Abstract
Objective:
This umbrella review provides an overview of the consistency and gaps in the evidence base on eggs and cardiometabolic health.
Design:
PubMed, Web of Science, Cochrane Library, the Nutrition Evidence Systematic Review and Agency for Healthcare Research and Quality databases were screened for evidence-based reviews in English that assessed human studies on egg consumption and cardiometabolic outcomes.
Results:
Seven systematic reviews and fifteen meta-analyses were identified, with eighteen of these published since 2015. Overall, the systematic reviews were of low quality, while meta-analyses were of moderate- to high-quality. No association of increased egg intake and risks of heart disease or stroke in the general population were found in the meta-analyses. Increased risk of heart failure was noted in two meta-analyses that analysed the same three cohort studies. Five recent meta-analyses reported no increased risk of type 2 diabetes mellitus (T2DM) in the general population, although increased risk in US-based populations only has been reported. Older (<2013) meta-analyses reported increased risks of cardiovascular disease (CVD) or heart disease in T2DM populations, and no recent evidence-based reviews were identified. Finally, only one meta-analysis reported intervention studies specifically on eggs and biomarkers (i.e. lipids), and the results contradicted those from observation studies.
Conclusions:
Recent evidence-based reviews conclude that increased egg consumption is not associated with CVD risk in the general population. More research is needed on the positive associations between egg consumption and heart failure and T2DM risk, as well as CVD risk in diabetics, before firm conclusions can be made.
Keywords: Metabolic syndrome, Stroke, Hypertension, Observational, Clinical, RCT
The growing prevalence of cardiometabolic disease, which includes CVD, stroke, and type 2 diabetes mellitus (T2DM)(1,2), is a leading concern for policymakers in the United States and globally(3). While the US Burden of Disease Collaboration has reported that a decrease has been observed in some aspects of CVD over the past two decades, other components have increased(4). Specifically, ischemic heart disease (IHD) and ischemic stroke were the first and tenth leading causes of mortality in 2016, accounting for 544 800 and 113 300 deaths, respectively(4). Moreover, diabetes incidence increased from the twelfth to the eighth cause of death between 1990 and 2016, and was the third highest cause for disability in 2016, behind low-back pain and major depressive disorders(4). Individuals with T2DM are also at higher risk for CVD(5). While the pathogenesis of cardiometabolic disease is multifactorial, diet has been identified as a major risk factor, and was implicated in 529 299 US deaths in 2016, with >85 % due to CVD and diabetes(4).
It is now clear that diet plays an important role in risks of CVD and diabetes, but elucidating the impact of specific dietary factors is challenging, primarily due to the slow manifestation of these diseases and the complex interactions among nutrients. Therefore, much past work has focused on diet and biomarkers, such as total cholesterol (tChol), low-density lipoprotein cholesterol (LDL-C), ratio of LDL-C to high-density lipoprotein cholesterol (HDL-C), and blood glucose. For example, a strong relationship has been established between LDL-C and risk of CVD, with the data supporting that a 1 mmol/l reduction in LDL-C is associated with a 20 % reduction in coronary artery disease (CAD)(6). This has led to past US Dietary Guidelines emphasizing a reduction of dietary cholesterol(7).
Egg yolks are among the cholesterol-rich foods, delivering around 141 and 234 mg of cholesterol per one chicken egg, depending on the size, and, therefore, past dietary guidelines have included limiting egg consumption. However, more recent data have suggested that dietary cholesterol is not a major contributor to tChol and LDL-C increases, with other factors in foods, primarily saturated and trans fats, playing a larger role(7,8). Furthermore, blood cholesterol is under tight homeostasis, mainly regulated by the endogenous cholesterol synthesis in the liver(9). Thus, in line with this, the 2015–2020 US Dietary Guidelines(10) removed the limit on dietary cholesterol although the policy continued to emphasize that cholesterol intake should be kept as low as possible. Further, the policy stated that, although egg yolk is high in cholesterol, eggs being a nutrient dense food can be consumed as part of a healthy diet ‘along with a variety of other choices and within and across the subgroup recommendations of the protein food groups’.
Early reviews of intervention studies on eggs and blood lipids (e.g. LDL-C) often combined data from low-cholesterol diets, such as decreasing saturated fat-containing meats along with eggs(11). Given that eggs are low in saturated fat (1·56 g per large chicken egg) and contain components that may decrease risk of certain cardiometabolic diseases, combining data on eggs with saturated fat-rich foods may not reflect the actual effect of eggs alone on health outcomes(12). Indeed, in contrast to the intervention studies that measured biomarkers, prospective cohort studies that assessed cardiometabolic disease outcomes reported associations of eggs with either decreased or null risks in the general population(13). Data from sub-groups of prospective studies, however, have been inconsistent, particularly in diabetics(12,13). Although numerous reviews on eggs and health have been published, most are narrative and, until recently, only a few systematic reviews and meta-analyses on the effect of eggs on cardiometabolic-related health outcomes have become available(14,15).
Given the role of eggs in delivering important nutrients, as well as the recent change in the policy on dietary cholesterol, renewed discussions on eggs and health have occurred in the literature(9,16). In addition, within the last two years, numerous evidence-based reviews have also been published. The objective of this umbrella review was to assess the totality of the evidence-based literature on the dietary consumption of eggs and cardiometabolic health in order to understand the areas of consensus, as well as the gaps in the existing evidence.
Materials and methods
Literature search and selection criteria
The literature search and reporting followed the standards of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA), and was conducted independently by two authors (DL, OC). The initial search was conducted in the PubMed (MEDLINE) database for reviews published from inception through 3 October 2018 with terms that included egg and eggs with dietary, consumption, intake or food (see Supplemental Table S1a). An updated search in PubMed (MEDLINE) was conducted on 29 April 2019, along with searches in Web of Science (WOS), Cochrane Library, the Nutrition Evidence Systematic Review (NESR), formerly the Nutrition Evidence Library (NEL), and Agency for Healthcare Research and Quality (AHRQ) EPC Evidence-Based Reports. Only studies that incorporated a systematic literature search, or were designated as systematic reviews or meta-analyses, and that were published in English and included assessment of studies conducted in humans were included. In addition, only studies that provided specific data on egg consumption were included. Studies on cancer, immune and allergy-related outcomes, and reproduction, as well as reviews not including studies conducted in humans, were excluded. Additional hand-searching and review of reference lists from the recent narrative reviews were also conducted, as well as ad hoc searches on Google.
Data extraction and analysis
The following were extracted from each review by two investigators (EM and DL) and reviewed by a third (OC): (i) first author name and year of publication; (ii) objective of the review; (iii) databases used for the search and years of publications covered in the review; (iv) general search terms and selection criteria; (v) number and type of studies included in the assessment; (vi) specific references/studies used by the authors for their assessments. For each systematic review, additional extracted information included: (vii) the authors’ conclusions; and (viii) limitations noted by the authors. For each meta-analysis, additional data extracted included (ix) the statistical analysis approach; and (x) the most adjusted and study-specific estimates for relative risk (RR) or hazard ratio (HR) with 95 % CI. Given that this review covers disparate endpoints of cardiometabolic health, no formal data analysis was conducted. However, outcomes of each meta-analysis were compared qualitatively, and the data used for each study compared to assess the amount of independent data that was included and level of independent analyses.
Quality of the reviews
Adherence to reporting quality of each review was assessed using the PRISMA checklist (http://www.prisma-statement.org/). Results for each review were expressed as a percentage of the required items, which included twenty-four for meta-analyses and nineteen for systematic reviews. Methodological quality was assessed using the Risk of Bias in Systematic Reviews (ROBIS; https://www.bristol.ac.uk/population-health-sciences/projects/robis/robis-tool/) assessment tool and the AMSTAR2 checklist (https://amstar.ca/Amstar-2.php). For quality assessments of systematic review using the ROBIS tool, the checklist items were adjusted to remove the elements not applicable to non-meta-analyses (i.e. item 13, identification of principal summary measures; item 14, description of methods of handling data and combining results of studies; item 15, description of assessment of risk of bias that may affect the cumulative evidence; item 21, reporting of results of each meta-analysis; and item 22, reporting of results of any assessment of risk of bias across studies). The score was adjusted accordingly with low, unclear, and high bias results indicated per each review, and a conclusion of low bias indicating higher quality. The AMSTAR2 checklist included sixteen items, with three items not applicable to systematic reviews (i.e. item 11, use of appropriate methods for meta-analysis; item 12, assessment of risk of bias in individual studies for meta-analysis; and item 15, inclusion of small study publication bias and the impact on the results). The original AMSTAR2 does not provide an overall score; however, subsequent validation papers(17,18) awarded each item scoring ‘yes’ one point and summed these to calculate an overall score. We modified this approach by adjusting the sum to a percentage, based on the maximum attainable points of 13 and 16 for systematic reviews and meta-analyses, respectively. Adherence to reporting quality and methodological quality scoring was conducted independently by two investigators (EM and OC) and scoring details for individual reviews are provided in supplemental materials (Supplemental Table S2).
Selection and characteristic of reviews
Search and selection results
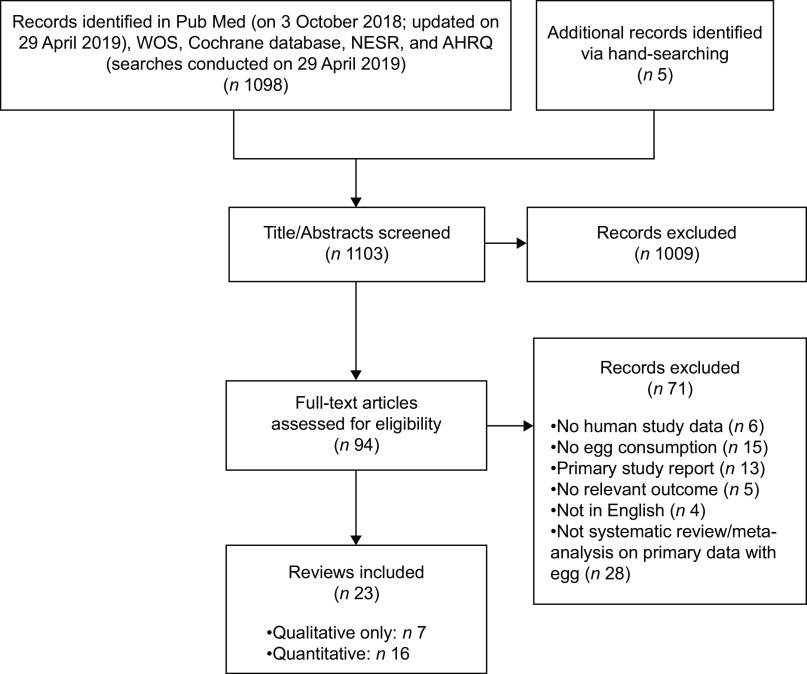
The search returned 1098 references and 1009 of these were excluded based on abstract screening (Fig. 1). A further seventy-one were excluded based on full-text screening (Supplemental Table S1b). A total of twenty-three reviews were included, of which seven were reviews utilizing systematic approaches, but without meta-analysis, and sixteen were meta-analyses of at least one cardiometabolic-relevant outcome.
Fig. 1.
PRISMA diagram
Of the seven reviews utilizing systematic approaches, three were on eggs and a relevant outcome(19-21), two represented comprehensive assessments but not full systematic reviews(22,23), and two were separate reports of the same search strategy and outcome relationship by the same author(24,25) and are, thus, considered together. Therefore, overall, six independent reviews were identified (Table 1). Three of the reviews included both prospective cohort and intervention studies(21-23), whereas one reported on intervention studies only(20) and three included only prospective cohort studies(19,24,25).
Table 1.
Characteristics of systematic and comprehensive narrative reviews on egg intake and CVD and/or diabetes
| Reference | Objective | Database/Publication years | Search terms*/Inclusion criteria | Included studies | Conclusions | Quality Rating† |
|---|---|---|---|---|---|---|
| Geiker et al. 2018(22) | Assess the recommendation to lower the dietary intake of cholesterol and especially the intake of egg to reduce the risk of CVD and T2DM |
Database: nr Years: within last 10 y of April–May 2015 (also included past MAs) |
Terms: egg, cholesterol, diabetes, cardiovascular Criteria: human studies published in English investigating the effect of egg consumption on risk markers of CVD or T2DM |
Sixteen PC and five other observational studies (sixteen CVD, six T2DM) Twenty-three intervention studies, all on CVD or relevant biomarker (e.g. blood lipids) |
≤7 eggs per week can safely be consumed, but in patients with established CVD or T2DM only with special emphasis on a healthy lifestyle. Intervention studies have not reported associations between increased egg consumption and risk markers for CVD and T2DM, whereas observational studies have found associations. Risk association in observational studies are more likely to be attributed to diet and lifestyle patterns and/or clusters of other risk factors in high-egg consumers. | PRISMA: 58 % ROBIS: Unclear Bias AMSTAR2: 15 % |
| Park et al., 2018(23) | Summarize the literature on egg consumption and the risk of metabolic disease. |
Database: PubMed, Embase Years: published through Dec. 2017 |
Terms: egg intake, egg consumption, metabolic syndrome, CHD, CVD, diabetes mellitus Criteria: nr |
Five RCT (three T2DM/MetS, two biomarkers); eighteen PC (nine T2DM/MetS, eight CVD or related, one both); three cross-sectional (two T2DM/MetS, one CVD) |
The literature review found conflicting results, with all three cross-sectionals, ten PC studies, and all five RCTs showing evidence of null effect or decreased risk to metabolic diseases, while eight of the PC studies reported an increased risk to one or more metabolic disease outcome. (Note: A cross-sectional study was also reported within this publication and only data from the literature review is reported herein). | PRISMA: 58 % ROBIS: Unclear Bias AMSTAR2: 8 % |
| Mente et al., 2009(19) | Evaluate dietary exposures and CHD using Bradford Hill criteria, identify dietary exposures that have sufficient RCT data to support the PC findings, and determine those that have insufficient evidence for conclusions |
Database: MEDLINE Years: 1950 through June 2007 |
Terms: nr Criteria: RCT or PC study published in English on diet and heart disease that reported RR and CI after adjustment for confounders. PC had to include estimates of dietary intake and have ≥1 y follow-up. RCTs had to compare dietary intervention with a control or placebo. |
Six cohorts, representing 258, 221 patients, details nr | Weak evidence of causality for eggs and CHD, with only one of four Bradford Hill criteria met for potential causal relationship with coronary outcomes and secondary events. No evidence of linear dose-response relationship was found. | PRISMA 79 % ROBIS: High Bias AMSTAR2: 31 % |
| Kerley CP 2018(24); Kerley CP 2018(25) |
Provide a comprehensive summary of the current evidence regarding dietary patterns/components and HF |
Database: MEDLINE, CINAHL, EMBASE, Cochrane Years: published through Oct. 2017 |
Terms: heart failure, numerous dietary components, specific diets (e.g. paleo, Mediterranean, PREDIMED, DART, DASH, etc.) Criteria: human, non-pharma with HF outcome; excluded salt/Na, alcohol, fluid restriction, micronutrient supplementation, over- or undernutrition |
Three PC on HF and eggs | Two of the three PC studies reported a positive association between risk of HF and egg consumption, while the other was null. Data were consistent with a previous MA that reported an elevated risk of HF with higher egg consumption. | PRISMA: 47 %; 32 % ROBIS: High Bias; High Bias AMSTAR2: 8 %; 15 % |
| Richard et al. 2017(20) | Assess the impact of egg consumption on CVD risk factors in individuals with T2DM or at risk of developing T2DM (e.g. prediabetes, insulin resistance or having MetS) | Database: PubMed, MEDLINE, EMBASE, Web of Science Years: through January 2017, with updated search on July 2017 |
Terms: egg, diabetes, glucose, insulin, MetS, blood lipids, CRP Criteria: published in English, RCTs, eggs as sole dietary manipulation, biomarkers of glycaemic control and/or CVD risk, intervention at least 4 weeks |
Ten intervention studies (seven MetS/ prediabetes; three T2DM) | Results from RCTs suggest that consumption of 6–12 eggs/week, in the context of a diet that is consistent with guidelines on CV health promotion, has no adverse effect on major CVD risk factors (e.g. tChol, LDL-C, TG, FBG, insulin, CRP) in individuals at risk for developing diabetes or with T2DM, with some evidence for an increase in HDL-C. However, studies were heterogeneous in design, population, and interventions, preventing firm conclusions. | PRISMA: 89 % ROBIS: Low Bias AMSTAR2: 38 % |
| Tran et al. 2014(21) | Review epidemiological and experimental evidence on the relationship between egg consumption and CVD risks among T2DM individuals, and T2DM risk in non-diabetic subjects |
Database: PubMed Years: through Nov. 2013 |
Terms: egg(s), diabetes, MetS, glucose, insulin, stroke, myocardial, atherosclerosis, CVD, CHD, CAD, dietary cholesterol, blood lipids Criteria: human studies published in English, for intervention included egg or dietary cholesterol consumption and biomarkers of CHD or T2DM in adults ≥19 y |
Seven PC on egg and CVD risk in diabetics; ten observational (nine reports) on egg and T2DM risk; six intervention studies on egg and CHD risk in diabetics; nine intervention studies on egg and CVD/ T2DM markers in non-diabetics |
Significant association between egg consumption and CVD and mortality in T2DM subjects, and some evidence for an association between incident T2DM, but lack of adjustment for dietary confounders was common. Limited evidence from experimental studies was identified. Studies among healthy individuals found suggestive evidence that dietary interventions that included eggs may reduce the risk of T2DM and MetS. Overall, heterogeneity in study design and populations, small sample sizes, and lack of control for confounders limited conclusions. | PRISMA: 63 % ROBIS: High Bias AMSTAR2: 15 % |
CAD, coronary artery disease; CRP, C-reactive protein; CV, cardiovascular; FBG, fasting blood glucose; HDL-C, high-density lipoprotein cholesterol; HF, heart failure; LDL-C, low-density lipoprotein cholesterol; MA(s), meta-analysis(es); MetS, metabolic syndrome; nr, not reported; PC, prospective cohort; PRISMA, preferred reporting items for systematic reviews and meta-analyses; RCT, randomized controlled trial; ROBIS, risk of bias in systematic reviews; RR, relative risk; T2DM, type-2 diabetes mellitus; tChol, total-cholesterol; TG, triglycerides.
Terms summarized for comparison of scope or search. See specific reports for full list of search terms and combinations.
Details on PRISMA, ROBIS, and AMSTAR2 assessments are provided in the methods section. Briefly, AMSTAR2 checklist items were scored at 1-point if present and zero if missing, and final assessment scores were presented as a percentage of adjusted the maximum attainable scores (19 and 13 points, respectively), with a higher score indicating a higher quality. ROBIS assessments for systematic reviews did not include Domain 4, as it was not applicable to non-meta-analyses, and the overall assessment was adjusted accordingly, with low risk of bias indicating higher quality. Finally, adherence to the PRISMA checklist was presented as a percentage of the maximum attainable scores (19 for systematic reviews).
The fifteen meta-analyses (Table 2) included nine reports of studies on risk of a relevant CVD outcome (e.g. heart disease, hypertension (HTN), heart failure (HF), and stroke) in the general population from prospective cohort data(14,15,26-31), and two meta-analyses included data from intervention studies on CVD risk factors (i.e. lipid biomarkers and obesity)(32,33). Three of these meta-analyses also included data on CVD risk in T2DM populations(14,15,29). Finally, two of these meta-analyses, along with five other meta-analyses, included data on risk of T2DM in the general population as well(14,15,34-38).
Table 2.
Characteristics of meta-analyses on egg intake and CVD and/or type 2 diabetes
| Reference | Objective | Database/Publ. years | Search terms*/Inclusion criteria | Included Studies | Statistical Analysis | Results | Quality rating† |
|---|---|---|---|---|---|---|---|
| Xu et al. 2018(39) | Update MAs on the associations of egg consumption with all-cause mortality and CVD-specific outcomes. |
Database: PubMed/MEDLINE Years: Jan. 2013–Aug. 2016. (to update previous MA by Li et al. 2013) |
Terms: egg, IHD, CHD, stroke, MI, CAD, all-cause, mortality Criteria: PC studies investigating egg intake and risk of IHD, stroke, or all-cause mortality |
Nine PC on IHD, nine PC on all stroke, five PC on haemorrhagic stroke, six PC on ischemic stroke. |
RR comparing highest to lowest intakes; fixed effect model when heterogeneity was low and random effects model when heterogeneity was high; Stata version 14.0 | No significant association of 7+ egg/week v. <1 egg/week for mortality from CVD [HR: 0·99 (0·76, 1·27)], IHD [HR: 0·92 (0·63, 1·36)], or stroke, [HR: 0·88 (0·57, 1·35)]. 7+eggs/week was not associated with risk of IHD [HR:0·97 (0·90, 1·05), ischemic stroke [HR: 0·91 (0·82, 1·01), or haemorrhagic stroke [HR: 0·88 (0·68, 1·14)], but a small reduction in risk of total stroke [HR: 0·91 (0·85, 0·98)]. | PRISMA: 79 % ROBIS: Low Bias AMSTAR2: 25 % |
| Zhang et al. 2018(31) | Examine the associations of red meat, poultry, and egg consumption with the risk of HTN |
Database: PubMed, Web of Science, Embase Years: through August 2017 |
Terms: HTN, blood pressure, meat, poultry, egg, poultry, cohort, incidence Criteria: PC studies reporting on red meat (unprocessed or processed), poultry, or egg intake and HTN |
Three PC on egg | Compared the highest to lowest egg intake; Stata version 11 | Egg consumption was significantly associated with lower risk of HTN [RR 0·79 (0·68, 0·91)]. | PRISMA: 96 % ROBIS: Low Bias AMSTAR2: 56 % |
| Bechthold et al. 2017(27) | Synthesize the data on twelve major food groups (whole grains, refined grains, vegetables, fruits, nuts, legumes, eggs, dairy, fish, red meat, processed meat, and sugar-sweetened beverages) and the risk of CHD, stroke, and HF |
Database: PubMed, Embase Years: through March 2017 (cross-referenced studies in other SR/MAs) |
Terms: food, whole grain, refined grain, cereal, pasta, rice, potato, vegetable, fruit, nut, legume, bean, egg, dairy, milk, yogurt, cheese, fish, seafood, meat, sugar sweetened beverage, CV, coronary, stroke, vascular, MI, HF Criteria: PC reporting association for at least one food group of interest in adults (≥18 y) and a CV outcome |
Eleven PC on CHD‡ten PC on stroke‡,§
four PC on HF‡ |
Compared different levels of intakes with Greenland and Longnecker method; random-effects model; Review Manager 5.3 and Stata version 14 software. | No association of egg intake and CHD risk [RR: 0·99 (0·94, 1·05)] or stroke [RR: 0·99 (0·93, 1·05)]. Positive association of egg intake and HF risk [RR: 1·25 (1·12, 1·39)]. No association for 50 g increments of daily egg intake and CHD risk [RR: 1·00 (0·95, 1·06)] or stroke [RR: 0·99 (0·93, 1·05)], but association with HF risk [RR: 1·16 (1·03, 1·31)]. | PRISMA: 100 % ROBIS: Low Bias AMSTAR2: 63 % |
| Khawaja et al. 2017(28) | Examine the association of egg consumption with incident HF in humans |
Database: PubMed, Cochrane, Google Scholar Years: published through May 2016. |
Terms: eggs, nutrition, heart failure Criteria: human, population-based PC published in English that compared incident HF event rates between two or more groups of egg intake |
Four PC on HF‡ | RR comparing the highest to the lowest category of egg consumption, random effects model, Comprehensive Meta-Analysis version 2.2.064 | Frequent egg intake (≥1/d) associated with increased HF incidence [RR: 1·25 (1·12, 1·39)]. | PRISMA: 83 % ROBIS: Low Bias AMSTAR2: 25 % |
| Schwingshackl et al. 2017(30) | Summarize the evidence on the relation of the intakes of twelve major food groups: whole grains, refined grains, vegetables, fruits, nuts, legumes, eggs, dairy, fish, red meat, processed meat, and sugar-sweetened beverages (SSB) with the risk of HTN. |
Database: PubMed, Scopus, Web of Science, Google Scholar Years: Published through June 2017 |
Terms: grain (whole, refined, etc.) cereal, vegetable, fruit, nut, legume, bean, egg, dairy, fish, seafood, meat, SSB, HTN, MetS, blood pressure Criteria: prospective, peer-reviewed, full-text available, includes ≥1 selected food group and HTN risk |
1 PC | RR comparing highest v. lowest egg intake; Random effect model; Dose-response analysis per Greenland and Longnecker; Review Manager 5.3 and Stata version 14 | Inverse association for highest v. lowest egg intake with HTN incidence [RR: 0·54 (0·32, 0·91)], or for each additional of 50 g/d [RR: 0·25 (0·08, 0·74)]. | PRISMA: 100 % ROBIS: Low Bias AMSTAR2: 56 % |
| Alexander et al. 2016(26) | Conduct an updated, comprehensive meta-analysis to estimate summary associations between egg consumption and CHD and stroke risk based on high v. low intakes |
Database: PubMed, Embase, Cochrane Years: published through August 2015.(update of Shin et al. 2013) |
Terms: eggs, dietary cholesterol, CVD, CHD, IHD, CAD, MI, HF, cerebrovascular, stroke, cholesterol Criteria: human PC or RCT published in English with RR and measures of variance for egg intake CV outcomes including CHD or stroke |
Nine PC on stroke§,||,¶, eight PC on CHD||,¶,** |
RR comparing highest v. lowest intake, Random-effects models, dose–response analysis, Comprehensive MA Software version 3.2.00089 | Consumption of approximately one egg a day was not associated with CHD risk [SRRE: 0·97 (0·88, 1·07)] and was instead, associated with decreased risk of stroke [SRRE: 0·88 (0·81, 0·97)]. | PRISMA: 88 % ROBIS: Low Bias AMSTAR2: 44 % |
| Rong et al. 2013(29) | To investigate and quantify the potential dose-responseassociation between egg consumption and risk of coronary heart disease and stroke |
Database: PubMed, Embase Years: Published prior to June 2012 |
Terms: CVD, CHD, MI, stroke, coronary disease, egg Criteria: PC on egg consumption and CHD or stroke relevant outcome reporting risks with 95 % CI for at least three quantitative categories of egg intake |
General population: seven PC on CHD||,¶,**, seven PC on stroke§,||. T2DM population: two PC on CHD||,¶, three PC on stroke¶. |
Risks for increases of 1 egg/d; Fixed effect model with negligible heterogeneity, Random effect model with significant heterogeneity; dose-response using Greenland and Longnecker method; Stata version 11.0 | No association of an increase of 1 egg/d with risks of CHD [RR: 0·99 (0·85, 1·15), total stroke [RR: 0·91 (0·81, 1·02)], fatal stroke [RR: 0·94 (0·80, 1·10)], or ischemic stroke [RR: 0·91 (0·82, 1·01)]. Increase of 1 egg/d significantly decreased haemorrhagic stroke risk [RR: 0·75 (0·57, 0·99)]. In T2DM population, increase of 1 egg/d significantly increased CHD risk [RR: 1·54 (1·14, 2·09)]. No significant effect of 1 egg/d increase on total stroke [RR: 0·80 (0·29, 2·15)]. |
PRISMA: 92 % ROBIS: Low Bias AMSTAR2: 63 % |
| Shin et al. 2013(15) | Quantitatively summarize the literature on egg consumption and risk of CVD, cardiac mortality, and type 2 diabetes | Database: PubMed, Embase Years: Published through March 2012 |
Terms: egg, CVD, CHD, MI, stroke, mortality/death, diabetes mellitus Criteria: human PC study published in English reporting HR with 95 % CI on egg intake (as per egg or g/d, not continuous) and CVD, mortality, or T2DM providing |
General population: two PC on CVD, five PC on IHD**, five PC on stroke, five PC on T2DM. T2DM population:four PC on CVD††. |
HRs comparing highest v. lowest egg intake; Random-effects model; Stata version 11 | No significant effect of high egg intake (≥1 egg/d) on risks of overall CHD [HR: 0·96 (0·88, 1·05)], IHD [HR: 0·97 (0·86, 1·09)], stroke [HR: 0·93 (0·81, 1·07)], IHD mortality [HR: 0·98 (0·77, 1·24)], or stroke mortality [HR: 0·92 (0·56, 1·50)]. In T2DM population, significant association of high egg intake with increased overall CVD risk [HR: 1·69 (1·09, 2·62). Increased risk for T2DM with high egg consumption [RR: 1·68 (1·41, 2·00)]. |
PRISMA: 92 % ROBIS: Low Bias AMSTAR2: 44 % |
| Li et al. 2013(14) | Assess the dose-response relationship between egg consumption and the risk of CVD and diabetes |
Database: MEDLINE Years: Published through Dec 2012 |
Terms: egg or egg consumption, diet cholesterol, CVD, diabetes, mortality, coronary heart disease, heart failure Criteria: cohort, case-control or cross-sectional on CVD (e.g. CHD, IHD, HF) or diabetes risk, reporting multi-variable adjusted risks with 95 % CI using lowest egg intake as reference; excluded studies in special populations (e.g. pregnant women) |
General population: ten PC¶,** and one cross-sectional on CVD, three PC‡‡,§§, one cross-sectional‖‖, and one case-control on T2DM. T2DM population: six PC** on CVD. |
RR of highest v. lowest egg intake; Fixed effect model with negligible heterogeneity, Random effect model with significant heterogeneity; dose-response using Greenland and Longnecker method; Stata version 10.0 | Significant association of high v. low egg intake on increased CVD risk [RR: 1·19 (1·02, 1·38)]. In T2DM population, significant association of high egg intake with increased overall CVD risk [RR: 1·83 (1·42, 2·37)]. Increased T2DM risk with high egg intake [HR: 1·42 (1·09, 1·86)]. No differences between studies conducted in US v. non-US populations. |
PRISMA: 88 % ROBIS: High Bias AMSTAR2: 44 % |
| Djousse et al. 2016(34) | Evaluate the relation of egg consumption with the risk of T2DM |
Database: PubMed, Ovid, Cochrane, Google Scholar Years: Published through October 2015. |
Terms: egg(s), diabetes/ diabetic Criteria: human PC studies published in English and reporting association between egg intake and incident T2DM |
Nine PC‡‡,§§,‖‖,¶¶ | RR comparing highest v. lowest egg intake; Both fixed and random estimates of effects; Stata version 13.1 | No association of high (<4 eggs/week) egg intake with T2DM risk [RR: 1·09 (0·99, 1·20, fixed-effect; RR: 1·06 (0·86, 1·30, random-effect]. Stratified analysis showed increased T2DM risk with ≥3 eggs/week for US-based studies [RR: 1·39 (1·21, 1·60)], but not in non-US-studies [RR: 0·89 (0·79, 1·02)]. | PRISMA: 88 % ROBIS: Low Bias AMSTAR2: 31 % |
| Tamez et al. 2016(36) | Quantify the association betweenhabitual egg intake and risk of T2DM |
Database: MEDLINE, Embase, EBSCOhost Years: Published through June 2015. |
Terms: egg(s), animal food, diabetes mellitus, diabetes Criteria: PC studies reporting multi-variable-adjusted RR on egg intake and T2DM risk in adults |
Twelve PC‡‡,§§,***,††† | RR for an increased intake of one egg per day for each report, random-effects model, Stata 11.2 for Mac | Increases of 1 egg/d associated with 13 % higher T2DM risk [RR: 1·13 (1·32, 1·64)]. Stratified analysis indicated 47 % higher risk with US studies [RR: 1·47 (1·32, 1·64)], but not significant for non-US studies [RR: 0·95 (0·83, 1·10)]. | PRISMA: 92 % ROBIS: Low Bias AMSTAR2: 63 % |
| Wallin et al. 2016(38) | Summarize available prospective evidence on the association between egg consumption and T2DM risk | Database: PubMed Years: Published through December 2015. |
Terms: egg, diabetes Criteria: PC studies reporting T2DM risk estimates by egg intake amounts |
13 PC‡‡,§§,‖‖,¶¶ | HR for each 3×/week egg increments; Random-effects model, Stata (version not reported) | No association between 3 eggs/week and T2DM [HR: 1·03 (0·96, 1·10)] overall, but significant when only studies in US included in analysis [HR: 1·18 (1·13, 1·24)] v. non-US studies [HR: 0·97 (0·90, 1·05)]. | PRISMA: 88 % ROBIS: High Bias AMSTAR2: 38 % |
| Tian et al. 2017(37) | Clarify the association of protein consumption with risk of T2DM | Database: PubMed, Embase Years: Published through 2017 | Terms: protein (dietary, plant, animal), diabetes, T2DM, human, red meat, processed meat, fish, seafood, egg, dairy, milk, yogurt, soy, legume, soy Criteria: cohort on T2DM incidence or mortality reporting RR and 95 % CI, intakes of dietary protein or other high-protein foods such as meat, fish, egg, dairy, soy |
6 PC‡‡,§§ | Summary RRs and 95 % CI comparing highest to lowest dietary protein intakes; Fixed model with no heterogeneity; Random model heterogeneity present; Comprehensive MA V2 | High v. low egg intakes were not associated with T2DM risk [RR: 1·03 (0·64, 1·67)]. | PRISMA: 88 % ROBIS: Low Bias AMSTAR2: 31 % |
| Schwingshackl et al. 2017(35) | Synthesize the knowledge about the relation between intake of twelve major food groups and risk of T2DM |
Database: PubMed/ MEDLINE (Ovid), Embase, Cochrane Central, Google Scholar Years: Published through Feb. 2017 |
Terms: grain (whole, refined, etc.) cereal, vegetable, fruit, nut, legume, bean, egg, dairy, fish, seafood, meat, SSB, diabetes Criteria: prospective, peer-reviewed, full-text available, includes ≥1 selected food group and T2DM risk; subjects ≥18 y free of T2DM at onset |
13 PC‡‡,§§ | RR comparing highest v. lowest egg intake; Random effect model; Dose-response analysis per Greenland and Longnecker; Review Manager 5.3 and Stata version 14 | No significant association for highest v. lowest egg intake [RR: 1·08 (0·95, 1·22)], or for each additional of 30 g/d [RR: 1·08 (0·95, 1·22)] with T2DM risk. Positive association for US-only studies in dose–response analysis, but not for Asian and European studies. |
PRISMA: 96 % ROBIS: Low Bias AMSTAR2: 69 % |
| Rouhani et al. 2017(32) | Conduct a meta-analysis of published RCTs to explore the quantitative effect of egg consumption on serum lipid concentrations |
Database: Medline, Proquest, Google Scholar Years: Published from Jan. 1999 to Nov. 2016. |
Terms: egg(s), cholesterol, HDL, LDL, TG, lipoprotein, hypercholesterolemia, Criteria: compared egg intake with egg substitute or no-egg diet for whole eggs (no egg whites only), regular eggs (not enriched), in healthy adults reporting fasting lipid profile (not postprandial lipid) |
27 RCTs | Effect size, Random-effects model, Stata version 11.0. | Significant association of egg intake with increased tChol [ES: 5·60 mg/dl (3·11, 8·09)], LDL-C [ES: 5·55 mg/dl (3·41, 7·69)], and HDL-C [ES: 2·13 mg/dl (1·10, 3·16)]. No significant association for tChol/HDL-C [ES: -0·01 (−0·08, 0·07)], LDL-C/HDL-C [ES: 0·16 (−0·28, 0·59)], or TG [ES: −0·43 mg/dl (−3·77, 2·92)]. | PRISMA: 96 % ROBIS: Low Bias AMSTAR2: 56 % |
| Schlesinger 2019(33) | Investigate the potential associations between twelve predefined food groups, including eggs, and the risk of overweight/obesity, abdominal obesity, and weight gain |
Database: PubMed, Web of Science
Years: Published through Aug. 2018 |
Terms: grain (whole, refined, etc.) cereal, pasta, rice, vegetable, fruit, nut, legume, bean, egg, dairy, yogurt, milk, cheese, fish, seafood, meat, SSB, body weight, obesity, overweight, adiposity, waist circumference, abdominal fat, waist to hip Criteria: prospective, peer-reviewed, full-text available, includes ≥1 selected food group and general overweight/obesity, abdominal obesity, or weight gain; subjects ≥18 y |
1 PC | RR comparing highest v. lowest egg intake; Random effect model; Dose-response analysis per Greenland and Longnecker; Review Manager 5.3 and Stata version 14 | No significant association for highest v. lowest egg intake [RR: 0·97 (0·59, 1·59)], or for each additional of 50 g/d [RR: 0·95 (0·63, 1·43)] with abdominal obesity. | PRISMA: 100 % ROBIS: Low Bias AMSTAR2: 63 % |
CAD, coronary artery disease; CV, cardiovascular; d, day; dL, deciliter; ES, effect size; g, gram; HDL-C, high-density lipoprotein cholesterol; HF, heart failure; HR, hazard ratio; HTN, hypertension; LDL-C, low-density lipoprotein cholesterol; MA(s), meta-analysis(es); mg, milligram; PC, prospective cohort; PRISMA, preferred reporting items for systematic reviews and meta-analyses; RCT, randomized controlled trial; ROBIS, risk of bias in systematic reviews; RR, relative risk; SSB, sugar-sweetened beverage; SR, systematic review; SRRE, summary relative risk estimates; T2DM, type-2 diabetes mellitus; tChol, total-cholesterol; TG, triglycerides.
Terms summarized for comparison of scope or search. See specific reports for full list of search terms and combinations.
Each PRISMA and AMSTAR2 required checklist items were assigned 1 point if reported in the manuscript and 0 if not, with maximum achievable scores of 24 and 16 points, respectively. The scores were adjusted as a percentage of the maximum available points.
Two cohorts (Swedish Mammography Cohort and Cohort of Swedish Men) were analysed separately and included in one report (Larsson et al., 2013).
Two cohorts (Health Professionals Follow-Up Study and Nurses’ Health Study) were analysed separately and included in one report (Bernstein et al. 2012).
Males and females from the same cohort were analysed separately in one report (Nakamura et al. 2004).
Males and females from the same cohort were analysed separately in one report (Scrafford et al. 2010).
Two cohorts (Health Professionals Follow-Up Study and Nurses’ Health Study) were analysed separately and included in one report (Hu et al. 1994).
Males and females from the same cohort were analysed separately in one report (Qureshi et al. 2007).
Two cohorts (Physicians’ Health Study I and Women’s Health Study) were analysed separately and included in one report (Djousse et al. 2009).
Males and females from the same cohort were analysed separately in one report (Djousse et al. 2010).
Males and females from the same sample were analysed separately in one report (Shi et al. 2011).
Males and females from the same cohort were analysed separately in one report (Djousse et al. 2015).
Males and females from the same cohort were analysed separately in one report (Kurotani et al. 2014).
Two cohorts were analysed together and included in one report (Vang et al. 2008).
Systematic reviews
The systematic reviews on egg consumption and cardiometabolic health are described in Table 1. Three of these reviews were generally broad, and included evidence on eggs and risk of cardiovascular-related outcomes and/or T2DM in the general population(19,22,23), with one of these combining data from a primary cross-sectional study in Korean adults with the literature review(23). Two of the reviews focused specifically on CVD risk in individuals with T2DM subjects or at risk of developing diabetes(20,21), while two focused on HF risk only(24,25).
Although most of the systematic reviews had similar study objectives, the number and type of studies included varied widely among reviews. This is likely due to the difference in search dates and eligibility criteria. For example, Tran et al.(21) included studies that not only examined the effect of egg intake, but also dietary cholesterol in general. Meanwhile, Richard et al.(20) selected only studies whereby eggs were the sole aspect of the diet that was manipulated with interventions that were at least four weeks long. In contrast, Geiker et al.(22), which included the most number of studies, had few restrictions on the studies that were included. The systematic reviews that included the fewest studies were those of Mente et al. (six cohorts)(19) and Kerley (three cohorts)(24,25), and the Kerley reviews(24,25) were also the most limited in scope focusing exclusively on HF.
As shown in Table 1, adherence to the PRISMA reporting checklist by the systematic reviews were mostly poor to fair, with Kerley et al.(24,25) having the poorest adherence (<50 %), and Richard et al.(20) and Mente et al.(19) with the best adherence (89 and 79 %, respectively). Methodological quality scores using AMSTAR2 generally followed the PRISMA reporting quality scores as well, with Kerley et al.(24) having one of the lowest AMSTAR2 scores along with Park et al.(23) and Richard et al.(20), and Mente et al.(19) having the highest scores. Risk of bias using ROBIS scoring was low for only one study(20), with unclear bias for another two(22,23). The Kerley reviews(24,25) were rated as having high risk of bias owing to poor ratings for ROBIS Domain 2 (identification and selection of studies) and Domain 3 (data collection and study appraisal), Mente et al.(19) was rated as having high risk of bias owing to poor ratings for ROBIS Domain 1 (study eligibility criteria) and Domain 2, and Tran et al.(21) was rated having high risk of bias owing to poor ratings in ROBIS Domains 1, 2 and 3.
Meta-analyses
The characteristics of the fifteen meta-analyses are provided in Table 2. These reviews covered different aspects of risk of cardiometabolic outcomes, with the vast majority (n 13) of the reviews including only evidence from prospective cohort studies(15,26-31,34-39), while one study included searches for prospective cohorts, case-controls, and cross-sectionals(14) and another included only intervention studies(32). Most meta-analyses estimated RR or HR by comparing the highest category of egg consumption with the lowest for each study.
Seven meta-analyses assessed the effect of egg consumption on CVD outcomes in the general population(14,15,26-29,39) with three also focusing on the T2DM population(14,15,29). Most of these included point estimates for an aspect of cardiovascular health, i.e. coronary heart disease (CHD), HF, myocardial infarction, or IHD (Table 2) while one review combined data on three outcomes (CHD, IHD, and HF)(14). Three meta-analyses only assessed risk factors for cardiometabolic disease, specifically HTN(30,31) and blood lipids(32). Seven assessed the effects of egg consumption on T2DM risk in the general population(14,15,34-38) and calculated point estimates for incidence of T2DM. Additionally, a few meta-analyses(14,26,27,29,30,32,34-36,38) also investigated the dose–response relationship of egg consumption with the respective outcomes.
As shown in Table 2, the majority of the meta-analyses had good adherence to the PRISMA reporting checklist, with three reviews including all 24 reporting requirements(27,30,33), with six additional reviews including at least 90 % of the required reporting items(15,29,31,32,35,36), and seven reviews including ~80 to 90 % of the required items(14,26,28,34,37-39). Methodological quality assessed by AMSTAR2 generally followed that of the PRISMA rating, although scores were lower overall, with the highest quality (addressing 50–70 % of checklist items) found for eight studies(27,29-33,35,36), while six reviews addressed between 30 and 50 % of items(14,15,26,34,37,38), and two reported low quality with less than 30 % of checklist items addressed(28,39). The ROBIS score indicated low bias, representing higher quality, for 13 reviews(15,26-32,34-37,39). Two studies(14,38) were rated as being at high risk for bias due to poor ratings for Domains 2 (identification and selection of studies) and 3 (data collection and study appraisal). Most studies explored potential sources of heterogeneity such as location, sex, length of follow-up, study quality, study design, number of participants, method of assessing dietary intake, age, whether the study controlled for diet or cholesterol level, and type of stroke or CVD. Only one analysis did not report assessing potential sources of heterogeneity(15).
Results
Three of the systematic reviews assessed intervention and observational data across different aspects of cardiometabolic outcomes and presented conclusions based on data in the general population as well as those at risk(21-23). For example, the review of Park et al.(23) addressed coronary heart health broadly as a component of cardiometabolic diseases and noted conflicting results across studies. In general, the only studies that found a positive association between risk of metabolic disease and egg consumption by these authors were prospective cohorts. Meanwhile, RCTs indicated that egg consumption did not affect lipid profile (n 2), inflammatory markers (n 2) or MetS risk (n 1). The Park et al. study(23) also included primary cross-sectional data on the association of egg consumption with risk of MetS, as well as several biomarkers (e.g. HTN, blood lipids), but did not provide details on how the data were combined in support of their conclusions.
Geiker et al.(22) concluded that up to seven eggs can be consumed per week without increasing risk of metabolic conditions in the generally healthy population, but did not conduct a separate meta-analysis. Instead, these authors based their conclusions primarily on five meta-analyses included in discussions below(14,15,26,29,34) as well as a meta-analysis on dietary cholesterol and CVD(40), with the addition of six observational studies in healthy people or subjects at high CVD risk that were not included in the previously published analyses. Geiker et al.(22) cautioned that the conclusion of up to seven eggs per day may not be applicable to people with established CVD or T2DM. Other systematic reviews focused more specifically on a particular cardiometabolic outcome and are, thus, discussed in the appropriate sections below.
Heart disease
Five meta-analyses(15,26,27,29,39) and one systematic review(19) reported on an aspect of coronary heart health separately, while one meta-analysis(14) combined data from all-cause mortality, CHD, IHD, stroke, and HF into one risk analysis (Table 3). Consistency was seen in the conclusions from these reviews for a null effect of eggs on total and fatal CHD, as all as IHD, but not for HF (see below). The datasets assessed in these reports varied but included from seven to eleven cohorts for each assessment (Table 4). For example, with respect to CHD and IHD, the recent reviews by Bechthold et al.(27) and Xu et al.(39) included the most datasets, with eleven and nine cohorts, respectively, and only four of these were in common across the reviews. Mente et al.(19) conducted an analysis of the strength of evidence of the link between dietary factors and CHD (Table 1). Based on nine prospective cohort studies, these authors reported that the overall evidence for eggs and CHD is weak using the Bradford-Hill criteria for strength, consistency, or biological gradient. Additionally, Bechthold et al. rated the level of evidence as having moderate confidence for the effect estimate such that further research may change the effect estimate(27).
Table 3.
Summary of results from meta-analyses
| Li 2013(14) | Shin 2013(15) | Rong 2013(29) | Bechthold 2017(27) | Xu 2018(39) | Alexander 2016(26) | Djousse 2016(34) | Tamez 2016(36) | Wallin 2016(38) | Khawaja 2017(28) | Tian 2017(37) | Schwingshackl 2017(35) | Schwingshackl 2017(30) | Rouhani 2017(32) | Zhang 2018(31) | Schlesinger 2019(33) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| General population | ||||||||||||||||
| CHD, IHD, HF | ↔ | ↔ | ||||||||||||||
| Abdominal obesity | ↔ | |||||||||||||||
| Lipid Biomarkers | ↔ | ↑tChol, ↑HDL-C ↑LDL-C↔TG ↔LDL-C/HDL-C |
||||||||||||||
| Total CHD | ↔ | ↔ | ↔ | ↔ | ||||||||||||
| Fatal CHD | ↔ | ↔ | ||||||||||||||
| IHD | ↔ | ↔ | ||||||||||||||
| HF | ↑ | ↑ | ||||||||||||||
| HTN | ↔ | ↓ | ↓ | |||||||||||||
| Total stroke | ↓ | ↔ | ↔ | ↓ | ↓ | |||||||||||
| Ischemic stroke | ↔ | ↓ | ↔ | ↔ | ||||||||||||
| Haemorrhagic stroke | ↔ | ↔ | ↔ | ↔ | ||||||||||||
| Fatal stroke | ↔ | ↔ | ||||||||||||||
| T2DM | ↑↔US v. non US | ↑ | ↔↑US only | ↔↑US only | ↔↑US only | ↔ | ↔↑US only | |||||||||
| T2DM population | ||||||||||||||||
| CVD | ↑ | ↑ | ↑ | |||||||||||||
| CHD | ↑ | |||||||||||||||
HF, heart failure; HTN, hypertension; T2DM, type 2 diabetes mellitus; US, United States; tChol, total cholesterol; HDL-C, high density lipoprotein-cholesterol; LDL-C, low density lipoprotein-cholesterol; TG, triglyceride.
↔ no change, ↑ increased risk, ↓ decreased risk.
Table 4.
Study selection for reviews on egg intake and heart health outcomes
| Meta-analyses | Systematic reviews | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Reference | Shin 2013(15) | Li 2013(14) | Rong 2013(29) | Alexander 2016(26) | Bechthold 2017(27) | Xu 2018(39) | Khawaja 2017(28) | Park 2008(23) | Tran 2014(21) | Geiker 2018(22) | Kerley† 2018(24,25) |
| Mann et al. Heart. 1997 | X | ||||||||||
| Hu et al. JAMA. 1999 | X* ‡ | X* ‡ | X* | X* | X* | X* | X | X | X | ||
| Nakamura et al. AJCN. 2004 | X* ‡ | X* | X* | X | |||||||
| Tanasescu et al. AJCN. 2004 | X‡ | ||||||||||
| Nakamura et al. BJN. 2006 | X | X | X | X | X | X | |||||
| Burke et al. Prev Med. 2007. | X | X | |||||||||
| Qureshi et al. Med Sci Monit. 2007 | X‡ | X‡ | X‡ | X | X | X | X | X | X | ||
| Nettleton et al. J Am Diet Assoc. 2008 | X | X | X | X | X | ||||||
| Djousse & Gaziano. AJCN. 2008 | X | X | X‡ | X | X | X | X | X | X | X | X |
| Djousse & Gaziano. Circulation. 2008 | X | X | X | X | |||||||
| Bernstein et al. Circulation. 2010 | X | ||||||||||
| Scrafford et al. Publ Health Nutr. 2011 | X* ‡ | X* ‡ | X* | X* | X | X | |||||
| Houston et al. Nutr Metab Cardiovasc Dis. 2011 | X‡ | X‡ | |||||||||
| Dilis et al. Br J Nutr. 2012 | X | ||||||||||
| Goldberg et al. Atherosclerosis. 2014 | X | X | X | ||||||||
| Haring et al. PLoS One. 2014 | X | X | |||||||||
| Larsson et al. AJCN. 2015 | X* | X* | X* | X | X | X | |||||
| Virtanen et al. AJCN. 2016 | X | X | X | ||||||||
| Guangzhou Biobank Cohort Study 2018 | X | ||||||||||
Analysis was performed separately on the male and female cohorts.
Kerley review included discussion of, and reference to, the Khawaja et al., 2017 meta-analysis.
Studies that included data for CVD risk in T2DM population.
Heart failure
Two meta-analyses assessed egg intake and HF(27,28) (Table 3), and both included the same data from three publications that represented four cohorts (Table 4). For the analyses, 105 999 subjects and 5059 cases of new onset HF were included in both analyses, which compared the highest (≥1 egg/d or 140 g/d) to the lowest intake, and both reported a pooled RR of 1·25 (95 % CI, 1·12, 1·39) with 0 % heterogeneity in the data. The meta-analysis conducted by Li et al.(14) included two of these three publications in their assessment of eggs and CVD risk, but did not report data on HF alone. Kerley(24,25) based his reviews of dietary patterns on the same three publications used in these meta-analyses as well, and noted that three of the prospective cohorts(41,42) reported a positive association, whereas a more recent cohort study only found an association in men who consumed >6 eggs weekly, but not in women or diabetics(43). One meta-analysis rated the effect estimate as having a moderate confidence such that further research may change the effect estimate(27).
Stroke
Five meta-analyses addressed eggs and stroke(15,26,27,29,39) with mixed conclusions (Table 3). Of these, Rong et al.(29) and Alexander et al.(26) included nearly identical data, with six studies in common and the latter review including an additional study that was published in 2012 (Table 5). The Bechthold et al.(27) review included the most recent publically available data. In contrast, the review of Xu et al.(39) included most of the earlier publications, along with a new prospective cohort that was presented within the review from the Guangzhou Biobank Cohort Study.
Table 5.
Study selection for reviews on egg intake and cerebrovascular outcomes
| Reference | Shin 2013(15) | Rong 2013(29) | Alexander 2016(26) | Bechthold 2017(27) | Xu 2018(39) |
|---|---|---|---|---|---|
| Hu et al. JAMA. 1999 | X* | X* | |||
| He et al. BMJ. 2003 | X | X | |||
| Sauvaget et al. Int J Epidemiol. 2003 | X | X | X | ||
| Nakamura et al. AJCN. 2004 | X* | X* | X* | ||
| Qureshi et al. Med Sci Monit. 2007 | X | X | X | X | X |
| Djousse & Gaziano. AJCN. 2008 | X | X | X | X | X |
| Scrafford et al. Publ Health Nutr. 2011 | X | X* | X* | ||
| Bernstein. Stroke. 2012 | X* | X* | X* | X* | |
| Misirli et al. Am J Epidemiol. 2012 | X | ||||
| Yaemsiri et al. Ann Neurol. 2012 | X | X | X | ||
| Goldberg et al. Atherosclerosis. 2014 | X | ||||
| Haring et al. Stroke. 2015 | X | ||||
| Larsson et al. AJCN. 2015 | X* | X* | |||
| Guangzhou Biobank Cohort Study 2018† | X |
Analysis was performed separately on the male and female cohorts.
Primary prospective cohort data included as one dataset in the analysis.
Taken together, the Bechthold et al.(27) and Xu et al.(39) reviews include the totality of evidence used in the other three reviews. The Xu et al.(39) study included nine studies that represented fourteen cohorts along with data from the Guangzhou Biobank Cohort Study, and Bechthold et al.(27) included eight publications representing ten cohorts. Xu et al.(39) compared higher (≥7 eggs/week) to low (<1 egg/week) consumers and found a small but significant reduction in stroke (HR: 0·91; 95 % CI, 0·85, 0·98), but no significant effect on mortality from stroke (HR: 0·88; 95 % CI, 0·57, 1·35). Bechthold et al.(27) reported no association of egg with risk of stroke (RR: 0·99; 95 % CI, 0·94, 1·05) for highest (~75 g/d) to lowest (~0 g) intakes. Further, no evidence of a dose-response was found. The other reviews included less evidence, and either reported null effects or similarly small inverse effects on risk of stroke. Furthermore, Bechthold et al. rated the level of confidence for the effect estimate as moderate such that further research may change the effect estimate(27). Therefore, the overall effect of eggs on risk of stroke was either null or slightly favourable, when comparing higher to lower intakes.
Diabetes risk
The meta-analyses on risk of T2DM with egg consumption included only prospective cohort studies, with the exception of Li et al.(14) who included one cross-sectional and one case-control study that were not in the other reviews. Only two primary studies were in common across these meta-analyses (Table 6). Despite being the most recent report, Tian et al.(37) only included five studies, in contrast with the other reviews published in the same year or the year before that included 8–12 studies(34-36,38).
Table 6.
Study selection for meta-analyses on egg intake and type 2 diabetes mellitus risk
| Reference | Location | Shin 2013(15) | Li 2013(14) | Djousse 2016(34) | Tamez 2016(36) | Wallin 2016(38) | Schwingshackl 2017(35) | Tian 2017(37) |
|---|---|---|---|---|---|---|---|---|
| Montonen et al. Eur J Clin Nutr. 2005 | Finland | X | X | X | ||||
| Vang et al. Ann Nutr Metab. 2008 | USA | X | X | X | ||||
| Djousse et al. Diabetes Care. 2009† | USA | X* | X* | X* | X* | X* | X* | X* |
| Djousse et al. AJCN. 2010 | USA | X* | X* | X* | X* | X* | X* | X* |
| Shi et al. Nutrition. 2011† | China | X* | ||||||
| Radzeviciene & Ostrauskas. Public Health Nutr. 2012† | Lithuania | X | ||||||
| Zazpe et al. Nutr Hosp. 2013 | Spain | X | X | X | X | |||
| Kurotani et al. Br J Nutr. 2014 | Japan | X* | X* | X* | X* | |||
| Ericson et al. AJCN. 2015† | Sweden | X | X | X | ||||
| Lajous et al. Br J Nutr. 2015 | France | X | X | X | X | |||
| Virtanen et al. AJCN. 2015 | Finland | X | X | X | X | X | ||
| Djousse et al. Clin Nutr. 2016 | USA | X* | X | X | X | X | ||
| Wallin et al. Diabetologia. 2016 | Sweden | X | X | |||||
| Virtanen et al. Br J Nutr. 2017 | Finland | X | ||||||
| Von Ruesten et al. Eur J Clin Nutr. 2013 | Germany | X |
Analysis was performed separately on the male and female cohorts.
Studies that reported increased risk of T2DM with egg consumption.
For egg intake and T2DM risk in the general population, two older reports(14,15) showed an increased risk for T2DM with high egg consumption. Li et al.(14) compared results between US and non-US studies and did not observe any differences. However, the more recent meta-analyses suggest that egg intake is associated with increased T2DM risk only among studies conducted in the US. Djousse et al.(34) reported that high egg consumption (<4 eggs/week) was not associated with the risk of T2DM in the total population, but a stratified analysis showed an elevated risk of T2DM with consumption of ≥3 eggs/week among US-based studies only. Similarly, Wallin et al.(38) reported that there was no overall association between egg intake of three servings/week and T2DM, but that consumption of three servings/week was positively associated with T2DM risk in studies conducted in the US only. Schwingshackl et al.(35) also reported no significant association with T2DM when the lowest and highest egg intakes were compared and for each additional 30 g/d, but the consumption of 30 g/d was positively associated with T2DM risk in studies conducted in the US, but not in Asia or Europe. Finally, Tamez et al.(36) reported that an increase of one egg/d is associated with 13 % higher risk of T2DM (RR: 1·13 [95 % CI 1·32, 1·64]). When stratified based on location, analysis of studies conducted in the US showed that an egg per day was associated with a 47 % higher risk of T2DM, whereas the association for studies conducted elsewhere was not statistically significant(36). Tian et al.(37) also did not observe any significant effect of egg intake on T2DM risk, but did not perform analysis comparing study locations. One meta-analysis rated the level of confidence for the effect estimate as moderate such that further research may change the effect estimate(35).
CVD risk in people with T2DM
For CVD outcomes in the T2DM population, only one study was included in all three meta-analyses (Table 3). In addition, Shin et al.(15) and Li et al.(14) had two studies in common, while Li et al.(14) and Rong et al.(29) had one study in common. In total, Li et al.(14) included five studies, Shin et al.(15) included four studies, and Rong et al.(29) included four studies. These three meta-analyses all found an increased risk for cardiovascular-related diseases with high egg consumption. Shin et al.(15) and Li et al.(14) both reported that high egg intake was significantly associated with increased overall CVD risk among T2DM population. Rong et al.(29) observed a RR:1·54 (95 % CI, 1·14, 2·09) for CHD with diabetes.
Based on their review of intervention studies, Richard et al.(20) reported that consumption of six to 12 eggs/week, in the context of a diet that is consistent with guidelines for heart health promotion, has no adverse effect on major CVD risk factors in individuals at risk of developing diabetes or with established T2DM. This is in agreement with the systematic review of prospective cohort studies by Tran et al.(21) for the general population; however, these authors noted that significant associations have been observed between increased egg consumption and CVD and mortality in people with T2DM. Both authors commented that the evidence was heterogeneous in study design, populations, and definitions of outcomes. Most notably, observational studies did not adjust analyses for confounders that could have an impact on study outcomes.
Risk factors for CVD
With respect to risk factors, only HTN and blood lipids appear to be well covered in the reviews on egg consumption. Geiker et al.(22) included risk factors in their systematic review, and noted that only two of the twenty-three intervention studies they selected for inclusion reported an increase in LDL-C with increased egg consumption, leading to their conclusion that high-quality RCTs have not found significant effects of increasing egg consumption on risk factors for CVD in healthy subjects or subjects with T2DM. However, these authors did not conduct a quantitative analysis. The only meta-analysis that reported on intervention studies specifically with egg consumption on blood lipids was that of Rouhani et al.(32), who reported that egg consumption was significantly associated with increases in tChol, LDL-C and HDL-C, but not triglyceride (TG) and the ratios of tChol/HDL-C or LDL-C/HDL-C. Of the twenty-seven intervention studies included by Rouhani et al.(32) and the twenty-three reviewed by Geiker et al.(22) only twelve were in common between the two reviews (Table 7). Additionally, both reviews reported quality assessments of all included studies and these ratings were not consistent between the two reviews.
Table 7.
Selection of intervention studies that assessed blood lipids
| Reference | Geiker 2017(22) | Rouhani 2017(32) |
|---|---|---|
| Ballesteros. Nutrients. 2015. | X | |
| Baumgartner. Nutrition. 2013. | X | X |
| Blesso. Food Funct. 2013. | X | |
| Blesso. Metabolism. 2013. | X | X |
| Bunger et al. Int J Food Sci Nutr. 2014. | X | |
| Burns-Whitmore et al. Nutr J. 2014. | X | |
| Cesar J Nutr. 2006 | X | |
| Chakrabarty Indian J Phisyol Pharmacol. 2002 | X | |
| Chakrabarty Indian J Phisyol Pharmacol. 2004 | X | |
| Clark J Nutr. 2006 | X | |
| Fuller. AJCN. 2015. | X | X |
| Goodrow. J Nutr. 2006. | X | X |
| Greene. J Nutr. 2005. | X | X |
| Greene Nutr Metab (Lond). 2006 | X | |
| Harman. Eur J Nutr. 2008. | X | X |
| Herron J Am Coll Nutr. 2002 | X | |
| Herron J Nutr. 2003 | X | |
| Herron Metabolism. 2004 | X | |
| Herron Atherosclerosis. 2006 | X | |
| Iglay et al. J Nutr Health Aging. 2009. | X | |
| Katz. Am Heart J. 2015. | X | |
| Knopp. Arterioscler Thromb Vasc Biol. 2003. | X | |
| Knopp. J Am Coll Nutr. 1997. | X | |
| Mayurasakorn et al. J Med Assoc Thai. 2008. | X | |
| Mutungi. J Nutr. 2008. | X | X |
| Nissinen et al. Br J Nutr. 2008. | X | |
| Njike et al. BMJ Open Diabet Res Care. 2016.* | X | |
| Njike. Nutr J. 2010. | X | X |
| Pearce. Br J Nutr. 2011. | X | X |
| Rueda. Nutrients. 2013. | X | X |
| Schwab Atherosclerosis. 2000 | X | |
| Severins Nutr Metab Cardiovasc Dis. 2015 | X | |
| Tannock. Circulation. 2005. | X | |
| van der Made. J Nutr. 2014. | X | X |
| Vander Wal. Int J Obes (Lond). 2008. | X | X |
| Vishwanathan et al. Am J Clin Nutr. 2009. | X | |
| Vislocky et al. J Nutr Biochem. 2009. | X | |
| Waters J Nutr. 2007 | X | |
| Wenzel. J Nutr. 2006. | X |
Assessed glycated haemoglobin, anthropometrics, blood pressure, and diet quality, but not blood lipids.
The effect of eggs on the risk of HTN was assessed in two meta-analyses(30,31), and both reported that egg consumption was inversely associated with risk for HTN (Table 3). Both reviews were conducted on the effect of different food groups on HTN, with eggs as a sub-group analysis. The Schwingshackl et al.(30) review included one prospective study with red meat, poultry, and eggs in an Iranian population (n 1152, 144 cases), which, comparing the highest tertile (~23 g/d) to the lowest tertile consumption, resulted in RR: 0·54 (95 % CI, 0·32, 0·91), with each 50 g/d intake associated with RR: 0·25 (95 % CI, 0·08, 0·74). Schwingshackl et al.(30) also rated the level of confidence for the effect estimate as very low due to the very limited and uncertain meta-evidence available. The Zhang et al.(31) analysis included two additional studies (n 8942, 1987 cases) and reported the overall multi-adjusted RR: 0·79 (95 % CI, 0·68, 0·91, P = 0·001) for the highest compared with the lowest egg consumption group, with no significant heterogeneity or observed publication bias. Finally, Schlesinger et al.(33) compared abdominal obesity in the highest and lowest egg consumers from two observational studies, one of which was a cross-sectional study in Korean adults (n 1663), reporting a RR: 0·97 (95 % CI, 0·59, 1·59), with each 50 g/d intake associated with RR: 0·95 (95 % CI, 0·63, 1·43)(33). These authors indicated the confidence for the effect estimate was very low such that the meta-evidence is very limited and uncertain.
Discussion
Eggs are a nutrient dense food, but their high cholesterol content makes them a food of concern due to the association of dietary cholesterol intake and increased risk for cardiometabolic diseases. Past recommendations from US Dietary Guidelines for Americans, American Heart Association, and American College of Cardiology have indicated limited consumption of dietary cholesterol, including eggs. However, the 2015–2020 DGA modified this recommendation to state ‘cholesterol is not a nutrient of concern for overconsumption’ because ‘adequate evidence is not available for a quantitative limit for dietary cholesterol specific to the dietary guideline’. In this umbrella review, we provided a comprehensive overview of reported evidence from systematic reviews and meta-analyses regarding the impact of egg consumption on CVD and T2DM risks.
Existing reviews consisting of both prospective cohort studies and intervention studies on egg consumption and cardiometabolic outcomes suggest that (i) egg intake is not associated with increased CVD risk in healthy individuals; (ii) conclusions on the effect of egg consumption on CVD risk in subjects with T2DM are different between prospective cohort studies and intervention studies; (iii) the positive association between egg consumption and T2DM risk are specific to US-based studies; (iv) egg consumptions are associated with increased risk for heart failure; and (v) there is a negative association between egg intake and risk of HTN.
In general populations, there were no significant effects of egg intake on overall CVD risk(14,39), ischemic stroke(26,29,39), fatal stroke(26,29), total CHD(26,27,29), fatal CHD(26,29), and ischemic heart disease(15,39). Two meta-analyses reported no effect of egg intake on total stroke(27,29), whereas three meta-analyses reported that egg intake is significantly associated with lower risk of total stroke(15,26,39). For haemorrhagic stroke, three meta-analyses reported no effect of egg intake(15,26,39), while one(29) reported that egg intake is significantly associated with lower risk of haemorrhagic stroke. Finally, the two meta-analyses that assessed egg intake and HF reported increased HF risk with egg intake(27,28). Overall, meta-analyses of prospective cohort studies suggest that egg consumption is not associated with increased risk of CVD in the general population, with the exception of HF.
The four meta-analyses on atherosclerosis cardiovascular disease (ASCVD; e.g. stroke, CHD) concluded that egg intake is not associated with ASCVD incidence in the overall population (diabetic and non-diabetic population)(14,15,26,29). However, HF incidence was reported to be associated with egg intake in the overall population(28). The reason behind the disparate conclusions may be related to the pathogenesis of these different diseases/disorders. Unlike ASCVD which have their origins in atherosclerosis, HF is a clinical syndrome that can result from any structural or functional cardiac disorders that impair the ability of the ventricle to fill with or eject blood(44). While CAD, a type of ASCVD, is a major cause of HF, other major causes include HTN, diabetes, and dilated cardiomyopathy, whereby 30 % of cases have been reported to relate to genetics(44). While the link between atherosclerosis, circulating cholesterol, and dietary cholesterol is still being debated, the observations that egg consumption is associated with HF, but not ASCVD in general populations, suggest that eggs, a source of dietary cholesterol, do not contribute to atherosclerosis but may contribute to HF via a mechanism(s) that remains to be elucidated. Furthermore, a causal relationship must be established between them, with consideration of additional factors such as lifestyle, dietary habits, mental stress, and genetic dispositions. Thus, additional investigations into the role of eggs on different types of CVD, with a focus on atherosclerotic v. non-atherosclerotic diseases, are warranted. Furthermore, the opposite effect of egg consumption on risk for HF and HTN requires further investigations because HTN is a contributing cause of HF.
Meta-analyses on the association between egg consumption and risk of T2DM are inconclusive. Of the five meta-analyses that compared data from studies conducted within the US and those conducted outside the US, four reported a positive relationship between egg intake and T2DM risk only in US populations but not in European and Japanese populations(34-36,38). The other meta-analysis(14) only included a total of four studies whereby two of the non-US-based studies were cross-sectional(45) and case-control(46) studies that were not included in the other meta-analyses. It should be noted that of the four US-based studies included among the five meta-analyses, only one prospective study reported significant positive association between egg consumption and T2DM risk and this study included two randomized trials, the Physicians’ Health Study I and the Women’s Health Study(47). Subsequent studies conducted by the same group did not show a significant relationship between egg intake and T2DM risk(48,49) and the different results between the newer and older studies merit some considerations. The difference in relationship between egg and T2DM risk between US-based and non-US based studies suggest that the impact of egg consumption may be confounded by lifestyle or dietary habits associated with the risk of T2DM. For example, the authors of these meta-analyses hypothesized that high consumers of eggs in the US may also indulge in other habits that contribute to T2DM risk, such as smoking, low physical activity, and excess saturated fat and caloric intakes. Additionally, food preparation methods (e.g. boiled or fried eggs, whole eggs or only egg whites) or concurrent consumption of other foods associated with increased diabetes risk (e.g. home fries, bacon) that are popular in the US may also partly account for the differences. Unfortunately, the authors of meta-analyses cited the lack of data on the overall quality of the diet and food preparation details within individual studies as a reason for not being able to pursue this line of investigation.
The positive association between egg consumption and risk for CVD and CHD among those with T2DM(14,15,29) raises the question of whether separate recommendations on egg consumption should be provided for individuals with diabetes. Currently, recommendations on egg consumption not only vary across countries, but also rarely account for diabetes status. However, these findings were based on a limited number (n ≤8) of older studies (2011 and older)(14,15,29). Therefore, further research is needed to better define the role of eggs on CVD risk in the T2DM population.
A striking gap in knowledge in the area of egg consumption and CVD risk is the lack of meta-analyses on intervention studies. The authors of one narrative review(22) attributed their decision to not conduct a meta-analysis on the effects of egg intake on CVD risk factors in individuals with T2DM or at risk for developing T2DM due to the heterogeneity of the studies, with the intervention trials differing in population, primary outcome, background diet, and amount of eggs used. Interestingly, the one meta-analysis on intervention studies reported that higher egg consumption increases tChol and LDL-C, surrogate markers for CVD in the general population(32). This is in contrast to meta-analyses on prospective cohort studies, which reported no association between egg intake and ASCVD risk. Because it is not time and cost efficient for intervention studies to measure actual CVD incidence, intervention studies have resorted to measuring surrogate markers of ASCVD risk and not CVD risk itself.
It is possible that the contradicting observations of the meta-analysis on intervention studies and those on prospective cohort studies are due to limitations in extrapolating changes of surrogate markers to changes in CVD risk. For example, although LDL-C is a key target for CVD risk reduction, the residual risk (i.e. the ongoing appreciable risk of major CV events in statin-treated patients who have achieved evidence-based lipid goals(50)), suggests LDL-C should not be used as the sole basis for CVD risk prediction. Indeed, predictive equations such as the new Pooled Cohort ASCVD Risk equation, the Framingham CHD 10-year risk, and the Framingham Risk Score for CVD 10-year risk have paired LDL-C with other risk factors such as age, tChol, HDL-C, systolic BP, diabetes status, and current smoking status to increase the predictability of CVD risk. Although several intervention studies collect all the different elements of the aforementioned equations, none have calculated CVD risk and included that as a study outcome. Thus, future studies should consider combinations of various risk markers to take advantage of the better predictive potential than that of respective measures in isolation.
The reviews included may not represent all reviews on egg consumption and cardiometabolic health because reviews not published in English or not using a systematic search strategy were excluded, and those not published in PubMed, WOS, Cochrane Library, NESR, and AHRQ may have been missed. However, effort was made during this review to hand search all references in selected narrative reviews in addition to ad hoc searches on Google. In addition, because this is an umbrella review, the primary studies included in all the selected reviews were not assessed in detail.
Conclusions
Recent reviews addressing the specific effect of eggs on cardiometabolic health risks consistently report that higher egg consumption is not associated with CVD risk, but a positive association was found with risk of HF. A decreased risk of HTN with higher egg consumption has also been reported, which is inconsistent with the HF findings since HTN is a major risk factor for HF. However, these findings are based on limited data and further research is needed to better understand the role of eggs in HTN and HF. In addition, higher egg consumption is not associated with risk of T2DM in the general population, but is positively associated with T2DM in US-based studies only, which also requires additional research, specifically focused on differences in US-based and European populations. These varying results may reflect the complexity of cardiometabolic health, and differential individual responses to eggs, which can be affected by health status (e.g. presence or absence of diabetes) and response to dietary cholesterol, and other physiological and lifestyle factors.
Acknowledgements
Acknowledgements: The authors would like to thank Dr Chad Cook and Deena Wang for assistance with an initial scoping review that led to the development of this project. Financial support: Partial support for this work was provided by the Egg Nutrition Council to Biofortis, Mérieux NutriSciences. Conflict of interest: D.L. received support for conducting an initial review from the Egg Nutrition Council. The development of the manuscript was supported by Biofortis, Mérieux NutriSciences. The Egg Nutrition Council had no influence on the formulation of review aims, search and screening of reviews, data extraction, interpretation, and writing of the article. Authorship: Conceptualization (D.L.); search and screening (D.L., O.C.); data extraction (D.L., O.C., E.M.); writing (D.L., O.C., E.M.). All authors read and approved the final version. Ethics of human subject participation: Not applicable.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1368980019002441.
click here to view supplementary material
References
- 1. Micha R, Penalvo JL, Cudhea F et al. (2017) Association between dietary factors and mortality from heart disease, stroke, and type 2 diabetes in the United States. JAMA 317, 912–924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. World Health Organization. (2015) International Statistical Classification of Diseases and Related Health Problems. 10th revision. Geneva, Switzerland: WHO Press. [Google Scholar]
- 3. Ronto R, Wu JH & Singh GM (2018) The global nutrition transition: trends, disease burdens and policy interventions. Public Health Nutr 21, 2267–2270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Global Burden of Cardiovascular Diseases C, Roth GA, Johnson CO et al. (2018) The burden of cardiovascular diseases among US states, 1990–2016. JAMA Cardiol 3, 375–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Garber AJ, Abrahamson MJ, Barzilay JI et al. (2018) Consensus statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the comprehensive type 2 diabetes management algorithm - 2018 executive summary. Endocr Pract 24, 91–120. [DOI] [PubMed] [Google Scholar]
- 6. Cholesterol Treatment Trialists C, Baigent C, Blackwell L et al. (2010) Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet 376, 1670–1681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sacks FM, Lichtenstein AH, Wu JHY et al. (2017) Dietary fats and cardiovascular disease: a presidential advisory from the American Heart Association. Circulation 136, e1–e23. [DOI] [PubMed] [Google Scholar]
- 8. Soliman GA. (2018) Dietary cholesterol and the lack of evidence in cardiovascular disease. Nutrients 10, 780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kuang H, Yang F, Zhang Y et al. (2018) The impact of egg nutrient composition and its consumption on cholesterol homeostasis. Cholesterol 2018, 6303810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. U.S. Department of Health and Human Services and U.S. Department of Agriculture (2015) Dietary Guidelines for Americans. Washington, DC: U.S. Government Printing Office. [Google Scholar]
- 11. Weggemans RM, Zock PL & Katan MB (2001) Dietary cholesterol from eggs increases the ratio of total cholesterol to high-density lipoprotein cholesterol in humans: a meta-analysis. Am J Clin Nutr 73, 885–891. [DOI] [PubMed] [Google Scholar]
- 12. Clayton ZS, Fusco E & Kern M (2017) Egg consumption and heart health: a review. Nutrition 37, 79–85. [DOI] [PubMed] [Google Scholar]
- 13. Fuller NR, Sainsbury A, Caterson ID et al. (2015) Egg consumption and human cardio-metabolic health in people with and without diabetes. Nutrients 7, 7399–7420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Li Y, Zhou C, Zhou X et al. (2013) Egg consumption and risk of cardiovascular diseases and diabetes: a meta-analysis. Atherosclerosis 229, 524–530. [DOI] [PubMed] [Google Scholar]
- 15. Shin JY, Xun P, Nakamura Y et al. (2013) Egg consumption in relation to risk of cardiovascular disease and diabetes: a systematic review and meta-analysis. Am J Clin Nutr 98, 146–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. David Spence J (2016) Dietary cholesterol and egg yolk should be avoided by patients at risk of vascular disease. J Transl Int Med 4, 20–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Shea BJ, Bouter LM, Peterson J et al. (2007) External validation of a measurement tool to assess systematic reviews (AMSTAR). PLoS One 2, e1350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Shea BJ, Hamel C, Wells GA et al. (2009) AMSTAR is a reliable and valid measurement tool to assess the methodological quality of systematic reviews. J Clin Epidemiol 62, 1013–1020. [DOI] [PubMed] [Google Scholar]
- 19. Mente A, de Koning L, Shannon HS et al. (2009) A systematic review of the evidence supporting a causal link between dietary factors and coronary heart disease. Arch Intern Med 169, 659–669. [DOI] [PubMed] [Google Scholar]
- 20. Richard C, Cristall L, Fleming E et al. (2017) Impact of egg consumption on cardiovascular risk factors in individuals with type 2 diabetes and at risk for developing diabetes: a systematic review of randomized nutritional intervention studies. Can J Diabetes 41, 453–463. [DOI] [PubMed] [Google Scholar]
- 21. Tran NL, Barraj LM, Heilman JM et al. (2014) Egg consumption and cardiovascular disease among diabetic individuals: a systematic review of the literature. Diabetes Metab Syndr Obes 7, 121–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Geiker NRW, Larsen ML, Dyerberg J et al. (2018) Egg consumption, cardiovascular diseases and type 2 diabetes. Eur J Clin Nutr 72, 44–56. [DOI] [PubMed] [Google Scholar]
- 23. Park SJ, Jung JH, Choi SW et al. (2018) Association between egg consumption and metabolic disease. Korean J Food Sci Anim Resour 38, 209–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kerley CP (2018) Dietary patterns and components to prevent and treat heart failure: a comprehensive review of human studies. Nutr Res Rev 32, 1–27. [DOI] [PubMed] [Google Scholar]
- 25. Kerley CP. (2018) A review of plant-based diets to prevent and treat heart failure. Card Fail Rev 4, 54–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Alexander DD, Miller PE, Vargas AJ et al. (2016) Meta-analysis of egg consumption and risk of coronary heart disease and stroke. J Am Coll Nutr 35, 704–716. [DOI] [PubMed] [Google Scholar]
- 27. Bechthold A, Boeing H, Schwedhelm C et al. (2017) Food groups and risk of coronary heart disease, stroke and heart failure: a systematic review and dose-response meta-analysis of prospective studies. Crit Rev Food Sci Nutr 59, 1–20. [DOI] [PubMed] [Google Scholar]
- 28. Khawaja O, Singh H, Luni F et al. (2017) Egg consumption and incidence of heart failure: a meta-analysis of prospective cohort studies. Front Nutr 4, 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Rong Y, Chen L, Zhu T et al. (2013) Egg consumption and risk of coronary heart disease and stroke: dose-response meta-analysis of prospective cohort studies. BMJ 346, e8539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Schwingshackl L, Schwedhelm C, Hoffmann G et al. (2017) Food groups and risk of hypertension: a systematic review and dose-response meta-analysis of prospective studies. Adv Nutr 8, 793–803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Zhang Y & Zhang DZ (2018) Red meat, poultry, and egg consumption with the risk of hypertension: a meta-analysis of prospective cohort studies. J Hum Hypertens 32, 507–517. [DOI] [PubMed] [Google Scholar]
- 32. Rouhani MH, Rashidi-Pourfard N, Salehi-Abargouei A et al. (2018) Effects of egg consumption on blood lipids: a systematic review and meta-analysis of randomized clinical trials. J Am Coll Nutr 37, 99–110. [DOI] [PubMed] [Google Scholar]
- 33. Schlesinger S, Neuenschwander M, Schwedhelm C et al. (2019) Food groups and risk of overweight, obesity, and weight gain: a systematic review and dose-response meta-analysis of prospective studies. Adv Nutr 10, 205–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Djousse L, Khawaja OA & Gaziano JM (2016) Egg consumption and risk of type 2 diabetes: a meta-analysis of prospective studies. Am J Clin Nutr 103, 474–480. [DOI] [PubMed] [Google Scholar]
- 35. Schwingshackl L, Hoffmann G, Lampousi AM et al. (2017) Food groups and risk of type 2 diabetes mellitus: a systematic review and meta-analysis of prospective studies. Eur J Epidemiol 32, 363–375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Tamez M, Virtanen JK & Lajous M (2016) Egg consumption and risk of incident type 2 diabetes: a dose-response meta-analysis of prospective cohort studies. Br J Nutr 115, 2212–2218. [DOI] [PubMed] [Google Scholar]
- 37. Tian S, Xu Q, Jiang R et al. (2017) Dietary protein consumption and the risk of type 2 diabetes: a systematic review and meta-analysis of cohort studies. Nutrients 9, E982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Wallin A, Forouhi NG, Wolk A et al. (2016) Egg consumption and risk of type 2 diabetes: a prospective study and dose-response meta-analysis. Diabetologia 59, 1204–1213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Xu L, Lam TH, Jiang CQ et al. (2018) Egg consumption and the risk of cardiovascular disease and all-cause mortality: Guangzhou Biobank Cohort Study and meta-analyses. Eur J Nutr 58, 1–12. [DOI] [PubMed] [Google Scholar]
- 40. Berger S, Raman G, Vishwanathan R et al. (2015) Dietary cholesterol and cardiovascular disease: a systematic review and meta-analysis. Am J Clin Nutr 102, 276–294. [DOI] [PubMed] [Google Scholar]
- 41. Larsson SC, Akesson A & Wolk A (2015) Egg consumption and risk of heart failure, myocardial infarction, and stroke: results from 2 prospective cohorts. Am J Clin Nutr 102, 1007–1013. [DOI] [PubMed] [Google Scholar]
- 42. Nettleton JA, Steffen LM, Loehr LR et al. (2008) Incident heart failure is associated with lower whole-grain intake and greater high-fat dairy and egg intake in the Atherosclerosis Risk in Communities (ARIC) study. J Am Diet Assoc 108, 1881–1887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Djousse L & Gaziano JM (2008) Egg consumption and risk of heart failure in the Physicians’ Health Study. Circulation 117, 512–516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Hunt SA, Abraham WT, Chin MH et al. (2009) 2009 focused update incorporated into the ACC/AHA 2005 Guidelines for the Diagnosis and Management of Heart Failure in Adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the International Society for Heart and Lung Transplantation. Circulation 119, e391–e479. [DOI] [PubMed] [Google Scholar]
- 45. Shi Z, Yuan B, Zhang C et al. (2011) Egg consumption and the risk of diabetes in adults, Jiangsu, China. Nutrition 27, 194–198. [DOI] [PubMed] [Google Scholar]
- 46. Radzeviciene L & Ostrauskas R (2012) Egg consumption and the risk of type 2 diabetes mellitus: a case-control study. Public Health Nutr 15, 1437–1441. [DOI] [PubMed] [Google Scholar]
- 47. Djousse L, Gaziano JM, Buring JE et al. (2009) Egg consumption and risk of type 2 diabetes in men and women. Diabetes Care 32, 295–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Djousse L, Kamineni A, Nelson TL et al. (2010) Egg consumption and risk of type 2 diabetes in older adults. Am J Clin Nutr 92, 422–427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Djousse L, Petrone AB, Hickson DA et al. (2016) Egg consumption and risk of type 2 diabetes among African Americans: the Jackson Heart Study. Clin Nutr 35, 679–684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Kones R (2013) Molecular sources of residual cardiovascular risk, clinical signals, and innovative solutions: relationship with subclinical disease, undertreatment, and poor adherence: implications of new evidence upon optimizing cardiovascular patient outcomes. Vasc Health Risk Manag 9, 617–670. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1368980019002441.
click here to view supplementary material