Abstract
Background
In the United States, the prevalence of obesity among adults has increased 3-fold since the 1980s, but patterns of incidence of new cases of obesity are not known.
Objectives
To examine the incidence of new cases of obesity: overall, by demographic and educational subgroups, by weight status, and changes during this century.
Methods
We analyzed adult (≥20 y) anthropometric records from the US nationally representative Panel Study of Income Dynamics from 2001 to 2017. Among those not having obesity (body mass index, BMI, ≥30 kg/m2) at first observation, we used Poisson models to estimate the incidence of obesity [cases/1000 person-years (PYs)] and incidence rate ratio (IRR).
Results
Among 13,888 adults followed for 115,797 PYs, the incidence of obesity in 2001–2017 was 28.1/1000 PYs (95% CI: 26.7, 29.7). Over the periods 2001–2005, 2005–2009, and 2009–2013, the incidence of obesity was stable, but in 2013–2017 the incidence increased by 18% compared to 2009–2013 [IRR: 1.18 (95% CI: 1.06, 1.30)]. Blacks had higher obesity incidence [47.9/1000 PYs (95% CI: 42.7, 53.1)] than Whites [26.2/1000 PYs (95% CI: 24.6, 27.9)]. Risk was particularly high among Black females [57.9/1000 PYs (95% CI: 49.1, 66.8)] and Black young adults (20–29 y) [65.5/1000 PYs (95% CI: 54.2, 76.7)]. Across race, obesity incidence was highest in young adults (20–29 y) [34.1/1000 PYs (95% CI: 31.5, 36.7)] and declined with age [age 70+ y: 18.9/1000 PYs (95% CI: 16.6, 21.8)]. Those with overweight had an obesity risk 7 times higher than those with normal weight [62.1/1000 PYs (95% CI: 58.8, 65.3) vs. 8.8/1000 PYs (95% CI: 8.1, 9.6)]. Those with less than high-school education had higher obesity incidence than those with education beyond high-school [39.4/1000 PYs (95% CI: 34.4, 44.4) vs. 24.7/1000 PYs (95% CI: 23.1, 26.3)].
Conclusions
Incidence of obesity was stable over the first 13 y of the last 2 decades but increased by 18% in 2013–2017. Blacks and younger adults were at highest risk, and those with overweight were also at high risk for developing obesity.
Keywords: adults, disparities, incidence, obesity, trends, United States
Introduction
Obesity is a major health problem globally [1] and a risk factor for type 2 diabetes [2], cardiovascular diseases [3], certain cancers [4], and premature mortality [5]. The longer a person is exposed to obesity, the higher the risk of developing other chronic diseases [6]. Because obesity, once established, is rarely reversed [7], prevention is of utmost importance, and, for successful prevention, we need to identify when and in whom obesity is most likely to present; this goal is addressable only with data on incidence of disease.
In the United States, recent patterns of obesity incidence at the national level have been documented for childhood, adolescence [7, 8], and for the transition to adulthood (ages 18–21 y) [7]. For adults, however, the only national representative longitudinal data dates 40 y back and focused on incidence of overweight and major weight gain (≥5 unit increase in BMI, in kg/m2). The study, using data from the First National Health and Nutrition Examination Survey Epidemiologic Follow-up Study, collected follow-up measures in 1981–1984 from adults first measured in 1971–1975 and found that the 10-y incidence of major weight gain in males and females was highest in those aged 25–34 y at baseline (3.9% for males and 8.4% for females) [9]. However, these data are out of date. When this study was conducted, the prevalence of adult obesity in the United States was stable around 12–14% [10]; since then, the prevalence has increased, reaching 42% in 2017–2018 [10, 11].
More recent studies of obesity incidence in the United States have relied on nonrepresentative cohorts (all-White cohort [12, 13]; primary healthcare [14]), or were restricted to specific age groups [18–21 y [7]]. From the 1950s to the 1990s, among Whites aged 40–55 y, the 8-y incidence of obesity increased from 5.8% to 14.8% [13]. A study of young adults (18–21 y) found no changes in annual incidence between the periods 1996–2001 and 2001–2008 [7].
Not only do we not have nationally representative data from the 21st century on the age-specific incidence of obesity in US adults, we also have no information on incidence patterns across race or socioeconomic status, further limiting our ability to understand risk and prevent new cases [15]. The lack of contemporary longitudinal studies also limits our understanding about how much the increasing prevalence is caused by more people developing obesity, people developing obesity at younger ages, and/or people with obesity surviving longer.
This study documents the incidence patterns of obesity across adulthood using a nationally representative sample from the US Panel Study of Income Dynamics (PSID) [16]. We present current estimates of age-specific incidence of obesity in the US population by sex, race, educational level, and weight status, and we demonstrate how incidence patterns have changed across the first 2 decades of the 21st century.
Methods
The PSID
The PSID was launched in 1968 as a nationally representative sample of over 18,000 people living in 5000 families in the United States; it has since continuously collected information on socioeconomic indicators in these people and their descendants. For the PSID to remain nationally representative, survey weights are calibrated to the population characteristics from the Current Population Survey or American Community Survey for each data wave [17].
The PSID is a dynamic open cohort of households, meaning that people and households enter the study through birth, marriage, and family formation and exit through death, divorce, and family dissolution. The PSID consist of the ‘Main Study’ and 5 supplement studies. Since 1999, the Main Study has biannually collected self-reported weight and height information about the household head and cohabiting partner/spouse. Since 2005, the supplement study ‘Transition into Adulthood’ has biannually collected height and weight data from a subsample of youth ages 18–29 y living in a PSID household [16, 18]. In total, between 2001 and 2017, 23,320 adults aged ≥20 y were eligible for data collection about height and weight data.
The data for this study were provided by the PSID as a deidentified dataset with no personal indicators, and so did not constitute ‘human subjects’ or ‘clinical investigation’ data. Therefore, no institutional review board review was required.
Defining incident obesity
In the PSID Main Study, weight and height for the household head and cohabiting partner/spouse are reported for both persons by either the head him/herself or by the partner/spouse using telephone interviews. In the Transition into Adulthood supplement, weight and height are reported by the person themselves. Other studies have shown that respondents tend to overestimate their height and underestimate their weight, more so among females [19] and young adults [20]. To address potential self-report bias, we developed a regression-based correction equation using data from the NHANES, which contains both self-reported and measured weight and height. This correction is similar to what has been implemented in other studies [21, 22]. Correction equations were estimated seperately for females and males and by age group, race, and education level. The modeled correction coefficients from the NHANES data were applied to reported height and weight data from the PSID. Model coefficients and analyses using the original reported data are in the Supplemental Methods and Supplemental Tables 1, 2, 3, and 4. Using the corrected height and weight, we calculated BMI as weight (kg)/height (m)2 to define normal weight (BMI < 25), overweight (25 ≤ BMI < 30), and obesity (BMI ≥ 30). A case of incident obesity was defined as the first time a person had a record of BMI ≥ 30 in PSID.
The adults entered the cohort at different time points and were followed for different durations due to left and right censoring. Therefore, we reported incident obesity as the incidence rate per 1000 person-years (PYs). We calculated PYs from the age at the first anthropometric record at or above 20 years of age. End of PYs was the midpoint between the last record below the obesity threshold and the record where the person first had a BMI ≥30 kg/m2 or when the last BMI was recorded, whichever occurred first.
Age-specific incidence was calculated for 10-year age groups (20–29, 30–39, 40–49, 50–59, 60–69, and 70+) as the number of new cases of obesity within an age group in those who did not have obesity in any previous records including in younger age groups. Age-specific PYs were calculated from the beginning of the age group (e.g., age 30 y) for those who had records from younger ages or from the age within the age group when the person had her/his first BMI record (e.g., age 35 y).
These estimates were also calculated separately for sex (female, male), race (White, Blacks, and Other Races), and education (<high school, high school degree, >high school). In the PSID, race is self-reported as White, Black/African American, American Indian/Alaska Native, Asian, Native Hawaiian or Pacific Islander, or Other Races (not specified). People can mention up to 4 races and we used the first one mentioned. To understand the difference in risk of obesity between normal weight and overweight, we also stratified by weight status at first anthropometric record (normal weight, overweight).
To investigate changes over time in the incidence of obesity, we created 4 equal-duration periods: 2001–2005, 2005–2009, 2009–2013, and 2013–2017. For each period, we included records from all people who did not have obesity the year when the period started, i.e., in 2001, 2005, 2009, and 2013, or when they entered the period, e.g., in 2003 for those in period 2001–2005.
Statistical analysis
We used Poisson regression to model incidence rates and calculate predictive margins to estimate incidence rates overall and by sex, age group, race, education, weight status, and period. Follow-up time was split into 1-year intervals for analytical purposes. Poisson regression can model event rates (i.e., events of obesity/time with the incorporation of an offset term given time of follow-up) and allows for both time-varying exposures and covariates [23]. We used the survey commands (svy) of Stata (version 15.1) to correct for cluster sample design and unequal probability of sampling by applying survey weights, stratum, and cluster provided by the PSID. With these adjustments, we ensured that the results were national representative of the adult US population between 2001 and 2017 [16].
Incidence rates are presented as cases per 1000 PYs. Overall rates and rates by education level are adjusted for age, sex, and race, while sex-, age-, and race-specific rates are adjusted for the two other demographic variables (e.g. for sex: age and race).
Using the Poisson models, we also tested differences in incidence over time by calculating incidence rate ratios (IRRs) for each period, with 2001–2005 as reference. We calculated IRRs for those with overweight (BMI ≥25 kg/m2) compared to those with normal weight (BMI <25 kg/m2) at first observation or at the beginning of an age group in the age-specific models.
Results
Of the 23,320 adults aged ≥20 y eligible for data collection on height and weight, we excluded those with missing information on year of birth (n = 50), and those who refused to provide (n = 55) or had missing information on height and weight (n = 206). We excluded records reported during pregnancy (records = 1690): 7 pregnant females had no records at other time points. Because at least 2 time points were needed to calculate incidence, we retained only those adults with at least 2 records of weight and height (n = 19,029). Respondents who had obesity at the first anthropometric record were not eligible for incident obesity (n = 5056). We excluded those with missing data on covariates (race, n = 85). The resulting analytic sample consisted of 13,888 adults born between 1904 and 1995, with ≥2 records of height and weight at ages ≥20 y (median records: 6, median follow-up: 10 PYs). These yielded 115,797 PYs of follow-up (Supplemental Figure 1). Characteristics of the study population at their first anthropometric record are summarized in Supplemental Table 5.
Incidence of obesity
Across the entire period, 2001–2017, national incidence of obesity among adults was 28.1 per 1000 PYs (Table 1). During the first 3 periods (2001–2005, 2005–2009, and 2009–2013), overall incidence of obesity was relatively stable: it was 34.1 per 1000 PYs during 2001–2005, 36.4 per 1000 PYs in 2005–2009, and 34.5 per 1000 PYs in 2009–2013 (Table 2). Compared to 2001–2005, the incidence of obesity had not increased by 2005–2009 (IRR: 1.06; 95% CI: 0.94, 1.19) or by 2009–2013 (IRR: 1.00; 95% CI: 0.90, 1.11) (Supplemental Table 6). In contrast, the incidence of obesity in 2013–2017 was 40.7 per 1000 PYs and thus, higher than in all other periods: 2001–2005, IRR: 1.18; (95% CI: 1.06, 1.30); 2005–2009, IRR: 1.12; (95% CI: 1.02, 1:22); 2009–2013, IRR: 1.18; (95% CI: 1.06, 1.30).
Table 1.
Incidence rates of adult obesity overall and by sex, race, age, and education
| Overall | Race |
|||
|---|---|---|---|---|
| White | Black | Other Races | ||
| Overall | 28.1 (26.7, 29.7) | 26.2 (24.6, 27.9) | 47.9 (42.7, 53.1) | 30.0 (24.1, 36.0) |
| Sex | ||||
| Females | 26.5 (24.7, 28.2) | 23.3 (21.5, 25.0) | 57.9 (49.1, 66.8) | 31.9 (23.8, 39.9) |
| Males | 30.2 (28.2, 32.2) | 29.6 (27.4, 31.9) | 38.5 (33.2, 43.9) | 28.5 (21.8, 35.1) |
| Age group | ||||
| 20–29 y | 34.1 (31.5, 36.7) | 31.1 (28.0, 34.2) | 65.5 (54.2, 76.7) | 37.1 (25.9, 48.3) |
| 30–39 y | 31.3 (28.0, 34.6) | 28.6 (24.8, 32.3) | 61.9 (49.8, 76.7) | 30.8 (16.9, 44.8) |
| 40–49 y | 29.6 (26.6, 32.5) | 27.6 (24.7, 30.6) | 50.2 (41.1, 59.3) | 31.8 (18.8, 44.9) |
| 50–59 y | 27.9 (24.8, 30.9) | 27.5 (24.3, 30.6) | 37.3 (25.4, 49.2) | 23.7 (16.4, 30.9) |
| 60–69 y | 22.9 (19.6, 26.3) | 21.3 (17.6, 24.9) | 33.7 (22.0, 45.3) | 33.4 (15.8, 51.0) |
| 70+ y | 18.9 (16.0, 21.8) | 17.2 (14.5, 20.0) | 33.7 (11.8, 55.6) | 29.9 (8.7, 49.1) |
| Education | ||||
| < High school | 39.4 (34.4, 44.4) | 35.6 (30.7, 40.4) | 54.9 (38.8, 70.9) | 60.0 (38.4, 81.8) |
| High school | 34.5 (31.5, 37.6) | 32.8 (29.4, 36.2) | 47.9 (41.0, 54.9) | 48.6 (33.8, 63.3) |
| > High school | 24.7 (23.1, 26.3) | 23.2 (21.4, 24.9) | 46.3 (39.2, 53.4) | 20.2 (14.8, 25.6) |
| n | 13,888 | 9118 | 3917 | 853 |
| New cases | 3933 | 2271 | 1434 | 228 |
| Person-years | 115,797 | 81,490 | 27,488 | 6818 |
Incidence is calculated as the incidence rate of new cases of obesity per 1000 person-years of follow-up and shown with 95% CIs using Poisson models. Obesity is defined as the first time a person has a BMI ≥30 kg/m2.
Overall incidence rates are adjusted for sex, race, and age. Sex-specific rates are adjusted for age and race. Age-specific rates are adjusted for race and sex. Race-specific rates are adjusted for sex and age. All incidence rates are shown as adjusted and weighted using survey weights, stratum, and cluster to reflect the US population in the period 2001–2017.
Table 2.
Incidence rates of adult obesity by period
| 2001–2005 | 2005–2009 | 2009–2013 | 2013–2017 | IRR for 2013–2017 vs. 2001–2005 |
|
|---|---|---|---|---|---|
| Overall | 34.1 (31.0, 37.2) | 36.4 (33.5, 39.3) | 34.5 (32.1, 37.0) | 40.7 (37.7, 43.6) | 1.18 (1.06, 1.30) |
| Sex | |||||
| Females | 30.9 (27.2, 34.6) | 35.6 (32.1, 39.1) | 33.7 (30.3, 37.2) | 38.1 (34.3, 41.9) | 1.21 (1.04, 1.41) |
| Males | 37.6 (33.2, 42.0) | 37.1 (32.3, 42.0) | 35.6 (32.0, 39.3) | 44.0 (39.6, 48.4) | 1.17 (1.02, 1.35) |
| Race | |||||
| White | 31.6 (28.3, 34.9) | 33.8 (30.8, 36.8) | 32.0 (29.0, 35.0) | 39.1 (35.8, 42.4) | 1.23 (1.10, 1.38) |
| Blacks | 60.3 (49.6, 71.02) | 62.0 (49.6, 74.3) | 61.4 (51.5, 71.2) | 57.9 (47.2, 68.6) | 0.96 (0.76, 1.21) |
| Other | 37.0 (24.2, 49.8) | 38.2 (25.2, 51.2) | 33.5 (24.0, 43.0) | 41.6 (28.2, 55.0) | 1.12 (0.85, 1.49) |
| Age group | |||||
| 20–29 y | 37.6 (31.2, 43.9) | 34.0 (29.2, 38.7) | 32.6 (27.1, 38.0) | 41.6 (35.2, 48.0) | 1.11 (0.88, 1.39) |
| 30–39 y | 38.4 (32.0, 44.8) | 35.5 (29.3, 41.8) | 37.8 (32.4, 43.3) | 46.4 (40.0, 53.0) | 1.21 (0.99, 1.48) |
| 40–49 y | 34.3 (28.5, 40.0) | 40.2 (33.9, 46.4) | 39.2 (33.5, 44.9) | 44.8 (36.6, 52.9) | 1.31 (1.03, 1.65) |
| 50–59 y | 37.6 (31.8, 43.4) | 37.6 (31.1, 44.0) | 34.2 (29.4, 39.0) | 46.6 (39.3, 54.0) | 1.24 (0.98, 1.57) |
| 60–69 y | 27.7 (18.2, 37.3) | 38.6 (29.3, 47.9) | 28.4 (22.3, 34.5) | 35.4 (28.4, 42.4) | 1.28 (0.88, 1.86) |
| 70+ y | 24.5 (17.1, 31.8) | 29.1 (20.9, 37.3) | 30.2 (21.6, 38.9) | 22.1 (15.2, 28.9) | 0.90 (0.60, 1.36) |
| Education | |||||
| < High school | 44.8 (35.6, 54.1) | 55.8 (47.1, 64.5) | 46.1 (37.2, 55.0) | 50.3 (39.5, 61.0) | 1.12 (0.88, 1.43) |
| High school | 38.1 (33.3, 42.9) | 45.1 (37.8, 52.3) | 45.8 (39.8, 51.7) | 50.1 (43.6, 56.6) | 1.32 (1.10, 1.57) |
| > High school | 30.6 (26.9, 34.4) | 30.9 (27.6, 34.2) | 28.7 (26.0, 31.5) | 36.8 (33.0, 40.5) | 1.20 (1.04, 1.38) |
| n | 8659 | 9217 | 9437 | 9136 | |
| New cases | 1164 | 1339 | 1363 | 1518 | |
| PYs | 28,682 | 31,215 | 32,084 | 30,919 | |
Incidence is calculated as new cases per 1000 PYs of follow-up (95% CIs) using Poisson models. Obesity is defined as the first time a person has a body mass index ≥30 kg/m2.Incidence rates are modeled over year and adjusted for sex, race, and age. IRR, incidence rate ratio; PYs, person-years of follow-up. Overall incidence rates are adjusted for sex, race, and age. Sex-specific rates are adjusted for age and race. Age-specific rates are adjusted for race and sex. Race-specific rates are adjusted for sex and age. All incidence rates are shown as adjusted and weighted using survey weights, stratum, and cluster to represent the US population in the 4 periods.
Incidence of obesity by demographic and educational subgroups
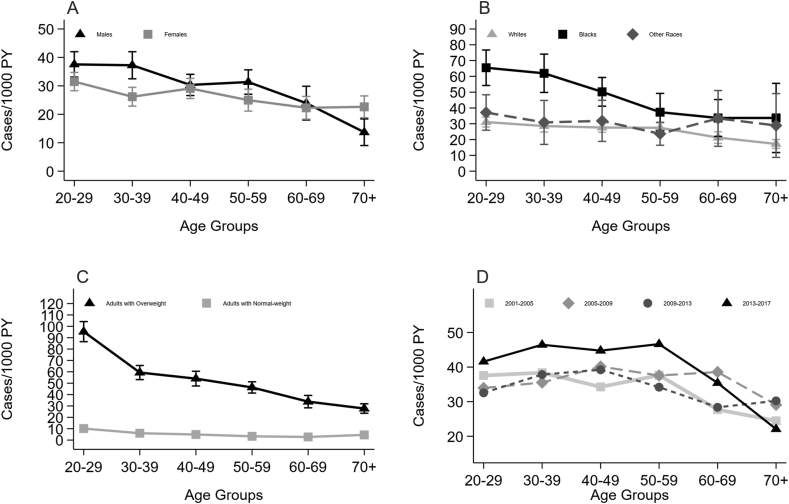
Obesity incidence was highest in young adulthood (age 20–29 y, 34.1/1000 PYs) and declined with age to a low of 18.9 cases per 1000 PYs at age 70+ y (Table 1). Overall, males had higher incidence of obesity than females (IRR: 1.14; 95% CI, 1.05, 1.23]). Across age groups, only in the age groups 20–29, 30–39, and 50–59 y was the incidence of obesity higher in males than females. At age 70+ y, the incidence of obesity was lower in males than females (Figure 1A and Supplemental Table 7).
Figure 1.
Age-specific incidence of obesity by sex, race, baseline weight status, and period. Shown is the age-specific incidence rate of obesity as cases per 1000 person-years (PYs) with 95% CIs, according to sex (A) (n: 6621 males; 7267 males); race (B) (n: 9118 Whites; 3917 Blacks; 853 Other Races); weight status at first anthropometric record (C) (n: 7379 with normal weight; 6509 with overweight); and by period (D) (n: 8959 in 2001–2005; 9217 in 2005–2009; 9437 in 2009–2013; 9136 in 2013–2017). Incidence rates were calculated using Poisson models. Normal weight is defined as a BMI <25 kg/m2, overweight is defined as a BMI ≥25 kg/m2 and <30 kg/m2, and obesity is defined as the first time a person has a BMI ≥30 kg/m2.
Obesity incidence among Blacks (47.9/1000 PYs) was almost double that of Whites (26.2/1000 PYs) (Table 1) (IRR: 1.82; 95% CI: 1.58, 2.07); those of Other Races tended to have a slightly higher incidence of obesity (30.0/1000 PYs) than Whites (IRR: 1.14; 95% CI: 0.92, 1.37). Compared to White females, the obesity incidence was more than double in Black females (IRR: 2.49; 95% CI: 2.04, 2.95) and 37% higher in females of Other Races (IRR: 1.37; 95% CI: 1.03, 1.71). Among males, compared to Whites, the obesity incidence was higher for Blacks (IRR: 1.30; 95% CI: 1.09, 1.51) and similar for Other Races (IRR: 0.96; 95%CI: 0.72, 1.20). Across all ages, Blacks had the highest incidence of obesity (Figure 1B). The difference between Blacks and Whites was largest in adults aged 20–29 y (IRR: 2.03; 95%CI: 1.57, 2.49]) and 30–39 y (IRR: 2.12; 95% CI: 1.56, 2.67) and decreased with age (Figure 1B) (Supplemental Table 7).
Those who had less than high-school education had higher obesity incidence than those with a high-school degree (IRR: 1.14; 95% CI: 1.01, 1.28) and those with education beyond high school (IRR: 1.59; 95%CI: 1.36, 1.83). In Blacks, there was no difference in incidence of obesity between those with different levels of education (Table 1). Between Blacks and Whites with education beyond high school, the difference in obesity incidence was larger than between Blacks and Whites with lower levels of education (IRR: 2.05; 95% CI: 1.70, 2.40 vs. IRR: 1.45; 95% CI: 1.01, 1.88).
For most subgroups, the incidence of obesity increased over the study period. The increase was mainly driven by a higher incidence in the period 2013–2017, whereas the incidence of obesity did not vary much across 2001–2005, 2005–2009, and 2009–2013 (Supplemental Table 6). By 2013–2017, the incidence of obesity had increased most for those aged 40-49 y (31%) followed by those aged 50–59 (24%) and 30–39 y (21%) (Table 2). Females experienced a 21% increase in the incidence of obesity (IRR: 1.21; 95%CI: 1.04, 1.41), whereas the increase for males was 17% (IRR: 1.17; 95%CI: 1.02, 1.35) (Table 2). The incidence of obesity increased among Whites (23%) and remained the same for Blacks and Other Races. In 2001–2005, Blacks had an obesity incidence 92% higher than Whites (IRR: 1.92; 95% CI: 1.52, 2.31), while its was 44% higher in 2013–2017 (IRR: 1.44; 95% CI: 1.15, 1.73).
In terms of educational level, the incidence of obesity increased most for those who had a high school degree (32% increase) followed by those with an education beyond high school (20%), whereas it remained the same for those with less than a high school degree.
Incidence of obesity by weight status
Adults who were overweight at their first anthropometric record were 7.0 (95% CI: 6.3, 7.7) times more likely to enter obesity than those with normal weight at their first anthropometric record (Table 3). This pattern was consistent for all demographic groups (Figure 1C and Table 3). Among both adults with normal weight and overweight, incidence of obesity was highest at ages 20–29 y (9.9/1000 PYs and 97.0/1000 PYs, respectively); for both groups the risk of obesity was halved by age 40–49 y (4.9/1000 PYs and 54.0/1000 PYs, respectively). The risk continued to decrease thereafter with increasing age (Table 3).
Table 3.
Incidence rates of adult obesity by baseline weight status
| Normal Weight |
Overweight |
IRR for overweight vs. normal weight | |||
|---|---|---|---|---|---|
| Incidence | IRR | Incidence | IRR | ||
| Overall | 8.8 (8.1, 9.6) | 62.1 (58.8, 65.3) | 7.0 (6.3, 7.7) | ||
| Sex | |||||
| Females | 10.0 (8.9, 11.0) | Ref | 67.3 (61.9, 72.6) | Ref | 6.8 (5.8, 7.7) |
| Males | 7.6 (6.6, 8.6) | 0.8 (0.7, 0.9) | 55.0 (51.7, 58.2) | 0.8 (0.7, 0.9) | 7.3 (6.3, 8.2) |
| Race | |||||
| White | 8.4 (7.6, 9.2) | Ref | 59.4 (56.0, 62.9) | Ref | 7.1 (6.3, 7.8) |
| Black | 13.8 (9.8, 17.8) | 1.7 (1.2, 2.3) | 87.2 (77.9, 96.5) | 1.4 (1.3, 1.6) | 6.3 (4.5, 8.2) |
| Other | 9.4 (6.5, 12.3) | 1.1 (0.8, 1.5) | 62.4 (49.4, 75.3) | 1.0 (0.8, 1.2) | 6.6 (4.5, 8.8) |
| Age group | |||||
| 20–29 y | 9.9 (8.3, 10.5) | Ref | 97.0 (88.5, 105.4) | Ref | 9.8 (8.0, 11.6) |
| 30–39 y | 6.1 (4.3, 7.8) | 0.6 (0.4, 0.9) | 59.3 (53.1, 65.6) | 0.6 (0.6, 0.7) | 9.8 (6.9, 12.7) |
| 40–49 y | 4.9 (3.5, 6.4) | 0.5 (0.4, 0.7) | 54.0 (47.6, 60.5) | 0.5 (0.5, 0.6) | 11.0 (7.3, 14.6) |
| 50–59 y | 3.3 (1.6, 5.0) | 0.3 (0.2, 0.6) | 46.3 (41.3, 51.3) | 0.5 (0.4, 0.5) | 13.9 (6.8, 21.0) |
| 60–69 y | 2.7 (1.0, 4.5) | 0.3 (0.1, 0.6) | 33.8 (28.3, 39.2) | 0.3 (0.3, 0.4) | 12.3 (4.5, 20.1) |
| 70+ y | 4.6 (1.7, 7.4) | 0.5 (0.3, 0.9) | 27.7 (23.6, 31.9) | 0.3 (0.2, 0.3) | 6.1 (2.5, 9.6) |
| Education | |||||
| < High school | 16.2 (12.4, 20.1) | 2.3 (1.7, 2.9) | 68..4 (57.9, 79.0) | 1.3 (1.1, 1.5) | 4.2 (3.0, 5.4) |
| High school | 12.7 (10.3, 15.0) | 1.7 (1.4, 2.0) | 71.6 (65.9, 77.2) | 1.2 (1.1, 1.4) | 5.7 (4.5, 6.8) |
| > High school | 7.1 (6.4, 7.8) | Ref | 58.1 (54.0, 62.2) | Ref | 8.2 (7.1, 9.2) |
| n | 7379 | 6509 | |||
| New cases | 800 | 3133 | |||
| PYs | 70,549 | 45,248 | |||
Weight status is at first anthropometric record. Normal weight is defined as a BMI <25 kg/m2, overweight is defined as a BMI ≥ 25 kg/m2 and <30 kg/m2, and obesity is defined as the first time a person has a body mass index ≥30 kg/m2. IRR, incidence rate ratio; PYs, person-years of follow-up; Ref, reference. Incidence is calculated as the incidence rate of new cases per 1000 PYs of follow-up (95% CIs) using Poisson models. Overall incidence rates are adjusted for sex, race, and age. Sex-specific rates are adjusted for age and race. Age-specific rates are adjusted for race and sex. Race-specific rates are adjusted for sex and age. All incidence rates are weighted using survey weights, stratum, and cluster to represent the US population between 2001 and 2017.
Among adults with normal weight at their first anthropometric record, Blacks had 70% higher incidence of obesity than Whites (IRR: 1.7; 95% CI: 1.2, 2.3). When comparing those with overweight at their first anthropometric record, Blacks had a 40% higher incidence of obesity than Whites (IRR: 1.4; 95% CI: 1.3, 1.6).
Discussion
To understand which people are at highest risk of developing obesity, at which ages new cases of obesity are most common, and how these patterns have changed over the past 2 decades, we calculated obesity incidence in a national representative prospective cohort from 2001–2017. We found that across this century, the incidence of obesity was relatively stable until 2013, but by 2013–2017, the incidence of obesity had increased by 18%. The risk of developing obesity differed across groups and was most commonly experienced by Blacks, especially Black females and Black adults under the age of 50 y, and by people with low levels of education. Across race, adults at the youngest ages (20–29 years) had higher incidence of obesity than older age groups. Among those with overweight, younger adults were more likely than older overweight adults to progress to obesity.
Over the last 2 decades, the obesity incidence increased by 18%, which mainly occurred in the period 2013–2019. In the 1990s, an obesity incidence rate of 14.8% was observed in White people followed over 8 y [13]. Though not directly comparable to our results, this suggests that the incidence of obesity has more than doubled over the last 2 decades. Our results show that the increase mainly occurred during the time period 2013–2017. This pattern is consistent with findings that the prevalence of obesity started to increase again from 2013–2014 after leveling in the late 2000s [24]. We observed a small decrease in the incidence of obesity from 2009–2013 compared to 2005–2009, contemporaneous with reported decreases in calorie intake [25], consumption of sugar-sweetened beverages and poor diets, and an increased intake of healthy foods [26].
A higher incidence at younger ages may be partly explained by the fact that the pool of adults who are eligible to enter obesity for the first time becomes smaller as more people have obesity [27]. For instance, 26% of the US population has obesity at ages 18–21 y [7], leaving 74% of the population eligible for incident obesity. Due to the high obesity incidence from age 20–29 y, even fewer people will be eligible at age 30+ y, and so on for the remaining ages. There may also be other explanations for younger adults having the highest risk of obesity; early adulthood is a phase where many start their own households and thus change their home environment. The proportion with low physical activity level increased from adolescence to young adulthood (mean age 25 y) [28], and the proportion consuming fast food ≥3 times a week increased from adolescence to young adulthood (mean age 21) [29].
A higher incidence at younger ages combined with national cross-sectional studies showing that the prevalence of obesity increases with age until age 60 y [30] indicates that those who developed obesity at younger ages may still have obesity at older ages. This argument is supported by a study of youths that found that obesity is rarely reversed, as only 2% of adolescents with obesity had no obesity in young adulthood [7]. This is especially of concern given that early onset of obesity is associated with longer exposure to excess weight and higher risks of cardiometabolic diseases [31].
Our estimates of a higher incidence of obesity in Blacks than in Whites across sex and age are consistent with published data on obesity prevalence [15, 30, 32]. Yet, incidence estimates contribute by showing that the differences in obesity are driven by higher incidence in those under age 40 y, demonstrating that Blacks have higher incidence of obesity and are exposed to longer duration of obesity. Although the obesity incidence by 2013–2017 had increased by 25% among Whites, no increases were observed among Blacks. Though the relative difference in obesity risk between Blacks and Whites decreased from 92% to 43%, race disparities in obesity incidence were still large in 2013–2017, which is consistent with published data on obesity prevalence [30].This suggests that the level hitherto interventions aiming at preventing obesity may have reached those at highest risk but not to a sufficient extent.
Obesity incidence was higher among those with less than high school education. Although this is consistent with published prevalence data [15], we have not found prevalence studies of the relationship between obesity, education, and race. Our results show that, in contrast to Whites and Other Races, there was no difference in incidence of obesity between Blacks with a high school degree and Blacks with an education beyond high school. Further, Blacks had higher obesity incidence than Whites at all education levels, and the difference was largest among those with highest level of education, suggesting that higher education is less protective against obesity among Blacks than among Whites. In 2013–2017, those with a high school education had reached the same incidence of obesity as those with less education. Educational attainment in the United States has increased over the last decades. Yet, our results show that those with the lowest education levels continued to have the highest risks of developing obesity; thus, even though the education levels of the population shifted upwards, the distribution of risk stayed consistent.
In the United States, only 30% of the adult population has a BMI categorizing them as normal weight. In this study, we show that the incidence of obesity in adults with overweight is 7 times higher than in adults with normal weight. Thus, overweight should not be considered a ‘new normal,’ but rather a temporary phase that often cascades into obesity. Younger adults with overweight were more likely than older overweight adults to progress to obesity, suggesting that preventing overweight among young adults should be a focus. For older adults, the results suggest that the older an adult is before entering the overweight category, the less likely he or she may be to progress to obesity. Thus, efficient obesity intervention measures may not need to prioritize older people with overweight; this finding aligns with studies showing that older adults with overweight have lower mortality risk than other weight groups [33].
This study used data representative of the US population covering nearly 2 decades. Biannual anthropometric reports generated a median of 6 measures per person and a median follow-up of 10 y (range 1–17), with a total of 115,797 PYs of follow up. There are also limitations. First, BMI does not measure adiposity and is not a strong measure to diagnose clinical obesity in an individual; however, at the population level, BMI is a good indicator [34]. Second, we used a regression equation to correct self-reported data, which resulted in 1) an exclusion of 598 (4%) more people due to obesity at first BMI record compared to the not-corrected data; 2) an overall higher incidence of obesity than in the uncorrected data. Thus, in line with the literature, the self-reported data underestimated BMI [19, 20]. However, the prevalence of obesity (Supplemental Table 5) was 5–6 percentage points lower than in prevalence studies [30, 32]. This suggests that despite the correction coefficient, BMI may still have been underestimated; if the number of incident obesity cases had been 5% higher, the incidence rates would had been 1–2 cases higher per 1000 PYs. In the PSID, height and weight for household head or spouse are self-reported for both persons, by either the head him/herself or by the spouse. We have not found literature on correction for proxy reports. Further, with a spousal report, we expect to encounter noise, not bias. That is, a spouse may report information about their spouse with some error, but there is no reason to believe that that would be systematic error that would introduce bias in a particular direction.
Incidence of obesity was stable during the first 3 quarters of this century, but in the period 2013–2017, obesity incidence among US adults increased by 18% and reached an incidence rate of 40.7 per 1000 PYs. This translates to an average of 4% of the adult population entered the obesity category each year in the period 2013–2017. Disparities and age differences were large, especially in Black females and young Black people. Even Blacks with an education beyond high school level had higher obesity incidence than Whites with the same education level. For younger adults, overweight may be a temporary stepping stone to obesity, whereas adults age 60+ with overweight were less likely to progress to obesity. Policies for prevention should focus on young adults, those with lower educational level, and Blacks irrespectively of educational level.
Author Contribution
The authors’ responsibilities were as follows – JN: developed the conception of the study, was responsible for the statistical analyses and the interpretation of data, and drafted, revised, and finalized the article; SAC: contributed to the study design, verified the data, supervised the statistical analyses, and contributed to the interpretation of data and development, revision, and finalization of the manuscript; KMVN: contributed to the study design, supervised the statistical analysis, and contributed to the interpretation of the data and development, revision, and finalization of the manuscript; and all authors: read and approved the final manuscript.
Conflict of interest
The authors report no conflicts of interest.
Funding
This study was supported by Independent Research Fund Denmark (DFF–7025-00053B, to JN) and the National Institute of Diabetes And Digestive And Kidney Diseases of the National Institutes of Health (P30DK111024, to KMVN, and 1R01DK115937, to SAC and KMVN). The funding agencies had no influence on the study design, analyses, or interpretation or the writing of this article. The authors had the final decision to submit the article for publication.
The authors are grateful to the PSID researchers for making the PSID data available. The collection of PSID data used in this study was partly supported by the National Institutes of Health under grant numbers R01 HD069609 and R01 AG040213, and the National Science Foundation under award numbers SES 1157698 and 1623684.
Data Availability
Data were accessed via the PSID website. PSID data are freely available for all registered users at the PSID website (https://psidonline.isr.umich.edu; accessed January 2020).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ajcnut.2022.10.012.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Ng M., Fleming T., Robinson M., Thomson B., Graetz N., Margono C., et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384(9945):766–781. doi: 10.1016/s0140-6736(14)60460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fox C.S., Pencina M.J., Meigs J.B., Vasan R.S., Levitzky Y.S., D’Agostino R.B., Sr Trends in the incidence of type 2 diabetes mellitus from the 1970s to the 1990s: the Framingham Heart Study. Circulation. 2006;113(25):2914–2918. doi: 10.1161/circulationaha.106.613828. [DOI] [PubMed] [Google Scholar]
- 3.Emerging Risk Factors Collaboration. Wormser D., Kaptoge S., Di Angelantonio E., Wood A.M., Pennells L., et al. Separate and combined associations of body-mass index and abdominal adiposity with cardiovascular disease: collaborative analysis of 58 prospective studies. Lancet. 2011;377(9771):1085–1095. doi: 10.1016/s0140-6736(11)60105-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Calle E.E., Rodriguez C., Walker-Thurmond K., Thun M.J. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med. 2003;348(17):1625–1638. doi: 10.1056/NEJMoa021423. [DOI] [PubMed] [Google Scholar]
- 5.Fontaine K.R., Redden D.T., Wang C., Westfall A.O., Allison D.B. Years of life lost due to obesity. JAMA. 2003;289(2):187–193. doi: 10.1001/jama.289.2.187. [DOI] [PubMed] [Google Scholar]
- 6.Hu Y., Bhupathiraju S.N., de Koning L., Hu F.B. Duration of obesity and overweight and risk of type 2 diabetes among US women. Obesity (Silver Spring) 2014;22(10):2267–2273. doi: 10.1002/oby.20851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gordon-Larsen P., The N.S., Adair L.S. Longitudinal trends in obesity in the United States from adolescence to the third decade of life. Obesity (Silver Spring) 2010;18(9):1801–1804. doi: 10.1038/oby.2009.451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cunningham S.A., Kramer M.R., Narayan K.M. Incidence of childhood obesity in the United States. N Engl J Med. 2014;370(5):403–411. doi: 10.1056/NEJMoa1309753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Williamson D.F., Kahn H.S., Remington P.L., Anda R.F. The 10-year incidence of overweight and major weight gain in US adults. Arch Intern Med. 1990;150(3):665–672. doi: 10.1001/archinte.1990.00390150135026. [DOI] [PubMed] [Google Scholar]
- 10.Flegal K.M., Carroll M.D., Kuczmarski R.J., Johnson C.L. Overweight and obesity in the United States: prevalence and trends, 1960–1994. Int J Obes Relat Metab Disord. 1998;22(1):39–47. doi: 10.1038/sj.ijo.0800541. [DOI] [PubMed] [Google Scholar]
- 11.Hales C.M., Carroll M.D., Fryar C.D., Ogden C.L. Vol. 360. National Center for Health Statistics; Hyattsville, Maryland: 2020. pp. 1–8. (Prevalence of obesity and severe obesity among adults: United States, 2017–2018. NCHS Data Brief). [PubMed] [Google Scholar]
- 12.Vasan R.S., Pencina M.J., Cobain M., Freiberg M.S., D’Agostino R.B. Estimated risks for developing obesity in the Framingham Heart Study. Ann Intern Med. 2005;143(7):473–480. doi: 10.7326/0003-4819-143-7-200510040-00005. [DOI] [PubMed] [Google Scholar]
- 13.Parikh N.I., Pencina M.J., Wang T.J., Lanier K.J., Fox C.S., D’Agostino R.B., et al. Increasing trends in incidence of overweight and obesity over 5 decades. Am J Med. 2007;120(3):242–250. doi: 10.1016/j.amjmed.2006.06.004. [DOI] [PubMed] [Google Scholar]
- 14.DeJesus R.S., Croghan I.T., Jacobson D.J., Fan C., St Sauver J. Incidence of obesity at 1 and 3 years among community dwelling adults: A population-based study. J Prim Care Community Health. 2022;13 doi: 10.1177/21501319211068632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hales C.M., Fryar C.D., Carroll M.D., Freedman D.S., Aoki Y., Ogden C.L. Differences in obesity prevalence by demographic characteristics and urbanization level among adults in the United States, 2013–2016. JAMA. 2018;319(23):2419–2429. doi: 10.1001/jama.2018.7270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Panel Study of Income Dynamics. Institute for Social Research, University of Michigan; February 2019. [Google Scholar]
- 17.Chang W.N.R., Heeringa S.G., Johnson D., Sastr N. Survey Research Center, Institute for Social Research University of Michigan; Ann Arbor, Michigan: 2021. Technical report: panel study of income dynamics 2019 PSID cross-sectional individual and family unit weight. [Google Scholar]
- 18.Panel study of income dynamics. Data on children and young adults. Survey Research Center, Institute for Social Research, University of Michigan; Ann Arbor, MI: 2020. https://psidonline.isr.umich.edu/Guide/Brochures/CDS.pdf [Internet] Available from: [Google Scholar]
- 19.Wen M., Kowaleski-Jones L. Sex and ethnic differences in validity of self-reported adult height, weight and body mass index. Ethn Dis. 2012;22(1):72–78. [PMC free article] [PubMed] [Google Scholar]
- 20.Stommel M., Schoenborn C.A. Accuracy and usefulness of BMI measures based on self-reported weight and height: findings from the NHANES & NHIS 2001–2006. BMC Public Health. 2009;9:421. doi: 10.1186/1471-2458-9-421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ezzati M., Martin H., Skjold S., Vander Hoorn S., Murray C.J. Trends in national and state-level obesity in the USA after correction for self-report bias: analysis of health surveys. J R Soc Med. 2006;99(5):250–257. doi: 10.1258/jrsm.99.5.250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Patel S.A., Winkel M., Ali M.K., Narayan K.M., Mehta N.K. Cardiovascular mortality associated with 5 leading risk factors: national and state preventable fractions estimated from survey data. Ann Intern Med. 2015;163(4):245–253. doi: 10.7326/m14-1753. [DOI] [PubMed] [Google Scholar]
- 23.Carstensen B. Age-period-cohort models for the Lexis diagram. Stat Med. 2007;26(15):3018–3045. doi: 10.1002/sim.2764. [DOI] [PubMed] [Google Scholar]
- 24.Hales C.M., Fryar C.D., Carroll M.D., Freedman D.S., Ogden C.L. Trends in obesity and severe obesity prevalence in US youth and adults by sex and age, 2007–2008 to 2015–2016. JAMA. 2018;319(16):1723–1725. doi: 10.1001/jama.2018.3060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ford E.S., Dietz W.H. Trends in energy intake among adults in the United States: findings from NHANES. Am J Clin Nutr. 2013;97(4):848–853. doi: 10.3945/ajcn.112.052662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rehm C.D., Peñalvo J.L., Afshin A., Mozaffarian D. Dietary intake among US adults, 1999–2012. JAMA. 2016;315(23):2542–2553. doi: 10.1001/jama.2016.7491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vaupel J.W., Yashin A.I. Heterogeneity’s ruses: some surprising effects of selection on population dynamics. Am Stat. 1985;39(3):176–185. doi: 10.1080/00031305.1985.10479424. [DOI] [PubMed] [Google Scholar]
- 28.Neumark-Sztainer D., Wall M.M., Chen C., Larson N.I., Christoph M.J., Sherwood N.E. Eating, activity, and weight-related problems from adolescence to adulthood. Am J Prev Med. 2018;55(2):133–141. doi: 10.1016/j.amepre.2018.04.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Larson N.I., Neumark-Sztainer D.R., Story M.T., Wall M.M., Harnack L.J., Eisenberg M.E. Fast food intake: longitudinal trends during the transition to young adulthood and correlates of intake. J Adolesc Health. 2008;43(1):79–86. doi: 10.1016/j.jadohealth.2007.12.005. [DOI] [PubMed] [Google Scholar]
- 30.Flegal K.M., Kruszon-Moran D., Carroll M.D., Fryar C.D., Ogden C.L. Trends in obesity among adults in the United States, 2005 to 2014. JAMA. 2016;315(21):2284–2291. doi: 10.1001/jama.2016.6458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Power C., Thomas C. Changes in BMI, duration of overweight and obesity, and glucose metabolism: 45 years of follow-up of a birth cohort. Diabetes Care. 2011;34(9):1986–1991. doi: 10.2337/dc10-1482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Flegal K.M., Carroll M.D., Ogden C.L., Curtin L.R. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303(3):235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 33.Cheng F.W., Gao X., Mitchell D.C., Wood C., Still C.D., Rolston D., et al. Body mass index and all-cause mortality among older adults. Obesity (Silver Spring) 2016;24(10):2232–2239. doi: 10.1002/oby.21612. [DOI] [PubMed] [Google Scholar]
- 34.Flegal K.M., Shepherd J.A., Looker A.C., Graubard B.I., Borrud L.G., Ogden C.L., et al. Comparisons of percentage body fat, body mass index, waist circumference, and waist-stature ratio in adults. Am J Clin Nutr. 2009;89(2):500–508. doi: 10.3945/ajcn.2008.26847. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data were accessed via the PSID website. PSID data are freely available for all registered users at the PSID website (https://psidonline.isr.umich.edu; accessed January 2020).