tissue or upon recruitment from the circulation (Figure 1) [35–37]. Examples of cells activated by epithelium-derived cytokines are dendritic cells (DCs) and ILC2s, which further promote the polarization towards the type 2 immunity by activating T-cells and consequently B-cells. Molecular pathophysiology of T2 asthma is fuelled by activated GATA-3+ CRTH2+ ILC2s as well as Th2 cells that produce substantial amounts of the hallmark type 2 cytokines: IL-4, IL-5, and IL-13. Increased numbers of conventional ILC2s in peripheral blood were found in patients with severe asthma and correlated with disease severity [38]. These ILC2s are likely recruited to the lungs, as increased expression of lung homing receptors was found in blood ILC2s of asthmatic individuals [39,40]. Indeed, a significant increase of IL-5+, IL-13+, and CRTH2+ ILC2s was demonstrated in the sputum of asthmatic patients, 24-48 hours post-allergen challenge coincided with a decrease in blood ILC2s [41]. In line with these findings, PGD2 pathway was found to be up-regulated and correlated to high levels of type 2 inflammatory products in patients with severe uncontrolled T2 asthma [42]. Recently, a novel ILC2 subtype expressing CD45RO was identified in the blood of patients with severe and uncontrolled T2 asthma. CD45RO+ ILC2s are derived from resting CD45RA+ ILC2s upon activation by epithelial alarmins IL-33 and TSLP. Importantly, CD45RO+ ILC2 and their signature cytokines IL-5 and lL-13 were increased in inflamed mucosal tissues and in the circulation of patients suffering from chronic inflammatory diseases mediated by T2 inflammation, including CRSwNP and (late-onset) severe eosinophilic asthma [43,44]. Compared with conventional CD45RA+ ILC2s, these CD45RO+ ILC2s display an unclarified corticosteroid resistance [40,45]. A large body of evidence shows that the impaired activity, expression, and translocation of glucocorticosteroid receptor (GR) alpha plays a significant role in mediating the defective signalling of steroid pathways resulting in corticosteroid resistance. Studies have shown that increased concentrations of type 2 cytokines in the local airway tissues affect GRα translocation and promote corticosteroid resistance, while other studies postulated the defective interaction between GR and transcription factors from the NF-κB and AP-1 families to play a critical role in corticosteroid signalling [46–49]. However, the cause behind the corticosteroid resistance within the already heterogenic population of asthma probably varies between individuals, which constitutes an urgent need for a more personalized medicine approach when treating individual asthma patients.
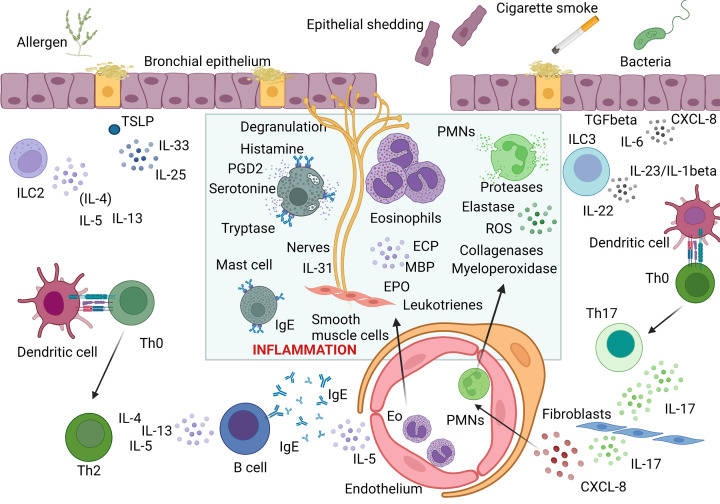
Figure 1. Cellular and cytokine interactions involved in allergic (Type 2) and non-allergic (non-Type 2) asthma.
Type 2 immune response is initiated when inhaled allergens trigger epithelial release of thymic stromal lymphopoietin (TSLP), IL-33 and IL-25 which induce type 2 responses via activation of type 2 innate lymphoid cells (ILC2), as well as activation and differentiation of Th2 cells. In this pathway, IL-4 and IL-13 regulate isotype switching in B cells to IgE production while IL-5 regulates eosinophil recruitment and activation. Effector phase of Type 2 immune response is dependent on allergen crosslinking of specific IgE on mast cells and basophils leading to their degranulation and release of histamine, serotonin and other mediators and proinflammatory cytokines. Furthermore, activated eosinophils recruited to the site of allergic inflammation release eosinophilic cationic protein (ECP), major basic protein (MBP) or eosinophilic peroxidase. The mixture of inflammatory mediators and cytokines including IL-4, IL-13, and IL-31 directly affect epithelial cells and induce their shedding, stimulate mucus overproduction, oedema, and bronchoconstriction. In non-type 2 immune response, environmental stimuli including cigarette smoke and microbes lead to a release of neutrophilic chemokine CXCL8, either directly from epithelial cells or fibroblasts via ILC3-mediated IL-17 pathway controlled by epithelial IL-6 and TGF beta. Recruited activated neutrophils release reactive oxygen species (ROS), myeloperoxidase, proteases, elastases and collagenases leading to epithelial cell damage and mucus hyperproduction. Created with BioRender Sofware (Ref.n.WV25BY7AMN).
In contrast with T2 eosinophilic non-atopic asthma which usually manifests at a later age (late-onset), the allergic subset of T2 asthma usually presents at a young age (early-onset). This subtype is characterized by positive allergy skin tests, increased serum total and specific IgE and clinical symptoms upon allergen exposure. Notwithstanding, little is known about the precise roles of cells from the innate and adaptive immune compartments specifically in early-onset allergic asthma as compared with other subsets of T2 non-atopic asthma [50]. In allergic asthma, allergen-specific CD4+ Th2 cells drive inflammatory responses. A differentiation of allergen-specific Th2 cells from naive T cells occurs in draining lymph nodes and is followed by migration to the respiratory tract, most likely through the expression of homing markers, including CCR4 [51–53]. IL-2 signalling was shown to be required for lung homing and retention of long-lived allergen-specific memory Th2 [54]. Adding to the complexity of asthma endotypes, some patients may show both Th17 and T2-mediated airway inflammation, with Th2/ILC2 and Th17/ILC3 profiles and their signature cytokines [55]. Variations in T-cell subtypes in distinct asthma phenotypes including distinct T2 cytokine profiles were demonstrated. In severe asthma, IL-4+/IL-17+ T-cells in BALF expressed higher IL-4 levels compared with IL-4+ T cells. Single-positive IL-4+ T-cells were more frequent in less severe asthma indicating a pathogenic role for IL-4 high cells [56].
Eosinophils, due to their pleiotropic effect on various cell types, are perhaps the most recognized cells in the pathophysiology of T2 asthma. Eosinophils are found at inflamed mucosal sites and upon activation they are capable of producing and releasing numerous pro-inflammatory mediators, including IL-5, IL-13, eotaxins, cysteinyl leukotrienes (CysLTs; including LTC4, LTD4, and LTE4), major basic protein (MBP), eosinophil peroxidase (EPX), eosinophil cationic protein (ECP), and eosinophil-derived neurotoxin (EDN) [57]. Eosinophils significantly contribute to airway tissue remodelling by producing pro-fibrotic factors and consequently activating bronchial fibroblasts [58]. Furthermore, CRSwNP-derived eosinophils enhance IL-5 and IL-13 production by ILC2s, while eosinophil-derived LTD4 was shown to activate naïve ILC2s towards IL-4 secretion [59,60]. In T2 asthma, basophils are recruited to the airway tissues and bronchial walls likely due to increased concentrations of local inflammatory mediators. Activated basophils, as well as mast cells, produce histamine and lipid mediators, prostaglandin D2 (PGD2) and CysLTs [61]. Building on the notion of ILC2 activation by effector cells, one study demonstrated that basophils secreted IL-4 that directly modulated ILC2 towards increased IL-5 production in T2 pathologies [62]. In contrast, a more recent study demonstrated that basophils primed ILC2s to respond to neuron-derived signals necessary to maintain tissue integrity and in this context a dual function of basophils as potent inhibitors of type 2 inflammation was proposed [63].
In children, the eosinophilic phenotype is commonly present which is associated with early-onset disease with atopy, impaired lung function and increased airway hyperresponsiveness [64].
Non-T2 asthma
Non-T2 asthma (also known as type 2-low-, or non-eosinophilic asthma) is a heterogeneous condition which may comprise several underlying mechanisms including the influx of CD4+ type 1 T helper (Th1) and type 17 T helper (Th17) cells, type 1 and type 3 innate lymphoid cells (ILC1 and ILC3 respectively), neutrophils as well as increased levels of pro-inflammatory mediators in the lung tissues, among others including IL-1ß, IL-6, IL-8, IL-17A/F, IL-22, IFN-γ, and TNF-α. Studies point out that an imbalance in Th17/Treg cells may play a role in corticosteroid-resistant neutrophilic asthma [50,65]. In addition to the dysbalanced immune cell makeup, the pathophysiology of non-T2 asthma may also be mediated by structural abnormalities of the ASM and dysregulated neuronal activation [43,45]. Non-T2 asthma is further subclassified into neutrophilic and paucigranulocytic, depending on the cellular findings in sputum specimens [19,25]. In contrast with T2 asthma, non-T2 is less well defined and largely lacks clinically applicable biomarkers while biologics targeting the presumed underlying mechanisms did not show clinical efficacy so far.
Chronic rhinosinusitis
CRS is a common chronic inflammatory disorder of the upper airways with an estimated prevalence of approximately 10–15% in the general adult population [66,67]. CRS has a multifactorial aetiology involving several precipitating factors (genetic and environmental) interacting with the upper airway epithelial barrier to trigger inflammatory pathways [68]. Being a frequently occurring comorbid condition in lower airway disorders such as bronchiectasis [69] and asthma (prevalence increasing with asthma severity), physicians are advised to proactively assess both the upper and lower airways in patients as CRS has been associated with worse disease outcome [1,70,71].
Based on endoscopic or imaging findings, CRS comprises two major clinical phenotypes, i.e., with (CRSwNP) or without (CRSsNP) nasal polyps (NP); the latter being approximately twice as prevalent. Although less prevalent, CRSwNP is the most cumbersome phenotype which often coexists in patients with more severe asthma [22,72,73]. Indeed, increasing evidence shows close links at different levels between CRSwNP and asthma, specifically: both conditions are linked through the underlying T2 inflammation, which underscores the united airways concept in this disease subset [72].
An additional clinical subset of CRSwNP and late-onset T2 asthma includes aspirin-exacerbated respiratory disease (AERD) or nonsteroidal anti-inflammatory drugs (NSAIDs) exacerbated respiratory disease (NSAID-ERD). As part of the previously termed ‘Samter's triad’, patients with AERD/NSAID-ERD present with asthma and concomitant CRSwNP with often intractable disease [72,74,75]. The T2-driven pathophysiological mechanism underlying AERD/NSAID-ERD is related to dysregulated arachidonic acid (AA) metabolism and cysteinyl leukotrienes (CysLTs) overproduction [76].
Apart from the aforementioned ‘traditional’ classification, CRS phenotypes are highly heterogeneous and show a substantial geographical with racial variability across inflammatory profiles. For example, in Caucasian populations, CRSwNP most frequently presents with a type 2 inflammatory (eosinophilic) profile, while in Asian populations mixed inflammatory profiles in both CRS clinical phenotypes have been found [72,77]. This aspect should also be taken into consideration in clinical assessment and subsequent treatment plan [78,79].
Based on increased levels of inflammatory proteins and cytokine profiles, CRS (with and without NP) comprises three different endotypes, i.e., T1 characterised by type1 cytokines IFN-γ and TGF-β, T2 by type2 proteins and cytokines IgE and IL-4, IL-5, and IL-13, and T3 by Th17 cytokine IL-17A [77,80,81].
In T2 CRSwNP, eosinophils usually make up the predominant inflammatory cells [82], while ILC2s, B-cells, macrophages, dendritic cells, mast cells and basophils have also been found [28]. Patients with this CRS subtype, may also present with increased levels of FeNO and normal or elevated serum total IgE [83]. However, recent data also point towards the involvement of neutrophils in this subtype [29]. Furthermore, in several studies of CRSsNP, both eosinophils and neutrophils have been demonstrated in upper airway samplings [77].
While NP are commonly found in adults, they are rare in children under the age of 10 years. Furthermore, the presence of NP in children usually indicates underlying systemic diseases, such as cystic fibrosis, primary ciliary dyskinesia or immunodeficiencies. The association with asthma and other allergic/eosinophilic comorbidities is not as clearly expressed in children [84].
Airway remodelling in asthma and CRS
Structural changes including epithelial abnormalities, subepithelial matrix deposition, ASM cell alterations and mucus hyperproduction contribute to airway remodelling in asthma resulting in small airways disease, non-specific AHR and accelerated lung function decline leading to fixed airflow obstruction [85]. Recent advances in cell biology allowed deeper understanding of the role of diverse non-immune cells contributing to the pathophysiological features of asthma such as AHR [86–88]. Recent data show structural airway changes such as increase in ASM mass and MUC5AC expression in both T2 and non-T2 severe asthma while submucosal glands hyperplasia is associated with T2 intermediate and T2-low asthma [89]. These insights should further move the identification of novel targets for asthma treatment [90,91].
Airway epithelial cells are capable of producing large amounts of cytokines, antimicrobial peptides and multiple proteases, and thus, contribute to the creation of a physical barrier restraining both pathogens and allergens [92,93]. Airway epithelial cells share similar features with innate immune cells, such as the expression of pattern recognition receptors (PRRs) and the secretion of cytokines/chemokines, including IL-6, IL-8, IL-25, IL-33 and CCL20, CCL17 [92,94].
Under specific conditions, such as allergen-mediated epithelial damage, airway epithelial cells lose their protective function, become highly pro-inflammatory and, by promoting airway remodelling, they become crucial players in asthma pathophysiology [95]. Epithelial damage is also characterized by a functional impairment of intercellular junctions caused by the disruption of junctional proteins [92,96]. This phenomenon further increases epithelial permeability and has been demonstrated in all asthma phenotypes [92] as well as in CRSwNP [97]. While DCs mainly impact the differentiation of Th cells into Th1 phenotype, epithelial cells also activate ILC2s and fibroblasts, thus promoting type 2 inflammation and remodelling [98,99]. Eventually, a large proportion of epithelial cells differentiate into mucus-secreting goblet cells [100].
Furthermore, IL-4 and IL-13 released from ILC2s and Th2 cells directly stimulate airway epithelial cells and induce mucus overproduction [101,102]. Dynamic interactions between the innate and adaptive immune cells dictate the polarization of the T-cell immune response [103]. PRRs located on the epithelial cells recognize allergens/infectious antigens and secrete both chemokines and cytokines [104]. As DCs receive cytokine signals from the airway epithelium, the fate of the immune response is decided. Indeed, epithelial cells largely control the differentiation of local DCs [92].
DCs act as antigen presenting cells (APCs) but their actions can vary according to their phenotype [105]. Myeloid and plasmacytoid DCs are the two major phenotypes in human lungs, characterized by either CD11c+/hi, BDCA1+ (CD1c)/BDCA3+ (CD141), and HLA-DR+ for mDCs, or BDCA2CD123+ (IL-3 receptor), CD11c−+ (CD303), BDCA4+ (CD304), HLA-DR+, and ILT7 for pDCs [106]. Antigens are primarily recognized by PRRs of the epithelium and the type of antigenic exposure drives the spectrum of produced cytokine/chemokines, the attraction of DCs and the generation of T-cell subtypes [106,107]. The generally accepted hygiene hypothesis highlights the importance of bacterial stimulation in early childhood, which primes the DCs to induce Th1 polarization and, thus protection against allergies [108]. Different types of allergens, but also non-allergenic proteins, can be discriminated based on diverse surface patterns, such as glycosylation [109]. Other allergens, such as various pollens, may release pollen-associated lipid mediators (PALMs) to trigger the immune response [110]. Glycosylation is essential for recognition by lung epithelial cells and DCs [109]. The most common glycosylation pattern among allergens is mannosylation [85]. While certain antigens are highly immunogenic, some factors were also demonstrated to drive DCs towards tolerogenic phenotype [106,107]. Among these factors, smoking has been shown to alter the functionality of DCs [106].
Another crucial component of airway remodelling represents ASM abnormalities (hypertrophy and hyperplasia) [111]. Structural changes in the ASM cells result in an imbalance between the contractility and relaxation of ASM and subsequently lead to (fixed) airway narrowing and AHR to various stimuli [112]. The increase in the ASM layer is clearly connected to a decreased lung function in asthma. ASM cells are also capable of secreting chemokines, such as CCL11, CXCL10, and CX3CL1, promoting recruitment of mast cells [113]. The release of contractile mediators by mast cells is thought to be particularly responsible for the impairment of ASM contraction [112]. Adhesive and costimulatory molecules expressed on ASM cells further allow interactions with T cells. Several studies showed the capability of ASM cells to migrate within the airway wall [114].
Lung function is also regulated by a network of afferent and efferent nerves [115]. Airway nerves mediate reflexes, as well as ASM contraction [116]. Most airway afferent nerves are unmyelinated C-fibers, however, other fibre types can be activated in the presence of chemical or mechanical factors [116,117]. Efferent fibers consist of parasympathetic, sympathetic, and non-adrenergic non-cholinergic (NANC) nerves regulating different aspects of ASM tone and bronchoconstriction [116,117]. In asthma, both bronchoconstriction and AHR were previously associated with neuronal activity [118]. Therefore, anticholinergics efficiently serve as modulators of the increased cholinergic tone in the airways [119]. Similarly to changes in DC phenotype, also the neuronal activity in asthma may change due to plasticity and remodelling of airway nerves [117]. Neurotrophins are factors that broadly influence the neuronal plasticity and are released by various cell types in the airways, such as neurons, epithelial cells, ASM cells and leukocytes [116]. Neurotrophin expression was shown to be significantly increased in asthma and thus, novel therapeutics have been designed to target the neuronal plasticity [116].
Dysregulation of the DC-epithelium interactions also represents a crucial aspect in CRSwNP pathophysiology [120]. In CRSwNP, defective epithelial barrier leads to increased tissue permeability and cellular damage which promotes chronic (type 2)-inflammation and remodelling [120,121].
Until recently, no truly disease-modifying therapies existed for asthma and/or CRSwNP. However, in terms of airway remodelling, a study including mild asthmatics receiving only SABA showed that three infusions with anti- IL-5 monoclonal antibody mepolizumab reduced the expression of extracellular matrix proteins (tenascin, lumican, and procollagen III) in the bronchial basement membrane. It also reduced TGF-β1 level in BAL fluid and TGF-β1 mRNA expression in eosinophils [122]. Early interventions with (biologic) treatments targeting (and affecting) components of airway remodelling may change this perspective in the future [123]. Obviously, long-term studies with adequate disease outcomes should provide the answer.
The role of microbiome
Several triggers and external factors (e.g., stress, age, lifestyle, diet, body composition, and medications) can directly or indirectly interfere with our immune system. In this complex interplay, it has become evident that the microbiome plays an important regulatory or even ‘disease driving or modulating’ role [124]. For instance, nutritional products, supplements and medications can alter the composition of the microbiome and thus indirectly affect the immune system [125]. Coinciding with a decreased diversity of beneficial commensals and prevailing pathogens (gut microbial dysbiosis) and a decline in immunity later in life, a potential link with late-onset asthma has been suggested [126]. More recently, other associations between (environmental and endogenous) microbiota and asthma phenotypes have been suggested [127,128].
An increasing number of studies support the existence of the gut-lung axis and the role of gut microbiome alteration in the pathogenesis of chronic inflammatory diseases including asthma and COPD. Only recently, this association has been underscored by data from a large prospective population-based study (FINRISK02; n = 7115 adults; follow-up over 15 years) using metagenomic sequencing of stool samples [129]. Particularly, the abundance of Escherichia, Enterococcus, Clostridium, Veillonella, and Bacteroides fragilis was found to be associated with a higher incidence of asthma over time [129]. In another study, gut abundance of Clostridium sp. during the first 3 months of life was found to be related to preschool-onset of asthma [130]. Lipopolysaccharide (LPS), an endotoxin originating from the cell wall of Gram-negative bacteria present in the airways and gut of asthmatics, may be responsible for NF-κB dependent inflammation leading to asthma [131]. Also patients with allergic rhinitis display a reduced gut microbial diversity with lower a Firmicutes to Bacteroidetes ratio as compared with healthy controls [132,133]. In CRS, both microbial dysbiosis and Staphylococcus aureus colonization may contribute to its pathogenesis [128] while the latter also associates with the occurrence of concomitant asthma [134]. The nasal bacteriome of patients with allergic rhinitis with and without asthma assessed by 16S rRNA high-throughput sequencing was found to be both compositionally and structurally distinct from healthy controls and to differ in metabolic pathways mainly related to degradation and biosynthesis processes [135].
Therapeutic approaches targeting gut microbiome, e.g., with pre- or probiotics or faecal microbial transplantation (FMT) may be beneficial components of asthma management and several studies with tailored approaches are currently ongoing in different patient populations [131]. In this respect, a probiotic preparation was found to increase microbiome diversity in patients with allergic rhinitis with or without concomitant asthma and to decrease their rhinitis symptom score, improved quality of life, reduced the percentage of blood activated eosinophils and basophils and the serum levels of IL-4 and IL-5 [136].
The role of the microbiome in health and disease as well as the effects of new and existing therapeutic modalities, including the long-term application of corticosteroids and biologics, on the composition of the microbiome in the context of disease control and remission is a new area of exploration with the potential to further shape personalized medicine.
Biomarkers in asthma and CRSwNP
Clinically applicable biomarkers help clinicians to define inflammatory asthma phenotypes and to identify responders to (biologic) treatments [14,137]. Similarly with the one airway concept reflected in asthma and allergic rhinitis, asthma with concomitant CRSwNP also share similar underlying pathways, most often type 2 eosinophilic inflammation [128] although geographical differences in underlying mechanisms exist [138]. Increased eosinophil numbers can almost always be detected in the circulation or in the airway tissues of these patients, yet they are not the key effector cells in all patients. Apart from blood eosinophils, exhaled FeNO and (to a lesser degree) serum periostin levels also serve as surrogate markers of type 2 inflammation, which is being applied to phenotype/endotype both asthma and CRSwNP patients (Table 1).
Table 1. Biomarkers in asthma.
| Biomarker | Characteristics |
|---|---|
| T2 asthma biomarkers | |
| Sputum eosinophils (≥3%) | ● Semi-invasive method, available in specialized centers ● Indicative of more intense eosinophilic airway inflammation, poor adherence to inhaled corticosteroids (ICS), poor asthma control and more frequent exacerbations [140,141] ● Highest at night – lowest at midday [142] ● Sputum eosinophil‐guided management of severe asthma leads to a substantial reduction in exacerbations [143] ● Better biomarker in patients on OCS compared with blood eosinophils [144,145] |
| Blood eosinophils (>150 or >300 cells/μl) | ● Significant circadian variations during the day (highest at night, lowest at midday) + intrapersonal fluctuations [142] ● Affected by parasitic infections and systemic corticosteroids [7,46,146] ● ≥ 300 cells/μl associated with eosinophilic inflammation and more frequent exacerbations [147,148] |
| Fractioned exhaled nitric oxide (FeNO) | ● Easily measurable and reproducible point-of-care biomarker [149,150] ● Does not correlate with sputum eosinophils [151] ● Influenced by ICS use, smoking, atopy, dietary nitrate intake and viral infection [149,152] value >50 ppb in adults often reflects eosinophilic inflammation [151] |
| Exhaled volatile organic compounds (VOCs) | ● Composite biomarker not yet validated for clinical practice ● Influenced by medication, microbiome [153,154] |
| Total serum IgE | ● Not accurate in atopic and obese patients [155] ● Currently only used for the calculation of omalizumab dose |
| Serum periostin | ● Promotes adhesion and migration of epithelial cells, mucus production, eosinophil infiltration and subepithelial fibrosis thus driving airway remodelling [156,157] ● Correlates with blood eosinophils, serum total IgE, eosinophil cationic protein (ECP), and transforming growth factor-β (TGF-β1) [158] ● Superior in predicting fixed airflow obstruction [159] |
| Dipeptidyl peptidase‐4 (DPP‐4) | ● Biomarker for predicting the response to anti–IL‐13 treatment [160] |
| Prostaglandin D2 | ● Derived from the arachidonic acid metabolism [161] ● Biomarker of AERD/NSAID-ERD [161] |
| Eosinophil cationic protein (ECP) | ● Increased during asthma exacerbations [162] ● Reduced after treatment [162] ● May be used as a marker for corticosteroid induction [162] |
| Eosinophil derived neurotoxin (EDN) | ● High in severe and uncontrolled asthma, especially with persistent airflow limitation [162,163,166] ● Higher serum levels detected at the exacerbation rather than the stable phase of asthma [162,164] ● Promotes the production of matrix metalloproteinase 9 (MMP-9) thus plays a role in airway inflammation as well as in airway remodelling [165] |
| Urinary leukotriene E4 (LTE4) | ● The most reliable biomarker for the diagnosis of NSAID-ERD– NSAID-ERD is associated with chronic rhinosinusitis (CRS) with or without nasal polyps [167–169] ● Increased urinary levels were correlated with lung function decline in T2 severe asthma [167] ● uLTE4 is helpful in order to better endotype patients with CRS and to predict disease severity [170] |
| Bromotyrosine | ● Urine biomarker ● May predict exacerbations despite the lack of correlation with other more commonly used biomarkers, such as FeNO and sputum eosinophils [173] |
| Non-T2 asthma biomarkers | |
| Sputum neutrophilia | ● In the absence of airway infection, indicates a distinct inflammatory phenotype, i.e., neutrophilic asthma. ● Sputum neutrophil counts correlate with the gene expression of sputum IL‐17A and IL‐8 [2] ● Neutrophil extracellular traps (NETs) down-regulate the expression of the tight junction protein of epithelial cells, thus leading to the damage of epithelial cells together with eosinophil degranulation [171] |
| Serum calprotectin | ● Correlates with increased sputum neutrophils [172] |
| S100A9 (calcium-binding protein A9, calgranulin B) | ● Significantly higher in patients with neutrophilic asthma [173] |
| Serum IL‐17 | ● Increased in severe compared to milder asthma [174] |
| Soluble TNF and IL‐8 | ● Increased levels during asthma Exacerbations [175] ● Increased serum levels have been found in severe asthma compared with healthy subjects [174] ● Associated with elevated peripheral blood neutrophils [176] |
| NLRP3 and IL‐1β | ● Increased in neutrophilic asthma [177,178] |
| Serum chitinase-3-like protein 1 (CHI3L1) and YKL40 | ● Both correlate with sputum neutrophils, myeloperoxidase, Il-8, And Il-6 ● Both induce subepithelial fibrosis [179] ● Considered as potential biomarkers of airway remodeling in neutrophilic asthma [179] |
In a cohort of patients with severe asthma, the sinonasal mucosal thickness was correlated with levels of systemic (blood eosinophils) and lower airways (sputum eosinophils, FeNO) type 2 biomarkers, indicative of more severe disease [139]. There is now a substantial body of evidence demonstrating that patients with more prominent underlying inflammation usually show a better clinical response to treatment with T2-targeted biologics (Table 1; Table 2) [7,50,140–179].
Targeted therapy of asthma with or without CRS
Presently, several T2-biologic treatment options exist, blocking the following targets: IgE, IL-5 and IL-5R, IL-4R, and TSLP. A short outline per biologic is provided underneath including the mechanism of action and clinical effectiveness (Table 2, Figure2).
Table 2. Targeting immune mechanisms and therapeutic options in T2 and non-T2 inflammation.
| Target | Approach | Name | Company | Patients | Status/clinical phase | |
|---|---|---|---|---|---|---|
| IgE | IgE (Cε3 domain-site involved in binding to FcRI) | Humanized IgG1 MoAb | Omalizumab | Novartis | Asthma Urticaria CRSwNP |
Approved |
| IgE (Cε3 domain) | Humanized MoAb | Ligelizumab | Novartis | Asthma Urticaria |
3 | |
| IgE (M1 segment) | Humanized MoAb | Quilizumab | Genentech | Asthma | 2 | |
| IgE (Cε3 domain) | Humanized MoAb | MEDI4212 | MedImmune LLC | Asthma | 1 | |
| CεmX domain of membrane-bound IgE | Humanized MoAb | FB825 | Oneness Biotech Co | Asthma | 2 | |
| IL-4/IL-13 | IL4Ra (subunit common to IL-4 and IL-13 receptors | Human MoAb | Dupilumab | Regeneron/Sanofi | atopic dermatitis asthma CRSwNP EoE |
Approved |
| IL-4+IL-13 receptors | Recombinant IL-4 variant | Pitrakinra | Aerovance | Atopic dermatitis asthma |
2 | |
| IL-4+IL-13 | 2 MoAbs (VAK694+dectrecumab) | QBX258 | Novartis | Asthma | 2 | |
| IL-4R | Suman IgG2 MoAb | AMG317 | Amgen | Asthma | 2 | |
| IL-4 | Humanized MoAb | Pascolizumab | GSK | Asthma | 3 | |
| IL-4 | Human MoAb | VAK694 | Novartis | Asthma, pollinosis | 2 | |
| IL-4 | Soluble recombinant IL-4R | Altrakincept | Amgen | Asthma | Terminated | |
| IL-13 | Humanized MoAb | Lebrikizumab | Lilly | Atopic dermatitis | 3 | |
| IL-13 | Human MoAb | Tralokinumab | LeoPharma | Atopic dermatitis | Approved | |
| IL-13 | Humanized MoAb | Anrukinzumab | Wyeth | Asthma | 2 | |
| IL-13 | Humanized MoAb | GSK679586 | GSK | Asthma | 2 | |
| IL-13 | Human MoAb | dectrecumab (QAX576) | Novartis | Eosinophilic esophagitis | 2 | |
| IL-13 receptor α1 subunit (IL-13Rα1) | Human MoAb | ASLAN 004 | Aslan Pharmaceuticals | Eczema | 1 | |
| IL-5 | IL-5 | Humanized IgG1 MoAb | Mepolizumab | GSK | Asthma, EGPA HES CRSwNP |
Approved |
| IL-5 | Humanized MoAb | Reslizumab | Teva | Asthma | Approved | |
| IL-5Ralpha | Humanized MoAb | Benralizumab | AstraZeneca | Asthma | Approved | |
| IL-5R | Long-acting MoAb | Depemokimab | GSK | Asthma | 3 | |
| Other molecules regulating T2 inflammation | TSLP | Humanized MoAb | Tezepelumab | AstraZeneca/Amgen | Asthma | Approved |
| TSLP | Neutralizing antibody fragment (inhaled form) | CSJ117 | Novartis | Asthma | 2b | |
| TSLP receptor | Human MoAb | ASP7266 | Upstream Bio | Asthma | 1 | |
| IL-33 | MoAb | Tozorakimab/MEDI3506 | AstraZeneca | Asthma | 2 | |
| IL-33 | Human MoAb | Itepekimab | Regeneron/Sanofi | Asthma | 2 | |
| ST2 (IL-33R) | MoAb | Astegolimab | Hoffmann-La Roche | Asthma | 2b | |
| IL-33R | MoAb | Melrilimab (GSK3772847) | GSK | Healthy subjects | 1 | |
| IL-25 | MoAb | ABM125 | Abeome | Asthma | 1/2 | |
| Tryptase tetramers | MoAb | MTPS9579A | Roche/Genetech | Astma | 2a | |
| CRTh2(PGD2 receptor) | Antagonist (small molecule) | Fevipiprant QAW039) | Novartis | Asthma | Terminated | |
| CRTh2(PGD2 receptor) | Antagonist (small molecule) | Setipiprant | Actelion | Asthma | 2 | |
| IL-9 | Humanized MoAb | Enokizumab | AstraZeneca/MedImmune | Asthma | 2 | |
| IL-22 | Human MoAb | Fezakinumab | Rockefeller University | Atopic dermatitis | 2 | |
| IL-31 | Humanized MoAb | Nemolizumab | Galderma | Atopic dermatitis | 3 | |
| CCR3 (eotaxin receptor) | Inhibitor (small molecule) | GW766944 | Glaxo | Asthma | 2 | |
| Singlec 8 | Humanized MoAb | Lirentelimab | Allakos Inc. | Atopic dermatitis Eosinophilic esophagitis and Duodenitis |
2, 3 | |
| Potential targets in non T2 inflammation | IL-17 | Humanized MoAb | Secukinumab | Novartis | Asthma | Terminated, * |
| IL-17RA | Human MoAb | Brodalumab | Amgen | Asthma | Terminated | |
| C5 | Humanized MoAb | Eculizumab | Alexion | Asthma | 2 | |
| CXCR2 | Receptor antagonist (small molecule) | AZD5069 | AstraZeneca | Asthma | 2 | |
| CXCR1/2 | Receptor antagonist (small molecule) | SCH527123 | MSD | Asthma | 2 | |
| IL-6 | Humanized MoAb | Tocilizumab | Roche | Asthma | Small proof‐of‐concept clinical trial, * | |
| IL-1 | rIL-1 receptor antagonist | Anakinra | Sobi | Asthma | 2, * | |
| IL-1 alpha | Human MoAb | Bermekimab | Janssen | Atopic dermatitis | 2b | |
| Reactive aldehyde species (RASP) | RASP inhibitor (small molecule) | ADX-629 | Aldeyra | Asthma | 2 | |
| TNF | TNFR:Fc | Etanercept | Sobi | Asthma | 2, * | |
| TNF | Chimeric MoAb | Infliximab | MSD | Asthma | 2, * | |
| TNF | Human MoAb | Golimumab | Centocor | Asthma | 2, * | |
*Other indications have been previously approved (within rheumatology; inflammatory bowel disease, psoriasis, autoinflammatory diseases, etc.)
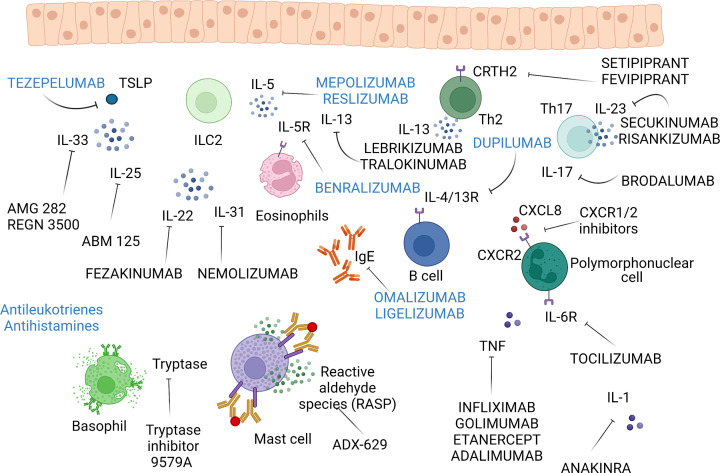
Figure 2. Biologic therapy of bronchial asthma and other allergic disorders.
Most of the current monoclonal antibodies and inhibitors target type 2 inflammation (registered biologics in blue letters). Anti – IgE therapy with omalizumab and ligelizumab is already very effective and safe approach to treat patients with difficult asthma. Similarly, anti-IL-5 monoclonal antibodies, particularly mepolizumab, represent an effective therapy of eosinophilic inflammation. Type 2 inflammation can be downregulated also by dupilumab targeting common subunit shared by IL-4 and IL-13 receptors. Recently, tepelezumab directed against thymic stromal lymphopoietin (TSLP) represents another perspective monoclonal antibody modulating type 2 inflammation with another drugs against alarmins IL-33 and IL-25 in clinical studies. Also the inhibitors of CRTH2 (receptor for PDG2) such as fevipiprant are in clinical studies. In non-type 2 inflammation, no biologics are registered for the therapy of asthma with monoclonal antibodies inhibiting IL-17/IL-23 pathway without sufficient clinical effects, so far. In the effector phases of allergic inflammation, antihistamines and leukotrienes are used for decades with emerging inhibitors of tryptase or reactive aldehyde species (RASP) and monoclonal antibodies blocking pro-inflammatory cytokines IL-6, IL-1 and IL-31 in clinical studies. In the case of anti-TNF therapy, the risk potential adverse effects prevail over benefits in asthma therapy. Finally, chemokine receptor inhibitors may represent another tool to block recruitment of immune cells in allergic inflammation. Created with BioRender Sofware (Ref.n.AB25BY6SZW).
Targeting IgE
Omalizumab, a recombinant humanized anti-IgE monoclonal antibody, was the first biologic drug aimed at uncontrolled severe allergic asthma, which effectively reduced severe asthma exacerbations, improved asthma symptoms and lung function, and decreased the use of inhaled glucocorticosteroids with a long established (almost 20 years), favourable safety profile. It is approved for patients with allergic asthma older than 6 years [180]. In addition to binding free IgE, omalizumab also downregulates high- and low-affinity Fc receptors for IgE (FcεRI and FcεRII - CD23) expressed on membranes of immune cells, particularly mast cells and eosinophils [181]. More recently, omalizumab also showed efficacy in patients with CRSwNP irrespective of allergy – improving both endoscopic, patient reported and clinical outcomes [182].
Based on the success of this approach, new monoclonal antibodies targeting different epitopes on the IgE molecule emerged. Ligelizumab, a high-affinity IgG1kappa humanized anti-IgE monoclonal antibody was shown to be very potent in IgE binding to the FcεRI, but failed to significantly improve asthma control and exacerbation rates in severe asthma, possibly because of its faster clearance as compared to omalizumab [183]. Quilizumab, a humanized afucosalyted IgG1 monoclonal antibody, directed against the M1 prime segment of membrane-expressed IgE (mIgE), down-regulated serum IgE levels without sufficient clinical effects in patients with inadequately controlled asthma [184] or chronic spontaneous urticaria [185]. MEDI4212, a human IgG1 monoclonal antibody, effectively inhibited binding of IgE to FcεRI and decreased IgE serum concentration ex vivo [186]. This antibody was well tolerated and in atopic subjects down-regulated serum IgE levels better than omalizumab; however, this effect appeared transient [187]. A new humanized monoclonal antibody FB825 against CepsilonX domain of the mIgE generated for the depletion of IgE producing B cells is currently evaluated in atopic dermatitis (NCT03758716) and allergic asthma (NCT05008965) without any published data, yet.
Targeting IL-4R (anti-IL4/IL-13)
The relevance of IL-4 and IL-13 in the pathophysiology of asthma has been extensively addressed throughout various studies and reports [188,189]. Both cytokines are involved in IgE production, as well as airway hyperresponsiveness and airway remodelling [188]. The effects of IL-4 and IL-13 are primarily driven by their interactions with immune cells but also by their binding to specific receptors on bronchial fibroblasts, myofibroblasts, and airway smooth muscle cells [190,191]. Both IL-4 and IL-13 activate the α-subunit of the IL-4 receptor (IL-4Rα) and thus, their mechanism of action can be blocked simultaneously through a therapeutic blockade of the IL-4Rα [192]. However, IL-4 also activates a γC subunit of the IL-4 receptor, whereas IL-13 binds to the IL-13 receptor α1 subunit (IL-13Rα1) [192]. Dupilumab is a fully human anti-IL-4Rα monoclonal antibody approved by both the European Medicines Agency (EMA) and the US Food and Drug Administration (FDA) for the treatment of uncontrolled severe asthma [192]. Clinical efficacy of dupilumab has been demonstrated throughout various studies in patients with T2 (moderate to severe) uncontrolled asthma and mainly reflected in the reductions in exacerbation rates, improvement in asthma control and lung function [193–196].
Following a positive phase IIb study [197], a phase 3 clinical trial (Liberty Asthma Quest) evaluating the efficacy and safety of dupilumab in patients with moderate-to-severe asthma, showed a greater treatment response in patients with higher baseline T2 biomarker levels (i.e. blood eosinophils and FeNO), and thus, supports the use of this biologic in patients with a more prominent T2 inflammation. Similarly, in another phase 3 study (Liberty Asthma Venture), dupilumab treatment allowed reductions in OCS use in patients with corticosteroid-dependent severe asthma while improved clinical outcomes as well as FEV1 [198]. In a pooled patient population with severe CRSwNP with comorbid asthma, dupilumab improved both the upper and lower airway outcome measures as well as HRQoL [199] and is currently considered the leading biologic in patients with CRSwNP with or without concomitant asthma. More recently, dupilumab showed clinical efficacy in children (aged 6–11 years) with uncontrolled moderate-to-severe asthma (VOYAGE study), by significantly reducing asthma exacerbation rates and by improving lung function and asthma control [200]. Presently, dupilumab is indicated for the treatment of severe asthma in patients older than 12 years in Europe and for children above 6 years in the US. In children with uncontrolled atopic dermatitis under 6 years, dupilumab improved Eczema Area and Severity Index (EASI-75) and was well tolerated [201]. Recently, dupilumab gained regulatory approval also for the therapy of eosinophilic esophagitis [202].
Another therapeutic agent targeting both IL-4 and IL-13, pitrakinra, a dual IL-4/IL-13 antagonist, reduced asthma exacerbations only in a subgroup of patients with specific gene polymorphisms of IL-4 receptor [203].
Targeted drugs aiming for selective inhibition of IL-13 include lebrikizumab, tralokinumab, anrukinzumab, decrecumab, GSK679586, and ASLAN 004. Out of these agents, only lebrikizumab and tralokinumab have reached phase 3 clinical trials so far. Lebrikizumab, a humanized monoclonal antibody targeting IL-13, was previously shown to improve asthma symptoms particularly in patients with a high serum IgE level, high blood eosinophil counts, and an increased expression of interleukin-13–related genes in the lung [204]. However, in phase 3 clinical trial in patients with uncontrolled T2 asthma, lebrikizumab did not consistently show a significant reduction in asthma exacerbations [205] and hence, further development for asthma has been discontinued. Tralokinumab, a fully human monoclonal antibody neutralizing IL-13 has proven effectiveness in atopic dermatitis, however, a randomized double-blind clinical trial in patients with corticosteroid-dependent asthma failed to demonstrate oral corticosteroid-sparing effects [206] and hence further development for asthma has been discontinued. Furthermore, a study by Panettieri et al. demonstrated inconsistent efficacy of tralokinumab in the treatment of asthma exacerbation frequency, thus, questioning the role of blocking IL-13 alone in managing severe asthma [207].
Among selective IL-4 inhibitors, pascolizumab, AMG-317 and VAK694, were those to reach phase 2 of clinical development. Pascolizumab and VAK694 are monoclonal antibodies neutralizing IL-4 while AMG 317 is an IL-4 receptor antagonist [208]. Although in clinical trials, pascolizumab was shown to be well tolerated, it failed in phase 2 and hence has been discontinued [209]. VAK694 failed to provide additional benefit when added to subcutaneous immunotherapy regardless of the reduction of allergen specific IL-4 producing cells [210]. Similarly, AMG 317 failed to show clinical efficacy in patients with moderate to severe asthma [211] and trials with soluble recombinant IL-4R, altrakincept, used in a nebulized form, were discontinued in phase 1/2 [212].
Targeting IL-5
Targeting IL-5 has become a well-established therapy for patients with uncontrolled severe asthma caused predominantly by T2 inflammation with eosinophilia [213]. Mepolizumab, one of the first approved anti-IL-5 monoclonal antibodies, was shown in large placebo-controlled trials to cause a substantial reduction in exacerbations in addition to steroid sparing effect in steroid dependent eosinophilic asthma [214–216]. Moreover, mepolizumab use was not associated with major side effects and thus, became a standard treatment option for severe eosinophilic asthma [217]. A study by Caminati et al. providing real-life evidence on mepolizumab treatment confirmed its favorable safety profile and most importantly, its corticosteroid-sparing effect in daily clinical practice [218]. So far, mepolizumab is the only licensed anti-IL-5 therapy which has also been approved for children over 6 years old with a dosing schedule of 40 mg every 4 weeks. Adolescents older than 12 years receive the same dose (100 mg) as adults. Mepolizumab also significantly increased the number of weeks in remission in patients with eosinophilic granulomatosis with polyangiitis (EGPA) [219], reduced flare up rates in subjects with hypereosinophilic syndrome (HES) [220] and reduced the risk of sinus surgery in patients with severe CRSwNP [221,222].
Similar to mepolizumab, reslizumab targets IL-5 and blocks the subsequent recruitment and activation of eosinophils. In clinical trials, reslizumab was associated with reduction in exacerbations, improvements in lung function, and quality of life [223,224]. The real-world outcomes associated with reslizumab use in patients with severe eosinophilic asthma were demonstrated by Wechsler et al. [225]. who showed an excellent treatment response, while only 3.3% of the patients were classified as non-responders [225]. In patients with CRSwNP, a single intravenous infusion of reslizumab reduced the size of nasal polyps for 4 weeks in half of the patients with nasal IL-5 levels predicting the response, decreased nasal ECP levels persisted for 12 weeks only in responders [226]. Benralizumab, another currently approved anti-IL-5 agent, is directed against the alpha subunit of the IL-5 receptor [227]. It was associated with a reduction of ASM, myofibroblasts, and airway expression of TGF-β1 [84]. In a study by Kavanagh et al., the real-life evidence on benralizumab treatment in severe eosinophilic asthma showed significant improvements in all clinical outcome measures, such as FEV1, Asthma Control Questionnaire (ACQ6) and Mini-Asthma Quality of Life Questionnaire (mAQLQ) [228] scores. This was particularly relevant in patients with a strongly eosinophilic phenotype that were classified as super-responders [228]. Furthermore, benralizumab showed efficacy in patients with severe CRSwNP by decreasing nasal blockage score in a randomized placebo controlled study [229] Depemokimab, a long-acting anti-IL-5 receptor monoclonal antibody, is currently being evaluated in phase III clinical trials in severe uncontrolled asthma with an eosinophilic phenotype (NCT04719832).
Targeting alarmins
Bronchial epithelium derived cytokines, also called alarmins, include thymic stromal lymphopoietin (TSLP), IL-33, and IL-25, regulate the differentiation of ILC2 and Th2 lymphocytes [230] and represent other potential targets of biologic therapy. TSLP with potent T2-inducing capacity [231] can be effectively blocked by humanized monoclonal antibody tezepelumab by preventing TLSP binding to its receptor. Tezepelumab was recently FDA-approved for the add-on maintenance treatment of adult and pediatric patients with severe asthma a 12 years and older [232], showing a substantial reduction in asthma exacerbation rates irrespective of baseline T2 biomarkers. In a phase 2 (CASCADE) study, tezepelumab reduced inflammatory cells (eosinophils, neutrophils, T cells and mast cells) in bronchial submucosa [233,234]. In the NAVIGATOR (phase 3) study, tezepelumab substantially reduced asthma exacerbation rates, improved asthma control, quality of life as well as lung function in all patients – with better outcomes in those with a T2 inflammatory profile. In the present study, tezepelumab substantially decreased blood eosinophils, serum IgE as well as FeNO, suggestive of its interaction with multiple inflammatory pathways [235]. However, in another phase 3 (SOURCE) asthma study, tezepelumab failed to allow OCS dose reduction in the overall study population, while OCS reduction could be achieved in patients with a T2-profile (baseline blood eosinophils ≥150 cells/μL) [236].
Another anti-TSLP drug, CSJ117, a neutralizing antibody fragment, is currently being tested in an inhaled formulation in patients with severe uncontrolled asthma (NCT04410523). An alternative approach to block TSLP is targeting its receptor. A fully human monoclonal antibody against TSLP receptor (TLPR), ASP7266, is currently being evaluated in pre-clinical studies and in a monkey experimental model completely inhibited induced allergic skin reactions [237].
IL-33 is a member of IL-1 cytokine family potentiating both Th1 and Th2 responses [101]. IL-33 directly activates Th2 lymphocytes, eosinophils, mast cells and basophils [238]. Itepekimab, a human IgG4P anti-IL-33 monoclonal antibody, improved asthma control, quality of life and lung function in patients with moderate-to-severe asthma [239]. Furthermore, tozorakimab, a human IgG1 monoclonal antibody against IL-33 is currently being tested in COPD (NCT05166889). Similarly for IL-25, no data regarding blocking monoclonal antibody, ABM125, have been published, yet. No significant improvement in asthma exacerbations or in lung function were observed with humanized anti-IL-9 monoclonal antibody enokizumab [240].
Targeting other molecules involved inT2 inflammation
Although initial studies with fevipiprant, an oral antagonist of chemoattractant receptor-homologous molecule on T-helper type-2 cells (CRTH2) serving as a receptor of prostaglandin D2, showed promising efficacy in patients with allergic asthma [241], the phase 3 studies failed to confirm clinical effectiveness in asthma [242] or CRSwNP and concomitant asthma [243]. Similarly, another oral CRTH2 inhibitor, setipiprant, despite showing (modest) efficacy in two allergen challenge studies [244,245], failed to improve symptoms in patients with allergic rhinitis [246].
Inhibition of CCR3 receptor for eotaxin, a chemokine attracting eosinophils, by specific inhibitor GW766994 failed to reduce blood or sputum eosinophilia and to improve lung function in patients with asthma [247].
Nemolizumab, a humanized monoclonal antibody against IL-31 receptor markedly reduced pruritus in patients with atopic dermatitis [248] and down-regulated skin inflammatory biomarkers [249]. This pro-inflammatory cytokine from the IL-6 family might also be a target in related airway diseases.
Lirentelimab (AK002), a humanized, nonfucosylated IgG1 monoclonal antibody targeting an anti–sialic acid–binding immunoglobulin-like lectin 8 (Siglec-8) expressed by eosinophils and mast cells has been tested in a Phase 2 study in antihistamine-refractory patients with chronic urticaria leading to improved disease control [250]. There are also ongoing studies with lirentelimab in eosinophilic esophagitis (NCT04322708) and duodenitis (NCT04856891).
Targeting pathways of non-T2 mechanisms
Compared to T2-biologic therapies, with anti-IgE and anti-IL-5 therapies globally used to treat severe allergic and eosinophilic asthma (+/- CRS), respectively, and with IL-4/13R inhibition being highly effective in atopic dermatitis, CRSwNP +/- severe asthma, targeting non-T2 mechanisms with monoclonal antibodies or inhibitors has been much less explored as well as less successful, so far.
Different approaches have been tested to either down-regulate recruitment of neutrophils to the airways, or inhibit cytokines associated with Th1/Th17 inflammation. CXCR1 and CXCR2 receptors for chemokines attracting preferentially neutrophils, particularly CXCL8/IL-8, CXCL3/Groα or CXCL5/ENA-78, seemed to be natural targets to reduce recruitment of these cells. Treatment with AZD5069, a CXCR2 antagonist, failed to reduce exacerbation rates in patients with uncontrolled persistent asthma [251] despite capability to reduce sputum neutrophils [252]. Similarly, a dual CXCR1/2 inhibitor SCH527123 was found to be safe and reduced sputum neutrophils but similarly failed to show adequate clinical impact in patients with severe asthma [253].
A study with humanized anti-IL-17 monoclonal antibody, secukinumab, in asthmatics (NCT01478360) was terminated requiring changes in study design and human anti-IL-17RA antibody brodalumab failed to show clinical efficacy in severe asthma [254].
Inhibition of the pro-inflammatory cytokine TNF-α has been proven to be very efficacious in multiple chronic diseases, including rheumatoid arthritis and inflammatory bowel diseases, and has also been tested in asthma. Infliximab, a humanized monoclonal antibody, was well-tolerated and decreased exacerbation rates in patients with symptomatic moderate asthma [255]. On the other hand, in moderate-to-severe persistent asthma, etanercept, a soluble TNF-alpha receptor, failed to induce beneficial effects [256]. Following treatment with golimumab, a human anti-TNF monoclonal antibody, no effect on severe exacerbations or lung function were found. Furthermore, adverse events including severe infections and malignancies occurred in golimumab treated subjects [257]. A higher risk of TB reactivation during anti-TNF therapy by infliximab or adalimumab represents another potential obstacle [258]. Hence, the individual risk/benefit assessment should be considered for each asthma patient before using TNF-blockers.
IL-1 is another important pro-inflammatory cytokine with a potential role in bronchial asthma [259]. Anakinra, a recombinant human IL-1 receptor antagonist (IL-1RA) was found to improve airway hyperreactivity and down-regulate T1 and T3 responses in an experimental model of asthma induced by fungi sensitization [260]. The initiated clinical study in asthmatics (NCT04035109) was recently stopped by COVID-19 pandemic (according to ClinicalTrials.gov). Regarding other options for IL-1 blocking, a clinical study with bermekimab, an anti-IL-1α monoclonal antibody in patients with atopic dermatitis (NCT04990440) has been terminated due to low efficacy.
Pro-inflammatory effects of IL-6 may be inhibited by a humanized monoclonal antibody against IL-6 receptor, tocilizumab, which failed to show protection against allergen-induced bronchoconstriction in asthmatic subjects [261].
More recently, blocking of IL-22 by the human monoclonal antibody fezakinumab affected transcription of multiple genes associated with severe neutrophilic asthma and atopic dermatitis [262]. In a randomized, double-blind 2a study, fezakinumab improved both clinical symptoms and molecular disease score in patients with moderate to severe atopic dermatitis [263] .
Among new drugs targeting inflammatory mediators, a clinical study with the inhibitor of reactive aldehyde species, ADX-629, is currently recruiting patients with mild asthma (NCT04728711). Furthermore, MTPS9579A, a monoclonal antibody inhibiting tryptase activity by its dissociation from active tetramers into inactive monomers showed a favourable safety profile [264]; currently, its safety and efficacy are being tested in a clinical trial in more severe asthma [NCT04092582].
In addition to targeting immune mechanisms, antibiotic treatment with macrolides seems to reduce the rate of exacerbations requiring hospitalization and improve symptom scores in severe asthma [265]. Macrolides may be effective also in CRS with low serum IgE suggesting non-T2 inflammation [266]. In patients with severe asthma (often with pronounced airway narrowing) unresponsive to maximal pharmacotherapy, bronchial thermoplasty may improve clinical outcomes [267].
Emerging approaches for asthma treatment
Multiple other potential therapeutic targets are being explored in experimental models of asthma and associated disorders including cytokines, membrane molecules and intracellular signalling pathways.
One of the cytokines of interest is IL-37, an anti-inflammatory cytokine from the IL-1 family inhibiting the production of T2 cytokines in mononuclear cells stimulated with an allergen. Furthermore, IL-37 down-regulated also IL-1β- and IL-33-induced expression of pro-inflammatory cytokines in cultures of airway epithelial cells [268].
IL-11 is a pleiotropic cytokine which was found to be up-regulated in patients with moderate and severe asthma [269] and, given its role in T2 differentiation, might be another potential therapeutic target.
On the other hand, another cytokine, IL-3 is down-regulated in the mucosa of asthmatic children and intranasal rIL-3 effectively reduced airway eosinophilia and mucus production in a murine model of allergic asthma [270].
Protective effects may also be provided by meteorin β/IL-41 showing anti-inflammatory effects in a murine model of allergic asthma [271].
Airway smooth muscle cells may be targeted by inhibition of stromal-interacting molecule 1 (STIM1) which regulates their proliferation and migration, with induction of multiple asthma-associated proteins and driving of the airway hyperreactivity in a murine model of asthma [272].
Selective inhibitor of NLRP3, OLT1177® (dapansutrile), down-regulated T2 and pro-inflammatory cytokines, caspase-1 activity, reduced lung inflammatory cells and airway hyperreactivity in a model of ovalbumin-induced asthma [273].
Poly (ADP-ribose) polymerase (PARP) is involved in the regulation of multiple genes involved in the pathogenesis of bronchial asthma including lung expression of VCAM-1 [274] and in an experimental model, PAR inhibitor olaparib reduced T2 cytokine release in house dust mite exposed mice [275].
Another approach to targeting immune cell communication is to either block or engage with their membrane molecules. CD200R engagement with CD200-Fc reduced activation, proliferation and production of type 2 cytokines in isolated lung ILC2s and downregulated airway hyperreactivity in a humanized mouse model [276].
Dual inhibition of OX40L and CD30L reduced eosinophilic inflammation and inhibited effector memory Th2 lymphocytes expansion in house dust mite challenged mice [277].
In addition to the already mentioned receptor for PGD2, CRTH2, there are multiple other eicosanoid receptors studied as potential targets of asthma therapy as reviewed recently [278,279].
Inhibition of purinergic receptors regulating the release of alarmins HMGB and IL-33 can attenuate experimental asthma onset and reduce the severity of a rhinovirus-induced asthma exacerbation [280].
Intranasal administration of standardized bacterial lysate OM-85 protected against experimental allergic asthma by multiple mechanisms including effects on airway epithelial cells, regulation of IL-33 and type 2 responses, and by DC tolerogenic reprogramming [281].
In experimental models, inhibitors of phosphoinositide-3-kinase (PI3K) and specifically PI3K-Δ were found to decrease total IgE, and T2 cytokines IL-4, IL-5, and IL-13 together with down-regulation of proinflammatory cytokines TNF-α and IL-1β while having no effect on IL-6 [282]. A dual phosphoinositide 3-kinase (PI3K)γΔ inhibitor AZD8154 is currently tested in an inhalation form in a clinical study [283].
To target anaphylaxis, the fast acting IgE inhibitors based on designed ankyrin repeat protein (DARPin) scaffolds were engineered to neutralize free IgE, dissociate preformed IgE/FcεRI complexes and actively remove prebound IgE from FcεRI on blood basophils [284].
In the future, using of microRNAs (miRNAs) inhibiting translation and upregulating mRNA degradation may be an alternative approach to target specific cells or cytokines involved in allergic inflammation [285]. Intracellular signalling of asthma related pathophysiological changes such as Goblet cell metaplasia may be experimentally inhibited also by antisense oligonucleotides [286].
Summary
Asthma affects over 350 million people globally, and a substantial proportion of this population has concomitant CRS. While many patients can reach a satisfactory disease control with standard therapies (topical corticosteroids with or without long-acting bronchodilators), many others remain uncontrolled with an increased risk for severe exacerbations and accelerated lung function decline [24] or require systemic corticosteroids imposing serious side effects including what has recently been referred to as ‘people remodelling’, i.e., permanent damage due to corticosteroids [1,287].
An expanding number of biologics targeting T2 asthma (+/- comorbid CRSwNP) has already entered clinical practice showing clinical effectiveness in distinct (partly overlapping) inflammatory phenotypes/endotypes: anti-IgE (omalizumab), anti-IL5 (mepolizumab, reslizumab)/anti-IL5R (benralizumab), anti-IL4Rα (anti-IL4/IL-13; dupilumab), and only recently anti-alarmin TSLP (tezepelumab) [1,288]. However, differences in age indications exist among the available biologics. Presently, omalizumab, mepolizumab and dupilumab may be used in adults and children with asthma aged 6–11 years; tezepelumab is available for adults and children aged 12 years and over, while studies in younger children are ongoing.
Apart from offering targeted treatment options and preventing toxic effects associated with corticosteroid-overuse, these new molecules further helped to unravel underlying mechanisms and to define disease subsets. Based on their respective mechanisms of action, some biologics may achieve disease remission [289] and even show disease-modifying potential in distinct patient populations [123]. These potential aspects (and their persistence) are presently being addressed in a number of clinical studies.
So far, no biologic therapies have shown consistent clinical benefits in non-T2 asthma, although the lack of a (sputum) inflammatory signature may present a significant bias in patients well-controlled by ICS with or without targeted treatments [290]. Hence, a clinically practical approach to non-T2 asthma is best guided by identifying (and subsequent treatment) treatable traits both intrapulmonary, e.g., airway infections, airway narrowing and airway hyperresponsiveness as well as extrapulmonary causes: comorbid conditions, obesity, smoking, occupational exposure, etc [131,291,292]. Better understanding of the underlying pathways on a molecular level may lead to new therapeutic approaches further improving personalized care of patients with asthma and CRS.
Abbreviations
- AA
arachidonic acid
- AERD
aspirin-exacerbated respiratory disease
- AHR
airway hyperresponsiveness
- APC
antigen presenting cell
- ASM
airway smooth muscle
- BALF
bronchoalveolar lavage fluid
- CCL
C-C motif chemokine ligand
- CCR3
C-C chemokine receptor type 3
- CCR4
CC-chemokine receptor 4
- CD
cluster of differentiation
- CD200-Fc
CD200 fusion protein
- CD200R
CD200 receptor
- CD30L
CD30 ligand
- CD45RA
cluster of differentiation 45RA
- CD45RO
cluster of differentiation 45RO
- CRS
chronic rhinosinusitis
- CRSsNP
chronic rhinosinusitis without nasal polyps
- CRSwNP
chronic rhinosinusitis with nasal polyps
- CRTH2
chemoattractant receptor-homologous molecule on T-helper type-2 cells
- CRTH2+
prostaglandin D2 receptor 2 positive
- CXCL
C-X-C motif chemokine ligand
- CysLTs
cysteinyl leukotrienes
- DARPin
designed ankyrin repeat protein
- DC
dendritic cell
- ECP
eosinophil cationic protein
- EDN
eosinophil-derived neurotoxin
- EMA
European Medicines Agency
- EPX
eosinophil peroxidase
- FcεRI
High-affinity Fc receptor for IgE
- FcεRII
CD23 low-affinity Fc receptor for IgE
- FDA
U.S. Food and Drug Administration
- FeNO
fractional exhaled nitric oxide
- FEV1
forced expiratory volume in 1 second
- HLA-DR
human leukocyte antigen-DR
- HMGB
high mobility group box
- HRQoL
health-related quality of life
- IFN-γ
interferon-γ
- IgE
immunoglobulin E
- IgG4P
immunoglobulin G4P
- IL
interleukin
- ILCs
innate lymphoid cells
- LTC4
leukotriene C4
- LTD4
leukotriene D4
- LTE4
leukotriene E4
- MBP
major basic protein
- mDC
myeloid dendritic cell
- mIgE
membrane-expressed IgE
- miRNAs
microRNA
- NCT
ClinicalTrials.gov Identifier (National Clinical Trial)
- NLRP3
NOD-like receptor family, pyrin domain-containing protein 3
- Non-T2
Non-type 2
- NP
nasal polyps
- NSAID-ERD
nonsteroidal anti-inflammatory drugs exacerbated respiratory disease
- NSAID
nonsteroidal anti-inflammatory drug
- OCS
oral corticosteroids
- PALM
pollen-associated lipid mediator
- PARP
poly (ADP-ribose) polymerase
- pDC
plasmacytoid dendritic cell
- PGD2
prostaglandin D2
- PI3K
Phosphoinositide-3-kinase
- PRR
pattern recognition receptor
- RANTES
regulated on activation, normal T cell expressed and secreted
- Siglec-8
sialic acid–binding immunoglobulin-like lectin 8
- SOURCE
Phase 3 study evaluating the safety and efficacy of tezepelumab on OCS dose-reduction in asthma
- STIM1
stromal-interacting molecule 1
- T1
Type 1
- TGF-β
transforming growth factor-β
- Th
T helper
- Th1
T helper cell type 1
- Th17
Type 17 T helper
- Th17/Treg
Type 17 T helper/Regulatory T cells
- Th2
CD4+ T helper cell type 2
- TLPR
TSLP receptor
- TNF-α
tumor necrosis factor-α
- TSLP
Thymic stromal lymphopoietin
- VCAM-1
vascular cell adhesion molecule-1
Data Availability
This review manuscript does not contain original data.
Competing Interests
The authors declare that there are no competing interests associated with the manuscript.
CRediT Author Contribution
Ilja Striz: Conceptualization, Writing—original draft, Writing—review & editing. Kornel Golebski: Writing—original draft, Writing—review & editing. Zuzana Strizova: Writing—original draft, Writing—review & editing. Stelios Loukides: Writing—original draft, Writing—review & editing. Petros Bakakos: Writing—original draft, Writing—review & editing. Nicola A. Hanania: Writing—original draft, Writing—review & editing. Milos Jesenak: Writing—original draft, Writing—review & editing. Zuzana Diamant: Conceptualization, Writing—original draft, Writing—review & editing.
References
- 1.Chipps B.E., Murphy K.R. and Oppenheimer J. (2022) 2020 NAEPP Guidelines Update and GINA 2021-Asthma Care Differences, Overlap, and Challenges. J. Allergy Clin. Immunol. Pract. 10, S19–S30 10.1016/j.jaip.2021.10.032 [DOI] [PubMed] [Google Scholar]
- 2.De Prins L., Raap U., Mueller T., Schmid-Grendelmeier P., Haase C.H., Backer V.et al. (2022) White Paper on European Patient Needs and Suggestions on Chronic Type 2 Inflammation of Airways and Skin by EUFOREA. Front Allergy 3, 889221 10.3389/falgy.2022.889221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Berankova K., Uhlik J., Honkova L. and Pohunek P. (2014) Structural changes in the bronchial mucosa of young children at risk of developing asthma. Pediatr. Allergy Immunol. 25, 136–142 10.1111/pai.12119 [DOI] [PubMed] [Google Scholar]
- 4.Busse W.W. (2010) The relationship of airway hyperresponsiveness and airway inflammation: Airway hyperresponsiveness in asthma: its measurement and clinical significance. Chest 138, 4S–10S 10.1378/chest.10-0100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Janulaityte I., Januskevicius A., Rimkunas A., Palacionyte J., Vitkauskiene A. and Malakauskas K. (2022) Asthmatic eosinophils alter the gene expression of extracellular matrix proteins in airway smooth muscle cells and pulmonary fibroblasts. Int. J. Mol. Sci. 23, 4086 10.3390/ijms23084086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tliba O. and Panettieri R.A. Jr (2019) Paucigranulocytic asthma: uncoupling of airway obstruction from inflammation. J. Allergy Clin. Immunol. 143, 1287–1294 10.1016/j.jaci.2018.06.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Diamant Z., Boot J.D., Mantzouranis E., Flohr R., Sterk P.J. and Gerth van Wijk R. (2010) Biomarkers in asthma and allergic rhinitis. Pulm. Pharmacol. Ther. 23, 468–481 10.1016/j.pupt.2010.06.006 [DOI] [PubMed] [Google Scholar]
- 8.Thamrin C., Frey U., Kaminsky D.A., Reddel H.K., Seely A.J., Suki B.et al. (2016) Systems biology and clinical practice in respiratory medicine. The Twain Shall Meet. Am. J. Respir. Crit. Care Med. 194, 1053–1061 10.1164/rccm.201511-2288PP [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Silkoff P.E., Moore W.C. and Sterk P.J. (2019) Three major efforts to phenotype asthma: severe asthma research program, asthma disease endotyping for personalized therapeutics, and unbiased biomarkers for the prediction of respiratory disease outcome. Clin. Chest Med. 40, 13–28 10.1016/j.ccm.2018.10.016 [DOI] [PubMed] [Google Scholar]
- 10.Wenzel S.E. (2012) Asthma phenotypes: the evolution from clinical to molecular approaches. Nat. Med. 18, 716–725 10.1038/nm.2678 [DOI] [PubMed] [Google Scholar]
- 11.Woodruff P.G., Modrek B., Choy D.F., Jia G., Abbas A.R., Ellwanger A.et al. (2009) T-helper type 2-driven inflammation defines major subphenotypes of asthma. Am. J. Respir. Crit. Care Med. 180, 388–395 10.1164/rccm.200903-0392OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hammad H. and Lambrecht B.N. (2021) The basic immunology of asthma. Cell 184, 1469–1485 10.1016/j.cell.2021.02.016 [DOI] [PubMed] [Google Scholar]
- 13.de Groot J.C., Ten Brinke A. and Bel E.H. (2015) Management of the patient with eosinophilic asthma: a new era begins. ERJ Open Res. 1, 00024–2015 10.1183/23120541.00024-2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Green R.H., Brightling C.E., McKenna S., Hargadon B., Parker D., Bradding P.et al. (2002) Asthma exacerbations and sputum eosinophil counts: a randomised controlled trial. Lancet 360, 1715–1721 10.1016/S0140-6736(02)11679-5 [DOI] [PubMed] [Google Scholar]
- 15.Frossing L., Silberbrandt A., Von Bulow A., Backer V. and Porsbjerg C. (2021) The prevalence of subtypes of type 2 inflammation in an unselected population of patients with severe asthma. J. Allergy Clin. Immunol. Pract. 9, 1267–1275 10.1016/j.jaip.2020.09.051 [DOI] [PubMed] [Google Scholar]
- 16.Fokkens W.J., Lund V., Bachert C., Mullol J., Bjermer L., Bousquet J.et al. (2019) EUFOREA consensus on biologics for CRSwNP with or without asthma. Allergy 74, 2312–2319 10.1111/all.13875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fokkens W.J., Lund V.J., Hopkins C., Hellings P.W., Kern R., Reitsma S.et al. (2020) European position paper on rhinosinusitis and nasal polyps 2020. Rhinology 58, 1–464 10.4193/Rhin20.401 [DOI] [PubMed] [Google Scholar]
- 18.Matucci A., Bormioli S., Nencini F., Chiccoli F., Vivarelli E., Maggi E.et al. (2021) Asthma and chronic rhinosinusitis: how similar are they in pathogenesis and treatment responses? Int. J. Mol. Sci. 22, 3340 10.3390/ijms22073340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Diamant Z., Vijverberg S., Alving K., Bakirtas A., Bjermer L., Custovic A.et al. (2019) Toward clinically applicable biomarkers for asthma: An EAACI position paper. Allergy 74, 1835–1851 10.1111/all.13806 [DOI] [PubMed] [Google Scholar]
- 20.Alving K., Diamant Z., Lucas S., Magnussen H., Pavord I.D., Piacentini G.et al. (2020) Point-of-care biomarkers in asthma management: time to move forward. Allergy 75, 995–997 10.1111/all.14045 [DOI] [PubMed] [Google Scholar]
- 21.Khatri S.B., Iaccarino J.M., Barochia A., Soghier I., Akuthota P., Brady A.et al. (2021) Use of fractional exhaled nitric oxide to guide the treatment of asthma: an official american thoracic society clinical practice guideline. Am. J. Respir. Crit. Care Med. 204, e97–e109 10.1164/rccm.202109-2093ST [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moore W.C., Bleecker E.R., Curran-Everett D., Erzurum S.C., Ameredes B.T., Bacharier L.et al. (2007) Characterization of the severe asthma phenotype by the National Heart, Lung, and Blood Institute's Severe Asthma Research Program. J. Allergy Clin. Immunol. 119, 405–413 10.1016/j.jaci.2006.11.639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bourdin A., Bjermer L., Brightling C., Brusselle G.G., Chanez P., Chung K.F.et al. (2019) ERS/EAACI statement on severe exacerbations in asthma in adults: facts, priorities and key research questions. Eur. Respir. J. 54, 1900900 10.1183/13993003.00900-2019 [DOI] [PubMed] [Google Scholar]
- 24.O'Byrne P.M., Pedersen S., Lamm C.J., Tan W.C., Busse W.W. and Group SI (2009) Severe exacerbations and decline in lung function in asthma. Am. J. Respir. Crit. Care Med. 179, 19–24 10.1164/rccm.200807-1126OC [DOI] [PubMed] [Google Scholar]
- 25.Sze E., Bhalla A. and Nair P. (2020) Mechanisms and therapeutic strategies for non-T2 asthma. Allergy 75, 311–325 10.1111/all.13985 [DOI] [PubMed] [Google Scholar]
- 26.Barnes P.J. (2017) Cellular and molecular mechanisms of asthma and COPD. Clin. Sci. (Lond.) 131, 1541–1558 10.1042/CS20160487 [DOI] [PubMed] [Google Scholar]
- 27.Papi A., Brightling C., Pedersen S.E. and Reddel H.K. (2018), Asthma Lancet 391, 783–800 10.1016/S0140-6736(17)33311-1 [DOI] [PubMed] [Google Scholar]
- 28.Stevens W.W., Lee R.J., Schleimer R.P. and Cohen N.A. (2015) Chronic rhinosinusitis pathogenesis. J. Allergy Clin. Immunol. 136, 1442–1453 10.1016/j.jaci.2015.10.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Poposki J.A., Klingler A.I., Stevens W.W., Suh L.A., Tan B.K., Peters A.T.et al. (2022) Elevation of activated neutrophils in chronic rhinosinusitis with nasal polyps. J. Allergy Clin. Immunol. 149, 1666–1674 10.1016/j.jaci.2021.11.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wenzel S.E. (2006) Asthma: defining of the persistent adult phenotypes. Lancet 368, 804–813 10.1016/S0140-6736(06)69290-8 [DOI] [PubMed] [Google Scholar]
- 31.Lambrecht B.N. and Hammad H. (2015) The immunology of asthma. Nat. Immunol. 16, 45–56 10.1038/ni.3049 [DOI] [PubMed] [Google Scholar]
- 32.Wawrzyniak P., Wawrzyniak M., Wanke K., Sokolowska M., Bendelja K., Ruckert B.et al. (2017) Regulation of bronchial epithelial barrier integrity by type 2 cytokines and histone deacetylases in asthmatic patients. J. Allergy Clin. Immunol. 139, 93–103 10.1016/j.jaci.2016.03.050 [DOI] [PubMed] [Google Scholar]
- 33.Sweerus K., Lachowicz-Scroggins M., Gordon E., LaFemina M., Huang X., Parikh M.et al. (2017) Claudin-18 deficiency is associated with airway epithelial barrier dysfunction and asthma. J. Allergy Clin. Immunol. 139, 72e1–81e1 10.1016/j.jaci.2016.02.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Heijink I.H., Kies P.M., Kauffman H.F., Postma D.S., van Oosterhout A.J. and Vellenga E. (2007) Down-regulation of E-cadherin in human bronchial epithelial cells leads to epidermal growth factor receptor-dependent Th2 cell-promoting activity. J. Immunol. 178, 7678–7685 10.4049/jimmunol.178.12.7678 [DOI] [PubMed] [Google Scholar]
- 35.Wagener A.H., Zwinderman A.H., Luiten S., Fokkens W.J., Bel E.H., Sterk P.J.et al. (2014) dsRNA-induced changes in gene expression profiles of primary nasal and bronchial epithelial cells from patients with asthma, rhinitis and controls. Respir. Res. 15, 9 10.1186/1465-9921-15-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Golebski K., Roschmann K.I., Toppila-Salmi S., Hammad H., Lambrecht B.N., Renkonen R.et al. (2013) The multi-faceted role of allergen exposure to the local airway mucosa. Allergy 68, 152–160 10.1111/all.12080 [DOI] [PubMed] [Google Scholar]
- 37.Gandhi V.D. and Vliagoftis H. (2015) Airway epithelium interactions with aeroallergens: role of secreted cytokines and chemokines in innate immunity. Front Immunol. 6, 147 10.3389/fimmu.2015.00147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yu Q.N., Tan W.P., Fan X.L., Guo Y.B., Qin Z.L., Li C.L.et al. (2018) Increased Group 2 innate lymphoid cells are correlated with eosinophilic granulocytes in patients with allergic airway inflammation. Int. Arch Allergy Immunol. 176, 124–132 10.1159/000488050 [DOI] [PubMed] [Google Scholar]
- 39.van der Ploeg E.K., Golebski K., van Nimwegen M., Fergusson J.R., Heesters B.A., Martinez-Gonzalez I.et al. (2021) Steroid-resistant human inflammatory ILC2s are marked by CD45RO and elevated in type 2 respiratory diseases. Sci. Immunol. 6, eabd3489 10.1126/sciimmunol.abd3489 [DOI] [PubMed] [Google Scholar]
- 40.Weston C.A., Rana B.M.J. and Cousins D.J. (2019) Differential expression of functional chemokine receptors on human blood and lung group 2 innate lymphoid cells. J. Allergy Clin. Immunol. 143, 410e9–413e9 10.1016/j.jaci.2018.08.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chen R., Smith S.G., Salter B., El-Gammal A., Oliveria J.P., Obminski C.et al. (2017) Allergen-induced Increases in Sputum Levels of Group 2 Innate Lymphoid Cells in Subjects with Asthma. Am. J. Respir. Crit. Care Med. 196, 700–712 10.1164/rccm.201612-2427OC [DOI] [PubMed] [Google Scholar]
- 42.Fajt M.L., Gelhaus S.L., Freeman B., Uvalle C.E., Trudeau J.B., Holguin F.et al. (2013) Prostaglandin D(2) pathway upregulation: relation to asthma severity, control, and TH2 inflammation. J. Allergy Clin. Immunol. 131, 1504–1512 10.1016/j.jaci.2013.01.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.McDowell P.J. and Heaney L.G. (2020) Different endotypes and phenotypes drive the heterogeneity in severe asthma. Allergy 75, 302–310 10.1111/all.13966 [DOI] [PubMed] [Google Scholar]
- 44.Simpson J.L., Grissell T.V., Douwes J., Scott R.J., Boyle M.J. and Gibson P.G. (2007) Innate immune activation in neutrophilic asthma and bronchiectasis. Thorax 62, 211–218 10.1136/thx.2006.061358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kyriakopoulos C., Gogali A., Bartziokas K. and Kostikas K. (2021) Identification and treatment of T2-low asthma in the era of biologics. ERJ Open Res. 7, 00309–2020 10.1183/23120541.00309-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ito K., Chung K.F. and Adcock I.M. (2006) Update on glucocorticoid action and resistance. J. Allergy Clin. Immunol. 117, 522–543 10.1016/j.jaci.2006.01.032 [DOI] [PubMed] [Google Scholar]
- 47.Adcock I.M., Ford P.A., Bhavsar P., Ahmad T. and Chung K.F. (2008) Steroid resistance in asthma: mechanisms and treatment options. Curr. Allergy Asthma Rep. 8, 171–178 10.1007/s11882-008-0028-4 [DOI] [PubMed] [Google Scholar]
- 48.Loke T.K., Mallett K.H., Ratoff J., O'Connor B.J., Ying S., Meng Q.et al. (2006) Systemic glucocorticoid reduces bronchial mucosal activation of activator protein 1 components in glucocorticoid-sensitive but not glucocorticoid-resistant asthmatic patients. J. Allergy Clin. Immunol. 118, 368–375 10.1016/j.jaci.2006.04.055 [DOI] [PubMed] [Google Scholar]
- 49.Adcock I.M. and Lane S.J. (2003) Corticosteroid-insensitive asthma: molecular mechanisms. J. Endocrinol. 178, 347–355 10.1677/joe.0.1780347 [DOI] [PubMed] [Google Scholar]
- 50.Kuruvilla M.E., Lee F.E. and Lee G.B. (2019) Understanding Asthma Phenotypes, Endotypes, and Mechanisms of Disease. Clin. Rev. Allergy Immunol. 56, 219–233 10.1007/s12016-018-8712-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.van Helden M.J. and Lambrecht B.N. (2013) Dendritic cells in asthma. Curr. Opin. Immunol. 25, 745–754 10.1016/j.coi.2013.10.002 [DOI] [PubMed] [Google Scholar]
- 52.Lu Y., Kared H., Tan S.W., Becht E., Newell E.W., Van Bever H.P.S.et al. (2018) Dynamics of helper CD4 T cells during acute and stable allergic asthma. Mucosal. Immunol. 11, 1640–1652 10.1038/s41385-018-0057-9 [DOI] [PubMed] [Google Scholar]
- 53.Muehling L.M., Lawrence M.G. and Woodfolk J.A. (2017) Pathogenic CD4(+) T cells in patients with asthma. J. Allergy Clin. Immunol. 140, 1523–1540 10.1016/j.jaci.2017.02.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hondowicz B.D., An D., Schenkel J.M., Kim K.S., Steach H.R., Krishnamurty A.T.et al. (2016) Interleukin-2-dependent allergen-specific tissue-resident memory cells drive asthma. Immunity 44, 155–166 10.1016/j.immuni.2015.11.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Domvri K., Porpodis K., Tzimagiorgis G., Chatzopoulou F., Kontakiotis T., Kyriazis G.et al. (2019) Th2/Th17 cytokine profile in phenotyped Greek asthmatics and relationship to biomarkers of inflammation. Respir. Med. 151, 102–110 10.1016/j.rmed.2019.03.017 [DOI] [PubMed] [Google Scholar]
- 56.Irvin C., Zafar I., Good J., Rollins D., Christianson C., Gorska M.M.et al. (2014) Increased frequency of dual-positive TH2/TH17 cells in bronchoalveolar lavage fluid characterizes a population of patients with severe asthma. J. Allergy Clin. Immunol. 134, 1175e7–1186e7 10.1016/j.jaci.2014.05.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Brussino L., Heffler E., Bucca C., Nicola S. and Rolla G. (2018) Eosinophils target therapy for severe asthma: critical points. Biomed. Res. Int. 2018, 7582057 10.1155/2018/7582057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Durrani S.R., Viswanathan R.K. and Busse W.W. (2011) What effect does asthma treatment have on airway remodeling? Current perspectives J. Allergy Clin. Immunol. 128, 439–448, quiz 49-50 10.1016/j.jaci.2011.06.002 [DOI] [PubMed] [Google Scholar]
- 59.Bal S.M., Bernink J.H., Nagasawa M., Groot J., Shikhagaie M.M., Golebski K.et al. (2016) IL-1beta, IL-4 and IL-12 control the fate of group 2 innate lymphoid cells in human airway inflammation in the lungs. Nat. Immunol. 17, 636–645 10.1038/ni.3444 [DOI] [PubMed] [Google Scholar]
- 60.Pelly V.S., Kannan Y., Coomes S.M., Entwistle L.J., Ruckerl D., Seddon B.et al. (2016) IL-4-producing ILC2s are required for the differentiation of TH2 cells following Heligmosomoides polygyrus infection. Mucosal Immunol. 9, 1407–1417 10.1038/mi.2016.4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Mendez-Enriquez E. and Hallgren J. (2019) Mast cells and their progenitors in allergic asthma. Front. Immunol. 10, 821 10.3389/fimmu.2019.00821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kim B.S., Wang K., Siracusa M.C., Saenz S.A., Brestoff J.R., Monticelli L.A.et al. (2014) Basophils promote innate lymphoid cell responses in inflamed skin. J. Immunol. 193, 3717–3725 10.4049/jimmunol.1401307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Inclan-Rico J.M., Ponessa J.J., Valero-Pacheco N., Hernandez C.M., Sy C.B., Lemenze A.D.et al. (2020) Basophils prime group 2 innate lymphoid cells for neuropeptide-mediated inhibition. Nat. Immunol. 21, 1181–1193 10.1038/s41590-020-0753-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Gibson P.G., Simpson J.L., Hankin R., Powell H. and Henry R.L. (2003) Relationship between induced sputum eosinophils and the clinical pattern of childhood asthma. Thorax 58, 116–121 10.1136/thorax.58.2.116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hu Y., Chen Z., Zeng J., Zheng S., Sun L., Zhu L.et al. (2020) Th17/Treg imbalance is associated with reduced indoleamine 2,3 dioxygenase activity in childhood allergic asthma. Allergy Asthma Clin. Immunol. 16, 61 10.1186/s13223-020-00457-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Palmer J.N., Messina J.C., Biletch R., Grosel K. and Mahmoud R.A. (2019) A cross-sectional, population-based survey of U.S. adults with symptoms of chronic rhinosinusitis. Allergy Asthma Proc. 40, 48–56 10.2500/aap.2019.40.4182 [DOI] [PubMed] [Google Scholar]
- 67.Passali D., Cingi C., Cambi J., Passali F., Muluk N.B. and Bellussi M.L. (2016) A survey on chronic rhinosinusitis: opinions from experts of 50 countries. Eur. Arch. Otorhinolaryngol. 273, 2097–2109 10.1007/s00405-015-3880-6 [DOI] [PubMed] [Google Scholar]
- 68.Hellings P.W. and Steelant B. (2020) Epithelial barriers in allergy and asthma. J. Allergy Clin. Immunol. 145, 1499–1509 10.1016/j.jaci.2020.04.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Peters A.T., Bose S., Guo A., Li N., Benjamin M., Prickett M.et al. (2021) Prevalence of bronchiectasis in patients with chronic rhinosinusitis in a tertiary care center. J. Allergy Clin. Immunol. Pract. 9, 3188e2–3195e2 10.1016/j.jaip.2021.04.054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ek A., Middelveld R.J., Bertilsson H., Bjerg A., Ekerljung L., Malinovschi A.et al. (2013) Chronic rhinosinusitis in asthma is a negative predictor of quality of life: results from the Swedish GA(2)LEN survey. Allergy 68, 1314–1321 10.1111/all.12222 [DOI] [PubMed] [Google Scholar]
- 71.Denlinger L.C., Phillips B.R., Ramratnam S., Ross K., Bhakta N.R., Cardet J.C.et al. (2017) Inflammatory and comorbid features of patients with severe asthma and frequent exacerbations. Am. J. Respir. Crit. Care Med. 195, 302–313 10.1164/rccm.201602-0419OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Laidlaw T.M., Mullol J., Woessner K.M., Amin N. and Mannent L.P. (2021) Chronic rhinosinusitis with nasal polyps and asthma. J. Allergy Clin. Immunol. Pract. 9, 1133–1141 10.1016/j.jaip.2020.09.063 [DOI] [PubMed] [Google Scholar]
- 73.Khan A., Vandeplas G., Huynh T.M.T., Joish V.N., Mannent L., Tomassen P.et al. (2019) The Global Allergy and Asthma European Network (GALEN rhinosinusitis cohort: a large European cross-sectional study of chronic rhinosinusitis patients with and without nasal polyps. Rhinology 57, 32–42 10.4193/Rhin17.255 [DOI] [PubMed] [Google Scholar]
- 74.Lee R.U. and Stevenson D.D. (2011) Aspirin-exacerbated respiratory disease: evaluation and management. Allergy Asthma Immunol. Res. 3, 3–10 10.4168/aair.2011.3.1.3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Buchheit K., Bensko J.C., Lewis E., Gakpo D. and Laidlaw T.M. (2020) The importance of timely diagnosis of aspirin-exacerbated respiratory disease for patient health and safety. World J. Otorhinolaryngol. Head Neck Surg. 6, 203–206 10.1016/j.wjorl.2020.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Laidlaw T.M. and Boyce J.A. (2023) Updates on immune mechanisms in aspirin-exacerbated respiratory disease. J. Allergy Clin. Immunol., 151301–309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kato A., Schleimer R.P. and Bleier B.S. (2022) Mechanisms and pathogenesis of chronic rhinosinusitis. J. Allergy Clin. Immunol. 149, 1491–1503 10.1016/j.jaci.2022.02.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Polzehl D., Moeller P., Riechelmann H. and Perner S. (2006) Distinct features of chronic rhinosinusitis with and without nasal polyps. Allergy 61, 1275–1279 10.1111/j.1398-9995.2006.01132.x [DOI] [PubMed] [Google Scholar]
- 79.Wang X., Zhang N., Bo M., Holtappels G., Zheng M., Lou H.et al. (2016) Diversity of TH cytokine profiles in patients with chronic rhinosinusitis: A multicenter study in Europe, Asia, and Oceania. J. Allergy Clin. Immunol. 138, 1344–1353 10.1016/j.jaci.2016.05.041 [DOI] [PubMed] [Google Scholar]
- 80.Tomassen P., Vandeplas G., Van Zele T., Cardell L.O., Arebro J., Olze H.et al. (2016) Inflammatory endotypes of chronic rhinosinusitis based on cluster analysis of biomarkers. J. Allergy Clin. Immunol. 137, 1449e4–1456e4 10.1016/j.jaci.2015.12.1324 [DOI] [PubMed] [Google Scholar]
- 81.Bachert C. and Akdis C.A. (2016) Phenotypes and emerging endotypes of chronic rhinosinusitis. J. Allergy Clin. Immunol. Pract. 4, 621–628 10.1016/j.jaip.2016.05.004 [DOI] [PubMed] [Google Scholar]
- 82.Akdis C.A., Bachert C., Cingi C., Dykewicz M.S., Hellings P.W., Naclerio R.M.et al. (2013) Endotypes and phenotypes of chronic rhinosinusitis: a PRACTALL document of the European Academy of Allergy and Clinical Immunology and the American Academy of Allergy, Asthma & Immunology. J. Allergy Clin. Immunol. 131, 1479–1490 10.1016/j.jaci.2013.02.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Olonisakin T.F., Moore J.A., Barel S., Uribe B., Parker D., Bowers E.M.R.et al. (2022) Fractional exhaled nitric oxide as a marker of mucosal inflammation in chronic rhinosinusitis. Am. J. Rhinol. Allergy 19458924221080260 10.1177/19458924221080260 [DOI] [PubMed] [Google Scholar]
- 84.Heath J., Hartzell L., Putt C. and Kennedy J.L. (2018) Chronic rhinosinusitis in children: pathophysiology, evaluation, and medical management. Curr. Allergy Asthma Rep. 18, 37 10.1007/s11882-018-0792-8 [DOI] [PubMed] [Google Scholar]
- 85.Hough K.P., Curtiss M.L., Blain T.J., Liu R.-M., Trevor J., Deshane J.S.et al. (2020) Airway remodeling in asthma. Front. Med. 7, 191.Available from: https://www.frontiersin.org/article/10.3389/fmed.2020.00191 10.3389/fmed.2020.00191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Erle D.J. and Sheppard D. (2014) The cell biology of asthma. J. Cell Biol. 205, 621–631 10.1083/jcb.201401050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Banno A., Reddy A.T., Lakshmi S.P. and Reddy R.C. (2020) Bidirectional interaction of airway epithelial remodeling and inflammation in asthma. Clin. Sci. (Lond.) 134, 1063–1079 10.1042/CS20191309 [DOI] [PubMed] [Google Scholar]
- 88.Joseph C. and Tatler A.L. (2022) Pathobiology of airway remodeling in asthma: the emerging role of integrins. J Asthma Allergy 15, 595–610 10.2147/JAA.S267222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Khalfaoui L., Symon F.A., Couillard S., Hargadon B., Chaudhuri R., Bicknell S.et al. (2022) Airway remodelling rather than cellular infiltration characterizes both type2 cytokine biomarker-high and -low severe asthma. Allergy 77, 2974–2986 10.1111/all.15376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Pavord I.D., Hanania N.A. and Corren J. (2022) Controversies in allergy: choosing a biologic for patients with severe asthma. J. Allergy Clin. Immunol. Pract. 10, 410–419 10.1016/j.jaip.2021.12.014 [DOI] [PubMed] [Google Scholar]
- 91.Lommatzsch M. and Stoll P. (2016) Novel strategies for the treatment of asthma. Allergo J. Int. 25, 11–17 10.1007/s40629-016-0093-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Heijink I.H., Kuchibhotla V.N.S., Roffel M.P., Maes T., Knight D.A., Sayers I.et al. (2020) Epithelial cell dysfunction, a major driver of asthma development. Allergy 75, 1902–1917 10.1111/all.14421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Hiemstra P.S., McCray P.B. Jr and Bals R. (2015) The innate immune function of airway epithelial cells in inflammatory lung disease. Eur. Respir. J. 45, 1150–1162 10.1183/09031936.00141514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Striz I., Brabcova E., Kolesar L. and Sekerkova A. (2014) Cytokine networking of innate immunity cells: a potential target of therapy. Clin. Sci. (Lond.) 126, 593–612 10.1042/CS20130497 [DOI] [PubMed] [Google Scholar]
- 95.Laulajainen-Hongisto A., Toppila-Salmi S.K., Luukkainen A. and Kern R. (2020) Airway epithelial dynamics in allergy and related chronic inflammatory airway diseases. Front. Cell Development. Biol. 8, 204.Available from: https://www.frontiersin.org/article/10.3389/fcell.2020.00204 10.3389/fcell.2020.00204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Yuksel H. and Turkeli A. (2017) Airway epithelial barrier dysfunction in the pathogenesis and prognosis of respiratory tract diseases in childhood and adulthood. Tissue Barriers 5, e1367458 10.1080/21688370.2017.1367458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Wynne M., Atkinson C., Schlosser R.J. and Mulligan J.K. (2019) Contribution of epithelial cell dysfunction to the pathogenesis of chronic rhinosinusitis with nasal polyps. Am. J. Rhinol. Allergy 33, 782–790 10.1177/1945892419868588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Kato A. (2019) Group 2 innate lymphoid cells in airway diseases. Chest 156, 141–149 10.1016/j.chest.2019.04.101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Matsumoto H., Niimi A., Tabuena R.P., Takemura M., Ueda T., Yamaguchi M.et al. (2007) Airway wall thickening in patients with cough variant asthma and nonasthmatic chronic cough. Chest 131, 1042–1049 10.1378/chest.06-1025 [DOI] [PubMed] [Google Scholar]
- 100.Ha E.V.S. and Rogers D.F. (2016) Novel therapies to inhibit mucus synthesis and secretion in airway hypersecretory diseases. Pharmacology 97, 84–100 10.1159/000442794 [DOI] [PubMed] [Google Scholar]
- 101.Striz I. (2017) Cytokines of the IL-1 family: recognized targets in chronic inflammation underrated in organ transplantations. Clin. Sci. (Lond.) 131, 2241–2256 10.1042/CS20170098 [DOI] [PubMed] [Google Scholar]
- 102.Alevy Y.G., Patel A.C., Romero A.G., Patel D.A., Tucker J., Roswit W.T.et al. (2012) IL-13-induced airway mucus production is attenuated by MAPK13 inhibition. J. Clin. Invest. 122, 4555–4568 10.1172/JCI64896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Walsh K.P. and Mills K.H. (2013) Dendritic cells and other innate determinants of T helper cell polarisation. Trends Immunol. 34, 521–530 10.1016/j.it.2013.07.006 [DOI] [PubMed] [Google Scholar]
- 104.Lambrecht B.N. and Hammad H. (2012) The airway epithelium in asthma. Nat. Med. 18, 684–692 10.1038/nm.2737 [DOI] [PubMed] [Google Scholar]
- 105.Patente T.A., Pinho M.P., Oliveira A.A., Evangelista G.C.M., Bergami-Santos P.C. and Barbuto J.A.M. (2019) Human dendritic cells: their heterogeneity and clinical application potential in cancer immunotherapy. Front. Immunol. 9, 3176.Available from: https://www.frontiersin.org/article/10.3389/fimmu.2018.03176 10.3389/fimmu.2018.03176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Gaurav R. and Agrawal D.K. (2013) Clinical view on the importance of dendritic cells in asthma. Expert Rev. Clin. Immunol. 9, 899–919 10.1586/1744666X.2013.837260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Gill M.A. (2012) The role of dendritic cells in asthma. J. Allergy Clin. Immunol. 129, 889–901 10.1016/j.jaci.2012.02.028 [DOI] [PubMed] [Google Scholar]
- 108.Romagnani S. (2004) The increased prevalence of allergy and the hygiene hypothesis: missing immune deviation, reduced immune suppression, or both? Immunology 112, 352–363 10.1111/j.1365-2567.2004.01925.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Altmann F. (2007) The role of protein glycosylation in allergy. Int. Arch. Allergy Immunol. 142, 99–115 10.1159/000096114 [DOI] [PubMed] [Google Scholar]
- 110.Gilles S., Mariani V., Bryce M., Mueller M.J., Ring J., Behrendt H.et al. (2009) Pollen allergens do not come alone: pollen associated lipid mediators (PALMS) shift the human immune systems towards a T(H)2-dominated response. Allergy, Asthma Clin. Immunol.: Off. J. Canadian Soc. Allergy Clin. Immunol. 5, 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Zuyderduyn S., Sukkar M.B., Fust A., Dhaliwal S. and Burgess J.K. (2008) Treating asthma means treating airway smooth muscle cells. Eur. Respir. J. 32, 265–274, Available from: https://erj.ersjournals.com/content/erj/32/2/265.full.pdf 10.1183/09031936.00051407 [DOI] [PubMed] [Google Scholar]
- 112.Ozier A., Allard B., Bara I., Girodet P.O., Trian T., Marthan R.et al. (2011) The pivotal role of airway smooth muscle in asthma pathophysiology. J. Allergy 2011, 7427 10.1155/2011/742710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Dileepan M., Sarver A.E., Rao S.P., Panettieri R.A. Jr, Subramanian S. and Kannan M.S. (2016) MicroRNA mediated chemokine responses in human airway smooth muscle cells. PloS ONE 11, e0150842 10.1371/journal.pone.0150842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Mahn K., Hirst S.J., Ying S., Holt M.R., Lavender P., Ojo O.O.et al. (2009) Diminished sarco/endoplasmic reticulum Ca2+ ATPase (SERCA) expression contributes to airway remodelling in bronchial asthma. Proc. Natl. Acad. Sci. 106, 10775–10780, Available from: https://www.pnas.org/content/pnas/106/26/10775.full.pdf 10.1073/pnas.0902295106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Audrit K.J., Delventhal L., Aydin Ö. and Nassenstein C. (2017) The nervous system of airways and its remodeling in inflammatory lung diseases. Cell Tissue Res. 367, 571–590 10.1007/s00441-016-2559-7 [DOI] [PubMed] [Google Scholar]
- 116.Kistemaker L.E.M. and Prakash Y.S. (2019) Airway innervation and plasticity in asthma. Physiology (Bethesda). 34, 283–298 10.1152/physiol.00050.2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Undem B.J. and Carr M.J. (2002) The role of nerves in asthma. Curr. Allergy Asthma Rep. 2, 159–165 10.1007/s11882-002-0011-4 [DOI] [PubMed] [Google Scholar]
- 118.Chapman D.G. and Irvin C.G. (2015) Mechanisms of airway hyper-responsiveness in asthma: the past, present and yet to come. Clin. Exp. Allergy: J. Br. Soc. Allergy Clin. Immunol. 45, 706–719 10.1111/cea.12506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Kolahian S. and Gosens R. (2012) Cholinergic regulation of airway inflammation and remodelling. J. Allergy 2012, 681258 10.1155/2012/681258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Chalermwatanachai T., Vilchez-Vargas R., Holtappels G., Lacoere T., Jáuregui R., Kerckhof F.-M.et al. (2018) Chronic rhinosinusitis with nasal polyps is characterized by dysbacteriosis of the nasal microbiota. Sci. Rep. 8, 7926 10.1038/s41598-018-26327-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Stevens W.W., Schleimer R.P. and Kern R.C. (2016) Chronic rhinosinusitis with nasal polyps. J. Allergy Clin. Immunol. Pract. 4, 565–572 10.1016/j.jaip.2016.04.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Flood-Page P., Menzies-Gow A., Phipps S., Ying S., Wangoo A., Ludwig M.S.et al. (2003) Anti-IL-5 treatment reduces deposition of ECM proteins in the bronchial subepithelial basement membrane of mild atopic asthmatics. J. Clin. Invest. 112, 1029–1036 10.1172/JCI17974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Busse W.W., Melen E. and Menzies-Gow A.N. (2022) Holy Grail: the journey towards disease modification in asthma. Eur. Respir. Rev. 31, 210183 10.1183/16000617.0183-2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Hou K., Wu Z.X., Chen X.Y., Wang J.Q., Zhang D., Xiao C.et al. (2022) Microbiota in health and diseases. Signal Transduct. Target Ther. 7, 135 10.1038/s41392-022-00974-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Turnbaugh P.J., Ridaura V.K., Faith J.J., Rey F.E., Knight R. and Gordon J.I. (2009) The effect of diet on the human gut microbiome: a metagenomic analysis in humanized gnotobiotic mice. Sci. Transl. Med. 1, 6ra14 10.1126/scitranslmed.3000322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Chotirmall S.H. and Burke C.M. (2015) Aging and the microbiome: implications for asthma in the elderly? Expert Rev. Respir. Med. 9, 125–128 10.1586/17476348.2015.1002473 [DOI] [PubMed] [Google Scholar]
- 127.Vandenborght L.E., Enaud R., Urien C., Coron N., Girodet P.O., Ferreira S.et al. (2021) Type 2-high asthma is associated with a specific indoor mycobiome and microbiome. J. Allergy Clin. Immunol. 147, 1296e6–1305e6 10.1016/j.jaci.2020.08.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Laulajainen-Hongisto A., Toppila-Salmi S.K., Luukkainen A. and Kern R. (2020) Airway epithelial dynamics in allergy and related chronic inflammatory airway diseases. Front Cell Dev Biol. 8, 204 10.3389/fcell.2020.00204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Liu Y., Teo S.M., Meric G., Tang H.H.F., Zhu Q., Sanders J.G.et al. (2023) The gut microbiome is a significant risk factor for future chronic lung disease. J. Allergy Clin. Immunol. 151, 943–952 10.1016/j.jaci.2022.12.810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Stiemsma L.T., Arrieta M.C., Dimitriu P.A., Cheng J., Thorson L., Lefebvre D.L.et al. (2016) Shifts in Lachnospira and Clostridium sp. in the 3-month stool microbiome are associated with preschool age asthma. Clin. Sci. (Lond.) 130, 2199–2207 10.1042/CS20160349 [DOI] [PubMed] [Google Scholar]
- 131.Lad N., Murphy A.M., Parenti C., Nelson C.P., Williams N.C., Sharpe G.R.et al. (2021) Asthma and obesity: endotoxin another insult to add to injury? Clin. Sci. (Lond.) 135, 2729–2748 10.1042/CS20210790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Watts A.M., West N.P., Zhang P., Smith P.K., Cripps A.W. and Cox A.J. (2021) The gut microbiome of adults with allergic rhinitis is characterised by reduced diversity and an altered abundance of key microbial taxa compared to controls. Int. Arch. Allergy Immunol. 182, 94–105 10.1159/000510536 [DOI] [PubMed] [Google Scholar]
- 133.Yamaguchi T., Nomura A., Matsubara A., Hisada T., Tamada Y., Mikami T.et al. (2023) Effect of gut microbial composition and diversity on major inhaled allergen sensitization and onset of allergic rhinitis. Allergol Int. 72, 135–142 10.1016/j.alit.2022.06.005 [DOI] [PubMed] [Google Scholar]
- 134.Kim Y.C., Won H.K., Lee J.W., Sohn K.H., Kim M.H., Kim T.B.et al. (2019) Staphylococcus aureus Nasal Colonization and Asthma in Adults: Systematic Review and Meta-Analysis. J. Allergy Clin. Immunol. Pract. 7, 606e9–615e9 10.1016/j.jaip.2018.08.020 [DOI] [PubMed] [Google Scholar]
- 135.Perez-Losada M., Castro-Nallar E., Laerte Boechat J., Delgado L., Azenha Rama T., Berrios-Farias V.et al. (2023) Nasal Bacteriomes of Patients with Asthma and Allergic Rhinitis Show Unique Composition, Structure, Function and Interactions. Microorganisms 11, 10.3390/microorganisms11030683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Torre E., Sola D., Caramaschi A., Mignone F., Bona E. and Fallarini S. (2022) A pilot study on clinical scores, immune cell modulation, and microbiota composition in allergic patients with rhinitis and asthma treated with a probiotic preparation. Int. Arch Allergy Immunol. 183, 186–200 10.1159/000518952 [DOI] [PubMed] [Google Scholar]
- 137.Svenningsen S. and Nair P. (2017) Asthma endotypes and an overview of targeted therapy for asthma. Front. Med. (Lausanne) 4, 158 10.3389/fmed.2017.00158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Nakayama T., Lee I.T., Le W., Tsunemi Y., Borchard N.A., Zarabanda D.et al. (2022) Inflammatory molecular endotypes of nasal polyps derived from White and Japanese populations. J. Allergy Clin. Immunol. 149, 1296e6–1308e6 10.1016/j.jaci.2021.11.017 [DOI] [PubMed] [Google Scholar]
- 139.ten Brinke A., Grootendorst D.C., Schmidt J.T., De Bruine F.T., van Buchem M.A.et al. (2002) Chronic sinusitis in severe asthma is related to sputum eosinophilia. J. Allergy Clin. Immunol. 109, 621–626 10.1067/mai.2002.122458 [DOI] [PubMed] [Google Scholar]
- 140.Pizzichini M.M., Popov T.A., Efthimiadis A., Hussack P., Evans S., Pizzichini E.et al. (1996) Spontaneous and induced sputum to measure indices of airway inflammation in asthma. Am. J. Respir. Crit. Care Med. 154, 866–869 10.1164/ajrccm.154.4.8887576 [DOI] [PubMed] [Google Scholar]
- 141.Berry M., Morgan A., Shaw D.E., Parker D., Green R., Brightling C.et al. (2007) Pathological features and inhaled corticosteroid response of eosinophilic and non-eosinophilic asthma. Thorax 62, 1043–1049 10.1136/thx.2006.073429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Durrington H.J., Gioan-Tavernier G.O., Maidstone R.J., Krakowiak K., Loudon A.S.I., Blaikley J.F.et al. (2018) Time of Day Affects Eosinophil Biomarkers in Asthma: Implications for Diagnosis and Treatment. Am. J. Respir. Crit. Care Med. 198, 1578–1581 10.1164/rccm.201807-1289LE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Petsky H.L., Cates C.J., Lasserson T.J., Li A.M., Turner C., Kynaston J.A.et al. (2012) A systematic review and meta-analysis: tailoring asthma treatment on eosinophilic markers (exhaled nitric oxide or sputum eosinophils). Thorax 67, 199–208 10.1136/thx.2010.135574 [DOI] [PubMed] [Google Scholar]
- 144.Korevaar D.A., Westerhof G.A., Wang J., Cohen J.F., Spijker R., Sterk P.J.et al. (2015) Diagnostic accuracy of minimally invasive markers for detection of airway eosinophilia in asthma: a systematic review and meta-analysis. Lancet Respir. Med. 3, 290–300 10.1016/S2213-2600(15)00050-8 [DOI] [PubMed] [Google Scholar]
- 145.Kostikas K., Zervas E. and Gaga M. (2014) Airway and systemic eosinophilia in asthma: does site matter? Eur. Respir. J. 44, 14–16 10.1183/09031936.00034514 [DOI] [PubMed] [Google Scholar]
- 146.Spector S.L. and Tan R.A. (2012) Is a single blood eosinophil count a reliable marker for “eosinophilic asthma?” J. Asthma 49, 807–810 10.3109/02770903.2012.713428 [DOI] [PubMed] [Google Scholar]
- 147.Tran T.N., Khatry D.B., Ke X., Ward C.K. and Gossage D. (2014) High blood eosinophil count is associated with more frequent asthma attacks in asthma patients. Ann. Allergy Asthma Immunol. 113, 19–24 10.1016/j.anai.2014.04.011 [DOI] [PubMed] [Google Scholar]
- 148.Chiappori A., De Ferrari L., Folli C., Mauri P., Riccio A.M. and Canonica G.W. (2015) Biomarkers and severe asthma: a critical appraisal. Clin. Mol. Allergy 13, 20 10.1186/s12948-015-0027-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Dweik R.A., Sorkness R.L., Wenzel S., Hammel J., Curran-Everett D., Comhair S.A.et al. (2010) Use of exhaled nitric oxide measurement to identify a reactive, at-risk phenotype among patients with asthma. Am. J. Respir. Crit. Care Med. 181, 1033–1041 10.1164/rccm.200905-0695OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Pavord I.D., Afzalnia S., Menzies-Gow A. and Heaney L.G. (2017) The current and future role of biomarkers in type 2 cytokine-mediated asthma management. Clin. Exp. Allergy 47, 148–160 10.1111/cea.12881 [DOI] [PubMed] [Google Scholar]
- 151.Dweik R.A., Boggs P.B., Erzurum S.C., Irvin C.G., Leigh M.W., Lundberg J.O.et al. (2011) An official ATS clinical practice guideline: interpretation of exhaled nitric oxide levels (FENO) for clinical applications. Am. J. Respir. Crit. Care Med. 184, 602–615 10.1164/rccm.9120-11ST [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Kostikas K., Minas M., Papaioannou A.I., Papiris S. and Dweik R.A. (2011) Exhaled nitric oxide in asthma in adults: the end is the beginning? Curr. Med. Chem. 18, 1423–1431 10.2174/092986711795328436 [DOI] [PubMed] [Google Scholar]
- 153.de Vries R., Dagelet Y.W.F., Spoor P., Snoey E., Jak P.M.C., Brinkman P.et al. (2018) Clinical and inflammatory phenotyping by breathomics in chronic airway diseases irrespective of the diagnostic label. Eur. Respir. J. 51, 10.1183/13993003.01817-2017 [DOI] [PubMed] [Google Scholar]
- 154.Fens N., van der Sluijs K.F., van de Pol M.A., Dijkhuis A., Smids B.S., van der Zee J.S.et al. (2015) Electronic nose identifies bronchoalveolar lavage fluid eosinophils in asthma. Am. J. Respir. Crit. Care Med. 191, 1086–1088 10.1164/rccm.201411-2010LE [DOI] [PubMed] [Google Scholar]
- 155.Fontanella S., Frainay C., Murray C.S., Simpson A. and Custovic A. (2018) Machine learning to identify pairwise interactions between specific IgE antibodies and their association with asthma: A cross-sectional analysis within a population-based birth cohort. PLoS Med. 15, e1002691 10.1371/journal.pmed.1002691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Sehra S., Yao W., Nguyen E.T., Ahyi A.N., Tuana F.M., Ahlfeld S.K.et al. (2011) Periostin regulates goblet cell metaplasia in a model of allergic airway inflammation. J. Immunol. 186, 4959–4966 10.4049/jimmunol.1002359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Blanchard C., Mingler M.K., McBride M., Putnam P.E., Collins M.H., Chang G.et al. (2008) Periostin facilitates eosinophil tissue infiltration in allergic lung and esophageal responses. Mucosal. Immunol. 1, 289–296 10.1038/mi.2008.15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Matsumoto H. (2014) Serum periostin: a novel biomarker for asthma management. Allergol Int. 63, 153–160 10.2332/allergolint.13-RAI-0678 [DOI] [PubMed] [Google Scholar]
- 159.Takahashi K., Meguro K., Kawashima H., Kashiwakuma D., Kagami S.I., Ohta S.et al. (2019) Serum periostin levels serve as a biomarker for both eosinophilic airway inflammation and fixed airflow limitation in well-controlled asthmatics. J. Asthma 56, 236–243 10.1080/02770903.2018.1455855 [DOI] [PubMed] [Google Scholar]
- 160.Wan X.C. and Woodruff P.G. (2016) Biomarkers in severe asthma. Immunol. Allergy Clin. North Am. 36, 547–557 10.1016/j.iac.2016.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Carr T.F. and Kraft M. (2018) Use of biomarkers to identify phenotypes and endotypes of severeasthma. Ann. Allergy Asthma Immunol. 121, 414–420 10.1016/j.anai.2018.07.029 [DOI] [PubMed] [Google Scholar]
- 162.Tiotiu A. (2018) Biomarkers in asthma: state of the art. Asthma Res. Pract. 4, 10 10.1186/s40733-018-0047-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.An J., Lee J.H., Sim J.H., Song W.J., Kwon H.S., Cho Y.S.et al. (2020) Serum eosinophil-derived neurotoxin better reflect asthma control status than blood eosinophil counts. J. Allergy Clin. Immunol. Pract. 8, 2681e1–2688e1 10.1016/j.jaip.2020.03.035 [DOI] [PubMed] [Google Scholar]
- 164.Kim C.K., Callaway Z., Fletcher R. and Koh Y.Y. (2010) Eosinophil-derived neurotoxin in childhood asthma: correlation with disease severity. J. Asthma 47, 568–573 10.3109/02770901003792833 [DOI] [PubMed] [Google Scholar]
- 165.Tsuda T., Maeda Y., Nishide M., Koyama S., Hayama Y., Nojima S.et al. (2019) Eosinophil-derived neurotoxin enhances airway remodeling in eosinophilic chronic rhinosinusitis and correlates with disease severity. Int. Immunol. 31, 33–40 10.1093/intimm/dxy061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Lee Y., Lee J.H., Yang E.M., Kwon E., Jung C.G., Kim S.C.et al. (2019) Serum levels of eosinophil-derived neurotoxin: a biomarker for asthma severity in adult asthmatics. Allergy Asthma Immunol. Res. 11, 394–405 10.4168/aair.2019.11.3.394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Woo S.D., Luu Q.Q. and Park H.S. (2020) NSAID-exacerbated respiratory disease (NERD): from pathogenesis to improved care. Front. Pharmacol. 11, 1147 10.3389/fphar.2020.01147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Daffern P.J., Muilenburg D., Hugli T.E. and Stevenson D.D. (1999) Association of urinary leukotriene E4 excretion during aspirin challenges with severity of respiratory responses. J. Allergy Clin. Immunol. 104, 559–564 10.1016/S0091-6749(99)70324-6 [DOI] [PubMed] [Google Scholar]
- 169.Park H., Choi Y., Jung C.G. and Park H.S. (2017) Potential biomarkers for NSAID-exacerbated respiratory disease. Mediators Inflamm. 2017, 8160148 10.1155/2017/8160148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Choby G., Low C.M., Levy J.M., Stokken J.K., Pinheiro-Neto C., Bartemes K.et al. (2022) Urine leukotriene E4: implications as a biomarker in chronic rhinosinusitis. Otolaryngol. Head Neck Surg. 166, 224–232 10.1177/01945998211011060 [DOI] [PubMed] [Google Scholar]
- 171.Pham D.L., Ban G.Y., Kim S.H., Shin Y.S., Ye Y.M., Chwae Y.J.et al. (2017) Neutrophil autophagy and extracellular DNA traps contribute to airway inflammation in severe asthma. Clin. Exp. Allergy 47, 57–70 10.1111/cea.12859 [DOI] [PubMed] [Google Scholar]
- 172.Decaesteker T., Seys S., Hox V., Dilissen E., Marijsse G., Manhaeghe L.et al. (2017) Serum and sputum calprotectin, a reflection of neutrophilic airway inflammation in asthmatics after high-altitude exposure. Clin. Exp. Allergy 47, 1675–1677 10.1111/cea.13043 [DOI] [PubMed] [Google Scholar]
- 173.Hur G.Y., Ye Y.M., Yang E. and Park H.S. (2020) Serum potential biomarkers according to sputum inflammatory cell profiles in adult asthmatics. Korean J. Intern. Med. 35, 988–997 10.3904/kjim.2019.083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Agache I., Ciobanu C., Agache C. and Anghel M. (2010) Increased serum IL-17 is an independent risk factor for severe asthma. Respir. Med. 104, 1131–1137 10.1016/j.rmed.2010.02.018 [DOI] [PubMed] [Google Scholar]
- 175.Norzila M.Z., Fakes K., Henry R.L., Simpson J. and Gibson P.G. (2000) Interleukin-8 secretion and neutrophil recruitment accompanies induced sputum eosinophil activation in children with acute asthma. Am. J. Respir. Crit. Care Med. 161, 769–774 10.1164/ajrccm.161.3.9809071 [DOI] [PubMed] [Google Scholar]
- 176.Silvestri M., Bontempelli M., Giacomelli M., Malerba M., Rossi G.A., Di Stefano A.et al. (2006) High serum levels of tumour necrosis factor-alpha and interleukin-8 in severe asthma: markers of systemic inflammation? Clin. Exp. Allergy 36, 1373–1381 10.1111/j.1365-2222.2006.02502.x [DOI] [PubMed] [Google Scholar]
- 177.Berry M.A., Hargadon B., Shelley M., Parker D., Shaw D.E., Green R.H.et al. (2006) Evidence of a role of tumor necrosis factor alpha in refractory asthma. N. Engl. J. Med. 354, 697–708 10.1056/NEJMoa050580 [DOI] [PubMed] [Google Scholar]
- 178.Manni M.L., Trudeau J.B., Scheller E.V., Mandalapu S., Elloso M.M., Kolls J.K.et al. (2014) The complex relationship between inflammation and lung function in severe asthma. Mucosal Immunol. 7, 1186–1198 10.1038/mi.2014.8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Yang Y., Jia M., Ou Y., Adcock I.M. and Yao X. (2020) Airway epithelial cell damage in asthma: mechanisms and biomarkers [DOI] [PubMed] [Google Scholar]
- 180.Busse W., Corren J., Lanier B.Q., McAlary M., Fowler-Taylor A., Cioppa G.D.et al. (2001) Omalizumab, anti-IgE recombinant humanized monoclonal antibody, for the treatment of severe allergic asthma. J. Allergy Clin. Immunol. 108, 184–190 10.1067/mai.2001.117880 [DOI] [PubMed] [Google Scholar]
- 181.Djukanovic R., Wilson S.J., Kraft M., Jarjour N.N., Steel M., Chung K.F.et al. (2004) Effects of treatment with anti-immunoglobulin E antibody omalizumab on airway inflammation in allergic asthma. Am. J. Respir. Crit. Care Med. 170, 583–593 10.1164/rccm.200312-1651OC [DOI] [PubMed] [Google Scholar]
- 182.Wu Q., Yuan L., Qiu H., Wang X., Huang X., Zheng R.et al. (2021) Efficacy and safety of omalizumab in chronic rhinosinusitis with nasal polyps: a systematic review and meta-analysis of randomised controlled trials. BMJ Open 11, e047344 10.1136/bmjopen-2020-047344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Trischler J., Bottoli I., Janocha R., Heusser C., Jaumont X., Lowe P.et al. (2021) Ligelizumab treatment for severe asthma: learnings from the clinical development programme. Clin. Transl. Immunol. 10, e1255 10.1002/cti2.1255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Harris J.M., Maciuca R., Bradley M.S., Cabanski C.R., Scheerens H., Lim J.et al. (2016) A randomized trial of the efficacy and safety of quilizumab in adults with inadequately controlled allergic asthma. Respir. Res. 17, 29 10.1186/s12931-016-0347-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Harris J.M., Cabanski C.R., Scheerens H., Samineni D., Bradley M.S., Cochran C.et al. (2016) A randomized trial of quilizumab in adults with refractory chronic spontaneous urticaria. J. Allergy Clin. Immunol. 138, 1730–1732 10.1016/j.jaci.2016.06.023 [DOI] [PubMed] [Google Scholar]
- 186.Cohen E.S., Dobson C.L., Kack H., Wang B., Sims D.A., Lloyd C.O.et al. (2014) A novel IgE-neutralizing antibody for the treatment of severe uncontrolled asthma. MAbs 6, 756–764 10.4161/mabs.28394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Sheldon E., Schwickart M., Li J., Kim K., Crouch S., Parveen S.et al. (2016) Pharmacokinetics, Pharmacodynamics, and Safety of MEDI4212, an Anti-IgE Monoclonal Antibody, in Subjects with Atopy: A Phase I Study. Adv. Ther. 33, 225–251 10.1007/s12325-016-0287-8 [DOI] [PubMed] [Google Scholar]
- 188.Gour N. and Wills-Karp M. (2015) IL-4 and IL-13 signaling in allergic airway disease. Cytokine 75, 68–78 10.1016/j.cyto.2015.05.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Kau A.L. and Korenblat P.E. (2014) Anti-interleukin 4 and 13 for asthma treatment in the era of endotypes. Curr. Opin. Allergy Clin. Immunol. 14, 570–575 10.1097/ACI.0000000000000108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Hashimoto S., Gon Y., Takeshita I., Maruoka S. and Horie T. (2001) IL-4 and IL-13 induce myofibroblastic phenotype of human lung fibroblasts through c-Jun NH2-terminal kinase-dependent pathway. J. Allergy Clin. Immunol. 107, 1001–1008 10.1067/mai.2001.114702 [DOI] [PubMed] [Google Scholar]
- 191.Moynihan B.J., Tolloczko B., Bassam S.E., Ferraro P., Michoud M.-C., Martin J.G.et al. (2008) IFN-γ, IL-4 and IL-13 modulate responsiveness of human airway smooth muscle cells to IL-13. Respir. Res. 9, 84 10.1186/1465-9921-9-84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Le Floc'h A., Allinne J., Nagashima K., Scott G., Birchard D., Asrat S.et al. (2020) Dual blockade of IL-4 and IL-13 with dupilumab, an IL-4Rα antibody, is required to broadly inhibit type 2 inflammation. Allergy 75, 1188–1204 10.1111/all.14151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Rabe K.F., Nair P., Brusselle G., Maspero J.F., Castro M., Sher L.et al. (2018) Efficacy and safety of dupilumab in glucocorticoid-dependent severe asthma. N. Engl. J. Med. 378, 2475–2485 10.1056/NEJMoa1804093 [DOI] [PubMed] [Google Scholar]
- 194.Corren J., Castro M., O'Riordan T., Hanania N.A., Pavord I.D., Quirce S.et al. (2020) Dupilumab efficacy in patients with uncontrolled, moderate-to-severe allergic asthma. J. Allergy Clin. Immunol. Pract. 8, 516–526 10.1016/j.jaip.2019.08.050 [DOI] [PubMed] [Google Scholar]
- 195.Brusselle G.G. and Koppelman G.H. (2022) Biologic therapies for severe asthma. N. Engl. J. Med. 386, 157–171 10.1056/NEJMra2032506 [DOI] [PubMed] [Google Scholar]
- 196.Castro M., Corren J., Pavord I.D., Maspero J., Wenzel S., Rabe K.F.et al. (2018) Dupilumab efficacy and safety in moderate-to-severe uncontrolled asthma. N. Engl. J. Med. 378, 2486–2496 10.1056/NEJMoa1804092 [DOI] [PubMed] [Google Scholar]
- 197.Wenzel S., Castro M., Corren J., Maspero J., Wang L., Zhang B.et al. (2016) Dupilumab efficacy and safety in adults with uncontrolled persistent asthma despite use of medium-to-high-dose inhaled corticosteroids plus a long-acting beta2 agonist: a randomised double-blind placebo-controlled pivotal phase 2b dose-ranging trial. Lancet 388, 31–44 10.1016/S0140-6736(16)30307-5 [DOI] [PubMed] [Google Scholar]
- 198.Rabe K.F., Nair P., Brusselle G., Maspero J.F., Castro M., Sher L.et al. (2018) Efficacy and safety of dupilumab in glucocorticoid-dependent severe asthma. N. Engl. J. Med. 378, 2475–2485 10.1056/NEJMoa1804093 [DOI] [PubMed] [Google Scholar]
- 199.Laidlaw T.M., Bachert C., Amin N., Desrosiers M., Hellings P.W., Mullol J.et al. (2021) Dupilumab improves upper and lower airway disease control in chronic rhinosinusitis with nasal polyps and asthma. Ann. Allergy Asthma Immunol. 126, 584e1–592e1 10.1016/j.anai.2021.01.012 [DOI] [PubMed] [Google Scholar]
- 200.Bacharier L.B., Maspero J.F., Katelaris C.H., Fiocchi A.G., Gagnon R., de Mir I.et al. (2021) Dupilumab in children with uncontrolled moderate-to-severe asthma. N. Engl. J. Med. 385, 2230–2240 10.1056/NEJMoa2106567 [DOI] [PubMed] [Google Scholar]
- 201.Paller A.S., Simpson E.L., Siegfried E.C., Cork M.J., Wollenberg A., Arkwright P.D.et al. (2022) Dupilumab in children aged 6 months to younger than 6 years with uncontrolled atopic dermatitis: a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 400, 908–919 10.1016/S0140-6736(22)01539-2 [DOI] [PubMed] [Google Scholar]
- 202.Aceves S.S., Dellon E.S., Greenhawt M., Hirano I., Liacouras C.A. and Spergel J.M. (2022) Clinical guidance for the use of dupilumab in eosinophilic esophagitis: a yardstick. Ann. Allergy Asthma Immunol. 3, 371–378, 10.1016/j.anai.2022.12.014 [DOI] [PubMed] [Google Scholar]
- 203.Slager R.E., Otulana B.A., Hawkins G.A., Yen Y.P., Peters S.P., Wenzel S.E.et al. (2012) IL-4 receptor polymorphisms predict reduction in asthma exacerbations during response to an anti-IL-4 receptor alpha antagonist. J. Allergy Clin. Immunol. 130, 516e4–522e4 10.1016/j.jaci.2012.03.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Corren J., Lemanske R.F., Hanania N.A., Korenblat P.E., Parsey M.V., Arron J.R.et al. (2011) Lebrikizumab treatment in adults with asthma. N. Engl. J. Med. 365, 1088–1098 10.1056/NEJMoa1106469 [DOI] [PubMed] [Google Scholar]
- 205.Hanania N.A., Korenblat P., Chapman K.R., Bateman E.D., Kopecky P., Paggiaro P.et al. (2016) Efficacy and safety of lebrikizumab in patients with uncontrolled asthma (LAVOLTA I and LAVOLTA II): replicate, phase 3, randomised, double-blind, placebo-controlled trials. Lancet Respiratory Med. 4, 781–796 10.1016/S2213-2600(16)30265-X [DOI] [PubMed] [Google Scholar]
- 206.Busse W.W., Brusselle G.G., Korn S., Kuna P., Magnan A., Cohen D.et al. (2019) Tralokinumab did not demonstrate oral corticosteroid-sparing effects in severe asthma. Eur. Respir. J. 53, 1800948, Available from: https://erj.ersjournals.com/content/erj/53/2/1800948.full.pdf 10.1183/13993003.00948-2018 [DOI] [PubMed] [Google Scholar]
- 207.Panettieri R.A. Jr., Sjöbring U., Péterffy A., Wessman P., Bowen K.et al. (2018) Tralokinumab for severe, uncontrolled asthma (STRATOS 1 and STRATOS 2): two randomised, double-blind, placebo-controlled, phase 3 clinical trials. Lancet Respiratory Med. 6, 511–525 10.1016/S2213-2600(18)30184-X [DOI] [PubMed] [Google Scholar]
- 208.Yalcin A.D., Onbasi K., Uzun R., Herth F. and Schnabel P.A. (2020) Human(ized) monoclonal antibodies in atopic patients - state of the art. Cent Eur. J. Immunol. 45, 195–201 10.5114/ceji.2020.97909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Bagnasco D., Ferrando M., Varricchi G., Passalacqua G. and Canonica G.W. (2016) A critical evaluation of Anti-IL-13 and Anti-IL-4 strategies in severe asthma. Int. Archives Allergy Immunol. 170, 122–131 10.1159/000447692 [DOI] [PubMed] [Google Scholar]
- 210.Chaker A.M., Shamji M.H., Dumitru F.A., Calderon M.A., Scadding G.W., Makatsori M.et al. (2016) Short-term subcutaneous grass pollen immunotherapy under the umbrella of anti-IL-4: A randomized controlled trial. J. Allergy Clin. Immunol. 137, 452e9–461e9 10.1016/j.jaci.2015.08.046 [DOI] [PubMed] [Google Scholar]
- 211.Corren J., Busse W., Meltzer E.O., Mansfield L., Bensch G., Fahrenholz J.et al. (2010) A randomized, controlled, phase 2 study of AMG 317, an IL-4Ralpha antagonist, in patients with asthma. Am. J. Respir. Crit. Care Med. 181, 788–796 10.1164/rccm.200909-1448OC [DOI] [PubMed] [Google Scholar]
- 212.Borish L.C., Nelson H.S., Lanz M.J., Claussen L., Whitmore J.B., Agosti J.M.et al. (1999) Interleukin-4 receptor in moderate atopic asthma. A phase I/II randomized, placebo-controlled trial. Am. J. Respir. Crit. Care Med. 160, 1816–1823 10.1164/ajrccm.160.6.9808146 [DOI] [PubMed] [Google Scholar]
- 213.Drick N., Seeliger B., Welte T., Fuge J. and Suhling H. (2018) Anti-IL-5 therapy in patients with severe eosinophilic asthma – clinical efficacy and possible criteria for treatment response. BMC Pulmonary Med. 18, 119 10.1186/s12890-018-0689-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Bel E.H., Wenzel S.E., Thompson P.J., Prazma C.M., Keene O.N., Yancey S.W.et al. (2014) Oral glucocorticoid-sparing effect of mepolizumab in eosinophilic asthma. N. Engl. J. Med. 371, 1189–1197 10.1056/NEJMoa1403291 [DOI] [PubMed] [Google Scholar]
- 215.Nair P., Wenzel S., Rabe K.F., Bourdin A., Lugogo N.L., Kuna P.et al. (2017) Oral glucocorticoid-sparing effect of benralizumab in severe asthma. N. Engl. J. Med. 376, 2448–2458 10.1056/NEJMoa1703501 [DOI] [PubMed] [Google Scholar]
- 216.Pavord I.D., Korn S., Howarth P., Bleecker E.R., Buhl R., Keene O.N.et al. (2012) Mepolizumab for severe eosinophilic asthma (DREAM): a multicentre, double-blind, placebo-controlled trial. Lancet 380, 651–659 10.1016/S0140-6736(12)60988-X [DOI] [PubMed] [Google Scholar]
- 217.Lugogo N., Domingo C., Chanez P., Leigh R., Gilson M.J., Price R.G.et al. (2016) Long-term efficacy and safety of mepolizumab in patients with severe eosinophilic asthma: a multi-center, open-label, Phase IIIb study. Clin. Ther. 38, 2058.e1–2070.e1 10.1016/j.clinthera.2016.07.010 [DOI] [PubMed] [Google Scholar]
- 218.Caminati M., Cegolon L., Vianello A., Chieco Bianchi F., Festi G., Marchi M.R.et al. (2019) Mepolizumab for severe eosinophilic asthma: a real-world snapshot on clinical markers and timing of response. Expert Rev. Respiratory Med. 13, 1205–1212 10.1080/17476348.2019.1676734 [DOI] [PubMed] [Google Scholar]
- 219.Wechsler M.E., Akuthota P., Jayne D., Khoury P., Klion A., Langford C.A.et al. (2017) Mepolizumab or placebo for eosinophilic granulomatosis with polyangiitis. N. Engl. J. Med. 376, 1921–1932 10.1056/NEJMoa1702079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Rothenberg M.E., Roufosse F., Faguer S., Gleich G.J., Steinfeld J., Yancey S.W.et al. (2022) Mepolizumab reduces hypereosinophilic syndrome flares irrespective of blood eosinophil count and interleukin-5. J. Allergy Clin. Immunol. Pract. 10, 2367e3–2374e3 10.1016/j.jaip.2022.04.037 [DOI] [PubMed] [Google Scholar]
- 221.Fokkens W.J., Mullol J., Kennedy D., Philpott C., Seccia V., Kern R.C.et al. (2022) Mepolizumab for chronic rhinosinusitis with nasal polyps (SYNAPSE): In-depth sinus surgery analysis. Allergy 78, 812–821 10.1111/all.15434 [DOI] [PubMed] [Google Scholar]
- 222.Bachert C., Sousa A.R., Lund V.J., Scadding G.K., Gevaert P., Nasser S.et al. (2017) Reduced need for surgery in severe nasal polyposis with mepolizumab: Randomized trial. J. Allergy Clin. Immunol. 140, 1024e14–1031e14 10.1016/j.jaci.2017.05.044 [DOI] [PubMed] [Google Scholar]
- 223.Ortega H.G., Liu M.C., Pavord I.D., Brusselle G.G., FitzGerald J.M., Chetta A.et al. (2014) Mepolizumab treatment in patients with severe eosinophilic asthma. N. Engl. J. Med. 371, 1198–1207 10.1056/NEJMoa1403290 [DOI] [PubMed] [Google Scholar]
- 224.Castro M., Zangrilli J., Wechsler M.E., Bateman E.D., Brusselle G.G., Bardin P.et al. (2015) Reslizumab for inadequately controlled asthma with elevated blood eosinophil counts: results from two multicentre, parallel, double-blind, randomised, placebo-controlled, phase 3 trials. Lancet Respiratory Med. 3, 355–366 10.1016/S2213-2600(15)00042-9 [DOI] [PubMed] [Google Scholar]
- 225.Wechsler M.E., Peters S.P., Hill T.D., Ariely R., DePietro M.R., Driessen M.T.et al. (2021) Clinical outcomes and health-care resource use associated with reslizumab treatment in adults with severe eosinophilic asthma in real-world practice. Chest 159, 1734–1746 10.1016/j.chest.2020.11.060 [DOI] [PubMed] [Google Scholar]
- 226.Gevaert P., Lang-Loidolt D., Lackner A., Stammberger H., Staudinger H., Van Zele T.et al. (2006) Nasal IL-5 levels determine the response to anti-IL-5 treatment in patients with nasal polyps. J. Allergy Clin. Immunol. 118, 1133–1141 10.1016/j.jaci.2006.05.031 [DOI] [PubMed] [Google Scholar]
- 227.Canonica G.W., Harrison T.W., Chanez P., Menzella F., Louis R., Cosio B.G.et al. (2022) Benralizumab improves symptoms of patients with severe, eosinophilic asthma with a diagnosis of nasal polyposis. Allergy 77, 150–161 10.1111/all.14902 [DOI] [PubMed] [Google Scholar]
- 228.Kavanagh J.E., Hearn A.P., Dhariwal J., d'Ancona G., Douiri A., Roxas C.et al. (2021) Real-world effectiveness of benralizumab in severe eosinophilic asthma. Chest 159, 496–506 10.1016/j.chest.2020.08.2083 [DOI] [PubMed] [Google Scholar]
- 229.Bachert C., Han J.K., Desrosiers M.Y., Gevaert P., Heffler E., Hopkins C.et al. (2022) Efficacy and safety of benralizumab in chronic rhinosinusitis with nasal polyps: A randomized, placebo-controlled trial. J. Allergy Clin. Immunol. 149, 1309e12–1317e12 10.1016/j.jaci.2021.08.030 [DOI] [PubMed] [Google Scholar]
- 230.Hong H., Liao S., Chen F., Yang Q. and Wang D.Y. (2020) Role of IL-25, IL-33, and TSLP in triggering united airway diseases toward type 2 inflammation. Allergy 75, 2794–2804 10.1111/all.14526 [DOI] [PubMed] [Google Scholar]
- 231.Soumelis V. and Liu Y.J. (2020) The discovery of human TSLP as a critical epithelial cytokine in type 2 immunity and allergic disease. Nat. Immunol. 21, 1471–1473 10.1038/s41590-020-0720-7 [DOI] [PubMed] [Google Scholar]
- 232.Mullard A. (2022) FDA approves first-in-class TSLP-targeted antibody for severe asthma. Nat. Rev. Drug Discov. 21, 89 10.1038/d41573-022-00013-5 [DOI] [PubMed] [Google Scholar]
- 233.Emson C., Diver S., Chachi L., Megally A., Small C., Downie J.et al. (2020) CASCADE: a phase 2, randomized, double-blind, placebo-controlled, parallel-group trial to evaluate the effect of tezepelumab on airway inflammation in patients with uncontrolled asthma. Respir. Res. 21, 265 10.1186/s12931-020-01513-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Diver S., Khalfaoui L., Emson C., Wenzel S.E., Menzies-Gow A., Wechsler M.E.et al. (2021) Effect of tezepelumab on airway inflammatory cells, remodelling, and hyperresponsiveness in patients with moderate-to-severe uncontrolled asthma (CASCADE): a double-blind, randomised, placebo-controlled, phase 2 trial. Lancet Respir. Med. 9, 1299–1312 10.1016/S2213-2600(21)00226-5 [DOI] [PubMed] [Google Scholar]
- 235.Menzies-Gow A., Corren J., Bourdin A., Chupp G., Israel E., Wechsler M.E.et al. (2021) Tezepelumab in adults and adolescents with severe, uncontrolled asthma. N. Engl. J. Med. 384, 1800–1809 10.1056/NEJMoa2034975 [DOI] [PubMed] [Google Scholar]
- 236.Wechsler M.E., Menzies-Gow A., Brightling C.E., Kuna P., Korn S., Welte T.et al. (2022) Evaluation of the oral corticosteroid-sparing effect of tezepelumab in adults with oral corticosteroid-dependent asthma (SOURCE): a randomised, placebo-controlled, phase 3 study. Lancet Respir. Med. 10, 650–660 10.1016/S2213-2600(21)00537-3 [DOI] [PubMed] [Google Scholar]
- 237.Numazaki M., Abe M., Hanaoka K., Imamura E., Maeda M., Kimura A.et al. (2022) ASP7266, a novel antibody against human thymic stromal lymphopoietin receptor for the treatment of allergic diseases. J. Pharmacol. Exp. Ther. 380, 26–33 10.1124/jpet.121.000686 [DOI] [PubMed] [Google Scholar]
- 238.Borish L. and Steinke J.W. (2011) Interleukin-33 in asthma: how big of a role does it play? Curr. Allergy Asthma Rep. 11, 7–11 10.1007/s11882-010-0153-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Wechsler M.E., Ruddy M.K., Pavord I.D., Israel E., Rabe K.F., Ford L.B.et al. (2021) Efficacy and safety of itepekimab in patients with moderate-to-severe asthma. N. Engl. J. Med. 385, 1656–1668 10.1056/NEJMoa2024257 [DOI] [PubMed] [Google Scholar]
- 240.Oh C.K., Leigh R., McLaurin K.K., Kim K., Hultquist M. and Molfino N.A. (2013) A randomized, controlled trial to evaluate the effect of an anti-interleukin-9 monoclonal antibody in adults with uncontrolled asthma. Respir. Res. 14, 93 10.1186/1465-9921-14-93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Bateman E.D., Guerreros A.G., Brockhaus F., Holzhauer B., Pethe A., Kay R.A.et al. (2017) Fevipiprant, an oral prostaglandin DP2 receptor (CRTh2) antagonist, in allergic asthma uncontrolled on low-dose inhaled corticosteroids. Eur. Respir. J. 50, 1700670 10.1183/13993003.00670-2017 [DOI] [PubMed] [Google Scholar]
- 242.Brightling C.E., Gaga M., Inoue H., Li J., Maspero J., Wenzel S.et al. (2021) Effectiveness of fevipiprant in reducing exacerbations in patients with severe asthma (LUSTER-1 and LUSTER-2): two phase 3 randomised controlled trials. Lancet Respir. Med. 9, 43–56 10.1016/S2213-2600(20)30412-4 [DOI] [PubMed] [Google Scholar]
- 243.Gevaert P., Bachert C., Maspero J.F., Cuevas M., Steele D., Acharya S.et al. (2022) Phase 3b randomized controlled trial of fevipiprant in patients with nasal polyposis with asthma (THUNDER). J. Allergy Clin. Immunol. 10.1016/j.jaci.2021.12.759 [DOI] [PubMed] [Google Scholar]
- 244.Singh D., Cadden P., Hunter M., Pearce Collins L., Perkins M., Pettipher R.et al. (2013) Inhibition of the asthmatic allergen challenge response by the CRTH2 antagonist OC000459. Eur. Respir. J. 41, 46–52 10.1183/09031936.00092111 [DOI] [PubMed] [Google Scholar]
- 245.Diamant Z., Sidharta P.N., Singh D., O'Connor B.J., Zuiker R., Leaker B.R.et al. (2014) Setipiprant, a selective CRTH2 antagonist, reduces allergen-induced airway responses in allergic asthmatics. Clin. Exp. Allergy 44, 1044–1052 10.1111/cea.12357 [DOI] [PubMed] [Google Scholar]
- 246.Ratner P., Andrews C.P., Hampel F.C., Martin B., Mohar D.E., Bourrelly D.et al. (2017) Efficacy and safety of setipiprant in seasonal allergic rhinitis: results from Phase 2 and Phase 3 randomized, double-blind, placebo- and active-referenced studies. Allergy Asthma Clin. Immunol. 13, 18 10.1186/s13223-017-0183-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Neighbour H., Boulet L.P., Lemiere C., Sehmi R., Leigh R., Sousa A.R.et al. (2014) Safety and efficacy of an oral CCR3 antagonist in patients with asthma and eosinophilic bronchitis: a randomized, placebo-controlled clinical trial. Clin. Exp. Allergy 44, 508–516 10.1111/cea.12244 [DOI] [PubMed] [Google Scholar]
- 248.Kabashima K., Matsumura T., Komazaki H., Kawashima M. and Nemolizumab J.P.S.G. (2020) Trial of nemolizumab and topical agents for atopic dermatitis with pruritus. N. Engl. J. Med. 383, 141–150 10.1056/NEJMoa1917006 [DOI] [PubMed] [Google Scholar]
- 249.Sidbury R., Alpizar S., Laquer V., Dhawan S., Abramovits W., Loprete L.et al. (2022) Pharmacokinetics, safety, efficacy, and biomarker profiles during nemolizumab treatment of atopic dermatitis in adolescents. Dermatol. Ther. (Heidelb) 12, 631–642 10.1007/s13555-021-00678-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Altrichter S., Staubach P., Pasha M., Singh B., Chang A.T., Bernstein J.A.et al. (2022) An open-label, proof-of-concept study of lirentelimab for antihistamine-resistant chronic spontaneous and inducible urticaria. J. Allergy Clin. Immunol. 149, 1683e7–1690e7 10.1016/j.jaci.2021.12.772 [DOI] [PubMed] [Google Scholar]
- 251.O'Byrne P.M., Metev H., Puu M., Richter K., Keen C., Uddin M.et al. (2016) Efficacy and safety of a CXCR2 antagonist, AZD5069, in patients with uncontrolled persistent asthma: a randomised, double-blind, placebo-controlled trial. Lancet Respir. Med. 4, 797–806 10.1016/S2213-2600(16)30227-2 [DOI] [PubMed] [Google Scholar]
- 252.Watz H., Uddin M., Pedersen F., Kirsten A., Goldmann T., Stellmacher F.et al. (2017) Effects of the CXCR2 antagonist AZD5069 on lung neutrophil recruitment in asthma. Pulm. Pharmacol. Ther. 45, 121–123 10.1016/j.pupt.2017.05.012 [DOI] [PubMed] [Google Scholar]
- 253.Nair P., Gaga M., Zervas E., Alagha K., Hargreave F.E., O'Byrne P.M.et al. (2012) Safety and efficacy of a CXCR2 antagonist in patients with severe asthma and sputum neutrophils: a randomized, placebo-controlled clinical trial. Clin. Exp. Allergy 42, 1097–1103 10.1111/j.1365-2222.2012.04014.x [DOI] [PubMed] [Google Scholar]
- 254.Busse W.W., Holgate S., Kerwin E., Chon Y., Feng J., Lin J.et al. (2013) Randomized, double-blind, placebo-controlled study of brodalumab, a human anti-IL-17 receptor monoclonal antibody, in moderate to severe asthma. Am. J. Respir. Crit. Care Med. 188, 1294–1302 10.1164/rccm.201212-2318OC [DOI] [PubMed] [Google Scholar]
- 255.Erin E.M., Leaker B.R., Nicholson G.C., Tan A.J., Green L.M., Neighbour H.et al. (2006) The effects of a monoclonal antibody directed against tumor necrosis factor-alpha in asthma. Am. J. Respir. Crit. Care Med. 174, 753–762 10.1164/rccm.200601-072OC [DOI] [PubMed] [Google Scholar]
- 256.Holgate S.T., Noonan M., Chanez P., Busse W., Dupont L., Pavord I.et al. (2011) Efficacy and safety of etanercept in moderate-to-severe asthma: a randomised, controlled trial. Eur. Respir. J. 37, 1352–1359 10.1183/09031936.00063510 [DOI] [PubMed] [Google Scholar]
- 257.Wenzel S.E., Barnes P.J., Bleecker E.R., Bousquet J., Busse W., Dahlen S.E.et al. (2009) A randomized, double-blind, placebo-controlled study of tumor necrosis factor-alpha blockade in severe persistent asthma. Am. J. Respir. Crit. Care Med. 179, 549–558 10.1164/rccm.200809-1512OC [DOI] [PubMed] [Google Scholar]
- 258.Dixon W.G., Hyrich K.L., Watson K.D., Lunt M., Galloway J., Ustianowski A.et al. (2010) Drug-specific risk of tuberculosis in patients with rheumatoid arthritis treated with anti-TNF therapy: results from the British Society for Rheumatology Biologics Register (BSRBR). Ann. Rheum. Dis. 69, 522–528 10.1136/ard.2009.118935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Rossios C., Pavlidis S., Hoda U., Kuo C.H., Wiegman C., Russell K.et al. (2018) Sputum transcriptomics reveal upregulation of IL-1 receptor family members in patients with severe asthma. J. Allergy Clin. Immunol. 141, 560–570 10.1016/j.jaci.2017.02.045 [DOI] [PubMed] [Google Scholar]
- 260.Godwin M.S., Reeder K.M., Garth J.M., Blackburn J.P., Jones M., Yu Z.et al. (2019) IL-1RA regulates immunopathogenesis during fungal-associated allergic airway inflammation. JCI Insight 4, e129055 10.1172/jci.insight.129055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Revez J.A., Bain L.M., Watson R.M., Towers M., Collins T., Killian K.J.et al. (2019) Effects of interleukin-6 receptor blockade on allergen-induced airway responses in mild asthmatics. Clin. Transl. Immunol. 8, e1044 10.1002/cti2.1044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Badi Y.E., Pavel A.B., Pavlidis S., Riley J.H., Bates S., Kermani N.Z.et al. (2022) Mapping atopic dermatitis and anti-IL-22 response signatures to type 2-low severe neutrophilic asthma. J. Allergy Clin. Immunol. 149, 89–101 10.1016/j.jaci.2021.04.010 [DOI] [PubMed] [Google Scholar]
- 263.Guttman-Yassky E., Brunner P.M., Neumann A.U., Khattri S., Pavel A.B., Malik K.et al. (2018) Efficacy and safety of fezakinumab (an IL-22 monoclonal antibody) in adults with moderate-to-severe atopic dermatitis inadequately controlled by conventional treatments: A randomized, double-blind, phase 2a trial. J. Am. Acad. Dermatol. 78, 872e6–881e6 10.1016/j.jaad.2018.01.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Rymut S.M., Sukumaran S., Sperinde G., Bremer M., Galanter J., Yoshida K.et al. (2022) Dose-dependent inactivation of airway tryptase with a novel dissociating anti-tryptase antibody (MTPS9579A) in healthy participants: A randomized trial. Clin. Transl. Sci. 15, 451–463 10.1111/cts.13163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Undela K., Goldsmith L., Kew K.M. and Ferrara G. (2021) Macrolides versus placebo for chronic asthma. Cochrane Database Syst. Rev. 11, CD002997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Seresirikachorn K., Kerr S.J., Aeumjaturapat S., Chusakul S., Kanjanaumporn J., Wongpiyabovorn J.et al. (2021) Predictive factors for identifying macrolide responder in treating chronic rhinosinusitis. Rhinology 59, 284–291 10.4193/Rhin20.649 [DOI] [PubMed] [Google Scholar]
- 267.Chupp G., Kline J.N., Khatri S.B., McEvoy C., Silvestri G.A., Shifren A.et al. (2022) Bronchial Thermoplasty in Patients With Severe Asthma at 5 Years: The Post-FDA Approval Clinical Trial Evaluating Bronchial Thermoplasty in Severe Persistent Asthma Study. Chest 161, 614–628 10.1016/j.chest.2021.10.044 [DOI] [PubMed] [Google Scholar]
- 268.Schroder A., Lunding L.P., Zissler U.M., Vock C., Webering S., Ehlers J.C.et al. (2022) IL-37 regulates allergic inflammation by counterbalancing pro-inflammatory IL-1 and IL-33. Allergy 77, 856–869 10.1111/all.15072 [DOI] [PubMed] [Google Scholar]
- 269.Minshall E., Chakir J., Laviolette M., Molet S., Zhu Z., Olivenstein R.et al. (2000) IL-11 expression is increased in severe asthma: association with epithelial cells and eosinophils. J. Allergy Clin. Immunol. 105, 232–238 10.1016/S0091-6749(00)90070-8 [DOI] [PubMed] [Google Scholar]
- 270.Krammer S., Yang Z., Zimmermann T., Xepapadaki P., Geppert C.I., Papadopoulos N.G.et al. (2022) An Immunoregulatory Role of Interleukin-3 in Allergic Asthma. Front Immunol. 13, 821658 10.3389/fimmu.2022.821658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Gao X., Leung T.F., Wong G.W., Ko W.H., Cai M., He E.J.et al. (2022) Meteorin-beta/Meteorin like/IL-41 attenuates airway inflammation in house dust mite-induced allergic asthma. Cell Mol. Immunol. 19, 245–259 10.1038/s41423-021-00803-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Johnson M.T., Xin P., Benson J.C., Pathak T., Walter V., Emrich S.M.et al. (2022) STIM1 is a core trigger of airway smooth muscle remodeling and hyperresponsiveness in asthma. Proc. Natl. Acad. Sci. U. S. A. 119, e2114557118 10.1073/pnas.2114557118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Lunding L.P., Skouras D.B., Vock C., Dinarello C.A. and Wegmann M. (2022) The NLRP3 inflammasome inhibitor, OLT1177((R)), ameliorates experimental allergic asthma in mice. Allergy 77, 1035–1038 10.1111/all.15164 [DOI] [PubMed] [Google Scholar]
- 274.Echeverri Tirado L.C., Ghonim M.A., Wang J., Al-Khami A.A., Wyczechowska D., Luu H.H.et al. (2019) PARP-1 is critical for recruitment of dendritic cells to the lung in a mouse model of asthma but dispensable for their differentiation and function. Mediators Inflamm. 2019, 1656484 10.1155/2019/1656484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Ghonim M.A., Pyakurel K., Ibba S.V., Wang J., Rodriguez P., Al-Khami A.A.et al. (2015) PARP is activated in human asthma and its inhibition by olaparib blocks house dust mite-induced disease in mice. Clin. Sci. (Lond.) 129, 951–962 10.1042/CS20150122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Shafiei-Jahani P., Helou D.G., Hurrell B.P., Howard E., Quach C., Painter J.D.et al. (2021) CD200-CD200R immune checkpoint engagement regulates ILC2 effector function and ameliorates lung inflammation in asthma. Nat. Commun. 12, 2526 10.1038/s41467-021-22832-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Gracias D.T., Sethi G.S., Mehta A.K., Miki H., Gupta R.K., Yagita H.et al. (2021) Combination blockade of OX40L and CD30L inhibits allergen-driven memory TH2 cell reactivity and lung inflammation. J. Allergy Clin. Immunol. 147, 2316–2329 10.1016/j.jaci.2020.10.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Powell W.S. (2021) Eicosanoid receptors as therapeutic targets for asthma. Clin. Sci. (Lond.) 135, 1945–1980 10.1042/CS20190657 [DOI] [PubMed] [Google Scholar]
- 279.Diamant Z., Aalders W., Parulekar A., Bjermer L. and Hanania N.A. (2019) Targeting lipid mediators in asthma: time for reappraisal. Curr. Opin. Pulm. Med. 25, 121–127 10.1097/MCP.0000000000000544 [DOI] [PubMed] [Google Scholar]
- 280.Werder R.B., Ullah M.A., Rahman M.M., Simpson J., Lynch J.P., Collinson N.et al. (2022) Targeting the P2Y13 Receptor Suppresses IL-33 and HMGB1 Release and Ameliorates Experimental Asthma. Am. J. Respir. Crit. Care Med. 205, 300–312 10.1164/rccm.202009-3686OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Pivniouk V., Gimenes-Junior J.A., Ezeh P., Michael A., Pivniouk O., Hahn S.et al. (2022) Airway administration of OM-85, a bacterial lysate, blocks experimental asthma by targeting dendritic cells and the epithelium/IL-33/ILC2 axis. J. Allergy Clin. Immunol. 149, 943–956 10.1016/j.jaci.2021.09.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Kim J.S., Jeong J.S., Kwon S.H., Kim S.R. and Lee Y.C. (2020) Roles of PI3K pan-inhibitors and PI3K-delta inhibitors in allergic lung inflammation: a systematic review and meta-analysis. Sci. Rep. 10, 7608 10.1038/s41598-020-64594-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Sadiq M.W., Asimus S., Belvisi M.G., Brailsford W., Fransson R., Fuhr R.et al. (2022) Characterisation of pharmacokinetics, safety and tolerability in a first-in-human study for AZD8154, a novel inhaled selective PI3Kgammadelta dual inhibitor targeting airway inflammatory disease. Br. J. Clin. Pharmacol. 88, 260–270 10.1111/bcp.14956 [DOI] [PubMed] [Google Scholar]
- 284.Pennington L.F., Gasser P., Brigger D., Guntern P., Eggel A. and Jardetzky T.S. (2021) Structure-guided design of ultrapotent disruptive IgE inhibitors to rapidly terminate acute allergic reactions. J. Allergy Clin. Immunol. 148, 1049–1060 10.1016/j.jaci.2021.03.050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Canas J.A., Rodrigo-Munoz J.M., Sastre B., Gil-Martinez M., Redondo N. and Del Pozo V. (2020) MicroRNAs as potential regulators of immune response networks in asthma and chronic obstructive pulmonary disease. Front. Immunol. 11, 608666 10.3389/fimmu.2020.608666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Carrer M., Crosby J.R., Sun G., Zhao C., Damle S.S., Kuntz S.G.et al. (2020) Antisense Oligonucleotides Targeting Jagged 1 Reduce House Dust Mite-induced Goblet Cell Metaplasia in the Adult Murine Lung. Am. J. Respir. Cell Mol. Biol. 63, 46–56 10.1165/rcmb.2019-0257OC [DOI] [PubMed] [Google Scholar]
- 287.St-Germain O., Lachapelle P., Pavord I.D. and Couillard S. (2022) Tackling ‘People Remodelling’ in Corticosteroid-dependent Asthma with Type-2 Targeting Biologics and a Formal Corticosteroid Weaning Protocol. touchrev. Respir. Pulmon. Dis. 7, 44–47 10.17925/USRPD.2022.7.2.44 [DOI] [Google Scholar]
- 288.Roth-Walter F., Adcock I.M., Benito-Villalvilla C., Bianchini R., Bjermer L., Caramori G.et al. (2019) Comparing biologicals and small molecule drug therapies for chronic respiratory diseases: An EAACI Taskforce on Immunopharmacology position paper. Allergy 74, 432–448 10.1111/all.13642 [DOI] [PubMed] [Google Scholar]
- 289.Thomas D., McDonald V.M., Pavord I.D. and Gibson P.G. (2022) Asthma remission: what is it and how can it be achieved? Eur. Respir. J. 60, 2102583 10.1183/13993003.02583-2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Ntontsi P., Loukides S., Bakakos P., Kostikas K., Papatheodorou G., Papathanassiou E.et al. (2017) Clinical, functional and inflammatory characteristics in patients with paucigranulocytic stable asthma: Comparison with different sputum phenotypes. Allergy 72, 1761–1767 10.1111/all.13184 [DOI] [PubMed] [Google Scholar]
- 291.Agusti A., Bafadhel M., Beasley R., Bel E.H., Faner R., Gibson P.G.et al. (2017) Precision medicine in airway diseases: moving to clinical practice. Eur. Respir. J. 50, 1701655 10.1183/13993003.01655-2017 [DOI] [PubMed] [Google Scholar]
- 292.Hinks T.S.C., Levine S.J. and Brusselle G.G. (2021) Treatment options in type-2 low asthma. Eur. Respir. J. 57, 2000528 10.1183/13993003.00528-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
This review manuscript does not contain original data.